Borderline personality versus bipolar
Borderline Personality Disorder vs. Bipolar Disorder
Written by Mary Jo DiLonardo
In this Article
- Bipolar Disorder
- Borderline Personality Disorder
Borderline personality and bipolar: These two disorders are often confused. They both have symptoms of impulsiveness and mood swings. But they are different disorders and have different treatments.
Bipolar Disorder
Also known as manic depression, bipolar disorder causes swings in mood, energy, and the ability to function throughout the day.
Symptoms: Bipolar disorder is defined by alternating periods of depression and mania that can last from days to months. Unlike borderline personality disorder, the mood swings of bipolar disorder are not triggered by interpersonal conflicts, last for days to weeks or months rather than minutes to hours, and episodes are, by definition, accompanied by changes in sleep, energy, speech, and thinking
During times of mania, symptoms might include:
- An excessively happy or angry, irritated mood
- More physical and mental energy and activity than normal
- Racing thoughts and ideas
- Talking more and faster
- Making big plans
- Risk taking
- Impulsiveness (substance abuse, sex, spending, etc.
)
- Less sleep, but no feeling of being tired
- Poor judgement
During periods of depression, symptoms might include:
- Drop in energy
- Lasting sadness
- Less activity and energy
- Restlessness and irritability
- Problems concentrating and making decisions
- Worry and anxiety
- No interest in favorite activities
- Feelings of guilt and hopelessness; suicidal thoughts
- Change in appetite or sleep patterns
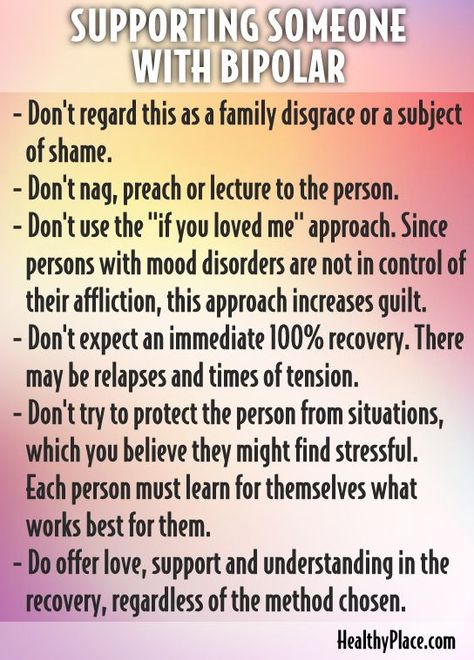
Treatment: Most people with bipolar disorder need lifelong treatment to keep their condition managed. This usually includes medicine -- usually mood stabilizers, and sometimes also antipsychotics or antidepressants. Therapy can also help people with bipolar disorder understand it and develop skills to handle it.
Borderline Personality Disorder
Borderline personality disorder involves a longstanding pattern of abrupt, moment-to-moment swings -- in moods, relationships, self-image, and behavior (in contrast to distinct episodes of mania or depression in people with bipolar disorder) that are usually triggered by conflicts in interactions with other people. People with borderline personality disorder can experience overly strong emotional responses to upsetting life events and often try to hurt themselves. They often have chaotic relationships with people.
People with borderline personality disorder can experience overly strong emotional responses to upsetting life events and often try to hurt themselves. They often have chaotic relationships with people.
People with borderline personality disorder are more likely to have other mental health problems, too. They are also more likely to have had some type of trauma as a child than people with bipolar disorder, although trauma in itself does not cause borderline personality disorder. They often also can have problems with addictions, eating disorders, body image, and anxiety.
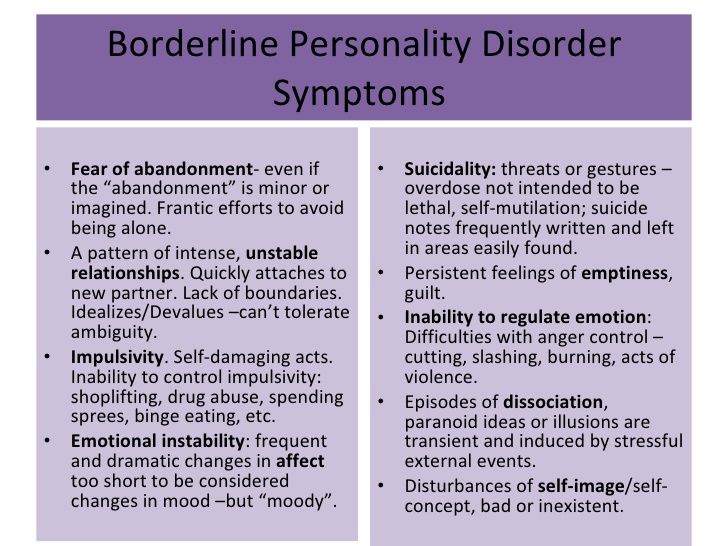
Symptoms: A person with borderline personality disorder has trouble controlling their thoughts and managing their feelings, and often has impulsive and reckless behavior. Here are the condition's main symptoms:
- Frantic efforts to avoid feeling abandoned
- History of unstable, intense relationships
- Tendency to view people and situations as either "all good" or "all bad"
- Poor self-image
- Impulsiveness (spending, sex, substance abuse, etc.
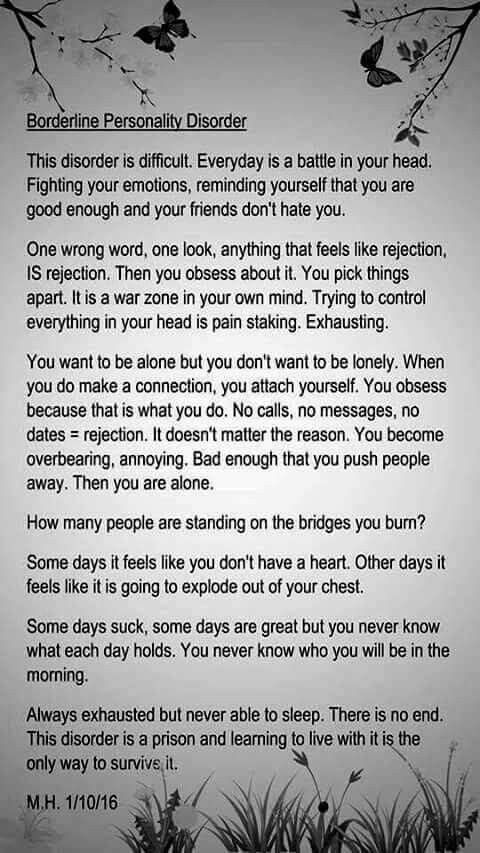 )
) - Self-harm (e.g., cutting) or suicidal behavior
- Mood swings involving anger and depression, usually in response to stressful events or relationships
- Feelings of emptiness
- Problems managing anger and unpleasant emotions
- Paranoia
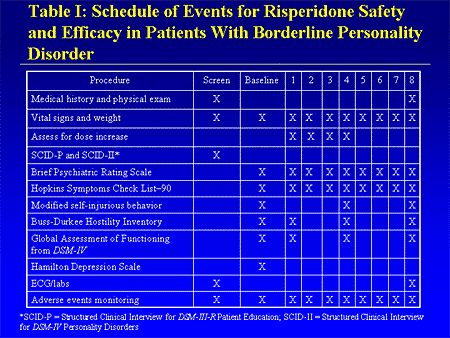
Treatment: Long-term treatment is usually necessary for people with borderline personality disorder. Treatment mainly involves specific forms of psychotherapy, such as dialectical behavior therapy (DBT) or transference-focused psychotherapy (TFP) aimed at helping people manage impulses (such as suicidal urges or tendencies to self-harm when they feel upset), feelings of distress or anger, and emotional oversensitivity to interactions with other people. Medications are also sometimes used to help with these symptoms, although they are not always effective and not considered to be the main focus of treatment in borderline personality disorder. Sometimes, short hospital stays are also needed to manage times of crisis that involve threats to safety and well-being.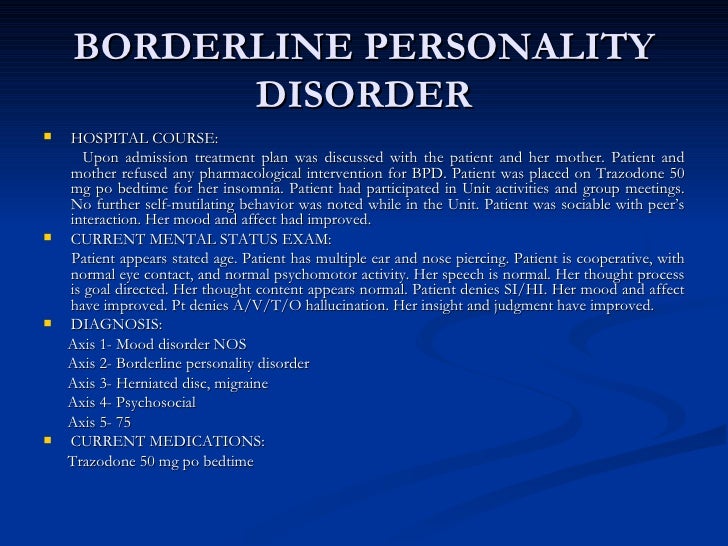
The difference between bipolar and borderline personality disorder
Learn the differences between these two disorders, how to spot the signs of each, and how to treat them.
What is bipolar disorder vs. borderline personality disorder? Both diagnoses have been in the headlines, but many may wonder: what’s the difference?
Changing moods can often be a natural response to stressful situations. But for some, mood shifts are so extreme that they could be a sign of these more serious conditions, both of which are characterized in part by major mood swings, according to Frank Yeomans, M.D., Ph.D., director of training at the NewYork-Presbyterian Borderline Personality Disorder Resource Center, an internationally recognized center for the study of personality disorders.
“This partial similarity in mood shifts, going from an extremely high mood to a very low mood, causes many people, including some clinicians, to confuse the two disorders,” says Dr. Yeomans, who is also a clinical associate professor of psychiatry at Weill Cornell Medicine Department of Psychiatry and an adjunct associate professor of psychiatry at the Columbia University Vagelos College of Physicians and Surgeons Center for Psychoanalytic Training and Research. “Yet they are two distinct and serious diagnoses with different symptoms that require different methods of treatment.”
Yeomans, who is also a clinical associate professor of psychiatry at Weill Cornell Medicine Department of Psychiatry and an adjunct associate professor of psychiatry at the Columbia University Vagelos College of Physicians and Surgeons Center for Psychoanalytic Training and Research. “Yet they are two distinct and serious diagnoses with different symptoms that require different methods of treatment.”
Mental health has moved more into the spotlight since the onset of the pandemic, with COVID-19 triggering a 25% increase in the prevalence of depression and anxiety worldwide, according to the World Health Organization. As for bipolar disorder and borderline personality disorder, these illnesses affect millions of Americans. Bipolar disorder is estimated to affect somewhere between 1 and 2.8% of U.S. adults, and studies show the prevalence of borderline personality disorder to range from 1.4 to 5.9% of the American adult population.
How do you know if you or someone you love suffers from one of these disorders? And how can you tell the difference? Health Matters spoke with Dr. Yeomans to define these disorders and explain the telltale signs and how to treat them.
Yeomans to define these disorders and explain the telltale signs and how to treat them.
What does borderline personality disorder look like?
Dr. Yeomans: Those with the disorder have extremely intense emotions that can shift rapidly from a negative, depressed state to an elated one, but with a predominance of negative feeling states. In this psychiatric illness, the extreme and intense mood swings often are precipitated by reactions to events (“trigger events”) that are disproportionate to the event and that someone else might take in stride. The illness is also characterized by rejection-sensitivity, chaotic relationships, and an overall difficulty in managing emotions.
For example, if a boyfriend or girlfriend does not return your call, instead of being annoyed and moving on, the combination of dejection and anger in a person with borderline personality disorder could possibly lead the person to cut their own wrists. Such destructive actions, usually of an impulsive nature, are a way of putting intense feelings, like rejection and anger, that you can’t tolerate, into action in an attempt to discharge the emotion rather than to continue to feel its intensity. The behavioral manifestations of intense emotions, in addition to self-cutting, include substance abuse, eating disorders, and sexual promiscuity — dramatic ways of behaving that stem from not being able to manage emotions.
The behavioral manifestations of intense emotions, in addition to self-cutting, include substance abuse, eating disorders, and sexual promiscuity — dramatic ways of behaving that stem from not being able to manage emotions.
In discussing disorders that involve changes in mood, it is important to make clear that not all depressed states indicate a psychiatric condition. If your spouse walks out on you or you lose a parent, it’s normal to feel depressed. In such cases, the depression may be an ongoing, terribly low, dejected mood but is appropriate to the circumstances. The borderline person demonstrates more reactivity to relatively minor events and demonstrates contradictory emotions that erupt over a short time.
How does borderline personality disorder affect relationships?
People with borderline personality disorder have relationships that can be chaotic and intense, veering between a desperate neediness for others to an intense anger or dismissal of others when feeling rejected, even in situations where the other person may in fact be neutral or even positive.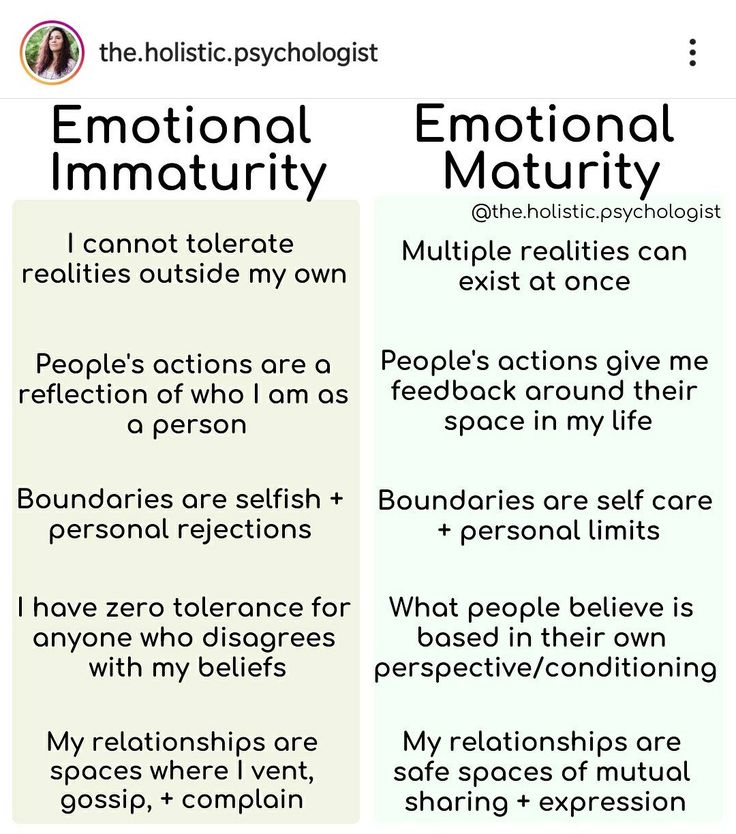 Individuals with borderline personality disorder have difficulty accurately reading people’s emotions and trusting others. There is a difficulty with how the individual perceives others. Once, when a borderline patient told me a sad story that brought tears to my eyes, he became very angry because he was convinced that my tears, rather than an expression of empathy, were my way of mocking.
Individuals with borderline personality disorder have difficulty accurately reading people’s emotions and trusting others. There is a difficulty with how the individual perceives others. Once, when a borderline patient told me a sad story that brought tears to my eyes, he became very angry because he was convinced that my tears, rather than an expression of empathy, were my way of mocking.
Where does the behavior stem from?
It comes from a combination of an emotionally charged temperament and the lack of a solid sense of self. Without a clear and coherent identity, the individual depends on what’s happening around them to determine what they feel and what they do.
What is the cause of this disorder?
There is no single cause of borderline personality disorder, though studies suggest that certain traits, especially a temperament characterized by intense emotional reactions, stem to a large degree from genetics.
Developmental factors, including problems with emotional attunement between a developing child and caregivers, seem to play a role, as do physical or sexual abuse, or emotional neglect.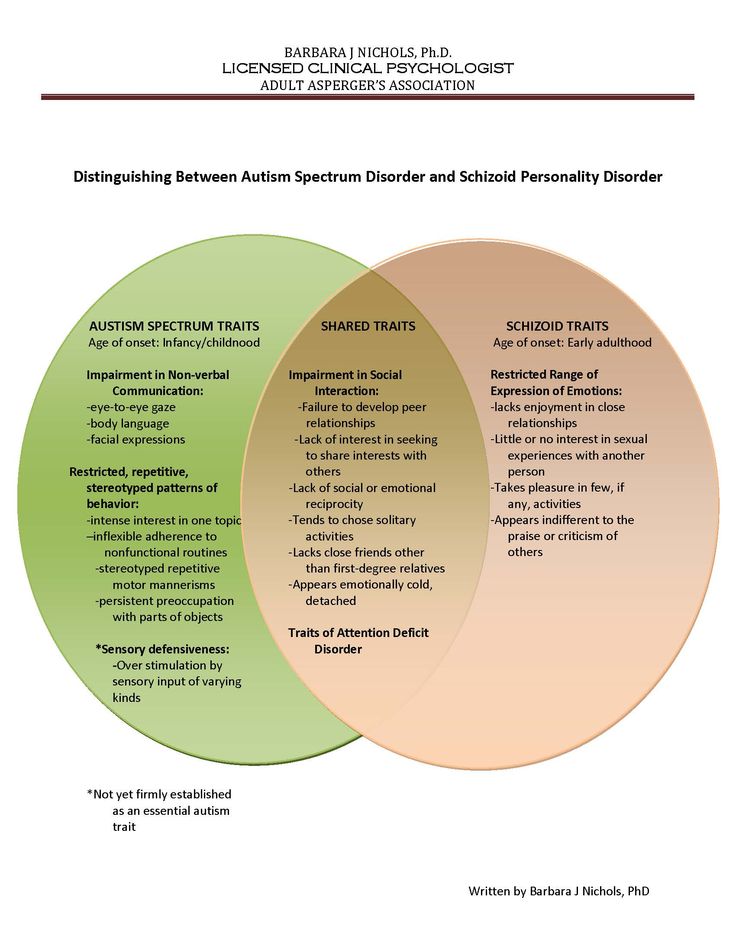 However, it’s important to note that in cases with a history of trauma, the disorder seems to stem from a combination of temperament and trauma rather than trauma alone, since many people who have experienced trauma early in life do not go on to develop serious psychiatric illnesses.
However, it’s important to note that in cases with a history of trauma, the disorder seems to stem from a combination of temperament and trauma rather than trauma alone, since many people who have experienced trauma early in life do not go on to develop serious psychiatric illnesses.
How is borderline personality disorder treated?
There is no medication that successfully treats the condition, although they may help reduce some specific symptoms, such as intense anxiety. Evidence-based models of psychotherapy are the treatment of choice. Dialectical behavioral therapy operates from the assumption that those with borderline personality disorder lack skills necessary to tolerate intense emotions or thoughts.
Transference-focused psychotherapy emphasizes the observation and interpretation of patient behavior in the relationship with the therapist to help identify unrecognized or distorted internal emotional states that are activated in relations with others and then to integrate them into a more coherent sense of self that includes emotional balance.
Mentalization-based therapy similarly helps individuals recognize their mental states and be aware of them in their relations with others.
Good psychiatric management is based on a case management model that combines a focus on the environment of the patient, psychoeducation, supportive therapy, and possibly family therapy.
What is bipolar disorder?
Like borderline personality disorder, sufferers experience extreme shifts in mood but between depressed states and episodes of mania, the bipolar patient may experience periods of stable mood.
For example, someone with bipolar disorder in a depressed state could be totally dejected, hopeless, and morbid, with no will to live. If they are in a manic state, they might be up all night writing page after page of a novel or playing music, with a sense that they have passed into a special state of genius. They might speak at a rapidly accelerated pace, with actions that are out of sync with appropriate social behavior — like disrobing and dancing in a park without awareness that it’s inappropriate. A full-blown manic episode shows a period of energy that could go on for days without any relief and would exhaust anybody else. In between the depressed and manic states, they may have periods of stable mood. In another variant of the disorder, some bipolar patients experience repeated depressive states without full-blown manic states; this is referred to as bipolar 2.
A full-blown manic episode shows a period of energy that could go on for days without any relief and would exhaust anybody else. In between the depressed and manic states, they may have periods of stable mood. In another variant of the disorder, some bipolar patients experience repeated depressive states without full-blown manic states; this is referred to as bipolar 2.
What is the cause of bipolar disorder?
Bipolar disorder is rooted in brain chemistry, structure and functioning, as well as genetics and family history.
How is bipolar disorder treated?
Bipolar disorder can be treated with medication, most often with lithium, which helps stabilize mood. More recently, other mood stabilizers have been developed that doctors might prescribe largely on a trial-and-error basis, depending on side effects for individual patients. Psychotherapy is usually helpful as well to aid the person in managing complications in his life that stem from the episodes of illness, and to monitor adherence to the medication regimen.
What are the key differences between the disorders?
When a person with bipolar disorder is not in a manic or depressive episode, they demonstrate stability that the borderline personality does not show. If a bipolar person is between episodes, they can function pretty well in the world. They can have in-depth relationships that might be disturbed by their periods of illness, but when they are not experiencing episodes, they have a stability that you do not see in the borderline person.
Bipolar disorder is more rooted in the biology of the nervous system and more responsive to medication. Borderline pathology strongly involves the psychological level of the mind – the way meaning is generated – in addition to the biology of the brain and nervous system. A more biological condition like bipolar lacks these deeply rooted psychological aspects, or ways of seeing the world and perceiving the self and others, that characterizes borderline disorders.
Mood swings of bipolar disorder are more random and less related to events than those of borderline. Those with bipolar might have a hair-trigger kind of response during an episode, whereas the borderline person has a hair-trigger response all of the time.
Those with bipolar might have a hair-trigger kind of response during an episode, whereas the borderline person has a hair-trigger response all of the time.
What is important for people to know?
Each is a serious illness, and those suffering need to seek out the proper treatment. Both illnesses can be successfully treated. Too often, individuals with borderline personality disorder are treated for depression or bipolar, when it is a more complex problem. It is essential for patients with borderline personality disorder to see a specialist. A lot of general therapists do not do a good job with this patient population: It’s like sending somebody who needs cardiac surgery to a general surgeon.
We recognize that finding the right specialist for this disorder is a problem people all across the country and the world have. To address this, we established a unique and valuable resource, the NewYork-Presbyterian Borderline Personality Disorder Resource Center. The Resource Center is a website and call center devoted to education about the disorder and to referring people to the proper specialists.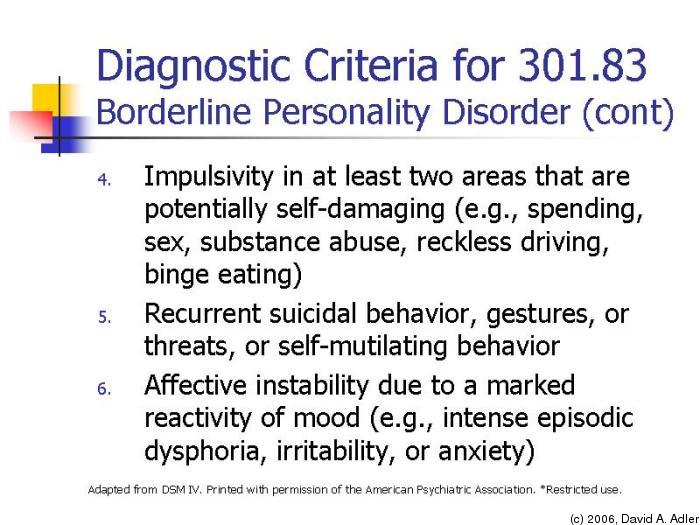 We’ve had calls from literally all over the world and have connected people with help all the way from Australia to Russia and every place in between. In addition to the website, the center has an office at the NewYork-Presbyterian Westchester Behavioral Health Center campus staffed by a senior social worker.
We’ve had calls from literally all over the world and have connected people with help all the way from Australia to Russia and every place in between. In addition to the website, the center has an office at the NewYork-Presbyterian Westchester Behavioral Health Center campus staffed by a senior social worker.
Learn more about psychiatry and mental health services at NewYork-Presbyterian.
At A Glance
Featured Expert
-
Psychiatry and Behavioral Health Services
Consult an Expert
Find a Doctor or call
877-697-9355
Share This Story
Read More: Mental Health, anxiety, bipolar disorder, borderline personality disorder, Borderline Personality Disorder Resource Center, depressed, Frank Yeomans, personality, psychiatrist, psychiatry, therapy
Bipolar personality disorder - manic depressive psychosis: signs, causes, treatment , creative ideas.
 This feeling is incomparable! I'm happy! What is wrong with me? Where does this cyclicality come from? - this is how a typical patient suffering from bipolar disorder describes his condition. What is it?
This feeling is incomparable! I'm happy! What is wrong with me? Where does this cyclicality come from? - this is how a typical patient suffering from bipolar disorder describes his condition. What is it? Bipolar affective disorder or bipolar personality disorder, in other words, manic-depressive psychosis is a pronounced form of mental disorder, which is characterized by a change of pole, manifested in sharp and frequent mood swings: from unearthly euphoria to complete decline, depression and even aggression. In psychiatry, such swings (disorders) are defined by the term "affective disorders", which range from manic euphoria (hypomania) to depressive decline. In individual cases, the patient may manifest only mania or only depression for a fairly long period of time, as well as mixed, borderline states, called borderline disorder in clinical psychology.
Bipolar disorder. Early name
The disease in question was first described by psychiatrists from France, whose names were Falre and Bayarzhe in 1854, but the official recognition of this pathology as an independent nosological element in psychiatry happened only in 1896.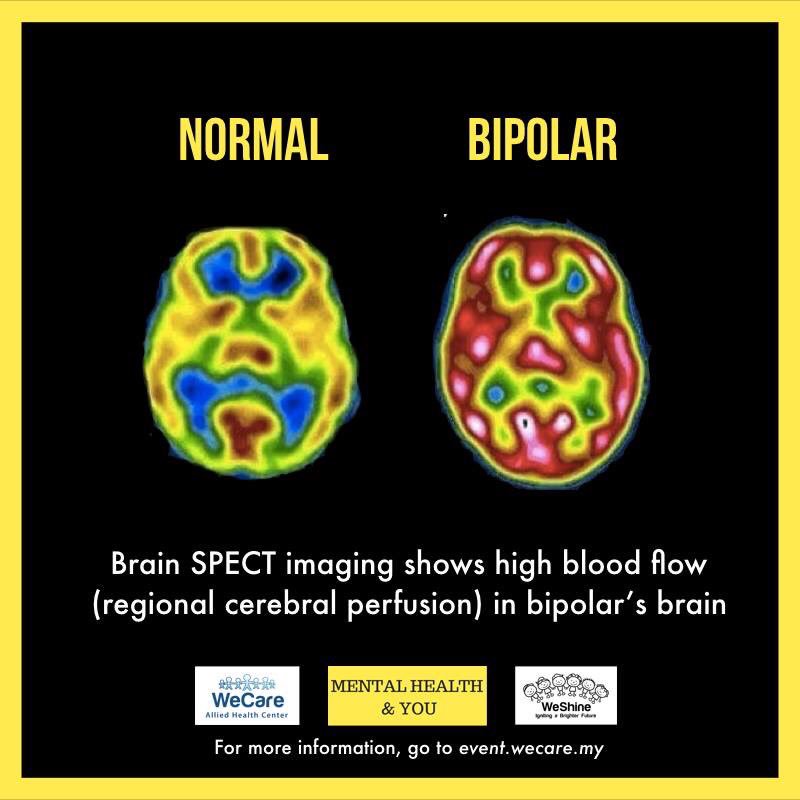 Initially, bipolar disorder was classified as manic-depressive psychosis (MDP), but in the international ICD-10 classification it is called bipolar affective disorder. The name change was made due to the fact that, in accordance with the key symptoms of the disease itself, psychosis may not always be observed. Today, in clinical psychology and psychiatry, there is also the concept of manic depressive disorder (MDD), the signs of which at certain points differ from the characteristics of bipolar disorder. This will be discussed below.
Initially, bipolar disorder was classified as manic-depressive psychosis (MDP), but in the international ICD-10 classification it is called bipolar affective disorder. The name change was made due to the fact that, in accordance with the key symptoms of the disease itself, psychosis may not always be observed. Today, in clinical psychology and psychiatry, there is also the concept of manic depressive disorder (MDD), the signs of which at certain points differ from the characteristics of bipolar disorder. This will be discussed below.
What is meant by bipolar disorder now?
What is BAD like?
Bipolar disorder in classical psychiatry is divided into three forms:
- Unipolar . It differs in that the manic phase is smoothed out, and therefore the diagnosis is complicated. Often the patient is diagnosed simply with depression, as it is quite difficult to catch a manic episode. These include states of mania (hypomania) and depressive psychosis, which occur periodically.

- The bipolar form includes both phases in its anamnesis, and therefore can be called manic-depressive.
- Intermission . In this variant, light intervals between phases can last up to several years or be absent altogether.
Clinical forms of bipolar disorder
In general, any typification of bipolar disorder is based on the predominance of either depressive or manic episodes in the pathogenesis. As noted above, the disease can be bipolar (characterized by two types of affective destruction) or unipolar (there is one affective disorder) forms. The bipolar form is usually considered in more detail, as it includes subforms.
- Cyclically intermittent - a consistent and rather structured alternation of the phases of mania and depression, delimited by a light interval.
- Non-cyclic intermittent - Chaotic alternation of phase change. Usually, in such patients, phases of the same type follow each other.
 For example, several phases of depression pass, followed by a lucid interval, and then episodes of mania reappear.
For example, several phases of depression pass, followed by a lucid interval, and then episodes of mania reappear. - Double - two episodes of affect succeed each other, during which there is no light gap.
- Circular form of bipolar disorder is characterized by a permanent change of polar phases with a complete absence of a light period. The total number of main phases in this disorder is determined by the individual psychological characteristics of the patient. Someone may have multiple affective episodes during their life, while someone has only one. Each of the polar episodes, on average, can be observed for several months. Moreover, according to statistics, a manic episode is less common than a depressive one, and its duration is usually much shorter. In some people, the disease proceeds with the presence of mixed episodes, characterized by an intense change of ups and downs.
Nosova Polina Sergeevna
Leading psychiatrist
- OWN more and those around them with mood swings, they ask themselves: where did this disease come from, what served as the prerequisites for its appearance? What triggers episodes of mania and depression in the body.
 The general answer is: genetics, biochemical platform and stress factor. It is important to note that the factors that trigger the disorder itself and the factors that influence the degree and contour of its development differ from each other.
The general answer is: genetics, biochemical platform and stress factor. It is important to note that the factors that trigger the disorder itself and the factors that influence the degree and contour of its development differ from each other. Genetic predisposition determines the possibility of developing the disease, but the realization of this possibility is mainly associated with the presence of stress. Any traumatic life situation, be it divorce or violence, loss, can serve as a trigger that provokes intensive development.
How does bipolar disorder start?
In most cases, the onset of the disorder reveals itself as a depressive episode, much less often as a manic episode. The starting manic episode is more common in men. It is worth paying close attention to the first episode, since the subsequent ratio of the phase change often depends on it. If the beginning is depressive, then in the future most episodes will be similar. It is also worth considering the age of the patient: the earlier a depressive episode occurred in a person’s life, the more likely it is that in the future he will be pursued by manic-depressive phases.

Causes and prerequisites for the development of bipolar disorder.
The specific reasons for the development of this type of disorder have not been established, however, scientists refer to endogenous (external, environmental) and internal (genetic) prerequisites, however, as in many other psychopathy. In other words, heredity significantly increases the risk of transmitting the disease to the next generations, and the conditions and quality of life can affect the speed and intensity of the manifestation of the disease. The model of raising a child with a genetic predisposition also has a great influence. If his emotions are taken into account by his parents, EQ (emotional intelligence) is taken into account, then with other data, the possibility of the onset of the disease is significantly reduced.
Thus, conditionally possible causes of bipolar affective disorder can be combined into 5 groups:
- Genetic predisposition .
- Social .
 Environmental factors, quality and standard of human life.
Environmental factors, quality and standard of human life. - Psychological . Presence or absence of comorbidities. General stress resistance of the individual.
- Stress factor . The presence of traumatic events that affect the onset of the disease or relapse.
- Hormonal disorders, mechanical injuries, metabolic disorders of chemical and other substances in the body .
Risk groups
As with many other psychopathic disorders, the risk of development is determined by certain types of personality.
- Schizoid personality type. Schizoids are prone to solitude, social phobia, the same type of activity, lack of empathy. The mentality is rational.
- Statothymic personality type. This type needs absolute structuring of everything that surrounds him; on a personal level, he is characterized by the highest levels of responsibility and scrupulousness.
- Melancholic personality type. Melancholic people get tired quickly, are very restrained in expressing feelings and emotions, but deeply experience everything inside. These people are quite suspicious and anxious, which provokes the development of neuroses in most cases.
It is worth noting that women are more susceptible to this disorder than men, for uncertain reasons.
Signs of bipolar disorder
Bipolar disorder, like any other psychopathic disorder, involves several stages: from mild to severe in the case of a manic episode, and from simple to anesthetic in a depressive variant. Each stage has its own set of symptoms.
Nevertheless, psychiatrists identify a number of early signs, the recognition of which will help to determine not only the impending disorder itself, but also its phase.
So, signs of mania that should not be ignored.
- Sleep disorders characterized by reduced hours of rest.
- Rapid speech with thought jumps.
- Impulsivity .
- Deconcentration of attention , expressed in frequent and chaotic change of activity.
- Mania of grandiosity
- Risky behavior and adrenaline cravings
For the stage of bipolar depression, in principle, the same components are characteristic, only with a minus sign.
- Periods of causeless sadness and fear last from several hours or longer.
- Severe social phobia appears, contacts with friends and relatives are difficult.
- Loss of interest in past hobbies.
- Change in appetite and taste preferences.
- Asthenia, chronic fatigue syndrome.
General symptoms of bipolar disorder also depend on the phase of the disease and its stage.
A manic episode includes three stages:
- Mild , another name is hypomania .
 Excellent mood, personal and social uplift, increased patient's ability to work and level of sociability are characteristic. A person becomes talkative, excitable, but at the same time distracted. The level of libido rises. It is worth noting that often the patient may manifest not euphoria, but dysphoria, which means causeless irritability and aggressiveness towards others, although other signs of hypomania remain the same.
Excellent mood, personal and social uplift, increased patient's ability to work and level of sociability are characteristic. A person becomes talkative, excitable, but at the same time distracted. The level of libido rises. It is worth noting that often the patient may manifest not euphoria, but dysphoria, which means causeless irritability and aggressiveness towards others, although other signs of hypomania remain the same. - Moderate (mania without psychotic manifestations). Mental and physical activity increase, insomnia and deconcentration of attention appear, which is why efficiency is lost, megalomania manifests itself.
- Severe mania or depressive psychosis . At this stage, psychotic symptoms appear, including psychomotor agitation, a tendency to violence, and hysteria. It becomes increasingly difficult for the patient to make logical connections, hallucinosis and delusions may develop, including "delusions of high origin" (the patients think that their relatives had a noble pedigree) or "delusions of grandeur" (that they themselves are very famous).
 Sometimes not only labor, but also social skills are lost.
Sometimes not only labor, but also social skills are lost.
A depressive episode is conventionally divided into 5 possible forms:
- A simple form with a history of the “depressive triad” (asthenia, intellectual retardation and lack of intensity of life).
- Hypochondriacal . The patient is tormented by a feeling of fear regarding the presence of a terrible, unknown and incurable disease.
- Delusional - the depressive triad is supplemented by delusions of accusation. The patient begins to blame himself for everything.
- Agitated includes all of the above symptoms, except for motor passivity.
- Anesthetic – there is a feeling of disappearance of all possible sensations, instead of which there is only emptiness.
The alternation of the above states is also referred to as manic-depressive or circular psychosis, which is essentially the same thing. In the event that polar conditions are present simultaneously, then the patient is diagnosed with a "mixed mood", which indicates the presence of a bipolar disorder.
In the event that polar conditions are present simultaneously, then the patient is diagnosed with a "mixed mood", which indicates the presence of a bipolar disorder.
Treatment of bipolar disorder.
Unfortunately, it will not be possible to stabilize the described disorder only by the psychotherapeutic method, however, much depends on the phase. In the most severe phase, characterized by an absolute psychotic affective state, psychotherapy, as such, is essentially powerless, and the patient needs competent drug treatment, including antipsychotics and antidepressants, with the help of which a specialist performs drug alignment. The main task at this stage is the removal of the acute phase, and then it is already possible to proceed to psychotherapy aimed at determining the underlying cause of the current state. At a deep psychopathic level, in the vast majority of cases, the patient is driven by the desire to get what he cannot achieve in a normal state: to fulfill a dream, to release his demons, to succumb to instincts.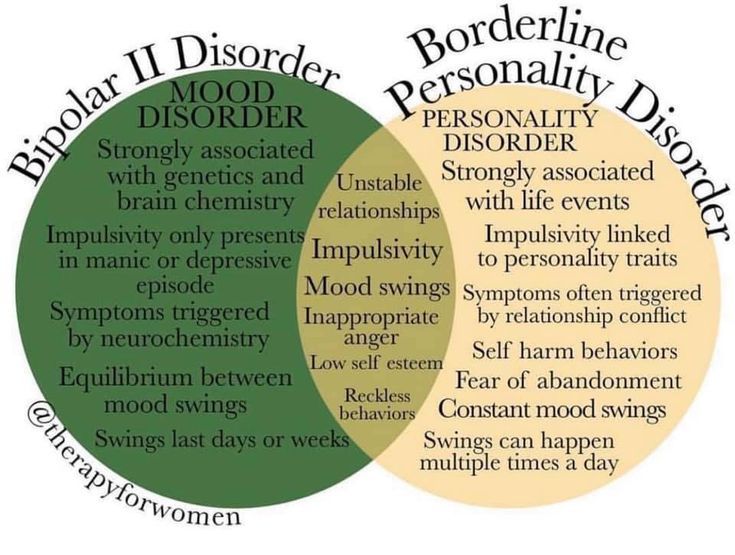 The depressive period, on the contrary, immerses a person in himself and makes it possible, finally, to get to know himself. In the light interval, the patient cannot do either, because he is not ready to get acquainted with his feelings and remember what is unpleasant. He chooses avoidance due to permanent impulse suppression. The main task of psychotherapy is to help a person adapt his desires in a socially acceptable way, not plunging into a state of manic-depressive psychosis, but due to the development of emotional intelligence. In clinical psychology, this method is called actualization.
The depressive period, on the contrary, immerses a person in himself and makes it possible, finally, to get to know himself. In the light interval, the patient cannot do either, because he is not ready to get acquainted with his feelings and remember what is unpleasant. He chooses avoidance due to permanent impulse suppression. The main task of psychotherapy is to help a person adapt his desires in a socially acceptable way, not plunging into a state of manic-depressive psychosis, but due to the development of emotional intelligence. In clinical psychology, this method is called actualization.
Manic-depressive psychosis (MDP) and bipolar affective disorder (BAD)
As noted above, manic-depressive psychosis (MDP) or syndrome is essentially a terminological synonym for bipolar disorder. The subtle point associated with the renaming of the diagnosis lies rather in the plane of ethical standards. In itself, the definition of "psychosis" does not have the best effect on the patient's perception of his condition, as well as on the attitude of others around him.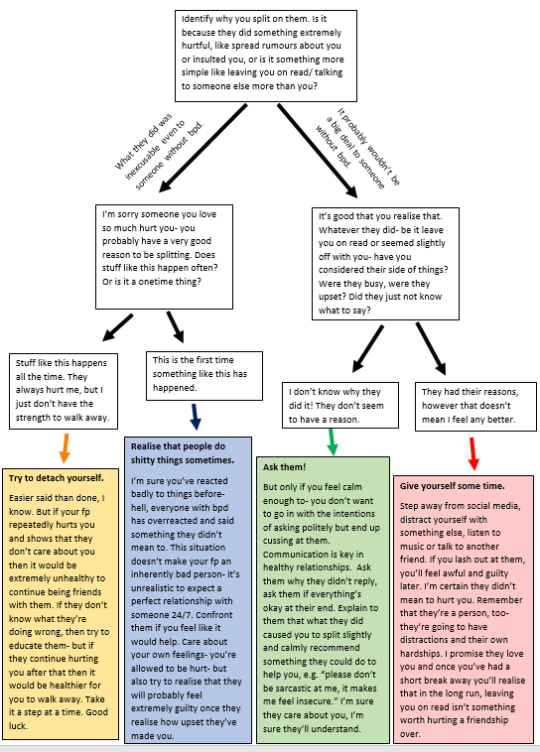 Moreover, in BAD, psychopathic destructions are not always observed in the same way as acute attacks of mania or depression.
Moreover, in BAD, psychopathic destructions are not always observed in the same way as acute attacks of mania or depression.
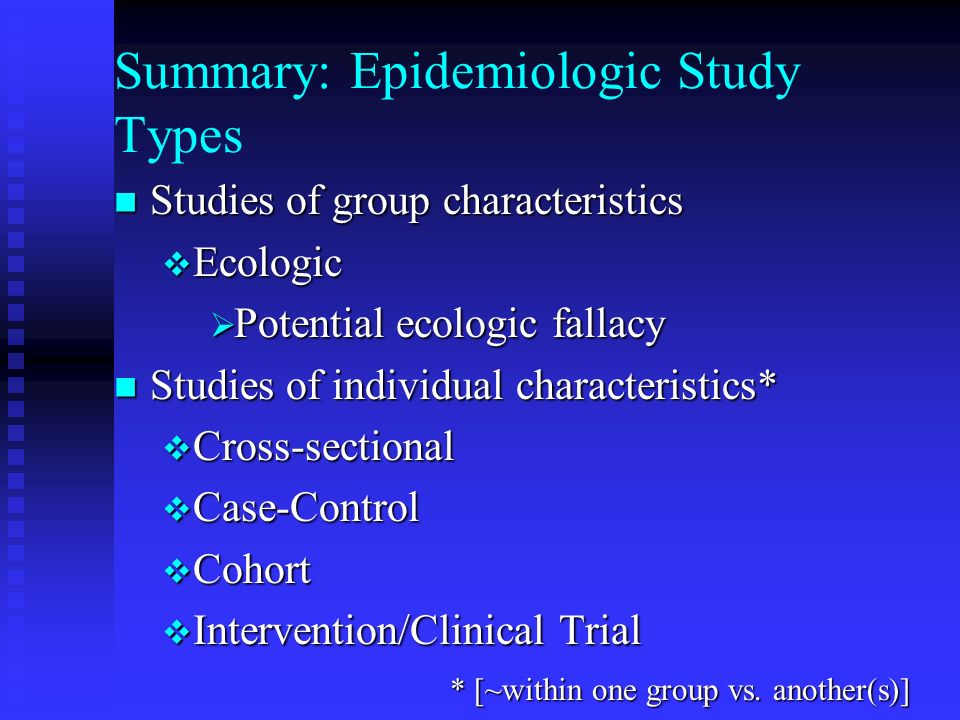
Borderline Personality Disorder (BPD)
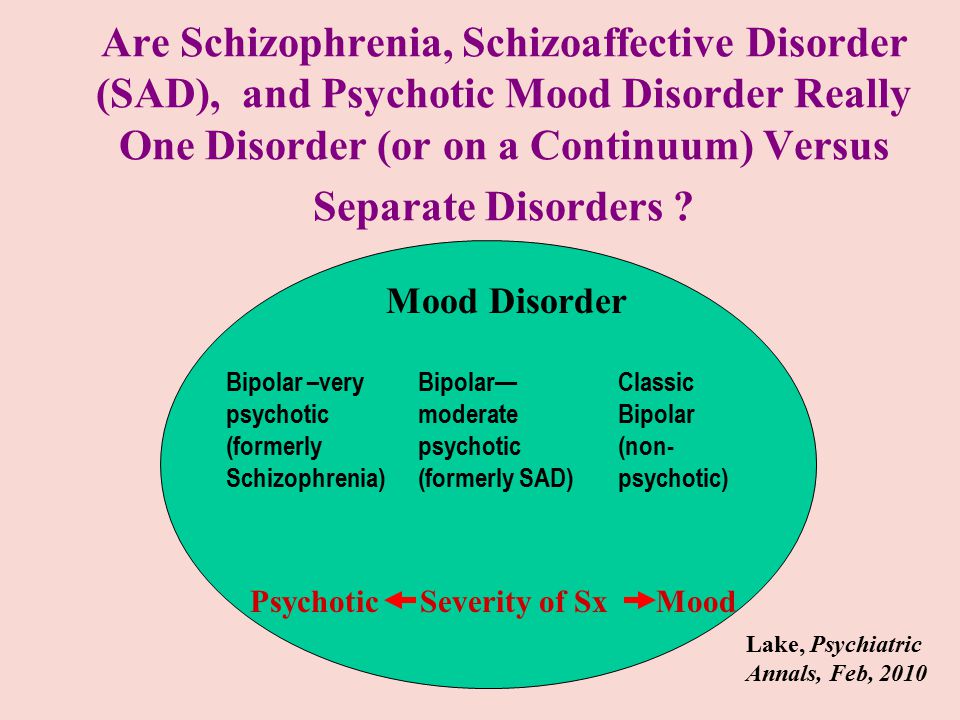
It is often difficult to tell the difference between bipolar and borderline without being a mental health professional. Both diseases are part of the same spectrum of disorders, and their manifestations are quite similar, but the main difference is that bipolar disorder is episodic, that is, it manifests itself in periods of varying duration, while borderline disorder is permanent in nature. Both conditions are characterized by increased emotionality, impulsiveness and “swing” of mood, however, bipolar personality disorder and borderline are two different nosological units that require different treatment and approach.
People with BPD constantly experience mood changes that affect behavior and personal perception of themselves, relationships with others, and energy resourcefulness. With bipolar personality disorder, the patient exhibits approximately the same symptoms, but not on a permanent basis, but in cycles, the frequency of which varies from several days to several months.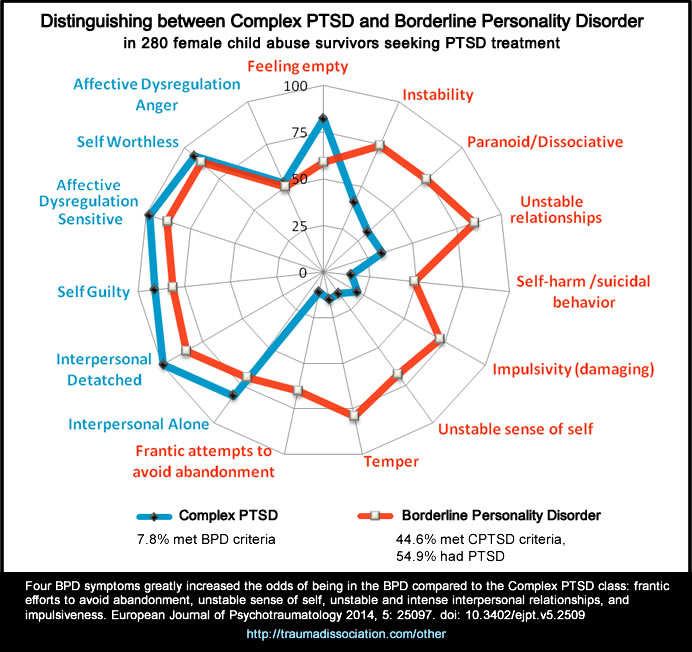 Borderline disorder is a rarer diagnosis than bipolar disorder.
Borderline disorder is a rarer diagnosis than bipolar disorder.
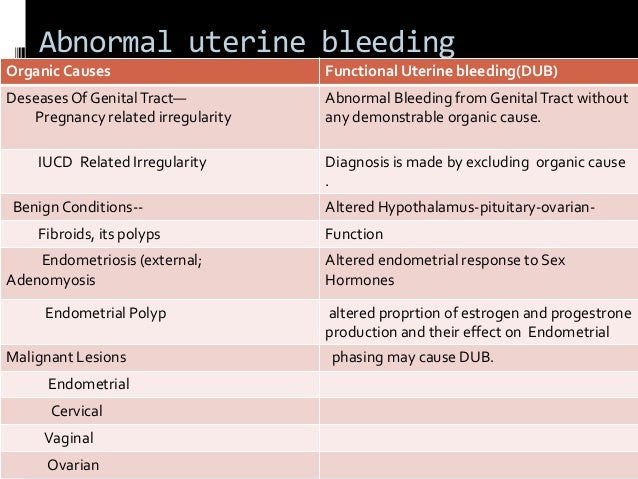
Bipolar disorder and women
Postpartum depression
Paradoxically, women are more susceptible to manic-depressive psychosis. The trigger factor for the development of the disease and its entry into the acute phase can be any period associated with hormonal changes. According to statistics, most diagnoses were made to women against the background of postpartum depression, as well as during menopause. Critical days can also affect mood swings and other consequences. The signs and symptoms of a depressive state characteristic of women do not differ much from those of men, however, there are distinctive features: in the prevailing majority, these are tearfulness, hysteria, increased emotionality and the need for increased attention from others. The help of a psychologist, and most often a psychiatrist, is simply necessary for patients who are depressed due to hormonal changes. According to statistics, most of the female suicides are associated with postpartum bipolar depression.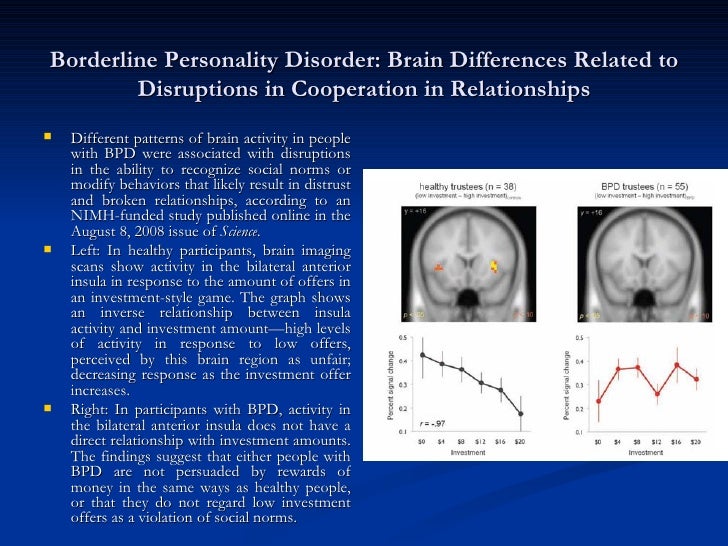 That is why a young mother needs the support of relatives and a specialist. Any fluctuations in the mood of a woman during this period should by no means be ignored. With age, by the way, in the anamnesis of female depression, hypochondria, in other words, anxiety, unreasonable fear and bad forebodings, begins to take an increasing place. It is not recommended to treat depression on your own or with folk remedies. Any psychopathic disorders of hormonal pathogenesis require a comprehensive study and observation, including both medication and psychotherapy.
That is why a young mother needs the support of relatives and a specialist. Any fluctuations in the mood of a woman during this period should by no means be ignored. With age, by the way, in the anamnesis of female depression, hypochondria, in other words, anxiety, unreasonable fear and bad forebodings, begins to take an increasing place. It is not recommended to treat depression on your own or with folk remedies. Any psychopathic disorders of hormonal pathogenesis require a comprehensive study and observation, including both medication and psychotherapy.
Living with Borderline and Bipolar Personality Disorder
This text was written by the Community and retains the author's style and spelling.
Sweet Em
Author profile
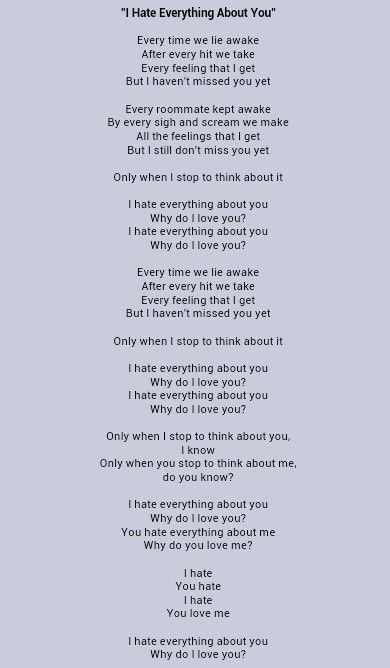
I am 29 years old and work as a manager in the capital. Six months ago, my boyfriend almost killed me.
I began to understand why I ended up in this situation and after months of searching and visiting doctors, I found out that I have a combination of borderline and bipolar personality disorder.
How my disorders manifest themselves
Ever since I was a child, I have noticed that my psyche is arranged somehow differently. For example, I had mood swings. I could study disgustingly all year, and in May I was overwhelmed by such euphoria that I corrected all my grades.
In March and February I usually have depression. In December, unbearable euphoria again. I can't make any plans for life, and even for the next couple of days, because I don't know what mood I will be in 10 minutes. I can arrange to meet with a friend in the evening, and by the time it's time to go out, change my mind and cancel everything for no good reason.
In the morning, I usually collect myself and my reality piece by piece. I explain to myself who I am, what I do, how I came to this, I also have to look in the mirror and weigh myself, this helps me determine what I am today. In general, it seems to me that the one who connects life with me will be very lucky, he will never wake up with the same person.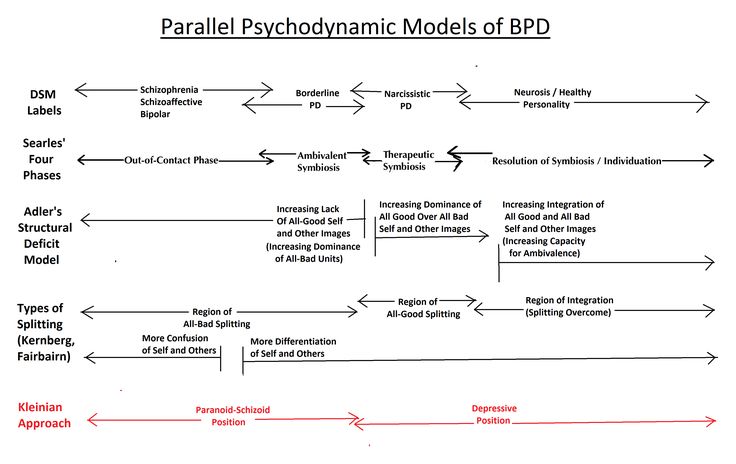
How I was diagnosed
As a result, my mood swings created a lot of problems for me. In moments of euphoria, I could both correct all my grades, and take a loan, marry a person simply because he is good, I could have champagne breakfast on Monday at 10 am or starve for a week. And the person who almost killed me was very suitable for my need for such a swing.
When it all happened, I couldn't sleep at first. I was tormented by insomnia, and if not for it, I would not have gone to a psychologist, then to a psychiatrist, then to a neurologist, then to another psychiatrist. In total, I spent 33,000 rubles on sessions with a psychologist. I had a neurologist and a psychiatrist from the field of evidence-based medicine, I decided that it would be better to pay more right away, but then I would not be assigned unnecessary studies or useless additional appointments. In total, the neurologist cost me 5000 R, and the psychiatrist the same amount.
What treatment was chosen
When I was diagnosed, they prescribed an antipsychotic, it cost about 1000 R. But the fact is that the neurologist prescribed me a medicine in a dose of 25 mg, and the psychiatrist recommended increasing it gradually to 300 mg. At about 100 mg, I began to turn into a vegetable and realized that I was not ready for treatment and stopped taking pills, visiting doctors and generally doing anything with my disorder, except to recognize myself and study its manifestations in me.
But the fact is that the neurologist prescribed me a medicine in a dose of 25 mg, and the psychiatrist recommended increasing it gradually to 300 mg. At about 100 mg, I began to turn into a vegetable and realized that I was not ready for treatment and stopped taking pills, visiting doctors and generally doing anything with my disorder, except to recognize myself and study its manifestations in me.
I keep a mood diary and hope it will help me predict future spikes. This will help to know when I will again turn into a tear-off and arrange a revelry for several days, and when I will lie and shed tears and not leave the house for weeks.
How my disorders affect my work and personal life
This is difficult. For example, if a person has an eye or a toothache, he says: yeah, you need to go to the doctor and get treated. You just make a decision, and you know that you can rely on yourself and take care of yourself. And when you have conditionally broken exactly the function that is needed for making decisions, you cannot rely on yourself.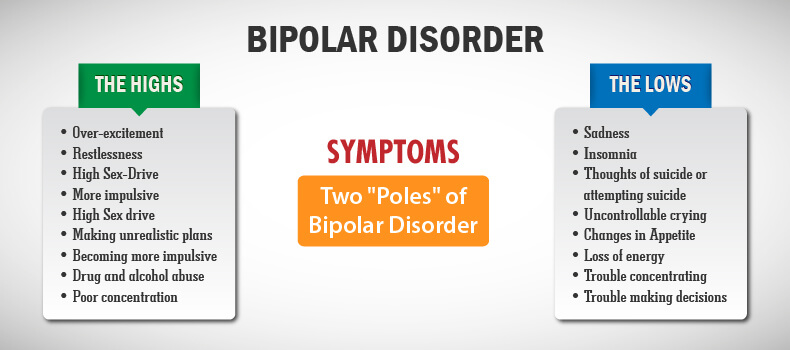 Because eternal sabotage takes place in the head. Thus, I also take care of my health spontaneously. In the summer, I underwent an examination for 40,000 R, recently I had a laser vision correction for 120,000 R, but I still have not reached an endocrinologist.
Because eternal sabotage takes place in the head. Thus, I also take care of my health spontaneously. In the summer, I underwent an examination for 40,000 R, recently I had a laser vision correction for 120,000 R, but I still have not reached an endocrinologist.
My disorder also affects my work quite strongly, I can make a volume during the recovery phase that a normal person cannot take out even in a month. And then I can’t even take on elementary tasks and put them off until the last minute. This is with regard to bipolar oscillations, they are longer.
And border jumps occur several times a day. For example, in the morning I may respond sharply to someone because I am in derealization or depersonalization. They demand some momentary decisions from me, but I cannot determine who I am and what my reality is. Then, after half an hour or an hour, I dot all the i's and come to a state of bliss, and to the one whom I was rude to, I can say that I will do everything, that I adore him, that we will definitely find a solution now. I think for many who work with me, it is not easy.
I think for many who work with me, it is not easy.
As for my personal life, I think that's understandable. I always needed some kind of nerve-wracking. That's when I got it enough, I finally thought about it.
How I feel now
Now I am not being treated by doctors or drugs. Moreover, now they are difficult to get, and it would be sad if I were sitting deeply on 300 mg now, when suddenly there would be problems with supplies.
It seems to me that the mere awareness of the presence of these disorders has helped me more than all of psychotherapy. And the diagnosis helped me learn more about myself than in the previous 29 years.years. Now, in a sense, I even use these disorders to my advantage. I have almost learned to predict when I will have a euphoria phase, and I try to concentrate all my workload on these days. I know that I will do it and I will do it cool. Conversely, when dark days come, I now prepare for them. I look for any philosophical movie, I lay it on my sofa, I buy sweets or wine, and I just surrender to this state. Finally, I realize that it will pass, and because of that, all this has become much easier to endure.
Finally, I realize that it will pass, and because of that, all this has become much easier to endure.
Evgenia Streletskaya's video about this disease helped me a lot. She is the only one I read to learn more about my disorder who said that the border guards are very unusual, creative, cool, extraordinary and I preferred to think of myself that way. Thanks to this path, I realized that living in harmony with myself is not just not having any disorders or other health problems, it is precisely treating this as a scientist, as an observer, with care and interest.
How I feel about doctors
At some point, one of the doctors advised me to be hospitalized because I said I wanted to do something bad to myself. But that was during moments of insomnia and severe PTSD. And the doctor sent me the best treatment options in Moscow, she figured everything out for me. It seems to me that psychiatrists are the most caring in the world.
Still, after February 24, another doctor was very worried that I would be left without medicines, of course I didn’t tell her that I didn’t take them, but convinced me that I had a supply and that it was enough for me.