All or nothing thinking ocd
How It Can Limit You and How to Stop
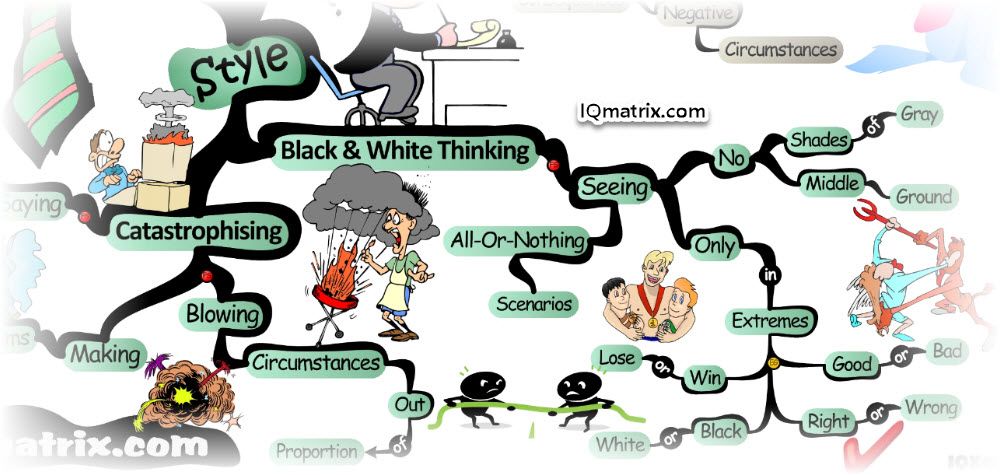
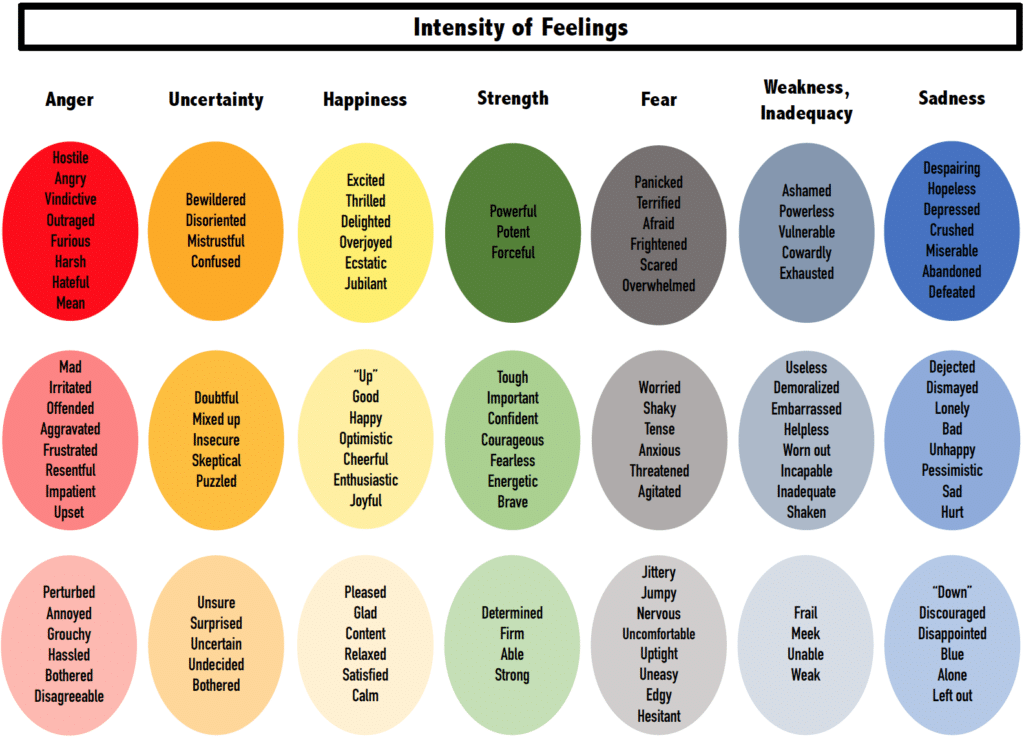
Black and white thinking is the tendency to think in extremes: I am a brilliant success, or I am an utter failure. My boyfriend is an angel, or He’s the devil incarnate.
This thought pattern, which the American Psychological Association also calls dichotomous or polarized thinking, is considered a cognitive distortion because it keeps us from seeing the world as it often is: complex, nuanced, and full of all the shades in between.
An all-or-nothing mindset doesn’t allow us to find the middle ground. And let’s face it: There’s a reason most people don’t live on Everest or in the Mariana Trench. It’s hard to sustain life at those extremes.
Most of us engage in dichotomous thinking from time to time. In fact, some experts think this pattern may have its origins in human survival — our fight or flight response.
But if thinking in black and white becomes a habit, it can:
- hurt your physical and mental health
- sabotage your career
- cause disruption in your relationships
(Note: There is conversation in the sexual health and mental health fields about NOT referring to dichotomous or polarized thinking in terms of ‘black and white thinking’ as it could be interpreted as referring color and race. More often, professionals refer to it as extremes or polarizations.)
Here, we discuss:
- how to recognize polarized thoughts
- what they could be telling you about your health
- what you can do to develop a more balanced outlook
Certain words can alert you that your thoughts are becoming extreme.
- always
- never
- impossible
- disaster
- furious
- ruined
- perfect
Of course, these words aren’t bad in themselves. However, if you notice that they keep coming up in your thoughts and conversations, it could be a signal that you’ve adopted a black and white perspective on something.
It can harm your relationships
Relationships happen between individuals, whether they see each other as family, friends, neighbors, co-workers, or something else entirely.
And because people have ups and downs (to phrase it dichotomously), plus quirks and inconsistencies, conflicts inevitably arise.
If we approach normal conflicts with dichotomous thinking, we’ll probably draw the wrong conclusions about other people, and we’ll miss opportunities to negotiate and compromise.
Worse still, black and white thinking can cause a person to make decisions without thinking about the impact of that decision on themselves and others involved.
Examples may include:
- suddenly moving people from the “good person” category to the “bad person” category
- quitting a job or firing people
- breaking up a relationship
- avoiding genuine resolution of the issues
Dichotomous thinking often shifts between idealizing and devaluing others. Being in a relationship with someone who thinks in extremes can be really difficult because of the repeated cycles of emotional upheaval.
It can keep you from learning
I’m bad at math. Most math teachers hear this proclamation over and over during the school year.
It’s the product of a success or failure mindset, which is a natural outgrowth of a grading system that defines failure (scores of 0–59) as over half the grading scale.
Some courses even have a simple binary to measure learning: pass or fail. One or the other.
It’s all too easy to fall into dichotomous thinking about your academic accomplishments.
A growth mindset, which is becoming increasingly popular, encourages students to recognize incremental progress toward mastery — to see themselves moving closer to being able to do what they have set out to do.
It can limit your career
Dichotomous thinking makes and sticks to rigidly defined categories: My job. Their job. My role. Their role.
In many collaborative work environments where roles shift, expand, and re-form, having rigid limits can keep you and the organization from achieving goals.
A 2017 study examined the workings of a Dutch film studio.
It found that some ambiguity in people’s roles and responsibilities had positive overall effects on the creative project, even though some conflicts arose as people expanded the scope of their work.
Black and white thinking can also limit how you think of your career prospects.
During the 2008 financial crisis, many people lost jobs they’d held for a long time.
Whole sectors slowed or stopped hiring. The crisis forced people to look expansively at their skill sets, rather than clinging fiercely to a rigid idea of what they could do.
Thinking of your career as fixed and narrowly defined could cause you to miss out on possibilities you might find enriching, literally and figuratively speaking.
It can disrupt healthy eating habits
Several studies have found a connection between eating disorders and dichotomous thinking.
Black and white thinking can cause people to:
- look at certain foods as good or bad
- look at their own bodies as either perfect or revolting
- eat in binge-purge, all-or-nothing cycles
Researchers have also found that dichotomous thinking can lead people to create rigid dietary restraints, which can make it hard to maintain a healthy relationship with food.
Some black and white thinking is normal, but persistent dichotomous thought patterns are associated with a number of conditions.
Narcissism (NPD)
NPD is a condition that causes:
- an exaggerated sense of self-importance
- a deep need for attention
- a profound lack of empathy for others
Black and white thinking is one of the symptoms of this personality disorder.
Researchers have found that the tendency toward dichotomous thinking makes it much harder for people with NPD to get the help they need because they may devalue and discard therapists too quickly.
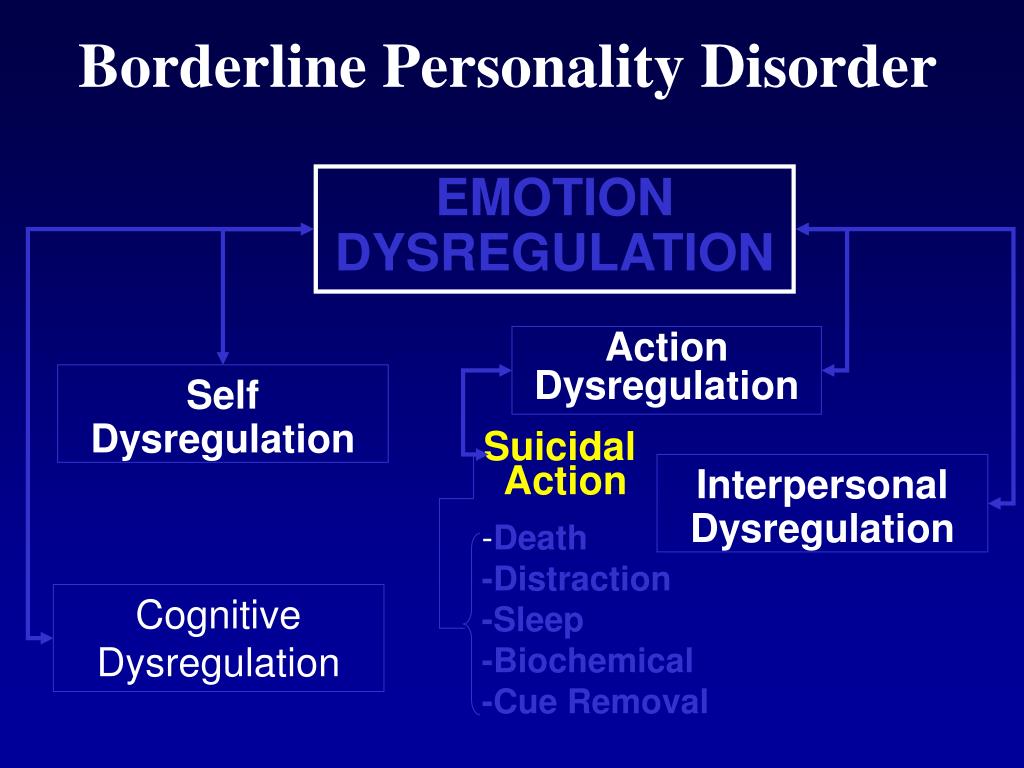
Borderline personality disorder (BPD)
The National Institutes of Mental Health describe BPD as a mental illness that causes people to “experience intense episodes of anger, depression, and anxiety.”
People with BPD:
- usually have problems controlling impulses
- often experience black and white thinking
- may struggle with interpersonal relationships
In fact, studies have found that the tendency to think in polar opposites is at the heart of the problems many people with BPD have in their relationships.
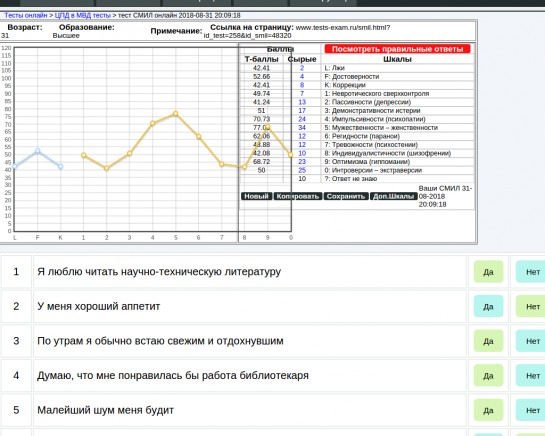
Obsessive compulsive disorder (OCD)
Some psychologists think people who have OCD usually think in all-or-nothing patterns because the ability to put something into a firm category may give them a sense of control over their circumstances.
Dichotomous thinking makes it possible for people to maintain a rigid perfectionism, and that can make it harder to get help.
If a person has a setback, it would be easy to see that as a total failure of therapy instead of viewing it as a momentary hiccup in the overall progression.
Anxiety and depression
People who are vulnerable to anxiety and depression may have a tendency to think in absolutes.
A 2018 study that examined the natural speech of people with anxiety and depression found much more frequent use of “absolutist” language among them than in control groups.
All-or-nothing thinking can also cause us to ruminate, which can worsen anxiety or depression.
It’s also worth noting that researchers have found a connection between black and white thinking and negative perfectionism.
Researchers have found black and white thinking is present when people are dealing with anxiety and depression.
Racism and homophobia
It’s been surmised that dichotomous thinking may be at the root of some of our most persistent social divisions.
Racist, transphobic, and homophobic ideologies often fixate on “in” groups and “out” groups in society.
These ideologies tend to involve projecting negative qualities almost exclusively on the “out” group.
Negative stereotypes are typically used to describe members of those groups who they believe are unlike themselves.
Although personality disorders and mental health conditions are sometimes genetic, there isn’t enough research to say conclusively that black and white thinking itself is inherited.
It has, however, been linked to childhood or adult trauma.
Researchers think that when we experience trauma, we may develop dichotomous thinking patterns as a coping strategy or to try to protect ourselves from future harm.
Black and white thinking can really make things difficult for you personally and professionally, and has been linked to mental health conditions that are treatable.
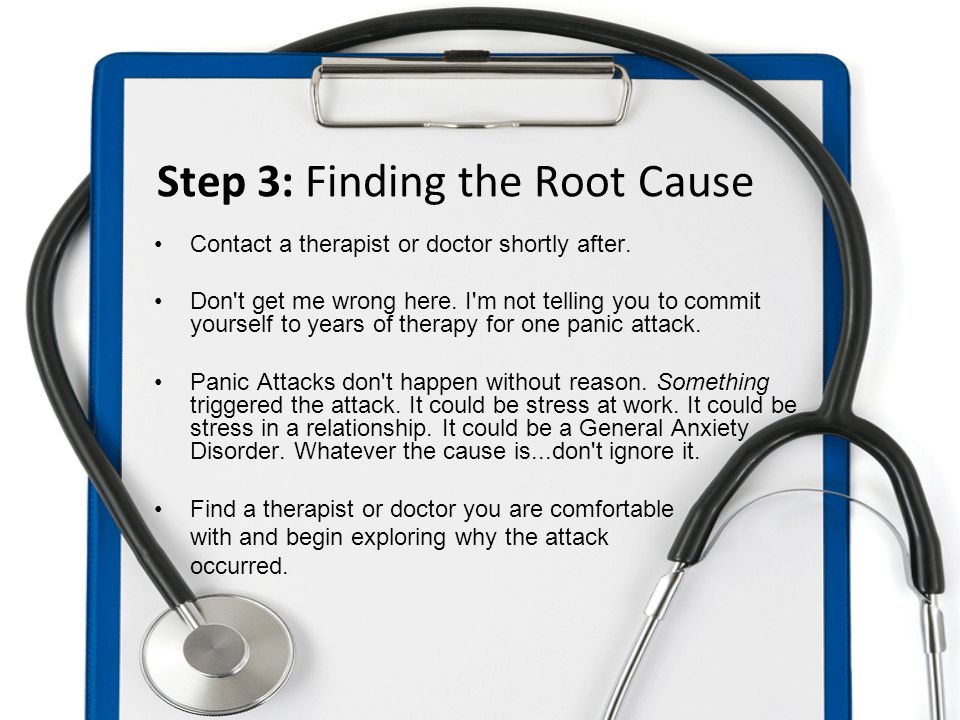
For these reasons, it’s important to talk to a psychotherapist or mental health professional if you notice that thinking in extremes is affecting your health, relationships, or mood.
You may want to work with someone who is trained in cognitive behavioral therapy, because it has been proven effective in dealing with dichotomous thinking.
You may also find it helpful to try some of these methods:
- Try to separate what you do from who you are. When we equate our performance on a single metric with our overall worth, we’re going to become vulnerable to black and white thinking.
- Try listing options. If black and white thinking has you locked into only two outcomes or possibilities, as an exercise, write down as many other options as you can imagine.
 If you’re having trouble getting started, try coming up with three alternatives at first.
If you’re having trouble getting started, try coming up with three alternatives at first. - Practice reality reminders. When you feel paralyzed by black and white thinking, say or write small factual statements, like There are several ways I can solve this problem, I’ll make a better decision if I take time to get more information, and Both of us may be partially right.
- Find out what other people think. Black and white thinking can keep you from seeing things from someone else’s perspective. When you’re in conflict with someone, calmly ask clarifying questions so you can come to a clear understanding of their viewpoint.
Black and white thinking is a tendency to think in extremes. While it’s normal from time to time, developing a pattern of dichotomous thinking can interfere with your health, relationships, and career.
It’s associated with anxiety, depression, and a number of personality disorders, so if you find yourself hampered by thinking in black and white, it’s important to talk to a therapist.
A therapist can help you to learn some strategies to gradually change this thought pattern and live a healthier and more fulfilling life.
OCD and Black-and-White Thinking | Psych Central
It’s common for people with OCD to think in extremes, known as black-and-white thinking.
Obsessive-compulsive disorder (OCD) is a serious mental health condition that affects your thoughts (obsessions) and behaviors (compulsions).
The condition often involves cognitive distortions, which are inaccurate, unhelpful, and irrational beliefs that make us feel bad about ourselves. There are many types of cognitive distortion, and black-and-white thinking – also called all-or-nothing thinking — is common in OCD.
Rather than seeing that life comes in shades of gray, people who tend toward black-and-white thinking think in extremes. This is a rigid thinking pattern that doesn’t allow for the complexities of life.
Some examples include:
- “I made a mistake. I always fail.
 I am a failure,” versus, “I sometimes make mistakes.”
I am a failure,” versus, “I sometimes make mistakes.” - “That person hurt me once, so they are an evil person,” versus, “That person does bad things sometimes.”
- “It’s raining, so my day is totally ruined,” versus, “The rain is a shame, but there are still some good parts about the day.”
People who consistently fall into this type of thinking have trouble accepting uncertainty. They may use words like “never,” “always,” and “totally.”
While everybody falls into extreme thinking sometimes, mental health conditions like anxiety, depression, and OCD can mean it’s very difficult to move away from.
All-or-nothing thinking can have negative impacts on your life. For example, it could cause you to walk away from salvageable friendships after the first conflict, or you might quit a job as soon as you dislike something about it.
For people with OCD, extreme thinking can keep you locked in a self-perpetuating cycle of obsessions and compulsions.
OCD is also known as the doubting disorder. It can be hard for people with OCD to accept uncertainty.
It can be hard for people with OCD to accept uncertainty.
For example, people who engage in compulsions do so to find a 100% guarantee that their intrusive thoughts (obsessions) are untrue. This may cause them to experience all-or-nothing thought patterns more often than most.
For example, someone with OCD could have the intrusive thought that they might have given their family an illness. They might then think “I risked getting my family sick, so I’m a terrible person,” versus, “Maybe I got my family sick, but I’m still a good person overall.”
Many OCD obsessions are in themselves examples of black-and-white thinking. For example:
- “If I don’t do this ritual and my mother dies, then it will be my fault,” versus, “Whether or not I do this ritual, my mother could die. It won’t be all my fault.”
- “If I go even a mile over the speed limit then I might kill someone and that will mean I’m an evil person,” versus, “Driving is inherently risky and one mistake doesn’t make a person evil.
 ”
”
People with OCD may also have extreme thoughts about their treatment and recovery process. Examples include:
- “There’s no way I’m ever going to get better — my case is too severe,” versus, “I might get better even if I feel like I won’t.”
- “I’m always going to feel this way,” versus, “I don’t know how I’ll feel tomorrow.”
- “I always do my therapy exercises but they never work for me,” versus, “Therapy hasn’t been as helpful as I’d hoped, but it does work around half of the time.”
Lastly, many people with OCD have co-occurring depression. In fact, depression is the most common comorbid disorder for people with OCD.
Depression could also lead to extreme thoughts for people with OCD, like:
- “No one wants to hang out with me because of my OCD,” versus, “Some people have rejected me, but some people have wanted to get to know me.”
- “OCD has ruined my life; I’m never going to be happy,” versus, “There are good things about my life that I’m grateful for too.
 ”
” - “I missed a dose of my medication. I’m always messing up. I’m a disaster,” versus, “I missed a dose of my medication, and I’ll start up again today. I’m allowed to make mistakes.”
There are several effective treatment methods for OCD. According to the American Psychiatric Association, the most effective and recommended treatments are:
- medication
- a specific type of cognitive behavioral therapy (CBT) called exposure and response prevention (ERP)
- or a combination of both
ERP works well for people with OCD. It challenges people to intentionally activate obsessions, then resist the urge to engage in a compulsion, in a safe, supportive environment.
Medication can also be very helpful for OCD. Selective serotonin reuptake inhibitors (SSRIs) are usually the recommended medication.
OCD is a mental health condition that makes it difficult for people to accept uncertainty. This can involve a type of cognitive distortion called black-and-white thinking.
If you have OCD you can find relief from your symptoms by talking with a mental health professional and receiving treatment.
You can start looking for an OCD specialist by using the International OCD Foundation’s resource directory. Psych Central’s How to Find Mental Health Support resource may also help.
“Wash your hands 10 times so nothing happens”: how obsessive-compulsive disorder is manifested (and treated)
Health
In obsessive-compulsive disorder (OCD), a person is tormented by obsessive thoughts and actions that he cannot stop. E Clinical psychologist Svetlana Malysheva, an expert at the Not in Vain Medical Solutions Foundation, tells how to suspect this anxiety disorder and help yourself or a loved one.
What is obsessive-compulsive disorder and how common is it?
Obsessive-compulsive disorder (OCD) or obsessive compulsive disorder is the most difficult anxiety disorder to treat. However, it is diagnosed only in 2-3% of people in the world. Why? A person is embarrassed to talk about the problem even with relatives, and even more so - to seek help from a psychologist and psychotherapist. Although there are many people around us with various mental illnesses, with whom it is possible to live qualitatively in society.
However, it is diagnosed only in 2-3% of people in the world. Why? A person is embarrassed to talk about the problem even with relatives, and even more so - to seek help from a psychologist and psychotherapist. Although there are many people around us with various mental illnesses, with whom it is possible to live qualitatively in society.
Obsessive-compulsive disorder usually manifests itself at 20-25 years of age. In men - before puberty, in women - closer to 20 years. OCD is also sometimes seen in children and adolescents.
How does obsessive-compulsive disorder manifest itself?
In OCD, a person is tormented by obsessive thoughts (obsessions) and actions (compulsions) that he cannot stop. For example, thoughts about the threat of contamination of one's own body: a person washed his hands, left the bathroom, and it seems to him that he is already dirty. The idea of cleanliness becomes very important, and keeps spinning in the head like a broken record that does not turn off and torments a person. He has to come up with all sorts of rituals to calm himself: “If I wash my hands five times before going out, then they will definitely be clean.” As psychotherapist Mehmet Sungur says, “A person with OCD doesn’t wash his hands, he washes his mind.”
He has to come up with all sorts of rituals to calm himself: “If I wash my hands five times before going out, then they will definitely be clean.” As psychotherapist Mehmet Sungur says, “A person with OCD doesn’t wash his hands, he washes his mind.”
The more a person with OCD follows the rituals, the more they confirm the underlying phobia.
Constantly washing hands, a person confirms the idea that germs will kill him if ... he does not wash his hands right now. The vicious circle is fixed, the cycle is closed.
A person with OCD cannot stop - he constantly mixes thoughts in his head, tries to keep the outside world under control. If something goes wrong, he may experience emotions that he cannot cope with and again begins to come up with some kind of rituals.
Patients with obsessive-compulsive disorder may fear that they will behave aggressively, or feel that their thoughts are inappropriate or immoral and feel guilty about them. In this case, the specialist has to work with thoughts, not with behavior.
OCD is also based on a feeling of some kind of threat and constant doubts about whether the person did everything for something to happen or, conversely, not to happen. A person doubts all the time, takes on super-responsibility for everything that can happen to him, shows excessive alertness. For example, it endlessly checks to see if the sockets at home are turned off to prevent short circuits and fires, which it poses as a threat.
A person with OCD considers himself a key link in the chain of any, even external, events beyond his control. It seems to him that if he can imagine the worst outcome in his head, then he must do something to avoid it.
Why does OCD occur?
- Biological causes eg birth trauma, developmental delay.
- Genetic and personality traits - perfectionism, preoccupation with details, rules, order, indecisiveness, excessive conscientiousness, excessive desire to do everything right.
 However, they only increase the likelihood of OCD, but this is not a direct causal relationship. For example, even if both parents are diagnosed with schizophrenia, there is only a 10% chance that a child will have schizophrenia.
However, they only increase the likelihood of OCD, but this is not a direct causal relationship. For example, even if both parents are diagnosed with schizophrenia, there is only a 10% chance that a child will have schizophrenia.
Freud spoke of the "personality triad"—pedantry, stinginess, and stubbornness—as characteristics of a person suffering from OCD. Freud's followers believed that a child's delay in the anal stage of development (difficulties with toilet training and fixation at the anal stage) may indicate that a person will develop OCD, but modern research has not tested this thesis.
Neo-Freudians said that the occurrence of OCD is associated with self-esteem - the lower a person's self-esteem, the more likely he is to develop one or another disorder, including OCD.
Behaviorists have noted that human behavior and disorders are a learned pattern.
- Education. Many experts have noted that the parents of a child who subsequently develops OCD are overly demanding and tightly control the child.
 In such families, a ban is imposed on emotions, on certain behavior.
In such families, a ban is imposed on emotions, on certain behavior.
The future development of OCD can also be influenced by the perfectionism of parents, when a child cannot make a mistake, when it is considered a catastrophe, as well as ambivalent, opposite in meaning messages - when one behavior can be praised today, and scolded tomorrow. However, this style of parenting can cause various disorders.
OCD is a set of factors that coincided in a certain period of a person's life. These factors can provoke any retraumatization, re-injury.
If a person had a psychological trauma in childhood, for example, a child was abused, then any difficult event in his life, any crisis situation can start the disorder again. Something happens and OCD symptoms get worse.
When and how is OCD diagnosed?
First of all, you don't need to diagnose yourself, only a specialist can do it!
We very often have to not confirm the diagnosis, but to support the person with the words: “Wait, you are going through a difficult period in your life, suffering is normal! This is not about a diagnosis, it is objectively difficult! And the person is surprised: “Wow! I thought I was sick!"
Spot diagnosis is important!
We can call a person prone to obsession, but not diagnose him with obsessive-compulsive disorder. And the next question is whether such a condition will become pathological, whether it will acquire clinical manifestations.
And the next question is whether such a condition will become pathological, whether it will acquire clinical manifestations.
According to the Diagnostic and Statistical Manual of Mental Illnesses (DSM), we give OCD when a person's compulsive behavior takes more than an hour a day. If less than an hour, then you need to understand whether a person is prone to obsessions by nature or is this a specific disorder.
Unfortunately, in the treatment of obsessive-compulsive disorder, people often use non-scientific methods (esotericism, energy coaching), although medicine should work here.
Diagnosis must be carried out by a doctor!
With disorders and suspected disorders, it is very important to consult a doctor - a psychiatrist or psychotherapist. Only he can make a diagnosis. For example, I, as a clinical psychologist, cannot make a diagnosis. I can only notice that something is wrong and immediately refer my patient for a consultation with a doctor.
Why is OCD dangerous?
Any anxiety disorder can so exhaust a person that he may have suicidal thoughts. If a person cannot cope with emotions, does not see the prospect, depression can join OCD when a person does not leave the house or washes his hands until they bleed. This is a very pronounced degree of pathology, when a person needs help, and the sooner she comes, the less the risk of suicide will be.
Is it possible to get rid of OCD?
OCD is a chronic disease. However, the skills acquired during psychotherapy remain with the person forever. The task of the patient is not to avoid "kickbacks", but to learn how to use these skills and quickly return to normal.
Cognitive Behavioral Therapy shows 50-80% effectiveness in the treatment of OCD, and this is a very good result, recognized all over the world. In difficult situations, psychotherapy is combined with medication support, and this is also a very important point, since anxiety disorders also have a neurobiological basis, which means that it is important to take into account the nuances of the work of brain neurotransmitters. OCD treatment is a piece of jewelry!
OCD treatment is a piece of jewelry!
There is no one size fits all way to help different people with OCD. What may work in terms of psychological tools with one patient may not work with another. This is a joint work with a specialist through building a trusting contact.
We often offer all sorts of behavioral experiments to prove to a person that his thoughts are dysfunctional, unrealistic, what "magical" thinking is, takes away his energy and strength, prevents him from living.
How can such an experiment be arranged?
By the time it is carried out, we have already established psychotherapeutic contact with the patient. A person trusts a specialist, he knows that he is not alone. Under such conditions, at first we can only ask the patient to imagine in his head how, for example, he touches a dirty bill and applies it to his face - such an action can cause a person to have terrible anxiety and real fear.
- Sometimes specialists write a document (commitment) that they take full responsibility, for example, for turning off the iron in the patient's house.
It seems to a person: if he can imagine the worst possible scenario (iron not turned off, fire), then he must do something to prevent it. He seems to become responsible for what he only imagines in his head. “If I can imagine it, then I am responsible for the consequences.” By concluding such a contract, the specialist seems to “take” this responsibility upon himself and removes it from the patient.
- Many behavioral experiments can be devised, and they will show a person that an action that scares him is actually not as scary as it seems.
We scale these emotions, observe how a person copes with them. At first, a person is very scared, then the emotion begins to subside, and the person realizes that this did not kill him, he did it. For some time, a person gets used to this state.
This is a step-by-step work with a clear tracking of experiences, this is learning, in the process of which a person builds a new style of response and new neural connections, which we reinforce with the help of behavioral experiments, a cognitive approach, work with thoughts.
Personal experience: "How I was treated for OCD"
What should I do if the disorder returns?
When we work with a disorder in the CBT paradigm, it is usually short-term therapy. We do not have the task of "hooking" the patient on ourselves - we believe that a person is able to cope on his own and be responsible for his health, including mental health. Therefore, regular meetings are held first, and then we increase the time interval between them, we can switch to maintenance therapy, for example, once a month or every three months.
The specialist's task is to teach the patient certain skills, train them and let them live their life that has already changed for the better.
It is important for a person with chronic anxiety disorder or any physical illness to develop the skill of self-management in order to independently understand when something is not right. In the process of therapy, we always develop an individual plan for the prevention of relapses, so if a rollback occurs, the patient knows what to do about it.
If you notice symptoms of OCD in yourself or a loved one
If a person notices that their behavior is out of the normal range, thoughts or rituals become obsessive and affect the quality of life, then it is worth contacting a specialist. It could be a psychiatrist or a psychotherapist.
Author: Anna Mikhailova.
The material was prepared by Prevention.Media, an educational project of the Not in vain Foundation.
Follow our news on Telegram
Author:
Katerina Reznikova,
Is there a way out of the inner prison? — Monoclair
Headings : Latest articles, Psychology
Did you find something useful here? Help us stay free, independent and free with any donation:
Donate
Magical thinking as an attempt to control reality arose in primitive times.
 Then, not knowing the laws of the objective world, people tried to protect themselves from the blows of fate with specific rituals. Surprisingly, today, in the 21st century, during the heyday of science and free access to knowledge, many still obsess over "magic rituals" in an attempt to influence the ever-changing world. What is magical thinking, why is it dangerous and what is obsessive-compulsive disorder, we understand together with practicing psychologists and leading researchers.
Then, not knowing the laws of the objective world, people tried to protect themselves from the blows of fate with specific rituals. Surprisingly, today, in the 21st century, during the heyday of science and free access to knowledge, many still obsess over "magic rituals" in an attempt to influence the ever-changing world. What is magical thinking, why is it dangerous and what is obsessive-compulsive disorder, we understand together with practicing psychologists and leading researchers. Each new century sets conditions for humanity that it was not ready for: the First and Second World Wars struck the world with their unprecedented cruelty and broke the psyche of entire generations, and the relatively stable XXI fell upon us with the daily variability of reality. Being in the so-called information society, we daily receive information flows of very different, sometimes polar content, we are forced to master new programs and techniques, regularly improve our skills in order to maintain a source of income, rethink social processes and, most importantly, come to terms with the absolute instability of everyday life.
The demands that modernity imposes on us affect a huge amount of mental resources. Meanwhile, the need for stability is still one of the basic ones for us. Reality is accelerating, and in these difficult conditions, more and more people resort to the so-called "magical thinking". Its essence lies in the fact that a person begins to think that his thoughts, actions or words have a certain impact on the reality around him.
It is worth noting that Ivan Petrovich Pavlov, who studied the human tendency to try to program the surrounding reality, was also engaged in the study of this phenomenon.
As modern experts note, such a habit can develop into addiction, and in this case, the person will explain all his victories and defeats by the fact that he “was rude to someone in public transport”, “didn’t borrow money for a friend”, “didn’t listen to the annoying him a comrade”, etc. Variants of "magical actions" are deeply individual and diverse.
In addition, according to Doctor of Sociology V. S. Svechnikov and the competitor of the Department of Cultural Studies of the SSTU L.N. Chevtaeva, myths about magic are firmly rooted in the collective unconscious. They note:
S. Svechnikov and the competitor of the Department of Cultural Studies of the SSTU L.N. Chevtaeva, myths about magic are firmly rooted in the collective unconscious. They note:
Sane citizens of Russia, businessmen, politicians, doctors, scientists understand that any mysterious phenomena are always of interest to the masses and are the basis for various kinds of speculation.
This was especially noticeable in the 90s. In a period of absolute instability, people with particular zeal turned to all kinds of magicians, fortune-tellers and psychics. During this time, and later in the 2000s. television, radio and other media supported the interest of the masses in everything “mysterious”: A. Kashpirovsky’s programs, shows with psychics, calls to the studio to “magicians” who “resolved” any problems at a distance were especially popular - from husband’s alcoholism to serious diseases.
In this regard, the Russian Academy of Sciences even created a special Commission to combat pseudoscience and falsification of scientific research.
At the same time, it is interesting that many understand the illogicality of "magical thinking" and speak out against such a method of controlling reality. However, a study conducted in the UK by psychologist E. Subbotsky showed the opposite. One of the experiments is described as follows:
Adult subjects were asked to imagine their future life. After that, they were told that a) a magic spell cast on their future life would change this life for better or worse (mythical suggestion), and b) changing the numbers on the computer screen would change their future life for better or worse (ordinary suggestion). All subjects denied that changing the numbers on the computer screen could affect their future lives, but in their actions they demonstrated their belief in this possibility.
Thus, it can be said that mentally healthy people are aware of the absurdity of "magic spells", however, an irrational grain deeply embedded in the unconscious, in some cases associated with childhood trauma, as well as with culture (tales, myths, tales, sayings and local superstitions) prevents them from thinking rationally and greatly increases anxiety levels.
This is precisely what "magical thinking" is dangerous for. Getting the illusion of control over the world, a person begins to strive for "absolute omnipotence" and tries to program the uncontrollable. In cases where his actions coincide with obtaining the expected result, he increasingly believes that he has found a "magic way" to control the environment. Otherwise, he blames himself for supposedly “wrong” thoughts or actions.
The habit of thinking "magically" is fraught with the fact that seemingly harmless actions quickly progress into a real mental illness - obsessive-compulsive disorder (hereinafter - OCD), bringing severe, sometimes unbearable suffering to a person.
OCD is an obsessive condition characterized by obsessions and compulsions, where an obsession is a persistent, highly frightening or unpleasant thought that comes into the mind of the patient against his will, and a compulsion is a special, deeply individual ritual that helps to temporarily get rid of obsessive thoughts.
Thus, the consciousness of a person with varying degrees of frequency is visited by phobic, sometimes disgusting, thoughts unusual for the individual. Among the most common are the fear of contracting a dangerous, incurable disease, catching a virus, failing at work or school, losing a loved one, etc. Sometimes the patient is faced with nasty and unusual images of violence, cruelty, sexual perversion, intentions to cause someone moral or physical harm.
Thoughts that have nothing to do with the patient's personality drive him crazy, drive him into a panic. To get rid of them, he tries to perform absurd rituals invented by him. The most frequent ones are constant washing of hands, avoiding stepping on certain steps of stairs, arranging books and other objects in the “right” order, etc. Rituals can be very different. For example, some people are afraid to repost or like on social media simply because they think “something bad” might happen.
Psychologist-consultant A. V. Duhareva notices:
V. Duhareva notices:
A person believes that the repetition of certain actions can protect him from the vicissitudes of fate. Often from such clients you can hear phrases like: “if I do everything right, then nothing will happen”, “the main thing is to turn off the light with the right / good thought”, “if I made a mistake in the sequence of actions, then it is important to start all over again”, etc. P.
OCD usually occurs for a variety of reasons. This can be both a consequence of a passion for magical thinking, and childhood trauma, stress, moral and physical exhaustion, heavy workload at work, instability in professional activities.
The danger lies in the fact that in reality there are no "magic" rituals. But sincerely believing in their power, the patient can spend hours just washing their hands, turning door handles a certain number of times, rewriting social media messages, choosing the “correct word order”, etc. The fear behind each ritual varies significantly each individual person. For example, people with anorexia may forbid themselves from saying certain words or letters for fear of gaining weight. At the same time, rituals bring only temporary relief, forcing a person to independently immerse himself in an inner prison full of unbearable suffering.
For example, people with anorexia may forbid themselves from saying certain words or letters for fear of gaining weight. At the same time, rituals bring only temporary relief, forcing a person to independently immerse himself in an inner prison full of unbearable suffering.
Interestingly, most OCD sufferers really understand the absurdity of the situation, but can't fix anything. As a rule, they hide their illness, fearing condemnation and ridicule. According to WHO, in 2013, 1 to 3% of the population suffered from OCD. However, according to experts, this figure is greatly underestimated.
It is also important that, in addition to most people who are aware of the illogicality of their actions, patients with a "psychopathic level of organization will believe that rituals really save them from fatal consequences."
The good news is that this disease is curable. The advice of psychiatrists is universal. A person should carefully monitor his condition and effort of will, try to break the chain of his own “cause and effect relationship”, trying to identify in the cause of success or failure not a sign of “correct performance of magical actions”, but a real act, to realize the level of anxiety that interferes with a full life, for example, in the form of relationship problems, an eating disorder, a stressful job, an unstable business. Psychotherapists also offer to bring rituals to the point of absurdity, that is, for example, to close and open doors until the moment when a person simply gets tired and realizes the meaninglessness of this action. Moreover, doctors recommend visualizing my fears, imagining what would happen if I “lost my job”, “gained weight”, “broke up with a toxic partner”, etc. In this case, the patient, albeit with more discomfort and high anxiety, works out alternative options that help him remove fatal scenarios from his life.
Psychotherapists also offer to bring rituals to the point of absurdity, that is, for example, to close and open doors until the moment when a person simply gets tired and realizes the meaninglessness of this action. Moreover, doctors recommend visualizing my fears, imagining what would happen if I “lost my job”, “gained weight”, “broke up with a toxic partner”, etc. In this case, the patient, albeit with more discomfort and high anxiety, works out alternative options that help him remove fatal scenarios from his life.
As a rule, patients diagnosed with obsessive-compulsive disorder undergo both drug therapy (usually with the help of antidepressants and tranquilizers) and visit a psychotherapist who not only helps to get rid of obsessive thoughts, but also tries to help the client find and neutralize reason for his anxiety. After all, everything that happens to us, be it OCD or a panic attack, is, in fact, a signal that something is going wrong in our lives. And our psyche begins to rebel, demanding a more careful attitude towards ourselves and our lives.