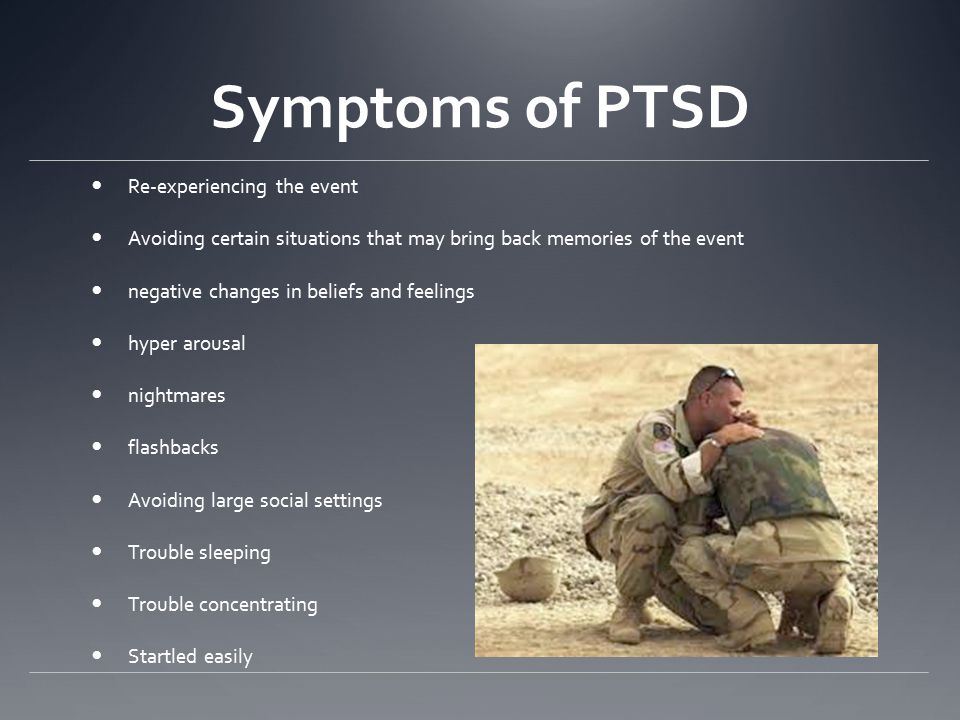
Are nightmares a symptom of ptsd
What Can Cause PTSD Nightmares and How Can it Be Treated?
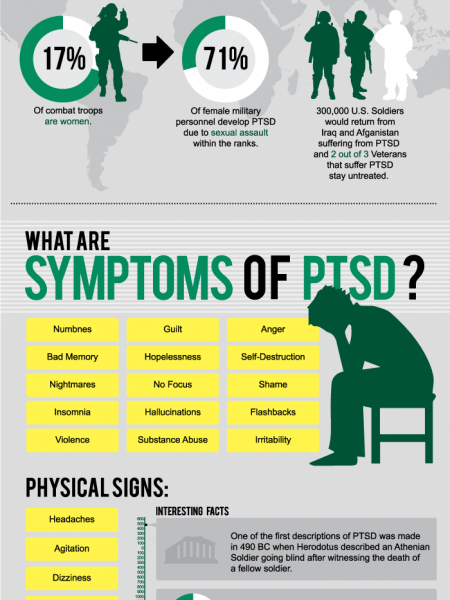
When someone experiences nightmares from PTSD, they can seem very real to them. They might feel like they are back in a situation that is not safe, the traumatic experience that caused the disruption in the first place.
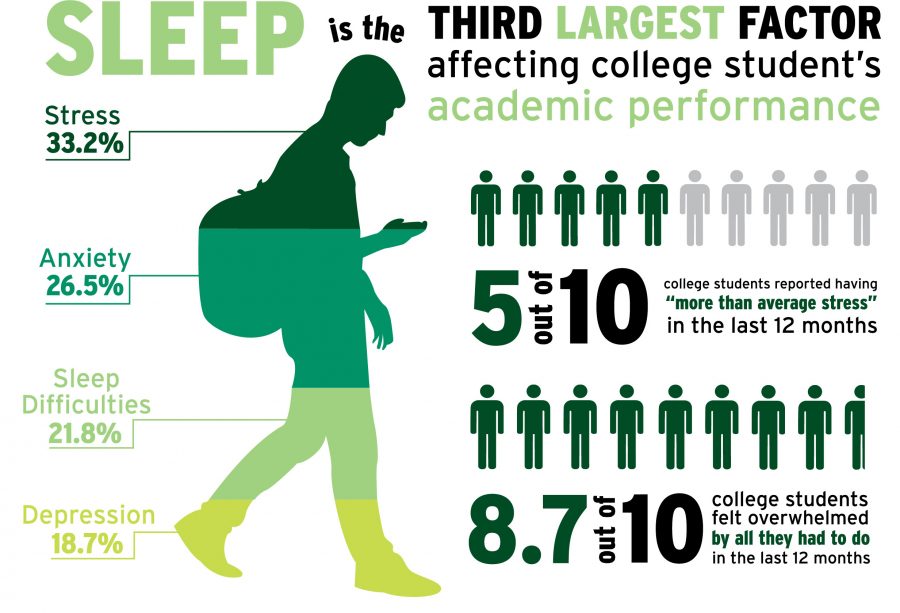
Symptoms can keep them awake or unable to fall asleep for long periods of time. Sleep is essential to healing the body, keeping it healthy, and feeling secure. Find out why nightmares occur with PTSD and how to offer support for someone who is struggling.
Challenges with SleepThe brain and body are wired for sleep at certain hours of the day. When it is dark, people feel tired and ready for rest.
When it is light, people typically feel ready to do things like work, go out with friends, socialize, and take part in activities. Shift workers often struggle with staying up during the nighttime hours and sleeping when it is light outside.
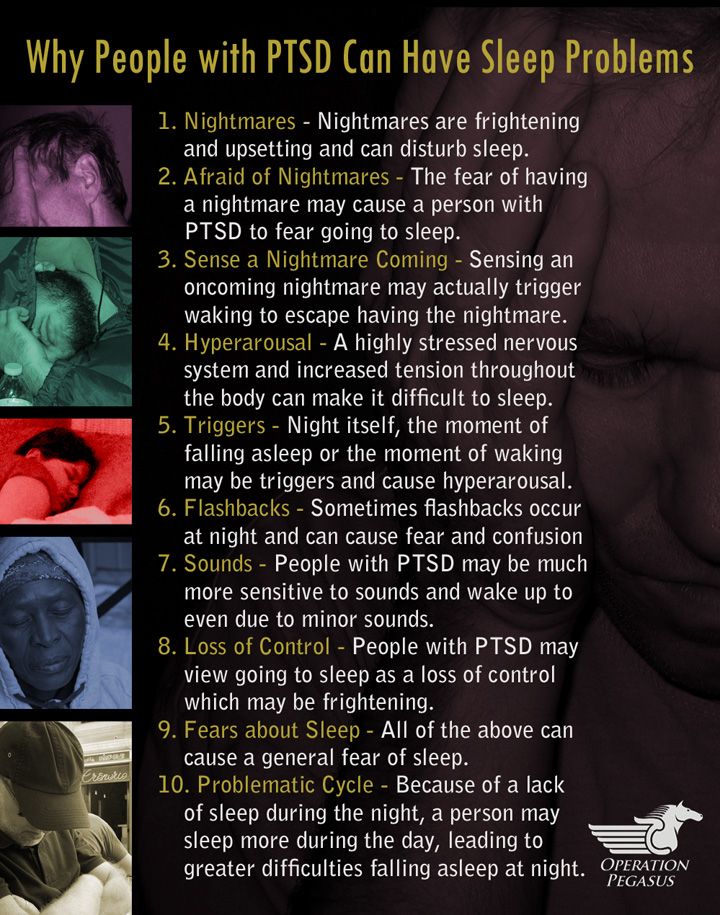
A full night of sleep with PTSD can be challenging and taxing on the body. Nightmares are part of the symptoms of PTSD, which impact overall sleep quality.
With a night’s rest, sleep includes REM and non-REM sleep, alternating cycles throughout the night. Disruptions due to PTSD can cause feelings of hopelessness and despair as a person desperately wants to sleep but cannot.
When they do sleep, they are disturbed by dreams that put them back in a situation where they feel in harm’s way.
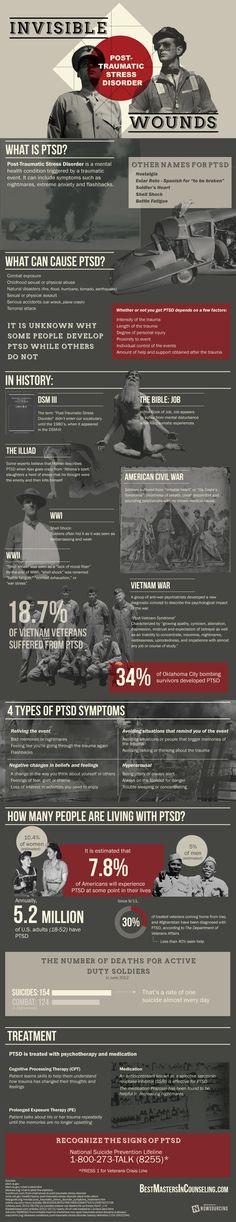
Impact on PTSDNightmares are a feature of PTSD. Even general nightmares can feel life-threatening, but with PTSD, they are actually tied to an existing trauma that happened in the near or far past.
Replaying traumatic events over and over can cause a struggle for someone to cope. A nightmare usually involves replaying the traumatic event, feeling like they are right back there again.
For veterans, this might mean re-witnessing horrific events or even deaths of people they witnessed while on combat missions. Physical abuse, violence, and other things can be triggering the nightmares and inability to sleep.
When someone fears going to sleep and is not wanting to go to bed, that can be traumatic. Sleep avoidance in combination with affected sleep cycles causes people to feel less connected to family, their work, and social life. They risk suicidal thoughts and are three times more likely to suffer PTSD-related risk factors such as addiction.
Treatment OptionsDual diagnosis, or experiencing PTSD symptoms with substance use, are not uncommon. It is one way people use to numb the feelings of pain and stress, including flashbacks and nightmares.
Appropriate treatment varies but every person should be evaluated thoroughly to see how they are coping with the nightmares and subsequent issues related to PTSD. This might include looking at relationships, work, and family life to see where they suffer the impact.
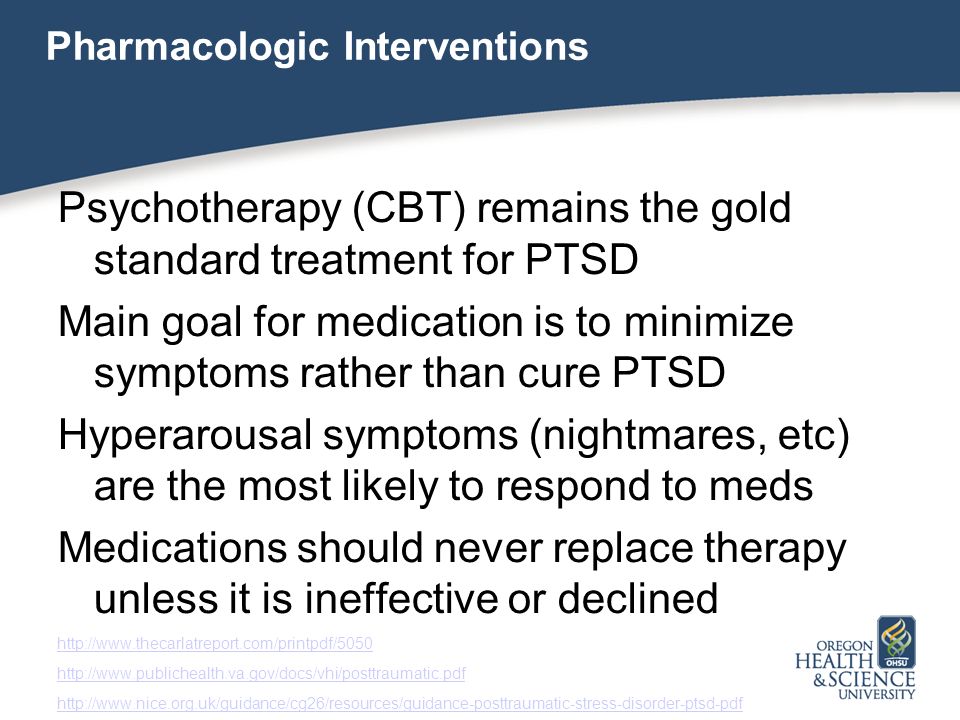
Cognitive Behavioral Therapy (CBT)CBT is used to identify and adjust thoughts, emotions, and behaviors they struggle with.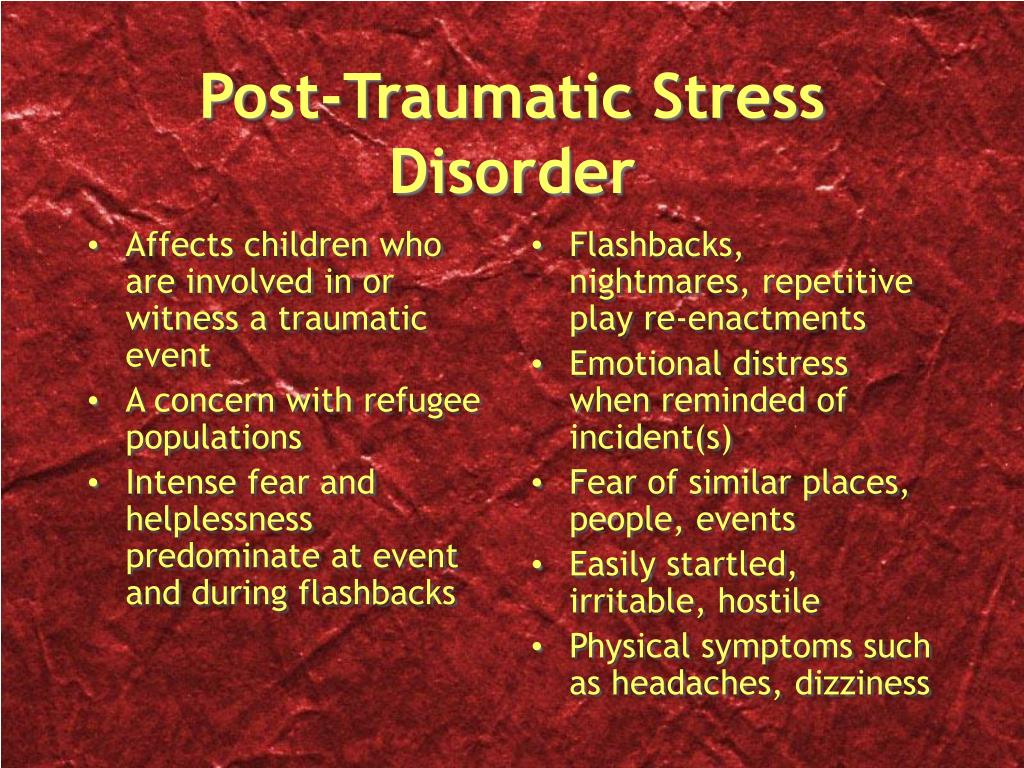 These can include sleep therapies, self-exposure therapy, desensitization, and lucid dreaming therapy.
These can include sleep therapies, self-exposure therapy, desensitization, and lucid dreaming therapy.
CBT is a time to sit down with a therapist and work out what has gone on to see if there are identified triggers that may be helpful to work on. The techniques can be used in combination or alone, though future research is needed to determine the best practices related to trauma.
MedicationMedication for PTSD nightmares has had controlled trials and limited studies. One of the drugs looks to reduce the central nervous system’s sympathetic output.
This can help with people who have PTSD because their CNS output is relatively high. With controlled studies and the effects on sleep, this helps them to reduce nightmares.
Other proposed nightmare medications can be prescribed but must be closely monitored, especially with people who experience substance abuse or misuse of opioid and painkiller medications. They may be more sensitive to addictive medication and need to be mindful of what they use.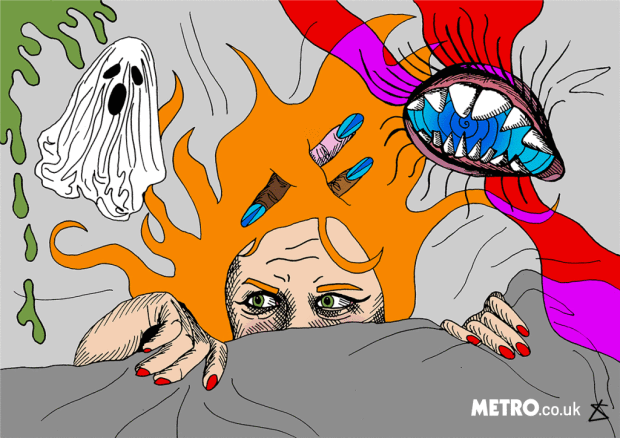
People who struggle with symptoms of PTSD often feel they are not safe or have moments of uncertainty over safety. Practicing good sleep hygiene involves adequate time for sleep.
Keeping electronic devices use to a minimum and away from the bedroom an hour before bed is most ideal. Sleeping when the body is tired is essential.
Whenever that is, let the body rest. Drop other activities for the time being that are non-essential and get rest.
Get help for substance use disorders and seek support for stress that may kick up negative feelings. Try some exercise to release stress and don’t worry about getting up and going to do things that don’t feel comfortable right now.
Helping a Loved One Through PTSDLoved ones who struggle with symptoms of PTSD can have trouble letting go. Research done on nightmares directly related to PTSD show that support is critical for them but it can be difficult to know how to help.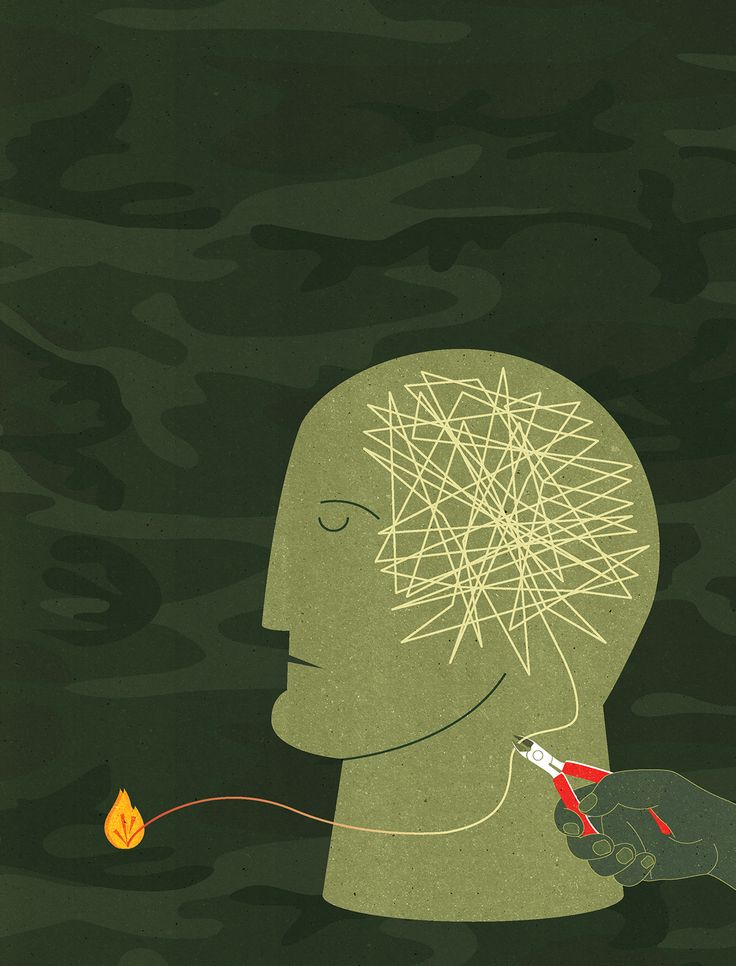
Seeking individual therapy for them is crucial. Veterans and first responders can use therapies to help align their thoughts and feelings in a different way so they view the world more openly rather than closing off and isolating themselves when they are struggling.
Alcohol and substance use disorders require dual diagnosis treatment when occurring with symptoms of PTSD. It helps to have someone come alongside and help deal with the symptoms.
Recovery groups and community support systems are also important so people know they are not alone in dealing with the reality of addiction and mental health issues.
Forge is a place to come and recover your life from addiction. We help you reimagine what is possible and create the life you’ve been dreaming of.
Call us today: 1-888-224-7312
Management of nightmares in patients with posttraumatic stress disorder: current perspectives
1. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2003. [Google Scholar]
5th ed. Washington, DC: American Psychiatric Association; 2003. [Google Scholar]
2. Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. 2013;170(4):372–382. [PMC free article] [PubMed] [Google Scholar]
3. Leskin GA, Woodward SH, Young HE, Sheikh JI. Effects of comorbid diagnoses on sleep disturbance in PTSD. J Psychiatr Res. 2002;36(6):449–452. [PubMed] [Google Scholar]
4. Heim C, Nemeroff CB. Neurobiology of posttraumatic stress disorder. CNS Spectr. 2009;14(1 Suppl 1):13–24. [PubMed] [Google Scholar]
5. Davis JL, Byrd P, Rhudy JL, Wright DC. Characteristics of chronic nightmares in a trauma-exposed treatment-seeking sample. Dreaming. 2007;17(4):187–198. [Google Scholar]
6. Detweiler MB, Arif S, Candelario J, et al. Salem VAMC-U.S. Army fort Bragg warrior transition clinic telepsychiatry collaboration: 12-month operation clinical perspective. Telemed J E Health. 2012;18(2):81–86. [PubMed] [Google Scholar]
7. Davies J.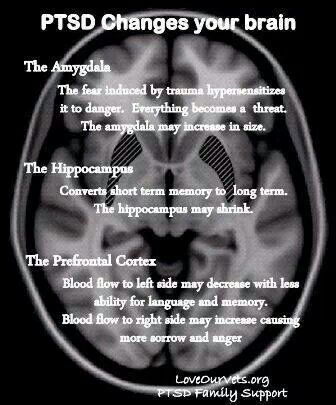 Treating Post-trauma Nightmares: A Cognitive Behavioral Approach. New York: Springer; 2009. [Google Scholar]
Treating Post-trauma Nightmares: A Cognitive Behavioral Approach. New York: Springer; 2009. [Google Scholar]
8. Clum GA, Nishith P, Resick PA. Trauma-related sleep disturbance and self-reported physical health symptoms in treatment-seeking female rape victims. J Nerv Ment Dis. 2001;189(9):618–622. [PMC free article] [PubMed] [Google Scholar]
9. Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33(1):69–74. [PMC free article] [PubMed] [Google Scholar]
10. van Liempt S, van Zuiden M, Westenberg H, Super A, Vermetten E. Impact of impaired sleep on the development of PTSD symptoms in combat veterans: a prospective longitudinal cohort study. Depress Anxiety. 2013;30(5):469–474. [PubMed] [Google Scholar]
11. Kobayashi I, Sledjeski EM, Spoonster E, Fallon WF, Delahanty DL. Effects of early nightmares on the development of sleep disturbances in motor vehicle accident victims. J Trauma Stress. 2008;21(6):548–555. [PubMed] [Google Scholar]
J Trauma Stress. 2008;21(6):548–555. [PubMed] [Google Scholar]
12. Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. 2008;12(3):169–184. [PubMed] [Google Scholar]
13. Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43(2):139–149. [PMC free article] [PubMed] [Google Scholar]
14. Sjöström N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatry Res. 2009;170(2–3):208–211. [PubMed] [Google Scholar]
15. Sjöström N, Waern M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30(1):91–95. [PubMed] [Google Scholar]
16. Panagioti M, Gooding PA, Tarrier N. A meta-analysis of the association between posttraumatic stress disorder and suicidality: the role of comorbid depression.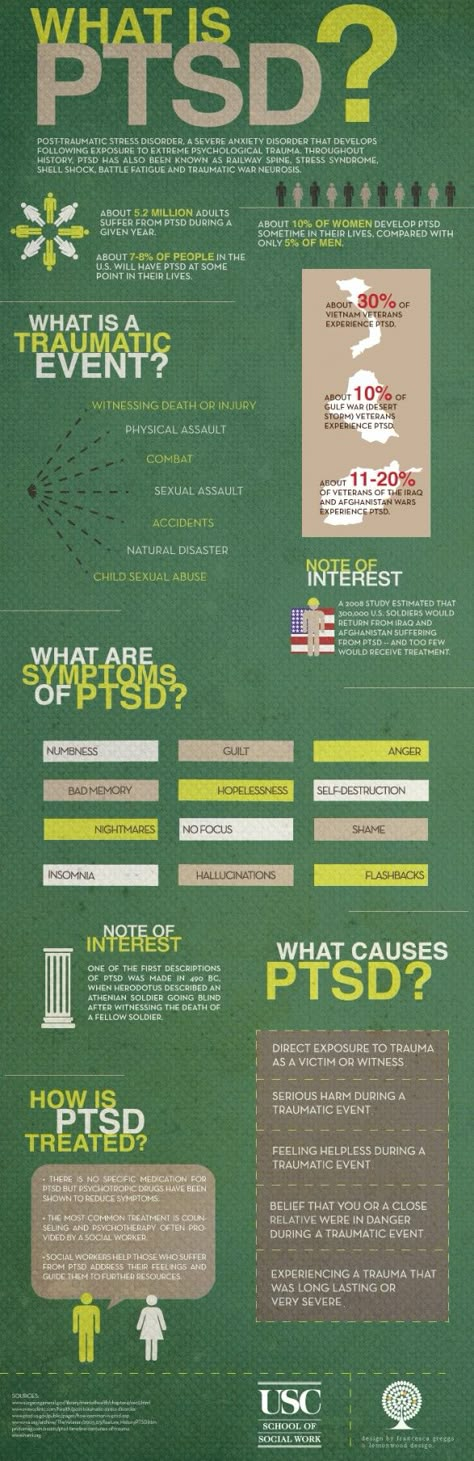 Compr Psychiatry. 2012;53(7):915–930. [PubMed] [Google Scholar]
Compr Psychiatry. 2012;53(7):915–930. [PubMed] [Google Scholar]
17. Sareen J, Houlahan T, Cox BJ, Asmundson GJ. Anxiety disorders associated with suicidal ideation and suicide attempts in the National Comorbidity Survey. J Nerv Ment Dis. 2005;193(7):450–454. [PubMed] [Google Scholar]
18. Littlewood DL, Gooding PA, Panagioti M, Kyle SD. Nightmares and suicide in posttraumatic stress disorder: the mediating role of defeat, entrapment, and hopelessness. J Clin Sleep Med. 2016;12(3):393–399. [PMC free article] [PubMed] [Google Scholar]
19. Nadorff MR, Nadorff DK, Germain A. Nightmares: under-reported, undetected, and therefore untreated. J Clin Sleep Med. 2015;11(7):747–750. [PMC free article] [PubMed] [Google Scholar]
20. Simor P, Horváth K, Gombos F, Takács KP, Bódizs R. Disturbed dreaming and sleep quality: altered sleep architecture in subjects with frequent nightmares. Eur Arch Psychiatry Clin Neurosci. 2012;262(8):687–696. [PubMed] [Google Scholar]
21. Phelps AJ, Kanaan RAA, Worsnop C, Redston S, Ralph N, Forbes D.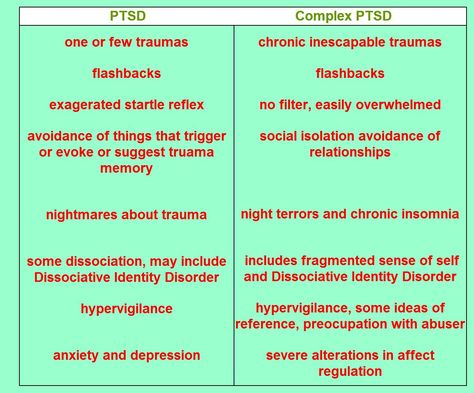 An ambulatory polysomnography study of the post-traumatic nightmares of post-traumatic stress disorder. Sleep. 2018;41(1) [PubMed] [Google Scholar]
An ambulatory polysomnography study of the post-traumatic nightmares of post-traumatic stress disorder. Sleep. 2018;41(1) [PubMed] [Google Scholar]
22. Tamanna S, Parker JD, Lyons J, Ullah MI. The effect of continuous positive air pressure (CPAP) on nightmares in patients with post-traumatic stress disorder (PTSD) and obstructive sleep apnea (OSA. J Clin Sleep Med. 2014;10(6):631–636. [PMC free article] [PubMed] [Google Scholar]
23. Committee on the Assessment of Ongoing Effects in the Treatment of Posttraumatic Stress Disorder; Institute of Medicine . Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations. Washington, DC: National Academies Press; 2012. [Google Scholar]
24. Foa EB, Steketee G, Rothbaum BO. Behavioral/cognitive conceptualizations of post-traumatic stress disorder. Behav Ther. 1989;20:155–176. [Google Scholar]
25. Marks I. Rehearsal relief of a nightmare. Br J Psychiatry. 1978;133(5):461–465. [PubMed] [Google Scholar]
26. Krakow B, Zadra A. Clinical management of chronic nightmares: imagery rehearsal therapy. Behav Sleep Med. 2006;4(1):45–70. [PubMed] [Google Scholar]
Krakow B, Zadra A. Clinical management of chronic nightmares: imagery rehearsal therapy. Behav Sleep Med. 2006;4(1):45–70. [PubMed] [Google Scholar]
27. Augedal AW, Hansen KS, Kronhaug CR, Harvey AG, Pallesen S. Randomized controlled trials of psychological and pharmacological treatments for nightmares: a meta-analysis. Sleep Med Rev. 2013;17(2):143–152. [PubMed] [Google Scholar]
28. Hansen K, Höfling V, Kröner-Borowik T, Stangier U, Steil R. Efficacy of psychological interventions aiming to reduce chronic nightmares: a meta-analysis. Clin Psychol Rev. 2013;33(1):146–155. [PubMed] [Google Scholar]
29. Krakow B, Hollifield M, Johnston L, et al. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA. 2001;286(5):537–545. [PubMed] [Google Scholar]
30. Krakow B, Kellner R, Neidhardt J, Pathak D, Lambert L. Imagery rehearsal treatment of chronic nightmares: with a thirty month followup.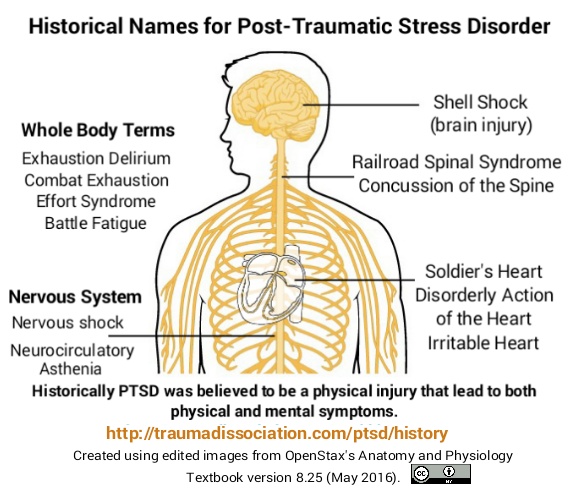 J Behav Ther Exp Psychiatry. 1993;24(4):325–330. [PubMed] [Google Scholar]
J Behav Ther Exp Psychiatry. 1993;24(4):325–330. [PubMed] [Google Scholar]
31. Thünker J, Pietrowsky R. Effectiveness of a manualized imagery rehearsal therapy for patients suffering from nightmare disorders with and without a comorbidity of depression or PTSD. Behav Res Ther. 2012;50(9):558–564. [PubMed] [Google Scholar]
32. Forbes D, Phelps AJ, McHugh AF, Debenham P, Hopwood M, Creamer M. Imagery rehearsal in the treatment of posttraumatic nightmares in Australian veterans with chronic combat-related PTSD: 12-month follow-up data. J Trauma Stress. 2003;16(5):509–513. [PubMed] [Google Scholar]
33. Nappi CM, Drummond SP, Thorp SR, McQuaid JR. Effectiveness of imagery rehearsal therapy for the treatment of combat-related nightmares in veterans. Behav Ther. 2010;41(2):237–244. [PubMed] [Google Scholar]
34. Cook JM, Harb GC, Gehrman PR, et al. Imagery rehearsal for post-traumatic nightmares: a randomized controlled trial. J Trauma Stress. 2010;23(5):553–563. [PubMed] [Google Scholar]
35. Lu M, Wagner A, Van Male L, Whitehead A, Boehnlein J. Imagery rehearsal therapy for posttraumatic nightmares in U.S. veterans. J Trauma Stress. 2009;22(3):236–239. [PubMed] [Google Scholar]
Lu M, Wagner A, Van Male L, Whitehead A, Boehnlein J. Imagery rehearsal therapy for posttraumatic nightmares in U.S. veterans. J Trauma Stress. 2009;22(3):236–239. [PubMed] [Google Scholar]
36. Casement MD, Swanson LM. A meta-analysis of imagery rehearsal for post-trauma nightmares: effects on nightmare frequency, sleep quality, and posttraumatic stress. Clin Psychol Rev. 2012;32(6):566–574. [PMC free article] [PubMed] [Google Scholar]
37. Harb GC, Phelps AJ, Forbes D, Ross RJ, Gehrman PR, Cook JM. A critical review of the evidence base of imagery rehearsal for post-traumatic nightmares: pointing the way for future research. J Trauma Stress. 2013;26(5):570–579. [PubMed] [Google Scholar]
38. Manber R, Carney C, Edinger J, et al. Dissemination of CBTI to the non-sleep specialist: protocol development and training issues. J Clin Sleep Med. 2012;8(2):209–218. [PMC free article] [PubMed] [Google Scholar]
39. Zayfert C, Deviva JC. Residual insomnia following cognitive behavioral therapy for PTSD. J Trauma Stress. 2004;17(1):69–73. [PubMed] [Google Scholar]
J Trauma Stress. 2004;17(1):69–73. [PubMed] [Google Scholar]
40. Davis JL, Wright DC. Exposure, relaxation, and rescripting treatment for trauma-related nighmares. J Trauma Dissociation. 2006;7(1):5–18. [PubMed] [Google Scholar]
41. Davis JL, Wright DC. Randomized clinical trial for treatment of chronic nightmares in trauma-exposed adults. J Trauma Stress. 2007;20(2):123–133. [PubMed] [Google Scholar]
42. Davis JL, Rhudy JL, Pruiksma KE, et al. Physiological predictors of response to exposure, relaxation, and rescripting therapy for chronic nightmares in a randomized clinical trial. J Clin Sleep Med. 2011;7(6):622–631. [PMC free article] [PubMed] [Google Scholar]
43. Balliett NE, Davis JL, Miller KE. Efficacy of a brief treatment for nightmares and sleep disturbances for veterans. Psychol Trauma. 2015;7(6):507–515. [PubMed] [Google Scholar]
44. Ho FY, Chan CS, Tang KN. Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2016;43:90–102. [PubMed] [Google Scholar]
Clin Psychol Rev. 2016;43:90–102. [PubMed] [Google Scholar]
45. Rhudy JL, Davis JL, Williams AE, et al. Cognitive-behavioral treatment for chronic nightmares in trauma-exposed persons: assessing physiological reactions to nightmare-related fear. J Clin Psychol. 2010;66(4):365–382. [PubMed] [Google Scholar]
46. Pruiksma KE, Cranston CC, Rhudy JL, Micol RL, Davis JL. Randomized controlled trial to dismantle exposure, relaxation, and rescripting therapy (ERRT) for trauma-related nightmares. Psychol Trauma. 2018;10(1):67–75. [PubMed] [Google Scholar]
47. Wolpe J. Behavioral Therapy Techniques. New York: Pergamon Press; 1967. [Google Scholar]
48. Cellucci AJ, Lawrence PS. The efficacy of systematic desensi-tization in reducing nightmares. J Behav Ther Exp Psychiatry. 1978;9(2):109–114. [Google Scholar]
49. Kellner R, Neidhardt J, Krakow B, Pathak D. Changes in chronic nightmares after one session of desensitization or rehearsal instructions. Am J Psychiatry. 1992;149(5):659–663. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
50. Miller WR, Dipilato M. Treatment of nightmares via relaxation and desensitization: a controlled evaluation. J Consult Clin Psychol. 1983;51(6):870–877. [PubMed] [Google Scholar]
51. Shapiro F. Eye movement desensitization: a new treatment for post-traumatic stress disorder. J Behav Ther Exp Psychiatry. 1989;20(3):211–217. [PubMed] [Google Scholar]
52. Wilson DL, Silver SM, Covi WG, Foster S. Eye movement desensitization and reprocessing: effectiveness and autonomic correlates. J Behav Ther Exp Psychiatry. 1996;27(3):219–229. [PubMed] [Google Scholar]
53. Cusack K, Jonas DE, Forneris CA, et al. Psychological treatments for adults with posttraumatic stress disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2016;43:128–141. [PubMed] [Google Scholar]
54. Silver SM, Brooks A, Obenchain J. Treatment of Vietnam War veterans with PTSD: a comparison of eye movement desensitization and reprocessing, biofeedback, and relaxation training. J Trauma Stress. 1995;8(2):337–342. [PubMed] [Google Scholar]
J Trauma Stress. 1995;8(2):337–342. [PubMed] [Google Scholar]
55. Van Eeden F. A study of dreams. PSPR. 1913;26:431–461. [Google Scholar]
56. Harb GC, Greene JL, Dent KM, Ross RJ. 1077 Lucid dreaming in veterans with PTSD: non-nightmare dreams and nightmares. Sleep. 2017;40(suppl_1):A401. [Google Scholar]
57. Dudai Y. The neurobiology of consolidations, or, how stable is the engram? Annu Rev Psychol. 2004;55(1):51–86. [PubMed] [Google Scholar]
58. Dębiec J, Bush DE, Ledoux JE. Noradrenergic enhancement of reconsolidation in the amygdala impairs extinction of conditioned fear in rats – a possible mechanism for the persistence of traumatic memories in PTSD. Depress Anxiety. 2011;28(3):186–193. [PMC free article] [PubMed] [Google Scholar]
59. Gazarini L, Stern CA, Carobrez AP, Bertoglio LJ. Enhanced noradrenergic activity potentiates fear memory consolidation and reconsolidation by differentially recruiting α1- and β-adrenergic receptors. Learn Mem. 2013;20(4):210–219. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
60. Raskind MA, Dobie DJ, Kanter ED, Petrie EC, Thompson CE, Peskind ER. The alpha1-adrenergic antagonist prazosin ameliorates combat trauma nightmares in veterans with posttraumatic stress disorder: a report of 4 cases. J Clin Psychiatry. 2000;61(2):129–134. [PubMed] [Google Scholar]
61. Raskind MA, Thompson C, Petrie EC, et al. Prazosin reduces nightmares in combat veterans with posttraumatic stress disorder. J Clin Psychiatry. 2002;63(7):565–568. [PubMed] [Google Scholar]
62. Taylor F, Raskind MA. The alpha1-adrenergic antagonist prazosin improves sleep and nightmares in civilian trauma posttraumatic stress disorder. J Clin Psychopharmacol. 2002;22(1):82–85. [PubMed] [Google Scholar]
63. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003–1010. [PubMed] [Google Scholar]
64. Germain A, Richardson R, Moul DE, et al.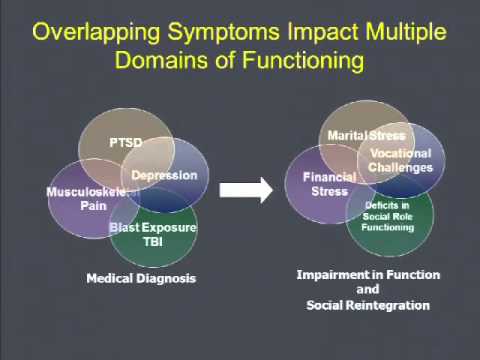 Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US Military Veterans. J Psychosom Res. 2012;72(2):89–96. [PMC free article] [PubMed] [Google Scholar]
Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US Military Veterans. J Psychosom Res. 2012;72(2):89–96. [PMC free article] [PubMed] [Google Scholar]
65. Khachatryan D, Groll D, Booij L, Sepehry AA, Schütz CG. Prazosin for treating sleep disturbances in adults with posttraumatic stress disorder: a systematic review and meta-analysis of randomized controlled trials. Gen Hosp Psychiatry. 2016;39:46–52. [PubMed] [Google Scholar]
66. Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507–517. [PubMed] [Google Scholar]
67. Koola MM, Varghese SP, Fawcett JA. High-dose prazosin for the treatment of post-traumatic stress disorder. Ther Adv Psychopharmacol. 2014;4(1):43–47. [PMC free article] [PubMed] [Google Scholar]
68. Morgenthaler TI, Auerbach S, Casey KR, et al. Position paper for the treatment of nightmare disorder in adults: an American Academy of Sleep Medicine position paper.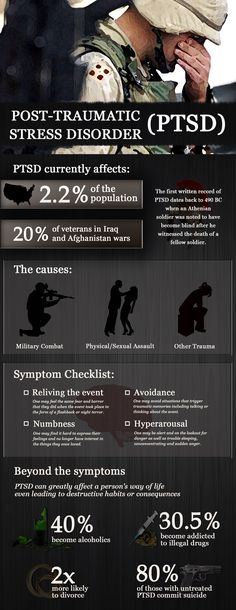 J Clin Sleep Med. 2018;14(6):1041–1055. [PMC free article] [PubMed] [Google Scholar]
J Clin Sleep Med. 2018;14(6):1041–1055. [PMC free article] [PubMed] [Google Scholar]
69. Nirmalani-Gandhy A, Sanchez D, Catalano G. Terazosin for the treatment of trauma-related nightmares: a report of 4 cases. Clin Neuropharmacol. 2015;38(3):109–111. [PubMed] [Google Scholar]
70. Salviati M, Pallagrosi M, Valeriani G, Carlone C, Todini L, Biondi M. On the role of noradrenergic system in PTSD and related sleep disturbances. The use of terazosin in PTSD related nightmares: a case report. Clin Ter. 2013;164(2):133–137. [PubMed] [Google Scholar]
71. Detweiler M, Pagadala B, Candelario J, Boyle J, Detweiler J, Lutgens B. Treatment of post-traumatic stress disorder nightmares at a veterans affairs medical center. J Clin Med. 2016;5(12):117. [PMC free article] [PubMed] [Google Scholar]
72. Sethi R, Vasudeva S. Doxazosin for the treatment of nightmares: does it really work? A case report. Prim Care Companion CNS Disord. 2012;14(5) [PMC free article] [PubMed] [Google Scholar]
73. Roepke S, Danker-Hopfe H, Repantis D, et al. Doxazosin, an alpha-1-adrenergic-receptor antagonist, for nightmares in patients with posttraumatic stress disorder and/or borderline personality disorder: a chart review. Pharmacopsychiatry. 2017;50(1):26–31. [PubMed] [Google Scholar]
Roepke S, Danker-Hopfe H, Repantis D, et al. Doxazosin, an alpha-1-adrenergic-receptor antagonist, for nightmares in patients with posttraumatic stress disorder and/or borderline personality disorder: a chart review. Pharmacopsychiatry. 2017;50(1):26–31. [PubMed] [Google Scholar]
74. Alao A, Selvarajah J, Razi S. The use of clonidine in the treatment of nightmares among patients with co-morbid PTSD and traumatic brain injury. Int J Psychiatry Med. 2012;44(2):165–169. [PubMed] [Google Scholar]
75. Kinzie JD, Leung P. Clonidine in Cambodian patients with posttraumatic stress disorder. J Nerv Ment Dis. 1989;177(9):546–550. [PubMed] [Google Scholar]
76. Boehnlein JK, Kinzie JD, Sekiya U, Riley C, Pou K, Rosborough B. A ten-year treatment outcome study of traumatized cambodian refugees. J Nerv Ment Dis. 2004;192(10):658–663. [PubMed] [Google Scholar]
77. Wendell K, Maxwell M. Evaluation of clonidine and prazosin for the treatment of nightime post traumatic stres disorder symptoms. Fed Pract. 2015:8–14. [Google Scholar]
78. Graham RL, Leckband S, Endow-Eyer R. PTSD nightmares: prazosin and atypical antipsychotics. Curr Psychiatr. 2012;11:59–62. [Google Scholar]
79. Schotte A, Janssen PF, Gommeren W, et al. Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology. 1996;124(1–2):57–73. [PubMed] [Google Scholar]
80. Richelson E. Receptor pharmacology of neuroleptics: relation to clinical effects. J Clin Psychiatry. 1999;60(Suppl 10):5–14. [PubMed] [Google Scholar]
81. David D, De Faria L, Mellman TA. Adjunctive risperidone treatment and sleep symptoms in combat veterans with chronic PTSD. Depress Anxiety. 2006;23(8):489–491. [PubMed] [Google Scholar]
82. Stanovic JK, James KA, Vandevere CA. The effectiveness of risperidone on acute stress symptoms in adult burn patients: a preliminary retrospective pilot study. J Burn Care Rehabil. 2001;22(3):210–213. [PubMed] [Google Scholar]
83. Khachiyants N, Ali R, Kovesdy CP, Detweiler JG, Kim KY, Detweiler MB. Effectiveness of risperidone for the treatment of nightmares in veterans with posttraumatic stress disorder. J Clin Psychopharmacol. 2010;30(6):735–737. [PubMed] [Google Scholar]
Khachiyants N, Ali R, Kovesdy CP, Detweiler JG, Kim KY, Detweiler MB. Effectiveness of risperidone for the treatment of nightmares in veterans with posttraumatic stress disorder. J Clin Psychopharmacol. 2010;30(6):735–737. [PubMed] [Google Scholar]
84. Jakovljević M, Sagud M, Mihaljević-Peles A. Olanzapine in the treatment-resistant, combat-related PTSD--a series of case reports. Acta Psychiatr Scand. 2003;107(5):394–396. [PubMed] [Google Scholar]
85. Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry. 2002;159(10):1777–1779. [PubMed] [Google Scholar]
86. Butterfield MI, Becker ME, Connor KM, Sutherland S, Churchill LE, Davidson JRT. Olanzapine in the treatment of post-traumatic stress disorder: a pilot study. Int Clin Psychopharmacol. 2001;16(4):197–203. [PubMed] [Google Scholar]
87. Deng C, Weston-Green K, Huang XF. The role of histaminergic h2 and h4 receptors in food intake: a mechanism for atypical antipsychotic-induced weight gain? Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(1):1–4. [PubMed] [Google Scholar]
2010;34(1):1–4. [PubMed] [Google Scholar]
88. Weston-Green K, Huang XF, Deng C. Alterations to melanocortinergic, GABAergic and cannabinoid neurotransmission associated with olanzapine-induced weight gain. PLoS One. 2012;7(3):e33548. [PMC free article] [PubMed] [Google Scholar]
89. Robert S, Hamner MB, Kose S, Ulmer HG, Deitsch SE, Lorberbaum JP. Quetiapine improves sleep disturbances in combat veterans with PTSD: sleep data from a prospective, open-label study. J Clin Psychopharmacol. 2005;25(4):387–388. [PubMed] [Google Scholar]
90. Britnell SR, Jackson AD, Brown JN, Capehart BP. Aripiprazole for post-traumatic stress disorder: a systematic review. Clin Neuropharmacol. 2017;40(6):273–278. [PubMed] [Google Scholar]
91. Lambert MT. Aripiprazole in the management of post-traumatic stress disorder symptoms in returning Global War on Terrorism veterans. Int Clin Psychopharmacol. 2006;21(3):185–187. [PubMed] [Google Scholar]
92. Dillard ML, Bendfeldt F, Jernigan P.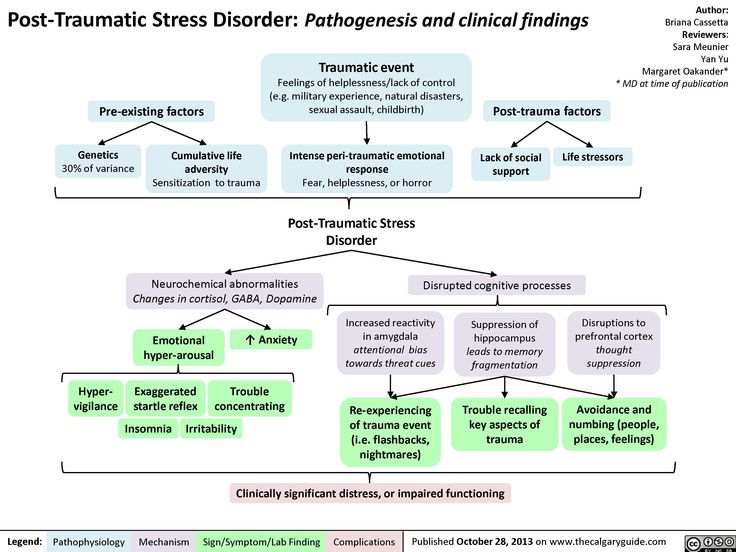 Use of thioridazine in post-traumatic stress disorder. South Med J. 1993;86(11):1276–1278. [PubMed] [Google Scholar]
Use of thioridazine in post-traumatic stress disorder. South Med J. 1993;86(11):1276–1278. [PubMed] [Google Scholar]
93. De Boer M, Op den Velde W, Falger PJ, Hovens JE, de Groen JH, van Duijn H. Fluvoxamine treatment for chronic PTSD: a pilot study. Psychother Psychosom. 1992;57(4):158–163. [PubMed] [Google Scholar]
94. Neylan TC, Metzler TJ, Schoenfeld FB, et al. Fluvoxamine and sleep disturbances in posttraumatic stress disorder. J Trauma Stress. 2001;14(3):461–467. [PubMed] [Google Scholar]
95. Lepkifker E, Dannon PN, Iancu I, Ziv R, Kotler M. Nightmares related to fluoxetine treatment. Clin Neuropharmacol. 1995;18(1):90–94. [PubMed] [Google Scholar]
96. Arora G, Sandhu G, Fleser C. Citalopram and nightmares. J Neuropsychiatry Clin Neurosci. 2012;24(2):E43. [PubMed] [Google Scholar]
97. Lewis JD. Mirtazapine for PTSD nightmares. Am J Psychiatry. 2002;159(11):1948–1949. [PubMed] [Google Scholar]
98. Mathews M, Basil B, Evcimen H, Adetunji B, Joseph S. Mirtazapine-induced nightmares. Prim Care Companion J Clin Psychiatry. 2006;8(5):311. [PMC free article] [PubMed] [Google Scholar]
Mirtazapine-induced nightmares. Prim Care Companion J Clin Psychiatry. 2006;8(5):311. [PMC free article] [PubMed] [Google Scholar]
99. Menon V, Madhavapuri P. Low-Dose mirtazapine-induced nightmares necessitating its discontinuation in a young adult female. J Pharmacol Pharmacother. 2017;8(4):182–184. [PMC free article] [PubMed] [Google Scholar]
100. Rottach KG, Schaner BM, Kirch MH, et al. Restless legs syndrome as side effect of second generation antidepressants. J Psychiatr Res. 2008;43(1):70–75. [PubMed] [Google Scholar]
101. Neylan TC, Lenoci M, Maglione ML, et al. The effect of nefazodone on subjective and objective sleep quality in posttraumatic stress disorder. J Clin Psychiatry. 2003;64(4):445–450. [PubMed] [Google Scholar]
102. Davidson JR, Weisler RH, Malik ML, Connor KM. Treatment of post-traumatic stress disorder with nefazodone. Int Clin Psychopharmacol. 1998;13(3):111–114. [PubMed] [Google Scholar]
103. Boehnlein JK, Kinzie JD, Ben R, Fleck J. One-year follow-up study of posttraumatic stress disorder among survivors of Cambodian concentration camps. Am J Psychiatry. 1985;142(8):956–959. [PubMed] [Google Scholar]
One-year follow-up study of posttraumatic stress disorder among survivors of Cambodian concentration camps. Am J Psychiatry. 1985;142(8):956–959. [PubMed] [Google Scholar]
104. Warner MD, Dorn MR, Peabody CA. Survey on the usefulness of trazodone in patients with PTSD with insomnia or nightmares. Pharmacopsychiatry. 2001;34(4):128–131. [PubMed] [Google Scholar]
105. Harsch HH. Cyproheptadine for recurrent nightmares. Am J Psychiatry. 1986;143(11):1491–1492. [PubMed] [Google Scholar]
106. Brophy MH. Cyproheptadine for combat nightmares in post-traumatic stress disorder and dream anxiety disorder. Mil Med. 1991;156(2):100–101. [PubMed] [Google Scholar]
107. Gupta S, Popli A, Bathurst E, Hennig L, Droney T, Keller P. Efficacy of cyproheptadine for nightmares associated with posttraumatic stress disorder. Compr Psychiatry. 1998;39(3):160–164. [PubMed] [Google Scholar]
108. Clark RD, Canive JM, Calais LA, Qualls C, Brugger RD, Vosburgh TB. Cyproheptadine treatment of nightmares associated with posttraumatic stress disorder. J Clin Psychopharmacol. 1999;19(5):486–487. [PubMed] [Google Scholar]
J Clin Psychopharmacol. 1999;19(5):486–487. [PubMed] [Google Scholar]
109. Abrams TE, Lund BC, Bernardy NC, Friedman MJ. Aligning clinical practice to PTSD treatment guidelines: medication prescribing by provider type. Psychiatr Serv. 2013;64(2):142–148. [PubMed] [Google Scholar]
110. Greenbaum MA, Neylan TC, Rosen CS. Symptom presentation and prescription of sleep medications for veterans with posttraumatic stress disorder. J Nerv Ment Dis. 2017;205(2):1–118. [PubMed] [Google Scholar]
111. Guina J, Rossetter SR, Derhodes BJ, Nahhas RW, Welton RS. Benzodiazepines for PTSD: a systematic review and meta-analysis. J Psychiatr Pract. 2015;21(4):281–303. [PubMed] [Google Scholar]
112. Braun P, Greenberg D, Dasberg H, Lerer B. Core symptoms of post-traumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry. 1990;51(6):236–238. [PubMed] [Google Scholar]
113. Cates ME, Bishop MH, Davis LL, Lowe JS, Woolley TW. Clonazepam for treatment of sleep disturbances associated with combat-related posttraumatic stress disorder. Ann Pharmacother. 2004;38(9):1395–1399. [PubMed] [Google Scholar]
Ann Pharmacother. 2004;38(9):1395–1399. [PubMed] [Google Scholar]
114. Abramowitz EG, Barak Y, Ben-Avi I, Knobler HY. Hypnotherapy in the treatment of chronic combat-related PTSD patients suffering from insomnia: a randomized, zolpidem-controlled clinical trial. Int J Clin Exp Hypn. 2008;56(3):270–280. [PubMed] [Google Scholar]
115. Passie T, Emrich HM, Karst M, Brandt SD, Halpern JH. Mitigation of post-traumatic stress symptoms by Cannabis resin: a review of the clinical and neurobiological evidence. Drug Test Anal. 2012;4(7–8):649–659. [PubMed] [Google Scholar]
116. Greer GR, Grob CS, Halberstadt AL. PTSD symptom reports of patients evaluated for the New Mexico Medical Cannabis Program. J Psychoactive Drugs. 2014;46(1):73–77. [PubMed] [Google Scholar]
117. Zuardi AW. Cannabidiol: from an inactive cannabinoid to a drug with wide spectrum of action. Rev Bras Psiquiatr. 2008;30(3):271–280. [PubMed] [Google Scholar]
118. Fraser GA. The use of a synthetic cannabinoid in the management of treatment-resistant nightmares in posttraumatic stress disorder (PTSD) CNS Neurosci Ther. 2009;15(1):84–88. [PMC free article] [PubMed] [Google Scholar]
2009;15(1):84–88. [PMC free article] [PubMed] [Google Scholar]
119. Jetly R, Heber A, Fraser G, Boisvert D. The efficacy of nabilone, a synthetic cannabinoid, in the treatment of PTSD-associated nightmares: a preliminary randomized, double-blind, placebo-controlled cross-over design study. Psychoneuroendocrinology. 2015;51:585–588. [PubMed] [Google Scholar]
120. Jinwala FN, Gupta M. Synthetic cannabis and respiratory depression. J Child Adolesc Psychopharmacol. 2012;22(6):459–462. [PubMed] [Google Scholar]
121. Sweeney B, Talebi S, Toro D, et al. Hyperthermia and severe rhabdomyolysis from synthetic cannabinoids. Am J Emerg Med. 2016;34(1):121.e1–121.e2. [PubMed] [Google Scholar]
122. Takematsu M, Hoffman RS, Nelson LS, Schechter JM, Moran JH, Wiener SW. A case of acute cerebral ischemia following inhalation of a synthetic cannabinoid. Clin Toxicol. 2014;52(9):973–975. [PubMed] [Google Scholar]
123. Lapoint J, James LP, Moran CL, Nelson LS, Hoffman RS, Moran JH. Severe toxicity following synthetic cannabinoid ingestion. Clin Toxicol. 2011;49(8):760–764. [PMC free article] [PubMed] [Google Scholar]
Severe toxicity following synthetic cannabinoid ingestion. Clin Toxicol. 2011;49(8):760–764. [PMC free article] [PubMed] [Google Scholar]
124. MacFarlane V, Christie G. Synthetic cannabinoid withdrawal: a new demand on detoxification services. Drug Alcohol Rev. 2015;34(2):147–153. [PubMed] [Google Scholar]
125. Rodgman CJ, Verrico CD, Worthy RB, Lewis EE. Inpatient detoxification from a synthetic cannabinoid and control of postdetoxification cravings with naltrexone. Prim Care Companion CNS Disord. 2014;16(4) [PMC free article] [PubMed] [Google Scholar]
126. Degenhardt L, Hall W. Is cannabis use a contributory cause of psychosis? Can J Psychiatry. 2006;51(9):556–565. [PubMed] [Google Scholar]
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.
This booklet deals with signs,
symptoms and treatments for PTSD.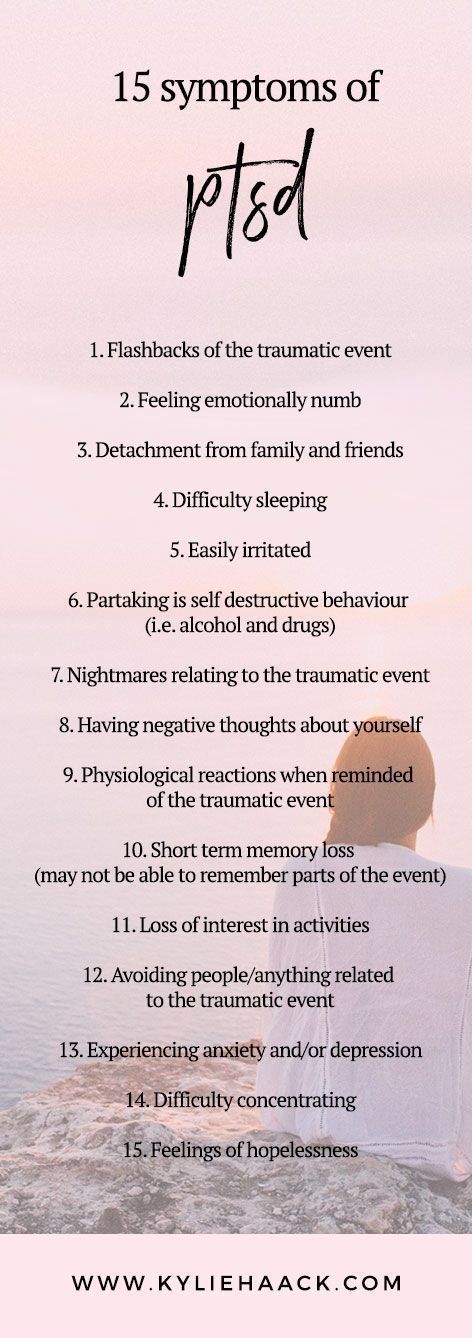
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident.
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension.
PTSD is a very serious condition that needs to be treated.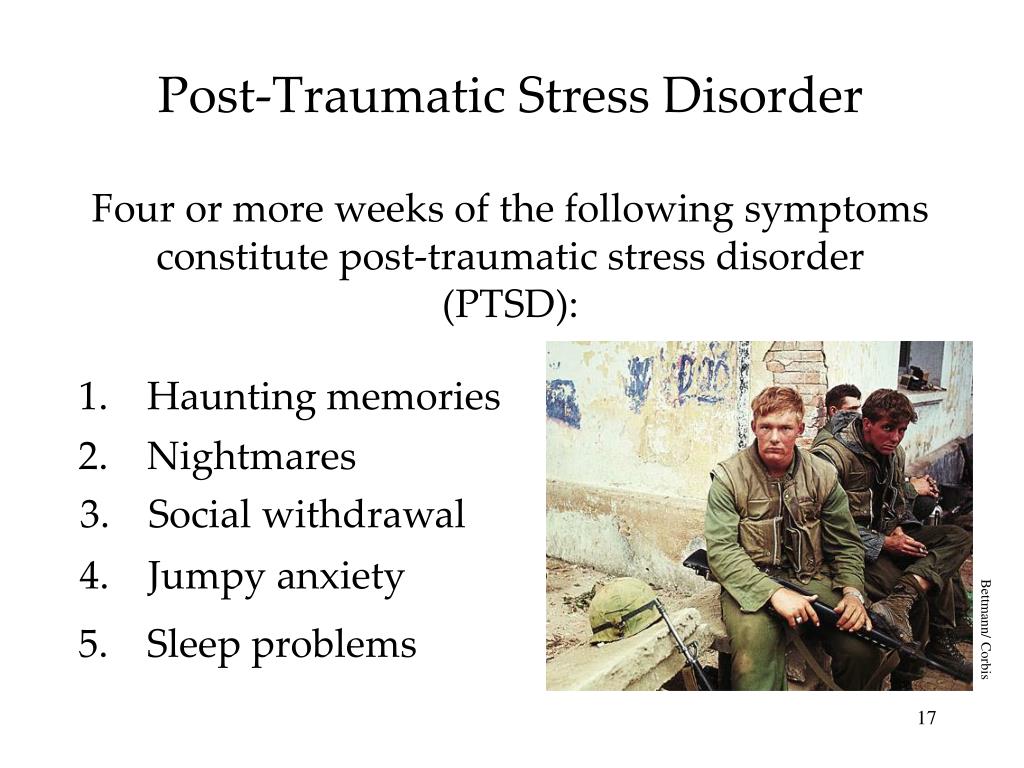
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment.
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event. you try to hold on away from anything that might remind you of the experience.
you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last?
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this condition?
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men.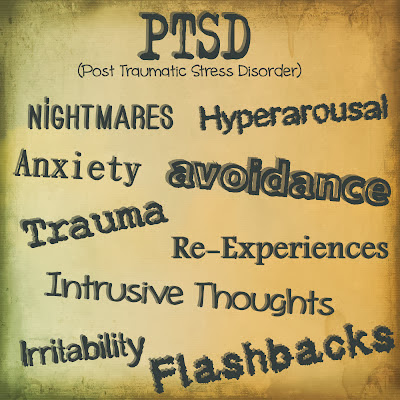 The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
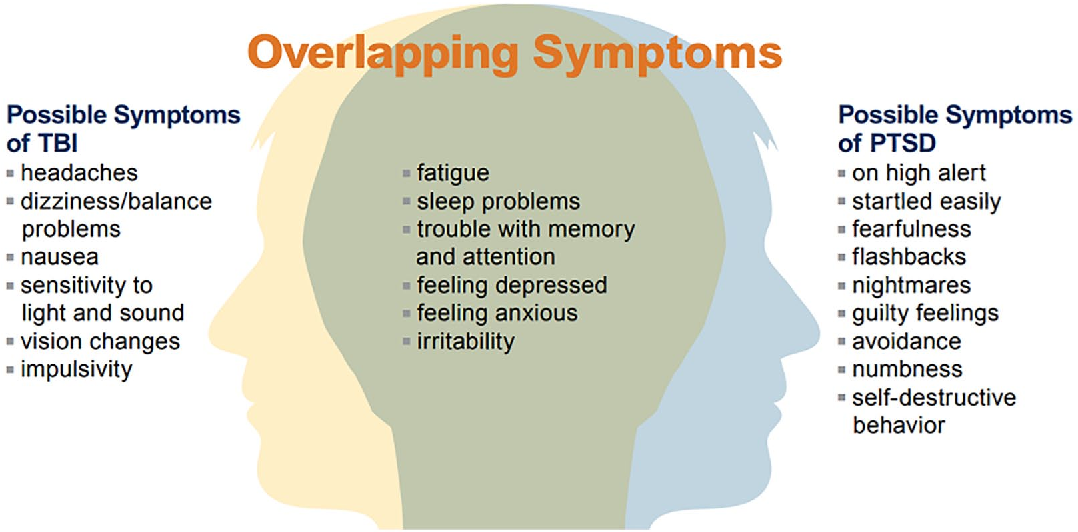
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD.
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What should I do to help myself in this situation?
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
Your doctor may prescribe medicine to help reduce your fear or tension.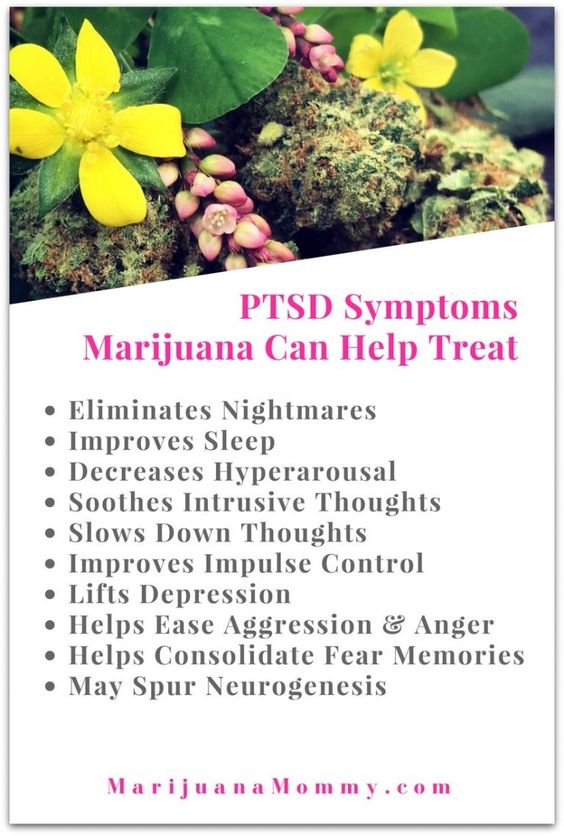 However, it should be borne in mind that usually several weeks before the medicine starts to work.
However, it should be borne in mind that usually several weeks before the medicine starts to work.
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military. MST can happen with men and women, and can occur in peacetime, during war training or during the war.
MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear. The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). 4
4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress. 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.
7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.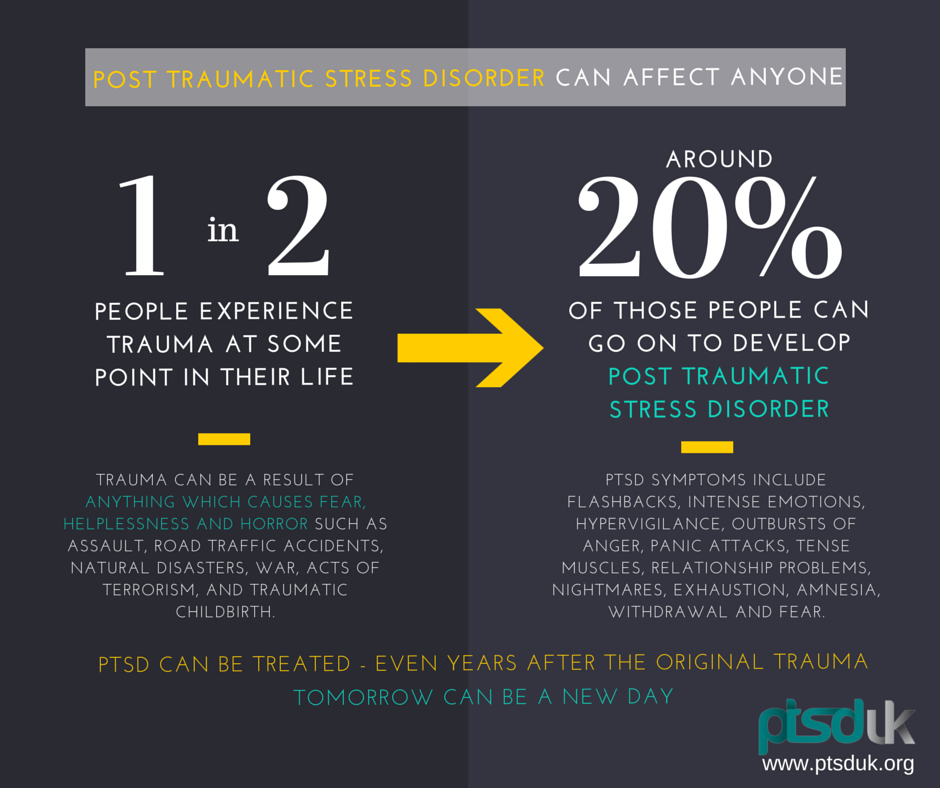
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate.
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced. NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced. 9
9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation.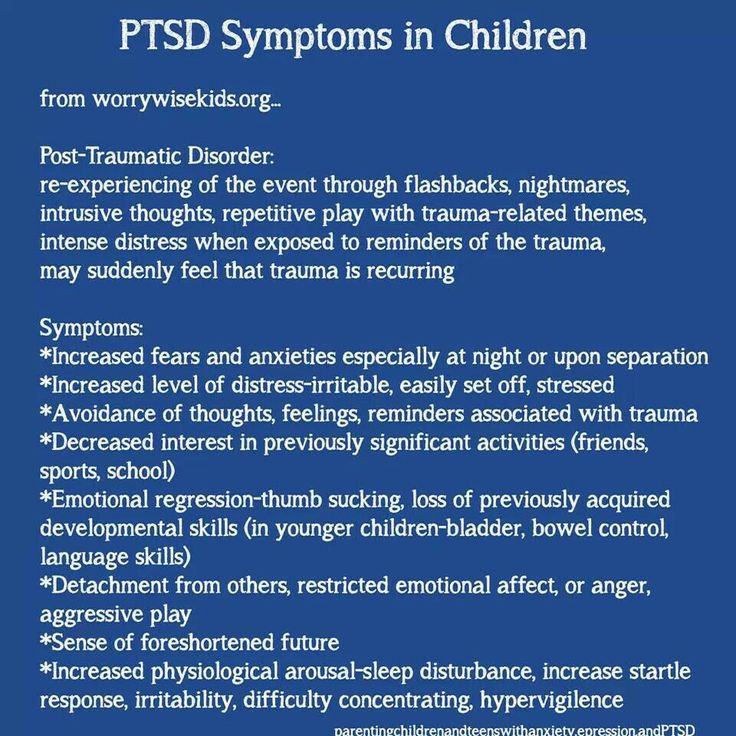 First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal.
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease.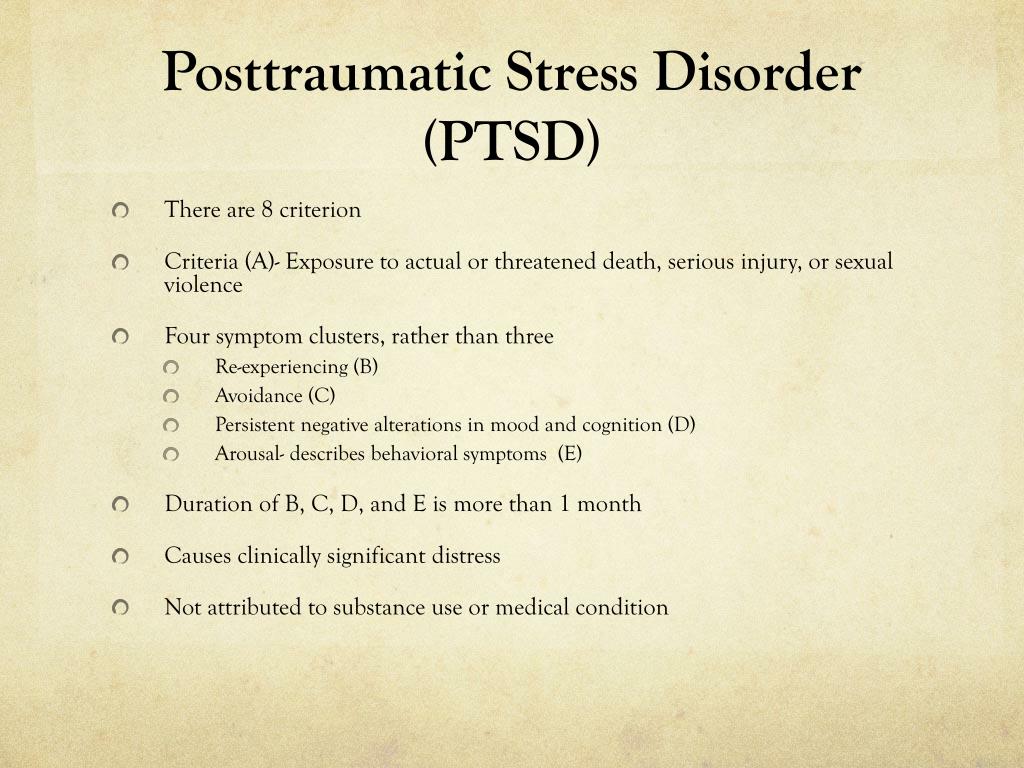 During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: nimhinfo@nih.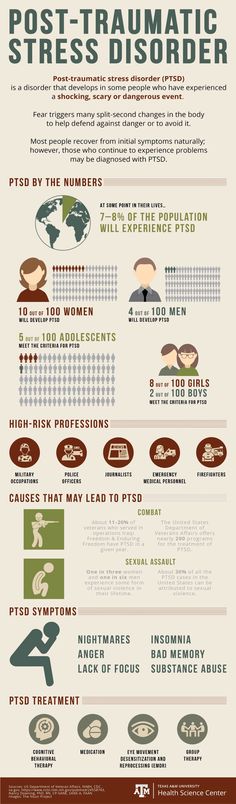 gov
gov
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www.ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction.
 Nature. Nov 7 2002;420(6911):70-74.
Nature. Nov 7 2002;420(6911):70-74. - 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus. Nat Neurosci. Mar 2005;8(3):365-371.
- Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711.
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder.
 Biol Psychiatry. Feb 3 2006.
Biol Psychiatry. Feb 3 2006. - Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
- Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634.
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F. Hogan, PhD
Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Division of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www.omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Division of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
Post-traumatic stress disorder (PTSD) | English translation
However, most people realize what has happened after a few weeks, sometimes a little longer, and then their symptoms will begin to disappear.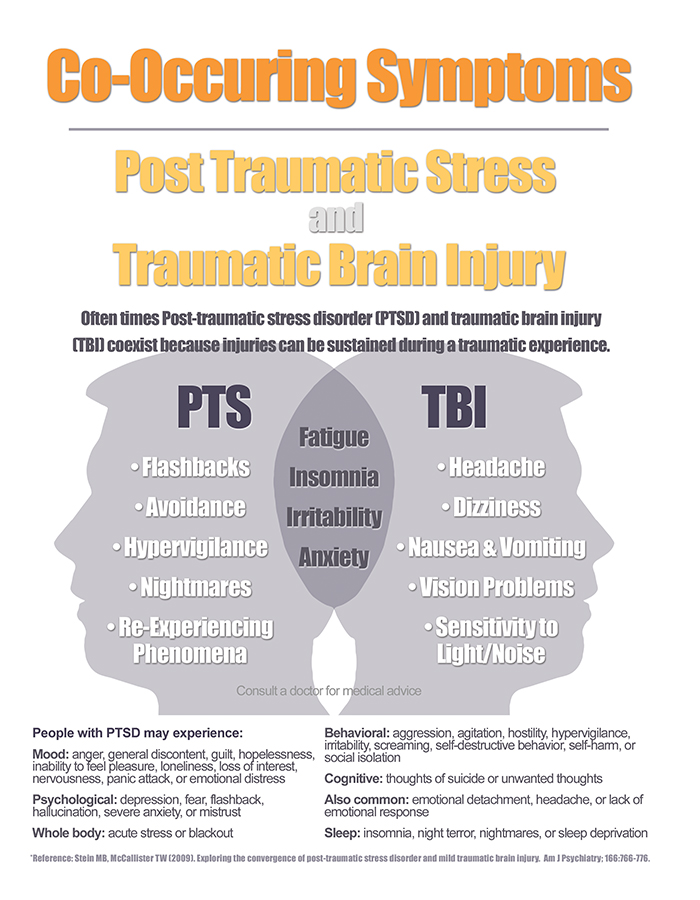
Research shows that certain groups of people are at increased risk of developing post-traumatic stress disorder. The risk of developing post-traumatic stress disorder is reduced when a person has:
Any traumatic event can cause PTSD, although the more severe the shock, the more likely it is to develop PTSD. For example, PTSD is more likely to develop if the event:
- is sudden and unexpected
- lasts for a long time
- happens when you are caught in a trap that you cannot get out of
- was caused by people
- causes a lot of death
- causes injury
- includes children
If you are still stressed and in an uncertain state, it will be difficult to get rid of the symptoms of PTSD.
How do I know that I have overcome a traumatic experience?
You may have already gotten over the traumatic event if you can:
- think about it without worrying
- not feel like you are under constant threat
- not think about it all the time
Why is PTSD not always diagnosed?
There are a number of reasons why a person with PTSD may not be diagnosed.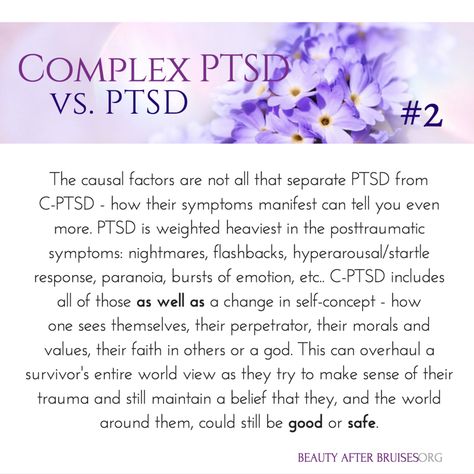
Stigma and misunderstanding
People with PTSD often avoid talking about their feelings to avoid thinking about the traumatic event.
Some people believe that the symptoms they are experiencing (such as avoidance or emotional numbness) help them cope and do not realize that they are caused by PTSD.
When people are very ill, it is difficult for them to believe that they are able to feel the way they did before the traumatic event. This may discourage them from getting help.
There is also a common misconception that only military personnel suffer from PTSD. In fact, PTSD can happen to anyone, and any experience of PTSD is real.
Misdiagnosis
Some people with PTSD may be misdiagnosed with conditions such as anxiety or depression. Some people have other mental and physical health problems that make PTSD go unnoticed.
They may also experience medically unexplained symptoms such as:
- gastrointestinal disorders
- pain syndromes
- headaches
These symptoms may mean that their PTSD goes unnoticed.
Other difficulties
Some people with PTSD may also have other problems, such as difficulties in human relationships or addiction to alcohol and drugs. They may be caused by post-traumatic stress disorder, but these problems will manifest themselves more clearly than PTSD itself.
Can children develop PTSD?
PTSD can develop at any age. In addition to the symptoms of PTSD common to adults, children may also experience:
- Nightmares - In children, these dreams may or may not reflect an actual traumatic event.
- Repetitive play - some children act out a traumatic event during play. For example, a child who has been in a serious traffic accident may recreate the accident with toy cars.
- Physical symptoms - they may complain of abdominal pain and headaches.
- Fear of imminent death - they may find it hard to believe that they will live long enough to become adults.
What are the treatments for PTSD?
There are a number of different treatments for PTSD, including trauma-focused cognitive behavioral therapy (TF-CBT), eye movement desensitization and processing (EMDR), and medications.
Psychotherapy
Psychotherapy for PTSD will focus on the traumatic experience, not your past life. They will help you with the following:
- Acceptance - learn to accept the fact that although you cannot change what happened, you can think differently about the event, the world around you and your life.
- Remembrance of the event - remembering what happened, you will not feel fear or anxiety. You will be able to think about what happened when you yourself want it, and not through obsessive thoughts or memories.
- Explaining your experiences in words - by saying out loud what happened, your mind will be able to push the memories away and do other things.
- Finding a sense of security - helps you better control your feelings. This will make you feel more secure and eliminate the need to avoid memories.
All psychotherapy must be administered by a properly trained and accredited professional. Sessions are usually conducted by the same therapist at least once a week, with a total duration of at least 8-12 weeks.
Sessions usually last about an hour, sometimes they can last up to 90 minutes.
Therapy for PTSD includes:
Trauma-focused Cognitive Behavioral Therapy
A form of talking therapy that can help you change the way you think. Over time, this can help you feel better and behave differently. It is usually done individually, although there is evidence that CBT for trauma can also be done in groups.
Eye Movement Desensitization and Reprocessing (EMDR)
A technique that uses eye movements to help the brain process traumatic memories.
You will be asked to remember the traumatic event and what it made you think and feel. While you do this, you will be prompted to move your eyes or receive other "two-way stimulation" such as tapping your hand. It turns out that this reduces the emotional burden experienced in connection with the traumatic memory and helps to cope with the trauma.
GERD must be carried out by a qualified person. EPDH usually requires 8-12 sessions, lasting from 60 to 90 minutes.
Some other forms of talking therapy may be useful for treating certain symptoms (eg, poor sleep) in people for whom EMRT or CBT have not been effective for trauma.
Medications
If you have tried various treatments for post-traumatic stress disorder and find that they do not work for you, your doctor may prescribe antidepressants.
Selective serotonin reuptake inhibitors (SSRIs) are antidepressants that can help reduce symptoms of post-traumatic stress disorder. They can also help you if you are suffering from depression.
If SSRIs are not working for you, you may be offered other drugs, but this should usually be done on the advice of a mental health professional.
Which treatment is more effective?
There is evidence that Cognitive Behavioral Therapy for Trauma and Eye Movement Desensitization and Reprocessing are the best first line treatments. Medication can help those who refuse talking therapy or cannot easily access it.
Which treatment should I take first?
Trauma-focused psychological therapy (TF-CBT or EMBT) should be offered prior to medication, to the extent possible. This is in line with the UK National Institute for Health and Clinical Excellence (NICE) guidelines.
How can I help myself?
There are some things you can do to help you get better if you develop PTSD. Your therapist will help with this and make sure you apply them in a timely manner:
Stick to your daily routine - As far as possible, try to return to or maintain your normal daily routine. By continuing to lead a life as normal as possible, you can gain a sense of support.
By continuing to lead a life as normal as possible, you can gain a sense of support.
Talk to someone you trust - Although you shouldn't feel like you need to talk to everyone about what happened, talking to someone you trust can help you sort out your feelings in a safe environment. It can also help to talk to someone who has gone through the same thing as you, or someone who has gone through something similar before, as long as it doesn't hurt you.
Try relaxation exercises - Try self meditation and other relaxation exercises. Relaxing with PTSD can be challenging, so talk to your therapist about exercises or activities that can help you.
Return to work or school - if you feel empowered, it can help you return to work, school or university by giving you a sense of routine. However, you should try to avoid situations in which you may be subjected to further injury or severe stress.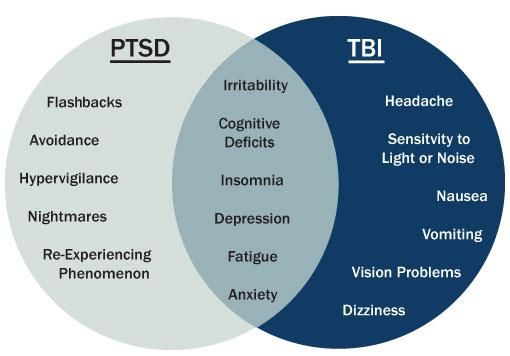 It is usually best to work in a supportive, low-stress environment before starting treatment.
It is usually best to work in a supportive, low-stress environment before starting treatment.
Eat and exercise regularly - Try to eat at regular times, even if you don't feel hungry. If you feel fit, try to exercise regularly. It can also help you feel tired before bed.
Spend time with others - Spending time with the people you care about will help you feel supported.
Expect to get better - Concentrating on thoughts that you will feel better over time will be useful for your recovery. Remember that you should not strain yourself in an attempt to recover faster.
Go back to where the traumatic event happened - If you feel you can do it, you may want to go back to where the traumatic event happened. Talk to your therapist or doctor if you are considering this so they can support you through this step.
There are also some things you should avoid while recovering. However, doing the "right things" can be very difficult, and you shouldn't feel guilty if you find yourself doing any of the following:
However, doing the "right things" can be very difficult, and you shouldn't feel guilty if you find yourself doing any of the following:
Self-criticism - PTSD symptoms are not a sign of weakness. This is a normal reaction to violent experiences.
Keep your feelings to yourself. If you have PTSD, don't feel guilty about sharing your thoughts and feelings with others. Talking about how you are feeling can help your recovery.
Expect everything to go back to normal quickly - PTSD may take some time to heal. Try not to demand too much of yourself in a short amount of time.
Stay away from other people. Spending a lot of time alone can increase your sense of isolation and make you feel less well.
Drink alcohol or smoke. Although alcohol can help you relax, and coffee and nicotine can act as stimulants, they can make you feel worse over time if you experience symptoms associated with post-traumatic stress disorder.
Overwork. Post-traumatic stress disorder can make it difficult to sleep, but as much as possible, try to stick to your normal sleep patterns and stay up late, as this can make you feel worse. You can learn more about good sleep in our resource.
Finally, you should be careful while driving. After a traumatic episode, people may have more accidents.
What is complex PTSD?
Some people develop complex post-traumatic stress disorder, caused by an experience or series of events that is extremely threatening or terrifying. These events can occur in childhood or adulthood.
Often such events are difficult or impossible to avoid. For example:
- torture
- slavery
- genocide
- living in war zones
- continuous domestic violence
- repeated sexual and physical abuse
In addition to PTSD symptoms, people with complex PTSD may also:
- emotions and emotional reactions
- have difficulty maintaining relationships and feelings of closeness with other people
How do I recover from complex PTSD?
People with complex post-traumatic stress disorder are characterized by a lack of trust in other people and in the world at large.
Emotional stabilization
During the stabilization phase, you will learn to trust your therapist and to understand and manage feelings of distress and alienation.
As part of stabilization, you can familiarize yourself with the work with supports - "grounding techniques". This can help you focus on familiar physical sensations and remind you that you are living in the present, not the past.
Stabilization can help you "disconnect" your feelings of fear and anxiety from the memories and the emotions they evoke, helping to make those memories less frightening.
The goal of stabilization is so that you can eventually live your life free from anxiety or memories.
Sometimes stabilization may be the only help needed.
Trauma-focused therapy
Trauma-focused therapy, including EMDR (Eye Movement Desensitization and Processing) or trauma-focused cognitive behavioral therapy, can help you deal with traumatic experiences. Other types of psychotherapy, including psychodynamic psychotherapy, may also be helpful. For complex post-traumatic stress disorder, care must be taken as these treatments can make things worse if not used properly.
Other types of psychotherapy, including psychodynamic psychotherapy, may also be helpful. For complex post-traumatic stress disorder, care must be taken as these treatments can make things worse if not used properly.
Reintegration and recovery
Reintegration into your normal life can help you adjust to the real world at a time when you have emerged from the dangerous situation you were in before. This can help you begin to see yourself as a person with a choice.
Reintegration can help you:
- be compassionate towards yourself and others
- restore trust in yourself and others
- renew friendships, intimate relationships, and activities that promote your health and well-being
Medications
As with PTSD, antidepressants or other medications may be used along with psychotherapy. Medication may also be used if psychotherapy does not help or is not available to you. It would also be helpful to have a mental health professional help you oversee your medication.
Self Help
If you develop complex PTSD, it may be helpful to try to do ordinary things that have nothing to do with your past traumatic experience.
They can include:
- To make friends
- get a job
- to engage regular physical exercises
- Learn to relax
- Find the hobby
- To start homemade
These things can help you allerately start the world around you . However, this can take time, and there is no need to be ashamed that at first these things will seem difficult to you or you will not be able to do them right away.
How do you know if someone has PTSD?
If you know someone who has just experienced a traumatic event, there are a few things you should be aware of. These moments may be signs that a person is not coping:
- Changes in behavior - low productivity at work, lateness, sick leave, minor accidents.
- Changes in emotions - anger, irritability, depression, lack of interest and lack of concentration.
- Changes in thought - preoccupation with threats or fears, negative outlook on the future
- Unexpected physical symptoms such as shortness of breath, nervousness or abdominal pain.
If you think a person may be showing signs of PTSD, you can suggest that they talk to their doctor. If you don't feel close enough to him for such a recommendation, talk to someone in his family or friends who could do it for you.
They may also find it helpful to refer to information about PTSD, such as this resource, to help identify the difficulties they face.
How can I help someone who has experienced a traumatic event?
For those who have experienced a traumatic event, the following may help:
- Be there - invite people to be with them. If they refuse, you can reassure them that you will be with them if they change their mind. Should not be imposed, but try to convince them to accept your help.
- Listen - try not to pressure people if they don't want something. If they want to talk, try to listen without interrupting or trying to share your own experience with them.
- Ask general questions - When you ask questions, try to keep them general and non-judgmental. For example, you might ask, "Have you talked about this with anyone else?" or “Can I help you find more help?”
- Offer real (practical) help - Some people may have difficulty taking care of themselves or doing daily activities. Offer help, such as cleaning the house or preparing meals;
Try not to tell people:
- That you know how they feel - even if you have experienced something like this, people experience situations differently. Comparing your experience with that of others is not always helpful;
- How lucky they are to be alive - people who have experienced traumatic events often don't think they are "lucky".