Another name for hydroxyzine
Mental Health Medications | NAMI: National Alliance on Mental Illness
Brand names:
- Vistaril®
- Capsule: 25 mg, 50 mg
- Liquid: 25 mg/5 ml suspension
- Atarax®
- Tablet: 10 mg, 25 mg, 50 mg
- Liquid: 10 mg/5 ml
- Injection: 25 mg/ml, 50 mg/ml
Generic name: hydroxyzine (hye DROKS i zeen)
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
What Is Hydroxyzine And What Does It Treat?
Hydroxyzine is an antihistamine. It is approved for the treatment of anxiety. However, hydroxyzine is also used to treat difficulty sleeping, nausea, vomiting, itching, skin rash, and allergies.
Symptoms of anxiety include:
- Feeling nervous
- Feeling fearful
- Excessive worrying
- Difficulty sleeping
- Difficulty concentrating
- Irritability
What Is The Most Important Information I Should Know About Hydroxyzine?
Do not drive a car or operate machinery until you know how this medication affects you because you may notice that you feel tired or dizzy.
Hydroxyzine is not a controlled substance. It does not have the risk of addiction like some other medications used to treat anxiety e.g., lorazepam (Ativan®), alprazolam (Xanax®), clonazepam (Klonopin®), and other benzodiazepines.
Are There Specific Concerns About Hydroxyzine And Pregnancy?
If you are planning on becoming pregnant, notify your healthcare provider to best manage your medications. People living with anxiety disorders who wish to become pregnant face important decisions. It is important to discuss this with your doctor and caregivers.
Hydroxyzine should not be used in the first trimester of pregnancy. Studies that were done with mice and rats found an increased risk of birth defects. The risk to humans in the first trimester is unclear due to lack of well-controlled studies in humans. Hydroxyzine may be used in the second and third trimesters of pregnancy, but it should not be used during or just prior to labor. Use of hydroxyzine during labor may increase seizure risk in infants, decrease fetal heart rate, and increase side effects when combined with narcotics.
Regarding breastfeeding, use is not recommended since hydroxyzine does pass into breast milk. Infants who have received other antihistamines have experienced drowsiness, irritability, or unusual excitement. In addition, it may lower milk production in the mother.
What Should I Discuss With My Healthcare Provider Before Taking Hydroxyzine?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you experience side effects from your medications, discuss them with your healthcare provider. Some side effects may pass with time, but others may require changes in the medication.
- Any other psychiatric or medical problems you have, including obstructive sleep apnea
- All other medications you are currently taking (including over the counter products and herbal and nutritional supplements) and any medication allergies you have, including allergies to cetirizine (Zyrtec®) or levocetirizine (Xyzal®)
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment.
 Your provider can explain how these different treatments work with the medication
Your provider can explain how these different treatments work with the medication - If you are elderly or are prone to falls
- If you are pregnant, plan to become pregnant, or are breast-feeding
- If you drink alcohol or use drugs
- If you have a heart condition known as a prolonged QT interval
How Should I Take Hydroxyzine?
Hydroxyzine may be taken with or without food. Take with food if you experience an upset stomach.
Hydroxyzine may be taken every day at regular times or on an as needed (“PRN”) basis. Typically, your healthcare provider will limit the number of doses you should take in one day.
Your health care provider will determine the dose and method of taking the medication that is right for you based upon your response.
If you take the medication every day (instead of ‘as needed’), use a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take it. You may also ask a family member or a friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Hydroxyzine?
If you miss a dose of hydroxyzine, take it as soon as you remember, unless it is closer to the time of your next dose. Discuss this with your healthcare provider. Do not double your next dose or take more than what is prescribed.
What Should I Avoid While Taking Hydroxyzine?
Avoid drinking alcohol and using illegal drugs while you are taking hydroxyzine. They may decrease the benefits (e.g., worsen your condition) and increase the adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Hydroxyzine?
If an overdose occurs call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
Symptoms of overdose include severe drowsiness, dry mouth, difficulty urinating, headache, rapid heartbeat, confusion, impaired coordination, slow reflexes, seizures, or coma.
A specific treatment to reverse the effects of hydroxyzine does not exist.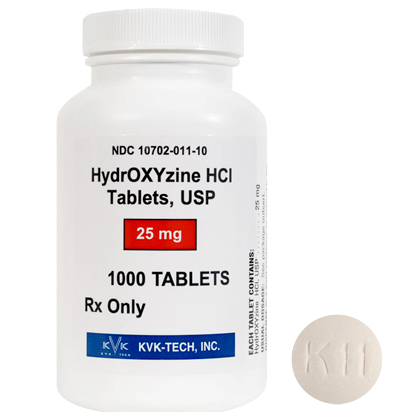
What Are Possible Side Effects Of Hydroxyzine?
Common side effects
- Dizziness, drowsiness, fatigue, dry mouth
- Urinary retention, blurred vision, confusion, irritability
- Headache
Rare/serious side effects
- Allergic reaction (difficulty breathing; hives; swelling of your lips, tongue or face)
- Increased heart rate, unsafe heart beat (long QT on ECG), confusion, hallucinations
- Priapism (an erection in males that does not go away after 4 hours)
- Skin rash known as acute generalized exanthematous pustulosis (AGEP)
Are There Any Risks For Taking Hydroxyzine For Long Periods Of Time?
To date, there are no known problems associated with the long-term use of hydroxyzine. It is a safe and effective medication when used as directed.
Physician should reassess periodically the usefulness of the drug for the individual patient.
What Other Medications May Interact With Hydroxyzine?
The following medications may increase the levels and effects of hydroxyzine:
- Other antihistamines, such as diphenhydramine (Benadryl®) and cetirizine (Zyrtec®)
- Other medications with anticholinergic effects, such as benztropine (Cogentin®)
- Other medications that can cause drowsiness, such as zolpidem (Ambien®)
- Other medications that increase the heart’s QT interval such as amitriptyline (Elavil®), citalopram (Celexa®), and methadone.
How Long Does It Take For Hydroxyzine To Work?
Symptoms of anxiety or insomnia may improve within hours of the first dose of medication.
Summary of FDA Black Box Warnings
Hydroxizine does not have any black box warnings.
Provided by
(September 2021)
©2021 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Hydroxyzine for Anxiety — How It Works
When asked to think of medications commonly used to treat anxiety, chances are high that selective serotonin reuptake inhibitors (SSRIs)—such as Lexapro and Zoloft—or benzodiazepines—like Ativan, Xanax, and Klonopin —frequently come to mind. But these are not the only kinds of medications that can effectively treat anxiety. Another option to consider is hydroxyzine, a prescription antihistamine that is approved to treat anxiety. (Hydroxyzine for sleep is also a common treatment.)
This Minded Medication Guide will take a closer look at hydroxyzine for anxiety to help you when talking with your doctor, prescribing nurse, or Minded provider to choose the right medication for your treatment plan.
Read on to learn more about this medication, including:
- What is hydroxyzine?
- How does hydroxyzine work for anxiety?
- What is the best dose of hydroxyzine for anxiety?
- What are some of the possible side effects of hydroxyzine?
- What cautions should you be aware of before, during, and after using hydroxyzine for anxiety?
- How long does it take for hydroxyzine to work for anxiety?
- How does hydroxyzine compare to other types of anxiety medications?
Minded Medication Guides, including Zoloft vs Prozac and Wellbutrin vs Lexapro, are intended as educational aids only. They are not intended as medical advice for individual conditions or treatment. They are not a substitute for a medical exam, nor do they replace the need for services provided by medical professionals. Talk to your doctor, nurse, or pharmacist before taking any prescription medication or following any treatment or regimen.
Talk to your doctor, nurse, or pharmacist before taking any prescription medication or following any treatment or regimen.
Hydroxyzine is an antihistamine used to treat anxiety. It is also sometimes used to treat:
- Allergies
- Difficulty sleeping
- Itching
- Nausea
- Skin rash
- Vomiting
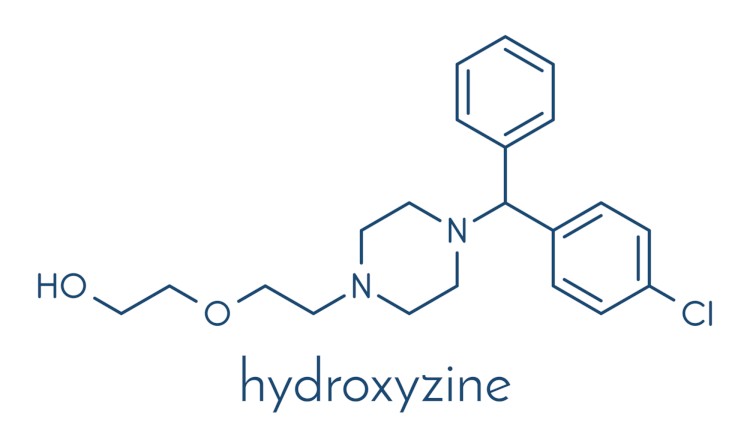
As with all antihistamines, hydroxyzine works by reducing the effects of histamine (a chemical in your body that produces an allergic reaction).
However, while many antihistamines are available over-the-counter (without a prescription), hydroxyzine is a prescription medication. You may see it listed as hydroxyzine hydrochloride (hydroxyzine HCL) or hydroxyzine pamoate (hydroxyzine pam). It may also be listed under the brand name Vistaril.
How does hydroxyzine for anxiety work?
While hydroxyzine is an antihistamine, it is also a serotonin antagonist. In other words, taking hydroxyzine or Vistaril for anxiety works similarly to taking SSRIs—another type of medication used to treat anxiety—by making more serotonin available in your brain. As a serotonin antagonist, hydroxyzine boosts the levels of serotonin in your brain by blocking it from being reabsorbed into the nerves in your brain (called neurons). Serotonin is a neurotransmitter that plays a role in keeping your mood balanced. It also affects feelings of contentment, optimism, and satisfaction, and your overall sense of well-being.
In other words, taking hydroxyzine or Vistaril for anxiety works similarly to taking SSRIs—another type of medication used to treat anxiety—by making more serotonin available in your brain. As a serotonin antagonist, hydroxyzine boosts the levels of serotonin in your brain by blocking it from being reabsorbed into the nerves in your brain (called neurons). Serotonin is a neurotransmitter that plays a role in keeping your mood balanced. It also affects feelings of contentment, optimism, and satisfaction, and your overall sense of well-being.
{{ads-green-dots="/templates/cta"}}
When taking hydroxyzine for anxiety, it can be prescribed in capsule, tablet, and liquid forms. As mentioned above, this medication is available as hydroxyzine hydrochloride (hydroxyzine HCL) or hydroxyzine pamoate (hydroxyzine pam). While hydroxyzine pamoate is available in both generic and branded forms (branded as Vistaril), hydroxyzine hydrochloride is only available as a generic. (The branded version of hydroxyzine HCL, called Atarax, was discontinued.)
(The branded version of hydroxyzine HCL, called Atarax, was discontinued.)
Hydroxyzine pamoate for anxiety
Hydroxyzine pamoate (Vistaril):
Capsules
- 25 mg
- 50 mg
Liquid
- 25 mg/5 ml
Hydroxyzine HCL for anxiety
Hydroxyzine hydrochloride (HCL)
Tablets
- 10 mg
- 25 mg
- 50 mg
Liquid
- 10 mg/5 ml
Best dose of hydroxyzine for anxiety
When prescribing hydroxyzine for anxiety, doctors and nurse practitioners typically recommend taking it in multiple doses throughout the day. For adults, 50 to 100 mg (taken 4 times a day) is typical, though some people may need higher doses to achieve symptom relief. For children under the age of 6 years old, no more than 50 mg per day (divided into small doses) is recommended.
Hydroxyzine can be taken daily (with or without food) at regularly scheduled times or on an as-needed basis. If you have an upset stomach after taking hydroxyzine, you may want to take it with food. Your doctor or prescribing nurse will provide you with instructions on how often and when to take this medication, as well as the maximum amount to take in a day.
If you miss a dose of hydroxyzine, either take the missed dose as soon as you remember—or, if it is closer to the time when you would take your next dose, just take the next dose.
Which is better for anxiety: hydroxyzine HCL vs hydroxyzine pam?
Both hydroxyzine hydrochloride (HCL) and hydroxyzine pamoate (pam) can be prescribed to treat anxiety. The main difference between the two is the form that each is available in—hydroxyzine HCL is available in tablets and liquid, while hydroxyzine pam is available in capsules and liquid.
You may prefer one form of medication over the other (tablets vs capsules), or you may find that one or the other works better for you personally. Your doctor, prescribing nurse, or Minded professional can work with you to determine which form of this medication is best for your anxiety treatment plan.
Your doctor, prescribing nurse, or Minded professional can work with you to determine which form of this medication is best for your anxiety treatment plan.
Hydroxyzine side effects
Common side effects of hydroxyzine include:
- Blurred vision
- Confusion
- Dizziness
- Drowsiness
- Dry mouth
- Fatigue
- Headache
- Irritability
- Urinary retention (when your bladder does not empty all the way)
Talk to your doctor or the experts at Minded if you experience any of these or other side effects.
Rare or serious side effects of hydroxyzine include:
- Allergic reaction to the medication, even though the medication generally is taken to reduce allergic reactions (symptoms of this could include: difficulty breathing; hives; and swelling in your lips, tongue, or face)
- Confusion
- Hallucinations
- Increased heart rate and/or abnormal heartbeat
- Priapism (an erection lasting longer than 4 hours)
- Skin rash (called acute generalized exanthematous pustulosis, or AGEP)
Seek medical attention right away if you experience any of these (or other) serious side effects.
Hydroxyzine warnings
Drinking alcohol is not recommended while taking hydroxyzine. Alcohol can decrease the benefits of medications like hydroxyzine and increase their side effects (such as sedation). Alcohol also can impair memory and judgment, accidentally resulting in taking a higher dose of hydroxyzine than prescribed, which could induce an accidental overdose.
Symptoms of a hydroxyzine overdose include:
- Coma
- Confusion
- Decreased coordination
- Difficulty urinating
- Drowsiness
- Dry mouth
- Headache
- Rapid heartbeat
- Slowed reflexes
- Seizures
Always discuss your anxiety treatment plan with your doctor if you are pregnant or planning on becoming pregnant. Hydroxyzine should typically not be taken during the first trimester of pregnancy. While you may take it during the second and third trimesters, it should not be taken right before or during labor.
Because hydroxyzine can be passed to your baby through breast milk, taking it while breastfeeding is not recommended.
Tell your doctor or a Minded professional about any other medications or supplements you may be taking to determine if hydroxyzine might have any negative interactions with them.
When taking hydroxyzine or Vistaril for anxiety, how long does it take to work?
If you're taking hydroxyzine for anxiety, you will find that it is relatively fast-acting compared to some other medications, like SSRIs. While you may have to take SSRIs for a few weeks before you start to see improvement in your anxiety symptoms, with hydroxyzine, you may notice your symptoms begin to improve quickly, often within hours of first taking it.
How long does hydroxyzine last for anxiety?
The effects of hydroxyzine typically last 3 to 4 hours.
SSRIs vs hydroxyzine for anxiety
While you can take selective serotonin reuptake inhibitors (SSRIs) or hydroxyzine for anxiety, there are some key differences to keep in mind.
- How quickly your anxiety symptoms begin to decrease: While you may notice that your anxiety symptoms begin to decrease hours after first taking hydroxyzine, the benefits of SSRIs may not begin to become apparent until a few weeks after you start taking them.
- How often you take the medications: Hydroxyzine is typically taken in multiple doses throughout the day. SSRIs usually are taken once daily.
- Common side effects: Both hydroxyzine and SSRIs come with a risk of side effects, but the side effects for each are different.
- Common side effects of hydroxyzine include: blurred vision, confusion, dizziness, dry mouth, fatigue, headache, irritability, urinary retention
- Common side effects of SSRIs include: dizziness, drowsiness, dry mouth, headache, insomnia, nervousness, sexual problems, stomach upset, weight gain, and/or weight loss
- Whether they can be taken during pregnancy and/or while breastfeeding: Hydroxyzine can be taken during the second and third trimesters, but not during the first trimester or right before or during labor.
 SSRIs may be taken during pregnancy, with the approval of an OB-GYN doctor. Neither hydroxyzine nor SSRIs should be taken while breastfeeding without first talking to your OB-GYN doctor or pediatrician.
SSRIs may be taken during pregnancy, with the approval of an OB-GYN doctor. Neither hydroxyzine nor SSRIs should be taken while breastfeeding without first talking to your OB-GYN doctor or pediatrician.
Benzodiazepines vs hydroxyzine for anxiety
Benzodiazepines—such as Xanax and Ativan and Klonopin—are another type of medication that can be used to treat anxiety. Like hydroxyzine, these medications are relatively fast-acting—your symptoms may begin to decrease within hours of taking your first dose. Also, like taking hydroxyzine for anxiety, benzodiazepines are typically taken in multiple doses throughout the day. There are, however, several important differences between hydroxyzine and benzodiazepines to consider.
- Common side effects: Both hydroxyzine and benzodiazepines come with a risk of side effects, but the side effects for each are different.
- Common side effects of hydroxyzine include: blurred vision, confusion, dizziness, dry mouth, fatigue, headache, irritability, urinary retention
- Common side effects of benzodiazepines include: decreased coordination, difficulty concentrating, dizziness, drowsiness, fatigue, lightheadedness
- Whether they can be taken during pregnancy and/or while breastfeeding: Hydroxyzine can be taken during the second and third trimesters, but not during the first trimester or right before or during labor.
 Benzodiazepines typically should not be taken during pregnancy. Neither hydroxyzine nor benzodiazepines should be taken while breastfeeding without talking to your OB-GYN doctor or pediatrician.
Benzodiazepines typically should not be taken during pregnancy. Neither hydroxyzine nor benzodiazepines should be taken while breastfeeding without talking to your OB-GYN doctor or pediatrician. - How long they are usually used for: While hydroxyzine may be taken long-term, benzodiazepines are typically prescribed for short-term use (weeks or months).
Another thing to keep in mind is that even though the Drug Enforcement Administration has classified benzodiazepines as controlled substances, they are considered safe for most people who take them for anxiety. The risk of dependence or abuse is higher in people with a history of a substance use disorder as well as those who take more than the prescribed dose of the medication.
On the other hand, hydroxyzine is not a controlled substance and does not carry the same risk of dependency or abuse.
Hydroxyzine vs Benadryl for anxiety
While hydroxyzine and Benadryl (the brand name for diphenhydramine) are both antihistamines, this does not mean they can both be used to treat anxiety. Benadryl, which is available over-the-counter (meaning it does not require a prescription) is not approved to treat anxiety—it is approved to treat hay fever, allergies, and cold symptoms. In fact, increased anxiety, agitation, and nervousness are potential side effects of Benadryl.
Benadryl, which is available over-the-counter (meaning it does not require a prescription) is not approved to treat anxiety—it is approved to treat hay fever, allergies, and cold symptoms. In fact, increased anxiety, agitation, and nervousness are potential side effects of Benadryl.
Additionally, while hydroxyzine is considered safe for long-term use, Benadryl may increase your risk of developing dementia if used long-term, according to a 2015 study published in CMAJ. A 2017 study published in Neurology Clinical Practice also found that there is a risk of becoming dependent on or misusing Benadryl. However, as with benzodiazepines, this risk may be higher in people who have a history of addiction.
If you are looking for a fast-acting medication that can be taken long-term for anxiety treatment, it may be worth discussing hydroxyzine with your doctor, prescribing nurse, or a Minded professional.
When comparing hydroxyzine to other common types of anxiety medications, it is important to remember that each type of medication has its own pros and cons. And while there are some similarities between the different kinds of medications, there are also some key differences. For example:
And while there are some similarities between the different kinds of medications, there are also some key differences. For example:
- Whether it is safe for long-term use: Like SSRIs (and generally unlike benzodiazepines), hydroxyzine can be taken long-term.
- The number of doses taken per day: Like benzodiazepines (and unlike SSRIs), hydroxyzine is taken in multiple doses throughout the day rather than once daily.
- How quickly symptom relief may begin: Hydroxyzine is fast-acting (like benzodiazepines), with symptoms typically starting to improve within a few hours of the first dose (compared to a few weeks for SSRIs).
- Whether it is safe to drink alcohol while taking this medication: Drinking alcohol is not recommended while on hydroxyzine (the same is true of SSRIs and benzodiazepines).
- Whether this medication can be taken during pregnancy or while breastfeeding: Hydroxyzine can be taken during the second and third trimesters of pregnancy (except right before and during labor).
 SSRIs and benzodiazepines typically should not be taken during pregnancy. None of these medications should be taken while breastfeeding.
SSRIs and benzodiazepines typically should not be taken during pregnancy. None of these medications should be taken while breastfeeding.
To find out if hydroxyzine could work for your anxiety treatment, visit Minded and get a free assessment. Minded offers online appointments with board-certified psychiatrists and nurse practitioners. If you already have a hydroxyzine prescription, Minded can help you refill or renew it online. Our team of professionals can also assist with adjusting your dosage or advising you about other medications that might be a good fit for your needs.
ANTIHISTAMINS: from diphenhydramine to telfast | #03/01
Historically, the term "antihistamines" means drugs that block H1-histamine receptors, and drugs that act on H2-histamine receptors (cimetidine, ranitidine, famotidine, etc.) are called H2-histamine blockers. The former are used to treat allergic diseases, the latter are used as antisecretory agents.
Histamine, this most important mediator of various physiological and pathological processes in the body, was chemically synthesized in 1907 year. Subsequently, it was isolated from animal and human tissues (Windaus A., Vogt W.). Even later, its functions were determined: gastric secretion, neurotransmitter function in the central nervous system, allergic reactions, inflammation, etc. Almost 20 years later, in 1936, the first substances with antihistamine activity were created (Bovet D., Staub A.). And already in the 60s, the heterogeneity of histamine receptors in the body was proven and three of their subtypes were identified: H1, H2 and H3, differing in structure, localization and physiological effects that occur during their activation and blockade. Since that time, an active period of synthesis and clinical testing of various antihistamines begins.
Subsequently, it was isolated from animal and human tissues (Windaus A., Vogt W.). Even later, its functions were determined: gastric secretion, neurotransmitter function in the central nervous system, allergic reactions, inflammation, etc. Almost 20 years later, in 1936, the first substances with antihistamine activity were created (Bovet D., Staub A.). And already in the 60s, the heterogeneity of histamine receptors in the body was proven and three of their subtypes were identified: H1, H2 and H3, differing in structure, localization and physiological effects that occur during their activation and blockade. Since that time, an active period of synthesis and clinical testing of various antihistamines begins.
Numerous studies have shown that histamine, acting on the receptors of the respiratory system, eyes and skin, causes characteristic allergy symptoms, and antihistamines that selectively block H1-type receptors can prevent and stop them.
Most of the antihistamines used have a number of specific pharmacological properties that characterize them as a separate group. These include the following effects: antipruritic, decongestant, antispastic, anticholinergic, antiserotonin, sedative and local anesthetic, as well as the prevention of histamine-induced bronchospasm. Some of them are not due to histamine blockade, but to structural features.
These include the following effects: antipruritic, decongestant, antispastic, anticholinergic, antiserotonin, sedative and local anesthetic, as well as the prevention of histamine-induced bronchospasm. Some of them are not due to histamine blockade, but to structural features.
Antihistamines block the action of histamine on H1 receptors by the mechanism of competitive inhibition, and their affinity for these receptors is much lower than that of histamine. Therefore, these drugs are not able to displace histamine bound to the receptor, they only block unoccupied or released receptors. Accordingly, H1 blockers are most effective in preventing immediate allergic reactions, and in the case of a developed reaction, they prevent the release of new portions of histamine.
According to their chemical structure, most of them are fat-soluble amines, which have a similar structure. The core (R1) is represented by an aromatic and/or heterocyclic group and is linked via a nitrogen, oxygen or carbon (X) molecule to the amino group. The core determines the severity of antihistamine activity and some of the properties of the substance. Knowing its composition, one can predict the strength of the drug and its effects, such as the ability to penetrate the blood-brain barrier.
The core determines the severity of antihistamine activity and some of the properties of the substance. Knowing its composition, one can predict the strength of the drug and its effects, such as the ability to penetrate the blood-brain barrier.
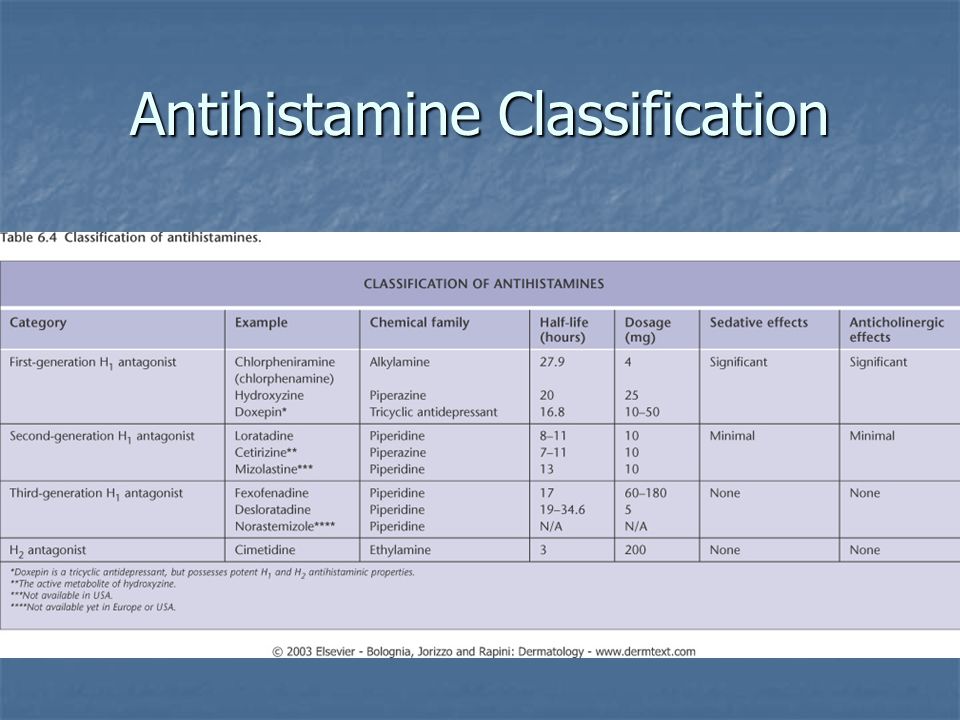
There are several classifications of antihistamines, although none of them is generally accepted. According to one of the most popular classifications, antihistamines are divided into first and second generation drugs according to the time of creation. First-generation drugs are also called sedatives (according to the dominant side effect), in contrast to non-sedative second-generation drugs. At present, it is customary to isolate the third generation: it includes fundamentally new drugs - active metabolites that, in addition to the highest antihistamine activity, exhibit the absence of a sedative effect and the cardiotoxic effect characteristic of second-generation drugs (see table).
In addition, according to the chemical structure (depending on the X-bond), antihistamines are divided into several groups (ethanolamines, ethylenediamines, alkylamines, derivatives of alphacarboline, quinuclidine, phenothiazine, piperazine and piperidine).
First generation antihistamines (sedatives). All of them are well soluble in fats and, in addition to H1-histamine, also block cholinergic, muscarinic and serotonin receptors. Being competitive blockers, they reversibly bind to H1 receptors, which leads to the use of rather high doses. The following pharmacological properties are most characteristic of them.
- Sedative effect is determined by the fact that most of the first generation antihistamines, being easily dissolved in lipids, penetrate well through the blood-brain barrier and bind to the H1-receptors of the brain. Perhaps their sedative effect consists of blocking the central serotonin and acetylcholine receptors. The degree of manifestation of the sedative effect of the first generation varies in different drugs and in different patients from moderate to severe and increases when combined with alcohol and psychotropic drugs. Some of them are used as sleeping pills (doxylamine). Rarely, instead of sedation, psychomotor agitation occurs (more often in medium therapeutic doses in children and in high toxic doses in adults).
 Due to the sedative effect, most drugs should not be used during tasks that require attention. All first-generation drugs potentiate the action of sedative and hypnotic drugs, narcotic and non-narcotic analgesics, monoamine oxidase inhibitors and alcohol.
Due to the sedative effect, most drugs should not be used during tasks that require attention. All first-generation drugs potentiate the action of sedative and hypnotic drugs, narcotic and non-narcotic analgesics, monoamine oxidase inhibitors and alcohol. - The anxiolytic effect characteristic of hydroxyzine may be due to the suppression of activity in certain areas of the subcortical region of the CNS.
- Atropine-like reactions associated with the anticholinergic properties of drugs are most characteristic of ethanolamines and ethylenediamines. Manifested by dry mouth and nasopharynx, urinary retention, constipation, tachycardia and visual impairment. These properties ensure the effectiveness of the discussed remedies in non-allergic rhinitis. At the same time, they can increase obstruction in bronchial asthma (due to an increase in sputum viscosity), exacerbate glaucoma and lead to infravesical obstruction in prostate adenoma, etc.
- Antiemetic and antiswaying effects are also likely to be associated with the central anticholinergic effect of the drugs.
 Some antihistamines (diphenhydramine, promethazine, cyclizine, meclizine) reduce the stimulation of vestibular receptors and inhibit the function of the labyrinth, and therefore can be used for motion sickness.
Some antihistamines (diphenhydramine, promethazine, cyclizine, meclizine) reduce the stimulation of vestibular receptors and inhibit the function of the labyrinth, and therefore can be used for motion sickness. - A number of H1-histamine blockers reduce the symptoms of parkinsonism, which is due to the central inhibition of the effects of acetylcholine.
- Antitussive action is most characteristic of diphenhydramine, it is realized through a direct action on the cough center in the medulla oblongata.
- The antiserotonin effect, which is primarily characteristic of cyproheptadine, determines its use in migraine.
- α1-blocking effect with peripheral vasodilation, especially inherent in phenothiazine antihistamines, can lead to a transient decrease in blood pressure in sensitive individuals.
- Local anesthetic (cocaine-like) action is characteristic of most antihistamines (due to a decrease in membrane permeability to sodium ions). Diphenhydramine and promethazine are stronger local anesthetics than novocaine.
 However, they have systemic quinidine-like effects, manifested by prolongation of the refractory phase and the development of ventricular tachycardia.
However, they have systemic quinidine-like effects, manifested by prolongation of the refractory phase and the development of ventricular tachycardia. - Tachyphylaxis: decrease in antihistamine activity with long-term use, confirming the need for alternating drugs every 2-3 weeks.
- It should be noted that first-generation antihistamines differ from second-generation antihistamines in the short duration of exposure with a relatively rapid onset of clinical effect. Many of them are available in parenteral forms. All of the above, as well as low cost, determine the widespread use of antihistamines today.
Moreover, many of the qualities that were discussed allowed the “old” antihistamines to occupy their niche in the treatment of certain pathologies (migraine, sleep disorders, extrapyramidal disorders, anxiety, motion sickness, etc.) that are not associated with allergies. Many first-generation antihistamines are included in combination preparations used for colds, as sedatives, hypnotics, and other components.
The most commonly used are chloropyramine, diphenhydramine, clemastine, cyproheptadine, promethazine, phencarol, and hydroxyzine.
Chloropyramine (Suprastin) is one of the most widely used sedative antihistamines. It has significant antihistamine activity, peripheral anticholinergic and moderate antispasmodic action. Effective in most cases for the treatment of seasonal and year-round allergic rhinoconjunctivitis, angioedema, urticaria, atopic dermatitis, eczema, itching of various etiologies; in parenteral form - for the treatment of acute allergic conditions requiring emergency care. Provides a wide range of usable therapeutic doses. It does not accumulate in the blood serum, so it does not cause an overdose with prolonged use. Suprastin is characterized by a rapid onset of effect and short duration (including side effects). At the same time, chloropyramine can be combined with non-sedating H1-blockers in order to increase the duration of the antiallergic effect. Suprastin is currently one of the best-selling antihistamines in Russia. This is objectively related to the proven high efficiency, controllability of its clinical effect, the availability of various dosage forms, including injections, and low cost.
Suprastin is currently one of the best-selling antihistamines in Russia. This is objectively related to the proven high efficiency, controllability of its clinical effect, the availability of various dosage forms, including injections, and low cost.
Diphenhydramine , best known in our country under the name diphenhydramine, is one of the first synthesized H1-blockers. It has a fairly high antihistamine activity and reduces the severity of allergic and pseudo-allergic reactions. Due to the significant anticholinergic effect, it has an antitussive, antiemetic effect and at the same time causes dry mucous membranes, urinary retention. Due to lipophilicity, diphenhydramine gives pronounced sedation and can be used as a hypnotic. It has a significant local anesthetic effect, as a result of which it is sometimes used as an alternative for intolerance to novocaine and lidocaine. Diphenhydramine is presented in various dosage forms, including for parenteral use, which determined its widespread use in emergency therapy. However, a significant range of side effects, unpredictability of consequences and effects on the central nervous system require increased attention in its application and, if possible, the use of alternative means.
However, a significant range of side effects, unpredictability of consequences and effects on the central nervous system require increased attention in its application and, if possible, the use of alternative means.
Clemastine (tavegil) is a highly effective antihistamine similar in action to diphenhydramine. It has a high anticholinergic activity, but to a lesser extent penetrates the blood-brain barrier. It also exists in an injectable form, which can be used as an additional remedy for anaphylactic shock and angioedema, for the prevention and treatment of allergic and pseudo-allergic reactions. However, hypersensitivity to clemastine and other antihistamines with a similar chemical structure is known.
Cyproheptadine (peritol), along with antihistamine, has a significant antiserotonin effect. In this regard, it is mainly used in some forms of migraine, dumping syndrome, as an appetite enhancer, in anorexia of various origins. It is the drug of choice for cold urticaria.
It is the drug of choice for cold urticaria.
Promethazine (pipolfen) - a pronounced effect on the central nervous system determined its use in Meniere's syndrome, chorea, encephalitis, sea and air sickness, as an antiemetic. In anesthesiology, promethazine is used as a component of lytic mixtures to potentiate anesthesia.
Quifenadine (phencarol) - has less antihistamine activity than diphenhydramine, but is also characterized by less penetration through the blood-brain barrier, which determines the lower severity of its sedative properties. In addition, fenkarol not only blocks histamine H1 receptors, but also reduces the content of histamine in tissues. May be used in the development of tolerance to other sedative antihistamines.
Hydroxyzine (atarax) - despite the existing antihistamine activity, it is not used as an antiallergic agent. It is used as an anxiolytic, sedative, muscle relaxant and antipruritic agent.
Thus, first-generation antihistamines that affect both H1- and other receptors (serotonin, central and peripheral cholinergic receptors, a-adrenergic receptors) have different effects, which determined their use in a variety of conditions. But the severity of side effects does not allow us to consider them as drugs of first choice in the treatment of allergic diseases. The experience gained with their use has allowed the development of unidirectional drugs - the second generation of antihistamines.
Second generation antihistamines (non-sedating). Unlike the previous generation, they almost do not have sedative and anticholinergic effects, but differ in their selective action on H1 receptors. However, for them, a cardiotoxic effect was noted to varying degrees.
The following properties are the most common for them.
- High specificity and high affinity for H1 receptors with no effect on choline and serotonin receptors.

- Rapid onset of clinical effect and duration of action. Prolongation can be achieved due to high protein binding, accumulation of the drug and its metabolites in the body, and delayed elimination.
- Minimal sedation when using drugs at therapeutic doses. It is explained by the weak passage of the blood-brain barrier due to the peculiarities of the structure of these funds. Some particularly sensitive individuals may experience moderate drowsiness, which is rarely the reason for discontinuing the drug.
- No tachyphylaxis with long-term use.
- The ability to block the potassium channels of the heart muscle, which is associated with prolongation of the QT interval and cardiac arrhythmias. The risk of this side effect increases when antihistamines are combined with antifungals (ketoconazole and itraconazole), macrolides (erythromycin and clarithromycin), antidepressants (fluoxetine, sertraline and paroxetine), grapefruit juice, and in patients with severe liver dysfunction.

- No parenteral formulations, but some (azelastine, levocabastine, bamipine) are available as topical formulations.
Below are second-generation antihistamines with their most characteristic properties.
Terfenadine is the first antihistamine drug without CNS depressant action. Its creation in 1977 was the result of a study of both the types of histamine receptors and the features of the structure and action of existing H1-blockers, and laid the foundation for the development of a new generation of antihistamines. Currently, terfenadine is used less and less, which is associated with its increased ability to cause fatal arrhythmias associated with prolongation of the QT interval (torsade de pointes).
Astemizol is one of the longest-acting drugs of the group (the half-life of its active metabolite is up to 20 days). It is characterized by irreversible binding to H1 receptors. Virtually no sedative effect, does not interact with alcohol. Since astemizole has a delayed effect on the course of the disease, it is not advisable to use it in an acute process, but it may be justified in chronic allergic diseases. Since the drug has the ability to accumulate in the body, the risk of developing serious heart rhythm disturbances, sometimes fatal, increases. Due to these dangerous side effects, the sale of astemizole in the United States and some other countries has been suspended.
Since astemizole has a delayed effect on the course of the disease, it is not advisable to use it in an acute process, but it may be justified in chronic allergic diseases. Since the drug has the ability to accumulate in the body, the risk of developing serious heart rhythm disturbances, sometimes fatal, increases. Due to these dangerous side effects, the sale of astemizole in the United States and some other countries has been suspended.
Acrivastine (semprex) is a drug with high antihistamine activity with minimal sedative and anticholinergic effects. A feature of its pharmacokinetics is a low level of metabolism and the absence of cumulation. Acrivastine is preferred in cases where there is no need for permanent antiallergic treatment due to the rapid onset of effect and short-term effect, which allows for a flexible dosing regimen.
Dimetendene (Fenistil) is the closest to the first generation antihistamines, but differs from them in a significantly less pronounced sedative and muscarinic effect, higher antiallergic activity and duration of action.
Loratadin (Claritin) is one of the most purchased second-generation drugs, which is quite understandable and logical. Its antihistamine activity is higher than that of astemizole and terfenadine, due to the greater strength of binding to peripheral H1 receptors. The drug is devoid of a sedative effect and does not potentiate the effect of alcohol. In addition, loratadine practically does not interact with other drugs and does not have a cardiotoxic effect.
The following antihistamines are topical preparations and are intended to relieve local manifestations of allergies.
Levocabastin (Histimet) is used as an eye drop for the treatment of histamine-dependent allergic conjunctivitis or as a spray for allergic rhinitis. When applied topically, it enters the systemic circulation in a small amount and does not have undesirable effects on the central nervous and cardiovascular systems.
Azelastine (Allergodil) is a highly effective treatment for allergic rhinitis and conjunctivitis. Used as a nasal spray and eye drops, azelastine has little to no systemic effects.
Used as a nasal spray and eye drops, azelastine has little to no systemic effects.
Another topical antihistamine, bamipine (soventol), in the form of a gel, is intended for use in allergic skin lesions accompanied by itching, insect bites, jellyfish burns, frostbite, sunburn, and mild thermal burns.
Third generation antihistamines (metabolites). Their fundamental difference is that they are active metabolites of antihistamines of the previous generation. Their main feature is the inability to influence the QT interval. Currently, there are two drugs - cetirizine and fexofenadine.
Cetirizine (Zyrtec) is a highly selective peripheral H1 receptor antagonist. It is an active metabolite of hydroxyzine, which has a much less pronounced sedative effect. Cetirizine is almost not metabolized in the body, and the rate of its excretion depends on the function of the kidneys. Its characteristic feature is its high ability to penetrate the skin and, accordingly, its effectiveness in skin manifestations of allergies. Cetirizine neither experimentally nor in the clinic showed any arrhythmogenic effect on the heart, which predetermined the area of practical use of metabolite drugs and determined the creation of a new drug, fexofenadine.
Cetirizine neither experimentally nor in the clinic showed any arrhythmogenic effect on the heart, which predetermined the area of practical use of metabolite drugs and determined the creation of a new drug, fexofenadine.
Fexofenadine (telfast) is the active metabolite of terfenadine. Fexofenadine does not undergo transformations in the body and its kinetics does not change with impaired liver and kidney function. It does not enter into any drug interactions, does not have a sedative effect and does not affect psychomotor activity. In this regard, the drug is approved for use by persons whose activities require increased attention. A study of the effect of fexofenadine on the QT value showed, both in the experiment and in the clinic, the complete absence of a cardiotropic effect when using high doses and with long-term use. Along with maximum safety, this remedy demonstrates the ability to stop symptoms in the treatment of seasonal allergic rhinitis and chronic idiopathic urticaria. Thus, the pharmacokinetics, safety profile and high clinical efficacy make fexofenadine the most promising of the antihistamines at present.
Thus, the pharmacokinetics, safety profile and high clinical efficacy make fexofenadine the most promising of the antihistamines at present.
So, in the doctor's arsenal there is a sufficient amount of antihistamines with different properties. It must be remembered that they provide only symptomatic relief from allergies. In addition, depending on the specific situation, you can use both different drugs and their diverse forms. It is also important for the physician to be aware of the safety of antihistamines.
| I generation | II generation | III generation |
|
|
|
Return
Insomnia, or peace we only dream of Part 3.
 Sleeping pills of various groups - melatonin, herbal and others
Sleeping pills of various groups - melatonin, herbal and others Drugs that can be bought without a prescription, used during pregnancy and which we do not yet have.
Antihistamines (H1-receptor blockers)
Everyone knows such anti-allergic drugs as diphenhydramine, suprastin or pipolfen , they block histamine-sensitive H1 receptors. These receptors are located on the surface of mast cell membranes and vascular endothelium, so their blockade leads to an anti-allergic effect - a decrease in swelling and itching. The same H1 receptors are also located in the hypothalamus, the brain “conductor” of rhythms. Stimulation with histamine activates the brain, and partial blockade with antiallergic drugs ( diphenhydramine, suprastin ) causes a side effect such as drowsiness. Unlike other anti-allergic drugs, doxylamine acts mainly only on the H1 receptors of the hypothalamus and blocks the brain activating system - histaminergic (resets the "speed"), which causes a hypnotic effect.
Doxylamine (Doxylamine) (Donormil, Reslip, Slipzon) - 15 mg, 1 tablet 20-30 minutes before bedtime. Use with caution in the elderly with prostatic hypertrophy and glaucoma. Approved for use during pregnancy but not recommended for lactation.
Another member of this group is hydroxyzine (Atarax), which has been used for over 60 years to treat hives and itching (see bit.ly/2yrbgRe),
but, unlike other first-generation antiallergic drugs, it has a greater affinity for the H1 receptors of the hypothalamus, and in addition, it binds to dopamine and serotonin receptors, which are “tied” in the pathogenesis of anxiety and depression. It helps mainly with generalized anxiety disorder (such a psychotype is always anxious, joyless, everyone is enraged ... that is, when anxiety is not associated with external factors). Hydroxyzine is not the main drug for treating anxiety, but if, for some reason, there are problems with other drugs (side effects, special prescription . ..), you can try using it as a sleeping pill (sleeping effect by reducing the overall level of anxiety).
..), you can try using it as a sleeping pill (sleeping effect by reducing the overall level of anxiety).
Hydroxyzine (Hydroxyzine) (Atarax, Hydroxyzine) - 25 mg, 20-30 minutes before bedtime.
Melatonin
A hormone produced by the pineal gland at night. By binding to receptors in the hypothalamus, it affects daily (circadian) rhythms, especially in the initial stages of sleep. Efficacy has been proven in the syndrome of delayed onset of sleep (falling asleep only at 2-4 nights), with other forms of insomnia it is problematic. A common mistake is taking 30 minutes before bedtime (as it is written in the instructions). It should be taken 1-2 hours before the expected falling asleep (bioavailability time is about 60 minutes), and dim the light 1.5-2 hours before, which contributes to the production of endogenous melatonin. The hypnotic effect is very individual and depends on many factors that are not yet completely understood. According to a 2013 Huffington Post study, melatonin supplements speed up falling asleep by 7 minutes, but only increase sleep duration by 8 minutes, so don't be fooled!
According to a 2013 Huffington Post study, melatonin supplements speed up falling asleep by 7 minutes, but only increase sleep duration by 8 minutes, so don't be fooled!
Melatonin (Melatonin) (Velson, Melaxen, Melarena, Melarithm, Sonnovan, Circadin) - 3 mg, 1 tablet, 1-2 hours before bedtime.
Melatonin receptor agonists
Mechanism of action - drugs in this group are agonists (stimulators) of melatonin receptors, which become more sensitive to the action of endogenous melatonin, which causes a hypnotic effect.
Ramelteon (Ramelteon) - 8 mg (not registered in the Russian Federation). Useful only for problems with falling asleep, but, importantly, can be used in patients with moderate sleep apnea and COPD;
Tasimelteon (Tasimelteon ) - 20 mg (not registered in the Russian Federation). May cause headaches but is not addictive.
Orexin receptor antagonists
Mechanism of action – antagonist (blocker) of receptors of one of the brain activating systems – orexin/hypocretin (i. e. reduces “speed”-activity of the brain). The double name is due to the fact that two groups of researchers discovered it and are still arguing who is “chief”.
e. reduces “speed”-activity of the brain). The double name is due to the fact that two groups of researchers discovered it and are still arguing who is “chief”.
Lemborexant (Lemborexant ) - 5-10 mg, Suvorexant (Suvorexant ) - 10-20 mg (not registered in the Russian Federation).
Antidepressants with sedative effects
European guidelines (2017) emphasize that “classic sleeping pills” (see Part 2) are not recommended for use in people over 60 years of age due to memory impairment and risk falls (for example, taking zopiclone regularly increases the risk of falls by 4.3 times!). As an alternative, it is proposed to take sedative antidepressants, which do not have muscle relaxant properties (falls) and do not form an addictive effect.
Paroxetine (Paroxertine) (Adepress, Paxil, Pleasil, Reksetin) - 10-20 mg, 30-40 minutes before bedtime;
Trazodone (Trazodone) (Trittico) - 50 mg, 30 minutes before bed;
Mirtazapine (Mirtazapine) (Calyxta) - 15-30 mg, 30-40 minutes before bedtime;
Doxepin (Doxepin) - 3-6 mg (not registered in the Russian Federation). It is prescribed to maintain sleep (early awakenings and night awakenings).
It is prescribed to maintain sleep (early awakenings and night awakenings).
Another drug that neurologists like to prescribe for the prevention of chronic headaches (in general medical practice, for some reason, they are afraid of it). It can also be successfully used as a sleeping pill, especially for anxiety and depressive disorders.
Amitriptyline (Amitriptyline) - 10 mg, 30-40 minutes before bedtime (tablets in pharmacies are usually at a dose of 25 mg, you can take ½ tablet at night).
Anticonvulsants
The drugs in this group have no registered indications for the treatment of insomnia, but due to their (side) sedative and hypnotic effects, they can be used in patients with pain syndromes.
Pregabalin (Pregabalin) (Lyrica ) - 150 mg, 30 minutes before bed;
Gabapentin (Gabapentin) (Gabagamma, Catena, Convalis) - 300 mg, one hour before bedtime.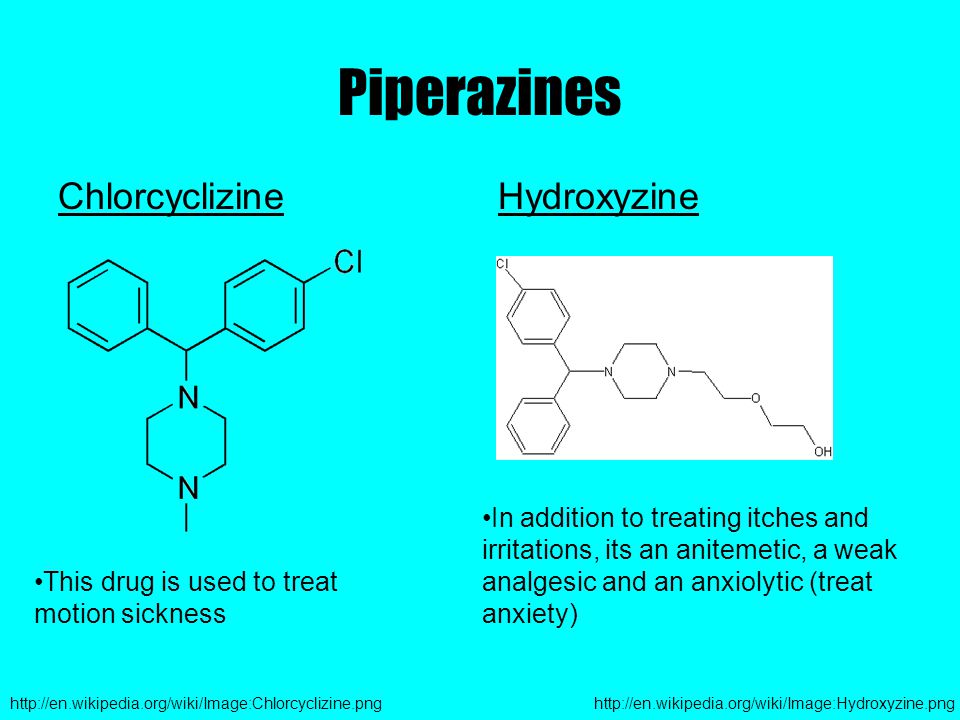
Herbal preparations
The holy faith of our people in the harmlessness and special purity of "natural" - herbal medicines (which is what marketers use) is indestructible. For some reason, no one remembers that the main toxic substances (before the use of gases) in the history of mankind were of plant origin. Do herbal remedies help with sleep disorders?
The fact is that high-quality placebo-controlled studies of the effect of valerian, motherwort, chamomile, St. John's wort, hops preparations on sleep ... have not been conducted. Of all these herbal preparations, valerian has been the most studied, but reviews of meta-analyses have not shown a positive effect on sleep, and those doses that do are on the verge of toxic liver damage. Although many patients claim that these funds help them. Whether it's a placebo effect or a sedative effect (due to a particular sensitivity to them), in combination with cognitive-behavioral therapy, herbal preparations can be effective, with fewer side effects compared to benzodiazepines.