Binge eating disorder prognosis
Binge Eating Disorder - StatPearls
Continuing Education Activity
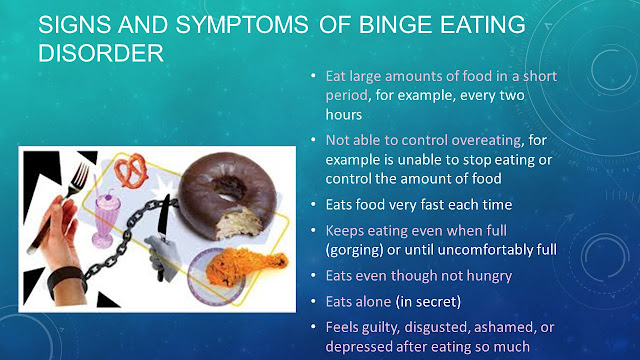
Binge eating disorder is an eating disorder associated with various psychological and non-psychological issues with some degree of impairment of daily life and a few severe impairments. According to The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), binge eating disorder consists of (1) Consuming a larger amount of food than other people would be able to consume in similar circumstances and similar period (usually within a two hour period). (2) Lack of control of eating and feeling guilty after eating. Episodes of binge eating disorder occur every week (at least once a week) for three months and not associated with compensatory behavior. This activity reviews the evaluation and management of patients with binge eating disorder and highlights the role of the interprofessional healthcare team in the care of patients with this condition.
Objectives:
Identify the etiology of binge eating disorder.
Outline the appropriate history, physical examination, and evaluation of binge eating disorder.
Review the treatment and management options available for binge eating disorder.
Describe interprofessional team strategies for improving care coordination and communication to manage binge eating disorder and improve outcomes.
Access free multiple choice questions on this topic.
Introduction
Binge eating disorder (BED) is a condition marked by episodes of consuming food in a larger amount than is normal in a short time. These episodes occur every week over three months. It is an individual diagnosis different from bulimia nervosa.[1][2] Binge eating disorder is associated with various psychological and non-psychological issues with some degree of impairment of daily life and a few severe impairments. General medical disorders such as obesity, diabetes, hypertension, and chronic pain are some of its comorbid conditions. It most commonly presents in obese individuals, but it is not limited to them.[3][4] The presenting complaint of people with binge eating disorder is weight gain. The prevalence of this disorder increases with an increase in body weight, and obesity is the frequent comorbidity.
It most commonly presents in obese individuals, but it is not limited to them.[3][4] The presenting complaint of people with binge eating disorder is weight gain. The prevalence of this disorder increases with an increase in body weight, and obesity is the frequent comorbidity.
Etiology
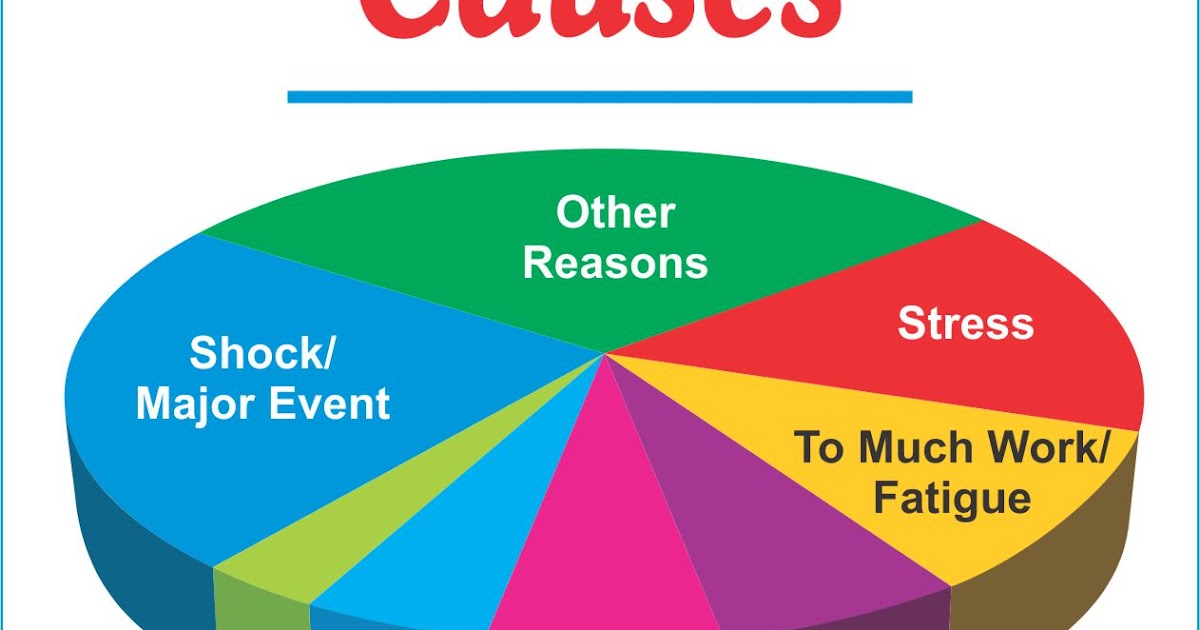
Binge eating disorder can result from numerous psychological, social, cultural, and biological factors. Some of the risk factors for binge eating disorder include:[5][6]
1) Childhood obesity
2) Loss of controlled eating in childhood
3) Perfectionism
4) Conduct problems
5) Substance abuse
6) Family weight concerns and eating problems
7) Family conflicts and parenting problems
8) Parental psychopathology
9) Physical and sexual abuse
10) Mental health impairment
11) Mu-opioid (e.g., OPRM1) receptor and dopamine (e.g., DRD2) receptors genes involvement
12) Distorted body image perception
13) Intestinal microbiota alteration
Epidemiology
Binge eating disorder is more common in women than men and usually occurs around the age of 23 years. [7] The lifetime prevalence of this disorder in the United States is 2.6%. Approximately 79% of people with binge eating disorder have one psychiatric disorder; 49% of people possess a lifetime history of two or more comorbid disorders.[7] Prevalent comorbid conditions with binge eating disorder include:[8]
[7] The lifetime prevalence of this disorder in the United States is 2.6%. Approximately 79% of people with binge eating disorder have one psychiatric disorder; 49% of people possess a lifetime history of two or more comorbid disorders.[7] Prevalent comorbid conditions with binge eating disorder include:[8]
Specific phobia (37%)
Social phobia (32%)
Post-traumatic stress disorder (26%)
Alcohol abuse or dependence (21%)
Another analysis showed that of those with more than one diagnosis, 65% had anxiety disorders, 46% had mood disorders, 43% had impulse-control disorders, and 23% had substance use disorders.[9]
Pathophysiology
Binge eating disorder has the same neurobiology as substance use disorder. Research has proposed several models to explain the pathophysiology of binge eating disorder.[10] It occurs due to difficulty in reward processing and inhibitory control. The prominent affect regulation model emphasizes the role of negative affect in binge eating disorder. According to this model, binge-eating episodes are triggered by negative affect and provide relief from them. Difficulties in emotional regulation and reduced emotional awareness have correlations with binge eating disorder. Additionally, interpersonal problems also carry associations with this disorder. Furthermore, neuroimaging studies showed hyperactivity of the medial orbitofrontal cortex and hypoactivity in the prefrontal network in individuals with binge eating disorder.[11][12]
According to this model, binge-eating episodes are triggered by negative affect and provide relief from them. Difficulties in emotional regulation and reduced emotional awareness have correlations with binge eating disorder. Additionally, interpersonal problems also carry associations with this disorder. Furthermore, neuroimaging studies showed hyperactivity of the medial orbitofrontal cortex and hypoactivity in the prefrontal network in individuals with binge eating disorder.[11][12]
The food addiction hypothesis states that individuals with high impulsivity and reward sensitivity experience an addictive response to certain foods, for example, high sugar and high-fat foods. Still, they do not develop tolerance or show withdrawal symptoms.[13]
An increased volume of the insula of the left orbitofrontal cortex is a known factor in eating disorders. The insula and frontal operculum are the two regions of the brain that are responsible for processing the basic sensory information about food. The ventral striatum, which includes nucleus accumbens and putamen, and caudate are accountable for evaluating and identifying the rewarding nature of food. The dorsal caudate, ventrolateral prefrontal cortex, parietal cortex, and dorsal anterior cingulate cortex, are the regions of the brain responsible for controlling food-related responses.[14] Patients with binge eating disorder demonstrate low impulse control activity in the prefrontal cortex (PFC), inferior frontal gyrus, ventrolateral PFC, and the insula.[15]
The ventral striatum, which includes nucleus accumbens and putamen, and caudate are accountable for evaluating and identifying the rewarding nature of food. The dorsal caudate, ventrolateral prefrontal cortex, parietal cortex, and dorsal anterior cingulate cortex, are the regions of the brain responsible for controlling food-related responses.[14] Patients with binge eating disorder demonstrate low impulse control activity in the prefrontal cortex (PFC), inferior frontal gyrus, ventrolateral PFC, and the insula.[15]
Polymorphism in the serotonin transporter dopamine receptor D and mu-opioid receptors have links to binge eating disorder.[16]
History and Physical
History [4]
The clinician should inquire about the following points to help diagnose patients with binge eating disorder.
1) Age of onset of binge eating episodes
2) Frequency of binge eating episodes
3) Duration of episodes
4) Amount of food
5) Feelings associated with binge disorder
6) Any compensatory behavior (vomiting, purging, laxative use)
7) Comorbid conditions (psychological problems, obesity, diabetes)
8) Emotional triggers (abandonment and stress)
9) Societal pressure
10) Media input (binge eating as an acceptable method to cope with stress)
11) Childhood emotional abuse
12) Childhood restriction of calorie intake or disordered eating behavior in childhood
13) Suicidal ideation
14) Substance misuse
15) Physical and sexual abuse
16) Body image perception
15) Family history of binge eating
Physical Examination
The patient should have an examination to assess for comorbidities associated with obesity due to binge eating disorder.
i) Blood pressure requires regular checking.
ii) Blood glucose requires regular monitoring.
iii) Examine for physical or sexual abuse if there is high suspicion.
The tools commonly used to evaluate binge eating disorder are as follows:
1) Binge eating scale
2) Three-factor eating questionnaire
3) Body shape questionnaire
4) Eating disorders examination (EDE)
5) Structured clinical interview for the diagnosis of DSM disorders
6) Questionnaire of eating and weight patterns
Evaluation
The evaluation of the patient with binge eating disorder includes the psychiatric, medical, and nutritional evaluation of the patient.
Psychiatric Status
Patients should have an evaluation for:
a) Psychiatric comorbidities (depression and substance abuse disorder)
b) Person image of body shape and weight
c) Self-esteem
Medical Status
Medical status evaluation should include comorbidities and parameters associated with obesity and excess body weight which are:
a) Waist circumference
b) Body mass index (measure height and weight)
c) Hypertension
d) Hyperlipidemia
e) Diabetes mellitus
f) Gastroesophageal reflux disease
g) Hepatobiliary disease
h) Coronary artery disease
i) Obstructive sleep apnea
j) Hypothyroidism
Nutritional Status
Assess the nutritional status of the person by asking:
a) Dieting and lifetime weight history
b) Physical activity and exercise
c) Current eating pattern and choice of food
d) Intensity and frequency of binge eating episodes
f) Types of overeating (overeating at meals, night eating, snacking, and grazing)
Treatment / Management
The type of treatment provided to binge eating disorder, treatment setting, and healthcare person involved in the therapy of patients with binge eating disorder depends upon treatment goals. Treatment goals may include working on:
Treatment goals may include working on:
1) Excessive body weight
2) Binge eating episodes
3) Extreme concern for body image
4) Comorbid psychiatric conditions (anxiety, substance use disorder, and depression)
Available treatment options for binge eating disorder include:
1) Psychotherapy
2) Pharmacotherapy
3) Weight loss treatment
1) Psychotherapy:
Psychotherapy is the first-line treatment option for binge eating disorder. According to several clinical trials, psychotherapy has a more significant clinical effect than pharmacotherapy. Common psychotherapy options are:
a) Cognitive-behavioral therapy
b) Interpersonal psychotherapy
c) Dialectical behavioral therapy
A) Cognitive Behavioral Therapy (CBT):
CBT is the psychotherapy of choice for binge eating disorder based on the results of several randomized controlled trials. The patient can receive CBT either from a clinician or through a self-help program without clinician involvement.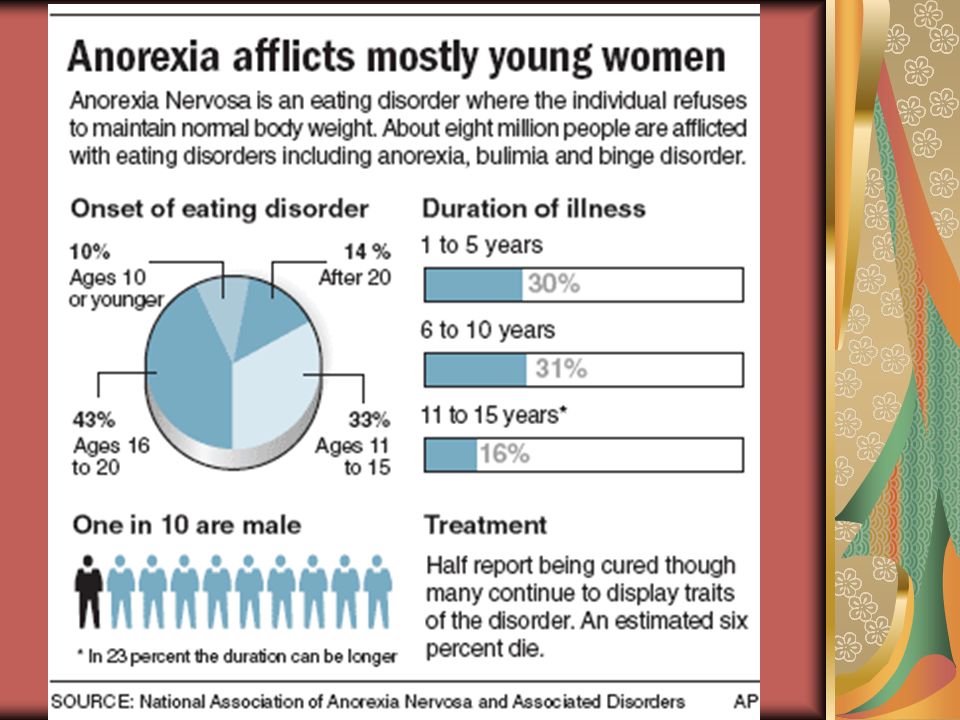 Research shows that CBT has higher abstinence, is well-tolerated, and maintains remission for 1 or 2 years. A quick change in symptoms of patients with binge eating disorder is a good prognostic sign. Binge eating disorder patients with comorbid anorexia nervosa or bulimia nervosa do not respond well to CBT.[17]
Research shows that CBT has higher abstinence, is well-tolerated, and maintains remission for 1 or 2 years. A quick change in symptoms of patients with binge eating disorder is a good prognostic sign. Binge eating disorder patients with comorbid anorexia nervosa or bulimia nervosa do not respond well to CBT.[17]
Self-help based CBT is as effective for treating binge eating disorder as clinician-led CBT. Treatment settings have an effect on self-help based CBT. Delivering self-help based CBT in specialty settings, for example, eating disorder clinics, is more effective than delivering in a primary care setting. A self-help program focuses upon creating a regular pattern of eating, monitoring eating habits, learning self-control techniques, and learning problem solving more effectively. Hardcopy, web-based content, workbook, or smartphone application can be used to implement this program.[18][19] These materials provide:
i) Step by step approach to therapy
ii) Education regarding binge eating disorder.
B) Interpersonal Psychotherapy:
Interpersonal psychotherapy can take place in a group format or individual format. Psychotherapy does not focus on weight loss, but weight changes do occur due to stopping binge eating. It can also be provided in combination with CBT if the patient has complex psychopathology that may include interpersonal problems, low self-esteem, and perfectionism.[8][20][21] The following are the steps of the therapeutic strategy of psychotherapy:
i) Identify the area (most probably interpersonal area) that links to binge eating disorder.
ii) Focus mainly on experimentation or constructive changes in the problematic relevant regions (interpersonal) with little focus on binge eating.
C) Dialectical Behavioral Therapy:
Dialectical behavioral therapy consists of educating patients about the skills which are needed to manage problematic behavior associated with emotional dysregulation.[22] This therapy helps patients in balancing the dichotomous feelings, behavior, and thinking.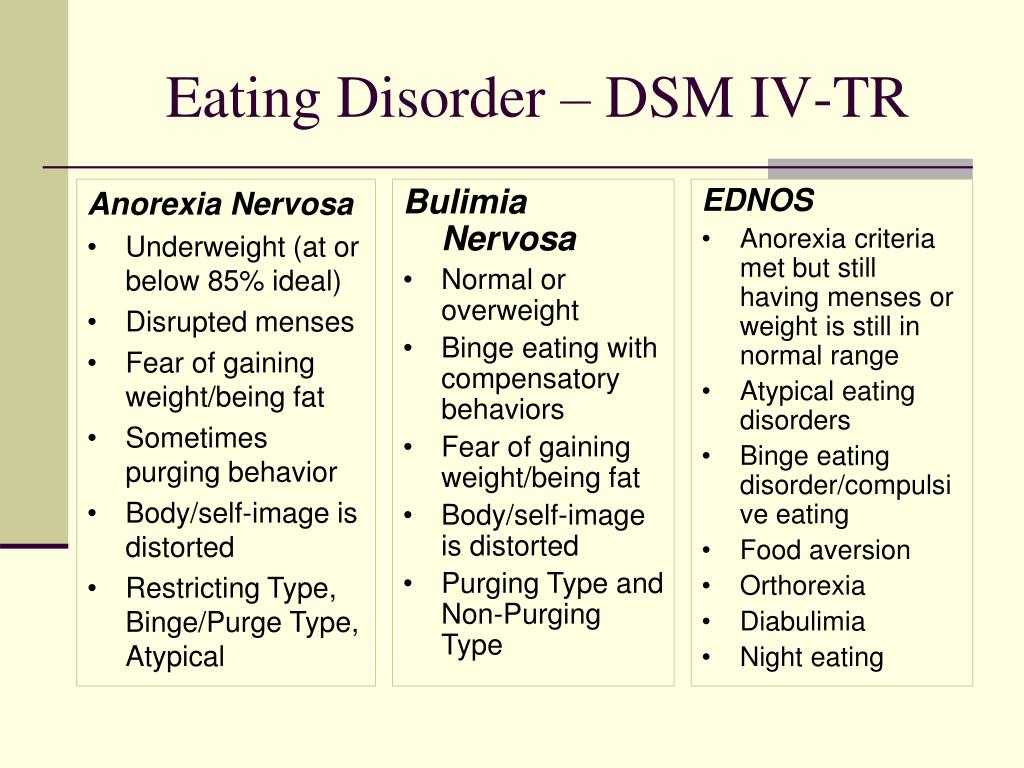 The skills highlighted in this therapy include:
The skills highlighted in this therapy include:
i) Watchful eating
ii) Emotional balance
iii) Tolerance of unpleasant circumstances
iv) Prevention of relapses
2) Pharmacotherapy:
Pharmacotherapy should be used as first-line therapy in patients who:
i) Do not have access to psychotherapy
ii) Decline psychotherapy
iii) Prefer medications
Medications that can be useful for binge eating disorder include:
i) Selective serotonin reuptake inhibitors (SSRIs) - sertraline, fluoxetine, fluvoxamine, escitalopram, citalopram
ii) Antiepileptic drugs - zonisamide and topiramate
iii) Attention deficit hyperactivity disorder (ADHD) medications - lisdexamfetamine, and atomoxetine)
iv) Medication for shift work disorder - armodafinil
v)
Selective serotonin reuptake inhibitors (SSRIs) should be the first-line pharmacotherapy for binge eating disorder. Antiepileptic medications or medications used for ADHD are an option if a patient fails one or two courses of SSRI. Randomized controlled trials have reported a promising role of topiramate, lisdexamfetamine, and methylphenidate in causing abstinence from binge eating disorder as well as in weight reduction. Limitations for using these medications have been due to the side effects of these medications. Topiramate can cause somnolence, paraesthesias, and cognitive impairment. Lisdexamfetamine and methylphenidate may cause anorexia, gastrointestinal disorder, headache, insomnia, sympathetic nervous system arousal, as well as dependence, and potential misuse.[23][24][25] Lisdexamfetamine is FDA-approved for the treatment of moderate to severe BED in adults aged 18 to 55.
Randomized controlled trials have reported a promising role of topiramate, lisdexamfetamine, and methylphenidate in causing abstinence from binge eating disorder as well as in weight reduction. Limitations for using these medications have been due to the side effects of these medications. Topiramate can cause somnolence, paraesthesias, and cognitive impairment. Lisdexamfetamine and methylphenidate may cause anorexia, gastrointestinal disorder, headache, insomnia, sympathetic nervous system arousal, as well as dependence, and potential misuse.[23][24][25] Lisdexamfetamine is FDA-approved for the treatment of moderate to severe BED in adults aged 18 to 55.
3) Obesity or weight loss treatment: Most of the patients with binge eating disorder seek treatment for weight reduction rather than binge eating. All obese patients should be evaluated closely for binge eating disorder.[8]
i) Low and very low-calorie diet and exercise is the best option for losing weight. Behavioral weight loss therapy is a strategy designed to reduce binge eating as a result of weight loss indirectly.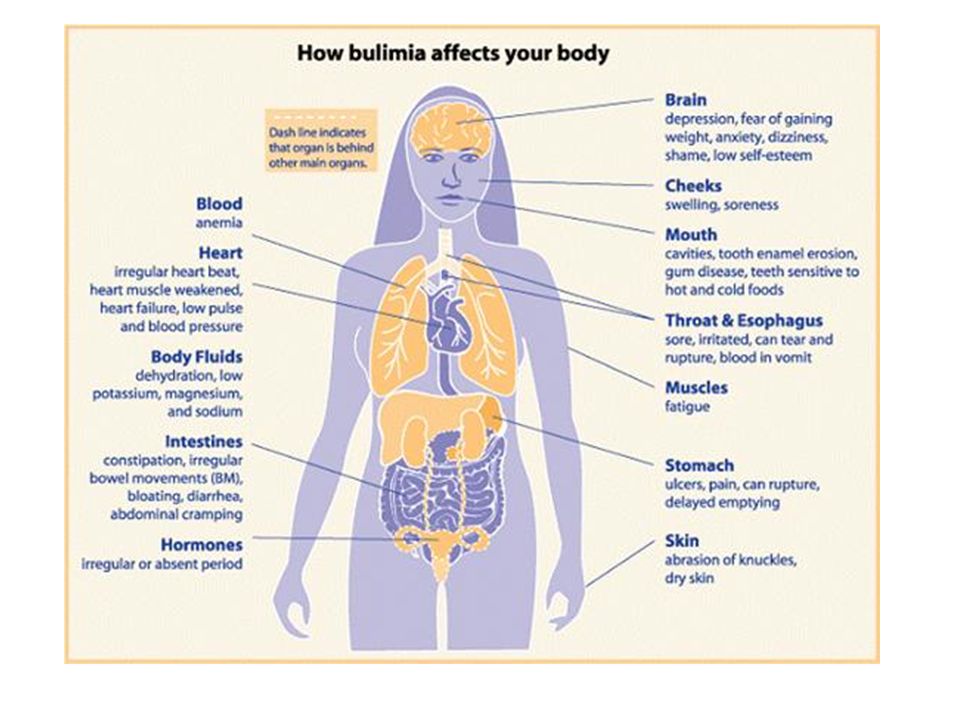 A randomized controlled trial concluded that behavioral weight loss therapy showed remission of binge eating disorder in 44 percent of patients. Moderate calorie restriction, exercise, and improved nutrition with nutritional counseling and rehabilitation are some of the specific components of behavioral weight loss therapy.
A randomized controlled trial concluded that behavioral weight loss therapy showed remission of binge eating disorder in 44 percent of patients. Moderate calorie restriction, exercise, and improved nutrition with nutritional counseling and rehabilitation are some of the specific components of behavioral weight loss therapy.
ii) Pharmacotherapy provides short-term weight loss in obese patients. Different classes of medications exert different clinical effects. Pharmacologic agents should be chosen based on patient preference, patient comorbidities, potential adverse effects, and insurance coverage, cost of medication of choice for obesity include:
a) Lorcaserin and liraglutide (daily injections)
b) Orlistat
c) Combination phentermine-extended release topiramate
d) Combination naltrexone-bupropion
e) Phenteramine
f) Benzphenteramine
g) Phendimetrazine
h) Diethylpropion
iii) Bariatric surgery can also be helpful for obese patients with binge eating disorder. Binge eating after bariatric surgery is associated with poor weight outcomes.
Binge eating after bariatric surgery is associated with poor weight outcomes.
iv) Psychotherapy has no role in reducing weight in obese patients with binge eating disorder.
Differential Diagnosis
Diseases that come under the differential diagnosis of binge eating disorder are as follows:
Bulimia nervosa - Binge eating disorder differs from bulimia nervosa in that there is no compensatory behavior (laxative misuse, fasting, or self-induced vomiting) after eating to prevent weight gain
Anxiety disorder - Anxiety disorder also has associations with binge eating; however, the patient will only receive a diagnosis of binge eating disorder when binging episodes occur every week for three months
Kleine-Levin syndrome - Episodes of binges associated with excessive sleep
Mood disorder - Episodes of binges occur with other psychological features of mood disorder
Prognosis
Long-term outcome studies of binge eating disorder demonstrate that the prognosis of binge eating disorder is better than other eating disorders with a more favorable remission rate.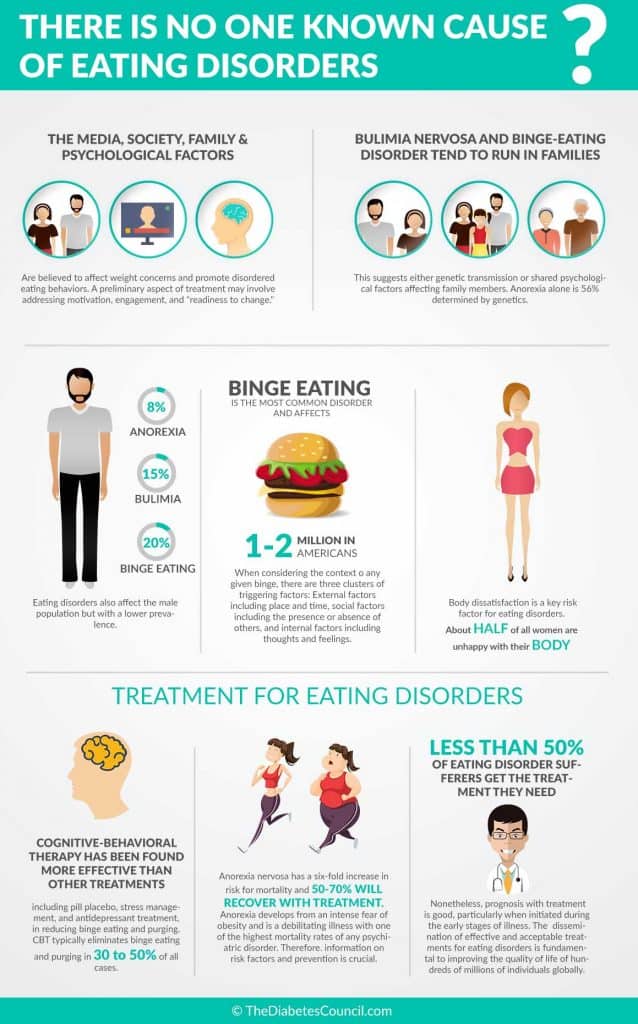 The tendency of binge eating disorder to convert to other eating disorders is very small. Only a few studies have reported increased odds of migration to bulimia nervosa. Depressive symptoms and substance abuse are two significant adverse mental health outcomes of binge eating disorder.[26]
The tendency of binge eating disorder to convert to other eating disorders is very small. Only a few studies have reported increased odds of migration to bulimia nervosa. Depressive symptoms and substance abuse are two significant adverse mental health outcomes of binge eating disorder.[26]
Binge eating disorder in childhood predicts excess weight gain in adolescent and young women. It also independently increased the risk of obesity-related complications, for example, metabolic syndrome.[27][28][29]
Complications
Most of the patients with binge eating disorder are obese. Binge eating disorder and obesity, most of the time, coexist and share complications.[4][30] The complications of these two disorders include:[31][32][33]
1) Muscular pain
2) Neck, shoulder, and lower back pain
3) Impairment resulting from physical health problems after adjustment of BMI
4) Hypertension
5) Diabetes
6) Asthma - respiratory illness
7) Coronary artery diseases and heart failure
8) Hyperlipidemia
9) Weight gain
10) Menstrual dysfunction (amenorrhea, oligomenorrhea)
11) Cortisol hormones disbalance (blunted cortisol response to stress test and decreased urinary cortisol levels)
12) Cancer (colon, breast, endometrial, gall bladder, and other)
13) Osteoarthritis
14) Sleep apnea
15) Obesity hypoventilation syndrome
16) Non-alcoholic fatty liver disease
17) Gallbladder disease
18) Metabolic syndrome
Deterrence and Patient Education
Patients should have counseling regarding the disorder and how to cope with binges. Awareness of binge episodes and knowledge of strategies for self-control help prevent the vicious cycle of binges-guilt-binges. Over-evaluating body shape and weight produce dysfunctional eating and dieting behavior, which causes physiological and psychological vulnerability to episodes of binge eating.[34] Patients should be told to:
Awareness of binge episodes and knowledge of strategies for self-control help prevent the vicious cycle of binges-guilt-binges. Over-evaluating body shape and weight produce dysfunctional eating and dieting behavior, which causes physiological and psychological vulnerability to episodes of binge eating.[34] Patients should be told to:
i) Monitor eating patterns and keep a record of each meal, snacks, and trigger of binge episodes
ii) Identify triggers, which include under-eating, ingesting disinhibiting substances, breaking self or clinician created dietary rule system, or becoming dysphoric
iii) Create a pattern of eating with only three to four hours gap between meals. The patient should gradually implement the pattern
iv) Avoid places, activities, and people that trigger binge eating
v) Learn to solve a problem if causing binges by identifying the problem, generating multiple solutions, thinking through each solution, and choosing one problem at a time upon which to act
vi) Recognize food that leads to binge episodes
vii) Identify the single event that leads to episodes
viii) Weigh himself or herself once per week to avoid excessive weight checking or avoidance of weighing at all
Enhancing Healthcare Team Outcomes
The management of patients with binge eating disorder should be with the help of an interprofessional team, including a medical clinician, psychologist, psychiatrists, pharmacists, nutritionists, social workers, educational professionals, endocrinologists, and nurses. Counseling from nutritionists plays an essential role in organizing and planning meals as well as behavioral weight loss therapy for these patients.[35] As binge eating disorder is mostly associated with comorbid psychological conditions, the involvement of psychologists helps manage binge eating disorder. These patients should receive treatment in an outpatient setting.[22] Clinicians should be well trained in evaluating and managing patients with this disorder. Patient management can also include a self-help program.[21] Bariatric and psychiatric nurses are involved with patient and family education, monitoring of patients, and documentation for the team. Pharmacists evaluate prescribed medications for appropriateness, dosage, and drug interactions, and report any concerns to the rest of the team. These are but a few examples of interprofessional team collaboration that can improve patient outcomes. [Level 5]
Counseling from nutritionists plays an essential role in organizing and planning meals as well as behavioral weight loss therapy for these patients.[35] As binge eating disorder is mostly associated with comorbid psychological conditions, the involvement of psychologists helps manage binge eating disorder. These patients should receive treatment in an outpatient setting.[22] Clinicians should be well trained in evaluating and managing patients with this disorder. Patient management can also include a self-help program.[21] Bariatric and psychiatric nurses are involved with patient and family education, monitoring of patients, and documentation for the team. Pharmacists evaluate prescribed medications for appropriateness, dosage, and drug interactions, and report any concerns to the rest of the team. These are but a few examples of interprofessional team collaboration that can improve patient outcomes. [Level 5]
Clinicians should be aware that patients with binge eating disorder are vulnerable to shame and stigma and find it distressing to share it with healthcare professionals. [36] The management and information should be tailored to the age and level of development. Healthcare professionals should also keep in mind to assess for signs of bullying, teasing, abuse, and neglect. Team members should address any misconception regarding binge eating disorder that the patients or their families might have. The clinician should communicate with the patient properly, and the patient's weight and appearance should be addressed with care. Patients with binge eating disorder require assessment promptly following the identification of the disorder.[37] The clinician and all interprofessional team members should show empathy, respect, and compassion, and provide suitable information for binging eating disorder and obesity.[38] Patient family members, guardians, teachers, and peers should also be encouraged to support the patient during treatment. Patient family members should also undergo assessment for eating disorder, and their mental health and practical support, and the team should offer emergency plans if the patient is at high risk of a psychiatric event.
[36] The management and information should be tailored to the age and level of development. Healthcare professionals should also keep in mind to assess for signs of bullying, teasing, abuse, and neglect. Team members should address any misconception regarding binge eating disorder that the patients or their families might have. The clinician should communicate with the patient properly, and the patient's weight and appearance should be addressed with care. Patients with binge eating disorder require assessment promptly following the identification of the disorder.[37] The clinician and all interprofessional team members should show empathy, respect, and compassion, and provide suitable information for binging eating disorder and obesity.[38] Patient family members, guardians, teachers, and peers should also be encouraged to support the patient during treatment. Patient family members should also undergo assessment for eating disorder, and their mental health and practical support, and the team should offer emergency plans if the patient is at high risk of a psychiatric event.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Walsh BT, Sysko R. Broad categories for the diagnosis of eating disorders (BCD-ED): an alternative system for classification. Int J Eat Disord. 2009 Dec;42(8):754-64. [PMC free article: PMC2818502] [PubMed: 19650083]
- 2.
Wilfley DE, Citrome L, Herman BK. Characteristics of binge eating disorder in relation to diagnostic criteria. Neuropsychiatr Dis Treat. 2016;12:2213-23. [PMC free article: PMC5010172] [PubMed: 27621631]
- 3.
Sheehan DV, Herman BK. The Psychological and Medical Factors Associated With Untreated Binge Eating Disorder. Prim Care Companion CNS Disord. 2015;17(2) [PMC free article: PMC4560195] [PubMed: 26445695]
- 4.
Kornstein SG, Kunovac JL, Herman BK, Culpepper L. Recognizing Binge-Eating Disorder in the Clinical Setting: A Review of the Literature.
 Prim Care Companion CNS Disord. 2016;18(3) [PMC free article: PMC5035811] [PubMed: 27733955]
Prim Care Companion CNS Disord. 2016;18(3) [PMC free article: PMC5035811] [PubMed: 27733955]- 5.
Hilbert A. Binge-Eating Disorder. Psychiatr Clin North Am. 2019 Mar;42(1):33-43. [PubMed: 30704638]
- 6.
Raevuori A, Lukkariniemi L, Suokas JT, Gissler M, Suvisaari JM, Haukka J. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016 Jun;49(6):542-52. [PubMed: 26875554]
- 7.
Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, de Graaf R, Maria Haro J, Kovess-Masfety V, O'Neill S, Posada-Villa J, Sasu C, Scott K, Viana MC, Xavier M. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013 May 01;73(9):904-14. [PMC free article: PMC3628997] [PubMed: 23290497]
- 8.

Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010 Jan;67(1):94-101. [PMC free article: PMC3757519] [PubMed: 20048227]
- 9.
Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007 Feb 01;61(3):348-58. [PMC free article: PMC1892232] [PubMed: 16815322]
- 10.
Schreiber LR, Odlaug BL, Grant JE. The overlap between binge eating disorder and substance use disorders: Diagnosis and neurobiology. J Behav Addict. 2013 Dec;2(4):191-8. [PMC free article: PMC4154572] [PubMed: 25215200]
- 11.
Dingemans A, Danner U, Parks M. Emotion Regulation in Binge Eating Disorder: A Review. Nutrients. 2017 Nov 22;9(11) [PMC free article: PMC5707746] [PubMed: 29165348]
- 12.
Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment.
 Psychol Bull. 2011 Jul;137(4):660-681. [PMC free article: PMC3100657] [PubMed: 21574678]
Psychol Bull. 2011 Jul;137(4):660-681. [PMC free article: PMC3100657] [PubMed: 21574678]- 13.
Schulte EM, Grilo CM, Gearhardt AN. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev. 2016 Mar;44:125-139. [PMC free article: PMC5796407] [PubMed: 26879210]
- 14.
McClure SM, Laibson DI, Loewenstein G, Cohen JD. Separate neural systems value immediate and delayed monetary rewards. Science. 2004 Oct 15;306(5695):503-7. [PubMed: 15486304]
- 15.
Balodis IM, Molina ND, Kober H, Worhunsky PD, White MA, Rajita Sinha, Grilo CM, Potenza MN. Divergent neural substrates of inhibitory control in binge eating disorder relative to other manifestations of obesity. Obesity (Silver Spring). 2013 Feb;21(2):367-77. [PMC free article: PMC3610836] [PubMed: 23404820]
- 16.
Himmerich H, Bentley J, Kan C, Treasure J. Genetic risk factors for eating disorders: an update and insights into pathophysiology.
 Ther Adv Psychopharmacol. 2019;9:2045125318814734. [PMC free article: PMC6378634] [PubMed: 30800283]
Ther Adv Psychopharmacol. 2019;9:2045125318814734. [PMC free article: PMC6378634] [PubMed: 30800283]- 17.
Sysko R, Hildebrandt T, Wilson GT, Wilfley DE, Agras WS. Heterogeneity moderates treatment response among patients with binge eating disorder. J Consult Clin Psychol. 2010 Oct;78(5):681-90. [PMC free article: PMC2948417] [PubMed: 20873903]
- 18.
Striegel-Moore RH, Wilson GT, DeBar L, Perrin N, Lynch F, Rosselli F, Kraemer HC. Cognitive behavioral guided self-help for the treatment of recurrent binge eating. J Consult Clin Psychol. 2010 Jun;78(3):312-21. [PMC free article: PMC2880824] [PubMed: 20515207]
- 19.
Lynch FL, Striegel-Moore RH, Dickerson JF, Perrin N, Debar L, Wilson GT, Kraemer HC. Cost-effectiveness of guided self-help treatment for recurrent binge eating. J Consult Clin Psychol. 2010 Jun;78(3):322-33. [PMC free article: PMC2880825] [PubMed: 20515208]
- 20.
Murphy R, Straebler S, Cooper Z, Fairburn CG.
 Cognitive behavioral therapy for eating disorders. Psychiatr Clin North Am. 2010 Sep;33(3):611-27. [PMC free article: PMC2928448] [PubMed: 20599136]
Cognitive behavioral therapy for eating disorders. Psychiatr Clin North Am. 2010 Sep;33(3):611-27. [PMC free article: PMC2928448] [PubMed: 20599136]- 21.
Wilfley DE, Agras WS, Telch CF, Rossiter EM, Schneider JA, Cole AG, Sifford LA, Raeburn SD. Group cognitive-behavioral therapy and group interpersonal psychotherapy for the nonpurging bulimic individual: a controlled comparison. J Consult Clin Psychol. 1993 Apr;61(2):296-305. [PubMed: 8473584]
- 22.
American Psychiatric Association. Treatment of patients with eating disorders,third edition. American Psychiatric Association. Am J Psychiatry. 2006 Jul;163(7 Suppl):4-54. [PubMed: 16925191]
- 23.
Vocks S, Tuschen-Caffier B, Pietrowsky R, Rustenbach SJ, Kersting A, Herpertz S. Meta-analysis of the effectiveness of psychological and pharmacological treatments for binge eating disorder. Int J Eat Disord. 2010 Apr;43(3):205-17. [PubMed: 19402028]
- 24.
Reas DL, Grilo CM.
 Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity (Silver Spring). 2008 Sep;16(9):2024-38. [PMC free article: PMC3650491] [PubMed: 19186327]
Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity (Silver Spring). 2008 Sep;16(9):2024-38. [PMC free article: PMC3650491] [PubMed: 19186327]- 25.
Brambilla F, Samek L, Company M, Lovo F, Cioni L, Mellado C. Multivariate therapeutic approach to binge-eating disorder: combined nutritional, psychological and pharmacological treatment. Int Clin Psychopharmacol. 2009 Nov;24(6):312-7. [PubMed: 19794312]
- 26.
Hilbert A, Bishop ME, Stein RI, Tanofsky-Kraff M, Swenson AK, Welch RR, Wilfley DE. Long-term efficacy of psychological treatments for binge eating disorder. Br J Psychiatry. 2012 Mar;200(3):232-7. [PMC free article: PMC3290797] [PubMed: 22282429]
- 27.
Schaumberg K, Welch E, Breithaupt L, Hübel C, Baker JH, Munn-Chernoff MA, Yilmaz Z, Ehrlich S, Mustelin L, Ghaderi A, Hardaway AJ, Bulik-Sullivan EC, Hedman AM, Jangmo A, Nilsson IAK, Wiklund C, Yao S, Seidel M, Bulik CM. The Science Behind the Academy for Eating Disorders' Nine Truths About Eating Disorders.
Eur Eat Disord Rev. 2017 Nov;25(6):432-450. [PMC free article: PMC5711426] [PubMed: 28967161]
- 28.
Franko DL, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, Herzog DB. A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. Am J Psychiatry. 2013 Aug;170(8):917-25. [PMC free article: PMC4120076] [PubMed: 23771148]
- 29.
Steinhausen HC. Outcome of eating disorders. Child Adolesc Psychiatr Clin N Am. 2009 Jan;18(1):225-42. [PubMed: 19014869]
- 30.
McCuen-Wurst C, Ruggieri M, Allison KC. Disordered eating and obesity: associations between binge-eating disorder, night-eating syndrome, and weight-related comorbidities. Ann N Y Acad Sci. 2018 Jan;1411(1):96-105. [PMC free article: PMC5788730] [PubMed: 29044551]
- 31.
Algars M, Huang L, Von Holle AF, Peat CM, Thornton LM, Lichtenstein P, Bulik CM. Binge eating and menstrual dysfunction. J Psychosom Res. 2014 Jan;76(1):19-22. [PMC free article: PMC3909535] [PubMed: 24360136]
- 32.
Rosenberg N, Bloch M, Ben Avi I, Rouach V, Schreiber S, Stern N, Greenman Y. Cortisol response and desire to binge following psychological stress: comparison between obese subjects with and without binge eating disorder. Psychiatry Res. 2013 Jul 30;208(2):156-61. [PubMed: 23083917]
- 33.
Lavagnino L, Amianto F, Parasiliti Caprino M, Maccario M, Arvat E, Ghigo E, Abbate Daga G, Fassino S. Urinary cortisol and psychopathology in obese binge eating subjects. Appetite. 2014 Dec;83:112-116. [PubMed: 25149200]
- 34.
Ely AV, Cusack A. The Binge and the Brain. Cerebrum. 2015 Sep-Oct;2015 [PMC free article: PMC4919948] [PubMed: 27358667]
- 35.
Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010 Feb 13;375(9714):583-93. [PubMed: 19931176]
- 36.
Becker AE, Hadley Arrindell A, Perloe A, Fay K, Striegel-Moore RH. A qualitative study of perceived social barriers to care for eating disorders: perspectives from ethnically diverse health care consumers.
Int J Eat Disord. 2010 Nov 01;43(7):633-47. [PMC free article: PMC3020364] [PubMed: 19806607]
- 37.
Treasure J, Nazar BP. Interventions for the Carers of Patients With Eating Disorders. Curr Psychiatry Rep. 2016 Feb;18(2):16. [PMC free article: PMC4718944] [PubMed: 26781554]
- 38.
Sim LA, McAlpine DE, Grothe KB, Himes SM, Cockerill RG, Clark MM. Identification and treatment of eating disorders in the primary care setting. Mayo Clin Proc. 2010 Aug;85(8):746-51. [PMC free article: PMC2912736] [PubMed: 20605951]
Binge Eating Disorder - StatPearls
Continuing Education Activity
Binge eating disorder is an eating disorder associated with various psychological and non-psychological issues with some degree of impairment of daily life and a few severe impairments. According to The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), binge eating disorder consists of (1) Consuming a larger amount of food than other people would be able to consume in similar circumstances and similar period (usually within a two hour period). (2) Lack of control of eating and feeling guilty after eating. Episodes of binge eating disorder occur every week (at least once a week) for three months and not associated with compensatory behavior. This activity reviews the evaluation and management of patients with binge eating disorder and highlights the role of the interprofessional healthcare team in the care of patients with this condition.
Objectives:
Identify the etiology of binge eating disorder.
Outline the appropriate history, physical examination, and evaluation of binge eating disorder.
Review the treatment and management options available for binge eating disorder.
Describe interprofessional team strategies for improving care coordination and communication to manage binge eating disorder and improve outcomes.
Access free multiple choice questions on this topic.
Introduction
Binge eating disorder (BED) is a condition marked by episodes of consuming food in a larger amount than is normal in a short time. These episodes occur every week over three months. It is an individual diagnosis different from bulimia nervosa.[1][2] Binge eating disorder is associated with various psychological and non-psychological issues with some degree of impairment of daily life and a few severe impairments. General medical disorders such as obesity, diabetes, hypertension, and chronic pain are some of its comorbid conditions. It most commonly presents in obese individuals, but it is not limited to them.[3][4] The presenting complaint of people with binge eating disorder is weight gain. The prevalence of this disorder increases with an increase in body weight, and obesity is the frequent comorbidity.
Etiology
Binge eating disorder can result from numerous psychological, social, cultural, and biological factors. Some of the risk factors for binge eating disorder include:[5][6]
1) Childhood obesity
2) Loss of controlled eating in childhood
3) Perfectionism
4) Conduct problems
5) Substance abuse
6) Family weight concerns and eating problems
7) Family conflicts and parenting problems
8) Parental psychopathology
9) Physical and sexual abuse
10) Mental health impairment
11) Mu-opioid (e. g., OPRM1) receptor and dopamine (e.g., DRD2) receptors genes involvement
12) Distorted body image perception
13) Intestinal microbiota alteration
Epidemiology
Binge eating disorder is more common in women than men and usually occurs around the age of 23 years.[7] The lifetime prevalence of this disorder in the United States is 2.6%. Approximately 79% of people with binge eating disorder have one psychiatric disorder; 49% of people possess a lifetime history of two or more comorbid disorders.[7] Prevalent comorbid conditions with binge eating disorder include:[8]
Specific phobia (37%)
Social phobia (32%)
Post-traumatic stress disorder (26%)
Alcohol abuse or dependence (21%)
Another analysis showed that of those with more than one diagnosis, 65% had anxiety disorders, 46% had mood disorders, 43% had impulse-control disorders, and 23% had substance use disorders.[9]
Pathophysiology
Binge eating disorder has the same neurobiology as substance use disorder. Research has proposed several models to explain the pathophysiology of binge eating disorder.[10] It occurs due to difficulty in reward processing and inhibitory control. The prominent affect regulation model emphasizes the role of negative affect in binge eating disorder. According to this model, binge-eating episodes are triggered by negative affect and provide relief from them. Difficulties in emotional regulation and reduced emotional awareness have correlations with binge eating disorder. Additionally, interpersonal problems also carry associations with this disorder. Furthermore, neuroimaging studies showed hyperactivity of the medial orbitofrontal cortex and hypoactivity in the prefrontal network in individuals with binge eating disorder.[11][12]
The food addiction hypothesis states that individuals with high impulsivity and reward sensitivity experience an addictive response to certain foods, for example, high sugar and high-fat foods. Still, they do not develop tolerance or show withdrawal symptoms. [13]
An increased volume of the insula of the left orbitofrontal cortex is a known factor in eating disorders. The insula and frontal operculum are the two regions of the brain that are responsible for processing the basic sensory information about food. The ventral striatum, which includes nucleus accumbens and putamen, and caudate are accountable for evaluating and identifying the rewarding nature of food. The dorsal caudate, ventrolateral prefrontal cortex, parietal cortex, and dorsal anterior cingulate cortex, are the regions of the brain responsible for controlling food-related responses.[14] Patients with binge eating disorder demonstrate low impulse control activity in the prefrontal cortex (PFC), inferior frontal gyrus, ventrolateral PFC, and the insula.[15]
Polymorphism in the serotonin transporter dopamine receptor D and mu-opioid receptors have links to binge eating disorder.[16]
History and Physical
History [4]
The clinician should inquire about the following points to help diagnose patients with binge eating disorder.
1) Age of onset of binge eating episodes
2) Frequency of binge eating episodes
3) Duration of episodes
4) Amount of food
5) Feelings associated with binge disorder
6) Any compensatory behavior (vomiting, purging, laxative use)
7) Comorbid conditions (psychological problems, obesity, diabetes)
8) Emotional triggers (abandonment and stress)
9) Societal pressure
10) Media input (binge eating as an acceptable method to cope with stress)
11) Childhood emotional abuse
12) Childhood restriction of calorie intake or disordered eating behavior in childhood
13) Suicidal ideation
14) Substance misuse
15) Physical and sexual abuse
16) Body image perception
15) Family history of binge eating
Physical Examination
The patient should have an examination to assess for comorbidities associated with obesity due to binge eating disorder.
i) Blood pressure requires regular checking.
ii) Blood glucose requires regular monitoring.
iii) Examine for physical or sexual abuse if there is high suspicion.
The tools commonly used to evaluate binge eating disorder are as follows:
1) Binge eating scale
2) Three-factor eating questionnaire
3) Body shape questionnaire
4) Eating disorders examination (EDE)
5) Structured clinical interview for the diagnosis of DSM disorders
6) Questionnaire of eating and weight patterns
Evaluation
The evaluation of the patient with binge eating disorder includes the psychiatric, medical, and nutritional evaluation of the patient.
Psychiatric Status
Patients should have an evaluation for:
a) Psychiatric comorbidities (depression and substance abuse disorder)
b) Person image of body shape and weight
c) Self-esteem
Medical Status
Medical status evaluation should include comorbidities and parameters associated with obesity and excess body weight which are:
a) Waist circumference
b) Body mass index (measure height and weight)
c) Hypertension
d) Hyperlipidemia
e) Diabetes mellitus
f) Gastroesophageal reflux disease
g) Hepatobiliary disease
h) Coronary artery disease
i) Obstructive sleep apnea
j) Hypothyroidism
Nutritional Status
Assess the nutritional status of the person by asking:
a) Dieting and lifetime weight history
b) Physical activity and exercise
c) Current eating pattern and choice of food
d) Intensity and frequency of binge eating episodes
f) Types of overeating (overeating at meals, night eating, snacking, and grazing)
Treatment / Management
The type of treatment provided to binge eating disorder, treatment setting, and healthcare person involved in the therapy of patients with binge eating disorder depends upon treatment goals. Treatment goals may include working on:
1) Excessive body weight
2) Binge eating episodes
3) Extreme concern for body image
4) Comorbid psychiatric conditions (anxiety, substance use disorder, and depression)
Available treatment options for binge eating disorder include:
1) Psychotherapy
2) Pharmacotherapy
3) Weight loss treatment
1) Psychotherapy:
Psychotherapy is the first-line treatment option for binge eating disorder. According to several clinical trials, psychotherapy has a more significant clinical effect than pharmacotherapy. Common psychotherapy options are:
a) Cognitive-behavioral therapy
b) Interpersonal psychotherapy
c) Dialectical behavioral therapy
A) Cognitive Behavioral Therapy (CBT):
CBT is the psychotherapy of choice for binge eating disorder based on the results of several randomized controlled trials. The patient can receive CBT either from a clinician or through a self-help program without clinician involvement. Research shows that CBT has higher abstinence, is well-tolerated, and maintains remission for 1 or 2 years. A quick change in symptoms of patients with binge eating disorder is a good prognostic sign. Binge eating disorder patients with comorbid anorexia nervosa or bulimia nervosa do not respond well to CBT.[17]
Self-help based CBT is as effective for treating binge eating disorder as clinician-led CBT. Treatment settings have an effect on self-help based CBT. Delivering self-help based CBT in specialty settings, for example, eating disorder clinics, is more effective than delivering in a primary care setting. A self-help program focuses upon creating a regular pattern of eating, monitoring eating habits, learning self-control techniques, and learning problem solving more effectively. Hardcopy, web-based content, workbook, or smartphone application can be used to implement this program.[18][19] These materials provide:
i) Step by step approach to therapy
ii) Education regarding binge eating disorder.
B) Interpersonal Psychotherapy:
Interpersonal psychotherapy can take place in a group format or individual format. Psychotherapy does not focus on weight loss, but weight changes do occur due to stopping binge eating. It can also be provided in combination with CBT if the patient has complex psychopathology that may include interpersonal problems, low self-esteem, and perfectionism.[8][20][21] The following are the steps of the therapeutic strategy of psychotherapy:
i) Identify the area (most probably interpersonal area) that links to binge eating disorder.
ii) Focus mainly on experimentation or constructive changes in the problematic relevant regions (interpersonal) with little focus on binge eating.
C) Dialectical Behavioral Therapy:
Dialectical behavioral therapy consists of educating patients about the skills which are needed to manage problematic behavior associated with emotional dysregulation.[22] This therapy helps patients in balancing the dichotomous feelings, behavior, and thinking. The skills highlighted in this therapy include:
i) Watchful eating
ii) Emotional balance
iii) Tolerance of unpleasant circumstances
iv) Prevention of relapses
2) Pharmacotherapy:
Pharmacotherapy should be used as first-line therapy in patients who:
i) Do not have access to psychotherapy
ii) Decline psychotherapy
iii) Prefer medications
Medications that can be useful for binge eating disorder include:
i) Selective serotonin reuptake inhibitors (SSRIs) - sertraline, fluoxetine, fluvoxamine, escitalopram, citalopram
ii) Antiepileptic drugs - zonisamide and topiramate
iii) Attention deficit hyperactivity disorder (ADHD) medications - lisdexamfetamine, and atomoxetine)
iv) Medication for shift work disorder - armodafinil
v)
Selective serotonin reuptake inhibitors (SSRIs) should be the first-line pharmacotherapy for binge eating disorder. Antiepileptic medications or medications used for ADHD are an option if a patient fails one or two courses of SSRI. Randomized controlled trials have reported a promising role of topiramate, lisdexamfetamine, and methylphenidate in causing abstinence from binge eating disorder as well as in weight reduction. Limitations for using these medications have been due to the side effects of these medications. Topiramate can cause somnolence, paraesthesias, and cognitive impairment. Lisdexamfetamine and methylphenidate may cause anorexia, gastrointestinal disorder, headache, insomnia, sympathetic nervous system arousal, as well as dependence, and potential misuse.[23][24][25] Lisdexamfetamine is FDA-approved for the treatment of moderate to severe BED in adults aged 18 to 55.
3) Obesity or weight loss treatment: Most of the patients with binge eating disorder seek treatment for weight reduction rather than binge eating. All obese patients should be evaluated closely for binge eating disorder.[8]
i) Low and very low-calorie diet and exercise is the best option for losing weight. Behavioral weight loss therapy is a strategy designed to reduce binge eating as a result of weight loss indirectly. A randomized controlled trial concluded that behavioral weight loss therapy showed remission of binge eating disorder in 44 percent of patients. Moderate calorie restriction, exercise, and improved nutrition with nutritional counseling and rehabilitation are some of the specific components of behavioral weight loss therapy.
ii) Pharmacotherapy provides short-term weight loss in obese patients. Different classes of medications exert different clinical effects. Pharmacologic agents should be chosen based on patient preference, patient comorbidities, potential adverse effects, and insurance coverage, cost of medication of choice for obesity include:
a) Lorcaserin and liraglutide (daily injections)
b) Orlistat
c) Combination phentermine-extended release topiramate
d) Combination naltrexone-bupropion
e) Phenteramine
f) Benzphenteramine
g) Phendimetrazine
h) Diethylpropion
iii) Bariatric surgery can also be helpful for obese patients with binge eating disorder. Binge eating after bariatric surgery is associated with poor weight outcomes.
iv) Psychotherapy has no role in reducing weight in obese patients with binge eating disorder.
Differential Diagnosis
Diseases that come under the differential diagnosis of binge eating disorder are as follows:
Bulimia nervosa - Binge eating disorder differs from bulimia nervosa in that there is no compensatory behavior (laxative misuse, fasting, or self-induced vomiting) after eating to prevent weight gain
Anxiety disorder - Anxiety disorder also has associations with binge eating; however, the patient will only receive a diagnosis of binge eating disorder when binging episodes occur every week for three months
Kleine-Levin syndrome - Episodes of binges associated with excessive sleep
Mood disorder - Episodes of binges occur with other psychological features of mood disorder
Prognosis
Long-term outcome studies of binge eating disorder demonstrate that the prognosis of binge eating disorder is better than other eating disorders with a more favorable remission rate. The tendency of binge eating disorder to convert to other eating disorders is very small. Only a few studies have reported increased odds of migration to bulimia nervosa. Depressive symptoms and substance abuse are two significant adverse mental health outcomes of binge eating disorder.[26]
Binge eating disorder in childhood predicts excess weight gain in adolescent and young women. It also independently increased the risk of obesity-related complications, for example, metabolic syndrome.[27][28][29]
Complications
Most of the patients with binge eating disorder are obese. Binge eating disorder and obesity, most of the time, coexist and share complications.[4][30] The complications of these two disorders include:[31][32][33]
1) Muscular pain
2) Neck, shoulder, and lower back pain
3) Impairment resulting from physical health problems after adjustment of BMI
4) Hypertension
5) Diabetes
6) Asthma - respiratory illness
7) Coronary artery diseases and heart failure
8) Hyperlipidemia
9) Weight gain
10) Menstrual dysfunction (amenorrhea, oligomenorrhea)
11) Cortisol hormones disbalance (blunted cortisol response to stress test and decreased urinary cortisol levels)
12) Cancer (colon, breast, endometrial, gall bladder, and other)
13) Osteoarthritis
14) Sleep apnea
15) Obesity hypoventilation syndrome
16) Non-alcoholic fatty liver disease
17) Gallbladder disease
18) Metabolic syndrome
Deterrence and Patient Education
Patients should have counseling regarding the disorder and how to cope with binges. Awareness of binge episodes and knowledge of strategies for self-control help prevent the vicious cycle of binges-guilt-binges. Over-evaluating body shape and weight produce dysfunctional eating and dieting behavior, which causes physiological and psychological vulnerability to episodes of binge eating.[34] Patients should be told to:
i) Monitor eating patterns and keep a record of each meal, snacks, and trigger of binge episodes
ii) Identify triggers, which include under-eating, ingesting disinhibiting substances, breaking self or clinician created dietary rule system, or becoming dysphoric
iii) Create a pattern of eating with only three to four hours gap between meals. The patient should gradually implement the pattern
iv) Avoid places, activities, and people that trigger binge eating
v) Learn to solve a problem if causing binges by identifying the problem, generating multiple solutions, thinking through each solution, and choosing one problem at a time upon which to act
vi) Recognize food that leads to binge episodes
vii) Identify the single event that leads to episodes
viii) Weigh himself or herself once per week to avoid excessive weight checking or avoidance of weighing at all
Enhancing Healthcare Team Outcomes
The management of patients with binge eating disorder should be with the help of an interprofessional team, including a medical clinician, psychologist, psychiatrists, pharmacists, nutritionists, social workers, educational professionals, endocrinologists, and nurses. Counseling from nutritionists plays an essential role in organizing and planning meals as well as behavioral weight loss therapy for these patients.[35] As binge eating disorder is mostly associated with comorbid psychological conditions, the involvement of psychologists helps manage binge eating disorder. These patients should receive treatment in an outpatient setting.[22] Clinicians should be well trained in evaluating and managing patients with this disorder. Patient management can also include a self-help program.[21] Bariatric and psychiatric nurses are involved with patient and family education, monitoring of patients, and documentation for the team. Pharmacists evaluate prescribed medications for appropriateness, dosage, and drug interactions, and report any concerns to the rest of the team. These are but a few examples of interprofessional team collaboration that can improve patient outcomes. [Level 5]
Clinicians should be aware that patients with binge eating disorder are vulnerable to shame and stigma and find it distressing to share it with healthcare professionals. [36] The management and information should be tailored to the age and level of development. Healthcare professionals should also keep in mind to assess for signs of bullying, teasing, abuse, and neglect. Team members should address any misconception regarding binge eating disorder that the patients or their families might have. The clinician should communicate with the patient properly, and the patient's weight and appearance should be addressed with care. Patients with binge eating disorder require assessment promptly following the identification of the disorder.[37] The clinician and all interprofessional team members should show empathy, respect, and compassion, and provide suitable information for binging eating disorder and obesity.[38] Patient family members, guardians, teachers, and peers should also be encouraged to support the patient during treatment. Patient family members should also undergo assessment for eating disorder, and their mental health and practical support, and the team should offer emergency plans if the patient is at high risk of a psychiatric event.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Walsh BT, Sysko R. Broad categories for the diagnosis of eating disorders (BCD-ED): an alternative system for classification. Int J Eat Disord. 2009 Dec;42(8):754-64. [PMC free article: PMC2818502] [PubMed: 19650083]
- 2.
Wilfley DE, Citrome L, Herman BK. Characteristics of binge eating disorder in relation to diagnostic criteria. Neuropsychiatr Dis Treat. 2016;12:2213-23. [PMC free article: PMC5010172] [PubMed: 27621631]
- 3.
Sheehan DV, Herman BK. The Psychological and Medical Factors Associated With Untreated Binge Eating Disorder. Prim Care Companion CNS Disord. 2015;17(2) [PMC free article: PMC4560195] [PubMed: 26445695]
- 4.
Kornstein SG, Kunovac JL, Herman BK, Culpepper L. Recognizing Binge-Eating Disorder in the Clinical Setting: A Review of the Literature.
Prim Care Companion CNS Disord. 2016;18(3) [PMC free article: PMC5035811] [PubMed: 27733955]
- 5.
Hilbert A. Binge-Eating Disorder. Psychiatr Clin North Am. 2019 Mar;42(1):33-43. [PubMed: 30704638]
- 6.
Raevuori A, Lukkariniemi L, Suokas JT, Gissler M, Suvisaari JM, Haukka J. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016 Jun;49(6):542-52. [PubMed: 26875554]
- 7.
Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, de Graaf R, Maria Haro J, Kovess-Masfety V, O'Neill S, Posada-Villa J, Sasu C, Scott K, Viana MC, Xavier M. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013 May 01;73(9):904-14. [PMC free article: PMC3628997] [PubMed: 23290497]
- 8.
Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010 Jan;67(1):94-101. [PMC free article: PMC3757519] [PubMed: 20048227]
- 9.
Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007 Feb 01;61(3):348-58. [PMC free article: PMC1892232] [PubMed: 16815322]
- 10.
Schreiber LR, Odlaug BL, Grant JE. The overlap between binge eating disorder and substance use disorders: Diagnosis and neurobiology. J Behav Addict. 2013 Dec;2(4):191-8. [PMC free article: PMC4154572] [PubMed: 25215200]
- 11.
Dingemans A, Danner U, Parks M. Emotion Regulation in Binge Eating Disorder: A Review. Nutrients. 2017 Nov 22;9(11) [PMC free article: PMC5707746] [PubMed: 29165348]
- 12.
Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment.
Psychol Bull. 2011 Jul;137(4):660-681. [PMC free article: PMC3100657] [PubMed: 21574678]
- 13.
Schulte EM, Grilo CM, Gearhardt AN. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev. 2016 Mar;44:125-139. [PMC free article: PMC5796407] [PubMed: 26879210]
- 14.
McClure SM, Laibson DI, Loewenstein G, Cohen JD. Separate neural systems value immediate and delayed monetary rewards. Science. 2004 Oct 15;306(5695):503-7. [PubMed: 15486304]
- 15.
Balodis IM, Molina ND, Kober H, Worhunsky PD, White MA, Rajita Sinha, Grilo CM, Potenza MN. Divergent neural substrates of inhibitory control in binge eating disorder relative to other manifestations of obesity. Obesity (Silver Spring). 2013 Feb;21(2):367-77. [PMC free article: PMC3610836] [PubMed: 23404820]
- 16.
Himmerich H, Bentley J, Kan C, Treasure J. Genetic risk factors for eating disorders: an update and insights into pathophysiology.
Ther Adv Psychopharmacol. 2019;9:2045125318814734. [PMC free article: PMC6378634] [PubMed: 30800283]
- 17.
Sysko R, Hildebrandt T, Wilson GT, Wilfley DE, Agras WS. Heterogeneity moderates treatment response among patients with binge eating disorder. J Consult Clin Psychol. 2010 Oct;78(5):681-90. [PMC free article: PMC2948417] [PubMed: 20873903]
- 18.
Striegel-Moore RH, Wilson GT, DeBar L, Perrin N, Lynch F, Rosselli F, Kraemer HC. Cognitive behavioral guided self-help for the treatment of recurrent binge eating. J Consult Clin Psychol. 2010 Jun;78(3):312-21. [PMC free article: PMC2880824] [PubMed: 20515207]
- 19.
Lynch FL, Striegel-Moore RH, Dickerson JF, Perrin N, Debar L, Wilson GT, Kraemer HC. Cost-effectiveness of guided self-help treatment for recurrent binge eating. J Consult Clin Psychol. 2010 Jun;78(3):322-33. [PMC free article: PMC2880825] [PubMed: 20515208]
- 20.
Murphy R, Straebler S, Cooper Z, Fairburn CG.
Cognitive behavioral therapy for eating disorders. Psychiatr Clin North Am. 2010 Sep;33(3):611-27. [PMC free article: PMC2928448] [PubMed: 20599136]
- 21.
Wilfley DE, Agras WS, Telch CF, Rossiter EM, Schneider JA, Cole AG, Sifford LA, Raeburn SD. Group cognitive-behavioral therapy and group interpersonal psychotherapy for the nonpurging bulimic individual: a controlled comparison. J Consult Clin Psychol. 1993 Apr;61(2):296-305. [PubMed: 8473584]
- 22.
American Psychiatric Association. Treatment of patients with eating disorders,third edition. American Psychiatric Association. Am J Psychiatry. 2006 Jul;163(7 Suppl):4-54. [PubMed: 16925191]
- 23.
Vocks S, Tuschen-Caffier B, Pietrowsky R, Rustenbach SJ, Kersting A, Herpertz S. Meta-analysis of the effectiveness of psychological and pharmacological treatments for binge eating disorder. Int J Eat Disord. 2010 Apr;43(3):205-17. [PubMed: 19402028]
- 24.
Reas DL, Grilo CM.
Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity (Silver Spring). 2008 Sep;16(9):2024-38. [PMC free article: PMC3650491] [PubMed: 19186327]
- 25.
Brambilla F, Samek L, Company M, Lovo F, Cioni L, Mellado C. Multivariate therapeutic approach to binge-eating disorder: combined nutritional, psychological and pharmacological treatment. Int Clin Psychopharmacol. 2009 Nov;24(6):312-7. [PubMed: 19794312]
- 26.
Hilbert A, Bishop ME, Stein RI, Tanofsky-Kraff M, Swenson AK, Welch RR, Wilfley DE. Long-term efficacy of psychological treatments for binge eating disorder. Br J Psychiatry. 2012 Mar;200(3):232-7. [PMC free article: PMC3290797] [PubMed: 22282429]
- 27.
Schaumberg K, Welch E, Breithaupt L, Hübel C, Baker JH, Munn-Chernoff MA, Yilmaz Z, Ehrlich S, Mustelin L, Ghaderi A, Hardaway AJ, Bulik-Sullivan EC, Hedman AM, Jangmo A, Nilsson IAK, Wiklund C, Yao S, Seidel M, Bulik CM. The Science Behind the Academy for Eating Disorders' Nine Truths About Eating Disorders.
Eur Eat Disord Rev. 2017 Nov;25(6):432-450. [PMC free article: PMC5711426] [PubMed: 28967161]
- 28.
Franko DL, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, Herzog DB. A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. Am J Psychiatry. 2013 Aug;170(8):917-25. [PMC free article: PMC4120076] [PubMed: 23771148]
- 29.
Steinhausen HC. Outcome of eating disorders. Child Adolesc Psychiatr Clin N Am. 2009 Jan;18(1):225-42. [PubMed: 19014869]
- 30.
McCuen-Wurst C, Ruggieri M, Allison KC. Disordered eating and obesity: associations between binge-eating disorder, night-eating syndrome, and weight-related comorbidities. Ann N Y Acad Sci. 2018 Jan;1411(1):96-105. [PMC free article: PMC5788730] [PubMed: 29044551]
- 31.
Algars M, Huang L, Von Holle AF, Peat CM, Thornton LM, Lichtenstein P, Bulik CM. Binge eating and menstrual dysfunction. J Psychosom Res. 2014 Jan;76(1):19-22. [PMC free article: PMC3909535] [PubMed: 24360136]
- 32.
Rosenberg N, Bloch M, Ben Avi I, Rouach V, Schreiber S, Stern N, Greenman Y. Cortisol response and desire to binge following psychological stress: comparison between obese subjects with and without binge eating disorder. Psychiatry Res. 2013 Jul 30;208(2):156-61. [PubMed: 23083917]
- 33.
Lavagnino L, Amianto F, Parasiliti Caprino M, Maccario M, Arvat E, Ghigo E, Abbate Daga G, Fassino S. Urinary cortisol and psychopathology in obese binge eating subjects. Appetite. 2014 Dec;83:112-116. [PubMed: 25149200]
- 34.
Ely AV, Cusack A. The Binge and the Brain. Cerebrum. 2015 Sep-Oct;2015 [PMC free article: PMC4919948] [PubMed: 27358667]
- 35.
Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010 Feb 13;375(9714):583-93. [PubMed: 19931176]
- 36.
Becker AE, Hadley Arrindell A, Perloe A, Fay K, Striegel-Moore RH. A qualitative study of perceived social barriers to care for eating disorders: perspectives from ethnically diverse health care consumers.
Int J Eat Disord. 2010 Nov 01;43(7):633-47. [PMC free article: PMC3020364] [PubMed: 19806607]
- 37.
Treasure J, Nazar BP. Interventions for the Carers of Patients With Eating Disorders. Curr Psychiatry Rep. 2016 Feb;18(2):16. [PMC free article: PMC4718944] [PubMed: 26781554]
- 38.
Sim LA, McAlpine DE, Grothe KB, Himes SM, Cockerill RG, Clark MM. Identification and treatment of eating disorders in the primary care setting. Mayo Clin Proc. 2010 Aug;85(8):746-51. [PMC free article: PMC2912736] [PubMed: 20605951]
Eating disorder - compulsive overeating, treatment of psychogenic nervous overeating in Moscow
Everyone at least once got up from the table with a feeling of a full stomach. If this happens infrequently, then there is no cause for concern. If the episodes are repeated, or so you are trying to get rid of stress, bad mood, it is worth suspecting the development of a nervous eating disorder. Compulsive overeating, namely eating in uncontrollable sizes, repeated episodically. The disease often occurs against the background of mental disorders, sometimes contributes to gaining excess weight, obesity. Therapy is carried out by a psychiatrist, interacting with a nutritionist, a psychologist. nine0003
Article content:
- Disease description
- Symptoms
- Diagnostics
- Treatment
- Complications and neglected forms
Seek medical attention if symptoms occur. The information on the page is for reference only and cannot be used for self-diagnosis and self-treatment.
Nervous eating disorder - description of the disease
According to the Diagnostic and Statistical Manual of Mental Illness, psychogenic overeating (hyperphagic reaction to stress) is an independent disease that has a separate code 307.51. A patient with eating disorders is used to dealing with negative emotional stress, bouts of binge eating. The disease is manifested by a brutal appetite, which requires an abnormal amount of food with a high calorie content to satisfy it. Serious factors (loss of a family member, injury) and minor reasons - a raised voice, a missed bus, etc. can provoke a nervous attack. Nervous eating disorder is caused by mental causes, there is no physiology in a causal relationship. Food in this case is a tonic that allows you to forget about the problem for a while, to relax. The patient, who has experienced a nervous shock, does not try to feed the stomach, but to drown out the feelings. nine0003
It is important to distinguish between physiological hunger and appetite of a nervous nature. This is an important step towards recovery, selection of treatment:
| Nervous hunger | Physical hunger |
|---|---|
| May occur against the background of satiety, occurs unexpectedly and abruptly. | Develops gradually, the body does not require urgent saturation. |
| During attacks, the body requires unhealthy food - fast food, fatty foods, sweets, starchy foods, etc. are in priority. nine0040 | You can satisfy your appetite with any food, homemade and healthy food. |
| The portion size is much larger than usual, there is no control over the amount eaten. | A person eats exactly as much as needed to satisfy hunger. |
| The portion size is much larger than usual, there is no control over the amount eaten. | The physical need for food is disguised as a feeling of "sucking in the pit of the stomach", weakness. nine0040 |
| Feelings of guilt and shame arise after eating. | After eating, a feeling of satisfaction comes, strength appears. |
The causes of mental disorders can be genetic.
Compulsive eating disorder - symptoms
The basis of nervous overeating is the satisfaction of emotional needs, the solution of life problems, the ability to temporarily forget about loneliness, etc. However, food is a temporary salvation, after a short satisfaction comes a feeling of shame for weak willpower, guilt for the amount of food eaten. Eating disorder symptoms are often confused with other eating disorders. The symptoms of bulimia echo the clinical picture of compulsive overeating. nine0003
An eating disorder or compulsive overeating is accompanied by the following symptoms:
- food becomes the only way to get rid of melancholy, sadness and other negative emotions;
- ED patient prefers to eat alone, hiding bouts of binge eating;
- lack of satiety after a sufficient amount of food consumed;
- Stress causes regular overeating even when there is no physical need for food; nine0010
- a patient with eating disorders eats abnormally large portions in a short period of time;
- Gluttony aggravated during stress, emotional experiences.
The main manifestation of compulsive eating disorder is loss of control over appetite. Even with conscious overeating, a person cannot stop. A psychogenic disorder is more likely to affect people with an unstable psyche who take events to heart. At risk are teenagers and women. Men also suffer from eating disorders, but much less frequently and, unlike women, do not seek to part with negative eating habits, taking them for granted. nine0003
Diagnosis and treatment of psychogenic overeating
If you suspect nervous overeating, you should immediately seek help. You can make an appointment with a psychiatrist.
The Diagnostic and Statistical Manual of Mental Illness contains criteria, if 3 of them are met, the diagnosis of Eating Disorder - Binge Eating is confirmed:
- you prefer to eat alone;
- you experience discomfort from the amount eaten; nine0010
- you often sit down to eat when you don't feel hungry;
- after eating, guilt overcomes, self-loathing appears;
- regardless of the size of the portion you eat quickly, the food is not chewed thoroughly.
The doctor performs a control weighing, finds out what the patient's weight was in the recent past, how quickly the figure on the scales has changed. Then he selects the tactics of treatment in accordance with the anamnesis.
Treatment
Therapy of patients suffering from nervous overeating should be complex. Eating disorders are treated by a psychiatrist, psychotherapist, psychologist, nutritionist. The family doctor in this situation is not competent due to the lack of necessary knowledge and experience in the treatment of ED.
"CIRPP" specializes in the study, treatment of ED and adheres to complex tactics:
- drug therapy;
- psychotherapy effective for eating disorders; nine0010
- power restoration.
In the course of psychotherapy, individual and group methods are used, the main task of which is setting the right goals, teaching self-control, developing incentives, healthy beliefs.
Read more in the article:
Compulsive overeating: advice from a psychotherapist
Much attention in the treatment of eating disorders is given to nutrition, sometimes hospitalization is recommended. The clinic has created comfortable conditions for the treatment of patients, if necessary, emergency medical care is provided, an intensive care unit is provided. Usually, binge eating is treated on an outpatient basis. At first, support and control of loved ones at home is recommended. nine0003
To book an appointment with the Center for the Study of Eating Disorders in Moscow, call +7(499) 703-20-51 or use the online form.
Complications and neglected forms
An eating disorder (overeating) is fraught with the development of serious consequences - obesity and atherosclerosis. The patient experiences chronic emotional dissatisfaction, which leads to prolonged depression and causes suicidal thoughts.
Unless treated for destructive binge, there is a high risk of developing complications:
- Distance from relatives and family as the condition worsens, refusal of family dinners and friendly meetings. A person with eating disorders prefers a secluded lifestyle to hide behavioral deviations.
- Often a depressive state becomes the cause of addiction to alcohol and drugs. So the patient with ED tries to compensate for dissatisfaction with life.
- Compulsive nervous overeating affects health. Common complications include obesity, arthritis, high cholesterol, hypertension, and heart and kidney failure. The liver, gastrointestinal tract suffer from excessive uncontrolled nutrition, the character changes for the worse - irritability and anger prevail. nine0010
- Given the severity of complications, you should not postpone a visit to the doctor and self-medicate. Subject to timely treatment, the prognosis of therapy for compulsive disorder is favorable.
Make an appointment in Moscow by calling +7(499) 703-20-51 or fill out the online form. Psychiatrist, psychotherapist, narcologist. nine0170
Compulsive overeating
Another reason for extra pounds is overeating. People who have a disease like obesity overeat everything. Have you ever asked yourself why you are doing this?
It turns out that the main cause of compulsive overeating is a psychological disorder. That is, the problem here is not in your organ structure, not in some established traditions of overeating, but it is deep inside. Binge eating is just a reaction to the stress you are experiencing. If you still don't know if you have this problem, let's define its symptoms. nine0003
Overeating symptoms:
- repetitive binge eating disorder;
- your meal does not last long;
- you see your comfort in food;
- you eat in large quantities, while you are not hungry;
- you do not remember how much and what you ate;
- eating "to satiety";
- you are ashamed of the fact that you overeat.
Such overeating is also called emotional and, accordingly, the hunger that you experience is also emotional. How does a relapse situation usually occur? Some kind of problem happens to you, or you are not satisfied with the state of things, life itself is not satisfied, and you, sad from all this, go to the kitchen in the hope of consoling yourself there. As if food has become the only meaning of life. Or when you are in a bad mood and don’t know what to do with yourself and remember about the chocolate bar that is in your refrigerator and your soul immediately calms down. Do you recognize yourself? nine0003
Why is overeating dangerous?
Let's now determine what you risk by overeating each time. The main consequence, as you already understood, is obesity, which after itself creates a bunch of other consequences. These include high blood pressure, diabetes mellitus, affected joints and spine, circulatory problems, problems of the cardiovascular system, etc. And by the way, the life of an obese person is reduced by almost 50%.
What else does overeating lead to? In patients with this disease, metabolism is also disturbed. And another danger is associated with the pancreas. The fact is that when a person consumes a huge amount of food (and it’s far from healthy - this is one of the features of overeating), the pancreas is disrupted. She is unable to digest such an amount of food, as a result she "gives" us such a disease as pancreatitis. For those who don't know, pancreatitis is inflammation of the pancreas, which in turn can cause breathing problems. nine0003
How to treat overeating?
As a rule, the prognosis of the treatment of overeating is favorable. The main thing is that you yourself are interested in this. It will not be superfluous to go to a psychotherapist. And it’s best to immediately sign up for special programs for obese patients, where you will get rid of all your disorders.
Although we are confident that you can overcome your illness yourself. How to deal with overeating? Let's make a list of useful tips.
- First, identify the specific causes of your problem. Do you overeat because you are stressed, afraid of a problem, or out of boredom? Decide on this. nine0010
- So you've found the cause of your binge eating, now you need to target it. You must get rid of all your fears, self-doubt.
As a rule, people who have lost a lot of extra pounds immediately begin to feel in a new way: they immediately become more confident in themselves and feel comfortable among people. Therefore, maybe for you a slender body will be the solution to all problems?
- If you suffer from the syndrome of flight from all problems, deal with it in the same way. It is much easier to solve the problem than to suffer later, knowing how many unresolved cases you have. nine0010
- If you are depressed, find the cause. In the end, change your life: go to another country, sign up for some creative or sports section. There you will find people who will certainly revive the love of life in you.
If you feel that you cannot cope with all the problems alone, then do not be shy, talk to friends, parents, make an appointment with a psychotherapist, if it makes you feel better. The main thing is not to sit still and fight your problem, because postponing treatment for later, we lose so many days of life, so many minutes of emotions that we will regret it all our lives later.