Best time of day to take cymbalta for fibromyalgia
Treating Fibromyalgia With Cymbalta: Side Effects, Benefits
Written by Kelli Miller
Medically Reviewed by David Zelman, MD on February 12, 2022
In this Article
- What Is Cymbalta?
- How Does Cymbalta Work?
- How Do You Take Cymbalta?
- Benefits of Cymbalta
- Side Effects
- Risks and Warnings
- Drug Interactions
- Before You Take Cymbalta
- Who Should Not Take Cymbalta?
Fibromyalgia is a perplexing and often disabling disorder that affects millions of Americans. However, new treatments are offering hope to those living with the pain of fibromyalgia. Cymbalta is a medication approved to manage the unique symptoms of fibromyalgia. Is this medicine right for you? Here is what you need to know, from the pros and cons to who should -- and should not -- take this drug.
What Is Cymbalta?
Cymbalta (duloxetine) is an antidepressant used for the treatment of fibromyalgia. Fibromyalgia is a chronic disorder that causes widespread muscle pain and tenderness, trouble sleeping, and overwhelming tiredness.
Cymbalta belongs to a class of medications called serotonin and norepinephrine reuptake inhibitors (SNRIs). The FDA previously approved Cymbalta for the treatment of depression, generalized anxiety disorder, and diabetic peripheral neuropathic pain. The agency approved Cymbalta for the management of fibromyalgia in adults in June 2008.
A similar medication, called Savella (milnacipran), gained FDA approval in early 2009.
How Does Cymbalta Work?
Scientists are not exactly certain how Cymbalta helps make patients with fibromyalgia feel better; fibromyalgia itself is poorly understood. Many believe the pain is due to changes in the nervous system which cause nerve cells to fire off too many signals along pain pathways. This makes a person overly sensitive to things that would normally not be painful.
Researchers think that Cymbalta helps calm down these pain signals by increasing the level of two naturally occurring substances called serotonin and norepinephrine. These substances, which are found in the brain and other parts of the nervous system, can affect mood and are believed to help control and suppress feelings of pain. Cymbalta and other SNRIs block serotonin and norepinephrine from re-entering cells, and therefore increase the levels of these substances. This process is thought to improve mood and relieve pain in patients with fibromyalgia.
These substances, which are found in the brain and other parts of the nervous system, can affect mood and are believed to help control and suppress feelings of pain. Cymbalta and other SNRIs block serotonin and norepinephrine from re-entering cells, and therefore increase the levels of these substances. This process is thought to improve mood and relieve pain in patients with fibromyalgia.
How Do You Take Cymbalta?
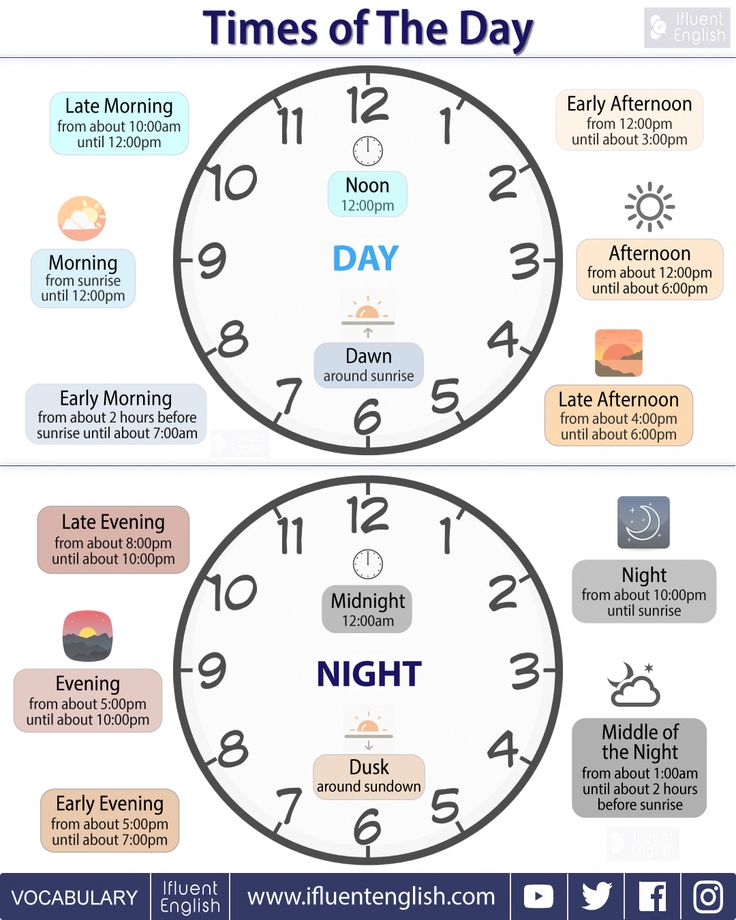
Cymbalta is a capsule that you take by mouth once a day. The recommended dose is 60 milligrams a day. However, your doctor will likely tell you to take 30 milligrams a day for the first week, before increasing you to the full dose. It is important to keep in mind that there is no evidence to suggest that taking more than 60 milligrams a day will further reduce your pain. In fact, doing so increases your chances of side effects.
If the medicine upsets your stomach, you can try taking it with a meal or some crackers. You should not drink alcohol when taking Cymbalta.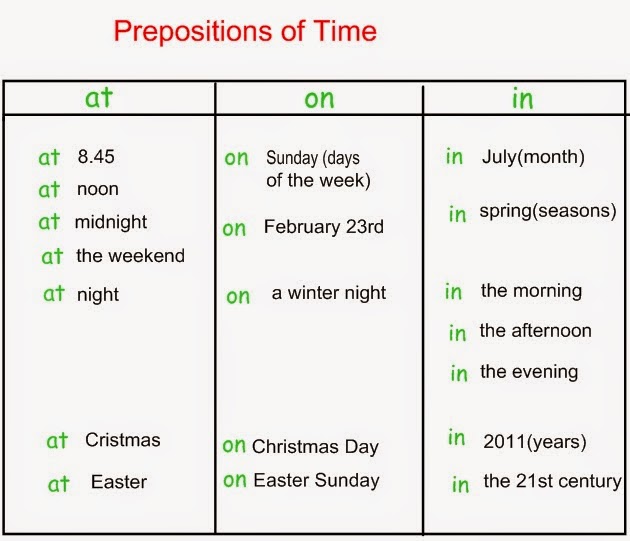 Doing so can increase your risk of liver damage.
Doing so can increase your risk of liver damage.
If you miss a dose, you should take it as soon as you remember -- unless it is close to the time when you are supposed to take the next one. If so, skip the missed dose, and go back to your regular medication schedule. Never double your dose to catch up.
You should not suddenly stop taking this medicine. Doing so may cause unpleasant side effects, including nausea and headache. If you wish or need to stop taking Cymbalta, your doctor will tell you how to reduce your dose gradually over time.
Benefits of Cymbalta
In clinical trials, Cymbalta significantly and quickly improved pain. More than half of the patients with fibromyalgia said they felt much better within one week. Pain relief may be greater in patients who also have existing depression, although those without depression also have a significant improvement in symptoms.
Other benefits of Cymbalta:
- Pain relief is proven to be significant for at least three months of treatment.
 However treatment should be based on your individual response.
However treatment should be based on your individual response. - Less pain allows you to get back to your daily routine.
- Better sleep leads to improved quality of life.
- More refreshing sleep may allow muscle tissues to heal.
Also, SNRIs often have less bothersome side effects than tricyclic antidepressants (such as amitriptyline), which are sometimes prescribed to those with fibromyalgia.
Side Effects
The most common side effects for Cymbalta are:
- Constipation
- Dry mouth
- Nausea
Other side effects that may occur include:
- Decreased appetite (may include anorexia)
- Decreased sex drive
- Drowsiness or sleepiness
- Increased sweating
- Jitters, nervousness, or restlessness (agitation)
- Urinary hesitation
You may feel dizzy upon standing when you first start taking Cymbalta or when your dose is increased. This is due to a drop in blood pressure, and is known as orthostatic hypotension. Your health care provider may want to check your blood pressure from time to time while you are taking Cymbalta.
Your health care provider may want to check your blood pressure from time to time while you are taking Cymbalta.
Risks and Warnings
Cymbalta and other antidepressants may increase the risk for suicidal thoughts and behaviors in people under age 24. After you are prescribed Cymbalta, your doctor will monitor you closely for unusual behavior changes, new or worsening signs of depression, or suicidal thoughts.
Cymbalta may cause a drop in salt (sodium) levels in the blood, a potentially life-threatening condition called hyponatremia. Older adults, particularly those who take diuretics ("water pills") are more likely to develop this complication. Hyponatremia can cause headaches, confusion, weakness, and in severe cases can lead to fainting, seizures, coma, and death.
Some patients taking Cymbalta have developed liver problems. In rare cases, this has lead to liver failure and death. Contact your health care provider immediately if you develop any of the following symptoms while taking Cymbalta:
- Dark colored urine
- Itching
- Pain in the right, upper belly area
- Unexplained flu-like symptoms
- Yellow skin or eyes (jaundice)
Drug Interactions
In rare cases, a life-threatening condition called serotonin syndrome has occurred in patients who have taken Cymbalta.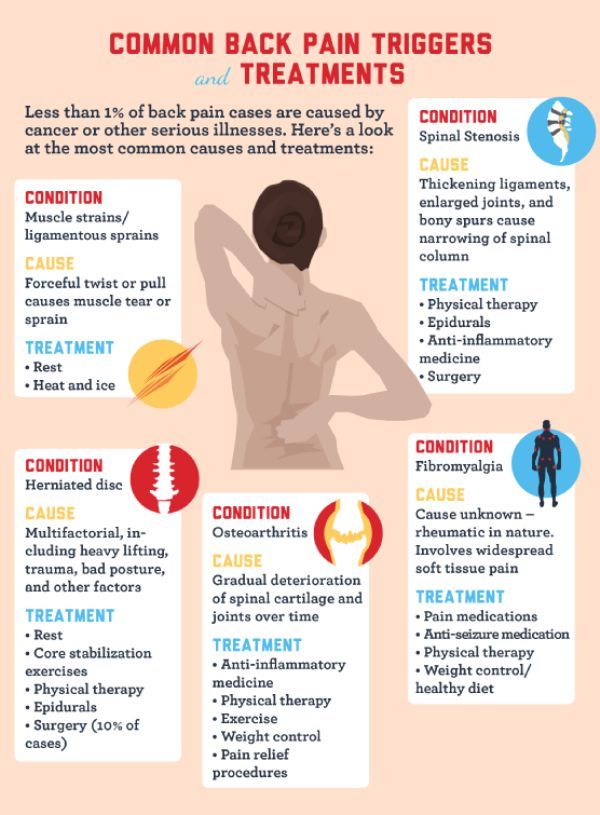 Serotonin syndrome most often results when someone takes two or more medications that increase the body's serotonin levels at the same time. You need serotonin for your brain and nerve cells to function, but too much of it can be dangerous. Serotonin syndrome can lead to rapid changes in blood pressure, muscle rigidity, seizures, and even death.
Serotonin syndrome most often results when someone takes two or more medications that increase the body's serotonin levels at the same time. You need serotonin for your brain and nerve cells to function, but too much of it can be dangerous. Serotonin syndrome can lead to rapid changes in blood pressure, muscle rigidity, seizures, and even death.
This is why it is so important that your health care providers know what medications you are taking. Always tell them about all the medicines you take, including over-the-counter drugs and herbs and supplements.
Drugs that may interact with Cymbalta and cause serotonin syndrome include:
- Cough medicines that contain dextromethorphan
- Monoamine oxidase inhibitors (MAOIs)
- Nausea and heartburn medications such as metoclopramide (Reglan) and ondansetron (Zofran)
- Pain medications, including meperidine (Demerol, a painkiller) and tramadol (Ultram)
- St. John's wort
- Triptans, used to treat migraine headaches
Other drugs may also interact with Cymbalta, including:
- Blood thinners, including warfarin, aspirin, and nonsteroidal anti-inflammatory drugs (NSAIDs).
 Taking Cymbalta with such medications may increase your chances for bleeding events.
Taking Cymbalta with such medications may increase your chances for bleeding events.
Before You Take Cymbalta
Tell your doctor about any other medical conditions you may have. The drug should be prescribed with caution in those who have:
- A history of seizures or mania
- Conditions that slow gastric emptying (sometimes occurs in those with diabetes)
- Diabetes (Cymbalta may affect blood sugar levels)
- High blood pressure or heart disease
- Liver disease
- Kidney disease
Who Should Not Take Cymbalta?
You should not take Cymbalta if you:
- Are taking a medication called thioridazine
- Are taking a medicine called MAOI or have used one in the last 14 days
- Have uncontrolled narrow-angle glaucoma
In animal studies Cymbalta has demonstrated adverse effects on a developing fetus. No adequate or well-controlled studies of the drug have been performed in pregnant or breastfeeding women. Women who are breastfeeding, pregnant, or planning to become pregnant should talk to their doctor about whether or not Cymbalta is right for them. You should only take Cymbalta if the benefits outweigh the risks.
Women who are breastfeeding, pregnant, or planning to become pregnant should talk to their doctor about whether or not Cymbalta is right for them. You should only take Cymbalta if the benefits outweigh the risks.
Fibromyalgia Guide
- Overview & Facts
- Symptoms & Signs
- Treatment & Care
- Living With Fibromyalgia
Cymbalta for Fibromyalgia: Does it Work?
For anyone living with fibromyalgia, having a healthcare provider suggest an antidepressant may come as a surprise.
But duloxetine (Cymbalta) is approved by the Food and Drug Administration (FDA) to help fibromyalgia patients cope with joint and muscle pain, fatigue, sleep disturbance, and other symptoms.
Since Cymbalta is more commonly prescribed for the treatment of depression and anxiety, it’s natural to wonder how it also works for fibromyalgia.
While you should always discuss any treatment option with your doctor, this article will help you understand more.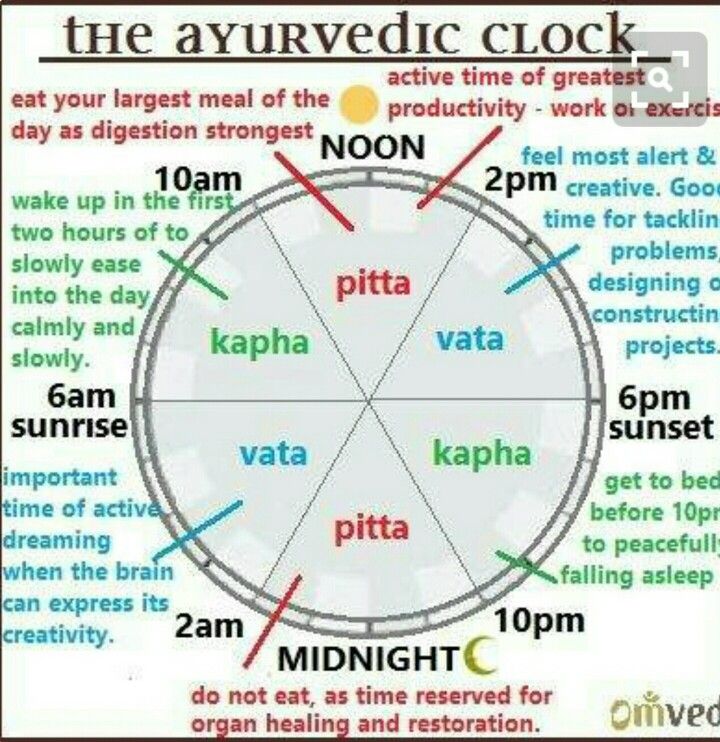 First we’ll cover how Cymbalta works and if it helps with pain relief.
First we’ll cover how Cymbalta works and if it helps with pain relief.
Then we’ll discuss other uses of Cymbalta, its adverse effects and standard dosage, and other medications that help treat fibromyalgia.
How Does Cymbalta Work?
The underlying cause of fibromyalgia is difficult to understand, but research suggests the condition is caused by excessive nerve stimulation.
The brain’s pain receptors become overstimulated and sensitive.
This can cause you to feel pain or more intense pain in parts of your body even when nothing is causing discomfort.
Cymbalta is a serotonin-norepinephrine reuptake inhibitor (SNRI). It helps levels of the neurotransmitters norepinephrine and serotonin remain higher in the brain by blocking their reabsorption.
People who have fibromyalgia often have low levels of these neurotransmitters, or their brains ineffectively use them.
Norepinephrine and serotonin play a role in the perception of pain, so increasing their levels is thought to dampen the pain response.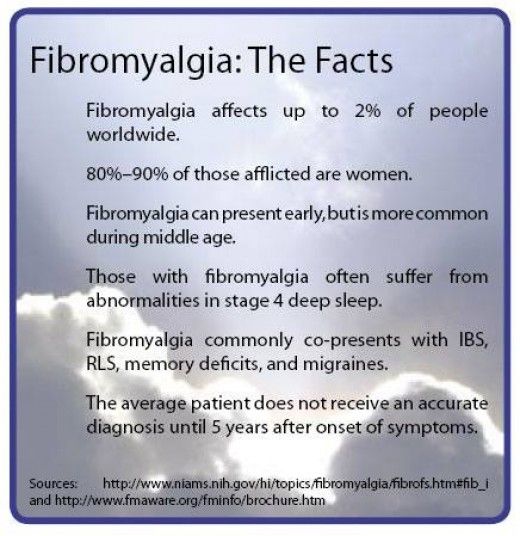
Have questions about fibromyalgia? Talk to a doctor through K Health.
Get StartedCan Cymbalta Reduce Fibromyalgia Pain?
Many clinical trials indicate that Cymbalta effectively reduces fibromyalgia pain and also helps improve sleep and quality of life.
According to animal studies, duloxetine reduces two pain types associated with fibromyalgia: hyperalgesia and allodynia. Hyperalgesia means someone is overly sensitive to pain—smaller discomforts feel like more significant pains to them.
Allodynia is when things that aren’t typically considered painful (like light pressure from brushing your hair or gently rubbing a cotton swab over your skin) feel bothersome and uncomfortable.
Other Uses for Cymbalta
In addition to fibromyalgia, Cymbalta is approved by the FDA to treat the following disorders:
- Major depressive disorder
- Generalized anxiety disorder
- Chronic musculoskeletal pain
- Diabetic peripheral neuropathy
Side Effects of Cymbalta
Most side effects of Cymbalta are usually minor and go away over time.
The most common potential side effects associated with Cymbalta are:
- Nausea
- Dry mouth
- Drowsiness
- Constipation
- Decreased appetite
- Increased sweating
Other potential adverse events include:
- Headache
- Fatigue
- Diarrhea
- Insomnia
- Dizziness
- Abdominal pain
- Sexual side effects such as decreased sex drive
If you experience any of the following more serious side effects, contact your doctor immediately:
- High fever
- Flu-like symptoms
- Dark urine
- Rapid heartbeat
- Seizures
- Hallucinations
- Confusion
- Unusual blisters/peeling skin
- Vomiting
- Intense mood swings
- Changes in vision
- Suicidal thoughts
Cymbalta Precautions
Just like other antidepressants, Cymbalta carries a black box warning indicating that there is increased risk of developing worsening depression, suicidal thinking and behavior.
This occurs most often in children, adolescents, and young adults, but can happen to anyone.
If you or your loved ones are taking this medication or any antidepressant, watch out for the following warning signs that will require immediate medical attention:
- Unusual changes in behavior
- Worsening symptoms of depression including hopelessness, feeling of worthlessness
- Increase in conversations about death
- Thoughts or talk of self-harm
If any of the above symptoms occur, it’s important to seek immediate medical attention.
Cymbalta is not safe for some people with certain medical conditions or who are taking certain medications. Contraindications include:
- Hypersensitivity or allergy to any ingredients in Cymbalta
- MAO inhibitor use within the prior 14 days, such as linezolid or methylene blue
- Severe kidney disease
- Liver disease, including cirrhosis
- Uncontrolled narrow-angle glaucoma
- Alcohol abuse
- Low sodium caused by syndrome of inappropriate ADH secretion (SIADH)
Caution is advised if the following conditions exist:
- Bleeding disorders or current use of NSAIDs, aspirin, or other anticoagulant use
- Hypertension on current blood pressure- medications
- Arrhythmia
- Heart disease
- Diabetes
- Seizure disorder
- Bipolar disorder
- Use of other antidepressant medications, pain medications, herbal remedies.

There are other conditions that can predispose to unsafe side effects of any medication, including Cymbalta.
Discuss your medical history and current medications, including over the counter medications, with your healthcare provider, so that the safest decisions on your treatment plan can be made.
Cymbalta Dosage for Fibromyalgia
The dosage of Cymbalta for the treatment of fibromyalgia typically begins at 30 milligrams (mg) a day for a week. Depending on how an individual responds to this, doctors typically increase the dosage to 60 mg daily.
Dosages higher than 60 mg a day provide no additional benefit and instead increase the risk of more serious side effects.
Never suddenly stop taking Cymbalta or discontinue the drug without speaking to your healthcare provider. If you suddenly stop taking the drug, you could experience withdrawal symptoms.
Other Medications that Treat Fibromyalgia
Cymbalta isn’t the only option to treat and help manage fibromyalgia.
Other treatment options include:
- Other SNRI: ilnacipran (Savella) and off-label use of venlaxafine (Effexor)
- Anti-seizure drugs: Gabapentin (Neurontin) and pregabalin (Lyrica) have FDA approval to treat the pain of fibromyalgia.
- Pain relievers: Prescription medication pain relievers like tramadol (Ultram) or over-the-counter (OTC) pain relievers like ibuprofen (Advil, Motrin) and acetaminophen (Tylenol) can also help manage pain.
Have questions about fibromyalgia? Talk to a doctor through K Health.
Get StartedWhen to See a Doctor
Contact your doctor if you take Cymbalta for fibromyalgia and:
- Your symptoms of fibromyalgia worsen
- You forget to take a dose of Cymbalta
- You are interested in switching your medication
Seek immediate medical care if you start to experience any of the more serious side effects of Cymbalta (such as hallucinations, high fevers, and intense mood swings).
If you’re having a mental health emergency, call 911 or go to the nearest emergency room. You can also get free 24/7 support from a suicide and crisis expert by calling or texting 988. If you’d prefer to chat online, you can chat with a suicide and crisis expert by visiting the Lifeline Chat.
How K Health Can Help
Think you might need a prescription for Cymbalta (Duloxetine)?
K Health has clinicians standing by 24/7 to evaluate your symptoms and determine if Cymbalta is right for you.
Get started by checking your symptoms and connecting with a medical professional.
Frequently Asked Questions
How long does it take Cymbalta to work for fibromyalgia?
Cymbalta is recommended as a first-line treatment for fibromyalgia. Many patients report improvements in pain within a week of starting the drug.
Many patients report improvements in pain within a week of starting the drug.
When is the best time to take Cymbalta for fibromyalgia?
There is no hard and fast rule for the best time to take Cymbalta. What matters most is taking the prescription at the same time every day. However, if you feel the prescription drug makes you drowsy, it’s best to take the medication in the evening.
Does Cymbalta help with fibro fatigue?
Cymbalta should help with fibro fatigue. Since it eases fibromyalgia pain, it likely will also lessen fibro fatigue.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
Always talk to your doctor about the risks and benefits of any treatment.
K Health has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
-
CYMBALTA (Duloxetine Delayed-Release Capsules) for Oral Use. (2004).
https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021427s049lbl.pdf -
Cymbalta for Fibromyalgia Pain - Predictive Value of Small Fiber Changed.
 (2019).
(2019).
https://clinicaltrials.gov/ct2/show/NCT01619566 -
Duloxetine for the Treatment of Fibromyalgia. (2011).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056054/ -
Efficacy of Duloxetine in Patients With Fibromyalgia: Pooled Analysis of 4 Placebo-Controlled Clinical Trials.
 (2009).
(2009).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2781036/ -
Fibromyalgia. (2020).
https://www.cdc.gov/arthritis/basics/fibromyalgia.htm -
The Local and Systemic Actions of Duloxetine in Allodynia and Hyperalgesia Using a Rat Skin Incision Pain Model.
 (2015).
(2015).
https://pubmed.ncbi.nlm.nih.gov/26049779/ -
A Study of Duloxetine in Fibromyalgia. (2015).
https://clinicaltrials.gov/ct2/show/NCT01552057
Fibromyalgia - treatment, symptoms, causes, diagnosis
Fibromyalgia is a chronic disease characterized by pain, stiffness and soreness of the muscles, tendons, and joints. Fibromyalgia is also characterized by sleep disturbance, chronic fatigue, depression, anxiety, and bowel dysfunction. Fibromyalgia is sometimes called fibromyalgic syndrome or fibrositis.
Fibromyalgia is also characterized by sleep disturbance, chronic fatigue, depression, anxiety, and bowel dysfunction. Fibromyalgia is sometimes called fibromyalgic syndrome or fibrositis.
Although fibromyalgia is one of the most common diseases affecting muscles, the cause is still unknown. Tissues that are a source of pain are not accompanied by inflammation of this tissue. And therefore, pain, which causes a lot of inconvenience for the patient, does not lead to irreversible changes and destruction of tissues. In addition, there is no damage to internal organs. In this regard, fibromyalgia differs from rheumatic diseases such as rheumatoid arthritis, SLE, or polymyositis. In these diseases, inflammation of the tissues occurs - this is the main cause of pain, stiffness, soreness in the joints, tendons and muscles, and, in addition, damage to both tissues and internal organs occurs.
Causes
The cause of fibromyalgia is unknown. Fibromyalgia patients experience pain in response to stimuli that are not normally perceived as painful. Studies have shown that patients with fibromyalgia have elevated levels of a neurotransmitter (called substance P) and nerve growth factor in their cerebrospinal fluid. In addition, patients with fibromyalgia have reduced levels of serotonin in the brain. A study of pain in fibromyalgia suggested hypersensitivity of the central nervous system. Scientists have also noted disturbances in pain perception in patients with fibromyalgia.
Studies have shown that patients with fibromyalgia have elevated levels of a neurotransmitter (called substance P) and nerve growth factor in their cerebrospinal fluid. In addition, patients with fibromyalgia have reduced levels of serotonin in the brain. A study of pain in fibromyalgia suggested hypersensitivity of the central nervous system. Scientists have also noted disturbances in pain perception in patients with fibromyalgia.
In addition, patients with fibromyalgia reported a decrease in slow eye movements during sleep (which partly explains the feeling of fatigue after sleep or frequent awakenings). The debut of fibromyalgia is often associated with a psychological factor, trauma or infection.
Who is prone to fibromyalgia
Fibromyalgia affects mainly women (up to 80% women suffer) aged 35 to 55 years. Much less frequently, fibromyalgia occurs in men, children, and the elderly. The disease may appear on its own or be associated with other diseases such as SLE or rheumatoid arthritis.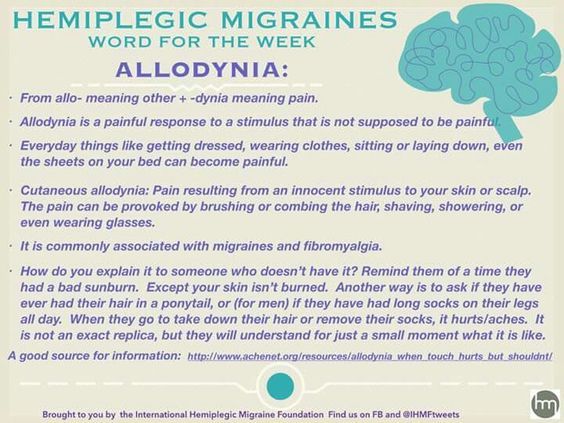 The prevalence of this disease varies from country to country. For example, in Sweden and Great Britain 1% and in the USA - 4%.
The prevalence of this disease varies from country to country. For example, in Sweden and Great Britain 1% and in the USA - 4%.
Symptoms
The universal symptom of fibromyalgia is, of course, pain. As mentioned above, fibromyalgia pain is not caused by tissue inflammation. Instead, patients seem to have hypersensitivity to various sensory stimuli and an unusually low pain threshold. Minor sensory stimulations that do not usually cause great distress to other people can be significant and disruptive in patients with fibromyalgia.
Fibromyalgia pain can be in different parts of the body, and on both sides. Most often, pain occurs in the neck, buttocks, shoulders, in the chest, in the upper body. Sensitive zones are limited areas where there is increased sensitivity.
Fatigue occurs in 90% of patients. Fatigue may be associated with pathological disturbances in sleep phases, which is often observed in these patients. Normally, there are several levels of sleep depth. A person needs to be in a deep stage of sleep for a longer time in order to restore the body's strength. Fibromyalgia patients lack a deep, restorative level of sleep (called the slow eye movement stage). As a result, patients wake up in the morning feeling tired and with heaviness in the muscles and a feeling of lack of sleep (although the number of hours of sleep was sufficient).
A person needs to be in a deep stage of sleep for a longer time in order to restore the body's strength. Fibromyalgia patients lack a deep, restorative level of sleep (called the slow eye movement stage). As a result, patients wake up in the morning feeling tired and with heaviness in the muscles and a feeling of lack of sleep (although the number of hours of sleep was sufficient).
Mental or emotional problems occur in more than half of patients with fibromyalgia. These disorders include poor concentration, impaired fixation memory, irritability, and depressed mood. And due to the fact that the diagnosis of fibromyalgia is difficult to verify, such patients are often diagnosed with depression.
Other symptoms of fibromyalgia may include migraine headaches or tension headaches, various sensations of numbness or tingling in various parts of the body. In addition, there may be discomfort in the abdomen (spasmodic bowel) irritated bladder (frequent sometimes painful urination). But the examination does not show signs of inflammation in the intestines or bladder. Each patient with fibromyalgia is unique in their own way, and symptoms can occur in various combinations.
But the examination does not show signs of inflammation in the intestines or bladder. Each patient with fibromyalgia is unique in their own way, and symptoms can occur in various combinations.
Diagnosis
There are no tests or x-rays to support the diagnosis of fibromyalgia. Tests and examinations are prescribed to rule out other diseases. The diagnosis of fibromyalgia is based on the history of the disease and physical examination findings. In patients with chronic pain, the diagnosis of fibromyalgia can be made based on the detection of tender points (up to 80% of cases), the presence of tissue inflammation and the exclusion of other diseases. Many diseases have symptoms similar to fibromyalgia. For example, these are diseases such as:0003
- Low thyroid hormone levels (hypothyroidism),
- Vitamin D deficiency
- Increased function of the parathyroid glands (causes an increase in the level of calcium in the blood),
- Muscle diseases accompanied by muscle pain (polymyositis),
- Bone disorders, with bone pain (Paget's disease),
- Increased blood calcium level (hypercalcemia),
- Infectious diseases (hepatitis, Epstein-Bar virus, AIDS),
- Oncological diseases.
Although blood tests do not confirm fibromyalgia, they are essential for the differential diagnosis. Therefore, it is necessary to do blood tests for thyroid hormones, the level of calcium in the blood (to rule out hypercalcemia, hyperparathyroidism, hypothyroidism). Alkaline phosphatase levels are often elevated in patients with Paget's disease. Creatine phosphokinase is often elevated in patients with polymyositis. A detailed blood test and blood biochemistry allows diagnosing hepatitis.
Fibromyalgia may present on its own or in association with systemic rheumatic diseases. In systemic rheumatological diseases (SLE, rheumatoid arthritis, polymyositis), inflammation and damage to various tissues and organs occurs. For the diagnosis of these diseases, such analyzes as ESR plasma protein levels, antinuclear factor, C reactive protein, sialic acid are important. With fibromyalgia, these tests are within the normal range.
Treatment
Because the symptoms of fibromyalgia vary greatly from patient to patient, treatment programs must be personalized for each patient. Fibromyalgia treatment programs are most effective when combined with pharmacological and non-pharmacological treatments.
Fibromyalgia treatment programs are most effective when combined with pharmacological and non-pharmacological treatments.
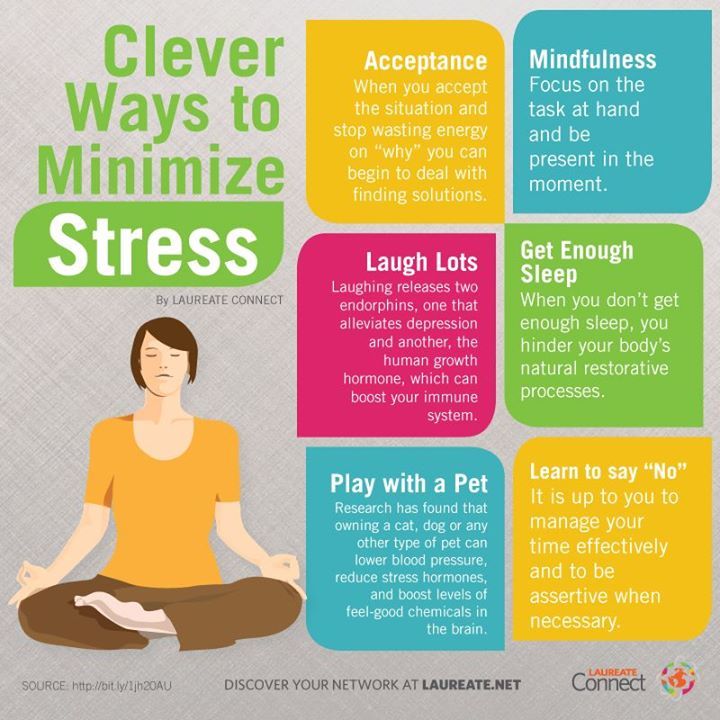
Stress reduction
It is practically impossible to measure stress levels in different patients. For some people, spilled milk on the table is almost a tragedy. And for others, even if the tank drives into the room, there will be no concern. A good effect for reducing stress is given by biofeedback and relaxation techniques. Sometimes, changes in environmental factors (such as noise, temperature, weather changes) are enough to increase the symptoms of fibromyalgia. And the impact on these factors can have a positive impact. Optimal amount of sleep is very helpful.
Exercise therapy
Low-intensity physical activity such as swimming, cycling, walking Especially beneficial in the morning. The mechanism by which exercise influences fibromyalgia is not known. One factor may be improved sleep (prolongation of REM sleep).
Diet
There is no specific diet for the treatment of fibromyalgia.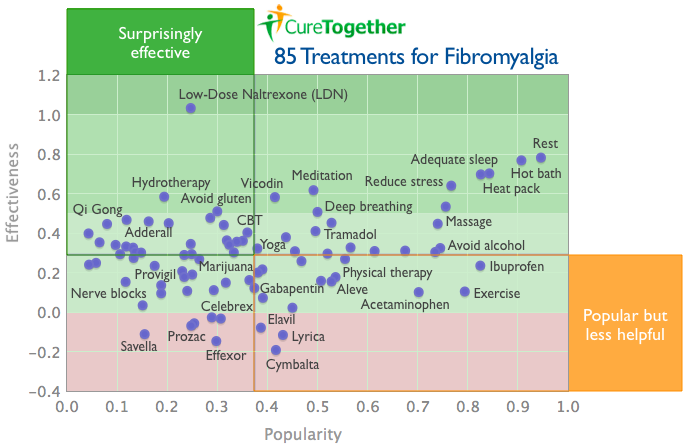 It is recommended to avoid drinking alcohol and coffee in the evening in order to improve sleep. In the presence of irritable bowel syndrome, it is necessary to avoid products that provoke violations of the gastrointestinal tract.
It is recommended to avoid drinking alcohol and coffee in the evening in order to improve sleep. In the presence of irritable bowel syndrome, it is necessary to avoid products that provoke violations of the gastrointestinal tract.
Drug treatment
Traditionally, tricyclic antidepressants, commonly used to treat depression, have been considered the most effective. In the treatment of fibromyalgia, tricyclic antidepressants are used at dosages several times lower than in the treatment of depression. Tricyclic antidepressants relieve fatigue to some extent, reduce muscle pain, and improve sleep. Science believes this is due to a change in the levels of a neurotransmitter called serotonin. A tricyclic antidepressant is, for example, amitriptyline or doxepin. Practice has shown that the combination of drugs such as fluoxetine (Prozac) with a reduced dose of amitriptyline increases the reduction of symptoms, improves sleep and well-being. But these drugs unfortunately have side effects.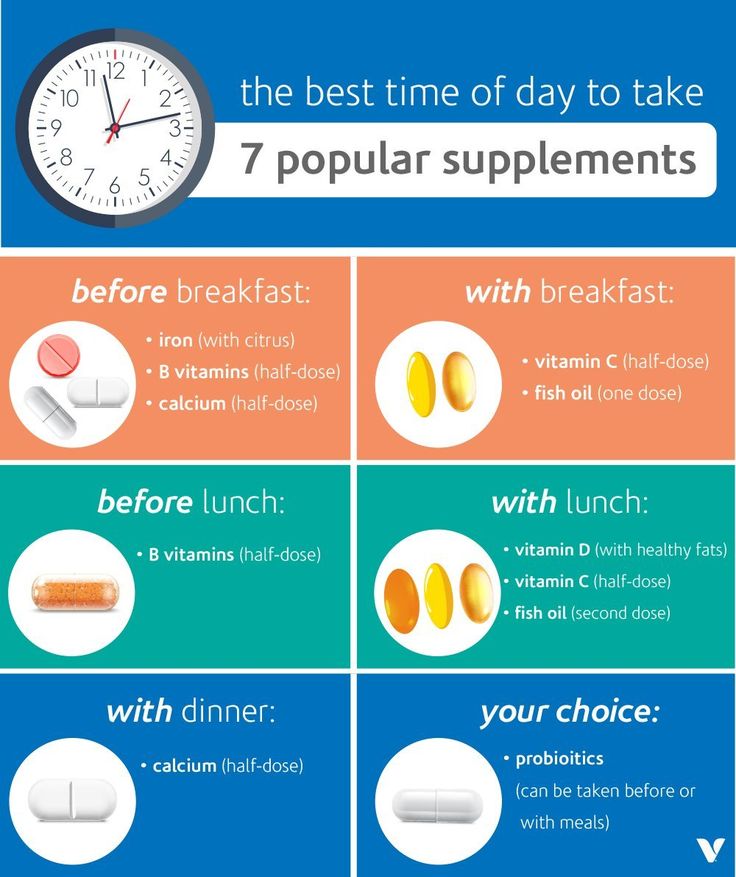 In 2007, a drug called Lyrica (pregabalin) was synthesized and it was the first drug designed specifically for fibromyalgia. Lyrica significantly reduces pain in patients with fibromyalgia. Moreover, the drug has a wide therapeutic range (allows you to choose the dosage depending on the symptoms). Another drug called Neurontin (gabapentin) has a similar effect. And more recently, drugs have been synthesized that instantly increase the level of two neurotransmitters in the brain (serotonin and norepinephrine). These drugs are duloxetine (Cymbalta) and milnacipran (Savella).
In 2007, a drug called Lyrica (pregabalin) was synthesized and it was the first drug designed specifically for fibromyalgia. Lyrica significantly reduces pain in patients with fibromyalgia. Moreover, the drug has a wide therapeutic range (allows you to choose the dosage depending on the symptoms). Another drug called Neurontin (gabapentin) has a similar effect. And more recently, drugs have been synthesized that instantly increase the level of two neurotransmitters in the brain (serotonin and norepinephrine). These drugs are duloxetine (Cymbalta) and milnacipran (Savella).
In addition to antidepressants, NSAIDs are often prescribed for fibromyalgia. But their effectiveness is not as obvious as in rheumatological conditions.
Massage and acupuncture often have some effect in the treatment of fibromyalgia.
Treatment of fibromyalgia in Nizhny Novgorod
Fibromyalgia syndrome has been and remains one of the most mysterious and problematic in terms of diagnosis and definition of this condition, the mechanisms of its formation, approaches to treatment.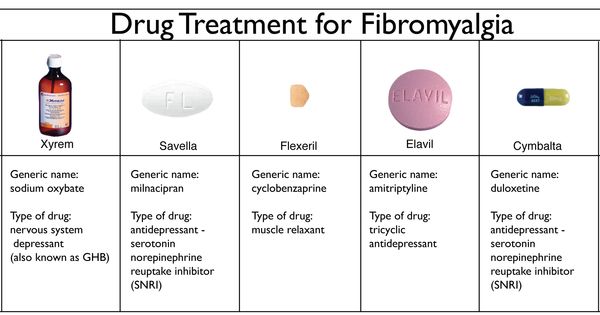 For a long time, fibromyalgia was referred to as idiopathic, that is, “inexplicable from a medical point of view” conditions due to unknown causes of development, physiological bases, and diagnostic criteria.
For a long time, fibromyalgia was referred to as idiopathic, that is, “inexplicable from a medical point of view” conditions due to unknown causes of development, physiological bases, and diagnostic criteria.
Today, fibromyalgia is classified as a chronic pain syndrome, which is based on the phenomenon of central sensitization. The same group includes chronic fatigue syndrome, myofascial pain syndrome, tension headache and others.
In simple terms, central sensitization refers to a sharp increase in the sensitivity of the nervous system in response to ordinary stimuli in everyday life. This is manifested by chronic pain and increased pain sensitivity to non-painful influences.
In the development of fibromyalgia also play a role: dysfunction of the autonomic nervous system, disruption of the relationship between the nervous and endocrine systems of regulation, and others.
Despite the rather non-specific and general manifestations of fibromyalgia, the absence of laboratory and other changes during the examination of the patient, it is not a psychosomatic condition/disease.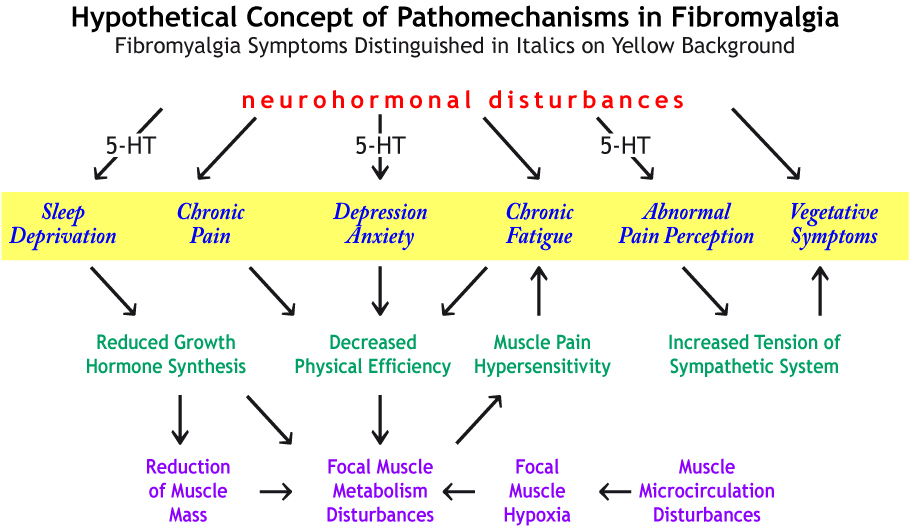 Fibromyalgia is included in the international classification of diseases (ICD - 10) as an independent nosological unit, that is, a diagnosis.
Fibromyalgia is included in the international classification of diseases (ICD - 10) as an independent nosological unit, that is, a diagnosis.
Fibromyalgia is characterized by a triad of symptoms:
- Chronic pain
- Sleep disorder
- Depression and fatigue
Important! The diagnosis of fibromyalgia is made only after the exclusion of other diseases that can manifest themselves with similar symptoms: arthritis, arthrosis, neurological diseases, and so on. That is, in the absence of laboratory changes, signs of pathology during research (MRI, X-ray, ultrasound, and others).
Fibromyalgia: the problem of chronic pain or “when nothing works”
The main clinical and characteristic manifestation of fibromyalgia is a chronic pain syndrome. Fibromyalgia patients seek medical attention from rheumatologists (joint pain), neurologists, therapists and other specialists for constantly disturbing pain "throughout the body", in which "nothing helps". A person with fibromyalgia is highly sensitive not only to painful stimuli, but also to any other: heat, cold, and even weak tactile (touch).
A person with fibromyalgia is highly sensitive not only to painful stimuli, but also to any other: heat, cold, and even weak tactile (touch).
Fibromyalgia pain has the following characteristics:
- Constant. Pain can change its intensity during the day, but in general it accompanies a person constantly. Pain duration: at least 3 consecutive months.
- In all muscles, joints - diffuse, multifocal. It is often difficult for the patient to localize the pain.
- Various character: deep, dull, burning.
- Exhausting: many patients find it difficult to do even everyday physical activity (climbing stairs, walking), as the pain is associated with a feeling of fatigue, “development”.
- Exacerbates in a state of fatigue, emotional stress, excessive physical activity, as well as with immobility, cooling, prolonged postural overstrain.
Pain is often accompanied by other unusual sensations throughout the body, such as tingling, numbness, goosebumps, and other health problems (stomach pain, digestive problems, pain when urinating, headaches, etc. ).
).
"Pain does not come alone"
Other signs of fibromyalgia - depression and poor sleep
- 96% of patients with fibromyalgia complain of sleep problems: difficulty falling asleep, insomnia, frequent awakenings in the middle of the night, shallow sleep that does not bring a feeling of rest and rejuvenation. Some patients talk about vivid dreams of an unpleasant nature, nightmares. The consequence of poor sleep is fatigue, decreased mental performance and cognitive functions: memory, attention.
- Depression is also a companion of fibromyalgia, it is closely associated with pain. Approximately half of the patients complain of a reduced background of mood, loss of the ability to enjoy almost everything, interest in the environment. The person becomes astenized and apathetic.
Diagnosis of fibromyalgia
A prerequisite for diagnosis is the exclusion of any other diseases and syndromes accompanied by chronic pain or other manifestations of fibromyalgia.
The doctor asks the patient in detail about the nature, time of onset of pain, provoking factors, the effect of painkillers and all complaints. It is easy for an experienced neurologist to suspect fibromyalgia already at the stage of a conversation with a patient.
Pain in the so-called tender points of the body is no less significant. These points are the places of attachment of the tendons, when exposed to (pressure), painful sensations occur that are not associated with pathological changes in the tissues in these areas (trauma, inflammation, and so on). A total of 18 such points were identified. To confirm the diagnosis of fibromyalgia, confirmation of tenderness in 11 or more of them is necessary.
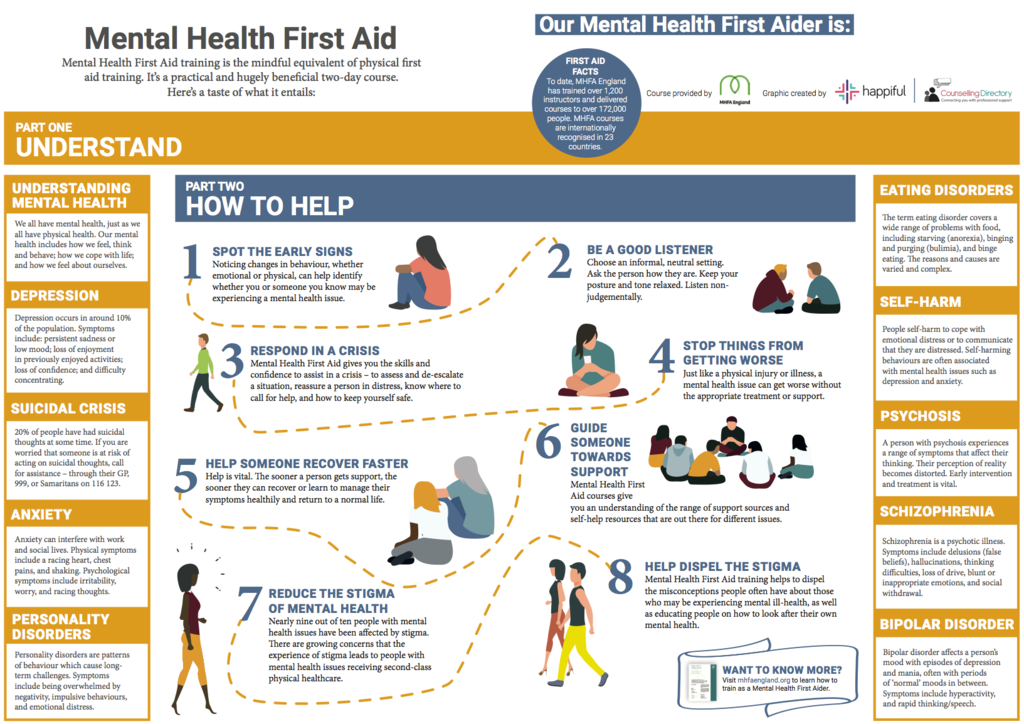
Treatment of fibromyalgia
Increasing knowledge of the mechanisms of chronic pain formation has significantly increased the effectiveness of fibromyalgia treatment and expanded the range of drugs that relieve pain and other manifestations of the disease. For the effective treatment of fibromyalgia, it is necessary to prescribe several groups of drugs and the participation of doctors of different specialties (neurologist, psychiatrist, psychotherapist, and others).
For the effective treatment of fibromyalgia, it is necessary to prescribe several groups of drugs and the participation of doctors of different specialties (neurologist, psychiatrist, psychotherapist, and others).
Pharmacological treatments for fibromyalgia target:
- relief of pain;
- correction of severe hypochondriacal fixation of patients on their experiences;
- normalization and improvement of sleep quality;
- depression correction.
Proper selection and combination of drugs is the key to successful relief from fibromyalgia symptoms!
Non-pharmacological treatments for fibromyalgia include:
- cognitive behavioral therapy;
- physiotherapy exercises;
- physiotherapy;
- acupuncture.
Treatment of fibromyalgia in Nizhny Novgorod
Diagnosis and complex treatment of fibromyalgia in Nizhny Novgorod is carried out at the TONUS LIFE Back Pain Treatment Center.