Cptsd emotional flashback
The Living Hell of Emotional Flashbacks
In our last article, we discussed the differences between post-traumatic stress disorder (PTSD) and complex post-traumatic stress disorder (CPTSD). One of these dissimilarities involves the living hell of emotional flashbacks.
In this piece, we shall examine the definition of emotional flashbacks and ways to manage them.
Should you become overwhelmed during this piece, please stop reading and do some grounding exercises. Afterward, put it aside and take this piece with you to your therapist’s office to read it together. As always, safety is primary.
What are Emotional Flashbacks?According to Pete Walker, emotional flashbacks are a complex mixture of intense and confusing reliving of past trauma from childhood. It is like living a nightmare while you are awake, with overwhelming sorrow, toxic shame, and a sense of inadequacy.
Filled with confusing and distressing emotions from the past, an emotional flashback is extremely painful.
In my experience, an emotional flashback causes me to feel nuclear war is about to begin, or I am in extreme danger. It just feels like something horrible is about to happen.
I become hypervigilant beyond my normal and want to isolate away from family and friends. Unfortunately, doing so only magnifies the feelings of abandonment and I get stuck in a loop of feeling in endangered and trying to reason my way out of my feelings of hopeless despair.
To make matters worse, I hear my inner critic repeating messages given to me in childhood calling me a loser, a nobody, a failure, and not a good person. These old tapes leave me without energy and sometimes feeling self-destructive.
Emotional Flashbacks and the BrainChronic exposure to abuse in childhood often leads to the development of complex post-traumatic stress disorder leaving the victims, now adults, reliving the abuse over again later in life in the form of emotional flashbacks.
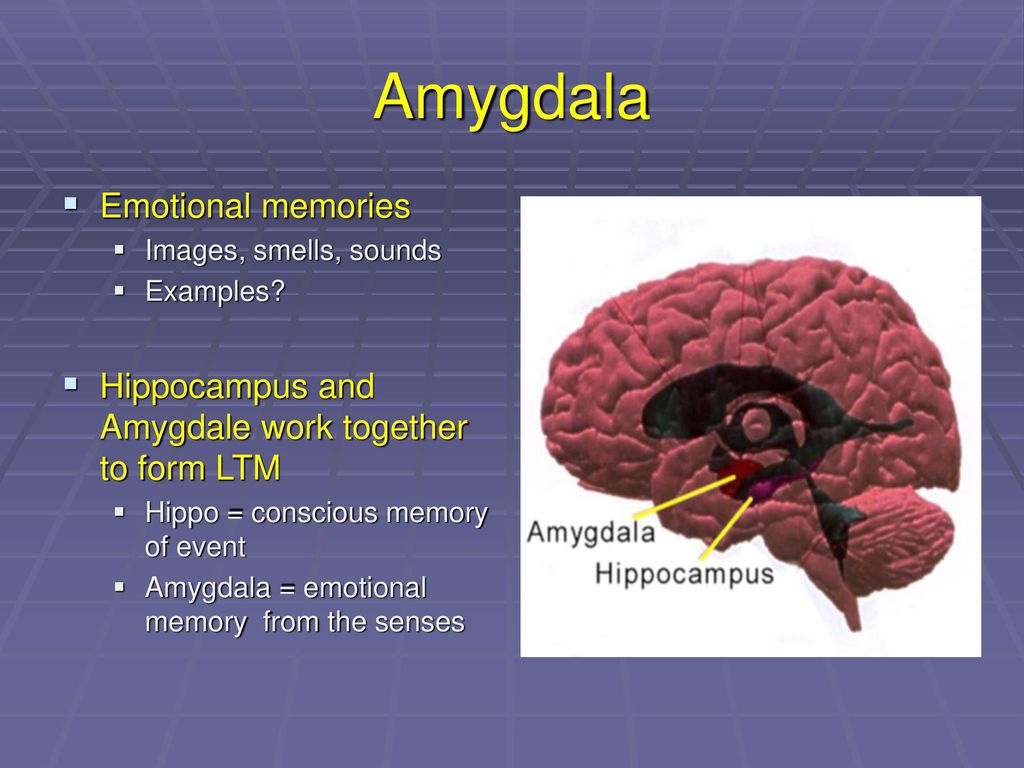
The original traumatic events harmed the brain’s ability to calm down from a potential or perceived danger recognized by an overactive amygdala.
To better understand this reaction, one must first comprehend two parts of the automatic nervous system (ANS), the sympathetic and parasympathetic nervous systems.
I found a wonderful description of these vital brain regions in an article written by Doctor Arielle Schwartz from 2016 titled The Neurobiology of Trauma1, it states:
“The autonomic nervous system (ANS) plays a significant role in our emotional and physiological responses to stress and trauma.
The ANS to have two primary systems: the sympathetic nervous system and the parasympathetic nervous system.
The sympathetic nervous system is associated with the fight or flight response and the release of cortisol throughout the bloodstream.
The parasympathetic nervous system puts the brakes on the sympathetic nervous system, so the body stops releasing stress chemicals and shifts toward relaxation, digestion, and regeneration.
The sympathetic and parasympathetic nervous systems are meant to work in a rhythmic alternation that supports healthy digestion, sleep, and immune system functioning. ”
”
Dr. Schwartz goes on to describe how the “rhythmic balance” between the sympathetic and parasympathetic nervous systems becomes disrupted by chronic child abuse, and that this lack of synching of the two leads to problems later.
During an emotional flashback, because your ANS is damaged and out of synch, the amygdala recognizes what it perceives as danger (trigger) and reacts triggering the fight/flight/freeze response. This reaction engages the sympathetic nervous system revving up your body and causing a significant amount of distress. However, unlike under normal circumstances, the parasympathetic nervous system does not engage to calm down the situation leaving a person stranded in yesterday.
The Actions of the Parasympathetic Nervous System to Perceived DangerOnce triggered in an adult, a damaged automatic nervous system causes a lot of distressing symptoms including immobilization, dissociation related to emotional flashbacks.
If you have ever observed a rabbit when they are frightened, their first response is to freeze to allow the danger to pass by them. This is akin to humans experiencing the freeze response made possible, like in the rabbit, courtesy of the amygdala.
Dissociation was a way for humans to stay immobilized, like the rabbit, so that we can either avoid or become invisible to predators. This survival mechanism separates our conscious awareness from our emotions and was very helpful in the days when protohumans inhabited the treetops.
Exposed to repetitive and horrific traumatic events, children use dissociation to keep going forward in their lives afterward by allowing them to disconnect their emotions from their conscious awareness.
However, this trick becomes a severe liability once the child becomes an adult, leaving us feeling anywhere from a mild sensation of fogginess to the extreme reaction of memory loss and lost time.
The emotions that we, as children, put aside through dissociation during an episode of abuse, are what roars back later in life as emotional flashbacks.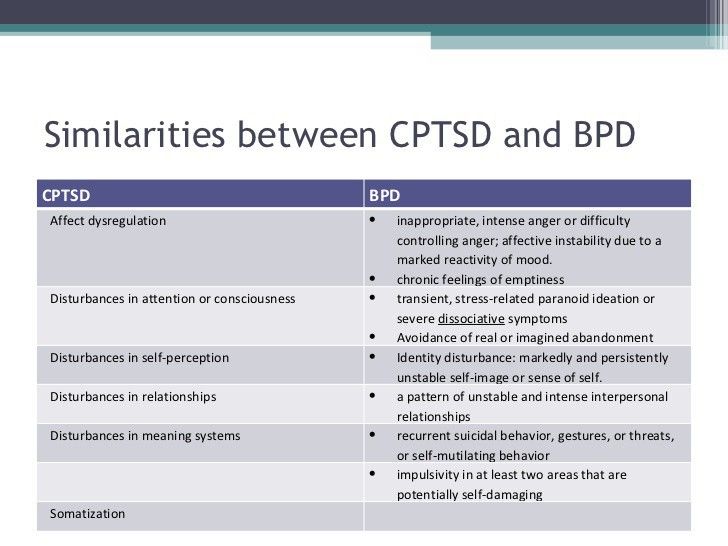
Backing up the piece by Dr. Schwartz is a research paper written by Bourne, Mackay & Holmes in 2013 called The Neural Basis of Flashback Formation: the Impact of Viewing Trauma.2
The authors of the paper wrote in their conclusion:
“Results provide the first prospective evidence that the brain behaves differently whilst experiencing emotional events that will subsequently become involuntary memories – flashbacks. Understanding the neural basis of analog flashback memory formation may aid the development of treatment interventions for this PTSD feature.”
Managing FlashbacksArielle Schwartz and Pete Walker, a licensed Marriage and Family Therapist, is the author of several books including The Complex PTSD Workbook and Complex PTSD from Surviving to Thriving. He is also a person who has lived experience with CPTSD and emotional flashbacks.
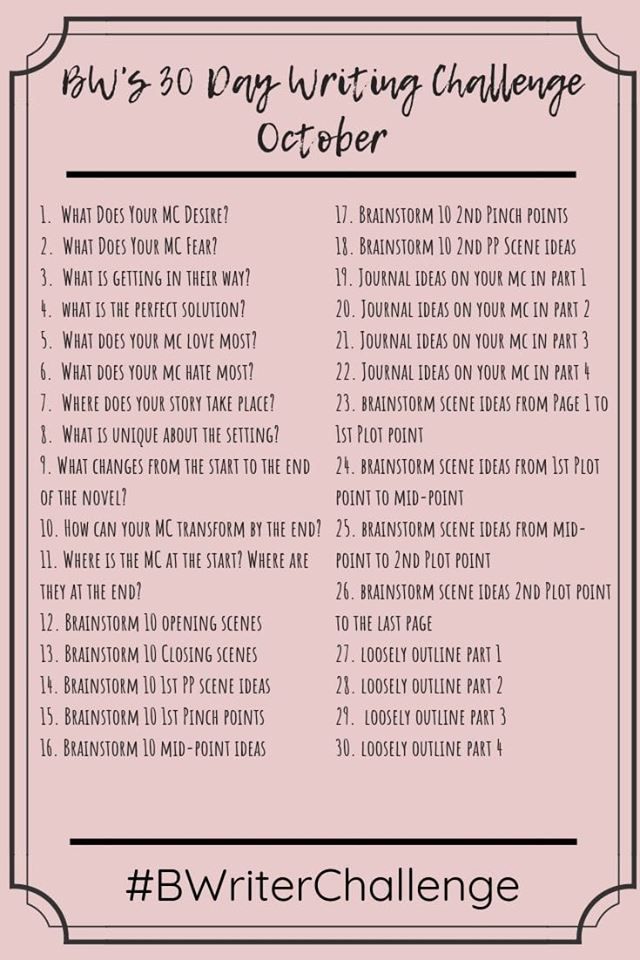
Included in the work, Complex PTSD from Surviving to Thriving are thirteen steps to manage flashbacks.
I normally do not copy and paste things that others have written, but I do not want to get any of these steps wrong in my interpretation of them. Please, make sure to seek out the links I have included above to get more and very important information about emotional flashbacks from the man who coined the phrase.
The Thirteen Steps to Managing Emotional Flashbacks-
Say to yourself: “I am having a flashback”.
Flashbacks take us into a timeless part of the psyche that feels as helpless, hopeless and surrounded by danger as we were in childhood. The feelings and sensations you are experiencing are memories that cannot hurt you now.
-
Remind yourself: “I feel afraid, but I am not in danger!
I am safe now, here in the present.” Remember you are now in the safety of the present, far from the danger of the past.
-
Own your right/need to have boundaries.
Remind yourself that you do not have to allow anyone to mistreat you; you are free to leave dangerous situations and protest unfair behavior.
-
Speak reassuringly to the Inner Child.
The child needs to know that you love her unconditionally- that she can come to you for comfort and protection when she feels lost and scared.
-
Deconstruct eternity thinking in childhood, fear and abandonment felt endless – a safer future was unimaginable.
Remember the flashback will pass as it has many times before.
-
Remind yourself that you are in an adult body with allies, skills, and resources to protect you that you never had as a child.
Feeling small and little is a sure sign of a flashback.
-
Ease back into your body. Fear launches us into ‘heady’ worrying or numbing and spacing out.
[a] Gently ask your body to Relax: feel each of your major muscle groups and softly encourage them to relax. (Tightened musculature sends unnecessary danger signals to the brain)
[b] Breathe deeply and slowly.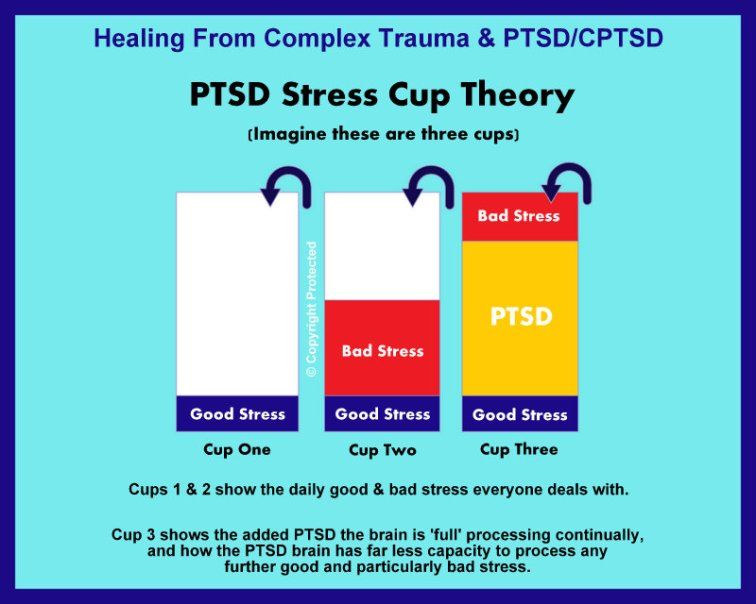 (Holding the breath also signals danger).
(Holding the breath also signals danger).
[c] Slow down: rushing presses the psyche’s panic button.
[d] Find a safe place to unwind and soothe yourself: wrap yourself in a blanket, hold a stuffed animal, lie down in a closet or a bath, take a nap.
[e] Feel the fear in your body without reacting to it. Fear is just an energy in your body that cannot hurt you if you do not run from it or react self-destructively to it.
-
Resist the Inner Critic’s (more about the Inner Critic in another post) Drasticizing and Catastrophizing:
[a] Use thought-stopping to halt its endless exaggeration of danger and constant planning to control the uncontrollable. Refuse to shame, hate or abandon yourself. Channel the anger of self-attack into saying NO to unfair self-criticism.
[b] Use thought-substitution to replace negative thinking with a memorized list of your qualities and accomplishments.
-
Allow yourself to grieve.
Flashbacks are opportunities to release old, unexpressed feelings of fear, hurt, and abandonment, and to validate – and then soothe – the child’s experience of helplessness and hopelessness.
Healthy grieving can turn our tears into self-compassion and our anger into self-protection.
-
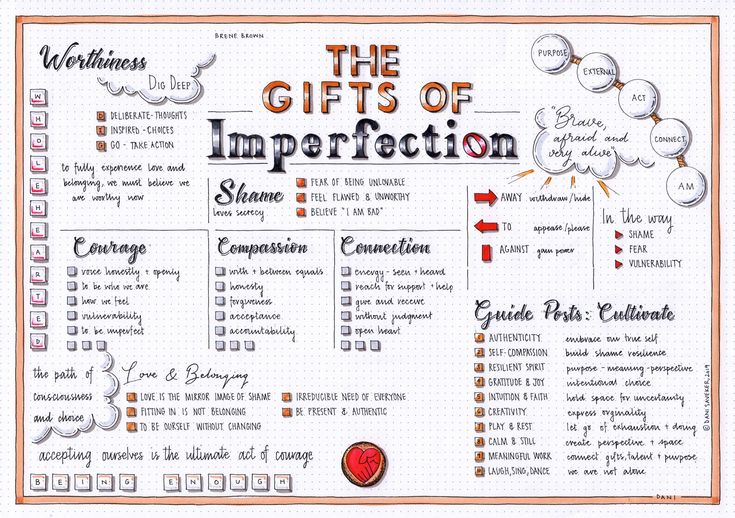
Cultivate safe relationships and seek support.
Take time alone when you need it, but don’t let shame isolate you. Feeling shame doesn’t mean you are shameful. Educate your intimates about flashbacks and ask them to help you talk and feel your way through them.
-
Learn to identify the types of triggers that lead to flashbacks.
Avoid unsafe people, places, activities and triggering mental processes.
Practice preventive maintenance with these steps when triggering situations are unavoidable.
-
Figure out what you are flashing back to.
Flashbacks are opportunities to discover, validate and heal our wounds from past abuse and abandonment.
They also point to our still unmet developmental needs and can provide motivation to get them met.
-
Be patient with a slow recovery process: it takes time in the present to become un-adrenalized, and considerable time in the future to gradually decrease the intensity, duration and frequency of flashbacks.
Real recovery is a gradually progressive process [often two steps forward, one step back], not an attained salvation fantasy. Don’t beat yourself up for having a flashback.
Ending Our Time TogetherPacked with information, I understand that this piece will take some time to digest. However, use the links I have given you and explore this topic further. In our next piece, we shall explore together the role of the Inner Critic and how it is involved in CPTD and emotional flashbacks.
Shirley Davis
My name is Shirley Davis and I am a freelance writer with over 40-years- experience writing short stories and poetry. Living as I do among the corn and bean fields of Illinois (USA), working from home using the Internet has become the best way to communicate with the world. My interests are wide and varied. I love any kind of science and read several research papers per week to satisfy my curiosity. I have earned an Associate Degree in Psychology and enjoy writing books on the subjects that most interest me.
Living as I do among the corn and bean fields of Illinois (USA), working from home using the Internet has become the best way to communicate with the world. My interests are wide and varied. I love any kind of science and read several research papers per week to satisfy my curiosity. I have earned an Associate Degree in Psychology and enjoy writing books on the subjects that most interest me.
Managing Emotional Flashbacks | CPTSDfoundation.org
In our first piece, we discussed the definition of emotional flashbacks and how they change survivors by interrupting their daily lives.
This article will attempt to explore what it is like to have an emotional flashback and the 13 steps to manage them proposed by Dr. Pete Walker.
A Short Recap of Emotional FlashbacksBefore we delve deeper into our topics for this piece, we must take a moment to recap the definition of emotional flashbacks.
Flashbacks are definable and connectable to a singular traumatic event and include a reliving of the event through the five senses. In a flashback, survivors are transported back in time to relive the trauma with all its sights, smells, sounds, and feelings.
In a flashback, survivors are transported back in time to relive the trauma with all its sights, smells, sounds, and feelings.
Emotional flashbacks are different. They seem disconnected from the current existence of the survivor and include the triggering of emotions instead of the five senses. Emotional flashbacks are like having a nightmare while you are awake.
Survivors experiencing emotional flashbacks are stranded in the feelings of being in danger, hopelessness, and helplessness that they felt in the actual traumatic events. If, for example, the survivor as a child was physically traumatized, they certainly would have felt anger, rage, and hopelessness at the same time. However, since they were only a helpless child, they could not escape or change their situation.
As an adult, this same survivor might be triggered by a situation that somehow connects with those emotions, but instead of remembering the incident as in a flashback, they experience all the agonizing emotions that went along with the traumatic experience even though they are safe today.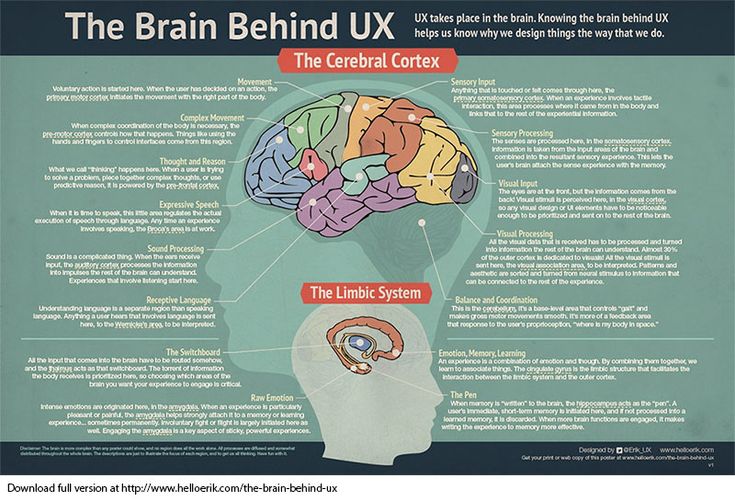
Emotional flashbacks are a symptom of complex post-traumatic stress disorder.
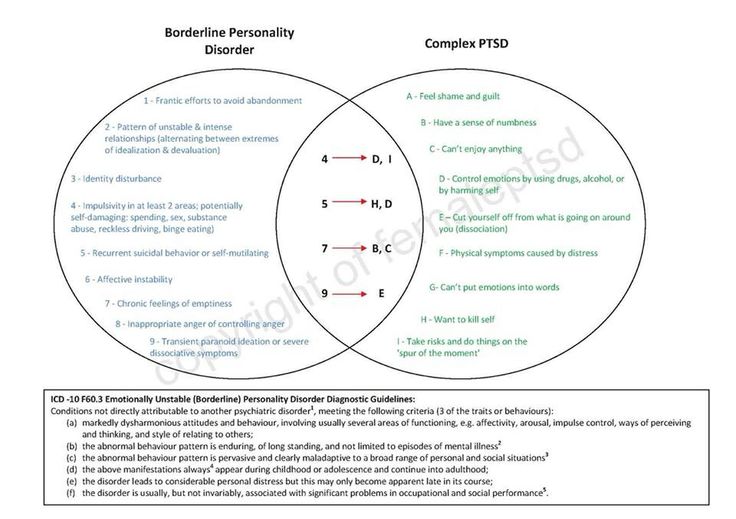
Complex Post-Traumatic Stress Disorder and Emotional FlashbacksComplex Post-Traumatic Stress Disorder (CPTSD) is a complicated diagnosis that has yet to appear in the Diagnostic and Statistical Manual of Mental Disorders (DSM).
CPTSD usually involves traumatic and long-term abuse. The following are a few examples.
- Sexual Abuse
- Emotional Abuse
- Neglect
- Physical Abuse
- Mental Abuse
- Domestic Abuse
- Human Trafficking
- Living as a Prisoner of War
- Living in a War Zone
- Surviving a Concentration or Internment Camp
Basically, CPTSD forms when a child feels they are in a situation where they cannot escape. To survive the emotional and physical trauma perpetrated on them by their abusers, these children learn to push emotions deep down inside to almost make them irretrievable.
The connection between complex post-traumatic stress disorder and emotional flashbacks is well-documented. The emotions that were ignored and stuffed in childhood can be triggered back to life again, presenting disconnected emotions that seemingly come from nowhere.
The emotions that were ignored and stuffed in childhood can be triggered back to life again, presenting disconnected emotions that seemingly come from nowhere.
One good example is a child who was emotionally abused daily by his family, telling him he was ugly and would never be anything. Although this child grew up to be a prosperous businessman, he still experiences times when he feels triggered to feel he is ugly and an imposter in his accomplishments.
The Experience of Having an Emotional FlashbackEmotional flashbacks are sudden and often prolonged regressions (amygdala hijackings) to the frightening and abandoned feeling-states of childhood.
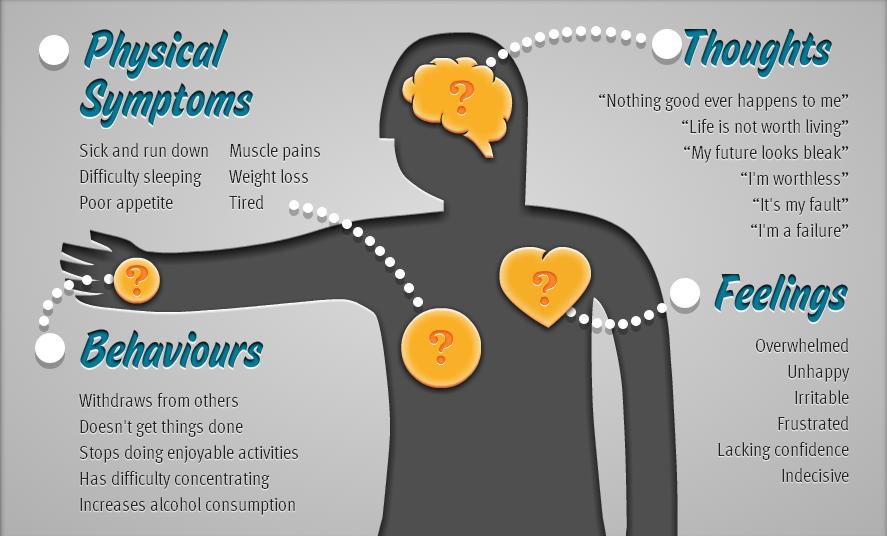
Emotional flashbacks are together with inappropriate and intense fight/flight instincts through the sympathetic nervous system. These instincts present as intense and confusing periods of shame, fear, despair, and anger that are manifested against the survivor or those around them.
Often, when the survivors’ primary emotion during an emotional flashback is fear, they feel panicky and overwhelmed.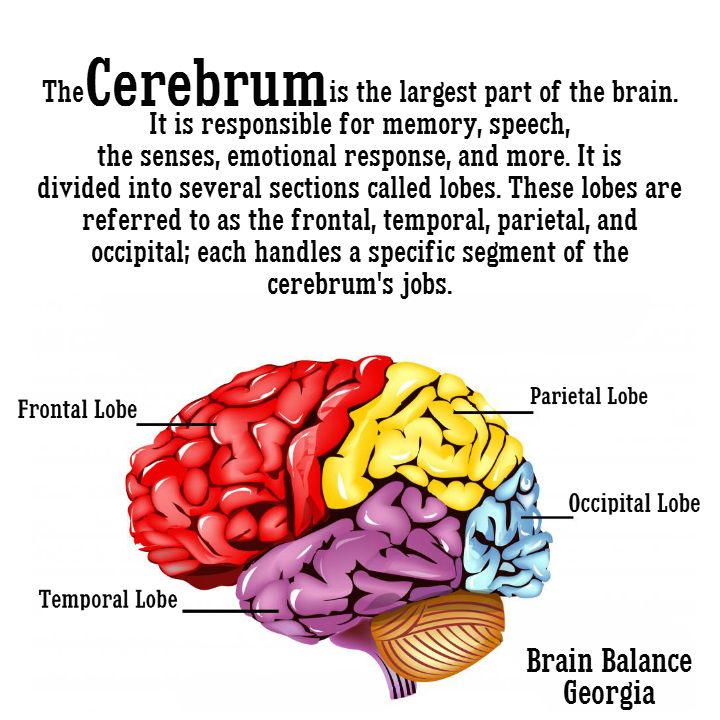 When the emotion of despair is dominant, it causes the survivor to feel numb, paralyzed, and feel that they need to hide.
When the emotion of despair is dominant, it causes the survivor to feel numb, paralyzed, and feel that they need to hide.
Such experiences typically come with toxic shame, which, as described in John Bradshaw’s Healing the Shame That Binds. Toxic shame aids in the overpowering sense that she is as stupid, worthless, or flawed.
Survivors often describe emotional flashbacks as feeling like something horrible is about to happen and that they must be on guard for any danger. It is an overwhelming sense that nuclear war is about to begin or that someone is going to die. The symptoms of emotional flashbacks are terrifying and extremely uncomfortable.
Dr. Pete WalkerTo help us understand emotional flashbacks better, it is essential to include a section on Pete Walker, a licensed psychotherapist who has a private practice in Berkeley, California.
Pete Walker specializes in treating adults who survived traumatization in childhood, especially those who experienced repeated exposure to abuse and neglect.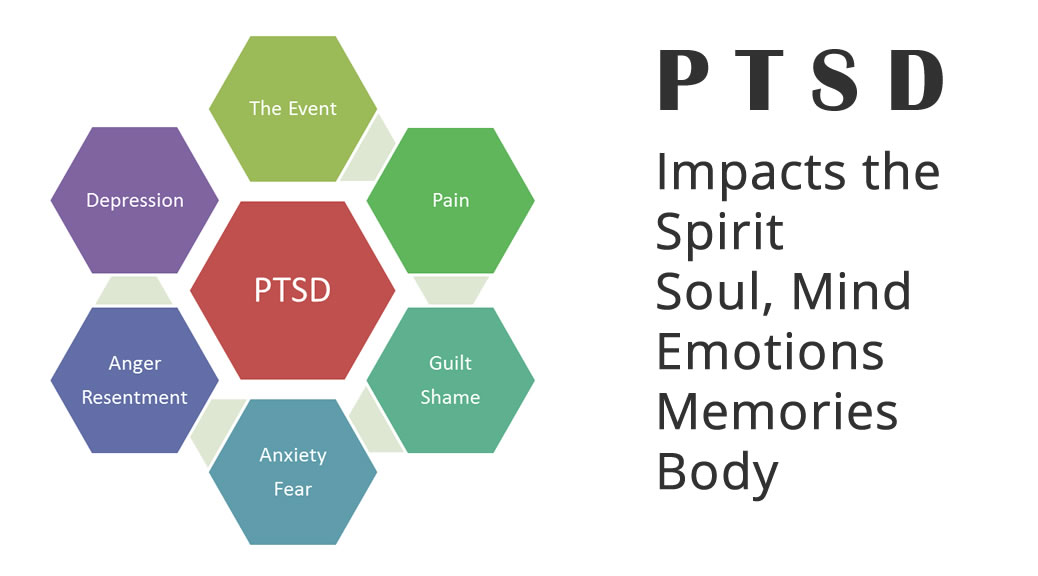 He is also a well-respected authority on the topic of emotional flashbacks.
He is also a well-respected authority on the topic of emotional flashbacks.
Mr. Walker offers the following definition of emotional flashbacks in his book Complex PTSD: From Surviving to Thriving.
“Emotional flashbacks are sudden and often prolonged regressions to the overwhelming feeling-states of being an abused/abandoned child. These feelings states can include overwhelming fear, shame, alienation, rage, grief, and depression. They also include unnecessary triggering of our fight/flight instincts.”
Regression is a defense mechanism that awakens when survivors face anxiety-filled events that cause them to retreat to a childhood state. In regression, full-grown adults flashback back to their emotions as children and feel abandoned, abused, and helpless or overwhelming emotions of fear, rage, shame, depression, and grief that trigger a strong fight/flight/freeze response.
According to Pete Walker, survivors experiencing emotional flashbacks are overwhelmed with emotions they cannot understand or recognize with events they may or may not remember or connect these emotions to.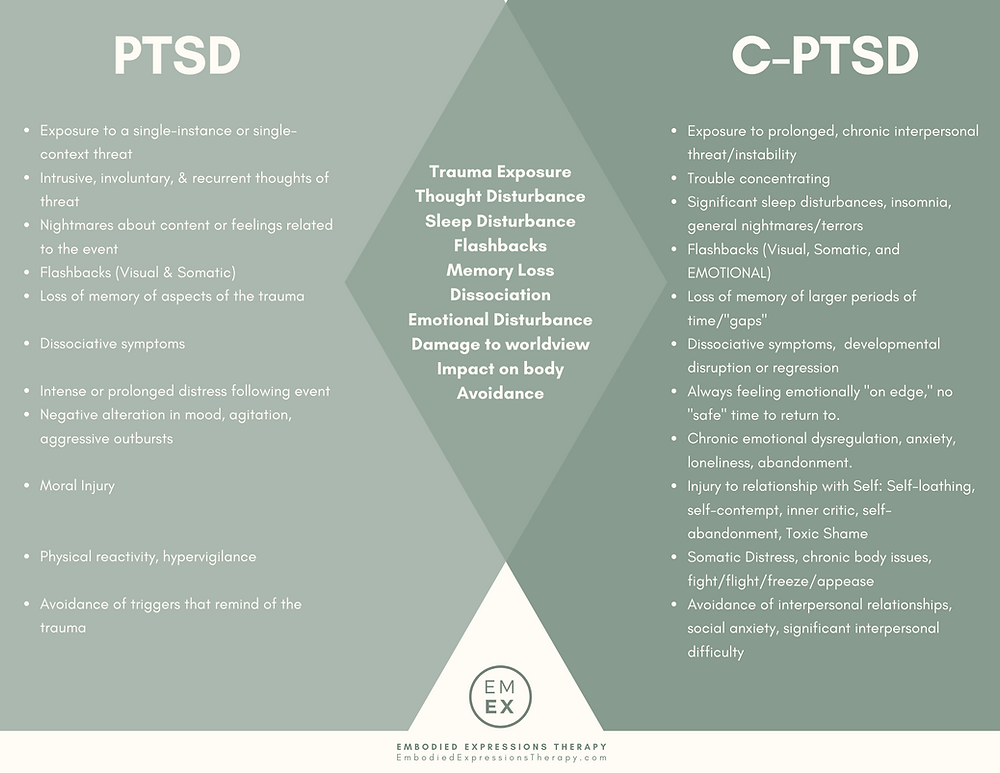
Pete Walker describes 13 Steps to Managing Emotional Flashbacks.
The 13 Steps to Managing Emotional FlashbacksAs stated, Pete Walker proposes on his website that there are thirteen steps toward managing and perhaps overcoming the effects of emotional flashbacks. These steps are available both on Mr. Walker’s website and in his book, Complex PTSD from Surviving to Thriving.
The 13 steps to managing emotional flashbacks are quoted from Pete Walker’s website below:
- Say to yourself: “I am having a flashback.”
Flashbacks take us into a timeless part of the psyche that feels as helpless, hopeless, and surrounded by danger as we were in childhood. The feelings and sensations you are experiencing are memories that cannot hurt you now.
- Remind yourself: “I feel afraid, but I am not in danger!
I am safe now, here in the present.” Remember, you are now in the safety of the present, far from the danger of the past.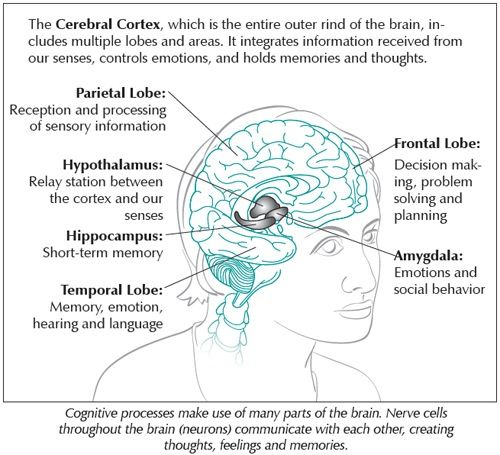
- Own your right/need to have boundaries.
Remind yourself that you do not have to allow anyone to mistreat you; you are free to leave dangerous situations and protest unfair behavior.
- Speak reassuringly to the Inner Child.
The child needs to know that you love her unconditionally- that she can come to you for comfort and protection when she feels lost and scared.
Deconstruct eternity thinking in childhood, fear and abandonment felt endless – a safer future was unimaginable.
- Remember, the flashback will pass as it has many times before.
Remind yourself that you are in an adult body with allies, skills, and resources to protect you that you never had as a child.
Feeling small and little is a sure sign of a flashback.
Ease back into your body. Fear launches us into ‘heady’ worrying or numbing and spacing out.
- Gently ask your body to Relax.
Feel each of your major muscle groups and softly encourage them to relax. Breathe deeply, find a safe place to soothe yourself, and allow yourself to feel the fear without reacting to it.
- Resist the Inner Critic’s (more about the Inner Critic in another post) Catastrophizing.
Use thought to stop the inner critic’s endless exaggeration of danger and constant planning to control the uncontrollable. Refuse to shame, hate, or abandon yourself. Channel the anger of self-attack into saying NO to unfair self-criticism.
Use thought substitution to replace negative thinking with a memorized list of your qualities and accomplishments.
- Allow yourself to grieve.
Flashbacks are opportunities to release old, unexpressed feelings of fear, hurt, and abandonment and to validate – and then soothe – the child’s experience of helplessness and hopelessness.
Healthy grieving can turn our tears into self-compassion and our anger into self-protection.![]()
- Cultivate safe relationships and seek support.
Take time alone when you need it, but don’t let shame isolate you. Feeling shame doesn’t mean you are shameful. Educate your intimates about flashbacks and ask them to help you talk and feel your way through them.
- Learn to identify the types of triggers that lead to flashbacks.
Avoid unsafe people, places, activities, and triggering mental processes.
Practice preventive maintenance with these steps when triggering situations are unavoidable.
- Figure out what you are flashing back to.
Flashbacks are opportunities to discover, validate, and heal our wounds from past abuse and abandonment. They also point to our still unmet developmental needs and can provide motivation to get them met.
- Be patient with a slow recovery process.
It takes time in the present to become un-adrenalized and considerable time in the future to gradually decrease the intensity, duration, and frequency of flashbacks. Real recovery is a gradually progressive process (often two steps forward, one step back), not an attained salvation fantasy.
Real recovery is a gradually progressive process (often two steps forward, one step back), not an attained salvation fantasy.
- Don’t beat yourself up for having a flashback.
Flashbacks happen without your consent and certainly without you wanting them to occur. So, why beat yourself up over something you have little control over.
In Closing
Emotional flashbacks are different from the other type of flashback. The survivor experiencing it experience the emotions without physically reliving the incident. Emotional flashbacks are often part of the diagnosis of complex post-traumatic stress disorder.
Dr. Pete Walker describes emotional flashbacks as sudden and often prolonged regressions into overwhelming feeling-states when a survivor experienced child abuse. The emotions that accompany emotional flashbacks are overwhelming and include fear, shame, alienation, grief, rage, and depression.
In our next piece, the CPTSD Foundation will explore how emotional flashbacks trigger the fight/flight/freeze/fawn response in their victims and what is going on in the brain during one.
“He saw it in her eyes. The anguish, the frustration. The terrible nothing that clawed inside and sought to smother her. She knew. It was there, inside. She had been broken.
Then she smiled. Oh, storms. She smiled, anyway.
It was the single most beautiful thing he’d seen in his entire life.” ~ Brandon Sanderson
References
Bradshaw, J. (2005). Healing the shame that binds you: Recovery classics edition. Health Communications, Inc.
Van der Kolk, B. A. (2002). The assessment and treatment of complex PTSD. Treating trauma survivors with PTSD, 127, 156.
Walker, P. 13 Steps for Managing Flashbacks. Retrieved from: http://pete-walker.com/13StepsManageFlashbacks.htm
Walker, P. (2009). Emotional flashback management in the treatment of Complex PTSD. Psychotherapy.net.
If you are a survivor or someone who loves a survivor and cannot find a therapist who treats complex post-traumatic stress disorder, please contact the CPTSD Foundation. We have a staff of volunteers who have been compiling a list of providers who treat CPTSD. They would be happy to give you more ideas about where to look for and find a therapist to help you. Go to the contact us page and send us a note stating you need help, and our staff will respond quickly to your request.
We have a staff of volunteers who have been compiling a list of providers who treat CPTSD. They would be happy to give you more ideas about where to look for and find a therapist to help you. Go to the contact us page and send us a note stating you need help, and our staff will respond quickly to your request.
Are you a therapist who treats CPTSD? Please, consider dropping us a line to add you to our growing list of providers. You would get aid in finding clients, and you would be helping someone find the peace they deserve. Go to the contact us page and send us a note, and our staff will respond quickly.
Shortly, CPTSD Foundation will have compiled a long list of providers who treat complex post-traumatic stress disorder. When it becomes available, we will be putting it on our website www.CPTSDFoundation.org.
Make sure to visit us and sign up for our weekly newsletter to help keep you informed on treatment options and much more for complex post-traumatic stress disorder.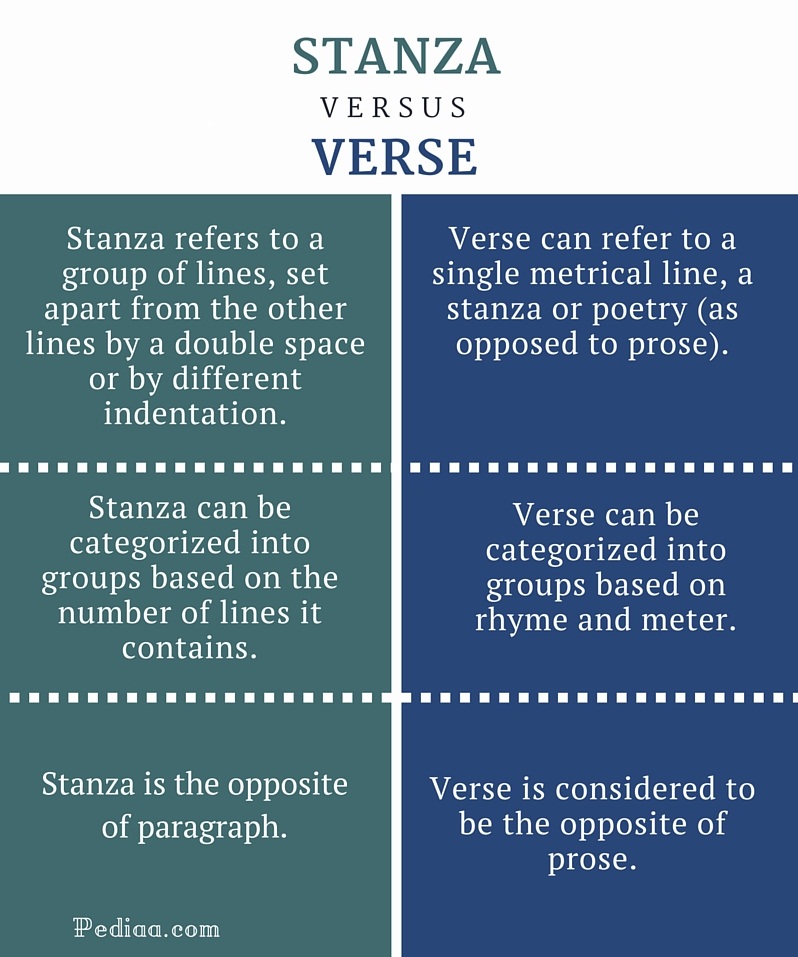
If you or a loved one live in the despair and isolation that comes with complex post-traumatic stress disorder, please, come to us for help. CPTSD Foundation offers a wide range of services, including:
- Daily Calls
- The Healing Book Club
- Support Groups
- Our Blog
- The Trauma-Informed Newsletter
- Daily Encouragement Texts
Today, CPTSD Foundation would like to invite you to our healing book club, reading a new book that began in September. The title of the latest featured book is The Body Keeps the Score by Bessel van der Kolk.
Led by Sabra Cain, the healing book club is only $7 per month. The fee goes towards scholarships for those who cannot afford access to materials offered by CPTSD Foundation.
Should you decide to join the Healing Book Club, please purchase your books through our Amazon link to help us help you.
All our services are reasonably priced, and some are even free. So, to gain more insight into how complex post-traumatic stress disorder is altering your life and how you can overcome it, sign-up; we will be glad to help you. If you cannot afford to pay, go to www.cptsdfoundation.org/scholarship to apply for aid. We only wish to serve you.
If you cannot afford to pay, go to www.cptsdfoundation.org/scholarship to apply for aid. We only wish to serve you.
The Connection Between Emotional Flashbacks and the Inner Critic
Flashbacks, Complex Post-Traumatic Stress Disorder, and the Brain
Shirley Davis
My name is Shirley Davis and I am a freelance writer with over 40-years- experience writing short stories and poetry. Living as I do among the corn and bean fields of Illinois (USA), working from home using the Internet has become the best way to communicate with the world. My interests are wide and varied. I love any kind of science and read several research papers per week to satisfy my curiosity. I have earned an Associate Degree in Psychology and enjoy writing books on the subjects that most interest me.
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.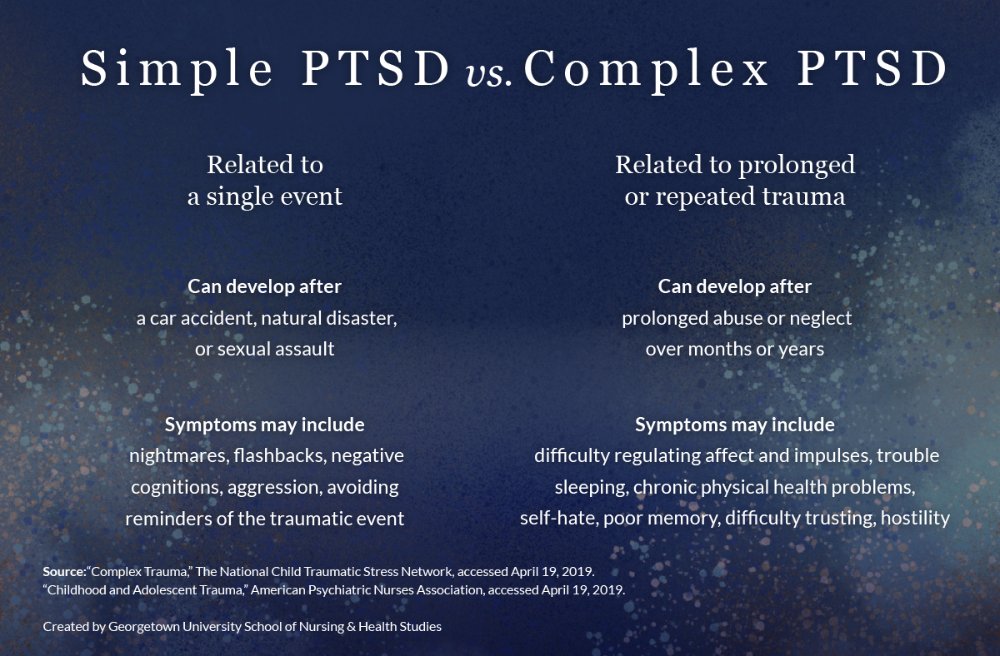
This booklet deals with signs,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident. nine0024
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension.
 nine0024
nine0024
PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment. nine0003
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event.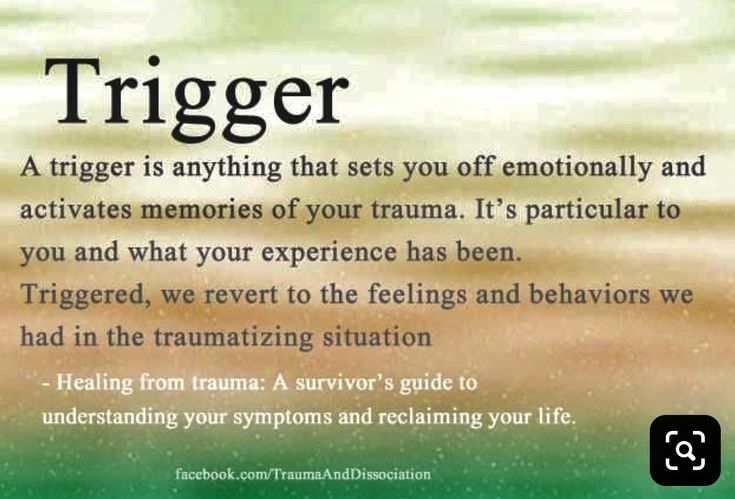 you try to hold on away from anything that might remind you of the experience.
you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last? nine0011
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this disease? nine0011
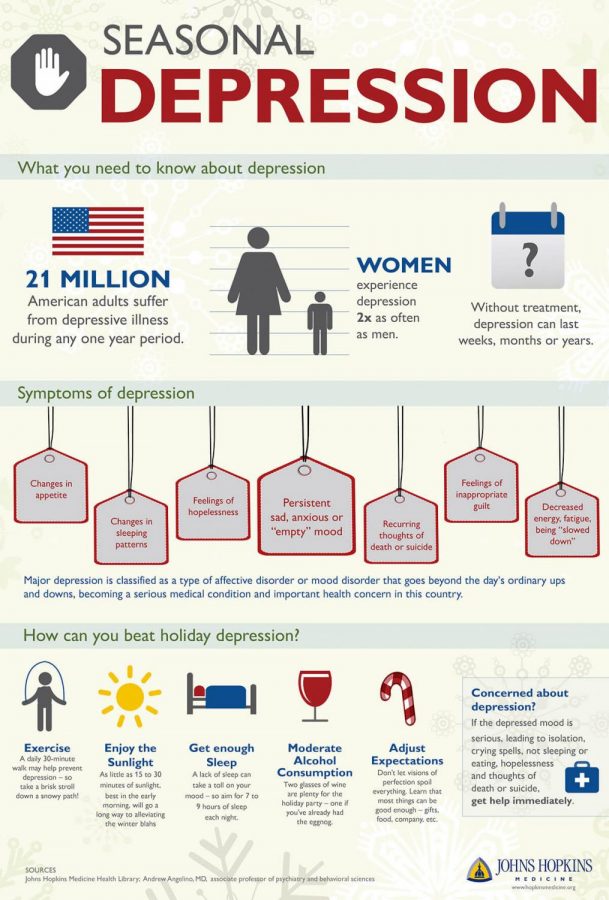
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men. The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse. nine0003
The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse. nine0003
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD. nine0003
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What should I do to help myself in this situation? nine0011
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses. nine0003
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
Your doctor may prescribe medicine to help reduce your fear or tension. However, it should be borne in mind that usually several weeks before the medicine starts to work. nine0003
nine0003
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories. nine0003
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD. nine0003
They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD. nine0003
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is. nine0003
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military.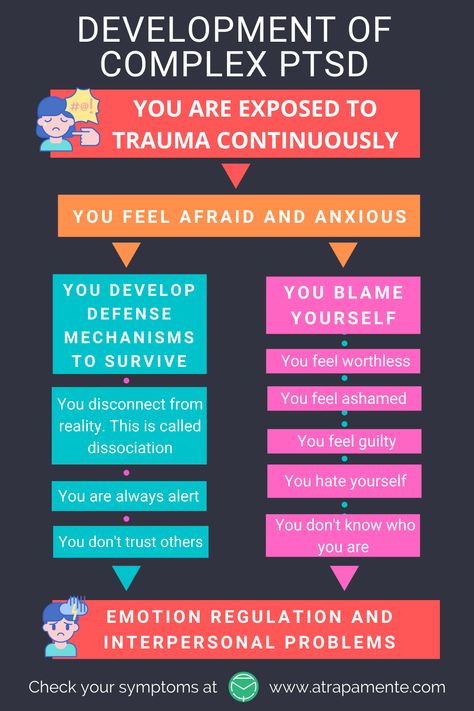 MST can happen with men and women, and can occur in peacetime, during war training or during the war.
MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear.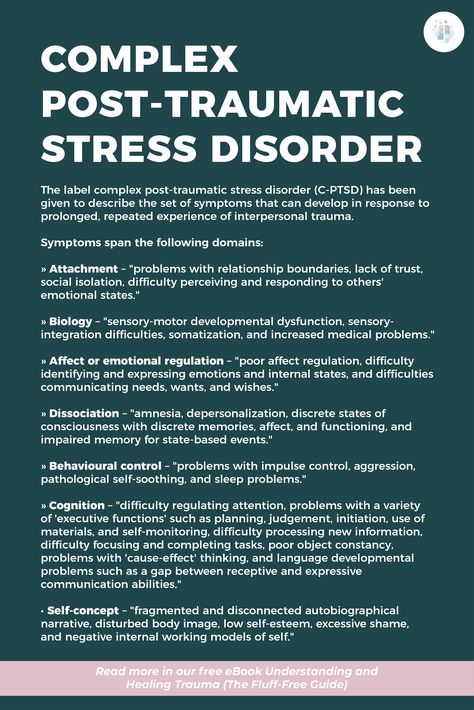 The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease. nine0003
The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease. nine0003
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. nine0184 1
nine0184 1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. nine0184 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" do not be afraid).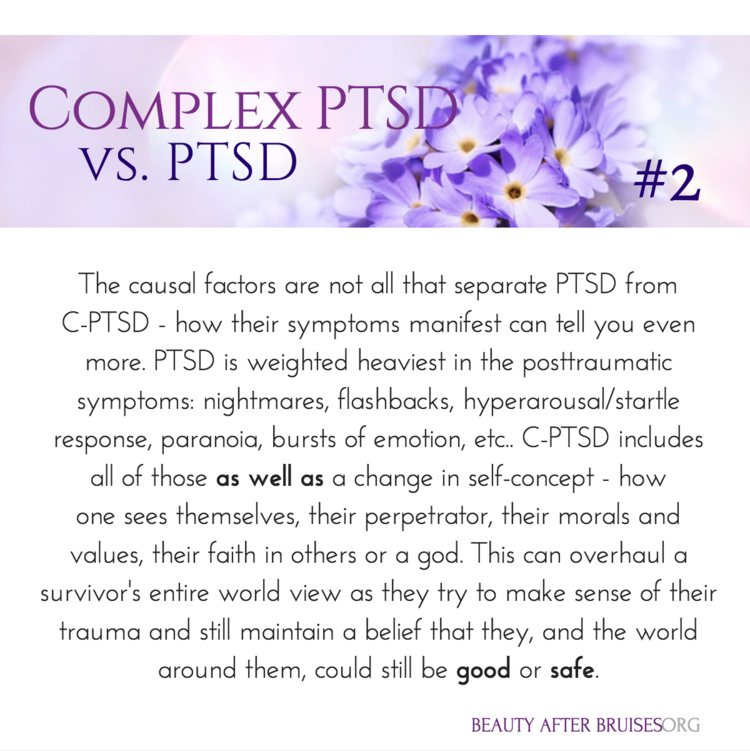 nine0184 4
nine0184 4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress. nine0184 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth.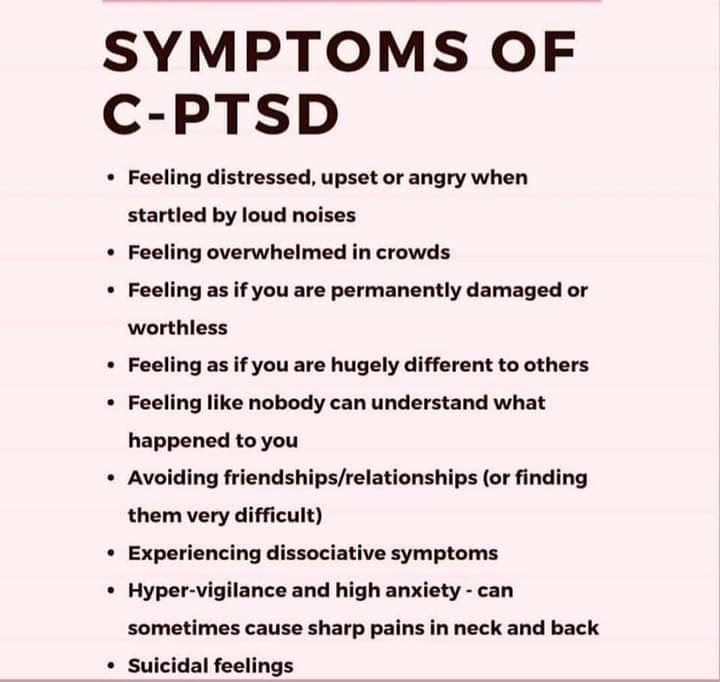 nine0184 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't. nine0003
nine0184 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't. nine0003
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate. nine0003
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced. NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced. 9
9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. nine0184 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. nine0184 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation.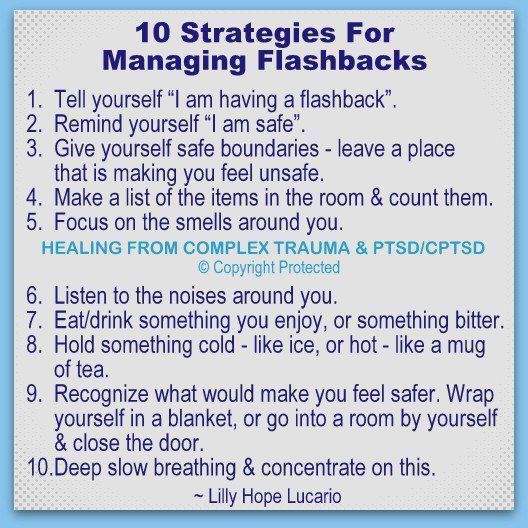 First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. nine0184 12
First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. nine0184 12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal. nine0003
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease. During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment. nine0003
During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment. nine0003
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: nimhinfo@nih.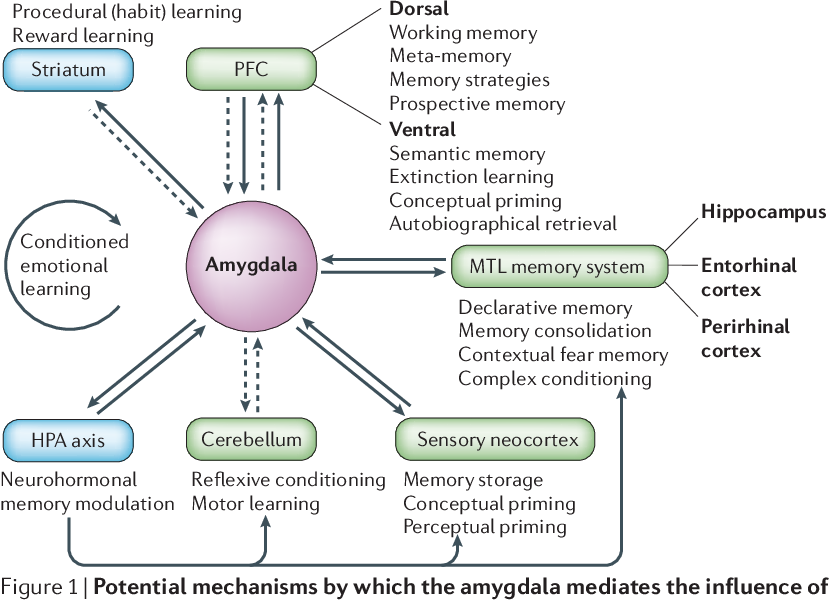 gov
gov
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www.ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction.
 Nature. Nov 7 2002;420(6911):70-74.
Nature. Nov 7 2002;420(6911):70-74. - 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus. Nat Neurosci. Mar 2005;8(3):365-371.
- Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711. nine0024
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder.
 Biol Psychiatry. Feb 3 2006.
Biol Psychiatry. Feb 3 2006. - Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
- Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634. nine0024
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F.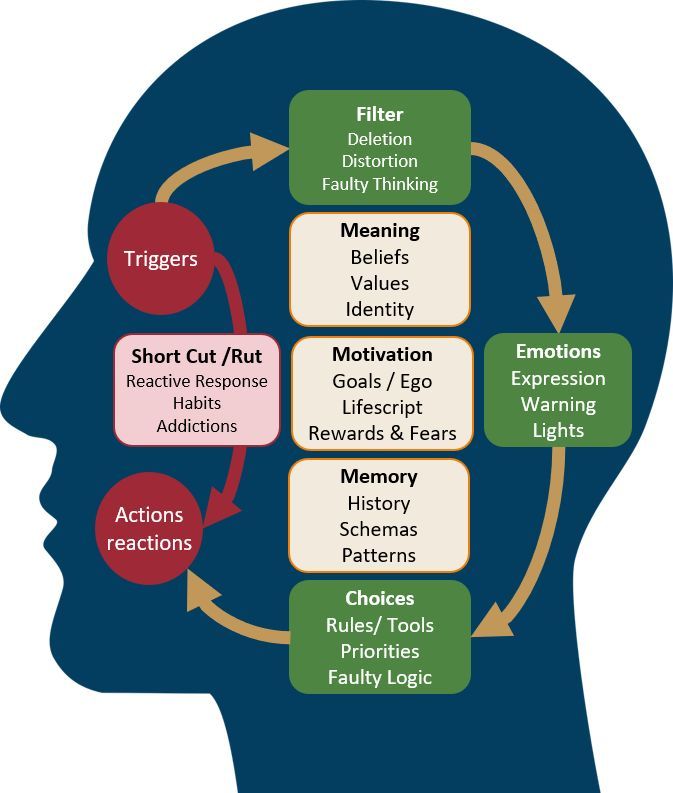 Hogan, PhD
Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Division of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www.omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Division of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
PTSD and complex PTSD: what happens when you live in a psychological war zone
Retrieved from https://thoughtcatalog. com/shahida-arabi/2018/03/ptsd-and-complex-ptsd- what-happens-when-youve-lived-in-a-psychological-war-zone/?fbclid=IwAR1LM5Mxpy_EWp51W8aSnw3rTST6UYEij2MV5QHvuyKJvV769C3Ia_jBPC0
com/shahida-arabi/2018/03/ptsd-and-complex-ptsd- what-happens-when-youve-lived-in-a-psychological-war-zone/?fbclid=IwAR1LM5Mxpy_EWp51W8aSnw3rTST6UYEij2MV5QHvuyKJvV769C3Ia_jBPC0
Complex post-traumatic disorder is a term not yet officially listed by the American Psychiatric Association (DSM-V) but is used by therapists because the effects of a single or time-limited experience of a traumatic event (PTSD) are very different from a situation where a person He was forced to cope with seemingly not deadly circumstances, but which lasted a long time, which he could not influence in any way. In a nutshell, the latter is much worse, especially considering that in the second case, the threat often comes from loved ones, and the victim is a child, although the description of this situation often does not seem so terrible: there were no explosions, collapsed houses, fires, etc. nine0003
--------
PTSD is commonly associated with combat victims, but this is not limited to those who have fought. Many survivors of childhood physical, emotional or sexual abuse suffer from symptoms of PTSD or complex PTSD.
Many survivors of childhood physical, emotional or sexual abuse suffer from symptoms of PTSD or complex PTSD.
Such people have been in invisible war zones, which nonetheless injure and leave wounds. About 8 million people can develop PTSD each year, and women are twice as likely as men to experience these symptoms, according to the National PTSD Center. nine0003
What are the symptoms of PTSD and complex PTSD?
There are four types of symptoms that are part of PTSD and there are additional symptoms for complex PTSD. Complex PTSD that develops due to chronic ongoing trauma is more common due to long-term domestic violence or childhood sexual and/or physical or emotional abuse. About 92% of people who meet the criteria for complex PTSD also meet the criteria for PTSD (Roth, et al. 1997). nine0003
It is recommended that you seek professional support if you experience any of these symptoms, especially if your symptoms last longer than one month, make you feel very unwell, and/or interfere with your ability to cope with everyday tasks.
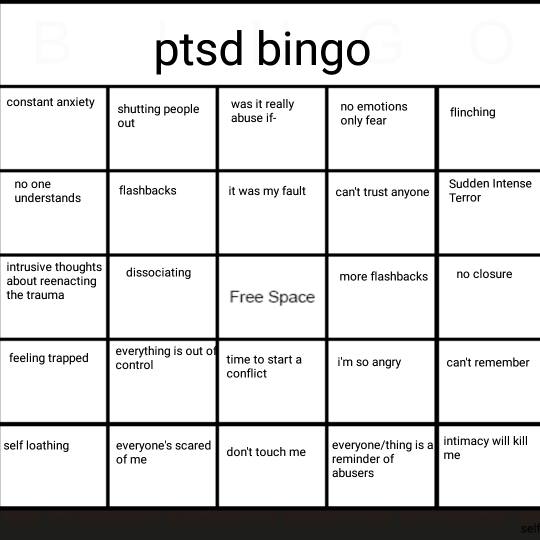
1. Flashbacks and re-experiencing trauma
PTSD: memories of the traumatic event, recurring nightmares, persistent unpleasant and frightening thoughts, physical symptoms of the trauma, vivid memories of the original event may be part of PTSD. You may also encounter triggers in everyday life - what you see, feel, hear, takes you back to the original event. It may look different. A woman who has experienced rape, hearing a voice similar to the voice of the rapist, feels the fear of attack. For the victim, the domestic trigger may be a raised voice. Triggers can seem minor or overwhelming, depending on the severity and duration of the injury. nine0003
Complex PTSD: According to psychotherapist Pete Walker (2013), you can also suffer from emotional flashbacks, where you “fall back” into the emotional state of the original event and become maladaptive as a result. Walker states that people with complex PTSD develop four "F" responses in response to emotional triggers: they may fight (fight), flee (flight), seek to please (fawn), or freeze (freeze).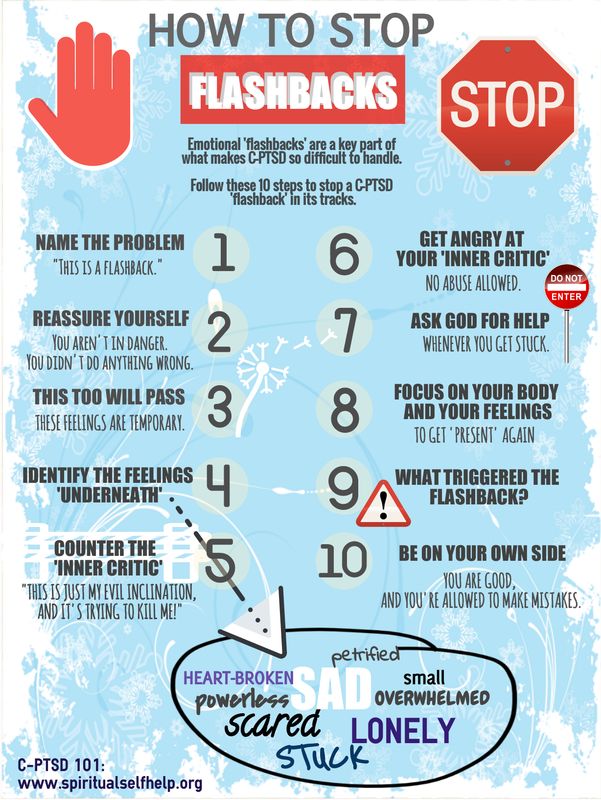 These are defensive responses, but in the end they can further harm the survivor, as they may not defend their personal boundaries or, conversely, may be too aggressive in protecting themselves. nine0003
These are defensive responses, but in the end they can further harm the survivor, as they may not defend their personal boundaries or, conversely, may be too aggressive in protecting themselves. nine0003
2. Avoiding situations that remind you of the traumatic event
PTSD: You go to great lengths to avoid memories or feelings associated with traumatic events. For example, if your relationship with your partner has been violent, you may want to be alone and avoid new acquaintances to protect yourself from a possible threat.
If you are a survivor of rape, you may want to avoid all physical contact, whether it be a massage or affection from a loved one. If you've been bullied, you may want to avoid crowded places, including noisy groups, or even work that involves frequent contact with other people. This may also include trying to avoid thoughts related to the trauma; you can constantly look for something to do so that you don't have to deal with the memories of the traumatic event. nine0003
nine0003
Complex PTSD: Throughout your life, you can go to any lengths to keep relationships and please others. As a result, there are often problems with personal boundaries and the protection of their rights, and a person who grew up in a situation of violence tends to build co-dependent relationships. You may be too afraid of disapproval, watching for the slightest sign of it, or avoiding anything that resembles the situation when you were left or abandoned.
As psychotherapist Pete Walker (2013) writes, “Abandonment depression is a complex, painful childhood experience that is recreated in an emotional memory. This is a return to the feeling of overwhelm, hopelessness and helplessness that overtakes a child who has experienced abuse and / or loneliness. At the core of the abandoned depression is a terrible mixture of fear and shame that coalesces around the murderous depression that the abandoned child suffers from.” nine0003
3. Distorted self-image and negative self-image, including self-blame and toxic shame
PTSD: After traumatic events, a change in self-perception occurs. You may suffer from low self-esteem, depression, intrusive thoughts, self-blame, memory lapses when remembering trauma, decreased interest in hobbies, and feelings of guilt.
You may suffer from low self-esteem, depression, intrusive thoughts, self-blame, memory lapses when remembering trauma, decreased interest in hobbies, and feelings of guilt.
Complex PTSD: People with complex PTSD may struggle with guilt, toxic shame, and feelings of difference or even inferiority. They may have a strong "inner critic" that comes from any experience of verbal, emotional, physical, or sexual abuse. This inner critic can judge everything you do or say, prevent you from trying new things or pursuing your goal, can lead to feelings of learned helplessness, and can often mimic the voices of any abusers you encounter, especially if you had toxic parents. nine0003
4. Hyperanxiety and hypervigilance
PTSD: You feel excessive anxiety. You may often be frightened, irritable or aggressive, take risks, and have difficulty concentrating or sleeping.
Complex PTSD: People with complex PTSD experience difficulty with emotional regulation, suicidal thoughts and self-isolation. They may harm themselves, develop addictions to substance abuse, and have difficulty trusting themselves and their intuition. They may end up in an unhealthy, abusive relationship due to what trauma expert Judith Herman calls "the constant search for a rescuer" (Herman, 1997). They may have a deep distrust of others, but at the same time they are extremely attentive to changes in everything around them and constantly monitor the slightest changes in the mood and behavior of others, changes in tone of voice or gestures.
They may harm themselves, develop addictions to substance abuse, and have difficulty trusting themselves and their intuition. They may end up in an unhealthy, abusive relationship due to what trauma expert Judith Herman calls "the constant search for a rescuer" (Herman, 1997). They may have a deep distrust of others, but at the same time they are extremely attentive to changes in everything around them and constantly monitor the slightest changes in the mood and behavior of others, changes in tone of voice or gestures.
Treatment of PTSD and Complex PTSD
Treatment of PTSD and Complex PTSD requires highly skilled therapy with an informed and supportive professional with whom it is safe to understand your triggers. Effective therapies include trauma-focused psychotherapy such as
long exposure therapy (PE) which involves facing the negative feelings you have been avoiding
cognitive behavioral therapy (CPT) which teaches the client to re-examine their thoughts about the trauma
rapid eye movement desensitization therapy (EMDR).