Alternatives to seroquel
Differences, similarities, and which is better for you
Abilify and Seroquel are antipsychotic medications that treat major depressive disorder, bipolar disorder, and schizophrenia. Compare these drugs to find out which one might be better for you.
Drug overview & main differences | Conditions treated | Efficacy | Insurance coverage and cost comparison | Side effects | Drug interactions | Warnings | FAQ
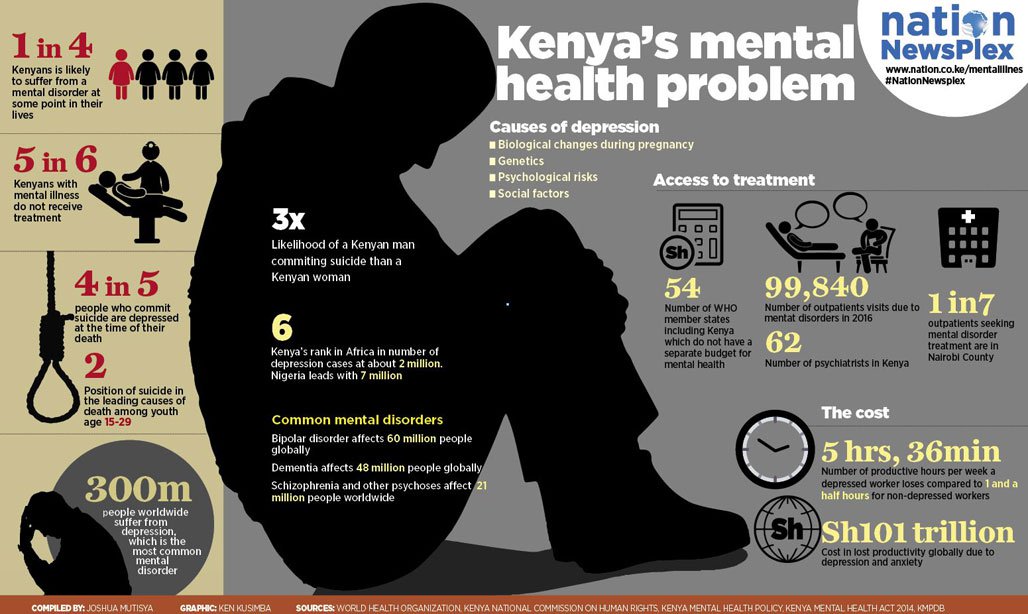
Abilify and Seroquel are two prescription drugs classified as atypical antipsychotics. Atypical antipsychotics are used in the treatment of mental health disorders such as major depression, bipolar disorder, and schizophrenia, among others. These disorders affect many people and greatly impact overall health and quality of life. Almost 20 million Americans, or 8% of the U.S. population, have had at least one major depressive episode. Bipolar disorder will affect over 4% of the population at some point in their lifetime. Schizophrenia is one of the leading causes of disability worldwide.
The approach to treating these disorders is unique to each patient. It often takes more than one treatment type to achieve relief or remission of symptoms. Other treatment types may include selective serotonin reuptake inhibitors (SSRIs), typical antipsychotics (first-generation antipsychotics), and group or individual therapy.
What are the main differences between Abilify vs. Seroquel
Abilify (aripiprazole) is a prescription medication belonging to a class of drugs known as atypical antipsychotics. Abilify is used in the treatment of mental health disorders such as depression, bipolar disorder, and schizophrenia, among others. Abilify has both partial agonist and antagonist activity at serotonin and dopamine receptors. Serotonin and dopamine are neurotransmitters known to play a role in many roles such as mood, disposition, agitation, sleep, movement, and digestion. Through its role at these receptors, Abilify is able to decrease the severity of symptoms related to depression and other mental health disorders.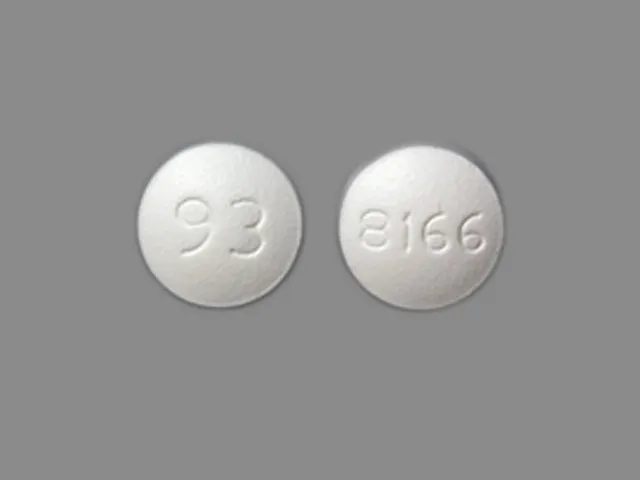 Abilify is available in multiple doses as an oral tablet and solution, an oral disintegrating tablet, an injection, and the newest formulation, Abilify MyCite. Abilify MyCite is an oral tablet with a built-in sensor to help monitor if and when you take your medication, your mood, and other factors through an app.
Abilify is available in multiple doses as an oral tablet and solution, an oral disintegrating tablet, an injection, and the newest formulation, Abilify MyCite. Abilify MyCite is an oral tablet with a built-in sensor to help monitor if and when you take your medication, your mood, and other factors through an app.
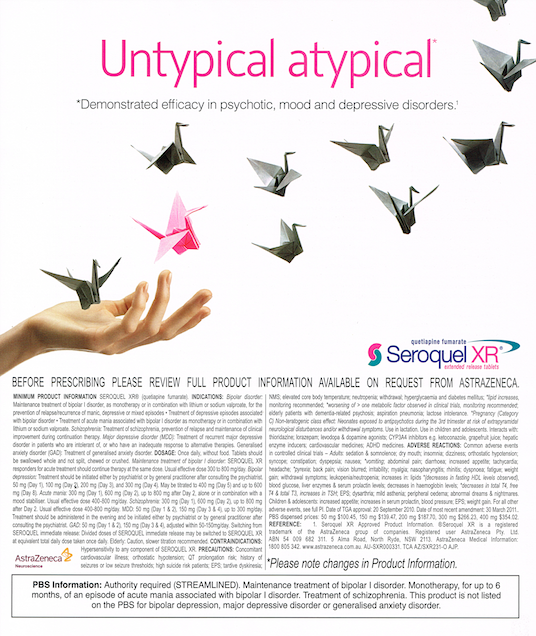
Seroquel (quetiapine) is also a prescription medication belonging to the class of drugs known as atypical antipsychotics. Seroquel only has antagonist effects on the serotonin and dopamine pathways. It is also used for major depression, bipolar disorder, and schizophrenia, like Abilify. Seroquel is available in a variety of dosages in both immediate-release and extended-release oral tablets.
Conditions treated by Abilify and Seroquel
Abilify and Seroquel are antipsychotic medications that share three common indications approved by the Food and Drug Administration (FDA): major depressive disorder, bipolar disorder, and schizophrenia Abilify also carried a unique indication for use in its ability to treat irritability associated with autistic disorder.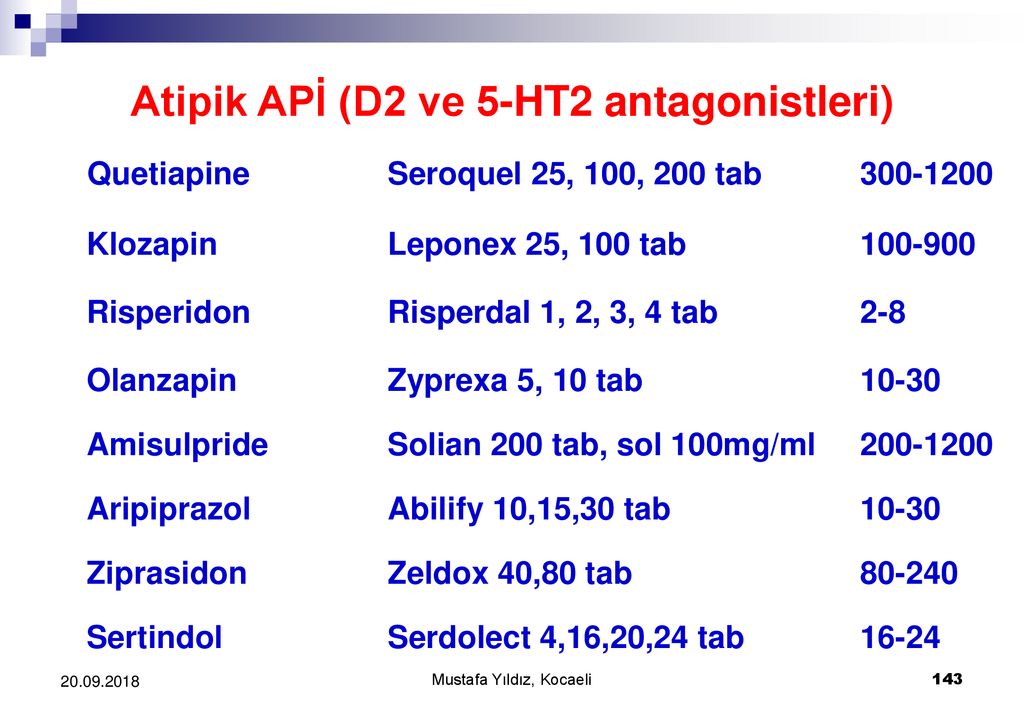 While Seroquel is approved as a singular treatment for depression, Abilify’s approval is only as an adjunct treatment in patients where other traditional antidepressants aren’t adequate.
While Seroquel is approved as a singular treatment for depression, Abilify’s approval is only as an adjunct treatment in patients where other traditional antidepressants aren’t adequate.
Both drugs are also used off-label, or without FDA approval, for other mental health disorders. Both have been used in treating psychosis associated with dementia. Remember, only your doctor can decide if one of these drugs is appropriate for you and your diagnosis.
Is Abilify or Seroquel more effective?
In a meta-analysis comparing 15 antipsychotic medications from multiple classes in the treatment of schizophrenia, each drug was compared to placebo for efficacy. While both drugs were significantly better than placebo and considered effective in the treatment of schizophrenia, Seroquel was found to show more improvement in symptoms as compared to placebo. Seroquel was also shown to cause more weight gain as compared to the other drugs. A randomized, double-blind clinical trial compared Seroquel and Abilify head to head and found them both to be effective in treating schizophrenia, with one not being significantly better than the other.
When comparing Abilify, Seroquel, and 2 other antipsychotics (risperidone and olanzapine) as adjunct treatments for depression, results from one analysis showed that adjunct treatment with either of these drugs lead to better treatment response and increased remission rates as well as less frequent psychiatric hospital stays.
This is not intended to be medical advice. Ultimately, only your psychiatric health care provider can determine which treatment approach is right for your disorder.
Coverage and cost comparison of Abilify vs. Seroquel
Abilify is a prescription drug that is covered by most commercial and Medicare insurance drug plans. The out-of-pocket price for Abilify can be as much as $1070 for a one-month supply. Luckily, SingleCare offers a savings coupon for Abilify and its generic, aripiprazole. You can get a 30 day supply of the generic for less than $10.
Seroquel is also a prescription drug that is covered by almost all commercial and Medicare insurance plans. The cost without insurance for a one-month of supply for Seroquel is over $250. With a SingleCare coupon, generic Seroquel is less than $5 at participating pharmacies.
The cost without insurance for a one-month of supply for Seroquel is over $250. With a SingleCare coupon, generic Seroquel is less than $5 at participating pharmacies.
Common side effects of Abilify vs. Seroquel
Abilify and Seroquel share many common potential adverse events, though the rate at which they typically occur can be very different for each drug. Adverse events with antipsychotic drugs can for some be so bothersome that they elect to discontinue therapy. It is important to have open conversations about your mental illness symptoms and the effects of your medications with your healthcare professional so that the best course of action can be determined.
Fatigue and sedation are two of the most common adverse effects of second-generation antipsychotics like Abilify and Seroquel. This is due to their affinity for histamine receptors. While sedation is a pronounced side effect for these drugs, second-generation antipsychotics are considered to be less sedating on average than first-generation, or typical, anti-psychotics. When prescribing antipsychotic medications, it is important to place value on the tolerability of the drug in order to achieve compliance.
When prescribing antipsychotic medications, it is important to place value on the tolerability of the drug in order to achieve compliance.
Source: DailyMed (Abilify) Dailymed (Seroquel)
Drug interactions of Abilify vs. Seroquel
Abilify and Seroquel are substrates of the enzyme CYP3A4, meaning their metabolism is dependent upon this enzyme. Other drugs which either induce or inhibit this enzyme will affect the metabolism and effects of both drugs.
The common antifungals itraconazole and ketoconazole are inhibitors of CYP3A4, and therefore the metabolism of Abilify and Seroquel is slowed down and blood levels are increased. Long term use of drugs that inhibit CYP3A4 may require a dose decrease adjustment to avoid toxicity. On the contrary, drugs which induce CYP3A4, such as carbamazepine, speed up the metabolism of Abilify and Seroquel, potentially causing subtherapeutic levels of the drug in your system.
Abilify is also partially metabolized by a second enzyme, CYP2D6. Quinidine, a drug given to treat or prevent malaria, has such an effect on Abilify levels that the Abilify dose needs to be reduced to half when a patient is also taking quinidine.
Quinidine, a drug given to treat or prevent malaria, has such an effect on Abilify levels that the Abilify dose needs to be reduced to half when a patient is also taking quinidine.
The following table is not intended to be an all-inclusive list of potential drug interactions. Please check with your pharmacist for a complete list.
Warnings of Abilify and Seroquel
Do not take Abilify or Seroquel if you have ever had any type of sensitivity or allergic reaction to either drug.
Both adults and children may experience an increase in depression and suicidal thoughts while on antidepressants and antipsychotic drugs. Children and young adults seem to experience a more significant increase in depression and suicidal thoughts. This risk exists until medications have these disorders in remission. These groups should be monitored closely while on these types of medications.
Caution should be used in elderly patients, especially those with dementia-related psychosis or Alzheimer’s disease. An increased risk of cerebrovascular events such as stroke are a concern in these patients.
An increased risk of cerebrovascular events such as stroke are a concern in these patients.
Neuroleptic Malignant Syndrome (NMS) is a risk of antipsychotic treatment. Symptoms include rigid muscles, altered mental status, and irregular pulse or blood pressure. While rare, it can be fatal, and patients should be monitored for signs and symptoms.
While alcohol does not have directly interact with Abilify or Seroquel, it is recommended that patients taking Abilify or Seroquel limit or avoid alcohol intake due to its ability to cause an altered mental state and physical impairment.
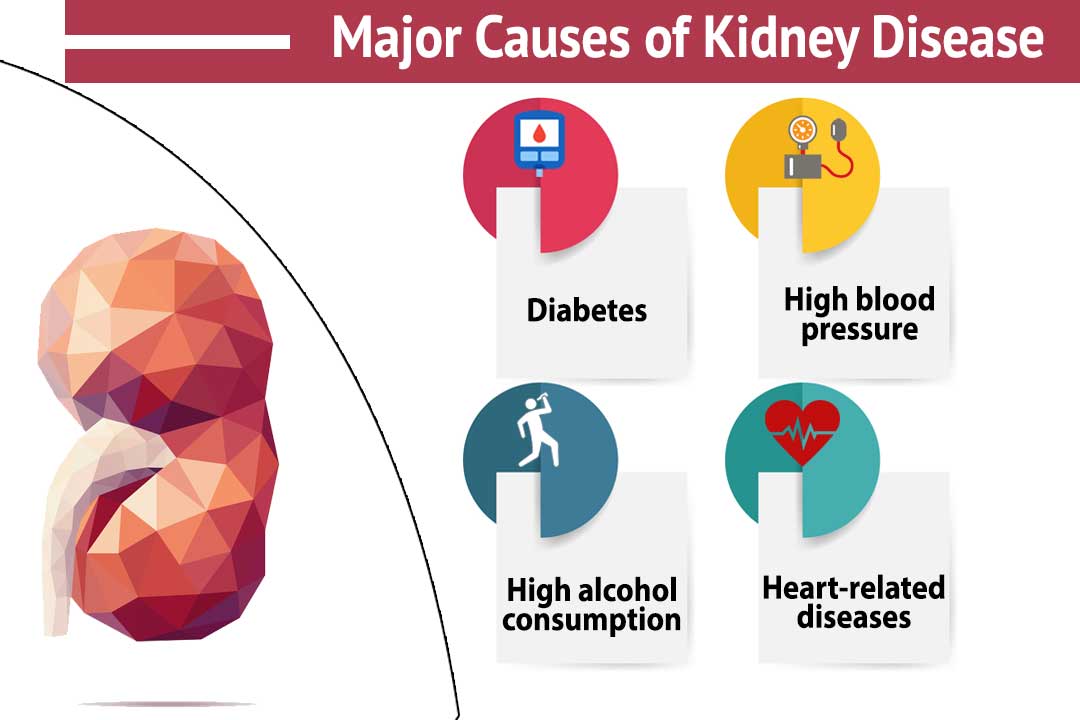
Atypical antipsychotics have been linked to metabolic changes in patients such as diabetes mellitus, obesity, and dyslipidemia (high cholesterol). In some cases, these conditions are corrected by stopping the drug, but they could be long-lasting. A systematic review looked at the metabolic changes caused by second-generation antipsychotics. While Abilify and Seroquel did both cause changes in cholesterol, specifically triglycerides, these changes were not as pronounced as with other drugs such as olanzapine. Parameters and positive symptoms related to these disorders should be monitored closely.
Parameters and positive symptoms related to these disorders should be monitored closely.
Frequently asked questions about Abilify vs. Seroquel
What is Abilify?
Abilify is an atypical antipsychotic prescription medication. It has effects on both serotonin and dopamine neurotransmitter pathways. It is available in multiple strengths as an oral tablet and solution, an orally disintegrating tablet (ODT), and a new tablet with an internal sensor.
What is Seroquel?
Seroquel is also an atypical antipsychotic prescription medication. It has effects on both serotonin and dopamine neurotransmitter pathways. It is available as oral immediate-release and extended-release tablets in various strengths.
Are Abilify and Seroquel the same?
Abilify and Seroquel are both atypical antipsychotics, but they are not the same. While they both block dopamine and serotonin action, Abilify is also a selective stimulator at these receptors. They have similar indications for use, but may also be used for unique indications as well.
Is Abilify or Seroquel better?
Abilify and Seroquel have both been proven to be very effective drugs. The results of one study indicated that Seroquel may have shown better improvement in symptoms, but also caused more metabolic changes and weight gain. Your physician will help you weigh which option is best for you.
Can I use Abilify or Seroquel while pregnant?
There are not enough studies to establish the safety of either drug in pregnant patients. However, fetal toxicity has been observed in animal studies, and therefore these drugs should only be used when the benefit absolutely outweighs the risk. Breast-feeding should not occur while patients are on these drugs.
Can I use Abilify or Seroquel with alcohol?
While alcohol does not directly interact with either drug, it is recommended that patients limit or avoid alcohol intake due to its ability to cause an altered mental state.
What is a good replacement for Seroquel?
Other atypical antipsychotics may be tried when Seroquel is not effective or has intolerable side effects. Those may include Risperdal, Rexulti, Zyprexa, or Latuda.
Those may include Risperdal, Rexulti, Zyprexa, or Latuda.
Does Abilify help with anxiety?
Abilify is not indicated in the treatment of anxiety. While many patients living with schizophrenia or bipolar disorder may experience anxiety, they may require additional treatment to control their anxiety.
Does Abilify help you sleep?
While not approved to treat insomnia, Abilify does cause a significant amount of drowsiness and somnolence. Patients may find that it helps with their sleep patterns when taken at night.
Seroquel Alternatives | Natural Alternatives to Seroquel
Alternative to Meds News & Blog Articles
Talk Therapy as an Alternative to Seroquel
There is a residential approach to the treatment of psychiatric symptoms such as schizophrenia called Open Dialogue. This mode of treatment was originally introduced in Finland and has become popular in other parts of the world as well. Benefits have been reported as less need for medication, fewer symptoms of psychosis, less frequent hospitalizations, and increased numbers of persons being able to re-enter the workforce. 11
11
Studies have found that CBT (talk therapy in private or group settings) can be as or even more effective in resolving psychiatric symptoms when medication may not help. There are many forms of talk therapy, including EMDR (eye-movement desensitization & reprocessing therapy) and exposure therapy that may be useful in treating PTSD symptoms.12-15
Correcting the Diet as a Seroquel Alternative
Alternative to Meds Center uses organic, clean food to design a diet that is not only crafted to be delicious but conducive to the reduction of sensitivities, balancing blood sugar, restoring needed nutrients that support a healthy microbiome, and stabilizing neurochemistry.
A diet that omits sugars, refined carbs, caffeine, gluten, MSG, and other chemicals has been proven effective as an alternative to medication for the mitigation of psychiatric symptoms.16,8,20,30
Diet has been often overlooked in the past but much research has shown it can be a highly effective strategy for mental and physical health.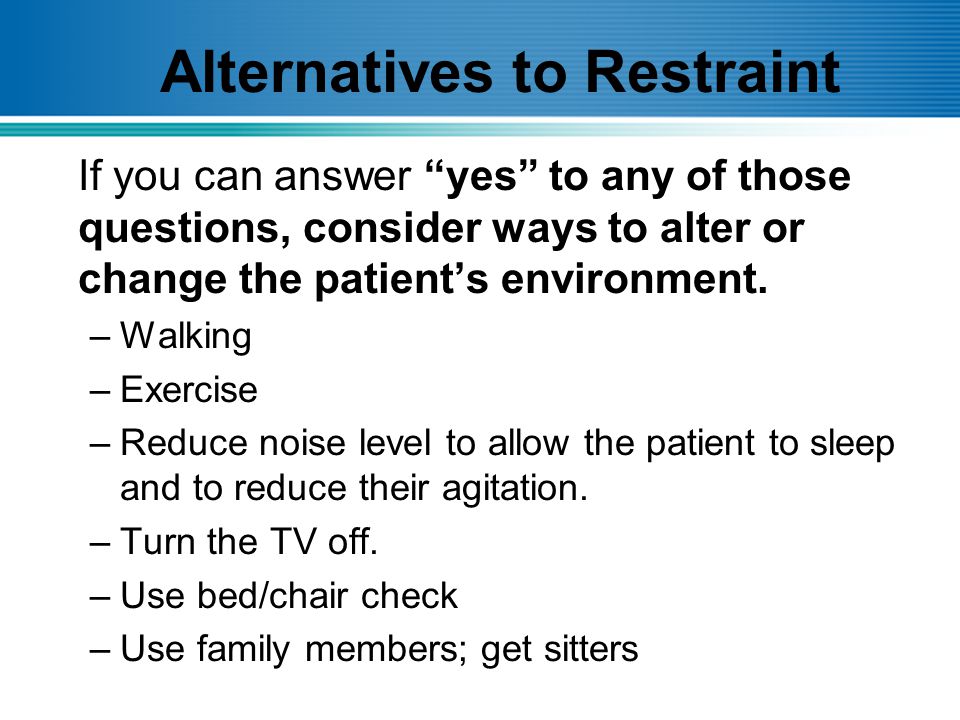
A corrected diet can result in many positive improvements such as a better energy level, a greater feeling of well-being, and a reduction of symptoms of bipolar, schizophrenia, psychosis, and other conditions. The other benefit is these changes can occur without having to endure the troubling side effects that can accompany antipsychotic medications.
Modifying the diet in treating psychiatric conditions such as schizophrenia is an ideal highly efficacious pillar in our Seroquel alternatives treatment plan at Alternative to Meds Center.16
Testing for Food Allergies, Nutrient Deficiencies
A person may have food allergies that were overlooked as well as deficiencies in certain nutrients. Testing for these and correcting what needs to be changed can offer an effective, drug-free alternative to Seroquel or other drugs. The best news is that these issues can be tested and resolved without pharmaceutical drugs.
Microbiome Support
A link has been discovered between the gut and the CNS that is of significance when a person wants to stabilize the neurochemistry.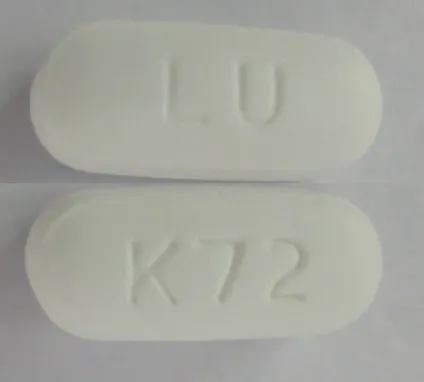 This link is termed the “gut-brain axis.”
This link is termed the “gut-brain axis.”
While more research will continue to enlighten how this link can affect our health, what is known is that inflammation in the intestinal tract can interfere with synaptic brain activity. A link between gut health and brain health is strongly suggested in research studies on the subject.
Probiotics can be used as an alternative to Seroquel. Probiotics can restore the healthy microorganisms in the gut, and according to Clapp et al’s 2017 study, probiotics may assist treatment and possibly prevention of psychiatric symptoms.25
Other research by Bonaz et al shows a relationship between the vagus nerve and the CNS and how a restored microbiome can be highly beneficial to balancing these functions.60
Blood Sugar Control as an Alternative to Seroquel
For efficient function, the brain needs an adequate blood sugar supply. An overabundance or lack of this nutrient can cause symptoms that can be (and often are) mistaken for psychiatric disorders. Blood sugar can be rebalanced without the need for heavy medication, and doing so will help maintain proper CNS function and support mental health naturally.28,29
Blood sugar can be rebalanced without the need for heavy medication, and doing so will help maintain proper CNS function and support mental health naturally.28,29
Supplements Used as Seroquel Alternatives
Tryptophan
Tryptophan has various functions in a healthy body. One is that it is a precursor for serotonin. A condition known as ATD (acute tryptophan depletion) has been linked to psychiatric symptoms such as aggression, low mood, and suicidal behavior or thinking, and some symptoms found in schizophrenic persons. This condition can be mitigated with supplementation, and with diet. Foods high in tryptophan include meats, dairy, fruits, and seeds. Consuming these foods in an adequate supply can act as a powerful alternative to Seroquel or other antipsychotic medications.31-33
Lithium Orotate
Toxic side effects are linked to Lithium Carbonate. However, lithium orotate is a trace mineral available in an over-the-counter supplement that can mitigate manic and depressive bipolar conditions. Lithium orotate is the trace mineral form of lithium and is another alternative to Seroquel that can be considered.37-44
Lithium orotate is the trace mineral form of lithium and is another alternative to Seroquel that can be considered.37-44
Vitamins as a Natural Alternative to Seroquel
Vitamins are essential for both physical and mental health. Each vitamin has numerous effects on the beautifully complex physical body. For example, vitamin E protects cell walls. Niacin is important for energy metabolism and the digestive tract (gut).10 Deficiencies can wreak havoc.
Important work by Dr. Abram Hoffer in the 1950s demonstrated the effects of high Vitamin C and niacin (vitamin B3) in his various studies done on groups of schizophrenia patients. The patients achieved a high remission rate and significant reduction or elimination of their psychiatric symptoms without the need for medication. Alternative to Meds Center uses effective orthomolecular treatments, such as these, to give our clients the opportunity to achieve success with natural alternatives to Seroquel. 45,46
45,46
Omega-3 Fatty Acids and Eicosapentaenoic acid (EPA)
Omega-3 fatty acids were shown to be effective as an alternative to Seroquel and other medications in some studies. EPA (eicosapentaenoic acid) is found in omega-3 fish oils and is thought to have beneficial effects in mitigating psychiatric symptoms such as those found in patients with schizophrenia, a safe alternative to Seroquel.34-36
Cleansing Toxic Accumulations
Neurotoxins such as chemicals used in cleaning, construction, home furnishings, foods, dentistry, and a host of other sources can be endocrine disruptors that contribute to psychiatric symptoms. Getting rid of them can support healthy neurochemistry making this an effective Seroquel alternative.47-52
Exercise, Fresh Air, Sunshine as Alternatives to Seroquel
Exercise, especially done out of doors in the fresh air and sunshine is probably the most underused alternative to Seroquel that there could be. Many studies have shown the positive benefits to mental well-being of getting oxygen into your lungs, sunshine on your skin, and getting your circulation going.
Many studies have shown the positive benefits to mental well-being of getting oxygen into your lungs, sunshine on your skin, and getting your circulation going.
A fascinating study by Mittal et al suggests that there is a link between this moderate to intense cardio exercise and healthy neurochemistry. Positive effects on cognitive function and mood were reported in persons with conditions such as schizophrenia and other psychiatric disorders.53,54
Quality Sleep
Sleep disturbances and sleep deficiencies occur quite often where mental health issues exist. As Seibum et al’s research shows, The ongoing strain of poor sleep can worsen symptoms a person may be suffering from. There are natural alternatives to Seroquel that can support better quality sleep that may help, such as relaxation routines, better sleep hygiene, CBT, melatonin, amino acid therapy, and many others.4,55
Avoid Alcohol, Cannabis, Other Drugs
A person may turn to alcohol, cannabis, or stimulants including caffeine in an attempt to manage troubling symptoms. However, doing so may actually increase symptoms over time. For example, psychosis is more likely to occur in persons using cannabis, as is shown in a clinical study by Ganesh et al.7 Caffeine can have a devastating effect when consumed in large quantities, and can induce psychiatric symptoms such as psychosis and manic symptoms. Persons with panic disorder and anxiety are apt to be more sensitive to stimulants such as caffeine.56-59,7,9
However, doing so may actually increase symptoms over time. For example, psychosis is more likely to occur in persons using cannabis, as is shown in a clinical study by Ganesh et al.7 Caffeine can have a devastating effect when consumed in large quantities, and can induce psychiatric symptoms such as psychosis and manic symptoms. Persons with panic disorder and anxiety are apt to be more sensitive to stimulants such as caffeine.56-59,7,9
Alcohol consumption is also connected to numerous health adverse effects, including negatively affecting the microbiome, according to Engan et al’s study on alcohol and its effects on the microbiota.61,8
Seroquel Alternatives vs Antipsychotic Medication Side Effects
If you have suffered debilitating Seroquel (aka quetiapine) side effects, or if this medication is not providing satisfactory results, discussing Seroquel alternatives would be worth the inquiry. There are many safe and well-lit avenues of holistic treatments, including various types of counseling, psychotherapy, and natural treatments that don’t cast the dark shadow of medication side effects. While counseling by itself, or regular acupuncture sessions1 alone cannot instantly replace the medication, such therapies add vital components to a comprehensive, carefully designed antipsychotic alternative treatment plan.
While counseling by itself, or regular acupuncture sessions1 alone cannot instantly replace the medication, such therapies add vital components to a comprehensive, carefully designed antipsychotic alternative treatment plan.
Do not despair if “alternative drugs” are the only other option you have been offered. Antipsychotic medications — and there are many of them — are likely to present the same or very similar adverse reactions. Seroquel belongs to the class of drugs called atypical (second-generation) antipsychotics. The FDA licensed this type of drug to “treat” schizophrenia and bipolar disorder. Alternatives to drug-based treatment have been found to be highly effective in reducing psychiatric symptoms, without inflicting the debilitating effects that long-term prescription drug treatments are known for.
Particularly disturbing are the findings of Vita et al concerning the loss of gray matter in persons with schizophrenia treated with antipsychotics (worsening with the length of treatment with antipsychotic medications).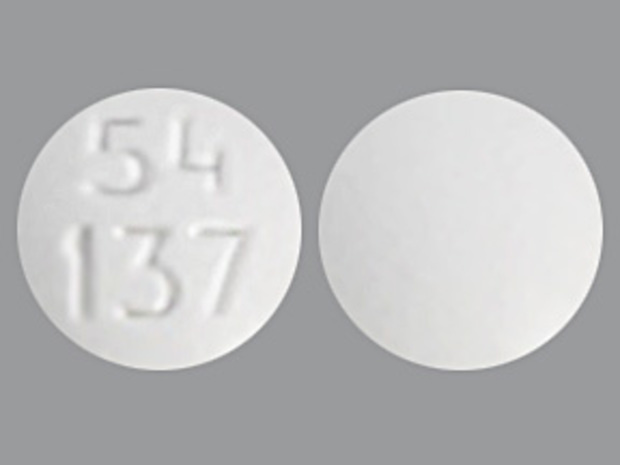 2 Such tragic side effects can be avoided with alternatives to Seroquel.
2 Such tragic side effects can be avoided with alternatives to Seroquel.
Substituting Other Drugs as Seroquel Alternatives
You may have tried other prescription drugs offered as alternatives to Seroquel. It is a common practice to substitute or switch atypical antipsychotics, typical (first-generation) antipsychotics, and mood stabilizer drugs for one another. Conventional medicine doctors are likely to recommend substituting other drugs when symptoms are not being adequately controlled by Seroquel. This is the way conventional medicine often works, through an exhaustive process of trial-and-error trying a series of different drugs either when they “stop working” or fail to work at all.3,5
We believe that there is a better way to tackle mental health conditions like bipolar disorder and schizophrenia. When antipsychotic medication is not working, it may be time to consider natural Seroquel alternatives. Natural therapies are always aimed at putting you one step closer to reaching your desired state of mental health.
Why Do Prescription Drugs Often Fail?
Even the drug companies admit that drugs stop working due to building tolerance to them over time.3,5
Instead of exploring alternatives to Seroquel, some medical experts simply call their patients “treatment-resistant,” a term the psychiatrists and drug-makers have cleverly borrowed from the biologists that originally meant the immunity that pathological bacteria develop to antibiotics. Maybe you were told (with a straight face) you have “treatment-resistant schizophrenia,” or “treatment-resistant depression”? 62
Do not worry. All it means is that the drugs didn’t work, and please know it wasn’t your fault.
The bottom line is that prescription drugs, beyond some attempts to promote theories that the drug companies try and push as factual, are not designed to address or resolve what the actual underlying problems are. So while you may feel a little relief from numbness while you are on the drug, the underlying condition continues and often worsens. The most successful antipsychotic alternatives to Seroquel need to include finding the underlying reasons for the original symptoms. We need to assess vital things like nutritional deficiencies, sleep deprivation,4 accumulations of environmental neurotoxins, a poor diet, an unhealthy lifestyle, genetic factors that can act as barriers to wellness, or an unsupportive or stressful surrounding. Then we can work to change the circumstances of those underlying reasons. Antipsychotic withdrawal must be done extremely carefully as part of a transition over to holistic treatments. We recommend you learn more about Seroquel withdrawal. Getting to the bottom of the cause(s) of symptoms, rather than focusing solely on numbing the symptoms with prescription drugs, can create happiness and success that is long-lasting and best of all, less reliant on prescription drugs.
The most successful antipsychotic alternatives to Seroquel need to include finding the underlying reasons for the original symptoms. We need to assess vital things like nutritional deficiencies, sleep deprivation,4 accumulations of environmental neurotoxins, a poor diet, an unhealthy lifestyle, genetic factors that can act as barriers to wellness, or an unsupportive or stressful surrounding. Then we can work to change the circumstances of those underlying reasons. Antipsychotic withdrawal must be done extremely carefully as part of a transition over to holistic treatments. We recommend you learn more about Seroquel withdrawal. Getting to the bottom of the cause(s) of symptoms, rather than focusing solely on numbing the symptoms with prescription drugs, can create happiness and success that is long-lasting and best of all, less reliant on prescription drugs.
Alternatives to Seroquel at Alternative to Meds Center
We have helped many of our clients who had an initial psychotic or bipolar episode to gradually reduce or eliminate their antipsychotic medications successfully. We use a thorough, gentle, and comprehensive approach that allows enough time to adjust, and heal which is greatly helped by utilizing natural alternatives to Seroquel and other harsh drugs.
We use a thorough, gentle, and comprehensive approach that allows enough time to adjust, and heal which is greatly helped by utilizing natural alternatives to Seroquel and other harsh drugs.
Please remember that when it comes to stopping antipsychotics, slow proves the best and safest way forward.63
Natural mental health is not a quick fix. We have been down that road ourselves and found it doesn’t provide long-term stable relief of symptoms. Rather, we take the time to investigate the root causes and then address what is found. If we can get a reduction in symptoms, this is a good point to launch a gentle Seroquel tapering while at the same time providing support in holistic ways and alternatives to Seroquel that continue to capitalize on these gains.
Please contact us for more information, as there is a lot to discover about the protocols we use, length of program, costs, insurance coverage, and of course the successes of our clients. Our staff roster includes not only holistic psychiatrists and medical doctors but also caregivers and therapists, some of whom have suffered similarly in the past.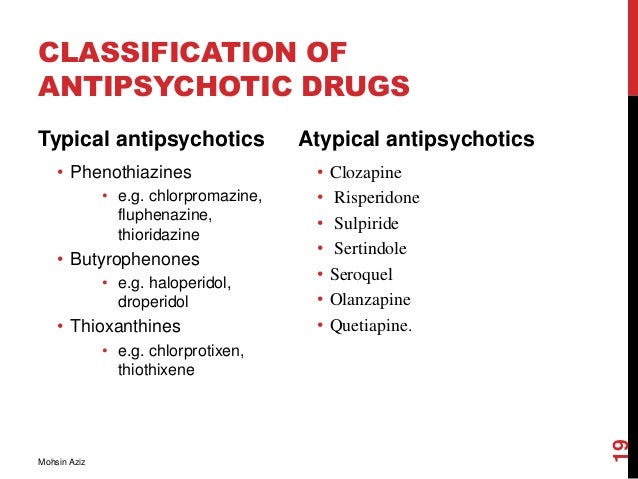 Through overcoming these challenges they have developed a passion to help others who not only need expertise but compassion on the journey back to natural mental health. We look forward to talking with you about our Seroquel alternatives programs delivered inpatient-style in our beautiful, tranquil, well-staffed facility.
Through overcoming these challenges they have developed a passion to help others who not only need expertise but compassion on the journey back to natural mental health. We look forward to talking with you about our Seroquel alternatives programs delivered inpatient-style in our beautiful, tranquil, well-staffed facility.
Approaches to optimize the treatment of depression in patients with Parkinson's disease
Pathological aging is often based on atrophy of cells in certain parts of the brain. Mental disorders accompanying such atrophic processes are classified as a separate group of mental illnesses of late age. This generalization is based on a number of similar characteristics for these forms [4]: slow inconspicuous onset and chronic steadily progressive course; poor prognosis due to the irreversibility of the disease process; gradual development of dementia up to "total" dementia; dominance of the endogenous pathological process; atrophy of the parenchyma of the brain and replacement hydrocephalus.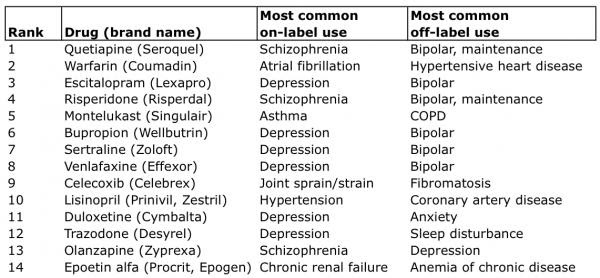 nine0003
nine0003
Parkinson's disease (PD) belongs to the group of degenerative diseases.
PD, or tremor paralysis, was described in 1817. This disease is classified as a degenerative-atrophic disease of the extrapyramidal system of the brain that develops at a late age. The average age of patients by the onset of the disease is 50-60 years. The course of the disease is usually chronically progressive [4, 9, 10].
This pathology affects an average of 100 to 300 people per 100,000 population worldwide. In Russia, patients with PD make up 8 to 10% of the population. The quality of life of patients with PD is drastically reduced. Such patients, gradually becoming disabled as the disease progresses and needing social rehabilitation and long-term care [1, 2], create a significant burden for society. Due to the increase in life expectancy and the aging of the population, the number of patients with parkinsonism is constantly increasing, which increases the relevance of the problem under consideration [24, 32].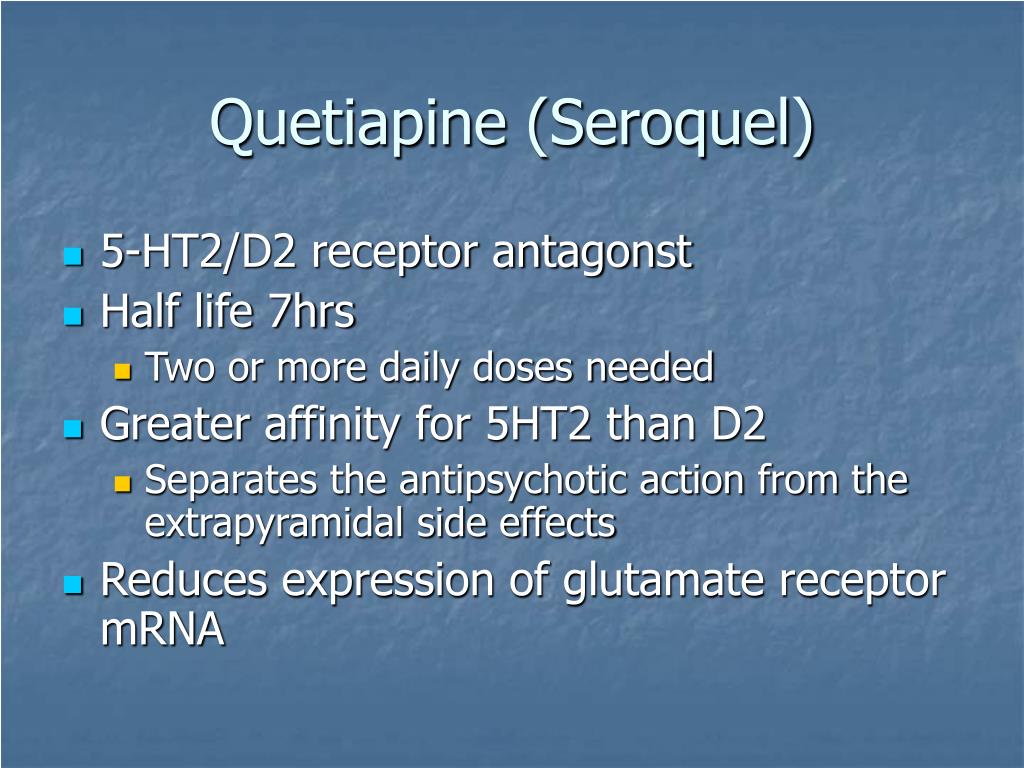 nine0003
nine0003
The purpose of this publication is to discuss the possibilities of providing adequate antidepressant therapy in patients with PD and to evaluate the effect of this therapy on the clinical severity of motor disorders and depressive symptoms in parkinsonism.
Depression is classified as a non-motor symptom of PD, which is also represented by autonomic disturbances, anxiety, and psychotic disorders (nightmares, hallucinations, illusions, and psychomotor agitation during sleep). Depression, in turn, is one of the most common types of affective disorders [3, 4]. According to different authors, the frequency of depression in the population is 3-10%, and in PD it occurs on average in 40-50% of patients. It has also been found that the frequency of depression in patients with PD significantly exceeds its occurrence in a number of other severe chronic diseases [2, 7, 19].].
Depression in PD can be endogenous or exogenous. Endogenous depression is associated with the monoamine deficiency characteristic of this disease; exogenous depression is associated with the patient's response to external factors, in this case we are talking about a reaction to a progressive chronic disease, its unfavorable socioeconomic prospects, and changes in relationships with colleagues and relatives [6].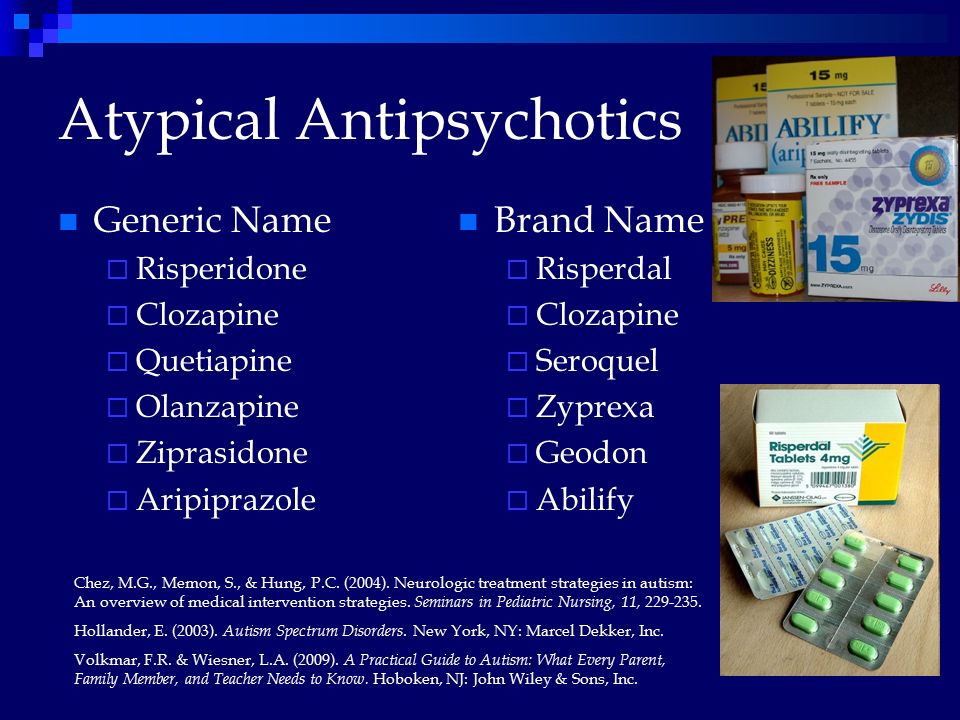
The presence of depression in PD correlates with a faster progression of cognitive (regulatory) disorders, the appearance of psychotic symptoms (small visual hallucinations, illusions). At the same time, it has been shown that the correction of depression has a positive effect on both motor and non-motor manifestations of PD - cognitive functions, sleep disturbances, and pain [8, 10, 22]. nine0003
Psychological factors play a significant role in the formation of depression in PD. Observations show that the most pronounced stress in patients is usually caused by the onset of the disease and the establishment of a diagnosis, and then severe complications in the later stages of the disease. This is consistent with the predominant detection of depressive disorders at the earliest and late stages of the disease. Dopamine deficiency in the brain in PD may additionally contribute to a decrease in adaptation to stress factors, which are the disease and associated changes in the quality of life. This assumption is based on data on an increase in dopamine utilization under conditions of experimental stress [9, 23].
This assumption is based on data on an increase in dopamine utilization under conditions of experimental stress [9, 23].
One of the main roles in the genesis of depression in PD is played by such changes in the physiological metabolism of the brain as a lack of dopamine production, as well as a violation of the production of norepinephrine and serotonin. It is believed that dysfunction of the serotonergic system is responsible for the occurrence of anxiety and aggression in patients with PD [28, 29].
One of the possible predisposing factors for the development of depression in PD is the presence of hereditary burden of depressive disorders. Close relatives of patients with PD have a higher incidence of depression. The relationship between the frequency of depression and the lateralization of PD symptoms, namely, the predominance of the severity of motor disorders on the right side, which indirectly indicates the greater importance of the left hemisphere in the formation of depressive disorders, was discussed [1, 10]. nine0003
nine0003
The diagnosis of major depression requires the presence of depressed mood and/or anhedonia for at least 2 weeks or more in combination with 5 or more of the following criteria that cause significant distress or impairment of daily activities. Minor depression is diagnosed when combined with 2-5 criteria. If depressed mood is combined with 2 other symptoms and is observed on most days in the last 2 years, dysthymia is diagnosed [3, 29].
nine0002 According to the DSM-IV, the criteria for depression are: depressed mood; decreased interests and ability to experience pleasure; a significant decrease or increase in appetite and body weight; sleep disorders; psychomotor agitation or lethargy; increased fatigue, loss of strength; feeling of own uselessness, ideas of guilt; decreased ability to concentrate, make decisions; recurring thoughts of death, suicidal attempts. Common signs of depression in patients with PD are persistent depression of mood, anhedonia (inability to experience pleasure), dysphoria, loss of appetite, changes in body weight, fatigue, sleep disturbance, low self-esteem, increased anxiety, irritability, suicidal thoughts, pessimistic thoughts about the future. At the same time, symptoms typical of endogenous depression, such as feelings of guilt, a sense of failure in life, or self-flagellation, are much less common in PD [30]. nine0003
At the same time, symptoms typical of endogenous depression, such as feelings of guilt, a sense of failure in life, or self-flagellation, are much less common in PD [30]. nine0003
Depression can appear at any stage of the course of PD, but often (in 30% of cases) precedes its first clinical motor manifestations (hypokinesia, rigidity, rest tremor) [13]. However, in most patients with PD, the severity of depressive symptoms is mild or moderate and meets the criteria for minor depression or dysthymia. Only in 3-8% of patients, depression is severe and reaches a psychotic level, but it, as a rule, does not end with suicidal attempts [30, 31]. nine0003
It is important to note the possible relationship between depression and the severity of the disease's motor symptoms. Some studies have found positive correlations between the frequency of depression and the severity of bradykinesia. Along with this, it was noted that depression is less common and less pronounced in patients with a predominantly tremulous form of PD. In particular, in patients with the akinetic-rigid form of PD, depression was detected in 38% of patients versus 15% with a predominantly tremulous form of the disease. The presence of a relationship between depression and bradykinesia probably indicates the presence of common pathophysiological mechanisms for the formation of these disorders. nine0003
In particular, in patients with the akinetic-rigid form of PD, depression was detected in 38% of patients versus 15% with a predominantly tremulous form of the disease. The presence of a relationship between depression and bradykinesia probably indicates the presence of common pathophysiological mechanisms for the formation of these disorders. nine0003
In some cases, the appearance of symptoms of depression is closely related to fluctuations in the effectiveness of drugs used to treat PD during the day. At the same time, depression occurs against the background of the end of the action of a single dose of drugs (in the “off” period) and disappears with the onset of the effect of the next dose (in the “on” phase) [2]. The presence of clinical features of depression, the manifestations of which are clearly “tied” to fluctuations in PD symptoms, made it possible to distinguish subtypes of depressive disorders based on the presence or absence of association with fluctuations in symptoms.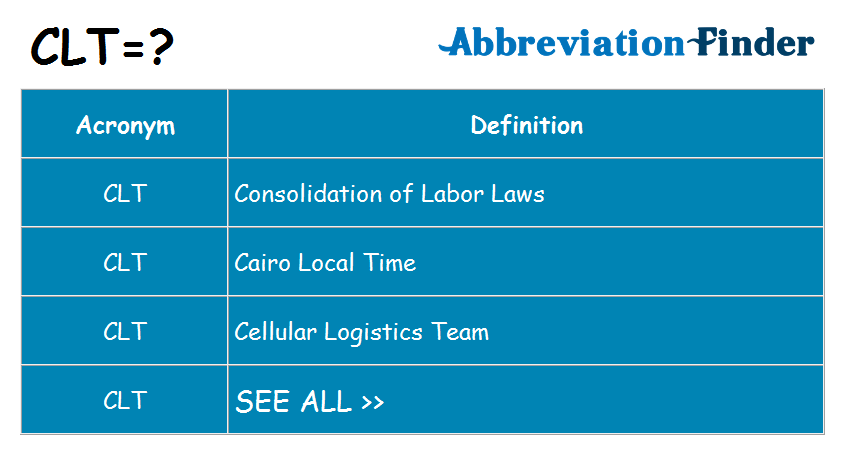 Thus, for depression associated with periods of "off" is characterized by an association with the severity of the main motor and non-motor symptoms (pain, autonomic disorders), the dependence of the appearance on the time of administration and dose of dopaminergic drugs. In contrast, depression that is not associated with “off” periods does not have a clear relationship with the severity of motor symptoms and the stage of PD, the regimen of dopaminergic therapy; may appear several years before the diagnosis of the main symptoms of PD. The presence of depression, the severity of which is closely dependent on the effectiveness of doses of levodopa, confirms the significant role of central dopaminergic dysfunction in its formation. It should also be borne in mind that depressive syndrome may be a side effect of β-blockers and benzodiazepines. It has been suggested that long-term treatment with levodopa in PD may lead to depression, possibly due to the effect of DOPA-containing drugs on serotonin metabolism.
Thus, for depression associated with periods of "off" is characterized by an association with the severity of the main motor and non-motor symptoms (pain, autonomic disorders), the dependence of the appearance on the time of administration and dose of dopaminergic drugs. In contrast, depression that is not associated with “off” periods does not have a clear relationship with the severity of motor symptoms and the stage of PD, the regimen of dopaminergic therapy; may appear several years before the diagnosis of the main symptoms of PD. The presence of depression, the severity of which is closely dependent on the effectiveness of doses of levodopa, confirms the significant role of central dopaminergic dysfunction in its formation. It should also be borne in mind that depressive syndrome may be a side effect of β-blockers and benzodiazepines. It has been suggested that long-term treatment with levodopa in PD may lead to depression, possibly due to the effect of DOPA-containing drugs on serotonin metabolism.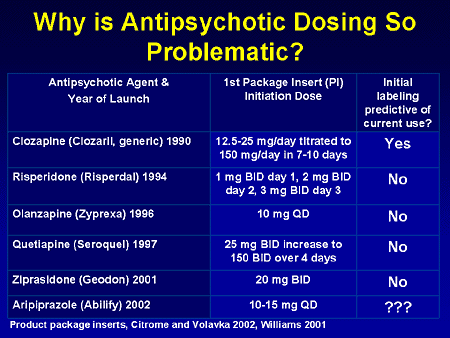 nine0003
nine0003
Depression in PD can often go undiagnosed or, on the contrary, be overdiagnosed. This is due to some common features that are characteristic of depression and PD. Such common symptoms that make it difficult to diagnose correctly are: a decrease in psychomotor activity, increased fatigue, decreased appetite, decreased libido, hypomia, hypophonia, impaired attention, and sleep disturbance [5, 8].
In clinical and research practice, for the screening diagnosis of depression, determining its severity, assessing the dynamics during therapy, quantitative scales and questionnaires are used: the Hamilton Depression Scale (HAM-D), the Beck Depression Inventory (BDI), the Hospital Anxiety and Depression Scale (HADS) , the Montgomery Asberg Depression Scale (MADRS). To assess the severity of depressive symptoms, it is recommended to use HAM-D, VDI, MADRS. nine0003
The presence of severe cognitive impairment makes it difficult to diagnose depression and requires informative assistance from the patient's relatives.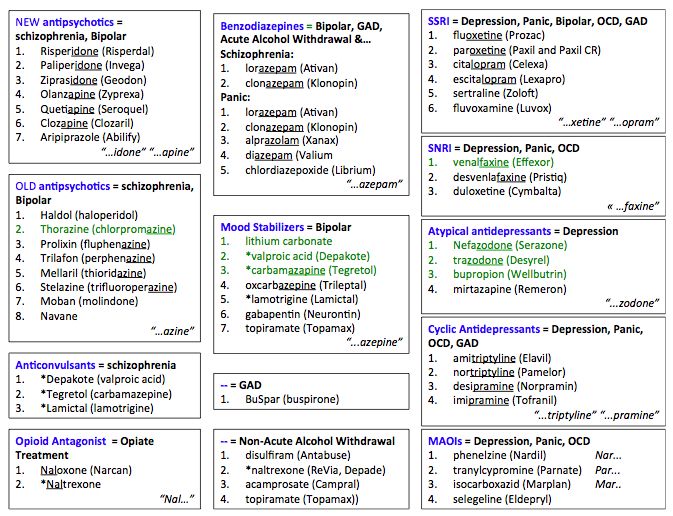 The Cornell Depression Scale for Dementia is used to assess depression in patients with dementia [3, 26].
The Cornell Depression Scale for Dementia is used to assess depression in patients with dementia [3, 26].
When making a diagnosis of depression, manifestations of anhedonia should be differentiated from apathy. Apathy is considered as a violation of motivation and is characterized by a decrease in goal-directed behavior, emotional and cognitive activity, and a narrowing of the circle of interests. This disorder can be both a manifestation of depression and an independent symptom of PD in patients without depressive disorders. According to observational studies, apathy is observed in 17-42% of patients with PD, while its comorbidity with depression is 12-30%. In addition to being associated with depression, manifestations of apathy in PD correlate with the presence of cognitive impairments (bradyphrenia, regulatory frontal disorders), and to a lesser extent, with the severity of motor symptoms of the disease [12, 16]. nine0003
A certain similarity with manifestations of depression and apathy has the phenomenon of increased fatigue. Fatigue is defined as a feeling of physical fatigue and lack of energy that interferes with daily life and is not associated with mental fatigue, drowsiness, or impaired motor function due to PD. This phenomenon is detected in 40-56% of patients with PD, while, like apathy, it can be a manifestation of depression, or a phenomenologically independent symptom of the disease [15]. nine0003
Fatigue is defined as a feeling of physical fatigue and lack of energy that interferes with daily life and is not associated with mental fatigue, drowsiness, or impaired motor function due to PD. This phenomenon is detected in 40-56% of patients with PD, while, like apathy, it can be a manifestation of depression, or a phenomenologically independent symptom of the disease [15]. nine0003
According to different authors, the depressive syndrome in PD worsens the quality of life indicators to a greater extent than the severity of movement disorders. Depression in PD impairs daily activity, the quality of life of patients, reduces compliance (willingness to comply with doctor's orders), aggravates the course of the underlying disease, and is often a risk factor for the development of dementia in PD. In addition, depression in patients with PD significantly worsens the quality of life of relatives living with the patient or caring for him [5]. nine0003
PD patients who experience prolonged depression despite adequate antiparkinsonian therapy require psychotherapy, antidepressants, and, in extreme cases, electroconvulsive therapy [10].
Treatment of depression in PD should primarily include adequate anti-Parkinsonian therapy to optimally control major movement disorders. Some antiparkinsonian drugs have an antidepressant effect (dopamine receptor agonists, type B MAO inhibitors) [5, 8, 11, 20, 21]. nine0003
Patients with depression should receive psychotherapy (rational and behavioral). It is very important to bring them information about the nature of the disease, methods of treating PD, techniques and devices in everyday life that improve activity. This information should be provided by the attending physician at the time of the patient's appointment, as well as in the form of popular benefits for patients and their relatives [2].
If the improvement in motor activity against the background of adequate PD therapy is not accompanied by a decrease in depressive symptoms, the patient is prescribed antidepressants. nine0003
The main properties of an ideal antidepressant include the speed of onset of the therapeutic effect, safety in case of overdose, minimal effect on somatic functions, minimal interaction with antiparkinsonian drugs. In addition, the simplicity of treatment regimens and titration of the therapeutic dose is important, which is important in PD patients with impaired cognitive functions and, above all, memory.
In addition, the simplicity of treatment regimens and titration of the therapeutic dose is important, which is important in PD patients with impaired cognitive functions and, above all, memory.
Usually, selective serotonin reuptake inhibitors (SSRIs), tricyclic and tetracyclic antidepressants, and, more rarely, MAO inhibitors are used to treat depression in PD [20, 21]. nine0003
Until now, SSRIs are the most commonly used in PD with the presence of a depressive syndrome. However, these drugs cannot be combined with the use of type B MAO inhibitors (selegiline) [25, 29, 30]. If there is no effect during the first 3 weeks, the dose of the antidepressant is increased, and if it is ineffective, it is replaced with another drug with a different mechanism of action (for example, a tricyclic antidepressant).
Tricyclic antidepressants are less preferred in PD, as they have anticholinergic side effects - they cause an increase in intraocular pressure, urinary retention, constipation, accommodation disturbance, arterial hypotension and heart rhythm disturbance. In addition, in patients with PD, they often cause visual hallucinations, disorientation, and lead to an increase in cognitive disorders characteristic of this disease [21]. nine0003
In addition, in patients with PD, they often cause visual hallucinations, disorientation, and lead to an increase in cognitive disorders characteristic of this disease [21]. nine0003
The risk group for the use of tricyclic antidepressants includes patients over the age of 60 years, with prostatic hypertrophy, glaucoma, orthostatic hypotension, myocardial infarction, cardiac arrhythmias.
In cases of depression during “off” periods, correction of fluctuations by changing the regimen of taking levodopa drugs and / or combining them with dopamine receptor agonists, COMT and MAO inhibitors is quite effective without additional prescription of antidepressants [4, 9].
Anxiety is a common symptom in PD. It occurs on average in 40% of cases. Anxiety disorders in PD can be manifested by general anxiety, panic attacks, social phobia, obsessive-compulsive disorders. According to DSM-IV, the criteria for anxiety are anxiety and 3 additional symptoms of the following: fatigue, fatigue, impaired concentration, irritability, muscle tension, sleep disturbances noted within the last 6 months [9, thirty].
Panic attacks occur in 24% of patients with PD. They are manifested by various paroxysmal mental, vegetative and somatic symptoms. The most common are paroxysmal tachycardia, tremor, difficulty breathing, hyperventilation, chest pain, frequent urination, hyperhidrosis, feeling of lightheadedness, dizziness. As a rule (in 90% of cases), panic attacks occur during the “off” period, when the action of antiparkinsonian drugs ends and an increase in motor disorders occurs [31]. nine0003
Treatment of patients with PD with manifestations of anxiety, first of all, should include the optimization of anti-Parkinsonian therapy with a decrease in "off" episodes. With insufficient effect, small doses of short-acting benzodiazepines are prescribed. In the presence of cognitive impairment in patients with PD, the dose of benzodiazepines should be lower, the course of treatment should not exceed 1.5 months in order to avoid addiction [30, 31].
Given the relationship between the pathogenesis of PD and a decrease in the number of dopaminergic neurons in various parts of the brain and a decrease in the functioning of the corresponding synaptic connections, these patients should not be prescribed drugs that aggravate monoamine metabolism disorders. nine0003
nine0003
Unfortunately, many antipsychotic drugs, the use of which is discussed for the treatment of depression, anxiety, dyssomnia, etc., associated with parkinsonism, as well as complications of levodopa therapy (such as hallucinations), give precisely negative correlations with the main manifestations of PD, increasing rigidity, bradykinesia (balanced antagonists of serotonin and dopamine receptors), enhancing the cognitive defect (atypical antipsychotics, anticholinergics). Having a high affinity for serotonin receptors, the antipsychotic seroquel has almost no effect on motor and cognitive functions, but often causes drowsiness and anxiety. nine0003
As for antidepressant drugs, the situation is even more complicated. The first representatives of this group - tricyclic antidepressants (amitriptyline) suppress the reuptake of monoamines [17, 22, 25]; monoamine oxidase inhibitors (phenelzine) block the catabolism of monoamines. These groups are quite effective in the treatment of depression, but have significant disadvantages in terms of tolerability and safety. Later developed SSRIs, norepinephrine reuptake inhibitors (SNRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) have a more favorable safety profile and more effectively eliminate comorbid anxiety that often accompanies stressful situations in acute somatic pathology, but do not surpass their predecessors in terms of effectiveness in relation to depression in chronic diseases [18, 20]. This becomes even more relevant when choosing a treatment when it comes to neurodegenerative pathology that lasts for life. nine0003
Later developed SSRIs, norepinephrine reuptake inhibitors (SNRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) have a more favorable safety profile and more effectively eliminate comorbid anxiety that often accompanies stressful situations in acute somatic pathology, but do not surpass their predecessors in terms of effectiveness in relation to depression in chronic diseases [18, 20]. This becomes even more relevant when choosing a treatment when it comes to neurodegenerative pathology that lasts for life. nine0003
In addition, all these drugs have monoaminergic mechanisms of action, which can, to varying degrees, but negatively affect the dopaminergic system, causing either worsening of the main clinical manifestations of parkinsonism or potentiation of the complications of levodopa therapy.
As an alternative, they tried to use NMDA-(N-methyl-D-aspartate) receptor antagonists, which cause a fairly rapid development of the antidepressant effect, but have pronounced undesirable psychomimetic effects [23]. nine0003
nine0003
As an innovative approach for the treatment of depression in PD, the use of valdoxan (agomelatine), which is an agonist of MT1-, MT2-melatonergic and antagonist of 5-HT2c-serotonergic receptors, can be considered. Melatonin is an important regulator of circadian rhythms that determine the structure of sleep and are directly related to the aging process of the body due to the weakening of the reactivity of the circadian clock to environmental stimuli [13, 14, 27]. When studying the therapeutic profile of Valdoxan, an increase in the release of dopamine and norepinephrine in the synaptic structures of the frontal cortex was found. The drug, being a melatonin agonist, exhibits pronounced antagonism to 5-HT2c receptors. The polysynaptic pathway of action of Valdoxan, which runs from the suprachiasmatic nucleus (SCN) to the ventrotegmental nucleus, originates from the mesocortical and mesolimbic dopaminergic pathways. Thus, the effect of 5-HT2c receptors located in the SCN on ascending dopaminergic transmission is mediated. Blockade of these receptors leads to the release of dopamine in the frontal cortex and an increase in transmission, the activity of which is weakened in depression [18, 21]. Features of the action of Valdoxan served as the rationale for its choice for the treatment of depression in PD. The authors of the article have their own preliminary observations. nine0003
Blockade of these receptors leads to the release of dopamine in the frontal cortex and an increase in transmission, the activity of which is weakened in depression [18, 21]. Features of the action of Valdoxan served as the rationale for its choice for the treatment of depression in PD. The authors of the article have their own preliminary observations. nine0003
Valdoxan treated 7 patients, 2 men and 5 women, the average age of which was 64 years, and the average duration of the disease - 14 years. The drug was prescribed at a dose of 25 mg per day for 6 months, after which the patients continued to be observed in order to establish the stability of the therapeutic effect. The main antiparkinsonian therapy did not change throughout the study period. Patients were examined using the Unified PD Rating Scale (UPDRS), the Sleep Quality Questionnaire (LSEQ), and the Hamilton Depression Rating Scale (HAM-D). nine0003
The data obtained allow us to speak not only about the possibility of correcting anxiety and depressive disorders, but also about the quality of sleep and wakefulness, as well as positive changes in relation to the symptoms of parkinsonism (due to increased dopaminergic transmission). It is important to note that this improvement was stable for 3-4 months after the end of Valdoxan treatment.
It is important to note that this improvement was stable for 3-4 months after the end of Valdoxan treatment.
A small number of patients does not yet allow generalizing conclusions about the effectiveness of Valdoxan. However, this observation may serve as a stimulus for new studies of the therapeutic spectrum of Valdoxan, including in degenerative diseases of the central nervous system. nine0003
In conclusion, it should be noted that PD undoubtedly requires an integrated therapeutic approach. This applies primarily to PD with depression.
Dangerous trend of prescribing antipsychotics to 3-year-olds
This is not an unfounded statement. It relies on statistics that show that the use of neuroleptics (they are also called antipsychotics) in children and adolescents in Europe and the United States increased significantly in the 2000s.
"It is of particular concern that drugs continue to be prescribed despite growing evidence of serious side effects from their use, which are even more pronounced in children and adolescents than in adults. " nine0003
" nine0003
This quote is from pediatrician David Rubin, professor at the University of Pennsylvania and director of the PolicyLab at the Children's Hospital of Philadelphia. Professor Rubin is a highly respected specialist in the field of work with children at high health risks in his country, co-author of 80 scientific studies, and his PolicyLab develops principles of medical care for children.
It's highly likely that Professor Rubin knows what he's talking about, but it's worth taking a look at at least a few relatively recent studies in this area. nine0003
Efficiency is limited
What are antipsychotics
These are drugs that act on the systems of neurotransmitters (signaling molecules in the brain), primarily dopamine.
They have been well studied in adult patients with schizophrenia and bipolar disorder, are quite effective in relieving severe symptoms of these diseases, and their appointment with an individual approach, reasonable dosing and well-calculated duration of the course is considered justified. nine0111 As far as pediatric practices are concerned, data on their effectiveness are scarce.
nine0111 As far as pediatric practices are concerned, data on their effectiveness are scarce.
Both first-generation antipsychotics (such as the now-meme-changing haloperidol) and second-generation antipsychotics, known as atypical antipsychotics, such as aripiprazole and risperidone, are in use today. Children are more likely to be prescribed drugs of the second group, as they are considered less harmful than older drugs.
If you are a parent of a child with developmental disabilities, whether it is autism, ADHD or intellectual disabilities, you must have come across the advice of a pediatrician, neurologist, psychiatrist, and even a defectologist to treat the child with Sonapax (active ingredient - thioridazine) or Rispolept (active ingredient - risperidone ). At the same time, they explain to you that the medicine will reduce the manifestations of autism, calm the baby, and even push the development of speech. nine0003
It can be said with absolute certainty that there is no scientific evidence for such claims, and the prescription of such drugs, in principle, can help solve only one problem: stop psychomotor agitation that leads to dangerous behavior.

A Columbia University study led by psychiatry professor Mark Alfson found that a number of drugs (eg, clozapine and olanzapine) actually help reduce aggression and disruptive behavior in children with ADHD. At the same time, Olfson is in no hurry to recommend their use, especially at an early age. Why, we will consider below. nine0003
A University of Arizona study published in November 2019 assessed the balance of benefits and harms of 26 drugs, including antipsychotics, in the treatment of children, adolescents and young people with autism.
They found that risperidone was prescribed particularly frequently. It was taken by 170 of the 505 study participants. At the same time, a decrease in aggression was observed in 40% of those who took it, a decrease in anxiety - in 21%, irritability - in 24%.
Quetiapine (Seroquel) helped reduce aggression and agitation in 28% of cases, olanzapine (Zyprexa) in 32% of cases.
As you can see, there are benefits from drugs, but they help at best 40% of patients.
However, there is a problem here too, and it is connected with the fact that we do not always understand what causes aggression, self-aggression and other types of destructive behavior in a small child, especially non-verbal.
“What are you complaining about?” Electroencephalography. Photo: Kirill Kukhmar/TASS
This question is asked by a doctor to an adult patient at the beginning of the appointment. In the case when he has a child who cannot speak, the question is addressed to parents who see the symptoms, but do not always understand their causes.
Meanwhile, the emotional state of a small patient and his destructive behavior is not always explained by an imbalance of neurotransmitters.
Unfortunately, it has not yet become normal practice to first exclude physical causes that could lead to the fact that a three- or five-year-old baby continuously screams, throws objects, hits himself or his parents, and only then prescribe antipsychotics. nine0003
nine0003
In the official clinical guidelines for the treatment of autism in our country today, there is no such item as electroencephalography. Meanwhile, autism is often accompanied by convulsive activity of the brain of varying degrees of intensity, not always reaching full-blown epilepsy, and sometimes taking forms that are completely different from epileptic seizures.
Episodes of spontaneous aggression in a child, arising, as described by parents, suddenly, out of the blue, in the process of seemingly calm play, not provoked by conflict, may be the result of an attack of convulsive brain activity. nine0003
In this case, antipsychotics not only won't help, but can even harm, as some of them lower the seizure threshold, in other words, make it easier for the trigger (and it can be a number of external factors) to provoke an attack.
Another likely cause of dangerous behavior is physical pain that the child cannot report, and his frustration results in self-harmful behavior: children can hit themselves in the stomach, in the face, bang their heads against the wall. nine0003
nine0003
There is a wealth of scientific evidence on the physical illnesses associated with autism, and gastroenterological disorders are common among them. Note that in a child without autism, but with undeveloped speech, abdominal pain also becomes a huge problem.
It is quite obvious that neuroleptics will not give anything in this case either. Those that have a strong hypnotic effect at the initial stage will make the child drowsy and quiet for several days, but this will exacerbate the problem rather than solve it. nine0003
Gastrointestinal examinations, as you might guess, are also not standard protocol recommendations for helping children with autism and other developmental disabilities.
In children with autism, such a disease as allergy is also common, and in some cases it does not give them typical manifestations. The child may not suffer from rhinitis, edema, tearing, skin rashes, but when in contact with seasonal plant pollen, such children's behavior deteriorates significantly. This was established by the American immunologist Dr. Marvin Boris. nine0003
This was established by the American immunologist Dr. Marvin Boris. nine0003
In this case, some antipsychotics (eg, risperidone) help. This is not surprising, since this drug has antihistamine activity, but if it's all about allergies, a much more meaningful approach would be to use targeted antiallergic drugs, which, although not harmless, are nowhere near as harmful as antipsychotics.
Another reason for a child's aggressive behavior can be banal lack of sleep. Sleep disturbance is very common in children with autism and other developmental disorders. nine0003
In this case, neuroleptics at the initial stage help to improve sleep, but over time, the hypnotic effect is leveled - the drug becomes addictive.
A careful and experienced physician, before prescribing an antipsychotic drug to a young patient, should make sure that his problematic behavior is not due to one of the above reasons.
And, finally, about the most important thing.
Side effects Photo: Mohamed abdelghaffar/Pexels
There are many of them.
Atypical antipsychotics are considered milder than first-generation antipsychotics, but they also cause side effects such as tremors, weight gain, high cholesterol, diabetes, tardive dyskinesia (tics, involuntary movements), early breast development in girls, and even in boys.
The favorite among this class of drugs both abroad and in Russia is risperidone, also known under the trademarks Risperdal and Rispolept. It is prescribed to very young children - starting from 5 years old, or even earlier. nine0003
Meanwhile, if we go back to a recent study from the University of Arizona, we see that risperidone reduces aggression and agitation in 40% of cases, but in 14% of patients, on the contrary, it causes or increases it.
In addition, 11% of those who took this drug developed behavioral problems that they did not have before.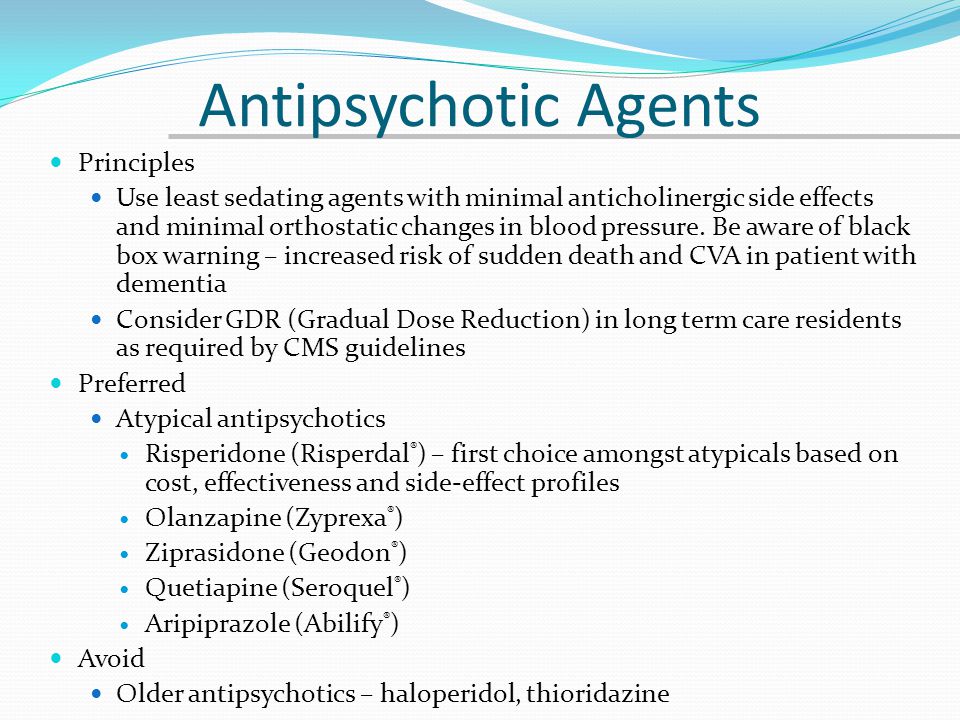 35% experienced weight gain.
35% experienced weight gain.
Not all Russian psychiatrists know that in 2013, the pharmaceutical company Johnson & Johnson, the manufacturer of risperdal, lost a lawsuit and was fined $1.1 billion for illegal marketing, namely, for downplaying the risk of side effects of the drug, in particular diabetes , as well as the development of the mammary glands in boys. According to the claims of the victims, the company is still paying. nine0003
In the Arizona study, drugs such as quetiapine and olanzapine (Seroquel and Zyprexa) tipped the balance of benefits and harms towards harms. Both drugs can cause weight gain, cognitive decline, and Zyprexa in 18% of patients causes / enhances aggressive behavior.
A 2018 Canadian team reviewed studies on the use of antipsychotics in children and young adults. The researchers concluded that the serious side effects of these drugs dictate the need to use them only in cases where the possibilities of other therapies have already been exhausted. nine0003
nine0003
Prof. Olfson, whose research we cited above, says the same.
“There are serious concerns that these drugs are being overused, especially in young children. Clinical guidelines and common sense dictate that they be used with great caution and only when other therapies have failed, that is, as a last resort.”
"Annoying Dissonance" Photo: Pavel Danilyuk/Pexels
This is how one can characterize the document "Autism Spectrum Disorders: Diagnosis, Treatment, Monitoring", which is the official clinical guidelines for psychiatrists working with children with ASD in our country. nine0003
“An important task of medical professionals dealing with autistic disorders… is to disseminate this knowledge (about drugs. - Ed.) both among doctors and other related professionals, as well as among parents. A persistent prejudice against drug treatment does not help to improve the condition of patients with autism, ”say the authors of the recommendations, Doctor of Medical Sciences N. V. Simashkova and E.V. Makushkin.
V. Simashkova and E.V. Makushkin.
This is strikingly different from what their foreign colleagues say and write, including in the conclusions of scientific studies, however, after reading this text, you will no longer be surprised when not only a doctor, but also , as indicated above, "specialists of a related profile" - a psychologist, defectologist and even a kindergarten teacher or school teacher. nine0003
The authors of the recommendations suggest using antipsychotics not only to stop aggression and psychomotor agitation, but also to use them “to improve cognitive functions”, although there are practically no serious scientific studies demonstrating such effects of these drugs.
Esteemed Doctors of Sciences also support the expansion of the list of antipsychotics for use in pediatric practice by adding drugs that have shown effectiveness in adults.
Perhaps the biggest surprise, if not amazement, is the recommendation to use the good old haloperidol in children from the age of three.
Also, from the age of 3, a child can be recommended periciazine, trifluoperazine and chlorpromazine, and the list for 5 and 6-year-olds expands even more. nine0003
Unfortunately, recommendations for pre-screening young patients for possible comorbidities are not included in these guidelines.
There is an alternative ABA therapy. Photo courtesy of adpo.edu.ru
And this is what the very scientists and psychiatrists who seem to be interested in promoting drug treatment are talking about.
Mark Olfson argues that aggressive behavior should be dealt with primarily by behavioral methods. nine0003
Professor of Psychiatry Christoph Correll, who wrote an editorial commentary on Olfson's article, states, "Behavior modification and family therapy should always be the first choice, but less than a quarter of children and adolescents receive this kind of help."
There are reasons for this: the lack of psychotherapists, the duration of family therapy, its high cost, problems with payment under the insurance policy.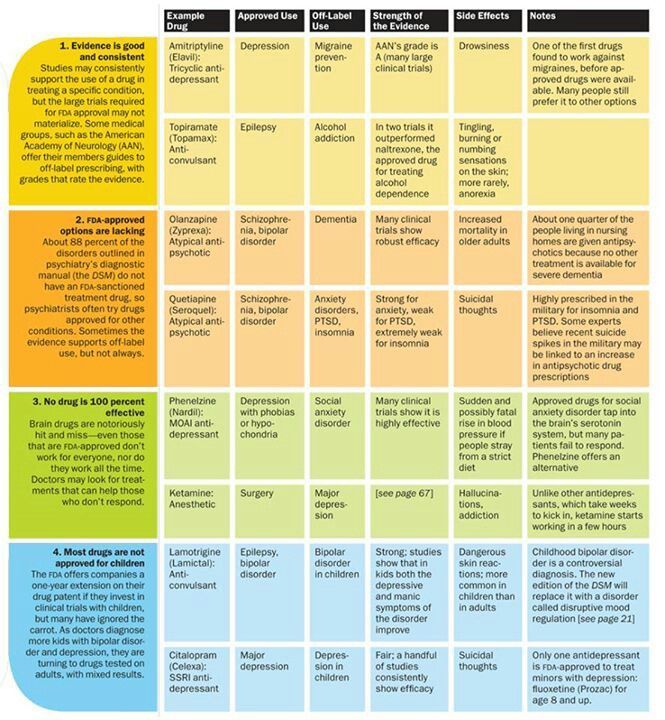
It is quick and easy to prescribe a pill and take it, it is less expensive for a doctor, for the healthcare system in general, and for parents both in the USA and in Europe, and even more so in Russia. nine0003
In the meantime, Applied Behavior Analysis based therapy (often referred to as ABA Therapy) is slowly becoming available in our country, which in a huge number of cases successfully copes with the most unpleasant and dangerous types of behavior.
Applied Behavior Analysis, ABA Therapy: Strength in Flexibility
Read more
This method requires parents to spend a lot of time and energy in selecting a specialist, their own training and very often dictates changes in the lifestyle of the whole family. nine0003
Of course, it also requires money, but what the child and the whole family gains cannot be overestimated.
Don't rush to give your child a pill.
If you still have to do this, consider the advice of the president of the Center for Autism Problems and an experienced mother of a young man with autism, Ekaterina Men: .