Adhd mood disorder
Mood Disorders & ADHD - HealthyChildren.org
The mood disorders most likely to be experienced by children with ADHD include dysthymic disorder, major depressive disorder (MDD), and bipolar disorder. Dysthymic disorder can be characterized as a chronic low-grade depression, persistent irritability, and a state of demoralization, often with low self-esteem. Major depressive disorder is a more extreme form of depression that can occur in children with ADHD and even more frequently among adults with ADHD. Dysthymic disorder and MDD typically develop several years after a child is diagnosed with ADHD and, if left untreated, may worsen over time. Bipolar disorder is a severe mood disorder that has only recently been recognized as occurring in children. Unlike adults who experience distinct periods of elation and significant depression, children with bipolar disorder present a more complex disturbance of extreme emotional instability, behavioral difficulties, and social problems.
There is significant overlap with symptoms of ADHD, and many children with bipolar disorder also qualify for a diagnosis of ADHD.
What to Look For
Every child feels discouraged or acts irritable once in a while. Children with ADHD, who so often must deal with extra challenges at school and with peers, may exhibit these behaviors more than most. If your child claims to be depressed, however, or seems irritable or sad a large portion of each day, more days than not, she may have a coexisting dysthymic disorder. To be diagnosed with dysthymic disorder, a child must also have at least 2 of the following symptoms:
- Poor appetite or overeating
- Insomnia or excessive sleeping
- Low energy or fatigue
- Low self-esteem
- Poor concentration or difficulty making decisions
- Feelings of hopelessness
Before dysthymic disorder can be diagnosed, children must have had these symptoms for a year or longer, although symptoms may have subsided for up to 2 months at a time within that year. The symptoms also must not be caused by another mood disorder, such as MDD or bipolar disorder, a medical condition, substance abuse, or just related to ADHD itself (low self-esteem stemming from poor functioning in school, for example). Finally, the symptoms must be shown to significantly impair your child’s social, academic, or other areas of functioning in daily life.
The symptoms also must not be caused by another mood disorder, such as MDD or bipolar disorder, a medical condition, substance abuse, or just related to ADHD itself (low self-esteem stemming from poor functioning in school, for example). Finally, the symptoms must be shown to significantly impair your child’s social, academic, or other areas of functioning in daily life.
Major depressive disorder is marked by a nearly constant depressed or irritable mood or a marked loss of interest or pleasure in all or nearly all daily activities. In addition to the symptoms listed previously for dysthymic disorder, a child with MDD may cry daily; withdraw from others; become extremely self-critical; talk about dying; or even think about, plan, or carry out a suicide attempt. Unlike the brief outbursts of temper exhibited by a child with ODD who does not get her way, a depressed child’s irritability may be nearly constant and not linked to any clear cause. Her inability to concentrate differs from ADHD-type inattention in that it is accompanied by other symptoms of depression, such as loss of appetite or loss of interest in favorite activities. Finally, the depression itself stems from no apparent cause—as opposed to being demoralized as a result of specific obstacles posed by ADHD or becoming depressed in response to parental divorce or any other stressful situation. (In fact, research has shown that the intactness of a child’s family and its socioeconomic status have little or no effect on whether a child develops MDD.) While children with ADHD/CD alone are not at higher than normal risk for attempting suicide, children with ADHD/CD who also have an MDD and are involved in substance abuse are more likely to make such an attempt and should be carefully watched.
Finally, the depression itself stems from no apparent cause—as opposed to being demoralized as a result of specific obstacles posed by ADHD or becoming depressed in response to parental divorce or any other stressful situation. (In fact, research has shown that the intactness of a child’s family and its socioeconomic status have little or no effect on whether a child develops MDD.) While children with ADHD/CD alone are not at higher than normal risk for attempting suicide, children with ADHD/CD who also have an MDD and are involved in substance abuse are more likely to make such an attempt and should be carefully watched.
Talk of suicide (even if you are not sure whether it is serious), a suicide attempt, self-injury, any violent behavior, or severe withdrawal should be considered an emergency that requires the immediate attention of your child’s pediatrician, psychologist, or local hospital.
A depressed child may admit to feeling guilty or sad, or she may deny having any problems.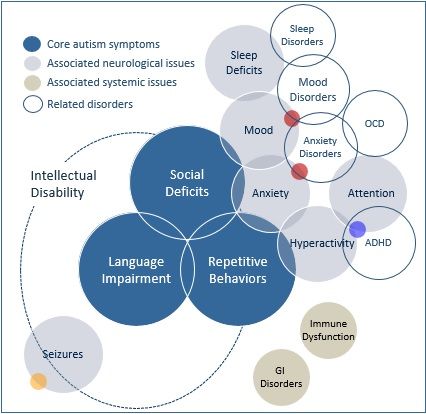 It is important to keep in mind the fact that many depressed children refuse to admit to their feelings, and parents often overlook the subtle behaviors that signal a mood disorder. By keeping in close contact with her teacher, bringing your child to each of her treatment reviews with her pediatrician, and including her in all discussions of her treatment as appropriate to her age, you can improve the chances that her pediatrician or mental health professional will detect any signs of developing depression, and that she will have someone to talk to about her feelings.
It is important to keep in mind the fact that many depressed children refuse to admit to their feelings, and parents often overlook the subtle behaviors that signal a mood disorder. By keeping in close contact with her teacher, bringing your child to each of her treatment reviews with her pediatrician, and including her in all discussions of her treatment as appropriate to her age, you can improve the chances that her pediatrician or mental health professional will detect any signs of developing depression, and that she will have someone to talk to about her feelings.
A child with bipolar disorder and ADHD is prone to explosive outbursts, extreme mood swings (high, low, or mixed mood), and severe behavioral problems. Such a child is often highly impulsive and aggressive, with prolonged outbursts typically “coming out of nowhere” or in response to trivial frustrations. She may have a history of anxiety. She may also have an extremely high energy level and may experience racing thoughts and inflated self-esteem or grandiosity, extreme talkativeness, physical and emotional agitation, overly sexual behavior, and/or a reduced need for sleep.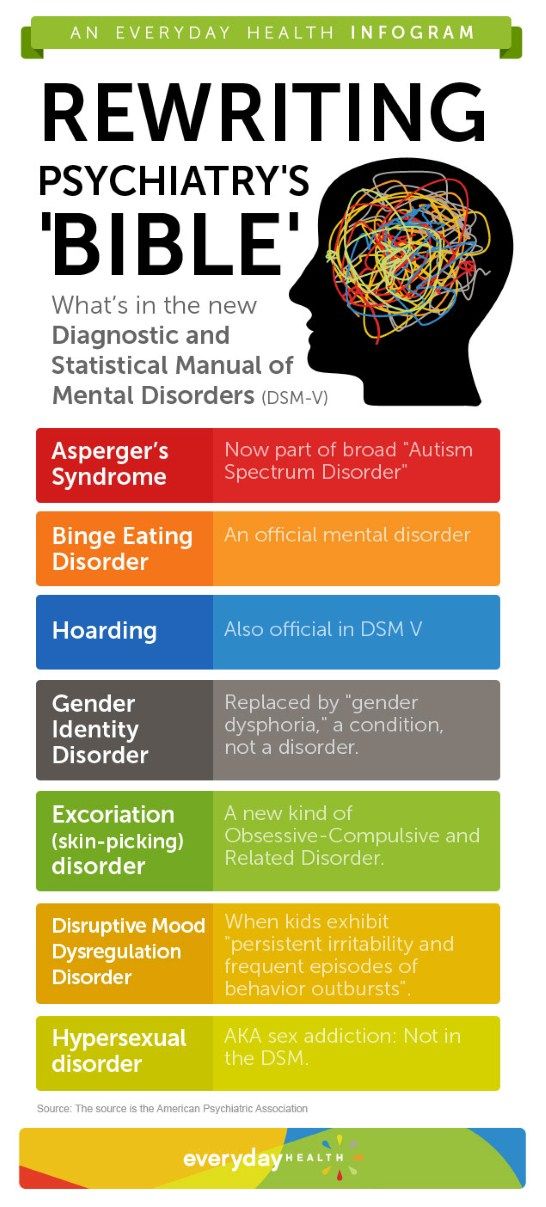 These symptoms can alternate with periods of depression or irritability, during which her behavior resembles that of a child with MDD. A child with ADHD/ bipolar disorder typically has poor social skills. Family relationships are often strained because of the child’s extremely unpredictable, aggressive, or defiant behavior. Early on the symptoms may only occur at home, but often begin to occur in other settings as the child gets older. Bipolar disorder is a
serious psychiatric disorder that can sometimes include psychotic symptoms (delusions/hallucinations) or self-injurious behavior such as cutting, suicidal thoughts/impulses, and substance abuse. Many children with bipolar disorder have a family history of bipolar disorder, mood disorder, ADHD, and/or substance abuse. Children with ADHD and bipolar disorder are at higher risk than those with ADHD alone for substance abuse and other serious problems during adolescence.
These symptoms can alternate with periods of depression or irritability, during which her behavior resembles that of a child with MDD. A child with ADHD/ bipolar disorder typically has poor social skills. Family relationships are often strained because of the child’s extremely unpredictable, aggressive, or defiant behavior. Early on the symptoms may only occur at home, but often begin to occur in other settings as the child gets older. Bipolar disorder is a
serious psychiatric disorder that can sometimes include psychotic symptoms (delusions/hallucinations) or self-injurious behavior such as cutting, suicidal thoughts/impulses, and substance abuse. Many children with bipolar disorder have a family history of bipolar disorder, mood disorder, ADHD, and/or substance abuse. Children with ADHD and bipolar disorder are at higher risk than those with ADHD alone for substance abuse and other serious problems during adolescence.
If your child has ADHD with coexisting bipolar disorder, her pediatrician will generally refer her to a child psychiatrist for further assessment, diagnosis, and recommendations for treatment.
Treatment
As with ADHD with anxiety disorders, treatment of ADHD with depression usually involves a broad approach. Treatment approaches may include a combination of cognitive-behavioral therapy, interpersonal therapy (focusing on areas of grief, interpersonal relationships, disputes, life transitions, and personal difficulties), traditional psychotherapy (to help with self-understanding, identification of feelings, improving self-esteem, changing patterns of behavior, interpersonal interactions, and coping with conflicts), as well as family therapy when needed.
Medication management approaches, as with ADHD and other coexisting conditions, include treating the most disabling condition first. If your child’s ADHD-related symptoms are causing most of her functioning problems, or the signs of depression are not completely clear, your child’s pediatrician is likely to start with stimulant medication to treat the ADHD. In cases when the depressive symptoms turn out to stem from poor functioning due to ADHD and not to a depressive disorder, they may diminish as the ADHD symptoms improve. If the ADHD and depressive symptoms improve, your child’s pediatrician will probably maintain stimulant treatment
alone. If her ADHD symptoms improve but her depression remains the same, even after a reasonable trial of the type of broad psychotherapeutic approach described previously, her pediatrician may add another medication, most commonly an SSRI—a class of medications including Prozac, Zoloft, Paxil, Luvox, and Celexa. Selective serotonin reuptake inhibitors can make the symptoms of bipolar disorder worse, so a careful evaluation must be completed before starting medication. If this approach is unsuccessful, you may be referred to a developmental/behavioral pediatrician or a psychiatrist, who may try other classes of medications.
If the ADHD and depressive symptoms improve, your child’s pediatrician will probably maintain stimulant treatment
alone. If her ADHD symptoms improve but her depression remains the same, even after a reasonable trial of the type of broad psychotherapeutic approach described previously, her pediatrician may add another medication, most commonly an SSRI—a class of medications including Prozac, Zoloft, Paxil, Luvox, and Celexa. Selective serotonin reuptake inhibitors can make the symptoms of bipolar disorder worse, so a careful evaluation must be completed before starting medication. If this approach is unsuccessful, you may be referred to a developmental/behavioral pediatrician or a psychiatrist, who may try other classes of medications.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
ADHD Vs Bipolar Disorder Symptoms & Treatment
Emotional dysregulation and moodiness are not included in the diagnostic criteria for ADHD – a detrimental omission, according to many researchers and clinicians. The reality is that children and adults with ADHD commonly experience irritability, low frustration tolerance, and mood lability – emotional symptoms that have long factored into resulting treatment and management plans.
However, emotional dysregulation is not exclusive to attention deficit hyperactivity disorder (ADHD or ADD). Chronic moodiness is also a central component of mood disorders like bipolar disorder, which may complicate the evaluation, diagnosis, and treatment process, particularly for adult patients. Differentiating moodiness as it appears in ADHD, bipolar disorder, and similar disorders is critically important — and not always straightforward.
Emotional Dysregulation Across Disorders
Emotional dysregulation, while present in many conditions, shows up in different ways and in different grades of severity. Making the distinction between characteristics of moodiness in ADHD, ODD, DMDD, and other disorders often requires studying the mood’s intensity and the degree to which it disrupts the individual’s functioning.
Making the distinction between characteristics of moodiness in ADHD, ODD, DMDD, and other disorders often requires studying the mood’s intensity and the degree to which it disrupts the individual’s functioning.
ADHD
Chronic Irritability
Many individuals with ADHD report feeling easily irritated and frustrated. Minor frustrations at home, work, and/or school, can cause substantial irritability. (Social pressures outside of the home may keep individuals from lashing out in these settings.) A scenario warranting a 2 on a 10-point scale, for example, can often feel like a 7 or 9 to a person with ADHD. They can be quick to anger, as a result, and may lash out with angry outbursts or through passive-aggressive behaviors. Frustrations, however, are often over quickly. Some may feel upset or regretful later, once the emotional overreaction has subsided.
Oppositional Defiant Disorder (ODD)
ODD is one of the most common comorbidities seen with ADHD. Roughly one-third to one-half of children with ADHD also have ODD, characterized by disruptive, defiant, and irritable behavior. Children with ODD can be quick and impulsive, or sullen and sustained, with their oppositional behaviors toward authority figures. ODD usually becomes apparent around age 12 and lasts until the start of adulthood. Most patients outgrow ODD, but for some, it may turn into conduct disorder, which typically involves delinquent activity, physical aggression, violence, theft, and/or destruction of property.
Children with ODD can be quick and impulsive, or sullen and sustained, with their oppositional behaviors toward authority figures. ODD usually becomes apparent around age 12 and lasts until the start of adulthood. Most patients outgrow ODD, but for some, it may turn into conduct disorder, which typically involves delinquent activity, physical aggression, violence, theft, and/or destruction of property.
[ODD vs. ADHD: The Facts About Oppositional Defiant Disorder and Attention Deficit]
Disruptive Mood Dysregulation Disorder (DMDD)
DMDD is a relatively new diagnostic category reserved for children over age 6. It is characterized by steady, persistent problems with mood dysregulation. A child with DMDD experiences severe and recurrent temper outbursts, either verbal or behavioral, that are grossly out of proportion and inconsistent with what is typically expected for a child their age. These outbursts typically occur three or more times a week. Between outbursts, children with DMDD are often persistently irritable or angry. To merit a diagnosis, these symptoms need to be chronically present for at least a year.
To merit a diagnosis, these symptoms need to be chronically present for at least a year.
DMDD is a way of categorizing major mood problems in children without the bipolar label.
Bipolar Disorder
Bipolar I Disorder
A main feature of bipolar I disorder is a distinct period of abnormally and persistently elevated, expansive, or irritable mood. Bipolar I may also be characterized by a period of “hypomania,” or out-of-the-ordinary, increased activity or energy lasting persistently for at least a week. Depressive moods may also occur concurrently or at other times. These moods are severe enough to cause marked impairment in social or occupational functioning, and often warrant psychiatric hospitalization. There may also be increased risk of suicide or suicide attempts.
To merit diagnosis, at least three of the following symptoms must be present:
- Inflated self-esteem or grandiosity
- Decreased need for sleep
- Pressured speech, racing thoughts
- Extreme distractibility (beyond what is associated with ADHD)
- Increase in agitation (restlessness) or goal-directed activity
- Excessive involvement in risky activity, including over-spending, sexual indiscretions, and/or heavy drinking (the latter often done in an attempt to calm down)
Bipolar I disorder is typically diagnosed around age 18, when a first episode occurs. Many but not all patients go on to experience more episodes.
Many but not all patients go on to experience more episodes.
[Read: Solving the ADHD-Bipolar Puzzle]
Bipolar II Disorder
Bipolar II disorder is usually less severe than bipolar type I, but it can be more complicated to diagnose and significantly impairing. With bipolar type II, there’s at least one hypomanic episode lasting at least four full consecutive days, as well as three or more of the symptoms outlined for bipolar I disorder. These episodes are usually not accompanied by psychotic symptoms; they are not severe enough to cause marked impairment in functioning or to require hospitalization.
Patients with bipolar type II will also meet the criteria for a current or past episode of major depression (MDD). With bipolar I, patients may or may not have accompanying MDD. A major depressive episode is marked by at least 5 of the following symptoms:
- Persistently depressed mood
- Markedly diminished interest or pleasure
- Significant increase or decrease in appetite
- Increased restlessness or slowing down
- Fatigue, loss of energy
- Feelings of guilt or worthlessness
- Diminished ability to think or concentrate
- Recurrent thoughts of death or suicide
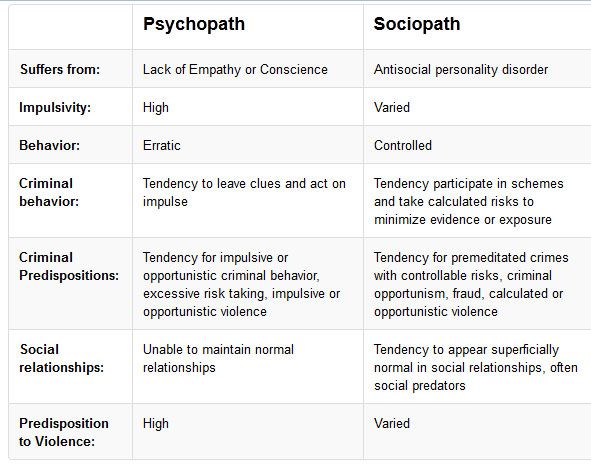
Bipolar Disorder vs.
 ADHD
ADHDBipolar disorder and ADHD do share some characteristics of moodiness, irritability, and other aspects of emotionality. The chart below differentiates these characteristics as they usually appear.
- + = presence
- – = absence
- ++ = more present
- +/– = may be present
- +++ = most present
| Symptom | ADHD | Bipolar |
| Irritability/Rage | +/- | +++ |
| Hyperactivity | ++ | +++ |
| Inattention | ++ | +++ |
| Depression | +/- | +++ |
| Substance abuse | + | +++ |
| Psychosis | – | ++ |
Bipolar Disorder in Children
Bipolar disorder in children is not always marked by clearly defined episodes of severe moods. Another factor complicating diagnosis is that about 80 percent of children and adolescents with bipolar disorder will also have ADHD, ODD, and/or major depressive episodes. This makes it difficult to tell whether a patient with ADHD and serious mood problems has severe ADHD, bipolar disorder, or both.
Another factor complicating diagnosis is that about 80 percent of children and adolescents with bipolar disorder will also have ADHD, ODD, and/or major depressive episodes. This makes it difficult to tell whether a patient with ADHD and serious mood problems has severe ADHD, bipolar disorder, or both.
But aiding diagnosis is the fact that ADHD and bipolar disorder are highly familial. (ADHD has a heritability index of .76; bipolar disorder is between .6 to .85.) Assessing for history of mood problems can help determine the diagnosis.
Mood Disorders and ADHD: Treatments and Considerations
Emotional dysregulation and severe moodiness in ADHD and bipolar disorder are often treated with medication. This intervention alone, however, is usually not sufficient. Through psychotherapy, patients and families can receive essential support around understanding and addressing problems with mood and emotional dysregulation, including:
- Identifying triggers to episodes involving family systems
- Using strategies to avoid worsening episodes
- Understanding family history of mood problems
- The limitations of medication
Clinicians should also consider that patients with bipolar type II may not warrant or choose to follow the treatments prescribed for bipolar I. In a hypomanic episode, for example, some patients may want to “tap in to” this energy for work or creative projects. In this case, it’s important to have a conversation with patients about recognizing the signs of an episode.
In a hypomanic episode, for example, some patients may want to “tap in to” this energy for work or creative projects. In this case, it’s important to have a conversation with patients about recognizing the signs of an episode.
ADHD and Bipolar Medication Options
The first course of action for treating bipolar disorder with ADHD is to stabilize mood, which can be addressed with medications like Lamictal, Abilify, Risperidone, Zyprexa, or Lithium.
Stimulant Medications
Though not explicitly approved to do so, stimulant medications for ADHD often improve moodiness in patients without a mood disorder. A patient’s effective dose is not based on their age, weight, or severity of symptoms, but rather how sensitive the patient’s body chemistry is to a particular medication. This requires monitoring and fine-tuning dosing to fit individual sensitivity as well as the patient’s lifestyle to ensure the medication is active when they most need it.
For patients with ADHD and bipolar disorder, however, stimulants may exacerbate symptoms of emotional dysregulation.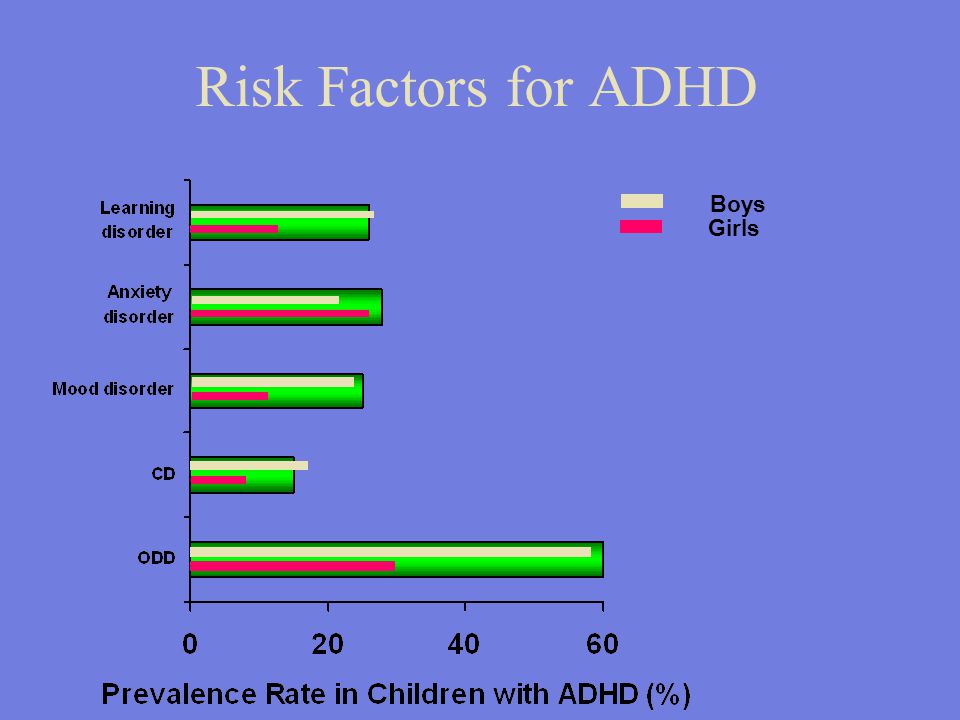 If levels of irritability or agitation are made worse on this medication, the clinician should instead prescribe a mood stabilizer to treat and reduce these issues. When the patient’s mood has stabilized but ADHD symptoms persist, stimulants can be added to treatment, but cautiously. The most prescribed stimulants are Vyvanse and Adderall XR.
If levels of irritability or agitation are made worse on this medication, the clinician should instead prescribe a mood stabilizer to treat and reduce these issues. When the patient’s mood has stabilized but ADHD symptoms persist, stimulants can be added to treatment, but cautiously. The most prescribed stimulants are Vyvanse and Adderall XR.
“Stimulant rebound” is also important factor for clinicians and patients to consider. Patients who report feeling or acting excessively wired and irritable, or who lose their “sparkle” while the stimulant is active, may be taking a dose that is too high or taking medication that does not work for them. But if these effects are occurring as the medication is wearing off, that’s a different issue of “stimulant rebound”, meaning that the medication is dropping off too fast. Usually, this issue can be fixed by administering a small dose of the short-acting version of the medicine, which smoothes its “exit ramp” and avoids these difficulties.
Nonstimulant Medications
Guanfacine-XR (Intuniv) is a nonstimulant approved for ADHD treatment that may help improve restlessness, impulsivity, and hyperactivity in patients with both ADHD and mood problems. This medication dosage needs to be increased slowly to a maximum of 4 mg per day.
This medication dosage needs to be increased slowly to a maximum of 4 mg per day.
SSRIs
Many prescribers are hesitant to add SSRIs to a bipolar treatment plan, as they can increase the risk of a hypomanic or manic episode and cause suicidal thoughts. But if a patient’s mood is stabilized and symptoms of depression persist, an SSRI like fluoxetine may help improve their mood to baseline. SSRIs should be monitored carefully, especially in the first several weeks of administration.
The Role of the Family
Parent Emotional Dysregulation
How families respond to moodiness and emotional outbursts can make a big difference. Should patients, especially children and adolescents, pursue therapy, it is also important to address parental temper and moods as well. Assessing interactions at home can reveal triggers and sensitive scenarios that contribute to mood instability.
Parental Polarization
A patient’s parents may not share the same approach to addressing irritability and moodiness. One parent may insist on patience and support, while the other adopts a “crackdown” approach. Often, each parent ends up taking a more extreme view over time. Both may fail to see how either approach could be right depending on the situation, to the detriment of the child. Therapy can be an appropriate setting for working through these issues.
One parent may insist on patience and support, while the other adopts a “crackdown” approach. Often, each parent ends up taking a more extreme view over time. Both may fail to see how either approach could be right depending on the situation, to the detriment of the child. Therapy can be an appropriate setting for working through these issues.
Mood Disorders: Next Steps
- Read: The ADHD-Anger Connection: New Insights into Emotional Dysregulation and Treatment Considerations
- Guide: Where ADHD and Bipolar Disorder Overlap
- Download: Bipolar Disorder and ADHD: How to Tell the Difference
The content for this article was derived from the ADDitude Expert Webinar “Is It Bipolar Disorder or ADHD Moodiness? A Guide to Getting the Right Diagnosis and Treatment” [Video Replay & Podcast #347] with Thomas E. Brown. Ph.D., and Ryan J. Kennedy, DNP, which was broadcast live on March 10, 2021.
SUPPORT ADDITUDE
Thank you for reading ADDitude. To support our mission of providing ADHD education and support, please consider subscribing. Your readership and support help make our content and outreach possible. Thank you.
To support our mission of providing ADHD education and support, please consider subscribing. Your readership and support help make our content and outreach possible. Thank you.
Previous Article Next Article
What is ADHD and why the diagnosis is not a sentence
Attention deficit hyperactivity disorder occurs in every tenth child. However, not all doctors can diagnose it. Without treatment, it progresses, worsening the quality of life. So how can you help ADHD patients?
What is ADHD
Attention deficit and/or hyperactivity disorder (ADHD) is a neurological-behavioral developmental disorder that occurs in childhood. Pathology has more than a dozen symptoms. The most common are the inability to concentrate for a long time, absent-mindedness, inattention, restlessness, irascibility, poor memory. From the side it seems that such a person seems to be “flying in the clouds”.
Doctors distinguish three subtypes of mental disorders.
- The first - with a predominance of attention deficit. The person cannot concentrate, is distracted, forgetful.
- The second is hyperactive and impulsive. When it is difficult to stay in one position for a long time and restrain emotional impulses.
- Third - mixed. Combines the features of the first and second. Occurs most often.
The listed symptoms are attributed to character traits, accusing a person or oneself of laziness, procrastination and conflict. In fact, it is not the individual who is “guilty”, but his brain and nervous system. According to the International Classification of Diseases, ADHD is classified as a hyperkinetic disorder.
In Russia, the syndrome is not well understood. Not all specialists are aware of it and know the evaluation criteria. Many do not understand how to diagnose and treat a disease, Olga Demyanenko, a family and child psychologist of the highest category, told RBC.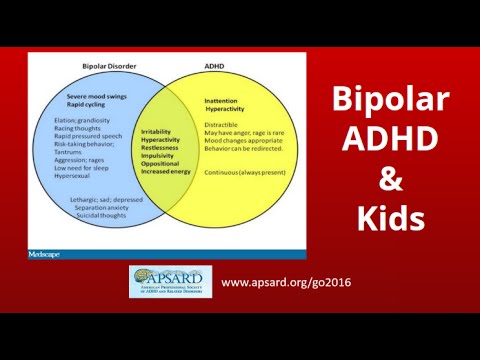 This leads to the fact that sometimes healthy children are given this diagnosis erroneously. And those who really suffer from ADHD do not get the help they need.
This leads to the fact that sometimes healthy children are given this diagnosis erroneously. And those who really suffer from ADHD do not get the help they need.
How to recognize ADHD in children
Some specialists can diagnose ADHD even in children under one year old. The main symptoms are severe excitability and hyperactivity. Babies often cry, scream, twitch their arms and legs, says Olga Demyanenko. In older children (4–5 years), attention deficit hyperactivity disorder (ADHD) manifests itself more clearly.
“The child is constantly on the move, it is difficult for him to sit still. And this is not connected with some kind of game - he needs movement in itself. He switches very quickly. He took one toy, played, then another. Also, he cannot keep his attention on something for a long time. He needs a switch, he gets tired quickly. Plus, it’s hard to calm down, he can’t fall asleep for a long time, ”says Demyanenko.
A child with ADHD finds it difficult to follow instructions and often does not even hear what is being said to him. Also, a small person cannot behave quietly and with restraint, even when there is no reason for concern. He talks loudly, laughs loudly, screams.
Also, a small person cannot behave quietly and with restraint, even when there is no reason for concern. He talks loudly, laughs loudly, screams.
How common is ADHD
The disorder affects approximately 2-10% of children. Research data on this matter vary. In boys, pathology is diagnosed several times more often than in girls.
Some children outgrow this syndrome. That is, mental functions are restored as they grow older. But this is not always the case. In adulthood, the syndrome is present in 2-4% of people, French researchers report in their work. More than half of the people who were diagnosed with ADHD in childhood have symptoms of the disease that persist into adulthood, Anna Portnova, head of the Department of Child and Adolescent Psychiatry at the Moscow Research Institute of Psychiatry, a branch of the National Medical Research Center for Psychiatry and narcology named after V.P. Serbsky" of the Ministry of Health of Russia.
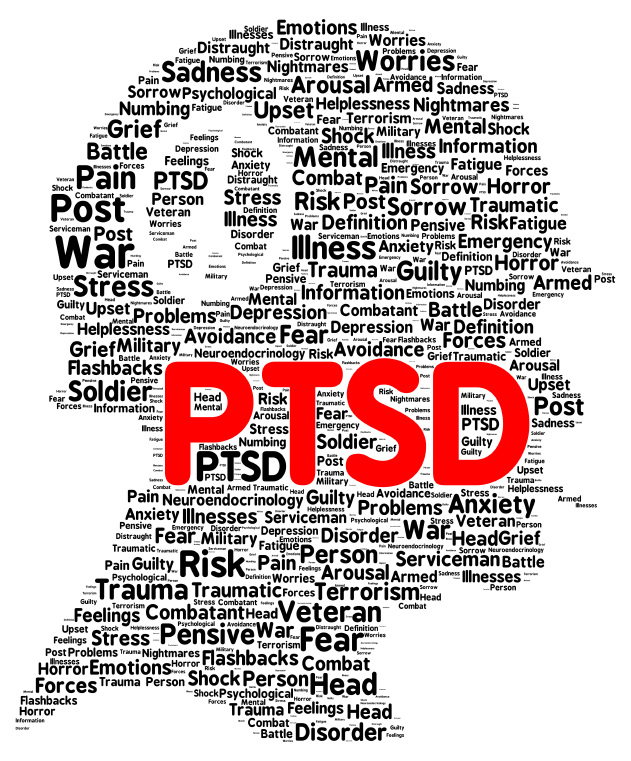
Adults show the same symptoms, including inattention, hyperactivity and impulsivity, and emotional dysregulation.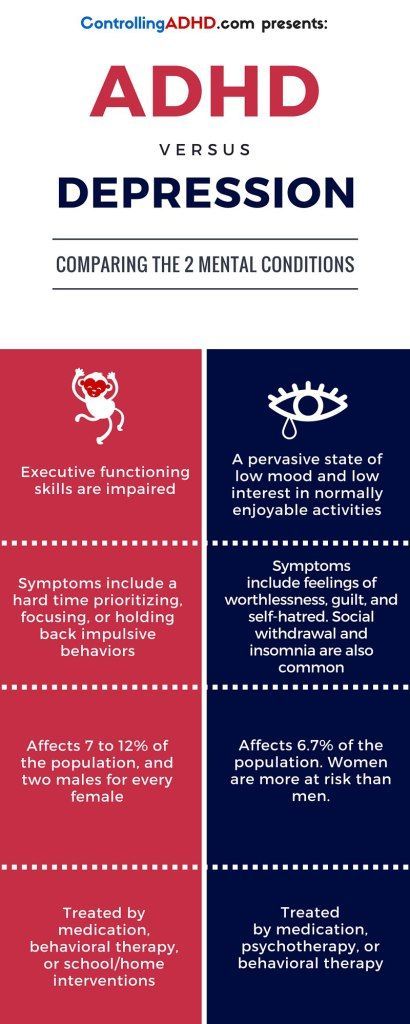 If the disease is not treated, in adulthood, ADHD in 80% of cases is superimposed by other mental disorders - anxiety disorders, neurodevelopmental disorders associated with the use of psychoactive substances, sleep disorders, restless legs syndrome. It's hard for people like that. All spheres of life "suffer" from this disease.
If the disease is not treated, in adulthood, ADHD in 80% of cases is superimposed by other mental disorders - anxiety disorders, neurodevelopmental disorders associated with the use of psychoactive substances, sleep disorders, restless legs syndrome. It's hard for people like that. All spheres of life "suffer" from this disease.
The degree of influence of ADHD on a person depends on his personal characteristics. One will be able to adapt and live normally, the other will go downhill. According to a recent study, among youth and adult offenders in police custody, prisons, probation and forensic psychiatric institutions, about 25% suffer from ADHD. They are at a disadvantage in the system because their symptoms are not recognized or misunderstood. Instead of providing psychiatric care, disciplinary sanctions are applied to them, which does not help.
Causes of ADHD
The work of the brain in children with ADHD and in healthy children is different, scientists from the Northern (Arctic) Federal University named after.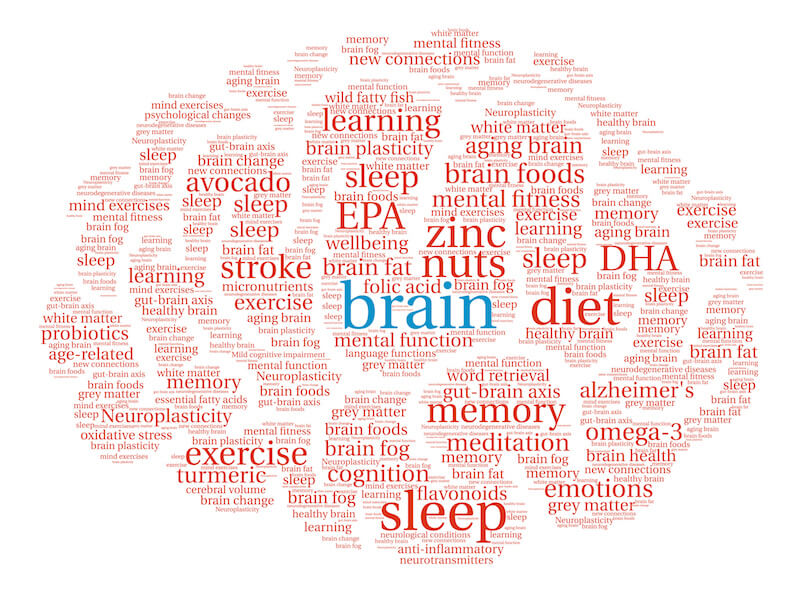 M.V. Lomonosov. With a mental disorder, the energy metabolism in the frontal sections of the brain changes. They are the key links in the regulation of behavior and emotions, and are also responsible for the function of programming and control. There is a decrease in metabolism and a decrease in the functional connections of the frontal regions with other brain structures. With ADHD, the left and right hemispheres do not “get along” well with each other, the connections between them are broken. “Imbalances in the relations of regulatory subcortical-stem structures” are noted.
M.V. Lomonosov. With a mental disorder, the energy metabolism in the frontal sections of the brain changes. They are the key links in the regulation of behavior and emotions, and are also responsible for the function of programming and control. There is a decrease in metabolism and a decrease in the functional connections of the frontal regions with other brain structures. With ADHD, the left and right hemispheres do not “get along” well with each other, the connections between them are broken. “Imbalances in the relations of regulatory subcortical-stem structures” are noted.
Doctors have not yet determined the exact cause of these disorders. It is believed that a significant role is played by hereditary predisposition. Also, ADHD in a child may develop due to the fact that his mother smoked during pregnancy, drank alcohol or drugs. The disorder may occur due to complications in childbirth or chronic illnesses of the mother.
Scientists from the Rostov State Medical University conducted a study and found that the uncontrolled use of digital technologies in childhood increases the symptoms of ADHD. And also leads to increased aggression and irritability, isolation, inability to control emotions, increased feelings of anxiety, anxiety and fear.
And also leads to increased aggression and irritability, isolation, inability to control emotions, increased feelings of anxiety, anxiety and fear.
How to treat ADHD
Attention Deficit Hyperactivity Disorder needs to be diagnosed by several specialists. This is a neurologist or neuropathologist, as well as a neuropsychologist or clinical psychologist and psychiatrist. Only after making sure that the diagnosis is correct, you need to take action.
Not only drugs are important for a child, but also the right psychological and pedagogical approach, warns Anna Portnova. According to her, a good teacher will put such a student on the first desk and will try to keep his attention. And the bad one will send him to the last one and will constantly make comments, thereby aggravating the child’s condition.
Cognitive behavioral therapy performed by a psychologist or psychiatrist is also effective in the diagnosis of ADHD.
There are drugs that improve brain function and activate attention function. But in Russia there are few registered. We simply do not have many drugs that have proven effectiveness, says Portnova. And this is a big problem.
But in Russia there are few registered. We simply do not have many drugs that have proven effectiveness, says Portnova. And this is a big problem.
Therapy with a psychologist is a more affordable option for correcting ADHD symptoms for Russians. And it is quite effective in most cases.
Still from the TV series The Good Doctor. Caption: The character on the show, Salen Morrison, has ADHD. She uses original methods for concentration: meditation, playing the ukulele, as well as many gadgets - fitness bracelets, tablets, etc.
How to live with ADHD as an adult
Attention deficit and/or hyperactivity disorder persists into adulthood. Experts say it is possible to adapt to this condition, even without the use of medication. A person with ADHD can be successful both in his personal life and in his profession. This can be achieved by controlling your habits, learning to recognize and use your strengths, and controlling your behavior.
Psychologists advise a person with ADHD to properly organize their workspace by removing unnecessary items from the table. For example, a stack of unnecessary papers or books. In order not to forget anything, you can make a to-do list every day. A great help for a person with this disorder can be a day planner, a calendar on a smartphone or computer. People with ADHD like to procrastinate. To avoid this, follow the principle: if a task can be completed in two minutes or less, do it now.
For example, a stack of unnecessary papers or books. In order not to forget anything, you can make a to-do list every day. A great help for a person with this disorder can be a day planner, a calendar on a smartphone or computer. People with ADHD like to procrastinate. To avoid this, follow the principle: if a task can be completed in two minutes or less, do it now.
People with ADHD find it difficult to properly manage their time. To avoid this, psychologists advise using a watch. When you start doing work, write down the time and say it out loud. For each task, it is necessary to allocate a certain time period. This is easy to do using a timer or an alarm clock. Let it fire at regular intervals. This makes it harder to lose track of time, a common problem for people with ADHD.
Adults with Attention Deficit and/or Hyperactivity Disorder are often overly impulsive. They jump from one task to another. This may interfere with work. Experts recommend always starting with the most important task. The main mistake is to take on too much work. Break large projects or assignments into smaller, manageable steps.
The main mistake is to take on too much work. Break large projects or assignments into smaller, manageable steps.
A healthy lifestyle is the main assistant for people with ADHD. Good nutrition, plenty of sleep, and regular exercise can help you stay calm, minimize mood swings, and fight any symptoms of anxiety and depression.
Attention Deficit Hyperactivity Disorder (ADHD)
Treatment of Attention Deficit Hyperactivity Disorder
Before starting treatment for ADHD, a specialist consultation is necessary. Make an appointment with a doctor in any way convenient for you: by phone or through the feedback form.
What is ADHD?
Attention Deficit Hyperactivity Disorder (ADHD) is a dysfunction of the central nervous system, manifested by difficulty concentrating and maintaining attention, learning and memory impairments, and information processing difficulties.
Children suffering from ADHD syndrome are not able to hold attention for a long time, they are distracted, forgetful, lose and forget their things, do not perceive the instructions and requests of adults from the first time, it is difficult for them to follow the daily routine.
Why is ADHD dangerous?
Attention disorders and hyperactivity in children lead to the fact that a school-age child with normal or high intelligence has impaired reading and writing skills, does not cope with school assignments, makes many mistakes in work performed and is not inclined to listen to the advice of adults. The child is a source of constant anxiety for those around him (parents, teachers, peers), as he interferes in other people's conversations and activities, overreacts to external stimuli (the reaction does not correspond to the situation). Such children hardly adapt in the team, their distinct desire for leadership has no actual reinforcement. Due to their impatience and impulsiveness, they often come into conflict with peers and teachers, which exacerbates existing learning disabilities. A child with attention deficit is also not able to foresee the consequences of his behavior, does not recognize authorities, which can lead to antisocial acts. Especially often antisocial behavior is observed in adolescence, when children with attention deficit hyperactivity disorder have an increased risk of developing persistent behavioral disorders and aggressiveness.
Types of ADHD in children
There are 3 types of the course of attention deficit hyperactivity disorder depending on the symptoms:
- Syndrome that combines attention deficit hyperactivity disorder
- Attention deficit disorder without hyperactivity disorder
- Non-attention deficit hyperactivity disorder
The frequency of attention deficit hyperactivity disorder, according to different authors, varies from 2.2 to 18% in school-age children. Almost every school class has at least one child with this condition.
Boys suffer from ADHD 2 times more often than girls, and boys are more likely to have isolated hyperactivity or hyperactivity in combination with attention disorders.
The prognosis of ADHD treatment
The prognosis of ADHD treatment in children is relatively favorable, since in a significant number of patients with the right approach, the symptoms of the disease disappear in adolescence.
However, in 30-70% of cases, clinical manifestations of attention deficit hyperactivity disorder (excessive impulsivity, irascibility, absent-mindedness, forgetfulness, restlessness, impatience, unpredictable, rapid and frequent mood changes) can also be observed in adults.
Symptoms and Diagnosis
Attention Deficit Disorder can be diagnosed if at least 6 of the following symptoms are present.
A child has an attention deficit if:
- Does not pay attention to details and makes mistakes in work
- Difficulty maintaining attention at work and play
- Does not listen to what is said to him
- Unable to follow instructions
- Unable to organize play or non-play structured activities (e.g. homework)
- Has difficulty performing tasks that require prolonged attention span
- Often loses things
- Often and easily distracted
- Sometimes forgetful
Diagnosis of hyperactivity requires at least 5 of the following symptoms.
The child is hyperactive if:
- Fidgets with arms and legs
- Often jumps up from his seat
- Hypermobile in situations where hypermobility is unacceptable
- Cannot play silent games
- Always on the move
- Talks a lot
- The child is impulsive if:
- Answers a question without hearing it
- Cannot wait for his turn
- Interferes with the conversations and games of others
- Mandatory characteristics of ADHD are also:
- Duration:
- symptoms persist for at least 6 months
- Persistence, spreading to all areas of life: adjustment disorders are observed in two or more types of environment (for example, at school and at home)
- Severity of violations: significant violations in training, social contacts, professional activity
- Excludes other psychiatric disorders: symptoms cannot be attributed solely to the course of another illness
What causes ADHD?
The formation of ADHD is based on neurobiological factors: genetic mechanisms and perinatal damage to the central nervous system (damage to the brain and spinal cord that occurs during pregnancy, childbirth and the early postpartum period), which can be combined with each other. It is they who determine changes in the functioning of the nervous system and violations of higher mental functions and behavior, corresponding to the picture of the syndrome.
It is they who determine changes in the functioning of the nervous system and violations of higher mental functions and behavior, corresponding to the picture of the syndrome.
In many cases, children with ADHD are additionally affected by negative socio-psychological factors (primarily family factors), which do not in themselves cause the development of ADHD, but always contribute to an increase in the child's symptoms and adaptation difficulties.
ADHD related disorders (so-called comorbid disorders).
Additional difficulties of intrafamily, school and social adaptation in children with ADHD may be associated with the formation of concomitant disorders that develop against the background of ADHD as the underlying disease in at least 70% of patients. Comorbid disorders in ADHD are represented by the following groups: oppositional defiant behavior, anxiety disorders, mood disorders, speech development disorders, learning difficulties, lack of coordination, awkwardness, tics). Other comorbid ADHD disorders may include sleep disturbances and involuntary urination during sleep.
Other comorbid ADHD disorders may include sleep disturbances and involuntary urination during sleep.
How is ADHD treated?
The best results in the treatment of Attention Deficit Hyperactivity Disorder are achieved with a combination of various methods, however, a neurologist should decide on the complex of necessary therapeutic measures.
Our doctors in the treatment of ADHD use a unique method of Biophysical neuromodulation, which triggers the internal mechanisms of self-regulation of the CNS structures and is able to restore the normal development of the child, positively affecting cognitive functions (attention, memory, speech). In addition, our method has a positive effect on metabolic processes in the nervous system and promotes the maturation of new brain cells. In cases where ADHD is combined with destructive behavior, anxiety disorders, neuroses, treatment is combined with micropolarization and interactive trainings of adaptive neurofeedback, which enhance synaptic transmission in different brain structures.