Dbt borderline personality treatment
Treating Borderline Personality Disorder | NAMI: National Alliance on Mental Illness
JUN. 07, 2017
By Luna Greenstein
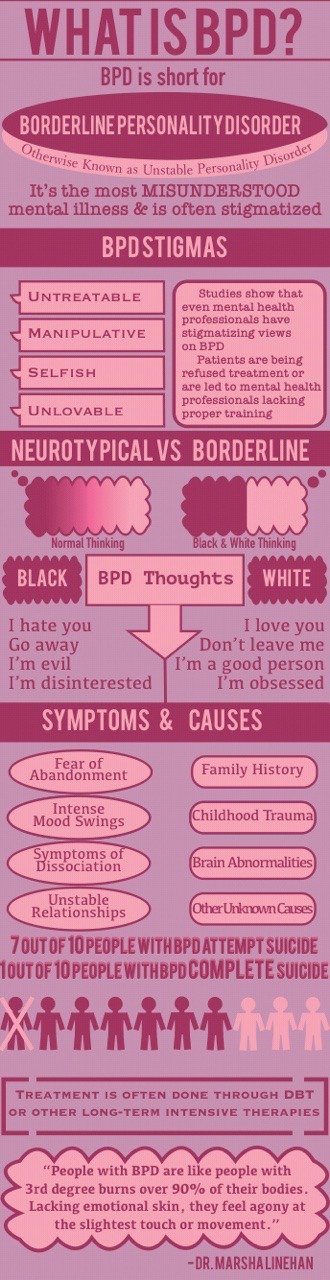
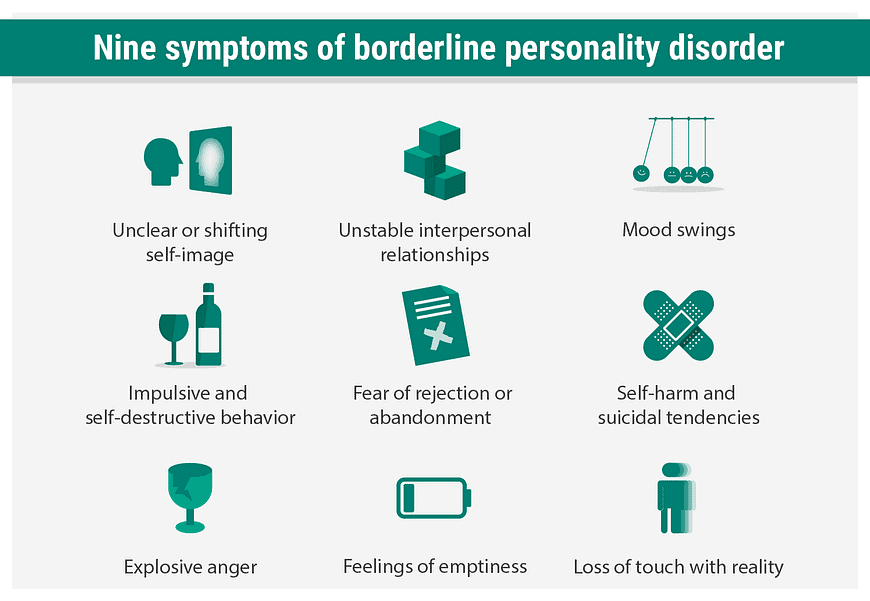
Imagine having difficulty controlling your thoughts and actions. Imagine that your sense-of-self is almost entirely dependent on your relationships with others. Imagine struggling to manage stress, rejection or conflict. This is what it’s like to live with Borderline Personality Disorder (BPD): a mental health condition characterized by a pattern of ongoing instability in moods, behavior, self-image and functioning.
BPD is a highly-misunderstood condition—even within the mental health field. So, to better understand this complex condition, I talked with a NAMI HelpLine volunteer who bravely told me his story.
Randy* was diagnosed with BPD at 17 after a suicide attempt landed him in the hospital. “The concept of being able to like yourself and want to live just went over my head,” he explained. “I also couldn’t handle being rejected. If I sent a text message and they didn’t get back to me for five minutes, I’d already be thinking about killing myself.”
After several years of talk therapy and one month of cognitive behavioral therapy, Randy's therapist suggested dialectical behavior therapy last January. Dialectical behavior therapy (DBT) is a cognitive behavioral treatment developed to help people manage symptoms that are considered “difficult to treat,” such as: impulsivity, interpersonal problems, emotional dysregulation, self-harm and suicidal behaviors. DBT works for a range of conditions (substance abuse, depression, PTSD, among others), but it was originally developed to treat chronically suicidal individuals with BPD.
Skill-Building Through DBT
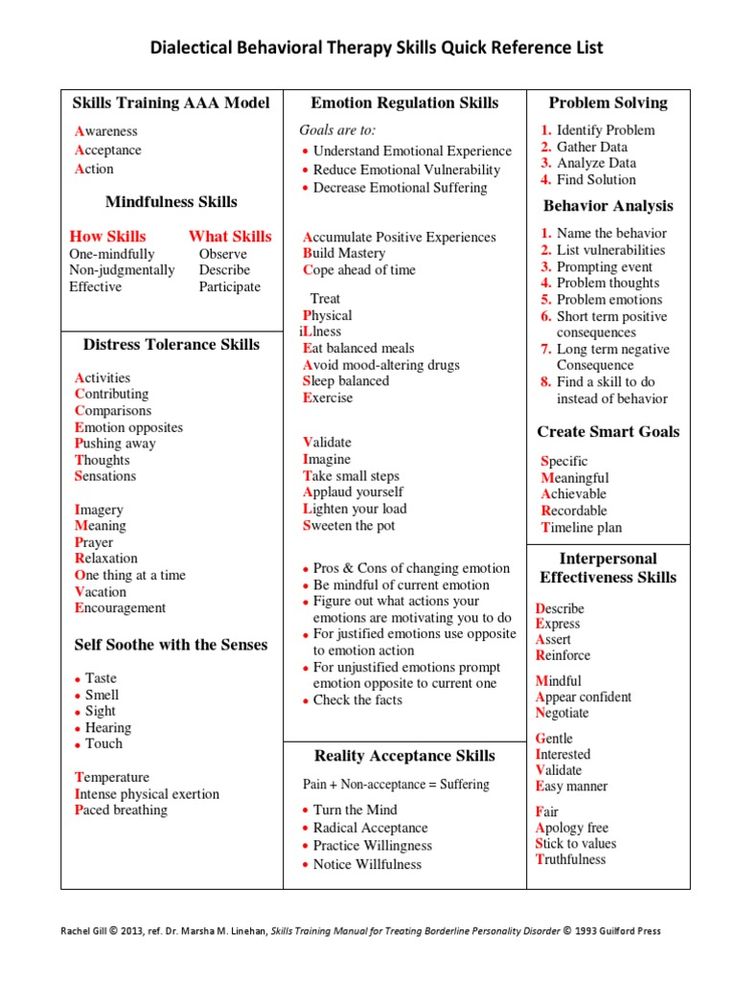
DBT is a combination of group therapy and individual treatment designed to help therapists offer the best treatment possible. What makes DBT unique and effective is its focus on teaching participants a set of behavioral skills that help them cope with their difficult symptoms. “The skills are what people talk about when they talk about DBT; they are the active ingredient in DBT,” explains the creator of DBT, Dr. Marsha Linehan. These skills include:
“The skills are what people talk about when they talk about DBT; they are the active ingredient in DBT,” explains the creator of DBT, Dr. Marsha Linehan. These skills include:
- Mindfulness: Being fully aware and present
- Distress Tolerance: Tolerating difficult or uncomfortable situations
- Interpersonal Effectiveness: Asking for what you want and saying no when you need to (while still maintaining self-respect and healthy relationships)
- Emotion Regulation: Changing emotions that you want to change
Each skill is a separate module of DBT and it takes a full year to go through all four modules in group therapy. Some may choose to repeat a module to help make those specific skills stick—like Randy, who repeated all the modules twice and the distress tolerance module three times because that’s the skill he struggles with the most. It takes a lot of time and energy to learn these coping mechanisms and implement them when symptoms flare.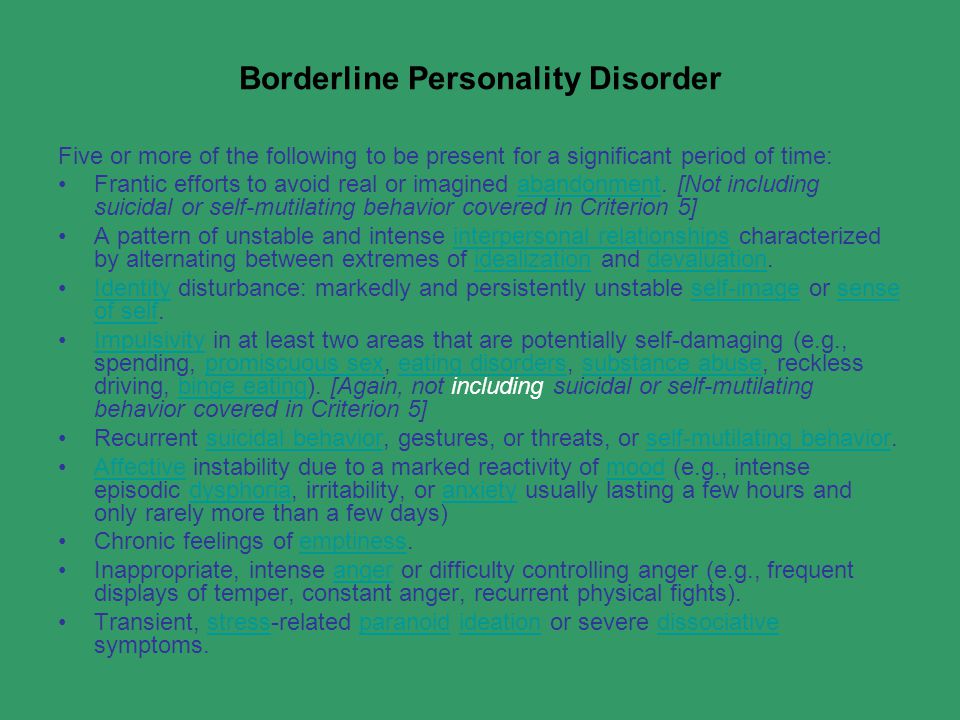
Everything in DBT is connected and works together to help people manage their symptoms. Skills are introduced in group therapy lessons and are learned through practice and homework. “We have a handbook,” Randy says. “It ranges from things like how to talk to someone you don’t agree with without getting emotional to ‘I’m freaking out, what do I do?’” This is followed with individual therapy that includes lessons tailored to each person so they can apply what they’ve learned to everyday life.
The Gold Standard
While it takes time and effort, the components of DBT work together effectively. Even though DBT has only been around for a couple decades, it has already improved and saved the lives of many. Research shows it’s incredibly effective—one study from 2014 showed that 77% of participants no longer met criteria for BPD diagnosis after undergoing treatment.
DBT is recognized as the “gold standard” for people with BPD. “It’s weird how much better I’ve gotten from it.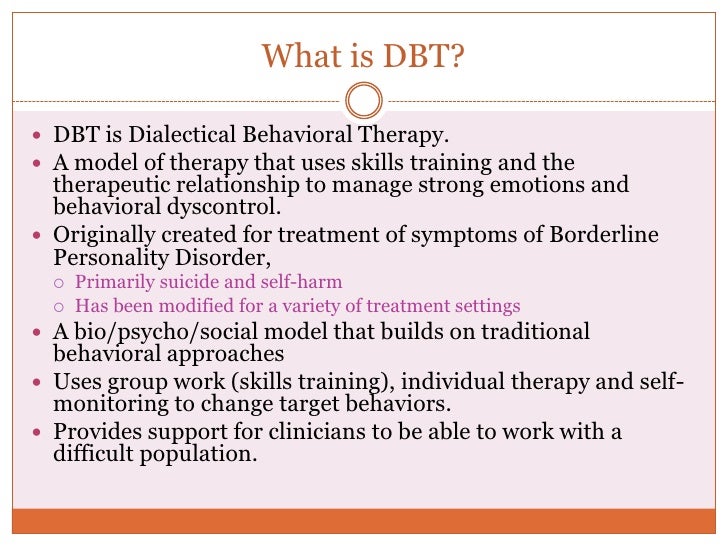 Looking back, I was so different; I didn’t know how to handle life. Sometimes I still don’t, but I’m getting there. I’m getting better.”
Looking back, I was so different; I didn’t know how to handle life. Sometimes I still don’t, but I’m getting there. I’m getting better.”
*Name has been changed to protect our volunteer's privacy
Laura Greenstein is communications coordinator at NAMI.
If you or someone you know is interested in entering a DBT program, you can search for a certified clinician here.
In addition, you can contact the NAMI HelpLine at 800-950-6264 or [email protected], and we will help direct you on how to find the closest DBT program.
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
LEARN MORE
Dialectical Behavior Therapy for Borderline Personality Disorder
Dialectical behavioral therapy (DBT) may improve symptoms of borderline personality disorder (BPD) by teaching skills that include mindfulness and emotion regulation.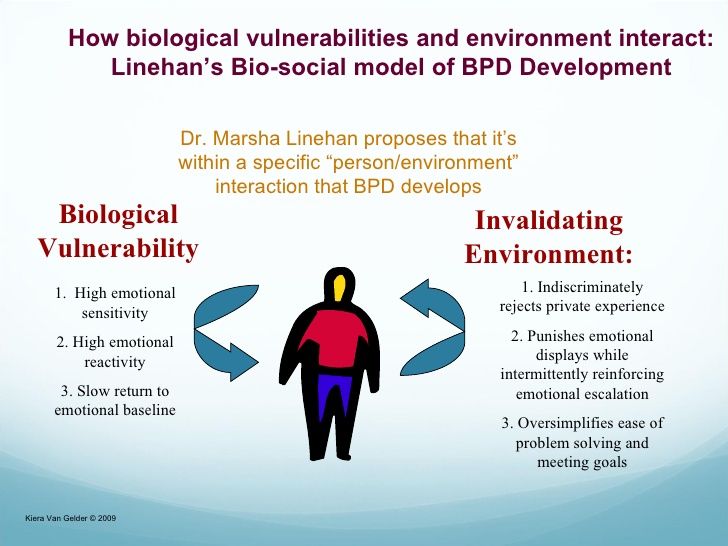
Marked by difficulties with emotional regulation, interpersonal relationships, self-image, thoughts of suicide, and other symptoms, living with borderline personality disorder (BPD) isn’t always easy. However, it’s possible to live a happy, fulfilling life with the right kind of treatment and support.
Research shows that the prognosis for BPD is good, especially for those who seek treatment through specialized therapy. The most popular and most effective form of therapy for BPD is dialectical behavioral therapy (DBT). This form of therapy was created for people with borderline personality disorder in mind.
If you’ve been diagnosed with BPD, know that you’re not alone. In fact, it’s estimated that about 1.6% of U.S. adults are affected by this condition.
DBT is a multifaceted treatment approach created by Dr. Marsha Linehan in the early 1990s. Linehan created DBT in hopes of providing relief to those living with BPD, a condition she’s experienced, as she later revealed in her book “Building a Life Worth Living: A Memoir.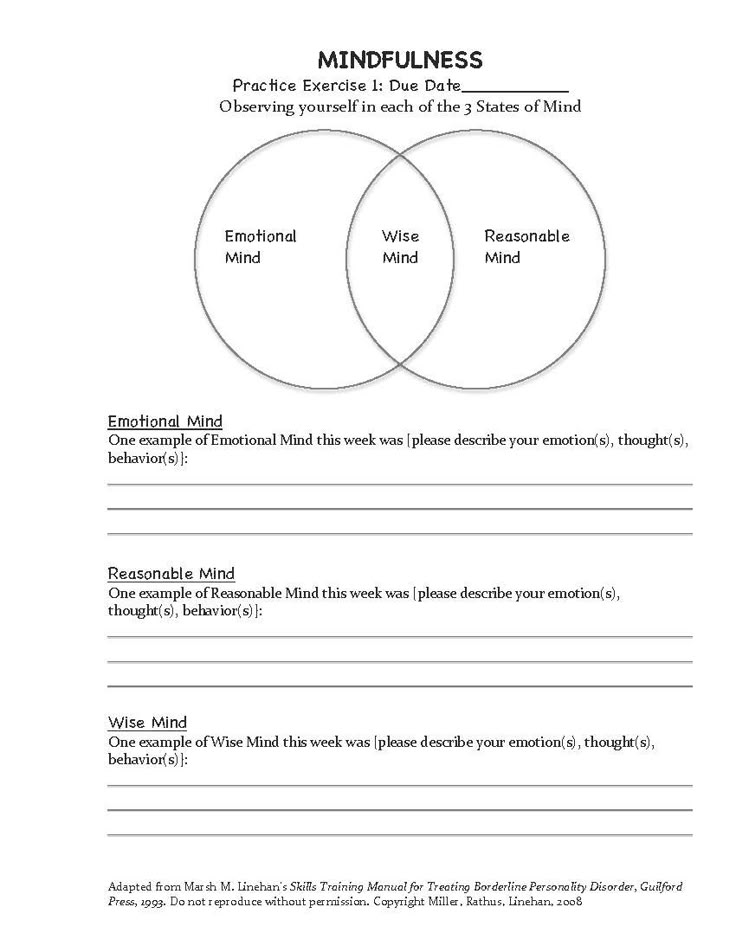 “
“
DBT, while created for BPD, has also been helpful for those with:
- substance use
- eating disorders
- attention deficit hyperactivity disorder (ADHD)
DBT is a skills-based treatment program broken into four main modules:
- Mindfulness. Mindfulness teaches you to focus on the here and now by becoming aware of your thoughts, feelings, and sensations.
- Interpersonal effectiveness. In this module, you learn, for example, how to communicate effectively, build and cultivate healthy relationships, and express your needs.
- Emotion regulation. DBT teaches you techniques to help you understand and manage your emotions.
- Distress tolerance. In this module, you learn techniques to manage overwhelming emotions or difficult situations.
Each module consists of various skills that are specific to that module’s theme. Some skills you may learn include:
- self-soothing
- wise mind
- radical acceptance
- building positive experiences
Each module consists of group and individual therapy, as well as homework assignments.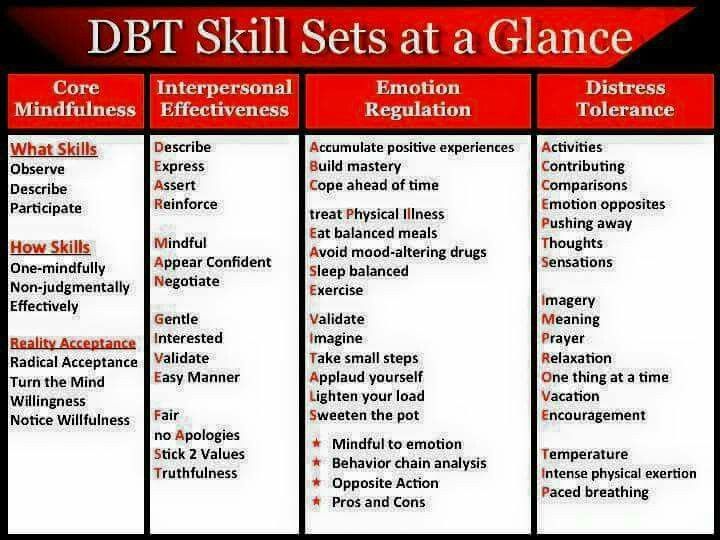 Your therapist may also be available for phone coaching in moments where skills may need to be practically applied.
Your therapist may also be available for phone coaching in moments where skills may need to be practically applied.
DBT is skills-based, meaning it’s both practical and achievable. Typically, a DBT program lasts 1 year.
Since those with BPD often experience black-and-white thinking, one of the foundations of DBT is literally within its name: dialectics.
Dialectics is defined as holding two seemingly opposite ideas at one time, considering both to be truths. In DBT, “dialectical” refers to the idea of needing both acceptance and change to help improve symptoms. This can bring greater balance and reduce black-and-white patterns of thought.
The other foundation of DBT is mindfulness. Through mindfulness, those living with BPD can learn to make more intentional, conscious decisions and decrease impulsivity and other unhelpful or potentially harmful behaviors over time.
One mindset taught during mindfulness is “wise mind,” which encourages dialectical thinking in crisis and normalcy.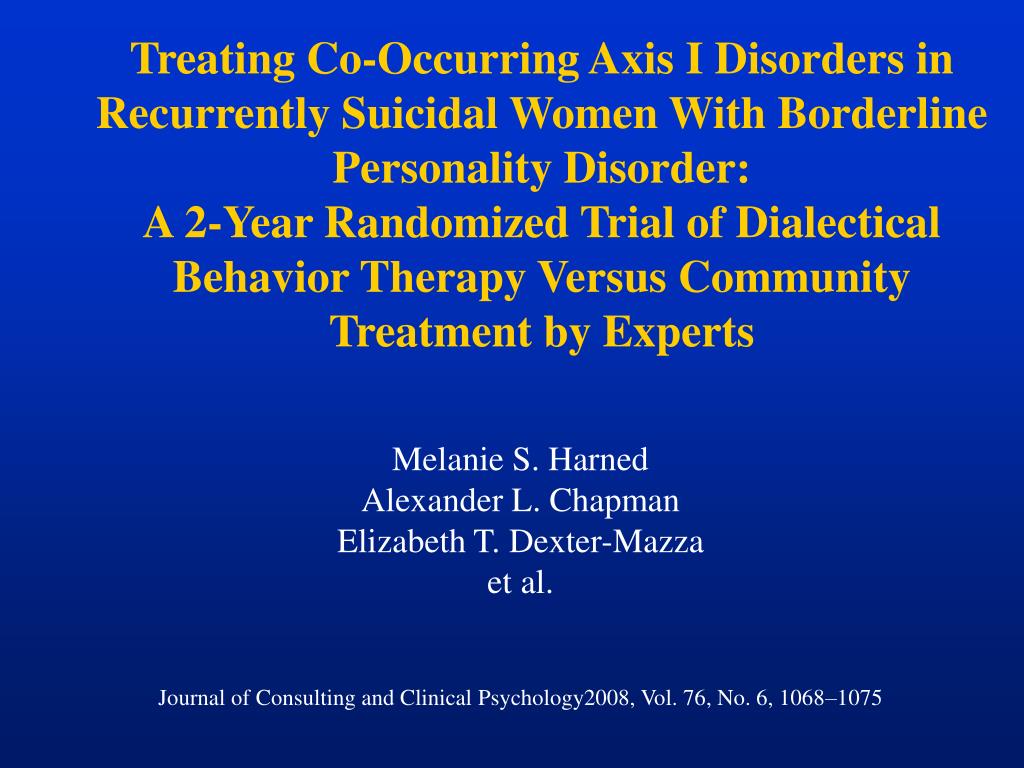 It also helps you to attend to your emotions and reason to make wise and balanced decisions.
It also helps you to attend to your emotions and reason to make wise and balanced decisions.
Ultimately, DBT helps those with BPD both function and flourish in their everyday lives.
What does research say about DBT?
Research has shown DBT to be the most effective form of treatment for those with BPD. In fact, one study found that after the first year of treatment, 77% of participants no longer met the diagnostic criteria of BPD.
DBT is particularly effective for improving:
- suicidal thoughts and behaviors
- difficulties with anger management
- overall daily functioning, including socially
BPD symptoms such as chronic feelings of emptiness, difficulties with personal relationships, and an intense fear of abandonment tend to be more difficult to treat with DBT — but not impossible.
It’s important to remember that BPD doesn’t look the same for everyone. Different people may have different symptoms, and though DBT may help many people with the condition, it may not work for everyone.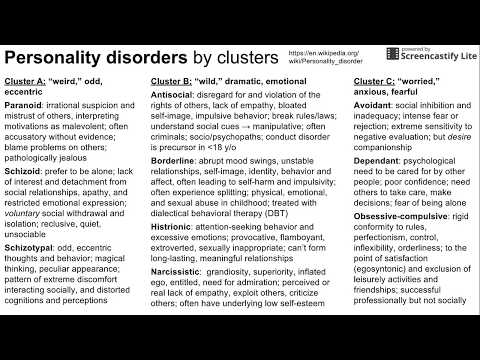
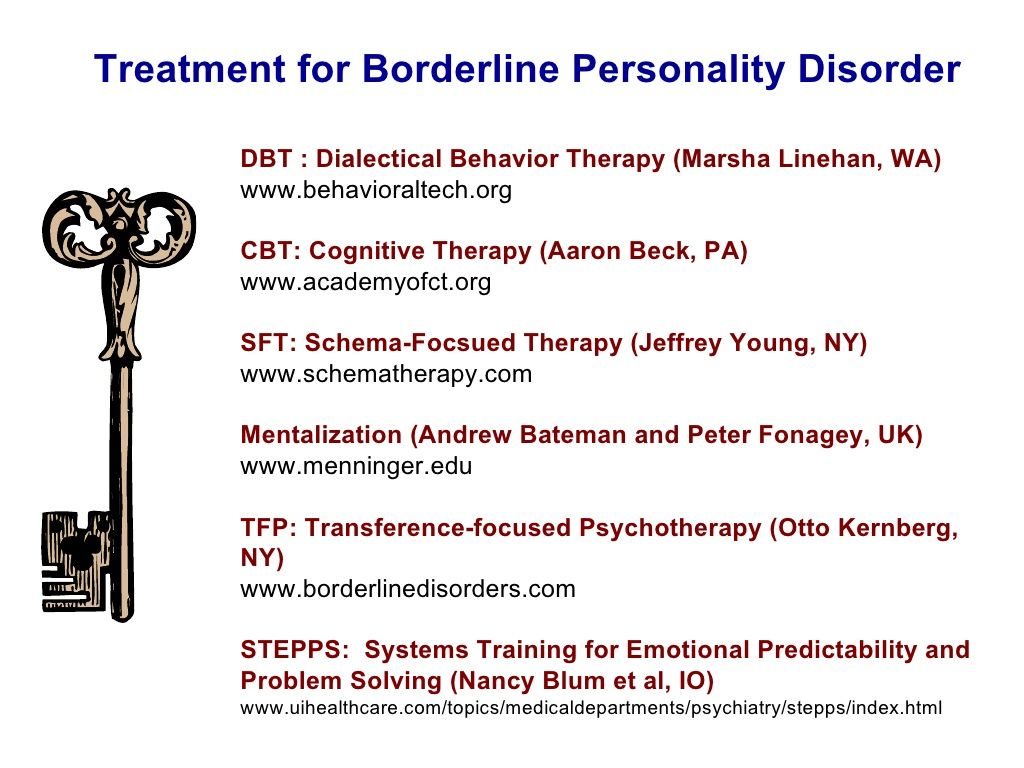
If you feel as if DBT isn’t helping you, there are many other options you can discuss with your treatment team, including:
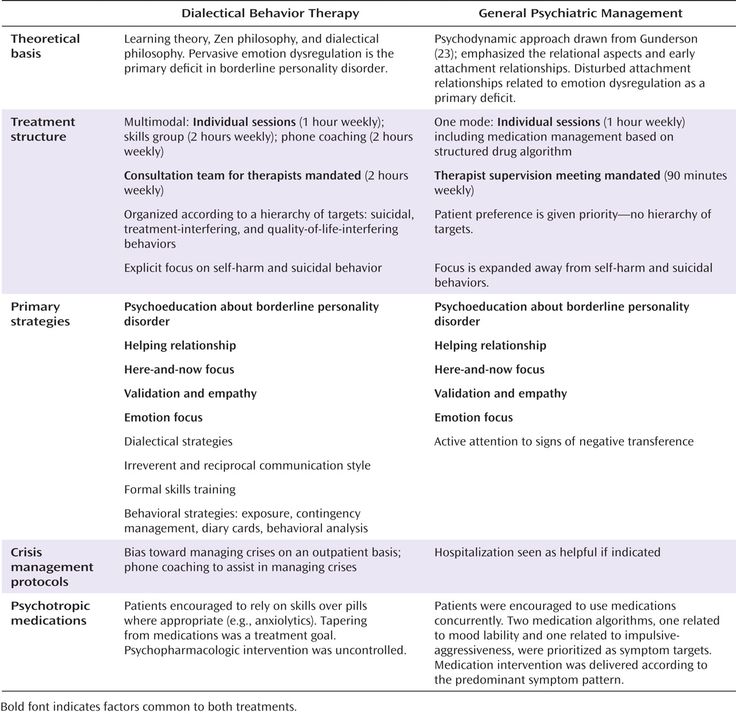
- Mentalization-based therapy (MBT). MBT helps people with BPD identify and understand their own and others’ actions, feelings, and thoughts.
- Transference-focused therapy (TFP). In TFP, your therapist allows you to “transfer” thoughts or feelings you may have about another person onto them, which may allow them to understand your symptoms better. In collaboration, you can work out ways to change behaviors or negative thinking that your BPD may cause.
- Good psychiatric management (GPM). GPM teaches you problem-solving and stress-management strategies to help with life difficulties and to better understand yourself.
- Schema-focused therapy (SFT). SFT helps people with BPD change negative patterns of thoughts, behavior, and emotions, which are known as “schemas.”
At times, short-term hospitalizations may be necessary.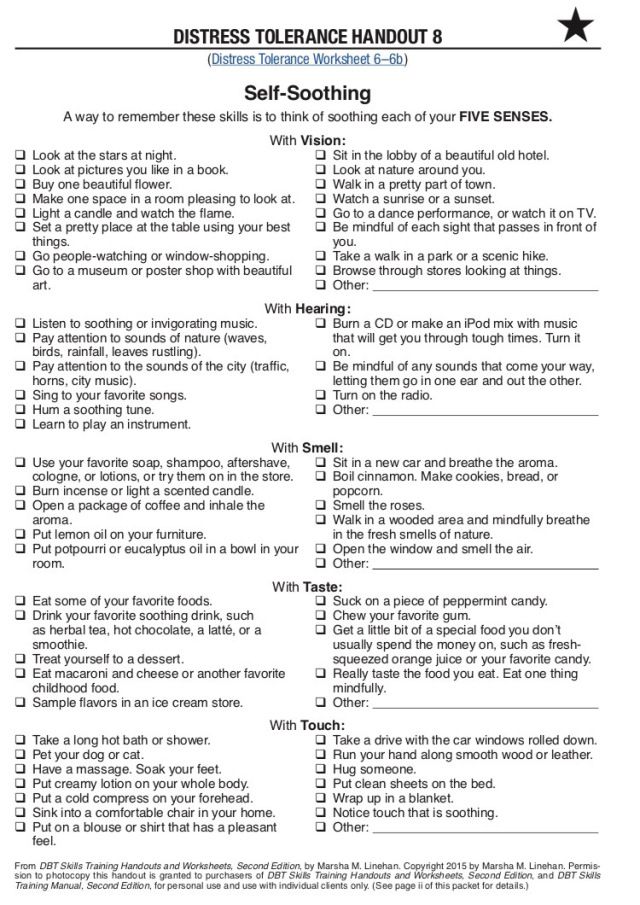 This is particularly true in times of extreme stress and when you experience suicidal or impulsive behaviors.
This is particularly true in times of extreme stress and when you experience suicidal or impulsive behaviors.
Currently, there is no medication specifically for BPD. Some people with co-occurring conditions such as anxiety or depression may benefit from taking antidepressants. Your doctor can help you figure out whether medication may be beneficial in your case.
Are you in a crisis or considering suicide?
If you’re having thoughts of suicide or self-harm, you can access free support right away with these resources:
- The National Suicide Prevention Lifeline. Call the Lifeline at 800-273-8255, 24 hours a day, 7 days a week.
- The Crisis Text Line. Text HOME to the Crisis Text Line at 741741.
- The Trevor Project. LGBTQIA+ and under 25 years old? Call 866-488-7386, text START to 678678, or chat online 24-7.
- Veterans Crisis Line. Call 800-273-8255, text 838255, or chat online 24-7.
- Befrienders Worldwide. This international crisis helpline network can help you find a local helpline.
Overall, dialectical behavior therapy (DBT) has been shown to be the most effective form of treatment for people with borderline personality disorder (BPD), especially if you experience thoughts of suicide or self-harm or want to reduce anger. It also helps with social skills and overall quality of life.
If you think DBT may be right for you, finding a qualified and experienced therapist in your area is crucial.
The National Education Alliance for Borderline Personality Disorder offers helpful tips when searching for a suitable therapist.
Plus, the Borderline Personality Disorder Resource Center maintains a database of healthcare professionals in the United States who have experience treating BPD. You can call them at 1-888-694-2273 or send them an email at [email protected].
Though living with BPD can be challenging at times, try to keep in mind that you’re not alone and that you can get better with the right treatment and support.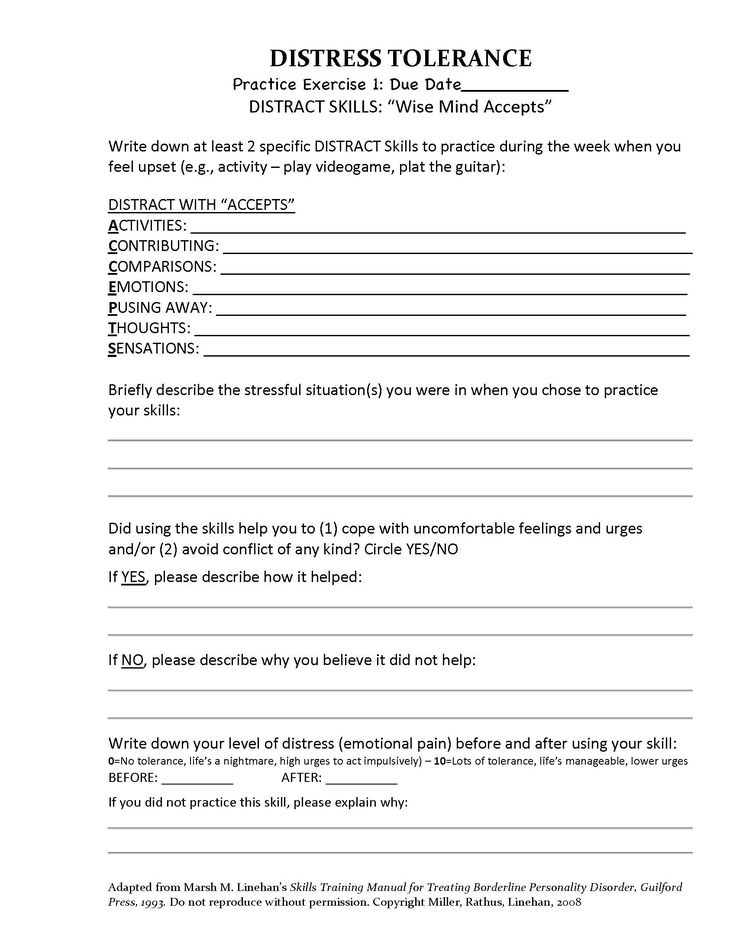
For family members and friends
If someone you care about has been diagnosed with BPD, and you’re interested in learning more about the condition and how to be a supportive ally, the National Education Alliance for Borderline Personality Disorder offers the Family Connections Program, a free 12-class course in which you learn about:
- BPD and its treatment
- DBT-based relationship skills
- how to take care of yourself
- how to communicate effectively
Keep in mind that the current wait time is 5–6 months, and you have to be 18 years or older to participate.
DBT - Mental Health Center
The lives of people with borderline personality disorder are often filled with harrowing emotional swings, relationship problems, self-harmful behavior, and chronic suicidality.
Dialectical behavior therapy (DBT) is a compassionate and proven model of care.
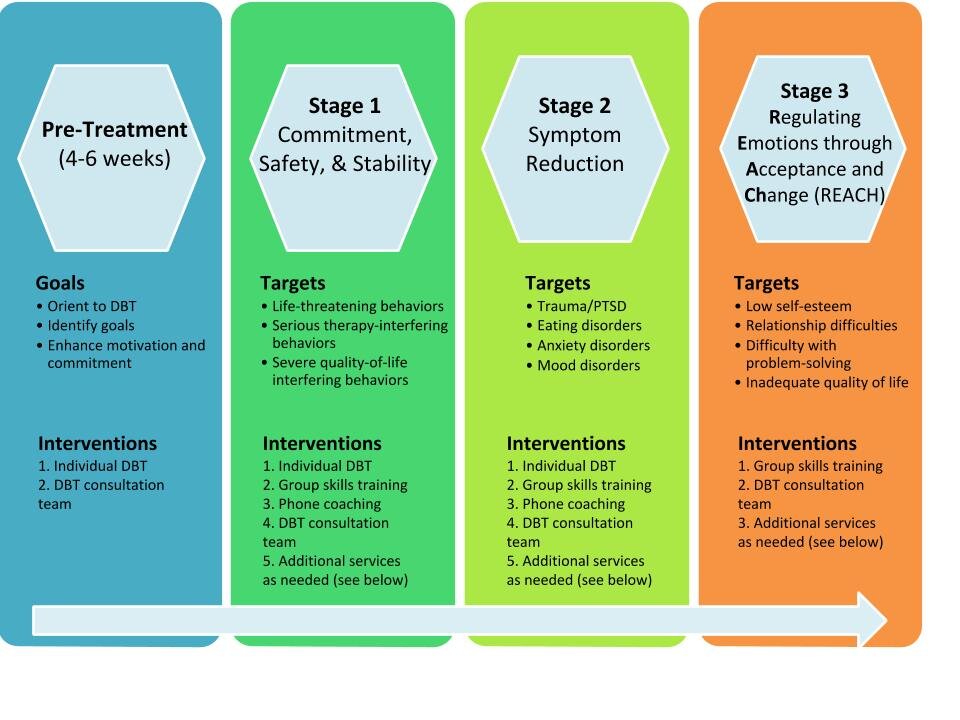
DBT is a comprehensive cognitive behavioral therapy system designed to treat complex, difficult to treat personality and behavioral disorders.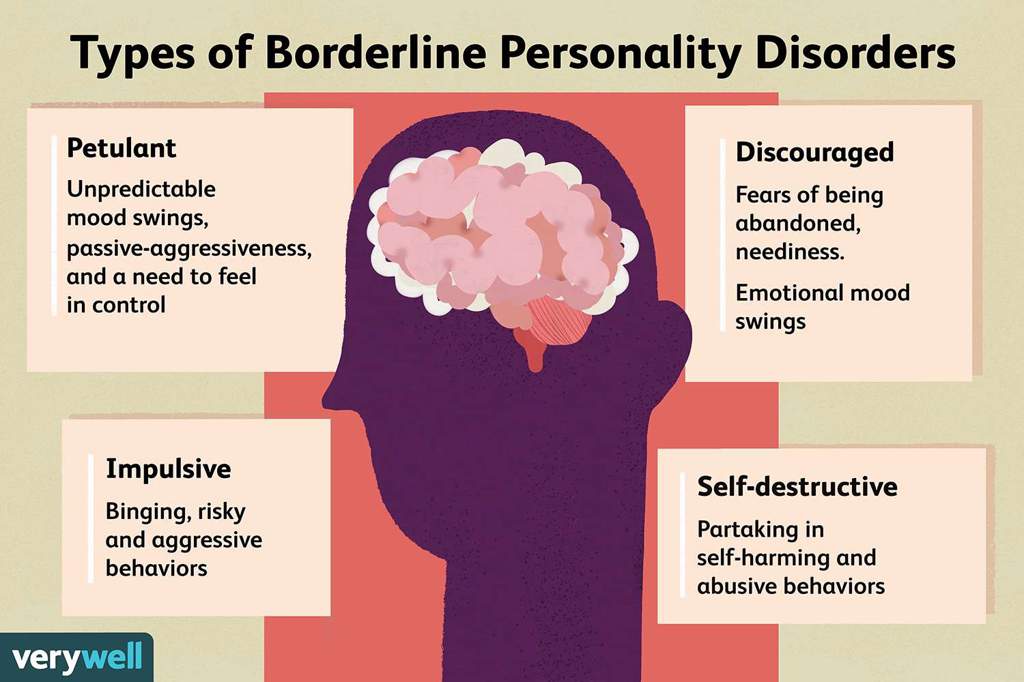 Initially developed for patients with chronic suicidal behavior, DBT has gradually evolved into a treatment for patients with multiple behavioral problems and borderline personality disorder (BPD). Since then, DBT adaptations have been developed for difficult-to-treat behavioral disorders associated with emotional dysregulation, including substance dependence, anorexia and bulimia, depression and suicidal behavior in adolescents, depression in the elderly, and bipolar affective disorder. There are versions of the DBT applicable to a variety of care formats, including outpatient and inpatient care, group therapy, and individual therapy. nine0003
Initially developed for patients with chronic suicidal behavior, DBT has gradually evolved into a treatment for patients with multiple behavioral problems and borderline personality disorder (BPD). Since then, DBT adaptations have been developed for difficult-to-treat behavioral disorders associated with emotional dysregulation, including substance dependence, anorexia and bulimia, depression and suicidal behavior in adolescents, depression in the elderly, and bipolar affective disorder. There are versions of the DBT applicable to a variety of care formats, including outpatient and inpatient care, group therapy, and individual therapy. nine0003
Dialectical Behavior Therapy is the global benchmark for helping people with borderline personality disorder, suicidal behavior and self-harm.
DBT is based on a combined deficit-motivation model of BPD, suggesting that (1) people with BPD lack important skills in interpersonal communication, self-regulation (including emotion management), and distress coping, and that (2) individual and environmental factors often block or suppress the acquisition and use of behavioral skills by patients and reinforce dysfunctional behavior.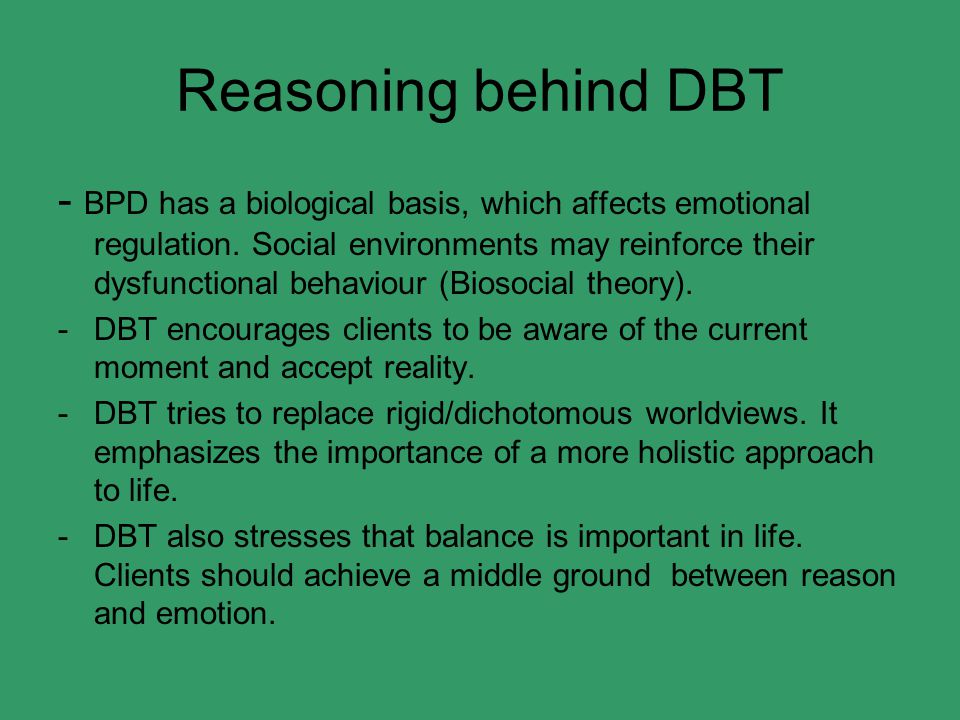 nine0003
nine0003
DBT combines basic behavior therapy strategies with mindfulness practices.
DBT starts from a balanced dialectical therapeutic position emphasizing the synthesis of opposites. The dialectical approach assumes the inevitability of the emergence in the therapy of suicidal patients with BPD of many opposites that are difficult to combine (the need for acceptance and change, passivity and activity, the patient's vulnerability and the need to actively contact the environment, etc.). DBT encourages the formation of flexible dialectical patterns of thinking and behavior instead of the rigid "black and white" type of thinking. nine0003
The fundamental dialectical balance in DBT is the balance between accepting the patient for who they are and helping them achieve change.
Acceptance procedures in DBT include mindfulness techniques (ie, attention to the present, taking a nonjudgmental stance, focusing on performance) as well as a range of validation and acceptance strategies. Change strategies in DBT include behavioral analysis of maladaptive behavior and solution techniques, including interpersonal skills training, emotional self-regulation, learning management (reinforcement and punishment in therapy), cognitive modification, and exposure-based strategies. nine0003
Change strategies in DBT include behavioral analysis of maladaptive behavior and solution techniques, including interpersonal skills training, emotional self-regulation, learning management (reinforcement and punishment in therapy), cognitive modification, and exposure-based strategies. nine0003
As part of a comprehensive treatment, DBT aims to achieve five main goals:
(1) expansion of the behavioral repertoire,
(2) increased motivation for change (through modification of suppression and reinforcement factors),
(3) generalization of new patterns of behavior beyond therapeutic space,
(4) structuring the therapeutic environment necessary for the implementation of the resources of the therapist and the patient,
(5) increasing the ability and motivation of the therapist to effectively help the patient. nine0003
In the standard DBT, these functions are distributed among various formats of care, including individual psychotherapy, group skills training, telephone coaching, and the DBT advisory group.
Website of the Dialectical Behavioral Therapy community in Russia — www.dbtrussia.org
Efficacy of DBT
DBT is the only therapy for borderline personality disorder (BPD) that has been sufficiently studied for meta-analytical calculations (confirming its effectiveness) [Cohen, 1992; Kliem et al, 2010]. A meta-analysis by Binks et al (2006) showed that DBT in BPD leads to a reduction in self-injurious and suicidal behavior and thinking.
The first randomized clinical trial of DBT compared the effectiveness of this type of therapy with standard psychiatric treatment [Linehan et al., 1991; Linehan et al., 1993; Linehan et al., 1994]. Patients on DBT were significantly less likely to engage in parasuicidal behavior during the year from study entry, report fewer parasuicidal episodes at each follow-up assessment, and have less medically serious parasuicidal acts and incomplete suicide attempts. DBT was more effective than standard treatment in preventing premature discontinuation of therapy, the most severe treatment-impeding behavior.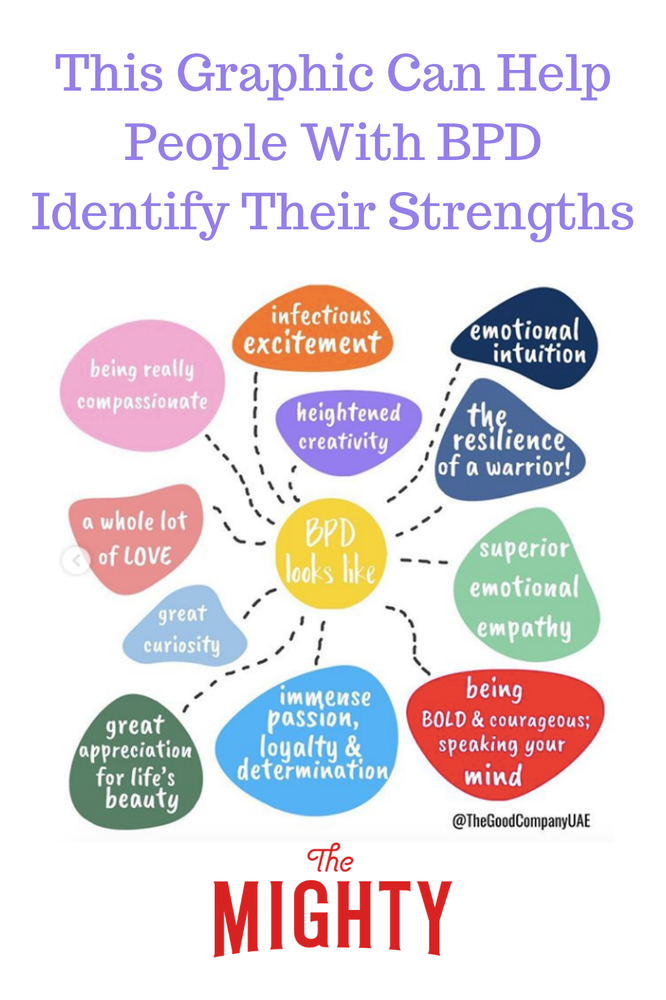 Patients treated with DBT were less likely to be hospitalized, spent fewer days in the hospital, and also showed greater improvement in global and social adjustment scales. Patients treated with DBT showed a significantly greater reduction in anger than patients in the control group. The superiority of DBT was maintained for one year after completion of therapy (i.e., for all two years of the study). Subsequently, 2 controlled randomized trials were performed that evaluated the effectiveness of DBT compared with standard treatment, as well as one case-control study comparing DBT with other types of psychotherapy. The results for most parameters confirmed the superiority of DBT noted in the first study. Koons et al. found that women with BPD who received the DBT program had greater reductions in self-injurious behavior, suicide attempts, and levels of depression compared to patients who received standard treatment. Finally, DBT (but not standard treatment) has been shown to lead to significant reductions in suicidal thoughts, feelings of hopelessness, anger, hostility, and dissociation [Koons et al.
Patients treated with DBT were less likely to be hospitalized, spent fewer days in the hospital, and also showed greater improvement in global and social adjustment scales. Patients treated with DBT showed a significantly greater reduction in anger than patients in the control group. The superiority of DBT was maintained for one year after completion of therapy (i.e., for all two years of the study). Subsequently, 2 controlled randomized trials were performed that evaluated the effectiveness of DBT compared with standard treatment, as well as one case-control study comparing DBT with other types of psychotherapy. The results for most parameters confirmed the superiority of DBT noted in the first study. Koons et al. found that women with BPD who received the DBT program had greater reductions in self-injurious behavior, suicide attempts, and levels of depression compared to patients who received standard treatment. Finally, DBT (but not standard treatment) has been shown to lead to significant reductions in suicidal thoughts, feelings of hopelessness, anger, hostility, and dissociation [Koons et al. , 2001]. In a sample of patients with addictive behaviors and BPD, DBT showed a greater improvement in substance abuse (based on structured interviews and urinalysis) both during treatment and at follow-up. DBT is accompanied by a large improvement in overall functioning and social adjustment during follow-up [Linehan et al., 1999].
, 2001]. In a sample of patients with addictive behaviors and BPD, DBT showed a greater improvement in substance abuse (based on structured interviews and urinalysis) both during treatment and at follow-up. DBT is accompanied by a large improvement in overall functioning and social adjustment during follow-up [Linehan et al., 1999].
DBT is recognized by various authoritative medical organizations in developed countries (American Psychiatric Association guidelines for the diagnosis and treatment of borderline personality disorder [Oldham J.M. et al., 2001; 2005]; suicidal behavior [Jacobs D.M. et al., 2003]; British National Institute guidelines for Health and Care Excellence [NICE, 2009]; Australian Government National Health and Medical Research Council [Commonwealth of Australia, 2013] Australian Guidelines for BPD Treatment [Commonwealth of Australia, 2013]) as the most evidence-based treatment modality of any modality for the treatment of BPD, self-injurious and suicidal behavior.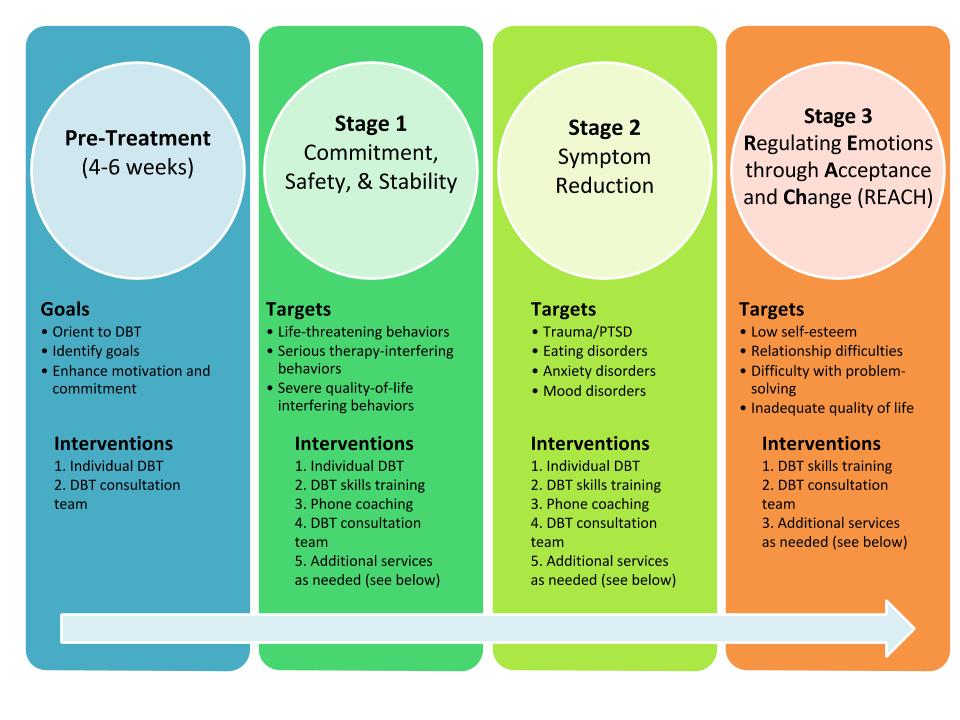 nine0003
nine0003
Long-term effect of DBT: reduction in hospital days
DBT targets (where possible) outpatient care and results in a significant reduction in the number and duration of hospitalizations, as confirmed by 12 comparative studies. Since DBT has a long-term effect, the amount of savings from using DBT increases every year after the intervention.
Thus, in the context of the current global and all-Russian trend towards a reduction in inpatient bed capacity, the use of DBT allows addressing the need for patients in medical care and reducing the need for repeated and prolonged hospitalizations. nine0003
Effective BPD treatment not only reduces health care costs, but also reduces the overall financial burden on society, including law enforcement, emergency services, social services, and the lost productivity of people with BPD, who often work below their capacity.
Reduction in the number of days in the hospital (data from randomized controlled trials DBT):
- Linehan et al (1991): patients treated with DBT for 12 months spent an average of 30.
 4 fewer days in the hospital than with conventional treatment; the decrease in hospital days persisted and became even more significant at follow-up a year later (Linehan et al, 1993).
4 fewer days in the hospital than with conventional treatment; the decrease in hospital days persisted and became even more significant at follow-up a year later (Linehan et al, 1993). - Linehan et al (1999): In treating patients with BPD and substance dependence, DBT was superior to standard treatment in clinical outcomes. There were no statistically significant differences in the number of days of hospitalization during 12 months of therapy and 4 months of follow-up between DBT and standard care. nine0062
- Linehan et al (2002): DBT was superior to another treatment modality (12 steps + structured validation) in a sample of patients with BPD and opiate dependence, including fewer hospitalizations and days spent in the hospital during 12 months of therapy. The average number of nights spent in police stations was 7.7 for DBT patients and 18.8 for the comparison group.
- Batcheler (2005) in a 3-year prospective study reported a reduction in average days of hospital stay from 25.
 04 (12 months pre-DBT) to 4 (12 months DBT) and 1.09(12 months from completion of DBT).
04 (12 months pre-DBT) to 4 (12 months DBT) and 1.09(12 months from completion of DBT). - Bassington & Krawitz (2006) reported on a DBT study in a psychiatric hospital. The authors noted a decrease in the number of days of stay in the hospital from 3.42 during the 6 months before the start of the DBT course to 1.2 during the 6 months of therapy.
- Linehan et al (2006): DBT was superior to expert-led eclectic therapy in most measures. During the year of therapy, a significantly lower number of patients in the DBT program, compared with conventional therapy, were hospitalized in a psychiatric hospital (DBT -19.6%, conventional psychotherapy - 48.9%), including those hospitalized due to suicidal thoughts (9.8% and 35.6%, respectively).
- Prendergast & McCausland (Australia, 2007) reported a reduction in the average number of days of hospital stay during the 6 months before and during DBT from 6.09 to 1.73.
- McMain et al (2009): DBT and general mental health care showed similar efficacy across most parameters.
 However, in the DBT group, there was a decrease in the number of days spent in the hospital during the last 4 months of 12 months of therapy compared with 4 months before treatment (10.52 days to 3.73 days). nine0062
However, in the DBT group, there was a decrease in the number of days spent in the hospital during the last 4 months of 12 months of therapy compared with 4 months before treatment (10.52 days to 3.73 days). nine0062 - Carter et al (2010) showed a 33% reduction in psychiatric hospital admissions in the DBT group compared with standard care. The number of days in the hospital is not given, the duration of hospitalizations did not differ significantly.
- Carter et al. (2010) in a 6-month randomized controlled trial showed that outpatient DBT resulted in a non-significant but larger reduction in hospital admissions compared to standard therapy (0.61 psychiatric hospital admissions per patient per 6 months of therapy compared with 0.91 for conventional therapy; for a non-psychiatric (somatic) hospital, the corresponding values were 0.5 and 1.4).
- Williams et al. (2010) reported that participation in the 20-week DBT skills training group resulted in a significant reduction in the number of days spent in hospital during treatment (from 2.
 79 to 0.57), with the patients with the most active inpatient care having the most decrease in indicators (from 16.18 to 1.36 days). The achieved improvement was maintained for 6 months after the end of the course (decrease from 17.56 to 3.33 days, p=0.06). nine0062
79 to 0.57), with the patients with the most active inpatient care having the most decrease in indicators (from 16.18 to 1.36 days). The achieved improvement was maintained for 6 months after the end of the course (decrease from 17.56 to 3.33 days, p=0.06). nine0062 - Pasieczny & Connor (2011) showed that patients treated with a 6-month course of DBT in the Australian public health system had a significant reduction in the number of days spent in hospital compared to waiting list and standard care (2.23 versus 13.6 days) with a comparable initial number of hospital days in both groups.
Economic efficiency of DPT
- American Psychiatric Association (1998) reported a reduction in treatment costs of $26,000 per patient per year with DBT compared to the previous year ($20-46,000), a 77% reduction in hospital days, a 76% reduction in day care days, days in the intensive care unit by 56%.
- Linehan and Heard (1991, 1999) reported that DBT resulted in an average reduction of $9,000 per patient per year.
- A Swedish study [Perseius, 2004] showed a reduction in therapy costs of $17,000 per patient per year of DBT compared to the previous year. Comparison of treatment costs per month before DBT and 18 months from DBT initiation shows a cost reduction of $6,000/patient ($8,000 and $2,000, respectively). nine0062
- Prendergast and McCausland (2007) found in an Australian public health study that the reduction in hospital admissions with DBT resulted in a reduction in pre/post 6-month DBT treatment costs of A$4,501 per 6 months per patient.
- Paisieczny and Connor (2011) in an Australian sample showed a reduction in treatment costs of A$5,927 per patient over a 6-month follow-up period when comparing DBT and standard care (Total cost of case management was A$12.196 and A$18,123 respectively).
- Amner (2012), in a Welsh public mental health service study: a prospective study in Wales showed a reduction in total health care costs of GB£1,741 during the year following the completion of a DBT course, compared with 12 months prior to treatment, in primarily due to a 20% reduction in the cost of hospital treatment.