Body dysmorphia therapy
A Therapist’s Guide for the Treatment of Body Dysmorphic Disorder
by Andrea Hartmann, PhD, Jennifer Greenberg, PsyD, & Sabine Wilhelm, PhD
Overview of CBT for BDD and its empirical support
Most patients with body dysmorphic disorder (BDD) do not seek psychiatric/psychological care, but look for costly surgical, dermatologic, and dental treatments to try to fix perceived appearance flaws (e.g., Phillips, et al., 2000), that often worsen BDD symptoms (e.g., Sarwer & Crerand, 2008). Two empirically-based treatments are available for the treatment of BDD: serotonin reuptake inhibitors (SRIs) (click here to learn more about medication treatment for BDD) and cognitive-behavioral therapy (CBT). Several studies have found CBT to successfully reduce BDD severity and related symptoms such as depression (McKay, 1999; McKay et al., 1997; Rosen et al., 1995; Veale et al., 1996; Wilhelm et al., 1999; Wilhelm et al., 2011; Wihelm et al., 2014).
CBT models of BDD (e. g., Veale, 2004; Wilhelm et al., 2013) incorporate biological, psychological, and sociocultural factors in the development and maintenance of BDD. The model proposes that individuals with BDD selectively attend to minor aspects of appearance as opposed to seeing the big picture. This theory is informed by clinical observations and neuropsychological (Deckersbach et al., 2000) and neuroimaging findings (Feusner et al., 2007; Feusner et al., 2010). Individuals with BDD also overestimate the meaning and importance of perceived physical imperfections. For example, when walking into a restaurant, a patient with BDD who has concerns about his nose might think, “Everyone in the restaurant is staring at my big, bulbous nose.” Patients are also more likely misinterpret minor flaws (e.g., perceived asymmetry) as major personal flaws (e.g., “If my nose is crooked, I am unlovable”) (Buhlmann et al., 2009; Veale, 2004). Self-defeating interpretations foster negative feelings (e.g., anxiety, shame, sadness) that patients try to neutralize with rituals (e.
 g., excessive mirror checking, surgery seeking) and avoidance (e.g., social situations). Because rituals and avoidance may temporarily reduce painful feelings they are negatively reinforced and thus maintain maladaptive beliefs and coping strategies.
g., excessive mirror checking, surgery seeking) and avoidance (e.g., social situations). Because rituals and avoidance may temporarily reduce painful feelings they are negatively reinforced and thus maintain maladaptive beliefs and coping strategies.
CBT for BDD typically begins with assessment and psychoeducation, during which the therapist explains and individualizes the CBT model of BDD. In addition, CBT usually includes techniques such as cognitive restructuring, exposure and ritual prevention, and relapse prevention. Some CBT for BDD includes perceptual (mirror) retraining. A modular CBT manual (CBT-BDD; Wilhelm et al., 2013) has been developed to target core symptoms of BDD and to flexibly address symptoms that affect some, but not all, patients. Additional modules might address depression, skin picking/hair plucking, weight and shape concerns, and cosmetic surgery seeking (e.g. Wilhelm et al., 2013). CBT-BDD has been shown to be effective in open (Wilhelm et al., 2011) and randomized control trials (Wilhelm et al.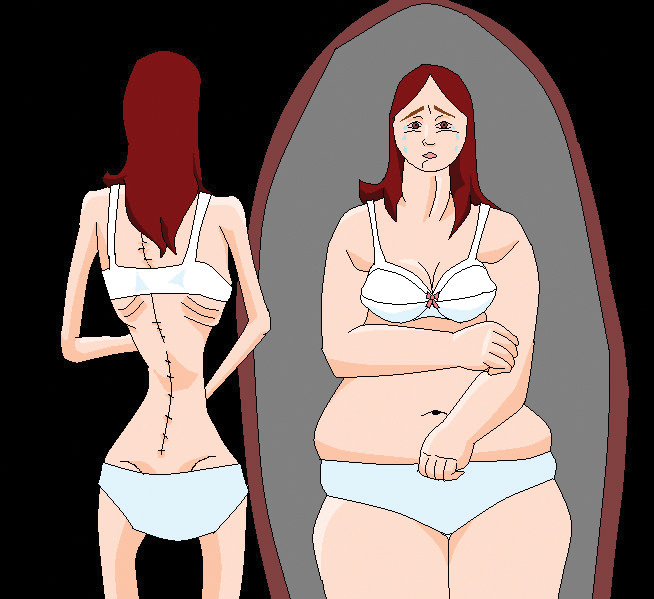 , 2014).
, 2014).
Assessment, motivational assessment, and psychoeducation
CBT begins with an assessment of BDD and associated symptoms. Clinicians should inquire about BDD-related areas of concern, thoughts, behaviors, and impairment. It is important to ask specifically about BDD symptoms as it often goes undetected in clinical settings (e.g., Grant et al., 2002) due to embarrassment and shame. Clinicians should be aware of clues in clinical presentation such as appearance (e.g., scarring due to skin picking) and behaviors (e.g, wearing camouflage), ideas or delusions of reference (e.g., feelings that people talk about them, stare at them), panic attacks (e.g., when looking into the mirror), depression, social anxiety, substance abuse and suicidal ideation as well as being housebound. Additionally, differential diagnosis should be clarified in a structured clinical interview including eating disorders, obsessive compulsive disorder, depression, and social phobia. Given the high rates of depression and suicidality in BDD, it is critical to evaluate depression and suicidality at the onset and regularly throughout treatment.
Given the high rates of depression and suicidality in BDD, it is critical to evaluate depression and suicidality at the onset and regularly throughout treatment.
For patients reluctant to try CBT or who hold highly delusional appearance beliefs, the therapist should incorporate techniques from motivational interviewing (MI; Miller & Rollnick, 2003) that have been adapted for the use in BDD (Wilhelm et al., 2013). In a first step, the therapist should empathize with the patient’s body image-related distress instead of directly questioning the validity of the beliefs (“I see that you really suffer because you are so worried because of the way you look. Let’s try to reduce this distress.”). Also, non-judgmental Socratic questioning can be employed (“What might be the advantages of trying CBT for BDD?“). The therapist can also discuss the discrepancy between BDD symptoms and the patient’s goals (“What should your life look like 10 years from now?“). In particular, for patients with poor insight it might be more helpful to address the usefulness of beliefs instead of the validity (e. g., “Are your beliefs preventing you from participating in activities you enjoy?“). MI strategies often need to be used throughout treatment.
g., “Are your beliefs preventing you from participating in activities you enjoy?“). MI strategies often need to be used throughout treatment.
Next, the therapist should provide psychoeducation about BDD, such as its prevalence, common symptoms, and differences between body image and appearance. Then, the therapist and patient develop an individualized model of BDD based on the patient’s specific symptoms. Such models include theories of how body image problems develop (including biological, sociocultural and psychological factors) (Wilhelm et al., 2013). It is important to explore factors in the patient’s current life that are serving to maintain body image concerns, including triggers for negative thoughts about appearance, interpretations of these thoughts, emotional reactions, and (maladaptive) coping strategies. This will help to inform the treatment and which specific modules are needed.
Cognitive strategies
Cognitive strategies include identifying maladaptive thoughts, evaluating them, and generating alternative thoughts. Therapists introduce patients to common cognitive errors in BDD, such as “all-or-nothing thinking” (e.g., “This scar makes me completely disgusting”) or “mindreading” (e.g., “I know my girlfriend wishes I had better skin”). Patients are then encouraged to monitor their appearance-based thoughts in and outside of the session and identify cognitive errors (e.g., “Why am I so nervous about riding the subway?” “I know others are staring at my nose and thinking how ugly it looks”. Cognitive distortion: “personalization”). After the patient has gained some skill in identifying maladaptive thoughts and cognitive errors, the therapist can start to evaluate thoughts with the patient (e.g., Rosen et al., 1995; Veale et al., 1996; Wilhelm et al., 2013). While it is often helpful to evaluate the validity of a maladaptive thought (e.g., “What is the evidence others are noticing or judging my nose?”), it can also be beneficial to examine its usefulness (e.g. “Is it really helpful for me to think that I can only be happy if my nose were straight?”; Wilhelm et al.
Therapists introduce patients to common cognitive errors in BDD, such as “all-or-nothing thinking” (e.g., “This scar makes me completely disgusting”) or “mindreading” (e.g., “I know my girlfriend wishes I had better skin”). Patients are then encouraged to monitor their appearance-based thoughts in and outside of the session and identify cognitive errors (e.g., “Why am I so nervous about riding the subway?” “I know others are staring at my nose and thinking how ugly it looks”. Cognitive distortion: “personalization”). After the patient has gained some skill in identifying maladaptive thoughts and cognitive errors, the therapist can start to evaluate thoughts with the patient (e.g., Rosen et al., 1995; Veale et al., 1996; Wilhelm et al., 2013). While it is often helpful to evaluate the validity of a maladaptive thought (e.g., “What is the evidence others are noticing or judging my nose?”), it can also be beneficial to examine its usefulness (e.g. “Is it really helpful for me to think that I can only be happy if my nose were straight?”; Wilhelm et al. , 2013), particularly for patients with poor insight. Once the patient has become adept at identifying and restructuring automatic appearance-related beliefs, deeper level (core) beliefs should be addressed. Common core beliefs in BDD include I’m unlovable” or “I’m inadequate” (Veale et al., 1996). These deeply held beliefs filter a patient’s experiences, and if not addressed, can thwart progress and long-term maintenance of gains. Core beliefs often emerge during the course of therapy. They can also be identified using the downward arrow technique, which involves the therapist asking repeatedly about the worst consequences of a patient’s beliefs (e.g., for the thought “People will think that my nose is huge and crooked,” the therapist would ask the patient, “What would it mean if people noticed your nose was big/crooked?”) until the core belief is reached (e.g., “If people noticed that my nose was big/crooked, they wouldn’t like me and this would mean that I am unlovable.”; Wilhelm et al.
, 2013), particularly for patients with poor insight. Once the patient has become adept at identifying and restructuring automatic appearance-related beliefs, deeper level (core) beliefs should be addressed. Common core beliefs in BDD include I’m unlovable” or “I’m inadequate” (Veale et al., 1996). These deeply held beliefs filter a patient’s experiences, and if not addressed, can thwart progress and long-term maintenance of gains. Core beliefs often emerge during the course of therapy. They can also be identified using the downward arrow technique, which involves the therapist asking repeatedly about the worst consequences of a patient’s beliefs (e.g., for the thought “People will think that my nose is huge and crooked,” the therapist would ask the patient, “What would it mean if people noticed your nose was big/crooked?”) until the core belief is reached (e.g., “If people noticed that my nose was big/crooked, they wouldn’t like me and this would mean that I am unlovable.”; Wilhelm et al. , 2013). Negative core beliefs can be addressed through cognitive restructuring, behavioral experiments, and strategies such as the self-esteem pie, which helps patients learn to broaden the basis of their self-worth to include non-appearance factors (e.g., skills, achievements, moral values).
, 2013). Negative core beliefs can be addressed through cognitive restructuring, behavioral experiments, and strategies such as the self-esteem pie, which helps patients learn to broaden the basis of their self-worth to include non-appearance factors (e.g., skills, achievements, moral values).
Exposure and ritual prevention (E/RP)
Prior to beginning E/RP, the therapist and patient should review the patient’s BDD model to help identify the patient’s rituals (e.g., excessive mirror checking) and avoidance behaviors (e.g., avoiding riding the subway) and discuss the role of rituals and avoidance in maintaining his symptoms. The therapist and patient jointly develop a hierarchy of anxiety provoking and avoided situations. Patients often avoid daily activities, or activities that could reveal one’s perceived flaw, including shopping (e.g., changing in a dressing room), going to the beach, intimate sexual encounters, going to work or class, or accepting social invitations. The hierarchy should include situations that would broaden a patient’s overall social experiences. For example, a patient might be encouraged to go out with friends twice per week instead of avoiding friends on days when he thought his nose looked really “huge.” The first exposure should be mildly to moderately challenging with a high likelihood for success. Exposure can be very challenging for patients, therefore, it is important for the therapist to provide a strong rationale for exposure, validate the patient’s anxiety while guiding him towards change, be challenging and encouraging, be patient and a cheerleader, and quickly incorporate ritual prevention. To reduce rituals, patients are encouraged to monitor the frequency and contexts in which rituals arise. The therapist then teaches patients strategies to eliminate rituals by first learning how to resist rituals (e.g., waiting before checking the mirror) or reduce rituals (e.g., wearing less makeup when out in public). The patient should be encouraged to use ritual prevention strategies during exposure exercises. It is often helpful to set up exposure exercises as a “behavioral experiment” during which they evaluate the validity of negative predictions (e.
For example, a patient might be encouraged to go out with friends twice per week instead of avoiding friends on days when he thought his nose looked really “huge.” The first exposure should be mildly to moderately challenging with a high likelihood for success. Exposure can be very challenging for patients, therefore, it is important for the therapist to provide a strong rationale for exposure, validate the patient’s anxiety while guiding him towards change, be challenging and encouraging, be patient and a cheerleader, and quickly incorporate ritual prevention. To reduce rituals, patients are encouraged to monitor the frequency and contexts in which rituals arise. The therapist then teaches patients strategies to eliminate rituals by first learning how to resist rituals (e.g., waiting before checking the mirror) or reduce rituals (e.g., wearing less makeup when out in public). The patient should be encouraged to use ritual prevention strategies during exposure exercises. It is often helpful to set up exposure exercises as a “behavioral experiment” during which they evaluate the validity of negative predictions (e. g., if I don’t wear my hat, someone will laugh at my thinning hair”). The goal of E/RP is to help patients practice tolerating distress and acquire new information to evaluate their negative beliefs (Wilhelm et al., 2013).
g., if I don’t wear my hat, someone will laugh at my thinning hair”). The goal of E/RP is to help patients practice tolerating distress and acquire new information to evaluate their negative beliefs (Wilhelm et al., 2013).
Perceptual retraining
Individuals with BDD often have a complex relationship with mirrors and reflective surfaces. A patient may vacillate between getting stuck for hours in the mirror scrutinizing, grooming, or skin picking, and active avoidance of seeing his reflection. Usually patients focus only on the body parts of concern and get very close to the mirror, which magnifies perceived imperfections and maintains maladaptive BDD beliefs and behaviors. Furthermore, patients tend to engage in judgmental and emotionally charged self-talk (“Your nose looks so disgusting”). Perceptual retraining helps to address distorted body image perception and helps patients learn to engage in healthier mirror-related behaviors (i.e., not getting too close to the mirror, not avoiding the mirror entirely). The therapist helps to guide the patient in describing his whole body (head to toe) while standing at a conversational distance from the mirror (e.g., two to three feet). Instead of judgmental language (e.g., “My nose is huge and crooked.”), during perceptual (mirror) retraining, patients learn to describe themselves more objectively (“There is a small bump on the bridge of my nose”). The therapist encourages the patient to refrain from rituals, such as zoning in on disliked areas or touching certain body parts. Perceptual retraining strategies can also be used to broaden patients attention in other situations in which the patient selectively attends to aspects of their and others’ appearance (e.g., while at work or out with friends). Patients are encouraged to practice attending to other things in the environment (e.g., the content of the conversation, what his meal tastes like) as opposed to his own or others’ appearance (Wilhelm et al., 2013).
The therapist helps to guide the patient in describing his whole body (head to toe) while standing at a conversational distance from the mirror (e.g., two to three feet). Instead of judgmental language (e.g., “My nose is huge and crooked.”), during perceptual (mirror) retraining, patients learn to describe themselves more objectively (“There is a small bump on the bridge of my nose”). The therapist encourages the patient to refrain from rituals, such as zoning in on disliked areas or touching certain body parts. Perceptual retraining strategies can also be used to broaden patients attention in other situations in which the patient selectively attends to aspects of their and others’ appearance (e.g., while at work or out with friends). Patients are encouraged to practice attending to other things in the environment (e.g., the content of the conversation, what his meal tastes like) as opposed to his own or others’ appearance (Wilhelm et al., 2013).
Brief overview over additional modules
Specific treatment strategies may be necessary to address symptoms affecting some but not all patients including: skin picking/hair pulling, muscularity and shape/weight, cosmetic treatment, and mood management (Wilhelm et al. , 2013). Habit reversal training can be used to address BDD-related skin picking or hair pulling. Patients with significant shape/weight concern, including those suffering from muscle dysmorphia often benefit from psychoeducation and cognitive-behavioral strategies tailored to shape/weight concerns. Therapists can use cognitive and motivational strategies to address maladaptive beliefs about the perceived benefits of surgery while at the same time helping the patient to nonjudgmentally explore the pros and cons of pursuing cosmetic surgery (Wilhelm et al., 2013). Depression is common in patients with BDD and may become treatment interfering (Gunstad & Phillips, 2003). Patients with significant depression can benefit from activity scheduling, as well as cognitive restructuring techniques for more severely depressed patients (Wilhelm et al., 2013).
, 2013). Habit reversal training can be used to address BDD-related skin picking or hair pulling. Patients with significant shape/weight concern, including those suffering from muscle dysmorphia often benefit from psychoeducation and cognitive-behavioral strategies tailored to shape/weight concerns. Therapists can use cognitive and motivational strategies to address maladaptive beliefs about the perceived benefits of surgery while at the same time helping the patient to nonjudgmentally explore the pros and cons of pursuing cosmetic surgery (Wilhelm et al., 2013). Depression is common in patients with BDD and may become treatment interfering (Gunstad & Phillips, 2003). Patients with significant depression can benefit from activity scheduling, as well as cognitive restructuring techniques for more severely depressed patients (Wilhelm et al., 2013).
Relapse Prevention
Treatment ends with relapse prevention focused on consolidation of skills and helping patients plan for the future. Therapists help patients expect and respond effectively to upcoming challenges (e.g., starting college, job interview, dating). Therapists may recommend self-therapy sessions in which patients set time aside weekly to review skills and set upcoming BDD goals. Booster sessions can be offered after treatment ends as a way to periodically assess progress and review CBT skills as needed (Wilhelm et al., 2013).
Therapists help patients expect and respond effectively to upcoming challenges (e.g., starting college, job interview, dating). Therapists may recommend self-therapy sessions in which patients set time aside weekly to review skills and set upcoming BDD goals. Booster sessions can be offered after treatment ends as a way to periodically assess progress and review CBT skills as needed (Wilhelm et al., 2013).
References
Buhlmann, U., Teachman, B. A., Naumann, E., Fehlinger, T., & Rief, W. (2009). The meaning of beauty: implicit and explicit self-esteem and attractiveness beliefs in body dysmorphic disorder. Journal of Anxiety Disorders, 23, 694-702.
Deckersbach, T., Savage, C. R., Phillips, K. A., Wilhelm, S., Buhlmann, U., & Rauch, S. L. (2000). Characteristics of memory dysfunction in body dysmorphic disorder. Journal of the International Neuropsychology Society, 6, 673-681.
Feusner, J. D., Bystritsky, A., Hellemann, G. , & Bookheimer, S. (2010). Impaired identity recognition of faces with emotional expressions in body dysmorphic disorder. Psychiatry Research, 179, 318-323.
, & Bookheimer, S. (2010). Impaired identity recognition of faces with emotional expressions in body dysmorphic disorder. Psychiatry Research, 179, 318-323.
Feusner, J. D., Townsend, J., Bystritsky, A., & Bookheimer, S. (2007). Visual information processing of faces in body dysmorphic disorder. Archives of General Psychiatry, 64, 1417-1425.
Grant, J. E., Kim, S. W., & Crow, S. J. (2001). Prevalence and clinical features of body dysmorphic disorder in adolescent and adult psychiatric inpatients. Journal of Clinical Psychiatry, 62, 517-522.
Gunstad, J., & Phillips, K.A. (2003). Axis I comorbidity in body dysmorphic disorder. Comprehensive Psychiatry, 44, 270-276.
McKay, D. (1999). Two-year follow-up of behavioral treatment and maintenance for body dysmorphic disorder. Behavior Modification, 23, 620-629.
McKay, D., Todaro, J., Neziroglu, F., Campisi, T., Moritz, E.K., Yaryura-Tobias, J.A. (1997). Body dysmorphic disorder: A preliminary evaluation of treatment and maintenance using exposure with response prevention. Behaviour Research and Therapy, 35, 67-70.
Body dysmorphic disorder: A preliminary evaluation of treatment and maintenance using exposure with response prevention. Behaviour Research and Therapy, 35, 67-70.
Miller, W.R. & Rollnick, S. (2002). Motivational interviewing: Preparing people for change (2nd edition). New York: Guilford Press.
Phillips, K. A., Dufresne, R. G., Jr., Wilkel, C. S., & Vittorio, C. C. (2000). Rate of body dysmorphic disorder in dermatology patients. Journal of the American Academy of Dermatolology, 42, 436-441.
Phillips, K. A., & Hollander, E. (2008). Treating body dysmorphic disorder with medication: evidence, misconceptions, and a suggested approach. Body Image, 51, 13-27.
Rosen, J.C., Reiter, J., & Orosan, P. (1995). Cognitive-behavioral body image therapy for body dysmorphic disorder. Journal of Consulting and Clinical Psychology, 63, 263-269.
Sarwer, D. B., & Crerand, C. E. (2008). Body dysmorphic disorder and appearance enhancing medical treatments. Body Image, 5, 50-58.
Body Image, 5, 50-58.
Veale, D. (2004). Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image, 1, 113-125.
Veale, D., Gournay, K., Dryden, W., Boocock, A., Shah, F., Willson, R. & Walburn, J. (1996).Body dysmorphic disorder: A cognitive behavioural model and pilot randomized control trial. Behaviour Research and Therapy, 34, 717-729.
Wilhelm, S., Otto, M. W., Lohr, B., & Deckersbach, T. (1999). Cognitive behavior group therapy for body dysmorphic disorder: a case series. Behavior Research and Therapy, 37, 71-75.
Wilhelm, S., Phillips, K. A., Didie, E., Buhlmann, U., Greenberg, J. L., Fama, J. M., Keshaviah, A., & Steketee, G. (2014). Modular Cognitive-Behavioral Therapy for Body Dysmorphic Disorder: A Randomized Controlled Trial. Behavior Therapy, 45, 314–327.
Wilhelm, S., Phillips, K. A., Fama, J. M., Greenberg, J. L., & Steketee, G. (2011). Modular cognitive-behavioral therapy for body dysmorphic disorder. Behavior Therapy, 42, 624-633.
Behavior Therapy, 42, 624-633.
Wilhelm S., Phillips K.A., & Steketee G. (2013). A cognitive behavioral treatment manual for body dysmorphic disorder. New York: Guilford Press.
More Than Alphabet Soup |
Body Dysmorphic Disorder (BDD)
- Understanding BDD
- Symptoms & Related Disorders
- Treatment
- ACT with CBT
- Resources
Jessica, 16, is overly concerned with the size of her head. She believes it is larger than the average person’s head. She goes out of her way to camouflage her head by wearing glasses and her hair down. In public she is convinced that others are staring at her and reacting with disgust. As a result of her preoccupation and her distress, she avoids school and socializing and prefers to spend her days in her room.
Jessica suffers from body dysmorphic disorder, often referred to as BDD, which is a preoccupation with an imagined or slight defect in appearance.
Treatment
Cognitive-behavioral therapy, or CBT, is the first line of treatment for BDD. This type of treatment typically involves a technique known as exposure and response prevention (ERP).
In BDD, exposure aims to decrease mirror checking, camouflaging, and other compulsive behaviors. It is also intended to prevent behaviors such as avoiding social situations. CBT is effective, but some people with BDD fail to respond. Some improve slightly, and some are unwilling to participate in ERP. For these reasons, it is useful to consider a different approach in conjunction with CBT.
Acceptance and commitment therapy, or ACT, is one such treatment. ACT focuses on tolerating thoughts and symptoms, rather than trying to change, dispute, and generate alternative interpretations to problems. People with resistant BDD may benefit from ACT because it teaches how to tolerate anxiety-provoking situations.
This type of therapy incorporates the core concepts of mindfulness, acceptance, and value-based living.
- Mindfulness: Developing the ability to be present in the moment and the ability to observe without making judgments.
- Acceptance: The ability to distinguish between pain and suffering and being able to tolerate and live with pain.
- Value-based living: The ability to live according to your values and not your symptoms; living fully now instead of waiting to reduce your symptoms
Mindfulness
The mindfulness aspect of ACT entails learning skills that aid in accepting thoughts and feelings. In the case of BDD, you practice the acceptance of thoughts such as “I have a big head” and feelings such as “I am unlovable.” This is achieved by engaging in a variety of mindfulness exercises such as taking a silent walk and simply observing thoughts, feelings, and sensations as they come up. Mindfulness allows you to realize that you can experience many events but that you are never defined by these events.
Acceptance
Many people with BDD experience intense feelings of suffering as a result of their preoccupation. In moments of struggle they avoid and try to control unpleasant thoughts. ACT helps them ride out moments of suffering and struggle.
First it addresses your willingness to experience common symptoms such as unwanted thoughts, images, and situations. Next comes the introduction of the idea that unpleasant internal stimuli are not as harmful as you assume.
With time, you will learn more flexible ways to respond to stressful thoughts that decrease suffering and struggle. ACT focuses on changing your reaction to triggers such as thoughts about your head instead of changing your thoughts about it.
Some people with BDD also suffer from depression. ACT aims to differentiate between a label and a thought.
Label: “I am depressed.”
vs.
Thought: “I am having the thought that I am depressed.”
This helps you learn the difference between a thought and a sense of self. In ACT, it is important to be aware that we are not our thoughts. This process assists in decreasing the emotion attached to such thoughts.
In ACT, it is important to be aware that we are not our thoughts. This process assists in decreasing the emotion attached to such thoughts.
Value-based Living
The third component of ACT involves value-based living. For many with BDD, their appearance is their only value. ACT helps identify other values, which can serve as guides to live your life. Clarification of values involves distilling urges and feelings to see what is truly meaningful to you.
For example, someone with BDD might appear to value appearance, but values-clarification exercises might reveal that the true values are human connectedness with corresponding desires to be loved and wanted. Therapeutically, this value can be pursued in ways that de-emphasize the importance of attractiveness. Part of this component includes an agreement to live life for its values and not for symptom reduction. In turn, this increases commitment to living a healthy life and assists in commitment to therapy.
Conclusion: A Meaningful Existence
ACT treatment goals include living a meaningful existence according to your values, focusing on the present moment, and tolerating emotions. It is clear that including ACT with CBT serves to increase the acceptance and motivation to engage in treatment.
It is clear that including ACT with CBT serves to increase the acceptance and motivation to engage in treatment.
Agnes Selinger, PhD, Southwestern Vermont Consortium
Fugen Neziroglu, PhD, ABBP, Director, Bio-Behavioral Institute
causes, symptoms, treatment and psychotherapy of dysmorphophobia in women
Dysmorphophobia syndrome is manifested by excessive concern about one's appearance, a desire to improve it, which subsequently turns into a painful state. A person feels dissatisfaction with his appearance, despite any changes. The reasons for the development of the disorder are the genetic predisposition of the diseased. Dysmorphophobia affects both women and men. For many, appearance is the main value on which success with the opposite sex and personal happiness depend. Also, the symptoms of the syndrome often appear in adolescence, regardless of gender, when a person evaluates himself as critically as possible. nine0003
Dysmorphophobia is directly related to mental disorders. Treatment should be carried out under the supervision of a specialist. Seeing a psychiatrist and psychotherapy will help you cope with the manic desire to improve your appearance, allow you to love yourself and recognize your uniqueness.
Treatment should be carried out under the supervision of a specialist. Seeing a psychiatrist and psychotherapy will help you cope with the manic desire to improve your appearance, allow you to love yourself and recognize your uniqueness.
Article content:
- Disease description
- Dysmorphophobia in adolescents
- Diagnostic methods
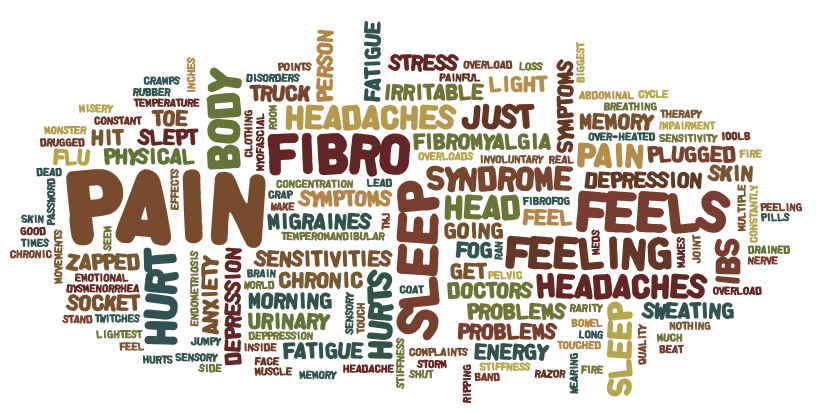
- Disease symptoms
- Causes
- Treatment of dysmorphophobia
- Cognitive behavioral therapy
- Group and individual therapy
- Forecasts
- Appeal to professionals
Description of the disease
Dysmorphophobia syndrome is a mental state in which a person is overly concerned about his appearance, cannot adequately assess the features of his own body, and does everything to correct far-fetched shortcomings. When upset, men and women begin to get involved in plastic surgery and diets. Often this leads to bulimia and anorexia. nine0041 When upset, there is a fear that it will not be possible to achieve an ideal figure. In this case, symptoms of severe depression develop, suicidal thoughts appear. Since all the problems are in the psyche, the perception of appearance by the sick and others is very different. Treatment of the disorder in women and men requires deep psychotherapy.
Often this leads to bulimia and anorexia. nine0041 When upset, there is a fear that it will not be possible to achieve an ideal figure. In this case, symptoms of severe depression develop, suicidal thoughts appear. Since all the problems are in the psyche, the perception of appearance by the sick and others is very different. Treatment of the disorder in women and men requires deep psychotherapy.
It is very important to teach the patient to value himself, because with dysmorphophobia there is no end point in transformations - the patient constantly finds new imperfections. nine0003
Dysmorphophobia in adolescents
It is adolescents who most often suffer from dysmorphophobia. When you grow up, you pay more attention to your appearance. Any features of one's own body and shortcomings are perceived negatively by the psyche of a teenager. The syndrome is often referred to as delusional, hypochondriacal, overvalued or obsessive disorders. It develops on fears that are associated with the characteristics of the human psyche.
It develops on fears that are associated with the characteristics of the human psyche.
The decision to treat body dysmorphic disorder is based on the presence of three features:
- painful certainty that there is a shortcoming - real and exaggerated, or far-fetched;
- relationship idea;
- depressed mood.
The main difficulty lies in the fact that adolescents hide their thoughts and fears, so treatment often begins after serious attempts to change their appearance.
If a teenager has symptoms of an illness, then he urgently needs a consultation with a psychiatrist and treatment with the help of psychotherapy. It is possible to notice the syndrome if you carefully observe the child, fix strange changes in behavior, habits, clothing style. The sick person most often stops sharing his experiences with loved ones, does not answer questions about a bad mood. nine0041 Relatives may notice indirect symptoms:
- excessive attention to oneself, search for an angle in which flaws will be invisible - a person constantly carries a mirror with him;
- painful attitude to photography - photos are removed from prominent places, because they allegedly serve as evidence of imperfections.

The disease must be treated by a psychiatrist, the patient also needs psychotherapy, without treatment the disease can progress. In the future, adult women may face problems in their personal lives and stress due to body dysmorphic disorder. nine0003
Diagnostic methods
As a rule, patients do not see the problem and the need for psychotherapy. Symptoms of the disease can be noticed by relatives and relatives.
According to the MBC-10, for body dysmorphophobia, the patient must have the following signs:
- preoccupation with an imperfection or disease of a physical nature that progresses rapidly;
- focusing on one or two organs;
- existing disorders are used to manipulate others; nine0016
- self-treatment, passion for various diets.
When symptoms are detected, it is necessary to understand the causes of their occurrence. The specialist will need to exclude the presence of other mental disorders.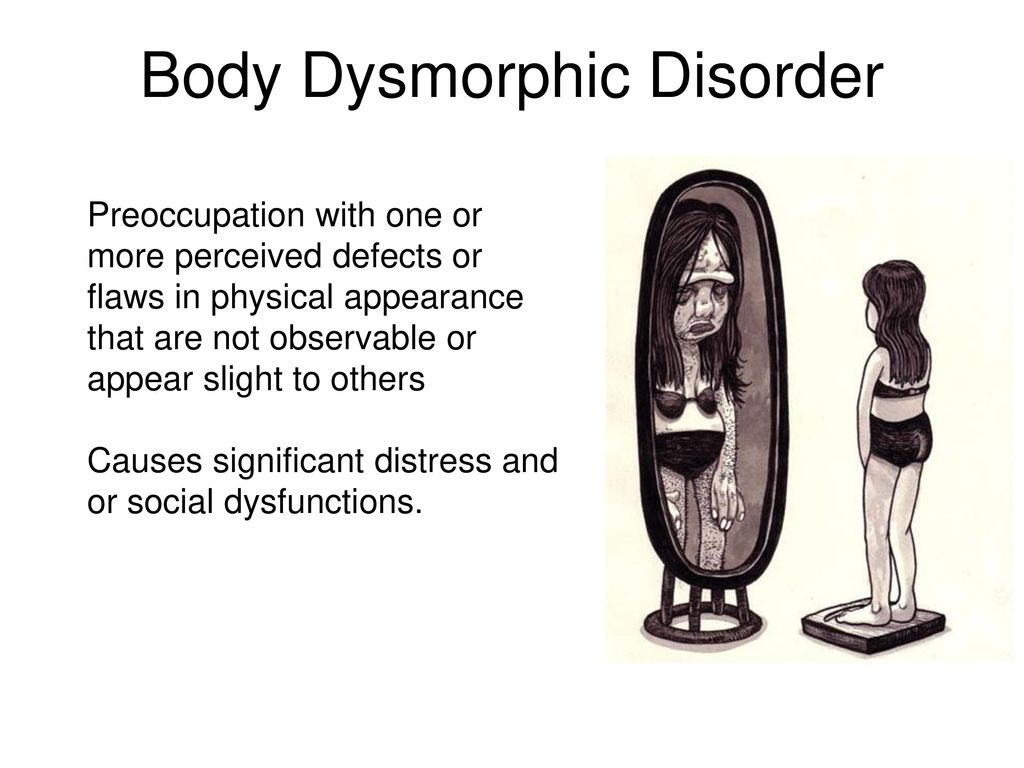
Symptoms of the disease
Excessive anxiety syndrome is manifested by a constant desire to look at one's reflection, evaluating appearance, fear of being photographed. Women who are overly concerned about their appearance constantly ask loved ones about their defects and try to hide them. nine0003
The development of dysmorphophobia syndrome affects all spheres of life, because the patient loses interest in studies, work, and strives for social isolation. In the absence of treatment, as a rule, there is an excessive passion for sports, diets. Women are beginning to save money for surgical operations. There may be problems such as:
- alcohol abuse;
- loss of concentration;
- panic attacks;
- search for ways to get rid of existing defects. nine0016
In women, symptoms include wearing a lot of make-up, wearing oversized clothes to hide imperfections. It is important to start treatment as soon as possible.
It is necessary to apply psychotherapy, and sometimes medication is required.
Causes of occurrence
There is a direct relationship between the effectiveness of psychotherapy treatment with an accurate understanding of why the syndrome of dysmorphophobia appeared. A man or woman can develop the disease for the following reasons:
- biological - disorders of neurotransmitter metabolism, anomalies in the development of the brain, the presence of a genetic predisposition of a woman or a man;
- psychological - injuries associated with criticism, lack of love and attention;
- social - pressure from the media, promotion of unhealthy body parameters, activation of fears associated with loneliness;
- personal - dysmorphophobia syndrome is characteristic of people with such qualities as timidity and insecurity, perfectionism, neurosis, increased sensitivity to criticism. nine0016
In rare cases, women or members of the opposite sex need treatment for the syndrome because of schizophrenia.
Body Dysmorphophobia Treatment
Body dysmorphic disorder in adolescents, women and men is treated with highly specialized psychotherapy. As a rule, during an exacerbation of depression, drug therapy is prescribed. It is possible to use antidepressants, tranquilizers to exclude suicide attempts, reduce anxiety and stabilize the condition. nine0003
Psychotherapy sessions begin in the second stage of treatment. Experts say that it is impossible to convince a woman or a man of wrong thoughts. Therefore, work is underway to adopt its appearance. It is strictly forbidden to allow plastic surgery or strict diets, as this leads to an exacerbation of the syndrome.
Treatment of body dysmorphic disorder is most often carried out on an outpatient basis, in advanced cases hospitalization is possible. This is necessary if psychotherapy does not help, there have been suicide attempts, the patient secretly continues to try to change himself. Treatment in a hospital allows you to isolate the patient from the effects of negative factors and eliminate the risks of deterioration.
nine0003
Cognitive behavioral therapy
Cognitive behavioral therapy is often used to treat a woman or a man. This approach is aimed at helping the patient get rid of the rituals associated with the constant assessment of their shortcomings. In the process of treatment, self-reflection is necessary:
- tracking one's condition;
- fixing the appearance of negative thoughts;
- overcoming negativity. nine0016
Cognitive Behavioral Therapy is aimed at making patients aware of their condition to the full extent and the dangerous consequences for health. This is the main condition for a successful recovery. This method can be combined with medication or other types of therapy.
Group and individual therapy
With various disorders of adequate perception of one's own body, it is important to combine individual work with group sessions. This approach provides the following benefits:
- important insights when face-to-face communication with a psychotherapist has reached an impasse;
- the opportunity to look at the problem from the outside;
- development of empathy, friendly support;
- receiving strength to fight the disease from people who are faced with the same problem;
- association with those who have already returned to society to a normal way of life;
- Get more resources and help to prevent relapse.
 nine0035
nine0035
Groups can also be visited after the end of the main course of treatment as a fixative therapy or preventive measure.
Predictions
With the development of the syndrome, patients usually seek help from dermatologists, nutritionists, and plastic surgeons. This not only does not bring relief, but also aggravates the course of the disease. Recovery is possible only when working with a qualified psychiatrist and psychologist. Properly used psychotherapy allows you to get a noticeable effect in 82% of cases if the patient continues to be treated. The support of loved ones contributes to a faster recovery. Multi-family therapy may be used. nine0003
Many patients benefit from the use of antidepressants. The choice of drug and dosage should be prescribed by the attending physician.
Contacting professionals
CIRC specializes in helping patients with body dysmorphic disorder. We use British guidelines for diagnosis and treatment, we use only modern methods to combat anorexia, bulimia and other disorders.
We offer professional outpatient and inpatient care. Full understanding of the problem without judgment and pressure. The clinic employs the best specialists who undergo supervision and regularly improve their qualifications abroad. To sign up for a consultation in Moscow, call +7(499) 703-20-51 or fill out the online form.
Author: Korshunova Anna Aleksandrovna
Head of the Center for the Study of Eating Disorders,
psychiatrist, psychotherapist.
Dysmorphophobia - more than just complexes | "Four Leaf Clover"
“Stop seeing only flaws”, “look how beautiful / handsome you are”, “people don’t have arms / legs and nothing, they live somehow”, “you just have a complex”, - this is how they usually try to calm a person who doubts in their attractiveness, not even suspecting that for a patient with body dysmorphic disorder these phrases will have exactly the opposite character. nine0003
nine0003
From time to time, the majority of people are characterized by dissatisfaction with their own body: an irregularly shaped nose, extra pounds, short legs and other “flaws” make you feel like “ugly ducklings”. However, if such experiences do not affect the course of daily life in any way, we do not take this as a pathology. But there are times when dissatisfaction with oneself is truly large-scale.
Dysmorphophobia is a mental disorder in which a person is overly concerned and preoccupied with a minor defect or feature of their body. In addition, he is sure that his “defect” is disgusting to others, and they condemn him for this “ugliness”. nine0041 The key word in this term is "excessive". That is, the whole difference between ordinary doubts and dysmorphophobia is in the intensity of experiences.
In the first case, a person can easily distract himself from depressing thoughts about his physical imperfection and engage in more pleasant activities.
In the second, he spends the lion's share of time looking at his “flaw” in front of a mirror, or vice versa, diligently avoids reflective surfaces; categorically refuses to be photographed or filmed on video; wraps himself from head to toe even in 30-degree heat, so as not to "shock" others with his body; make numerous tattoos all over his body to "hide" it; even bathes with his eyes closed, trying to come into contact with him as little as possible, since every such form of contact is disgusting. nine0003
nine0003
Some people do not stop at heavy thoughts about their "unattractiveness" and begin active measures to improve themselves. But endless trips to cosmetologists and plastic surgeons do not bring satisfaction with the result, since body dysmorphic disorder is a story about a violation of the perception of one's body, and not about some actual flaw.
Most often, the disorder occurs in the younger generation (mainly girls), starting in most cases from adolescence. At risk are those who had childhood psychological trauma associated with a lack of parental love and care, the sad experience of rejecting feelings, the lack of warm, trusting relationships in the family. brain). nine0003
Dysmorphophobia rarely comes alone. Paired with it, various anxiety disorders, mood disorders (bipolar disorder, dysthymia, but more often, of course, depression that occurs against the background of dysmorphophobia), personality traits, and eating disorders (bulimia, anorexia) are often observed.