Antihistamine as anti anxiety
The Surprising Effects of Antihistamines on Anxiety and Depression
Home > Featured for Drug Addiction > The Surprising Effects of Antihistamines on Anxiety and Depression
By Kristina Robb-Dover
Doctors sometimes prescribe a drug for use outside of its listed purposes, especially if it looks safe and they believe it will be effective. This off-label use is common with many classes of drugs. That includes antihistamines, which have emerged as a promising way to treat short-term anxiety.
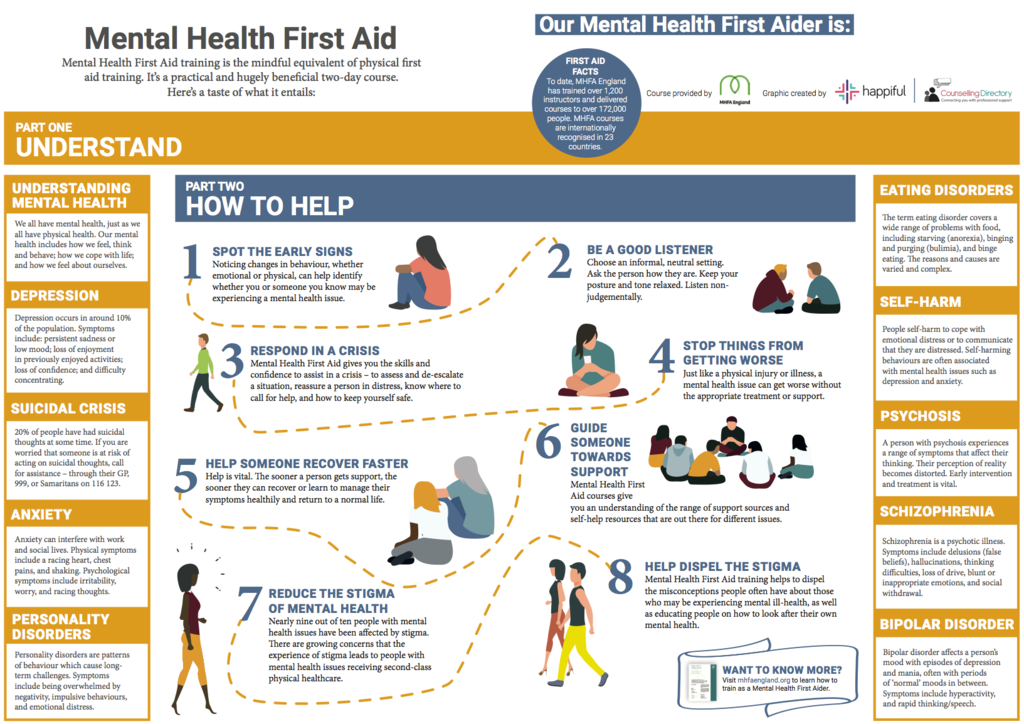
Anxiety disorders are the most common psychological conditions in the United States. This large class of conditions includes many specific disorders and affects an estimated 32% of American adults at least once in their lives. Often, this is a short-term issue. Many people experience bouts of anxiety, disturbed sleep or restlessness for 12 months or less. In these cases, certain antihistamine drugs have shown promising results for the off-label treatment of anxiety disorders.
Although the literature shows a link between antihistamines and anxiety treatment, the FDA hasn’t approved every antihistamine for this use. Only a doctor can give medical advice, and you should always consult with one before adjusting a course of medication. This is true even for over-the-counter drugs like Benadryl. Antihistamines aren’t an approved treatment for anxiety that lasts more than 12 months. They’re also not for use with serious psychotic or other disorders that require specialized care from a psychiatrist.
What Are Antihistamines?
Antihistamines are a class of drugs used to treat allergies and the symptoms of cold and flu. Usually available over the counter, these drugs work by suppressing some elements of the body’s natural immune system. The irritating symptoms associated with allergies are usually caused by a type of protein in the bloodstream called histamine. By blocking this chemical’s action, antihistamines can limit the negative effects of allergies and respiratory viruses.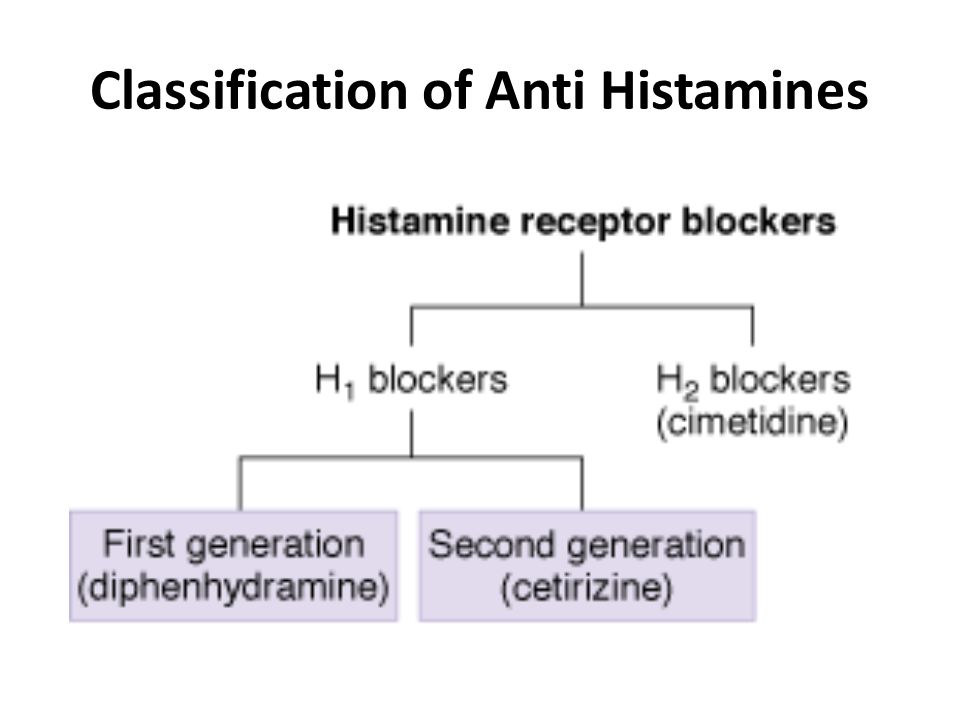
Benadryl
Benadryl is a leading brand of over-the-counter antihistamines. Its active ingredient is diphenhydramine, which can dry out the sinuses and prevent watery eyes. Off-label, Benadryl and its generic competitors can be used to treat motion sickness. Because diphenhydramine acts as a sedative, it can also be helpful for very short-term treatment of insomnia, ideally for a single night.
Benadryl has a shortlist of side effects, These are usually minor and go away on their own. Some rare symptoms can be serious and signal the need for medical attention. Relatively mild side effects include:
- Drowsiness
- Dizziness or vertigo
- Constipation or upset stomach
- Blurred vision
- Dry mouth/nose/throat
Many people who use Benadryl experience no noticeable side effects at all. Some effects are potentially serious, however. Call your doctor for advice immediately if you experience mood or mental changes, difficulty passing urine, or a fast/irregular heartbeat.
Hydroxyzine
Like Benadryl, hydroxyzine is an antihistamine. It has sedative properties and is frequently used off-label for many conditions. These include insomnia, nausea, vomiting, itching, and skin rashes. Unlike Benadryl, hydroxyzine has been approved by the FDA for the treatment of anxiety.
Hydroxyzine is available by prescription under the brand name Vistaril. It comes as a liquid oral suspension and may be taken daily for up to four months to treat anxiety. If your anxiety symptoms last longer than this, speak with your doctor about whether to continue taking the medicine. Don’t change the dose or discontinue Vistaril without first consulting with your doctor or pharmacist.
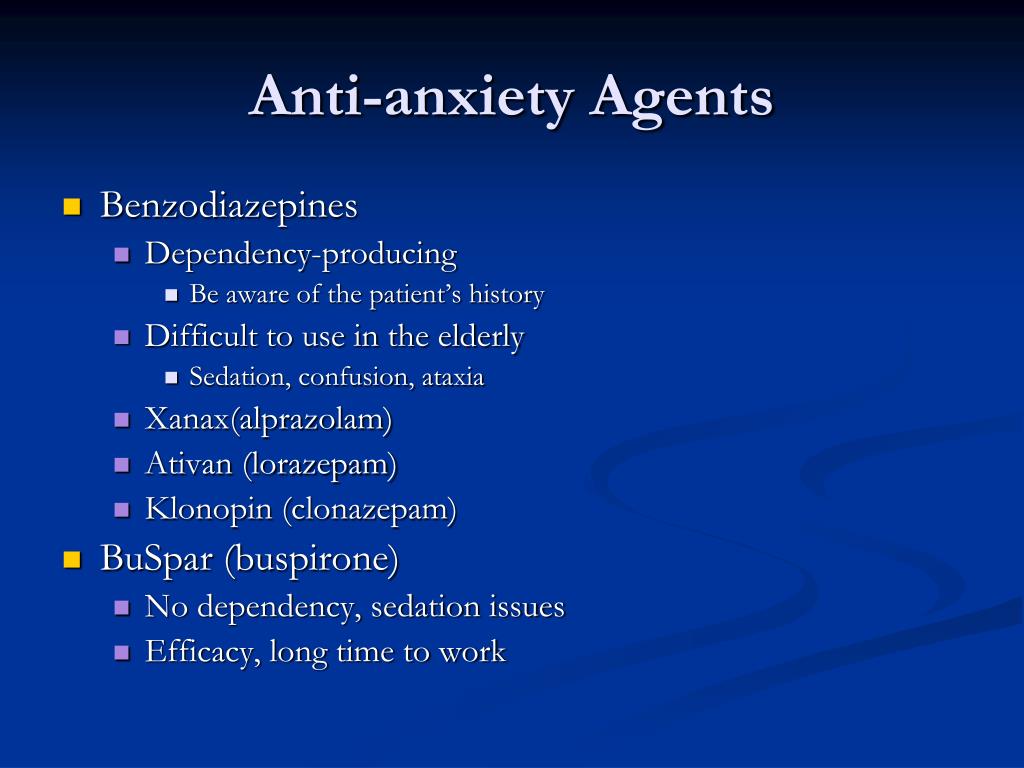
Some drugs have negative interactions with hydroxyzine. You may not be able to take it if you’re also taking drugs that cause drowsiness. This includes sleeping pills, narcotic pain relievers, muscle relaxants, or a benzodiazepine such as Xanax. It’s potentially dangerous to take hydroxyzine at the same time as certain other drugs.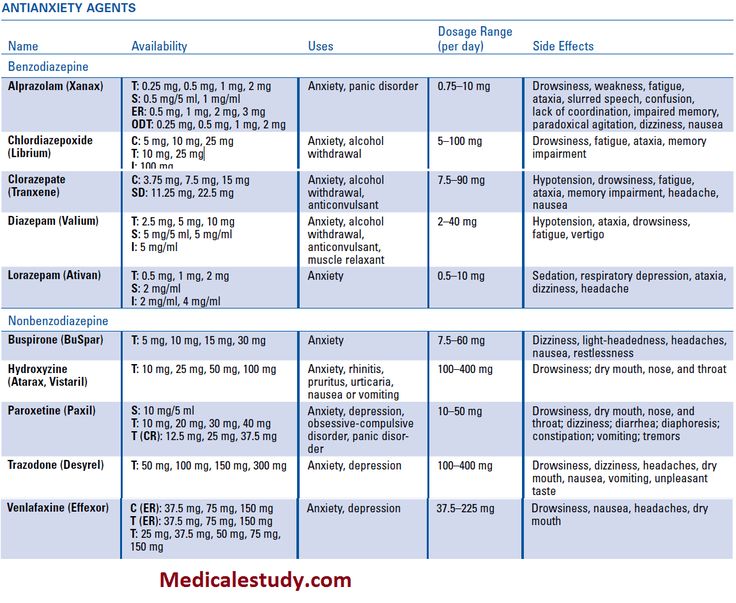 These include antidepressants, heart medicine, antipsychotics, and various drug cocktails used to treat HIV/AIDS, malaria, and cancer.
These include antidepressants, heart medicine, antipsychotics, and various drug cocktails used to treat HIV/AIDS, malaria, and cancer.
Treating Anxiety Disorders
Taking any medication is always a balancing act between the positive and negative effects of the drug. Taking antihistamines to treat anxiety and depression can be effective, but there are some drawbacks to consider. Major advantages of using commonly available antihistamines are their generally lower cost and easier availability than prescription anxiety drugs. Antihistamines are also generally less likely to cause dependence and addiction than other sedatives.
Antihistamines can be helpful over short time frames when used in conjunction with the nonmedical therapy you’re getting. It’s relatively easy to get some antihistamines, especially Benadryl. This encourages many people who prefer to avoid prescription drugs to use them instead. It may be preferable to neglecting to get any treatment at all for anxiety and depression.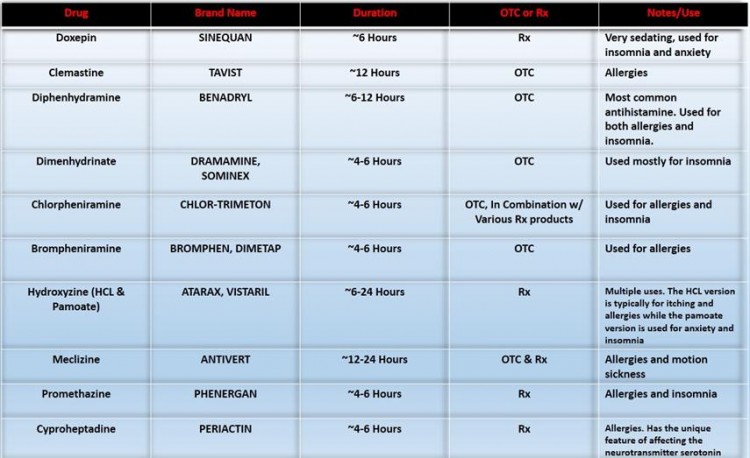
Taking antihistamines for off-label purposes isn’t without drawbacks, though. Most antihistamines are known to cause drowsiness during the day. This may be a problem for people who operate heavy machinery or otherwise have to remain alert. These drugs also aren’t effective for severe anxiety or depression, and they’re not a long-term treatment for any anxiety disorder.
Because of their ready availability, antihistamines could also potentially increase the risk of a negative interaction. This includes other prescriptions and over-the-counter drugs. Negative interactions can even happen with vitamins or nutritional supplements.
When to See a Doctor
You shouldn’t delay seeing a doctor when you have doubts about your medical condition or you’re about to start a new medication. Talk to your doctor or psychiatrist at the first sign of anxiety or depression as these are serious conditions that may need professional care. Always ask your doctor about potential drug interactions if you’re currently taking medication or herbal supplements for any reason. Seek help immediately if you take an antihistamine and experience a negative reaction, especially if it impairs your ability to breathe.
Seek help immediately if you take an antihistamine and experience a negative reaction, especially if it impairs your ability to breathe.
Anxiety and depression are both very serious emotional health issues that frequently need specialist care to treat. If you think you may be dealing with an anxiety disorder, call us at (833) 596-3502 right away. Our compassionate team of counselors knows what you’re going through and can help. Start your journey to lifelong recovery with us now.
Filed Under: Featured for Drug Addiction, Drug Addiction
About Kristina Robb-Dover
Kristina Robb-Dover is a content manager and writer with extensive editing and writing experience... read more
Benadryl For Anxiety: What You Need to Know
You’ve probably heard of Benadryl. It’s a common over-the-counter (OTC) antihistamine that’s often used to manage allergies. It also has a sedative effect, which means it can make you sleepy.
Because of this, some people use it for the short-term treatment of anxiety symptoms.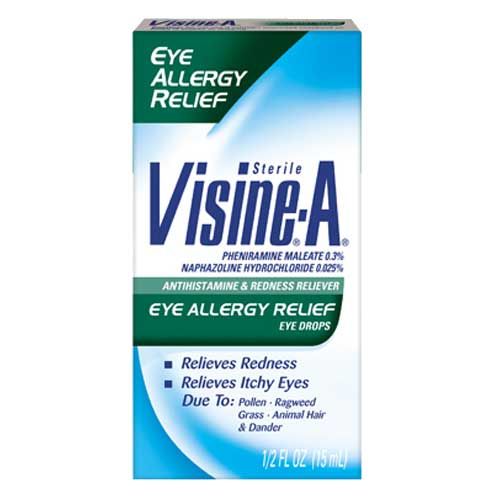
However, it’s not a long-term solution, and it doesn’t have FDA approval for the treatment of anxiety.
In this article, I’ll talk about what Benadryl is, how it may help anxiety, its side effects and risks, and other anxiety treatment options that may be safer and more effective.
What Is Benadryl?
Benadryl is a name brand for the antihistamine diphenhydramine.
Typically, Benadryl is used to relieve allergy symptoms like:
- Sneezing
- Itchy eyes
- Runny nose
- Itchy nose and throat
It can also be used to help manage symptoms of the common cold by reducing nasal congestion.
Benadryl risk factors
While Benadryl is safe for most people to take, you should avoid it if you have certain health conditions, including:
- Glaucoma
- Breathing problems
- Trouble urinating
You also shouldn’t use Benadryl:
- As a sleep aid for children
- With other products containing diphenhydramine
Though everyone reacts differently, Benadryl typically makes people drowsy.
Avoid driving, drinking alcoholic beverages, and taking any other type of sedative or sleeping pill after taking Benadryl.
Talk to a doctor online
Refill medications and get certain necessary prescriptions.
Start now
Does Benadryl Help Anxiety?
Although some people say that Benadryl helps their anxiety, it is not approved by the FDA for anxiety symptoms.
Therefore, do not take it for anxiety unless your healthcare provider specifically recommends it.
The only FDA-approved antihistamine for anxiety is hydroxyzine (Atarax, Vistaril).
For some people, this can be an effective alternative to benzodiazepines.
Although benzodiazepines can treat anxiety, they can also be addictive and have significant side effects.
According to research, hydroxyzine can treat anxiety symptoms, insomnia, and panic attacks. It’s safe for children and pregnant individuals, and it carries few side effects.
In contrast, Benadryl has not been extensively studied and is thought to be less effective for treating anxiety overall.
Benadryl and sleep
Antihistamines such as Benadryl make you feel sleepy by blocking excess production of histamine and histamine release in the brain.
Among other things, histamines (natural chemicals produced by the body) affect your sleep and wake cycles.
Typically, your brain’s histamine levels naturally decrease before you go to sleep. When antihistamines block histamine production, your brain thinks it’s time to sleep.
Some people take Benadryl as a sleep aid.
However, medical providers don’t recommend this because it hasn’t been tested and approved as a sleep aid.
Additionally, Benadryl may make you feel groggy and drowsy, may not help you fall asleep faster, and may do more harm by disturbing your normal sleep/wake cycle.
Since Benadryl isn’t recommended for anxiety, there is no suggested dose for this purpose.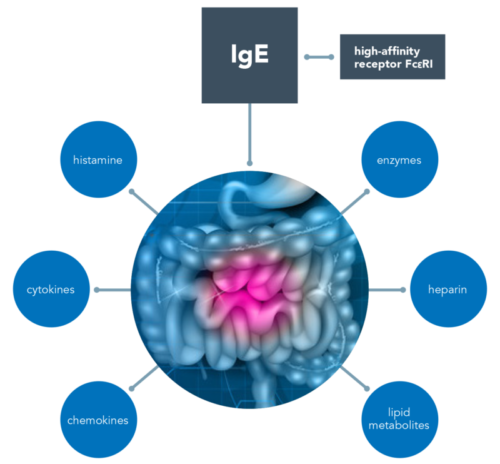
If you’re using Benadryl for hay fever or allergies, the typical dosage is 25 or 50 milligrams (mg) every 4–6 hours for anyone 12 and older.
In children aged 6–11, the recommended dosage is 12.5 or 25 mg every 4–6 hours. Children under six should only take Benadryl if recommended by their pediatrician.
Side Effects
Most antihistamines, including Benadryl, are generally well-tolerated. They don’t have many significant side effects, but you can develop a tolerance over time.
Some common side effects of Benadryl include:
- Sleepiness
- Grogginess
- Dry mouth
- Constipation
Risks and Warnings
Although it’s generally safe for most healthy individuals, Benadryl comes with some warnings.
Overdose
Taking too much Benadryl can cause an overdose.
This can lead to dangerous and potentially life-threatening symptoms such as:
- Agitation
- Confusion
- Hallucinations
- Delirium
- Seizures
- Heart problems
In very severe cases, a Benadryl overdose can cause coma and death.
If you or a loved one may have overdosed on Benadryl, seek immediate medical attention.
Call the poison control helpline at 800-222-1222 or, if someone is unconscious, having a seizure, or is having trouble breathing, call 911.
Interactions
Benadryl can interact with other medications and substances.
One common interaction is alcohol. If you’re taking Benadryl, consuming alcohol can exacerbate the sedation effect and make you very dizzy, drowsy, and sluggish.
Additionally, Benadryl can interact with some medications, including:
- Gabapentin (Neurontin)
- Tramadol (Ultram)
- Lisinopril (Zestril)
- Melatonin
- Trazodone
- Alprazolam (Xanax)
- Cetirizine (Zyrtec
Do not take Benadryl if you take any of these medications.
If you aren’t sure if a medication you’re taking interacts with Benadryl, contact your healthcare provider.
Anxiety Treatment Options
If you have anxiety, your doctor can work with you to create a treatment plan, which usually consists of a combination of medication and talk therapy.
Medications that can treat anxiety include:
- Selective serotonin reuptake inhibitors (SSRIs): These are often used to treat depression and anxiety. SSRIs include fluoxetine (Prozac), citalopram (Celexa), and sertraline (Zoloft).
- Serotonin-norepinephrine reuptake inhibitors (SNRIs): These are used to treat depression, anxiety, OCD, and other mood disorders. They include desvenlafaxine (Pristiq), duloxetine (Cymbalta), and levomilnacipran (Fetzima).
- Benzodiazepines: These sedative medications treat anxiety, seizures, and insomnia. They include alprazolam (Xanax), clonazepam (Klonopin), and diazepam (Valium). Benzodiazepines have serious side effects and can be habit-forming, so they are generally not used long term.
- Antipsychotics: Also called neuroleptics, these medications treat schizophrenia, psychosis, and anxiety. Antipsychotics include aripiprazole (Abilify), asenapine (Saphris), and cariprazine (Vraylar).

Your provider may also recommend psychotherapy or cognitive-behavioral therapy (CBT).
Therapy can help you understand your thoughts and provide you with additional tools to work through and manage anxiety symptoms when they arise.
Talk to a doctor online
Refill medications and get certain necessary prescriptions.
Start now
Seeking Help for Anxiety
If you have anxiety that’s affecting your life, contact your doctor.
They can evaluate your symptoms, help make the right diagnosis, and recommend treatments that can help you manage your anxiety.
How K Health Can Help
Did you know you can get affordable mental healthcare with the K Health app? Download K to check your symptoms, explore conditions and treatments, and if needed text with a healthcare provider in minutes. K Health’s AI-powered app is HIPAA compliant and based on 20 years of clinical data.
Frequently Asked Questions
Is Benadryl good for anxiety?
Do not take Benadryl for anxiety without a provider’s recommendation.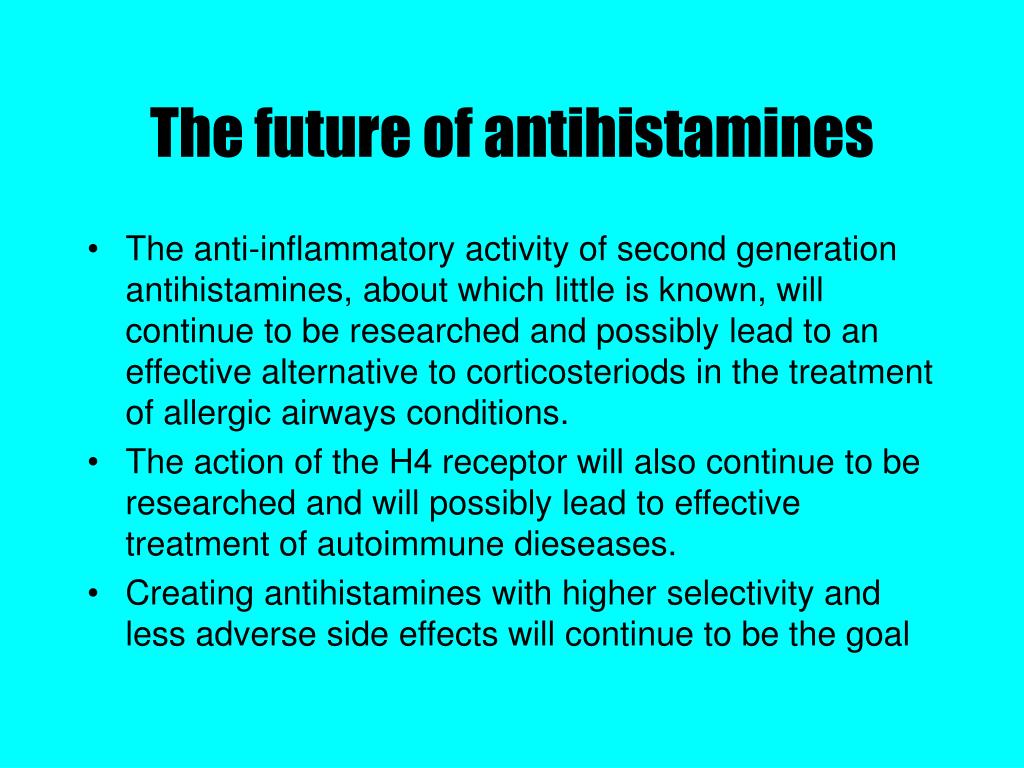 While some people say Benadryl helps their anxiety, it is not tested or approved for treating anxiety. Other medications, like SSRIs and SNRIs, can effectively treat anxiety symptoms.
While some people say Benadryl helps their anxiety, it is not tested or approved for treating anxiety. Other medications, like SSRIs and SNRIs, can effectively treat anxiety symptoms.
What kind of Benadryl helps with anxiety?
Benadryl is the brand name for diphenhydramine. All forms of diphenhydramine can treat allergies, hay fever, and common cold symptoms. None of them are approved to treat anxiety.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
K Health has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
We avoid using tertiary references.
-
Anxiety Disorders. (2022).
https://www.nimh.nih.gov/health/topics/anxiety-disorders -
Benadryl. (2022).
https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=702f9786-7ce9-43e4-921d-e1db09612127 -
Diphenhydramine Toxicity.
 (2022).
(2022).
https://www.ncbi.nlm.nih.gov/books/NBK557578/ -
New guideline provides clinical recommendations for specific insomnia drugs. (2017).
https://aasm.org/new-guideline-provides-clinical-recommendations-for-specific-insomnia-drugs/ -
Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment Options.
 (2020).
(2020).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7786299/ -
Treatment of anxiety disorders. (2017).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5573566/
ANTIHISTAMINS: from diphenhydramine to telfast | #03/01
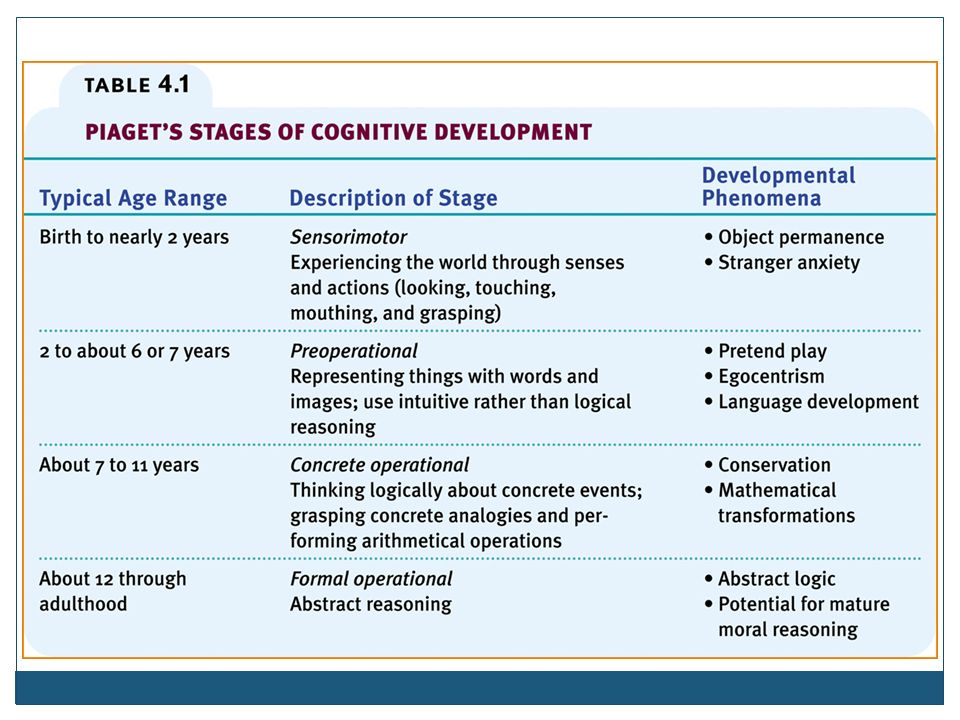
Historically, the term "antihistamines" means drugs that block H1-histamine receptors, and drugs that act on H2-histamine receptors (cimetidine, ranitidine, famotidine, etc.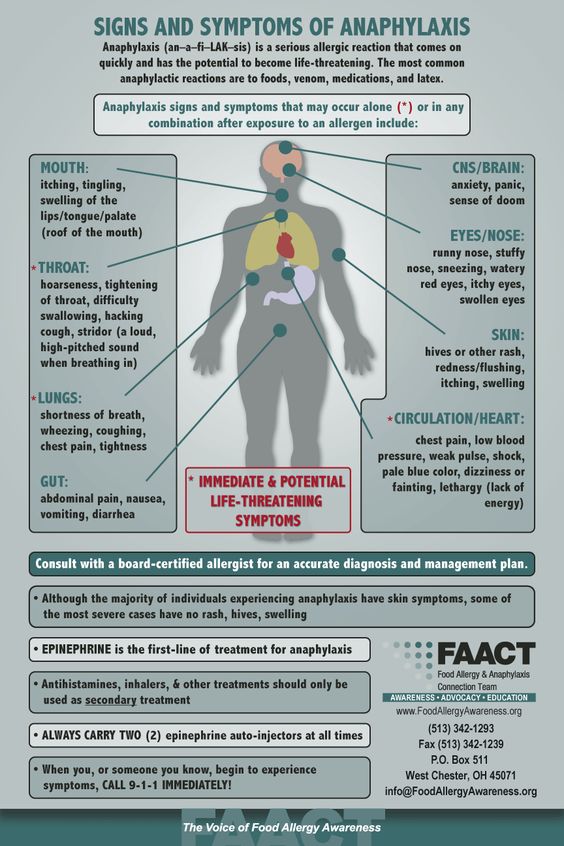 ) are called H2-histamine blockers. The former are used to treat allergic diseases, the latter are used as antisecretory agents.
) are called H2-histamine blockers. The former are used to treat allergic diseases, the latter are used as antisecretory agents.
Histamine, this most important mediator of various physiological and pathological processes in the body, was chemically synthesized in 1907 year. Subsequently, it was isolated from animal and human tissues (Windaus A., Vogt W.). Even later, its functions were determined: gastric secretion, neurotransmitter function in the central nervous system, allergic reactions, inflammation, etc. Almost 20 years later, in 1936, the first substances with antihistamine activity were created (Bovet D., Staub A.). And already in the 60s, the heterogeneity of histamine receptors in the body was proven and three of their subtypes were identified: H1, H2 and H3, differing in structure, localization and physiological effects that occur during their activation and blockade. Since that time, an active period of synthesis and clinical testing of various antihistamines begins.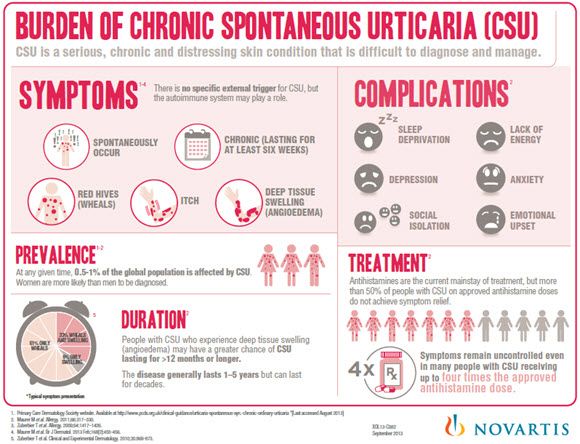
Numerous studies have shown that histamine, acting on the receptors of the respiratory system, eyes and skin, causes characteristic allergy symptoms, and antihistamines that selectively block H1-type receptors can prevent and stop them.
Most of the antihistamines used have a number of specific pharmacological properties that characterize them as a separate group. These include the following effects: antipruritic, decongestant, antispastic, anticholinergic, antiserotonin, sedative and local anesthetic, as well as the prevention of histamine-induced bronchospasm. Some of them are not due to histamine blockade, but to structural features.
Antihistamines block the action of histamine on H1 receptors by the mechanism of competitive inhibition, and their affinity for these receptors is much lower than that of histamine. Therefore, these drugs are not able to displace histamine bound to the receptor, they only block unoccupied or released receptors. Accordingly, H1 blockers are most effective in preventing immediate allergic reactions, and in the case of a developed reaction, they prevent the release of new portions of histamine.
According to their chemical structure, most of them are fat-soluble amines, which have a similar structure. The core (R1) is represented by an aromatic and/or heterocyclic group and is linked via a nitrogen, oxygen or carbon (X) molecule to the amino group. The core determines the severity of antihistamine activity and some of the properties of the substance. Knowing its composition, one can predict the strength of the drug and its effects, such as the ability to penetrate the blood-brain barrier.
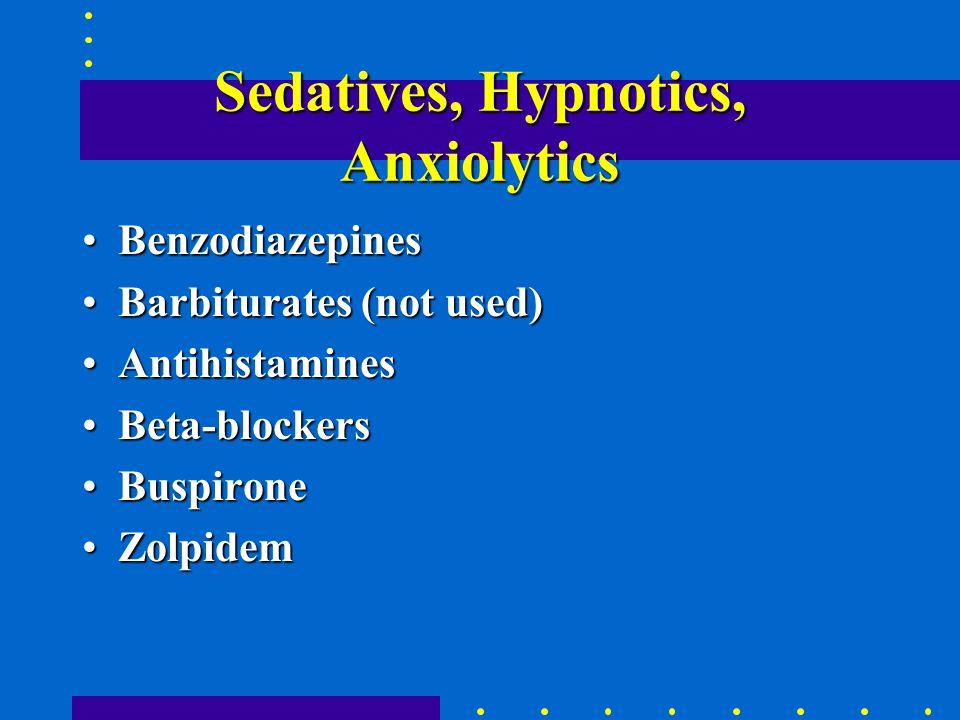
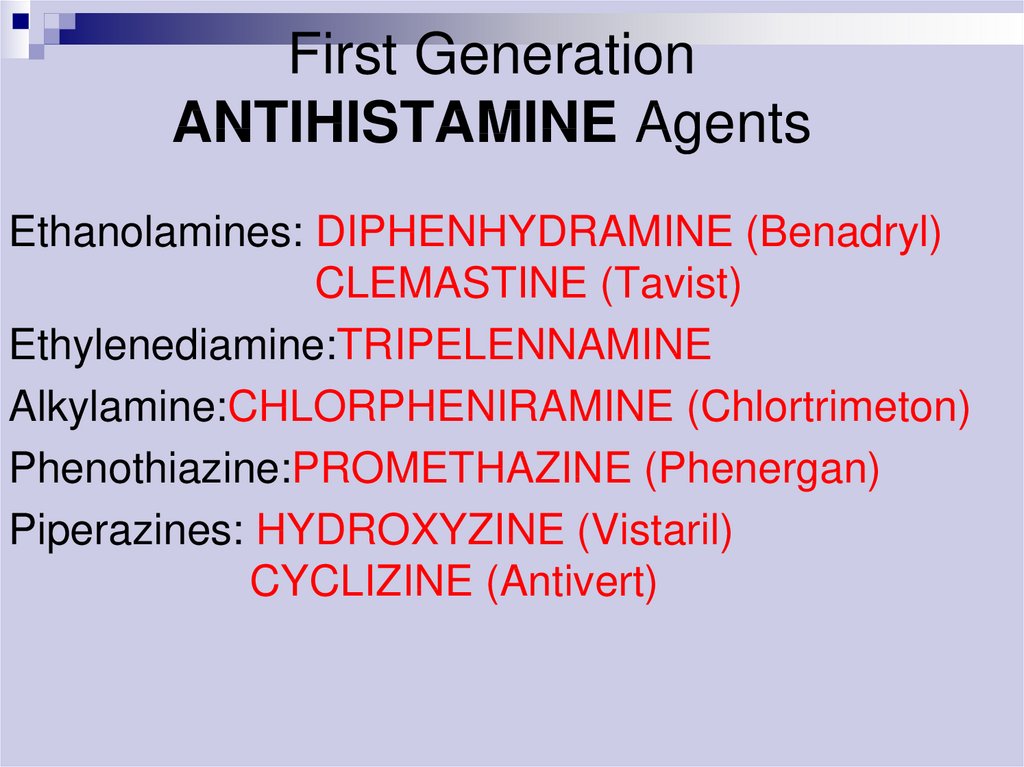
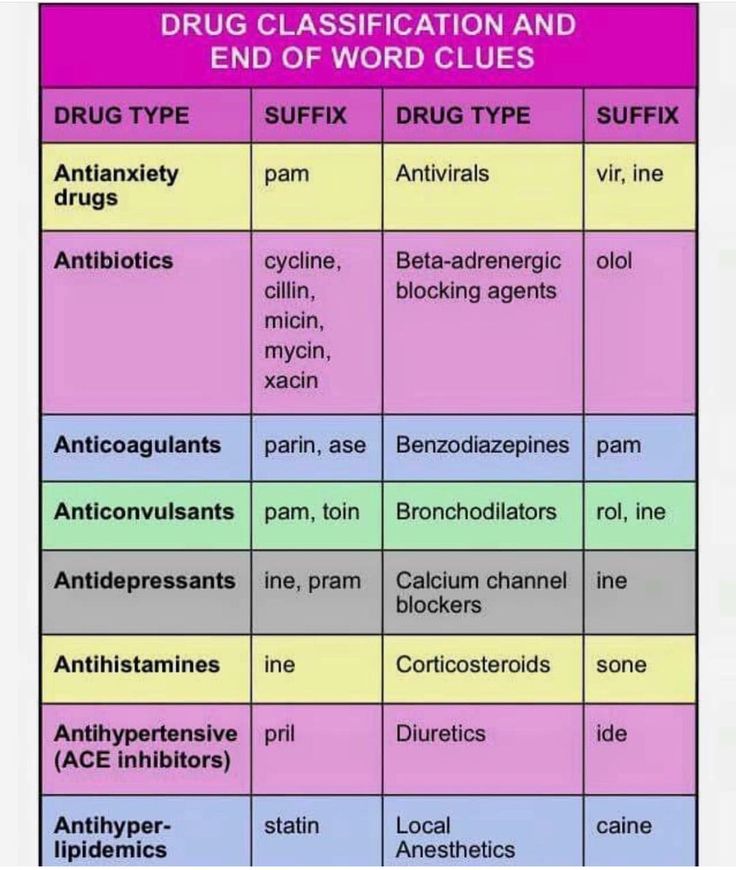
There are several classifications of antihistamines, although none of them is generally accepted. According to one of the most popular classifications, antihistamines are divided into first and second generation drugs according to the time of creation. First-generation drugs are also called sedatives (according to the dominant side effect), in contrast to non-sedative second-generation drugs. At present, it is customary to isolate the third generation: it includes fundamentally new drugs - active metabolites that, in addition to the highest antihistamine activity, exhibit the absence of a sedative effect and the cardiotoxic effect characteristic of second-generation drugs (see table).
In addition, according to the chemical structure (depending on the X-bond), antihistamines are divided into several groups (ethanolamines, ethylenediamines, alkylamines, derivatives of alphacarboline, quinuclidine, phenothiazine, piperazine and piperidine).
First generation antihistamines (sedatives). All of them are well soluble in fats and, in addition to H1-histamine, also block cholinergic, muscarinic and serotonin receptors. Being competitive blockers, they reversibly bind to H1 receptors, which leads to the use of rather high doses. The following pharmacological properties are most characteristic of them.
- Sedative effect is determined by the fact that most of the first generation antihistamines, being easily dissolved in lipids, penetrate well through the blood-brain barrier and bind to the H1-receptors of the brain. Perhaps their sedative effect consists of blocking the central serotonin and acetylcholine receptors. The degree of manifestation of the sedative effect of the first generation varies in different drugs and in different patients from moderate to severe and increases when combined with alcohol and psychotropic drugs.
 Some of them are used as sleeping pills (doxylamine). Rarely, instead of sedation, psychomotor agitation occurs (more often in medium therapeutic doses in children and in high toxic doses in adults). Due to the sedative effect, most drugs should not be used during tasks that require attention. All first-generation drugs potentiate the action of sedative and hypnotic drugs, narcotic and non-narcotic analgesics, monoamine oxidase inhibitors and alcohol.
Some of them are used as sleeping pills (doxylamine). Rarely, instead of sedation, psychomotor agitation occurs (more often in medium therapeutic doses in children and in high toxic doses in adults). Due to the sedative effect, most drugs should not be used during tasks that require attention. All first-generation drugs potentiate the action of sedative and hypnotic drugs, narcotic and non-narcotic analgesics, monoamine oxidase inhibitors and alcohol. - The anxiolytic effect characteristic of hydroxyzine may be due to the suppression of activity in certain areas of the subcortical region of the CNS.
- Atropine-like reactions associated with the anticholinergic properties of drugs are most characteristic of ethanolamines and ethylenediamines. Manifested by dry mouth and nasopharynx, urinary retention, constipation, tachycardia and visual impairment. These properties ensure the effectiveness of the discussed remedies in non-allergic rhinitis. At the same time, they can increase obstruction in bronchial asthma (due to an increase in sputum viscosity), exacerbate glaucoma and lead to infravesical obstruction in prostate adenoma, etc.
- Antiemetic and antiswaying effects are also likely to be associated with the central anticholinergic effect of the drugs. Some antihistamines (diphenhydramine, promethazine, cyclizine, meclizine) reduce the stimulation of vestibular receptors and inhibit the function of the labyrinth, and therefore can be used for motion sickness.
- A number of H1-histamine blockers reduce the symptoms of parkinsonism, which is due to the central inhibition of the effects of acetylcholine.
- Antitussive action is most characteristic of diphenhydramine, it is realized through a direct action on the cough center in the medulla oblongata.
- The antiserotonin effect, which is primarily characteristic of cyproheptadine, determines its use in migraine.
- α1-blocking effect with peripheral vasodilation, especially inherent in phenothiazine antihistamines, can lead to a transient decrease in blood pressure in sensitive individuals.
- Local anesthetic (cocaine-like) action is characteristic of most antihistamines (due to a decrease in membrane permeability to sodium ions).
 Diphenhydramine and promethazine are stronger local anesthetics than novocaine. However, they have systemic quinidine-like effects, manifested by prolongation of the refractory phase and the development of ventricular tachycardia.
Diphenhydramine and promethazine are stronger local anesthetics than novocaine. However, they have systemic quinidine-like effects, manifested by prolongation of the refractory phase and the development of ventricular tachycardia. - Tachyphylaxis: decrease in antihistamine activity with long-term use, confirming the need for alternating drugs every 2-3 weeks.
- It should be noted that first-generation antihistamines differ from second-generation antihistamines in the short duration of exposure with a relatively rapid onset of clinical effect. Many of them are available in parenteral forms. All of the above, as well as low cost, determine the widespread use of antihistamines today.
Moreover, many of the qualities that were discussed allowed the “old” antihistamines to occupy their niche in the treatment of certain pathologies (migraine, sleep disorders, extrapyramidal disorders, anxiety, motion sickness, etc.) that are not associated with allergies. Many first-generation antihistamines are included in combination preparations used for colds, as sedatives, hypnotics, and other components.
Many first-generation antihistamines are included in combination preparations used for colds, as sedatives, hypnotics, and other components.
The most commonly used are chloropyramine, diphenhydramine, clemastine, cyproheptadine, promethazine, phencarol, and hydroxyzine.
Chloropyramine (Suprastin) is one of the most widely used sedative antihistamines. It has significant antihistamine activity, peripheral anticholinergic and moderate antispasmodic action. Effective in most cases for the treatment of seasonal and year-round allergic rhinoconjunctivitis, angioedema, urticaria, atopic dermatitis, eczema, itching of various etiologies; in parenteral form - for the treatment of acute allergic conditions requiring emergency care. Provides a wide range of usable therapeutic doses. It does not accumulate in the blood serum, so it does not cause an overdose with prolonged use. Suprastin is characterized by a rapid onset of effect and short duration (including side effects). At the same time, chloropyramine can be combined with non-sedating H1-blockers in order to increase the duration of the antiallergic effect. Suprastin is currently one of the best-selling antihistamines in Russia. This is objectively related to the proven high efficiency, controllability of its clinical effect, the availability of various dosage forms, including injections, and low cost.
At the same time, chloropyramine can be combined with non-sedating H1-blockers in order to increase the duration of the antiallergic effect. Suprastin is currently one of the best-selling antihistamines in Russia. This is objectively related to the proven high efficiency, controllability of its clinical effect, the availability of various dosage forms, including injections, and low cost.
Diphenhydramine , best known in our country under the name diphenhydramine, is one of the first synthesized H1-blockers. It has a fairly high antihistamine activity and reduces the severity of allergic and pseudo-allergic reactions. Due to the significant anticholinergic effect, it has an antitussive, antiemetic effect and at the same time causes dry mucous membranes, urinary retention. Due to lipophilicity, diphenhydramine gives pronounced sedation and can be used as a hypnotic. It has a significant local anesthetic effect, as a result of which it is sometimes used as an alternative for intolerance to novocaine and lidocaine. Diphenhydramine is presented in various dosage forms, including for parenteral use, which determined its widespread use in emergency therapy. However, a significant range of side effects, unpredictability of consequences and effects on the central nervous system require increased attention in its application and, if possible, the use of alternative means.
Diphenhydramine is presented in various dosage forms, including for parenteral use, which determined its widespread use in emergency therapy. However, a significant range of side effects, unpredictability of consequences and effects on the central nervous system require increased attention in its application and, if possible, the use of alternative means.
Clemastine (tavegil) is a highly effective antihistamine similar in action to diphenhydramine. It has a high anticholinergic activity, but to a lesser extent penetrates the blood-brain barrier. It also exists in an injectable form, which can be used as an additional remedy for anaphylactic shock and angioedema, for the prevention and treatment of allergic and pseudo-allergic reactions. However, hypersensitivity to clemastine and other antihistamines with a similar chemical structure is known.
Cyproheptadine (peritol), along with antihistamine, has a significant antiserotonin effect. In this regard, it is mainly used in some forms of migraine, dumping syndrome, as an appetite enhancer, in anorexia of various origins. It is the drug of choice for cold urticaria.
In this regard, it is mainly used in some forms of migraine, dumping syndrome, as an appetite enhancer, in anorexia of various origins. It is the drug of choice for cold urticaria.
Promethazine (pipolfen) - a pronounced effect on the central nervous system determined its use in Meniere's syndrome, chorea, encephalitis, sea and air sickness, as an antiemetic. In anesthesiology, promethazine is used as a component of lytic mixtures to potentiate anesthesia.
Quifenadine (phencarol) - has less antihistamine activity than diphenhydramine, but is also characterized by less penetration through the blood-brain barrier, which determines the lower severity of its sedative properties. In addition, fenkarol not only blocks histamine H1 receptors, but also reduces the content of histamine in tissues. May be used in the development of tolerance to other sedative antihistamines.
Hydroxyzine (atarax) - despite the existing antihistamine activity, it is not used as an antiallergic agent.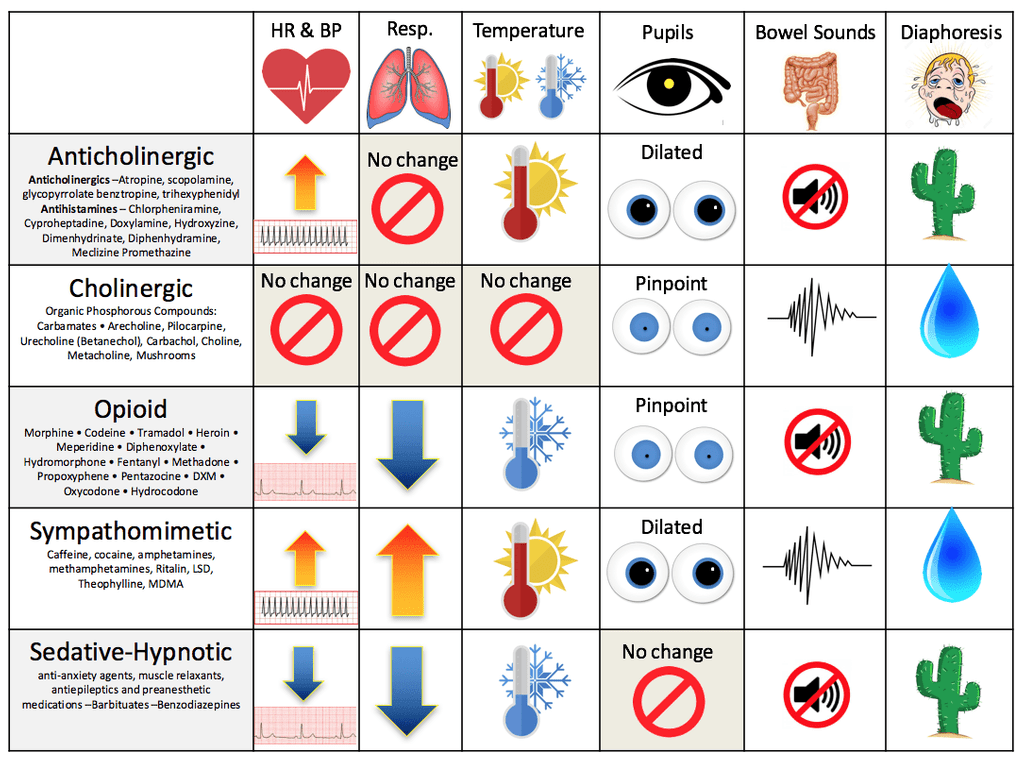 It is used as an anxiolytic, sedative, muscle relaxant and antipruritic agent.
It is used as an anxiolytic, sedative, muscle relaxant and antipruritic agent.
Thus, first-generation antihistamines that affect both H1- and other receptors (serotonin, central and peripheral cholinergic receptors, a-adrenergic receptors) have different effects, which determined their use in a variety of conditions. But the severity of side effects does not allow us to consider them as drugs of first choice in the treatment of allergic diseases. The experience gained with their use has allowed the development of unidirectional drugs - the second generation of antihistamines.
Second generation antihistamines (non-sedating). Unlike the previous generation, they almost do not have sedative and anticholinergic effects, but differ in their selective action on H1 receptors. However, for them, a cardiotoxic effect was noted to varying degrees.
The following properties are the most common for them.
- High specificity and high affinity for H1 receptors with no effect on choline and serotonin receptors.
- Rapid onset of clinical effect and duration of action. Prolongation can be achieved due to high protein binding, accumulation of the drug and its metabolites in the body, and delayed elimination.
- Minimal sedation when using drugs at therapeutic doses. It is explained by the weak passage of the blood-brain barrier due to the peculiarities of the structure of these funds. Some particularly sensitive individuals may experience moderate drowsiness, which is rarely the reason for discontinuing the drug.
- No tachyphylaxis with long-term use.
- The ability to block the potassium channels of the heart muscle, which is associated with prolongation of the QT interval and cardiac arrhythmias. The risk of this side effect increases when antihistamines are combined with antifungals (ketoconazole and itraconazole), macrolides (erythromycin and clarithromycin), antidepressants (fluoxetine, sertraline and paroxetine), grapefruit juice, and in patients with severe liver dysfunction.
- No parenteral formulations, but some (azelastine, levocabastine, bamipine) are available as topical formulations.
Below are second-generation antihistamines with their most characteristic properties.
Terfenadine is the first antihistamine drug without CNS depressant action. Its creation in 1977 was the result of a study of both the types of histamine receptors and the features of the structure and action of existing H1-blockers, and laid the foundation for the development of a new generation of antihistamines. Currently, terfenadine is used less and less, which is associated with its increased ability to cause fatal arrhythmias associated with prolongation of the QT interval (torsade de pointes).
Astemizol is one of the longest-acting drugs of the group (the half-life of its active metabolite is up to 20 days). It is characterized by irreversible binding to H1 receptors. Virtually no sedative effect, does not interact with alcohol.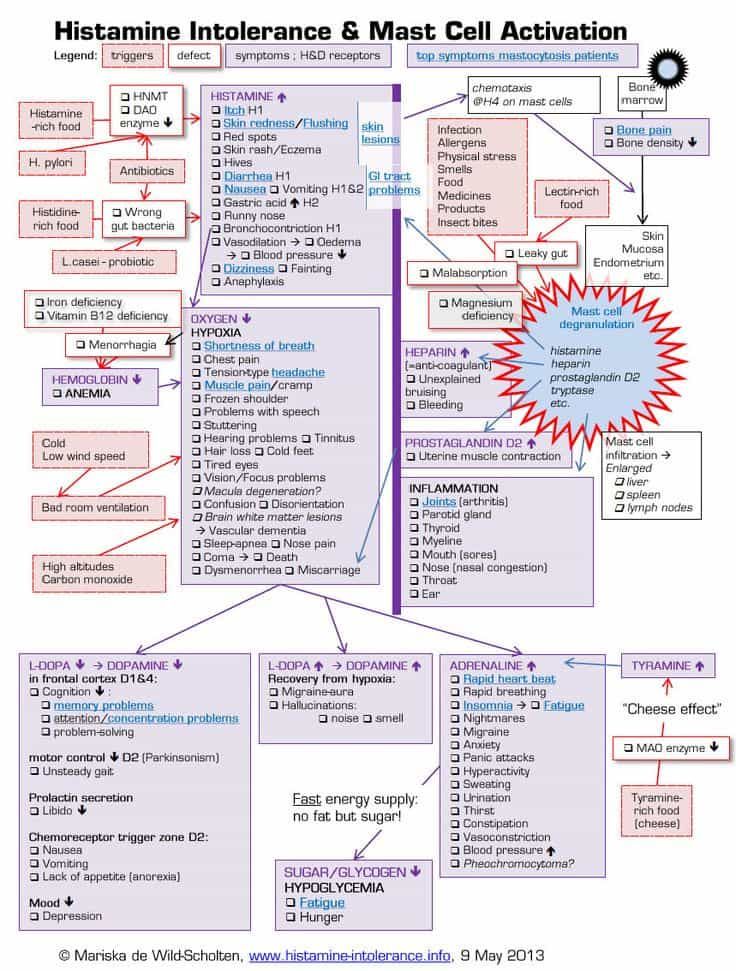 Since astemizole has a delayed effect on the course of the disease, it is not advisable to use it in an acute process, but it may be justified in chronic allergic diseases. Since the drug has the ability to accumulate in the body, the risk of developing serious heart rhythm disturbances, sometimes fatal, increases. Due to these dangerous side effects, the sale of astemizole in the United States and some other countries has been suspended.
Since astemizole has a delayed effect on the course of the disease, it is not advisable to use it in an acute process, but it may be justified in chronic allergic diseases. Since the drug has the ability to accumulate in the body, the risk of developing serious heart rhythm disturbances, sometimes fatal, increases. Due to these dangerous side effects, the sale of astemizole in the United States and some other countries has been suspended.
Acrivastine (semprex) is a drug with high antihistamine activity with minimal sedative and anticholinergic effects. A feature of its pharmacokinetics is a low level of metabolism and the absence of cumulation. Acrivastine is preferred in cases where there is no need for permanent antiallergic treatment due to the rapid onset of effect and short-term effect, which allows for a flexible dosing regimen.
Dimetendene (Fenistil) is the closest to the first generation antihistamines, but differs from them in a significantly less pronounced sedative and muscarinic effect, higher antiallergic activity and duration of action.
Loratadin (Claritin) is one of the most purchased second-generation drugs, which is quite understandable and logical. Its antihistamine activity is higher than that of astemizole and terfenadine, due to the greater strength of binding to peripheral H1 receptors. The drug is devoid of a sedative effect and does not potentiate the effect of alcohol. In addition, loratadine practically does not interact with other drugs and does not have a cardiotoxic effect.
The following antihistamines are topical preparations and are intended to relieve local manifestations of allergies.
Levocabastin (Histimet) is used as an eye drop for the treatment of histamine-dependent allergic conjunctivitis or as a spray for allergic rhinitis. When applied topically, it enters the systemic circulation in a small amount and does not have undesirable effects on the central nervous and cardiovascular systems.
Azelastine (Allergodil) is a highly effective treatment for allergic rhinitis and conjunctivitis. Used as a nasal spray and eye drops, azelastine has little to no systemic effects.
Used as a nasal spray and eye drops, azelastine has little to no systemic effects.
Another topical antihistamine, bamipine (soventol), in the form of a gel, is intended for use in allergic skin lesions accompanied by itching, insect bites, jellyfish burns, frostbite, sunburn, and mild thermal burns.
Third generation antihistamines (metabolites). Their fundamental difference is that they are active metabolites of antihistamines of the previous generation. Their main feature is the inability to influence the QT interval. Currently, there are two drugs - cetirizine and fexofenadine.
Cetirizine (Zyrtec) is a highly selective peripheral H1 receptor antagonist. It is an active metabolite of hydroxyzine, which has a much less pronounced sedative effect. Cetirizine is almost not metabolized in the body, and the rate of its excretion depends on the function of the kidneys. Its characteristic feature is its high ability to penetrate the skin and, accordingly, its effectiveness in skin manifestations of allergies.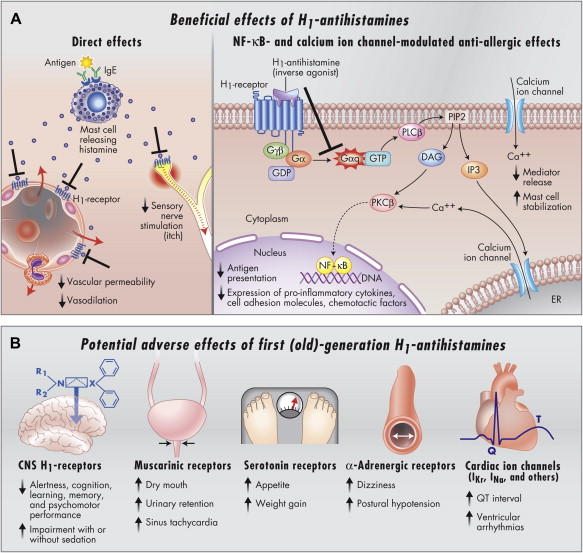 Cetirizine neither experimentally nor in the clinic showed any arrhythmogenic effect on the heart, which predetermined the area of practical use of metabolite drugs and determined the creation of a new drug, fexofenadine.
Cetirizine neither experimentally nor in the clinic showed any arrhythmogenic effect on the heart, which predetermined the area of practical use of metabolite drugs and determined the creation of a new drug, fexofenadine.
Fexofenadine (telfast) is the active metabolite of terfenadine. Fexofenadine does not undergo transformations in the body and its kinetics does not change with impaired liver and kidney function. It does not enter into any drug interactions, does not have a sedative effect and does not affect psychomotor activity. In this regard, the drug is approved for use by persons whose activities require increased attention. A study of the effect of fexofenadine on the QT value showed, both in the experiment and in the clinic, the complete absence of a cardiotropic effect when using high doses and with long-term use. Along with maximum safety, this remedy demonstrates the ability to stop symptoms in the treatment of seasonal allergic rhinitis and chronic idiopathic urticaria. Thus, the pharmacokinetics, safety profile and high clinical efficacy make fexofenadine the most promising of the antihistamines at present.
Thus, the pharmacokinetics, safety profile and high clinical efficacy make fexofenadine the most promising of the antihistamines at present.
So, in the doctor's arsenal there is a sufficient amount of antihistamines with different properties. It must be remembered that they provide only symptomatic relief from allergies. In addition, depending on the specific situation, you can use both different drugs and their diverse forms. It is also important for the physician to be aware of the safety of antihistamines.
| I generation | II generation | III generation |
|
|
|
Return
Antidepressants in gastroenterology practice uMEDp
Antidepressants are widely used in modern gastroenterology.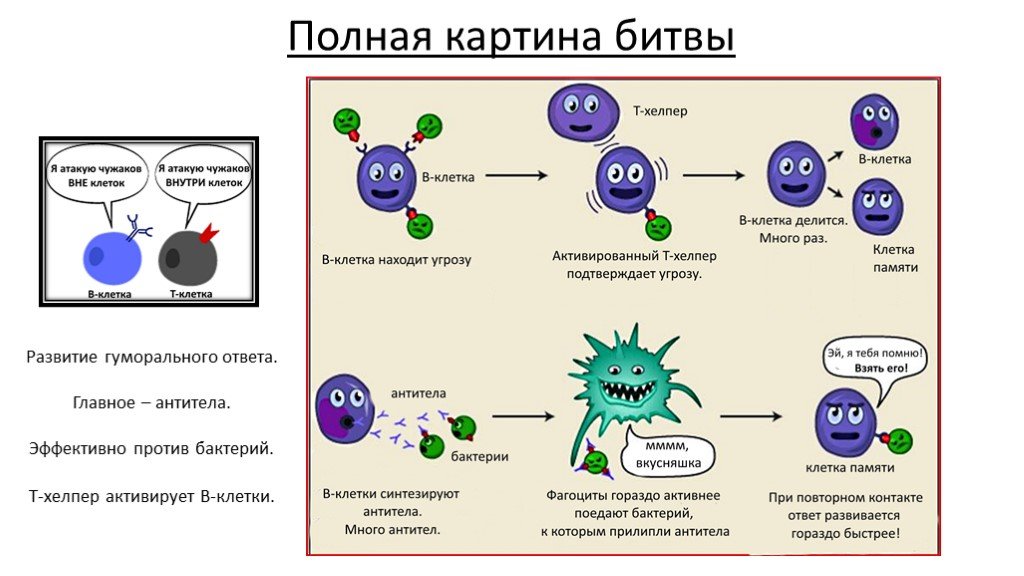 The article discusses the indications for prescribing antidepressants to patients with digestive disorders, discusses the features of antidepressant therapy in gastroenterological patients with comorbid pathology of the cardiovascular system. The main groups of antidepressants - selective serotonin reuptake inhibitors and tricyclic antidepressants - were compared in terms of their therapeutic effects and potential side effects.
The article discusses the indications for prescribing antidepressants to patients with digestive disorders, discusses the features of antidepressant therapy in gastroenterological patients with comorbid pathology of the cardiovascular system. The main groups of antidepressants - selective serotonin reuptake inhibitors and tricyclic antidepressants - were compared in terms of their therapeutic effects and potential side effects.
Pharmacological effects and clinical manifestations of potential side effects of TCAs
Antidepressants are an extensive group of drugs, the mechanism of action of which (with rare exceptions) is determined by a direct effect on the metabolism of neurotransmitters, primarily serotonin, as well as norepinephrine, and less often dopamine [1].
The main therapeutic effect of antidepressants is achieved due to their ability to influence pathologically reduced mood - depression. In this regard, the main indication for prescribing antidepressants are depressive states, which in somatic medicine (including in the practice of a gastroenterologist) include primarily endoform and somatogenic depressions pathogenetically associated with a somatic disease, as well as depressive reactions to the situation of the disease [2 ].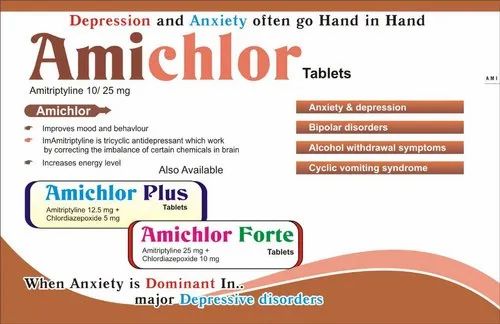
In gastroenterological practice, the anti-anxiety effect is of no less importance. The drugs of this group can be used as a monotherapy for an anxiety disorder or combined with gastroenterological agents in cases where disorders in the digestive system are somatic manifestations of an anxiety or somatoform disorder.
An indication for the appointment of antidepressants may be the relief of symptoms of the overlap of chronic diseases of the digestive system and depression, manifested by a variety of algic syndromes. For example, they include bulimia nervosa and anorexia, which often provoke a malfunction in the digestive organs.
Since the middle of the last century, many antidepressants with different mechanisms of action have been synthesized, and their number continues to grow. The main criteria for choosing an antidepressant, along with therapeutic efficacy, are safety, good tolerability, the absence of severe side effects, and a minimal risk of unwanted interactions with somatotropic drugs [3].
Currently, antidepressants are divided into three groups [1].
First-generation antidepressants include tricyclic antidepressants (TCAs) - amitriptyline, imipramine, pipofezin; as well as irreversible non-selective monoamine oxidase inhibitors - pirlindol. The drugs of this group have a powerful and undifferentiated effect on multiple receptor systems of the body. This mechanism of action causes a high probability of side effects of antidepressants of this group.
Second-generation drugs are selective serotonin reuptake inhibitors (SSRIs) - fluoxetine, fluvoxamine, sertraline, citalopram, as well as selective serotonin and norepinephrine reuptake inhibitors (SNRIs) - duloxetine.
Next-generation drugs include drugs with other and (or) mixed mechanisms of action, which are currently used by gastroenterologists relatively rarely.
Thus, in somatic practice, the use of second-generation drugs is preferable [3-5].
Use of SSRIs
SSRI drugs meet all of the above selection criteria.
The ratio of the severity of various effects (actually antidepressant, stimulant, anti-anxiety, sedative, anticholinergic) differs in different drugs of the group. The most important is the degree of stimulant and anti-anxiety effects, which serves to divide SSRIs [6, 7] into drugs with a predominantly stimulant effect (fluoxetine, paroxetine), drugs with a predominantly anti-anxiety effect (fluvoxamine) and drugs with a balanced effect (sertraline, citalopram).
This difference is important when determining the indications for choosing one or another drug depending on the clinical features of depression in a particular patient. In addition, drugs with a pronounced stimulating effect at the beginning of treatment cause increased anxiety, therefore, in the first two (sometimes four) weeks of treatment, it is necessary to prescribe anxiolytic drugs to prevent this undesirable effect.
Further, when describing drugs of the SSRI group [8], their international names are indicated, and in brackets are the most common trade names.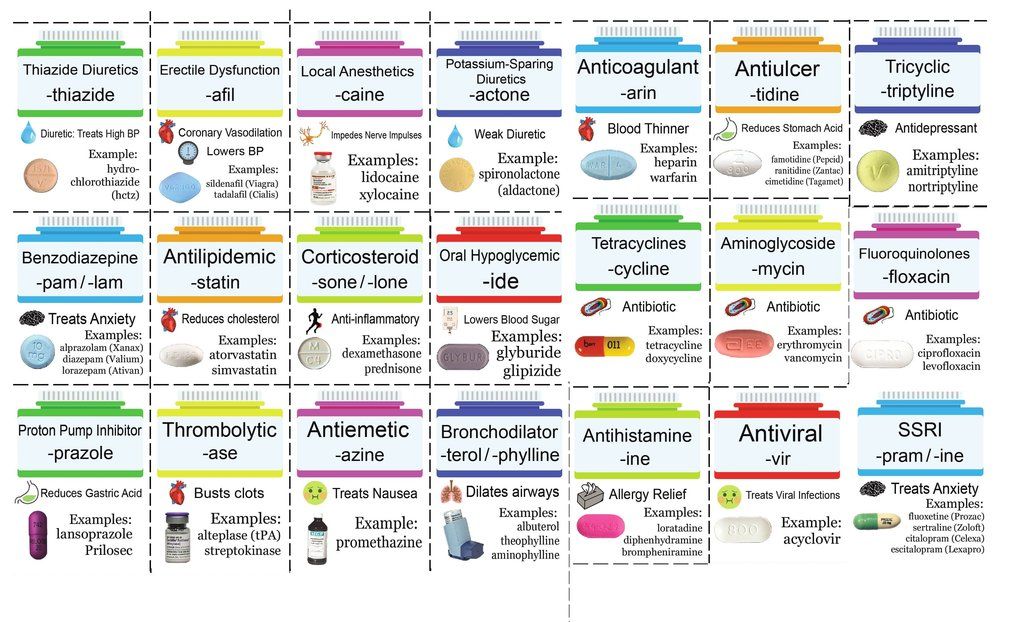
Fluoxetine (Prozac) is the most powerful of the stimulant drugs, so anxiolytics must be added in the first two to four weeks of treatment. The intrinsic anti-anxiety effect of fluoxetine is relatively weak and begins to appear no earlier than two weeks later. Due to the effect on appetite in the direction of reducing it, fluoxetine helps to reduce body weight, which is the purpose of its appointment in bulimia and obesity. The advantages in gastroenterological practice include the absence of nausea and constipation, the disadvantages are the lengthening of the time to reach orgasm (in about 40% of patients).
Paroxetine (Paxil, Reksetin) has a strong stimulating effect, as a result of which it can significantly increase anxiety at the beginning of therapy. In addition, this drug has the strongest effect on mood, up to its pathological increase. For this reason, gastroenterologists are not recommended to prescribe paroxetine without joint observation of the patient with a psychiatrist.
Fluvoxamine (Fevarin) differs from all drugs in the group by the strongest sedative effect with the weakest stimulating effect. In this regard, it is considered the drug of choice for anxious depression or in cases of prescribing an antidepressant for anxiety disorder. At the same time, it is used as monotherapy without additional enhancement of anxiolytic therapy. The advantages include a minimal negative effect on sexual function in comparison with other drugs in this group.
Sertraline (Zoloft, Stimuloton, Asentra) is one of the most widely used antidepressants in the world. Along with a pronounced antidepressant effect, the drug has an anxiolytic and mild stimulating effect. It is well tolerated and therefore can be used in elderly patients without dose reduction. Relatively rarely affects the decrease in libido (
Citalopram (Cipramil, Siozam, PRAM) and Escitalopram (Cipralex, Elycea, Selectra) are the weakest drugs of the SSRI group in terms of the strength of the antidepressant effect.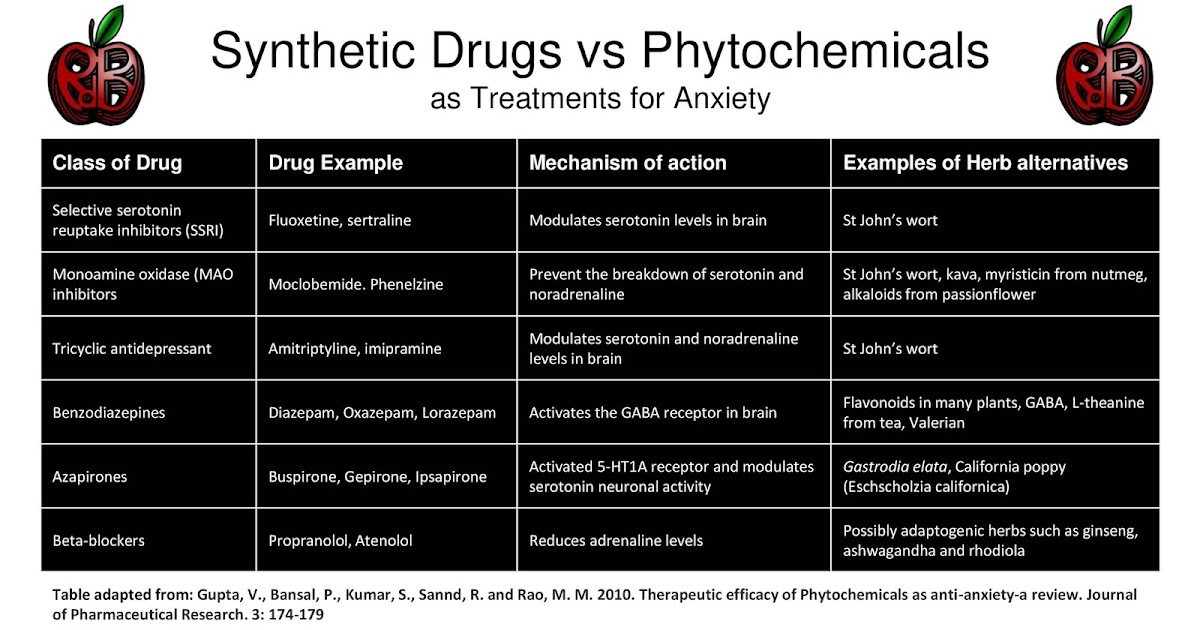 The positive aspects in this case are the best tolerability, safety when used with somatotropic agents, and the absence of cardiotoxicity. These drugs are recommended in the treatment of depression in somatic patients, as they are characterized by a balanced effect and rarely increase anxiety.
The positive aspects in this case are the best tolerability, safety when used with somatotropic agents, and the absence of cardiotoxicity. These drugs are recommended in the treatment of depression in somatic patients, as they are characterized by a balanced effect and rarely increase anxiety.
Based on the foregoing, a differentiated approach to prescribing an antidepressant is as follows:
- fluvoxamine is the drug of choice for anxious depression, as it has the most pronounced anti-anxiety effect;
- with the predominance of apathy and asthenia in the clinical picture, it is advisable to prescribe fluoxetine, since its stimulating effect manifests itself literally from the first days of administration;
- in anxiety-depressive disorder, antidepressants with a balanced effect should be recommended;
- in algic syndrome, the drug from the SNRI group duloxetine (Cymbalta) is more effective (compared to SSRIs).
When choosing a drug for antidepressant therapy in gastroenterological practice, in addition to the generally accepted ones, the following clarifications should be made:
- Nausea is a fairly common early side effect of SSRIs.
 The patient should be warned about this, adding that most often this symptom is mild and transient. Otherwise, the patient may assume an exacerbation of his gastroenterological disease and refuse to take the antidepressant. A much more rare manifestation of side effects may be vomiting;
The patient should be warned about this, adding that most often this symptom is mild and transient. Otherwise, the patient may assume an exacerbation of his gastroenterological disease and refuse to take the antidepressant. A much more rare manifestation of side effects may be vomiting; - Nausea is most severe during treatment with fluvoxamine. If this symptom is present as a sign of an exacerbation of a gastroenterological disease, it is better to initially choose a different antidepressant;
- Many SSRIs aggravate constipation. In the presence of persistent constipation, fluoxetine is the drug of choice;
- Long-lasting side effects of antidepressants that are important for gastroenterological practice include dry mouth. When conducting antidepressant therapy, it is necessary to control the intensity of this symptom. Since dry mouth is a manifestation of the excessive anticholinergic effect of the antidepressant, if this symptom is significant, it is necessary to reduce the dose of the antidepressant if possible;
- used in patients with chronic liver diseases, the hepatoprotector ademetionine (Heptral) has an antidepressant effect, but the strength of this effect is insignificant.

Before starting treatment with SSRIs, the patient must be explained the advisability of prescribing an antidepressant, possible side effects and the duration of treatment. When prescribing a drug with a stimulating effect, it is necessary to justify the need for additional prescription of a drug with an anxiolytic effect. In addition, it is worth emphasizing that the expected effect occurs no earlier than after four to six weeks of taking the drug at a therapeutic dose. Without knowing about this feature, the patient may stop taking the antidepressant without waiting for a therapeutic response.
Antidepressant therapy with SSRIs includes three stages [3, 8].
The first stage is the selection of a therapeutic dose. The first dose of the drug is 1/4 or 1/2 of a single dose, followed by a gradual increase depending on tolerance. Individual sensitivity to the drug may play a role, but it is difficult to predict before the start of therapy.
Therapy is considered ineffective if a clear improvement does not occur after four to six weeks of taking a sufficient dose of the drug.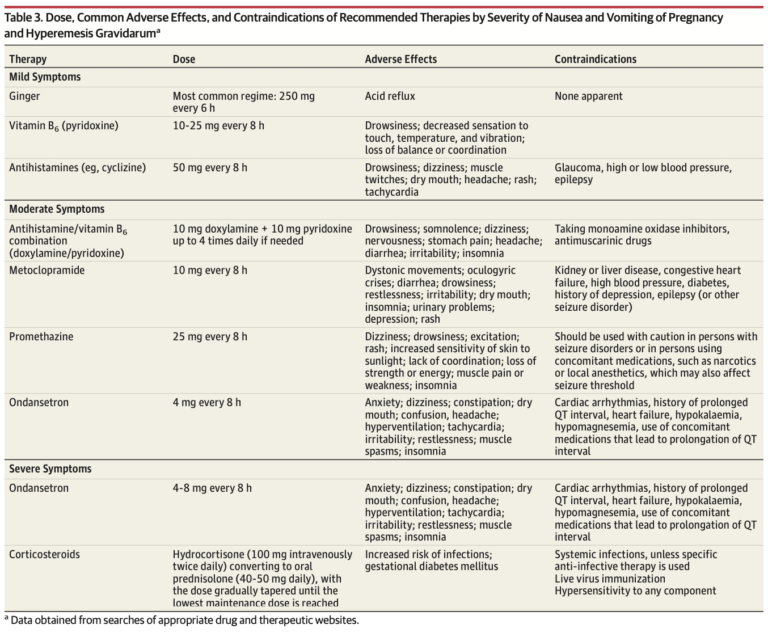 In this case, the question arises of replacing the drug. In most cases, by the 10-12th week of treatment, the symptoms of depression completely disappear. As practice shows, some patients perceive this as a cure, which is the reason for self-cessation of the drug.
In this case, the question arises of replacing the drug. In most cases, by the 10-12th week of treatment, the symptoms of depression completely disappear. As practice shows, some patients perceive this as a cure, which is the reason for self-cessation of the drug.
At the second stage, maintenance therapy is carried out. Numerous clinical observations indicate that the interruption of antidepressant therapy immediately after improvement in well-being in 80–90% of cases leads to a relapse of the disease. Contrary to popular belief, antidepressants are not associated with the risk of drug dependence, so the treatment of depression and panic disorder should be long enough. The course of maintenance therapy should be carried out for at least six to nine months. It is quite obvious that the patient will comply with these recommendations only if the drug is well tolerated.
The third stage is to cancel the drug. The general rule is the gradual withdrawal of any drug. It is recommended to first take a half dose for a month, then a half dose every other day. If symptoms of depression return, treatment should be continued.
If symptoms of depression return, treatment should be continued.
Application of TCA
The therapeutic effect of TCAs is manifested by powerful antidepressant and anti-anxiety effects. In addition, their advantage is a strong analgesic effect, which is more pronounced in comparison with SSRIs [3, 8].
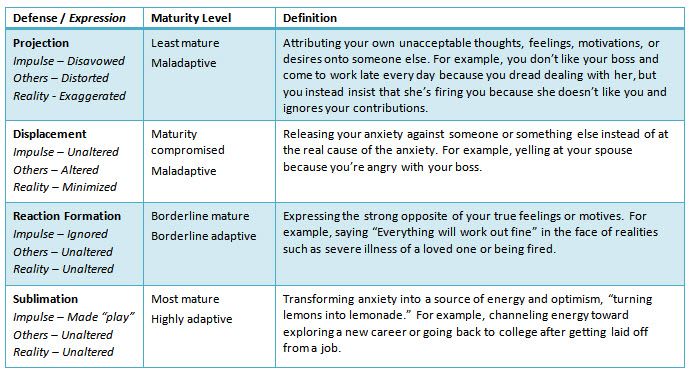
It is very important to emphasize the interaction of TCAs with various receptor structures and, as a result, the development of multiple effects (anticholinergic, adrenolytic, adrenomimetic). With significant severity, these effects are manifested by side effects of TCAs [3, 4]. The table presents the clinical manifestations of potential side effects of TCAs in comparison with the spectrum of their pharmacological effects.
The indicated side effects are most likely in the presence of comorbid somatic pathology, and therefore it is not recommended to prescribe TCAs to elderly and senile patients [3].
In young patients with moderate or moderate depression without comorbidities, TCAs still remain an important component of therapy.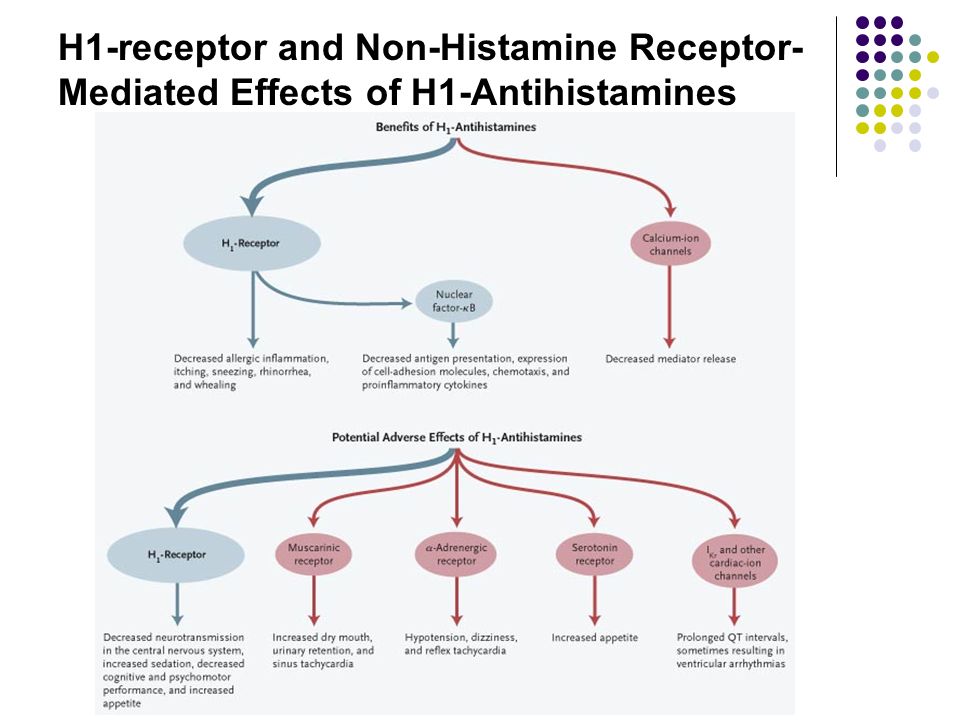 At the same time, it is necessary to remember such contraindications to the appointment of TCAs as glaucoma, heart rhythm disturbance, atrioventricular blockade, convulsive syndrome.
At the same time, it is necessary to remember such contraindications to the appointment of TCAs as glaucoma, heart rhythm disturbance, atrioventricular blockade, convulsive syndrome.
Amitriptyline (Triptizol) has received the greatest distribution in gastroenterology and is widely used in small doses. At the same time, it should be borne in mind that doses of 50 mg or less do not have an antidepressant effect, but only cause a sedative, anti-anxiety and hypnotic effect. The initial dose is 12.5 mg an hour before bedtime with a gradual increase depending on tolerance.
The antidepressant effect is achieved in a daily dose of at least 100 mg, which is poorly tolerated by somatic patients due to the above effects. In this regard, increasing the dose is possible only when observed together with a psychiatrist.
A useful property is the analgesic effect, which is more pronounced than that of SSRIs.
Side effects are associated with its anticholinergic (dry mucous membranes, constipation, urinary retention, tachycardia, disturbance of accommodation) and antihistamine (drowsiness, sedation) effects.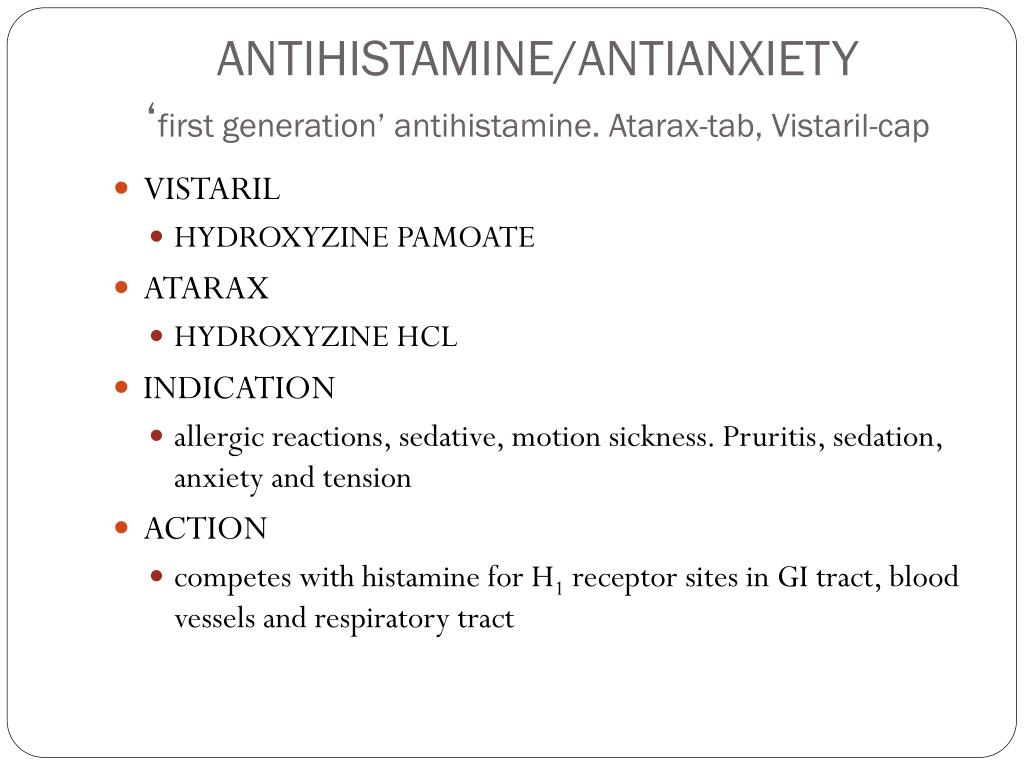
Pipofezin (Azaphen) is practically not used in psychiatry due to the weakness of the antidepressant effect. Indications for use are limited to shallow depressive disorders of the neurotic level. Anticholinergic side effects and cardiotoxicity are almost absent. It can be used in elderly, somatically debilitated patients, including in outpatient practice. The recommended dose is 75 mg per day divided into three doses.
The effectiveness of TCA treatment can be assessed no earlier than three to four weeks after the start of therapy.
When prescribing antidepressants to patients with chronic diseases of the digestive system, it is necessary to take into account comorbidity, primarily with diseases of the cardiovascular system.
Based on the likelihood and severity of possible side effects, three groups of antidepressants are distinguished depending on the degree of their cardiotoxicity [9]. In patients with comorbidity of gastroenterological and cardiac diseases, the use of drugs with a low degree of cardiotoxic risk is recommended.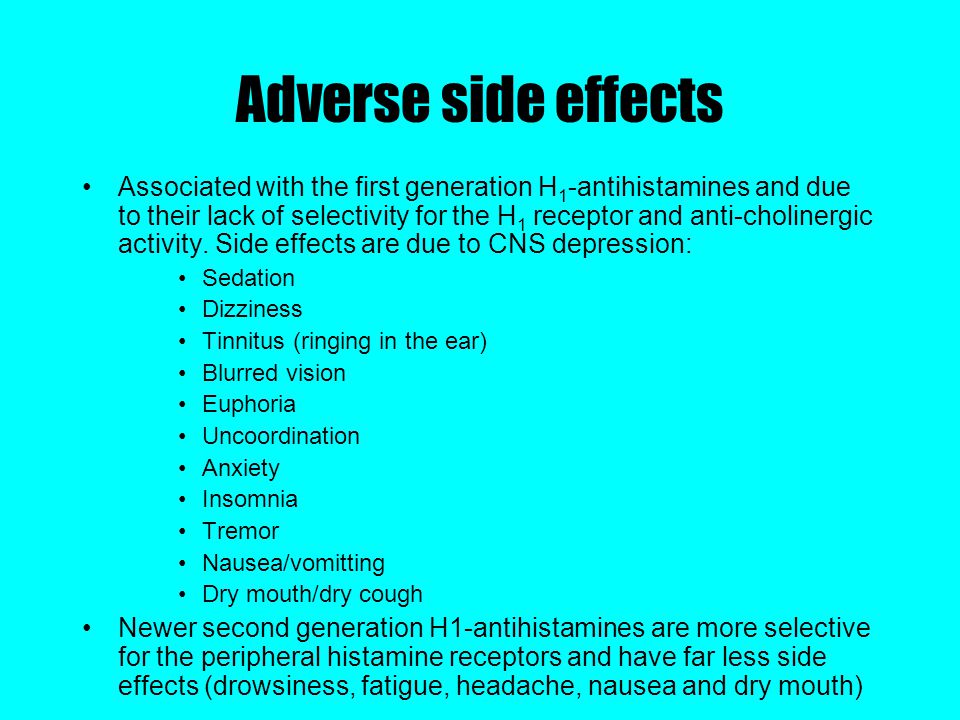 This group includes SSRIs (fluoxetine, sertraline, citalopram, fluvoxamine, paroxetine), from drugs of other groups - pirlindol, tianeptine, mirtazapine, mianserin, trazodone.
This group includes SSRIs (fluoxetine, sertraline, citalopram, fluvoxamine, paroxetine), from drugs of other groups - pirlindol, tianeptine, mirtazapine, mianserin, trazodone.
The average cardiotoxic risk includes the use of low doses of TCAs, which can cause side effects from the cardiovascular system (orthostatic hypotension, sinus tachycardia, rhythm and conduction disturbances, depression of contractility and a decrease in heart rate variability). When using them, it is necessary to take into account the possibility of worsening the somatic condition of the patient. Treatment with these drugs, if indicated, should be carried out in conjunction with a psychiatrist.
Drugs with a high cardiotoxic risk (which, in particular, include TCAs in medium and high doses) should not be used to treat patients with cardiovascular diseases.
Conclusion
Without a doubt, antidepressants have a wide range of indications for the appointment of gastroenterological patients.