Complex ptsd dsm 5 criteria
Complex Posttraumatic Stress Disorder (C-PTSD) symptoms and diagnostic criteria
What is Complex PTSD?
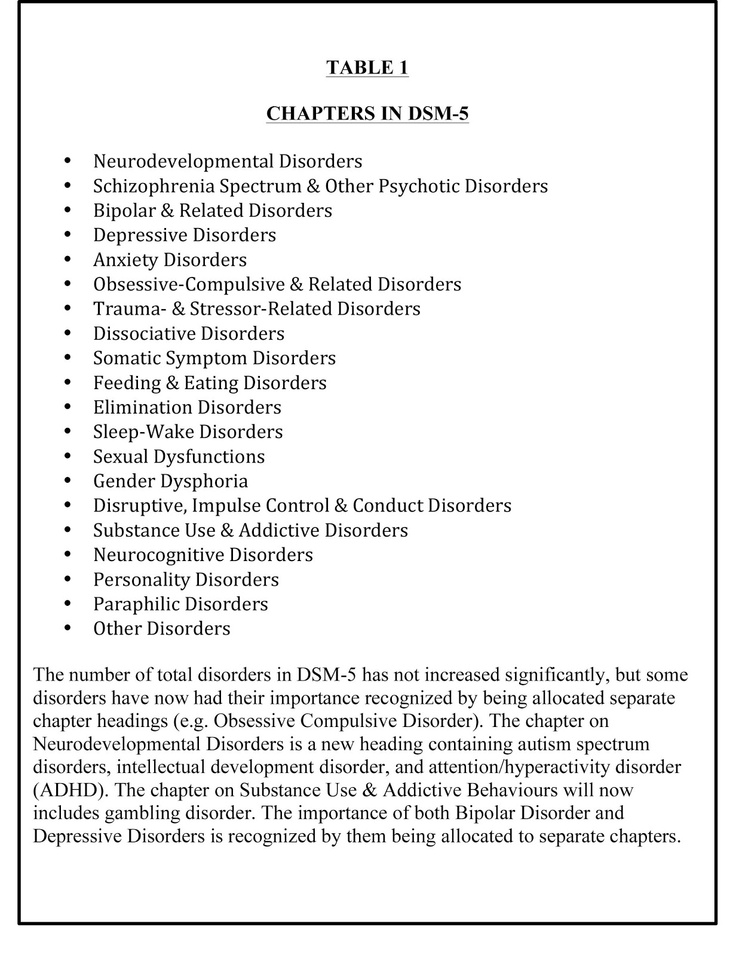
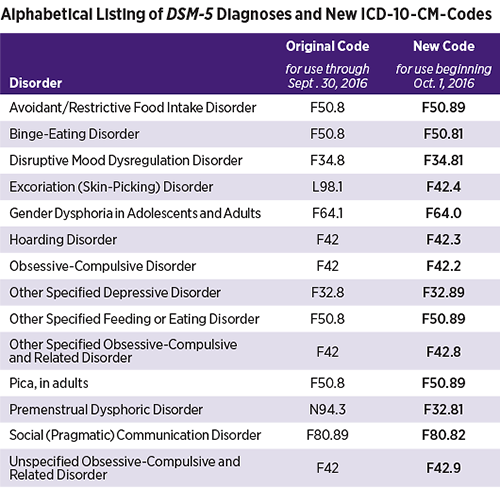
Complex Posttraumatic Stress Disorder, is the result of multiple traumatic events occurring over a period of time, often referred to as "complex trauma". Causes include multiple incidents of child abuse, particularly child physical abuse and child sexual abuse, prolonged domestic violence, concentration camp experiences, torture, slavery, and genocide campaigns.[3] Complex Post-traumatic Stress Disorder is not a diagnosis in the DSM-5 psychiatric manual, released in 2013,[5] but is planned for inclusion in the ICD-11 diagnostic manual, due for release in 2017. [3]
Dr Frank Ocher explains the wider impact of Complex PTSD.
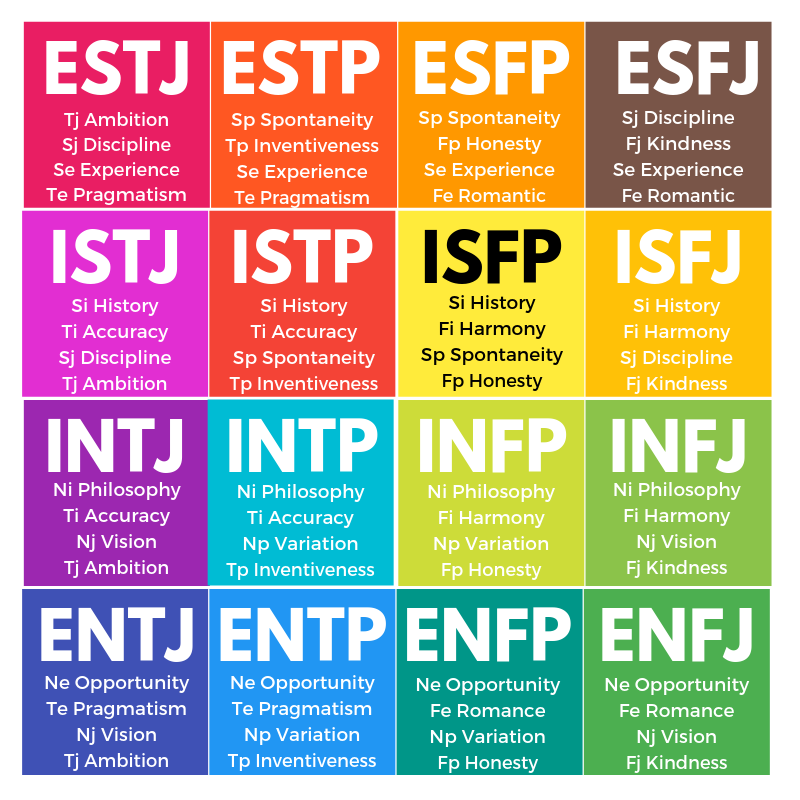
Differences between PTSD and Complex PTSD
The diagram shows the additional symptoms present in Complex PTSD, compared to PTSD, and is based on research from 2013. [6]
Complex PTSD Symptoms
- Interpersonal problems includes social and interpersonal avoidance (avoiding relationships), feeling distance or cut off from others, and never feeling close to another person.
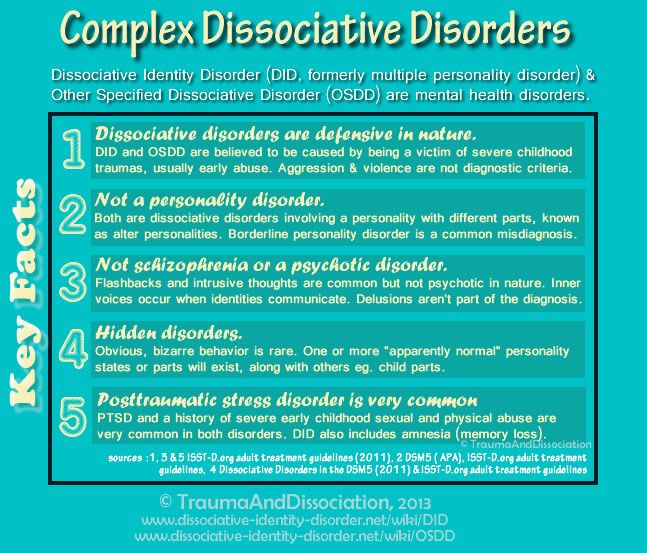
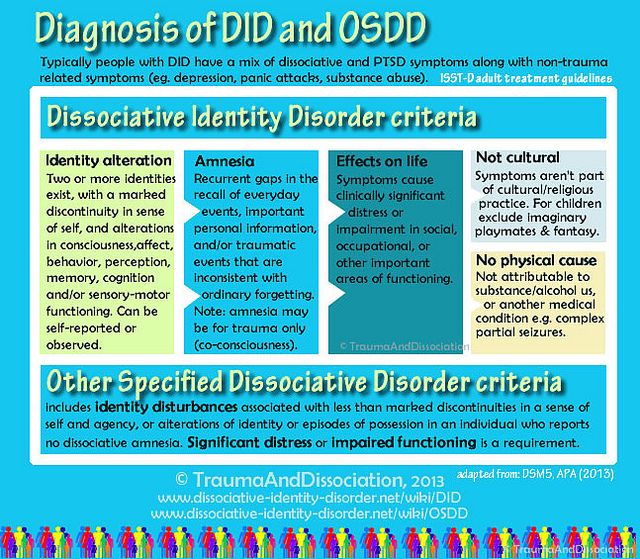
- Negative self-concept involves feelings of worthlessness and guilt. While survivors of PTSD may feel "not myself", a survivor of Complex PTSD may feel no sense of self at all or experience a changed personality; a few may feel as if they are no longer human at all (Lovelace and McGrady, 1980; Timerman, 1981).[1]:385-386. Believing yourself to be "contaminated, guilty, and evil" is commonly reported by survivors of Complex PTSD. A fragmented identity is common, with Dissociative Identity Disorder occurring in some people. [1]:386
- Interpersonal sensitivity includes having feelings which are easily hurt, anger/temper outbursts and difficulties with interpersonal relationships.
 Complex PTSD is normally the result of interpersonal trauma, the long duration of the trauma and the control of the perpetrator(s) prevents people from expressing anger or rage at the perpetrator(s) during the trauma; anger and rage both at perpetrators and the self can only be fully expressed after the trauma ends. Prolonged abuse normally leads to a loss of previously-held beliefs, with feelings of "being forsaken by both man and God". [1]:382,386
Complex PTSD is normally the result of interpersonal trauma, the long duration of the trauma and the control of the perpetrator(s) prevents people from expressing anger or rage at the perpetrator(s) during the trauma; anger and rage both at perpetrators and the self can only be fully expressed after the trauma ends. Prolonged abuse normally leads to a loss of previously-held beliefs, with feelings of "being forsaken by both man and God". [1]:382,386 - Affect dysregulation means being unable to manage your own emotions, and is often referred to as "difficulties with emotional regulation". The unexpressed anger and internalized rage resulting from the trauma may lead to self-destructive or reckless/risk taking behaviors, e.g., self-harm and/or suicide attempts, which may be driven by a sense of self-hatred. [1]:382, [6]
- People with Complex PTSD also meet the diagnostic criteria for PTSD, which are:
- a persistent sense of threat
, e.
 g. hypervigilance and being easily startled
g. hypervigilance and being easily startled - avoiding reminders of the traumas,
- and re-experiencing or reliving the traumas, for example flashbacks and intrusive thoughts about the trauma.
- a persistent sense of threat
, e.
In addition to the symptoms above, survivors of prolonged child abuse have an increased risk of both self-injury and repeated victimization, for example relationships with abusive people, sexual harassment, and rape. [1]:387
Judith Lewis-Herman, who first proposed Complex PTSD as a separate diagnosis, stated:
Observers who have never experienced prolonged terror, and who have no understanding of coercive methods of control, often presume that they would show greater psychological resistance than the victim in similar circumstances. The survivor's difficulties are all too easily attributed to underlying character problems, even when the trauma is known.When the trauma is kept secret, as is frequently the case in sexual and domestic violence, the survivor's symptoms and behavior may appear quite baffling, not only to lay people but also to mental health professionals. The clinical picture of a person who has been reduced to elemental concerns of survival is still frequently mistaken for a portrait of the survivor's underlying character." [1]:388
Complex PTSD, BPD and Personality Disorders
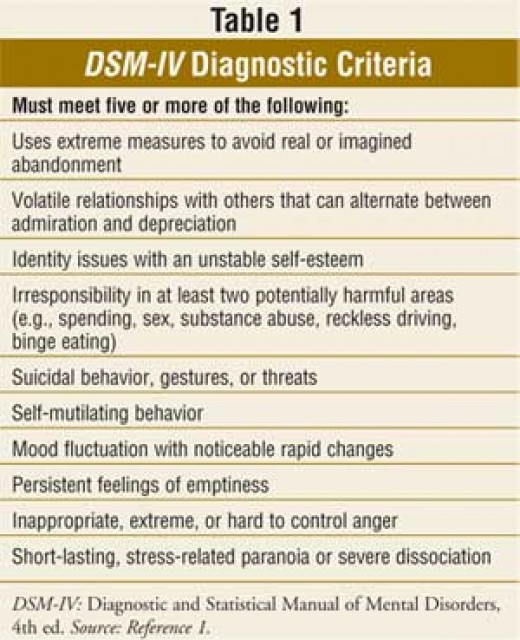
Recent research has produced detailed analysis of the symptoms of Complex PTSD, PTSD and Borderline Personality Disorder (BPD). Many people with BPD either have PTSD, or meet the proposed diagnostic criteria for Complex PTSD. Complex PTSD was shown to be a separate diagnosis from Borderline Personality Disorder because a significant number did not meet the diagnostic criteria for BPD (and vice versa).
In 1992, when first proposing Complex PTSD, Judith Lewis-Herman stated:
Concepts of personality developed in ordinary circumstances are frequently applied to survivors, without an understanding of the deformations of personality which occur under conditions of coercive control.Thus, patients who suffer from the complex sequelae of chronic trauma commonly risk being misdiagnosed as having personality disorders. They may be described as "dependent," "masochistic," or "self−defeating." Earlier concepts of masochism or repetition compulsion might be more use− fully supplanted by the concept of a complex traumatic syndrome.[1]:388
Complex PTSD was considered to be included within "associated features of PTSD" for the DSM-IV under the name Disorders of Extreme Stress Not Otherwise Specified (
), but this was not included in either the DSM-IV or DSM-V.[8]:23
See also: Enduring Personality Change After Catastrophic Experience
ICD 11 draft - Complex Post-traumatic Stress disorder
The ICD-11, which is currently a draft document, includes the diagnosis of Complex Post-traumatic Stress Disorder in the Disorders specifically associated with stress section, immediately after Post-traumatic Stress Disorder.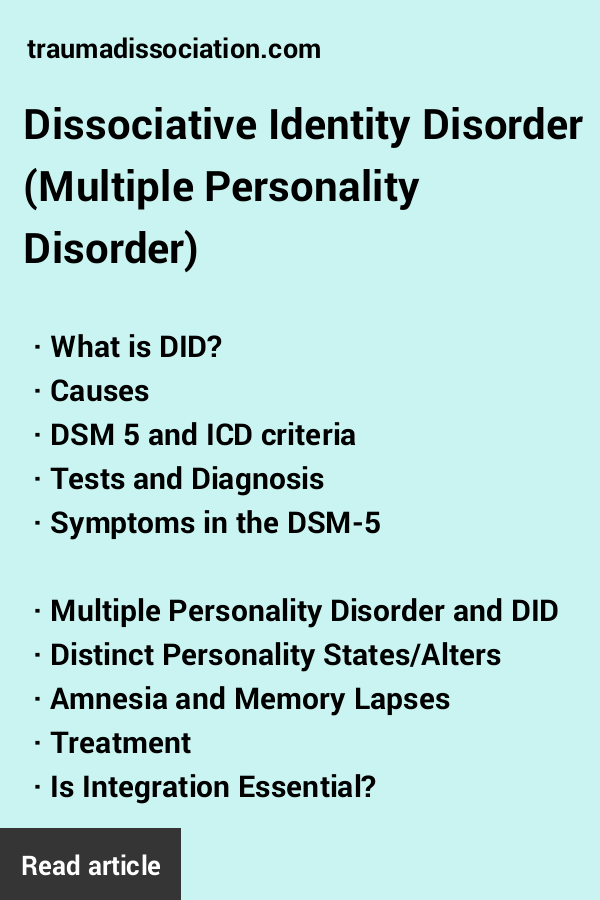 [3]
[3]
Complex Post-traumatic Stress DisorderCode Unknown
Definition
"Complex post-traumatic stress disorder (Complex PTSD) is a disorder that may develop following exposure to an event or series of events of an extreme and prolonged or repetitive nature that is experienced as extremely threatening or horrific and from which escape is difficult or impossible (e.g., torture, slavery, genocide campaigns, prolonged domestic violence, repeated childhood sexual or physical abuse).
The disorder is characterized by the core symptoms of PTSD; that is, all diagnostic requirements for PTSD have been met at some point during the course of the disorder. In addition, complex PTSD is characterized by
- 1) severe and pervasive problems in affect regulation;
- 2) persistent beliefs about oneself as diminished, defeated or worthless, accompanied by deep and pervasive feelings of shame, guilt or failure related to the stressor; and
- 3) persistent difficulties in sustaining relationships and in feeling close to others.
The disturbance causes significant impairment in personal, family, social, educational, occupational or other important areas of functioning."
Synonyms:
- Enduring personality change after catastrophic experience - EPCACE, which is ICD-10 diagnosis F62.0
Narrower Terms:
- Personality change after: concentration camp experiences
- Personality change after: disasters
- Personality change after: prolonged: captivity with an imminent possibility of being killed
- Personality change after: prolonged: exposure to life-threatening situations such as being a victim of terrorism
- Personality change after: torture [3]
Excludes:
- Post-traumatic stress disorder [3]
Lasted updated May 31, 2016. Criteria last updated by WHO on May 29, 2016.
Enduring Personality Change After Catastrophic Experience
The current ICD-10 includes a diagnosis of Enduring Personality Change After Catastrophic Experience (EPCACE) in the Disorders of adult personality and behavior section.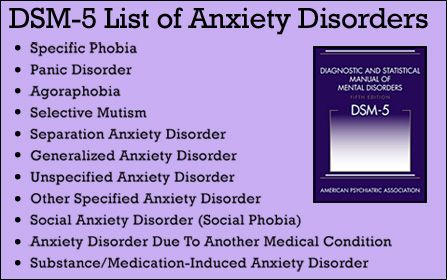 This is regarded as equivalent to Complex PTSD.[3]
This is regarded as equivalent to Complex PTSD.[3]
Code F62.0
"Enduring personality change may follow the experience of catastrophic stress. The stress must be so extreme that it is unnecessary to consider personal vulnerability in order to explain its profound effect on the personality. Examples include concentration camp experiences, torture, disasters, prolonged exposure to life-threatening circumstances (e.g. hostage situations - prolonged captivity with an imminent possibility of being killed). Post-traumatic stress disorder (F43.1) may precede this type of personality change, which may then be seen as a chronic, irreversible sequel of stress disorder. In other instances, however, enduring personality change meeting the description given below may develop without an interim phase of a manifest post-traumatic stress disorder.
However, longterm change in personality following short-term exposure to a lifethreatening experience such as a car accident should not be included in this category, since recent research indicates that such a development depends on a pre-existing psychological vulnerability.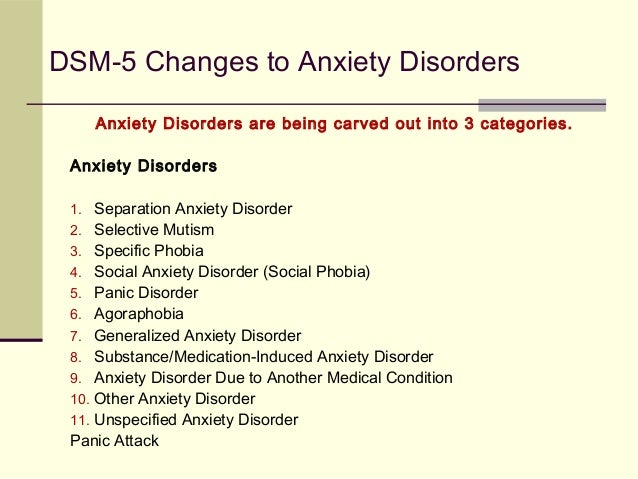 " [2]:163
" [2]:163
ICD-10 Diagnostic guidelines
The personality change should be enduring and manifest as inflexible and maladaptive features leading to an impairment in interpersonal, social, and occupational functioning. Usually the personality change has to be confirmed by a key informant. In order to make the diagnosis, it is essential to establish the presence of features not previously seen, such as:
- a hostile or mistrustful attitude towards the world;
- social withdrawal;
- feelings of emptiness or hopelessness;
- a chronic feeling of being "on edge", as if constantly threatened
- estrangement.
This personality change must have been present for at least 2 years, and should not be attributable to a pre-existing personality disorder or to a mental disorder other than post-traumatic stress disorder (F43.1).
Includes:
- Personality change after concentration camp experiences
- Personality change after disasters,
- Prolonged captivity with an imminent possibility of being killed
- Prolonged exposure to life-threatening situations such as being a victim of terrorism
- Torture
Exclude:
- post-traumatic stress disorder (F43.
 1) [2]:163-164
1) [2]:163-164 - Brain damage or disease which may cause similar clinical features must be ruled out.
Treatment for Complex PTSD
See also Treatment for Complex PTSD
References
1. Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. J Trauma Stress, 5(3), 377–391. doi:10.1007/bf00977235
2. World Health Organization. (1992). The ICD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines. Retrieved December 9, 2014, from http://www.who.int/classifications/icd/en/bluebook.pdf
3. World Health Organization. (May 31, 2016). ICD-11 Beta Draft (Joint Linearization for Mortality and Morbidity Statistics).
4. Cloitre, M., Courtois, C.A., Ford, J.D., Green, B.L., Alexander, P., Briere, J., Herman, J.L., Lanius, R., Stolbach, B.C., Spinazzola, J., Van der Kolk, B.A., Van der Hart, O. (2012).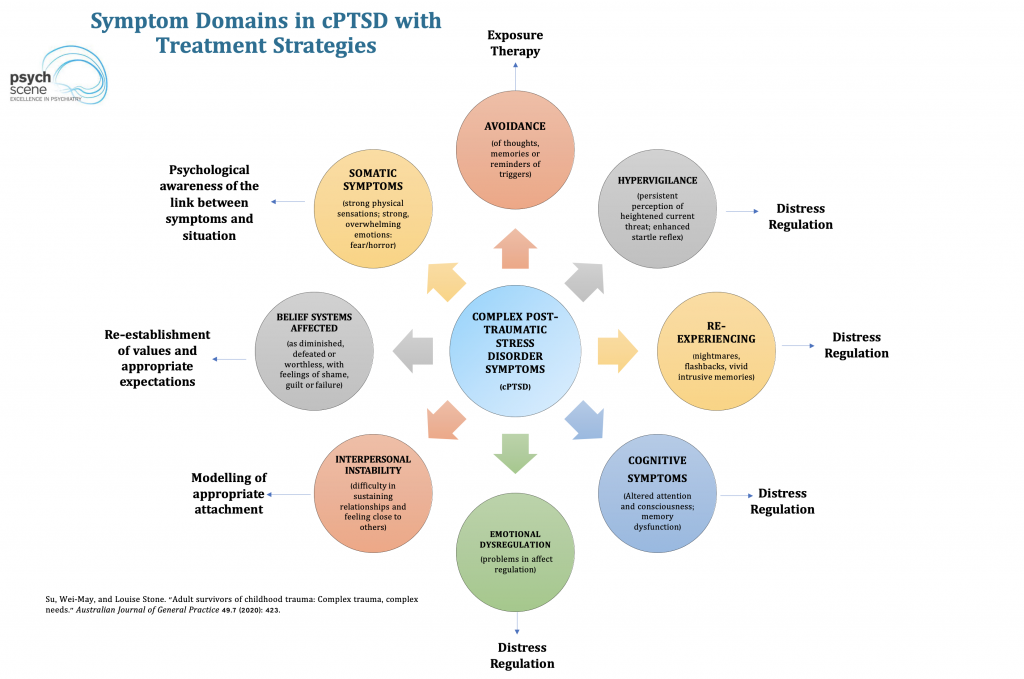 The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults. Retrieved from December 10, 2014 http://www.istss.org/ISTSS_Main/media/Documents/ComplexPTSD.pdf
The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults. Retrieved from December 10, 2014 http://www.istss.org/ISTSS_Main/media/Documents/ComplexPTSD.pdf
5. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. (5th ed.). Washington, D.C.: American Psychiatric Association. ISBN 0890425558.
6. Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. European Journal of Psychotraumatology, 4(0). doi:10.3402/ejpt.v4i0.20706
7. Cloitre, M., Garvert, D. W., Weiss, B., Carlson, E. B., & Bryant, R. A. (2014). Distinguishing PTSD, Complex PTSD, and Borderline Personality Disorder: A latent class analysis. European Journal of Psychotraumatology, 5(0). doi:10.3402/ejpt.v5.25097
8. Williams, M. B., (2002). The PTSD workbook simple, effective techniques for overcoming traumatic stress symptoms.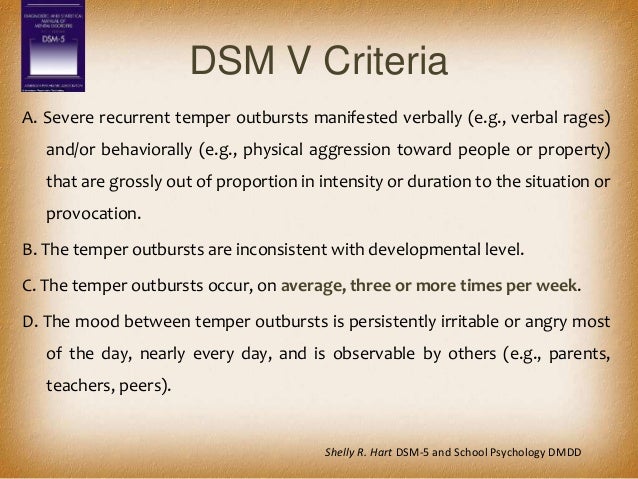 Oakland, Calif.: New Harbinger Publications. ISBN 160882148X.
Oakland, Calif.: New Harbinger Publications. ISBN 160882148X.
Cite this page
Complex Post-traumatic Stress Disorder. Traumadissociation.com. Retrieved from .
This information can be copied or modified for any purpose, including commercially, provided a link back is included. License: CC BY-SA 4.0
Complex Posttraumatic Stress Disorder (C-PTSD) symptoms and diagnostic criteria
What is Complex PTSD?
Complex Posttraumatic Stress Disorder, is the result of multiple traumatic events occurring over a period of time, often referred to as "complex trauma". Causes include multiple incidents of child abuse, particularly child physical abuse and child sexual abuse, prolonged domestic violence, concentration camp experiences, torture, slavery, and genocide campaigns.[3] Complex Post-traumatic Stress Disorder is not a diagnosis in the DSM-5 psychiatric manual, released in 2013,[5] but is planned for inclusion in the ICD-11 diagnostic manual, due for release in 2017. [3]
[3]
Dr Frank Ocher explains the wider impact of Complex PTSD.
Differences between PTSD and Complex PTSD
The diagram shows the additional symptoms present in Complex PTSD, compared to PTSD, and is based on research from 2013. [6]
Complex PTSD Symptoms
- Interpersonal problems includes social and interpersonal avoidance (avoiding relationships), feeling distance or cut off from others, and never feeling close to another person.
- Negative self-concept involves feelings of worthlessness and guilt. While survivors of PTSD may feel "not myself", a survivor of Complex PTSD may feel no sense of self at all or experience a changed personality; a few may feel as if they are no longer human at all (Lovelace and McGrady, 1980; Timerman, 1981).[1]:385-386.
 Believing yourself to be "contaminated, guilty, and evil" is commonly reported by survivors of Complex PTSD. A fragmented identity is common, with Dissociative Identity Disorder occurring in some people. [1]:386
Believing yourself to be "contaminated, guilty, and evil" is commonly reported by survivors of Complex PTSD. A fragmented identity is common, with Dissociative Identity Disorder occurring in some people. [1]:386 - Interpersonal sensitivity includes having feelings which are easily hurt, anger/temper outbursts and difficulties with interpersonal relationships. Complex PTSD is normally the result of interpersonal trauma, the long duration of the trauma and the control of the perpetrator(s) prevents people from expressing anger or rage at the perpetrator(s) during the trauma; anger and rage both at perpetrators and the self can only be fully expressed after the trauma ends. Prolonged abuse normally leads to a loss of previously-held beliefs, with feelings of "being forsaken by both man and God". [1]:382,386
- Affect dysregulation means being unable to manage your own emotions, and is often referred to as "difficulties with emotional regulation".
 The unexpressed anger and internalized rage resulting from the trauma may lead to self-destructive or reckless/risk taking behaviors, e.g., self-harm and/or suicide attempts, which may be driven by a sense of self-hatred. [1]:382, [6]
The unexpressed anger and internalized rage resulting from the trauma may lead to self-destructive or reckless/risk taking behaviors, e.g., self-harm and/or suicide attempts, which may be driven by a sense of self-hatred. [1]:382, [6] - People with Complex PTSD also meet the diagnostic criteria for PTSD, which are:
- a persistent sense of threat, e.g. hypervigilance and being easily startled
- avoiding reminders of the traumas,
- and re-experiencing or reliving the traumas, for example flashbacks and intrusive thoughts about the trauma.
In addition to the symptoms above, survivors of prolonged child abuse have an increased risk of both self-injury and repeated victimization, for example relationships with abusive people, sexual harassment, and rape. [1]:387
Judith Lewis-Herman, who first proposed Complex PTSD as a separate diagnosis, stated:
Observers who have never experienced prolonged terror, and who have no understanding of coercive methods of control, often presume that they would show greater psychological resistance than the victim in similar circumstances.The survivor's difficulties are all too easily attributed to underlying character problems, even when the trauma is known. When the trauma is kept secret, as is frequently the case in sexual and domestic violence, the survivor's symptoms and behavior may appear quite baffling, not only to lay people but also to mental health professionals. The clinical picture of a person who has been reduced to elemental concerns of survival is still frequently mistaken for a portrait of the survivor's underlying character." [1]:388
Complex PTSD, BPD and Personality Disorders
Recent research has produced detailed analysis of the symptoms of Complex PTSD, PTSD and Borderline Personality Disorder (BPD). Many people with BPD either have PTSD, or meet the proposed diagnostic criteria for Complex PTSD. Complex PTSD was shown to be a separate diagnosis from Borderline Personality Disorder because a significant number did not meet the diagnostic criteria for BPD (and vice versa).
In 1992, when first proposing Complex PTSD, Judith Lewis-Herman stated:
Concepts of personality developed in ordinary circumstances are frequently applied to survivors, without an understanding of the deformations of personality which occur under conditions of coercive control.Thus, patients who suffer from the complex sequelae of chronic trauma commonly risk being misdiagnosed as having personality disorders. They may be described as "dependent," "masochistic," or "self−defeating." Earlier concepts of masochism or repetition compulsion might be more use− fully supplanted by the concept of a complex traumatic syndrome.[1]:388
Complex PTSD was considered to be included within "associated features of PTSD" for the DSM-IV under the name Disorders of Extreme Stress Not Otherwise Specified (
), but this was not included in either the DSM-IV or DSM-V.[8]:23
See also: Enduring Personality Change After Catastrophic Experience
ICD 11 draft - Complex Post-traumatic Stress disorder
The ICD-11, which is currently a draft document, includes the diagnosis of Complex Post-traumatic Stress Disorder in the Disorders specifically associated with stress section, immediately after Post-traumatic Stress Disorder.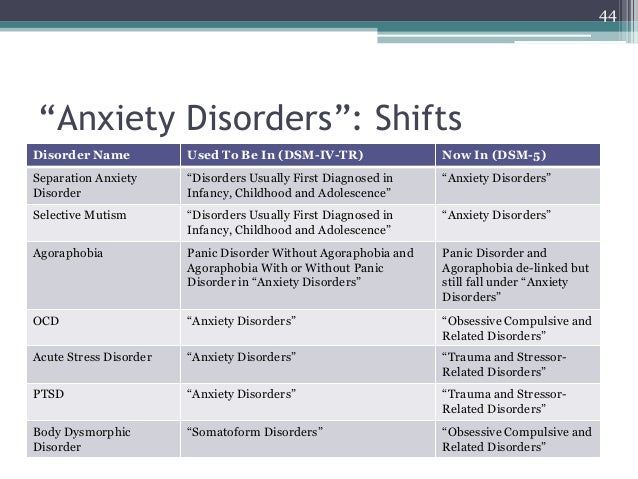 [3]
[3]
Complex Post-traumatic Stress DisorderCode Unknown
Definition
"Complex post-traumatic stress disorder (Complex PTSD) is a disorder that may develop following exposure to an event or series of events of an extreme and prolonged or repetitive nature that is experienced as extremely threatening or horrific and from which escape is difficult or impossible (e.g., torture, slavery, genocide campaigns, prolonged domestic violence, repeated childhood sexual or physical abuse).
The disorder is characterized by the core symptoms of PTSD; that is, all diagnostic requirements for PTSD have been met at some point during the course of the disorder. In addition, complex PTSD is characterized by
- 1) severe and pervasive problems in affect regulation;
- 2) persistent beliefs about oneself as diminished, defeated or worthless, accompanied by deep and pervasive feelings of shame, guilt or failure related to the stressor; and
- 3) persistent difficulties in sustaining relationships and in feeling close to others.
The disturbance causes significant impairment in personal, family, social, educational, occupational or other important areas of functioning."
Synonyms:
- Enduring personality change after catastrophic experience - EPCACE, which is ICD-10 diagnosis F62.0
Narrower Terms:
- Personality change after: concentration camp experiences
- Personality change after: disasters
- Personality change after: prolonged: captivity with an imminent possibility of being killed
- Personality change after: prolonged: exposure to life-threatening situations such as being a victim of terrorism
- Personality change after: torture [3]
Excludes:
- Post-traumatic stress disorder [3]
Lasted updated May 31, 2016. Criteria last updated by WHO on May 29, 2016.
Enduring Personality Change After Catastrophic Experience
The current ICD-10 includes a diagnosis of Enduring Personality Change After Catastrophic Experience (EPCACE) in the Disorders of adult personality and behavior section.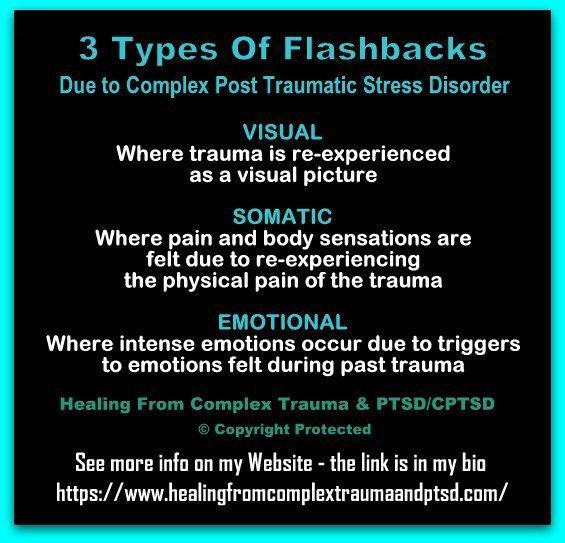 This is regarded as equivalent to Complex PTSD.[3]
This is regarded as equivalent to Complex PTSD.[3]
Code F62.0
"Enduring personality change may follow the experience of catastrophic stress. The stress must be so extreme that it is unnecessary to consider personal vulnerability in order to explain its profound effect on the personality. Examples include concentration camp experiences, torture, disasters, prolonged exposure to life-threatening circumstances (e.g. hostage situations - prolonged captivity with an imminent possibility of being killed). Post-traumatic stress disorder (F43.1) may precede this type of personality change, which may then be seen as a chronic, irreversible sequel of stress disorder. In other instances, however, enduring personality change meeting the description given below may develop without an interim phase of a manifest post-traumatic stress disorder.
However, longterm change in personality following short-term exposure to a lifethreatening experience such as a car accident should not be included in this category, since recent research indicates that such a development depends on a pre-existing psychological vulnerability.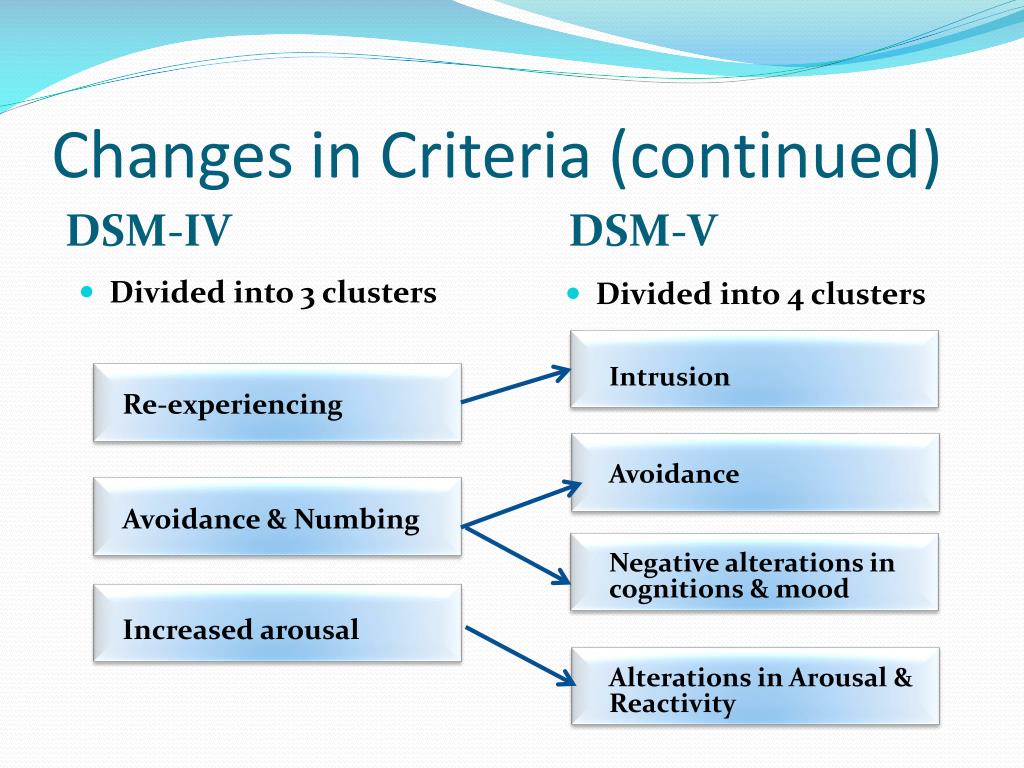 " [2]:163
" [2]:163
ICD-10 Diagnostic guidelines
The personality change should be enduring and manifest as inflexible and maladaptive features leading to an impairment in interpersonal, social, and occupational functioning. Usually the personality change has to be confirmed by a key informant. In order to make the diagnosis, it is essential to establish the presence of features not previously seen, such as:
- a hostile or mistrustful attitude towards the world;
- social withdrawal;
- feelings of emptiness or hopelessness;
- a chronic feeling of being "on edge", as if constantly threatened
- estrangement.
This personality change must have been present for at least 2 years, and should not be attributable to a pre-existing personality disorder or to a mental disorder other than post-traumatic stress disorder (F43.1).
Includes:
- Personality change after concentration camp experiences
- Personality change after disasters,
- Prolonged captivity with an imminent possibility of being killed
- Prolonged exposure to life-threatening situations such as being a victim of terrorism
- Torture
Exclude:
- post-traumatic stress disorder (F43.
 1) [2]:163-164
1) [2]:163-164 - Brain damage or disease which may cause similar clinical features must be ruled out.
Treatment for Complex PTSD
See also Treatment for Complex PTSD
References
1. Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. J Trauma Stress, 5(3), 377–391. doi:10.1007/bf00977235
2. World Health Organization. (1992). The ICD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines. Retrieved December 9, 2014, from http://www.who.int/classifications/icd/en/bluebook.pdf
3. World Health Organization. (May 31, 2016). ICD-11 Beta Draft (Joint Linearization for Mortality and Morbidity Statistics).
4. Cloitre, M., Courtois, C.A., Ford, J.D., Green, B.L., Alexander, P., Briere, J., Herman, J.L., Lanius, R., Stolbach, B.C., Spinazzola, J., Van der Kolk, B.A., Van der Hart, O. (2012).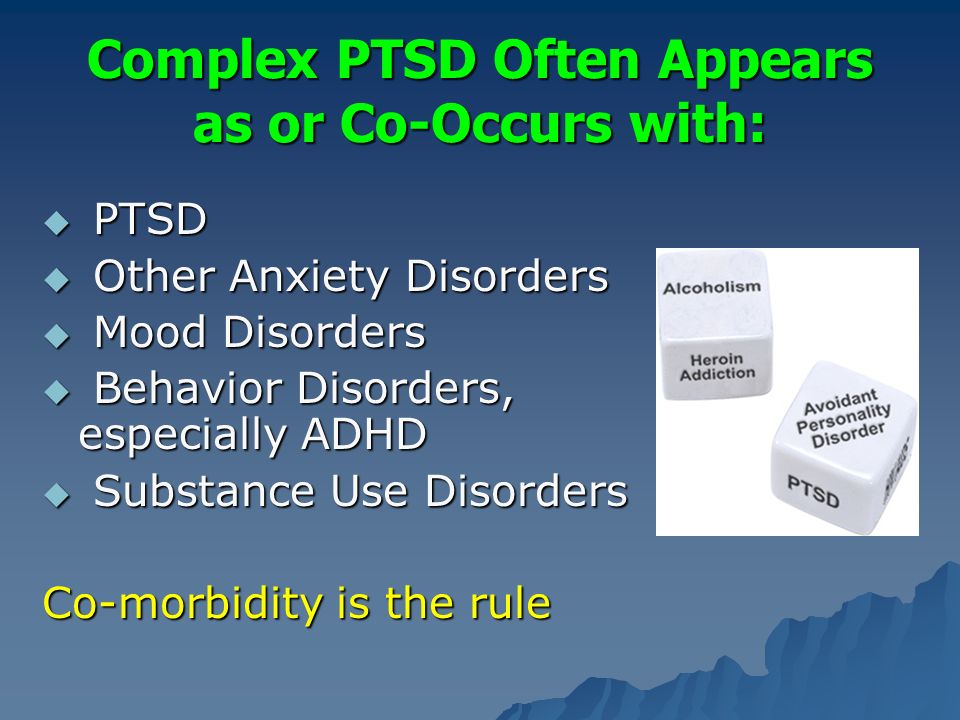 The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults. Retrieved from December 10, 2014 http://www.istss.org/ISTSS_Main/media/Documents/ComplexPTSD.pdf
The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults. Retrieved from December 10, 2014 http://www.istss.org/ISTSS_Main/media/Documents/ComplexPTSD.pdf
5. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. (5th ed.). Washington, D.C.: American Psychiatric Association. ISBN 0890425558.
6. Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. European Journal of Psychotraumatology, 4(0). doi:10.3402/ejpt.v4i0.20706
7. Cloitre, M., Garvert, D. W., Weiss, B., Carlson, E. B., & Bryant, R. A. (2014). Distinguishing PTSD, Complex PTSD, and Borderline Personality Disorder: A latent class analysis. European Journal of Psychotraumatology, 5(0). doi:10.3402/ejpt.v5.25097
8. Williams, M. B., (2002). The PTSD workbook simple, effective techniques for overcoming traumatic stress symptoms.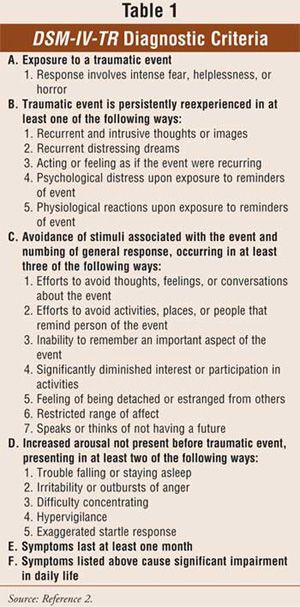 Oakland, Calif.: New Harbinger Publications. ISBN 160882148X.
Oakland, Calif.: New Harbinger Publications. ISBN 160882148X.
Cite this page
Complex Post-traumatic Stress Disorder. Traumadissociation.com. Retrieved from .
This information can be copied or modified for any purpose, including commercially, provided a link back is included. License: CC BY-SA 4.0
PTSD: what is it, symptoms, treatment
Psychological trauma can sit inside us for years and decades, undermining strength and exacerbating pain from time to time. A practicing psychologist talks about the nature of post-traumatic stress disorder and explains what might help to cope with it.
Arkady Volkov, psychotherapist, specialist of the service for the selection of psychologists Alter
Advertising on RBC www.adv.rbc.ru
What is PTSD
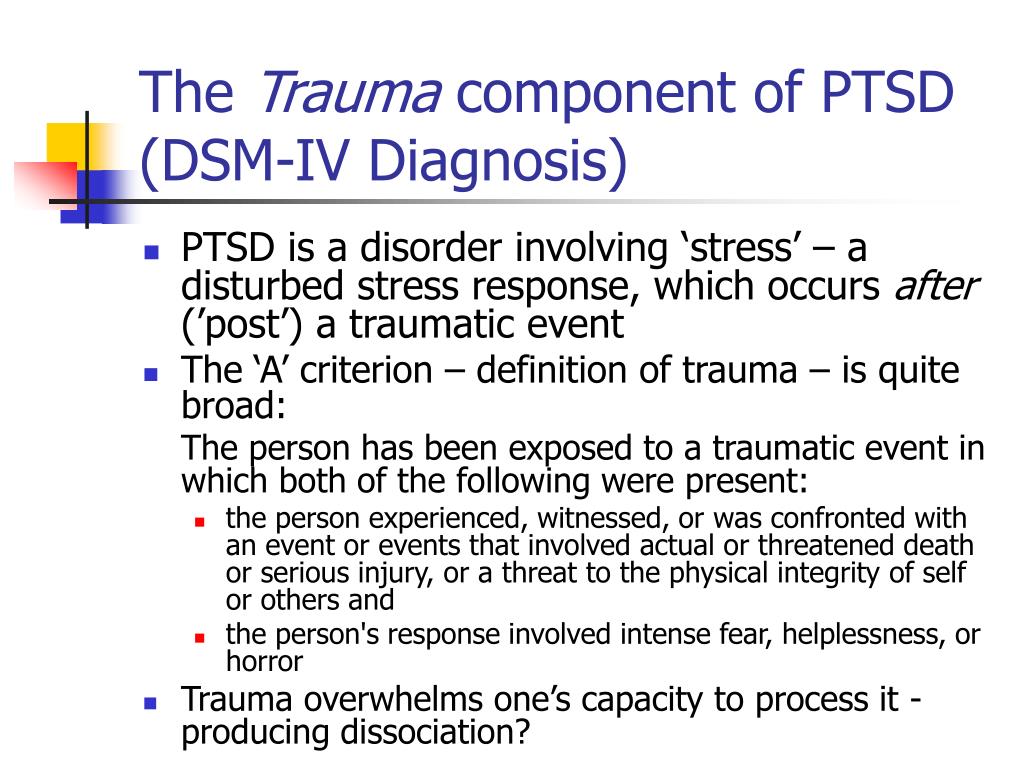
Each person has many mechanisms and resources at his disposal that allow him to live through difficult events, cope with difficulties, endure grief and loss, overcome disappointments and tragedies.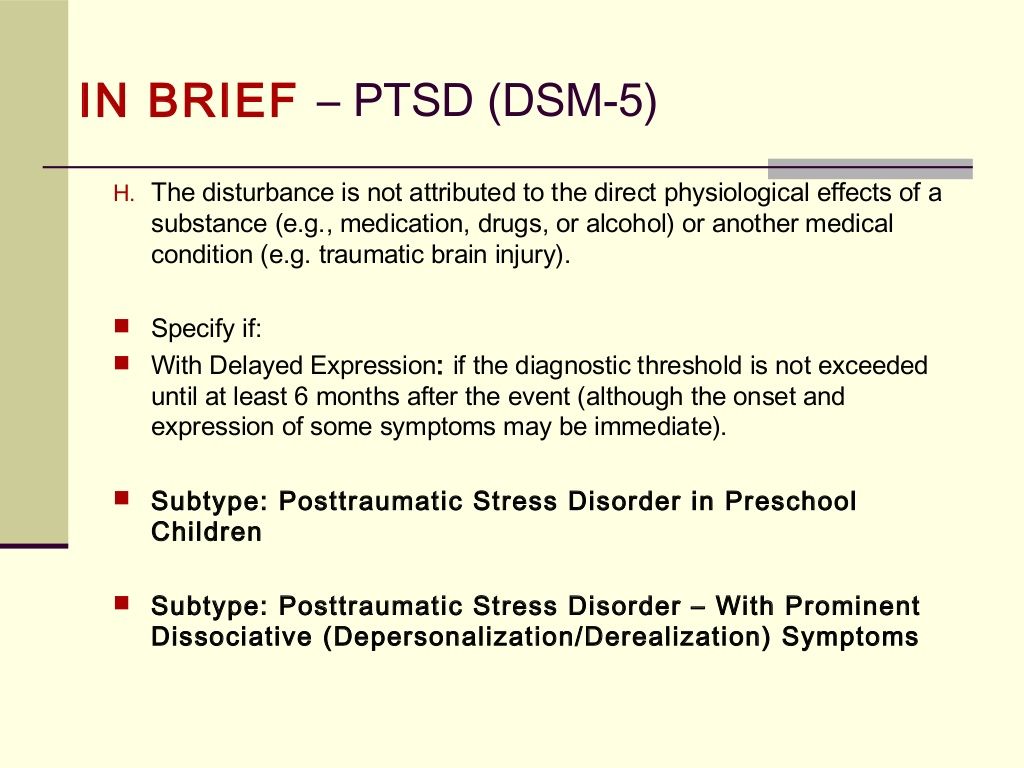 Nevertheless, sometimes we are faced with an event that, for one reason or another, we cannot cope with: it does not fit into our personal experience at all and turns out to be an insurmountable shock. Such events, usually associated with a real or perceived risk to life and health, are usually called traumas, and they can cause post-traumatic stress disorder - a mental disorder as a result of encountering a traumatic situation.
Nevertheless, sometimes we are faced with an event that, for one reason or another, we cannot cope with: it does not fit into our personal experience at all and turns out to be an insurmountable shock. Such events, usually associated with a real or perceived risk to life and health, are usually called traumas, and they can cause post-traumatic stress disorder - a mental disorder as a result of encountering a traumatic situation.
Studies show that almost 4% of people suffer from PTSD at least once during their lives. At the same time, statistics in different countries vary significantly: in China, 0.3% of respondents faced the problem, in the Netherlands — 7.4%, in Canada — 9.2% [1], [2].
Symptoms of PTSD
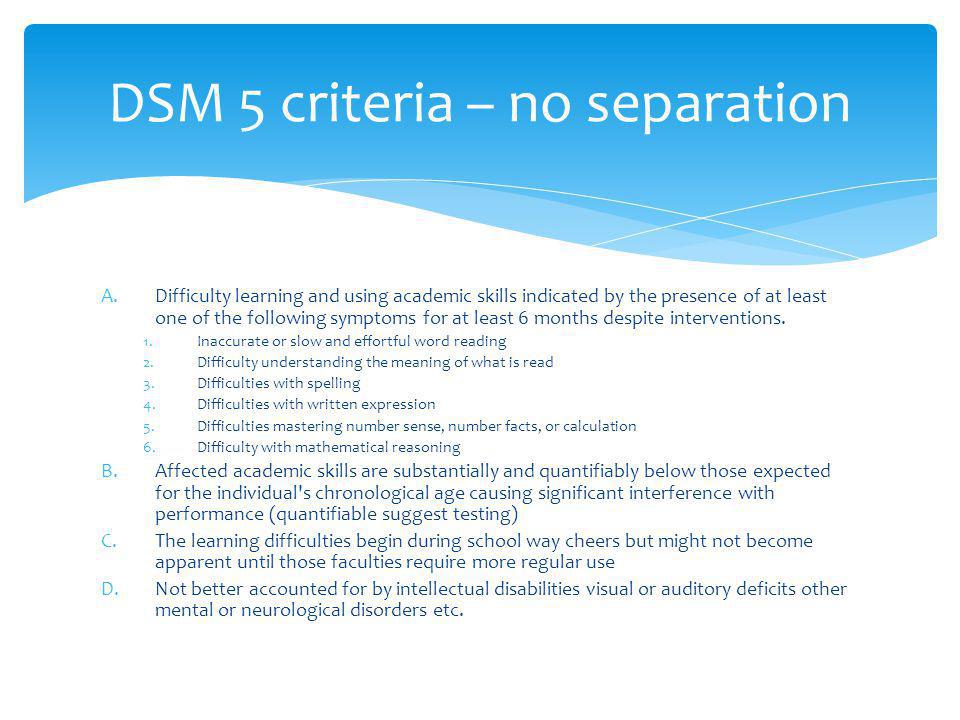
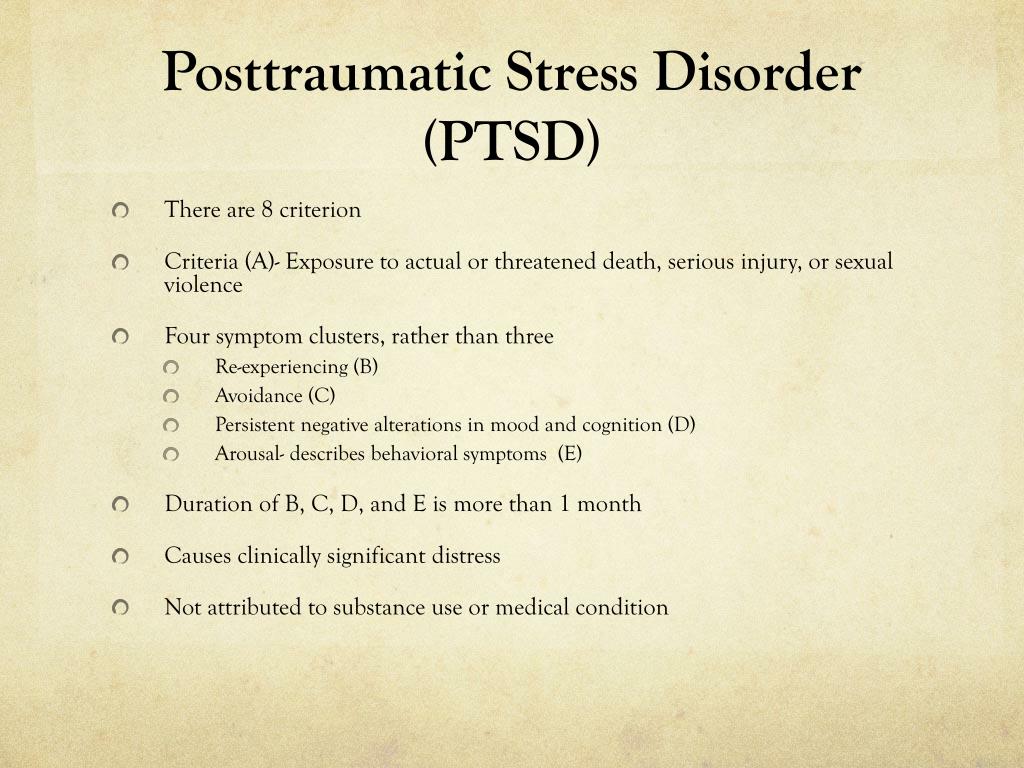
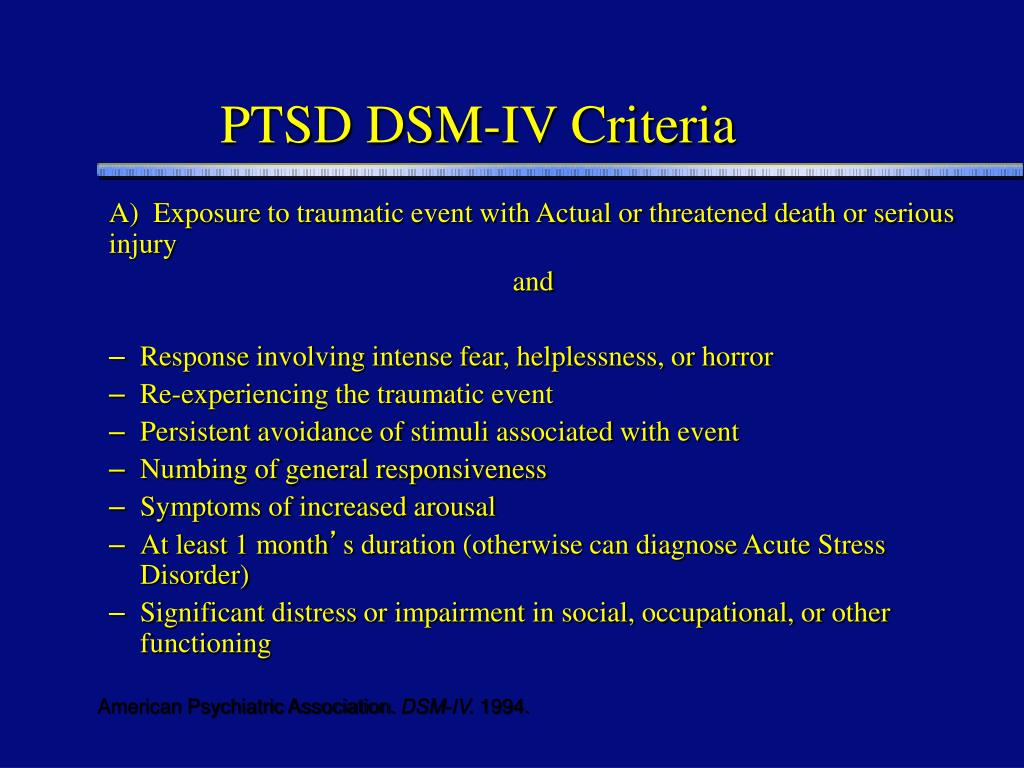
Currently, the two main medical diagnostic guidelines (DSM-5, the American Psychiatric Association's guidelines, and ICD-11, the World Health Organization's classification) state the following criteria to conclude that a person is suffering from PTSD:
- Encounter with a life or health threatening situation.
 At the same time, PTSD can develop in a situation where a person has become a victim of such an event, and if he was a witness to it, or if a similar event happened to his loved ones. This criterion also applies to professionals who, by the nature of their work, are faced with the consequences of traumatic events: doctors, firefighters, crisis psychologists, and so on.
At the same time, PTSD can develop in a situation where a person has become a victim of such an event, and if he was a witness to it, or if a similar event happened to his loved ones. This criterion also applies to professionals who, by the nature of their work, are faced with the consequences of traumatic events: doctors, firefighters, crisis psychologists, and so on.
- Presence of at least one of the symptoms of involuntary intrusive and disturbing memories of the event, nightmares, flashbacks, distressing experiences, or a physical reaction in situations that are reminiscent of the event.
- Avoidance of memories and thoughts about the event or anything that might remind of it.
- Disturbances in thinking and emotional state due to the experienced event: inability to remember important aspects of what happened, negative thoughts and beliefs about oneself and the world around, blaming oneself or others that the traumatic event occurred, lowered mood and negative emotions, decreased interest in the world around , feelings of isolation and alienation, reduced ability to experience positive emotions.
- Changes such as irritability and outbursts of anger, aggressive and dangerous behavior to self or others, increased alertness, startle response to minor stimuli, problems concentrating and sleeping.
To be diagnosed, the listed symptoms must last more than one month and cause significant distress or social difficulties.
© shutterstock
It is important to note that PTSD is often accompanied by other disorders, primarily depressive ones.
Diagnosis of PTSD, like any other mental disorder, can only be diagnosed by a qualified specialist, but yes to the following questions may be a reason to seek advice and get help (or just be more attentive to yourself or a loved one).
- Have you experienced or witnessed any traumatic event in your life (such as an accident, fire, extreme disaster, physical attack on you or your loved ones)?
During the last month:
- Did you return to this event in your thoughts (not wanting it) or dreams?
- Did you make an effort not to think about this event and avoid being reminded of it?
- Were you more tense than usual?
- Have you ever been frightened for minor reasons?
- Did you feel alienated from your usual activities and loved ones?
- Did you feel guilty or blame yourself or others for the event?
Causes and risk factors
There is still no definite answer to the question of what exactly causes PTSD.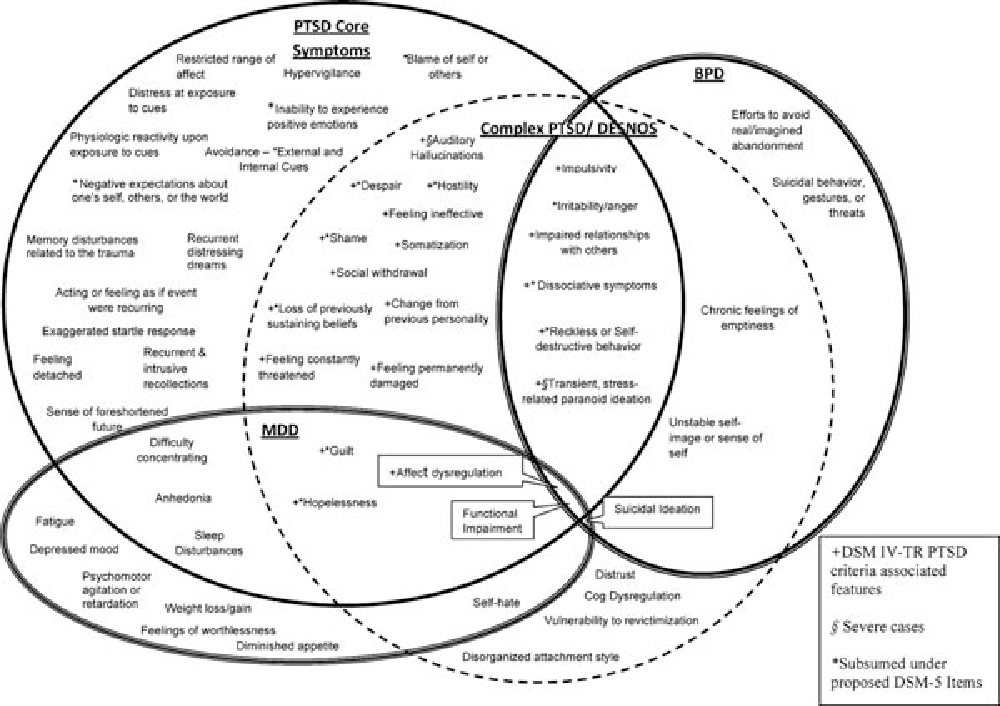 But research has led to some important assumptions.
But research has led to some important assumptions.
At the physiological level, the development of PTSD can be triggered by:
Increased levels of stress hormones
In case of danger, our body produces stress hormones, such as adrenaline, in order to switch into an active mode and somehow escape from the threat (this reaction is often called "fight or flight"). PTSD victims continue to produce large amounts of stress hormones even when the danger is no longer around. This can cause hyperarousal and emotional changes, and can also cause long-term negative health effects, including migraines, pain, and an increased risk of heart, lung, and digestive problems.
Changes in brain function
Trauma-induced stress can damage the hippocampus, the part of the brain involved in emotion and memory.
Disorders in the hippocampus can interfere with the proper processing of memories and dreams, so the anxiety they cause does not decrease over time.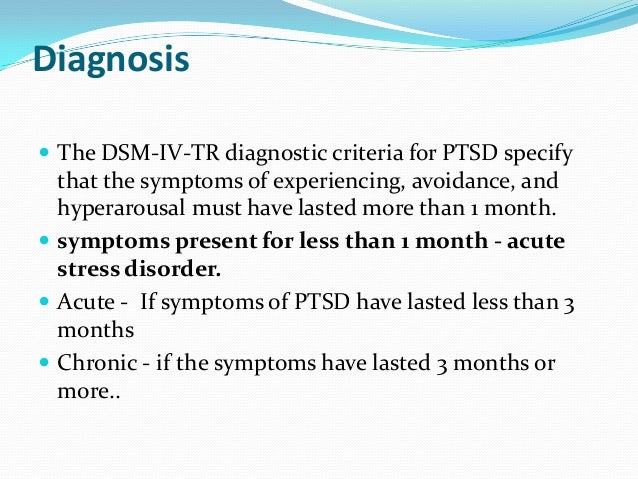 Such changes may explain the increased levels of fear and anxiety, memory and recall problems suffered by PTSD victims.
Such changes may explain the increased levels of fear and anxiety, memory and recall problems suffered by PTSD victims.
© shutterstock
Factors that can increase susceptibility to PTSD:
- Previous traumatic experiences. The stress of a trauma can have a cumulative effect, and a new traumatic experience can exacerbate the negative effects of a previous trauma.
- Experience of violence. People with a history of physical, emotional or sexual abuse tend to be more susceptible to post-traumatic stress.
- PTSD or depression in loved ones.
- Substance use experience.
- Lack of skills to cope with traumatic situations.
- Lack of social support. Good social and family relationships help mitigate the effects of stress and trauma. Conversely, people who lack supportive relationships and environments tend to be more vulnerable to stress and therefore more at risk for PTSD. Being in a social environment that cultivates shame, guilt, stigma, or self-hatred also contributes to the development of post-traumatic stress disorder.
- High level of stress in everyday life.
Treatment of PTSD
Approaches to the treatment of PTSD can be divided into two groups: medication and psychotherapy. Often methods of both groups are used in different combinations.
There are currently no medications specifically designed to treat PTSD, but there are many medications that work well for other conditions, such as depression and anxiety disorders, and have been shown to be effective in treating the symptoms of PTSD.
When it comes to psychotherapeutic methods, or "healing with a word", there are several approaches that demonstrate the greatest (and research-supported) effectiveness.
Cognitive Process Therapy
In this approach, the therapist invites the client to talk about the traumatic event and its aftermath and describe the experience in detail in a diary, which allows them to better see how the trauma is reflected in thoughts and find new ways to deal with it [3 ].
© shutterstock
EMDR - Eye Movement Desensitization and Processing
This approach is based on the notion that trauma disrupts the natural coping mechanisms inherent in each person and cannot be built into their experience and memory. The person is asked to focus on an external stimulus (eye movements from side to side directed by the therapist) and in parallel work through complex memories, thoughts and emotions associated with the trauma [4].
Body and creativity oriented approaches
Body Oriented Therapy aims to find resources through attention to bodily sensations, as well as gaining the opportunity to relive the traumatic experience from the position of an active actor, not a victim. Similar goals are set by approaches that use dance and participation in theatrical productions to gain the freedom and spontaneity that PTSD often deprives its victims of [5].
Living with PTSD
Trauma has a huge impact on many areas of our lives, but this does not mean that the problem cannot be solved, even if for one reason or another you do not have access to professional help.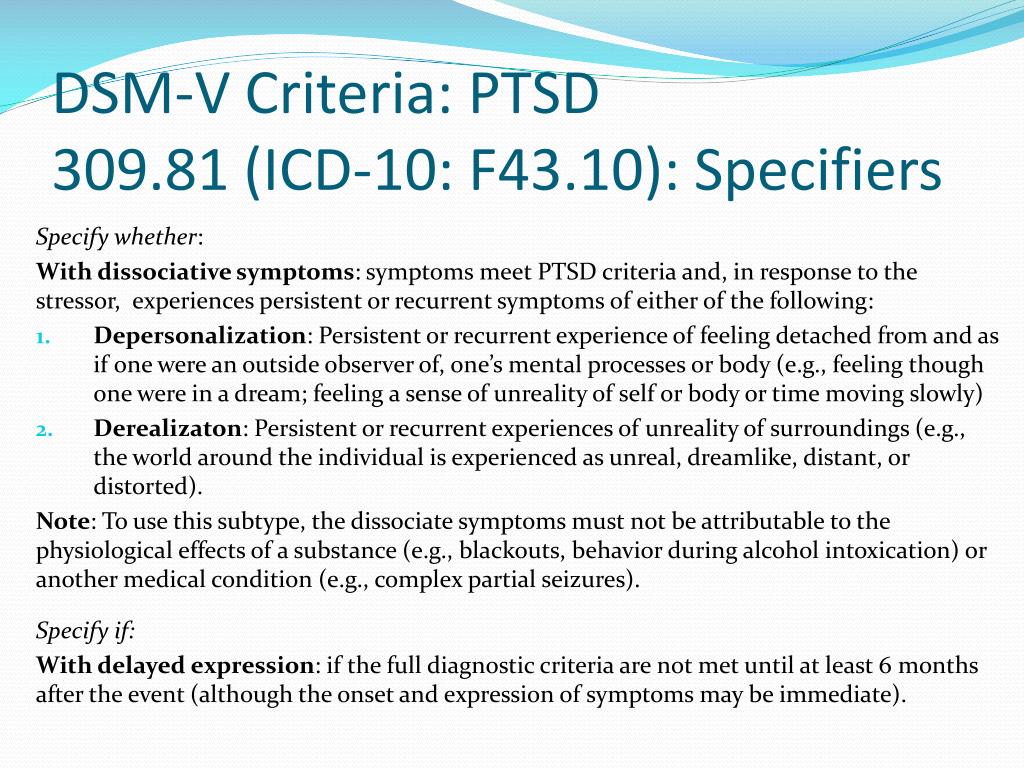
Of particular difficulty in working with PTSD is the very pain and severity of the traumatic experience, which often makes it necessary to avoid any reminders of the trauma, excluding the possibility of talking about it, as well as the devastating consequences for the view of oneself and the world around. All this makes it extremely difficult to build close relationships, seek support and help.
What can help you cope with PTSD
The very first and most important step is often the recognition of the traumatic experience, which opens up opportunities for conversation and subsequent rethinking. The devastating effect of trauma on the psyche is largely due to the fact that the traumatic event is completely knocked out of the normal course of our life, and it is extremely important to return, build it into our personal history.
Research demonstrates the high effectiveness of such a simple tool as writing about your experience: writing down your thoughts and memories of a traumatic event, trying to talk about the impact it had on your life, thoughts about the future.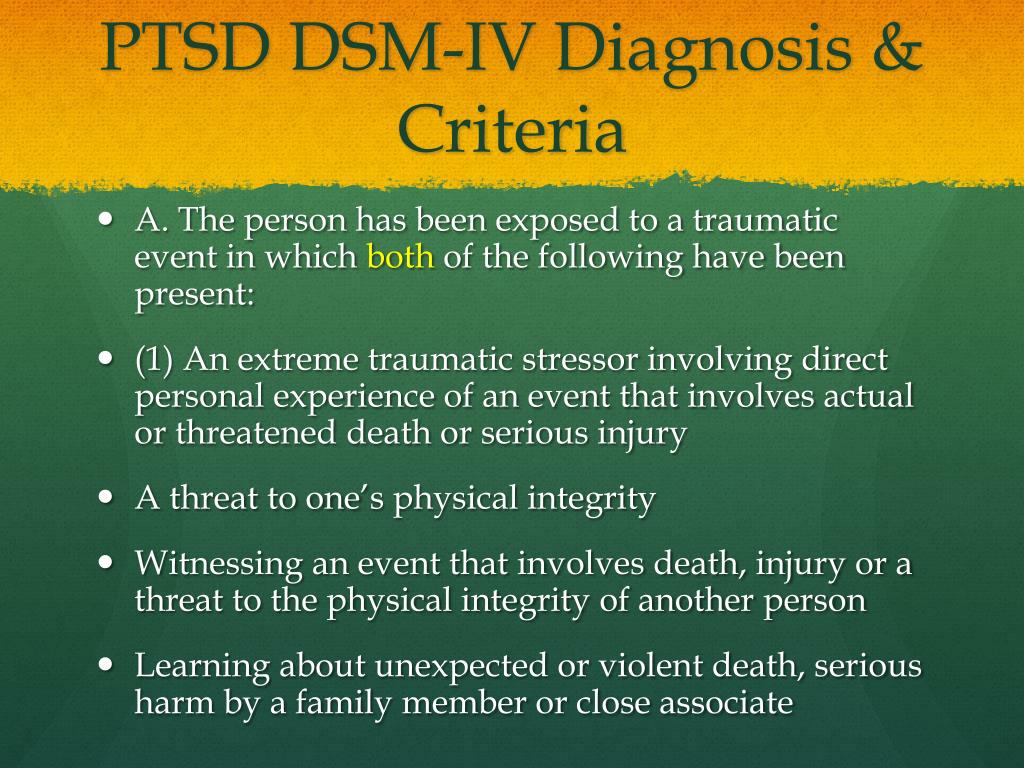
Since trauma affects the body in one way or another, physical exercise, yoga (or regular stretching), meditation, dancing, and even theater classes can be an important help in overcoming its consequences [6].
The support of relatives and friends plays a huge role. It's important to open yourself up and find someone you can talk to about what's bothering you.
However, overcoming PTSD on your own is not easy and can take a long time. Therefore, at the first opportunity, it is worth contacting a psychotherapist.
If your loved one has PTSD
If you notice symptoms of PTSD in a loved one, you can become a support for him and help him. At the same time, it is important to take into account that it can be extremely difficult for him to talk about the trauma and even return to it in his thoughts, so it is important to indicate your willingness to help and be there without exerting any pressure. Your very understanding and supportive presence, your willingness to share activities that bring joy and pleasure, a sense of stability and confidence can be beneficial.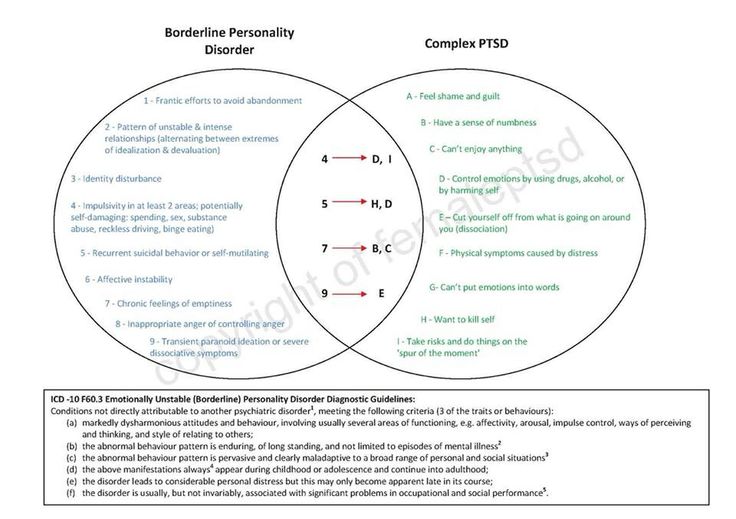 At the same time, you should learn more about both PTSD in general and about the features of its manifestation in your loved one (including triggers - situations, words or objects that can provoke memories of a traumatic experience).
At the same time, you should learn more about both PTSD in general and about the features of its manifestation in your loved one (including triggers - situations, words or objects that can provoke memories of a traumatic experience).
Books about PTSD
Tags: psychology
PTSD: SYMPTOMS AND DIAGNOSIS - Bizzfully
PTSD / CPTSD
Yanina Breidak 15/07/2020
I continue to talk about psychological trauma and this time I want to talk about mental disorders that are directly related to trauma, PTSD and CPTSD, their symptoms and diagnosis.
That is: there was a terrible, difficult event, the human psyche was not able to fully cope with this experience and digest it, and the person developed a certain disorder, which is not very comfortable to live with and which requires a certain correction.
Until recently, the main disorder associated with severe trauma was post-traumatic stress disorder, or PTSD.
This term appeared in the 70s of the last century and initially PTSD was more associated with people who survived military operations or disasters. For example, studies are still very common PTSD in people who served in the Vietnam War.
Let's see what criteria a person can be diagnosed with PTSD based on.
PTSD: ICD-10 symptoms
If we look at the ICD, then in the ICD-10 we will see such criteria.
A person with PTSD will have:
- intrusive memories (the so-called “flashbacks” - this is when shocking memories from the past invade the consciousness of a person and it seems to him that these terrible events are happening right now. That is, a person as if re-immersed in a stressful situation and cannot drive away and stop this memory in any way)
- a person may have obsessive thoughts of a negative nature, nightmares and insomnia
- a person may often fall into a state of numbness, emotional retardation and seem to be disconnected from the outside world and from all other people
- a person may specifically avoid any situations that even remotely remind him of a shock event
- also a person usually has hypervigilance and overcaution .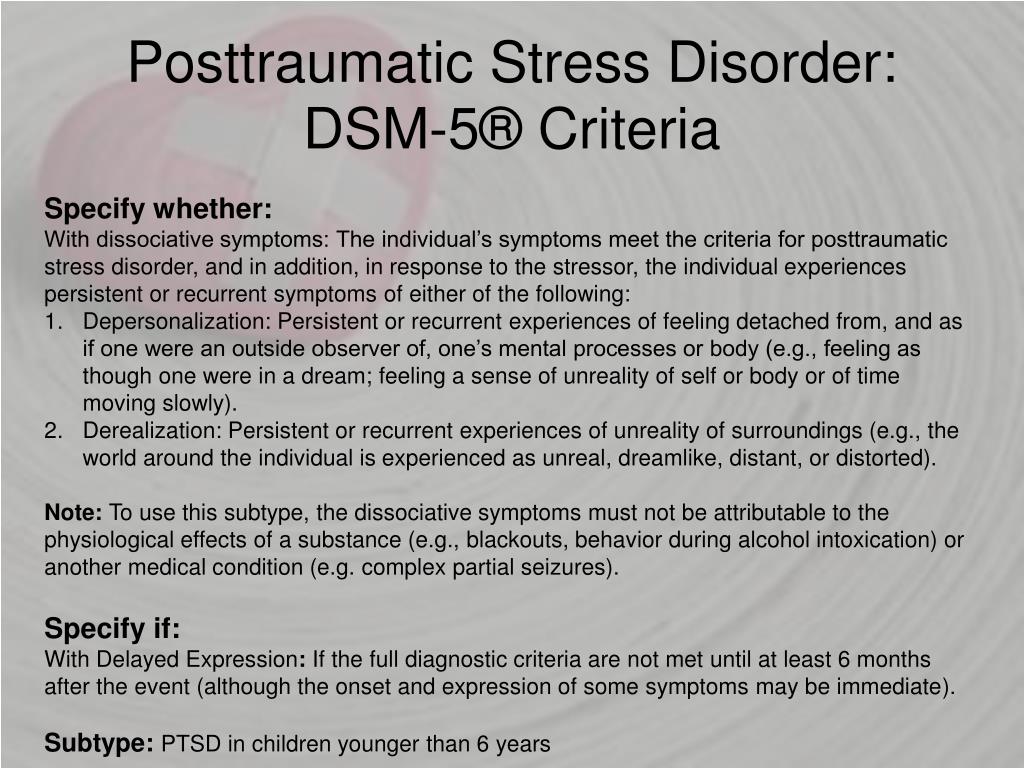 This is a person who never relaxes, but scans space all the time in search of danger
This is a person who never relaxes, but scans space all the time in search of danger
- a common symptom is also an increased reaction to any stress
- people with PTSD often have all anxiety and depressive symptoms
B ICD-10 this diagnosis and symptoms are described under number F43.1. And the ICD considers that PTSD appears as a reaction to a stressful event of a threatening nature. And the stressful event can be single or continuous.
PTSD: DSM-5 symptoms
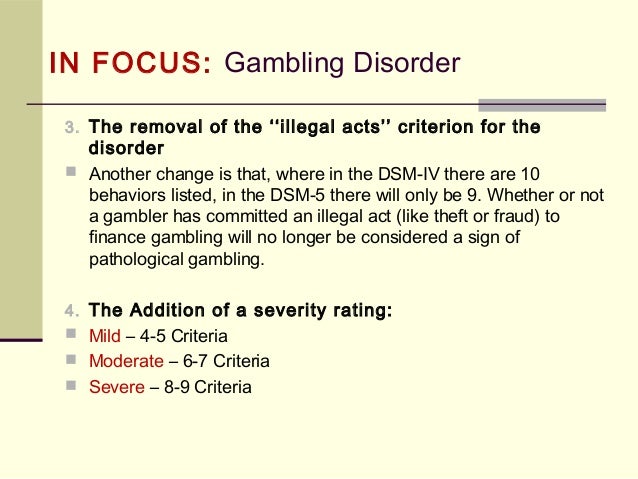
What does the American classification, DSM-5, tell us?
In the DSM-5, PTSD is numbered 309.81. And this is how it is described there.
DSM-5 says that PTSD can occur as a result of an extreme stressful event: when a person's life was threatened, when a person was seriously injured, or when a person was sexually assaulted. PTSD can also develop, if a person witnessed these shocking events - that is, he was not in danger himself, but he witnessed how other people suffered.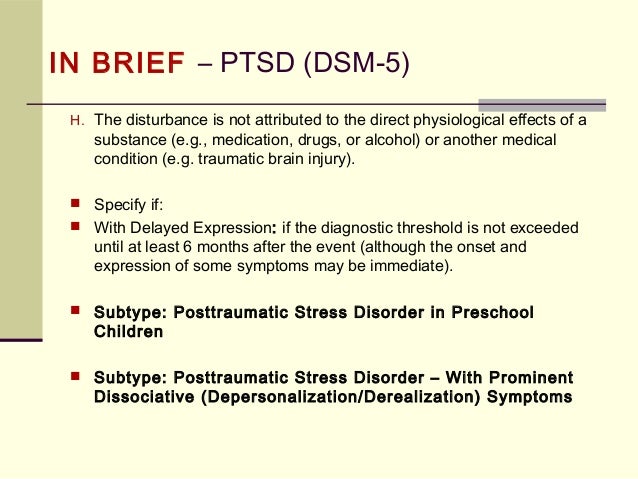 This can also lead to PTSD.
This can also lead to PTSD.
And here are the DSM-5 symptoms of PTSD:
persistent invading memories of stressful events
are nightmares about stressful events and there are not just memories that I perceive as memories, but these are precisely memory + active experience of this memory as if a stressful event is happening right now)
is avoiding situations that resemble a traumatic event
- a change in thinking and mood in a negative direction the bad thing is that no one can be trusted, it's the inability to experience any positive emotions, it can be memory loss associated with stressful events, and it can be such a general feeling of alienation from other people
- disorder of bodily regulation, i.e. - overreaction to some triggers that resemble a traumatic situation, and the inability of a person to regulate himself: he may suddenly become angry, or suddenly freeze, or he may have problems with concentration
– a person with PTSD will also have serious problems with social and professional life
And in order to make a diagnosis of PTSD according to this classification, it is necessary that this condition lasted longer than 1 month.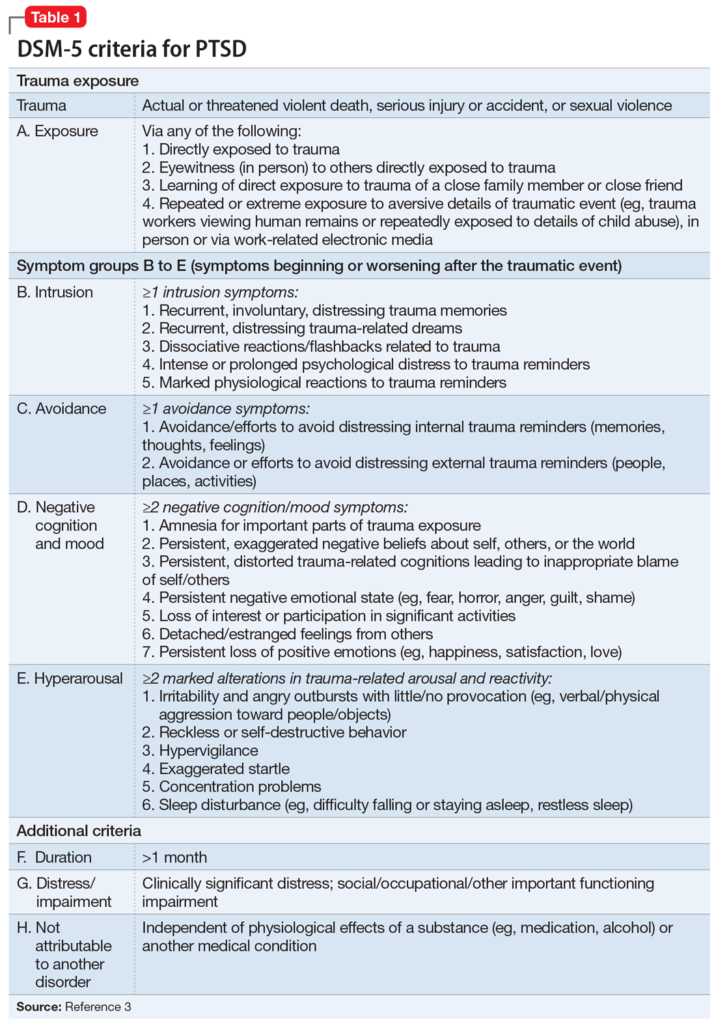
As we can see, the ICD and DSM criteria are very similar in terms of post-traumatic stress disorder.
And we understand that PTSD is a fairly complex disorder that includes both cognitive impairment and bodily impairment. That is, there is dysregulation both at the level of thoughts and at the level of our biological reactions: the work of memory, the work of various organs, hormones, and so on are disrupted.
Understandable with PTSD. What then is complex PTSD (CPTSD)?
Complex PTSD (CPTSD)
Complex PTSD (complex post-traumatic stress disorder) is a relatively new category that refers to prolonged or chronic trauma. And speaking of CPTSD, we mean interpersonal trauma, that is, trauma that was received in a relationship. And most often it means the relationship of children and their parents, or the relationship of children and other adults who raised them.
If a person grew up in a dysfunctional family, if everything was very, very bad with adults, if the child was subjected to physical, sexual and psychological abuse for a long time, then we can say that this person will have complex post-traumatic stress disorder.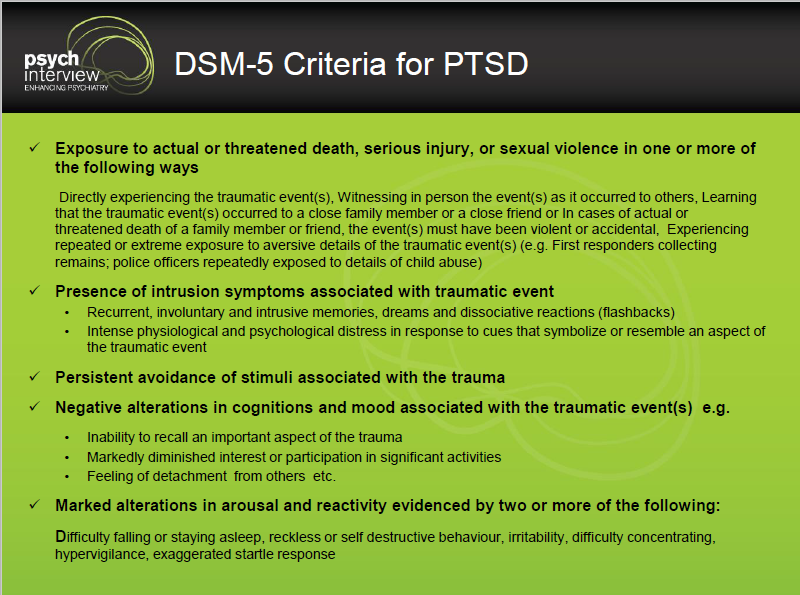
And there is one small problem with CPTSD. Many trauma researchers have long understood that such a diagnosis is needed because it occurs so often and in many people, but it was very difficult to push this idea to the masses. And the ICD and DSM classifications didn’t really want to include this category in their lists.
At the moment the situation is as follows:
– there is no diagnosis of “complex PTSD” in DSM-5. The DSM-5 only has the diagnosis of PTSD, which I talked about earlier.
- in ICD-10, which is still relevant, there is also no such diagnosis, but such a diagnosis will be in ICD-11, which is about to come into force.
And of course you can ask, what is the difference between PTSD and CPTSD? Why separate them at all? And why introduce some new category?
As it becomes clear from a detailed study of this topic, Sometimes the distinction between PTSD and CPTSD can be very important.
Because classically simple PTSD is not usually perceived as an attachment disorder, and the root of CPTSD is precisely an attachment disorder, it is a violation of trust in the world and other people.