Age range for schizophrenia
What is Schizophrenia? | NAMI: National Alliance on Mental Illness
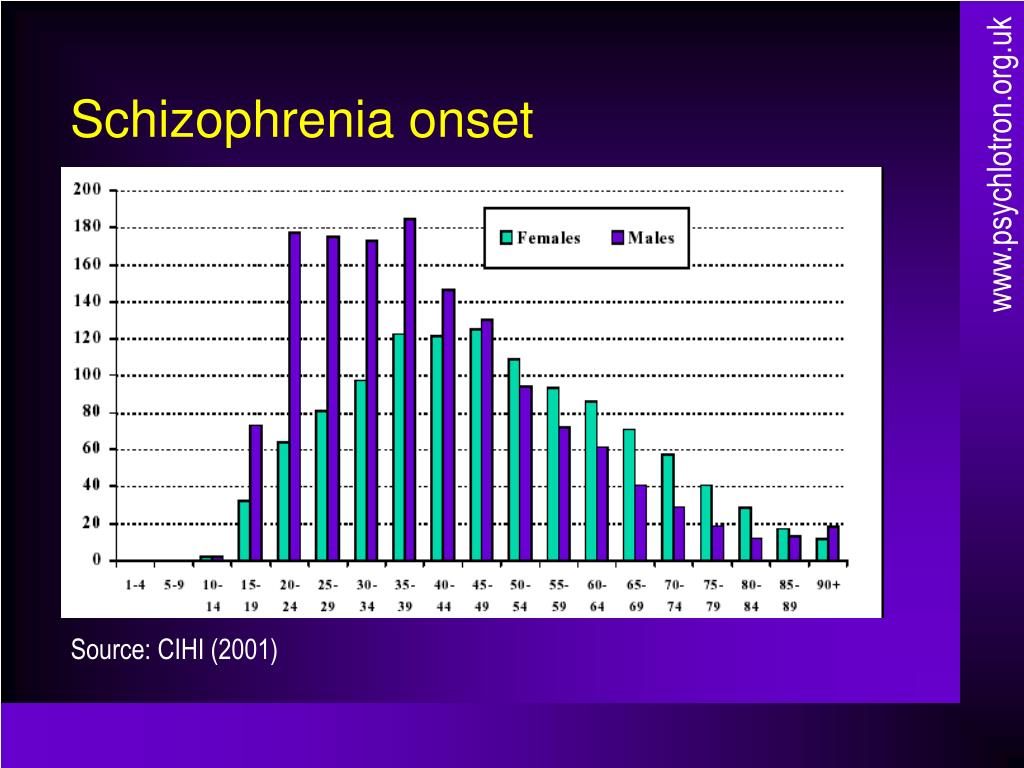
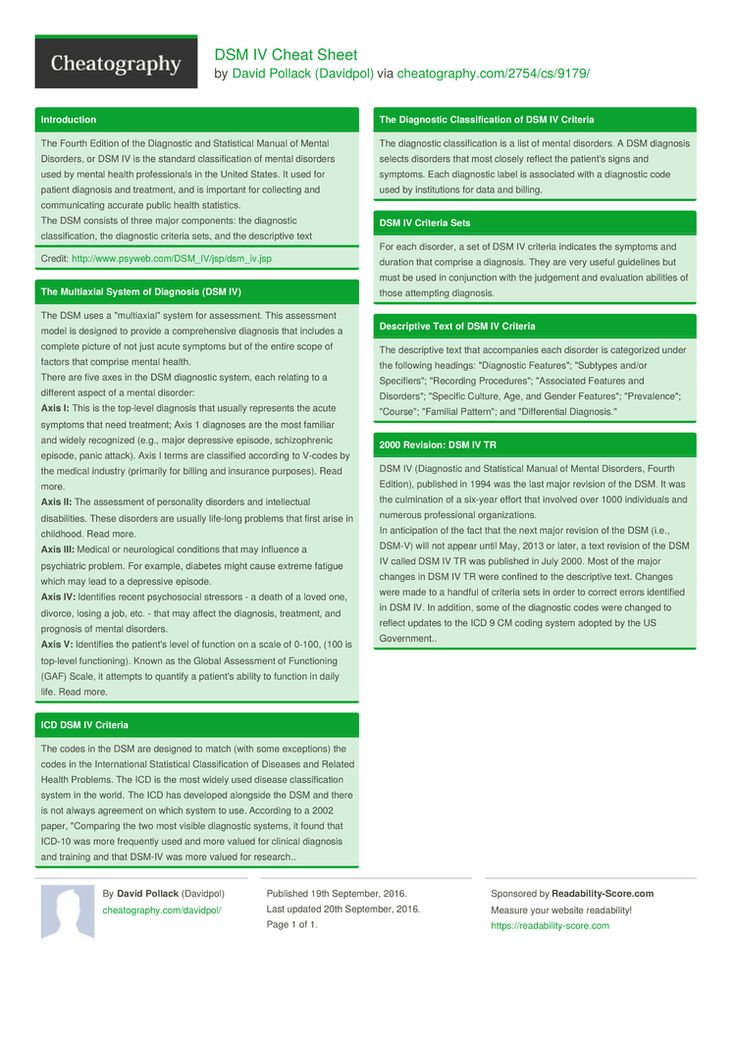
Schizophrenia is a serious mental illness that interferes with a person’s ability to think clearly, manage emotions, make decisions and relate to others. It is a complex, long-term medical illness. The exact prevalence of schizophrenia is difficult to measure, but estimates range from 0.25% to 0.64% of U.S. adults. Although schizophrenia can occur at any age, the average age of onset tends to be in the late teens to the early 20s for men, and the late 20s to early 30s for women. It is uncommon for schizophrenia to be diagnosed in a person younger than 12 or older than 40. It is possible to live well with schizophrenia.
Symptoms
It can be difficult to diagnose schizophrenia in teens. This is because the first signs can include a change of friends, a drop in grades, sleep problems, and irritability—common and nonspecific adolescent behavior. Other factors include isolating oneself and withdrawing from others, an increase in unusual thoughts and suspicions, and a family history of psychosis. In young people who develop schizophrenia, this stage of the disorder is called the "prodromal" period.
With any condition, it's essential to get a comprehensive medical evaluation in order to obtain the best diagnosis. For a diagnosis of schizophrenia, some of the following symptoms are present in the context of reduced functioning for a least 6 months:
Hallucinations. These include a person hearing voices, seeing things, or smelling things others can’t perceive. The hallucination is very real to the person experiencing it, and it may be very confusing for a loved one to witness. The voices in the hallucination can be critical or threatening. Voices may involve people that are known or unknown to the person hearing them.
Delusions. These are false beliefs that don’t change even when the person who holds them is presented with new ideas or facts.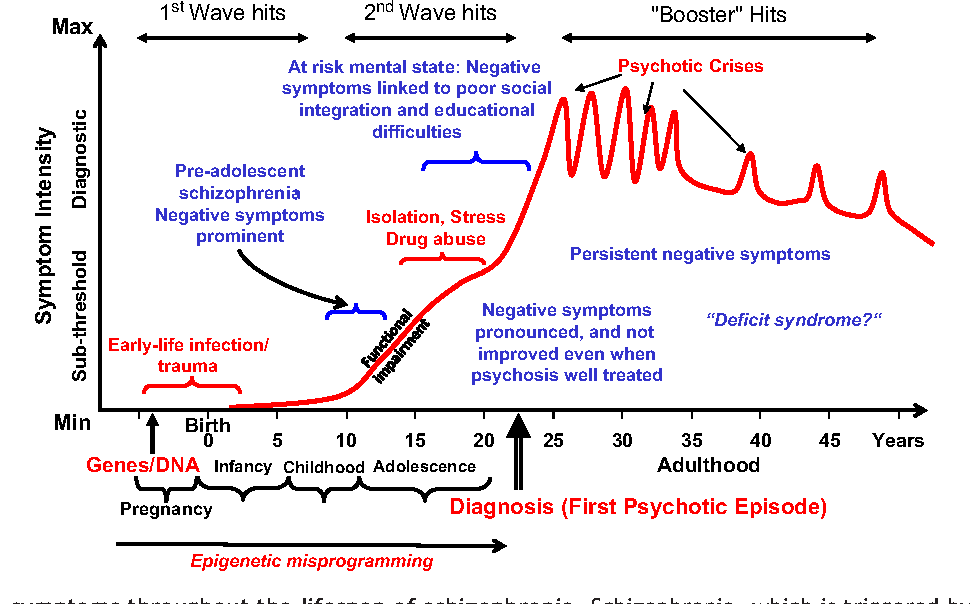 People who have delusions often also have problems concentrating, confused thinking, or the sense that their thoughts are blocked.
People who have delusions often also have problems concentrating, confused thinking, or the sense that their thoughts are blocked.
Negative symptoms are ones that diminish a person’s abilities. Negative symptoms often include being emotionally flat or speaking in a dull, disconnected way. People with the negative symptoms may be unable to start or follow through with activities, show little interest in life, or sustain relationships. Negative symptoms are sometimes confused with clinical depression.
Cognitive issues/disorganized thinking. People with the cognitive symptoms of schizophrenia often struggle to remember things, organize their thoughts or complete tasks. Commonly, people with schizophrenia have anosognosia or “lack of insight.” This means the person is unaware that he has the illness, which can make treating or working with him much more challenging.
Causes
Research suggests that schizophrenia may have several possible causes:
- Genetics.
 Schizophrenia isn’t caused by just one genetic variation, but a complex interplay of genetics and environmental influences. Heredity does play a strong role—your likelihood of developing schizophrenia is more than six times higher if you have a close relative, such as a parent or sibling, with the disorder
Schizophrenia isn’t caused by just one genetic variation, but a complex interplay of genetics and environmental influences. Heredity does play a strong role—your likelihood of developing schizophrenia is more than six times higher if you have a close relative, such as a parent or sibling, with the disorder - Environment. Exposure to viruses or malnutrition before birth, particularly in the first and second trimesters has been shown to increase the risk of schizophrenia. Recent research also suggests a relationship between autoimmune disorders and the development of psychosis.
- Brain chemistry. Problems with certain brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neurotransmitters allow brain cells to communicate with each other. Networks of neurons are likely involved as well.
- Substance use. Some studies have suggested that taking mind-altering drugs during teen years and young adulthood can increase the risk of schizophrenia.
 A growing body of evidence indicates that smoking marijuana increases the risk of psychotic incidents and the risk of ongoing psychotic experiences. The younger and more frequent the use, the greater the risk.
A growing body of evidence indicates that smoking marijuana increases the risk of psychotic incidents and the risk of ongoing psychotic experiences. The younger and more frequent the use, the greater the risk.
Diagnosis
Diagnosing schizophrenia is not easy. Sometimes using drugs, such as methamphetamines or LSD, can cause a person to have schizophrenia-like symptoms. The difficulty of diagnosing this illness is compounded by the fact that many people who are diagnosed do not believe they have it. Lack of awareness is a common symptom of people diagnosed with schizophrenia and greatly complicates treatment.
While there is no single physical or lab test that can diagnosis schizophrenia, a health care provider who evaluates the symptoms and the course of a person's illness over six months can help ensure a correct diagnosis. The health care provider must rule out other factors such as brain tumors, possible medical conditions and other psychiatric diagnoses, such as bipolar disorder.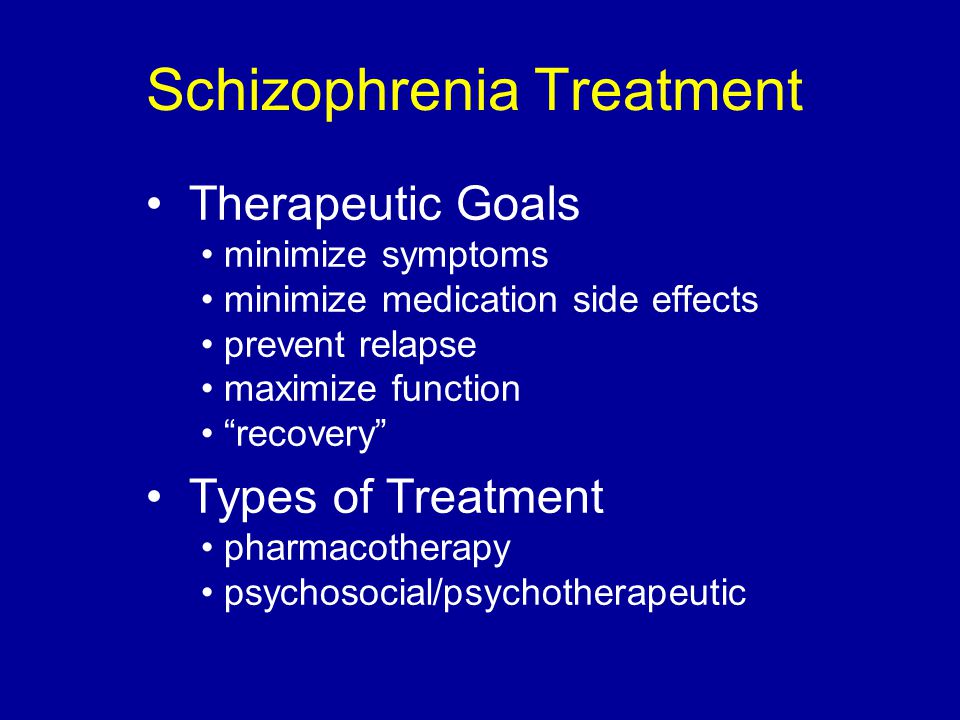
To be diagnosed with schizophrenia, a person must have two or more of the following symptoms occurring persistently in the context of reduced functioning:
- Delusions
- Hallucinations
- Disorganized speech
- Disorganized or catatonic behavior
- Negative symptoms
Delusions or hallucinations alone can often be enough to lead to a diagnosis of schizophrenia. Identifying it as early as possible greatly improves a person’s chances of managing the illness, reducing psychotic episodes, and recovering. People who receive good care during their first psychotic episode are admitted to the hospital less often, and may require less time to control symptoms than those who don’t receive immediate help. The literature on the role of medicines early in treatment is evolving, but we do know that psychotherapy is essential.
People can describe symptoms in a variety of ways. How a person describes symptoms often depends on the cultural lens she is looking through.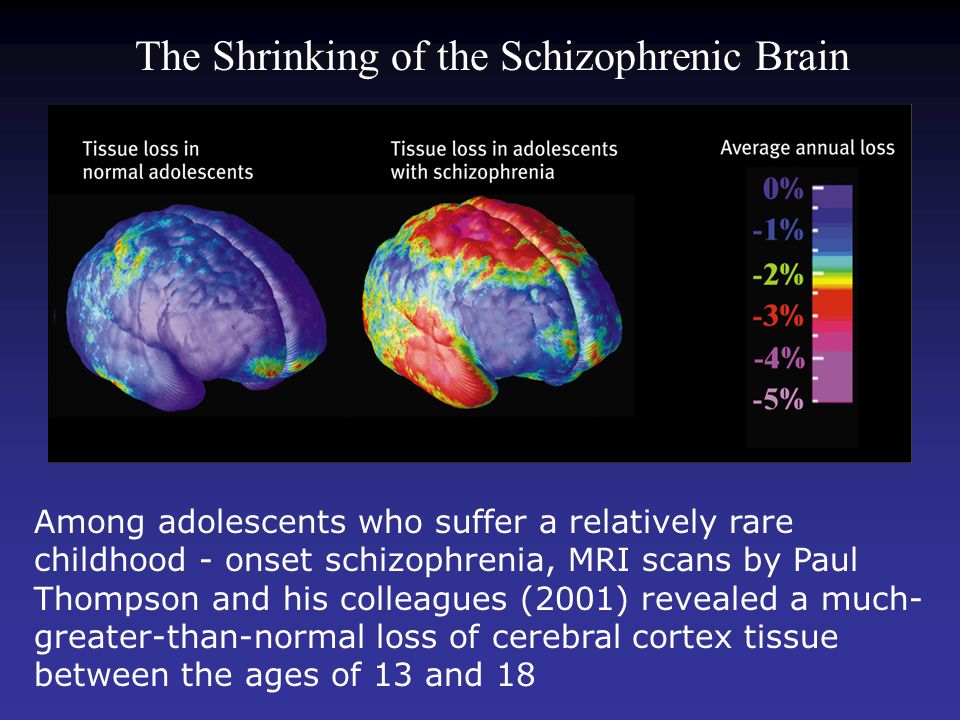 African Americans and Latinos are more likely to be misdiagnosed, potentially due to differing cultural perspectives or structural barriers. Any person who has been diagnosed with schizophrenia should try to work with a health care professional that understands his or her cultural background and shares the same expectations for treatment.
African Americans and Latinos are more likely to be misdiagnosed, potentially due to differing cultural perspectives or structural barriers. Any person who has been diagnosed with schizophrenia should try to work with a health care professional that understands his or her cultural background and shares the same expectations for treatment.
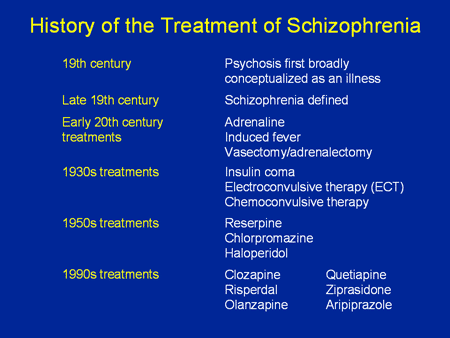
Treatment
There is no cure for schizophrenia, but it can be treated and managed in several ways.
- Antipsychotic medications
- Psychotherapy, such as cognitive behavioral therapy and assertive community treatment and supportive therapy
- Self-management strategies and education
Related Conditions
People with schizophrenia may have additional illnesses. These may include:
- Substance use disorders/ Dual Diagnosis
- Posttraumatic stress disorder (PTSD)
- Obsessive-compulsive disorder (OCD)
- Major depressive disorder
Successfully treating schizohprenia almost always improves these related illnesses.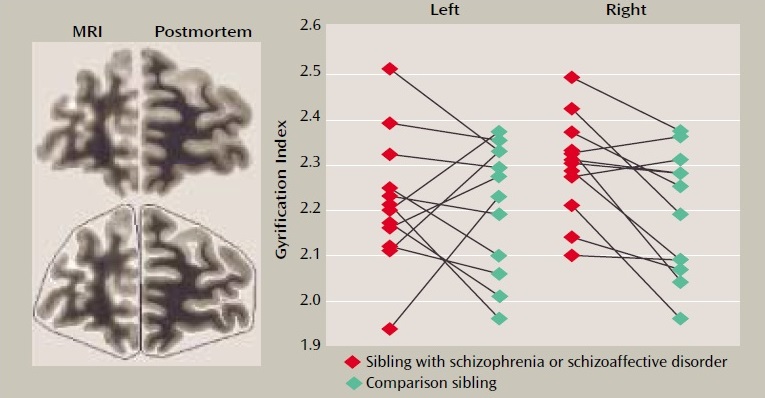 And successful treatment of substance misuse, PTSD or OCD usually improves the symptoms of schizophrenia.
And successful treatment of substance misuse, PTSD or OCD usually improves the symptoms of schizophrenia.
What is the average age of onset for schizophrenia?
Schizophrenia is a chronic mental health condition that causes psychosis, which is a disconnection from reality. Symptoms usually appear in a person’s 20s, though the average age of onset varies greatly from study to study.
One 2020 study found an average schizophrenia age of onset to be between 13.78 and 29.28 years old. Environmental, genetic, and other factors may affect the age of onset.
Additionally, the age of onset for schizophrenia may affect the condition’s course. Most studies show, for example, that people who develop schizophrenia in childhood or adolescence have more symptoms.
In addition to the onset of schizophrenia symptoms, many people with schizophrenia experience a prodrome. This is a group of mental health symptoms, such as depression, mood swings, and irritability, that may be present for months or even years before full-blown schizophrenia appears.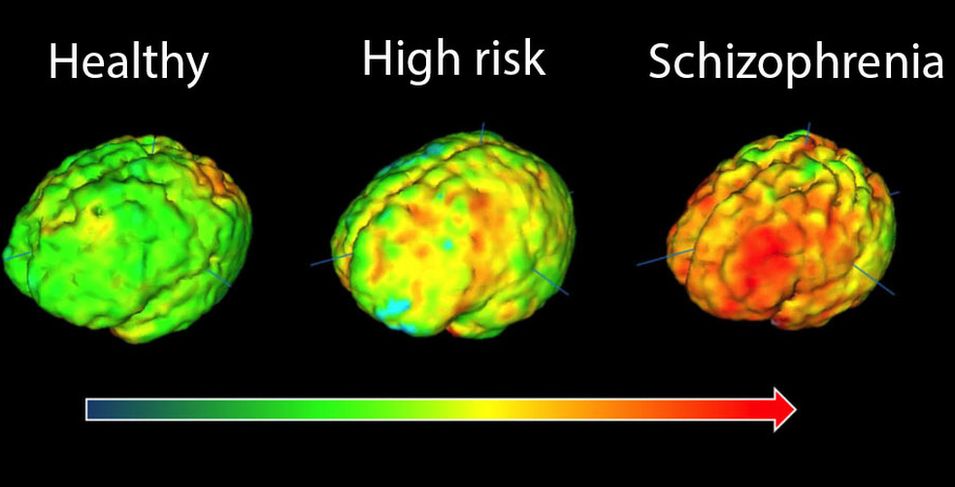
A 2014 study suggests that the schizophrenia prodrome may appear up to 9 years prior to the onset of the condition.
Knowing the average age of schizophrenia onset reveals little about whether or when an individual might develop this condition.
Keep reading to learn more about the average age of onset for schizophrenia, including early onset, late onset, and some early symptoms of the condition.
Symptoms of schizophrenia usually appear late in adolescence or early in adulthood.
However, less noticeable symptoms of schizophrenia, such as erratic moods or depression, may occur many years prior to diagnosis. Doctors call this a prodrome. Prodromal symptoms may indicate that a person has a higher risk of developing schizophrenia.
Adults of all ages may have symptoms of schizophrenia. However, it is rare for symptoms to appear for the first time after the age of 40. Schizophrenia in children under the age of 12 is rare.
The typical age of onset for schizophrenia symptoms is in the 20s, though people may develop other symptoms as early as 9 years before diagnosis.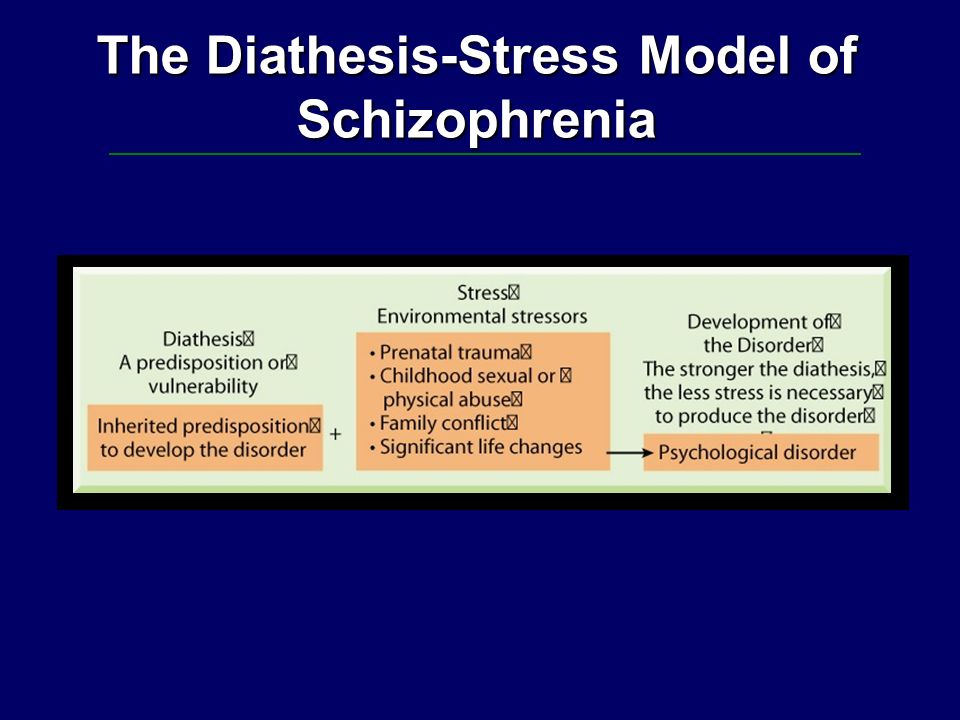 A 2020 study found the average age of onset for schizophrenia to be between 13.78 and 29.28 years.
A 2020 study found the average age of onset for schizophrenia to be between 13.78 and 29.28 years.
Early onset of schizophrenia occurs before a person’s 20s. It is very uncommon for children under the age of 12 to have symptoms of schizophrenia. Doctors call this very early-onset schizophrenia.
Early-onset schizophrenia occurs in teenagers ages 13–18. It is more common than childhood schizophrenia, but it is still fairly uncommon.
Numerous studies on early-onset schizophrenia have reached mixed conclusions about the course of the condition. However, more recent research suggests that symptoms tend to be more severe when they appear early in life.
A 2017 systematic review and meta-analysis correlated early-onset schizophrenia with:
- more hospitalizations
- more relapses
- more negative symptoms
- less social functioning
- less employment functioning
- less overall functioning
A 2014 study suggests that exposure to more environmental risk factors for schizophrenia in people with a genetic predisposition to the disease might cause symptoms to appear earlier in life.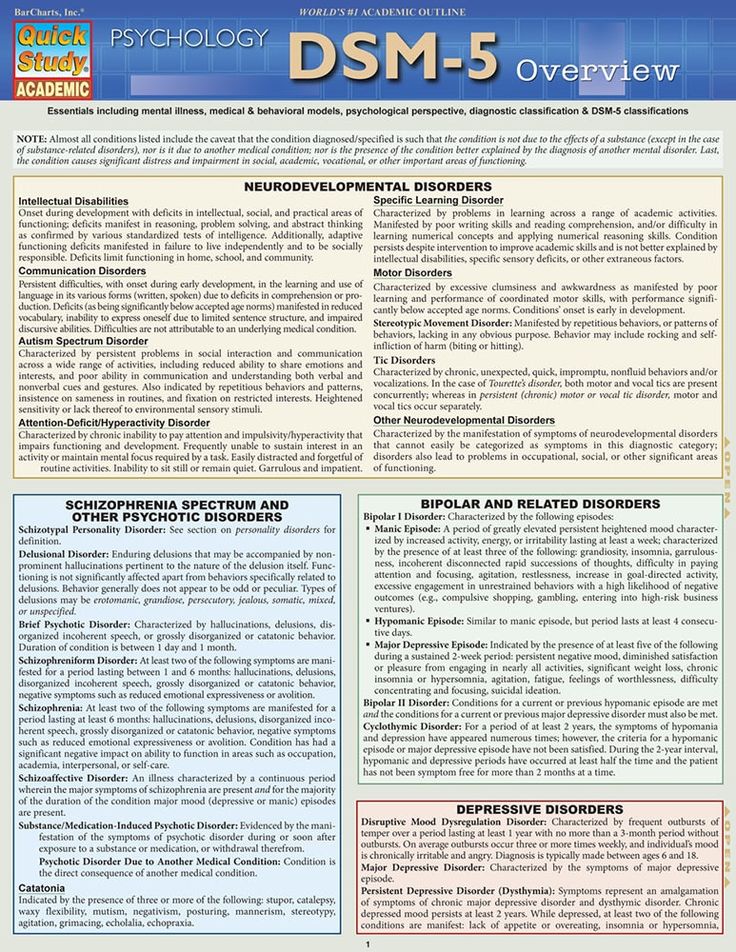
As much as 20% of people with schizophrenia develop symptoms after the age of 40, usually between the ages of 40 and 60. This is late-onset schizophrenia.
There is ongoing debate about whether this is the same disease, with the same risk factors, as schizophrenia that occurs prior to midlife or early-onset schizophrenia. A 2014 study highlights research suggesting that later onset of schizophrenia could be a unique disease subtype.
Very late-onset schizophrenia appears for the first time after age 60.
A 2018 study emphasizes the link between late-onset schizophrenia and other neurological disorders, such as dementia. People with late-onset schizophrenia are three times more likely to have dementia than their same-age peers.
Therefore, late-onset schizophrenia could be a risk factor for dementia.
Late-onset schizophrenia could also be a prodrome of other diseases. For example, it could be an early manifestation of certain types of dementia.
Schizophrenia affects a person’s ability to think clearly and to draw accurate conclusions about the world around them.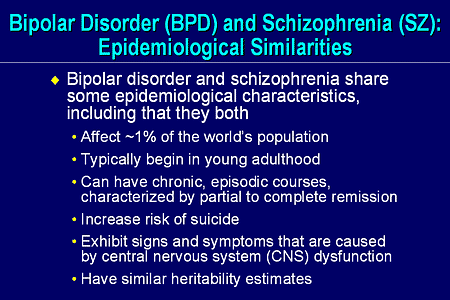 The symptoms include:
The symptoms include:
- hallucinations, or perceiving things others do not
- delusions, or thinking things that appear to be untrue
- changes in the expression of emotions
- cognitive issues
- difficulties in relationships with others
- atypical or socially unacceptable behaviors
Some, but not all, people who develop schizophrenia have other mental health symptoms before schizophrenia symptoms appear. These may include:
- depression
- anxiety
- irritability
- mood swings
- anger
- sleep difficulties
- suicidal thoughts
- obsessive and compulsive behaviors and thoughts
Learn more about the stages of schizophrenia here.
Like other mental illnesses, schizophrenia has complex biological, social, psychological, and developmental roots.
Genetics play an important role. A 2021 article reports that if both parents have schizophrenia, a person has a 40% chance of developing the condition.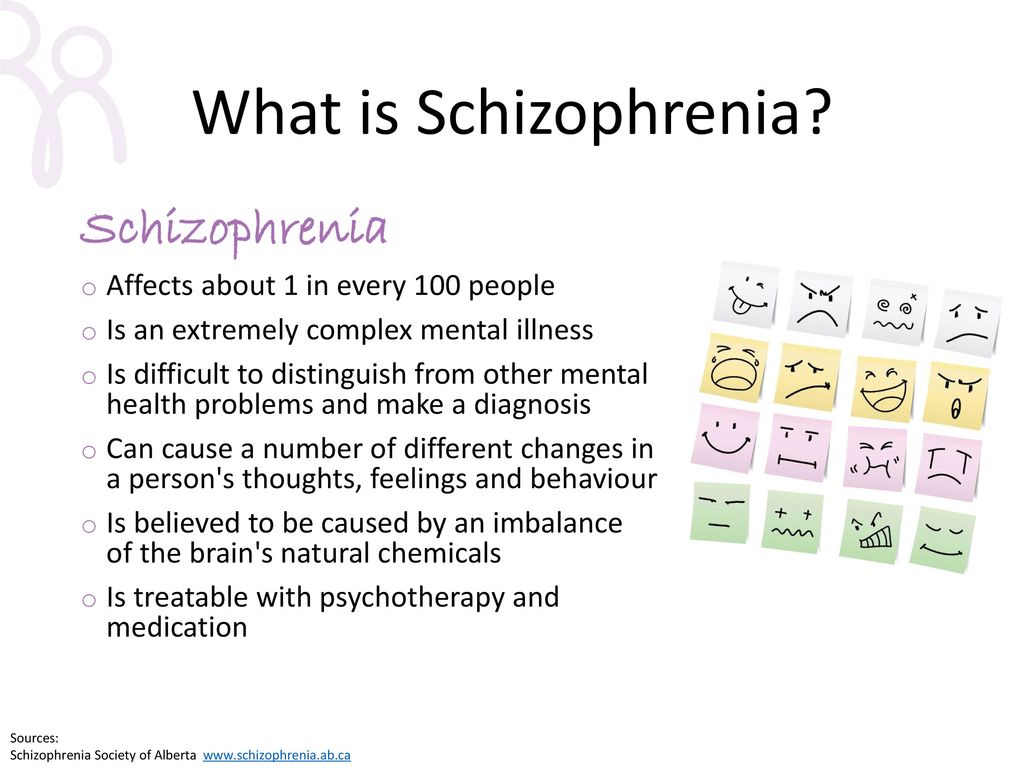 When one identical twin has schizophrenia, their twin also has the condition in 46% of cases.
When one identical twin has schizophrenia, their twin also has the condition in 46% of cases.
While a person cannot change their genes and this data points to the important role of genetics, it also shows that genes are not the only — or even necessarily, the most important — factor.
Recent research increasingly treats schizophrenia as a developmental condition, which means that factors that occur during development can increase the odds of schizophrenia, especially in people who are already at a genetically high risk.
A 2014 study found a correlation between environmental risk factors in people at a higher genetic risk for schizophrenia and the later development of schizophrenia symptoms.
Some early developmental risk factors include:
- inadequate prenatal nutrition
- infection in the gestational parent during pregnancy
- oxygen deprivation at birth
- trauma
- cannabis use
Minimizing these risk factors may reduce the risk of developing schizophrenia.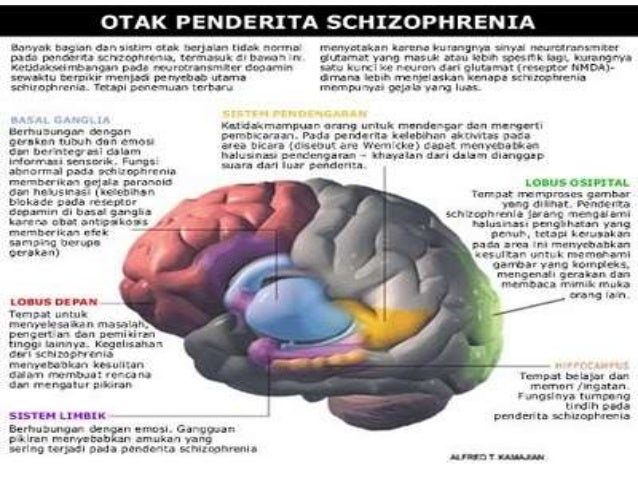 Quality prenatal care, access to healthy food and support during pregnancy, and support to ensure people only become pregnant when they are ready to care for themselves and the pregnancy may all reduce the risk of schizophrenia.
Quality prenatal care, access to healthy food and support during pregnancy, and support to ensure people only become pregnant when they are ready to care for themselves and the pregnancy may all reduce the risk of schizophrenia.
Similarly, measures that reduce the risk of childhood trauma, such as by reducing childhood poverty and supporting at-risk families, may help.
The correlation between cannabis use and schizophrenia is not clear, but people with a family history of the condition may wish to avoid cannabis, even medical cannabis.
Schizophrenia is a chronic illness that usually lasts a lifetime, though treatment can manage symptoms. Some people find full relief with treatment, while others may relapse or have to try several different treatments before getting any relief.
While the average age of schizophrenia onset can help with deciding how likely it is that a person’s symptoms stem from schizophrenia, people of any age can have schizophrenia.
Age is not a good predictor of schizophrenia risk, since many factors influence individual schizophrenia risk.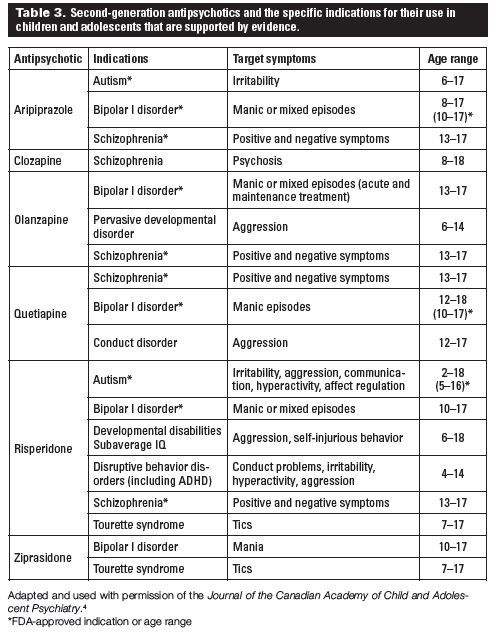 There is no age at which the risk of developing schizophrenia disappears.
There is no age at which the risk of developing schizophrenia disappears.
Many people with schizophrenia do not realize they have symptoms. This is because disconnection from reality and false beliefs are hallmarks of schizophrenia. Helping a person with schizophrenia seek treatment may be difficult.
People who think they might have schizophrenia, or whose loved ones have expressed concern, should contact a mental health professional or doctor for guidance.
FGBNU NTsPZ. ‹‹Endogenous mental illness››
Feedback form
Question about the work of the siteQuestion to a specialistQuestion to the administration of the clinic
email address
Name
Message text
The history of the development of the doctrine of late schizophrenia was analyzed in detail in the works of E. Ya. Sternberg (1969, 1972, 1983). An important role in the development of the relevant ideas was played by M. Bleuler (1943), who introduced the concept of "late schizophrenia" and defined the criteria for its diagnosis.
According to M. Bleuler, late schizophrenia includes psychoses that occur for the first time after 40 years and have clinical similarities with schizophrenia of earlier age periods. Despite age-related symptomatic features and atypical clinical picture of late schizophrenic psychoses [Klages W., 1961; Berner P., 1973; Ciompi J., Muller Ch., 1976], many researchers were adherents of M. Blueler's point of view [Gabriel E., 1978; Huber G., Gross G., Schuttler R., 1979].
A detailed study of the clinical picture and the course of late schizophrenia in the entire range of its manifestations was carried out at the Institute of Psychiatry of the USSR Academy of Medical Sciences by the staff of E. Ya. Sternberg. An important methodological aspect of the study was the use of a comparative age approach, in which the study of the clinical features of late schizophrenic psychoses was carried out in comparison with schizophrenia that manifested in earlier age periods.
In these studies, it was found that the systematics of schizophrenia, based on the allocation of the main forms of the course, is also adequate for late schizophrenia.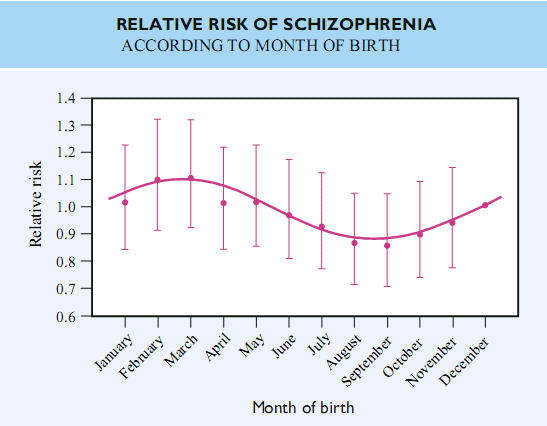 At the same time, significant features of morphogenesis were noted, reflecting the influence of late age on the course of schizophrenia. It has been established that at a later age there is a "blurring" of the clarity of the boundaries of individual forms of the course of schizophrenia, and within each of them the range of clinical variants is significantly reduced. So, among the continuously flowing schizophrenic psychoses, paranoid processes dominate, characterized by an average degree of progression. At the same time, among the continuous forms of schizophrenia, there are practically no variants of a low-progressive course, the clinical picture of which is determined by neurosis-like and psychopathic-like syndromes. Malignant processes are also relatively rare.
At the same time, significant features of morphogenesis were noted, reflecting the influence of late age on the course of schizophrenia. It has been established that at a later age there is a "blurring" of the clarity of the boundaries of individual forms of the course of schizophrenia, and within each of them the range of clinical variants is significantly reduced. So, among the continuously flowing schizophrenic psychoses, paranoid processes dominate, characterized by an average degree of progression. At the same time, among the continuous forms of schizophrenia, there are practically no variants of a low-progressive course, the clinical picture of which is determined by neurosis-like and psychopathic-like syndromes. Malignant processes are also relatively rare.
The range of psychopathological syndromes in late continuous schizophrenia is also limited. Here, 3 types of mental disorders prevail: delusions, hallucinations and phenomena of the syndrome of mental automatism. The dynamics of the late continuous process generally corresponds to the patterns of development of classical paranoid schizophrenia. However, at each stage of the development of the paranoid process, a certain incompleteness and limited development of the most typical syndromes for schizophrenia are revealed. For example, the paranoid delusions of persecution, which first appeared at a later age, are characterized by a small scale and specificity of the delusional plot. Often it takes the form of delusions of poisoning, accompanied by olfactory and gustatory hallucinations, as well as delusional interpretations of somatic disorders. The theme of “damage” that appeared in these cases is usually included in the general plot of persecution as a “special form of hooliganism” on the part of neighbors and is not the nonsense of theft that occurs in senile organic processes. The hallucinatory-paranoid stage of the course of late continuous schizophrenia is also characterized by a relatively small scale and specificity of the delirium plot. In these cases, along with verbal hallucinations, olfactory and tactile hallucinations are usually observed.
However, at each stage of the development of the paranoid process, a certain incompleteness and limited development of the most typical syndromes for schizophrenia are revealed. For example, the paranoid delusions of persecution, which first appeared at a later age, are characterized by a small scale and specificity of the delusional plot. Often it takes the form of delusions of poisoning, accompanied by olfactory and gustatory hallucinations, as well as delusional interpretations of somatic disorders. The theme of “damage” that appeared in these cases is usually included in the general plot of persecution as a “special form of hooliganism” on the part of neighbors and is not the nonsense of theft that occurs in senile organic processes. The hallucinatory-paranoid stage of the course of late continuous schizophrenia is also characterized by a relatively small scale and specificity of the delirium plot. In these cases, along with verbal hallucinations, olfactory and tactile hallucinations are usually observed.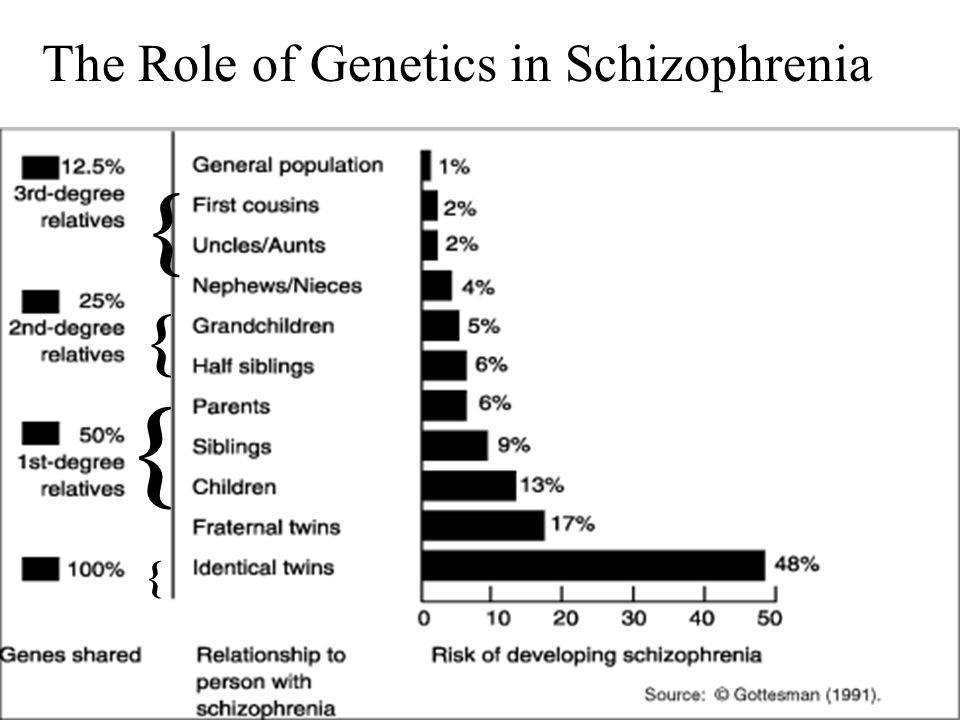 The emerging syndrome of mental automatism is usually reduced. The delirium of influence is fragmentary. The most pronounced and vivid are senestopathic automatisms. The structure of the developed paraphrenic syndrome is characterized by a combination of fantastic delusional ideas with themes of small-scale delusions. Negative manifestations in late schizophrenia are less profound than in earlier forms of this disease.
The emerging syndrome of mental automatism is usually reduced. The delirium of influence is fragmentary. The most pronounced and vivid are senestopathic automatisms. The structure of the developed paraphrenic syndrome is characterized by a combination of fantastic delusional ideas with themes of small-scale delusions. Negative manifestations in late schizophrenia are less profound than in earlier forms of this disease.
Late paroxysmal schizophrenia also undergoes age-related modification. In these cases, there is a general narrowing of the range of clinical manifestations, the frequency of forms that are transitional between recurrent and paroxysmal-progressive schizophrenia increases. As the age of manifestation increases, the difficulties of distinguishing between these forms of schizophrenia increase, so there is a point of view that it is not advisable to separate these forms of the course at a later age, and they should be considered together under the name "late paroxysmal schizophrenia".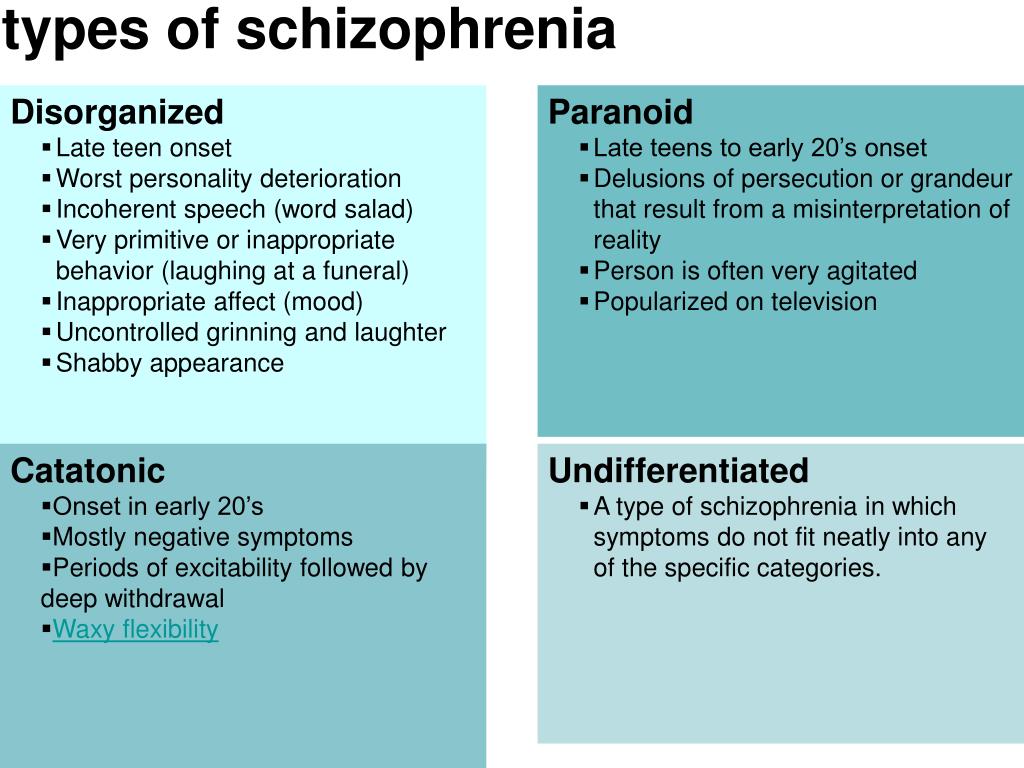
In most cases, the general structure of the resulting seizures corresponds to the structure of seizures of an earlier age period. The peculiarity consists only in the absence of seizures with oneiroid and catatonic disorders among the conditions that first appeared at a late age. An analysis of the psychopathological structure of seizures showed that they basically gravitate towards two main psychopathological poles, in one approaching schizoaffective psychoses (characteristic of recurrent schizophrenia), in the other - to attacks of a paranoid structure (typical of paroxysmal progredient schizophrenia). Naturally, a significant part of the seizures occupies, as it were, a transitional position in this general psychopathological continuum.
Among the attacks approaching the manifestations of recurrent schizophrenia, there are atypical affective states, affective-delusional and affective-hallucinatory syndromes. The severity, duration and frequency of these attacks are different. Attacks that develop with manic affect are shorter and more clearly defined, while depressive ones are more protracted, often showing a tendency to a chronic course. There is also a continuous (non-remission) course of atypical affective syndromes.
Attacks that develop with manic affect are shorter and more clearly defined, while depressive ones are more protracted, often showing a tendency to a chronic course. There is also a continuous (non-remission) course of atypical affective syndromes.
In affective-delusional attacks such as delusional depression or delusional mania, the degree of age-related change in symptoms is largely related to the severity of the manifestation of psychosis. So, in acute depressive-paranoid and acute manic-paraphrenic attacks, the influence of age on the symptoms of manifestations is minimal. Meanwhile, with prolonged delusional depressions and manias, both the affective manifestations of psychosis are subject to age-related influence (anxiety and a gloomy monotonous affect predominate in depressions, an angry-irritable or complacently euphoric affect predominates in manias), and the content of delusional disorders (themes of damage and sabotage against people from the immediate environment, hypochondriacal ideas, a combination of erotic and persecutory delusions).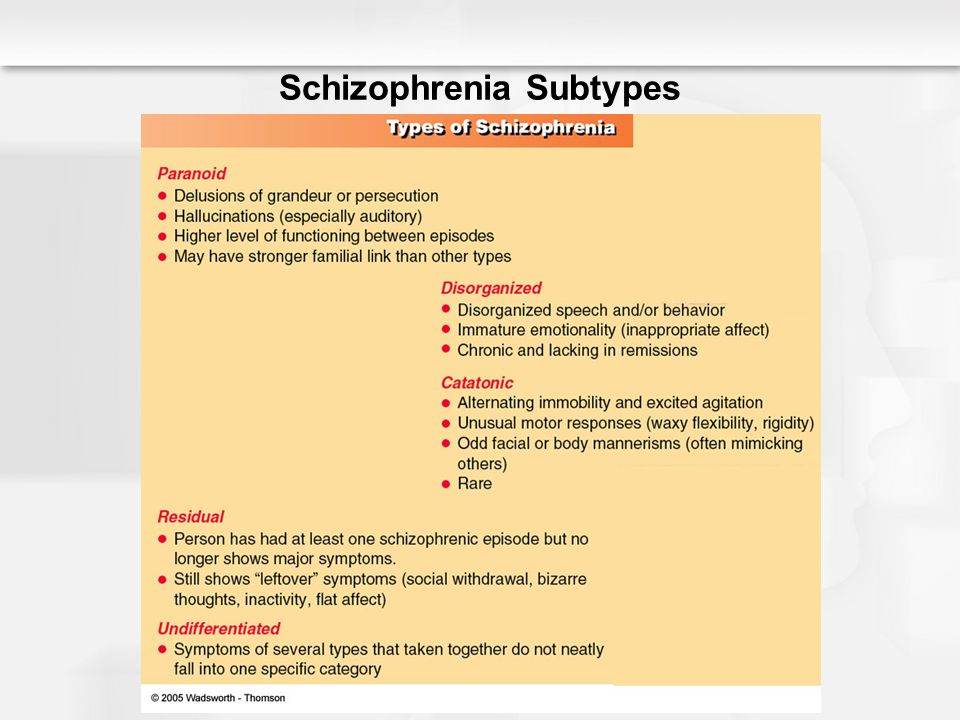
In other cases, attacks of late schizophrenia, similar in manifestation to paranoid schizophrenia, include such varieties of psychosis as paranoid states, hallucinosis, paranoid and paraphrenic states. The symptomatology of these psychoses generally corresponds to the successive stages of paranoid schizophrenia. However, as the age of manifestation increases, their clinical picture becomes more and more atypical. In delusional disorders, the so-called age-related theme dominates (various variants of delusions of material and moral damage, erotic delusions, and delusions of jealousy). Hallucinatory disorders quite often approach confabulations. In the clinical picture of the syndrome of mental automatism, predominantly senestopathic automatisms appear. Such psychoses sometimes develop in the form of short acute attacks. However, seizures are more often characterized by a protracted course.
Late-manifesting attacks of schizophrenic psychoses are characterized by a relatively small progression. In remissions with high constancy, residual delusional and hallucinatory disorders are observed, as well as a persistently changed affective background in the form of shallow subdepression or hypomania. Negative personality changes usually increase slowly in the form of autistic tendencies, emotional decline and intensification of psychopathic disorders that were characteristic of patients even before the manifestation of the disease (features of rigidity, conflict, self-will, eccentricity).
In remissions with high constancy, residual delusional and hallucinatory disorders are observed, as well as a persistently changed affective background in the form of shallow subdepression or hypomania. Negative personality changes usually increase slowly in the form of autistic tendencies, emotional decline and intensification of psychopathic disorders that were characteristic of patients even before the manifestation of the disease (features of rigidity, conflict, self-will, eccentricity).
Juvenile paroxysmal schizophrenia proceeding with the dominance of hallucinatory disorders in the structure of the first attack (clinical and clinical-camanestic study)
conclusions
significant heterogeneity of their picture, both in relation to the clinical and psychopathological structure, and the dynamics of the attack.
1.1. The spectrum of psychopathological disorders comorbid with the hallucinatory symptom complex that occurs during the studied manifest seizures is represented by a combination of delusional disorders with mental automatisms, affective disorders, catatonic symptoms and oneiroid inclusions in various combinations of their intensity, completeness and dynamics of manifestations.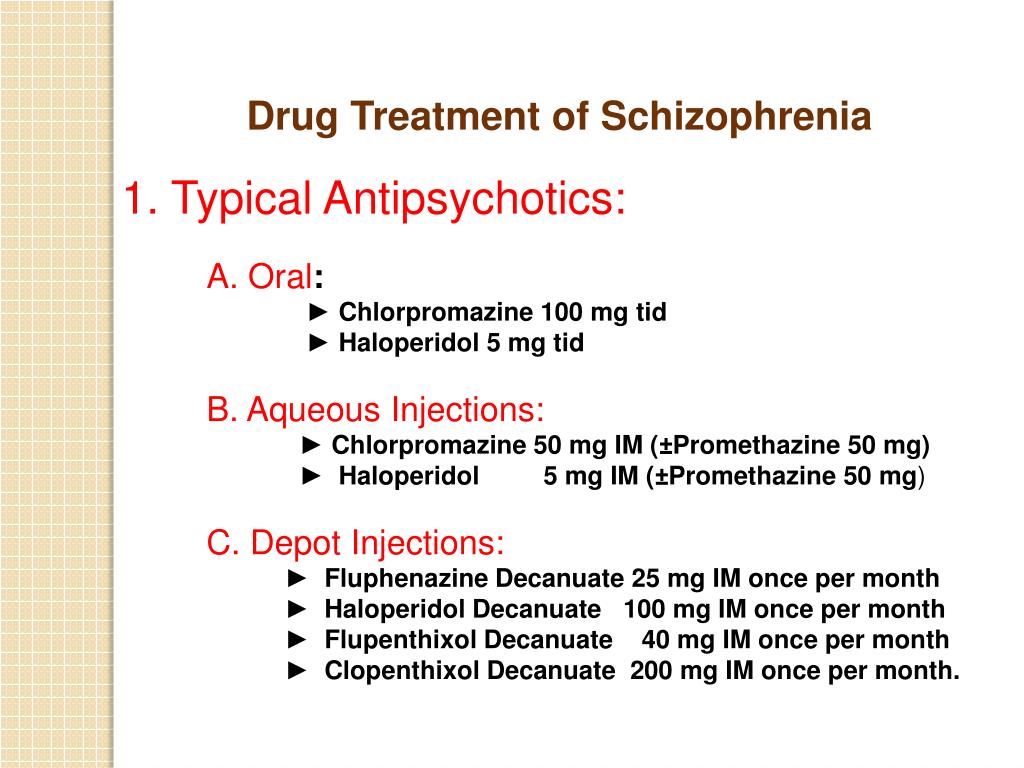
1.2. On the basis of the phenomenological approach to the analysis of the features of hallucinations in each of the studied patients in accordance with the parameters of their assessment adopted by researchers working in this field, two total patterns of their characteristics were determined: the first, reflecting the properties of sensoriality (perceptual-sensory) and the second, displaying signs thought disorders (apperceptive-intentional). The accumulation of properties of the perceptual-sensory pattern indicated a milder level of damage to mental activity, and the totality of signs of the apperceptive-intentional pattern, on the contrary, in favor of the formation of a deeper level of mental disorders.
1.3. The ratio of these phenomenological patterns, with varying degrees of severity, presented in the picture of hallucinatory disorders in the studied patients, found a clear correlation with the time of occurrence of hallucinations in them in the picture of a manifest attack: primary (primer mechanism) or secondarily (secondary mechanism of development of hallucinations).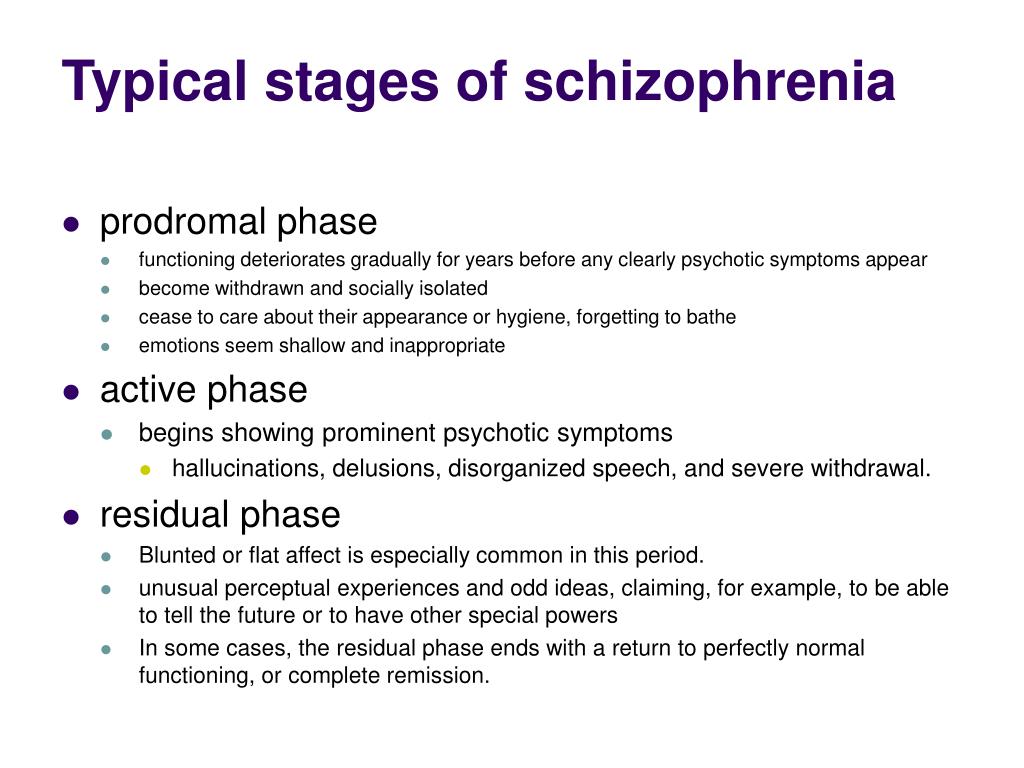
2. Based on the revealed differences in the time of occurrence of hallucinatory disorders in relation to delusional and other psychopathological symptoms in the structure of the emerging manifest attack and their phenomenological features, it turned out to be the most reasonable to distinguish two main typological clinical varieties of the first attacks of juvenile schizophrenia with the dominance of hallucinatory disorders.
2.1. The first typological variety, designated as seizures with a primer mechanism for the development of hallucinatory symptoms, included cases where hallucinatory disorders were formed primarily in relation to delusional and other psychopathological symptoms and were characterized mainly by the accumulation of the properties of an apperceptive-intentional pattern.
2.2. Within the framework of the second typological variety with a secondary mechanism for the development of hallucinatory disorders, in which the appearance of a hallucinatory symptom complex occurred at the stage of an already formed psychotic state, it was found necessary to distinguish two of its variants: one with the formation of a hallucinatory symptom complex in the structure of a delusional state, which differed in an emphasis in the representation of the properties of apperceptive - intentional pattern, and the second - with the development of hallucinations in the structure of an affective - delusional state, characterized by a distinct predominance of the properties of the perceptual - sensory pattern.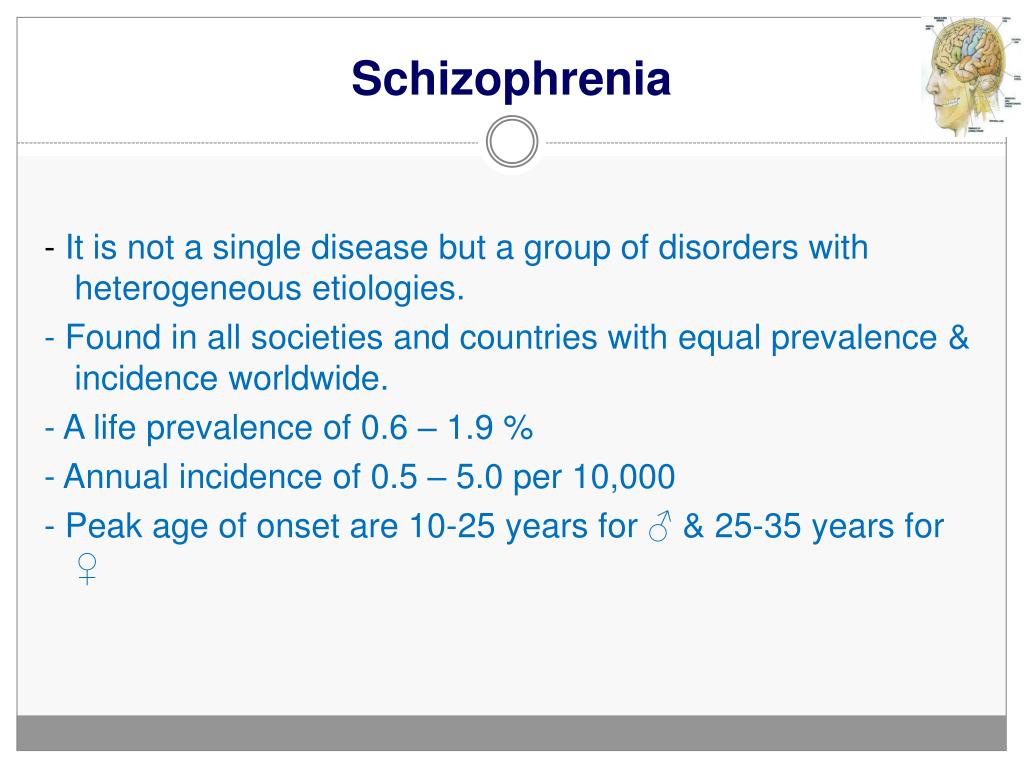
3. The analysis carried out on the basis of follow-up data regarding the features of the subsequent course of juvenile schizophrenia indicated its variability in the presence of clear differences in integrative types of outcomes, which made it possible to determine the preferred course of the disease for each of the identified types of manifest seizures.
3.1. With a typological variety with a primer mechanism for the development of a hallucinatory phenomenon, the most characteristic progredient type of the course of the disease, distinct negative personality changes, low quality of remissions at the time of catamnesis with the preservation of residual productive disorders in their structure and a distinct decrease in educational, social and labor adaptation, a relatively high level of disability .
3.2. For cases related to the typological variety of manifest seizures with a second development of hallucinations within the framework of delusional psychosis, the prevalence of the progredient type of the course of the disease, combined with a moderate degree of severity of negative personality changes, was characteristic, as well as a rather low quality of remissions (psychopathic type of remission) for catamnesis and, in general, a low level of social and labor adaptation.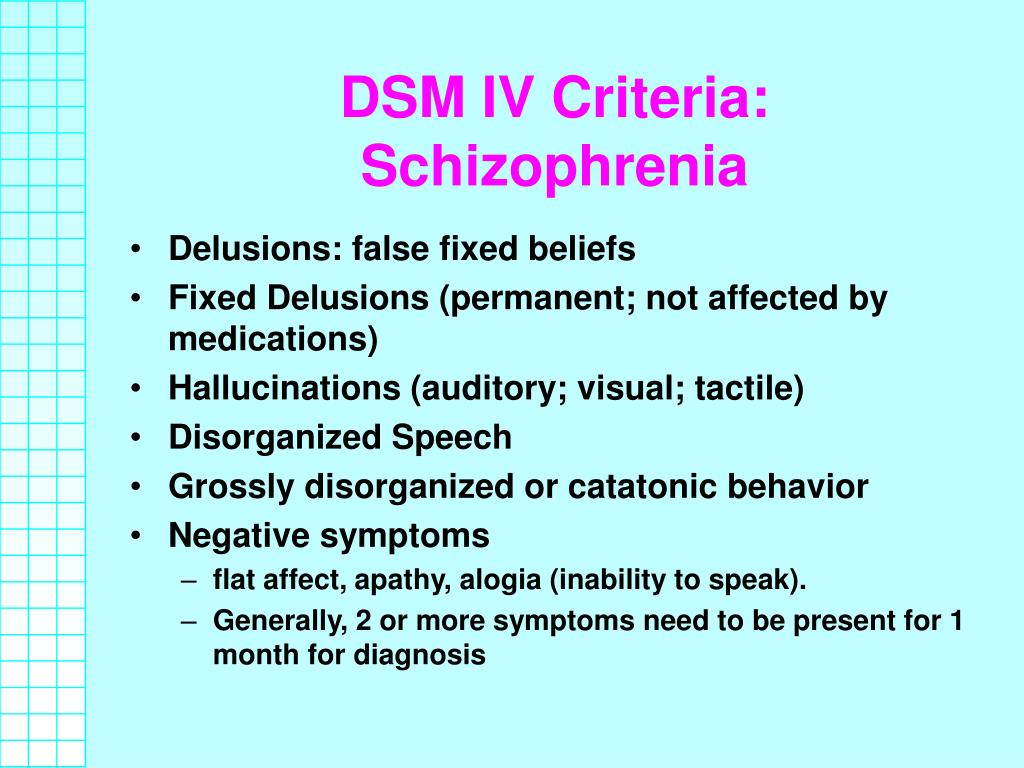
3.3. In cases with a typological variety of a manifest attack with a second development of hallucinatory disorders within the framework of affective-delusional psychosis, according to the catamnesis, the course of the disease was characterized by the predominance of the regenerative type of the course and the course of the “cliché” type; the severity of negative changes was the lowest among all groups (by the type of sthenic and asthenic schizodization), the quality of remissions was also quite high: remissions with thymopathic disorders predominated. The level of social, labor and educational adaptation to catamnesis in this group was the highest of the entire studied cohort.
4. To confirm the established data on the prognostic significance of the identified clinical varieties of the studied manifest seizures, a number of their clinical and pathogenetic characteristics were determined. The favorable parameters were: an acute onset of the disease, a personality type of sthenic and sensitive schizoids, as well as a hyperthymic warehouse; as prognostically unfavorable: the presence of an initial stage with a predominance of paranoid and negative disorders, its duration is more than 5 years, a personality warehouse, qualifying as mosaic, passive, deficient schizoids, as well as a delayed type of early dysontogenesis, an early age of onset (11–16 years) and earlier age of development of a manifest attack (16 - 19years).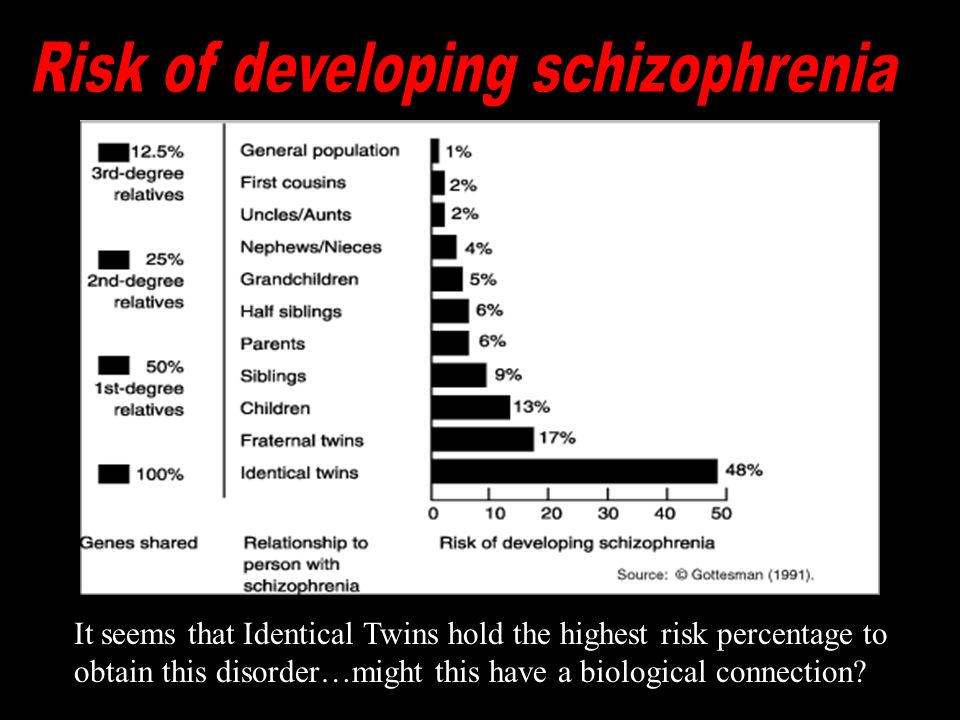
5. The data of the experimental - pathopsychological examination of patients, differing in clinical varieties of a manifest attack, confirmed the differences identified at the clinical level in the selected groups. A general deficit of social orientation and social regulation of activity and behavior, a decrease in the selectivity of cognitive processes and social perception, was established for all groups of patients. The greatest degree of decrease in cognitive functioning indicators was typical for patients with the primer mechanism of hallucinations, the least - in the group of patients with a second mechanism, with the formation of hallucinations in the structure of an affective-delusional state.
5.1. Neurophysiological examination revealed a range of characteristics of the characteristics of the profile and intensity of cognitive anomalies, demonstrating correlations with the selected clinical type of manifest seizures. In the first group, with a primer mechanism for the formation of hallucinations, cognitive impairments were most pronounced: all stages of processing significant stimuli, the processes of maintaining working memory, and evaluating the significance of information were impaired.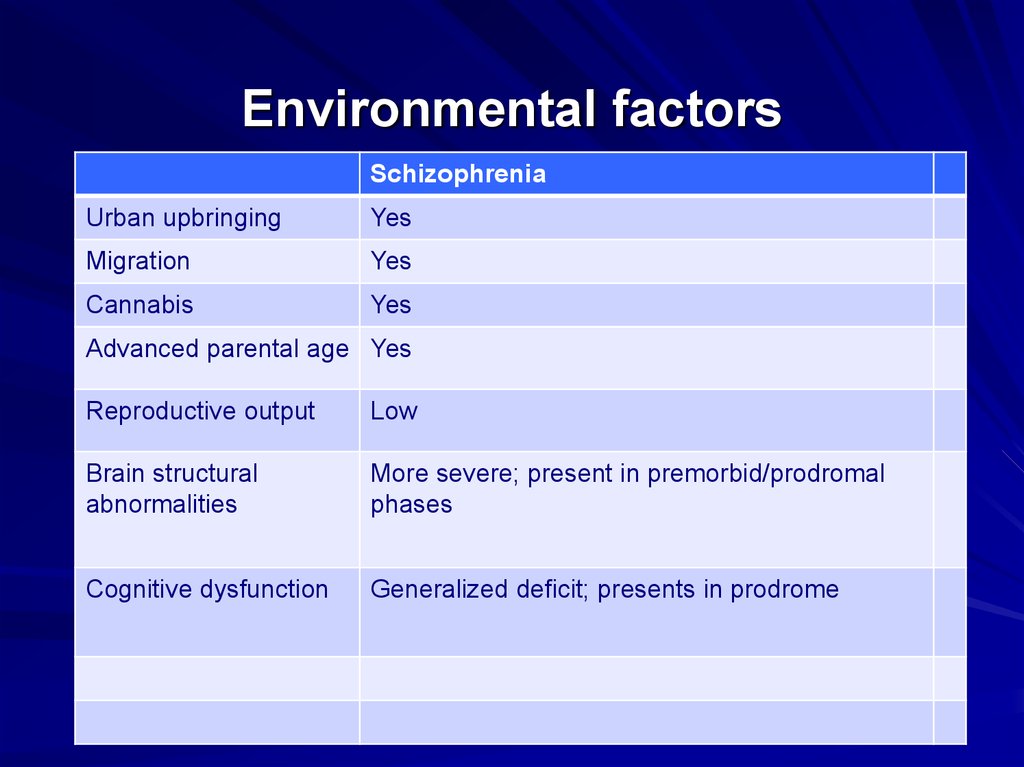 In patients with a secondary mechanism for the formation of a hallucinatory phenomenon in the structure of a delusional state, the initial stages of information processing are practically not disturbed, the focus of pathology here falls primarily on the processes associated with the classification of stimuli, the choice of a solution, and the provision of motor acts. In the group of patients where the hallucinatory phenomenon is formed in the structure of an affective-delusional state, this stage of target information processing turned out to be the most intact.
In patients with a secondary mechanism for the formation of a hallucinatory phenomenon in the structure of a delusional state, the initial stages of information processing are practically not disturbed, the focus of pathology here falls primarily on the processes associated with the classification of stimuli, the choice of a solution, and the provision of motor acts. In the group of patients where the hallucinatory phenomenon is formed in the structure of an affective-delusional state, this stage of target information processing turned out to be the most intact.
6. The provision of specialized psychopharmacological and psychotherapeutic care to the studied patients is generally implemented within the framework of the relevant section of the "Standards for the care of patients with schizophrenia" (2006). When choosing the direction and form of therapeutic action, the evaluation of the characteristics and properties of the hallucinatory phenomenon, the psychopathological spectrum of comorbid disorders, as well as the individual reactivity of patients, were decisive.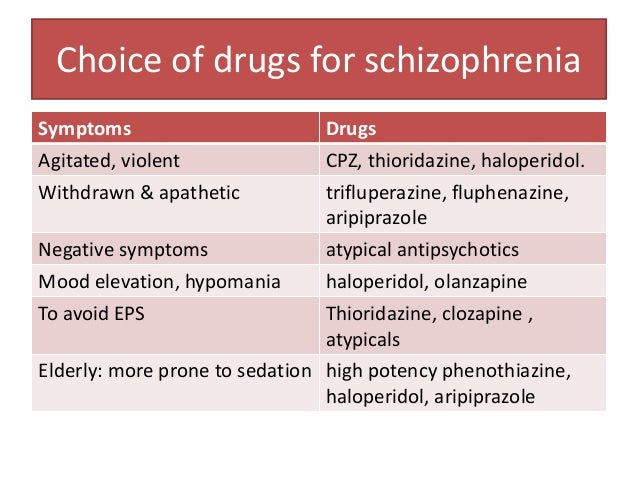 At the stage of remission formation, along with this, it was required to add methods of psychosocial and psychocorrectional assistance specially developed for adolescence, focused on the characteristics of the premorbid warehouse of patients, the degree of reduction of positive disorders, the quality of emerging negative changes and the level of compliance of adolescent patients.
At the stage of remission formation, along with this, it was required to add methods of psychosocial and psychocorrectional assistance specially developed for adolescence, focused on the characteristics of the premorbid warehouse of patients, the degree of reduction of positive disorders, the quality of emerging negative changes and the level of compliance of adolescent patients.
CONCLUSION
The relevance of this study was justified both by the persistent interest of scientists in the problem of the first psychotic episodes in schizophrenia, and by the controversial assessment of the role of the hallucinatory symptom complex that arises in their structure. Our examination of this cohort of patients with the involvement of clinical-psychopathological, phenomenological and clinical-catamnestic methods, as well as using the results of a number of paraclinical examinations (neurophysiological; experimental pathopsychological), allowed us to discuss a number of previously insufficiently covered provisions regarding the age-related features of clinical manifestations, typology and phenomenology of these conditions, features of the course of the disease and long-term outcomes, as well as to put forward a hypothesis about the prognostic role of some of the patterns we have identified.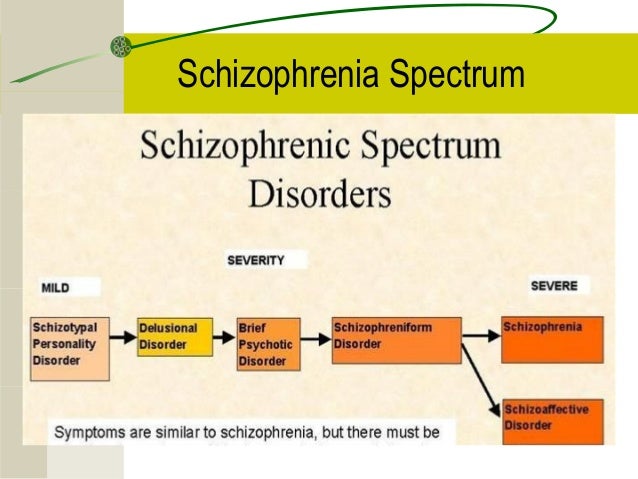
Clinical psychiatry is traditionally dominated by the view that assesses the formation of massive hallucinatory disorders in the structure of a manifest seizure as a component that reflects the participation of exogenous influence on the formation of an attack. At the same time, there is a certain amount of observations indicating the possibility of interpreting the appearance of hallucinatory disorders in a wider range, as an independent symptom complex, subject to the pathokinetic laws of an endogenous attack.
This study was conducted in a group for the study of mental illness of adolescence (Head - Prof. M.Ya. Director - Academician of the Russian Academy of Medical Sciences, Prof., Doctor of Medical Sciences A.S. Tiganov) in the period from 2005 to 2010. In total, within the framework of this study, 110 male patients were examined who were hospitalized for paroxysmal schizophrenia, manifested in adolescence by psychosis with dominance of hallucinatory disorders. All examined patients made up two groups of observations - clinical (52 patients) and follow-up (58 patients).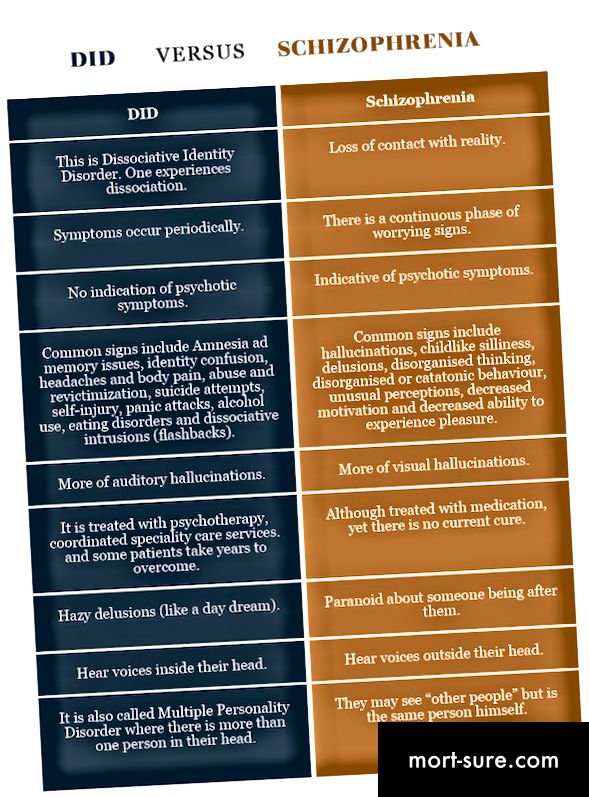 With the nosological qualification of patients at the time of initial hospitalization, they were assigned to the F20 category. The following were used as inclusion criteria: dominance of hallucinatory disorders in the structure of a manifest endogenous seizure; the onset of the disease within adolescence; the development of a manifest attack of the disease in adolescence, which, according to modern estimates, includes patients from 15 to 24 years old.
With the nosological qualification of patients at the time of initial hospitalization, they were assigned to the F20 category. The following were used as inclusion criteria: dominance of hallucinatory disorders in the structure of a manifest endogenous seizure; the onset of the disease within adolescence; the development of a manifest attack of the disease in adolescence, which, according to modern estimates, includes patients from 15 to 24 years old.
To confirm the statistical validity of the analyzed data, statistical analysis methods used for small sample sizes based on such indicators as the mean and standard deviation, in particular, the Student's method, were used. A two-tailed t-test, Pearson's x (chi-square) test for qualitative data, was used to establish the t relationship between parameters presented as alternative variables. Significance level p<0.05 was considered significant.
The clinical and follow-up groups had no differences in the distribution of patients according to the typological varieties of the first manifest seizures, the age of the patients at the time of the onset of the disease and the manifestation of psychosis, according to socio-demographic characteristics, which made it possible to extrapolate the data obtained in the process of studying follow-up cases to the entire cohort of patients.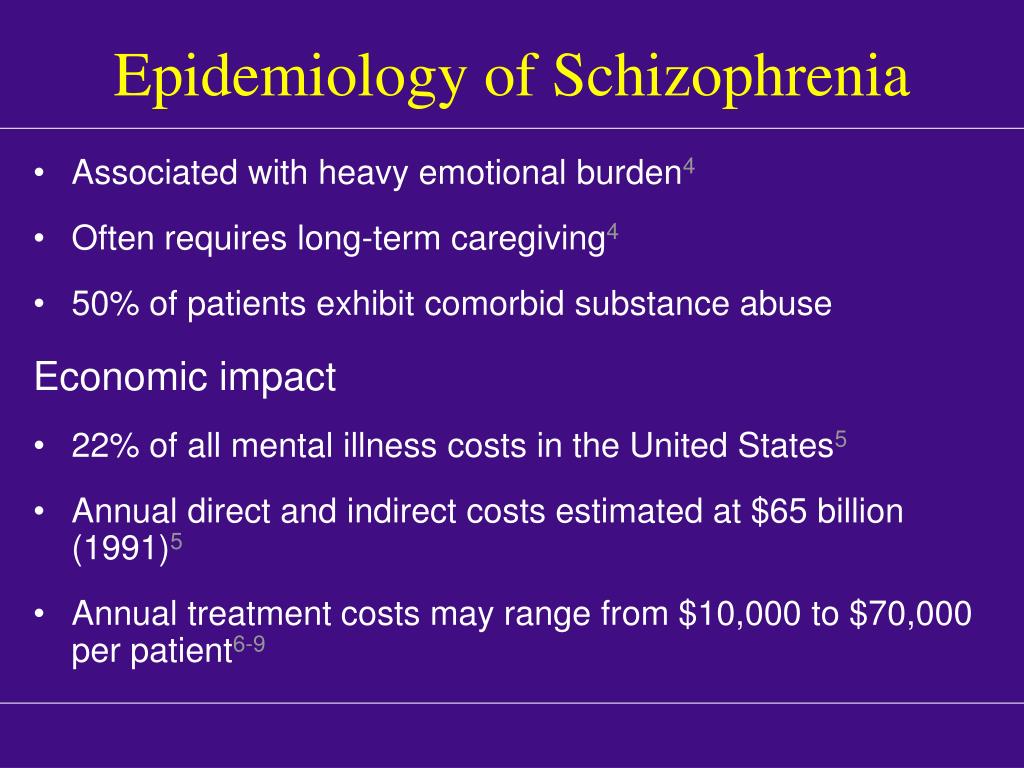
In the course of the study, data were obtained from a detailed clinical and psychopathological analysis of hallucinatory disorders in the structure of manifest attacks of juvenile schizophrenia and a number of their essential features were established, which made it possible to divide the studied cohort into typological varieties. Moreover, it turned out that in the structure of a manifest attack of juvenile schizophrenia, hallucinatory disorders showed a large polymorphism of properties and characteristics, and therefore, for their most detailed qualification, a clinical and phenomenological analysis of the structure of hallucinations was used. For this purpose, a number of qualitative characteristics of hallucinations described earlier by researchers were summarized [Rudnev V.I 19eleven; Vitke O., 1924; Zhislin S.G. 1935; Kronfeld A.S., 1936; Rybalsky M.I., 1982; Bleuler E. 1920; Schneider K. 1930; Heilburn A., Blum N. 1984, Zward & Polak 2001; Stephane M. et al., 2003], and two patterns were identified, including sensory properties or signs of impaired thinking involved in the formation of a hallucinatory phenomenon.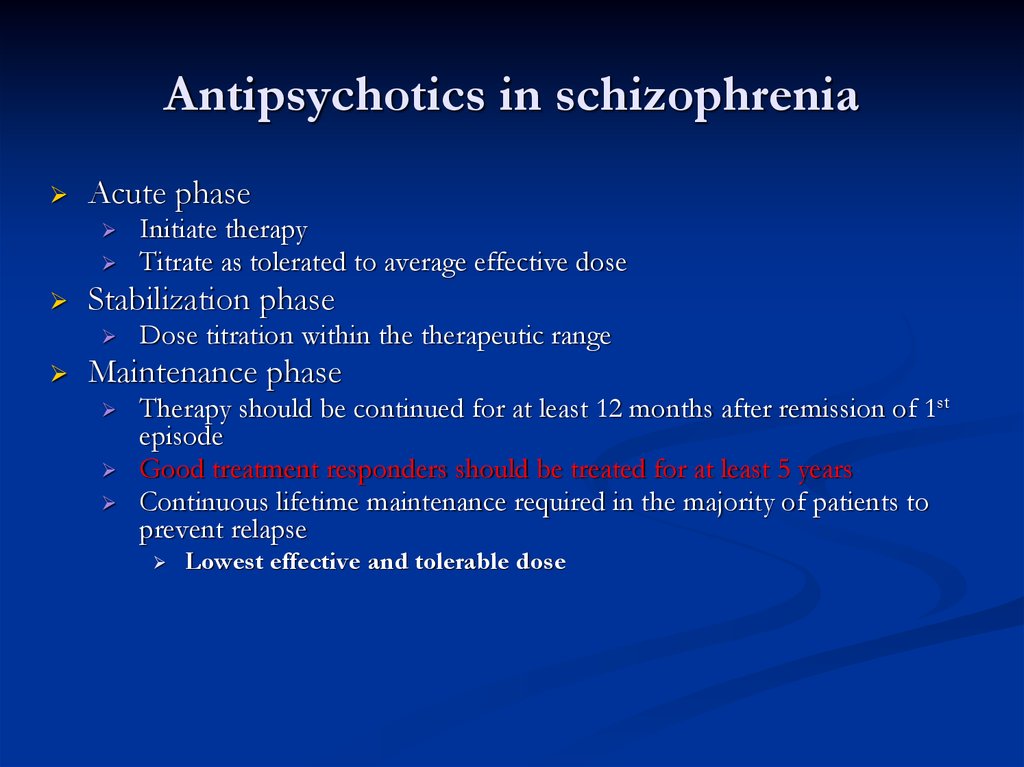 They were involved as a tool for a clearer understanding of the depth of mental disorders that occur in patients. The first - perceptually - structural pattern, included a set of phenomenological properties of hallucinations, indicating the leading role of the sensory component in the pathogenesis of hallucinations; the second, apperceptive-intentional pattern, combined features and properties that reflected the dominance of pathologically disturbed thinking in the formation of a hallucinatory phenomenon.
They were involved as a tool for a clearer understanding of the depth of mental disorders that occur in patients. The first - perceptually - structural pattern, included a set of phenomenological properties of hallucinations, indicating the leading role of the sensory component in the pathogenesis of hallucinations; the second, apperceptive-intentional pattern, combined features and properties that reflected the dominance of pathologically disturbed thinking in the formation of a hallucinatory phenomenon.
In the course of a detailed analysis of the structure of a manifest attack in the studied patients, two of their typological varieties were identified, differing in the time of onset, the nature and dynamics of hallucinatory disorders and their qualitative structure, identified on the basis of the use of the identified phenomenological patterns.
The first group of seizures included conditions in which hallucinatory disorders were formed primarily in relation to other psychopathological symptoms, and was designated as a typological variety with a primer mechanism for the development of hallucinatory symptoms.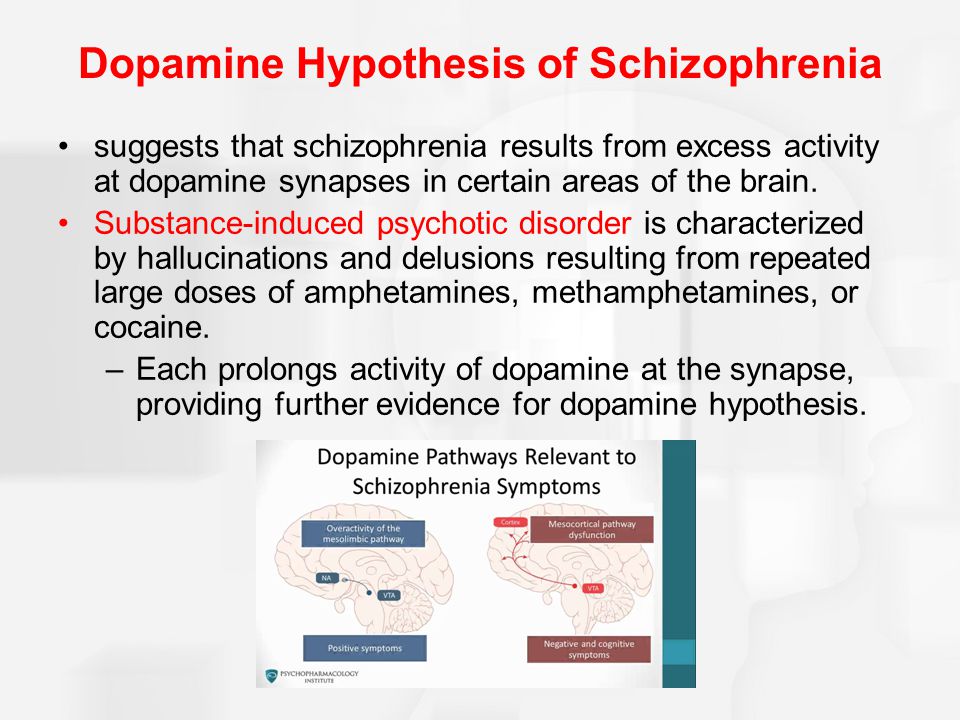 As the analysis showed, it was these cases that were characterized by those phenomenological characteristics that belonged to the second pattern of characteristics of hallucinatory disorders, i.e. reflected a deeper level of involvement of thinking. The second group - seizures, in the structure of which hallucinatory disorders arose secondarily, against the background of an emerging delusional or affective-delusional state, was designated as a typological variety with a second mechanism of their formation. Here, according to the results of the phenomenological analysis, the features of hallucinatory disorders reflected to a greater extent the properties of the perceptual-sensory pattern, which was a sign of a milder impairment of mental activity.
As the analysis showed, it was these cases that were characterized by those phenomenological characteristics that belonged to the second pattern of characteristics of hallucinatory disorders, i.e. reflected a deeper level of involvement of thinking. The second group - seizures, in the structure of which hallucinatory disorders arose secondarily, against the background of an emerging delusional or affective-delusional state, was designated as a typological variety with a second mechanism of their formation. Here, according to the results of the phenomenological analysis, the features of hallucinatory disorders reflected to a greater extent the properties of the perceptual-sensory pattern, which was a sign of a milder impairment of mental activity.
In the first typological variety (20 clinical; 21 follow-up patients), hallucinatory disorders in the picture of psychosis occurred earlier or simultaneously with delusional or other psychopathological symptoms. The onset of the attack is subacute with adynamic depression associated with a tendency to hypochondriacal apprehensions or meaningless anxiety, against which the rapid formation of hallucinatory products occurred without the delusional development of the latter.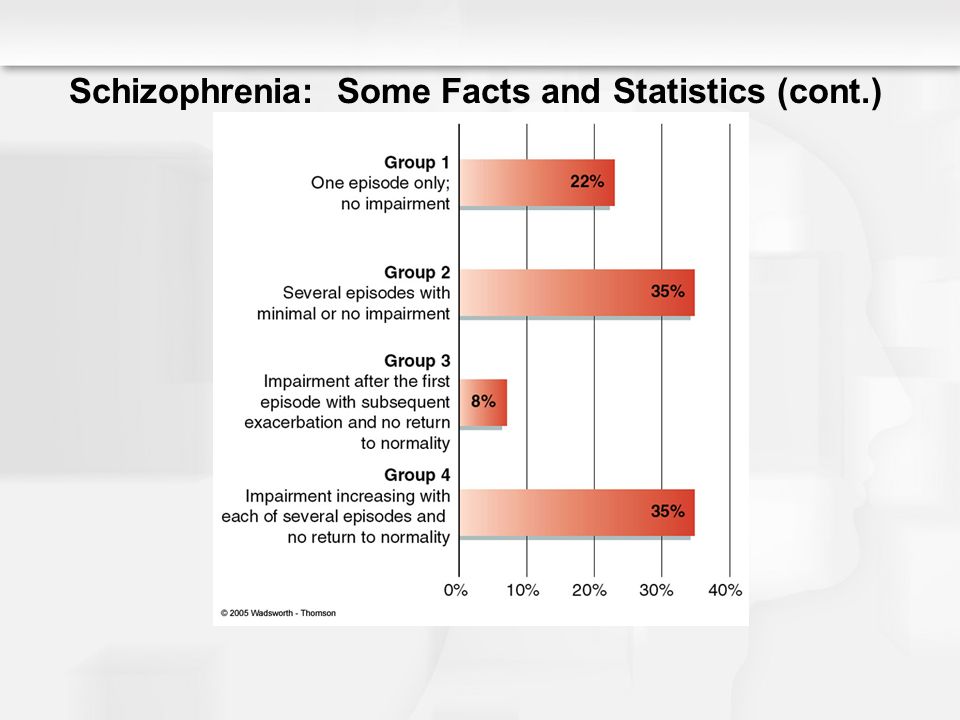 The formation of a hallucinatory symptom complex occurred sequentially with functional hallucinosis of unclear content, hypnogogic and hypnopompic verbal deceptions of perception. Hallucinations quickly occupied a leading position in the structure of the attack, taking on the character of a polyvocal true hallucinosis with specific content and its subsequent evolution, a gradual increase in the duration of existence, an increase in intensity and the formation of structural completeness. Subsequently, the leading position of hallucinatory disorders in the picture of psychosis was maintained throughout its entire duration, and they were transformed into pseudohallucinations. At the same time, they acquired a stereotypical, monotonous character, devoid of affective modulation, their delusional interpretation was almost completely absent. In general, with this type of seizures, hallucinations were stereotyped, monotonous, did not have significant sensory brightness and affective saturation.
The formation of a hallucinatory symptom complex occurred sequentially with functional hallucinosis of unclear content, hypnogogic and hypnopompic verbal deceptions of perception. Hallucinations quickly occupied a leading position in the structure of the attack, taking on the character of a polyvocal true hallucinosis with specific content and its subsequent evolution, a gradual increase in the duration of existence, an increase in intensity and the formation of structural completeness. Subsequently, the leading position of hallucinatory disorders in the picture of psychosis was maintained throughout its entire duration, and they were transformed into pseudohallucinations. At the same time, they acquired a stereotypical, monotonous character, devoid of affective modulation, their delusional interpretation was almost completely absent. In general, with this type of seizures, hallucinations were stereotyped, monotonous, did not have significant sensory brightness and affective saturation.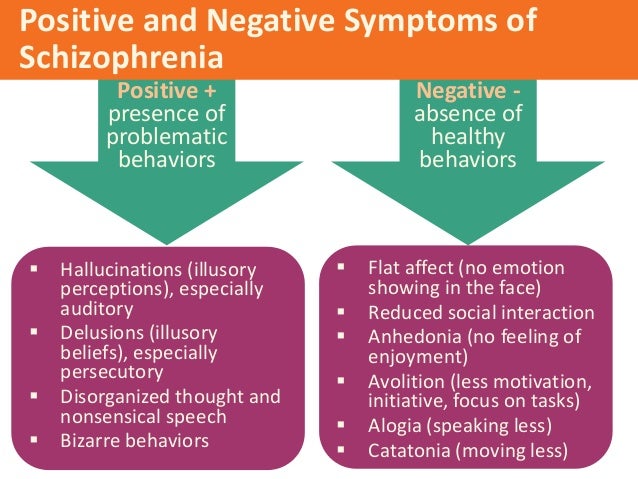 Perceptual delusions in such patients almost never influenced their behavior; did not create in them premises of motivational activity. Hallucinatory products served as a substrate for the emerging non-expanded delusional ideas of relationship, spoilage, and hypochondriacal content. Delusional disorders were thematically closely related to it, while their verbalization was difficult, and there was practically no ideation. There was a poorly systematized interpretive delirium, mainly persecutory content, which had the character of a “small-scale” delirium, involving the immediate environment. Often there was an attachment of individual elements of the Kandinsky-Clerambault syndrome, more often in the form of certain types of mental automatism with the addition of the phenomena of "small" catatonia. Thus, with this typological variety, there was a clear tendency to accumulate the features of an apperceptive-intentional phenomenological pattern, which testified in favor of a deep internal connection between hallucinatory disorders that were forming and thought disorders, which, taking into account the qualitatively low protracted exit from an attack with a tendency to actualize psychotic disorders, the formation residual symptoms and long-term persistence of cognitive dysfunction.
Perceptual delusions in such patients almost never influenced their behavior; did not create in them premises of motivational activity. Hallucinatory products served as a substrate for the emerging non-expanded delusional ideas of relationship, spoilage, and hypochondriacal content. Delusional disorders were thematically closely related to it, while their verbalization was difficult, and there was practically no ideation. There was a poorly systematized interpretive delirium, mainly persecutory content, which had the character of a “small-scale” delirium, involving the immediate environment. Often there was an attachment of individual elements of the Kandinsky-Clerambault syndrome, more often in the form of certain types of mental automatism with the addition of the phenomena of "small" catatonia. Thus, with this typological variety, there was a clear tendency to accumulate the features of an apperceptive-intentional phenomenological pattern, which testified in favor of a deep internal connection between hallucinatory disorders that were forming and thought disorders, which, taking into account the qualitatively low protracted exit from an attack with a tendency to actualize psychotic disorders, the formation residual symptoms and long-term persistence of cognitive dysfunction.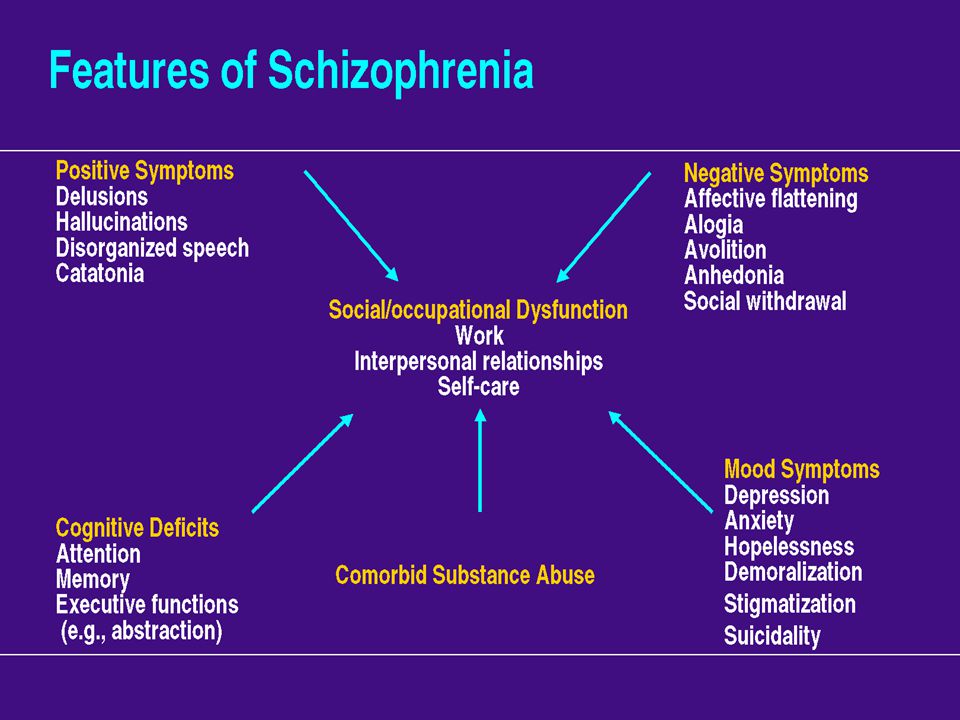
In the second typological variety (32 clinical and 37 follow-up patients), hallucinatory disorders arose secondarily (secondarily) in the structure of an emerging delusional or affective-delusional state, and their formation and subsequent dynamics revealed clear differences within this group of patients.
So, in 17 patients of the clinical group and 20 patients of the follow-up group, hallucinatory phenomena appeared after the formation of a delusional state with a clear delusional plot with a tendency to systematize delusional ideas (persecution, poisoning, exposure), delusional behavior, i.e. within the framework of a delusional state. With this variant, single hypnagogic illusory deceptions gradually appeared, then there was an addition of true polyvocal hallucinatory disorders. By their properties, they were mostly monotonous, monotonous, but at the same time structurally complete, clearly localized in space, distinguished by increasing frequency, duration and intensity.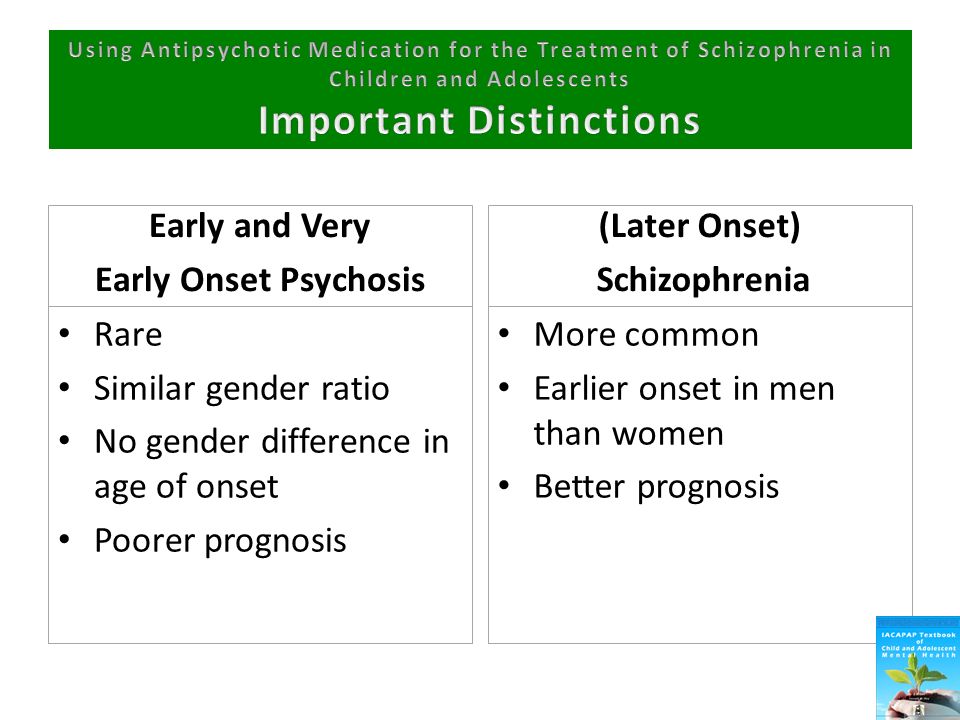 Deceptions of perception quickly acquired a dominant character in the structure of the psychotic state, their interaction with delusional disorders had the character of impregnation into the general outline of the emerging delusional plot. In fact, they were the cause of the formation of hallucinatory delirium. With this type of attack, early attachment of elements of the Kandinsky-Clerambault syndrome and its rapid development with the frequent formation of a picture of "total mastery" and the complete transition of true verbal hallucinosis into pseudohallucinations were noted. The stage of further pathokinesis of hallucinatory disorders was accompanied by a significant loss of their sensitivity, brightness, the motivational activity of hallucinatory disorders was realized indirectly, through the participation of a delusional interpretation of existing hallucinations and led to the performance by patients of certain actions, more often of a protective nature. As a phenomenological analysis showed, this typological group of seizures was characterized by the involvement of the properties of both patterns: at the stage of the formation of an attack, a predominant accumulation of qualities characteristic of the perceptual-structural pattern was found (hallucinations are thematically complex, intense, revealing a connection with a delusional plot, lack of criticism, participation of high motivational activity) , and at the stage of the already formed syndrome, while maintaining some properties of sensory, there was a tendency of the phenomenological properties of hallucinatory disorders to a combination of qualities of an apperceptive-intentional pattern, i.
Deceptions of perception quickly acquired a dominant character in the structure of the psychotic state, their interaction with delusional disorders had the character of impregnation into the general outline of the emerging delusional plot. In fact, they were the cause of the formation of hallucinatory delirium. With this type of attack, early attachment of elements of the Kandinsky-Clerambault syndrome and its rapid development with the frequent formation of a picture of "total mastery" and the complete transition of true verbal hallucinosis into pseudohallucinations were noted. The stage of further pathokinesis of hallucinatory disorders was accompanied by a significant loss of their sensitivity, brightness, the motivational activity of hallucinatory disorders was realized indirectly, through the participation of a delusional interpretation of existing hallucinations and led to the performance by patients of certain actions, more often of a protective nature. As a phenomenological analysis showed, this typological group of seizures was characterized by the involvement of the properties of both patterns: at the stage of the formation of an attack, a predominant accumulation of qualities characteristic of the perceptual-structural pattern was found (hallucinations are thematically complex, intense, revealing a connection with a delusional plot, lack of criticism, participation of high motivational activity) , and at the stage of the already formed syndrome, while maintaining some properties of sensory, there was a tendency of the phenomenological properties of hallucinatory disorders to a combination of qualities of an apperceptive-intentional pattern, i.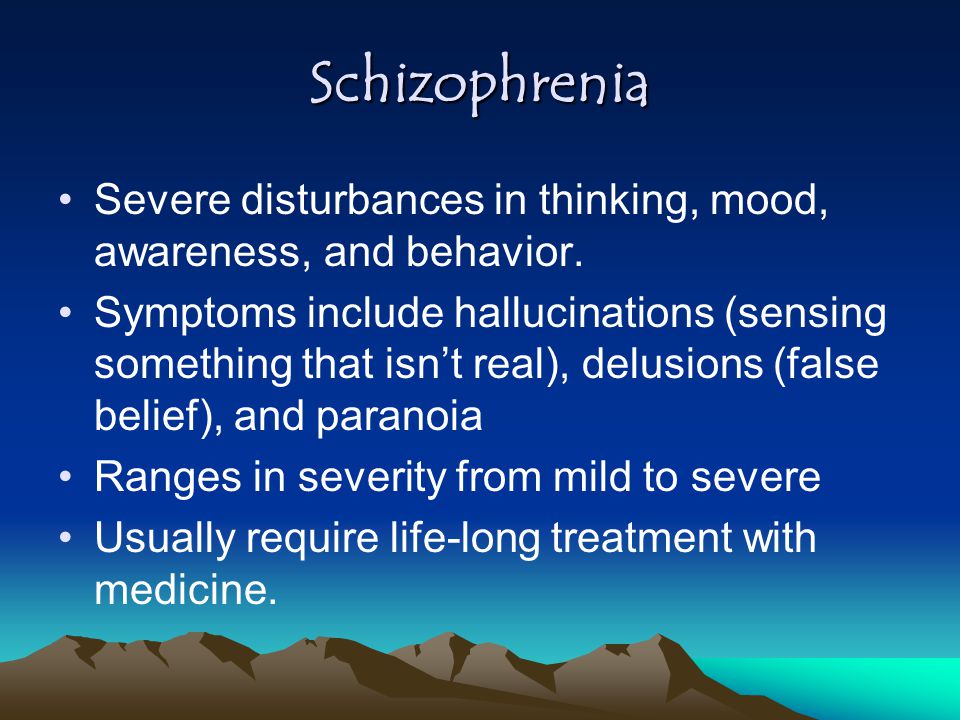 e. reflecting impaired thinking.
e. reflecting impaired thinking.
In another part of the patients (15 patients of the clinical group and 17 patients of the follow-up group), who constituted the second variant of the typological variety, where hallucinatory disorders arose in the structure of an affective-delusional state, the attack developed acutely, an acute sensual delirium with a changeable plot was formed. Hallucinatory disorders arose against the background of a rapidly expanding plot of delusional disorders and existed at first in the form of separate acoasms, hallucinoids, illusory verbal hallucinosis, and only later, at the height of the state, did a picture of true verbal hallucinosis develop, thematically, as a rule, reflecting the content of delusional experiences. The hallucinations were polyvocalic in nature, were sensory bright, thematically scolding or laudatory, depending on the pole of the affect involved in their genesis. Moreover, their content was changeable, unstable, structurally incomplete and more often had an abstract nature of ideas that had the property of fulminant changeability, which correlated with the polymorphism of delusional experiences that had a paraphrenic character. Hallucinatory disorders were perceived as an undoubted belonging to reality, their information-verbal component in this case almost always determined the behavior of patients, which, along with a complete lack of criticism of perceptual deceptions and a high level of their affective saturation, had a significant impact on the behavioral acts of patients and became the cause of actions. that had the character of autoaggression. At the height of the attack, the condition was complicated by the addition of generalized catatonic disorders.
Hallucinatory disorders were perceived as an undoubted belonging to reality, their information-verbal component in this case almost always determined the behavior of patients, which, along with a complete lack of criticism of perceptual deceptions and a high level of their affective saturation, had a significant impact on the behavioral acts of patients and became the cause of actions. that had the character of autoaggression. At the height of the attack, the condition was complicated by the addition of generalized catatonic disorders.
Interpretive delusions in these states were characterized by low specific gravity and weak systematization, the main place was occupied by sharp delusional ideas of perception and imagination. This typological group was characterized by a clear dominance of the phenomenological properties of hallucinations classified as a perceptually structural pattern, which indicated a high degree of sensoriality, as well as a lower intensity and rapid reversibility of signs of disturbed thinking.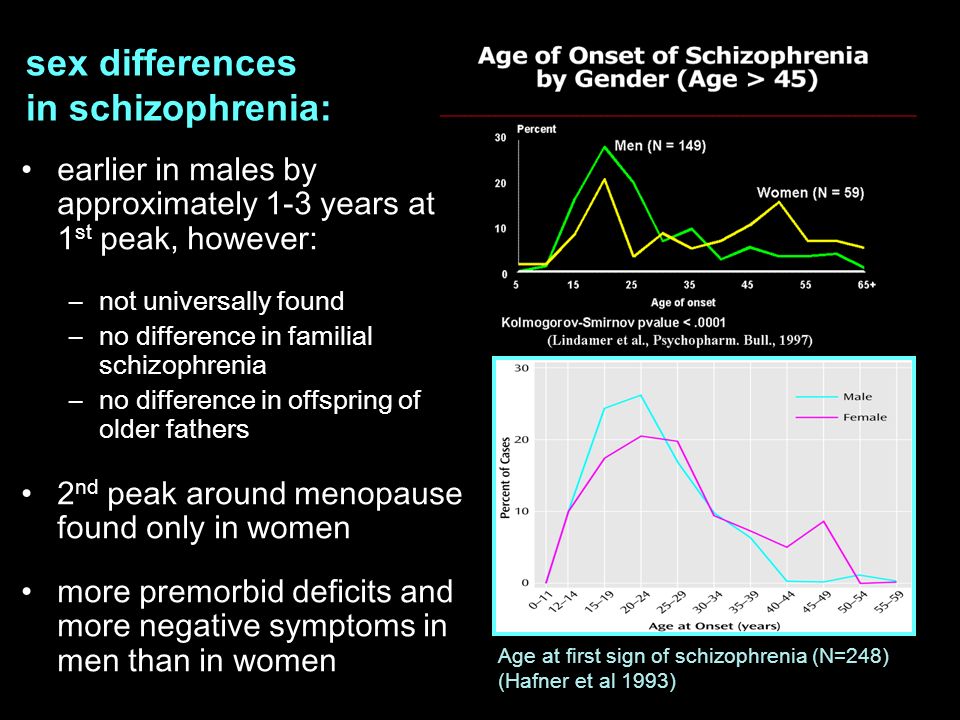
Thus, the data obtained at the stage of clinical-psychopathological and phenomenological analysis testified to the significant heterogeneity of hallucinatory symptoms that arose in the structure of the first manifest attacks of juvenile schizophrenia. Based on the data obtained, an assumption was formed that their clinical varieties in a certain way correlate with the degree of progression of the process and, therefore, can be used as criteria for predicting the nature of the further course of the disease, i.e. carry predictive information.
In order to confirm this hypothesis and search for other characteristics of the studied conditions that are informative for the prognosis, a clinical follow-up method was used. In the process of analyzing information about the nature of the course and outcomes of manifest attacks of juvenile schizophrenia occurring with the dominance of hallucinatory disorders, it was possible to identify significant differences in the degree of progression of the disease, the quality of the changes that occurred, and the level of social and labor adaptation in various typological varieties of these conditions identified by us.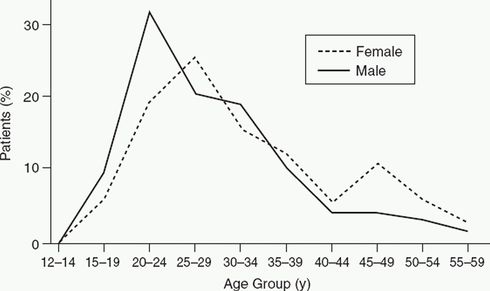 The combination of these characteristics served as the basis for determining the quality of the outcome. With a high degree of certainty (p<0.01), the most often favorable outcome was noted in the second typological type of seizures in the group of patients with secondary development of hallucinatory disorders, their formation in the structure of an affective-delusional state - here "favorable" and "relatively favorable" types of outcome were recorded in total in 58.8% of cases, and an "unfavorable" outcome was formed only in 5.9% of observations. These characteristics were the most unfavorable in the first typological variety of seizures with a primer mechanism for the development of hallucinatory disorders, where "relatively unfavorable" and "unfavorable" types of outcome were observed in 66.6% of patients (p<0.05), and a "favorable" outcome occurred. only in 4.8% of cases. The group of patients in which hallucinatory disorders formed secondarily (secondarily) in the structure of delusional psychosis occupied an intermediate position in terms of outcomes.
The combination of these characteristics served as the basis for determining the quality of the outcome. With a high degree of certainty (p<0.01), the most often favorable outcome was noted in the second typological type of seizures in the group of patients with secondary development of hallucinatory disorders, their formation in the structure of an affective-delusional state - here "favorable" and "relatively favorable" types of outcome were recorded in total in 58.8% of cases, and an "unfavorable" outcome was formed only in 5.9% of observations. These characteristics were the most unfavorable in the first typological variety of seizures with a primer mechanism for the development of hallucinatory disorders, where "relatively unfavorable" and "unfavorable" types of outcome were observed in 66.6% of patients (p<0.05), and a "favorable" outcome occurred. only in 4.8% of cases. The group of patients in which hallucinatory disorders formed secondarily (secondarily) in the structure of delusional psychosis occupied an intermediate position in terms of outcomes.
To confirm the results obtained, the study also included data from the analysis of other equally important parameters for the prognosis, such as the quality and severity of premorbid personality traits, the type of early ontogenetic development, the variant and duration of the initial stage, the age of onset of the disease and the age of manifestation of psychosis. The analysis confirmed the possibility of determining a number of prognostically significant clinical and pathogenetic characteristics, both favorable and unfavorable in relation to the prognosis of juvenile schizophrenia, manifested by attacks with the dominance of hallucinatory disorders. So, as prognostically favorable characteristics, one could consider the acute onset of the disease without a previous initial stage or its duration of no more than 2 years; the same category included mainly the initial stages with the dominance of affective symptoms. A statistically significant prognostically unfavorable value was found for the initial stages with a predominance of paranoid and negative disorders, as well as with a duration of more than 5 years.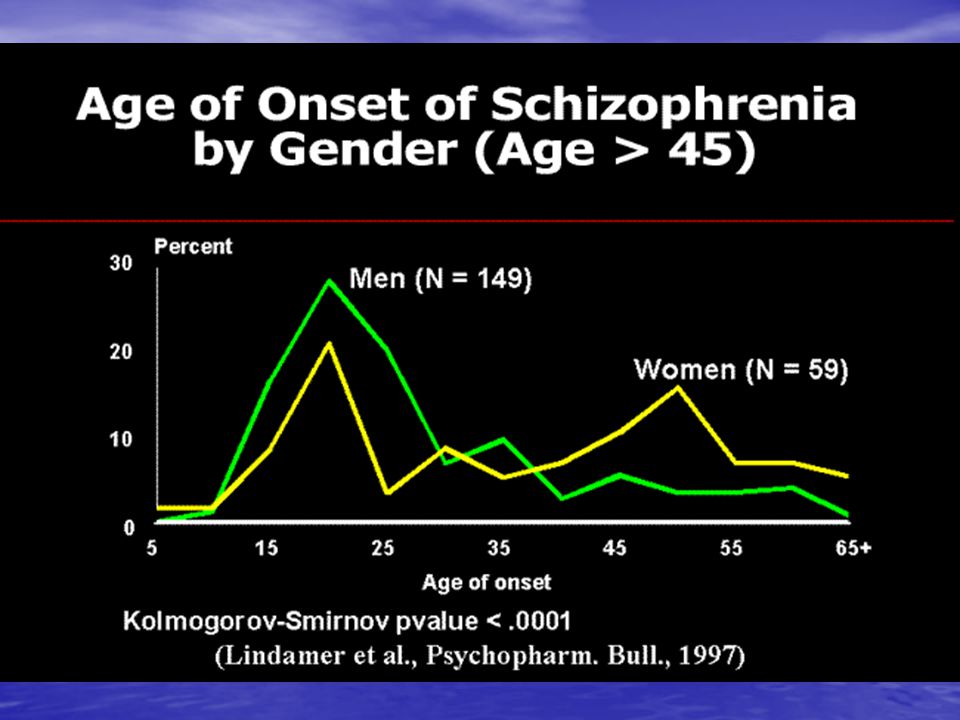
When considering premorbid personality traits, the following were classified as prognostically favorable: hyperthymic personality type, as well as sthenic and sensitive schizoids (p<0.01), and prognostically unfavorable - mosaic, passive and deficient schizoids (p<0.01) , and also here the delayed type of early dysontogenesis was more common. In addition, the severity of the premorbid personality anomaly turned out to be prognostically significant. The presence of a personality disorder (psychopathy) was found to be a statistically significant adverse prognostic factor (p<0.05). The early age of onset (11-16 years) obviously indicated unfavorable trends in the course of the disease, as well as the early age of onset of a manifest psychotic attack (16-19 years).years) (p<0.01).
Thus, it was possible to confirm the informative value of a number of clinical and pathogenetic parameters for the prognosis of juvenile schizophrenia, manifested by attacks with dominance of hallucinatory disorders. To obtain additional informative criteria that objectify the data obtained, experimental psychological tests were also used (together with the Department of Clinical Psychology of the NTsPZ RAMS (headed by Ph.D. S.N. Enikalopov) by senior researchers T.K. Meleshko and V.P. Kritskoy) and neurophysiological methods (together with the leading researcher of the laboratory of neurophysiology of the National Center for Health Sciences of the Russian Academy of Medical Sciences, Doctor of Biological Sciences I.S. Lebedeva, head of the laboratory, Doctor of Biological Sciences, Prof. A.F. Iznak)) examination of 166 patients. According to the experimental psychological study, a common deficit of social orientation and social regulation of activity and behavior was established for all 3 groups of patients, which resulted in a decrease in the selectivity of cognitive processes and social perception detected in them, that is, in the features of their cognitive style and communication . At the same time, the greatest degree of decrease in cognitive functioning was typical for patients of group I (p<0.
To obtain additional informative criteria that objectify the data obtained, experimental psychological tests were also used (together with the Department of Clinical Psychology of the NTsPZ RAMS (headed by Ph.D. S.N. Enikalopov) by senior researchers T.K. Meleshko and V.P. Kritskoy) and neurophysiological methods (together with the leading researcher of the laboratory of neurophysiology of the National Center for Health Sciences of the Russian Academy of Medical Sciences, Doctor of Biological Sciences I.S. Lebedeva, head of the laboratory, Doctor of Biological Sciences, Prof. A.F. Iznak)) examination of 166 patients. According to the experimental psychological study, a common deficit of social orientation and social regulation of activity and behavior was established for all 3 groups of patients, which resulted in a decrease in the selectivity of cognitive processes and social perception detected in them, that is, in the features of their cognitive style and communication . At the same time, the greatest degree of decrease in cognitive functioning was typical for patients of group I (p<0. 01). The smallest - for patients of groups II-6 (p<0.01). Common distinctive pathopsychological features in all compared subgroups turned out to be a significant number of patients with a polydependent cognitive style, which, as is known, contributes to the formation of sensory delusions and hallucinations in the structure of psychosis. That is, the data obtained indicate the existing correlation of a number of indicators ■ (cognitive style, cognitive activity, social and personal characteristics) of the studied pathopsychological syndrome with three variants of the typological variety of the manifest attack of juvenile endogenous psychosis, which occurs with the dominance of hallucinatory disorders, determined at the clinical level, which undoubtedly confirms their predictive value.
01). The smallest - for patients of groups II-6 (p<0.01). Common distinctive pathopsychological features in all compared subgroups turned out to be a significant number of patients with a polydependent cognitive style, which, as is known, contributes to the formation of sensory delusions and hallucinations in the structure of psychosis. That is, the data obtained indicate the existing correlation of a number of indicators ■ (cognitive style, cognitive activity, social and personal characteristics) of the studied pathopsychological syndrome with three variants of the typological variety of the manifest attack of juvenile endogenous psychosis, which occurs with the dominance of hallucinatory disorders, determined at the clinical level, which undoubtedly confirms their predictive value.
Neurophysiological examination of the studied continent of patients revealed a wide range of detected anomalies of neurophysiological parameters in all three examined groups. In the group of patients with a primer mechanism for the formation of a hallucinatory phenomenon, cognitive impairments were most pronounced: all stages of processing significant stimuli were disrupted - activation and / or synchronization in the activity of structures associated with the processing of physical parameters of sounds, automatic recording of memory traces, comparison of incoming stimuli (temporal wave range N100), processes of classification of stimuli, choice of solution, provision are slowed down 4
5 167
J* i 1 motor action (N200) and processes of maintaining working memory, evaluating the significance of information (P300).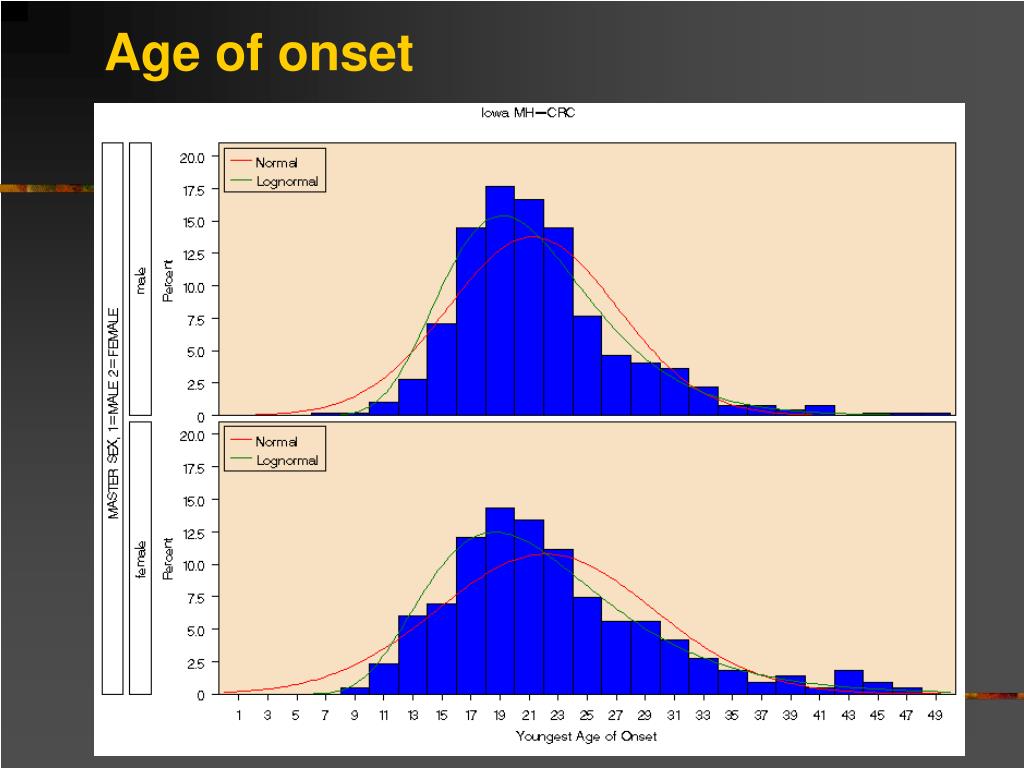 In contrast to this group, in patients with a second mechanism for the formation of a hallucinatory phenomenon in the structure of a delusional state, the initial stages of information processing are practically not disturbed, the focus of pathology here falls primarily on the N200 wave stage - the processes associated with the classification of stimuli, the choice of a solution, provision of motor acts. In the group of patients where the hallucinatory phenomenon is formed in the structure of an affective-delusional state, this stage of target information processing turned out to be the most intact. Thus, it was possible to establish some features of the studied characteristics of all three groups of the studied patients in relation to the profile and intensity of cognitive anomalies, which correlate with the established clinical varieties of manifest attacks of juvenile schizophrenia that occur with a predominance of a hallucinatory symptom complex, which confirms their importance for constructing prognostic criteria.
In contrast to this group, in patients with a second mechanism for the formation of a hallucinatory phenomenon in the structure of a delusional state, the initial stages of information processing are practically not disturbed, the focus of pathology here falls primarily on the N200 wave stage - the processes associated with the classification of stimuli, the choice of a solution, provision of motor acts. In the group of patients where the hallucinatory phenomenon is formed in the structure of an affective-delusional state, this stage of target information processing turned out to be the most intact. Thus, it was possible to establish some features of the studied characteristics of all three groups of the studied patients in relation to the profile and intensity of cognitive anomalies, which correlate with the established clinical varieties of manifest attacks of juvenile schizophrenia that occur with a predominance of a hallucinatory symptom complex, which confirms their importance for constructing prognostic criteria.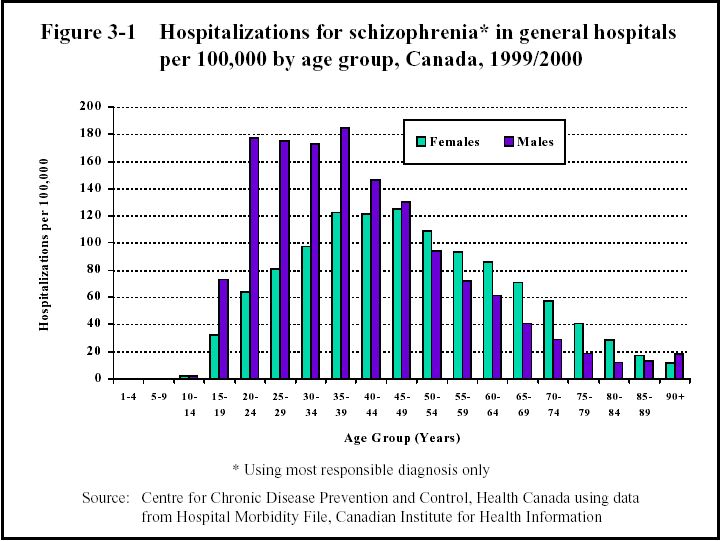
In the present study, general principles for the treatment of patients with schizophrenia manifesting in adolescence with seizures dominated by hallucinatory disorders were determined (in accordance with the recommendations given in the "Standards of care for patients with schizophrenia", 2006). It turned out to be possible to attribute the following to the main principles: at the stage of relief therapy, the choice of drugs was determined by the severity of hallucinatory symptoms, as well as the degree of systematization and completeness of delusional constructions, the role and participation of symptoms of the affective and catatonic registers in the picture of psychosis. The main drugs were found to be antipsychotics (neuroleptics). Their therapeutic effect in each case depended on the characteristics of the psychopathological picture of the condition, its dynamics and individual susceptibility, and manifested itself on average during the first 2-8 weeks. Preference was given to drugs with a powerful incisive effect, both from the group of conventional and atypical antipsychotics, including parenteral ones.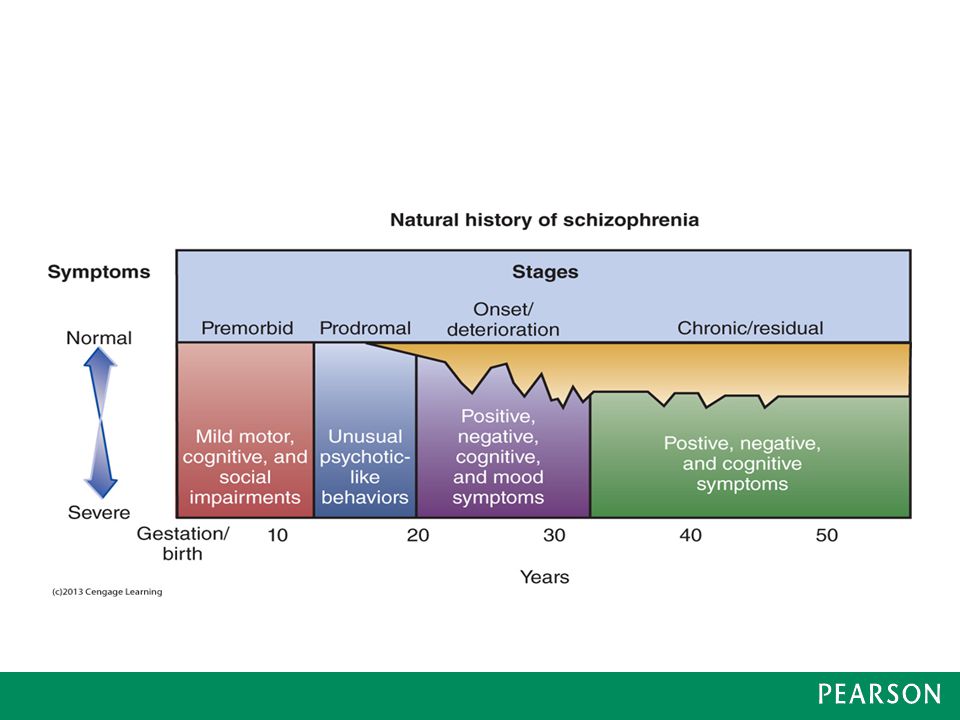 When stopping the severity of psychosis, at the stage of transition to stabilization of the state, the most optimal was the priority prescription of modern atypical antipsychotics. Subsequently, it was effective to join various psychotherapeutic and psycho-corrective measures aimed at understanding and understanding by patients of the pathological nature of the transferred condition, the formation of adequate behavioral strategies aimed at achieving the most rapid and complete readaptation and resocialization, which is especially relevant in adolescence. At the stage of long-term maintenance psychotropic therapy, the main goal was to maintain the achieved level of reduction of productive psychopathological symptoms, improve the quality of remission due to its positive effect on negative and cognitive disorders, as well as reduce the frequency of possible relapses, reduce the severity of symptoms with possible exacerbations of the disease and achieve the highest possible the level of social functioning of patients.
When stopping the severity of psychosis, at the stage of transition to stabilization of the state, the most optimal was the priority prescription of modern atypical antipsychotics. Subsequently, it was effective to join various psychotherapeutic and psycho-corrective measures aimed at understanding and understanding by patients of the pathological nature of the transferred condition, the formation of adequate behavioral strategies aimed at achieving the most rapid and complete readaptation and resocialization, which is especially relevant in adolescence. At the stage of long-term maintenance psychotropic therapy, the main goal was to maintain the achieved level of reduction of productive psychopathological symptoms, improve the quality of remission due to its positive effect on negative and cognitive disorders, as well as reduce the frequency of possible relapses, reduce the severity of symptoms with possible exacerbations of the disease and achieve the highest possible the level of social functioning of patients.