Can toddlers have ocd
Can Toddlers Develop OCD? - Unique Mindcare
Although we often think of obsessive-compulsive disorder (OCD) as an illness that affects mostly adults, between 1 and 3% of children will develop OCD. The average age of onset is approximately 10 years of age, although children as young as 5 or 6 may be diagnosed with the illness. Though children can start showing symptoms of OCD around age 3, it is extremely rare.
Why It May Seem Like Your Toddler Has OCD
Many toddlers like to sort objects by color, shape, size or texture. At this age, they are growing and changing rapidly and engaging in this sort of behavior can help them make sense of their limited world. It also shows cognitive development as they learn to make distinctions between characteristics and group items by their similarity. This stage of development is very normal and positive.
You’ll know this behavior is problematic if it begins to impact your toddler negatively. Sorting and organizing should be a positive part of play, so if it becomes an obsession and/or something your toddler begins to rely on to stop her fear or anxiety, and most especially if it’s affecting her normal activities, it’s time to get help.
Toddlers with OCD are sticklers for rules and order and need certain steps to be followed in a certain way. They may become very upset if a step is skipped or something is out of order and they likely seem very anxious a lot of the time.
Tips for Coping as a Parent of a Child With OCD
While there is no doubt that parenting children with OCD can be a challenge, there are ways to cope. Getting informed about OCD, particularly as it is experienced by children, is the essential first step that every parent of a child with OCD should undertake to become an effective advocate for their child.
Some key facts:
- Children with OCD often have less insight into their obsessions than adults and may not yet have the capacity to understand the irrational nature of their thoughts.
- The content of a child’s obsessions can be different from that of adults. For example, it is not uncommon for children with OCD to have specific obsessions related to the death of their parents.
 The rituals or compulsions of children also may be more likely to involve or be centered around family members.
The rituals or compulsions of children also may be more likely to involve or be centered around family members. - In most cases, the current recommended treatment for childhood-onset OCD is a combination of individual or group cognitive-behavior therapy (CBT), and when severe enough, medications that augment levels of the neurochemical serotonin such as selective serotonin reuptake inhibitors (SSRIs). SSRIs are used cautiously in children and adolescents as there has been some suggestion that they may increase the risk for suicide in this age group.
- About one-quarter of children with OCD have the PANDAS or autoimmune subtype. The PANDAS form of OCD has a few key characteristics, such as rapid onset of symptoms, that helps doctors distinguish it from more typical forms of childhood OCD. The PANDAS form of OCD may entail some differences in treatment, too.
Learning more about your child’s OCD will help to reduce your own stress levels and make it easier to carry through with at-home exposure exercises.
Why It Is Important to Get Involved With Your Child’s OCD Treatment
Research suggests that parental involvement is a strong predictor of cognitive-behavioral treatment success. Given the developmental cognitive limitations of children, the explanation of abstract concepts needs to be done in a way that is appropriate for the age of the child. Parents can be an invaluable resource in helping the therapist to develop ways of presenting material that will resonate with and make sense to the child.
On a day-to-day basis, parents can help remind young children that it is their OCD that is the “bad guy” who is responsible for their symptoms, and they and their parents and family are the “good guys.” Such a technique can help reduce the chances a child will feel blame or shame for having OCD.
Above all, work on fostering a strong partnership with the various professionals involved in your child’s care. Don’t be afraid to ask questions and ask about resources that you can take home to better absorb new information in small bits.
How to Engage Your Partner and/or Family
Each of us has different comfort levels when dealing with the emotional difficulties of others, even when it concerns our own family or children. If you are having trouble engaging your partner in becoming educated about your child’s OCD or helping out with at-home exposure exercises, talk about it, don’t sweep it under the rug. Often a partner’s reluctance to help out simply reflects their own anxiety about the situation and does not mean they don’t want to help the child.
If you are the single parent of a child with OCD, look into available resources within your community. A good starting point can be a support group where people share tips for coping with a child who has OCD.
In addition to your partner, the rest of the family must be involved and aware of what treatment entails, especially exposure and response prevention therapy (ERP). It is not unusual for both adults and children with OCD to ask others to participate in their compulsions and family members often oblige so as to reduce their loved one’s anxiety, especially when it is a child.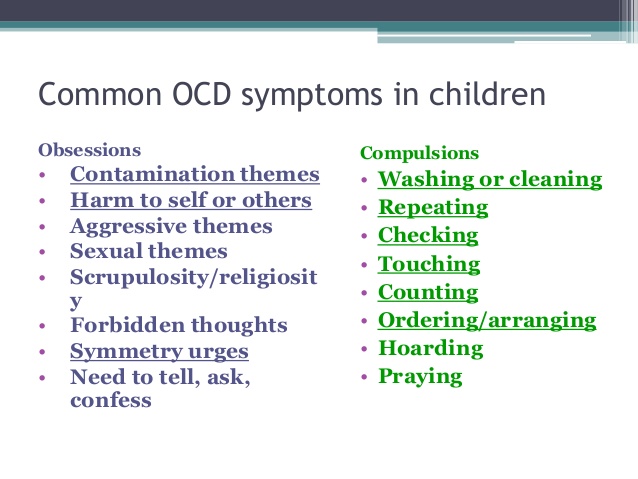 For treatment to work, compulsions need to stop and family members must be aware of this.
For treatment to work, compulsions need to stop and family members must be aware of this.
Don’t Give Up Hope
Finally, it is important to never give up hope. There are many different treatments available and if the first strategy doesn’t work there are often many other options available.
Sometimes it is simply a matter of finding the right therapist or the right combination of medication and psychotherapy. With the right treatment, many children are able to find relief from their symptoms.
Source
Obsessive-Compulsive Disorder (OCD) in Children
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is obsessive-compulsive disorder in children?
Obsessive-compulsive disorder (OCD) is a type of anxiety disorder. Obsessions are recurring thoughts. Compulsions are recurring behaviors.
A child with OCD has obsessive thoughts that are not wanted. They are linked to fears, such as touching dirty objects. He or she uses compulsive rituals to control the fears, such as excessive handwashing.
They are linked to fears, such as touching dirty objects. He or she uses compulsive rituals to control the fears, such as excessive handwashing.
As children grow, rituals and obsessive thoughts normally happen with a purpose and focus based on age. Preschool children often have rituals and routines around meals, bathing, and bedtime. These help stabilize their expectations and view of their world. School-aged children often create group rituals as they learn to play games, take part in team sports, and recite rhymes. Older children and teens start to collect objects and have hobbies. These rituals help children to socialize and learn to deal with anxiety.
When a child has OCD, obsessive thoughts and compulsive rituals can become very frequent and strong. They may interfere with daily living and normal development. OCD is more common in teens.
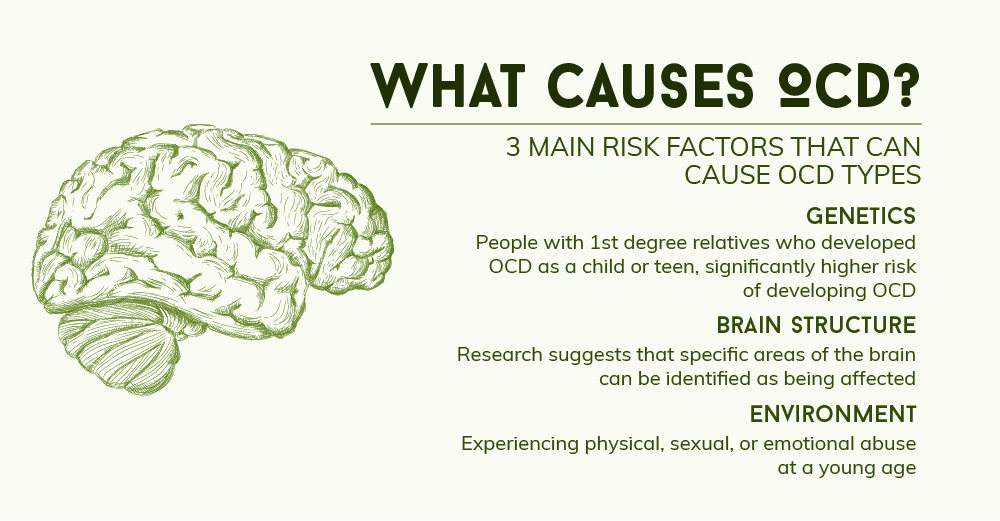
What causes OCD in a child?
The cause of OCD is not known. Research suggests it’s a brain problem. People with OCD don’t have enough of a chemical called serotonin in their brain.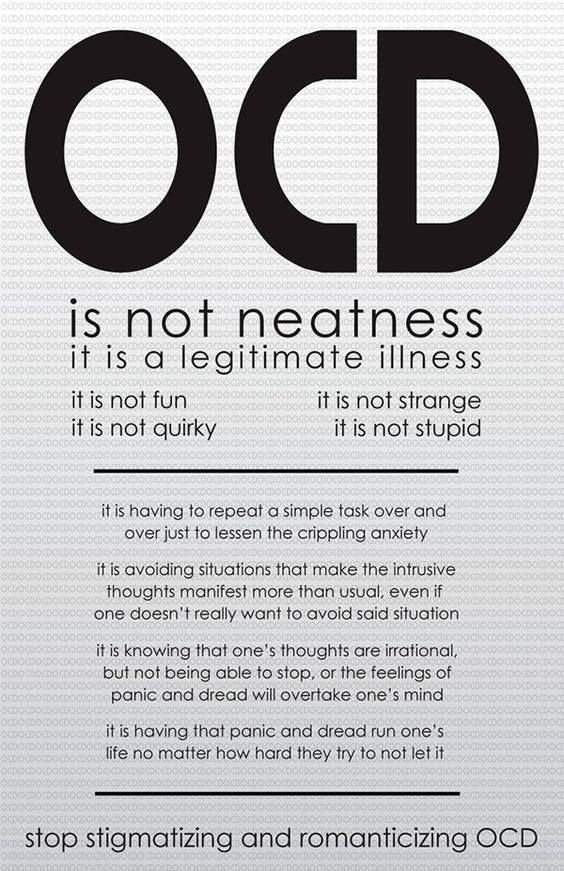
OCD tends to run in families. So it may be genetic. But it may also occur without a family history of OCD. In some cases, streptococcal infections may trigger OCD or make it worse.
What are the symptoms of OCD in a child?
Each child may have different symptoms. These are the most common symptoms:
- An extreme obsession with dirt or germs
- Repeated doubts, such as whether or not the door is locked
- Interfering thoughts about violence, hurting or killing someone, or harming oneself
- Long periods of time spent touching things, counting, and thinking about numbers and sequences
- Preoccupation with order, symmetry, or exactness
- Ongoing thoughts about doing offensive sexual acts or forbidden, taboo behaviors
- Troubled by thoughts that are against personal religious beliefs
- A great need to know or remember things that may be very minor
- Too much attention to detail
- Too much worrying about something bad occurring
- Aggressive thoughts, urges, or behaviors
Compulsive behaviors are the repetitive rituals used to ease anxiety caused by the obsessions. They can be excessive, disruptive, and time-consuming. They may interfere with daily activities and relationships. They may include:
They can be excessive, disruptive, and time-consuming. They may interfere with daily activities and relationships. They may include:
- Repeated handwashing (often 100 or more times a day)
- Checking and rechecking many times, such as making sure that a door is locked
- Following firm rules of order, such as putting on clothes in the very same order each day
- Hoarding objects
- Counting and recounting a lot
- Grouping objects or putting things in a certain order
- Repeating words spoken by oneself or others
- Asking the same questions again and again
- Repeatedly using four-letter words or making rude (obscene) gestures
- Repeating sounds, words, numbers, or music to oneself
The symptoms of OCD may seem like other health problems. Have your child see his or her healthcare provider for a diagnosis.
Have your child see his or her healthcare provider for a diagnosis.
How is OCD diagnosed in a child?
A child psychiatrist or other mental health expert can diagnose OCD. He or she will do a mental health evaluation of your child. To be diagnosed with OCD, your child must have obsessions and compulsions that are continuous, severe, and disruptive. They must harm your child’s day-to-day living.
In most cases, the activities of OCD such as handwashing or checking the locks on doors use up more than 1 hour each day. They also cause mental health distress and affect how your child thinks. In most cases, adults realize that their actions are not normal to some degree. But often children can't see that their behavior is irrational and abnormal.
How is OCD treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment for OCD often includes a combination of the following:
- Therapy with cognitive and behavioral methods.
 Cognitive methods help a child identify and understand his or her fears. They also teach a child new ways to better resolve or reduce those fears. Behavioral methods help the child and their family make pacts or rules to limit or change behaviors. One example is setting a maximum number of times a compulsive handwasher may wash his or her hands.
Cognitive methods help a child identify and understand his or her fears. They also teach a child new ways to better resolve or reduce those fears. Behavioral methods help the child and their family make pacts or rules to limit or change behaviors. One example is setting a maximum number of times a compulsive handwasher may wash his or her hands. - Family therapy. Parents play a vital role in any treatment process. A child’s school may also be included in care.
- Selective serotonin reuptake inhibitors (SSRIs). These medicines help raise serotonin levels in the brain.
- Antibiotics. Your child may need these medicines if his or her OCD is found to be linked to a streptococcal infection.
Teens with OCD may also have one or more types of eating disorders. These will also need treatment.
These will also need treatment.
How can I help prevent OCD in my child?
Experts don’t know at this time how to prevent OCD in children and teens. But if you notice signs of OCD in your child, you can help by getting an evaluation as soon as possible. Early treatment can ease symptoms and enhance your child’s normal development. It can also improve his or her quality of life.
How can I help my child live with OCD?
OCD can be treated, often with a combination of one-on-one therapy and medicines. You play a key supportive role in your child’s treatment. Here are things you can do to help your child:
- Keep all appointments with your child’s healthcare provider.
- Talk with your child’s healthcare provider about other providers who will be included in your child’s care. Your child may get care from a team that may include counselors, therapists, social workers, psychologists, and psychiatrists.
 Your child’s care team will depend on your child’s needs and how serious the OCD is.
Your child’s care team will depend on your child’s needs and how serious the OCD is. - Keep strong and open lines of communication with your child. Children with OCD can feel embarrassed about their disorder.
- Tell others about your child’s disorder. Work with your child’s healthcare provider and school to create a treatment plan.
- Reach out for support from local community services. Being in touch with other parents who have a child with OCD may be helpful.
Key points about OCD in children
- OCD is a type of anxiety disorder. A child with OCD has obsessive thoughts that are not wanted. They are linked to fears, such as touching dirty objects. The child uses compulsive rituals such as handwashing to control the fears. These rituals may feel rational or irrational to the person doing them.
 The child may not understand why they do these rituals. They may feel embarrassed that the behaviors occur and can't be controlled.
The child may not understand why they do these rituals. They may feel embarrassed that the behaviors occur and can't be controlled. - The exact cause of OCD is unknown. Children with OCD don’t have enough of a chemical called serotonin in their brain.
- Obsessive symptoms include repeated doubts and extreme preoccupation with dirt or germs.
- Compulsive behaviors include hoarding objects and checking things often.
- A mental health evaluation is needed to diagnose OCD.
- Treatment includes therapy and medicine.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests.
 Also write down any new instructions your provider gives you for your child.
Also write down any new instructions your provider gives you for your child. - Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Treatment of childhood obsessive-compulsive disorder OCD in Israel
Obsessive-compulsive disorder (OCD) is also known as obsessive-compulsive disorder. This disorder affects 1% to 4% of children. About half of cases begin in childhood and continue into adulthood.
This disorder affects 1% to 4% of children. About half of cases begin in childhood and continue into adulthood.
Anxiety is observed in children suffering from OCD, which manifests itself in a pronounced need to organize the world around them in a special way. They ask to retell what they have already been told many times, or to play the same game many times. nine0003
[SLIDER=1661]
R&D includes 2 components:
-
Obsessions or obsessions. The child constantly pronounces the same thought, returns to the same memories - both in the form of visual images and in the form of inner speech. The child may be constantly disturbed by the obsessive thought of pollution. He constantly wants to wash, avoid dirty places. He may require strict order in the house, symmetry in the arrangement of objects. If something is disturbed in his habits, this causes increased anxiety. The child may also be concerned about their own health and the health of their loved ones.
 nine0003
nine0003 -
Compulsive actions or obsessive behavior is the second component of the syndrome. We are talking about repetitive behavioral rituals, which must be observed strictly in a strict order, otherwise, according to the patient, something bad may happen. Such rituals include constantly washing hands, touching certain things in a certain order with the hands, and much more. It should be noted that children, unlike adult patients, try to tell their parents about their rituals, which increases the chances of recovery. Unfortunately, parents do not always listen to children's experiences, and this contributes to the further development of the disorder. nine0003
When diagnosing obsessive-compulsive disorder, the Matspen Center conducts a comprehensive study of the patient's mental state to identify or exclude another concomitant disease. A complete physical examination of the patient is also carried out in order to determine contraindications to certain medications, as well as to establish possible physical prerequisites for the development of OCD.
The main cause of OCD in a child may be structural or functional changes in the functioning of the anterior lobe of the brain - the ventral-medial pre-frontal cortex. This part of the brain is responsible for repetitive actions, rituals in human behavior. The pathology associated with the development of addictions to repetitive actions is also localized there. This area is associated with areas responsible for emotions, anxiety, thoughts and desires. In this way, a brain functional network is created that supports OCD. This cause can be revealed during an fMRI (functional magnetic resonance imaging). nine0003
Obsessive-compulsive disorder (OCD) in children and adolescents
STOP ALARM
15 sessions SELF-HYPNOSIS
4 lessons STOP SMOKING
session
UARU
We specialize in the treatment of Obsessive Compulsive Disorder (OCD) in children and adolescents and associated anxiety disorders
- Read this article
- Obsessive-compulsive disorder in children and adolescents - symptoms
- Treatment of Obsessive-Compulsive Disorder (OCD) in Children and Adolescents
Unfortunately, a large number of people, including many psychotherapists, mistakenly believe that obsessive-compulsive disorder is rare in children and adolescents.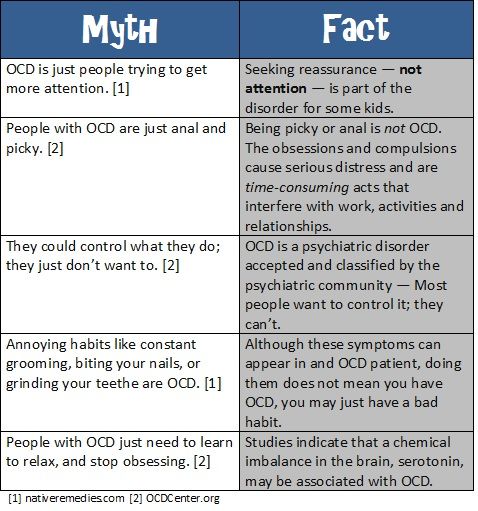 As a result, a large number of children and adolescents have OCD misdiagnosed as depression, attention deficit hyperactivity disorder (ADHD), conduct or conduct disorder, or other conditions. In fact, childhood OCD is quite common, occurring in approximately 1% of all children. In addition, recent studies show that about half of all adults diagnosed with OCD experienced these symptoms in childhood. nine0003
As a result, a large number of children and adolescents have OCD misdiagnosed as depression, attention deficit hyperactivity disorder (ADHD), conduct or conduct disorder, or other conditions. In fact, childhood OCD is quite common, occurring in approximately 1% of all children. In addition, recent studies show that about half of all adults diagnosed with OCD experienced these symptoms in childhood. nine0003
Obsessive Compulsive Disorder (OCD) in Children and Adolescents - Symptoms
In childhood, the symptoms of OCD can vary widely from one child to another. The following are some common examples of obsessive thoughts in children and adolescents who present with Obsessive-Compulsive Disorder:
- An exaggerated fear of being contaminated by contact with certain people or household items such as clothes, shoes or school books
- Unreasonable doubts about whether the child closed the door, window, turned off the light, stove or other household appliances
- Excessive concern with the appearance of homework
- Exaggerated concern about the symmetrical arrangement of household items such as shoelaces, school books, clothes or food
- Fear of accidentally harming parents, brother/sister, friend
- Superstitious fear that something bad might happen if apparently incoherent behavior is done (or does not happen)
Some common examples of compulsions in children and adolescents diagnosed with Obsessive Compulsive Disorder (OCD):
- Compulsive/repetitive hand washing, bathing or showering
- Behavioral rituals in which the child is required to touch certain parts of the body or perform certain body movements in a certain order or symmetrical shape
- Certain, repetitive bedtime rituals that interfere with normal falling asleep and sleep
- Obsessive repetition of certain words or prayers to assure oneself that nothing bad will happen
- Obsessive seeking reassurance from parents or teachers that they did no harm
- Avoiding / avoiding situations in which they think something bad might happen
In addition to the above symptoms, children and adolescents diagnosed with Obsessive-Compulsive Disorder may have secondary problems that result from their obsessions (obsessions) and/or compulsive behaviors (compulsions) and affect their daily lives. Academic problems, behavioral problems, peer conflicts, sleep disturbances, family conflicts are just some of the secondary symptoms that children and adolescents with OCD develop. Unfortunately, these difficulties often become the focus of psychotherapeutic attention, while Obsessive-Compulsive Disorder, which is actually the cause of this, remains without treatment. nine0003
Academic problems, behavioral problems, peer conflicts, sleep disturbances, family conflicts are just some of the secondary symptoms that children and adolescents with OCD develop. Unfortunately, these difficulties often become the focus of psychotherapeutic attention, while Obsessive-Compulsive Disorder, which is actually the cause of this, remains without treatment. nine0003
Like adults, children and adolescents diagnosed with obsessive-compulsive disorder perform compulsions (obsessive behaviors) and/or avoidance behaviors to reduce anxiety that is caused by unwanted, obsessive ideas (thoughts). While this appears to reduce anxiety and obsessions/thoughts at first glance, it actually only makes the symptoms worse and makes the person worse in the long run. This in turn leads to an increase in obsessive, unwanted thoughts (compulsions), which leads to an increase in compulsions and increased anxiety. During this cyclical process, the child develops "learned responses" in which he or she automatically becomes anxious in response to certain thoughts, objects, objects, or situations.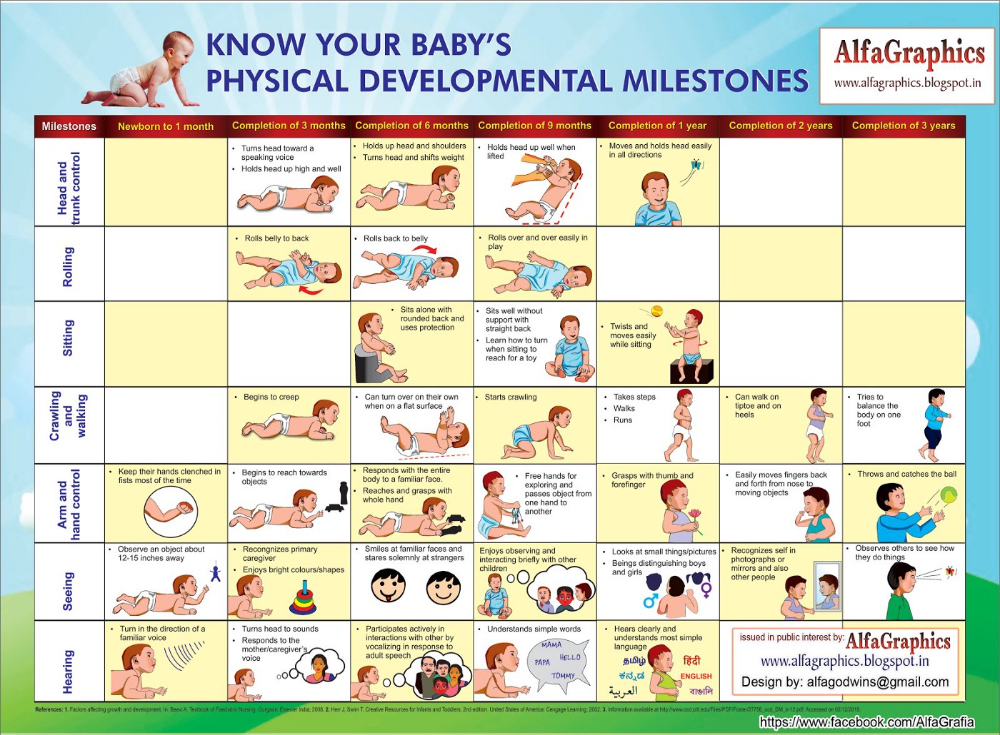 Although the specific thoughts and behaviors of OCD can vary significantly from person to person, this process is called the obsessive-compulsive cycle, and it is the same for all people who develop obsessive-compulsive disorder. For children and adolescents who suffer from OCD, this cycle can become an almost constant cycle of obsessions (obsessions) and obsessive behaviors (compulsions), and as a result will significantly interfere with daily life, both at home and at school. To learn more about what an obsessive-compulsive cycle is, click here. nine0003
Although the specific thoughts and behaviors of OCD can vary significantly from person to person, this process is called the obsessive-compulsive cycle, and it is the same for all people who develop obsessive-compulsive disorder. For children and adolescents who suffer from OCD, this cycle can become an almost constant cycle of obsessions (obsessions) and obsessive behaviors (compulsions), and as a result will significantly interfere with daily life, both at home and at school. To learn more about what an obsessive-compulsive cycle is, click here. nine0003
Obsessive-Compulsive Disorder (OCD) in Children and Adolescents - Treatment
CBT for OCD in Children and Adolescents
with OKR. One type of cognitive behavioral therapy, called Exposure and Response Prevention (EPR), has been identified by researchers as one of the most effective treatments for OCD in children (doi: 10.1001/jamapsychiatry.2014.170), adolescents, and adults. There is also another method of CBT called "Cognitive Restructuring" that is very valuable in treating children and adolescents who have obsessive-compulsive disorder.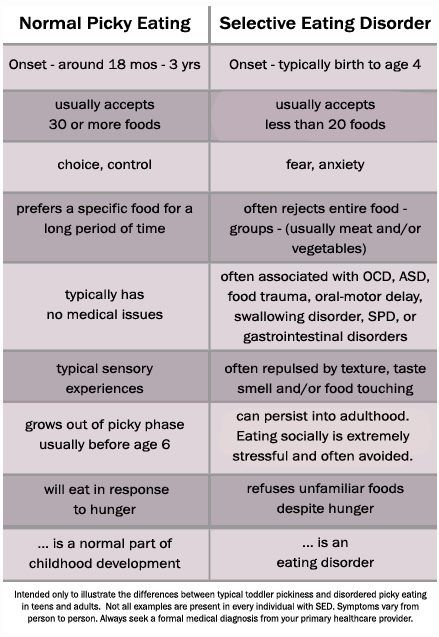 A variant of EPR has also been developed that is extremely effective for the treatment of OCD alone. Symptoms, OCD in its purest form are often observed in children and adolescents. This method is known as the "imagination" method and is based on the use of short stories that are based on the child's obsessive thoughts. In combination with the standard EPR method and cognitive restructuring, the mental representation method can significantly reduce the frequency and intensity of symptoms. To learn more about how Obsessive-Compulsive Disorder is treated with Cognitive Behavioral Therapy in children and adolescents, click here. nine0003
A variant of EPR has also been developed that is extremely effective for the treatment of OCD alone. Symptoms, OCD in its purest form are often observed in children and adolescents. This method is known as the "imagination" method and is based on the use of short stories that are based on the child's obsessive thoughts. In combination with the standard EPR method and cognitive restructuring, the mental representation method can significantly reduce the frequency and intensity of symptoms. To learn more about how Obsessive-Compulsive Disorder is treated with Cognitive Behavioral Therapy in children and adolescents, click here. nine0003
Hypnosis for the treatment of OCD in children and adolescents
Also, the treatment of children and adolescents diagnosed with obsessive-compulsive disorder is carried out using the Hypno-suggestive psychotherapy method (hypnosis and suggestion). Hypnosis is very effective when treating children and adolescents with OCD, it allows you to quickly make the required changes and fix them.
Treatment of OCD (Obsessive Compulsive Disorder) in Children and Adolescents with Cognitive Behavioral Therapy (CBT) via the Internet
According to the Center for Psychiatry Research at Karolinska Institutet in Sweden and Region Stockholm, Internet-based Cognitive Behavioral Therapy (CBT) can be as effective as conventional CBT. A study published in the journal JAMA could help make OCD treatment more accessible. 10.1001/jama.2021.3839
Results showed that stepwise online (digital) CBT reduced participants' OCD symptoms in the same way as conventional CBT.
"The study demonstrates the potential of technology when it comes to expanding access to evidence-based therapies for children and adolescents with OCD," says Principal Investigator Eva Serlachius, adjunct professor at Karolinska Institutet's Center for Psychiatry Research. “By offering low-intensity online (digital) intervention as the first step in treatment, clinics can save precious resources and devote their limited time to treating more patients or focusing on more complex cases.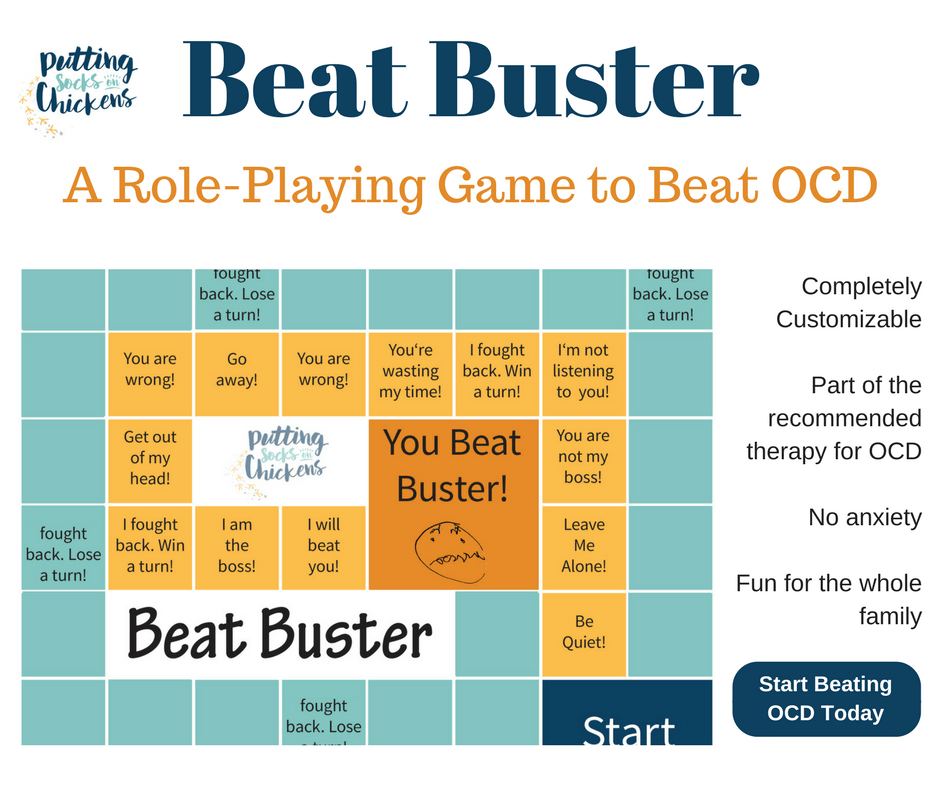 ” nine0003
” nine0003
OCD (Obsessive Compulsive Disorder) in Children and Adolescents - Group Treatment
In addition to individual psychotherapy, the Kyiv OCD Center runs a time-limited support group for adolescents who suffer from OCD and comorbid anxiety disorders. The group is focused on providing structured cognitive behavioral psychotherapy (CBT) for initial OCD and anxiety disorder. The goal of this short-term group for teenagers is to learn tools to better manage and reduce the symptoms of initial OCD and anxiety disorder, while at the same time helping them reduce feelings of isolation and shame. A secondary benefit is to help children with their social adjustment and academic performance, which are often worsened by their symptoms. nine0003
Peculiarities of treatment in children
It is important to focus on the fact that the treatment of OCD in children and adolescents, as well as associated anxiety disorders, is the same as for adults, but OCD, which developed in childhood, is based on specific age-related problems, which complicates the treatment process.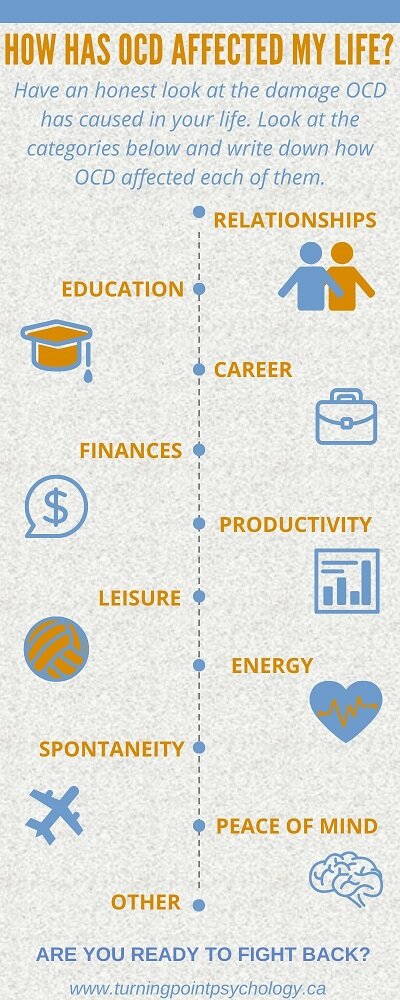 A large number of children and adolescents who suffer from OCD still do not have enough emotional and cognitive skills to completely eliminate their irrational fear and compulsive behavior. They have difficulty identifying and articulating their fear and/or difficulty in explaining why they do certain actions. They may also refuse to admit that their fear is exaggerated or unrealistic. In addition, children diagnosed with OCD may be reluctant to discuss their problems with anyone, even their parents. Also, children and adolescents with OCD may feel very uncomfortable or afraid of discussing their problem with a therapist. This behavior is not unusual for children and adolescents, as they have "magical thinking" - they believe that their fears will come true if they talk about them with a therapist or some other person. Other children may deny the symptoms, or refuse to do anything about them, in the hope that everything will go away on its own. Others simply want to avoid dealing with their OCD because they feel embarrassed or ashamed of it.
A large number of children and adolescents who suffer from OCD still do not have enough emotional and cognitive skills to completely eliminate their irrational fear and compulsive behavior. They have difficulty identifying and articulating their fear and/or difficulty in explaining why they do certain actions. They may also refuse to admit that their fear is exaggerated or unrealistic. In addition, children diagnosed with OCD may be reluctant to discuss their problems with anyone, even their parents. Also, children and adolescents with OCD may feel very uncomfortable or afraid of discussing their problem with a therapist. This behavior is not unusual for children and adolescents, as they have "magical thinking" - they believe that their fears will come true if they talk about them with a therapist or some other person. Other children may deny the symptoms, or refuse to do anything about them, in the hope that everything will go away on its own. Others simply want to avoid dealing with their OCD because they feel embarrassed or ashamed of it.