Adverse effects of ssris
Side effects - Selective serotonin reuptake inhibitors (SSRIs)
The side effects of selective serotonin reuptake inhibitors (SSRIs) can be troublesome at first, but most improve with time.
In general, SSRIs are better tolerated than most other types of antidepressants. The majority of people will only experience a few mild side effects when taking them.
It's important to persist with treatment, even if you're affected by side effects, as it will take several weeks before you begin to benefit from treatment. With time, you should find that the benefits of treatment outweigh problems related to side effects.
You'll usually see your doctor every few weeks when you first start taking SSRIs to discuss how well the medicine is working. However, you can contact your doctor at any point if you experience any particularly troublesome or persistent side effects.
For information about the side effects of a particular SSRI, check the information leaflet that comes with your medicine.
Common side effects
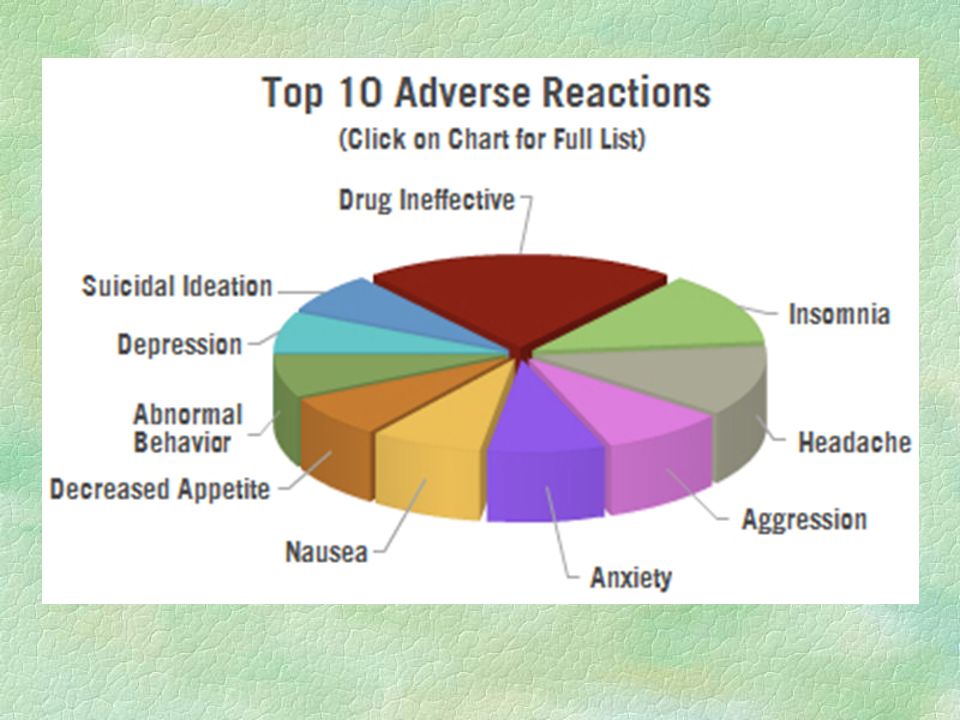
Common side effects of SSRIs can include:
- feeling agitated, shaky or anxious
- feeling or being sick
- indigestion
- diarrhoea or constipation
- loss of appetite and weight loss
- dizziness
- blurred vision
- dry mouth
- excessive sweating
- sleeping problems (insomnia) or drowsiness
- headaches
- loss of libido (reduced sex drive)
- difficulty achieving orgasm during sex or masturbation
- in men, difficulty obtaining or maintaining an erection (erectile dysfunction)
These side effects should improve over time, although some – such as sexual problems – can persist.
Less common side effects
Less common side effects of SSRIs can include:
- bruising or bleeding easily, including vomiting blood or bleeding from your bottom
- confusion
- movement problems, such as stiffness or shaking
- seeing or hearing things that aren't real (hallucinations)
- being unable to pee
Contact 111 or go to A&E immediately if you have any of these symptoms.
Serotonin syndrome
Serotonin syndrome is an uncommon, but potentially serious, set of side effects linked to SSRIs.
Serotonin syndrome occurs when the levels of a chemical in your brain called serotonin become too high. It's usually triggered when you take an SSRI in combination with another medicine (or substance) that also raises serotonin levels, such as another antidepressant or St John's wort.
It's usually triggered when you take an SSRI in combination with another medicine (or substance) that also raises serotonin levels, such as another antidepressant or St John's wort.
Symptoms of serotonin syndrome can include:
- confusion
- agitation
- muscle twitching
- sweating
- shivering
- diarrhoea
If you experience these symptoms, you should stop taking the medicine and seek immediate advice from your GP or specialist. If this isn't possible, call NHS 111.
Symptoms of severe serotonin syndrome include:
- a high temperature of 38C or above
- seizures (fits)
- irregular heartbeat (arrhythmia)
- loss of consciousness
If you or someone you know experiences symptoms of severe serotonin syndrome, seek emergency medical help immediately by dialling 999 and asking for an ambulance.
Hyponatraemia
Elderly people who take SSRIs may experience a severe fall in sodium (salt) levels known as hyponatremia. This may lead to a build-up of fluid inside the body's cells, which can be potentially dangerous.
This side effect occurs because SSRIs can block the effects of a hormone that helps to regulate levels of sodium and fluid in the body. Elderly people are vulnerable because fluid levels become more difficult for the body to regulate.
Mild hyponatremia can cause symptoms similar to depression or side effects of SSRIs, such as:
- feeling sick
- headache
- muscle pain
- reduced appetite
- confusion
More severe hyponatremia can cause the following symptoms:
- feeling listless and tired
- disorientation
- agitation
- psychosis
- seizures (fits)
The most serious cases of hyponatremia can cause you to stop breathing or go into a coma.
If you suspect that you or someone in your care has mild hyponatremia, call your GP or contact 111 for advice and stop taking SSRIs for the time being.
If you suspect severe hyponatremia, call 999 to ask for an ambulance.
Hyponatremia can be treated by feeding a sodium solution into the body through an intravenous drip.
Suicidal thoughts
Some people have suicidal thoughts and a desire to self-harm when they first take SSRIs. Young people under 25 seem particularly at risk.
Contact your GP or go to hospital immediately if you have thoughts of killing or harming yourself at any time while you're taking SSRIs.
It may be useful to tell a relative or close friend that you've started taking antidepressants and ask them to read the leaflet that comes with your medicine.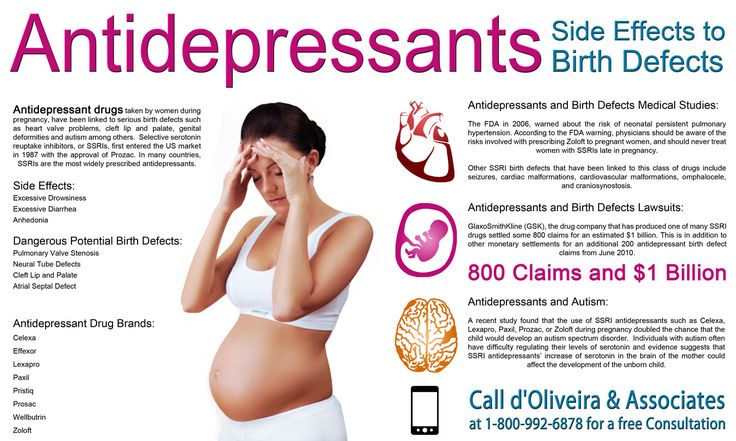 Ask them to tell you if they think your symptoms are getting worse, or if they're worried about changes in your behaviour.
Ask them to tell you if they think your symptoms are getting worse, or if they're worried about changes in your behaviour.
Reporting side effects
The Yellow Card Scheme allows you to report suspected side effects from any type of medicine you're taking. It's run by the medicines safety watchdog, the Medicines and Healthcare products Regulatory Agency (MHRA).
Page last reviewed: 8 December 2021
Next review due: 8 December 2024
Side effects - Antidepressants - NHS
The side effects of antidepressants can cause problems at first, but they generally improve with time.
It's important to continue treatment, even if you're affected by side effects, as it will take several weeks before you begin to benefit from treatment. With time, you should find that the benefits of treatment outweigh any problems from side effects.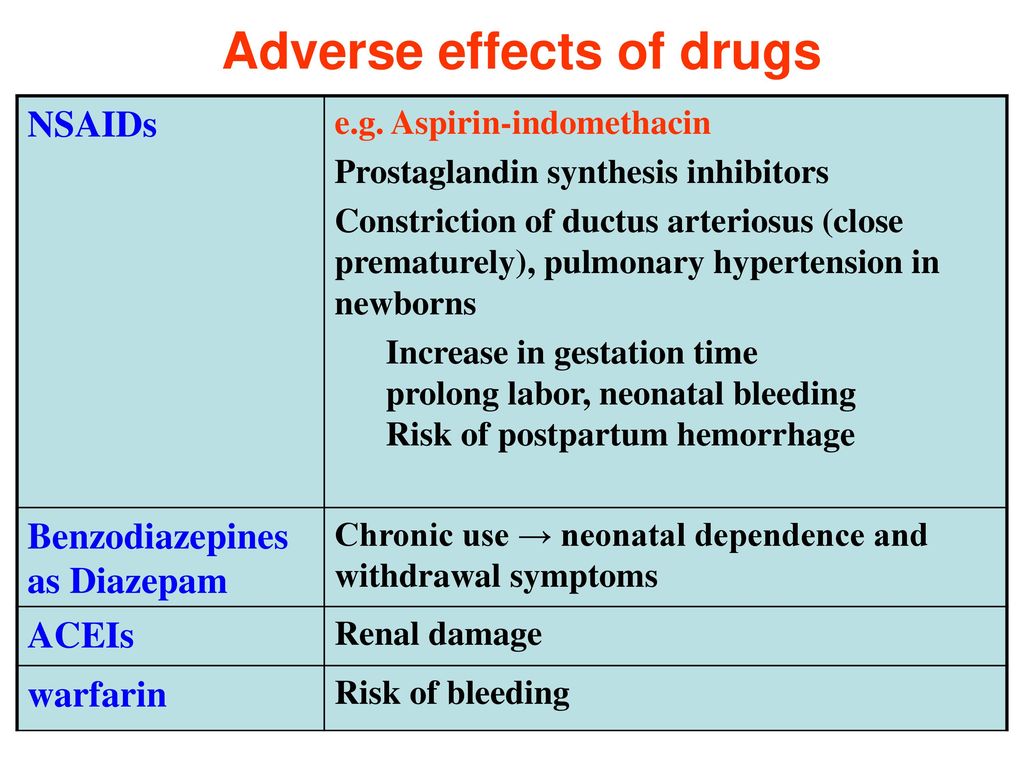
During the first few months of treatment, you'll usually see your doctor or a specialist nurse at least once every 2 to 4 weeks to see how well the medicine is working.
For more information about your specific medicine, see the patient information leaflet that comes with it.
SSRIs and SNRIs
Common side effects of selective serotonin reuptake inhibitors (SSRIs) and serotonin-noradrenaline reuptake inhibitors (SNRIs) can include:
- feeling agitated, shaky or anxious
- feeling and being sick
- indigestion and stomach aches
- diarrhoea or constipation
- loss of appetite
- dizziness
- not sleeping well (insomnia), or feeling very sleepy
- headaches
- loss of libido (reduced sex drive)
- difficulties achieving orgasm during sex or masturbation
- difficulties obtaining or maintaining an erection (erectile dysfunction)
These side effects should improve within a few weeks, although some can occasionally persist.
Tricyclic antidepressants (TCAs)
Common side effects of TCAs can include:
- dry mouth
- slight blurring of vision
- constipation
- problems passing urine
- drowsiness
- dizziness
- weight gain
- excessive sweating (especially at night)
- heart rhythm problems (arrhythmia), such as noticeable palpitations or a fast heartbeat (tachycardia)
The side effects should ease after a couple of weeks as your body begins to get used to the medicine.
Potential health risks
Serotonin syndrome
Serotonin syndrome is an uncommon, but potentially serious, set of side effects linked to SSRIs and SNRIs.
Serotonin syndrome occurs when the levels of a chemical called serotonin in your brain become too high. It's usually triggered when you take an SSRI or SNRI in combination with another medicine (or substance) that also raises serotonin levels, such as another antidepressant or St John's wort.
Symptoms of serotonin syndrome can include:
- confusion
- agitation
- muscle twitching
- sweating
- shivering
- diarrhoea
If you experience these symptoms, you should stop taking the medicine and get immediate advice from your GP or specialist. If this is not possible, call NHS 111.
Symptoms of severe serotonin syndrome include:
- seizures (fits)
- irregular heartbeat (arrhythmia)
- unconsciousness
If you experience symptoms of severe serotonin syndrome, get emergency medical help immediately by dialling 999 to ask for an ambulance.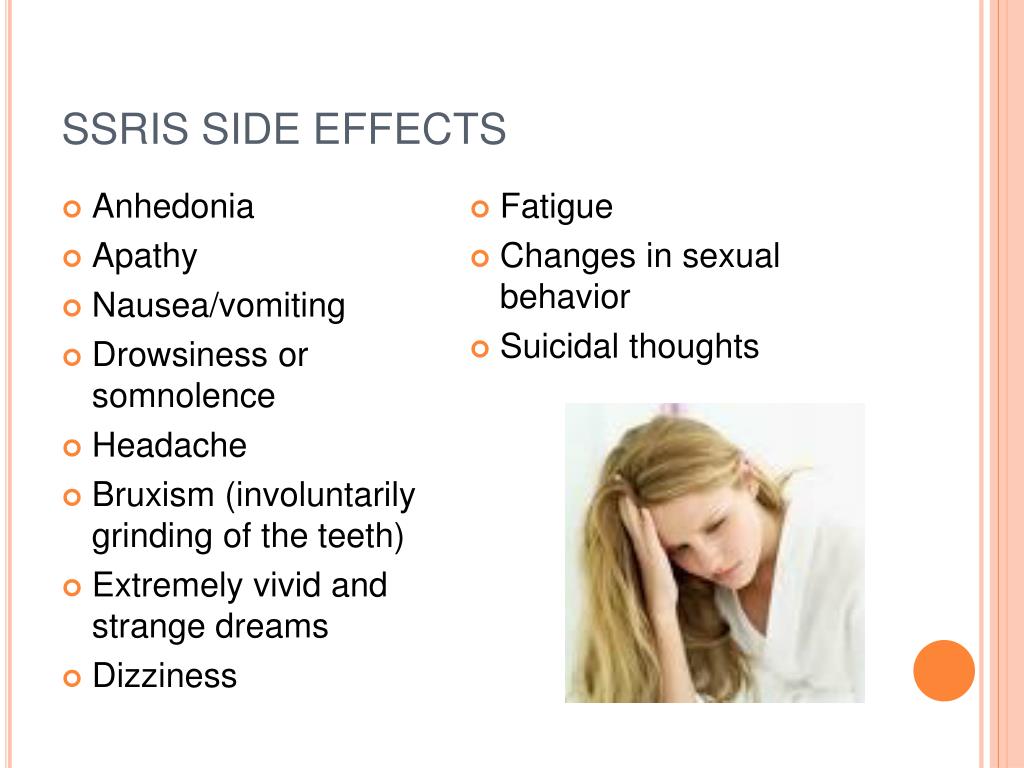
Hyponatraemia
Elderly people who take antidepressants, particularly those who take SSRIs, may experience a severe fall in sodium (salt) levels, known as hyponatraemia. This may lead to a build-up of fluid inside the cells of the body, which can be potentially dangerous.
This can happen because SSRIs can block the effects of a hormone that regulates levels of sodium and fluid in the body. Elderly people are vulnerable because fluid levels become more difficult for the body to regulate as people age.
Mild hyponatraemia can cause symptoms similar to depression or side effects of antidepressants, such as:
- feeling sick
- headache
- muscle pain
- reduced appetite
- confusion
More severe hyponatraemia can cause:
- feeling listless and tired
- disorientation
- agitation
- psychosis
- seizures (fits)
The most serious cases of hyponatraemia can cause you to stop breathing or enter a coma.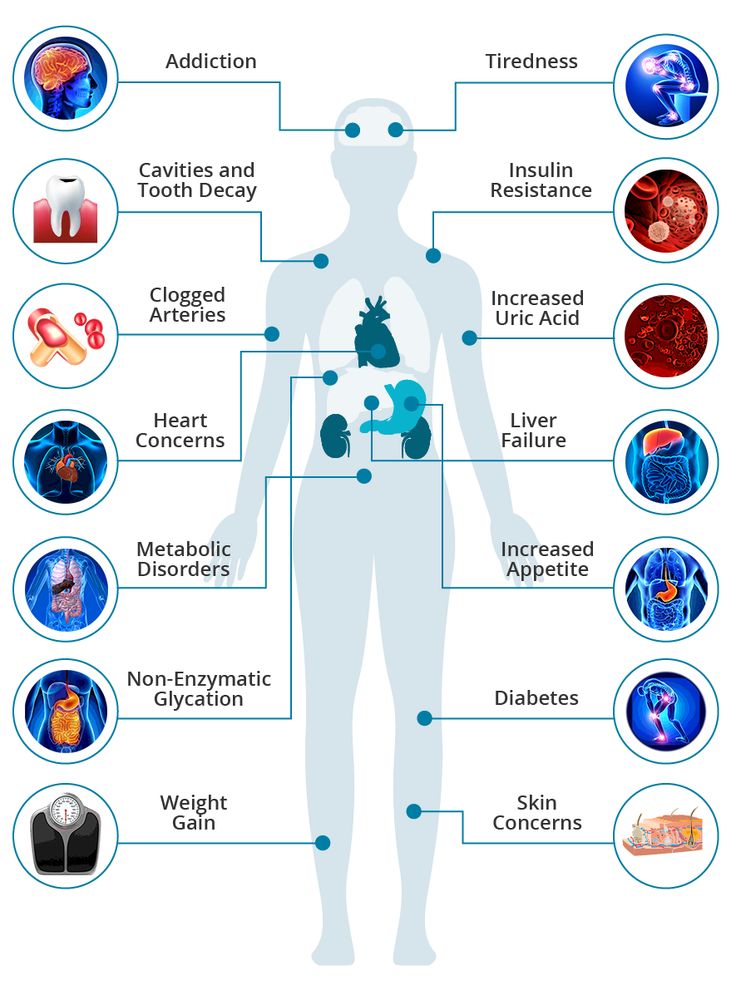
If you suspect mild hyponatraemia, you should call your GP for advice and stop taking SSRIs for the time being.
If you suspect severe hyponatraemia, call 999 and ask for an ambulance.
Hyponatraemia can be treated by feeding a sodium solution into the body through an intravenous drip.
Diabetes
Long-term use of SSRIs and TCAs has been linked to an increased risk of developing type 2 diabetes, although it's not clear if the use of these antidepressants directly causes diabetes to develop.
It may be that the weight gain some people using antidepressants experience increases the risk of them developing type 2 diabetes.
Suicidal thoughts
In rare cases, some people experience suicidal thoughts and a desire to self-harm when they first take antidepressants. Young people under 25 seem particularly at risk.
Contact your GP, or go to A&E immediately, if you have thoughts of killing or harming yourself at any time while taking antidepressants.
It may be useful to tell a relative or close friend if you've started taking antidepressants and ask them to read the leaflet that comes with your medicines. You should then ask them to tell you if they think your symptoms are getting worse, or if they're worried about changes in your behaviour.
Page last reviewed: 4 November 2021
Next review due: 4 November 2024
SIDE EFFECTS OF ANTIDEPRESSANTS (SSRIs) | Clinical Center "Psychiatry - Narcology"
Currently, the most commonly prescribed antidepressants are drugs from the group of selective serotonin reuptake inhibitors (SSRIs). For most, these medicines are safe and effective, but like all medicines, they can cause side effects. According to statistics, about 40% of patients taking antidepressants also experience side effects, in about 25% of cases they are quite unpleasant. Two of the most common side effects (sexual dysfunction and weight gain) are often the reason people stop taking these medications. nine0003
Two of the most common side effects (sexual dysfunction and weight gain) are often the reason people stop taking these medications. nine0003
Listed below are the 7 most common side effects of antidepressants that patients should be aware of:
1. SOMATIC SYMPTOMS.
When medications are first prescribed to treat depression, the most common physical symptoms are headache, nausea, joint and muscle pain, rash, and diarrhea. These symptoms are usually mild and temporary. The results of clinical studies have shown that nausea and headache are the most common. As a rule, these symptoms are adaptive in nature, as a rule, they pass on their own, without requiring discontinuation of the drug. nine0003
2. SLEEP DISTURBANCE.
Many patients, when first prescribed antidepressants, report problems with sleep: difficulty falling asleep or light sleep with frequent awakenings. Also, against the background of taking SSRIs, nightmares and sleepwalking can be observed.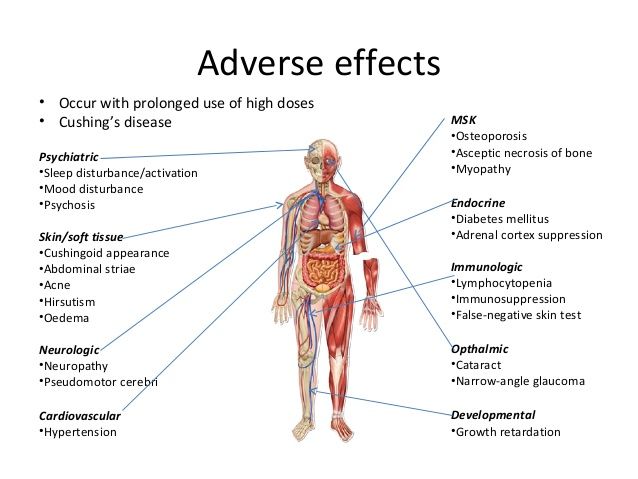 Studies have shown that about 22% of people taking antidepressants experience sleep problems.
Studies have shown that about 22% of people taking antidepressants experience sleep problems.
3. DAY SLEEPNESS .
Sleepiness during the day may be the result of a poor night's sleep, or the direct sedative effect of the antidepressant. In the case when it is a sedative effect, the problem can be solved by transferring the drug to the evening. nine0003
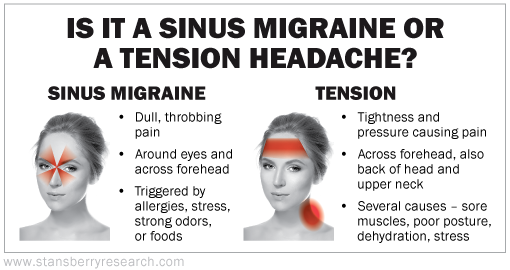
4. MIGRAINES
Due to the fact that people who are prone to depression also often suffer from migraines, you need to be careful when taking medications in combination. Medicines; used to treat migraines, triptans, like SSRIs, increase serotonin levels in the brain. If these drugs are used together, it can lead to the development of serotonin syndrome, which manifests itself in the form of headache, heart palpitations, hot flashes. Be sure to discuss with your doctor how to avoid the development of serotonin syndrome if you are prescribed medications of both groups. nine0003
5. WEIGHT SET.
WEIGHT SET.
Weight gain is one of the late side effects of antidepressants and is one of the most common reasons for refusing to continue taking or changing the drug. A good prevention of this side effect is moderate physical activity (for example, a 30-minute workout every other day). The likelihood of weight gain also depends on the drug that is prescribed. According to clinical trials, while taking paroxetine, about 25% of patients gain 7% of their weight. nine0003
6. SUICIDE .
The risk of suicide while taking antidepressants is currently under extensive investigation. According to most studies, compared with placebo, taking SSRIs or other antidepressants doubles the likelihood of suicidal thoughts. The overall risk of this side effect when taking antidepressants in adolescents and adults is 2 to 4 percent. One of the reasons for suicide while taking antidepressants is that medications increase activity, giving energy for the implementation of a suicidal plan. Regular follow-up by a doctor can reduce the risk of this side effect. nine0003
Regular follow-up by a doctor can reduce the risk of this side effect. nine0003
7. SEXUAL DYSFUNCTION.
Sexual dysfunction is one of the most common long-term side effects of SSRIs. These include decreased sexual desire, delayed ejaculation in men, and inability to achieve orgasm in women. Up to 60% of people taking SSRIs experience one of these side effects. And these are the side effects that patients are not ready to endure.
If you are concerned about any side effects, discuss them with your doctor. As a rule, you can find a solution for any of them. It is not recommended to stop taking medications on your own. nine0003
FGBNU NTsPZ. ‹‹Depression in General Medicine: A Guide for Physicians››
One of the main arguments in favor of the use of first-line antidepressants in the treatment of affective disorders in general medical practice is the minimal (compared to second-line drugs) severity of side effects.
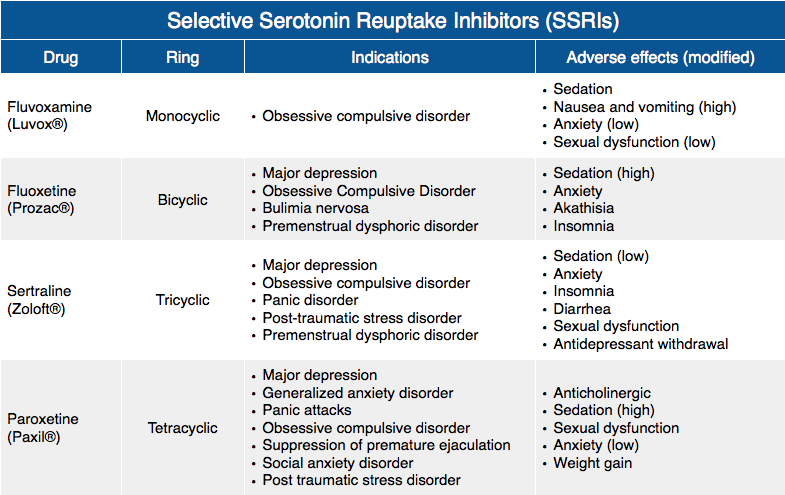
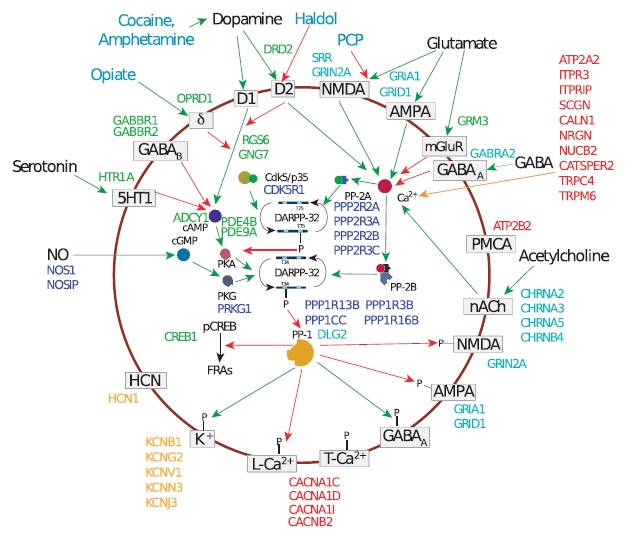
Differences in the complications of thymoanaleptic therapy are clearly seen when comparing the main manifestations of the undesirable effects of representatives of first-line antidepressants (SSRIs, SSOZS) and TCAs, which is clearly demonstrated by the data given in Table.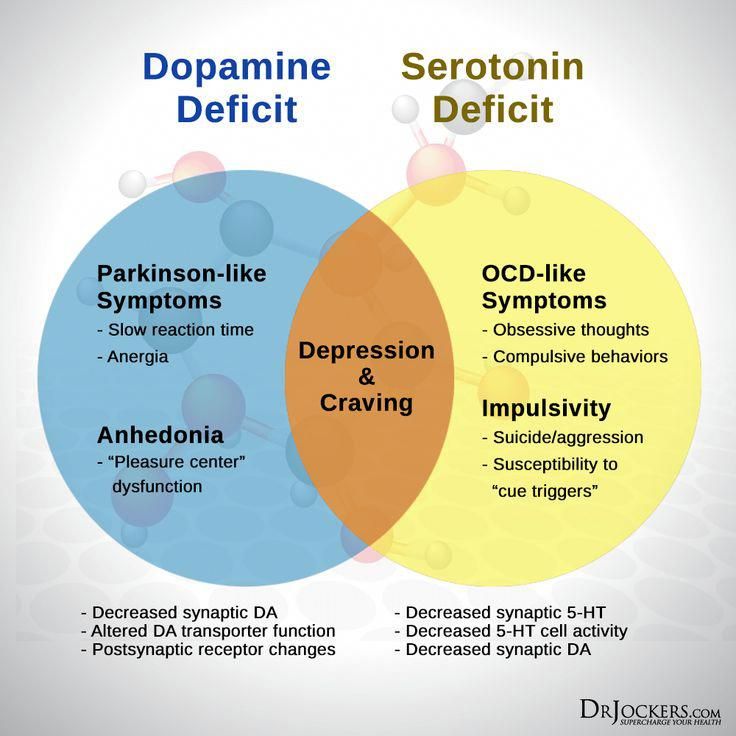 fourteen. nine0003
fourteen. nine0003
Nevertheless, it is impossible to completely exclude complications even when using sparing psychotropic drugs. The greatest likelihood of developing side effects of psychopharmacotherapy occurs in patients with somatic diseases, as well as in elderly people who show hypersensitivity to psychotropic drugs; in these contingents, even with careful dose titration, in addition to the main thymoanaleptic effect, side effects may also occur. nine0003
The main side effects of antidepressants include anticholinergic disorders of the central and autonomic nervous system, cardiovascular system, complications from the hematopoietic organs, metabolic and endocrine disorders (weight changes, sexual dysfunction, allergic reactions).
Side effects often appear in the initial stages of treatment (in the first 2 weeks) and sometimes persist for 3-4 weeks of therapy, and then reverse development. For more persistent and at the same time severe disorders, dose reduction is indicated, and, if necessary, therapy is discontinued.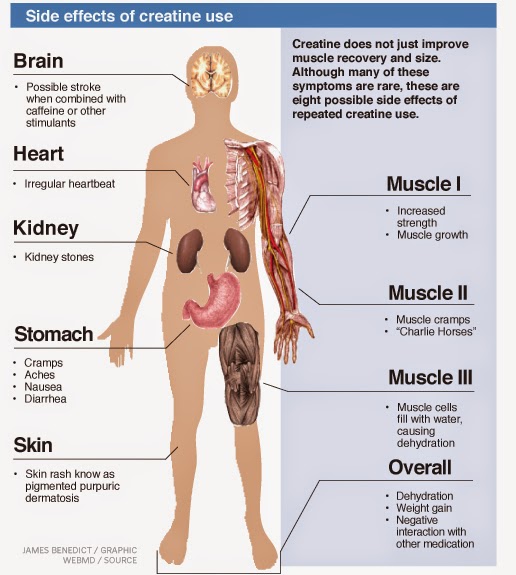 nine0003
nine0003
Treatment with tianeptine (SSOZS) is accompanied by a minimum of undesirable effects. Side effects of the drug are most often limited to complaints of dry mouth, nausea, and drowsiness during the day. Only in some cases, phenomena of transient orthostatic hypotension, dizziness, headaches, skin allergic reactions are also observed. The most common side effects of SSRIs are:
- nausea,
- dry mouth
- loss of appetite, nine0003
- vomit,
- diarrhea,
- constipation.
Along with this, undesirable effects from the autonomic and central nervous system are possible:
- dizziness,
headaches (citalopram)
- insomnia,
- increase (or appearance) of anxiety,
- nervousness
- a sense of inner tension.
The latter appear in the first weeks of treatment or with increasing doses. nine0003
There are transient extrapyramidal disorders in the form of tremor. As for other disorders (parkinsonism, akathisia, dyskinesias), judging by the data of a number of publications, they are recorded only in individual cases. The use of fluoxetine and paroxetine may be accompanied by increased bleeding and even bleeding.
As for other disorders (parkinsonism, akathisia, dyskinesias), judging by the data of a number of publications, they are recorded only in individual cases. The use of fluoxetine and paroxetine may be accompanied by increased bleeding and even bleeding.
During SSRI therapy, neurotoxic reactions (serotonin syndrome) affecting the gastrointestinal tract and nervous system are possible (colic in the abdomen , flatulence, loose stools, nausea, vomiting; tremor, dysarthria, muscle hypertonicity, hyperreflexia, myoclonic twitching, ataxia). In more severe cases, hyperthermia, confusion, symptoms of disorientation join [Malin D.I., 2000]. nine0003
Severe complications often occur in the process of drug interaction with combined use:
- SSRIs and MAOIs,
- SSRIs and OIMAO-A (moclobemide),
- TCA (anafranil) and OIMAO-A.
Along with side effects, the effects of antidepressants associated with overdose are of great importance (especially in the context of a general medical network).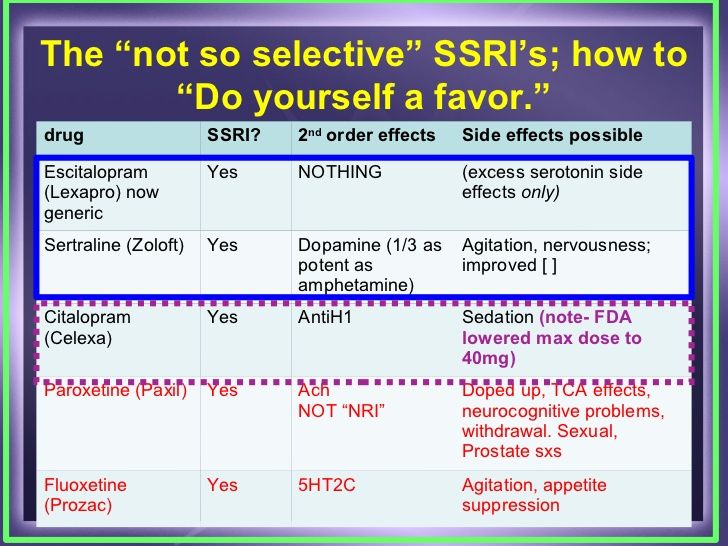 The risk of deliberately taking large amounts of drugs for suicidal purposes poses a safety advantage to first-line antidepressants. This is evidenced by comparative data on the safety of some first-line and second-line antidepressants, presented in Table. fifteen. nine0003
The risk of deliberately taking large amounts of drugs for suicidal purposes poses a safety advantage to first-line antidepressants. This is evidenced by comparative data on the safety of some first-line and second-line antidepressants, presented in Table. fifteen. nine0003
The safety of first-line drugs is indicated by the data of C. Las-mier et al. (1991) in relation to tianeptine. Taking large doses of this drug (from 12 to 60 tablets) (12 cases of suicidal use of tianeptine are summarized) does not lead to death and is not accompanied by significant (compared with the norm) deviations of the clinical and electrocardiological parameters of the cardiovascular system.
Table 15. Safety of antidepressants [based on R. Priest, D. Baldwin, 1994]
| Preparations | Hazard measure (number of deaths from overdose per 1 million prescriptions) | Degree of danger |
| First line antidepressants | ||
| Fluoxetine (Prozac) Fluvoxamine (Fevarin) Mianserin (Lerivon) | Less than 10 | Relatively dangerous |
| Second line antidepressants | ||
| Clomipramine (Anafranil) Maprotiline (Ludiomil) Trazadone (Tritgiko) | More than 10 | Potentially dangerous |
| Imipramine (Melipramine) Phenelzine (Nardil) | Over 20 | Dangerous |
| Amitriptyline Trianylcypramine (transamine) | Over 40 | Very dangerous |
With an overdose of milnacipran (ixel), vomiting, hyperventilation, and tachycardia are observed.