Best medicine for ocd and depression
Obsessive-compulsive disorder (OCD) - Diagnosis and treatment
Diagnosis
Steps to help diagnose obsessive-compulsive disorder may include:
- Psychological evaluation. This includes discussing your thoughts, feelings, symptoms and behavior patterns to determine if you have obsessions or compulsive behaviors that interfere with your quality of life. With your permission, this may include talking to your family or friends.
- Diagnostic criteria for OCD. Your doctor may use criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
- Physical exam. This may be done to help rule out other problems that could be causing your symptoms and to check for any related complications.
Diagnostic challenges
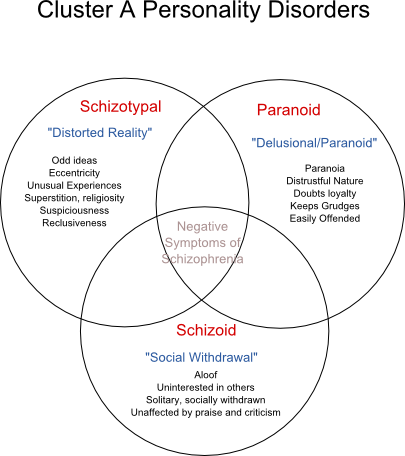
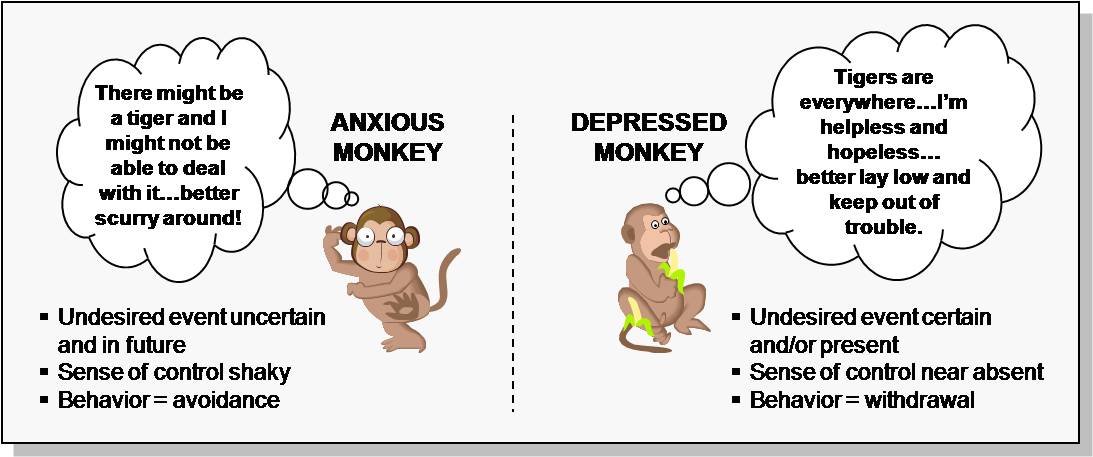
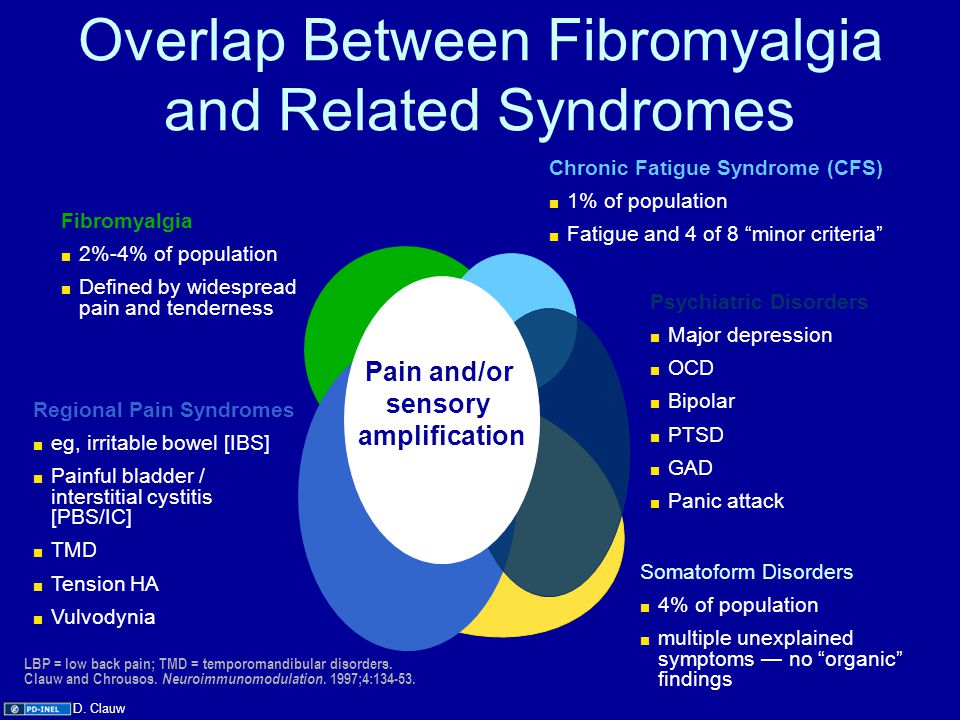
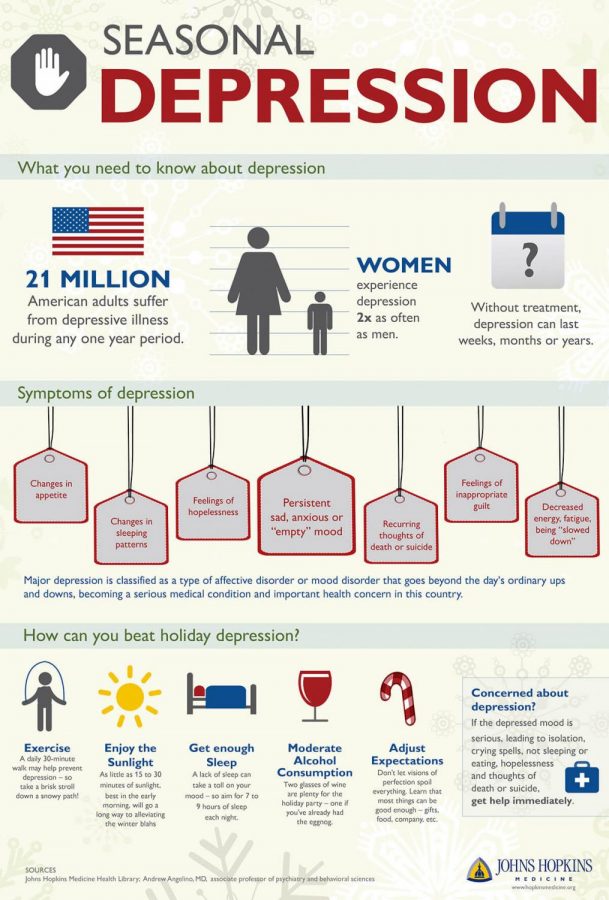
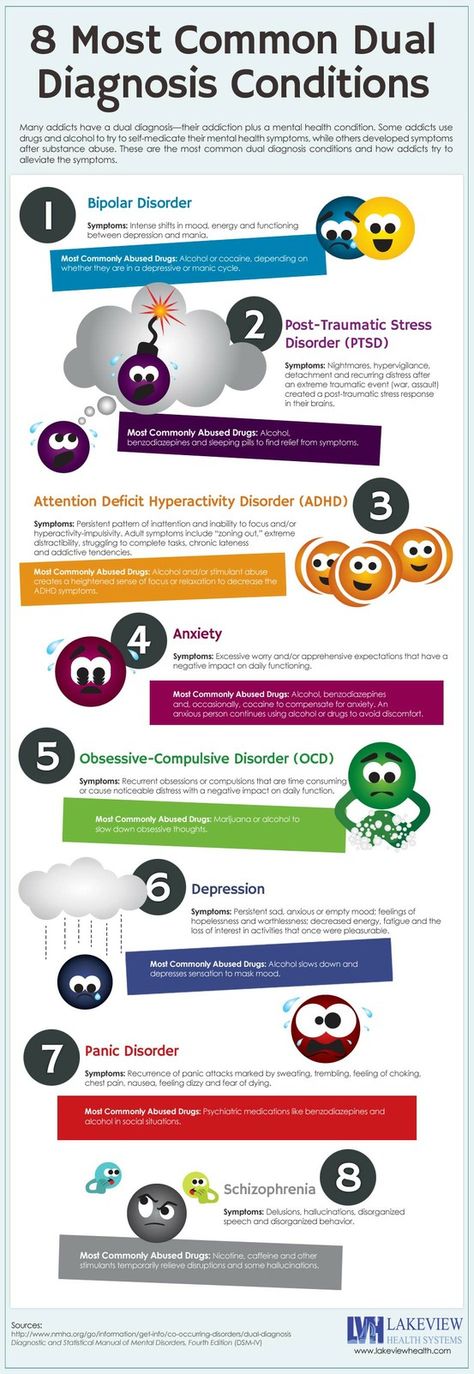
It's sometimes difficult to diagnose OCD because symptoms can be similar to those of obsessive-compulsive personality disorder, anxiety disorders, depression, schizophrenia or other mental health disorders. And it's possible to have both OCD and another mental health disorder. Work with your doctor so that you can get the appropriate diagnosis and treatment.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your Obsessive-compulsive disorder (OCD)-related health concerns Start Here
Treatment
Obsessive-compulsive disorder treatment may not result in a cure, but it can help bring symptoms under control so that they don't rule your daily life. Depending on the severity of OCD, some people may need long-term, ongoing or more intensive treatment.
The two main treatments for OCD are psychotherapy and medications. Often, treatment is most effective with a combination of these.
Psychotherapy
Cognitive behavioral therapy (CBT), a type of psychotherapy, is effective for many people with OCD.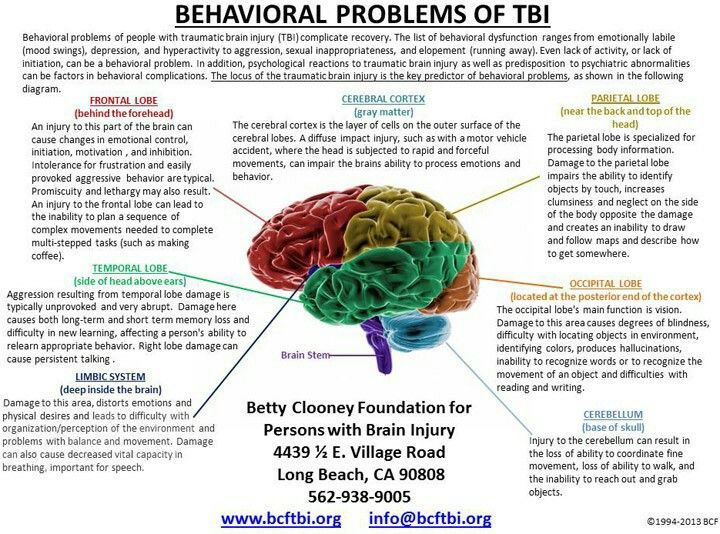 Exposure and response prevention (ERP), a component of CBT therapy, involves gradually exposing you to a feared object or obsession, such as dirt, and having you learn ways to resist the urge to do your compulsive rituals. ERP takes effort and practice, but you may enjoy a better quality of life once you learn to manage your obsessions and compulsions.
Exposure and response prevention (ERP), a component of CBT therapy, involves gradually exposing you to a feared object or obsession, such as dirt, and having you learn ways to resist the urge to do your compulsive rituals. ERP takes effort and practice, but you may enjoy a better quality of life once you learn to manage your obsessions and compulsions.
Medications
Certain psychiatric medications can help control the obsessions and compulsions of OCD. Most commonly, antidepressants are tried first.
Antidepressants approved by the U.S. Food and Drug Administration (FDA) to treat OCD include:
- Clomipramine (Anafranil) for adults and children 10 years and older
- Fluoxetine (Prozac) for adults and children 7 years and older
- Fluvoxamine for adults and children 8 years and older
- Paroxetine (Paxil, Pexeva) for adults only
- Sertraline (Zoloft) for adults and children 6 years and older
However, your doctor may prescribe other antidepressants and psychiatric medications.
Medications: What to consider
Here are some issues to discuss with your doctor about medications for OCD:
- Choosing a medication. In general, the goal is to effectively control symptoms at the lowest possible dosage. It's not unusual to try several drugs before finding one that works well. Your doctor might recommend more than one medication to effectively manage your symptoms. It can take weeks to months after starting a medication to notice an improvement in symptoms.
- Side effects. All psychiatric medications have potential side effects. Talk to your doctor about possible side effects and about any health monitoring needed while taking psychiatric drugs. And let your doctor know if you experience troubling side effects.
- Suicide risk. Most antidepressants are generally safe, but the FDA requires that all antidepressants carry black box warnings, the strictest warnings for prescriptions.
 In some cases, children, teenagers and young adults under 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. If suicidal thoughts occur, immediately contact your doctor or get emergency help. Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
In some cases, children, teenagers and young adults under 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. If suicidal thoughts occur, immediately contact your doctor or get emergency help. Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood. - Interactions with other substances. When taking an antidepressant, tell your doctor about any other prescription or over-the-counter medications, herbs or other supplements you take. Some antidepressants can make some other medications less effective and cause dangerous reactions when combined with certain medications or herbal supplements.
- Stopping antidepressants.
Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur. So stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, sometimes called discontinuation syndrome.
 Don't stop taking your medication without talking to your doctor, even if you're feeling better — you may have a relapse of OCD symptoms. Work with your doctor to gradually and safely decrease your dose.
Don't stop taking your medication without talking to your doctor, even if you're feeling better — you may have a relapse of OCD symptoms. Work with your doctor to gradually and safely decrease your dose.
Talk to your doctor about the risks and benefits of using specific medications.
Other treatment
Sometimes, psychotherapy and medications aren't effective enough to control OCD symptoms. In treatment-resistant cases, other options may be offered:
- Intensive outpatient and residential treatment programs. Comprehensive treatment programs that emphasize ERP therapy principles may be helpful for people with OCD who struggle with being able to function because of the severity of their symptoms. These programs typically last several weeks.
- Deep brain stimulation (DBS).
 DBS is approved by the FDA to treat OCD in adults age 18 years and older who don't respond to traditional treatment approaches. DBS involves implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that may help regulate abnormal impulses.
DBS is approved by the FDA to treat OCD in adults age 18 years and older who don't respond to traditional treatment approaches. DBS involves implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that may help regulate abnormal impulses. - Transcranial magnetic stimulation (TMS). The FDA approved a specific device (BrainsWay Deep Transcranial Magnetic Stimulation) to treat OCD in adults ages 22 to 68 years, when traditional treatment approaches have not been effective. TMS is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of OCD.
 During a TMS session, an electromagnetic coil is placed against your scalp near your forehead. The electromagnet delivers a magnetic pulse that stimulates nerve cells in your brain.
During a TMS session, an electromagnetic coil is placed against your scalp near your forehead. The electromagnet delivers a magnetic pulse that stimulates nerve cells in your brain.
Talk with your doctor to make sure you understand all the pros and cons and possible health risks of DBS and TMS if you're considering one of these procedures.
More Information
- Obsessive-compulsive disorder (OCD) care at Mayo Clinic
- Cognitive behavioral therapy
- Deep brain stimulation
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.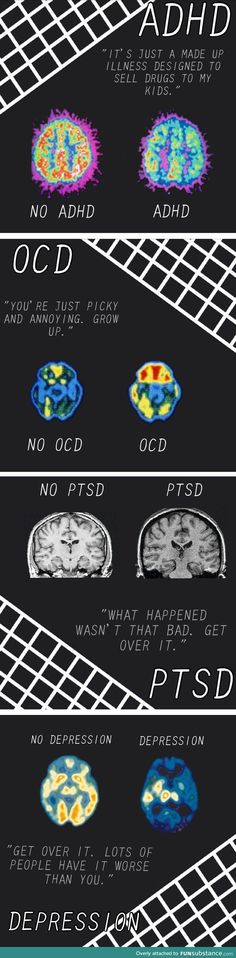
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Lifestyle and home remedies
Obsessive-compulsive disorder is a chronic condition, which means it may always be part of your life.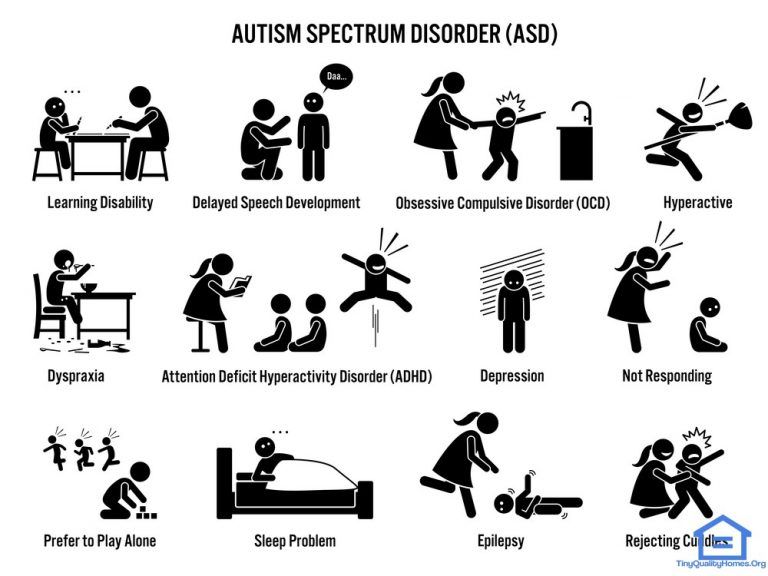 While OCD warrants treatment by a professional, you can do some things for yourself to build on your treatment plan:
While OCD warrants treatment by a professional, you can do some things for yourself to build on your treatment plan:
- Practice what you learn. Work with your mental health professional to identify techniques and skills that help manage symptoms, and practice these regularly.
- Take your medications as directed. Even if you're feeling well, resist any temptation to skip your medications. If you stop, OCD symptoms are likely to return.
- Pay attention to warning signs. You and your doctor may have identified issues that can trigger your OCD symptoms. Make a plan so that you know what to do if symptoms return. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
- Check first before taking other medications.
 Contact the doctor who's treating you for OCD before you take medications prescribed by another doctor or before taking any over-the-counter medications, vitamins, herbal remedies or other supplements to avoid possible interactions.
Contact the doctor who's treating you for OCD before you take medications prescribed by another doctor or before taking any over-the-counter medications, vitamins, herbal remedies or other supplements to avoid possible interactions.
Coping and support
Coping with obsessive-compulsive disorder can be challenging. Medications can have unwanted side effects, and you may feel embarrassed or angry about having a condition that requires long-term treatment. Here are some ways to help cope with OCD:
- Learn about OCD. Learning about your condition can empower you and motivate you to stick to your treatment plan.
- Stay focused on your goals. Keep your recovery goals in mind and remember that recovery from OCD is an ongoing process.

- Join a support group. Reaching out to others facing similar challenges can provide you with support and help you cope with challenges.
- Find healthy outlets. Explore healthy ways to channel your energy, such as hobbies and recreational activities. Exercise regularly, eat a healthy diet and get adequate sleep.
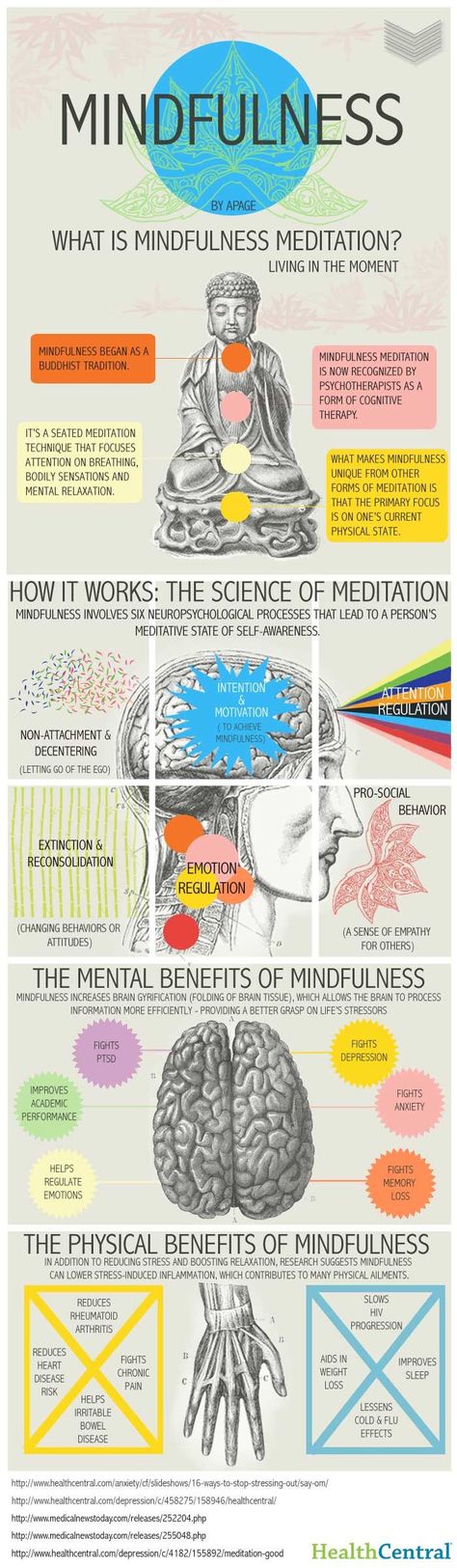
- Learn relaxation and stress management. In addition to professional treatment, stress management techniques such as meditation, visualization, muscle relaxation, massage, deep breathing, yoga or tai chi may help ease stress and anxiety.
- Stick with your regular activities. Try not to avoid meaningful activities. Go to work or school as you usually would. Spend time with family and friends. Don't let OCD get in the way of your life.
Preparing for your appointment
You may start by seeing your primary doctor. Because obsessive-compulsive disorder often requires specialized care, you may be referred to a mental health professional, such as a psychiatrist or psychologist, for evaluation and treatment.
Because obsessive-compulsive disorder often requires specialized care, you may be referred to a mental health professional, such as a psychiatrist or psychologist, for evaluation and treatment.
What you can do
To prepare for your appointment, think about your needs and goals for treatment. Make a list of:
- Any symptoms you've noticed, including the types of obsessions and compulsions youꞌve experienced and things that you may be avoiding because of your distress
- Key personal information, including any major stresses, recent life changes and family members with similar symptoms
- All medications, vitamins, herbal remedies or other supplements, as well as the dosages
- Questions to ask your doctor or therapist
Questions to ask might include:
- Do you think I have OCD?
- How do you treat OCD?
- How can treatment help me?
- Are there medications that might help?
- Will exposure and response prevention therapy help?
- How long will treatment take?
- What can I do to help myself?
- Are there any brochures or other printed material that I can have?
- Can you recommend any websites?
Don't hesitate to ask any other questions during your appointment.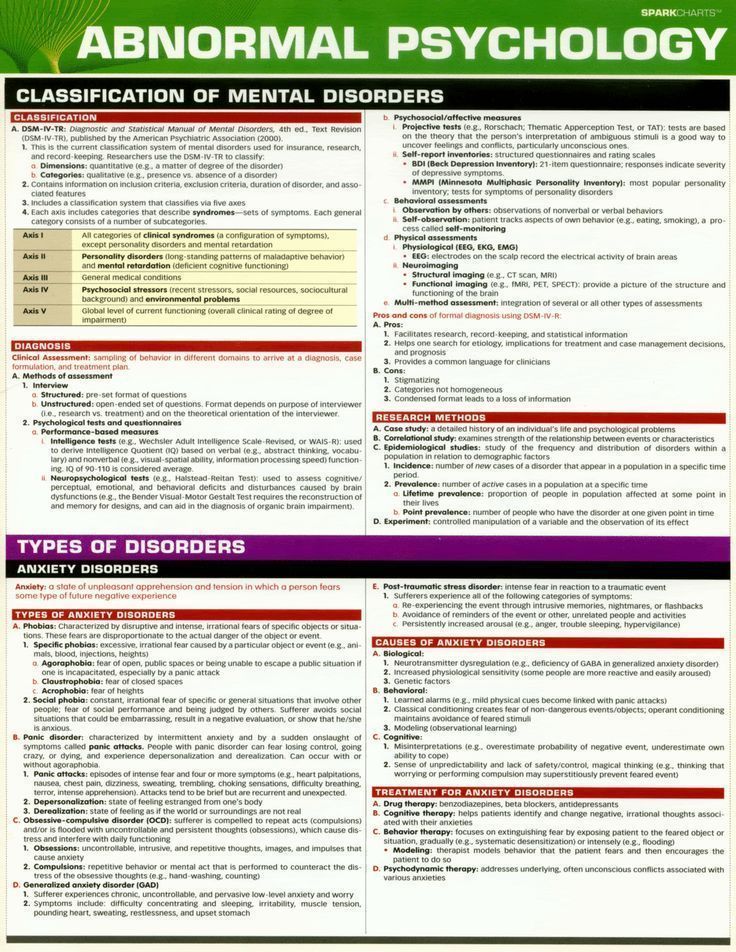
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- Do certain thoughts go through your mind over and over despite your attempts to ignore them?
- Do you have to have things arranged in a certain way?
- Do you have to wash your hands, count things or check things over and over?
- When did your symptoms start?
- Have symptoms been continuous or occasional?
- What, if anything, seems to improve the symptoms?
- What, if anything, appears to worsen the symptoms?
- How do the symptoms affect your daily life? Do you avoid anything because of your symptoms?
- In a typical day, how much time do you spend on obsessive thoughts and compulsive behavior?
- Have any of your relatives had a mental health disorder?
- Have you experienced any trauma or major stress?
Your doctor or mental health professional will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your appointment time.
Preparing and anticipating questions will help you make the most of your appointment time.
By Mayo Clinic Staff
Related
Associated Procedures
International OCD Foundation | Medications for OCD
PLEASE NOTE: The International OCD Foundation has no conflicts of interest or financial relationships related to the content of this web page.The following information refers to OCD medications in adults. For information on medication in children, click here.
Overview
- Medication is an effective treatment for OCD.
- About 7 out of 10 people with OCD will benefit from either medication or Exposure and Response Prevention (ERP). For the people who benefit from medication, they usually see their OCD symptoms reduced by 40-60%.
- For medications to work, they must be taken regularly and as directed by their doctor. About half of OCD patients stop taking their medication due to side effects or for other reasons. If you experience side effects, you should bring this up with your doctor so they can help you address them.
 They may be able to change your dose or find a different type of SRI that your system better tolerates.
They may be able to change your dose or find a different type of SRI that your system better tolerates.
What kinds of medications may help OCD?
The types of medication that research has shown to be most effective for OCD are a type of drug called a Serotonin Reuptake Inhibitor (SRI), which are traditionally used as an antidepressants, but also help to address OCD symptoms. (Note: Depression can sometimes result from OCD, and doctors can treat both the OCD and depression with the same medication.)
Do all antidepressants help OCD symptoms?
No! Some commonly used antidepressants have almost no effect whatsoever on OCD symptoms. Drugs, such as imipramine (Tofranil®) or amitriptyline (Elavil®), that are good antidepressants, rarely improve OCD symptoms.
Which Medications Help OCD?
The following antidepressants have been found to work well for OCD in research studies:
|
|
|
|
|
|
|
|
Have These Drugs Been Tested?
Anafranil has been around the longest and is the best-studied OCD medication. There is growing evidence that the other drugs are as effective. In addition to these carefully studied drugs, there are hundreds of case reports of other drugs being helpful. For example, duloxetine (Cymbalta®) has been reported to help OCD patients who have not responded to these other medications.
There is growing evidence that the other drugs are as effective. In addition to these carefully studied drugs, there are hundreds of case reports of other drugs being helpful. For example, duloxetine (Cymbalta®) has been reported to help OCD patients who have not responded to these other medications.
What Are the Usual Doses for These Drugs?
High doses are often needed for these drugs to work in most people.* Studies suggest that the following doses may be needed:
|
|
|
|
|
|
|
|
Which Drug Should Someone Try First?
Whenever any of the above drugs have been studied head to head, there seems to be no significant difference in how well they work. However, for any given patient, one drug may be very effective, and the others may not. The only way to tell which drug will be the most helpful with the least side effects is to try each drug for about 3 months. Remember! It is important not to give up after failing one or two drugs. Drugs work very differently for each person.
However, for any given patient, one drug may be very effective, and the others may not. The only way to tell which drug will be the most helpful with the least side effects is to try each drug for about 3 months. Remember! It is important not to give up after failing one or two drugs. Drugs work very differently for each person.
How Do These Medications Work?
It remains unclear as to how these particular drugs help OCD. The good news is that after decades of research, we know how to treat patients, even though we do not know exactly why our treatments work.
We do know that each of these medications affect a chemical in the brain called serotonin. Serotonin is used by the brain as a messenger. If your brain does not have enough serotonin, then your the nerves in your brain might not be communicating right. Adding these medications to your body can help boost your serotonin and get your brain back on track.
Are There Side Effects?- Yes.
 Most patients will experience one or more side effects from all of the medications listed above.
Most patients will experience one or more side effects from all of the medications listed above. - The patient and doctor must weigh the benefits of the drug against the side effects.
- It is important for the patient to be open about problems that may be caused by the medication. Sometimes an adjustment in dose or a switch in the time of day it is taken is all that is needed.
Who Should Not Take These Medications?
- Women who are pregnant or are breastfeeding should weigh the decision to take these drugs with their doctor. If severe OCD cannot be controlled any other way, research has indicated that these medications seem to be safe. Many pregnant women have taken them without difficulty. Some OCD patients choose to use exposure and response prevention (ERP) to minimize medication use during the first or last trimester of pregnancy. Click here to read more about the benefits and risks of using SRIs during pregancy and/or while breastfeeding.
- Very elderly patients should avoid Anafranil as the first drug tried, since it has side effects that can interfere with thinking and can cause or worsen confusion.
- Patients with heart problems should use special caution if taking Anafranil.
What if I cannot take even the smallest pill size of the medication?
Some patients are sensitive to these medications and can’t stand the effects that come with even the lowest dose. However, patients can start at very low doses (for example, 1-2 mg per day) and very slowly increase the dose. For most people, they will eventually be able to handle the medication at its normal dose.
Ask your doctor if you can try a lower dose by breaking pills in half or using a liquid form of medication to slowly increase your doses.
ALWAYS be sure to talk to your doctor before making any changes to the way you take your medications!
The following is one example as told by Dr. Michael Jenike:
“One woman, who was started on Prozac 20 mg/day, complained of bothersome side effects such as increased anxiety, shakiness, and terrible insomnia. She felt it made her OCD worse.
She had horrible side effects from even 12.5 mg of Anafranil, and later with low dosages of Paxil and Zoloft. She requested to start 1-2 mg/day of liquid Prozac, because she heard it was good from other patients that she met from a computer bulletin board. She felt no side effects, and over a period of a few weeks, she got up to 20 mg/day without the previous side effects that she had felt on this dose in the past. Under the supervision of her doctor, she continued to increase the Prozac to 60 mg/day over a couple more months. Her OCD gradually improved quite dramatically.”
Should I Take These Medications Only When I Am Feeling Stressed?
No. This is a common mistake. These medications are meant to be taken every day to keep your serotonin at a constant level. They are not taken like typical anti-anxiety meds, when you feel upset or anxious. It is best not to miss doses if possible. However, if you do miss a dose here or there, it is unlikely that any bad effect on OCD will occur.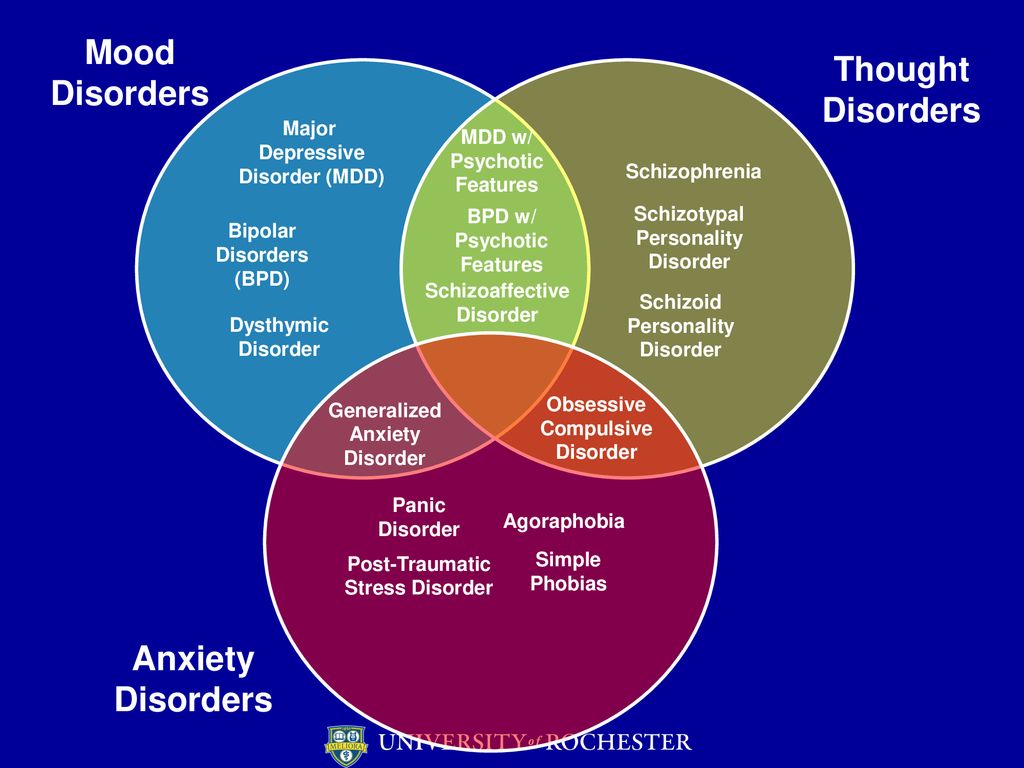 In fact, sometimes your doctor might tell you to skip doses to help manage troublesome side effects, like sexual problems.
In fact, sometimes your doctor might tell you to skip doses to help manage troublesome side effects, like sexual problems.
What Kind of Doctor Should I Look For to Prescribe These Medications?
Although any licensed physician can legally prescribe these drugs, it is probably best to deal directly with a board-certified psychiatrist who understands OCD. It is important to find a psychiatrist who has special knowledge about the use of drugs to treat mental health disorders. Click here to find a psychiatrist in your area. (Look for therapists with an MD or DO after their name.)
What If I am Afraid to Take My Medication Because I Have an Obsessional Fear About Drugs?
Usually with help from a doctor that you trust, your fears can be overcome. If you have fears about taking medication, ERP can be started first and part of the therapy can focus on these fears of medications.
How Long Does it Take for These Medications to Work?
It is important not to give up on a medication until you have been taking it as prescribed for 10 to 12 weeks.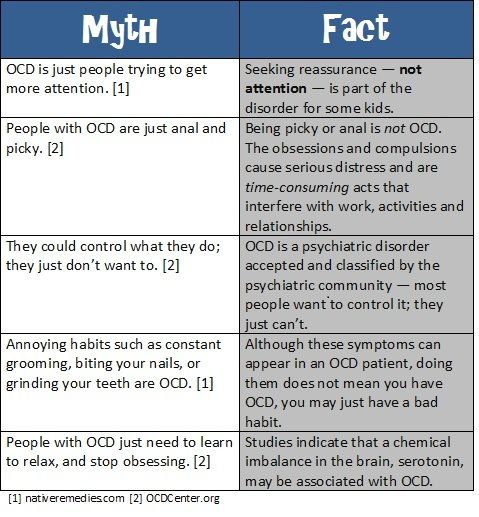 Many patients feel no positive effects for the first few weeks of treatment but then improve greatly.
Many patients feel no positive effects for the first few weeks of treatment but then improve greatly.
Will I Have to Take Medications Forever?
No one knows how long patients should take these medications once they have been effective. Some patients are able to stop their medications after a 6 to 12-month treatment period. It does appear that over half of OCD patients (and maybe many more) will need to be on at least a low dose of medication for years, perhaps even for life. It seems likely that the risk of relapse is lower if patients learn to use behavior therapy techniques while they are doing well on medications. And if medication is tapered slowly (even over several months), the ERP treatment may enable patients to control any symptoms that return when they stop taking the medication.
After medications are stopped, symptoms do not return immediately; they may start to return within a few weeks to a few months. If OCD symptoms return after a medication is stopped, most patients will have a good response if the medication is restarted.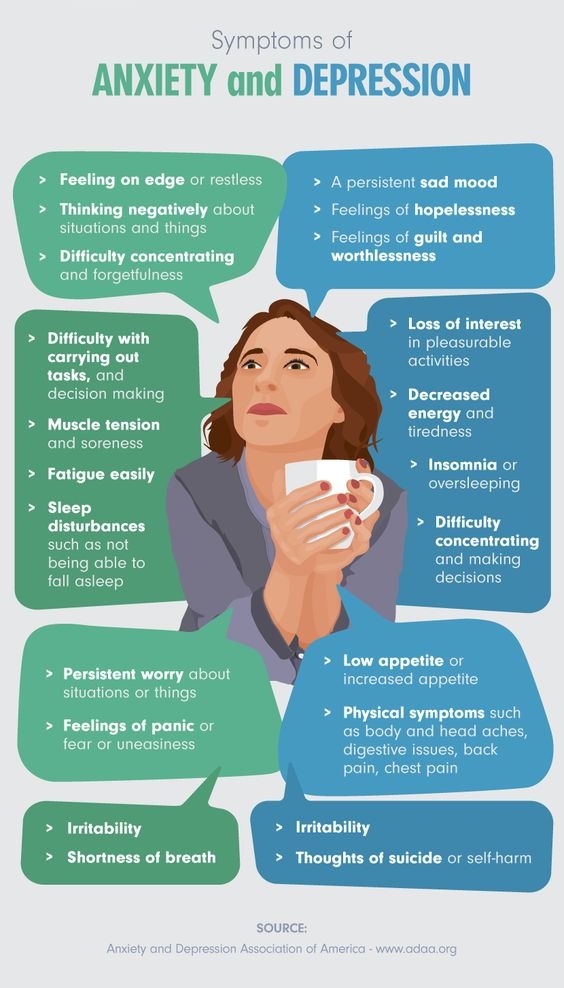
Can I Drink Alcohol While on These Medications?
Many patients drink alcohol while on these medications and handle it well, but be sure to ask your doctor or pharmacist if it is safe. It is important to keep in mind that alcohol may have a greater effect on individuals who are taking these medications; one drink could affect an individual as if it were two drinks. Also, alcohol may limit some of the medications’ benefits, so it may be wise to try not to drink alcohol during the first couple of months after starting any new medication.
Do I Need Other Treatments Too?
Most psychiatrists and therapists believe that combining a type of Cognitive Behavior Therapy (CBT), specifically Exposure and Response Prevention (ERP), and medication is the most effective approach.
What if I Can’t Afford My Medication?
Drug companies give doctors free samples of some medications. Doctors give these samples to patients who cannot afford the cost of the medications.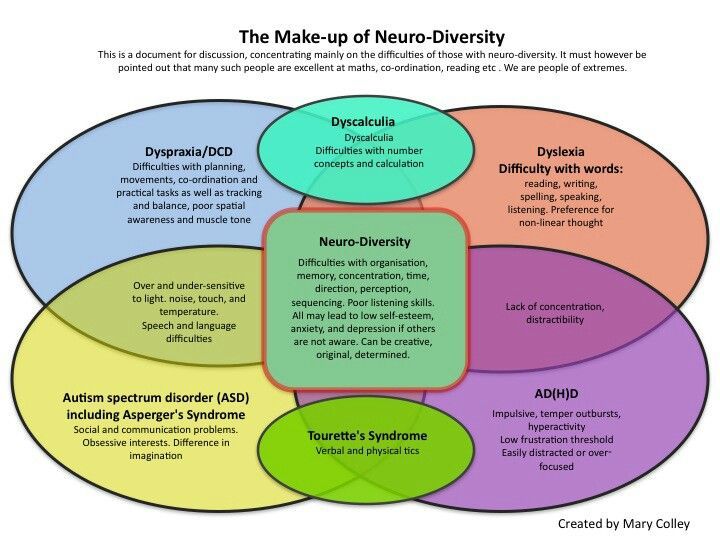
Most drug companies also have programs that help patients get these and other medications free or at a reduced cost. For more information, visit: www.pparx.org or call 1-888-477-2669.
By Michael Jenike, MD
Chair, International OCD Foundation’s Scientific Advisory Board
Harvard Medical School
* The FDA has issued some warnings on the use of this medication in higher doses. Please check with your physician.
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.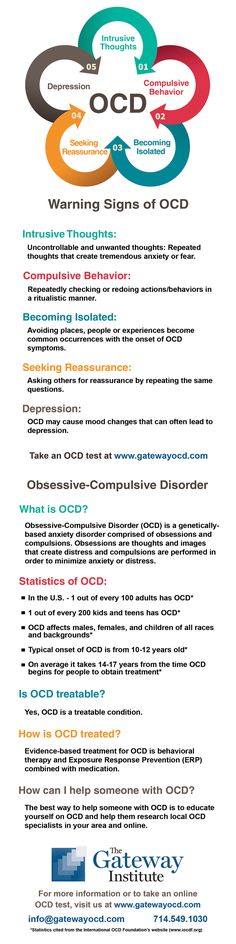
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
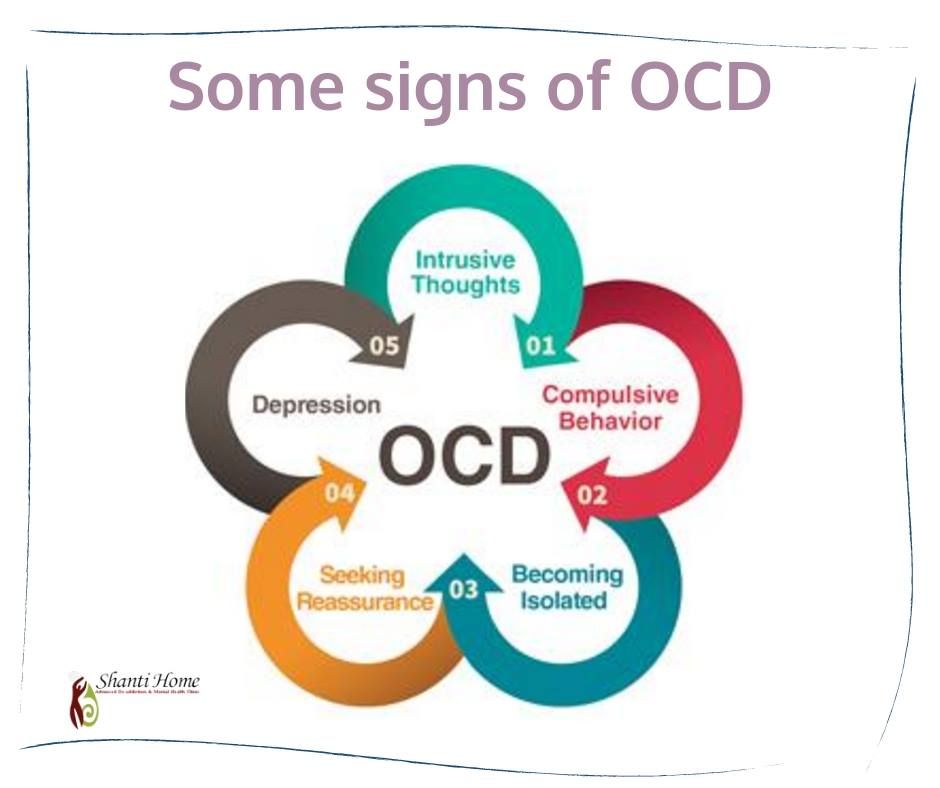
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive Compulsive Disorder - Mayo Clinic
Intrusive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.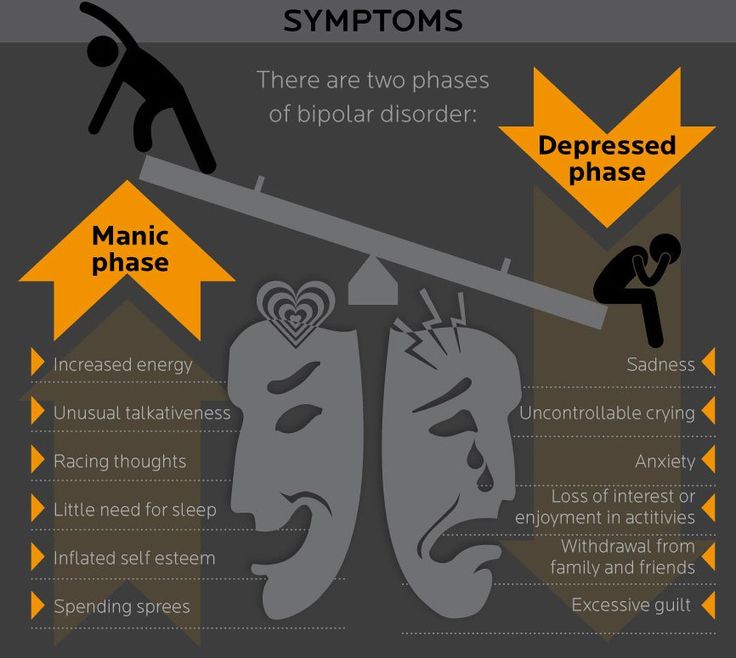
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person's condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasurable. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number.
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive behavioral therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On psychotherapeutic care"
Psychiatrists, psychotherapists and psychologists are involved in the treatment of OCD in Russia. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a neuropsychiatric dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalizationMy condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
This is how a referral for hospitalization to a day hospital looks like The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body.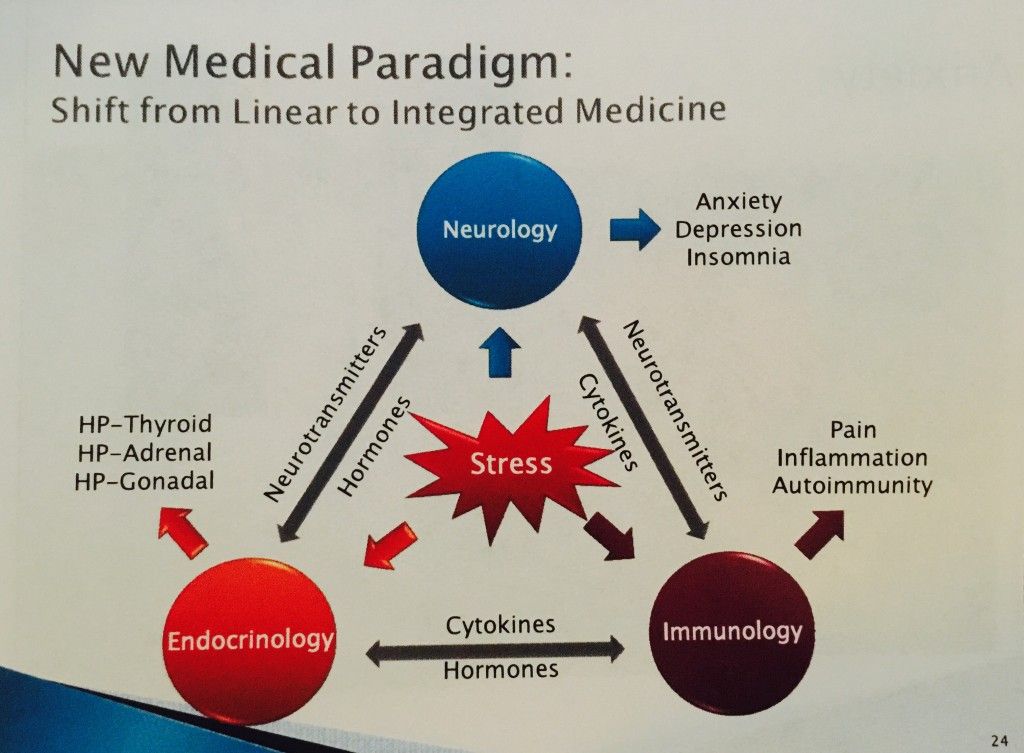 It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.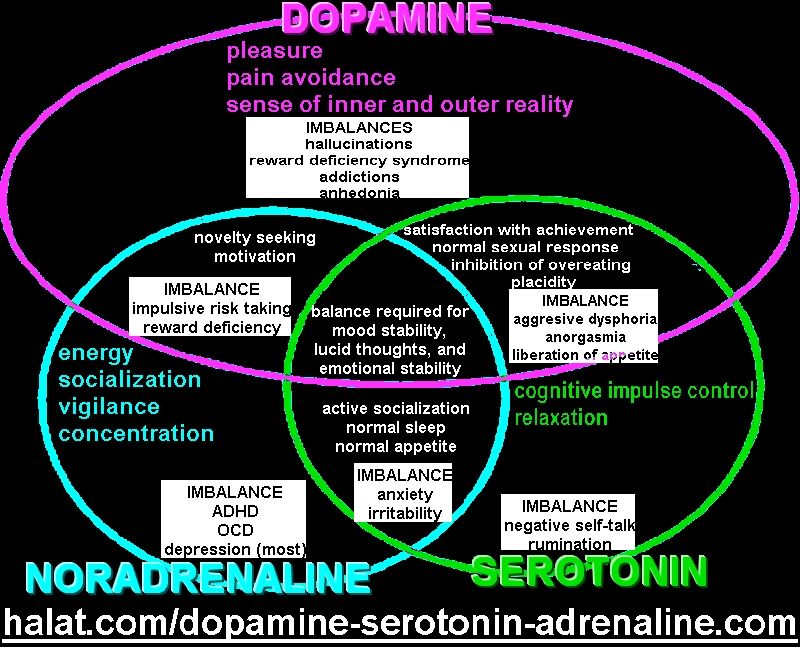
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I started taking medication, my mood would rise and my anxiety would go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.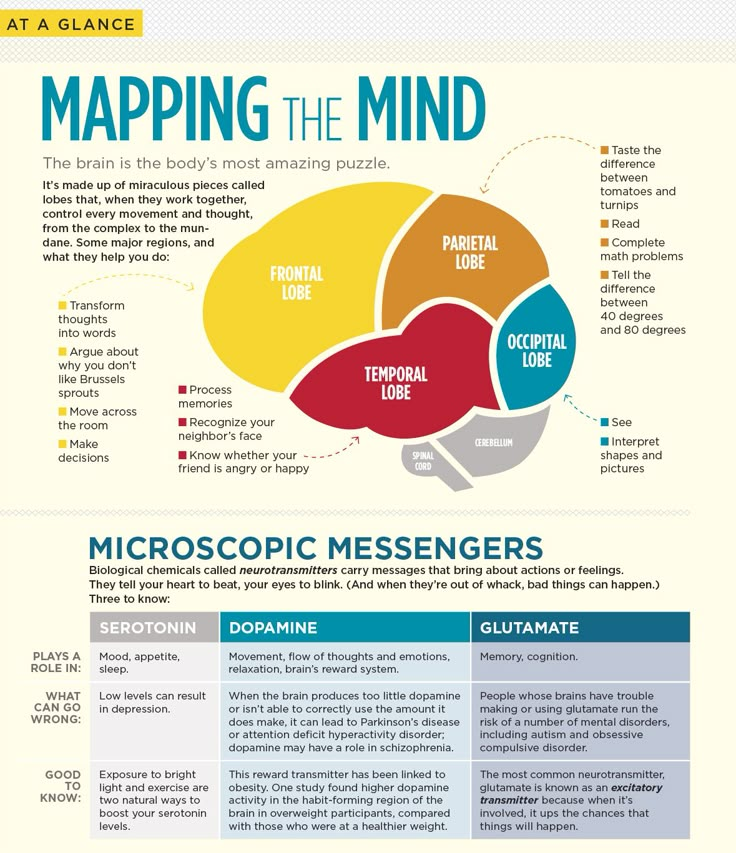
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope. They noticed the changes, but my young man did not let me stop the treatment
They noticed the changes, but my young man did not let me stop the treatment Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.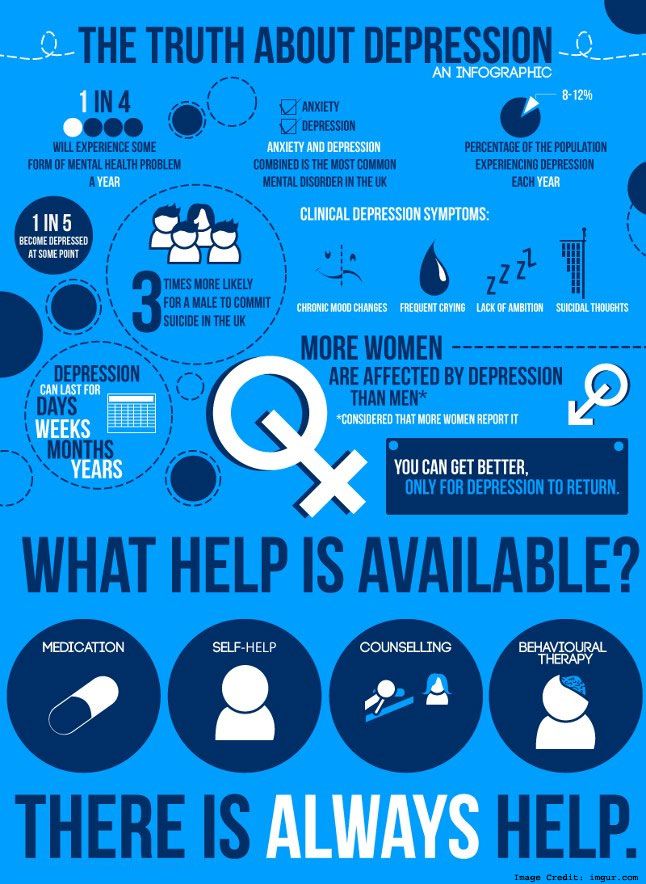
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 419 p
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refusedTreatment
Second hospitalization and psychotherapy After six months of outpatient treatment, the district psychiatrist recommended to be treated again in the hospital.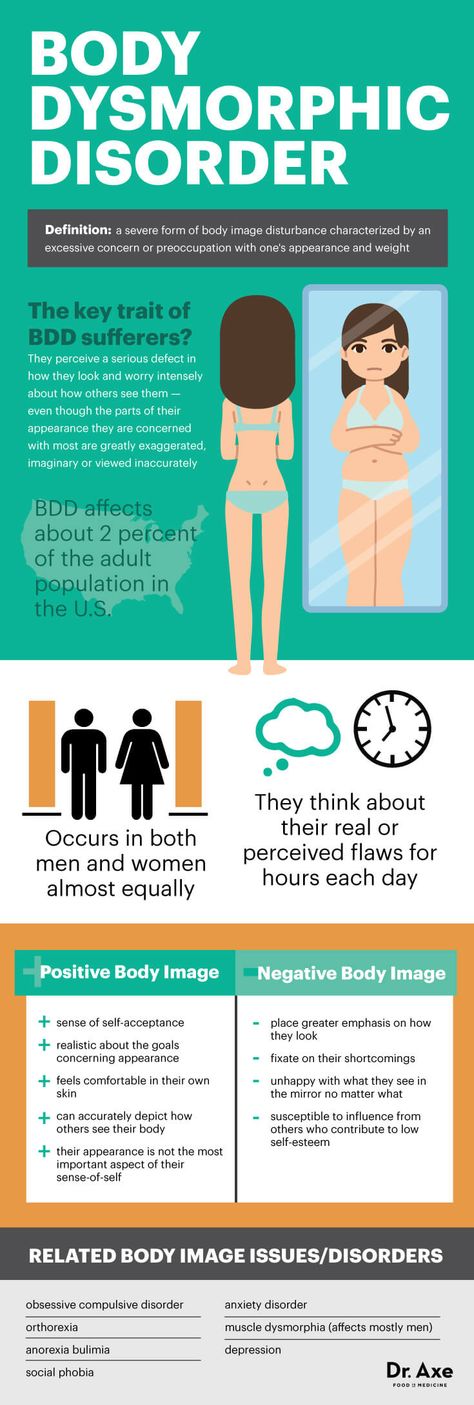 Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment.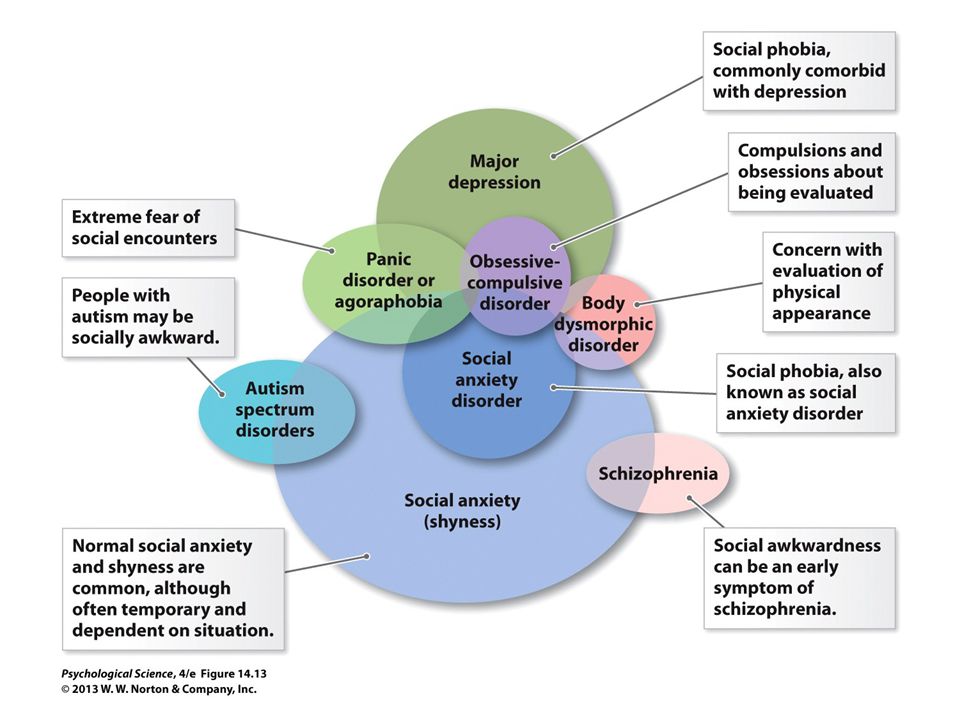 Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts.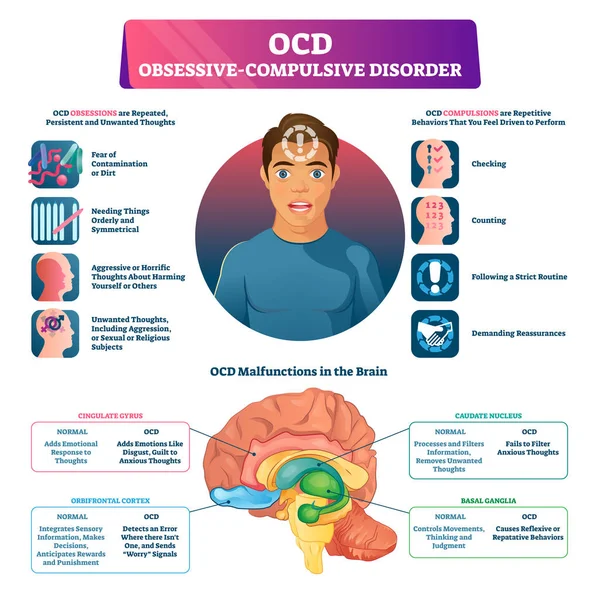 When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 R |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me.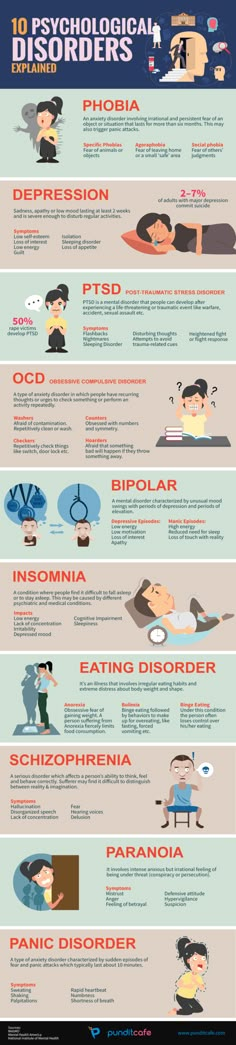 The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
- A visit to a neuropsychiatric dispensary will not prevent people with OCD from moving freely, driving a car, using weapons, or getting a job.
- Patients with OCD can receive care free of charge in state neuropsychiatric dispensaries or at their own expense in private clinics.
Did you also have an illness that affected your lifestyle or attitude? Share your story.
Tell
Psychiatrist on how to choose a treatment for depression
Since the time of the French philosopher René Descartes, scientists have been puzzled by the "problem of mind and body", especially in relation to mental illness. Depression, obsessive-compulsive disorder, and other conditions can be treated with both the body (antidepressants) and the mind (psychotherapy).
 So which way is more efficient? Psychiatrist David Burns addresses this issue in his book Mood Therapy - T&P publishes an excerpt.
So which way is more efficient? Psychiatrist David Burns addresses this issue in his book Mood Therapy - T&P publishes an excerpt.
Mood Therapy: Clinically Proven to Beat Depression Without Pills
David Burns
Alpina Publisher. 2019
Our mind is made up of thoughts and feelings, invisible and ephemeral. We know they exist because we experience them, but we don't know why or how they exist. Our body, on the other hand, is material: it is made up of blood, bones, muscles, fat, etc. Matter is made up of molecules, molecules are made up of atoms. This building material is inert. Presumably, atoms are not conscious. So how can the inert stuff in our brain give rise to a conscious mind that can see, feel, hear, love, and hate?
According to Descartes, our mind and body are connected in some way. Descartes called the region of the brain that connects these two of our essences, "the seat of the soul." For several centuries, philosophers have tried to determine where this "receptacle of the soul" is located. Now neuroscientists continue this search, trying to figure out how the brain creates emotions and conscious thoughts.
Now neuroscientists continue this search, trying to figure out how the brain creates emotions and conscious thoughts.
The belief that our mind is separate from our body is also reflected in how we approach depression treatment.
There are biological therapies that deal exclusively with the "body" and psychological ones that work with the "mind". Biological therapies usually involve medication, while psychological treatments typically involve talking therapy.
There is strong competition between the drug therapy and talk therapy camps. On average, psychiatrists are more likely to stick to the drug camp. This is due to the fact that they are trained primarily in medicine (they must receive a doctorate in medicine). They can prescribe medications and tend to follow the medical model of diagnosis and treatment.
If you go to see a psychiatrist when you are depressed, they will most likely tell you that your depression is caused by a chemical imbalance in your brain and recommend antidepressants.
If your family doctor treats you for depression, medication is also more likely. This is due to the fact that many family doctors lack knowledge in the field of psychotherapy, as well as the time to discuss life problems with patients.
Conversely, psychologists, clinical social workers, and other counselors in various fields rather belong to the talk therapy camp.
They have no medical training and cannot prescribe drugs*. Their training usually focuses primarily on the psychological and social factors that can cause depression. If you suffer from depression and see a therapist at a talk therapy camp, you will most likely be asked about the process of growing up and worldview, or about stressful experiences, such as losing a loved one or being fired. You may also be recommended psychotherapy, such as cognitive behavioral therapy. Be that as it may, there are many exceptions to this rule. Many non-medical therapists agree that biological factors do play a role in depression, and many psychiatrists are gifted psychotherapists. Psychiatrists and non-medical therapists sometimes work together to ensure that the patient gets the most benefit from both treatments.
Psychiatrists and non-medical therapists sometimes work together to ensure that the patient gets the most benefit from both treatments.
 — Approx. ed.
— Approx. ed. However, the division between the mind (psychological) and body (biological) schools is quite clear, and the dialogue between them is often tense, belligerent, and bitter. Political and financial considerations influence the tone of these discussions, sometimes even more than scientific discoveries. A number of recent studies suggest that there is too much hype about nothing in these disputes, and such a categorical distinction between mind and brain may be illusory. These studies indicate that antidepressants and psychotherapy can have equal effects on the mind and brain. In other words, they can have a similar effect.
For example, a classic study published in the Archives of General Psychiatry in 1992 by Drs. Lewis Baxter, Jeffrey Schwartz, Kenneth Bergman and their colleagues at the UCLA School of Medicine described changes in brain chemistry in 18 patients suffering from obsessive-compulsive disorder (OCD). Half of these patients received cognitive behavioral therapy and did not take medication. And the other half took antidepressants and did not undergo psychotherapy. Patients from the drug-free group underwent two-component individual and group psychotherapy. Its first component was exposure and reaction prevention. This is a behavioral therapy technique that helps patients resist the compulsive desire to check locks, wash their hands constantly, etc. And the second component was cognitive therapy using the techniques described in this book. Remember that the patients in this group did not receive any medication.
Positron emission tomography (PET) scan was used in this study to measure metabolic sugar (glucose) levels in various areas of the brain before treatment and ten weeks later. This method allows you to evaluate the activity of nerve endings in different areas of the brain. One area of the brain of particular interest is the so-called caudate nucleus in the right hemisphere.
Both treatments were effective, with the majority of patients in both groups improving and there were no significant differences in outcomes. This was not much of a surprise: previous studies had also shown that medications and cognitive behavioral therapy had a similar effect in treating OCD. However, the results of the PET study were unexpected. Scientists reported comparable levels of decreased activity in the right caudate nucleus in successfully treated patients, regardless of whether they were treated with drugs in the absence of psychotherapy or underwent psychotherapy and did not receive drugs. In addition, the symptoms and thought patterns of both groups improved about the same, that is, both types of treatment were equally effective. Finally, the degree of improvement in symptoms correlated significantly with the level of changes in the right caudate nucleus. In other words, the patients with the most marked improvement had, on average, the greatest decrease in nerve activity in the right caudate nucleus. A reduced level of activity meant that neural activity in that area of the brain calmed down, regardless of whether the patient was receiving drug treatment or undergoing psychotherapy.
One of the implications of this study is that excessive activity in the right caudate nucleus may influence the development or persistence of symptoms of obsessive-compulsive disorder. Another important implication is that
antidepressants and cognitive behavioral therapy may be equally effective in restoring brain structure and function.
Like most published studies, the above has several fairly significant shortcomings. One problem is that any observable changes in the brain that appear in a particular psychiatric disorder may be an effect rather than a cause. In other words, an increase in neural activity in the right caudate nucleus in patients with obsessive-compulsive disorder may simply reflect a larger picture of disorders in the brain and not be the cause of its symptoms. […]
Other studies have shown that antidepressants can help depressed patients change negative thought patterns. Indeed, in a study conducted at the Washington University School of Medicine in St. Louis by Drs. Ann Simons, Saul Garfield, and George Murphy, depressed patients were randomly assigned to either antidepressant medication alone or cognitive therapy alone. During the experiment, changes in negative thinking patterns in both groups of patients were studied. The researchers found that negative thinking in patients who responded positively to antidepressant therapy experienced the same improvement as in depressed patients who responded positively to cognitive therapy. Remember that patients who were treated with drugs did not receive psychotherapy, and cognitive therapy patients did not receive drugs. Thus, this study showed that drug treatment alters negative thinking in the same way that cognitive therapy does. The effects of antidepressants on beliefs and thoughts may explain the beneficial effects of the drugs as much or better than biological interpretations of their effects on various transmitter systems in the brain.
These landmark studies suggest that,
, it may be better to put aside such a sharp separation of mind and body and consider how different treatments can have the most beneficial effect on both the mind and brain systems.
![]()
This combined approach can lead to closer collaboration between therapists and researchers looking at the problem from different angles, and to faster progress in the study of emotional disorders.
Even if some cases of depression have a specific genetic or biological disorder, psychotherapy can help to correct these problems even without the use of drugs. Many studies, as well as my own clinical experience, have confirmed that severely depressed patients, whose condition appears to be very biologically based and accompanied by many physical symptoms, often show rapid improvement in response to drug-free cognitive therapy.
The reverse may also be true. I have worked many times with depressed patients who did not feel any progress after my numerous psychotherapeutic interventions. When I put them on antidepressants, it was a turning point for many, and psychotherapy also began to bring more results. It seemed that the medication actually helped them change their negative thought patterns as they recovered from their depression. […]
Suppose scientists discover that almost all forms of depression are due, at least in part, to genetic factors. Would this mean that depression should be treated exclusively with medication? The answer is: not necessarily. For example, a fear of blood is considered to be at least partially hereditary, but it can almost always be quickly cured with behavioral therapy. The most effective treatment for most phobias is to place the person in a frightening situation and force them to face it and experience the anxiety in a controlled manner until the fear subsides and disappears completely. Most patients are so intimidated by this method that they initially resist treatment. But if they can be persuaded to stay a little longer, the success rate is extremely high.
I experienced it first hand. As a child, I was horrified at the sight of blood. When, during our studies at the medical faculty, we had to take a blood test from each other from a vein, I was so reluctant to do this that I dropped out of school. The following year, I decided to take a job in the clinical laboratory at Stanford University Hospital specifically to try to overcome my fear. My job was only to take blood samples from a vein all day long. The first few times I experienced severe anxiety, but then I gradually got used to it. Soon I began to adore my new job. This shows that drug-free behavioral therapy can at least attenuate some genetic tendencies. […]
The converse is also true. If it were found that depression is solely due to environmental factors, and that genetics does not have any influence on it, this would not reduce the potential value of antidepressants. For example, if you happen to be near a person with a sore throat, you can also easily catch a sore throat, because the streptococcus bacteria that cause it are extremely contagious. It can be said that your sore throat is completely caused by the environment, not genetics. However, you will be treating her with an antibiotic, not behavioral therapy. […]
From a practical point of view, the question I face as a clinical psychologist is: what is the best treatment for each individual patient who suffers from depression, regardless of the cause of the disease? Whether genes play a decisive role or not, drugs can sometimes help, and sometimes psychotherapy is better. Sometimes the best treatment is just a combination of psychotherapy and antidepressants. […]
My own clinical experience has convinced me that "tube" treatment with drugs alone does not give the desired result in most patients. Apparently, effective psychological intervention does play a role,
even if you are lucky and have responded positively to taking antidepressants. If you learn the self-help techniques offered by cognitive therapy, such as those described in this book, I believe you will be better prepared for any future mood problems. […]
I have also experienced that certain negative beliefs and irrational thoughts can interfere with effective medication or psychotherapy. Next, I would like to debunk [a few] harmful myths. The first eight relate to drug treatment, and the last four relate to psychotherapy. When it comes to drugs, I think it's highly desirable to be careful about taking any drug, but an overly conservative approach based on dubious half-truths can also be devastating. I also believe that a moderately skeptical and cautious view should be taken with regard to psychotherapy, but excessive pessimism can also interfere with effective treatment.
“Taking this medicine will stop me from being me. I will behave and feel strange.”
One can hardly be more mistaken. […] In fact, many patients report feeling more like themselves after starting antidepressants. […]
"These drugs are extremely dangerous."
False. If you are under medical supervision and cooperate with your doctor, you will have no reason to worry when taking most antidepressants. Adverse reactions are rare and can usually be managed safely and effectively if you and your doctor work together. Antidepressants are much safer than depression itself. […]
"But the side effects will be unbearable."
No, with the right dosage, the side effects are usually mild and barely noticeable. And if, despite this, the medication brings you discomfort, you can usually change the drug to a drug that is just as effective, but with fewer side effects. […]
"I won't take a drug prescribed by a psychiatrist because that would mean I'm crazy."
This needs some clarity. Antidepressants are prescribed for depression, not insanity. If your doctor recommends that you take an antidepressant, it will indicate that you have a mood problem. This does not mean that the doctor thinks you are crazy. However, true madness is to refuse to take antidepressants because of such fear, because this can only bring you suffering and misery. Paradoxically, with the help of medication, you can feel more normal much faster. […]
“But other people will definitely look at me with contempt if I start taking antidepressants. They will consider me inferior."
This fear is unrealistic. Other people will never know if you are taking an antidepressant or not unless you tell them yourself. There are no other options. If you do tell someone, they will be more relieved. If a person cares about your condition, they may, on the contrary, begin to respect you more, because you are making an effort to cope with a painful mood disorder. […]
“It's embarrassing to take pills. I have to deal with depression myself."
Studies of mood disorders in various countries have clearly shown that many people can recover without medication if they actively follow a structured self-help program like the one described in this book. However, it is also true that psychotherapy does not work for everyone and that some depressed patients recover faster with antidepressants. In addition, in many cases, an antidepressant, as mentioned above, can make your task easier. […]
"I am so depressed and so stuck in it that only medication can help me. "
Both medication and psychotherapy can be very helpful in treating severe depression. I believe that both a passive attitude and an excessive hope that the medicine will do all the work for you are unreasonable. My own research has shown that
the desire to do something to help yourself already has a strong effect on the treatment of depression, whether you are on medication or not.
Patients who complete self-help tasks between sessions also seem to recover faster. So if you combine the drug with an appropriate form of psychotherapy, you will have more working tools in your arsenal. […]
“It is embarrassing to seek psychotherapeutic help, because it would mean that I am weak and neurotic. It is more acceptable to be treated with medication, because it means that my illness is of a medical nature, like diabetes.”
In fact, many depressed patients who are treated with both drugs and psychotherapy experience a sense of shame. […] Imagine, for example, that you have just discovered that a close friend has been treated for depression with psychotherapy and has benefited from the treatment. Ask yourself what you would say to this friend. Does “Oh, psychotherapy just show what a weakling and failed neurotic you are. You should have taken the drugs. What you did is just a disgrace"? And if you didn’t say this to a friend, why say the same to yourself? […]
"My problems are real, so psychotherapy probably won't help."
Cognitive therapy actually works best for people suffering from depression caused by real problems in life, including catastrophic medical problems such as end-stage cancer or limb amputation, bankruptcy, or severe relationship problems. […]
"My problems are hopeless, so neither psychotherapy nor drugs will help."
This is what your depression says, but the reality is completely different. Hopelessness is a common but terrifying symptom of depression that is caused by distorted thinking, just like other symptoms.