Adhd in children quiz
Does My Child Have ADHD? Symptom Test for Kids
ADHD Symptoms Test for Kids
Only a mental-health professional can tell for sure whether symptoms of distractibility, impulsivity, and hyperactivity are severe and persistent enough to suggest a positive diagnosis of attention deficit hyperactivity disorder. But if you are concerned that your child demonstrates ADHD symptoms, take this test to better measure his or her behaviors and to understand how ADHD in children is diagnosed.
This questionnaire is designed to determine whether your child demonstrates symptoms similar to those of attention deficit disorder (ADHD). If you answer yes to a significant number of these questions, consult a physician and a licensed mental health practitioner. An accurate diagnosis can only be made through clinical evaluation.
Based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
In class or at home, my child blurts out answers to questions before they are fully asked.
Very Often
Often
Sometimes
Rarely
Never
My child fails to complete an activity before moving to the next activity.
Very Often
Often
Sometimes
Rarely
Never
My child interrupts other peoples' activities and conversations.
Very Often
Often
Sometimes
Rarely
Never
My child interferes in the classroom because she/he has difficulty engaging in quiet activities without disturbing others.
Very Often
Often
Sometimes
Rarely
Never
Even the smallest distractions can throw my child off task.
Very Often
Often
Sometimes
Rarely
Never
My child tries to avoid activities that require sustained concentration and a lot of mental effort
Very Often
Often
Sometimes
Rarely
Never
My child acts as if she/he is driven by a motor.
Very Often
Often
Sometimes
Rarely
Never
My child loses things like homework and personal belongings.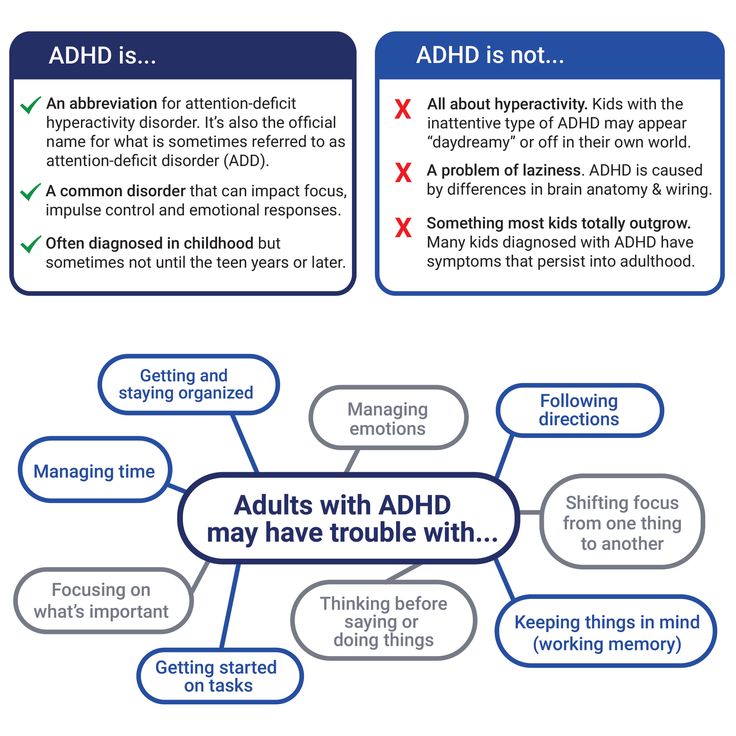
Very Often
Often
Sometimes
Rarely
Never
Even when spoken to directly, my child seems to not be paying attention.
Very Often
Often
Sometimes
Rarely
Never
My child forgets to do things, even when constantly reminded.
Very Often
Often
Sometimes
Rarely
Never
My child talks a lot, even when she/he has nothing much to say.
Very Often
Often
Sometimes
Rarely
Never
My child makes careless mistakes.
Very Often
Often
Sometimes
Rarely
Never
My child is disorganized and, even with my help, can't seem to learn how to become organized.
Very Often
Often
Sometimes
Rarely
Never
It's very difficult for my child to stay focused on homework or other tasks.
Very Often
Often
Sometimes
Rarely
Never
My child constantly seems to be fidgeting.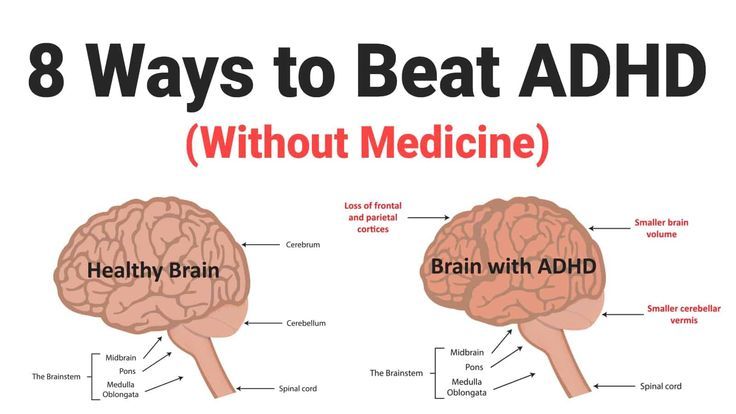
Very Often
Often
Sometimes
Rarely
Never
My child has problems remaining seated even when she/he is supposed to.
Very Often
Often
Sometimes
Rarely
Never
My child has difficulty waiting patiently to take turns, and butts ahead in lines or grabs toys from playmates.
Very Often
Often
Sometimes
Rarely
Never
(Optional) Would you like to receive these ADHD symptom test results — plus more helpful resources — via email from ADDitude?
Sign me up for your Parenting Children & Teens with ADHD newsletter.
Can’t see the self-test questions above? Click here to open this test in a new window.
ADHD in Children: Next Steps
1. Take This Test: Inattentive ADHD Symptoms in Children
2. Take This Test: ADHD Symptoms in Girls
3. Take This Test: Hyperactive and Impulsive ADHD Symptoms in Children
4. Take This Test: Oppositional Defiant Disorder in Children
Take This Test: Oppositional Defiant Disorder in Children
5. Take This Test: Sensory Processing Disorder in Children
6. Find: ADHD Specialists or Clinics Near You
7. Consult Our ADHD Treatment Guide for Children
Previous Article Next Article
Symptoms in Kids, Evaluations, Treatments
ADHD in Children
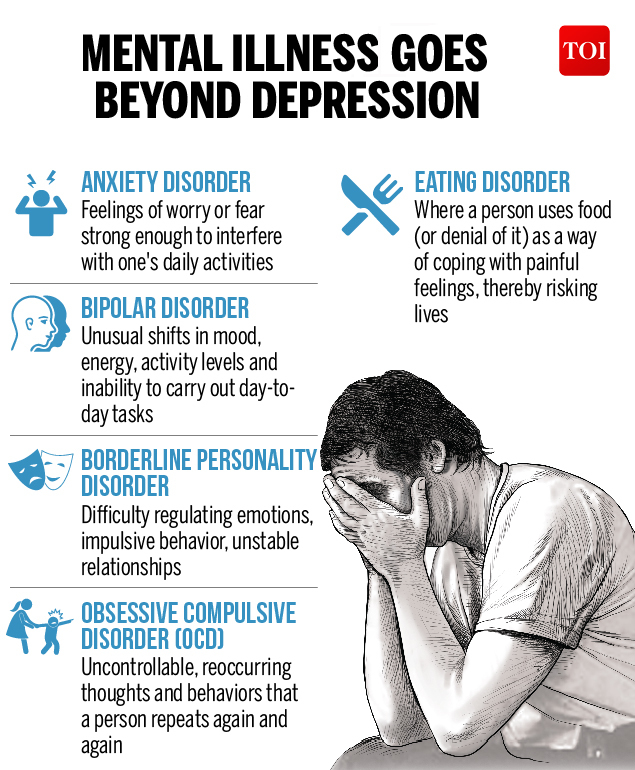
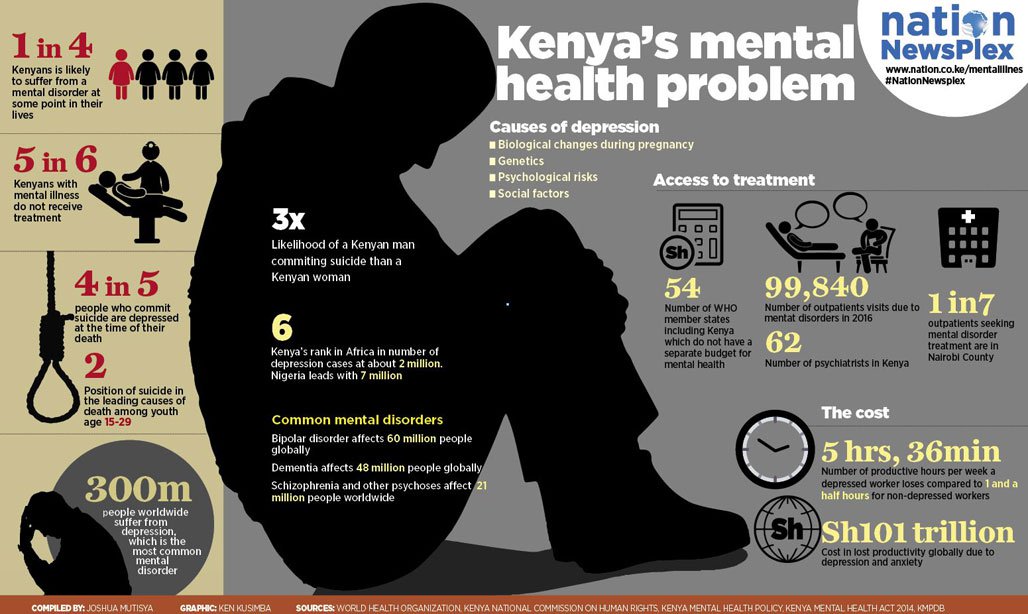
Attention deficit hyperactivity disorder (ADHD) is one of the most common childhood disorders, affecting between 5 and 11 percent of American children. ADHD in children may present through symptoms including inattentiveness, impulsivity, hyperactivity, fidgeting, excessive talking, trouble waiting turn, and difficulty following direction.
What Are Common Symptoms?
Your child is a wiggle worm. She can’t sit still and fidgets constantly. Does this mean she has attention deficit hyperactivity disorder (ADHD or ADD)?
Your child forgets to hand in his homework and typically writes down only half his assignments. Are these working memory glitches typical symptoms of ADHD in children?
Are these working memory glitches typical symptoms of ADHD in children?
Your student disrupts the classroom by blurting out answers, veering off topic, or getting up from his seat daily. Should he be evaluated for ADHD symptoms?
Or are these just typical childhood and adolescent behaviors that your kid with outgrow with time?
Only a qualified medical professional can evaluate and diagnose symptoms of ADHD in children. However, it’s critical for parents and educators to know the warning signs because early detection, ADHD treatment, and school accommodations can make a world of difference for a child with ADHD.
ADHD Symptoms in Kids
Although symptoms may differ depending on the type of ADHD diagnosed, some common symptoms of ADHD in kids are:
- Self-focused behavior
- Trouble waiting turn
- Emotional turmoil
- Fidgeting
- Problems playing quietly
- Trouble finishing tasks
- Lack of focus
- Forgetfulness
[Self-Test: Could Your Child Have ADHD?]
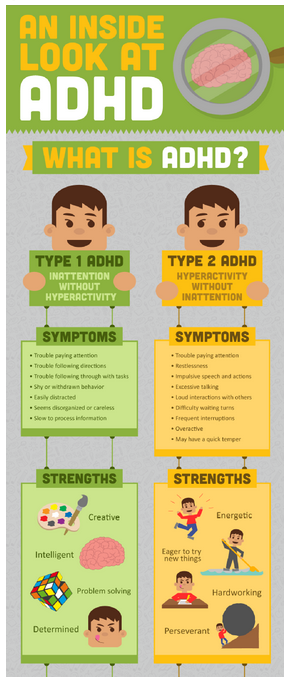
ADHD in Children: Hyperactive Vs.
 Inattentive Symptoms
Inattentive SymptomsThe stereotypical ADHD patient is a 9-year-old boy who loves to jump off dangerously high things and hates to focus on school work. In reality, only a fraction of people with ADHD fit this description. Children with hyperactive ADHD symptoms are difficult to ignore — they are the ones bouncing out of their chairs or clowning behind the teacher’s back, and are the first to be evaluated for and diagnosed with ADHD.
Meanwhile, the students with inattentive ADHD are quietly staring out the window at a bird while their work lays unfinished. According to the National Institute of Mental Health (NIMH), inattentive symptoms are far less likely to be recognized by parents, teachers, and medical professionals.1 As a result, individuals with inattentive ADHD rarely get the treatment they need. This leads to academic frustration, apathy, and undue shame that can last a lifetime.
ADHD in Children: Symptoms, Testing, and Diagnosis
ADHD is a genetic, brain-based condition, not just a deficit of executive functions.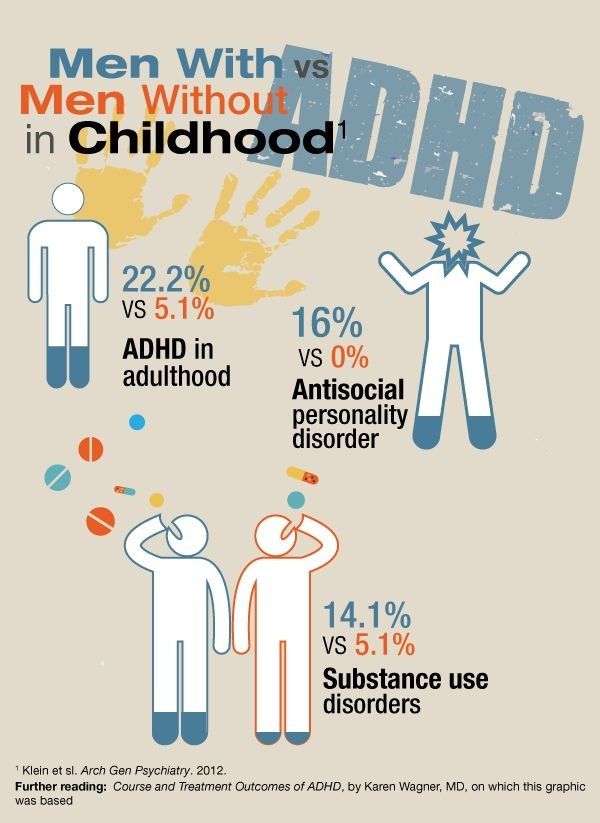 The Diagnostic and Statistical Manual of Mental Disorders (DSM-V) lists nine symptoms that suggest ADHD Primarily Inattentive, and nine that suggest ADHD Primarily Hyperactive-Impulsive. A child may be diagnosed with ADHD only if he or she exhibits at least six of the symptoms from one of the lists below, and if the symptoms have been noticeable for at least six months in two or more settings — for example, at home and at school. What’s more, the symptoms must interfere with the child’s functioning or development, and at least some of the symptoms must have been apparent before age 122. Older teens may need to demonstrate just five of these symptoms in multiple settings.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-V) lists nine symptoms that suggest ADHD Primarily Inattentive, and nine that suggest ADHD Primarily Hyperactive-Impulsive. A child may be diagnosed with ADHD only if he or she exhibits at least six of the symptoms from one of the lists below, and if the symptoms have been noticeable for at least six months in two or more settings — for example, at home and at school. What’s more, the symptoms must interfere with the child’s functioning or development, and at least some of the symptoms must have been apparent before age 122. Older teens may need to demonstrate just five of these symptoms in multiple settings.
A person with this Inattentive ADHD (formerly called ADD) will exhibit six of these nine symptoms:
- Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or during other activities (e.
 g., overlooks or misses details, turns in inaccurate work).
g., overlooks or misses details, turns in inaccurate work). - Often has difficulty sustaining attention in tasks or play activities (e.g., has difficulty remaining focused during lectures, conversations, or lengthy reading).
- Often does not seem to listen when spoken to directly (e.g., mind seems elsewhere, even in the absence of any obvious distraction).
- Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., starts tasks but quickly loses focus and is easily sidetracked).
- Often has difficulty organizing tasks and activities (e.g., struggle to manage sequential tasks, keep materials and belongings in order, organize work, manage time, and meet deadlines).
- Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.g., schoolwork or homework; for older adolescents and adults, this may include preparing reports, completing forms, reviewing lengthy papers).
- Often loses things necessary for tasks or activities (e.g., school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
- Is often easily distracted by extraneous stimuli (for older adolescents and adults, this may include unrelated thoughts).
- Is often forgetful in daily activities (e.g., doing chores, running errands; for older adolescents and adults, this may include returning calls, paying bills, keeping appointments).
[Self-Test: Symptoms of Inattentive ADHD in Children]
Primarily Hyperactive-Impulsive Type Symptoms
A person with this Hyperactive/Impulsive ADHD will exhibit six of these nine symptoms:
- Often fidgets with or taps hands or feet or squirms in seat.
- Often leaves seat in situations when remaining seated is expected (e.g., leaves his or her place in the classroom, in the workplace, or in other situations that require remaining in place).
- Often runs about or climbs in situations where it is inappropriate.
 (Note: In adolescents or adults, this may manifest as feeling restless.)
(Note: In adolescents or adults, this may manifest as feeling restless.) - Often unable to play or engage in leisure activities quietly.
- Is often “on the go,” acting as if “driven by a motor” (e.g., is unable to remain still — in restaurants or meetings, for example — for any extended time without significant discomfort; others may say the patient is restless, fidgety, or difficult to keep up with).
- Often talks excessively.
- Often blurts out an answer before a question has been completed (e.g., completes people’s sentences).
- Often has difficulty waiting his or her turn (e.g., while waiting in line, while speaking in conversations).
- Often interrupts or intrudes on others (e.g., butts into conversations, games, or activities; may start using other people’s things without asking or receiving permission; for adolescents and adults, may intrude into or take over what others are doing).”5
[Self-Test: Symptoms of Hyperactive Impulsive ADHD in Children]
Combined Type SymptomsTo have ADHD Combined Type, an individual must meet the guidelines of both ADHD Primarily Inattentive and ADHD Primarily Hyperactive-Impulsive – that is, they must exhibit six of the nine symptoms listed for each sub-type.
ADHD in Children: How a Diagnosis Is Made
No ADHD test alone can diagnose symptoms of ADHD. ADHD is a nuanced condition with three distinct sub-types (as detailed above), symptoms that appear along a spectrum of severity, and overlapping comorbid conditions (learning disabilities, oppositional defiant disorder, etc.) that often complicate diagnosis and treatment.
An evaluation for ADHD may start with a routine visit to the pediatrician, but chances are it won’t end it there. As a rule, most general practitioners are not trained in the idiosyncrasies of ADHD and its overlapping conditions, or not equipped to perform the in-depth evaluation needed.
Any ADHD evaluation worth its weight will begin by critically analyzing many aspects of the patient’s daily life, such as learning, memory, cognitive functioning, executive functioning, reasoning, social functioning, verbal and non-verbal communication. In cases where learning disabilities are suspected, the evaluation might include an intelligence test (IQ), and gauge math, reading, and writing skills.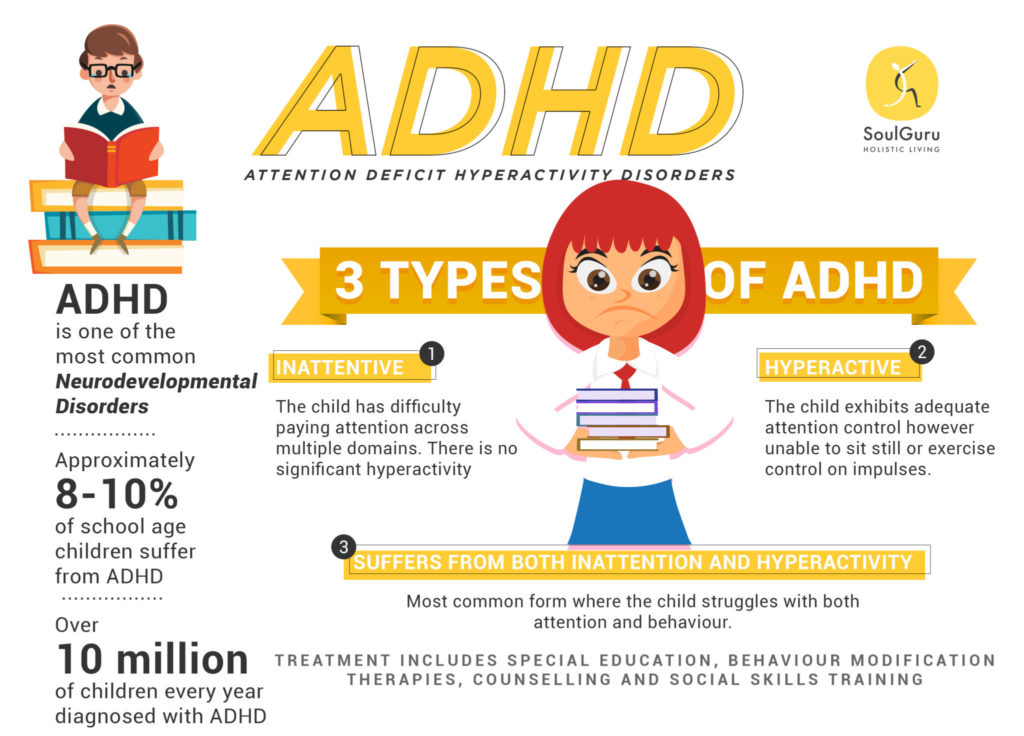 Full neuropsychological testing is not required, however, to diagnose ADHD. Educational testing normally occurs several months after any diagnosed ADHD has been successfully treated7.
Full neuropsychological testing is not required, however, to diagnose ADHD. Educational testing normally occurs several months after any diagnosed ADHD has been successfully treated7.
This information is gathered through a clinical interview, plus a thorough review of the child’s and the family’s medical history, various parent and/or teacher rating scales. An in-depth evaluation offers greater insight into strengths and weaknesses, and helps identify comorbid conditions, such as learning disabilities, depression, anxiety disorder, or autism spectrum disorder.
When performed thoroughly and effectively, a formal assessment should offer therapy, treatment, and educational strategies to address the specific needs it reveals or confirms.
Diagnoses Continue to Rise
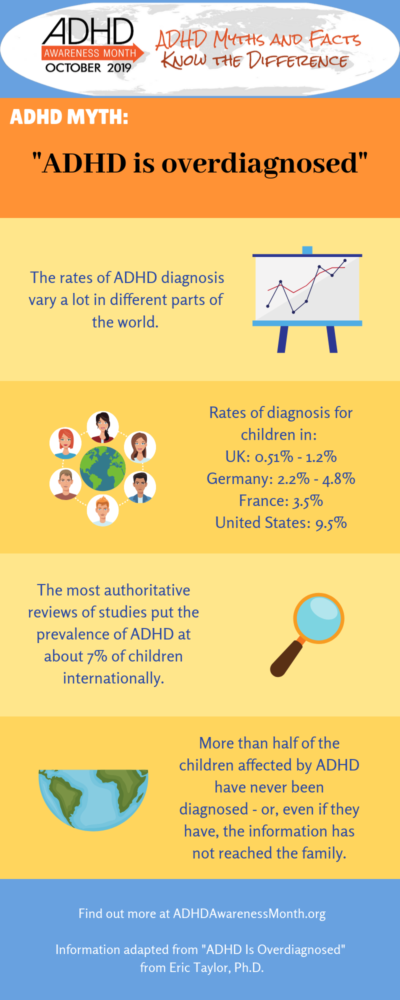
Diagnoses of ADHD have skyrocketed nearly 50 percent since 2003, bringing the total number of American children with ADHD to nearly 6 million, according to 2015 statistics from the Center for Disease Control and Prevention (CDC). 3
3
The CDC reports that 11 percent of all children in the U.S. aged 4-17 had an ADHD diagnosis by 2011. Boys are nearly three times more likely to be diagnosed with ADHD (13.2 percent) than are girls (5.6 percent),4 although the largest surge in rising ADHD diagnosis rates is currently attributed to girls and women.
ADHD Treatment Options for Children
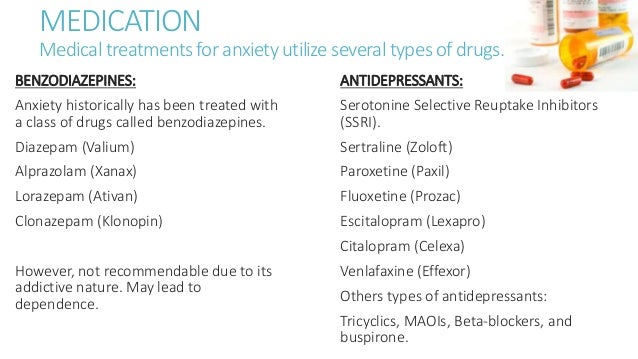
Stimulant Medication for ADHD in Children
Stimulant medication is the most recommended form of ADHD treatment for one simple reason: studies show it to be most effective. According to the American Academy of Pediatrics (AAP), 80 percent of the children who use stimulant medications, either alone or combined with behavior therapy, increase focus and decrease impulsivity.6 What’s more, the majority of children who use medication report having increased self-esteem, fewer disruptive behaviors, and improved relationships with parents, siblings, and teachers.
The clinical practice guidelines for ADHD, developed by the American Academy of Child and Adolescent Psychiatry (AACAP), recommend medication as the first-line treatment for ADHD in school-age children, citing a formal review of 78 studies on the treatment of ADHD, which “consistently supported the superiority of stimulant over the non-drug treatment. ”7
”7
Even the widely-cited Multi-Modal MTA Cooperative Group Study, which concluded that medication combined with behavior therapy is the optimal treatment of ADHD in children, conceded that “a pharmacological intervention for ADHD is more effective than a behavioral treatment alone.”8
Non-Stimulant Medications for ADHD in Children
Non-stimulant medications are a viable alternative for children who can’t tolerate or don’t experience the desired effects of stimulant medications. These medications do target neurotransmitters, but not dopamine specifically, like the stimulants do. While non-stimulants don’t carry the same side-effect risks as stimulants, they do have their own possible side effects.
Strattera, Intuniv, Kapvay are non-stimulant medications specifically recommended for ADHD. The classification also includes medications often prescribed off-label for ADHD — tricyclic antidepressants, and Wellbutrin, for example.
Therapy for ADHD in Children
While medication works on a neurological level to regulate the brain, behavior therapy addresses specific problem behaviors by structuring time at home, establishing predictability and routines, and increasing positive attention.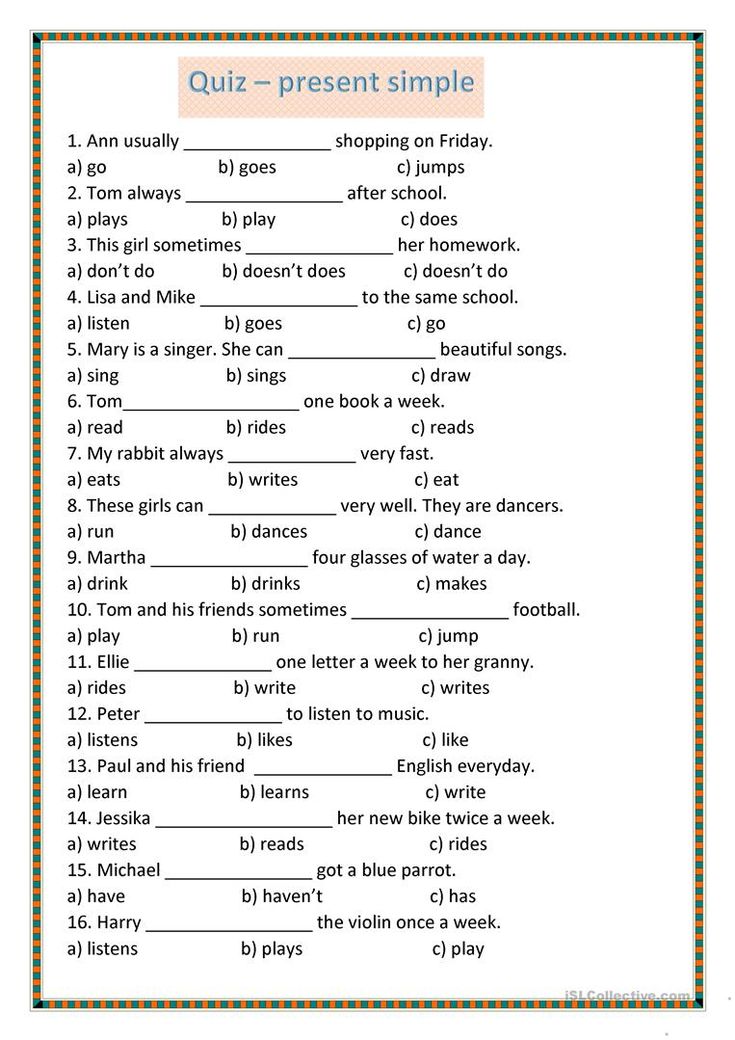 Behavior therapy operates on a simple premise: Parents and other adults in a child’s life set clear expectations for their child’s behavior — they praise and reward positive behavior and discourage negative behavior. Behavior therapy requires participation from parents and teachers.
Behavior therapy operates on a simple premise: Parents and other adults in a child’s life set clear expectations for their child’s behavior — they praise and reward positive behavior and discourage negative behavior. Behavior therapy requires participation from parents and teachers.
Diet and Nutrition for ADHD in Children
Poor diet and eating habits do not cause ADHD. However, parents of children with ADHD are finding that, while whole foods may not be a cure-all, diet changes can make a big difference for some kids with ADHD.
Research shows that diet and nutrition impact cognition, attention, sleep, and mood. According to the Harvard Health Blog, studies show that people who eat “clean” or “whole” diets high in vegetables, fruits, unprocessed grains, and lean meats, are more likely to experience better emotional health and 25 to 35 percent less likely to experience depression.9
Studies by Massachusetts Institute of Technology neuroscientist Richard Wurtman Ph. D., and others have shown that protein triggers alertness-inducing neurotransmitters, while carbohydrates trigger drowsiness. These findings support the popular belief that people with ADHD do better after eating a protein-rich breakfast and lunch.
D., and others have shown that protein triggers alertness-inducing neurotransmitters, while carbohydrates trigger drowsiness. These findings support the popular belief that people with ADHD do better after eating a protein-rich breakfast and lunch.
For optimal brain performance, children should eat more unprocessed foods, complex carbohydrates, proteins, vegetables, and fruits. That means avoiding artificial colors and flavors, chemical preservatives, and over-processed foods — all shown to exacerbate ADHD symptoms in some individuals.
Natural Supplements and Vitamins for ADHD in Children
It’s true that not everyone eats the right foods to achieve beneficial levels of certain nutrients, especially picky kids. But it’s also true that our bodies don’t always produce the nutrients we need, so we have to get some of them from supplements. There are many vitamins, herbs, and supplements that may diminish ADHD symptoms or address medication side effects in some individuals: Omega-3s, Zinc, Iron, Magnesium, Vitamin C, Valerian, Melatonin, Ginkgo, and Ginseng.
However, “all natural” is not synonymous with “safe.” Many herbs and supplements have side effects, may cause or worsen health problems, or interfere with prescription medications. Talk to your child’s doctor before starting any supplements. When your doctor asks if your child is taking any medications, be sure to tell him about all vitamins and supplements he takes on a daily basis.
Exercise for ADHD in Children
“Think of exercise as medication,” says John Ratey, M.D., an associate clinical professor of psychiatry at Harvard Medical School and author of Spark: The Revolutionary New Science of Exercise and the Brain. “Exercise turns on the attention system, the so-called executive functions — sequencing, working memory, prioritizing, inhibiting, and sustaining attention. On a practical level, it causes kids to be less impulsive, which makes them more primed to learn.”
Exercise causes the brain to release several important chemicals. Endorphins, for one — hormone-like compounds that regulate mood, pleasure, and pain. That same burst of activity also elevates the brain’s dopamine, norepinephrine, and serotonin levels. These brain chemicals affect focus and attention, which are in short supply in children with ADHD. “When you increase dopamine levels, you increase the attention system’s ability to be regular and consistent, which has many good effects,” explains Ratey, like reducing the craving for new stimuli and increasing alertness.
That same burst of activity also elevates the brain’s dopamine, norepinephrine, and serotonin levels. These brain chemicals affect focus and attention, which are in short supply in children with ADHD. “When you increase dopamine levels, you increase the attention system’s ability to be regular and consistent, which has many good effects,” explains Ratey, like reducing the craving for new stimuli and increasing alertness.
A 2015 study published in the Journal of Abnormal Psychology found that 30 minutes of exercise before school can help kids with ADHD focus and manage moods. It can even decrease the need for stimulant medications used to treat symptoms.10
Brain Training for ADHD in Children
Kids with ADHD can’t always hold on to information because their attention gets hijacked. Improving working memory capacity with brain training enables an individual to pay attention, resist distractions, manage emotions better, and learn.
“Working memory is the ability to hold information in your mind for several seconds, manipulate it, and use it in your thinking,” says Ari Tuckman, Psy. D., a clinical psychologist in West Chester, Pennsylvania. “It is central to concentration, problem solving, and impulse control.”
D., a clinical psychologist in West Chester, Pennsylvania. “It is central to concentration, problem solving, and impulse control.”
Brain-training therapies like neurofeedback and Cogmed are making a serious promise: increased attention and working memory without medication. The scientific community, however, is not convinced and insists that more rigorous studies are needed.11
Another form of brain training with some encouraging but inconclusive studies, neurofeedback uses brain exercises to reduce impulsivity and increase attentiveness. The brain emits different types of waves, depending on whether we are in a focused state or daydreaming. The goal of neurofeedback is to teach a person to produce brain-wave patterns that reflect focus. The result: Some ADHD symptoms — namely, impulsivity and distractibility — diminish.
Mindfulness and Meditation for ADHD in Children
For many children with ADHD, two persistent daily challenges are paying attention and maintaining self-regulation.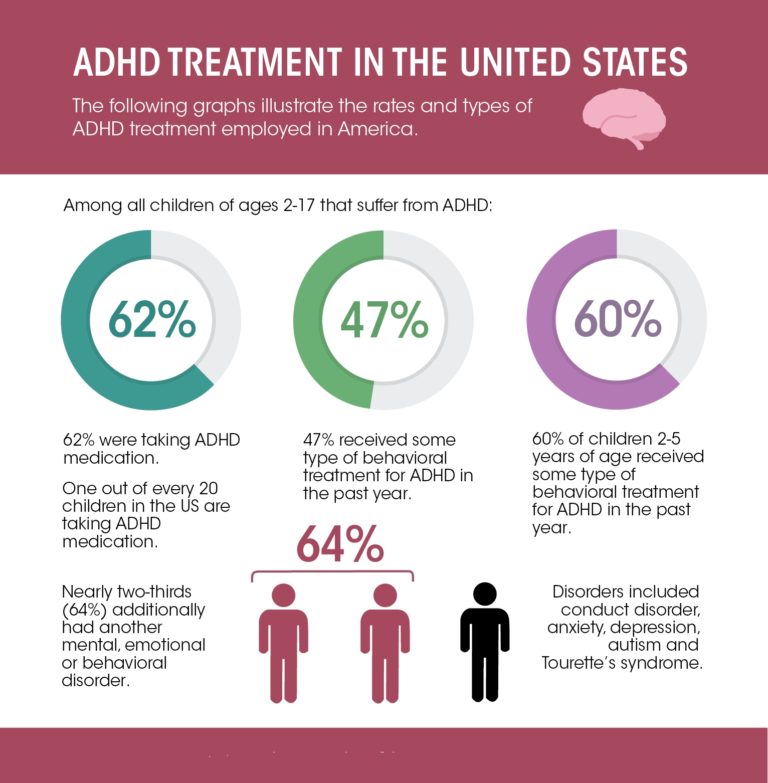 So it stands to reason that some kind of attention training that also hones self-control would be invaluable — and incredibly powerful. Indeed, a 2005 study at Arizona State University found that children who participated in mindfulness exercises had lower test anxiety and ADHD symptoms, and greater attention than kids who did not participate in the exercises.12
So it stands to reason that some kind of attention training that also hones self-control would be invaluable — and incredibly powerful. Indeed, a 2005 study at Arizona State University found that children who participated in mindfulness exercises had lower test anxiety and ADHD symptoms, and greater attention than kids who did not participate in the exercises.12
“Research suggests that anyone can improve attention by practicing mindfulness — cognitive fitness training aimed at building real-time and compassionate awareness of our lives rather than remaining lost in distraction, on autopilot,” explains Mark Bertin, M.D., in his book, Mindful Parenting for ADHD: A Guide to Cultivating Calm, Reducing Stress & Helping Children Thrive. “How does it work with the ADHD brain? ADHD is characterized by difficulties with executive function, not just attention, and mindfulness is an avenue to developing interrelated cognitive skills, many related to executive function, not just attention. ”
”
View Article Sources
1 Attention Deficit Hyperactivity Disorder. National Institute of Mental Health (2008). https://education.ucsb.edu/sites/default/files/hosford_clinic/docs/adhd_booklet.pdf
2 Association, American Psychiatric, ed. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington: American Psychiatric, 2014.
3 “Data & Statistics.” Centers for Disease Control and Prevention. Ed. Center for Disease Control. Centers for Disease Control and Prevention, 14 Feb. 2017. Web. 15 Mar. 2017.
4 Visser, Susanna N., Melissa L. Danielson, Rebecca H. Bitsko, Joseph R. Holbrook, Michael D. Kogan, Reem M. Ghandour, Ruth Perou, and Stephen J. Blumberg. “Trends in the Parent-Report of Health Care Provider-Diagnosed and Medicated Attention-Deficit/Hyperactivity Disorder: United States, 2003â2011.” Journal of the American Academy of Child & Adolescent Psychiatry 53. 1 (2014): n. pag. Web.
1 (2014): n. pag. Web.
5 Association, American Psychiatric, ed. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington: American Psychiatric, 2014.
6 Clinical Practice Guideline: Treatment of the School-Aged Child With Attention-Deficit/Hyperactivity Disorder. American Academy of Pediatrics (Oct. 2001). https://pediatrics.aappublications.org/content/108/4/1033
7 Pliszka, Steven. “Practice Parameter for the Assessment and Treatment of Children and Adolescents With Attention-Deficit/Hyperactivity Disorder.” Journal of the American Academy of Child & Adolescent Psychiatry 46.7 (2007): 894-921. Web.
8 The MTA Cooperative Group. A 14-Month Randomized Clinical Trial of Treatment Strategies for Attention-Deficit/Hyperactivity Disorder. Arch Gen Psychiatry. https://jamanetwork.com/journals/jamapsychiatry/article-abstract/205525
9 MD, Eva Selhub. “Nutritional Psychiatry: Your Brain on Food.” Harvard Health Blog. Harvard University, 17 Nov. 2015. Web. 14 Mar. 2017.
“Nutritional Psychiatry: Your Brain on Food.” Harvard Health Blog. Harvard University, 17 Nov. 2015. Web. 14 Mar. 2017.
10 Hoza, Betsy, Alan L. Smith, Erin K. Shoulberg, Kate S. Linnea, Travis E. Dorsch, Jordan A. Blazo, Caitlin M. Alerding, and George P. Mccabe. “A Randomized Trial Examining the Effects of Aerobic Physical Activity on Attention-Deficit/Hyperactivity Disorder Symptoms in Young Children.” Journal of Abnormal Child Psychology 43.4 (2014): 655-67. Web.
11 Gelad, Katleen, Tieme W. P. Janssen, Marleen Bink, Rosa Van Mourik, Athanasios Maras, and Jaap Oosterlaan. “Behavioral Effects of Neurofeedback Compared to Stimulants and Physical Activity in Attention-Deficit/Hyperactivity Disorder.” The Journal of Clinical Psychiatry (2016): n. pag. Web.
12 Dr. Maria Napoli, Paul Rock Krech, and Lynn C. Holley. “Mindfulness Training for Elementary School Students.” Journal Of Applied School Psychology (2005).
Previous Article Next Article
ADD(H) test for children
Authorization
Forgot password
Remember me
Register now
The SDVG. LIFE website is a continuation of the book and therefore new materials must meet the same standards as the book.
LIFE website is a continuation of the book and therefore new materials must meet the same standards as the book.
Hence the rules for discussion participants:
- - Civilized intellectual communication
- - No personal attacks
- - No policy
Pre-moderation has been introduced for the first few posts.
Welcome!
Create account
ADD(H) test for children
ADD(H) test for children up to 16 years of age inclusive in accordance with the American DSM-V methodology.
Number of questions: 18 .
For more information, see the article from the Notes.
...
To answer "Yes", the symptom must be:
- Stable during the last 6 months .
- Was expressed in measure not corresponding to the level of development .
- Had a negative impact on academic performance and/or professional activities .
...
The test is provided for informational purposes and is not intended to diagnose any disease.
Consult a doctor for diagnosis.
...
1
Often makes nervous movements with the hands or feet, or fidgets and wriggles while sitting in a chair.
Yes
No
2
Often interrupts or annoys others.
For example, breaks into conversation, games or activities without invitation; can use other people's things without asking; for teenagers or adults - they can interfere with someone else's work or continue someone else's work themselves.
Yes
No
3
Often has difficulty waiting in line.
For example, in the shop or at the game.
Yes
No
4
Often blurts out an answer before the question has been fully asked.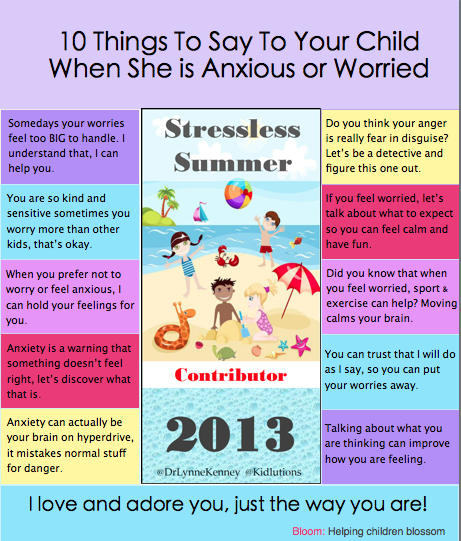
For example, completes sentences when others are speaking; cannot wait for their turn to join the conversation.
Yes
No
5
Often too talkative.
Yes
No
6
It is often in constant motion and behaves as if a motor was attached to it.
For example, absolutely unable or unable to stay comfortably in one place in restaurants or meetings; perhaps people around him consider him a restless person or a person with whom it is difficult to deal with.
Yes
No
7
Often finds it difficult to play or spend leisure time quietly.
Yes
No
8
Often runs back and forth without restraint or climbs in situations where this is unacceptable.
Note: Teenagers and adults may not be running, jumping or climbing, but may be restless and out of sorts.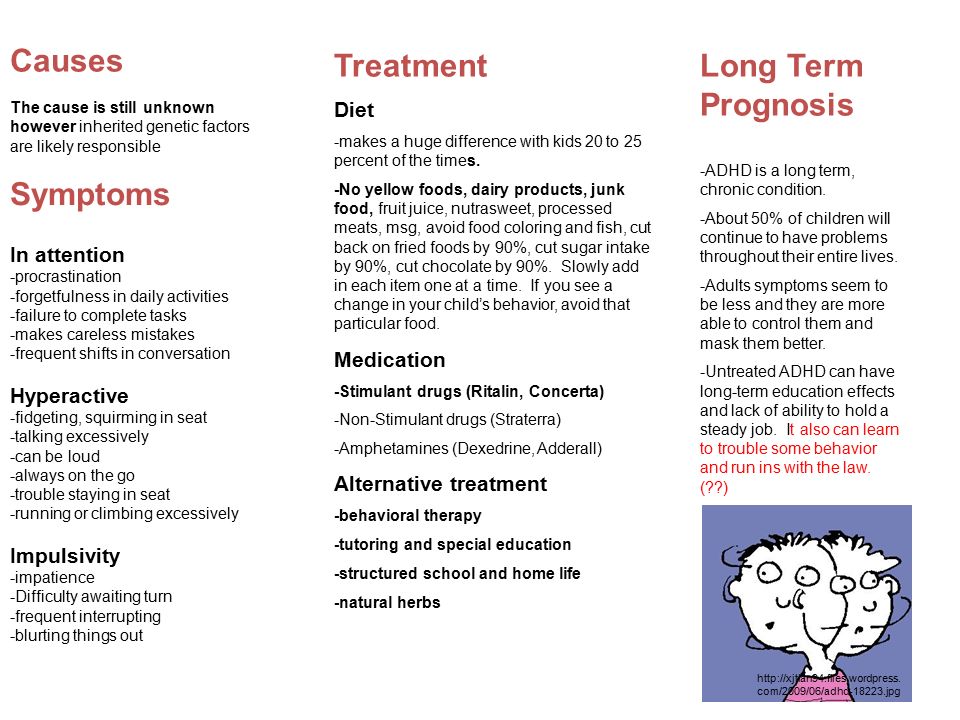
Yes
No
9
Often leaves his seat in class or in other situations where the person is expected to be seated.
For example, leaving one's seat in a classroom, in an office or other place of work, or in other situations where one is expected to be seated.
Yes
No
10
Often fails to pay due attention to details or makes careless mistakes in schoolwork, work, and other activities.
For example, does not notice or misses details, the work is done inaccurately.
Yes
No
eleven
Often forgetful in daily activities.
For example, forgetfulness in housework, while doing errands; for older teenagers and adults - they forget to return calls, pay bills, come to a meeting or appointment (to a doctor, for example).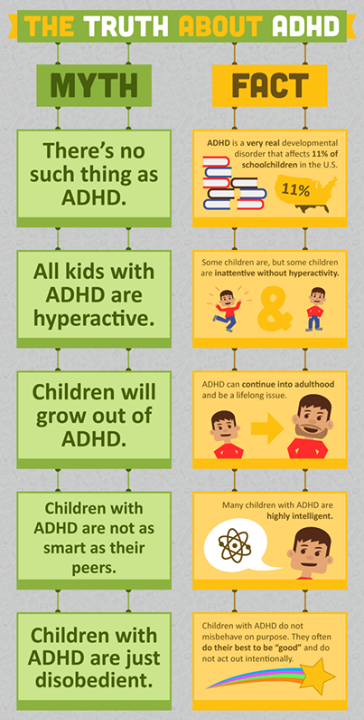
Yes
No
12
Often easily distracted by extraneous stimuli. For older teenagers and adults, this includes thoughts that are inappropriate for the time / place.
Yes
No
13
Often loses things needed for lessons or classes.
For example, notebooks, textbooks, pencils, books, tools, keys, paper forms, glasses, mobile phones.
Yes
No
14
Often avoids, dislikes, or reluctantly takes on things that require sustained mental effort.
For example, school assignments or school homework, for older teens and adults - preparing reports, filling out forms, studying long texts.
Yes
No
15
Often has difficulty organizing lessons and classes.
For example, trouble moving from one task in a chain to another, difficulty keeping materials and personal belongings in order, sloppy disorganized work, poor time management, failing to complete work on time.
Yes
No
16
Often does not follow instructions to the end and does not complete class work, chores, or duties in the workplace.
For example, starts work, but quickly loses focus and easily wanders off topic.
Yes
No
17
Often it seems that he does not listen to the speech addressed to him.
For example, his mind wanders somewhere else, even if there is no obvious distraction.
Yes
No
18
Often has difficulty maintaining attention when performing tasks or during games.
For example, has difficulty maintaining focus in lectures, during conversations, during long readings.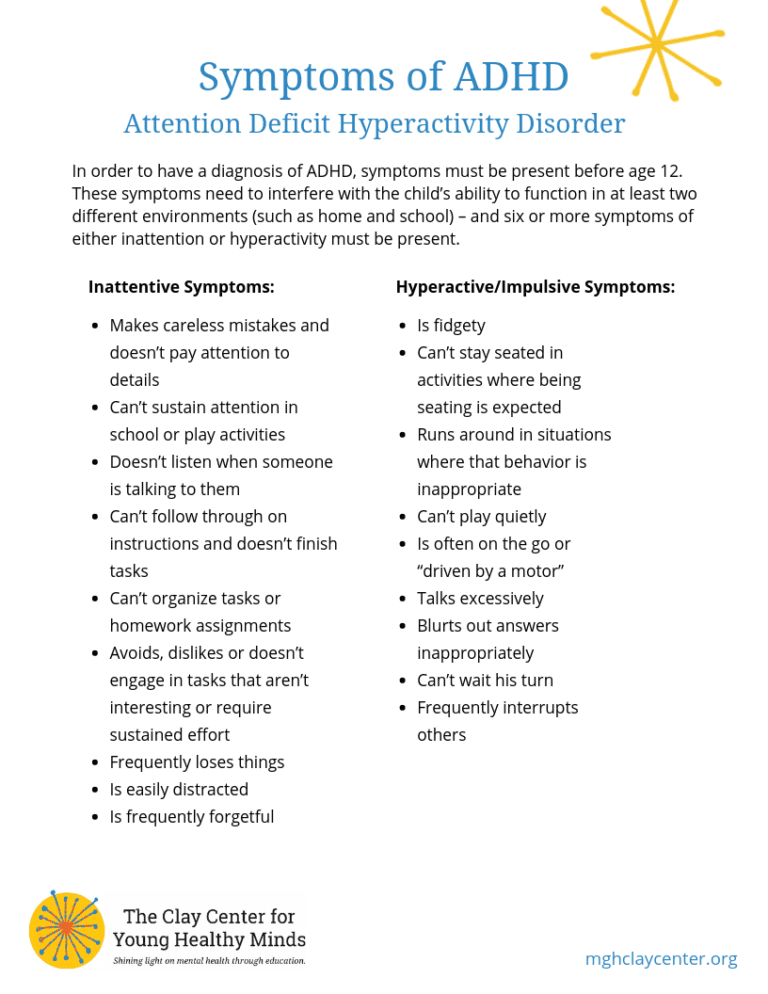
Yes
No
VR game helped to identify ADHD in children
To do this, scientists observed eye movements while children coped with everyday tasks
Scientists invited children with ADHD to go through a VR game to watch how their eyes move. It turned out that there are differences in the eye movement of children with the syndrome and those with neurotypical development when they need to focus on everyday tasks or targets. The researchers hope that this technology will help diagnose ADHD more accurately than classical methods. The results of the study were published in Scientific Reports .
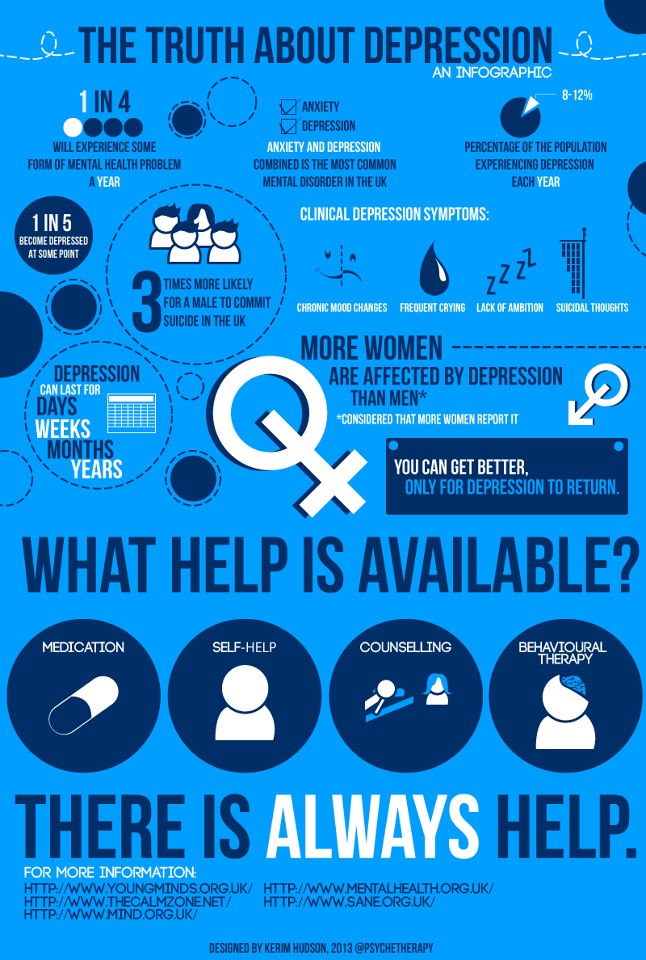
People with ADHD find it difficult to focus even on simple everyday tasks and are often distracted. Usually, in order to make this diagnosis, experts evaluate inattention, impulsivity and hyperactivity based on interviews, questionnaires or clinical observations - but all of these are often subject to subjective distortions. Therefore, doctors are still arguing about whether it is possible to find any quantitative markers to objectively diagnose ADHD.
For example, the eye movement of a person with ADHD can serve as such a marker. Previous research has confirmed that people with ADHD suffer from attention deficit disorder. They are worse at suppressing saccades (the rapid eye movements that allow us to scan the visual environment), so their eye movements are less accurate in relation to the target. It is also more difficult for such people to fixate on the target object: they more easily pay attention to strong stimuli. Therefore, one of the signs of ADHD in children can be the number and duration of fixation on bright objects that children are distracted by during tasks.
Liya Merzon from Aalto University (Finland), together with colleagues from Finland, Great Britain and France, decided to study the eye movements of children who play the game in virtual reality. In a previous study, scientists have already noticed that children often perform irrelevant actions when solving problems and, as a result, complete fewer tasks. They hoped to confirm these results with data collected about eye movement.
They hoped to confirm these results with data collected about eye movement.
The study involved 37 children with ADHD and a control group of 36 children with neurotypical development (9-13 years old). They had to go through two games and complete a number of tasks in them.
The first game, EPELI, simulated the real environment and real everyday tasks. It had 13 different scenarios to complete (for example, morning chores or returning from school), which consisted of four to six subtasks (for example, wash your hands, put your backpack back). Before each task, the dragon character gave the children instructions on all subtasks. The play environment simulated an apartment with a child's bedroom, a kitchen, a living room, a parent's bedroom, and a bathroom. Participants wore VR glasses and had to move around the virtual apartment and interact with objects using a controller. At the same time, there were 47 necessary items in the apartment and 243 more - irrelevant, distracting.
Based on the results of the game, scientists calculated various indicators, for example, the overall score based on the results of successfully completed tasks, the number of controller movements, and others. In all respects, the groups differed from each other: children with ADHD completed fewer subtasks, and their navigation was less efficient. On the other hand, they performed more controller movements (p = 0.0085) and actions in general (p = 0.0048) than the control group.
Participants with ADHD also had shorter saccades (average 57 ms versus 67 ms in the control group) with lower amplitude (average 5.44 degrees versus 6.29degrees at the control) in all tasks in the game. At the same time, the nature of eye movements differed between groups throughout the game and did not depend on specific scenarios or features of the stimulus.
An example of completing tasks in EPELI The researchers also found that children with different duration fix their eyes on relevant and irrelevant objects during tasks. But even taking into account the fact that children with ADHD kept their eyes on distracting objects longer compared to the control group, this effect did not reach a significant level (p = 0.060).
But even taking into account the fact that children with ADHD kept their eyes on distracting objects longer compared to the control group, this effect did not reach a significant level (p = 0.060).
In the second game, Shoot the Target, children had to find targets in virtual space and shoot at them by looking at the object. Children with ADHD coped worse with these tasks than participants in the control group (p = 0.0018), but scientists did not record differences in movements and their speed between groups. Just like in the previous game, the scientists noticed longer fixation, shorter saccades, and lower amplitude in children with ADHD.
Thus, VR eye tracking has served as a reliable marker of attention deficit. The authors of the work believe that eye movement can be used to make a more accurate diagnosis. But they admit that it is still difficult to understand whether differences in eye movement are a cause or effect. Perhaps participants with ADHD perform worse on tasks because they have difficulty with visual attention.