Bpd abuse cycle
Borderline Personality and The Hidden Abuse of Non Borderlines
Posted by A.J. Mahari and Reviewed by Ryan House, PsyD Clinical Psychologist
Borderline Personality Disorder (BPD) is highly associated with verbal abuse, emotional abuse, psychological abuse, physical abuse, and/or domestic violence often suffered by those who are non-borderline.
Recent findings suggest that further research is necessary to better understand the association and differentiation between psychological dysfunction and trauma processing, emotional regulation, distress tolerance, and interpersonal sensitivity of individuals diagnosed with BPD.
The propensity for abusiveness in those with BPD can be instigated by the narcissistic injury that is at the heart of the core wound of abandonment.
Borderline Personality And Abuse
Those diagnosed with Borderline Personality Disorder (BPD) or those with BPD who may not even know they have it, are more likely than the general population to be verbally, emotionally/psychologically, physically abusive.
But what is behind the connection between Borderline Personality and abuse?
The reality of this is such because borderlines lack a known, consistent self, and they struggle with abandonment fears and abandonment depression that stem directly from a primal core wound of abandonment that arrests their emotional and psychological development in the very first few months of life.
This arrested development impacts most, if not all, areas of relating and leaves borderlines unable to interact in age-appropriate healthy ways.
Ways of relating that unfold in the present and that aren’t layered with deep intra-psychic pain – pain that is unresolved.
Intra-Psychic Pain Is The Root
The roots of abuse in BPD, particularly in intimate significant other relationships with Non-Borderlines have their genesis in the borderline’s re-living of this deep intra-psychic pain.
Pain that is triggered through attempts to be emotionally intimate with someone else. The intimacy that non-personality-disordered people enjoy is stressful and overwhelming to the borderline.
It enlivens the borderline’s worst nightmare – the unresolved pain of the core wound of abandonment.
It arouses all the maladaptive defenses of the borderline because he/she re-experiences the terror and panic of either his/her past experience of feeling annihilated or engulfed and/or his/her fear of being annihilated or engulfed, often alternately when trying to be close to someone one else.
Approach-Avoidance Conflict
This sets up an approach-avoidance conflict, a “get-away-closer” style of trying to relate that has its roots in the “I hate-you-don’t-leave-me” struggle of the borderline who experiences any withdrawal of intense, close, (albeit also threatening) intimacy, attachment or bond as a threat to his or her safety at best, and entire existence (psychologically) at worst.
Add to this that when there is any distancing or break in the intensity and symbiotic-like closeness (if in fact closeness is ultimately achieved) the borderline then fears, and/or feels abandoned.
This conflict of fearing or re-experiencing annihilation versus engulfment and then the re-experiencing of the fear of or actual feelings of abandonment that the borderline experiences, often subconsciously, in trying to be in relationship to other, causes the borderline to be triggered back to his/her original core wound of abandonment feelings in such a way as to trigger the primal feelings of helplessness, loss of control, needs equaling survival, thwarted needs being akin with the death of the lost self.
This whirlwind of unregulated emotion meeting with fear and distrust generates the original feelings of rage that this core wound of abandonment aroused in the first place.
A Wound of Abandonment Can Feel Like Psychological Death
The core wound of abandonment, when one is very young and experiences it, is the experience of psychological death. It is intense and arouses the borderline to fight for survival while they experience the sheer terror of feeling like they might actually just die or be killed by what they are feeling.
This heightened state of arousal is both psychological and biological – it is physiological. It is a strong drive to survive and rage is at its core.
Borderline Rage
Rage is the most primal feeling generated and the most protective defense that a young infant can muster to try to have the caregiver return to once again provide some sense of being for the infant.
Feelings and reactions of rage are experienced by those who go on to develop BPD so early in life that they precede cognitive and verbal development.
This is what makes borderline rage so primal, so intense, and in the case of the borderline so raw and unmanageable in terms of often triggered dysregulated emotion of those with BPD.
It is pain that has long-since been dissociated from and abandoned by the borderline. This abandoned pain of BPD is the ignition switch that needs only the hint or flicker of an emotional flame to ignite a combustible, all-too-often abusive rage like no other.
This is what the borderline regresses to.
When the borderline is in a regressed and to varying degrees dissociated experience, the non-borderline partner is experienced by the borderline as that withdrawing or abandoning caretaker from the past that was needed for literal physical and psychological survival.
Issues That Trigger Rage
When the non-borderline partner, living, On The Other Side of BPD isn’t focusing 100% of his or her attention on the borderline (especially if you have actually attained closeness) and there is any experienced or even perceived break in the symbiotic connection that enables the borderline to feel somewhat secure (like the not having to attend to a child, or go to the washroom or any simple thing) – even when stressed by the closeness – and already beginning to cycle to the fear of the loss of it – the borderline will often react from this cesspool of ever-churning rage which is the protection for the very vulnerable and young abandoned pain of the borderline. This ends in a lashing out by the borderline personality, abuse is often the end result.
This ends in a lashing out by the borderline personality, abuse is often the end result.
Different Expressions of Borderline Rage
All rage is not expressed the same way. All borderlines do not abuse in the same ways.
As you will see in my next article, there are many different forms that the abuse generated by this narcissistic woundedness takes. Some borderlines rage, literally, they scream and yell and throw things or hit people.
While other borderlines (known as quiet or “acting in” borderlines) may rage in such passive-aggressive ways that the non-borderline might not realize that the borderline is raging.
Rage is Always Smoldering
This inherent free-floating, always-at-the-ready rage, if you will, is the root source of a lot of the varying types and styles of abuse that non-borderlines are bombarded with.
It can often be sudden and seem to come out of nowhere because the source of it is deep inside the psyche of the borderline.
Emotional And Psychological Arrest
Borderlines lack a known self. They have not been able to emotionally or psychologically mature beyond a very early stage of emotional developmental arrest.
An emotional/psychological arrest that takes place when the developing authentic self essentially experiences a death, is lost to the borderline and is then supplanted by the false self.
Why Life Can Seem Constantly Painful
Life, for those with BPD, is, to say the least, one devastatingly painful experience of trying to live and exist in the absence of a known self in the fragmented pieces of the blurred experience of the here and now enmeshed with the past.
It is one perpetual separation-individuation crisis void of the big picture until and unless it can be resolved.
Current Feelings Trigger Past Wounds
Borderlines do not learn how to cope with the feelings that they have in the here and now, that trigger past intense unresolved feelings of the actual loss of the psychological self.
Lack of Object Constancy
Borderlines lack the ability to hold in any consistent or congruent way object constancy.
They experience relatedness as being as fragile as out of sight out of mind.
A bond that a non-borderline feels exists between him/herself and the borderline whether he/she is in the presence of the borderline or not is not something that the borderline can psychologically remember, trust, or believe.
Object constancy or any connectedness or attachment that could be defined as “secure” is fleeting for the borderline who has not been able to develop object constancy.
The fleeting nature of this inability on the part of those with BPD to hold object constancy in any consistent or congruent way leaves those with BPD in a very painful place – literally between a rock and a hard place in what is the classic relational no-win of an untreated person with BPD.
Loss of Authentic Self
This loss of the authentic psychological self is re-experienced over and over again and the fear of it and the fear of the pain of it grows each and every time one is triggered back to it.
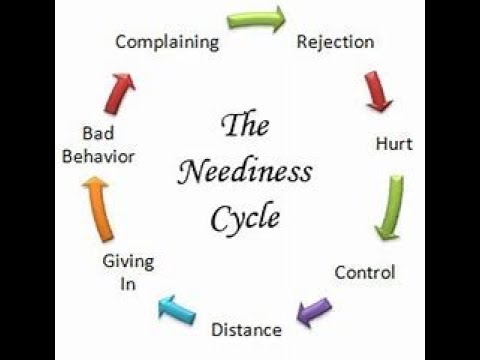
The Cycle Continues
This builds both anger and a continually proliferating inability to cope with it in any constructive way.
Anything short of intense symbiotic connection that is uninterrupted will once again send the borderline cycling back around the re-experiencing of everything associated with the core wound of abandonment.
As the borderline cycles back to this enraging and vulnerable – which isn’t tolerable – place of abandonment depression (Masterson) and abandonment trauma so too begins the apex of the likelihood of abuse.
Along with abuse of all sorts, the result of this cycle is often a punishing talionic impulse acted on in the heat of the triggered-dissociated moment by the borderline in what are known as repetition compulsions.
Borderline Personality And Abuse AwarenessMost borderlines, until and unless they have substantial and successful therapy are not consciously aware of what I am describing here.
- Some are totally oblivious to their behavior.
- Some see their behavior as a means to an end and take little to no responsibility for it or any of its consequences.
- Others understand that they have acted poorly again, pissed someone off, have once again made real the threat of and/or fear abandonment and loss, but they do not understand why they’ve done it.
- Similarly, they have no clue how to stop it.
- Others project it out onto the non-borderline and think that everything that has come from them was actually done to them by the non-borderline.
This can be a crazy-making experience for the non-borderline. This is of little consolation to the non-borderline, however. It does not, at all, justify the abuse.
Will a Person With BPD Ever Change?
However, clearly I write about this here to say that if a borderline is not getting treatment, and I mean for real, not just going through the motions type of treatment, there is no logical reason to even begin to believe that the abuse that any borderline in your life is perpetrating upon you will stop.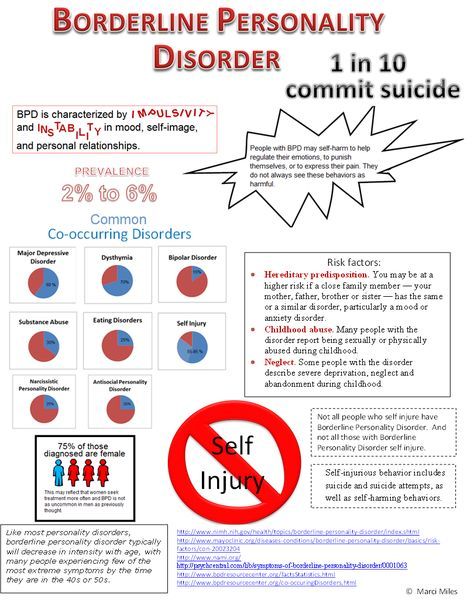
The very thing that you most want from your borderline (or wanted if you’ve left the relationship) in terms of what it means to have a relationship and to relate was not ever even on the table because the borderline is not an emotionally/psychologically mature being.
BPD’s Immature Relational Ability
The borderline is still a very wounded and very young child, emotionally, in terms of the ability or understanding of how to actually relate to others.
This is the case because what borderlines do is not relate to others for who they are but as an extension of the borderline – and more to the point – as an extension of the parent (usually mother) that most failed them or by whom the borderline most feels abandoned, for whatever reason(s).
No Concept of The Real Self
The borderline has no idea who he/she really is. He/she often feels as if he/she does not exist.
This is especially true if the borderline does not have an other to project all of his/her feelings out onto and an other from whom they then require the mirroring back of an identity of what is a painful lack of known self.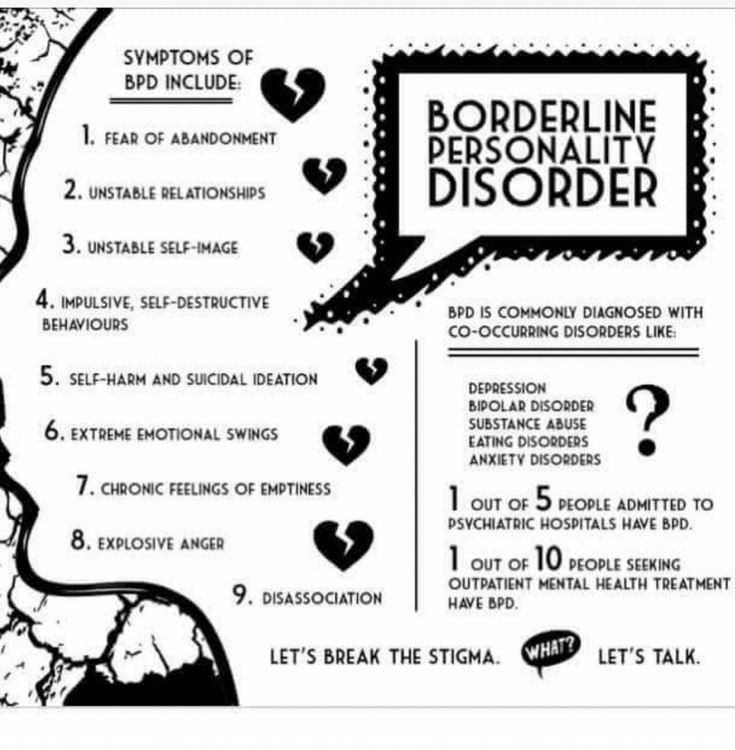
In her book, The Narcissistic/Borderline Couple, Joan Lachkar, Ph.D., writes,
“For the borderline, the focus is primarily on bonding and attachment issues. Borderlines often form addictive love relationships (including normal dependency), they form parasitic relationships, and project their needs in hostile, threatening ways. Because their defenses and demands are excessive, borderlines tend to remain in the dance, rarely achieving their aims.”
The dance that Lachkar refers to, in my past, for me, as I look back now many years into recovery when I was borderline, was one of seeking to re-invent, re-experience, re-do, the ruptured relationship with my mother.
This wound caused me to lose my authentic self to the defensive and manipulative abusive narcissistic defenses of the borderline false self in such a way that would once and for all satiate the developmental needs arrested at the time of my core wound of abandonment and teach me how to actually bond without feeling like it would kill me.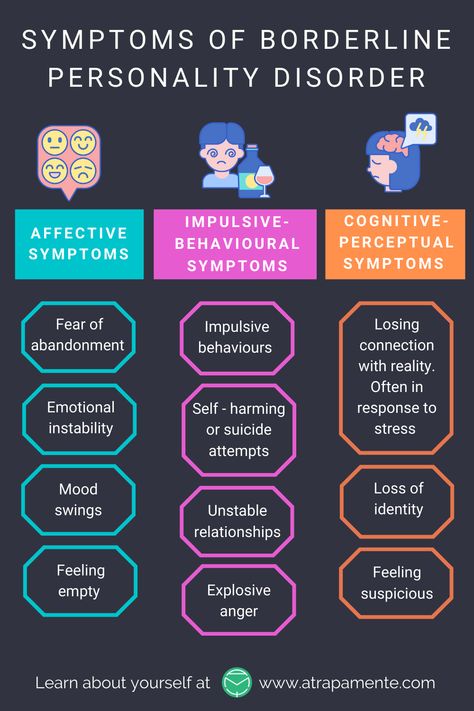
The dance, for me, was one of seeking to recreate and recapture that symbiotic relationship that I never had the chance to have with my mother, through others, in an end-justifies-the-means kind of way, that was, at times, very abusive to others in my life, in the past, on my part.
That dance was a complicated punishing and unforgiving dance of codependency through which I sought to resolve what for years seemed like the unresolvable woundedness that was the source of my rage and the abuse that I perpetrated against others in the name of trying to actually be psychologically born which is necessary in order to get on and stay on the road to recovery.
RELATED ARTICLE: Borderline Personality and Abuse
Narcissistic Defense Mechanisms
Most, if not all borderlines, have, as a result of this core wound of abandonment, a well-developed defense mechanism of narcissism and also have varying degrees of narcissistic injury that manifests in the and through the false self.
This narcissistic injury or wound and its subsequent usage as a defense mechanism along with the narcissism seen in the false self of those with BPD are not to be lumped together with Narcissistic Personality Disorder – they are not one and the same at all.
Incapable of Adult Intimacy
Borderlines who live from a false self and who do not have an active and keen awareness of their own core wound of abandonment and their abandoned pain are not capable of age-appropriate adult intimacy or relating.
It is from the core of this emotional dysfunction that borderlines end up abusing either themselves, others, or both. Non-borderlines, are often on the receiving end of many types of abuse.
The Pain Of Borderline Relating
The very nature of borderline relating makes for a dysfunctional and toxic relational style that non-borderlines will benefit greatly from learning more about so that they can deepen their understanding of BPD and also take care of themselves.
Many non-borderlines come to realize that they want and/or need to break free from the puzzling and painful maze that is borderline relating. Relating that is more often than not abusive.
What Non-Borderline’s Need To Do
If you are a non-borderline and you are being abused by someone with BPD, you need to take care of yourself. It won’t do you or the borderline any good to deny or excuse his or her abuse and think that having a personality disorder justifies it in any way – it does not.
You cannot control what a person with BPD does, but, you can make choices about what you will and what you will not live with. Once you make that choice you need to identify and make known boundaries that are firmly explained and firmly enforced consistently.
Many non-borderlines do not realize that the sane choice for them if the borderline in their lives is not getting help and/or cannot take personal responsibility and stop and change any and all abusive behavior and/or relating, is to leave, break free and take care of themselves.
Emotionally Abusive Borderline Relationships Information
Dealing with emotionally abusive borderline relationships can cause many to not recognize the signs of abuse because they feel love or empathy towards the borderline person.
Emotional abuse is usually subtle and often we do not know it is occurring. It could be controlling someone’s behavior in passive-aggressive ways, so they feel guilty about going out with their friends.
How do emotionally abusive borderline relationships get played out? Those with Borderline Personality Disorder (BPD) can portray themselves as the victim and their partner as the villain who becomes blamed for the problems.
Often, the person with BPD will react towards loved ones as if they were the abusers from their past, and take out vengeance and anger towards them.
When the person with BPD feels abandoned, they can become abusive or controlling as a way to defend against feelings of abandonment or feeling unworthy.
Often, the trail of destruction can adversely impact the relationship, causing the relationship to end pre-prematurely. Often, the person with BPD is unaware of how they drive their relationships away, which perpetuates the belief that others are abandoning them, all of the time.
Often, the person with BPD is unaware of how they drive their relationships away, which perpetuates the belief that others are abandoning them, all of the time.
Emotional abuse in Borderline Personality Disorder can be an everyday occurrence, without realizing it. Consider a typical example of a man with BPD who complains that his partner ignores all of his text messages, saying that she is rude and does not respond.
Whereas, she advised him that she was catching up with friends and wanted some time to herself. She checks her phone and finds messages of being accused of having an affair and not consider him.
She feels guilty about having fun with her friends and feels controlled, which repels her from contacting him, so she ignores his messages until she ends up becoming the person who does not care about his feelings, by ‘acting out’ the person that he projects her to be.
In this example, the man is avoiding the negative feelings that he has about himself, including insecurity and jealousy, by externalizing the blame, so that his partner has a problem that needs to be fixed.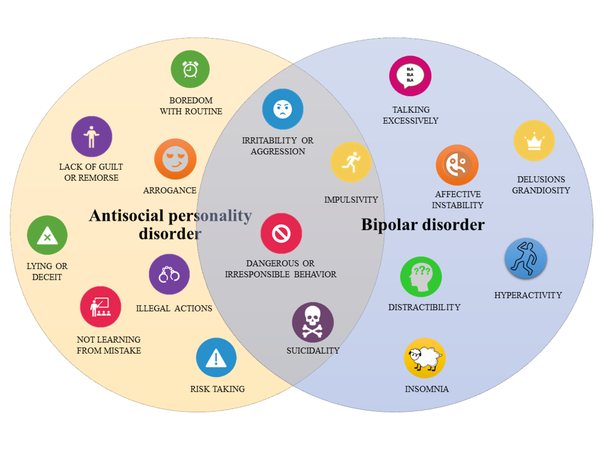 This prevents him from facing his feelings or dealing with his relationship.
This prevents him from facing his feelings or dealing with his relationship.
These relationships end up stuck in the blame game, due to the defense mechanism splitting. It in order for change to occur, it is necessary to deal with the splitting defensive pattern in the person who is borderline.
According to James Masterson, the borderline person holds onto a re-union fantasy of the hope that the Rewarding Loved Object (caregiver) will return and love them in the form of an adult relationship, causing them to cling to relationships.
When this does not occur, or they perceive abandonment, it triggers the Withdrawing Object fantasy, causing them to believe that everyone will eventually abandonment them because they feel not good enough.
Often, the emotional abuse in BPD occurs when defending against the perceived threat of abandonment, or avoiding feelings of abandonment, by holding onto a re-union fantasy of the Rewarding Object who will love them.
When the partner does not fit this fantasy, they’re perceived as unloving, uncaring or abandoning, becoming the Withdrawing Object.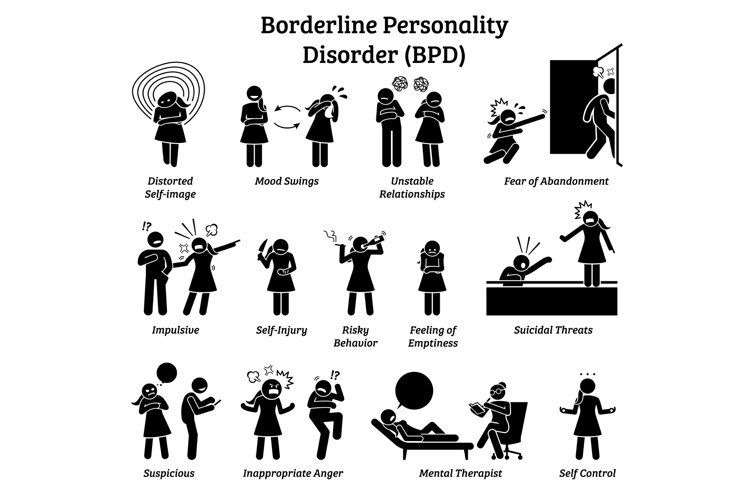 The person with BPD distorts the way they see others, as either ‘loving’ or ‘non-loving’, ‘good’ or ‘bad’.
The person with BPD distorts the way they see others, as either ‘loving’ or ‘non-loving’, ‘good’ or ‘bad’.
RELATED ARTICLE: Borderline Personality and Abuse Cycle
Those suffering from Borderline Personality Disorder use the defense mechanism called splitting, which causes them to see themselves and others as extremes of either ‘good’ or ‘bad’. This causes them to feel love or hate, happy or sad.
When the borderline person perceive others are abandoning them, they feel bad about themselves. Whereas, when they perceive others love them, this causes them to feel good about themselves. In this way, the person with BPD has a sense of self that is dependent upon how others treat them.
A person may feel that they are good because they please their partner and put lots of effort into making them happy, whereas they may feel that their partner is uncaring or unloving because they do not put the same effort into the relationship.
When the BPD person becomes triggered to feeling unworthy or abandoned, they project these feelings onto their partner, since they cannot tolerate them within themselves.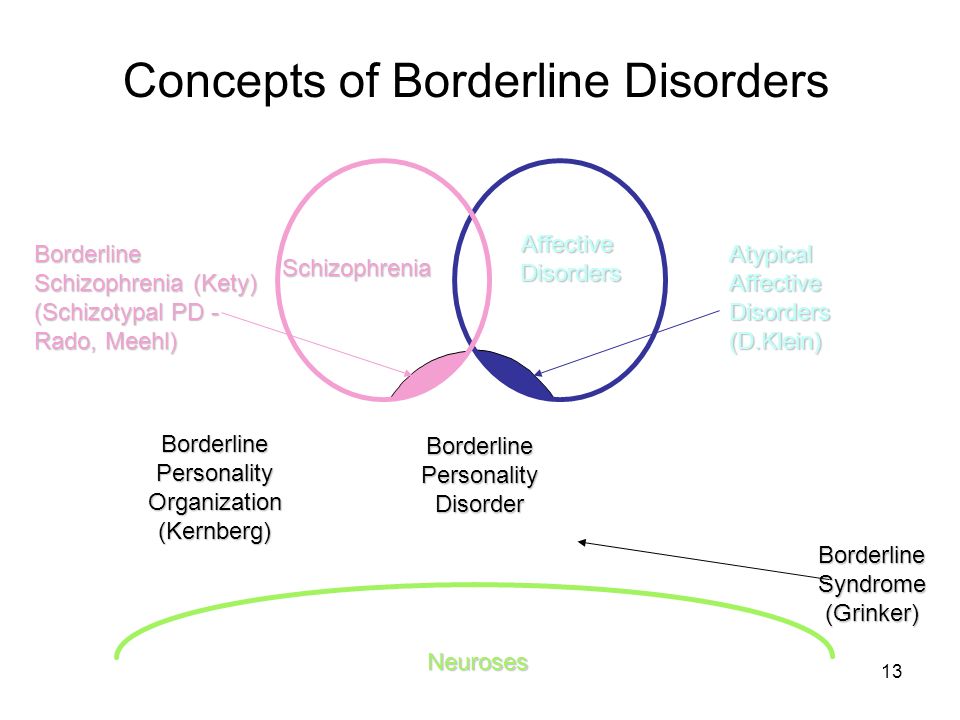 In this way, their partner becomes all bad, uncaring or mean, and treated accordingly.
In this way, their partner becomes all bad, uncaring or mean, and treated accordingly.
If a partner does not return a call, he can be depicted to be uncaring or rejecting.
Forgetting to call can trigger past feelings of being unwanted, that become so overwhelming that they are displaced onto the partner for treating them this way.
The partner can be on the receiving end of an abusive attack and feel wrongly accused.When a person perceives that their partner is causing the pain, they become the problem.
It becomes difficult to see any good in a partner if one puts their past wounds onto them, so they become the person who is seen as causing the hurt. It is easy to take out your anger on the person you feel is responsible for it.
The husband who came home late is seen as not caring about his wife. A wife may not think her spouse loves her, no matter what he says.
When the BPD person is caught in the negative side of the split, anything that their partner does can be seen as bad (unloving or uncaring), because it brings up how bad she feels (not good enough). Her partner could meet all her needs and it might not make the difference.
Her partner could meet all her needs and it might not make the difference.
If you are in a relationship with a person with BPD and feel blamed for things that do not represent your actions, there can be ways to manage this.
Dealing With Emotional Abuse In Borderline Personality Disorder- In dealing with emotional abuse in borderline personality disorder, it’s imperative to separate the behavior from the person who is borderline. Instead of judging the person, focus on the behavior that was hurtful and express how it impacted you, to set a limit on the behavior.
- Placating the aggressive behavior, or letting them get away with it, will only enable the behavior to continue through positive reinforcement.
- Instead of reacting, by feeling blamed or attacked, see their behavior as way to get out what they are feeling and use it as an opportunity to be curious about how they are feeling. This allows them to take responsibility for how they are feeling, rather than displacing their feelings onto others.
- It’s more effective to come back to the discussion when things are calm and be curious as to why they took your actions in a certain way, and point out that that it was not your intention; to challenge the perception.
- Show astonishment that they see you in a particular light, if it does not fit. “Why do you think I do not love you, when I missed your call”.
- After all this, if the emotional abusive borderline partner cannot own their behavior and take responsibility for addressing it, then you might want to ask yourself, ‘why do you put with it’?
In managing emotional abuse in BPD relationships, boundaries and limits are often necessary early, before the abusive behavior becomes set in stone. The person who is borderline needs to understand that their actions can hurt others, which is often outside of their awareness.
This needs to be said in a non-judgmental and non defensive manner, yet stated firmly with conviction. The unwanted behavior is addressed by not blaming the individual, otherwise it will trigger the negative self beliefs, which are likely to become defended against with rage and anger.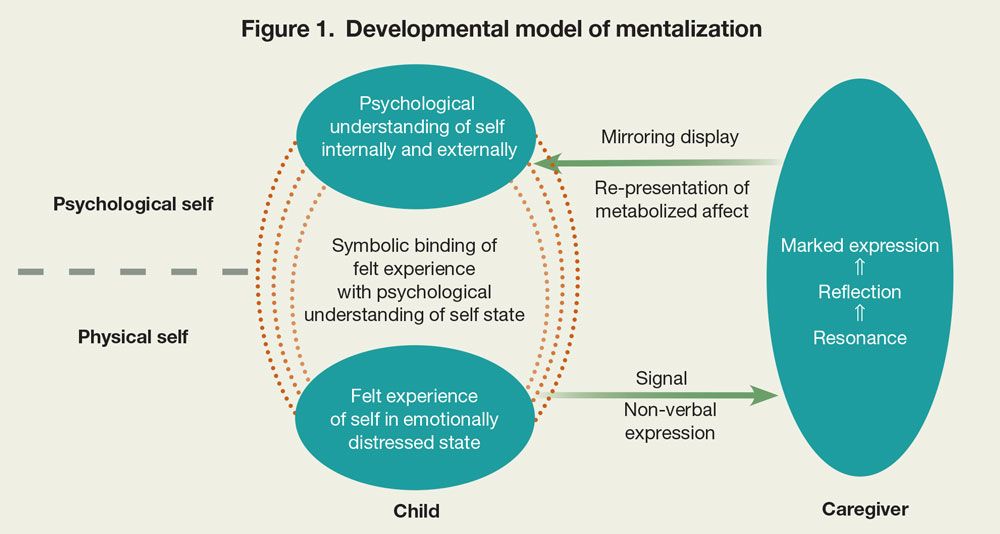
It more effective to understand the feelings behind the reaction, rather than react towards any accusatory or blaming behavior. It becomes easier to clarify what they feel, so you understand their feelings and point out any areas that you feel do not fit your actions.
It is wise to not say ” You’re wrong or crazy, otherwise you will become the person they fear. This will allow the person who is borderline to see that you are not the person you are accused to be.
This will assist them to see the situation more clearly, when they get more in touch with how they feel. This will assist them to deal with their feelings and take responsibility for their behavior.
When the person who is borderline is gently challenged on hurtful behavior, the defensive acting out behavior stops. The behavior improves, but it brings up the underlying bad feelings.
This can be a vulnerable time when the borderline needs containment for how they feel, since they will get in touch with past feelings and feelings of worthlessness.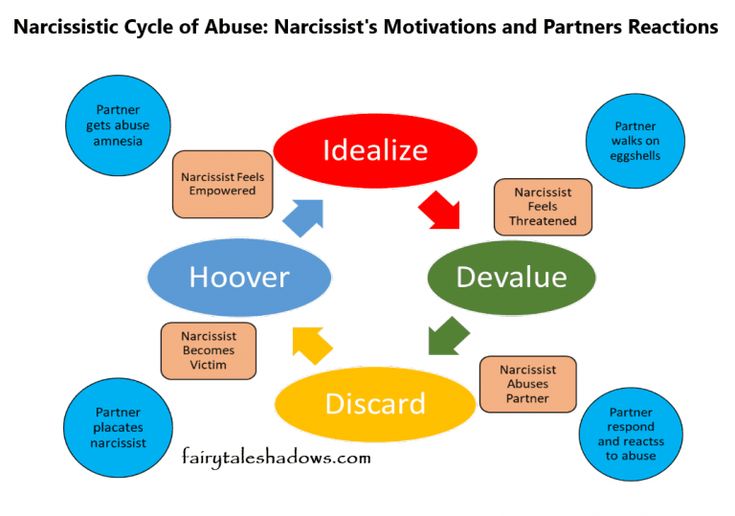
However, usually the feelings are too intense for the person who is borderline to handle on their own, and therefore it is imperative for them to attend counseling to process the underlying feelings.
Otherwise they will have no way to manage the feelings when they come up, causing them to get stuck in defensive patterns once again.
The defenses are there because the ‘self’ is not strong enough to face the intense feelings, so therapy is required to build the capacity and strength within themselves to manage the intense feelings.
Preventing Abuse In Borderline Personality DisorderNancy Carbone provides individual Counselling Melbourne services and couples counseling for those with personality difficulties. Nancy trained at International Masterson Institute in New York for the Psychanalytic Treatment of Personality Disorders.
You can visit https://www.counsellingservicemelbourne.com.au/personal-counselling/relationship-counselling/ . To visit more mental health articles at Counselling in Melbourne follow us on social media on Facebook and Twitter.
To visit more mental health articles at Counselling in Melbourne follow us on social media on Facebook and Twitter.
© All written content is copyright Nancy Carbone 2018
Borderline personality disorder
Borderline personality disorder ( BPD ) is a long-term mental illness. It is a type of Cluster B personality disorder. People diagnosed with PPD are often very impulsive and tend to have low self-esteem. The mood often changes quickly. For these reasons, such people often have trouble maintaining stable relationships. Often, people with BPD also suffer from other illnesses, such as clinical depression, or exhibit self-injurious behavior. Treating people with BPD is difficult and usually involves a combination of therapy and medication.
C.H. Hughes used the term "border zone" to describe a range of conditions bordering on mental disorders. Adolf Stern described some of the symptoms in 1938 and called them the "border group". Both psychotic and neurotic conditions have been observed in humans, so the term was considered appropriate at the time.
Youth by the Sea" is a painting by Edvard Munch, painted in 1904. It is part of Lind's frieze. According to art historian Nikolai Stang, this painting demonstrates the inability to establish contact with other people (which is one of the main symptoms of BPD). Some psychologists have diagnosed Munch as suffering from BPD
Symptoms
People diagnosed with BPD have severe mood swings. They perceive things as "all good" or "all bad" (split) and are often confused about their identity. They usually have a lot of problems in relationships with people. They have strong emotions that often change quickly. They are often reckless, destructive, or self-destructive.
Emotions
People with BPD experience emotions easier, deeper and longer than others. [10][11] Emotions can come back repeatedly and last for a long time. [11] Because of this, people with BPD may take longer than usual to return to a normal and stable emotional state.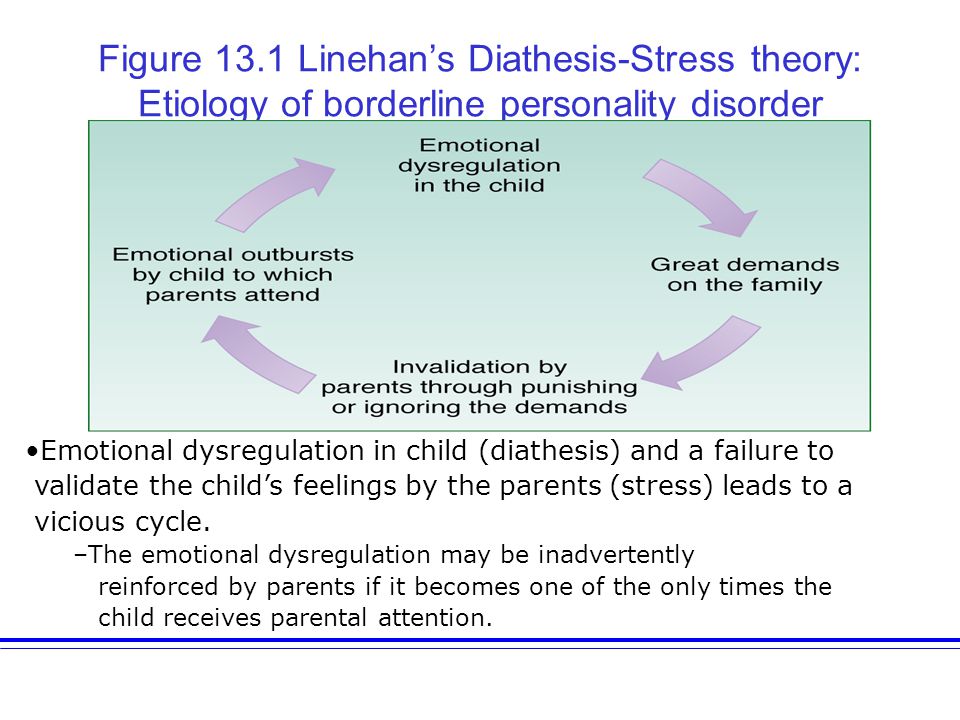 [12] This can have both positive and negative consequences. [12] People with BPD are often very happy and loving. [13] People with BPD are also often sad and angry. They feel emotions more strongly than most people: grief instead of sadness, rage instead of irritation, panic instead of anxiety. [13] People with BPD are particularly sensitive to feelings of abandonment, loneliness, and "failure". They are often aware of how strong their emotions are, and since they cannot control them, sometimes they close them completely. [12]
[12] This can have both positive and negative consequences. [12] People with BPD are often very happy and loving. [13] People with BPD are also often sad and angry. They feel emotions more strongly than most people: grief instead of sadness, rage instead of irritation, panic instead of anxiety. [13] People with BPD are particularly sensitive to feelings of abandonment, loneliness, and "failure". They are often aware of how strong their emotions are, and since they cannot control them, sometimes they close them completely. [12]
Their emotions are intense and change rapidly. Their most common mood swings are between anger and anxiety, and between depression and anxiety. [17]
Behavior
People with BPD often act impulsively, which means they do or say things that are not thoughtful. These behaviors can be dangerous and include: drug or alcohol abuse, too much or too little food, unsafe or frequent sex with multiple partners, spending a lot of money, and driving dangerously.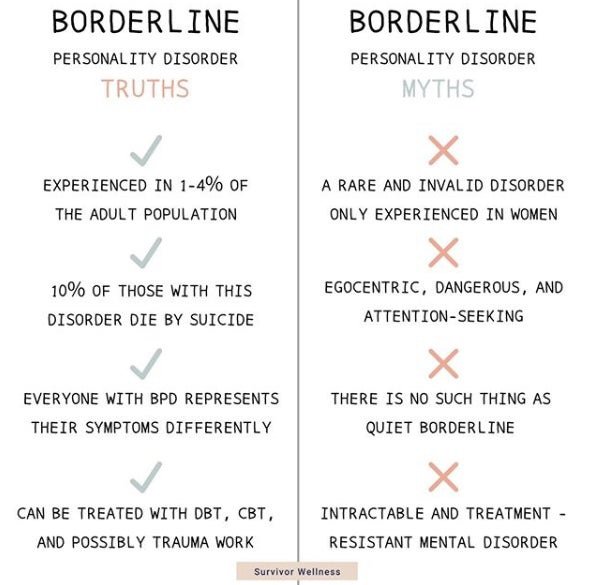 Impulsive behavior may also include leaving work or relationships, running away, and self-harm. [19]
Impulsive behavior may also include leaving work or relationships, running away, and self-harm. [19]
People with BPD sometimes act impulsively because it gives them instant relief from emotional pain. [19] However, in the long term, people with BPD experience even greater pain from the shame and guilt that follow these actions. [19] A cycle often begins when people with BPD feel emotional pain and act impulsively to relieve that pain. They then feel bad about what they have done and have a strong urge to act impulsively to relieve new pain. [19] Over time, impulsive behavior can become an automatic response to emotional pain. [19]
Self-harm and suicide
Self-harm is common among people with BPD. Sometimes people harm themselves by not wanting to commit suicide. Common methods include cuts, burns, headbutts, and drug overdoses. The reasons why people with BPD commit non-suicidal self-harm (NSSI) differ from the reasons for attempting suicide.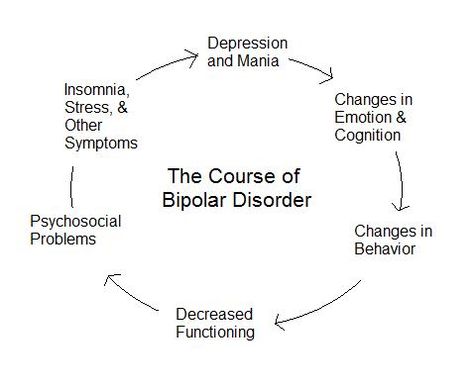 Their reasons for hurting themselves include expressing anger, punishing themselves, creating normal feelings, and distracting from emotional pain or difficult situations. When the goal is suicide, they usually try to kill themselves, believing that others will be better off without them. Both suicidal and non-suicidal self-harm is a response to negative emotions.
Their reasons for hurting themselves include expressing anger, punishing themselves, creating normal feelings, and distracting from emotional pain or difficult situations. When the goal is suicide, they usually try to kill themselves, believing that others will be better off without them. Both suicidal and non-suicidal self-harm is a response to negative emotions.
Interpersonal relationships
People with BPD can be very sensitive to how others treat them. They may feel very happy and grateful when they feel someone has been kind to them, and very sad or angry when they feel someone has hurt them. Their feelings towards others often change from positive to negative if they think they might lose someone, if they think that someone important to them doesn't care about them, or if something isn't as good as they are. expected. They think in extremes, perceiving things or people as "all good" or "all bad". This is sometimes called "black and white thinking". This includes going from admiring someone to devaluing them, often with a feeling of pure anger or dislike.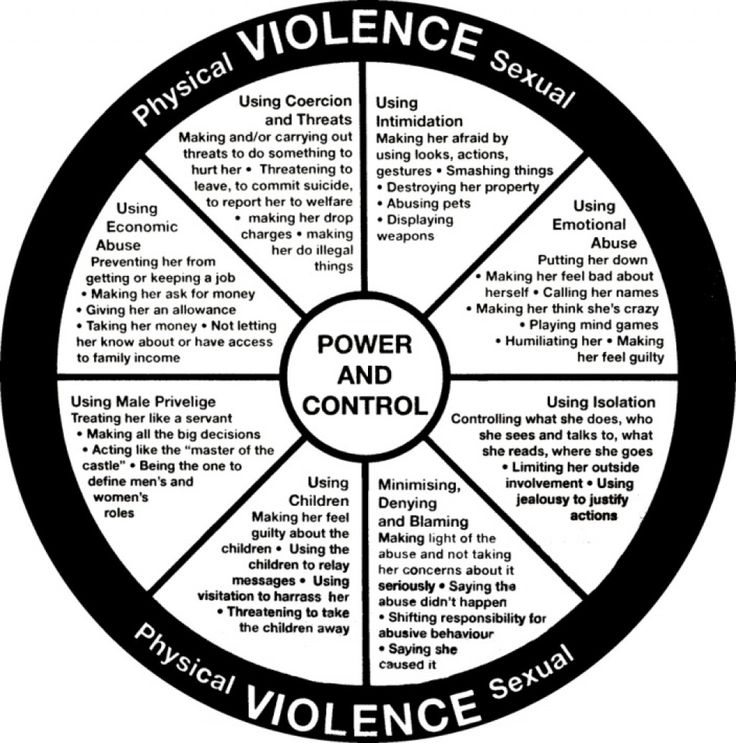 [28] The way they perceive themselves can also change rapidly from positive to negative.
[28] The way they perceive themselves can also change rapidly from positive to negative.
Despite a strong desire to feel close, people with BPD tend to experience anxiety, mixed feelings, or paranoia when it comes to their relationships. They often perceive the world as dangerous and bad. BPD is associated with high levels of stress and conflict in romantic relationships, abuse, and unwanted pregnancies. All this is characteristic of other types of personality disorders.
Self-esteem
People with BPD tend to have difficulty understanding their own identity. It is difficult for them to understand what they value and love. [35] They are often unaware of their long-term goals in relationships and work. They often find it difficult to make decisions and can change their mind quickly. These difficulties can leave people with BPD feeling "empty" and "lost". [35]
Cognitions
People with BPD get bored easily and have difficulty concentrating.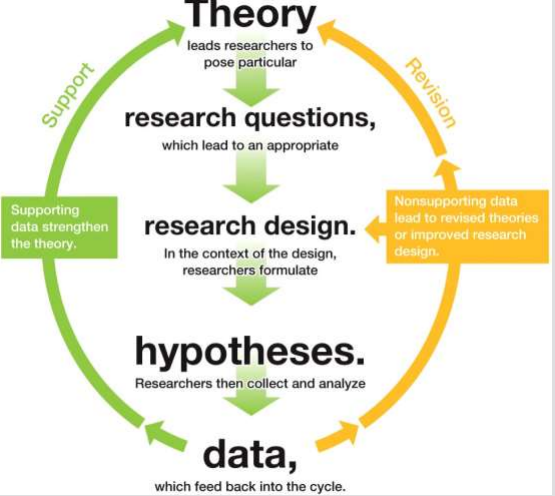 [35] People with BPD may disconnect or "dissociate" from people and things around them, which can be seen as an intense form of "disconnection". [36] This often occurs in response to a painful event or something that evokes memories of a painful event. This may help the person feel better for a short time, but may also have the undesirable side effect of blocking normal feelings. This results in people with BPD not being able to learn to deal with these feelings, and it may be difficult for them to make positive choices when they experience these emotions. [36] Sometimes other people may notice that a person with BPD is dissociated because their expression or voice may appear emotionless, or they may appear distracted. Sometimes when a person with BPD dissociates, other people don't see or know it's happening. [36]
[35] People with BPD may disconnect or "dissociate" from people and things around them, which can be seen as an intense form of "disconnection". [36] This often occurs in response to a painful event or something that evokes memories of a painful event. This may help the person feel better for a short time, but may also have the undesirable side effect of blocking normal feelings. This results in people with BPD not being able to learn to deal with these feelings, and it may be difficult for them to make positive choices when they experience these emotions. [36] Sometimes other people may notice that a person with BPD is dissociated because their expression or voice may appear emotionless, or they may appear distracted. Sometimes when a person with BPD dissociates, other people don't see or know it's happening. [36]
Knife cuts, on the upper arm. People with BPD often hurt themselves.
Diagnosis
Psychiatrists and other mental health professionals diagnose people with BPD using a book called the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR).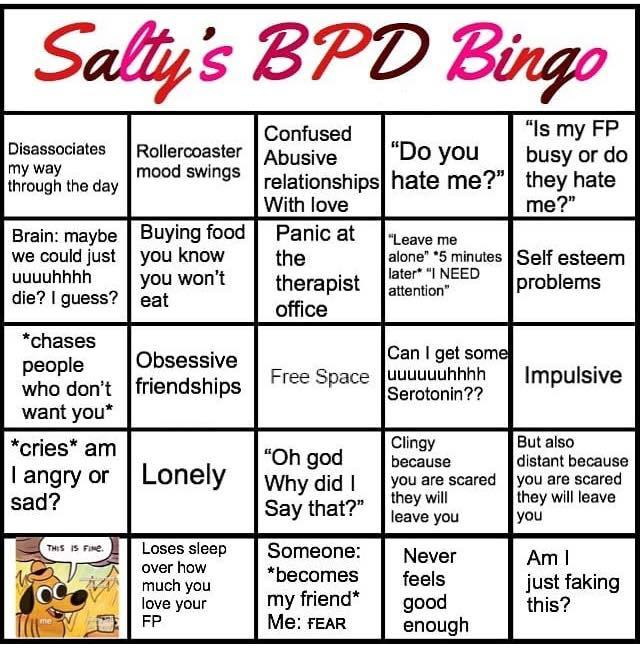 They look at the behavior of a person and his well-being. If a person has five or more of the following, the DSM-IV-TR says they have BPD.
They look at the behavior of a person and his well-being. If a person has five or more of the following, the DSM-IV-TR says they have BPD.
- They are afraid and try their best not to be abandoned or rejected
- Characterized by relationship problems, often thinking that other people are much better or much worse than they really are, and quickly move from one opinion to to another.
- Confused about self
- impulsiveness in dangerous activities (eg, casual sex, drinking too much alcohol or drug abuse, not eating or overeating, reckless driving)
- Attempts to commit suicide or self-harm
- Mood swings - sudden feelings of happiness, sadness or anxiety that can last for several hours
- Feeling empty or constantly bored
- Severe anger problems, often getting into fights
- Presence of severe paranoid thoughts
Comorbidity
Almost all people with BPD also have other psychiatric disorders such as mood disorders, attention deficit hyperactivity disorder, eating disorders, anxiety disorders (especially post-traumatic stress disorder) and other personality disorders.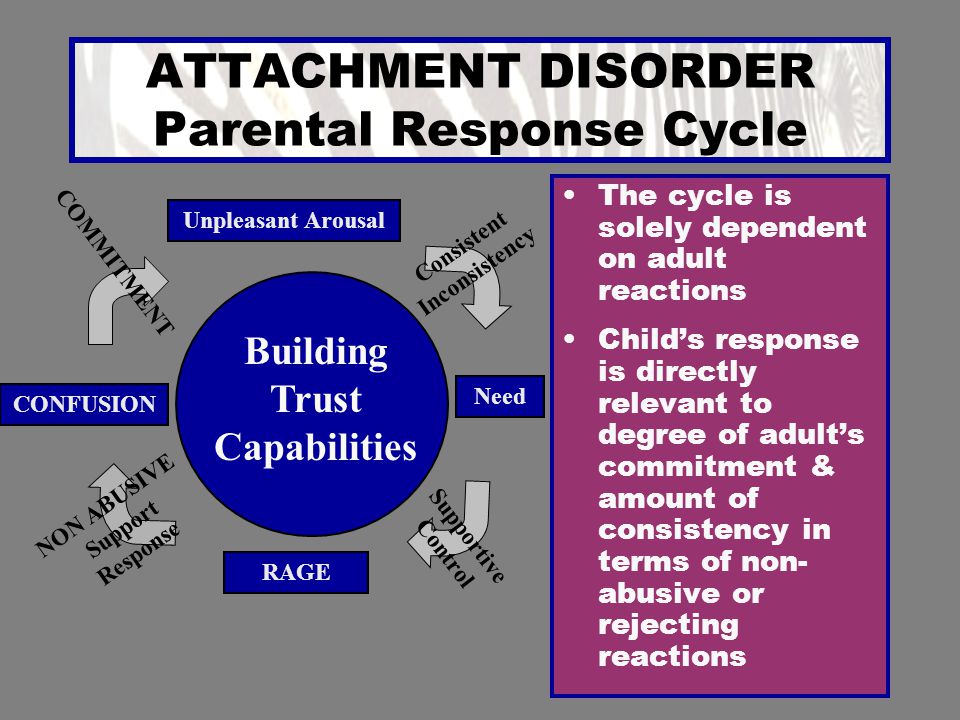 Most have or have had substance abuse and/or addiction. Self-harm and suicidal behavior are also common.
Most have or have had substance abuse and/or addiction. Self-harm and suicidal behavior are also common.
Other diseases that are common in BPD include diabetes, high blood pressure, chronic back pain, arthritis, and fibromyalgia.
Cause
The cause of BPD is unknown. There can be several reasons for the development of BPD. Some researchers believe that it may be caused by childhood trauma such as sexual abuse, physical abuse, and neglect. Many people with BPD have been abused as children. According to modern concepts, which demonstrate a functioning MRI, the neurotransmitters in the brain are not working properly, and messages are transmitted in an unusual way.
Treatment
BPD treatment is very difficult and time consuming. Today, most people with BPD are treated with various types of psychotherapy. One of them is called Dialectical Behavior Therapy. Drugs such as antidepressants, antipsychotics, or mood stabilizers are often used in addition to therapy.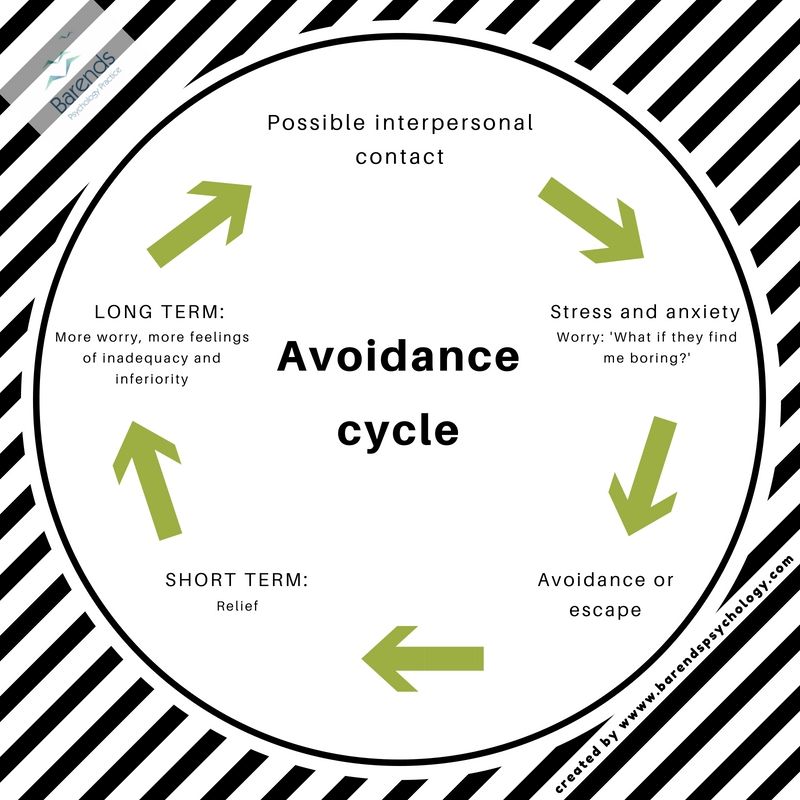 Many patients recover within 10 years.
Many patients recover within 10 years.
FAQ
Q: What is borderline personality disorder (BPD)?A: PPD is a long-term mental illness that is classified as a type of cluster B personality disorder. People diagnosed with BPD often have impulsive behavior, low self-esteem, and rapidly changing moods, which can make it difficult to maintain stable relationships.
Q: What other illnesses are commonly associated with BPD?
A: People with BPD may also suffer from clinical depression or engage in self-injurious behavior.
Q: How is BPD treated?
A: Treatment for people with BPD usually involves a combination of therapy and medication.
Q: Who first used the term "Frontier" to describe mental health conditions?
A: C.H. Huges was the first person to use the term "Frontier" to describe mental health conditions.
Q: When was the term "border group" coined?
A: The term "border line group" was coined by Adolf Stern at 1938 when he described some of the symptoms associated with borderline personality disorder (BPD).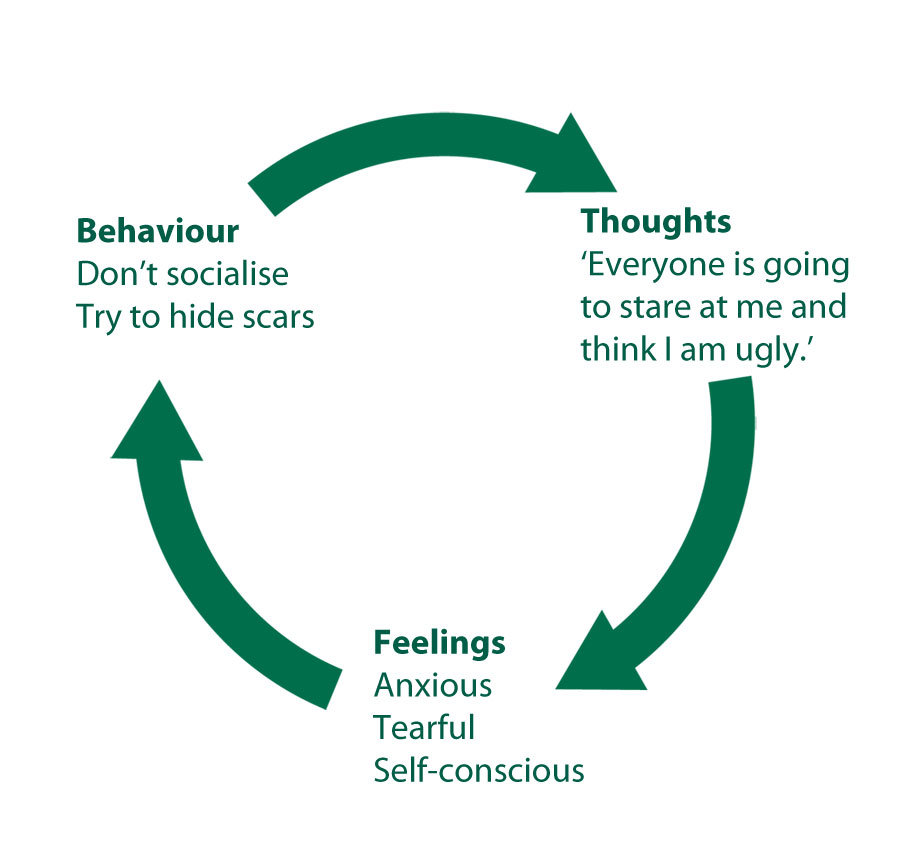
Q: What does the term "Border Strip" refer to?
A: The term "borderline" refers to a range of conditions that border on mental disorders, such as those seen in people diagnosed with borderline personality disorder (BPD).
Author
Alegsaonline.com - Borderline Personality Disorder - Leandro Alegsa - 2022-02-21 14:25:02 - url: https://ru.alegsaonline.com/art/13080Bibliographic references
- doi.org - 10.1111/j.1600-0447.2004.00466.x - pubmed.ncbi.nlm.nih.gov - 15819731 - new.borderlinepersonalitydisorder.com - "A BPD Brief" - doi.org - 10.1521 /pedi.1994.8.4.257-pubmed.ncbi.nlm.nih.gov - 3895199- doi.org - 10.1037/0021-843X.111.1.198- pubmed.ncbi.nlm.nih.gov - 11866174- doi.org - 10.1016 /j.jbtep.2005.06.001- pubmed.ncbi.nlm.nih.gov - 16018875- doi.org - 10.1159/000084813- pubmed.ncbi.nlm.nih.gov - 15802944- doi.org - 10.1037/0021-843X .109.3.451-pubmed.ncbi.nlm.nih.gov - 11016115- www.psychiatryonline.com - 301.83 Borderline Personality Disorder- doi.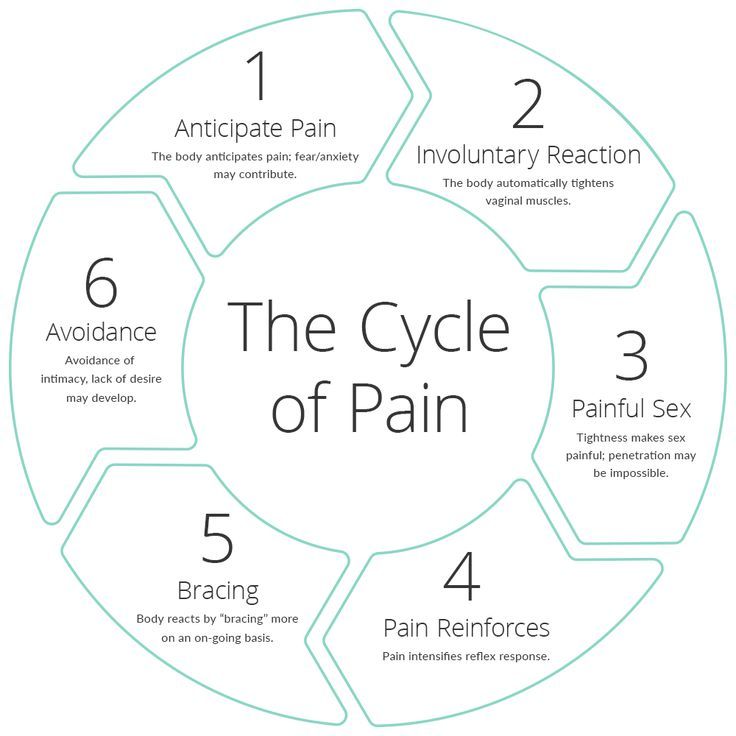 org - DOI: 10.1176/appi.books.9780890423349.3831
org - DOI: 10.1176/appi.books.9780890423349.3831 Sleep disorders in people with borderline personality disorder. - Information Portal
Substance abuse, self-harm, lifestyle and nutritional problems in people with borderline personality disorder (BPD) contribute to the risk of many negative physical health outcomes such as heart disease, diabetes, arthritis, and chronic sleep problems.
Sleep disturbance is common in young adults (15–25 years) with features of borderline personality disorder: unstable interpersonal relationships, emotions and self-image, and impulsive behavior (Jenkins, Thompson, Chanen). Compared with healthy young adults, people with BPD symptoms report worse subjective sleep quality and objectively show longer, late, and irregular sleep (Jenkins, Tiley, Lay, Wall, Vanwoerden, Penner).
Emotional dysregulation, a defining feature of BPD, is associated with sleep disturbance (according to Goldschmied, Palagini, Moretto). Emotion regulation difficulties disrupt sleep due to increased arousal and negative affect, while sleep problems exacerbate emotional dysregulation.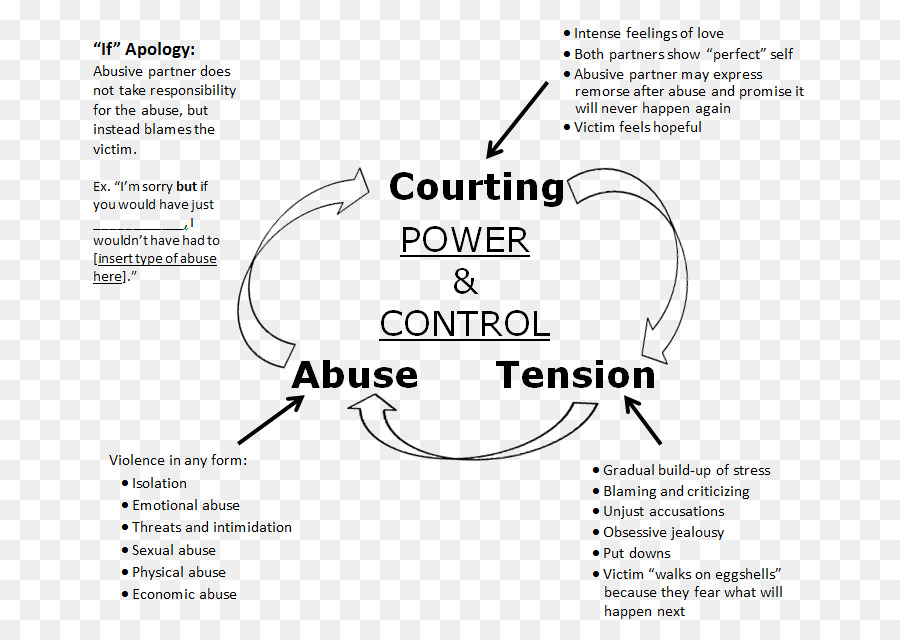 Young adults whose emotion regulation skills are still developing may be especially susceptible to the emotional consequences of poor sleep. Nightmares, which are common in people with BPD, can also exacerbate daytime emotional dysregulation and may even increase the risk of self-harm by heightening the response to trauma.
Young adults whose emotion regulation skills are still developing may be especially susceptible to the emotional consequences of poor sleep. Nightmares, which are common in people with BPD, can also exacerbate daytime emotional dysregulation and may even increase the risk of self-harm by heightening the response to trauma.
Other factors associated with emotional dysregulation, such as depression, anxiety, or stress, may underlie sleep problems. Although the sleep problems in BPD cannot be attributed solely to comorbid depression, the two disorders share similar manifestations of sleep disturbance. Awakening may be exacerbated by nightmares in people with BPD symptoms who report increased sleep anxiety and fear of falling asleep due to anticipation of a nightmare. Anxiety and stress-related arousal, combined with increased baseline arousal in BPD, may contribute to sleep disturbance.
When people with BPD get enough rest, their tendency to become paranoid and suspicious decreases.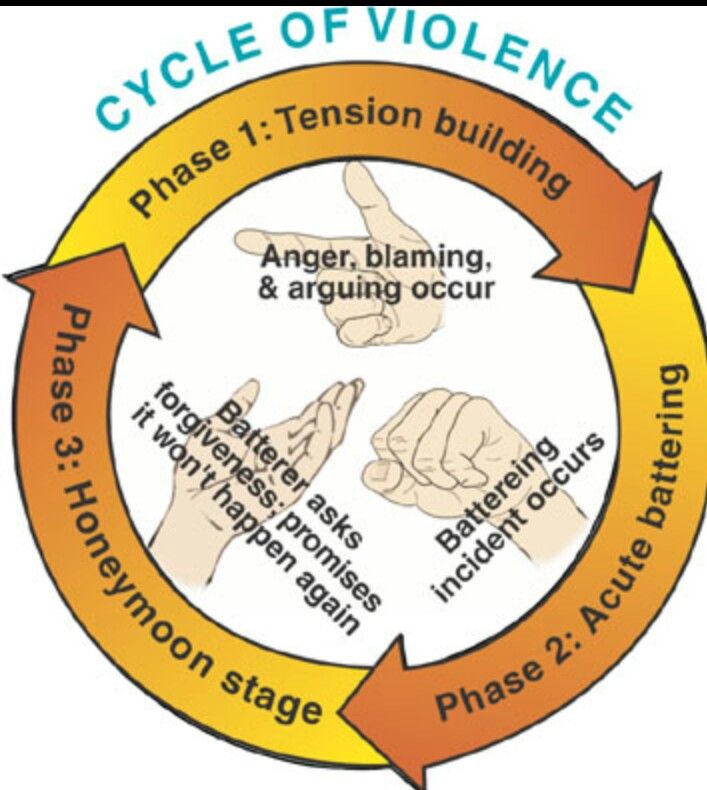 When insomnia sets in, suspicion and anxiety increase and a self-feeding cycle is formed.
When insomnia sets in, suspicion and anxiety increase and a self-feeding cycle is formed.
It is very important for people with BPD to optimize their sleep patterns, as good sleep will contribute to a productive day and reduce the risk of self-harm. Sleep disturbance is a biological vulnerability that will promote destructive behavior, relapse and longer recovery.
What should be done to improve sleep?
Advice for sleep disorders:
Go to bed at about the same time every night.
Get up at about the same time every morning.
Prepare your bedroom the way you like it (for example, many people pay attention to noise levels, light levels and temperature).
Pay close attention to what you eat before going to bed, as well as at the time of such meals.
Obsessive thoughts can disturb the sleep of any person. If you notice that thoughts are keeping you awake, focus all your attention on those thoughts. Define and label them. You may find that a thought is as fleeting as a sound or sensation.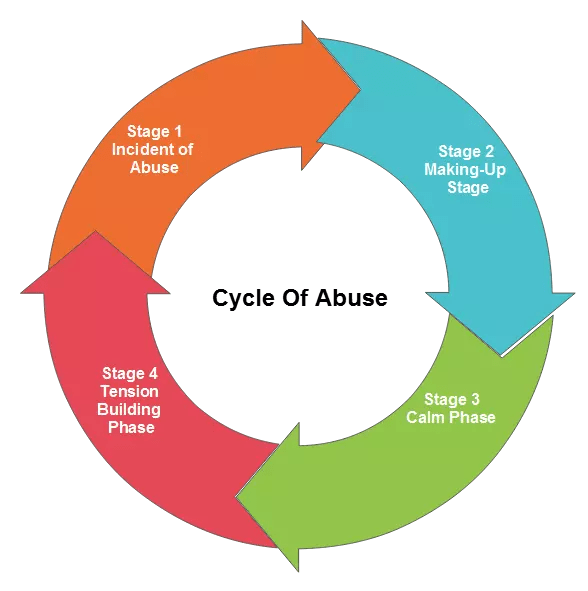
Physical awareness of the body is important in correcting sleep disorders. Think about one body part at a time. Focus on relaxing that spot and then move on. Step by step, let your whole body relax and move into a favorable sleep state.
Breathing exercises. In many cases, counting is the most successful. You can just count each breath. Another option is to count the length of each inhalation and then each exhalation.
Seek help from mental health professionals!
Improving sleep for people with borderline personality disorder can help them cope with stressful situations, use coping skills, and increase overall energy levels. In turn, improving your ability to cope with stress can further reduce sleep problems.
Sources
1. https://bpded.biomedcentral.com/articles/10.1186/s40479-022-00180-2
2. https://suffolkdbtjl.com/insomnia-and-borderline-personality-disorder -how-dbt-for-sleep-can-help/
3. https://www.