Can anxiety cause ocd tendencies
Could OCD Be the Cause of Your Stress and Anxiety?
You have probably heard people casually refer to themselves or someone they know as having OCD or obsessive compulsive disorder, usually in reference to a quirky behavior they have related to being very clean or organized. But the term is often misused and misunderstood. OCD is a very real mental health disorder.
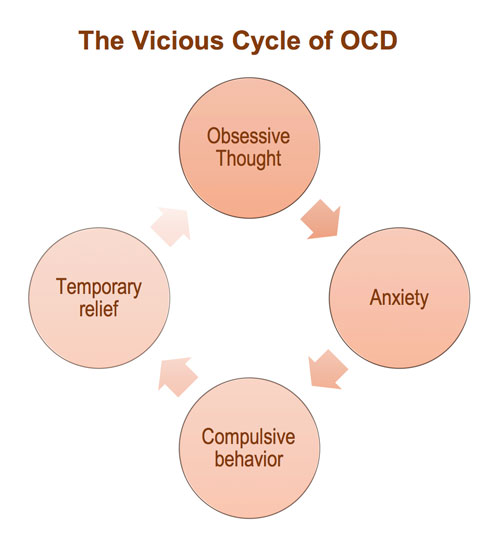
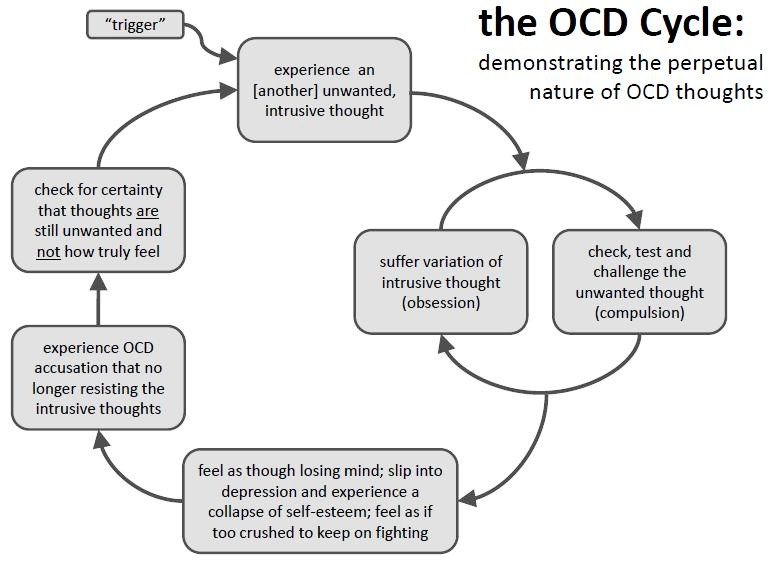
OCD stands for obsessive compulsive disorder. According to Dr. Jenys Allende, Executive Director for Mental Health Staffing at Legacy Treatment Services with locations throughout the state, including Northfield. OCD is a disorder which has intrusive thoughts that cause anxiety or stress. There may also be compulsions, which are mental or physical behaviors that an individual feels compelled to perform.
Dr. Allende gives the example of someone who is walking gingerly with a cake in their hand and you think for a moment of hitting the cake out of their hands.
“For someone without OCD, the thought lasts for a second and does not cause you any distress because it is something you would never do,” she said. “Now imagine you have OCD. That same person with the cake walks by and you think ‘I could just hit the cake out of their hands’. This time however you can’t stop thinking about it. Although you would not do it, still having this repetitive thought makes you feel like a bad person, and gives you anxiety. You have found that in these situations, arranging the books in your room by color helps you calm down. You feel so anxious you do the ritual but you miss an important meeting because you simply cannot stop arranging the books.”
What are the symptoms of OCD?
Dr. Allende said those with OCD have compulsions or rituals which are repetitive behaviors (e.g., washing, checking) or mental acts (e.g., praying, counting, repeating words silently) that the individual feels driven to perform in relation to an obsession or according to rules that must be applied rigidly or to achieve a sense of “completeness.”
Obsessions are repetitive and persistent thoughts (e. g., of contamination), images (e.g., of violent or horrific scenes), or urges (e.g., to stab someone). Obsessions are not pleasurable or experienced as voluntary. They are intrusive, unwanted, and cause marked distress or anxiety in most individuals. A person suffering from OCD attempts to ignore, avoid, or suppress obsessions or to neutralize them with another thought or action (e.g., performing a compulsion).
g., of contamination), images (e.g., of violent or horrific scenes), or urges (e.g., to stab someone). Obsessions are not pleasurable or experienced as voluntary. They are intrusive, unwanted, and cause marked distress or anxiety in most individuals. A person suffering from OCD attempts to ignore, avoid, or suppress obsessions or to neutralize them with another thought or action (e.g., performing a compulsion).
The most common categories for people with OCD
- Cleaning – Fears of contamination and cleaning rituals
- Symmetry – Symmetry obsessions and repeating, ordering, and counting compulsions
- Forbidden or taboo thoughts – Examples include aggressive, sexual, and religious obsessions, and related compulsions
- Harm (e.g., thoughts or images about harm befalling oneself or others and checking compulsions)
Habits can make the leap to needs
Dr. Allende explained that OCD gets thrown around as a term for someone who is rigid with their routine or worried about cleanliness.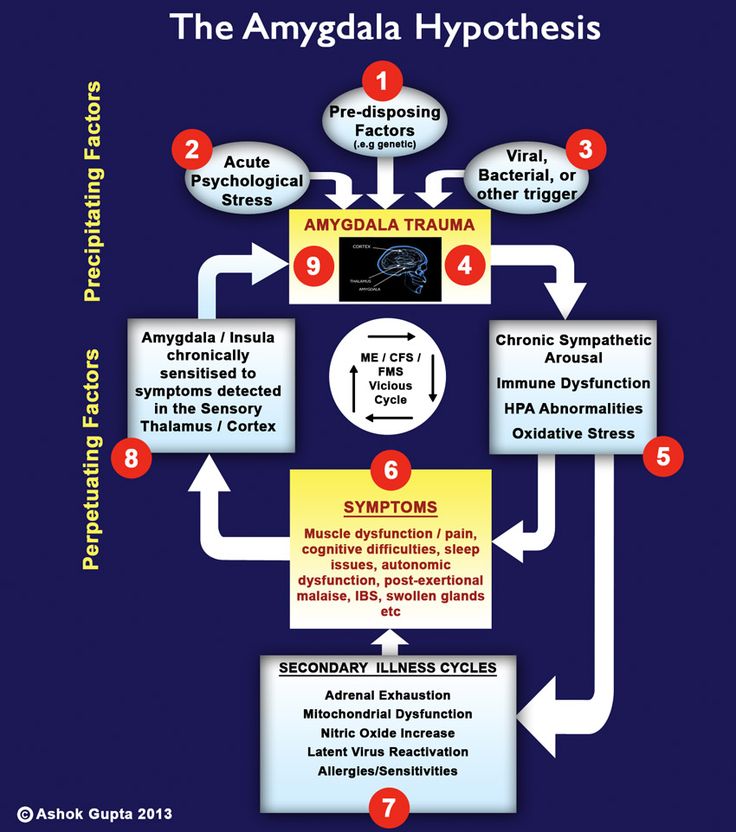 An obsession and or compulsion becomes OCD when it occurs most days for at least two weeks at a time. The obsession and/or compulsions also need to impair your ability to function, either because it causes significant distress or because it impairs your ability to perform daily activities. If a person is washing their hands a lot but they don’t really think about it twice, it is not OCD.
An obsession and or compulsion becomes OCD when it occurs most days for at least two weeks at a time. The obsession and/or compulsions also need to impair your ability to function, either because it causes significant distress or because it impairs your ability to perform daily activities. If a person is washing their hands a lot but they don’t really think about it twice, it is not OCD.
Whether those suffering with OCD will have both obsessions and compulsions or just one of them, Dr. Allende said it is difficult to answer. She indicated, epidemiological studies on OCD very rarely answer this question. Also, the disease is not very common as it affects only 1.2% of the population. Among those with OCD, it may take quite some time (up to nine years on average) for an individual to seek help for the disorder and the more severe the disease becomes, the more likely he/she will have both obsessions and compulsions
A Debilitating Disorder
OCD can be extremely debilitating, according to Dr.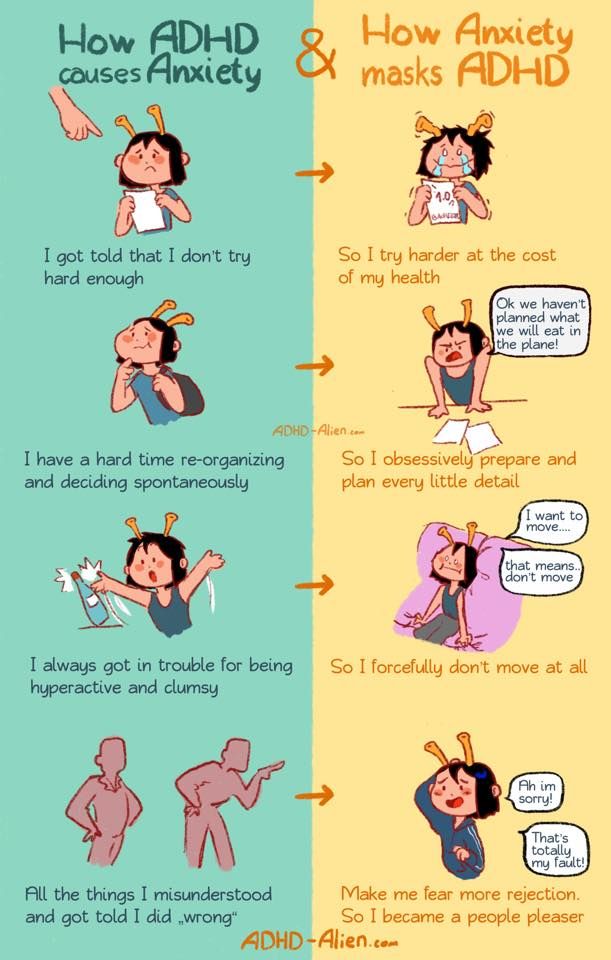 Allende. “I may be dating myself but there was a show on Nickelodeon called Double Dare in the 1990’s and its host was Mark Summers,” she said. “As a medical community, we have been very fortunate that Mr. Summers has shared his story many times to raise awareness for OCD. While on the show, Mr. Summers was always concerned about cleanliness and he got “slimed” every day. He describes rushing off set at the end of the show to immediately change his clothes. He also describes his compulsions of spending a lot of time arranging the tassels on his living room rug. He describes being labeled as difficult to work with and actually lost a job on Hollywood Squares due to his OCD and being labeled difficult. “
Allende. “I may be dating myself but there was a show on Nickelodeon called Double Dare in the 1990’s and its host was Mark Summers,” she said. “As a medical community, we have been very fortunate that Mr. Summers has shared his story many times to raise awareness for OCD. While on the show, Mr. Summers was always concerned about cleanliness and he got “slimed” every day. He describes rushing off set at the end of the show to immediately change his clothes. He also describes his compulsions of spending a lot of time arranging the tassels on his living room rug. He describes being labeled as difficult to work with and actually lost a job on Hollywood Squares due to his OCD and being labeled difficult. “
Dr. Allende added that her patients have had trouble completing school, difficulty with social situations to complete disability due to OCD. “My most severe case spent so much time on rituals and was so anxious about obsessions that they could not care for their daughter, or work,” said Dr. Allende. “It can be devastating.”
Allende. “It can be devastating.”
OCD is associated with reduced quality of life as well as high levels of social and occupational impairment. This can include:
- Time spent obsessing and acting on compulsions;
- Avoidance of situations that may trigger obsessions or compulsions that severely restrict functioning;
- Specific symptoms that can create specific obstacles. As examples:
- Obsessions about harm that can make relationships with family and friends feel hazardous, resulting in avoidance;
- Obsessions about symmetry that can derail the timely completion of school or work projects because the project never feels “just right,” potentially resulting in school failure or job loss;
- Individuals with contamination concerns who may avoid physicians due to fears of exposure to germs;
- Patients who may develop dermatological problems, such as skin lesions due to excessive washing; and
- Sometimes the symptoms of OCD interfere with its own treatment, e.
 g., when medications are considered contaminated.
g., when medications are considered contaminated.
How do you help to break through to people with OCD?
Fortunately, people with OCD are usually aware that there is a problem, as they are distressed or anxious about their symptoms. Dr. Allende said that they tend to know that something is not right. As an intervention, you want to strive to understand how the person feels rather than labeling them. For example: “I see you counting a lot lately.
” She went on to explain, using statements takes some of the judgement from the intervention. Avoid labeling (you have OCD) as people tend to become more defensive when they are labeled.
“The person may not be ready to reach out and that is OK,” Dr. Allende said. “You may want to approach a family member or someone close to the person with your concern in order to engage the person with you and you may want to avoid the traditional interventions where many people talk to their loved one at once.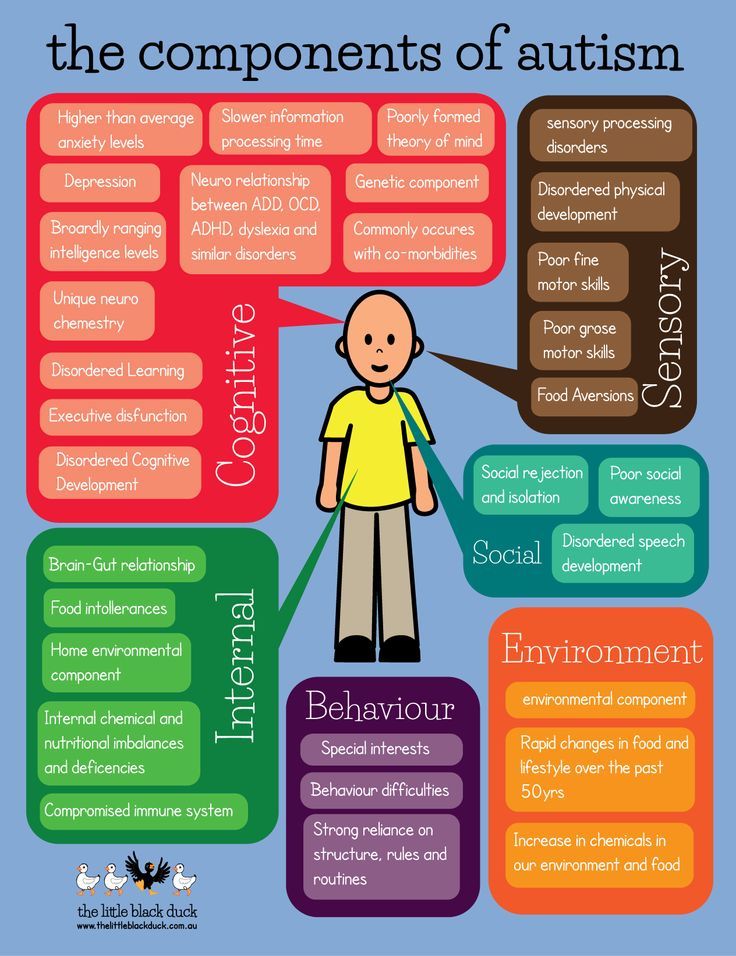 ”
”
Are OCD symptoms triggered?
According to Dr. Allende, something does not initially trigger OCD to emerge. She did add that OCD can emerge from head injuries or trauma, it is often a condition that develops in school-age children to young adults. An OCD episode can be triggered by anything that causes, stress, anxiety, and especially a feeling of lack of control. For example, if a person with OCD develops cancer, which can certainly trigger obsessions and compulsions, especially with cleanliness.
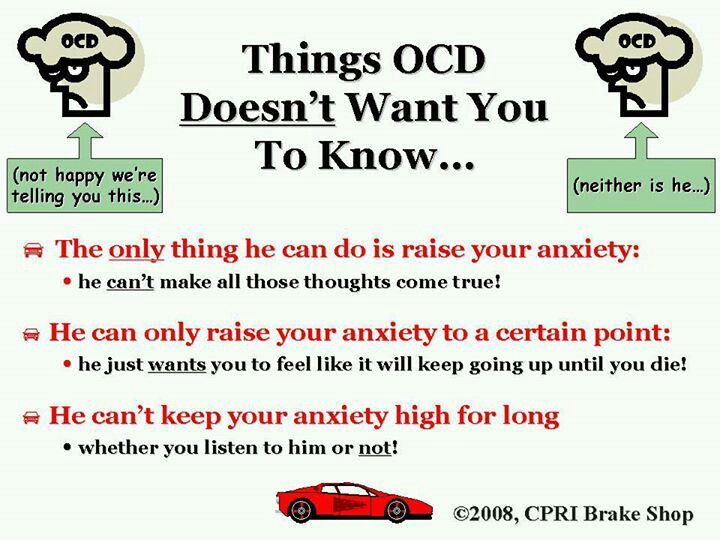
In OCD the first step is to recognize the feeling that leads to worsening obsessions or compulsions, explained Dr. Allende. “Anxiety can easily lead to an OCD, episode therefore a person can learn to recognize when they are anxious and use coping skills for the anxiety. Cognitive Behavioral Therapy is first line for OCD.” She added, “During therapy you do learn to recognize environmental triggers and use these triggers in exposure and response prevention. For example, an obsession with germs may be triggered by a doorknob as it may have germs. Exposure and response prevention exposes the patient to the doorknob for incrementally longer periods of time, while giving the patient coping skills such as breathing techniques, imagery, etc. to combat the feeling of anxiety. “
For example, an obsession with germs may be triggered by a doorknob as it may have germs. Exposure and response prevention exposes the patient to the doorknob for incrementally longer periods of time, while giving the patient coping skills such as breathing techniques, imagery, etc. to combat the feeling of anxiety. “
Coping skills for OCD
According to Dr. Allende, the goal for these intrusive and distressing thoughts is to recognize them as an unwelcome intrusion and allow them to pass by. For example, a patient may have an obsession with becoming aggressive. When this thought enters his mind, he is distressed by it since he would never hurt anyone. What follows can be a lot of negative self-talk (I am a terrible person, why do I want to hurt people). “I want people to turn it into the lady with the cake scenario,” said Dr. Allende. “You can have the obsessive thought and brush it off with “I would never do that”, rather than dwelling on the thought. Distraction techniques can be helpful in these circumstances.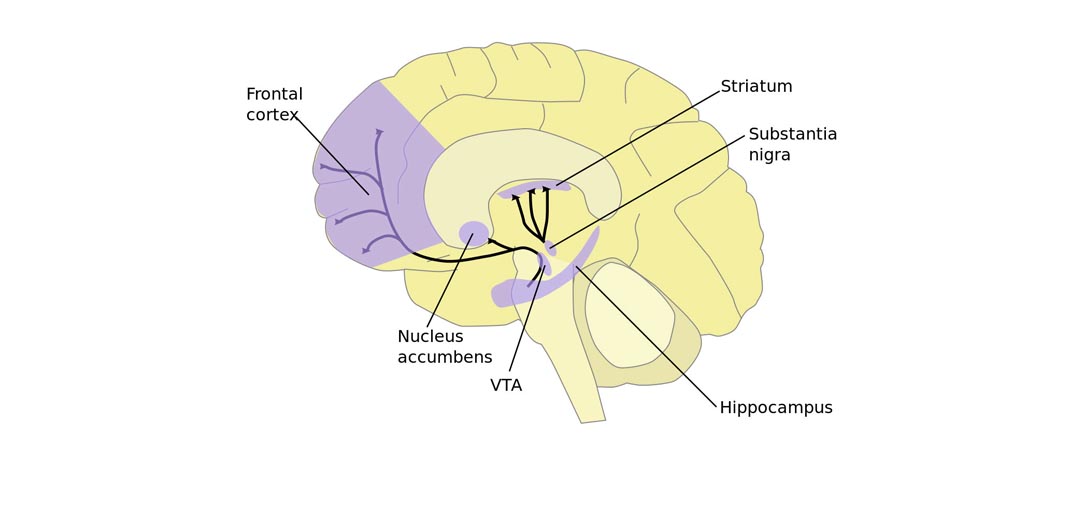 In OCD we are trying to extinguish or prevent thoughts, rather than analyzing them. The goal is to focus on obsession for smaller amounts of time and for this reason, journaling the thoughts would not be a recommended activity.”
In OCD we are trying to extinguish or prevent thoughts, rather than analyzing them. The goal is to focus on obsession for smaller amounts of time and for this reason, journaling the thoughts would not be a recommended activity.”
Treatments for OCD
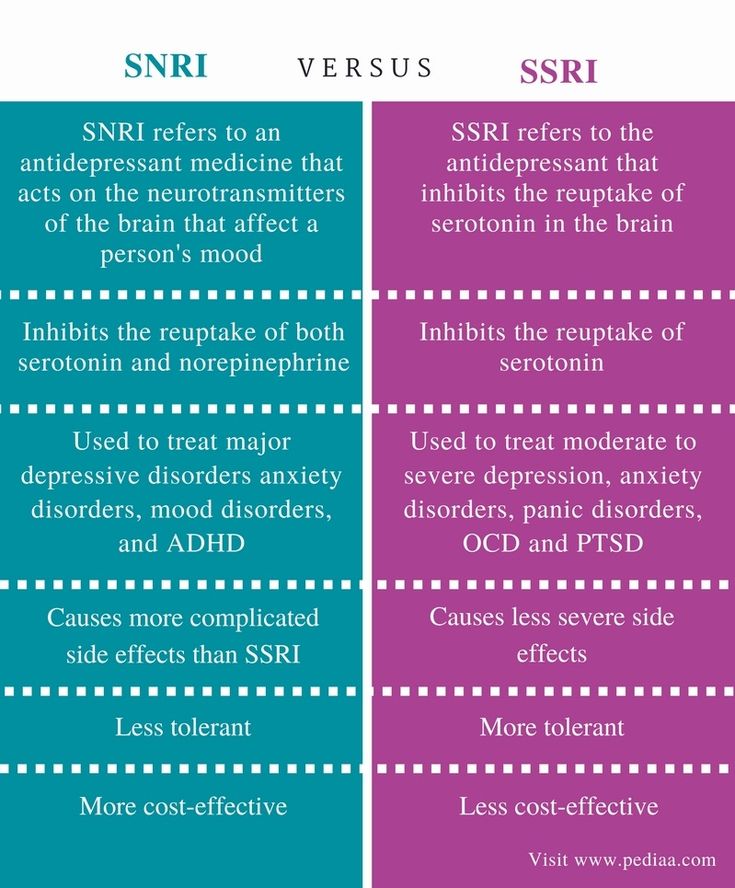
What treatment Dr. Allende recommends is based on each individual’s presentation. Some patients may be so anxious and overwhelmed that they are not able to participate in cognitive behavioral therapy (CBT), so medication may be best to start with. Other patients may present with milder cases when they can discuss their symptoms and they may be able to start with just CBT.
Cognitive behavioral therapy in addition to exposure and response prevention is the first-line treatment, according to Dr. Allende.
” Studies have found that medications with high serotonergic are the best choices for OCD,” she said. “First lines are the selective serotonin reuptake inhibitors (or SSRI’s) with the exclusion of Celexa and Lexapro. All other SSRI’s have an FDA indication for OCD. Clomipramine (an older tricyclic antidepressant) also has an indication for OCD; however, I do not use it first line due to its side effects (which include sedation, and dry mouth). The other concern with Clomipramine is that in overdose it can be fatal. With all psychiatric disorders there is always the possibility of suicide, therefore it is good practice to start with medications that cause the least harm in overdose first.”
All other SSRI’s have an FDA indication for OCD. Clomipramine (an older tricyclic antidepressant) also has an indication for OCD; however, I do not use it first line due to its side effects (which include sedation, and dry mouth). The other concern with Clomipramine is that in overdose it can be fatal. With all psychiatric disorders there is always the possibility of suicide, therefore it is good practice to start with medications that cause the least harm in overdose first.”
Is OCD hereditary?
Dr. Allende indicated that while OCD is not directly hereditary (as in if your mother has OCD, you have a 50% chance of getting OCD), there is a genetic component. Twin and familial studies of patients with OCD show a genetic component most prevalent in childhood onset OCD.
Can OCD be cured?
“I watched an interview with Mark Summers recently and when asked if he was cured, he said ‘80% cured - I don’t think I will ever be 100% cured’,” Dr. Allende said. “In 40-60% of patients with OCD, I see significant improvement with CBT and or SSRI’s. However, OCD at its core is an anxiety disorder. There are points in your life when you are going to be anxious and the severity of that anxiety can trigger OCD symptoms.
Allende said. “In 40-60% of patients with OCD, I see significant improvement with CBT and or SSRI’s. However, OCD at its core is an anxiety disorder. There are points in your life when you are going to be anxious and the severity of that anxiety can trigger OCD symptoms.
“I often tell my patients that everyone has a struggle. Some are diabetic, dyslexic, a worrier, or a person with OCD. Sometimes you face the struggle confidently and head on and other times the struggle seems overwhelming. OCD is your particular struggle, but you still have to learn to live to the fullest with OCD. Everyone has a struggle. You are not alone.”
OCD and anxiety: Link and relationship
OCD and anxiety: Link and relationship- Health Conditions
- Health Conditions
- Alzheimer's & Dementia
- Anxiety
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cancer
- Cardiovascular Health
- COVID-19
- Diabetes
- Environment & Sustainability
- Exercise & Fitness
- Eye Health
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Leukemia
- LGBTQIA+
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Nutrition
- Parkinson's Disease
- Psoriasis
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Health Conditions
- Health Products
- Health Products
- Nutrition & Fitness
- Vitamins & Supplements
- CBD
- Sleep
- Mental Health
- At-Home Testing
- Men’s Health
- Women’s Health
- Health Products
- Discover
- News
- Latest News
- Original Series
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- Podcasts
- Can diet help improve depression symptoms?
- Research highlights of 2022
- How Viagra became a new 'tool' for young men
- What makes breast cancer come back?
- How to understand chronic pain
- What is behind vaccine hesitancy?
- News
- Tools
- General Health
- Drugs A-Z
- Health Hubs
- Health Tools
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- Quizzes
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- General Health
- Connect
- About Medical News Today
- Who We Are
- Our Editorial Process
- Content Integrity
- Conscious Language
- Newsletters
- Sign Up
- Follow Us
- About Medical News Today
Medically reviewed by Nicole Washington, DO, MPH — By Zawn Villines on September 6, 2022
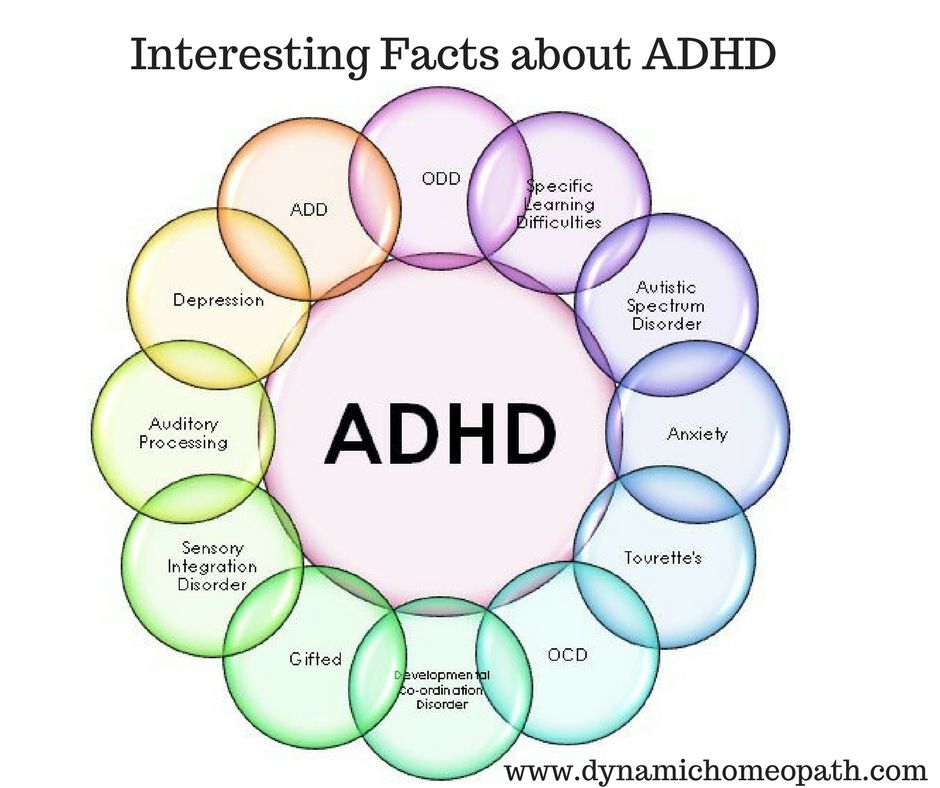
Obsessive-compulsive disorder (OCD) and anxiety are separate mental health conditions that have distinct symptoms but overlap in their causes and treatment. A person can have OCD and anxiety at the same time.
A person can have OCD and anxiety at the same time.
Although OCD is not a type of anxiety disorder, people with OCD experience very regular intrusive thoughts that can cause anxiety and interfere with everyday life.
Individuals may carry out repetitive behaviors or rituals and become more anxious if they cannot complete them. Common behaviors include washing, cleaning, and checking, ordering, and arranging objects.
While they are distinct mental health conditions, OCD and anxiety can overlap in their causes and treatment. The authors of the recent 2022 anxiety overview state that anxiety is underdiagnosed, despite being one of the most prevalent mental health conditions in the general population.
In addition, a 2022 overview of OCD states that the condition is undertreated.
This article considers the link between anxiety and OCD, discusses whether a person can have both OCD and anxiety, and provides information on the symptoms and treatment of OCD.
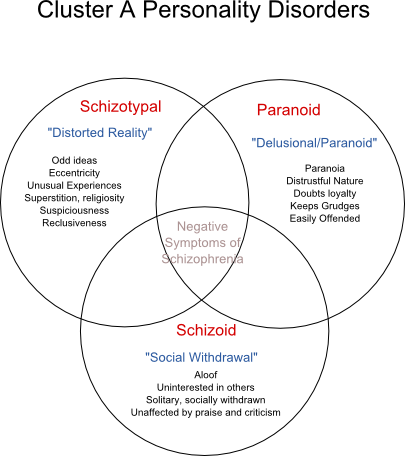
OCD and anxiety can overlap. However, they are separate mental health conditions.
However, they are separate mental health conditions.
The Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision (DSM-IV-TR) classified OCD as an anxiety disorder.
However, the most recent edition — the DSM-5–TR — classifies OCD as a separate mental health disorder under the Disorder Class “Obsessive-Compulsive and Related Disorders.” This section also includes body dysmorphic disorder, hoarding disorder, and a hair-pulling disorder called trichotillomania.
There is a wide range of anxiety disorders that are classified separately from OCD, which include:
- Generalized anxiety disorder (GAD): In GAD, people have chronic anxiety that can last for months or years. There may be no particular cause for their anxiety.
- Panic disorder: People with this type of anxiety have frequent panic attacks they do not expect.
- Social anxiety disorder: This involves intense fear of social situations in which a person may be watched or judged.
- Phobia-related disorders: Phobias relate to fear and aversion to specific objects and situations.
Characteristics
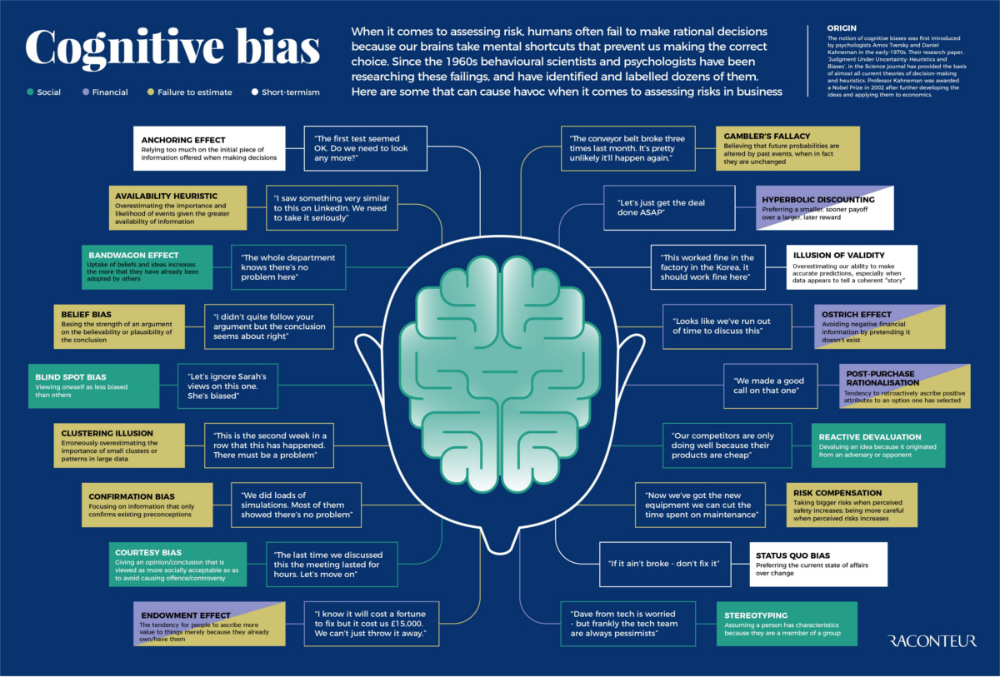
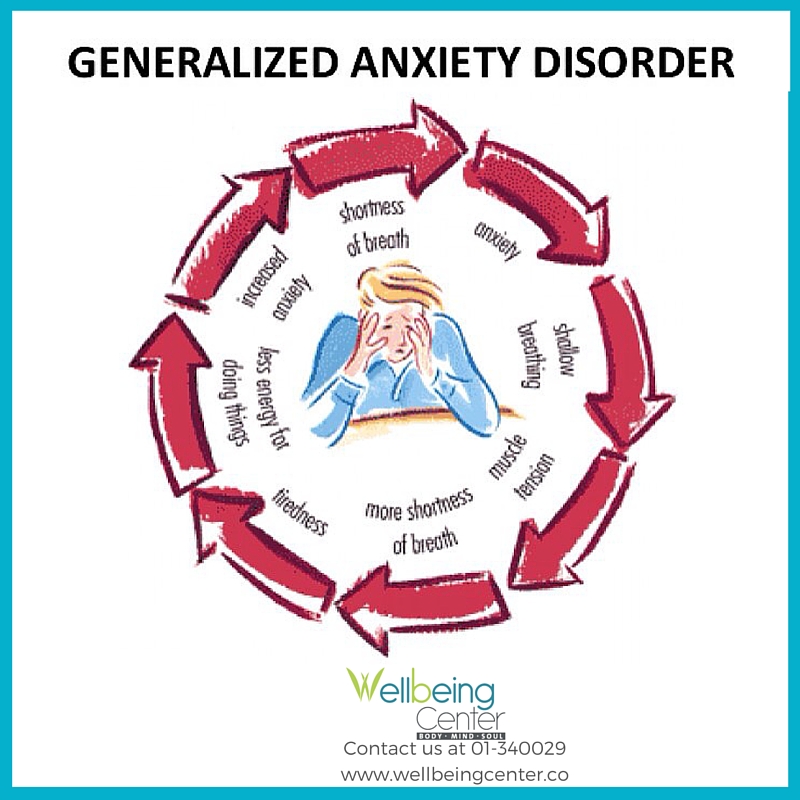
A 2022 overview of anxiety describes it as a “future-oriented” mood state, meaning those with anxiety disorders are often psychologically and behaviorally preparing for future events they anticipate may be a threat.
While people with OCD and anxiety can feel intense fear about certain situations or objects, those with OCD are more affected by recurrent thoughts, images, or behavioral urges that cause them anxiety.
They will respond to these recurring thoughts or urges by repetitively performing rituals such as handwashing or ordering objects.
A person with OCD may not be able to control their urge to engage with compulsions, and they may not enjoy performing them.
People with anxiety disorders typically will not feel the need to carry out these compulsions.
Causes
Scientists do not know what causes OCD. However, the mental health charity Mind in the United Kingdom lists the following as potential causes:
However, the mental health charity Mind in the United Kingdom lists the following as potential causes:
- Personal experiences: These may include childhood trauma, abuse, or bullying, or parents or carers that showed similar compulsive behaviors, which may lead to OCD stemming from learned behavior. Stressful events, chronic anxiety and stress, and pregnancy and childbirth may also play a role in the development of OCD.
- Personality traits: OCD may develop in people who hold themselves to high standards and are very neat and methodical. However, this is not true for everyone.
- Genetics: There is some evidence to show that people can inherit OCD from parents. However, studies often carry limitations. Overall, more research is needed.
The causes of anxiety are diverse and may include:
- Past experiences: Stressful experiences, including abuse, violence, prolonged illness, and the death of a loved one may, lead to anxiety.
 Experiencing difficult situations in childhood or adolescence may also cause anxiety. This can include neglect, bullying, social exclusion, and racism. Learn more about racism and mental health.
Experiencing difficult situations in childhood or adolescence may also cause anxiety. This can include neglect, bullying, social exclusion, and racism. Learn more about racism and mental health. - Stress: Prolonged stress can cause anxiety. This can be stress from work or school, having challenges with finances or housing, or going through a period of significant change or uncertainty.
- Health conditions: Living with serious and long-term health conditions can cause anxiety. Other mental health conditions may also cause a person to develop anxiety.
- Medication side effects: Certain medications, including psychiatric medication, can list anxiety as a side effect.
The symptoms of OCD include a combination of obsessions and compulsions.
Obsessions include:
- recurring intrusive and distressing thoughts, urges, and images a person cannot control
- the urge to stop intrusive thoughts, urges, and images with another thought or action
Compulsions include:
- responding to obsessions with repetitive behavior or mental patterns
- performing repetitive behaviors or mental patterns to reduce anxiety or prevent a perceived threat or negative consequence
Compulsions may not always clearly relate to the negative consequence a person is trying to avoid, and the action may seem excessive to other people. They can take up a lot of a person’s time.
They can take up a lot of a person’s time.
Common compulsions stem from fears about contamination, aggression or harm, sex, religion, and keeping their environment exactly as they want it.
A person only needs to show one compulsive behavior for a diagnosis. Some examples of compulsions include:
- repeatedly checking things, such as ensuring their door is locked
- frequent, excessive handwashing
- counting or tapping objects
- engaging in rituals such as prayer or repeating specific phrases
2019 and 2022 research state that OCD and anxiety can put a person at higher risk of suicide.
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.

- Try to remove any weapons, medications, or other potentially harmful objects.
If you or someone you know is having thoughts of suicide, a prevention hotline can help. The National Suicide Prevention Lifeline is available 24 hours per day at 800-273-8255. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 800-273-8255.
Click here for more links and local resources.
A person should speak with a doctor to discuss diagnosis and treatment if they are experiencing symptoms of OCD or anxiety.
Some people can have both OCD and an anxiety disorder.
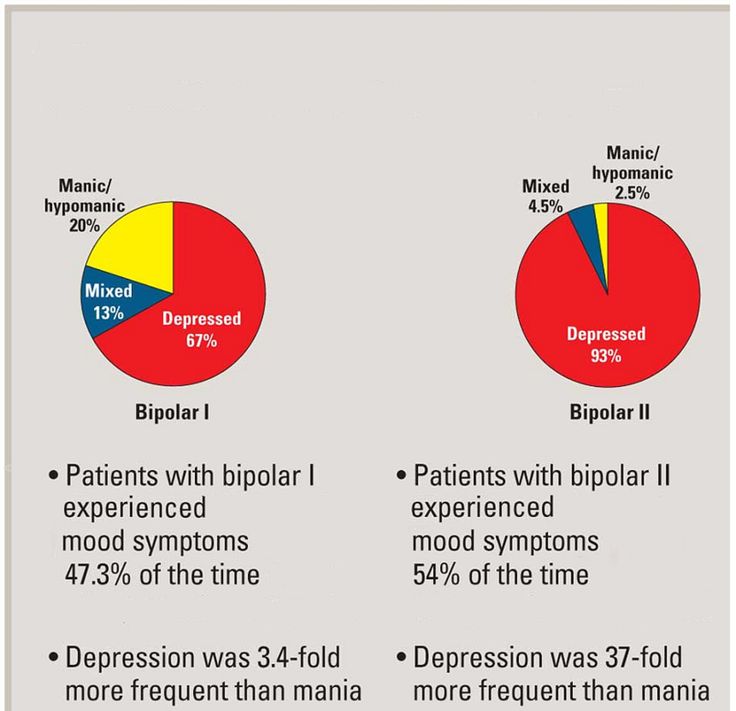
For instance, in a 2021 study, 33.56% of the 867 participants had both OCD and GAD.
This study found that people with OCD and GAD were more likely to have the following symptoms:
- severe anxiety
- avoidant behavior
- panic disorder
- social phobias
- specific phobias
- type II bipolar disorder
A person with OCD and GAD will typically have OCD symptoms and anxiety symptoms, such as:
- chronic anxiety with no identifiable cause
- feeling physically anxious
- muscle tension
- insomnia
- fatigue
- feeling irritable due to anxiety
A person may also have anxiety disorders, such as post-traumatic stress disorder (PTSD) and social anxiety disorder.
A person should work with a doctor to discuss their symptoms and understand whether they may have OCD, an anxiety disorder, or both.
The International OCD Foundation notes that CBT and medication are the most effective treatments for OCD.
Exposure and response prevention (ERP) therapy is a type of CBT.
2019 research states ERP is the first-line treatment for OCD. The authors write that up to 50% of people who have ERP on its own or in combination with medication will have a significant improvement in their symptoms. However, it does not work for everyone.
ERP involves a person working with a mental health doctor to talk about their compulsions, the fears or anxiety that might trigger them, and discuss the relationship between the two. A person may also share what they fear will happen if they do not perform their compulsive behaviors.
A person will then rank different situations from least distressing to most distressing.
After this, they will confront these situations with the support of the clinician and try to hold back from engaging in their compulsive behaviors or rituals.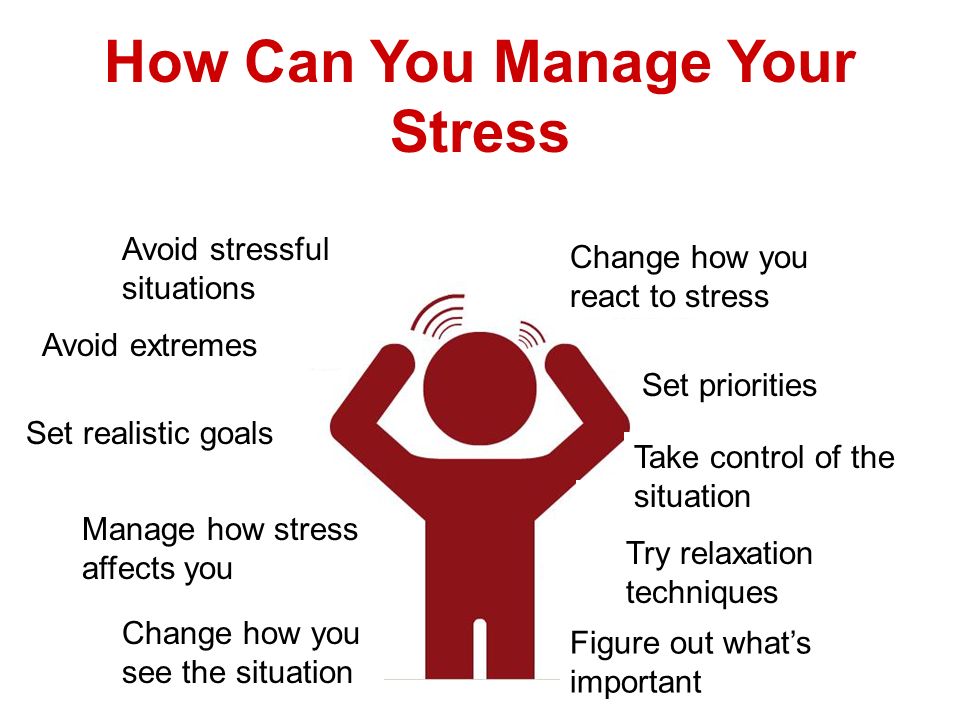 A person will do this in real-world settings and by imagining the situation.
A person will do this in real-world settings and by imagining the situation.
The aim of ERP is to help a person learn that engaging in the situations or tasks they find distressing and refraining from performing their compulsive behaviors will not lead to the negative consequences they fear.
Other treatment options include:
- Medication: Selective serotonin reuptake inhibitors (SSRI) medications are common treatments for OCD. A person may take a higher dose for OCD than for anxiety.
- Deep brain stimulation: When medication and therapy do not work, deep brain stimulation may help with OCD. This involves using an electrode to send out impulses that change the behavior of the brain. However, it is expensive and not often used.
Treatments for anxiety also include therapy and medication.
A doctor may prescribe:
- SSRIs
- serotonin-norepinephrine reuptake inhibitors (SNRIs)
- tricyclic antidepressants
- mild tranquilizers
- beta-blockers
- benzodiazepines
CBT is one of the most effective types of therapy for anxiety.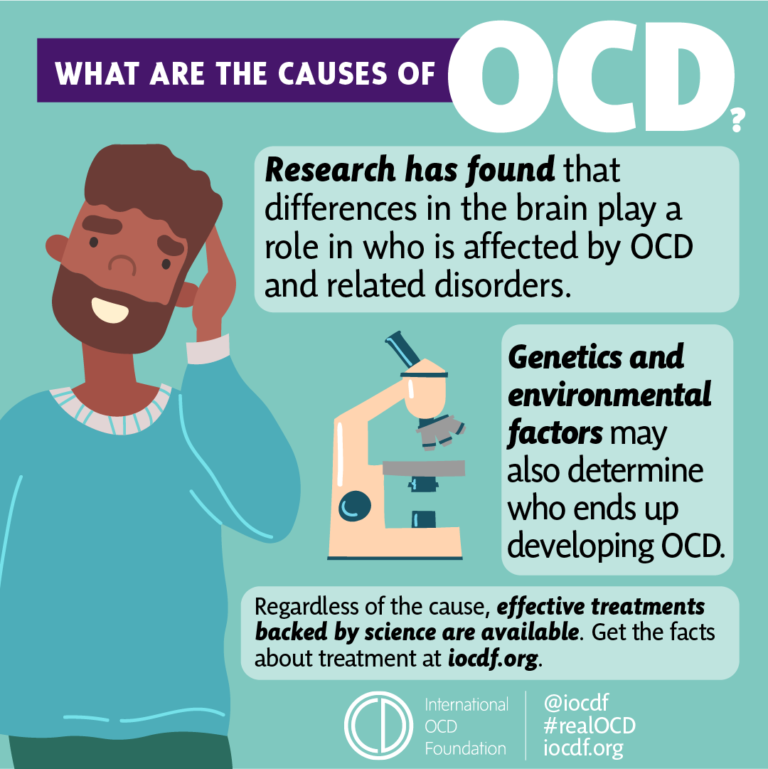 It aims to help a person identify negative thought patterns and beliefs that trigger and sustain their anxiety and adapt them to reduce their symptoms.
It aims to help a person identify negative thought patterns and beliefs that trigger and sustain their anxiety and adapt them to reduce their symptoms.
A person may also try exposure therapy for anxiety, which helps a person confront situations that cause them anxiety.
A person can work with a doctor to discuss which treatment is best for them.
While fear and anxiety play a role in both OCD and anxiety disorders, they are distinct mental health conditions.
The main difference between OCD and anxiety is that those with OCD will experience strong urges to carry out repetitive behaviors or mental patterns to reduce anxiety about a specific situation or fear. They will also feel anxious if they do not perform these actions. People with anxiety will typically not have these urges.
Medication and therapy can treat both anxiety and OCD.
Anyone living with OCD or anxiety should speak with a doctor to discuss treatment.
Last medically reviewed on September 6, 2022
- Mental Health
- Anxiety / Stress
- Psychology / Psychiatry
How we reviewed this article:
Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations.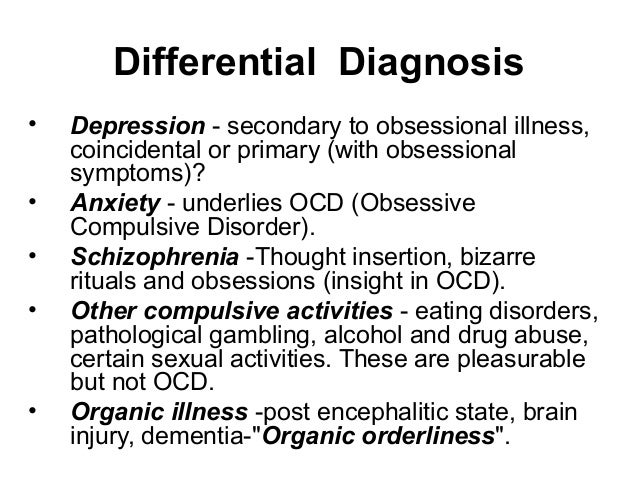 We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Anxiety and panic attacks. (2021).
https://www.mind.org.uk/information-support/types-of-mental-health-problems/anxiety-and-panic-attacks/causes/ - Brock, H., et al. (2022). Obsessive-compulsive disorder.
https://www.ncbi.nlm.nih.gov/books/NBK553162/ - Chand, S. P., et al. (2022). Anxiety.
https://www.ncbi.nlm.nih.gov/books/NBK470361/#article-17728_s3 - Eskander, N., et al. (2020). Psychiatric comorbidities and the risk of suicide in obsessive-compulsive and body dysmorphic disorder.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7494407 - Goodwin, G.
 M. (2015). The overlap between anxiety, depression, and obsessive-compulsive disorder.
M. (2015). The overlap between anxiety, depression, and obsessive-compulsive disorder.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4610610 - Hezel, D. M., et al. (2019). Exposure and response prevention for obsessive-compulsive disorder: A review and new directions.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6343408/ - Impact of the DSM-IV to DSM-5 changes on the national survey on drug use and health. (2016).
https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch4.t13/ - Munir, S., et al. (2022). Generalized anxiety disorder.
https://www.ncbi.nlm.nih.gov/books/NBK441870/ - Obsessive-compulsive disorder (OCD). (2019).
https://www.mind.org.uk/information-support/types-of-mental-health-problems/obsessive-compulsive-disorder-ocd/causes-of-ocd/ - Obsessive-compulsive disorder. (2019).
https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd - Pauls, D.
 L. (2010). The genetics of obsessive-compulsive disorder: A review.
L. (2010). The genetics of obsessive-compulsive disorder: A review.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181951/ - Sharma, P., et al. (2021). The impact of generalized anxiety disorder in obsessive-compulsive disorder patients [Abstract].
https://www.sciencedirect.com/science/article/abs/pii/S0165178121001955
Share this article
Medically reviewed by Nicole Washington, DO, MPH — By Zawn Villines on September 6, 2022
Related Coverage
How to cope with OCD
Living with OCD can be challenging, but in this Spotlight, we take a look at some habits that you can adopt that may help you to cope with it.
READ MORE
Best medications for OCD symptoms
Medically reviewed by Alexandra Perez, PharmD, MBA, BCGP
Usually, the first-line medication for reducing the symptoms of obsessive-compulsive disorder (OCD) is an antidepressant.
 Learn more here.
Learn more here.READ MORE
OCD and hypersexuality
Hypersexuality and OCD can refer to obsessions and compulsions relating to sex and sexual urges that may cause distress and impairment in daily life…
READ MORE
What is sexual orientation OCD (SO-OCD)?
Medically reviewed by Karin Gepp, PsyD
Sexual orientation OCD can involve unwanted, intrusive thoughts and doubts about a person's sexual orientation.
READ MORE
Is mindfulness beneficial for OCD?
Medically reviewed by Karin Gepp, PsyD
Is mindfulness an effective treatment option for OCD? Read on to learn more about this technique, including what it is and how it may treat OCD.
READ MORE
Obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental disorder that is characterized by the appearance of anxiety and various obsessive thoughts that provoke the performance of certain actions that have ritual significance for a person.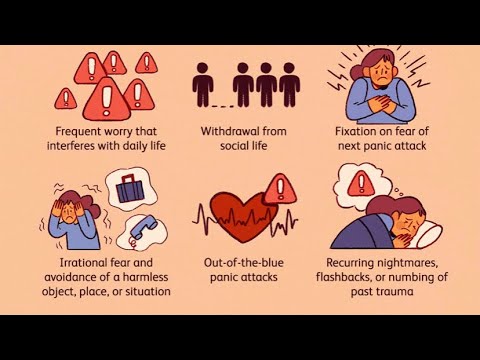 After performing the desired action, there is a decrease in the level of anxiety.
After performing the desired action, there is a decrease in the level of anxiety.
Contents
- Signs and symptoms
- Risk factors
- Treatment and therapy
- Conditions associated with obsessive-compulsive disorder
After performing the desired action, the alarm level is reduced.
Signs and symptoms
People with obsessive-compulsive disorder tend to experience obsessions, perform repetitive actions (compulsions), or both. These symptoms affect every aspect of a person's life: work, school, and personal relationships.
Obsessions are unwanted thoughts, images, urges, worries or doubts that keep popping up in a person's head and cause intense anxiety.
These may be:
- fear of germs or contamination;
- unwanted forbidden or taboo thoughts about sex, religion or harm;
- aggressive thoughts towards others or oneself;
- the desire to put things symmetrically, to keep things in perfect order.
Compulsions are repetitive behaviors that a person with obsessive-compulsive disorder feels compelled to do in response to an obsessive thought. Common compulsions include:
- excessive desire for cleanliness, constant washing of hands;
- placing things in a certain, exact order;
- multiple checks of the execution of actions: whether the door is locked, whether the iron or oven is turned off;
- compulsive account.
Not all rituals or habits are signs of obsessive-compulsive disorder, every person has situations when he double-checks something. People with obsessive-compulsive disorder usually:
- unable to control their thoughts or behavior, even if these thoughts or behavior are excessively intrusive;
- do not take pleasure in performing actions or rituals, but after performing they feel short-term relief from anxiety and mental experiences.
- experience problems or discomfort in daily life due to these thoughts or behaviors.
Some people with OCD have tics. Motor tics are sudden, short, repetitive movements such as blinking and other eye movements, facial grimacing, shrugging, and jerking the head or shoulder. Common vocal tics include repetitive throat clearing, snorting, or grunting.
Symptoms may come and go, get better or get worse over time. People with obsessive-compulsive disorder sometimes try to reduce their symptoms by avoiding situations that trigger them, and may use alcohol or drugs to calm them down. Most adults with obsessive-compulsive disorder are aware that their actions do not make sense. Children require special attention, as children may not be aware that their behavior is unusual.
Risk factors
Obsessive-compulsive disorder is a common disorder that affects adults, adolescents and children around the world. Most people are diagnosed by age 19. In boys, as a rule, the disease manifests itself earlier than in girls.
The causes of obsessive-compulsive disorder are unknown, but risk factors include:
Genetics
Twin and family studies have shown that people who have a first-degree relative (parent, sibling, or child) with OCD are at higher risk of developing the disorder.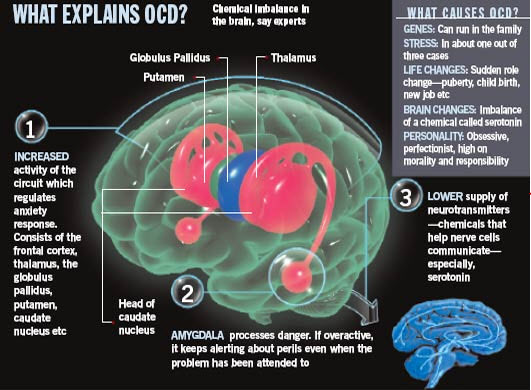 The risk is higher if a first-degree relative developed OCD during childhood or adolescence.
The risk is higher if a first-degree relative developed OCD during childhood or adolescence.
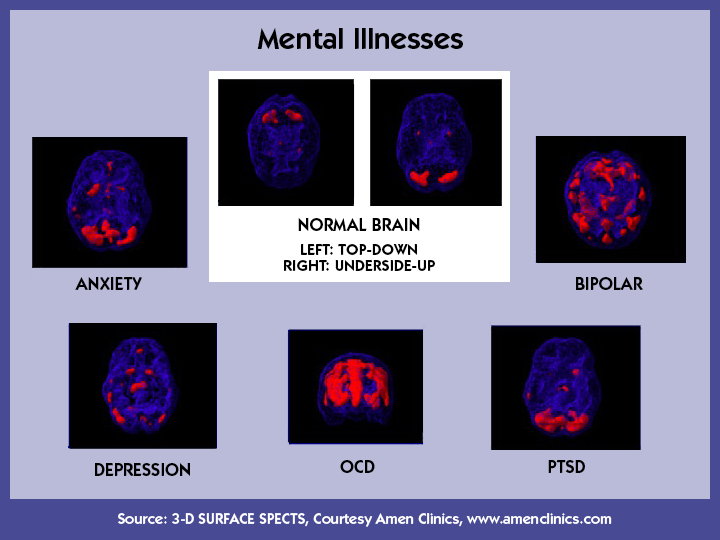
Structure and function of the brain
Studies have shown differences in the frontal cortex and subcortical structures of the brain in patients with obsessive-compulsive disorder. There seems to be an association between symptoms of obsessive-compulsive disorder and abnormalities in certain areas of the brain, but the exact pattern has not yet been identified.
Environment
Some studies show a link between childhood trauma and symptoms of obsessive-compulsive disorder. But more research is needed to better understand this relationship.
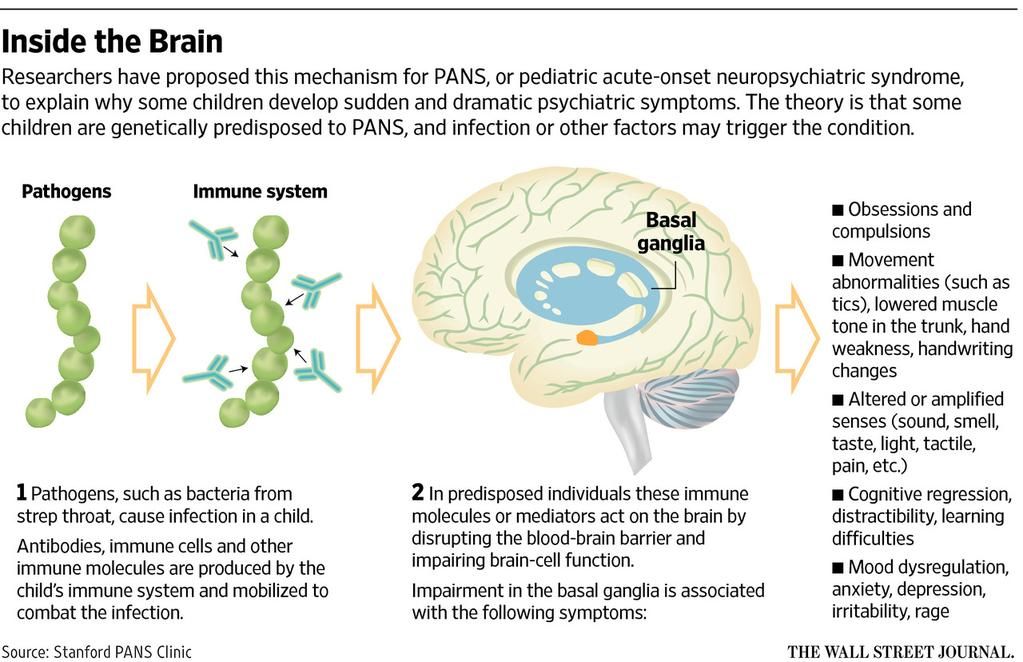
In some cases, children may develop symptoms of obsessive-compulsive disorder after having a streptococcal infection - this is called pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS).
Treatment and Therapy
Treatment for obsessive-compulsive disorder usually involves the use of certain drugs, psychotherapy, or a combination of both. Although most patients with this condition respond well to treatment, some patients may have symptoms. Studies show that high-frequency deep transcranial magnetic stimulation with an area of application in the areas of the brain involved in the process in obsessive-compulsive disorder is an effective method.
Although most patients with this condition respond well to treatment, some patients may have symptoms. Studies show that high-frequency deep transcranial magnetic stimulation with an area of application in the areas of the brain involved in the process in obsessive-compulsive disorder is an effective method.
Conditions associated with obsessive-compulsive disorder
There are other mental health problems that are similar to obsessive-compulsive disorder in that they involve repetitive thoughts, behaviors, or urges.
- Perinatal OCD is an obsessive-compulsive disorder during pregnancy or after childbirth.
- Body Dysmorphic Disorder is a disorder in which a person is overly concerned about a minor and sometimes perceived defect or feature of their body.
- Compulsive pinching of the skin is repeated touching of the skin to relieve anxiety. May be part of body dysmorphic disorder.
- Trichotillomania is an obsessive desire to pull out hair.
- Accumulation - a disorder in which a person collects, stores and gets rid of things with difficulty.
- Obsessive Compulsive Personality Disorder is a type of personality disorder. It has some of the traits associated with obsessive compulsive disorder, but it's a different, separate condition.
OCD is sometimes accompanied by other psychiatric disorders such as anxiety or depression. It is important to consider these and other disorders when making treatment decisions.
References:
https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml
https://www.mind.org.uk/information-support /types-of-mental-health-problems/obsessive-compulsive-disorder-ocd/about-ocd/
UA-ACIN-EIM-012021-053
to the list of articlesFind a doctor
What is obsession (obsessive thoughts): symptoms, how to get rid of?
- Symptoms of obsession
- What thoughts arise during obsession?
- How disorder appears
- Classification
- Diagnostics
- How to get rid of obsessive thoughts?
- Treatment
Image by fizkes on Shutterstock
Obsession is a condition in which a person is disturbed by intrusive thoughts. Alien images and urges to certain actions arise involuntarily. A person tries to isolate himself from these ideas, the state causes anxiety and discomfort. If treatment is not done in time, obsession leads to emotional exhaustion, depressive disorder, and the inability to adapt in society.
Alien images and urges to certain actions arise involuntarily. A person tries to isolate himself from these ideas, the state causes anxiety and discomfort. If treatment is not done in time, obsession leads to emotional exhaustion, depressive disorder, and the inability to adapt in society.
Symptoms
Obsessive thoughts accompany a number of psychological illnesses. They develop with neurosis, schizophrenia, depression, obsessive-compulsive disorder (OCD).
Signs that accompany obsession:
-
the inability to influence the appearance of obsessive thoughts, they arise against the will of a person;
-
thoughts are in no way connected with habitual reasoning, the emerging images are alien;
-
by an effort of will it is impossible to drive away these thoughts;
-
accompanied by anxiety, irritability;
-
the clarity of consciousness is preserved, the person adequately perceives what is happening.
Obsessive people have a hard time with intrusive thoughts. Against the background of clarity of consciousness, the patient understands the irrationality of the images that arise, but cannot influence the situation in any way. This is even more worrying.
If seizures occur regularly, the only way out is to consult a psychiatrist.
What thoughts come up when you have an obsession?
Obsessive thoughts during obsession are primarily directed at the person himself, his environment and state of health. The most common ones are:
-
the need for perfect order and symmetry;
-
constant counting of various objects, for example, steps;
-
worries about illness;
-
pollution concerns;
-
thoughts about accidents that should happen to a person or his relatives;
-
concerns about property damage;
-
aggressive, sexual, religious ideas that arise against the will;
-
unwillingness to perform any actions or rejection of any objects, objects.
Obsessive thoughts bring extremely negative emotions. Sometimes there is a desire to follow these ideas, then a person experiences compulsions: he performs actions against his will, in accordance with an obsessive idea. In this state, the patient experiences discomfort, suffering, it interferes with normal life. When an obsessive idea is combined with actions to realize it, obsessive-compulsive disorder (OCD) develops.
Against the background of OCD, a person performs actions that, as it seems to him, will protect him from negative events in life. He may, for example, make it a rule to touch trees, to avoid cracks in the road, because he believes that if he does not do this, irreparable things will happen. The person expects that performing these actions will reduce anxiety and get rid of obsessive thoughts. However, this does not alleviate the condition, the actions turn into a kind of ritual.
How the disorder appears
The cause of the obsessional state has not yet been precisely established.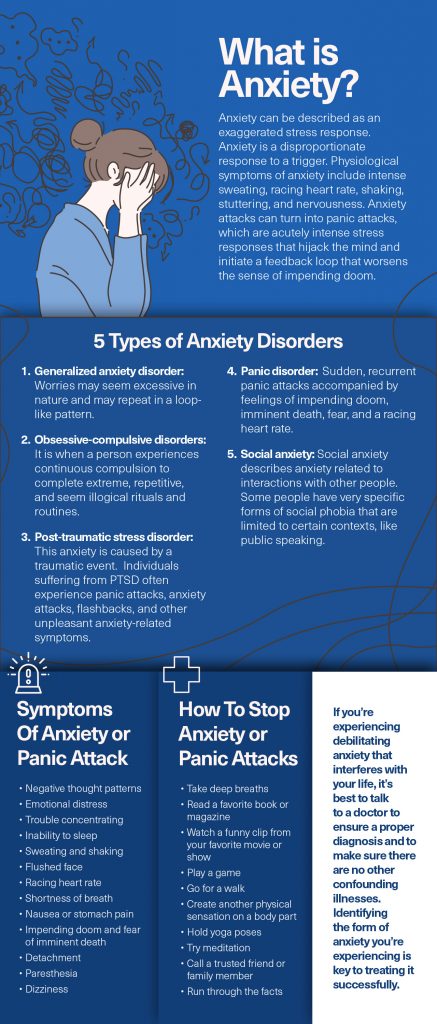 It can be preceded by prolonged stress, experienced psychological trauma, concentration on negative thoughts, and the impact of others. Not all people are prone to developing obsessions. Predisposing factors are:
It can be preceded by prolonged stress, experienced psychological trauma, concentration on negative thoughts, and the impact of others. Not all people are prone to developing obsessions. Predisposing factors are:
-
indecision;
-
restrained reactions with hypersensitivity;
-
self-esteem is reduced or vice versa is too high;
-
suspiciousness;
-
desire to dominate.
People are prone to the appearance of obsessions, in whose families a high sense of responsibility was instilled, perfectionism, when the child was kept within strict limits, immediacy was suppressed. The man had to keep his emotions inside. The result was an intrapersonal conflict.
There are different theories regarding the development of obsessions. According to Pavlov's theory, people with a certain type of nervous activity are prone to such a state: when there is an obsession with the processes of excitation along with inactivity.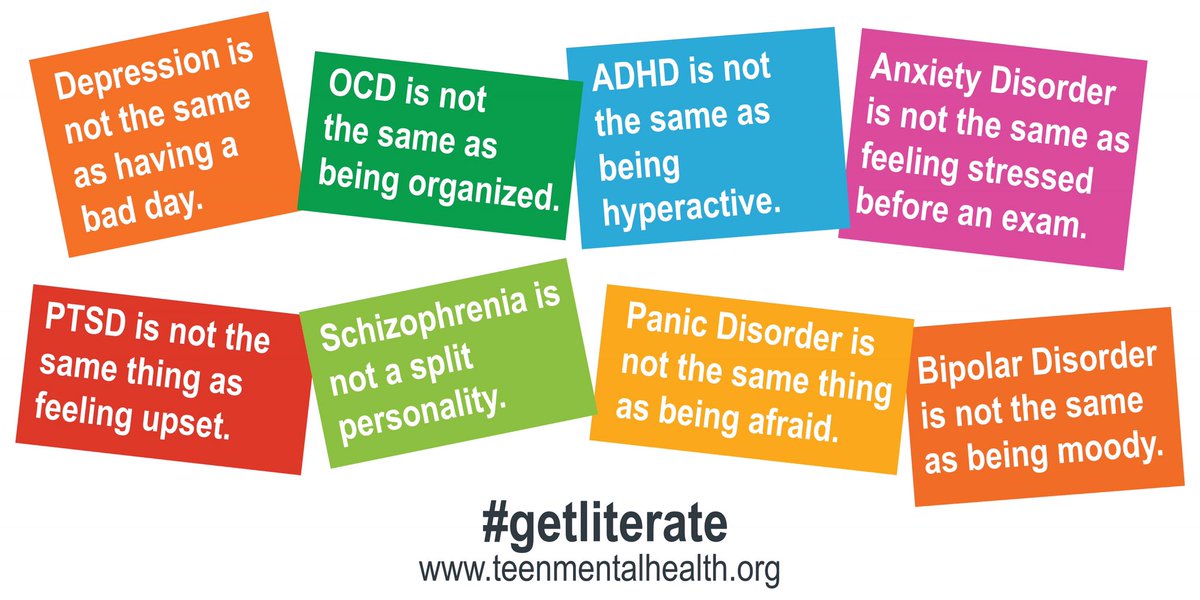 According to Freud's theory, disorder occurs involuntarily and is in no way controlled by consciousness. Occurs against a background of guilt.
According to Freud's theory, disorder occurs involuntarily and is in no way controlled by consciousness. Occurs against a background of guilt.
Classification
According to Jaspers' classification, obsessional disorders are abstract and figurative.
With an abstract form, there is no emotional coloring. Thoughts do not affect the mood of a person in any way, they do not contribute to changes in the psyche. These intrusive thoughts include:
-
arithmomania. A person constantly counts something (steps, cars, trees), remembers the numbers of telephones and cars. He is constantly busy with digital calculations;
-
highlighting words. Certain words from the phrases read are decomposed into letters;
-
memories. The same memory constantly arises in the memory, about which a person tries to tell the largest number of people. Tries to prove the magnitude and importance of this event;
-
sophistication.
 Regularly there are all sorts of reflections, devoid of any meaning.
Regularly there are all sorts of reflections, devoid of any meaning.
With the development of a figurative form of obsession, the patient experiences severe emotional experiences, mainly of a pessimistic nature:
-
doubts. Pursues uncertainty about the correctness of the actions taken. The patient will repeatedly check the result. This condition can manifest itself in situations such as returning home to check the turned off iron, gas. If this is not possible, the person experiences strong feelings;
-
concerns. Most often, this condition affects people whose activities may lead to litigation. These are doctors who have doubts about the quality of operations, accountants associated with large financial transactions, and other financially responsible persons in the enterprise. This category of people includes teachers who are responsible for the life and health of the child at school;
-
experiences.
 Constant thoughts about past events, mostly negative, tragic. Thoughts cause depression, remorse, guilt and regret, shame, tears, fear;
Constant thoughts about past events, mostly negative, tragic. Thoughts cause depression, remorse, guilt and regret, shame, tears, fear; -
attraction. Accompanied by a desire to commit an obscene act: swearing, fighting. Despite the vivid expression of a thought, most often it is not realized in action;
-
representation. When thoughts arise about the consequences of actions that a person could take. For example, how events will develop if he takes someone's life. Sometimes the thoughts are so intrusive that the person ceases to be aware of their irrationality;
-
antipathy. An unreasonable feeling of hostility towards people, most often close ones. For believers, it may arise in relation to religious figures.
Most often, intrusive thoughts are associated with the following factors:
-
intolerance to the slightest disorder;
-
fear of infection;
-
non-existent danger;
-
obsession of a sexual nature;
-
violence;
-
blasphemy.

There may be complex disorders, when some obsessive thoughts replace others.
Diagnostics
Ideas of an obsessive nature can also appear in other psychological illnesses. Therefore, a qualified specialist who understands the features of the clinical picture should carry out the diagnosis.
Diagnostic measures include:
-
Inspection. Collection of information about complaints, assessment of the clinical picture.
-
Pathopsychological research. Patient observation, interviews and experiments.
-
Surveys. With the help of neurotests and a neurophysiological test system, the severity of the processes is assessed.
How to get rid of obsessive thoughts?
If a person has signs of obsession, thoughts appear that cannot be fenced off, it is necessary to visit a psychiatrist for a consultation. If this is not done in a timely manner, the situation will worsen.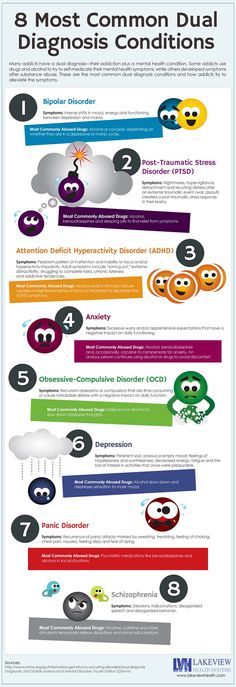 Often people with these disorders turn to alcohol or drugs to get away from the problem. However, as a result of taking alcoholic beverages, the symptoms of obsession only increase.
Often people with these disorders turn to alcohol or drugs to get away from the problem. However, as a result of taking alcoholic beverages, the symptoms of obsession only increase.
In addition to the basic therapy prescribed by the doctor, it is necessary to learn self-control. You can reduce the manifestations of obsession by the following actions:
-
learn more about the violation, this will allow you to accept the situation and tune in to the need for treatment;
-
talk about the problem to relatives, parents, spouses or children;
-
do not give up the usual activities;
-
normalize sleep and wakefulness;
-
give up alcohol and drugs;
-
play sports with moderate physical activity;
-
find a hobby that delivers emotional satisfaction;
-
avoid stressful activities.
Treatment
Psychotherapy and drug therapy can reduce the manifestations of the disease or completely get rid of OCD.