Support group partners with depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.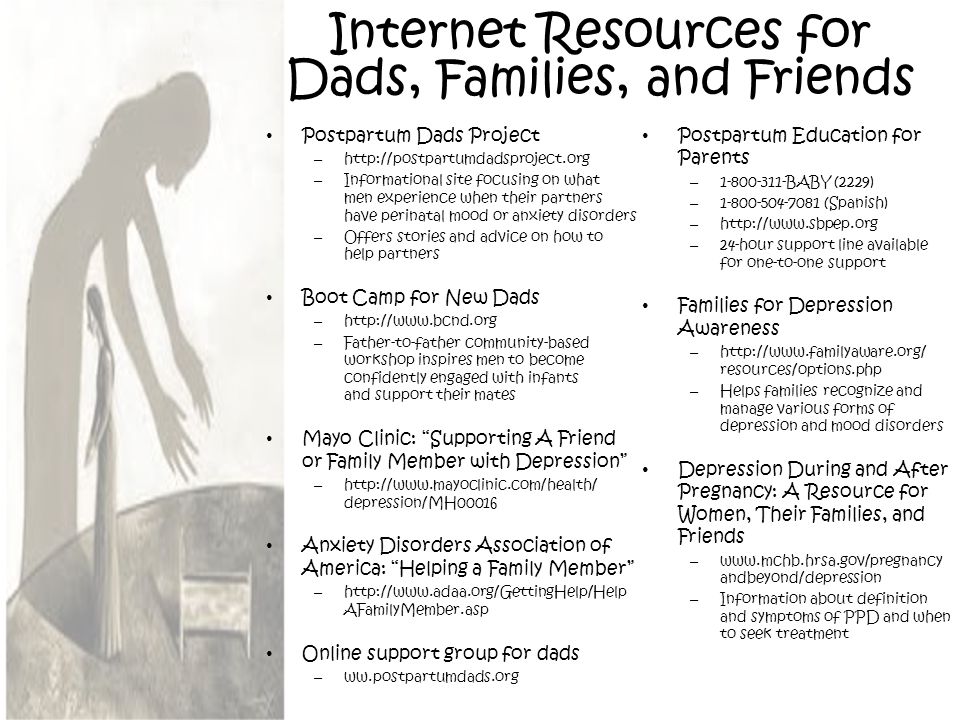
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Recovery and Recovery Support | SAMHSA
Recovery and Resilience
Resilience refers to an individual’s ability to cope with change and adversity. Resilience develops over time and gives an individual the capacity not only to cope with life’s challenges but also to be better prepared for the next stressful situation. Psychological resilience, the ability to cope with adversity and to adapt to stressful life events, varies widely from person to person and depends on environmental as well as personal factors. It refers to positive adaptation, or the ability to maintain mental and physical health despite participating in stressful situations. Resilience is playing up those protective factors so they can outweigh the risk factors. Optimism and the ability to remain hopeful are essential to resilience and the process of recovery.
Because recovery is a highly individualized process, recovery services and supports must be age appropriate and offered over the life course and flexible enough to ensure cultural relevancy. What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
Recovery and Relationships
The process of recovery is supported through relationships and social networks. This often involves family members who become the champions of their loved one’s recovery. They provide essential support to their family member’s journey of recovery and similarly experience the moments of positive healing as well as the difficult challenges. Families of people in recovery may experience adversities in their social, occupational, and financial lives, as well as in their overall quality of family life.
These experiences can lead to increased family stress, guilt, shame, anger, fear, anxiety, loss, grief, and isolation. The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
Peer support assists individuals to engage or stay connected to the recovery process through a shared understanding, respect, and mutual empowerment. Peer support extends beyond the reach of clinical treatment into the everyday environment providing non-clinical, strengths-based support. This relationship can help lay the foundation for SAMHSA’s four dimensions of recovery.
Recovery Support
SAMHSA advanced recovery support systems to promote partnering with people in recovery from mental and substance use disorders and their family members to guide the behavioral health system and promote individual, program, and system-level approaches that foster health and resilience; increase housing to support recovery; reduce barriers to employment, education, and other life goals; and secure necessary social supports in their chosen community.
Recovery support is provided in various settings. Recovery support services help people enter into and navigate systems of care, remove barriers to recovery, stay engaged in the recovery process, and live full lives in communities of their choice.
Recovery support services include culturally and linguistically appropriate services that assist individuals and families working toward recovery from mental and/or substance use problems. They incorporate a full range of social, legal, and other services (PDF | 409 KB). that facilitate recovery, wellness, and linkage to and coordination among service providers, and other supports shown to improve quality of life for people (and their families) in and seeking recovery.
Recovery support services may be provided before, during, or after clinical treatment, or may be provided to individuals who are not in treatment but seek support services.
These services, provided by professionals and peers, are delivered through a variety of community and faith-based groups, treatment providers, schools, and other specialized services. The broad range of service delivery options ensures the life experiences of all people are valued and represented.
The broad range of service delivery options ensures the life experiences of all people are valued and represented.
For example, in the United States there are 34 recovery high schools that help reduce the risk in high school environments for youth with substance use disorders. These schools typically have high retention rates and low rates of students returning to substance use.
Additionally, SAMHSA's Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS) advances effective recovery supports and services for people with mental or substance use disorders and their families.
Find more Publications and Resources on Recovery and Recovery Support.
A Guide to Funds for Depression, Bipolar Disorder, Schizophrenia
“Despite the fact that everyone is talking about depression now, in reality there is practically no place to get support,” says Marina Ris , founder of the Charity Fund for helping people with mental disorders "Just people. " For seven years, the organization has been helping people with severe disabilities, but this year it also opened its doors to anyone who experiences any mental difficulties, be it depression, anxiety disorders, affective conditions. “We can’t pay for therapy, but we can create a roadmap for everyone who comes to us.” Routes can be different depending on many factors: finances, socialization, family situation, temperament.
" For seven years, the organization has been helping people with severe disabilities, but this year it also opened its doors to anyone who experiences any mental difficulties, be it depression, anxiety disorders, affective conditions. “We can’t pay for therapy, but we can create a roadmap for everyone who comes to us.” Routes can be different depending on many factors: finances, socialization, family situation, temperament.
By calling the numbers on the foundation's website, you can tell about your problem - they will ask you and help you find out what kind of specialist you need and where to look for him.
"Just People" is not only a foundation, but also a community of patients who share information and support each other on the principle of peer support - when you can benefit from the experience of a person who had the same problems.
There is a sad pattern: faced with a mental disorder, people are often left without the most important thing for recovery - the support of loved ones. In most cases, it is difficult for relatives to understand what is happening, and even if they continue to love, this love can be quite cruel. “And the situation is generally complete abandonment or alienation - go, you are such a nobody to us - this, I would say, is 40%-50%, that is, it is also very common,” says Marina Rees. She advises, no matter how difficult it may be, to treat this state of affairs as normal, "and not as the end of the world" and seek help where it can be given.
In most cases, it is difficult for relatives to understand what is happening, and even if they continue to love, this love can be quite cruel. “And the situation is generally complete abandonment or alienation - go, you are such a nobody to us - this, I would say, is 40%-50%, that is, it is also very common,” says Marina Rees. She advises, no matter how difficult it may be, to treat this state of affairs as normal, "and not as the end of the world" and seek help where it can be given.
Because of him, she had to leave a successful legal career. At that time, this topic did not sound at all in society, everyone was afraid of a diagnosis, and even doctors said that normal life had come to an end. “I began to look for ways for myself, began to deal with psychotherapy, went through all possible schools until I found what I needed.”
For those who have faced a similar problem, Marina reminds them that it is difficult to find a suitable specialist, even an excellent psychotherapist who has helped a large number of people may not be suitable for you. You need to figure out what directions and methods are, choose something based on your characteristics and not despair because of unsuccessful attempts.
You need to figure out what directions and methods are, choose something based on your characteristics and not despair because of unsuccessful attempts.
After a woman with two children jumped out of a window in Moscow a year ago, more people started talking about postpartum depression. But this tragedy also created great fear - mothers with problems began to be stigmatized. This is a very harmful myth that makes it almost impossible to voice your problem in society. A woman is afraid that, at best, she will be called a bad mother, and at worst, her children will be taken away. In fact, about 13% of all women who give birth face postpartum depression, and they do not pose any threat, they just suffer a lot.
In this case, and without any psychiatric problems, mothers of babies are a special social group that is constantly condemned and severely deprived of rights in our society. Surviving depression in this extremely vulnerable position is especially difficult. And a separate task is to allocate time for treatment, because with a baby in her arms it is impossible without outside help.
And a separate task is to allocate time for treatment, because with a baby in her arms it is impossible without outside help.
“The most difficult thing is to find a resource to help yourself,” says Daria Utkina , one of the founders of the Care for Yourself project. - There is a myth that is being fanned in the media, we even saw booklets about this in the antenatal clinic: “Only close relatives of a woman can understand that she is depressed.” It is not true! The most frequent request to us is this: “How can I convey to my loved ones that this is not a whim and not selfishness, and I really need help?”
Interestingly, Darya herself experienced the exact opposite experience: “I am a depressed person, with extensive experience in personal therapy, but just after giving birth, everything was the opposite - I felt better than ever, and at the same time I saw women who had there is no depression in ordinary life, but after childbirth occurs. This makes it possible, on the one hand, to understand what can happen to a person, and on the other hand, to help her not fall into history - the birth of a child will destroy my life and everything will be bad! That is, as a helping practitioner, I see both the traumatic side of experience and the resource side.
The project began when Daria, while working as a doula, heard from a fellow lactation consultant that women with postpartum depression did not have a space on the Russian-language Internet where they could share their problem with someone. Then Daria created the “Take care of yourself” community on the social network. “It turned out that this decision, made in 10 seconds, is needed by many - people began to add, make reposts.” Community members follow certain communication rules that exclude judgment and unsolicited advice. The space where you can come and honestly write about your everyday life with a child turned out to be necessary for all mothers in general, and not only for those who are faced with a clinical diagnosis.
For those who want more specific thematic communication in a private setting, there is another direction of the project - paid support groups. These classes are conducted by the so-called peer consultants - women who also went through some difficult experience of motherhood, but, as a rule, they all also have some kind of specialized education and occupation - these are doulas, psychologists, doctors.
However, if you have been diagnosed with postpartum depression, you will of course need a psychiatrist or psychotherapist. To get an idea of where to start, you can listen to a podcast episode dedicated to the selection of a specialist.
According to Daria, success on the first try is incredible luck: in the case of a psychotherapist, it is usually possible to find a suitable specialist from the 5th or 6th time, but with psychiatrists it is even more difficult. Breastfeeding mothers often face either advice to drink motherwort or pressure to stop breastfeeding in order to take antidepressants. Although in fact there are a large number of drugs that are compatible with feeding, the most important thing is to choose the right one.
The Self Care Project has compiled a map of friendly psychiatrists and can help you with recommendations upon request. In addition, the site has a list of free contacts for seeking emergency psychological help.
A heroine suffering from bipolar disorder. Stills from Modern Love
Stills from Modern Love Anne Hathaway's character in an episode of Modern Love bursts with energy and radiates charm, and then suddenly can't get out of bed due to overwhelming fatigue - the life of a person with bipolar disorder looks like a continuous drama. “I have heard the opinion that this is an exaggeration, a romanticization,” says Alyona Shibarshina, the host of the Moscow support groups “Sunday BAR” . - But it seems to me that in this film a lot of things are similar to the truth. I like the musical at the beginning, as an allegory of hypomania - she is so good that everyone is dancing around, it seems that the whole world is open to you and all of you are friends.
The life of people suffering from bipolar disorder consists of alternating depressions and euphoric highs. However, mood swings are familiar to many, and it is often difficult to explain to others that the intensity of these surges can turn life into a nightmare. What to do if you suspect you have bipolar disorder?
“If an undiagnosed person wants to attend a meeting, I say you can come to the group and 'synchronize watches', see how your experience is similar to the participants' experience,” Alena says. “But you can’t make a diagnosis based on that alone. You need to see a psychiatrist to be sure. In my practice, people who came in with doubts, as a rule, were confirmed either with a diagnosis of bipolar disorder or other similar ones.
“But you can’t make a diagnosis based on that alone. You need to see a psychiatrist to be sure. In my practice, people who came in with doubts, as a rule, were confirmed either with a diagnosis of bipolar disorder or other similar ones.
Naturally, the main thing is to find a good specialist, but the problem is that this is quite difficult to do. Alena herself was unsuccessfully treated for chronic depression for seven years in the absence of a correct diagnosis. And since the treatment of bipolar disorder is completely different, for each period there are different drugs, Alena managed to go into remission only when she was diagnosed with bipolar disorder.
Such difficulties in diagnosis occur regularly and are due to the fact that people see the problem in depression, but in good condition they do not see anything special and do not talk about it. “But the problem is not only in depression,” Alena says, “the problem is also in the rises, which can turn into real mania and psychosis. People quit their jobs, take out loans, open businesses, move to other cities, go shopping or make new dangerous connections - in general, all sorts of things that affect life.
People quit their jobs, take out loans, open businesses, move to other cities, go shopping or make new dangerous connections - in general, all sorts of things that affect life.
Alena used to work in a managerial position with a lot of stress and irregular hours; because the treatment did not help for a long time, I had to quit:
“When I got better, I realized that I would like to do something useful, and I decided to run a support group. Here people share their stories, tell how they found a doctor, how they first told their loved ones. First of all, those who have just been diagnosed need help, of course. Often they don’t know what to do with it at all, because sometimes our doctors don’t tell us anything - they just say: “Here is the prescription, go.”
Bipolar Association also helps people with bipolar disorder. Its members will be able to share with you expert contacts and advice on where to go where you live.
Also, from anywhere in the country, you can join the Sunday BAR online meetings. Alyona compiled a list of support groups known to her in different regions. You can also open your own group, the NGO "Partnership of Equals" will help you with this for free.
Alyona compiled a list of support groups known to her in different regions. You can also open your own group, the NGO "Partnership of Equals" will help you with this for free.
If you find yourself with bipolar disorder, in addition to the first steps - the search for specialists and a circle of support - it is very important to constantly raise your awareness, knowledge relieves many fears. All information about bipolar disorder is collected on the site, here you will find translated scientific articles and tests, stories about feature films dedicated to the topic of bipolar disorder, and much more.
“The House of Herbs” is a project of the RBOOI “Emerald City”. Photo izumrud.moscow“Now you need to be treated, and we'll talk about the rest with you in 10 years”
In contrast to the diagnosis of "bipolar disorder", the diagnosis of "schizophrenia" not only does not have a romantic connotation, but remains in everyday life as frightening and repulsive as possible. Therefore, experts abandoned this term, replacing it with "schizophrenia spectrum disorders." The key word here is spectrum, since these are diseases with a very different picture, from severe ones that require outpatient monitoring to very mild ones that practically do not interfere with a normal life.
Therefore, experts abandoned this term, replacing it with "schizophrenia spectrum disorders." The key word here is spectrum, since these are diseases with a very different picture, from severe ones that require outpatient monitoring to very mild ones that practically do not interfere with a normal life.
And just like other mental disorders, this mental breakdown can appear suddenly, invading the most successful and active life under the influence of stress, too much pressure at work and other factors.
Those who become ill at an early age often have great problems with socialization and employment even with successful treatment - all because of the stigmatization that haunts schizophrenia spectrum disorders. “We discharged the girls from our wonderful 15th department of PKB No. 15 - behind so many conversations, tears and consolations, crises and a common victory, everyone is already relatives - and they leave, as if into a void,” recalls Nadezhda Stepunina , psychiatrist, psychotherapist and ideological inspirer of the Emerald City. Who will meet them? A doctor in a neuropsychiatric dispensary who doesn't have time to talk? A school where, God forbid, I could say that I was THERE... Fear for them pushed me to go to the outpatient service in order to be on the other side, to help without taking my life away. He made me look for effective ways to help different guys, including those who don’t leave the house at all.”
Who will meet them? A doctor in a neuropsychiatric dispensary who doesn't have time to talk? A school where, God forbid, I could say that I was THERE... Fear for them pushed me to go to the outpatient service in order to be on the other side, to help without taking my life away. He made me look for effective ways to help different guys, including those who don’t leave the house at all.”
Today the center helps adolescents and adults with mental disabilities to adapt. Everyone who turns to the "Emerald City" for help is offered an individual scheme. We can talk about visiting a psychotherapist or group classes, art therapy and leisure activities, as well as assistance in finding a job - it all depends on the state of the person and his request.
One of the possible ways to adapt is to become a “social trainer” and help those who are currently worse off to share experiences and make up for the lack of communication. “Coaches grow out of our patients,” explains Nadezhda Stepunina. “These guys know first hand what it’s like to be lonely and misunderstood, helpless, dependent, weak, and how to get out of it.”
“These guys know first hand what it’s like to be lonely and misunderstood, helpless, dependent, weak, and how to get out of it.”
Postpartum depression
Postpartum depression is a mental disorder that develops in some women in the first weeks or months after childbirth and is manifested by a feeling of extreme sadness and psychological instability. No new mother is immune to the development of postpartum depression, but women with previous episodes of depression have more severe and more frequent postpartum depression.
- Causes of postpartum depression
- Symptoms of postpartum depression
- Diagnosis of postpartum depression
- Treatment of postpartum depression
- Prevention of postpartum depression
At the same time, postpartum depression should be distinguished from a short-term feeling of sadness and sadness that occurs in the first days after childbirth, associated with abrupt changes caused by the birth of a child, and disappears on its own no later than 2 weeks, which is considered absolutely normal. Postpartum depression is a serious and long-term mental disorder of a woman that lasts for several weeks or months and seriously affects all aspects of life.
Postpartum depression is a serious and long-term mental disorder of a woman that lasts for several weeks or months and seriously affects all aspects of life.
Causes of postpartum depression
The exact cause of postpartum depression is not known, but a number of factors have been identified that increase the risk of depression. These include:
- depression before or during pregnancy;
- postpartum depression during a previous pregnancy;
- periods of sadness, sadness or depression associated with the menstrual cycle or that occurred while taking oral contraceptives;
- psychological problems;
- the presence of depression in close relatives;
- chronic stress;
- family problems, destructive relationships, unemployed partner, financial difficulties or absence of a partner;
- age of woman under 18 or over 40 years old
- overwork or lack of sleep;
- insufficient support from partner or family members;
- abnormal pregnancy, premature birth or birth of a child with congenital defects;
- unplanned, unwanted pregnancy.

Symptoms of postpartum depression
Typical symptoms of postpartum depression include:
- excessive despondency, anxious thoughts;
- tearfulness, mood swings;
- irritability;
- intellectual and motor retardation;
- fussiness and restlessness.
Less common symptoms of postpartum depression include:
- excessive fatigue;
- sleep disorders: insomnia or drowsiness;
- indifference to surrounding people and events;
- loss of interest in various activities, including sex;
- anxiety or panic attacks;
- loss of appetite or overeating;
- decreased interest in the child or increased anxiety;
- feeling of inadequacy or hopelessness, meaninglessness of life;
- possible suicidal thoughts.
Often a woman in a state of postpartum depression does not feel connected with her child, and is very burdened by this.
In addition to mental disorders, postpartum depression causes physical symptoms, including palpitations, chest pain, blood pressure instability, headaches, constipation, and abdominal discomfort.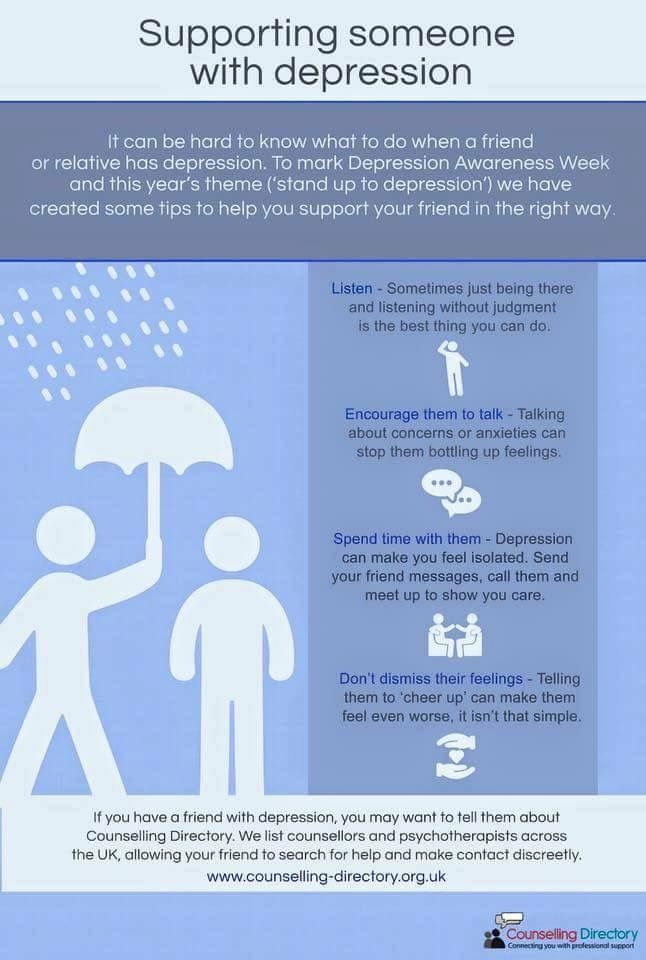
The duration of postpartum depression can range from a few weeks to several months or (in severe cases and if untreated) years.
Diagnosis of postpartum depression
The main way to diagnose this type of depression is a conversation with a specialist and a physical examination. Most often, a doctor or psychologist asks the patient to fill out a special questionnaire that allows you to determine the severity of depression and make an accurate diagnosis. In some cases, consultation with an endocrinologist, gynecologist, laboratory tests (blood chemistry, hormone levels) and other examinations may be required.
Treatment of postpartum depression
Currently, there are several approaches to the treatment of postpartum depression, with psychotherapy and antidepressants being the main methods. In severe cases, a woman with this diagnosis may require hospitalization, but as a rule, outpatient treatment is sufficient. When choosing medications for the treatment of depression, it is imperative to consider whether a woman is breastfeeding a child, since some antidepressants penetrate into breast milk and are contraindicated during breastfeeding. However, there are a number of effective medicines that can be taken to treat postpartum depression without stopping breastfeeding.
However, there are a number of effective medicines that can be taken to treat postpartum depression without stopping breastfeeding.
Prevention of postpartum depression
Like many other mental and physical illnesses, postpartum depression is easier to prevent than to cure. Therefore, all women who have recently given birth require increased attention from family members and medical personnel. To reduce the risk of developing postpartum depression will help to follow simple rules regarding the organization of the regime of work and rest, lifestyle, nutrition, communication with others and caring for the newborn. In order to prevent postpartum depression, a woman is recommended:
- redistribute family responsibilities between relatives and in the first weeks after childbirth deal only with matters related to the child;
- rest with the child;
- do not hesitate to seek help from family members, friends, relatives;
- do not keep doubts, fears and anxieties in yourself - discuss your feelings with loved ones;
- take time every day to take care of yourself - take a shower, do gymnastics, look after your appearance, wear beautiful clothes;
- arrange for yourself a proper, regular and balanced diet;
- go out of the house if possible, for example, to meet friends or go for a walk, do not lead a secluded life;
- spend time with husband or partner;
- communicate with other mothers, share experiences and feelings;
- If possible, join a support group for women with depression.