Auditory visual hallucination
Hallucinations and hearing voices
Hallucinations and hearing voices
Hallucinations refer to the experience of hearing, seeing or smelling things that are not there.
Often, these can be as intense and as real as sensory perceptions. There are different types of hallucinations.
- Hearing voices speaking when there is no-one there is known as an auditory hallucination. Voices can talk about very personal matters, which can be quite frightening. Often, other sounds like music, animal calls and the telephone ringing can be heard. These may be experienced as coming from anywhere in external space or ‘in the mind’. The noise volume varies from very quiet to very loud. The experience is different for different people.
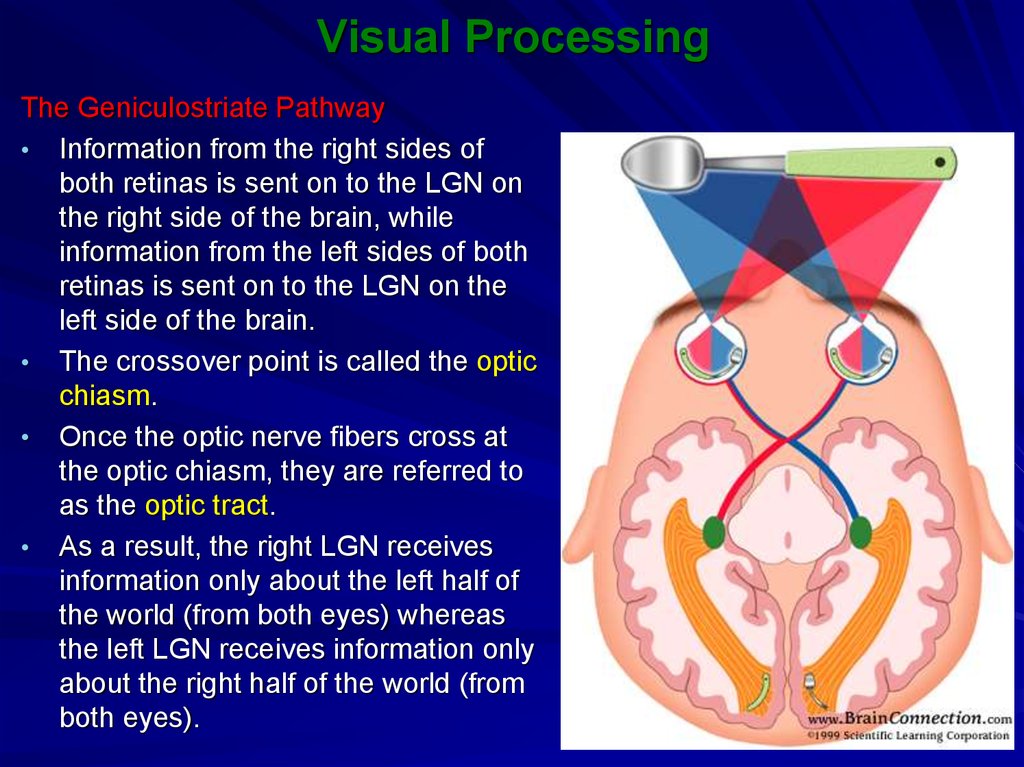
- Seeing images when there is nothing in the environment to account for it is a visual hallucination. Simple visual hallucinations may include flashes or geometric shapes.
Complex visual hallucinations may show faces, animals or scenes and may be called ‘visions’.
- Other types of hallucinations include feelings on the skin, smelling or tasting things that cannot be explained.
Causes of hallucinations
Intense negative emotions such as stress or grief can make people particularly vulnerable to hallucinations, as can conditions such as hearing or vision loss, and drugs or alcohol. It is believed that the mental processes which operate during hallucinations include memories and images which the brain has difficulty controlling. The way that individuals react to their hallucinations also impacts on how they feel about them.
People who are at increased risk of hallucinations
Hallucinations occur frequently in psychiatric conditions such as schizophrenia, bipolar disorder, post-traumatic disorder and borderline personality disorder, as well as in other disorders such as dementia and Parkinson’s. Auditory hallucinations are typically more common in psychiatric disease, and visual hallucinations in disorders of old age,
Auditory hallucinations are typically more common in psychiatric disease, and visual hallucinations in disorders of old age,
People who experience hallucinations do not necessarily suffer from a mental illness. It is quite common for people in the general population to experience passing and infrequent episodes of hallucination, and many people recover completely. People who have ongoing experiences which are distressing should seek professional advice.
Signs and symptoms
It is possible to lead a productive and meaningful life with hallucinations. For many, however, hallucinated voices or visions can be distressing and worrying. If you are troubled by hallucinations, it is best to seek help from your GP or mental health services, as they will help to work out what is causing the problem.
Treatment of hallucinations
There are different treatment options depending on the cause of hallucinations. Forms of help include psychological therapies and medications.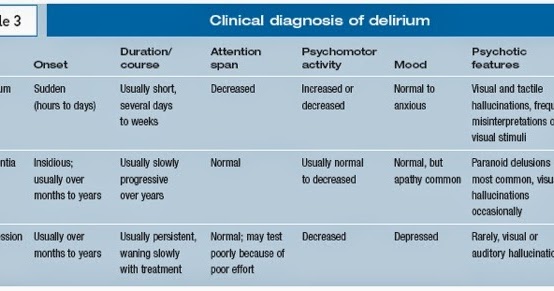 A well-organised system of help from friends, family and professionals provides the most effective treatment option.
A well-organised system of help from friends, family and professionals provides the most effective treatment option.
Living with hallucinations
Everyday strategies are very helpful for coping with hallucinations. These include:
- Connecting with people with similar experiences.
- Knowing that friends and/or family are there to provide support.
- Finding a meaning and purpose in your life.
- Accepting that it is an aspect of your personality which makes you who you are.
- Understanding that many people with hallucinations live happy and successful lives.
Practical advice for family and friends
- Accept that the person is experiencing voices or visions. These experiences are like real perceptions and can be very puzzling and frightening. Showing love and support will help the person to feel safe expressing their concerns to you.
- Encourage the person to describe their experiences. What is it like? Do they hear different voices? What do the voices say? These may account for feelings and emotions.

- Suggest that the person might be able to draw on their own particular strength to help them cope with or overcome the hallucinations. Their strengths may include problem solving), the practice of relaxation techniques, or verbalising their emotions.
- Do fun things together.
- Encourage the person to meet other people who experience hallucinations, and to read on the topic.
- Encourage people to attend support groups such as the Hearing Voices Network Australia (external site).
Where to get help
- See your GP or mental health worker
- Ring healthdirect Australia on 1800 022 222
- RuralLink for Rural and remote areas 1800 552 002.
Acknowledgements
Clinical Research Centre
This publication is provided for education and information purposes only. It is not a substitute for professional medical care. Information about a therapy, service, product or treatment does not imply endorsement and is not intended to replace advice from your healthcare professional. Readers should note that over time currency and completeness of the information may change. All users should seek advice from a qualified healthcare professional for a diagnosis and answers to their medical questions.
Readers should note that over time currency and completeness of the information may change. All users should seek advice from a qualified healthcare professional for a diagnosis and answers to their medical questions.
See also
- Parkinson's
Visual Hallucinations: Differential Diagnosis and Treatment
1. Asaad G, Shapiro B. Hallucinations: theoretical and clinical overview. Am J Psychiatry. 1986;143:1088–1097. [PubMed] [Google Scholar]
2. Manford M, Andermann F. Complex visual hallucinations: clinical and neurobiological insights. Brain. 1998;121:1819–1840. [PubMed] [Google Scholar]
3. Price J, Whitlock FA, Hall RT. The psychiatry of vertebrobasilar insufficiency with the report of a case. Psychiatr Clin (Basel) . 1983;16:26–44. [PubMed] [Google Scholar]
4. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol. 2003;48:58–72. [PubMed] [Google Scholar]
Surv Ophthalmol. 2003;48:58–72. [PubMed] [Google Scholar]
5. Burke W. The neural basis of the Charles Bonnet hallucinations: a hypothesis. J Neurol Neurosurg Psychiatry. 2002;73:535–541. [PMC free article] [PubMed] [Google Scholar]
6. Cogan DG. Visual hallucinations as release phenomena. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1973 Aug;188(2):139–150. [PubMed] [Google Scholar]
7. Merabet LB, Maguire D, Warde A, et al. Visual hallucinations during prolonged blindfolding in sighted subjects. J Neuroophthalmol. 2004 Jun;24(2):109–113. [PubMed] [Google Scholar]
8. First MB, Tasman A. San Francisco, Calif: Wiley; 2004. Schizophrenia and other psychotic disorders; p. 640. [Google Scholar]
9. Mueser KT, Bellack AS, Brady EU. Hallucinations in schizophrenia. Acta Psychiatr Scand. 1990;82:26–29. [PubMed] [Google Scholar]
10. Small IJ, Small JG, Andersen HJM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst. 1966;27:349–353. [PubMed] [Google Scholar]
11. Goodwin DW, Alderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76–80. [PubMed] [Google Scholar]
Goodwin DW, Alderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry. 1971;24:76–80. [PubMed] [Google Scholar]
12. Armstrong SC, Cozza KL, Watanabe KS. The misdiagnosis of delirium. Psychosomatics. 1997;38(5):433–439. [PubMed] [Google Scholar]
13. Swigart SE, Kishi Y, Thurber S, et al. Misdiagnosed delirium in patient referrals to a university-based hospital psychiatry department. Psychosomatics. 2008;49:104–108. [PubMed] [Google Scholar]
14. Webster R, Holroyd S. Prevalence of psychotic symptoms in delirium. Psychosomatics. 2000;41:519–522. [PubMed] [Google Scholar]
15. Gastfriend DR, Renner JA, Hackett TP. Alcoholic patients: acute and chronic. Massachusetts General Hospital Handbook of General Hospital Psychiatry. In: Stern TA, Fricchione GL, Cassem NH, et al., editors. 5th ed. Philadelphia, Pa: Mosby; 2004. pp. 203–216. eds. [Google Scholar]
16. Mitchell J, Vierkant AD. Delusions and hallucinations of cocaine abusers and paranoid schizophrenics: a comparative study. J Psychol. 1991;125:301–310. [PubMed] [Google Scholar]
Delusions and hallucinations of cocaine abusers and paranoid schizophrenics: a comparative study. J Psychol. 1991;125:301–310. [PubMed] [Google Scholar]
17. Ballard CG, O'Brien JT, Swann AG, et al. The natural history of psychosis and depression in dementia with Lewy bodies and Alzheimer's disease: persistence and new cases over 1 year of follow-up. J Clin Psychiatry. 2001;62(1):46–49. [PubMed] [Google Scholar]
18. Ala TA, Yang KH, Sung JH, et al. Hallucinations and signs of parkinsonism help distinguish patients with dementia and cortical Lewy bodies from patients with Alzheimer's disease at presentation: a clinicopathological study. J Neurol Neurosurg Psychiatry. 1997;62:16–21. [PMC free article] [PubMed] [Google Scholar]
19. Tiraboschi P, Salmon DP, Hansen LA, et al. What best differentiates Lewy body from Alzheimer's disease in early-stage dementia? Brain. 2006 Mar;129:729–735. [PubMed] [Google Scholar]
20. Harding AJ, Broe GA, Halliday GM. Visual hallucinations in Lewy body disease relate to Lewy bodies in the temporal lobe. Brain. 2002;125:391–403. [PubMed] [Google Scholar]
Brain. 2002;125:391–403. [PubMed] [Google Scholar]
21. Williams DR, Lees AJ. Visual hallucinations in the diagnosis of idiopathic Parkinson's disease: a retrospective autopsy study. Lancet Neurol. 2005;4:605–610. [PubMed] [Google Scholar]
22. Fenelon G, Mahieux F, Huon R, et al. Hallucinations in Parkinson's disease: prevalence, phenomenology and risk factors. Brain. 2000;123:733–745. [PubMed] [Google Scholar]
23. Lippa CF, Duda JE, Grossman M, et al. DLB/PDD Working Group: DLB and PDD boundary issues: diagnosis, treatment, molecular pathology, and biomarkers. Neurology. 2007;68:812–819. [PubMed] [Google Scholar]
24. Josephs KA, Whitwell JL, Boeve BF, et al. Visual hallucinations in posterior cortical atrophy. Arch Neurol. 2006;63:1427–1432. [PMC free article] [PubMed] [Google Scholar]
25. Levine DN, Lee JM, Fisher CM. The visual variant of Alzheimer's disease: a clinicopathologic case study. Neurology. 1993;43:305–313. [PubMed] [Google Scholar]
26. Rovner BW. The Charles Bonnet syndrome: a review of recent research. Curr Opin Ophthalmol. 2006;17(3):275–277. [PubMed] [Google Scholar]
The Charles Bonnet syndrome: a review of recent research. Curr Opin Ophthalmol. 2006;17(3):275–277. [PubMed] [Google Scholar]
27. Maeda K, Shirayama Y, Nukina S, et al. Charles Bonnet syndrome with visual hallucinations of childhood experience: successful treatment of 1 patient with risperidone [letter] J Clin Psychiatry. 2003;64(9):1131–1132. [PubMed] [Google Scholar]
28. Coletti Moja M, Milano E, Gasverde S, et al. Olanzapine therapy in hallucinatory visions related to Bonnet syndrome. Neurol Sci. 2005;26:168–170. [PubMed] [Google Scholar]
29. Lang UE, Stogowski D, Schulze D, et al. Charles Bonnet syndrome: successful treatment of visual hallucinations due to vision loss with selective serotonin reuptake inhibitors. J Psychopharmacol. 2007;21:553–555. [PubMed] [Google Scholar]
30. Critchley M. New York, NY: Raven; 1979. Modes of reaction to central blindness; p. 156. [Google Scholar]
31. Miller N. Walsh and Hoyt's Clinical Neuro-ophthalmology. Baltimore, Md: Williams and Wilkins; 1982. p. 144. [Google Scholar]
p. 144. [Google Scholar]
32. Aldrich MS, Alessi AG, Beck RW, et al. Cortical blindness: etiology, diagnosis and prognosis. Ann Neurol. 1987;21:149–158. [PubMed] [Google Scholar]
33. Goldenberg G, Müllbacker W, Nowak A. Imagery without perception: a case study of anosognosia for cortical blindness. Neuropsychologia. 1995;33:1373–1382. [PubMed] [Google Scholar]
34. Salanova V, Andermann F, Olivier A, et al. Occipital lobe epilepsy: electroclinical manifestations, electrocorticography, cortical stimulation, and outcome in 42 patients treated between 1930 and 1991: surgery of occipital lobe epilepsy. Brain. 1992 Dec;115:1655–1680. [PubMed] [Google Scholar]
35. Panayiotopoulos CP. Elementary visual hallucinations, blindness, and headache in idiopathic occipital epilepsy: differentiation from migraine. J Neurol Neurosurg Psychiatry. 1999;66:536–540. [PMC free article] [PubMed] [Google Scholar]
36. Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia. 1989;30:389–399. [PubMed] [Google Scholar]
Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia. 1989;30:389–399. [PubMed] [Google Scholar]
37. Devinsky O, Luciano D. Psychic phenomena in partial seizures. Semin Neurol. 1991;11(2):100–109. [PubMed] [Google Scholar]
38. Wieser HG. The phenomenology of limbic seizures. In: Wieser HG, Speckman E-J, Engel J, editors. The Epiletic Focus. London, England: John Libbey; 1987. eds. [Google Scholar]
39. Caplan JP, Epstein LA, Stern TA. Consultants’ conflicts: a case discussion of differences and their resolution. Psychosomatics. 2008;49(1):8–13. [PubMed] [Google Scholar]
40. Waters WE, O'Connor PJ. Prevalence of migraine. J Neurol Neurosurg Psychiatry. 1975;38:613–616. [PMC free article] [PubMed] [Google Scholar]
41. Goadsby PJ, Lipton RB, Ferrari MD. Migraine: current understanding and treatment. N Engl J Med. 2002;346:257–270. [PubMed] [Google Scholar]
42. Russell MB, Olesen J. A nosographic analysis of the migraine aura in a general population. Brain. 1996;119:355–361. [PubMed] [Google Scholar]
Brain. 1996;119:355–361. [PubMed] [Google Scholar]
43. Hadjikhani N, Sanchez del Rio M, Wu O, et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc Natl Acad Sci USA. 2001;98:4687–4692. [PMC free article] [PubMed] [Google Scholar]
44. Catafau JS, Rubio F, Serra JP. Peduncular hallucinosis associated with posterior thalamic infarction. J Neurol. 1992;239:89–90. [PubMed] [Google Scholar]
45. Aldrich MS. Diagnostic aspects of narcolepsy. Neurology. 1998 Feb;50(2 supp 1):S2–S7. [PubMed] [Google Scholar]
46. Ohayon MM, Priest RG, Caulet M, et al. Hypnagogic and hypnopompic hallucinations: pathological phenomena? Br J Psychiatry. 1996;169:459–467. [PubMed] [Google Scholar]
47. Broughton RJ. Neurology and dreaming. Psychiatric J University of Ottawa. 1982;7:101–110. [Google Scholar]
48. Nichols DE. Hallucinogens. Pharmacol Ther. 2004;101:131–181. [PubMed] [Google Scholar]
49. Cushing H. Distortions of the visual fields in cases of brain tumor (6th paper): the field defects produced by temporal lobe lesions. Brain. 1922;44:341–396. [Google Scholar]
Brain. 1922;44:341–396. [Google Scholar]
50. Horrax G, Putnam TJ. Distortions of the visual fields in cases of brain tumour: the field defects and hallucinations produced by tumours of the occipital lobe. Brain. 1932;55:499–523. [Google Scholar]
51. Sedes F, Baumann N, Turpin JC, et al. Psychiatric manifestations revealing inborn errors of metabolism in adolescents and adults. J Inherit Metab Dis. 2007;30:631–641. [PubMed] [Google Scholar]
52. Moellentine CK, Rummans TA. The varied neuropsychiatric presentations of Creutzfeldt-Jakob disease. Psychosomatics. 1999;40:260–263. [PubMed] [Google Scholar]
53. Brar HK, Vaddigiri V, Scicutella A. Of illusions, hallucinations and Creutzfeldt-Jakob disease (Heidenhain's variant) J Neuropsychiatry Clin Neurosci. 2005;17:124–126. [PubMed] [Google Scholar]
54. Furlan AJ, Henry CE, Sweeney PJ, et al. Focal EEG abnormalities in Heidenhain's variant of Jakob-Creutzfeldt disease. Arch Neurol. 1981;38(5):312–314. [PubMed] [Google Scholar]
55. Caplan JP. Diagnosis and treatment of agitation and delirium in the ICU patient. Irwin and Rippe's Intensive Care Medicine. In: Irwin RS, Rippe JM, editors. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2007. pp. 2287–2295. [Google Scholar]
Caplan JP. Diagnosis and treatment of agitation and delirium in the ICU patient. Irwin and Rippe's Intensive Care Medicine. In: Irwin RS, Rippe JM, editors. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2007. pp. 2287–2295. [Google Scholar]
Causes and symptoms of hallucinations. What to do and how to fight?
Dietary supplements cheap
In the process of hallucinations, a person sees or hears something that does not exist in reality. The phenomenon occurs for various reasons, it is important to understand in a timely manner why such a state occurs, how it develops and what to do about it.
What are hallucinations, what are they?
Hallucinations are images that appear in the human mind. Most often, these are symptoms of a psychological illness. A person may also experience auditory hallucinations. In healthy people, hallucinations can also occur, but as a result of severe overwork of the body. If this condition is not uncommon for you, then you should think about treatment.
If this condition is not uncommon for you, then you should think about treatment.
Free consultation now!
Online consultation with a specialist on your issue!
License number: LO-77-01-019036
Symptoms and signs of hallucinations
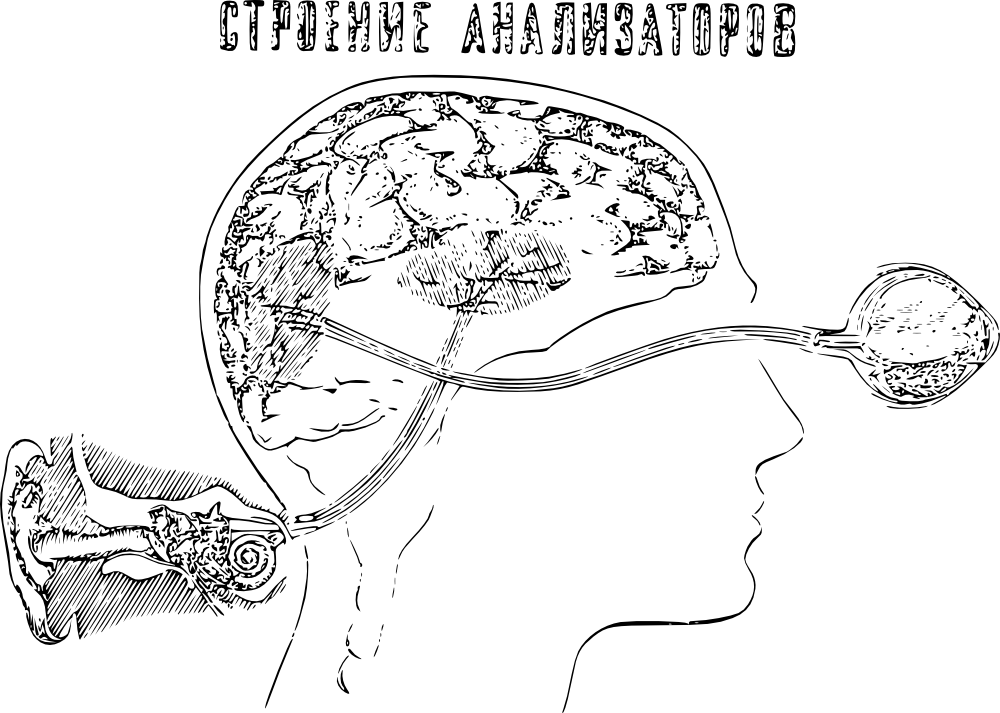
In simple terms, hallucinations occur as a result of a failure of any system responsible for the perception of the surrounding world. So some visual objects may seem to the patient or auditory perception may be distorted. Hallucinations are diagnosed by a psychiatrist.
Most often, at the initial stage, such hallucinations occur with closed eyes, when a person goes to sleep. This is preceded by frequent abuse of alcohol or drugs.
Hallucinations are true and false. The difference is this: true hallucinations - a person is confident in their reality, and does not question the fact that they do not exist in reality, and this is the result of a failure in his perceptual system. The patient sees such phenomena in the world around him.
The patient sees such phenomena in the world around him.
False hallucinations occur in the person's head. For example, the patient hears voices in his head, he may believe that someone communicates with him mentally and influences his condition and decisions. Such conditions are associated with schizophrenia.
Types of hallucinations
To understand what to work with, hallucinations must be classified into certain types.
It must also be said that all hallucinations are divided into 2 types.
- True hallucinations - a person perceives false objects in the surrounding world and believes that they are part of reality.
- False - the distortion of reality occurs in the patient's head. imply
Hallucinations can be simple or complex. Those. the failure may affect one or more organs of perception. And the more organs are subject to hallucinations, the more difficult the treatment is.
Visual hallucinations
As a result, false images of objects, people, living beings, various objects appear in the human mind, but the patient perceives them as part of reality. In addition, a person sees a certain sequence of actions (as if some plots of a film) and can take an active part in them. This happens after an overdose of alcohol, drugs, or incorrectly taking serious medications. Such visions haunt a person.
In addition, a person sees a certain sequence of actions (as if some plots of a film) and can take an active part in them. This happens after an overdose of alcohol, drugs, or incorrectly taking serious medications. Such visions haunt a person.
Auditory hallucinations
A person hears voices, various sounds, hears his name or is told to do something, but only he hears this in reality it does not exist. Auditory hallucinations are detected in acute mental illness, such as schizophrenia.
Can sometimes be caused by an overdose of various substances, similar to visual.
Olfactory hallucinations
Less common. A person smells non-existent odors. Occur after brain injury or schizophrenia. They can also appear after the passage of an infectious disease.
Taste hallucinations
The patient has sharp and unpleasant sensations in the oral region, as a result of which there is a refusal of any food.
Tactile hallucinations
A person feels that there is an object (creature) on the body that does not exist, there may also be a sensation of the object moving around the body. In this case, there is a feeling of sharp heat or cold. The patient has unpleasant tactile sensations on the body. Severe pain or itching.
Hypnagogic hallucinations
Appear when a person falls asleep (most often healthy). Awareness arises in the form of masks, plant monsters, and any other physical objects. Such hallucinations are a harbinger of an imminent mental disorder and a reason to consult a specialist, or call a psychiatrist at home.
Write to WhatsApp
COST OF TREATMENT
Causes hallucinations
Let's see why hallucinations can occur. Specialists of the medical center "Korsakov" identify the following reasons:
Excessive and systematic alcohol consumption.
Drug use.
Use and overdose of psychostimulants.
Schizophrenia.
Brain damage.
Influence of psychosis.
Syphilis.
Age. As a result of the aging of the body, changes occur that entail a failure of the organs of perception.
Frequent stress, pessimism, anxiety.
Hallucinogenic mushrooms.
Neoplasms of the brain.
Infection of the body.
Epileptic syndrome.
Heart disease.
Atherosclerosis.
Prolonged insomnia.
Causes of hallucinations in the elderly
In the elderly, the development of hallucinations may be due to age. This is the result of age-related changes in the organs of perception. Such people are characterized not only by auditory hallucinations, but also by visual and gustatory hallucinations. Elderly people with this disease begin to complain about strange smells in the room, an unpleasant taste in the mouth, etc.
What to do in case of hallucinations?
Today there are a huge number of methods for the treatment of hallucinations, and different methods are aimed at eliminating different types of hallucinations. It must be said that therapy is often aimed at curing the cause of hallucinations. But, unfortunately, it is not always possible to eliminate the cause of the disease. It is necessary that hallucinations or the disease that caused them be diagnosed by an experienced specialist. Do not be shy or wait for an exacerbation, you should consult a doctor immediately.
It must be said that therapy is often aimed at curing the cause of hallucinations. But, unfortunately, it is not always possible to eliminate the cause of the disease. It is necessary that hallucinations or the disease that caused them be diagnosed by an experienced specialist. Do not be shy or wait for an exacerbation, you should consult a doctor immediately.
Get a consultation at the psychiatric department of the KORSAKOV clinic.
How to identify hallucinations?
Diagnosis means to establish whether there is a difference with the illusory deception that a healthy person can have. It is necessary to look at the general condition and behavior of the patient, to check whether he has delusions or other mental illnesses. Analyze his facial expressions, gestures, check whether he has a feeling of anxiety, and based on the overall picture, draw a conclusion about the state of the person. So you can understand whether there is a disease, and if so, determine the degree.
How to deal with hallucinations?
The first step is to diagnose the cause of the hallucination and possible diseases. Next, you need to prescribe a course of appropriate treatment.
At the stage of diagnosis, an anamnesis is collected, it is specified what exactly the patient sees, hears and feels. A thorough examination of the visible, audible, felt is carried out, an examination is carried out and a method of treatment is selected. The method of observation and care of the patient is also selected.
Online consultation with a specialist
for your question!
License number: LO-77-01-019036
Treatment of hallucinations
The method of treatment depends on what the doctor finds out at the diagnostic stage. One of the methods for eliminating the pathology itself can be chosen. If it turns out that the cause cannot be eliminated, then the therapy is aimed at eliminating the symptoms, that is, the hallucinations themselves.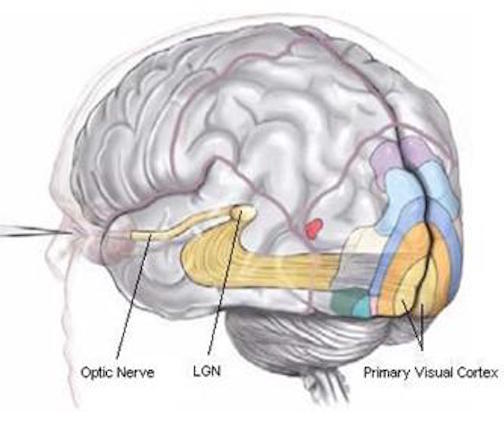 If the disease developed as a result of the use of any drugs, then they are canceled.
If the disease developed as a result of the use of any drugs, then they are canceled.
In case of poisoning by alcohol or drugs, cleansing of the gastrointestinal tract is prescribed. The patient will need rest and care.
A course of psychotherapy helps to cure hallucinations. Neurometabolic therapy and restorative medicine techniques are used.
Hallucinations | CLRC Handbook
A hallucination is an image, sound or other sensation that occurs in the mind of a sick person without an external stimulus. They can manifest themselves when the body is overworked or when there is a malfunction of the internal organs, especially the brain. Infectious diseases also affect the development of pathology.
Species
-
True. The patient sees, feels or hears something, but this phenomenon is bright, lively. The hallucination is real to the sufferer.
-
Pseudo-hallucinations. These are visions, sounds or sensations that occur outside of objective reality.
Important: false hallucinations usually depend on suggestion or the influence of external factors.
Hallucinations are different, depending on certain sense organs that perceive:
-
Visual. It can be whole storylines, mystical visions, just flashes of light or smoke. As well as animals, identical objects, vision of organs in one's body or foreign objects, etc.
-
Hearing. These include ordinary noises or sounds, as well as verbal ones: imperative, when a certain voice orders something to be done to the patient, usually it is negative; commenting - voices discuss the thoughts, feelings and sensations of the patient, they are also negative and judgmental; contrasting, when the patient hears 2 voices directed against each other, one at the same time condemns the patient, the other protects, but at the same time they give conflicting commands to the sufferer; motor speech - it seems to the patient that some forces speak for him, in an unknown language.
-
Olfactory. The patient complains of unpleasant odors.
-
Flavoring. An unpleasant taste may occur in the patient's mouth.
-
Tactile: fluid sensation, different temperatures, crawling insects, hugging.
-
Functional. Against the background of any objects or phenomena, imaginary images appear, sounds, etc.
-
Hallucinations of Bonn. An imaginary sensation is perceived by the analyzer, which has completely or partially lost its function.
-
Hemianoptic. Occur with a disease - hemianopia. This is when the patient sees only half of the field of view. Imaginary sensations arise in the area that does not see.
-
Hypnagogic and hypnopompic hallucinations. They can occur even in a healthy person. They appear in the form of imaginary images or sounds that accompany a person upon awakening or falling asleep. They are connected with the events of the day experienced.
Types of hallucinations depending on the analyzer:
-
Psychomotor, when the patient feels that part of his body is in motion.
-
Reflex, when a real impact on one analyzer, another one is excited.
-
Ecstatic. There are bright pictures or whole images in a state of altered consciousness.
Important: hallucinations must be able to distinguish from mirages and illusions, because they arise on the basis of other factors.
Causes
Misleading sights, sounds or sensations may occur when:
-
Dementia. It seems to the patient that objects are moving.
-
Parkinson's disease. Visual images appear: people, animals, objects, or even whole situations.
-
Migraine. Patients see flickering or colored zigzag lines in the central region of the visual field. They leave behind a white spot that disappears after half an hour.

-
Epilepsy. Visual images, in the form of bright spots or outlines.
-
Sleep disturbance. Usually occurs when waking up or falling asleep.
-
Brainstem infarction. Bright and colorful scenes appear. They usually carry a semantic load. They can last from 1 minute to several hours.
-
Tumor of the brain. Hallucinations can be of different types. It depends on the localization of the pathological process.
-
Creutzfeldt-Jakob disease. It arises on the basis of a prion infection and causes dystrophic processes in the cerebral cortex and spinal cord, basal ganglia. Visual hallucinations occur: color change, perception in reduced sizes, distortion of the characteristics of objects, etc.
-
Sclerosis of cerebral vessels. There are auditory and visual hallucinations.
-
Stroke.
In addition to the above reasons, hallucinations can be caused by: Aging.
-
Infectious diseases.
-
Pathology of internal organs.
-
Drug intoxication.
-
Poisoning by toxic substances.
Which doctor to contact
Hallucination is not a separate disease, but a symptom that occurs when an organ is damaged, in most cases the brain. But in order to identify the real cause of the pathology, you need to consult such specialists:
-
Psychiatrist.
-
Neurologist.
-
Oncologist.
-
Narcologist.
-
Infectionist.
Hallucinations are an important symptom that indicates that the patient has certain disturbances in the awareness of the surrounding reality. Often, patients are embarrassed or afraid to talk about the presence of hallucinations, because they think that only people with mental disorders experience hallucinatory experiences.
IMPORTANT! This is a false stable belief, with hallucinations it is necessary to work with different specialists. The fact is that hallucinations can occur due to the presence of a neoplasm or an infectious pathology.
Therefore, make an appointment with a specialist of our center - a psychiatrist, neurologist, oncologist, narcologist or infectious disease specialist to find the root of the problem and eliminate the symptom!
Make an appointment
Methods of treatment
Methods of treating a pathology depend on the causes that caused it. There is no single schema. For example, in case of poisoning with toxic substances, it is necessary to stop their effect on the body. In the presence of neurological causes, it is necessary to start appropriate therapy or relief of the acute form of the disease.
Treatment is usually carried out with:
Results
The prognosis of the development of hallucinations depends on the success of the treatment. That is, if the cause of the disease is found in time, treatment can be started, you can get rid of imaginary images, visions and sensations.
That is, if the cause of the disease is found in time, treatment can be started, you can get rid of imaginary images, visions and sensations.
Important: if the disease is not treatable, then the patient's normal condition must be maintained with medication.
Rehabilitation and lifestyle restoration
Rehabilitation includes:
-
Diagnosis of the cause of the disease.
-
Hospitalization.
-
Laboratory studies.
-
Complex treatment.
-
Disease control and treatment.
-
Forecasting.
-
Carrying out therapeutic and preventive measures after the main treatment.
Lifestyle in case of hallucinations
The further life of the patient depends on the causes that caused the pathology. If there is a disease that cannot be treated, then you need to constantly maintain normal life with the help of medicines.