Major depressive disorder diagnostic criteria
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.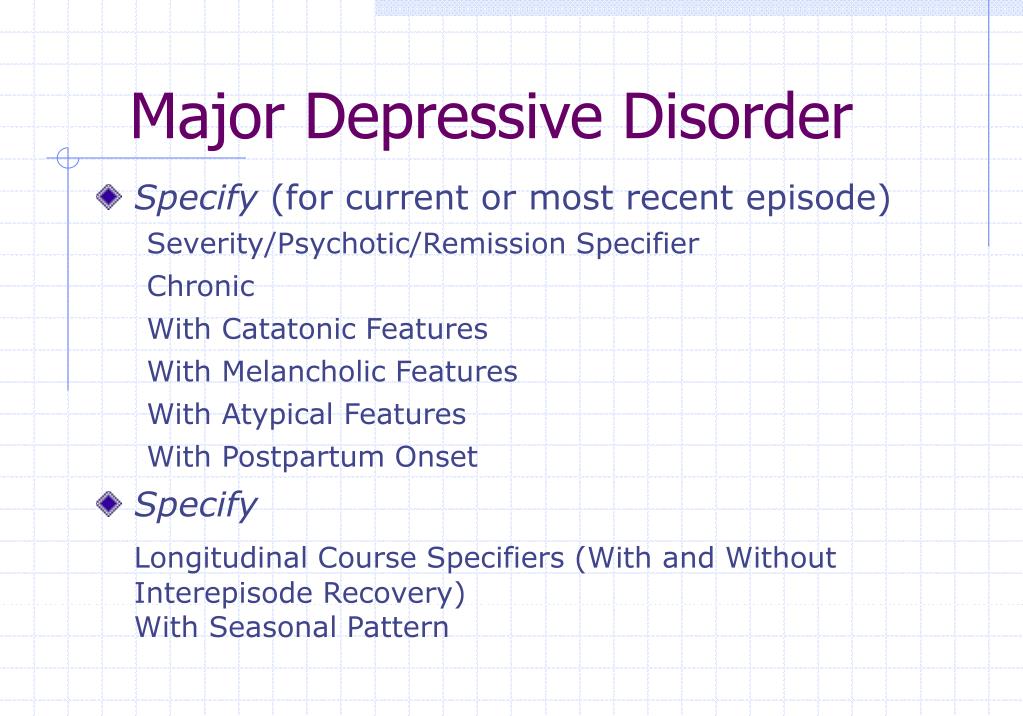
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
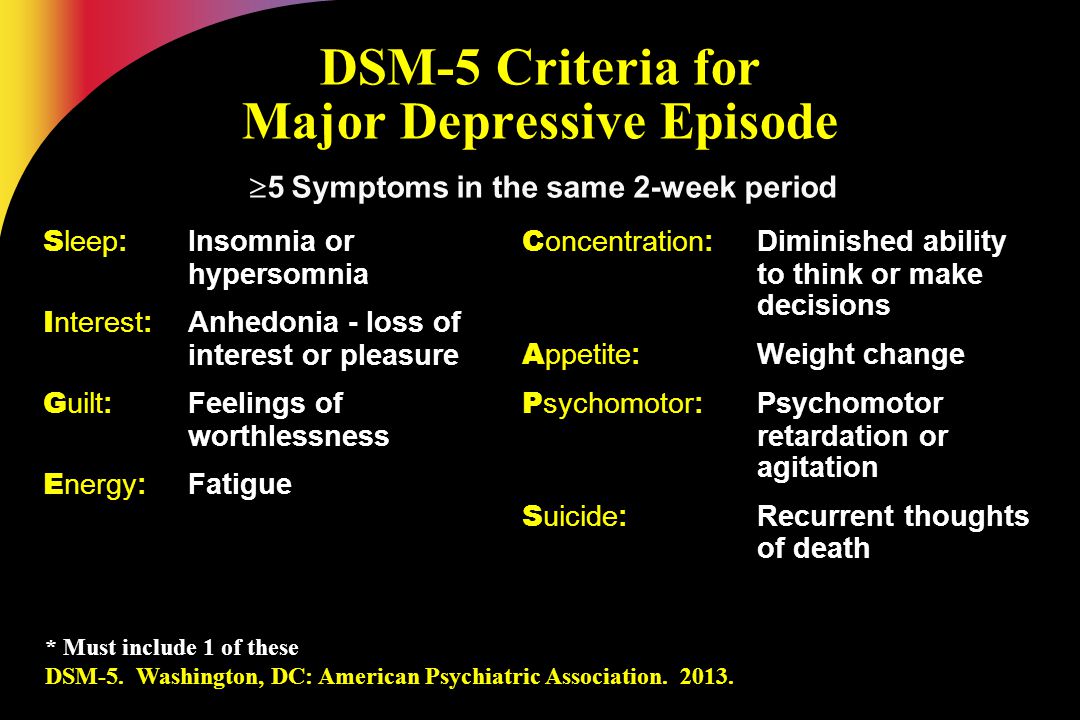
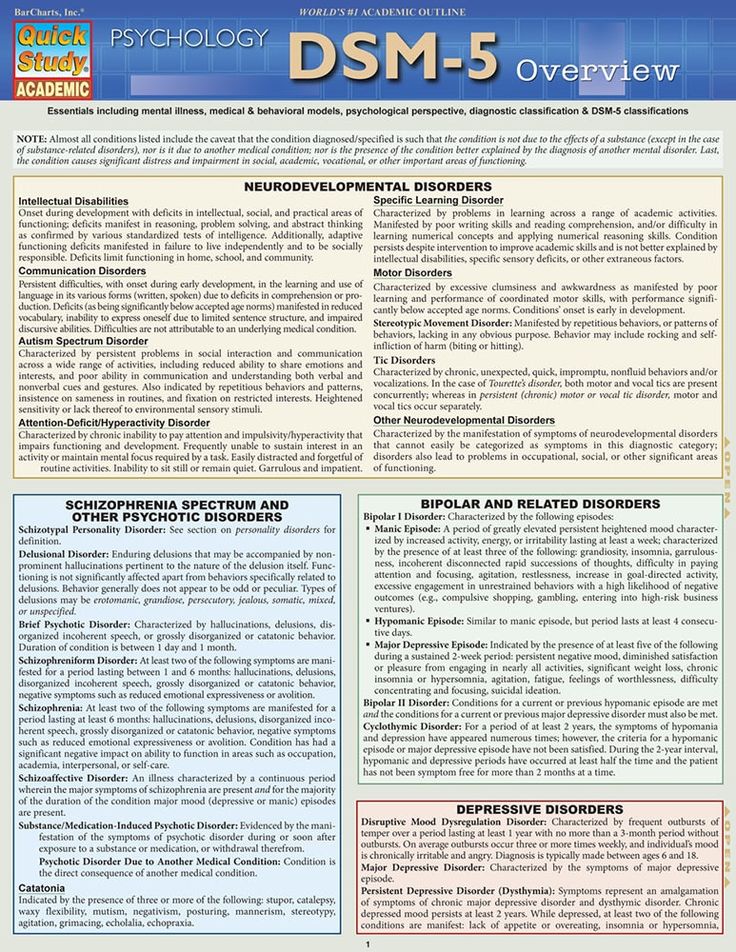
Depression Definition and DSM-5 Diagnostic Criteria
Depression
Depression, otherwise known as major depressive disorder or clinical depression, is a common and serious mood disorder
Jessica Truschel
Medical ReviewerFarah Fazel, PsyS
What is Depression?
Depression, otherwise known as major depressive disorder or clinical depression, is a common and serious mood disorder. Those who suffer from depression experience persistent feelings of sadness and hopelessness and lose interest in activities they once enjoyed. Aside from the emotional problems caused by depression, individuals can also present with a physical symptom such as chronic pain or digestive issues. To be diagnosed with depression, symptoms must be present for at least two weeks.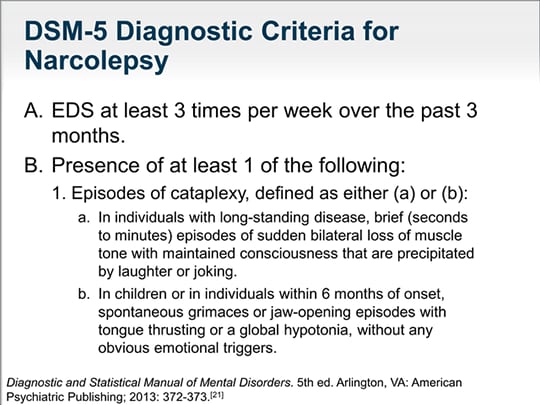
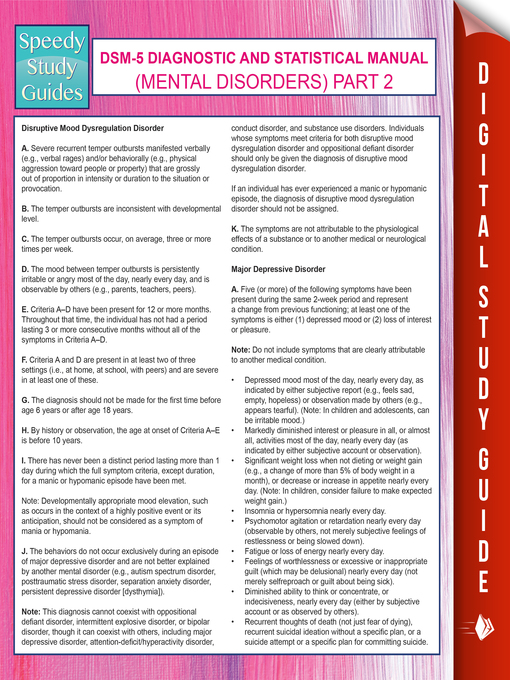
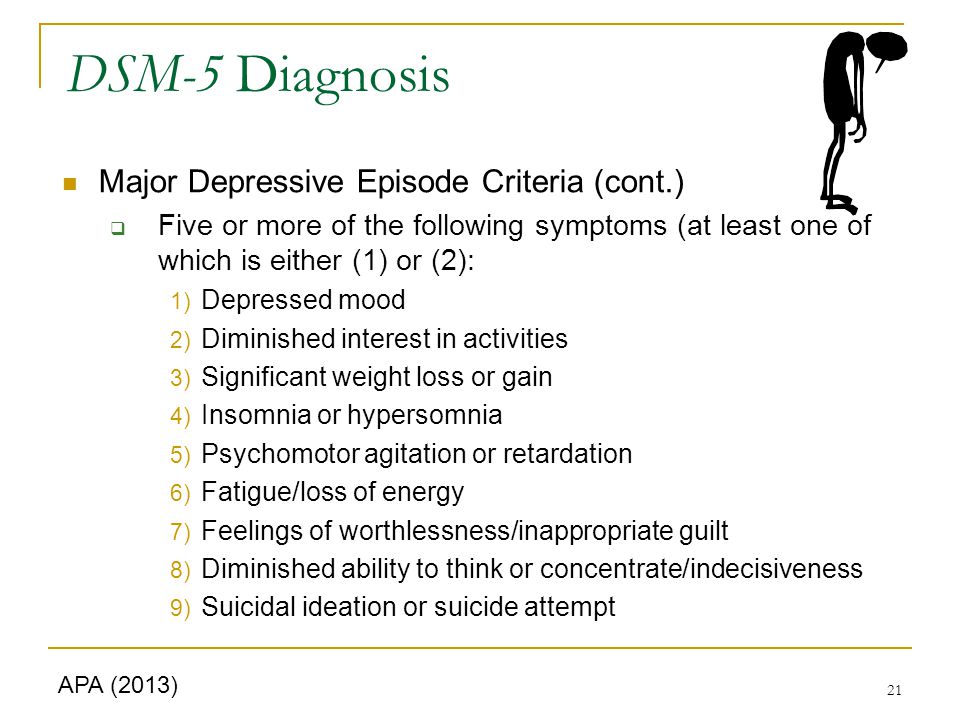
The DSM-5 outlines the following criterion to make a diagnosis of depression. The individual must be experiencing five or more symptoms during the same 2-week period and at least one of the symptoms should be either (1) depressed mood or (2) loss of interest or pleasure.
Depressed mood most of the day, nearly every day.
Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day.
Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day.
A slowing down of thought and a reduction of physical movement (observable by others, not merely subjective feelings of restlessness or being slowed down).
Fatigue or loss of energy nearly every day.
Feelings of worthlessness or excessive or inappropriate guilt nearly every day.
Diminished ability to think or concentrate, or indecisiveness, nearly every day.
Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
To receive a diagnosis of depression, these symptoms must cause the individual clinically significant distress or impairment in social, occupational, or other important areas of functioning. The symptoms must also not be a result of substance abuse or another medical condition.
Major depressive disorder is associated with high mortality, much of which is accounted for by suicide. As a result, if you think someone you care about may be suffering from depression it is important to know the warning signs of suicide and to take suicidal statements extremely seriously. An active statement by someone with suicidal ideation might be something like, “I’m going to kill myself,” but other passive statements such as, “I wish I could just go to sleep and never wake up,” are equally worrying. If someone with depression exhibits these verbal markers, encourage them to consult a mental health professional immediately.
Depressed individuals also present with irritability, brooding, and obsessive rumination, and report anxiety, phobias, excessive worry over physical health, and complain of pain.
The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM), the DSM-5, added two specifiers to further classify diagnoses:
With Mixed Features – This specifier allows for the presence of manic symptoms as part of the depression diagnosis in patients who do not meet the full criteria for a manic episode.
With Anxious Distress – The presence of anxiety in patients may affect prognosis, treatment options, and the patient’s response to them. Clinicians will need to assess whether or not the individual experiencing depression also presents with anxious distress.
What is the difference between depression and sadness? Given that the primary symptom associated with depression is sadness it can be hard to know how to make a distinction between the two psychological states.
But depression is more than just sadness, and not simply by a measure of degree. The difference doesn’t lie in the extent to which a person feels down, but rather in a combination of factors relating to the duration of these negative feelings, other symptoms, bodily impact, and the effect upon the individual’s ability to function in daily life.
Sadness is a normal emotion that everyone will experience at some point in his or her life. Be it the loss of a job, the end of a relationship, or the death of a loved one, sadness is usually caused by a specific situation, person, or event. When it comes to depression, however, no such trigger is needed. A person suffering from depression feels sad or hopeless about everything. This person may have every reason in the world to be happy and yet they lose the ability to experience joy or pleasure.
With sadness, you might feel down in the dumps for a day or two, but you’re still able to enjoy simple things like your favorite TV show, food, or spending time with friends.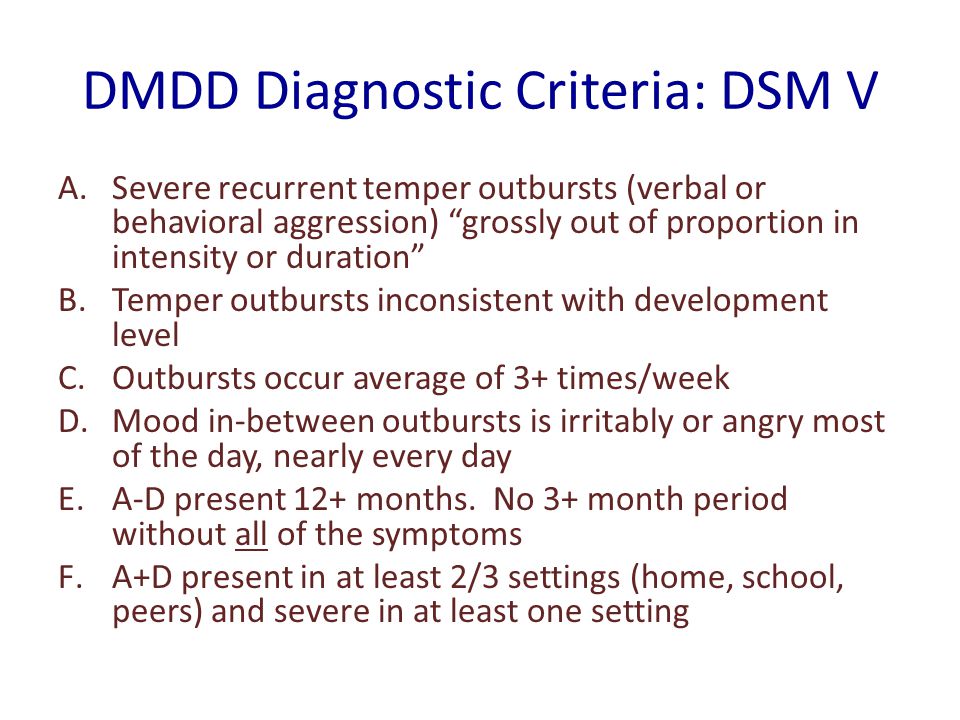 This isn’t the case when someone is dealing with depression. Even activities that they once enjoyed are no longer interesting or pleasurable.
This isn’t the case when someone is dealing with depression. Even activities that they once enjoyed are no longer interesting or pleasurable.
What’s more, when you experience sadness triggered by a certain something you’re still able to sleep as you usually would, remain motivated to do things, and maintain your desire to eat. Depression, on the other hand, is associated with serious disruption of normal eating and sleeping patterns, as well as not wanting to get out of bed all day.
In sadness, you might feel regret or remorse for something you said or did, but you won’t experience any permanent sense of worthlessness or guilt as you might with depression. One of the diagnostic features of depression is this kind of self-diminishing, negative thought patterns.
Finally, self-harm and suicidal inclinations don’t arise from non-depressive sadness. Those struggling with severe depression may have thoughts of self-harm, death, or suicide, or have a suicide plan.
If you’re feeling suicidal or just need to talk, call the National Suicide Prevention Lifeline for free at 1-800-273-8255.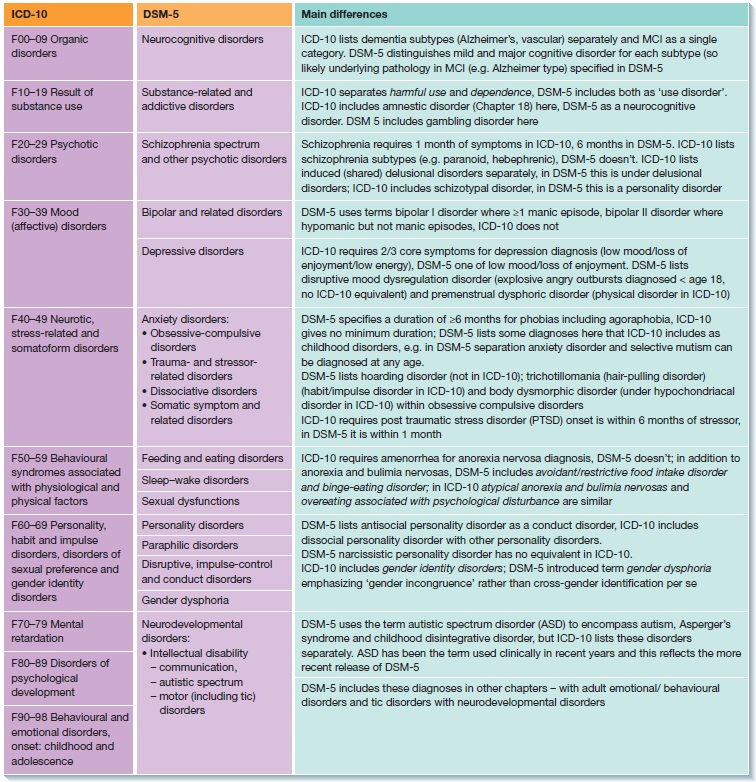 Or, simply call or text 988 to reach the crisis lifeline.
Or, simply call or text 988 to reach the crisis lifeline.
Although there is a clear distinction to be made between depression and sadness, it is possible for major depressive disorder to occur in addition to sadness resulting from a significant loss, such as bereavement, financial ruin, or a serious medical illness. The decision as to whether a diagnosis of depression should be made will depend on the judgment of the clinician treating the individual.
If you think you or someone you care about may be suffering from depression, we encourage you to seek help from a mental health professional. If you lack access to mental healthcare, you can find resources in Psycom's Affordable Therapy article.
The following online directories can be consulted to find a therapist in your area:
Psychology Today: https://therapists.psychologytoday.com/rms
GoodTherapy.org: http://www.goodtherapy.org/find-therapist.html
If you’re thinking about suicide, are worried about someone else, or just need emotional support, the emergency Lifeline network is available 24/7.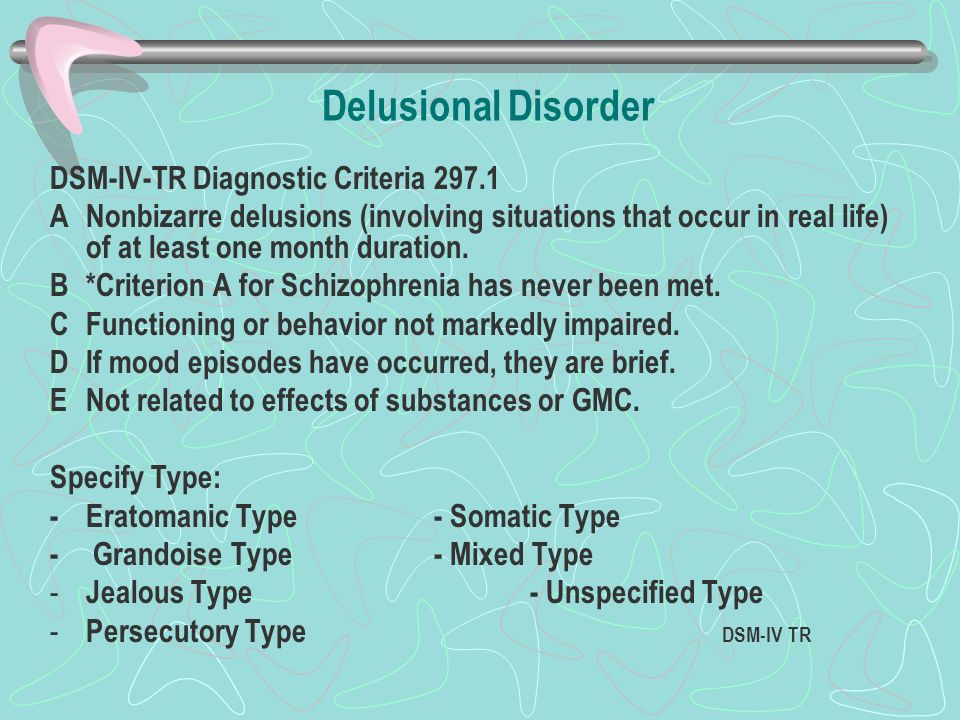 You can call 1-800-273-8255 or go to their website for a live chat.
You can call 1-800-273-8255 or go to their website for a live chat.
"Highlights of Changes from DSM-IV-TR to DSM-5". American Psychiatric Association. May 17, 2013. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Fifth edition. 2013.
Notes: This article was originally published July 24, 2018 and most recently updated August 26, 2022.
Major depressive disorders (clinical depression)
Depression is different from normal mood swings and short-term emotional responses to everyday problems. Prolonged moderate to severe depression can become a serious illness. This results in patients suffering greatly and doing poorly at work, at school and have problems in their families. At its worst, depression can lead to suicide.
Depression is a common illness worldwide, affecting more than 264 million people. Major depressive disorder is one of the most common forms of mental illness, affecting approximately one in six men and one in four women in their lives.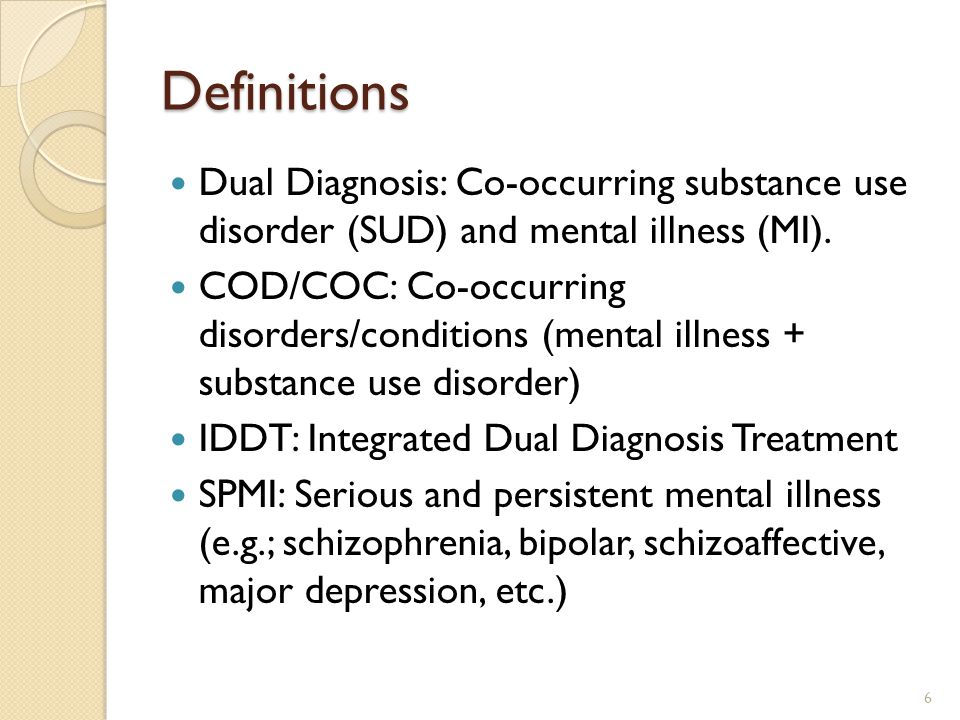
Major depressive disorder (MDD) is a severe condition characterized by low mood, decreased interests, poor cognitive function, and autonomic symptoms such as disturbed sleep or eating. MDD can develop in one in six adults during their lifetime and affects about twice as many women as men.
Main symptoms of depressive disorder
Symptoms of major depressive disorder (MDD) may include:
- depression almost every day
- loss of interest in activities you once enjoyed
- changes in appetite or weight
- sleep problems
- feeling lazy or restless
- low energy
- feelings of hopelessness or worthlessness
- trouble concentrating
- frequent thoughts of death or suicide
Recurrent depression:
This is a highly relapsing condition: at least 50% of people recovering from a first episode of depression have at least one additional episode in their lifetime, and about 80% of people have a history of two recurrent episodes.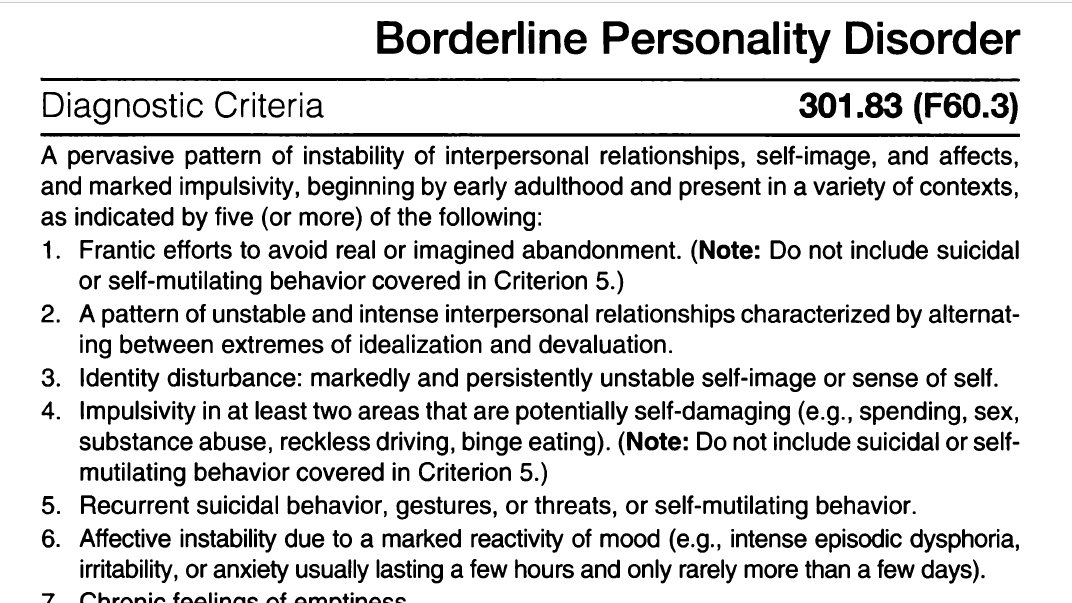
Episodes typically recur within five years of the first episode, and the average person with a history of depression will have five to nine depressive episodes in their lifetime.
Symptoms of recurrent depression:
- difficulty concentrating
- disturbed sleep
- reduced energy level
- constant light alarm
Major depression in adults:
Depression is a common adult disorder that often leads to poor quality of life and impaired role functioning. Depression is also associated with high rates of suicidal behavior and death. When depression occurs in the context of a medical illness, it is associated with increased healthcare costs, longer hospital stays, poor collaboration in treatment, etc.
Causes of depression in adults may be related to the difficulty of changing roles:
- low education and low income
- early pregnancy and childbirth
- divorces
- unstable work
- highly competitive and hard work
Major symptoms of depression in adults include:
- Mostly sad or depressed mood
- Loss of interest or pleasure and avoidance of social gatherings
- Decreased energy and frequent fatigue
- Decreased concentration and attention
- Decreased self-esteem and self-confidence
- Thoughts on guilt and unworthiness
- A gloomy and pessimistic view of the future
- Thoughts or actions of harming oneself or suicidal thoughts
- Sleep disturbance or insomnia
- Pronounced or reduced appetite
DSM-5 Criteria for Major Depressive Disorder
According to the DSM-5, the following criteria must be met for a diagnosis of major depression:
At least five of the following symptoms must have been present for at least two weeks and reflect a change in previous functionality.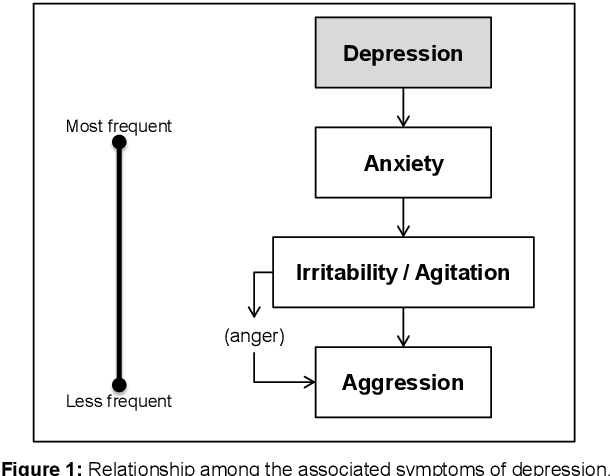 In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
- The person is depressed most of the day, almost every day, as noted by himself or others.
- He or she is not interested in all or most activities most of the day, almost every day.
- Every day a person gains or loses a large amount of weight or has a decreased or increased appetite.
- Almost every day he or she suffers from insomnia or hypersomnia.
- Every day a person experiences psychomotor disturbances that are visible to others and can also be reported.
- Almost every day he or she feels exhausted or tired.
- Almost every day a person has thoughts of worthlessness or guilt.
- Every day a person's ability to think, concentrate, or make judgments deteriorates.
- He or she has recurrent suicidal thoughts, suicidal thoughts (without a definite plan), a suicide attempt, or a definite plan to commit suicide.
- Symptoms listed above cause clinical distress or interfere with daily activities.
- The episode of depression is not associated with the physiological effect of the drug or other disease.
- The onset of the episode is not better explained by specific or unspecified schizophrenia spectrum illness or other psychotic disorders.
- The person has never had a manic or hypomanic episode.
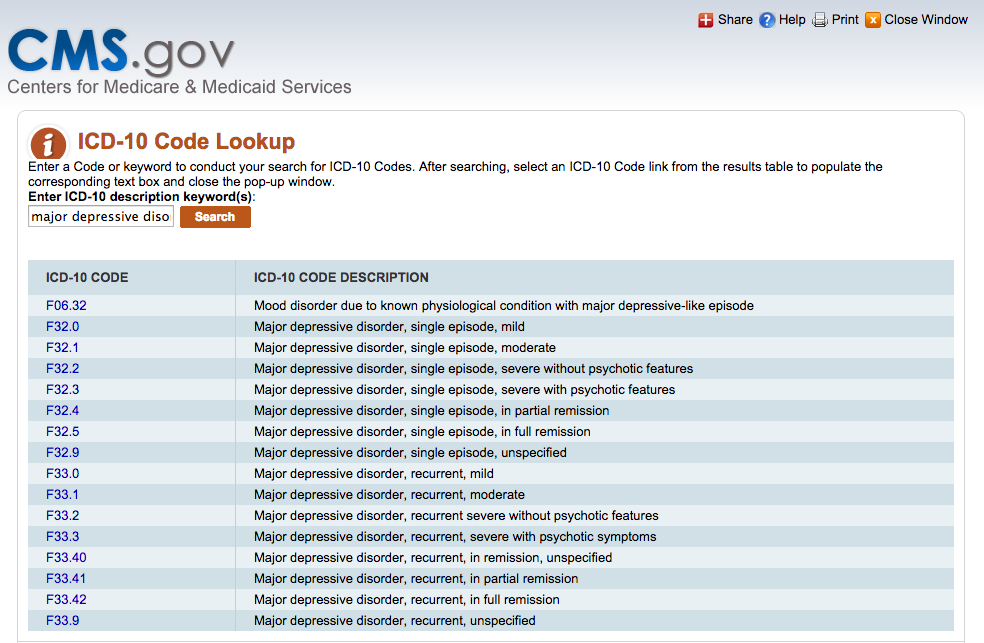
The diagnostic code for major depressive disorder is based on the frequency of recurrent episodes, the severity of the episodes, the presence of psychotic characteristics, and the state of remission. Below are the varieties of depression:
Severity of depression:
- Minor
- Moderate
- Heavy
- Psychotic
- In partial remission
- In complete remission
- Undefined
Epidemiology
Major depressive illness is a common mental illness. Its lifetime prevalence ranges from 5 to 17 percent.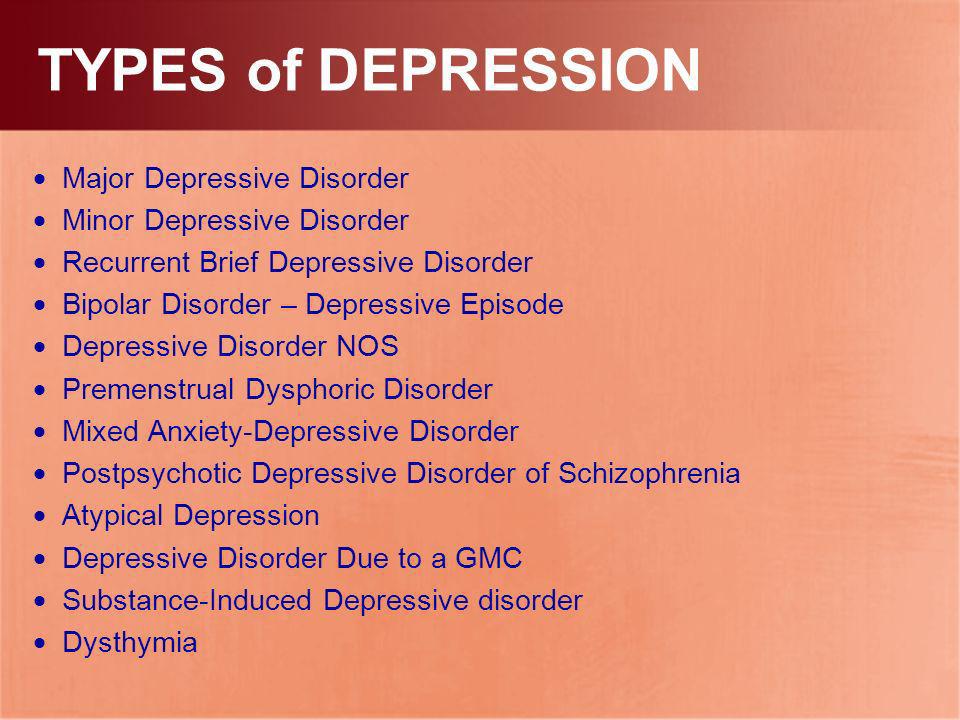 The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
MDD is more common in divorced, separated, or bereaved individuals who do not have meaningful interpersonal interactions. There is no difference in the prevalence of MDD between races or socioeconomic status. People with MDD often have comorbidities such as substance abuse, panic disorder, social anxiety disorder, and obsessive-compulsive disorder.
The presence of these comorbidities in people with MDD increases the risk of suicide. Depression is more common in older people with underlying medical problems. Depression is more common in rural areas than in cities.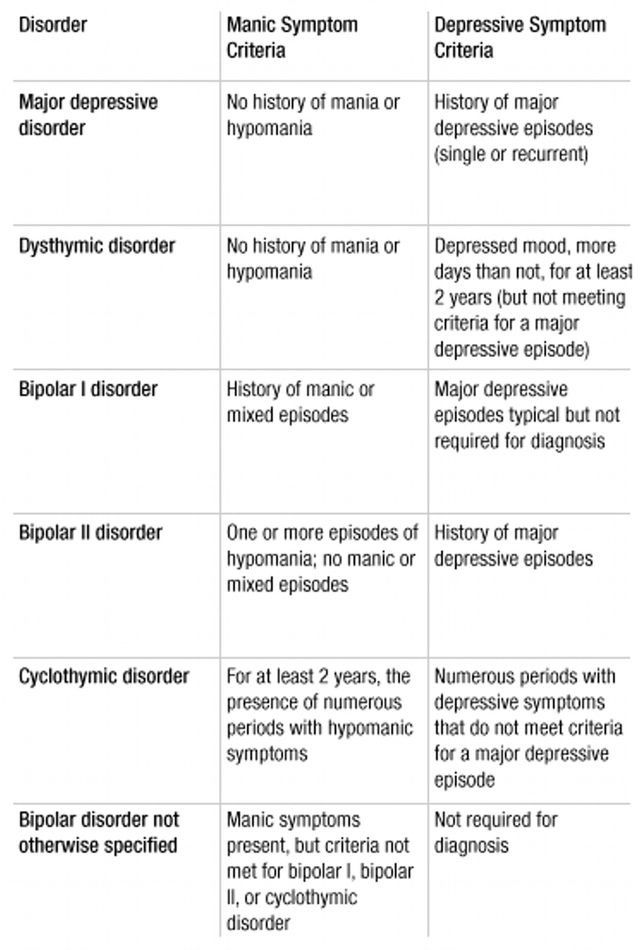
Pathophysiology of major depressive disorder
The genesis of major depressive disorder is believed to be multifaceted, with biological, genetic, environmental and psychological factors at play. It used to be thought that MDD was caused mainly by abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine.
This has been demonstrated by the use of several antidepressants in the treatment of depression, such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, and dopamine-norepinephrine receptor inhibitors. Serotonin metabolites have been found to decrease in people who have had suicidal thoughts. However, recent hypotheses suggest that this is largely due to more complex neuroregulatory systems and brain circuits, leading to subsequent disruption of the neurotransmitter systems.
GABA, an inhibitory neurotransmitter, as well as glutamate and glycine, important excitatory neurotransmitters, have been shown to play a role in the genesis of depression.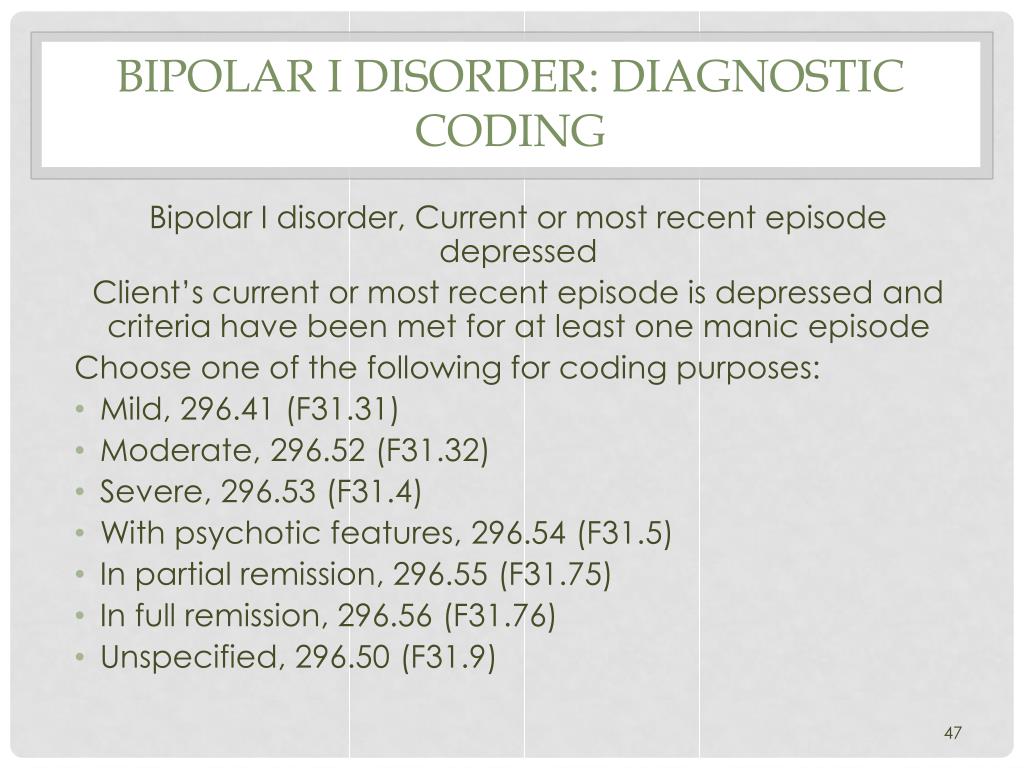 Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
The antidepressant properties of drugs that oppose NMDA receptors have been investigated. Thyroid and growth hormone imbalances have also been linked to mood disorders. Numerous adversity and trauma in childhood have been linked to the development of depression later in life.
Severe early stress can cause dramatic changes in neuroendocrine and behavioral responses, leading to anatomical abnormalities in the cerebral cortex and severe depression later in life. Structural functional tomography of the brain in people with depression revealed greater hyperintensity in the subcortical regions and a decrease in the metabolism of the anterior brain regions on the left.
Family, adoption and twin studies have shown that genes play a role in the risk of depression.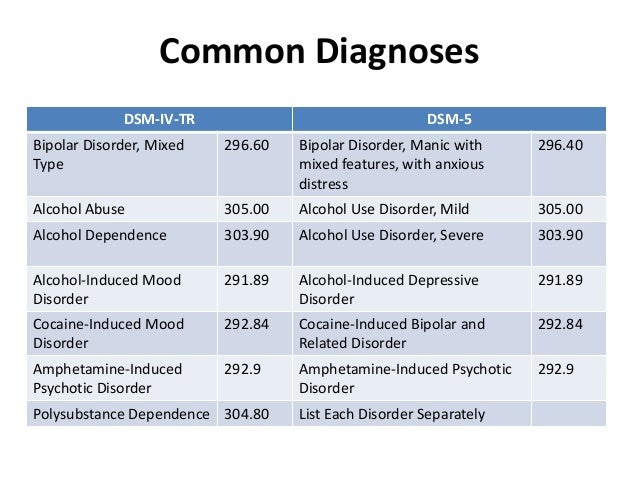 According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to the theory of learned helplessness, the onset of depression is associated with the experience of uncontrollable events. Depression, according to cognitive theory, results from cognitive errors in those who are predisposed to depression.
Somatic illnesses associated with depression
Somatic sensations are especially common in depression and other mental illnesses. Although somatic symptoms are common in depressed individuals, they are of much lesser importance than major depressive symptoms in the diagnosis of depression.
The clinical stages of sad mood are characterized by both painful and non-painful bodily symptoms.
Major depressive disorder diagnosis
Major depressive disorder is a clinical diagnosis; this is mainly determined by the patient's medical history and assessment of mental status.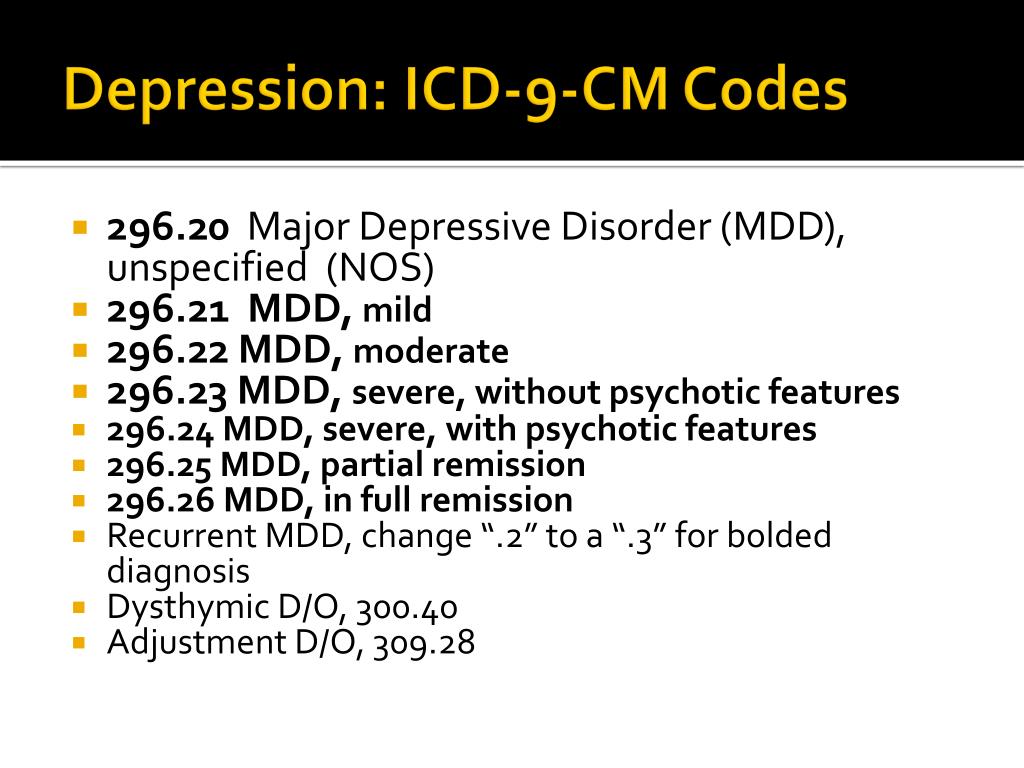 Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Although there are no objective tests to diagnose depression, routine laboratory tests such as CBC with a differential diagnosis, a comprehensive metabolic panel, thyroid-stimulating hormone, free T4, vitamin D, urinalysis, and toxicology screening are done to rule out organic or medical diseases. causes of depression.
People with depression often see their primary care physicians for medical problems related to their depression rather than seeking a mental health professional. In nearly half of the cases, patients deny experiencing depressive symptoms and are often referred to therapy by family members or sent by employers to be tested for social isolation and decreased activity. At each visit, it is critical to assess the patient for thoughts of suicide or murder.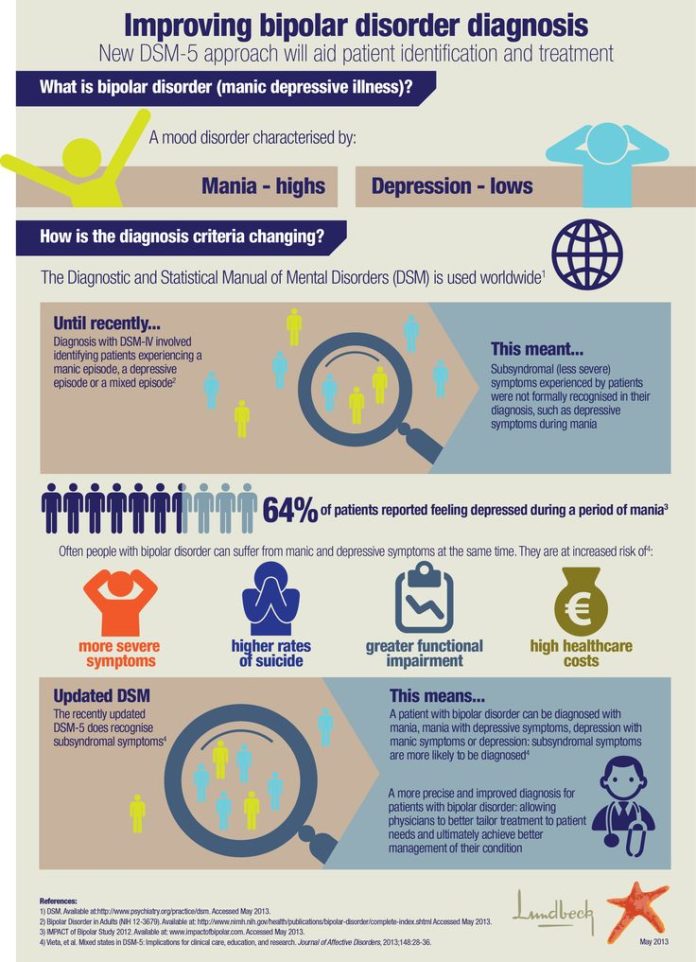
Being in a bad mood or feeling tense is common for all of us. When these feelings persist, you may suffer from depression or anxiety—or both. The self-assessment quizzes contain relevant questions to help you assess your current situation and develop a strategy to help you feel better sooner.
When you are going through a difficult moment, it is natural to feel depressed for a while; feelings like melancholy and loss help define who we are. However, if you feel sad or uncomfortable most of the time for an extended period of time, you may be suffering from depression.
Take a self-test to see if you are showing any warning signs of depression. This won't give you a diagnosis, but it will help you determine what to do next.
Major depressive disorder with psychotic features
Psychotic depression, also known as major depressive disorder with psychotic features, is a serious medical or mental illness that requires prompt treatment and constant monitoring by a physician or mental health professional.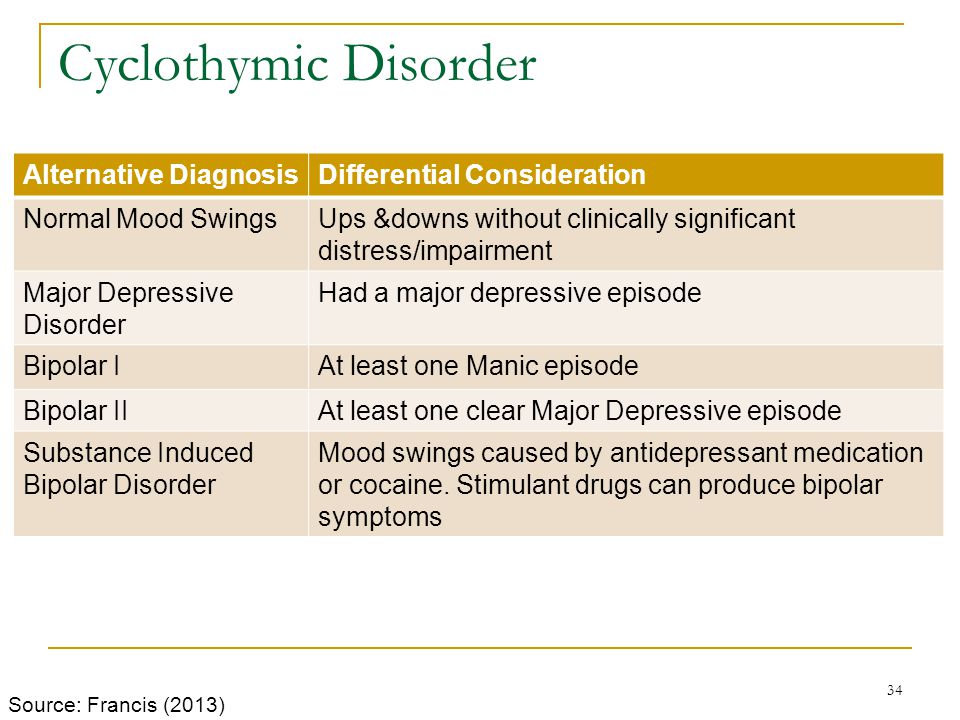
Major depression is a common mental condition that can have a detrimental effect on many aspects of a person's life. It affects mood and behavior as well as various bodily processes such as eating and sleeping. People who suffer from severe depression often lose interest in things they used to love and have difficulty doing daily activities. Sometimes they may even feel that life is not worth living.
Bipolar disorder (BD)
Depression in patients with bipolar disorder (BD) is a significant clinical problem. Since schizophrenia dominates even in the treatment of BD, depression is associated not only with schizophrenia, but also with BD and comorbid medical disorders with a high risk of suicide.
Diagnosis of bipolar disorder (BD) and risk factors:
Approximately 12-17% of cases of bipolar disorder are not recognized until the mood "transforms" into hypomania or mania, either spontaneously or under the influence of substances uplifting mood.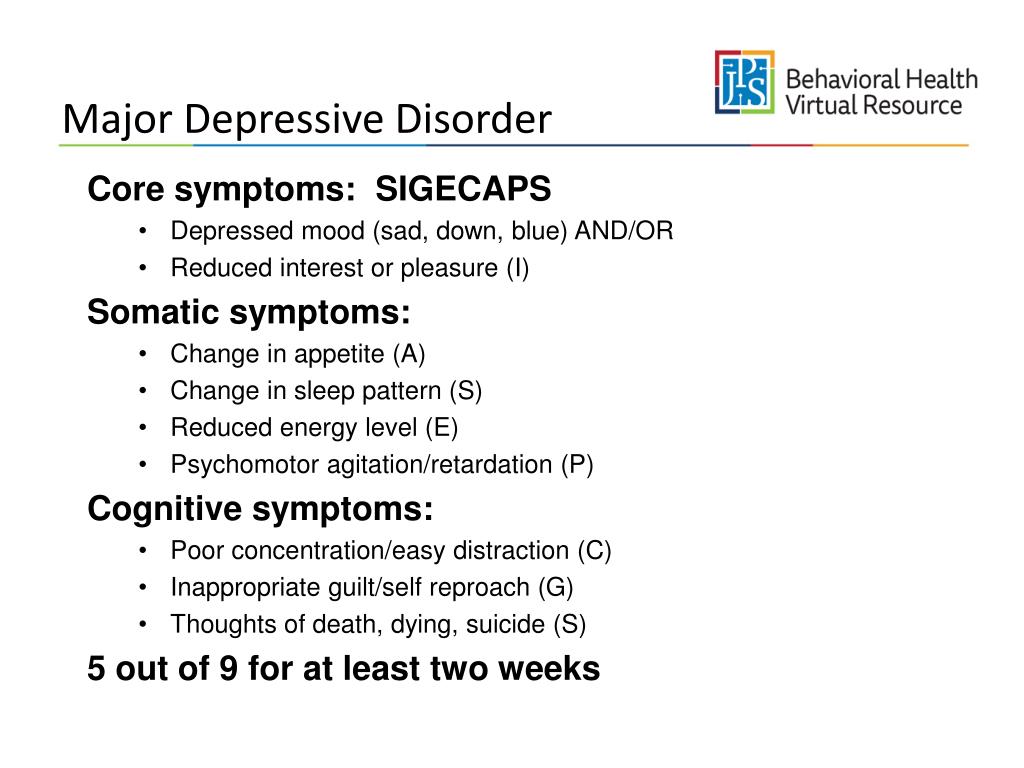
Factors suggesting a diagnosis of BD:
- Family mania, psychosis, "nervous breakdown" or psychiatric hospitalization
- Early onset, often with depressive symptoms
- Cyclothymic mood
- Multiple relapses (eg 4 episodes of depression in 10 years)
- Depression with characteristic agitation, anger, insomnia, irritability, talkativeness.
- Other features are "mixed" or hypomanic or psychotic symptoms.
- Clinically "worsens", especially with mixed properties, during antidepressant treatment.
- Suicidal thoughts and actions
- Alcohol or drug abuse
Major depressive disorder in children and adolescents:
Major depressive disorder (MDD) can have a significant impact onset during childhood and adolescence. Associated with this are poor school performance, interpersonal problems later in life, early parenthood, and an increased risk of other psychiatric and substance use disorders.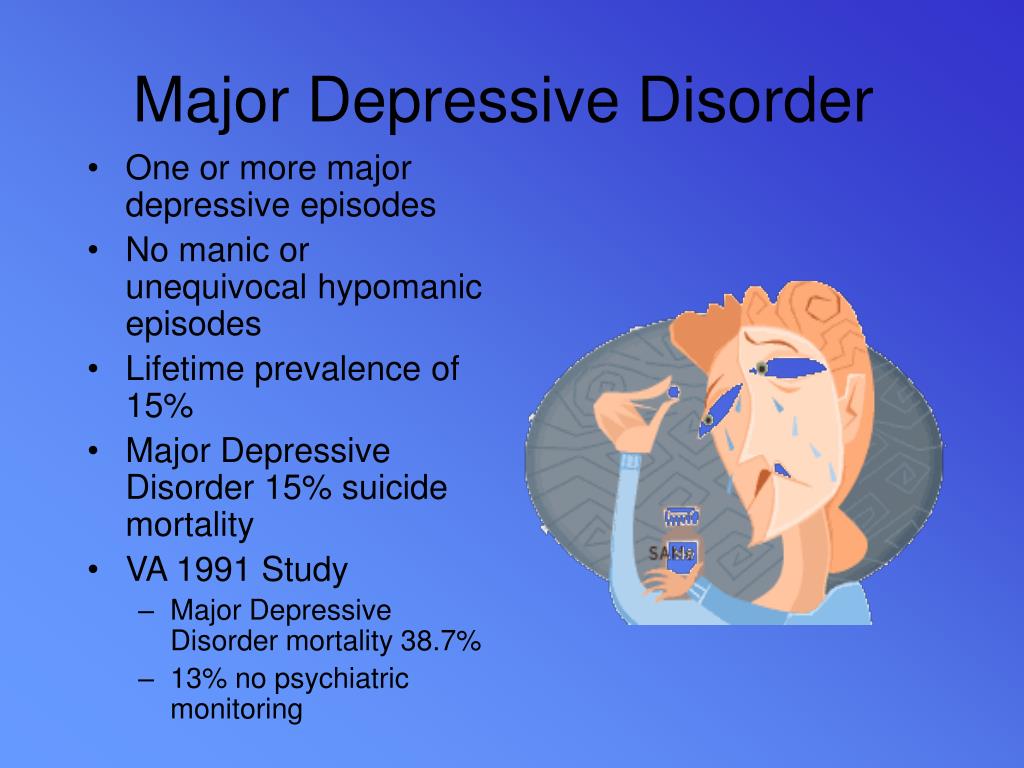 Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Symptoms of depression in children aged 3-8 years include:
- unsubstantiated claims.
- irritability
- less signs of depression
- anxiety
- behavioral changes
As the child becomes a teenager and adult, the presentation of symptoms meets the criteria for the Diagnostic and Statistical Manual of Mental Disorders (DSM-5):
- Irritability.
- Expected weight gain.
- Lethargy or inner restlessness.
- May be delusional and not limited to feelings of guilt.
Postpartum depression
Postpartum depression affects one in seven women (PPD). While most women recover quickly from childhood blues, PPD lasts much longer and has a significant impact on women's ability to return to normal activities.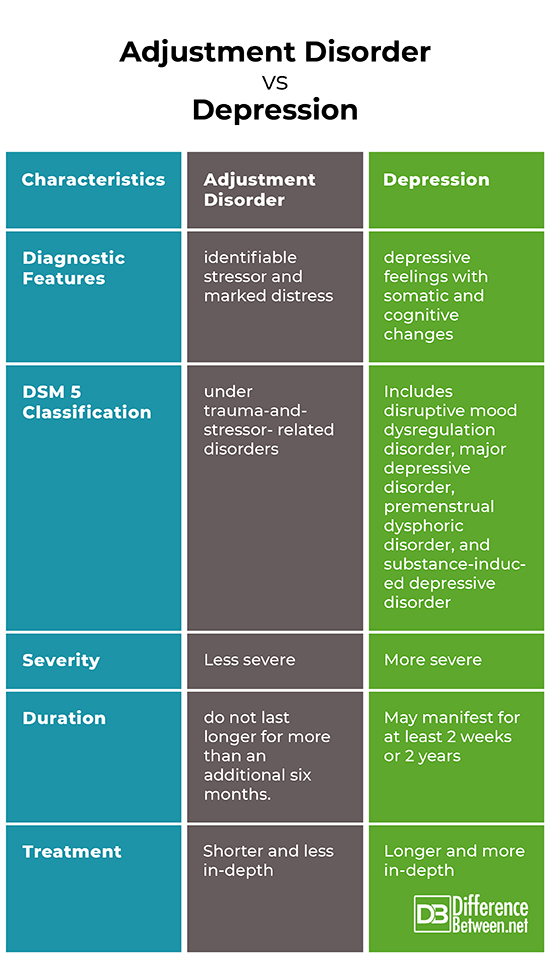
PDD affects the mother and her relationship with the child. PRD impairs maternal brain response and behavior. Postpartum depression most often occurs within 6 weeks after delivery. PDD affects 6.5 to 20% of women. It is more common in teenage girls, mothers who have given birth prematurely, and women living in cities.
In one study, African American and Hispanic mothers reported onset of symptoms within 2 weeks of birth, while white mothers reported onset of symptoms later.
Premenstrual dysphoric disorder
Premenstrual symptoms are a group of psychological, behavioral and physical symptoms that cyclically occur before menstruation and subsequently resolve after menstruation in women of reproductive age. Most women experience relatively mild pain and the symptoms do not interfere with their personal, social, or professional lives; however, 5% to 8% of women experience moderate or severe symptoms that can cause significant distress and functional impairment.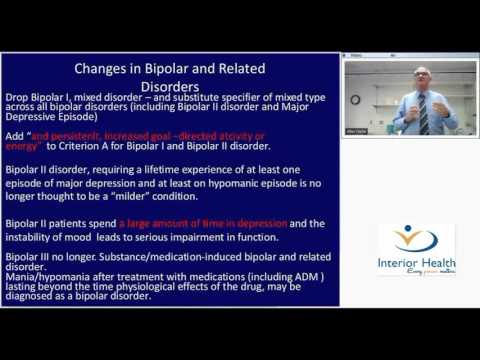
All women of reproductive age, from menarche to menopause, may have premenstrual symptoms. Premenstrual symptoms are a common problem for women of reproductive age. In the United States, 70 to 90 percent of women of reproductive age report at least some premenstrual pain.
Approximately one third of these women have symptoms severe enough to warrant a diagnosis of PMS. PMDD, the most severe type of premenstrual symptom complex, occurs in 3-8% of these women.
Treatment of major depressive disorder
Treatment of major depressive disorder (MDD) in adults:
Treatment options for major depressive disorder include medication, psychological, interventional, and lifestyle changes. Medications and/or psychotherapy are used initially to treat MDD.
Combination treatment, including both drugs and psychotherapy, has been shown to be more effective than either treatment alone. Electroconvulsive therapy has been shown to be more effective than any other treatment for severe major depression.
Patient psychotherapy:
Depression education and treatment can be provided to all patients. When appropriate, education may be provided to eligible family members.
Information about available treatment options will help patients make informed decisions, anticipate side effects, and follow prescribed treatment. Another important aspect of education was informing patients and concerned family members about the delayed duration of antidepressant onset of action.
Pharmacotherapy and acute treatment:
Antidepressants may be used as the primary treatment for patients with moderate or severe depression.
Clinical features that may indicate that the drug is a preferred therapeutic agent include a history of previous positive response to antidepressants, severity of symptoms, significant sleep disturbance and appetite disturbance.
Patients with severe depression with psychotic features will require antidepressant and antipsychotic and/or electroconvulsive therapy (ECT).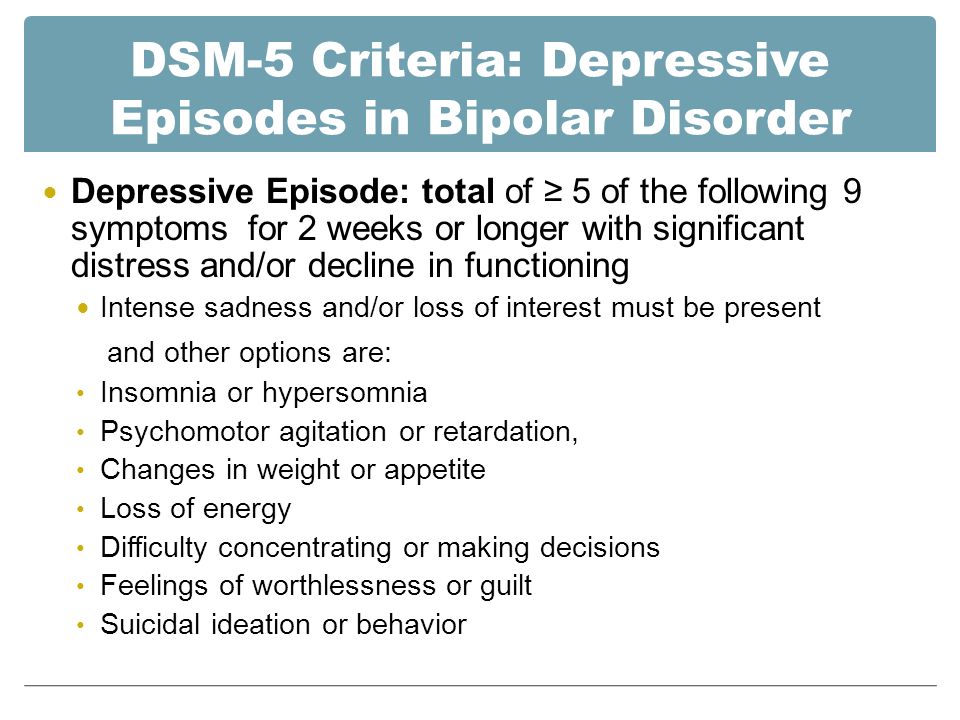
All antidepressants are effective, although their side effects vary. The following drugs have been approved by the FDA for the treatment of MDD:
- Fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine are examples of selective serotonin reuptake inhibitors (SSRIs). They are commonly used as first line therapy and are the most commonly prescribed antidepressants.
- Venlafaxine, duloxetine, desvenlafaxine, levomilnacipran and milnacipran are examples of serotonin and norepinephrine reuptake inhibitors (SNRIs). They are often used to treat depressed people who also have pain problems.
- Trazodone, vilazodone and vortioxetine are serotonin modulators.
- Bupropion and mirtazapine are examples of atypical antidepressants. When patients experience sexual side effects from SSRIs or SNRIs, they are often recommended as monotherapy or as adjunctive drugs.
- Amitriptyline, imipramine, clomipramine, doxepin, nortriptyline and desipramine are tricyclic antidepressants (TCAs).
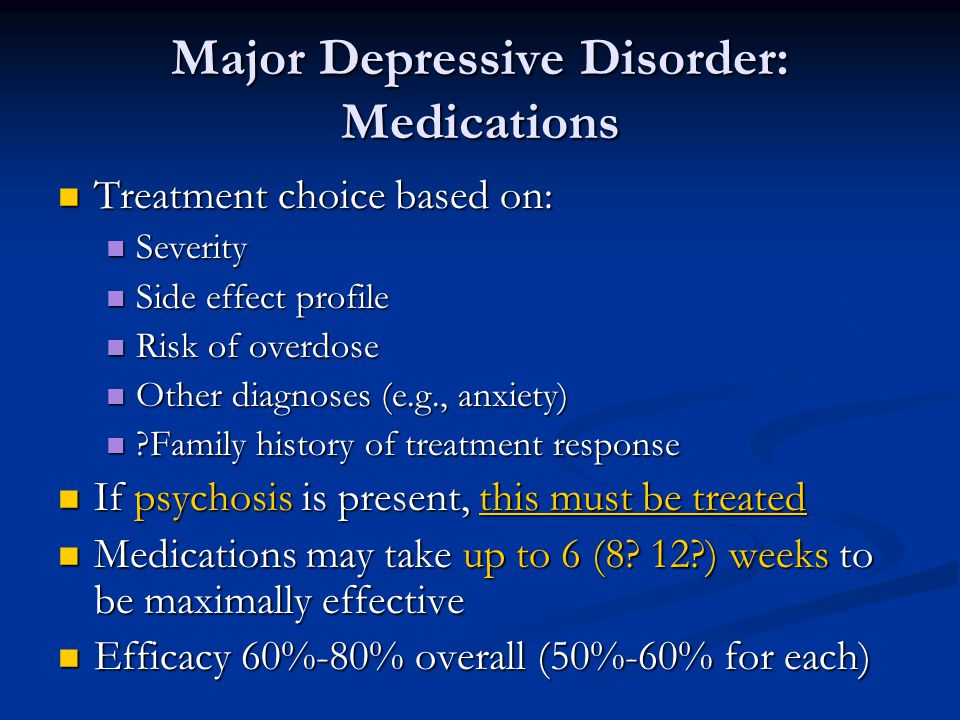
- Tranylcypromine, phenelzine, selegiline, and isocarboxazid are examples of monoamine oxidase inhibitors (MAOIs). Due to the high prevalence of side effects and death in overdose, MAOIs and TCAs are not commonly used.
- Other drugs that can be used to improve the effectiveness of antidepressants include mood stabilizers and antipsychotics.
The role of yoga and meditation in managing depression:
Originating in ancient India, yoga is recognized as a form of alternative medicine using mind-body practice. Yoga philosophy is based on 8 elements that are best described as the ethical principles of a meaningful and purposeful life. Yoga can help with depression through the following mechanisms:
- Muscle relaxation resulting in less pain
- Creating Balanced Energy
- Decreased breathing and heart rate
- Lowering blood pressure and cortisol levels
- Increase blood flow
- Reducing stress and anxiety through tranquility
- Improve pre-existing ailments such as arthritis, cancer, mental illness and more.
Treatment of major depressive disorder (MDD) in children and adolescents
Psychotherapy is important for both patients and their families, so everyone knows about the plan and goals of treatment. When the patient receives information, the severity of symptoms decreases. Mental education may include knowledge about the signs and symptoms of depression, the clinical course of the illness, the risk of exacerbation, treatment options, and parental advice on how to interact with depressed young people.
According to research by Sandra Mullen, psychotherapy, along with medication, is often recommended for the treatment of major depressive disorder (MDD) in children and adolescents diagnosed with depression, suicidal ideation, and transient hypomania/mania.
Treatment of bipolar depression
Bipolar depression remains a clinical problem. Treatment options are limited, especially in the treatment of the acute phase of bipolar depression. There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
Non-approved agents and treatments
Non-pharmacological drugs such as lamotrigine, antidepressants, modafinil, pramipexole, ketamine, and electroconvulsive therapy (ECT) are often prescribed for the treatment of acute bipolar depression.
Treatment of recurrent depression:
Some patients may experience recurrent episodes of depression throughout their lives unless supportive care is used to prevent relapse. Treatment should include psychotherapy and pharmacotherapy, and the dose should generally not be reduced after remission has been achieved.
Differential
Critical to rule out depressive disorder due to another medical condition, depressive disorder due to psychoactive substances/drugs, dysthymia, cyclothymia, bereavement, adjustment disorder with depressed mood, bipolar disorder, schizoaffective disorder, schizophrenia, anxiety disorders and eating disorders when assessed for DMD.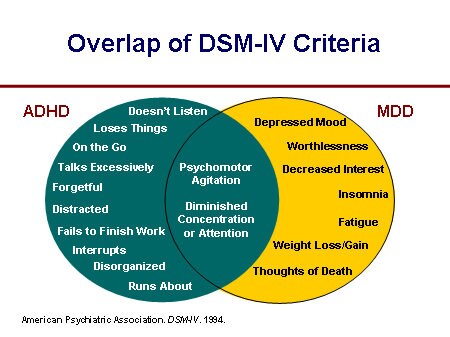 Depressive symptoms can develop as a result of the following factors:
Depressive symptoms can develop as a result of the following factors:
- Neurological causes such as cerebrovascular accident, multiple sclerosis, epilepsy, Parkinson's disease and Alzheimer's disease.
- Endocrine diseases such as diabetes, thyroid disease and adrenal disease.
- Metabolic disorders such as hypercalcemia, hyponatremia
- Drugs/substances causing dependence: steroids, antihypertensives, anticonvulsants, antibiotics, sedatives, sleeping pills, alcohol, stimulant withdrawal.
- Nutrient deficiencies such as vitamin D, B12, B6, iron or folate deficiency
- Infectious diseases such as HIV and syphilis
- Malignant neoplasms
Prognosis
Episodes of depression in untreated major depressive disorder can last 6 to 12 months. Approximately two-thirds of people with MDD think about suicide, and 10 to 15% commit suicide. MDD is a chronic relapsing disease; the recurrence rate after the first episode is about 50%, 70% after the second episode and 90% after the third episode.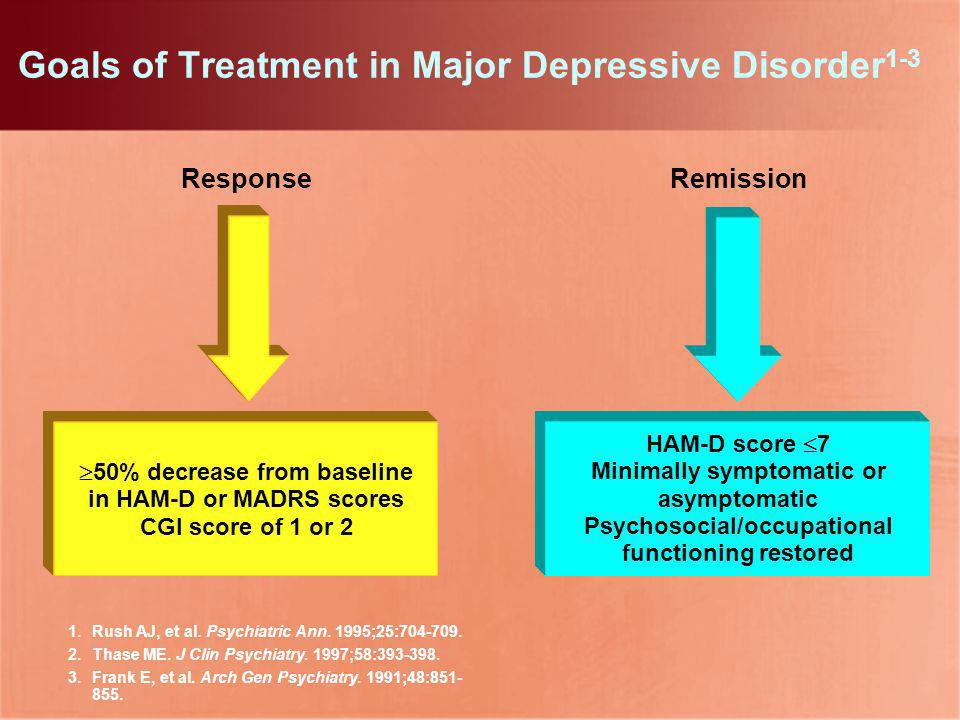 Approximately 5-10% of people with MDD develop bipolar disorder.
Approximately 5-10% of people with MDD develop bipolar disorder.
Patients with mild episodes, no psychotic symptoms, improved adherence, a reliable support system, and adequate premorbid functioning have a positive prognosis for MDD. In the presence of a concomitant mental disorder, personality disorder, multiple hospitalizations and advanced age, the prognosis is poor.
Complications
MDD is one of the leading causes of disability in the world. This not only causes severe functional impairment, but also negatively affects interpersonal relationships, reducing the quality of life. Individuals with MDD are at significant risk of developing comorbid anxiety and drug use disorders, which increase the risk of suicide.
Diabetes, hypertension, chronic obstructive pulmonary disease and coronary heart disease may be aggravated by depression. People who are depressed are more likely to engage in self-destructive behavior as a coping method. Left untreated, MDD can be quite debilitating.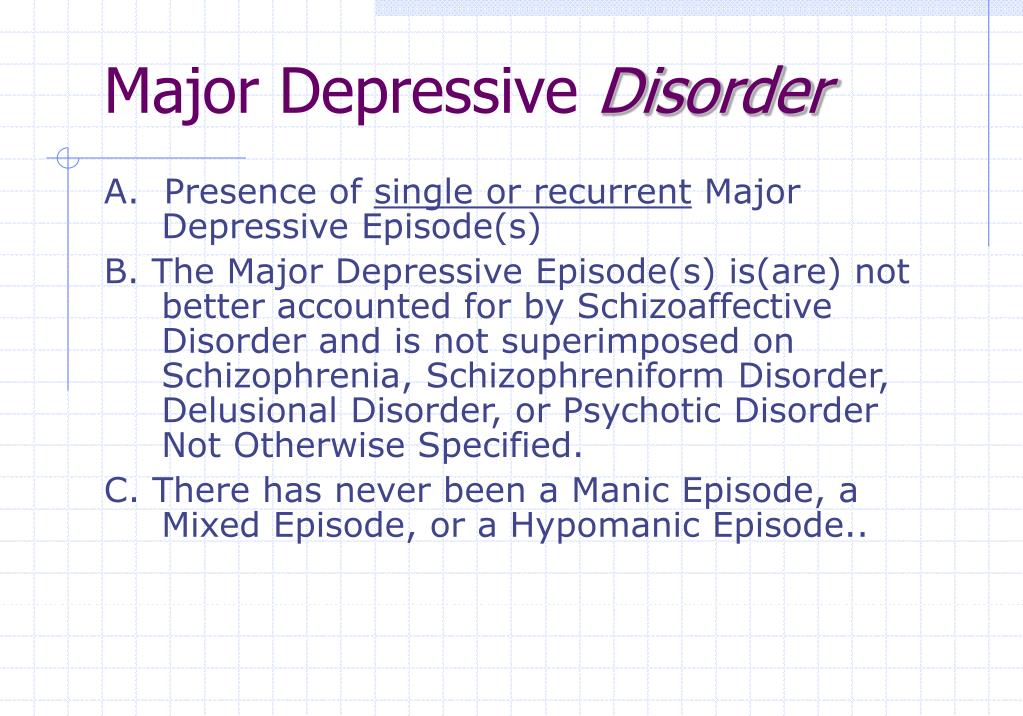
Findings
In 2008, WHO classified major depressive disorder (MDD) as the third leading cause of disease burden worldwide and is expected to be number one by 2030.
Diagnosis is made when a person has a persistently low or depressed mood, anhedonia (loss of interest in pleasure), feelings of guilt or worthlessness, lack of energy, poor concentration, changes in appetite, psychomotor retardation or agitation, trouble sleeping, or suicidal thoughts.
Effective and successful treatment of MDD requires a multidisciplinary approach. These collaborative services include primary care physicians and psychiatrists, as well as nurses, therapists, social workers and caregivers. Screening for depression in primary care settings is critical.
Major depressive disorder | is... What is Major Depressive Disorder?
Request "BDR" is redirected here; see also other meanings.
Major depressive disorder (MDD, clinical depression) - Unlike ordinary depression, which refers to almost any bad or depressed, dreary mood, major depressive disorder is a complex of symptoms. Moreover, MDD may not be accompanied by bad mood, depression or melancholy at all - the so-called depression without depression , or masked depression , somatized depression .
Moreover, MDD may not be accompanied by bad mood, depression or melancholy at all - the so-called depression without depression , or masked depression , somatized depression .
|
Contents
|
Historical information
The modern concept of depression is similar to the older concept of melancholia. Concept melancholy originates from "black bile", one of the "four moods" described by Hippocrates.
In the Middle Ages, however, many of the scientific achievements of ancient doctors were lost, and Major depressive disorder was long regarded as "devil possession".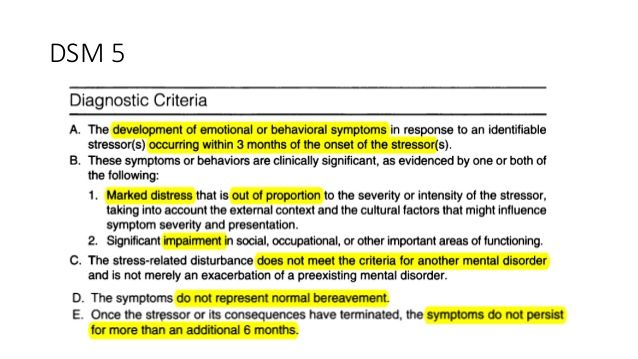 Appropriate treatment was offered: rites of exorcism, fasting or fasting, prayers. Patients with severe depressive arousal (agitation) were asked to be tied up and subjected to beatings. The revival of the approach to depression as a disease requiring medical intervention and treatment, and not rites of exorcism, began only in the late Middle Ages, during the era of the Renaissance and the growing interest in antiquity and its achievements.
Appropriate treatment was offered: rites of exorcism, fasting or fasting, prayers. Patients with severe depressive arousal (agitation) were asked to be tied up and subjected to beatings. The revival of the approach to depression as a disease requiring medical intervention and treatment, and not rites of exorcism, began only in the late Middle Ages, during the era of the Renaissance and the growing interest in antiquity and its achievements.
Symptoms and Diagnosis
If the symptoms described below last more than two weeks and begin to interfere with normal life, work or school, social functioning, then suspect MDD or a depressive syndrome, such as that associated with bipolar affective disorder.
- depressed mood most of the day or all day;
- loss of interest and pleasure;
- decreased energy and increased fatigue;
- reduced ability to concentrate and attention, indecision;
- decreased self-esteem and self-confidence;
- ideas of guilt and self-abasement;
- gloomy and pessimistic vision of the future;
- ideas or actions that lead to self-harm or suicide;
- disturbed sleep;
- disturbed appetite.
- weight loss (sometimes even with normal appetite).
The World Health Organization has developed a screening tool (rapid screening) to identify and determine the severity of major depressive disorder - a self-assessment test, the so-called major depression questionnaire [1] .
In 2012, transcriptome biomarkers specific for adolescents with major depressive disorder were detected in blood cells [2] . In addition, a partially overlapping set of biomarkers was found to distinguish between MDD and an anxiety disorder. If these results are confirmed in larger studies, in addition to a new approach to the diagnosis of MDD, this may lead to the development of individualized approaches to treatment.
Prevalence and causes
At least 16% of the population, according to sociological surveys, have experienced conditions that meet the ICD-10 diagnostic criteria for MDD at least once in their lives. However, less than half of the people who have experienced such conditions have sought or are seeking medical and/or psychological help and received an official diagnosis. Often patients try to remain silent about the symptoms of depression. Many are afraid of prescribing antidepressants and their side effects; some believe that keeping emotions under control is their own business, and not the care of a doctor; there are also fears that a mention of a case of depression will get into the medical record and somehow become known to the employer; finally, some are afraid of being referred to a psychiatrist for treatment. This suggests that therapists should make more use of screening tools, including short questionnaires, in cases that do not exclude depression. [3]
Often patients try to remain silent about the symptoms of depression. Many are afraid of prescribing antidepressants and their side effects; some believe that keeping emotions under control is their own business, and not the care of a doctor; there are also fears that a mention of a case of depression will get into the medical record and somehow become known to the employer; finally, some are afraid of being referred to a psychiatrist for treatment. This suggests that therapists should make more use of screening tools, including short questionnaires, in cases that do not exclude depression. [3]
Clinical depression is one of the leading causes of temporary disability in the United States and other developed countries today.
Major depressive disorder is also more common among the population of large cities and metropolitan areas compared with the population of small cities, towns and villages, more often among the population of developed countries than backward and developing ones.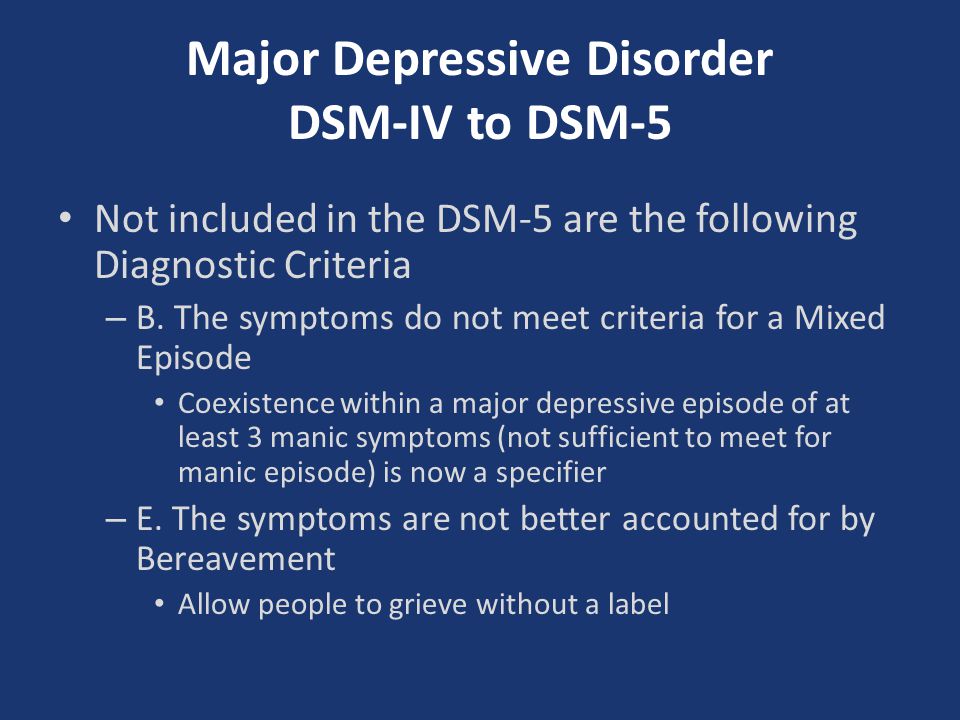 Probably, this difference is largely due to better diagnostics, a higher level of medicine and health care, and greater awareness of the population of developed countries and especially large cities about what depression is, and, as a result, more frequent visits to doctors. But crowding and overcrowding in large cities, a faster pace of life, higher levels of social demands, and more stress also seem to play a role in the greater prevalence of major depression in developed countries and in large cities.
Probably, this difference is largely due to better diagnostics, a higher level of medicine and health care, and greater awareness of the population of developed countries and especially large cities about what depression is, and, as a result, more frequent visits to doctors. But crowding and overcrowding in large cities, a faster pace of life, higher levels of social demands, and more stress also seem to play a role in the greater prevalence of major depression in developed countries and in large cities.
Major depressive disorder also occurs with increased frequency among people who are often stressed - for example, the unemployed, people with poor socioeconomic status (low-paid, homeless), people working in a difficult, boring, monotonous, unloved or uninteresting work, at work associated with an increased amount of stress and neuropsychic overload (like top managers). Often (but not always) MDD develops after a traumatic event, such as job loss, bankruptcy, serious illness or death of a loved one or loved one, divorce, moving to a new place with the loss of all previous social ties, etc.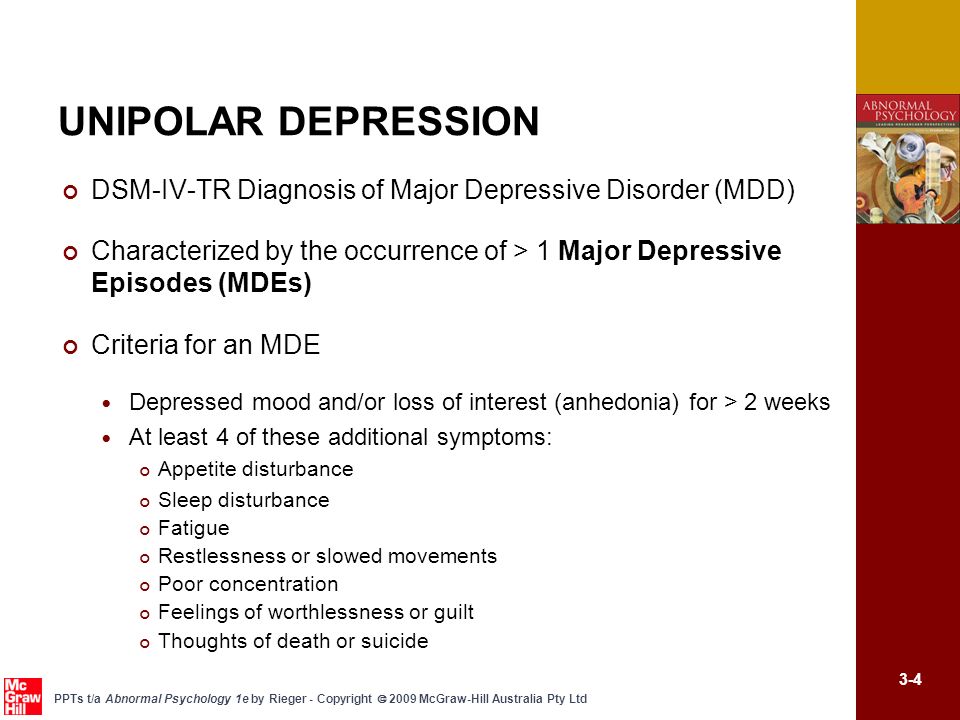 But often it develops and by itself, for no apparent reason, or from insignificant, at first glance, stress.
But often it develops and by itself, for no apparent reason, or from insignificant, at first glance, stress.
An increased incidence of clinical depression occurs in patients who have suffered or are suffering from migraine [4] [5] .
A large role in the development of MDD in adolescents and adults is played by the conditions in which this person grew and developed in childhood. It has been shown that in persons who were abused in childhood, adolescence or adolescence (physical abuse: tugging, slapping, slapping, beating, sexual seduction, rape - and/or psychological abuse: swearing, nagging by a parent (parents), explicit or veiled verbal or behavioral provocations on the part of a parent (parents) or other adult (adults) in relation to a child or adolescent in order to cause him or her feelings of guilt, shame, own inferiority, worthlessness), in adulthood, programming for stressful and depressive reactions, constant expectation of something bad; the “background” level of the stress hormone cortisol is elevated compared to the norm, and there is a sharper rise in cortisol levels with even minor stress than in the norm, and than in people who have been stressed and mistreated as adults and have matured.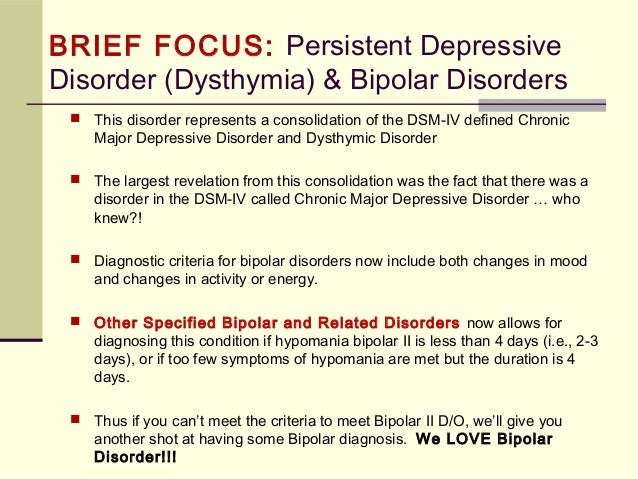 In these people, the incidence of "major depression" is more than 3 times the average frequency in the general population. Conversely, among patients with MDD, there is an increased proportion of people who were subjected to some form of violence, humiliation or maltreatment in childhood, adolescence or adolescence [6] Also, with an increased frequency, "major depression" develops in people whose relatives (especially immediate ones) suffered or suffer from such affective disorders as bipolar affective disorder, schizoaffective disorder and some other mental illnesses. This indicates the important role of hereditary, genetic predisposition in the development of major depression and the possible presence of common mechanisms for the development of a number of mental disorders that have an affective component in their composition.
In these people, the incidence of "major depression" is more than 3 times the average frequency in the general population. Conversely, among patients with MDD, there is an increased proportion of people who were subjected to some form of violence, humiliation or maltreatment in childhood, adolescence or adolescence [6] Also, with an increased frequency, "major depression" develops in people whose relatives (especially immediate ones) suffered or suffer from such affective disorders as bipolar affective disorder, schizoaffective disorder and some other mental illnesses. This indicates the important role of hereditary, genetic predisposition in the development of major depression and the possible presence of common mechanisms for the development of a number of mental disorders that have an affective component in their composition.
A number of adherents of the so-called psychoanalytic theory at one time completely denied the importance of hereditary predisposition, genetic and biochemical factors in the development of MDD.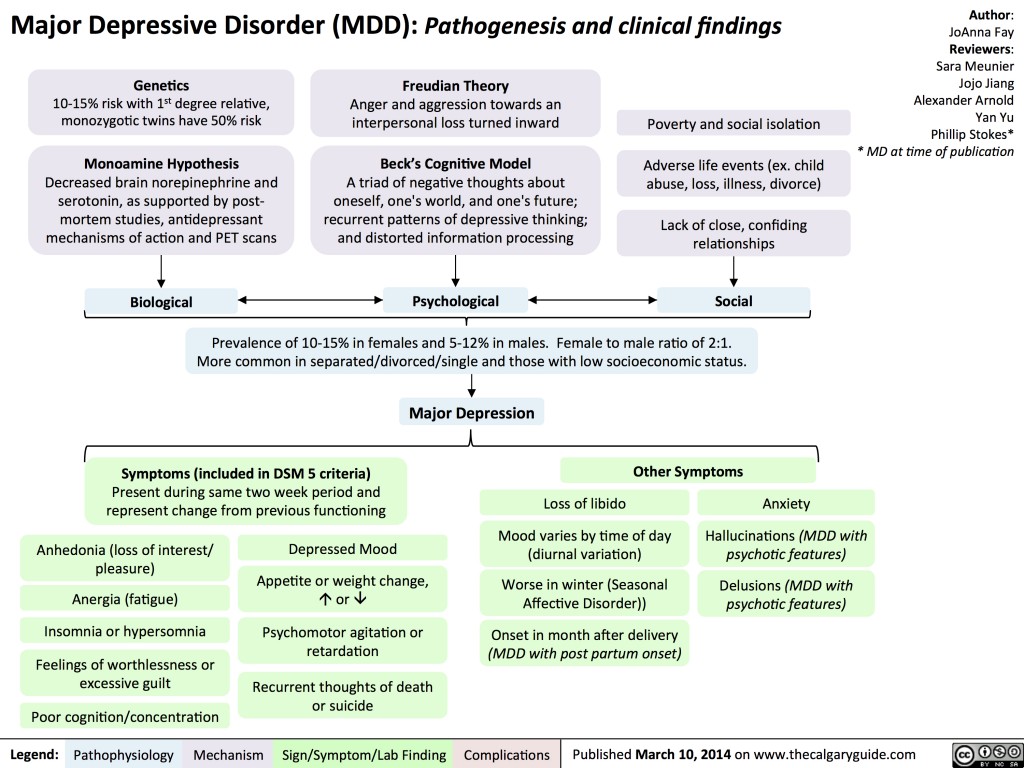 Proponents of the psychoanalytic theory of the origin of depression attached primary importance to childhood and adolescent psychotrauma, imprinting, and programming for stress. At the same time, a number of so-called biological psychiatrists completely denied the importance of childhood psychotrauma for the onset and development of "major depression" in an adult individual. The main importance in the biological theory of depression was given to genetic disorders and biochemical defects, as well as current or recent stress as a precipitating factor.
Proponents of the psychoanalytic theory of the origin of depression attached primary importance to childhood and adolescent psychotrauma, imprinting, and programming for stress. At the same time, a number of so-called biological psychiatrists completely denied the importance of childhood psychotrauma for the onset and development of "major depression" in an adult individual. The main importance in the biological theory of depression was given to genetic disorders and biochemical defects, as well as current or recent stress as a precipitating factor.
At present, it is generally accepted that the truth lies in the middle: in the development of any depression, hereditary and genetic factors are involved in different proportions, creating a predisposition to depression, reduced resistance to stress, and imprinting in childhood (which also creates a predisposition, programming for stressful and depressive reactions), and current chronic or recent acute stress as a trigger for depression.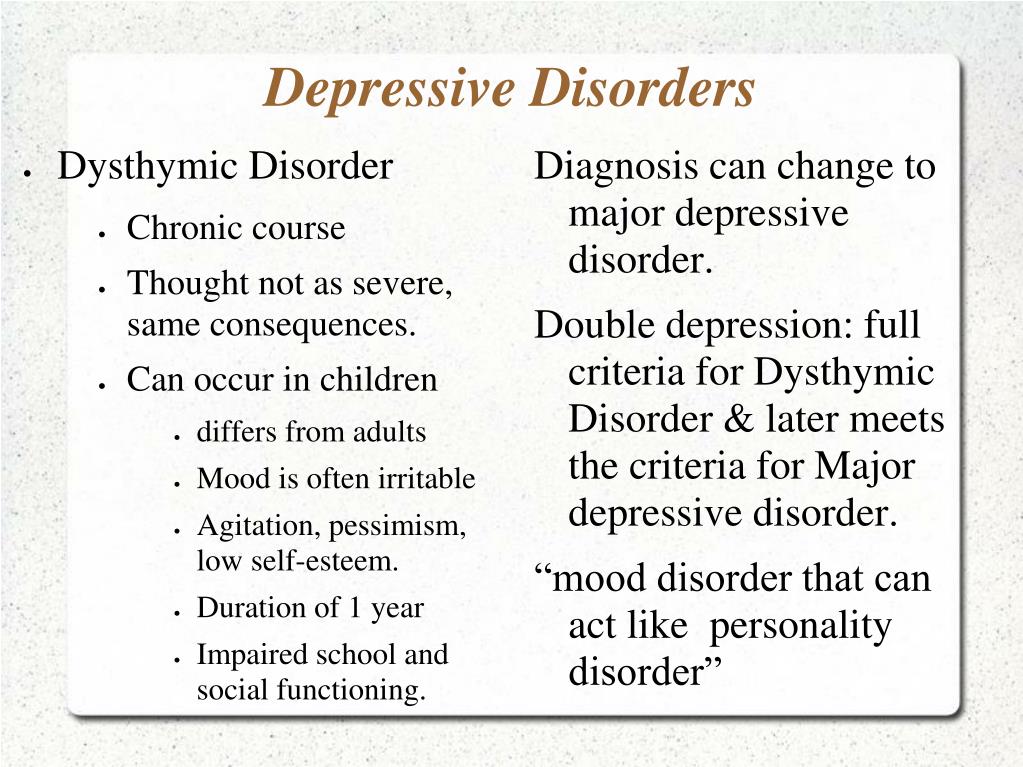 It is wrong to deny or underestimate the significance of any of these factors and reduce the complex, multifactorial pathogenetic mechanism leading to the development of depression to the influence of only one of the factors.
It is wrong to deny or underestimate the significance of any of these factors and reduce the complex, multifactorial pathogenetic mechanism leading to the development of depression to the influence of only one of the factors.
The importance of professional help
Because a person who has not experienced clinical depression himself or has not come close enough to it, it is not easy to understand its seriousness, he often perceives it as just a "bad mood". But major depression is a syndrome of concurrent symptoms that is much more than just sadness or low mood. A number of biological measurements, including measurements of the level of neurotransmitters in the brain, have shown that in depression there are serious changes in brain biochemistry and a general decrease in brain activity.
One consequence of this lack of understanding is that depressed patients are often criticized for being weak-willed and "unwilling to help themselves." But it is in the very nature of depression to influence a person's thoughts and actions in such a way that he becomes unable to do anything to improve his condition.
In connection with this preconceived notion, it should be emphasized that it is essential for the depressed patient to seek professional help. Without treatment, depression tends to progressively worsen, punctuated by temporary episodes of stabilization. Left untreated, depression usually develops in six months to two years before becoming chronic, lasting many years (if not lifelong) and difficult to treat. In the treatment of uncomplicated MDD, often (but not always) negative symptoms can disappear in a few weeks.
In a state of clinical depression, a person can harm himself socially (losing relationships with other people), professionally (losing his job), financially and even physically (up to suicide). Treatment can significantly reduce the likelihood of such damage, including reducing the risk of suicide, which can otherwise be a tragic but very common outcome. Therefore, the treatment of MDD is very productive, and sometimes vital.
Critically important in the treatment of clinical depression is the combination of pharmacotherapy (treatment with medications - antidepressants) with the actual psychotherapeutic work - namely, the study of mental states and personal reactions to these states.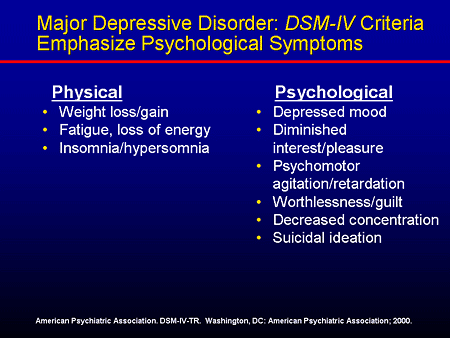 Such a study can be carried out by the attending psychotherapist or a specially trained psychologist. The essence of such work is to involve the patient in his own healing and in the prevention of opposition, resistance (which can occur in addition to the patient's consciousness) to the ongoing treatment.
Such a study can be carried out by the attending psychotherapist or a specially trained psychologist. The essence of such work is to involve the patient in his own healing and in the prevention of opposition, resistance (which can occur in addition to the patient's consciousness) to the ongoing treatment.
See also
- Depression
- Minor depression
- Manic-depressive psychosis
- Antidepressants
Literature
- Tiganov AS, Snezhnevsky AV, et al. Manual of psychiatry / Ed. Academician of the Russian Academy of Medical Sciences A. S. Tiganov. - M .: Medicine, 1999. - T. 1. - S. 555-635. — 712 p. — ISBN 5-225-02676-1
In the Brockhaus-Efron Encyclopedic Dictionary
- Melancholy // Brockhaus and Efron Encyclopedic Dictionary: In 86 volumes (82 volumes and 4 additional). - St. Petersburg, 1890-1907.
- Taedium vitae // Encyclopedic Dictionary of Brockhaus and Efron: In 86 volumes (82 volumes and 4 additional).
 - St. Petersburg, 1890-1907.
- St. Petersburg, 1890-1907.
Notes
- ↑ Bech P, Rasmussen N-A, Olsen LR, Noerholm V, Abildgaard W (August 2001). "The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity" 66 (2): 159-164. DOI:10.1016/S0165-0327(00)00309-8.
- ↑ K Pajer et al. (2012). "Discovery of blood transcriptomic markers for depression in animal models and pilot validation in subjects with early-onset major depression". Translational Psychiatry 2 (e101). DOI:10.1038/tp.2012.26.
- ↑ Robert A. Bell, PhD, Peter Franks, MD, Paul R. Duberstein, PhD, Ronald M. Epstein, MD, Mitchell D. Feldman, MD, MPhil, Erik Fernandez y Garcia, MD, MPH and Richard L. Kravitz, MD, MSPH (2011). Suffering in Silence: Reasons for Not Disclosing Depression in Primary Care. Annals of Family Medicine 9 : 439-446.