Can anxiety cause pain between shoulder blades
Anxiety And Back Pain - AnxietyCentre.com
Back pain, such as acute and chronic tension, stiffness, soreness, shooting pains, sharp stabbing pains, back spasms, and immobility are common symptoms of anxiety disorder, including anxiety and panic attacks, generalized anxiety disorder, social anxiety disorder, and obsessive-compulsive disorder, phobias, and others.
This article explains the relationship between anxiety and back pain symptoms.
Article Menu
- Symptom Descriptions
- Causes
- Treatment
- Therapy
- FAQ
- Prevalence
- Video
- Additional Comments
- References
Common Anxiety Back Pain Symptom Descriptions
- You get frequent back pain, tension, stiffness, soreness, or back spasms.
- It feels as if your back is often painful, tense, stiff, or sore.
- Your back is so sore that it causes mild to severe immobility.
- You regularly have back pain, back muscle tension, stiffness, and soreness.
- Your back feels unusually tense, stiff, or sore from normal tasks.
- Your sleep can also be disrupted due to chronic and unrelenting back pain.
- You get sharp, shooting, or stabbing pains in your back but you haven’t done anything to cause them.
- Anxiety back pain can also feel like a burning sensation in the back.
- You get unexplained pain and tension between the shoulder blades.
- You take pain relievers more frequently because of unrelieved back pain, tension, stiffness, and soreness.
- Your back muscles frequently spasm seemingly for no reason.
- You get acute or chronic back pain, tension, stiffness, soreness, shooting pains, or spasms seemingly for no reason. Your doctor has ruled out injury as the cause.
- Even gentle movements, such as bending over, twisting, or pivoting can cause sudden back pain.
- This symptom can also be experienced as a “pressure” anywhere on or in the back.

Anxiety back pain symptoms can affect one area of the back only, can shift and affect another area or areas in the back, can migrate all over and affect many areas of the back, or affect the entire back. They can also affect the upper back, middle of the back, or lower back only.
Back pain symptoms can occur rarely, frequently, or persistently. For example, you have back pain symptoms once in a while and not that often, have them off and on, or have them all the time.
Anxiety back pain symptoms can precede, accompany, or follow an escalation of other anxiety symptoms or occur by themselves. They can also precede, accompany, or follow an episode of nervousness, anxiety, fear, and stress, or occur “out of the blue” and for no apparent reason.
Back pain symptoms can range in intensity from slight, to moderate, to severe. They can also come in waves where they are strong one moment and ease off the next.
Back pain anxiety symptoms can change from day to day and from moment to moment.
All the above combinations and variations are common.
Anxiety back pain, tension, stiffness, soreness, spasms, and immobility symptoms can seem more disconcerting when undistracted, resting, trying to sleep, or when waking up.
To see if anxiety might be playing a role in your symptoms, rate your level of anxiety using our free one-minute instant results Anxiety Test, Anxiety Disorder Test, or Hyperstimulation Test.
The higher the rating, the more likely anxiety could be contributing to or causing your anxiety symptoms, including feeling like impending doom symptoms.
How Anxiety Causes Back Pain Symptoms
Medical Advisory
Talk to your doctor about all new, changing, persistent, and returning symptoms as some medical conditions and medications can cause anxiety-like symptoms.
Additional Medical Advisory Information.
When this symptom is caused by anxiety, stress, including anxiety-caused stress, is a common cause of acute and chronic back pain symptoms.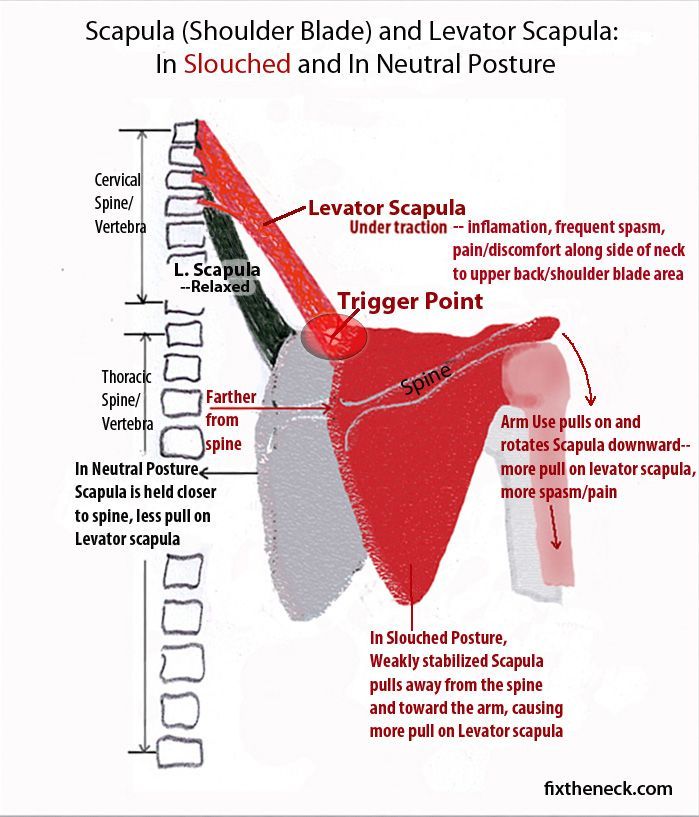 [1][2][3]
[1][2][3]
Here are some of the more common reasons why anxiety can cause acute and chronic back pain symptoms:
1. Stress response
Anxious behavior (which creates anxiety) activates the stress response, also known as the fight or flight response.[4][5]
The stress response causes many body-wide changes that prepare the body for immediate emergency action.
Visit our “Stress Response” article for more information about its many changes.
One of these changes includes tightening muscles so that the body is more resilient to injury. Tight muscles in the back can cause tension, stiffness, soreness, and restricted mobility.
In some instances, muscles can tighten so much that they become painful, sore, and spasm.
There are many muscle groups in the back. Any muscle or group of muscles can be affected by stress.
Anxiety and an accompanying stress response is a common cause of acute back pain, tension, stiffness, soreness, and muscle spasms.
As long as you're anxious and a stress response is active, you can have back pain symptoms.
2. Hyperstimulation
Frequent activation of the stress response, such as from overly anxious behavior, can cause the body to remain in a state of semi-stress response readiness. We call this state “stress-response hyperstimulation” since stress hormones are powerful stimulants.[6][7]
Visit our “Hyperstimulation” article for more information about the many ways hyperstimulation can affect the body.
Hyperstimulation can cause changes of an active stress response even though a stress response hasn’t been activated.
As such, hyperstimulation can keep the body stressed and muscles tight, including the muscles in the back. Chronic back pain is a common symptom of hyperstimulation.
Nervous System Excitation and Dysregulation
Hyperstimulation can also overly excite and stress the nervous system, which is primarily made up of neurons – cells that have an electrochemical makeup (the combination of electricity and chemicals).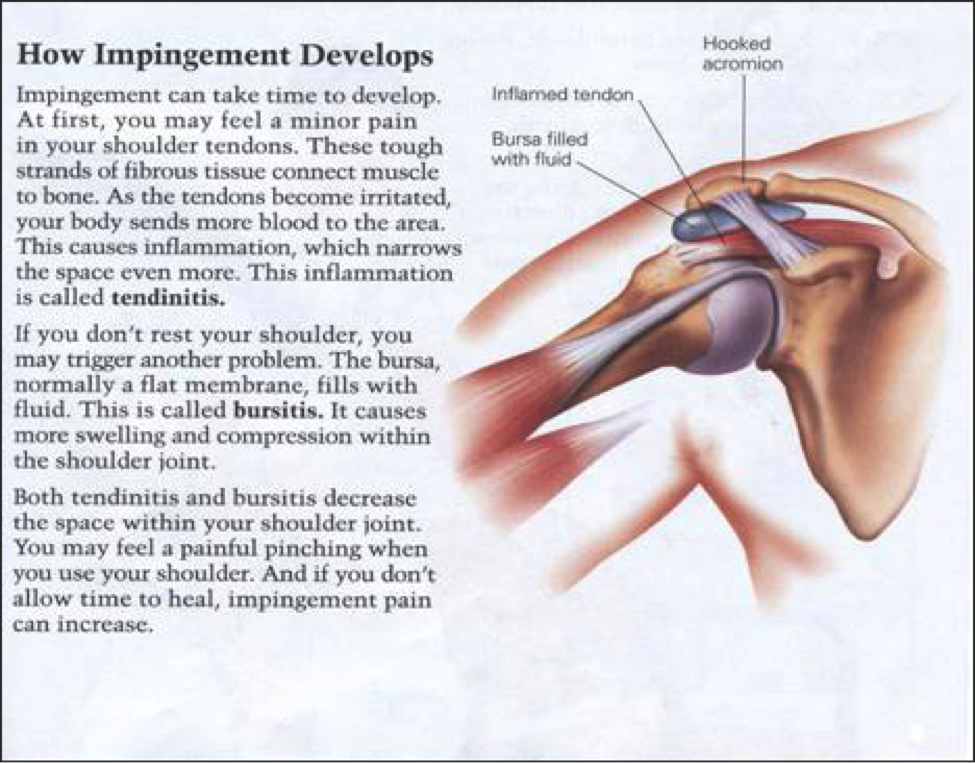
Overly excited neurons can act erratically,[8][9] affecting nerve impulses that control muscle movement and tension. Chronic muscle tension, twitching, pain, and spasms are common indications of an overly stressed nervous system.
Moreover, research has shown that stress increases sensitivity and reactivity to pain.[10] As such, an overly excited and stressed nervous system can cause issues with pain, including chronic back pain problems.
Many doctors who specialize in back pain problems, such as Dr. Sarno, are now seeing a direct correlation between stress, including anxiety-caused stress, and back pain and tension.
Other Factors
Other factors can cause stress and cause and aggravate anxiety back pain symptoms, including:
- Medication
- Recreational drugs
- Stimulants
- Sleep deprivation
- Fatigue
- Hyper and hypoventilation
- Low blood sugar
- Nutritional deficiencies
- Dehydration
- Hormone changes
- Pain
Select the relevant link for more information.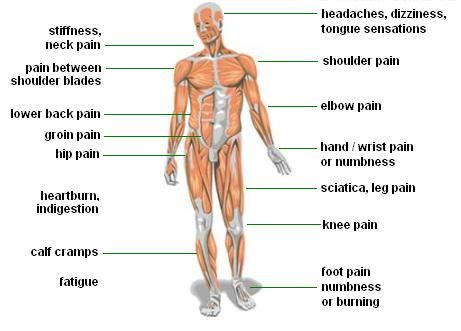
How To Get Rid Of Anxiety Back Pain Symptoms
When other factors cause or aggravate this anxiety symptom, addressing the specific cause can reduce and eliminate this symptom.
When an active stress response causes this symptom, ending the active stress response will cause this acute anxiety symptom to subside.
Keep in mind that it can take up to 20 minutes or more for the body to recover from a major stress response. But this is normal and needn’t be a cause for concern.
When hyperstimulation (chronic stress) causes back pain symptoms, eliminating hyperstimulation will stop anxiety back pain symptoms.
You can eliminate hyperstimulation by:
- Reducing stress.
- Containing anxious behavior (since anxiety creates stress).
- Regular deep relaxation.
- Avoiding stimulants.
- Regular light to moderate exercise.
- Eating a healthy diet of whole and natural foods.
- Passively accepting your symptoms until they subside.
- Being patient as your body recovers.
Visit our “60 Natural Ways To Reduce Stress” article for more ways to reduce stress.
As the body recovers from hyperstimulation, it stops sending symptoms, including anxiety back pain symptoms.
Symptoms of chronic stress subside as the body regains its normal, non-hyperstimulated health.
However, eliminating hyperstimulation can take much longer than most people think, causing symptoms to linger longer than expected.
As long as the body is even slightly hyperstimulated, it can present symptoms of any type, number, intensity, duration, frequency, and at any time, including this one.
Even so, since back pain is a common symptom of stress, including anxiety-caused stress, it's harmless and needn't be a cause for concern. It will subside when unhealthy stress has been eliminated and the body has had sufficient time to recover. Therefore, there is no reason to worry about it.
Anxiety symptoms often linger because:
- The body is still being stressed (from stressful circumstances or anxious behavior).
- Your stress hasn't diminished enough or for long enough.
- Your body hasn't completed its recovery work.
Addressing the reason for lingering symptoms will allow the body to recover.
Most often, lingering anxiety symptoms ONLY remain because of the above reasons. They AREN'T a sign of a medical problem. This is especially true if you have had your symptoms evaluated by your doctor and they have been solely attributed to anxiety or stress.
Chronic anxiety symptoms subside when hyperstimulation is eliminated. As the body recovers and stabilizes, all chronic anxiety symptoms will slowly diminish and eventually disappear.
Since worrying and becoming upset about anxiety symptoms create stress, these behaviors can interfere with recovery.
Passively accepting your symptoms – allowing them to persist without reacting to, resisting, worrying about, or fighting them – while doing your recovery work will cause their cessation in time.
Acceptance, practice, and patience are key to recovery.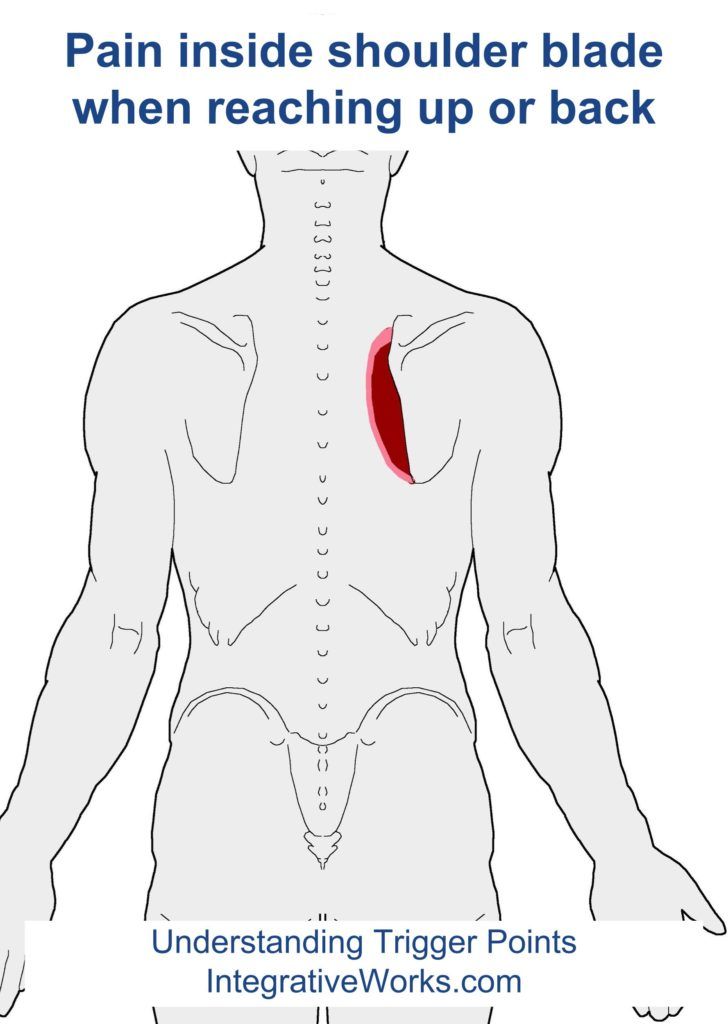
Keep in mind that it can take a long time for the body to recover from hyperstimulation. It's best to faithfully work at your recovery despite the lack of apparent progress.
However, if you persevere with your recovery work, you will succeed.
You also have to do your recovery work FIRST before your body can recover. The cumulative effects of your recovery work will produce results down the road. And the body's stimulation has to diminish before symptoms can subside.
- Reducing stress.
- Increasing rest.
- Faithfully practicing your recovery strategies.
- Passively accepting your symptoms.
- Containing anxious behavior.
- Being patient.
These will bring results in time.
When you do the right work, the body has to recover!
Short-term Remedies
Even though eliminating hyperstimulation will eliminate chronic anxiety symptoms, including back pain symptoms, some people have found the following strategies helpful.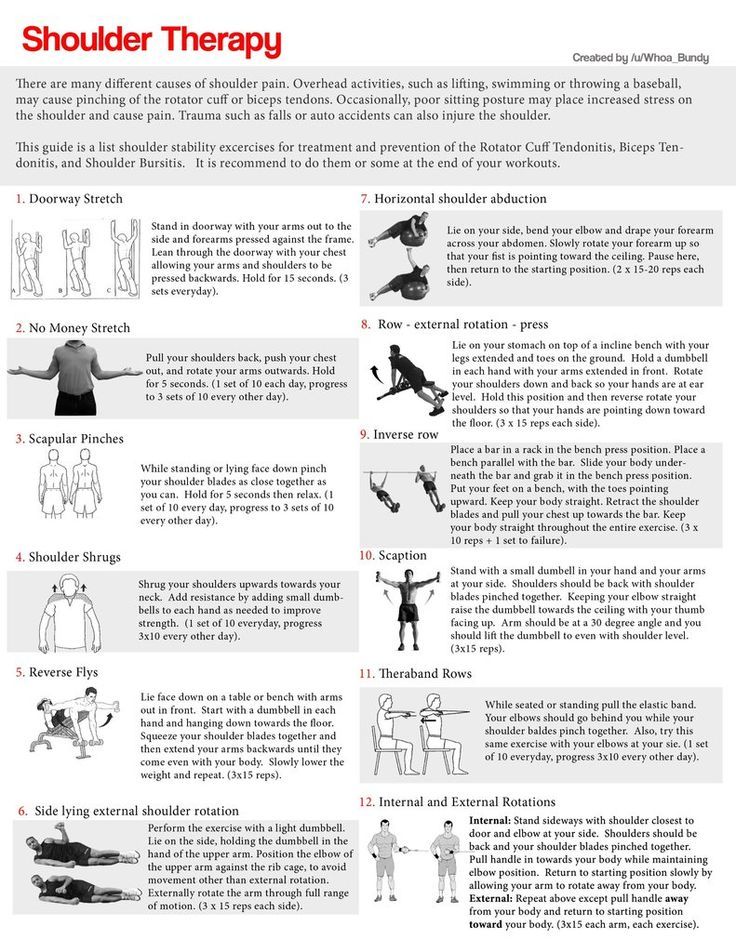
However, keep in mind that each person can have a unique symptom experience since each person is somewhat physically, chemically, psychologically, and emotionally unique. What might work for one person might not for another.
- Anything that reduces your body’s stress can help, such as deep relaxation, rest, and getting good sleep.
- Regular light to moderate exercise can also help loosen tight muscles, such as those responsible for chronic back pain.
- Heating pad (heat causes tight muscles to loosen).
- Having a warm bath.
- Have a massage.
- Vibrator on the back (vibration can help loosen tight muscles and stop muscle spasms).
- Avoiding stimulants (stimulants stress the body).
- Muscle relaxants.
- Gentle/mild stretching.
- TENS machine
- Slowing down a hectic schedule or lifestyle.
- Taking some time off so that your body can reduce its stress.
- Regular hobby/play time.

- Whirlpool or hot tub (as long as the heat is comfortable and not distressing).
- Having fun.
- Laughter.
- Being hugged, held, or caressed by your mate, spouse, or loved one.
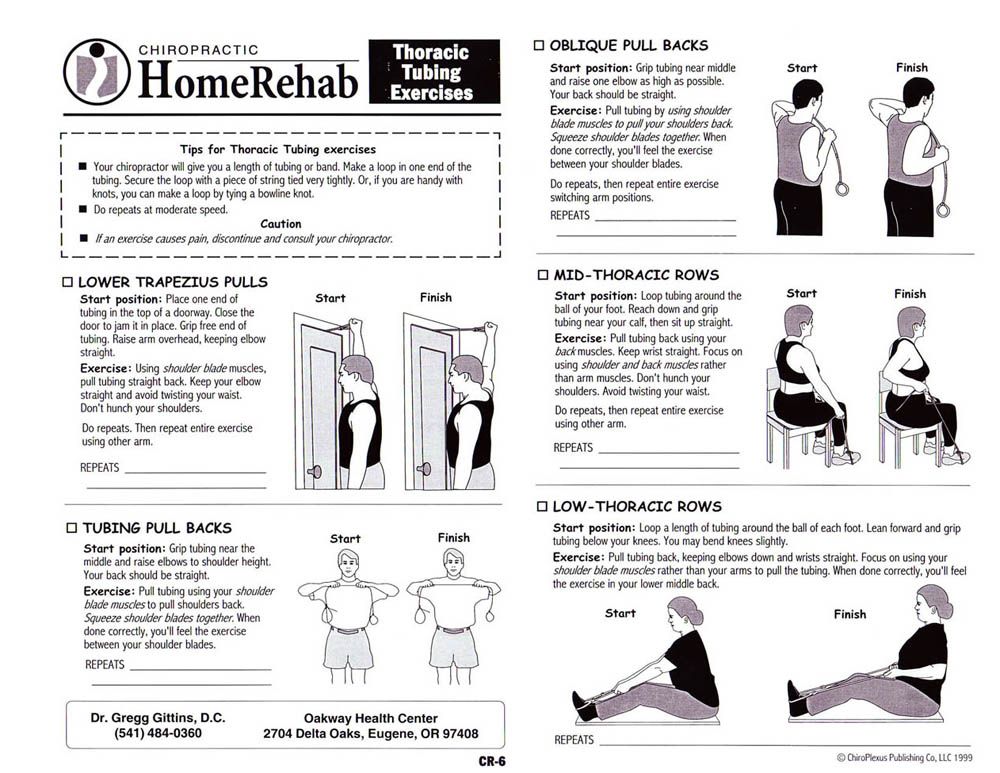
- Physiotherapy to relax and release tight back muscles.
- If you work at a computer – be sure to get up, move around, stretch, and loosen muscles every hour.
ANY activity that helps you relax can help alleviate tight muscles.
Therapy
Unidentified and unaddressed underlying factors cause issues with anxiety. As such, they are the primary reason why anxiety symptoms persist.[11][12][13]
Addressing your underlying factors (Level Two recovery) is most important if you want lasting success.
Addressing Level Two recovery can help you:
- Contain anxious behavior.
- Become unafraid of anxiety symptoms and the strong feelings of anxiety.
- End anxiety symptoms.
- Successfully address the underlying factors that so often cause issues with anxiety.
- End what can feel like out-of-control worry.
All our recommended anxiety therapists have had anxiety disorder and overcame it. Their personal experience with anxiety disorder and their Master's Degree and above professional training gives them insight other therapists don't have.
If you want to achieve lasting success over anxiety disorder, any one of our recommended therapists would be a good choice.
Working with an experienced anxiety disorder therapist is the most effective way to treat anxiety disorder, especially if you have persistent symptoms and difficulty containing anxious behavior, such as worry.
In many cases, working with an experienced therapist is the only way to overcome stubborn anxiety.
Anxiety Back Pain Frequent Questions
Can anxiety cause back pain?
Yes! Since anxiety stresses the body, and stress can cause muscle tension and back pain, anxiety can cause acute and chronic back pain symptoms. Stress, including anxiety-caused stress, is a common cause of persistent back problems, such as pain, tension, stiffness, soreness, pressure, spasms, and immobility.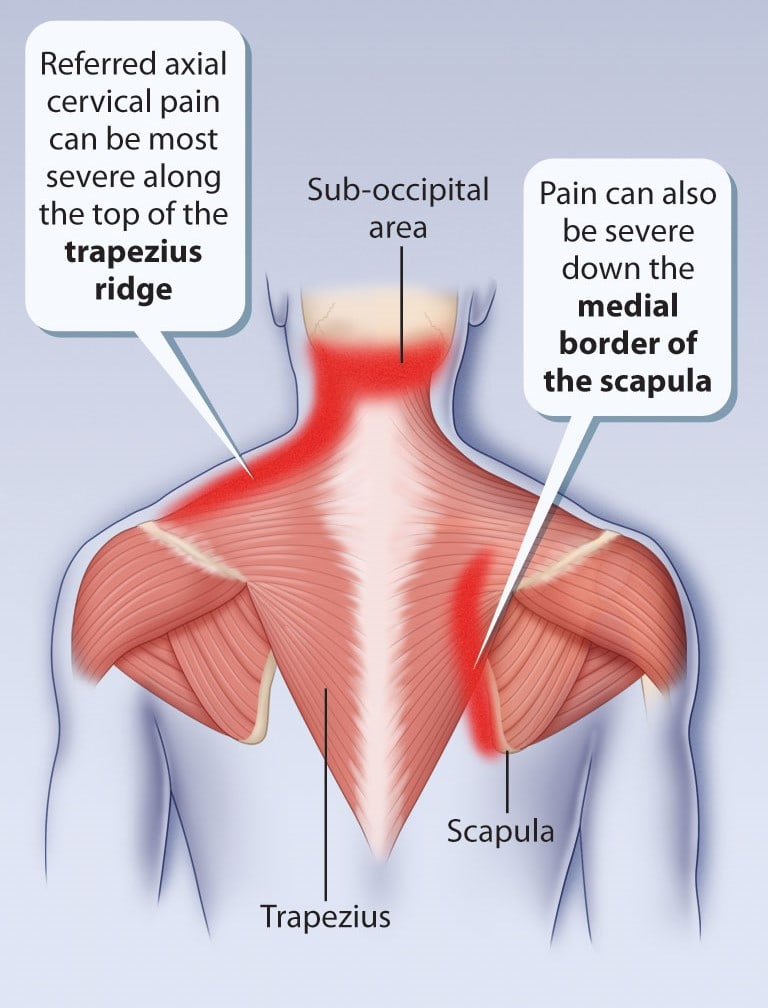
Can anxiety cause back pain at night?
Yes, anxiety can cause back pain at night. Many people notice their back pain is more severe and bothersome at night, causing problems with sleep.
Can anxiety back pain interfere with sleep?
Yes, anxiety back pain can cause problems with sleep, such as difficulty getting to sleep because of the pain, difficulty staying asleep because of being woken up with pain during the night, shorter restful sleep, and episodes of insomnia.
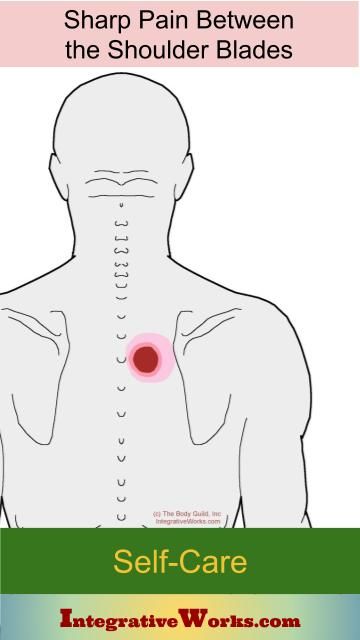
Can anxiety cause back pain between the shoulder blades?
Yes, anxiety can cause pain and burning between the shoulder blades. Many anxious people get back pain symptoms because of their anxiety issues, including between the shoulder blades.
Can anxiety cause a burning sensation in the back?
Yes, stress, including anxiety-caused stress, can cause pain and burning in the back and between the shoulder blades. Many anxious and stressed people get back pain and burning symptoms in the back.
Can back pain cause anxiety?
Anxiety is caused by apprehensive behavior. So back pain itself won’t cause anxiety. However, if you worry about back pain, worry can cause anxiety since worry is an example of apprehensive behavior.
Upper back pain between shoulder blades: Causes and treatment
Poor posture, injury, or problems with the spine can all lead to upper back pain. A common cause of pain between the shoulder blades is muscle strain.
Treatments for mild upper back pain include stretching exercises and pain relievers. Some cases of pain between the shoulder blades are preventable.
Someone with underlying spinal problems may need advice from a doctor or physical therapist to reduce pain and discomfort.
Share on PinterestStretching, maintaining good posture, relieving stress, and avoiding heavy lifting can help alleviate or prevent shoulder pain.There are several muscles of different shapes and sizes in the upper back, which help with neck, shoulder, and arm movements.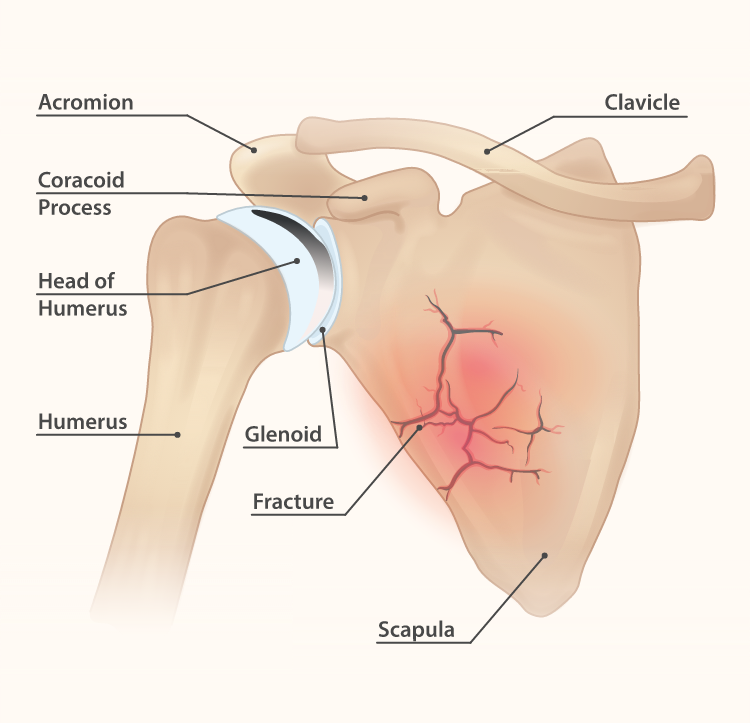
Injuries to these muscles can cause upper back pain. The feeling can be a dull ache or a sharp pain.
Exercise
Some forms of exercise increase the risk of injuring the upper back.
Throwing a ball overhead, lifting weights, and performing some swimming strokes can strain muscles between the shoulder blades. The repetition of these movements over time is a common cause of muscle strain.
Other symptoms of muscle strain include a feeling of weakness in the area, swelling, and muscle cramps.
People can treat a mild strain with ice, rest, and pain relievers. Most mild strains should heal within a couple of weeks.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce pain and swelling. It is important to try to avoid activities that strain the back muscles.
Applying an ice pack for up to 20 minutes every few hours can also reduce pain and swelling. Gently moving the shoulders at regular intervals can help reduce any stiffness.
Posture
How someone sits or stands can cause pain between the shoulder blades. Some positions that may put a strain on muscles in the upper back include:
Some positions that may put a strain on muscles in the upper back include:
- sitting at a desk for much of the day
- using an uncomfortable chair
- leaning over a laptop for long periods
- crossing the legs when sitting down
These postures can cause a dull ache between the shoulder blades.
Gently stretching the muscles in the upper back can help ease the pain. People can try rolling the shoulders forward and backward to reduce stiffness. Linking the hands behind the back and gently pulling the arms downward might also help.
Stress
Stress causes muscles in the body to become tense. The neck and shoulders are a common area of tension, which can cause pain between the shoulder blades.
Stress can also cause headaches if the shoulder muscles are tense for a long time.
Addressing the causes of stress, having a good support network, getting enough sleep, and exercising regularly can all reduce stress.
Lifting or carrying
Carrying or lifting something heavy can strain the upper back.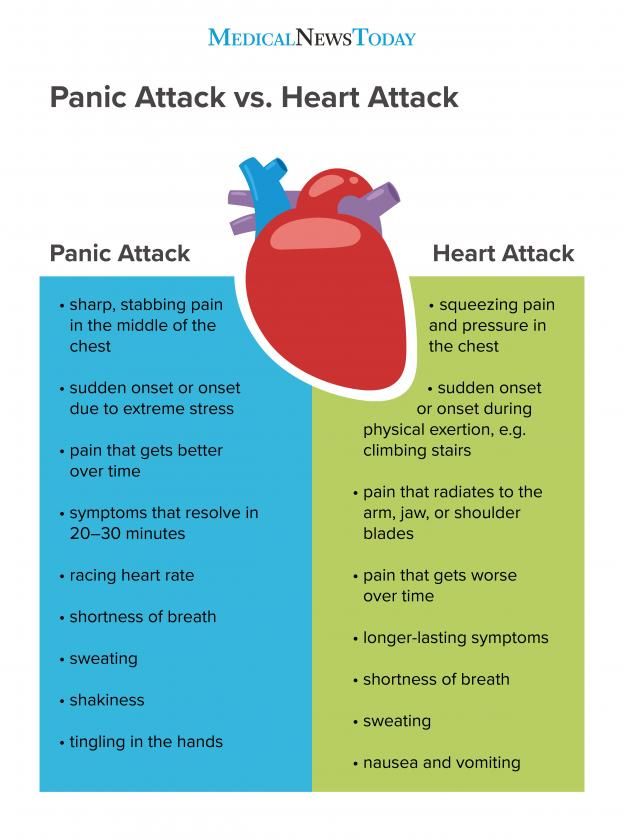 People should take care to use safe lifting practices when pushing, pulling, or lifting items.
People should take care to use safe lifting practices when pushing, pulling, or lifting items.
Carrying a shoulder bag puts weight on the shoulders, pulling on the muscles between the shoulder blades. Holding heavy shopping bags can also strain the arms and the muscles in the upper back.
People can avoid carrying too much weight on the shoulders by choosing backpacks with two straps to spread weight evenly and only carrying essential items. If necessary, a person can make more than one trip to avoid carrying several heavy bags at once.
Muscle injury
Injury to muscles in the upper back can cause pain between the shoulder blades.
Injuries might occur as a result of exercising, lifting something heavy, or falling. A tear can cause severe pain.
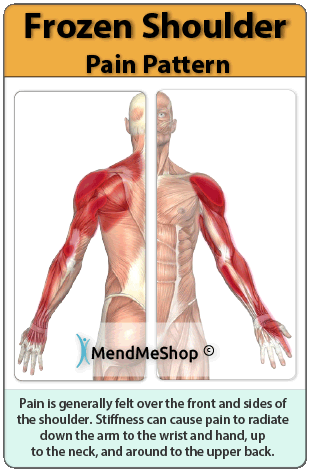
The rotator cuff muscles attach the arm to the shoulder blade. Injuring one or more of these muscles can cause pain in the upper back and shoulder. Such injuries can also cause difficulty in moving the arm or shoulder.
Treatment for mild or moderate muscle tears includes resting, applying an ice pack, and doing strengthening exercises. In some cases, a doctor may prescribe steroid injections to reduce swelling.
For about 20% of rotator cuff injuries, surgery is necessary to reattach a tendon.
Scoliosis
Scoliosis is a condition in which the spine has a sideways curve. A person’s shoulders or hips may look slightly uneven, or one shoulder might stick out.
Scoliosis does not always cause symptoms, but some people with this condition may experience back pain. Exercise will help strengthen muscles in the upper back and shoulders, which can reduce muscle strain and pain.
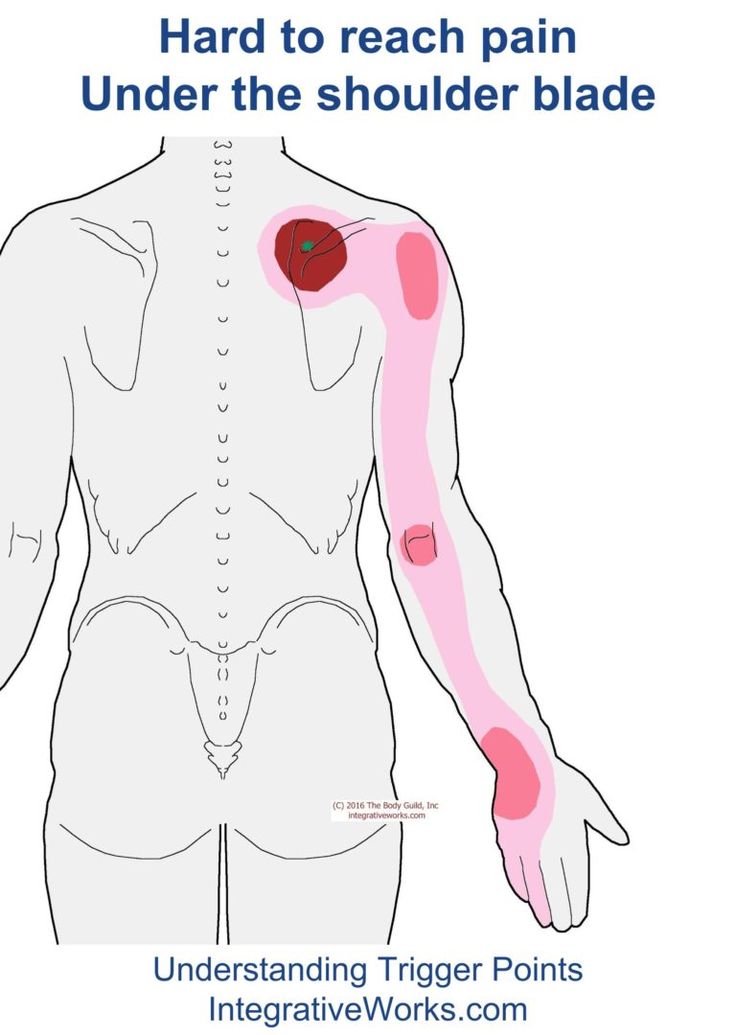
Myofascial pain syndrome
Myofascial pain syndrome is a long-term health condition that causes pain in specific muscle groups. Unlike with other chronic pain conditions, pain does not occur throughout the body.
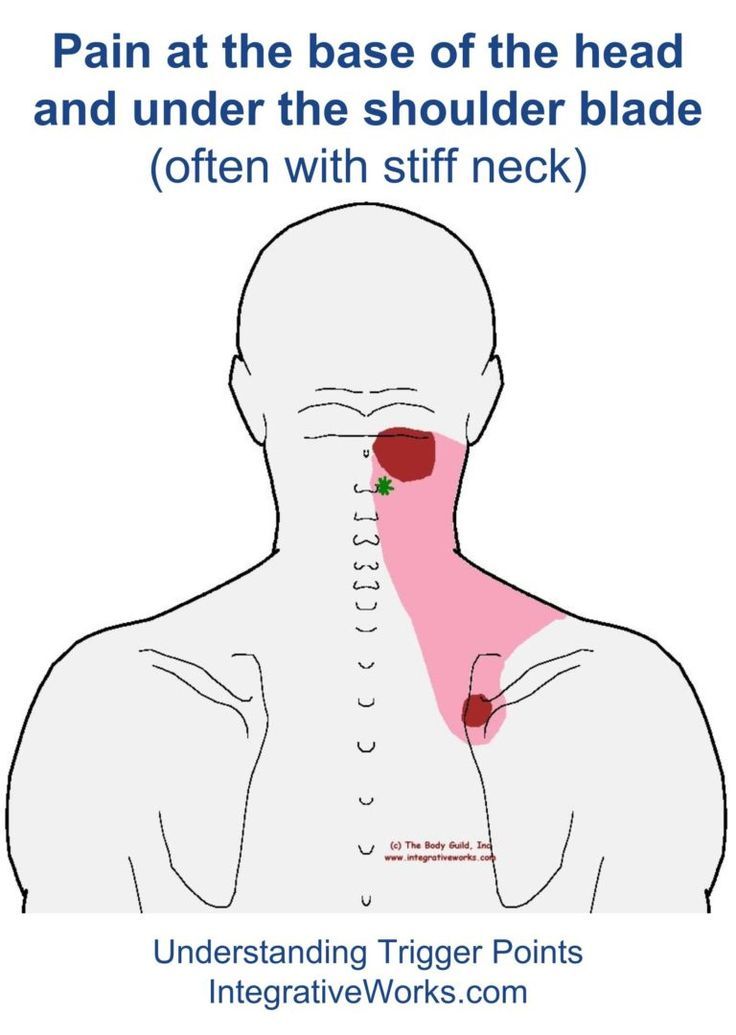
A trigger point in a muscle will cause pain in the area. In the upper back, it may cause pain across the group of muscles around the spine, neck, and shoulders.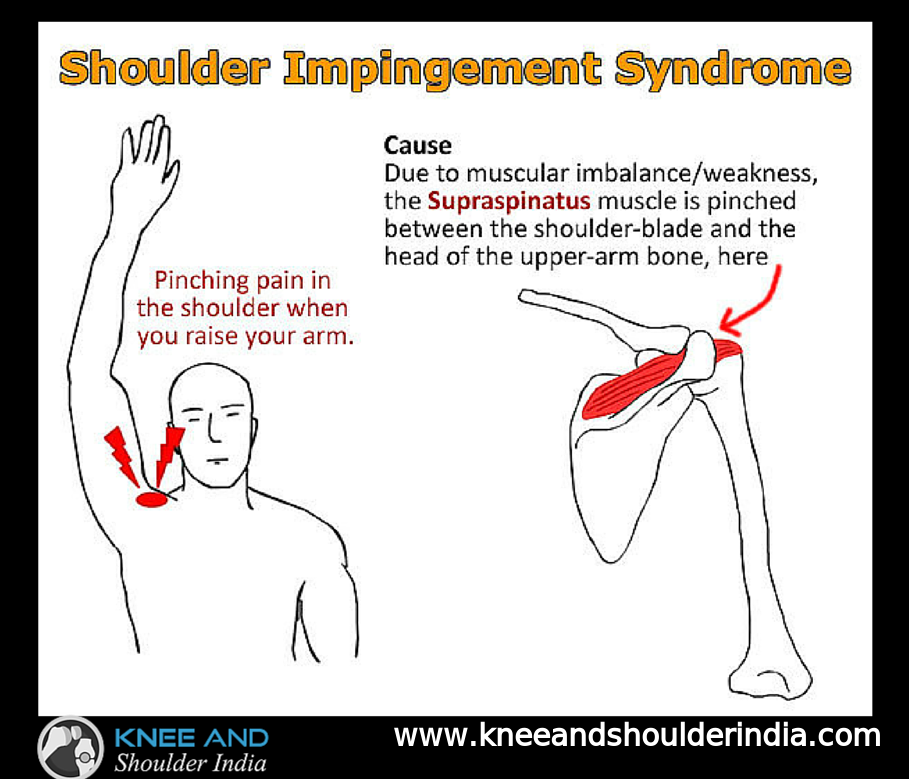
Treatment can include laser therapy, steroid injections, lifestyle changes, and massage.
Osteoarthritis
Gradual wear and tear of the joints over time can cause osteoarthritis. The symptoms include stiffness, pain, and swelling, which can cause difficulty in moving the joints.
Injuring or overusing the joints can increase the risk of osteoarthritis.
Some people have a job that requires frequent reaching overhead or heavy lifting. This work can lead to osteoarthritis in the shoulder joints and upper back pain later in life.
Maintaining good posture, keeping the muscles in the shoulders and upper back strong, and avoiding heavy lifting can help prevent pain between the shoulder blades.
People who sit at a desk for long periods may benefit from a comfortable chair to prevent upper back pain. They should try to keep the spine in a natural position without hunching the shoulders or pushing the neck forward.
Regular exercise can help a person maintain a moderate weight, which reduces strain on the back.
Stress can cause tension in the upper back and shoulders. Yoga or stretching exercises can help ease tight muscles.
It is easy to strain muscles in the upper back and cause pain between the shoulder blades. Common causes are leaning over a laptop, carrying heavy bags, or sitting in an uncomfortable seat for long periods.
Most causes of upper back pain are mild. However, some more serious problems can cause pain between the shoulder blades. It is important to seek medical advice for symptoms of scoliosis, osteoarthritis, or a muscle tear.
Pain between the shoulder blades: why it occurs and how to deal with it
Pain in the area of the shoulder blades happens quite often. It can be aching, dull or sharp. Sometimes it becomes a signal of serious health problems. What to do if you are worried about pain in the area of the shoulder blades, we are dealing with the neurologist of the Atlas Medical Center Alexander Gravchikov.
Causes of pain between the shoulder blades
There are many possible causes of shoulder pain.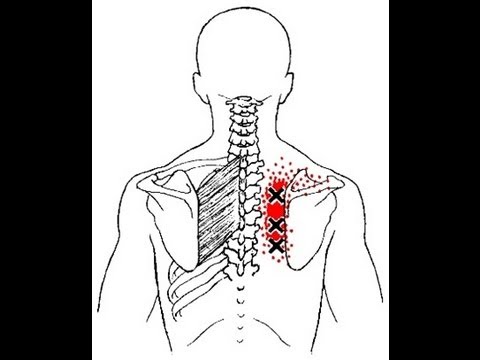
Alexander Gravchikov
neurologist of the medical center "Atlas"
- Pain between the shoulder blades or, more precisely, pain along the back of the back at the level of the thoracic spine occurs in every fourth person out of a hundred. And if pains at the level of the cervical and lumbar regions are studied quite well, then the causes of pain in the thoracic region are not always unambiguous. These can be:
- lesions of musculoskeletal structures in this area. It is common and does not pose a threat to life;
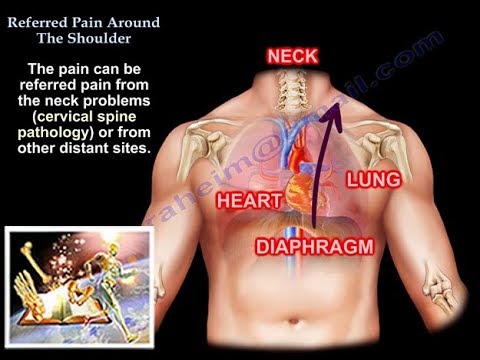
- serious diseases of internal organs - pathology of the heart and blood vessels, lungs, gastrointestinal tract, kidneys. In this case, pain can be reflected in the interscapular region;
- specific lesion of the spine due to inflammation, cancer or trauma.
All patients with pain in the interscapular region must undergo an ECG and, if necessary, other additional studies.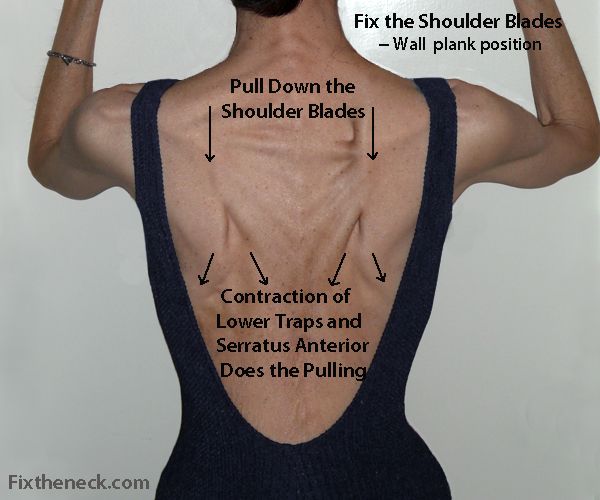
Sometimes pain in the shoulder blades can be a symptom of a heart attack, especially in women. In this case, it may be accompanied by discomfort in the chest area and difficulty in breathing. Acute, very intense pain in the middle and upper back can be caused by a diaphragmatic rupture or aortic dissection.
Pain between the shoulder blades: when to see a doctor
Pain is a signal that something is wrong with the body. If the pain between the shoulder blades does not go away within a few days, its cause should be determined. But if the pain is intense, accompanied by certain symptoms, this may mean that the condition is life-threatening and the person needs emergency medical care.
Alexander Gravchikov
neurologist of the medical center "Atlas"
— Doctors call “red flags” such symptoms 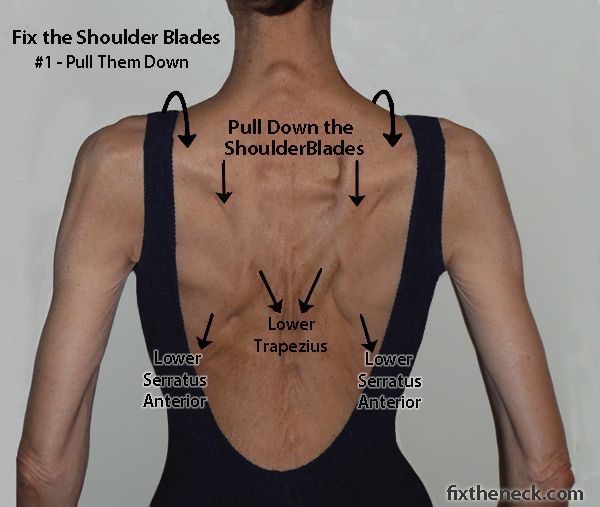 ), oncological diseases,
), oncological diseases,
Diagnostics for pain between the shoulder blades
First of all, in patients with pain between the shoulder blades, “red flags” are excluded. If there is a suspicion of a pathology of the internal organs or a specific lesion of the spine, an in-depth examination is carried out. If there are no such signs, the doctor will examine the muscles, spine and ribs. A standard neurological examination reveals damage to individual nerve roots and the spinal cord.
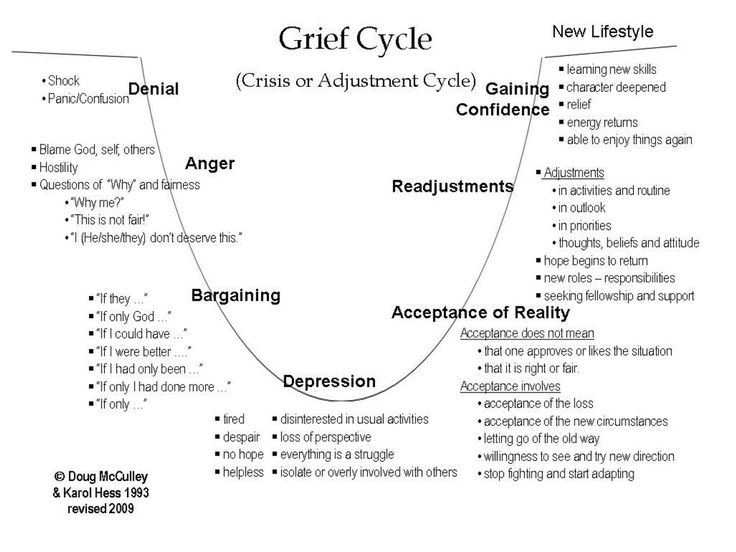
Chronic long-term pain may require psychotherapy and assessment of anxiety and depressive disorders.
If there is a suspicion of a tumor, inflammatory changes in the spine, anomalies in its development, fractures, then additional examination methods are needed:
- X-ray of the thoracic spine,
- computed or magnetic resonance imaging of the thoracic spine.
Alexander Gravchikov
neurologist of the medical center "Atlas"
- If serious causes of pain between the shoulder blades are excluded, then most likely it is musculoskeletal (non-specific) pain. It can be caused by:
- changes in the joints of the spine or joints between the ribs and the spine (facet syndrome). It occurs with sudden movements associated with the rotation of the body, when lifting and carrying weights, with a long stay in a static position, working with raised arms. This leads to overload of the joints and irritation of their capsules;
- myofascial pain syndrome.
 At the same time, the cause of suffering is not associated with damage to the spine, but lies in a change in the muscles. Such pain is manifested by muscle tension and the formation of special seals (trigger points) in them. They occur due to excessive stretching of the muscles if the body was not prepared for movement, prolonged exposure to an uncomfortable position, or exposure to cold (rarely high temperature). "Nourishing soil" for the development of myofascial pain syndrome are violations of the biomechanics of the body, such as different leg lengths, flat feet, pelvic distortions, and the like, as well as psychological disorders accompanied by depression, anxiety, sleep disorders. The nature of nutrition and metabolic disorders matter.
At the same time, the cause of suffering is not associated with damage to the spine, but lies in a change in the muscles. Such pain is manifested by muscle tension and the formation of special seals (trigger points) in them. They occur due to excessive stretching of the muscles if the body was not prepared for movement, prolonged exposure to an uncomfortable position, or exposure to cold (rarely high temperature). "Nourishing soil" for the development of myofascial pain syndrome are violations of the biomechanics of the body, such as different leg lengths, flat feet, pelvic distortions, and the like, as well as psychological disorders accompanied by depression, anxiety, sleep disorders. The nature of nutrition and metabolic disorders matter.
Treatment of pain between the shoulder blades
In many cases, especially if the cause of the pain is high muscle strain or injury, massage or physical therapy will help. The masseur can work out the area between the shoulder blades and relax the muscles. You can also purchase special devices for self-massage. If you have an injury or nerve entrapment, your doctor may refer you to a physical therapist who can tell you which exercises to do for you.
You can also purchase special devices for self-massage. If you have an injury or nerve entrapment, your doctor may refer you to a physical therapist who can tell you which exercises to do for you.
Alexander Gravchikov
neurologist of the medical center "Atlas"
— For acute pain, non-steroidal anti-inflammatory drugs (NSAIDs) and paracetamol are primarily used in combination with drugs that relieve muscle tension (muscle relaxants). It is justified to use blockades and hormonal drugs at points as close as possible to the source of pain.
Non-drug therapy is also important. The most effective manual therapy, which allows you to remove articular blocks. Massage, acupuncture, physiotherapy may be helpful. If there is a threat of damage to the spinal cord (myelopathy) or conservative treatment is ineffective, surgery may be required.
Self-care measures for pain between shoulder blades
If critical cases are excluded and your pain is not dangerous, you can relieve it in ways available at home.
Training
Physical activity has a positive effect on health, and in cases where pain in the shoulder blades bothers you, it is necessary to strengthen the muscles. After consulting with your doctor first and outside of the acute period, try doing pull-ups, push-ups, and other exercises to develop a strong back.
Stretch
Yoga, Pilates, stretching improve blood circulation and nutrition of muscles and joints, which has a positive effect on
mobility and relieves pain. Try this simple exercise:
- Extend your straight arm diagonally in front of you.
- With your free hand, try to pull her closer to you.
- Hold this position for 10 seconds.
- Repeat on the other side.
Certain foods can cause inflammation in the body and make your symptoms worse. Avoid processed foods, eat more vegetables and fruits, and foods rich in omega-3 fatty acids.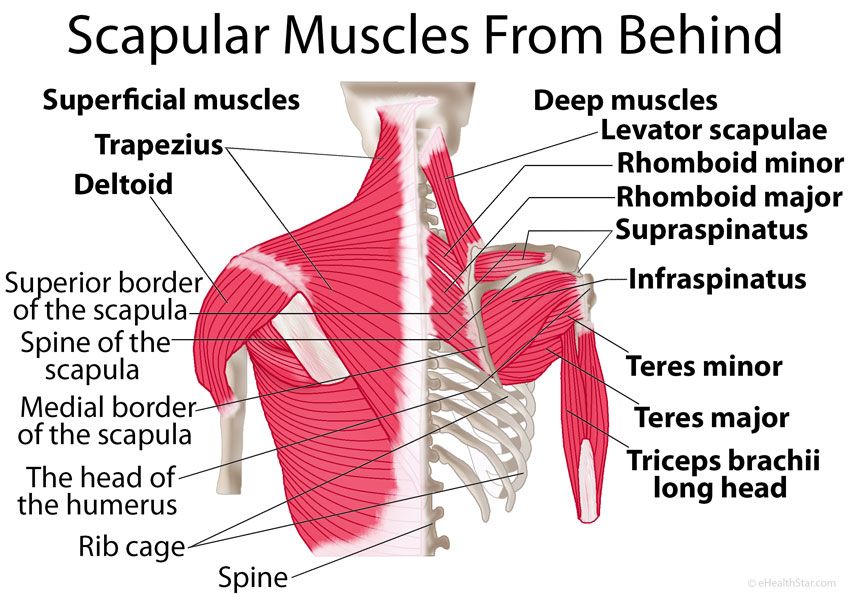
Sometimes you can get rid of pain in the shoulder blades simply by allowing yourself to rest for a couple of days. This is especially true if the pain is caused by an injury.
Prevention of pain between the shoulder blades
To prevent shoulder pain, follow our tips:
- Watch your posture. Try to stand and sit straight, do not slouch. You may need a special ergonomic chair or pillow to support your lower back.
- Do not lift heavy objects. If you train with weights, follow the technique of the exercises and work with the right weight. In everyday life, do not carry heavy bags on one shoulder.
- Don't sit too long. Get up from your desk often to stretch.
- Get used to good things. Eat right, sleep 7-8 hours a night, exercise at least three times a week. A healthy lifestyle will make you feel rested and energized, which will help you cope with pain.
Subscribe to The Challenger!
Share
In case of pain in the back and joints, the muscles must also be treated Medical On Group Tyumen
The occurrence of pain is an alarming signal of the body that a problem is developing in a certain area. Many reasons can lead to the occurrence of such discomfort. The most common culprits are degenerative-dystrophic processes (osteochondrosis, arthrosis), as well as various injuries, whether it be bruises, torn ligaments, or even just sprains or overstrain of untrained muscles.
Excessive loads on the elements of the musculoskeletal system or their physiological aging provokes the development of diseases.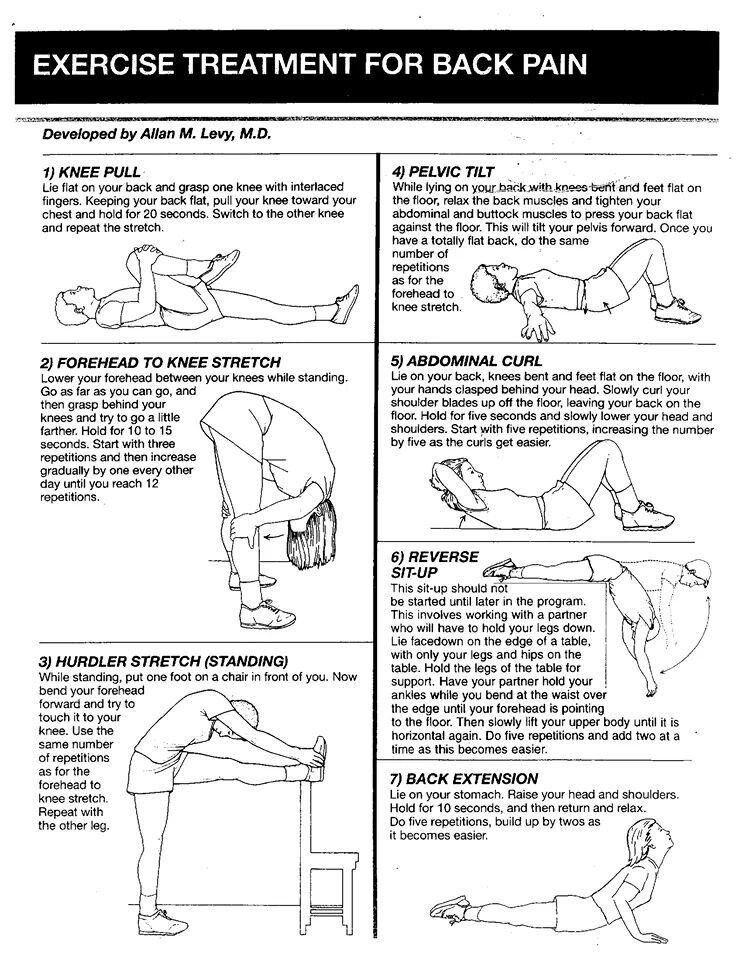 Therefore, even minor pains can be harbingers or causes of serious problems. Timely access to a doctor and proper treatment will allow: to prevent the progression of the pathology, relieve pain, prevent the occurrence of complications, as well as improve the prognosis of treatment and, in most cases, it will be possible to recover or achieve stable remission and prevent the disease from developing further. This improves the quality of life and restores working capacity.
Therefore, even minor pains can be harbingers or causes of serious problems. Timely access to a doctor and proper treatment will allow: to prevent the progression of the pathology, relieve pain, prevent the occurrence of complications, as well as improve the prognosis of treatment and, in most cases, it will be possible to recover or achieve stable remission and prevent the disease from developing further. This improves the quality of life and restores working capacity.
Pain in any location, for any reason, can trigger a "chain reaction" called myofascial pain syndrome. A person intuitively tries to choose the most comfortable position during pain, and even the usual movements are performed differently - those muscles that were previously used to a lesser extent begin to be actively involved. The body seeks to create a muscular frame in order to immobilize the painful area. Subsequently, it is precisely those muscles that have taken on an additional load that cause the occurrence of myofascial pain syndrome.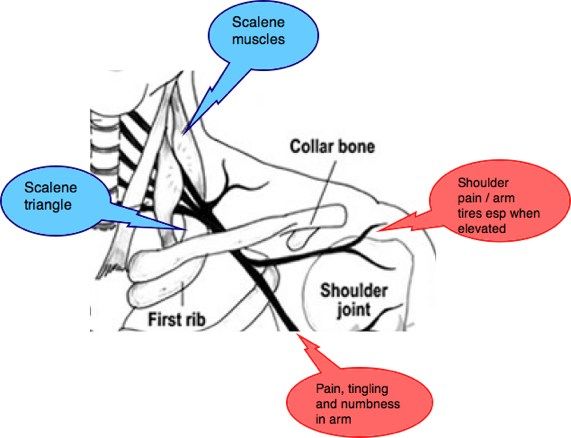
Myofascial pain syndrome (MBS) is a chronic, pathological condition caused by the formation of local muscle spasms or indurations represented by pain points (triggers). Pain can be provoked by pressing on these points, or by the movement of the muscles involved in the pathological process. This syndrome leads to limited range of motion and increased muscle fatigue.
When MBS occurs, pain spreads through the muscles from the source to the surrounding soft tissues, which is manifested by the appearance of new painful seals (pain points). These areas of muscle compaction are not large and have a diameter of 0.1-0.3 cm, but if a large number of them appear, they are grouped, thereby creating a trigger zone with a diameter of 1 cm or more. The appearance of pain points occurs with overstrain and microtraumatization of the muscle. MBS can cause a violation of the normal distribution of loads in the nearest joints and lead to early wear and even deformation (curvature).
Predisposing factors for the appearance of MBS are:
- Pathology of the spine. Degenerative-dystrophic diseases (osteochondrosis of any localization, arthrosis of the intervertebral joints), spinal injuries are a source of pain that provokes the back muscles to maintain an increased tone. Also, a factor provoking the occurrence of SMEs becomes a forced, due to pain, static position, which causes muscle strain.
- Pathology of the musculoskeletal system. spinal deformity, asymmetry of the lower extremities (one-sided shortening), asymmetry (skew) of the pelvis, transverse and longitudinal flat feet can lead to an incorrect, uneven distribution of the load on the muscles, as well as cartilage and bones of the body, which will determine the occurrence of not only MBS, but also diseases such as arthrosis, arthritis, synovitis, ligamentitis. 70% of the population has scoliotic spinal deformity and 50% flat feet of varying degrees.
- Forced posture.
 Work in a monotonous position of the body, fixation of the limbs, a static position lead to muscle overload.
Work in a monotonous position of the body, fixation of the limbs, a static position lead to muscle overload. - stereotyped movements. The same repetitive movements occur with the contraction of the same muscles, leading to their overstrain and improper distribution of tone.
- Inadequate loading, especially of untrained muscles. As a result, muscle strain and micro tears occur.
- bruises. Direct trauma to the muscle itself causes a violation of the structure of its fibers. The consequence of this is a violation of the function, if the function of some fibers decreases, then the function of others should increase, compensating for the lack of the first, which leads to an overload of the latter.
- Somatic diseases. Soreness of the internal organs, provokes tonic tension of certain muscle groups. With prolonged persistence of the pain syndrome, trigger points and chronic severe pain syndrome may form.
- Emotional overstrain. Various psycho-emotional reactions, such as stress, anxiety, can induce muscles to tonic tension.
 In turn, the occurrence of muscular-tonic states, and their persistence after an emotional experience, are capable of forming MBS and the gradual development of chronic back pain (osteochondrosis) radiating to the limbs.
In turn, the occurrence of muscular-tonic states, and their persistence after an emotional experience, are capable of forming MBS and the gradual development of chronic back pain (osteochondrosis) radiating to the limbs.
As a result of microtrauma or muscle overload, there is a violation of the transport of substances through the cell wall. Calcium ions are released, which leads to damage at the cellular level. An excess amount of calcium provokes the contraction of the myocyte (muscle cell). A muscle that is in a spasmodic state provides an increase in intramuscular pressure, which leads to a deterioration in microcirculation. With a long contraction, a large amount of work is performed, for which energy is expended, a period of relaxation is required to replenish energy. If there is no relaxation period for a long time, compensation mechanisms work: the energy in the cell is replenished not at the expense of newly arrived nutrients from the bloodstream, but at the expense of the available reserves inside itself, which leads to inefficient work.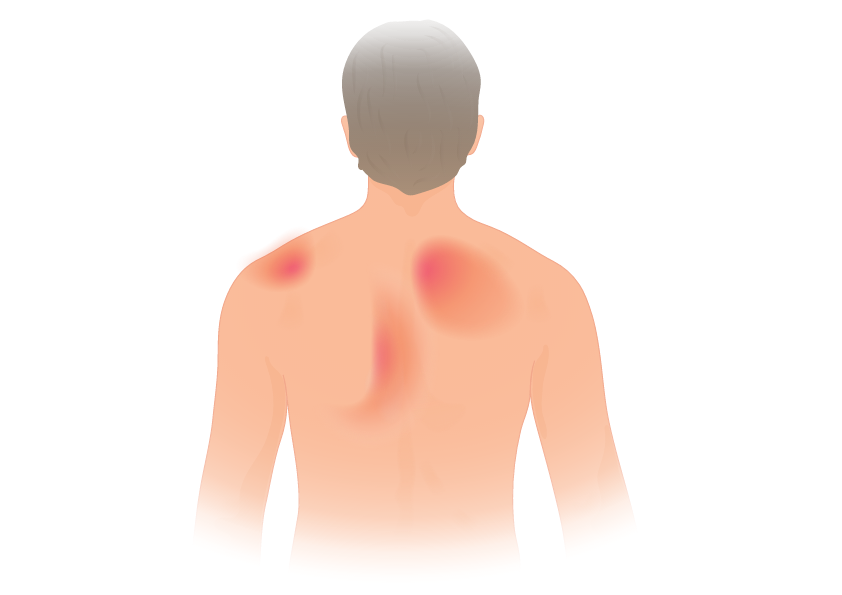 An even longer load, exceeding the capabilities of the muscle, causes a breakdown of compensatory mechanisms - the accumulation of toxins in the muscle tissue, and as a result, the formation of a trigger point. The resulting pain provokes muscle contraction. A vicious circle is formed: pain - muscle tension - pain. Also, a violation of the structure of the cartilage of the joint and bone can join this circle. When the pain spreads through the muscles, nerves may be involved, through which the pain syndrome can be transmitted to remote areas (for example, to give to the arms or legs with pain in the spine).
An even longer load, exceeding the capabilities of the muscle, causes a breakdown of compensatory mechanisms - the accumulation of toxins in the muscle tissue, and as a result, the formation of a trigger point. The resulting pain provokes muscle contraction. A vicious circle is formed: pain - muscle tension - pain. Also, a violation of the structure of the cartilage of the joint and bone can join this circle. When the pain spreads through the muscles, nerves may be involved, through which the pain syndrome can be transmitted to remote areas (for example, to give to the arms or legs with pain in the spine).
There are active and latent trigger points. Active pain points can appear during movement and even at rest. Latent points do not hurt at rest, but when you press them, a sharp pain occurs. There are 3 forms of myofascial pain syndrome: acute, subacute and chronic. In the acute form, the pain syndrome is maintained constantly and intensifies with movements. The subacute form is characterized by pain only during movements, and does not manifest itself at rest. In the chronic form of MBS, pain occurs only when the trigger point itself is pressed directly, and a feeling of discomfort may appear during movements.
In the chronic form of MBS, pain occurs only when the trigger point itself is pressed directly, and a feeling of discomfort may appear during movements.
Understanding the cause of the disease is required to select the right treatment. Therefore, in practice, the classification of MBS by etiology is used: it can be a primary myofascial pain syndrome, the root cause of which is direct damage to the muscle fiber - overstrain, microtears; as well as secondary MBS, the root cause in this case is pain in the joints, in the internal organs, in the spine.
MBS is not dangerous for life, but to a large extent it can worsen its quality, reduce working capacity and accelerate the wear of bone and cartilage structures of the musculoskeletal system. Chronic pain syndrome exhausts a person physically, has a bad effect on the psycho-emotional state, and can disturb sleep. Lack of sleep increases fatigue, negatively affecting life and work activity.
Most of the pain in degenerative pathologies of the musculoskeletal system is caused by myofascial pain syndrome.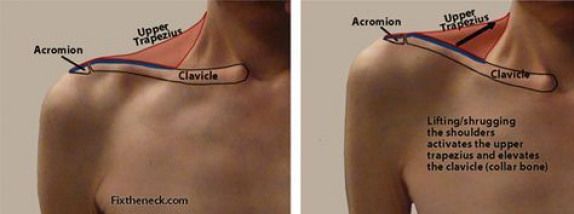 Even if you remove the primary source of pain, with an already formed MBS, the pain will not go away, moreover, the incorrect distribution of loads in neighboring areas from the affected muscles will provoke microtraumatization and inflammation. Therefore, it is important to treat not only arthrosis of the joints, protrusions and hernias of the intervertebral discs, bursitis, synovitis, but also the surrounding muscles.
Even if you remove the primary source of pain, with an already formed MBS, the pain will not go away, moreover, the incorrect distribution of loads in neighboring areas from the affected muscles will provoke microtraumatization and inflammation. Therefore, it is important to treat not only arthrosis of the joints, protrusions and hernias of the intervertebral discs, bursitis, synovitis, but also the surrounding muscles.
The advanced methods of treating myofascial syndrome are considered to be a set of measures that affect all links in the chain of pathological processes and provide relief from the primary source of pain, improve microcirculation in spasmodic muscles, by relaxing muscle tone and directly expanding the lumen of blood vessels, restoring intracellular metabolism and transport through the cell membrane, as well as stopping inflammation.
Combinations of some physiotherapy methods (Hil-therapy with a high-intensity laser, shock wave therapy, ultrasound treatment with medicines) with massage, various types of blockades, physical therapy and drug therapy, as well as the use of various orthopedic products, give a good effect.