Zoloft increasing dose
When Should You Increase Your Zoloft Dosage To Treat Anxiety?
Content
- Overview
- What is Zoloft?
- What is the proper Zoloft dosage for anxiety?
- When to increase your Zoloft dose for anxiety?
- Talk to your doctor first
- Factors that could impact whether you need a higher dose
- Zoloft’s effects on anxiety
- The lowdown
If you’ve been prescribed Zoloft to treat your anxiety, but it’s not quite doing the job, you might find it tempting to increase your dosage.
However, Zoloft is a psychiatric medicine, so it’s crucial you don’t take more or less than the dosage prescribed. However, your doctor may be able to prescribe a stronger dose if needed, if they determine that this is the right course of action.
Have you considered clinical trials for Anxiety?
We make it easy for you to participate in a clinical trial for Anxiety, and get access to the latest treatments not yet widely available - and be a part of finding a cure.
Check your eligibility
Zoloft, or sertraline as it is known under its generic name, is a psychiatric medicine used largely in the treatment of depression and anxiety.
Taken orally, Zoloft belongs to a group of antidepressants called selective serotonin reuptake inhibitors, or SSRIs. SSRIs are a commonly prescribed antidepressant that improves mood by blocking the mechanisms that absorb serotonin, allowing it to be available to the brain for longer.
This is important because serotonin is known for its ability to induce feelings of happiness. In fact, serotonin is often referred to as the “happy hormone.”
Starting Zoloft
The appropriate dosage of Zoloft will be determined by a doctor and is likely to differ depending on the patient and their individual needs.
Typically, 50 milligrams once a day is a standard starting dosage for adults with depression, obsessive-compulsive disorder, and premenstrual dysphoric disorder. Some conditions tend to start with a lower dose of 25 milligrams once a day, like panic disorder.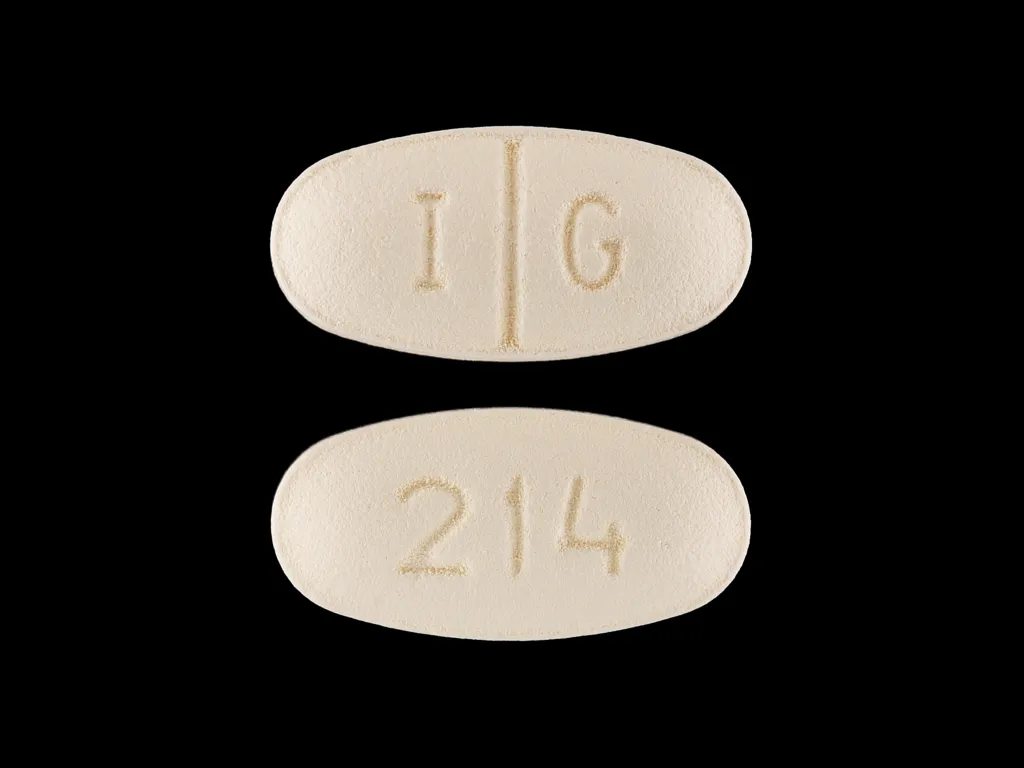
Maximum dose
Your Zoloft dose must stay within a safe range, so you’re unlikely to be prescribed anything higher than 150-200 milligrams per day. In the end, your dosage will depend on the condition being treated and your individual needs.
Children
Children can also benefit from Zoloft but will follow a different dosage regimen. This dose will be at the discretion of your doctor and is based on your child’s age, size, and therapeutic need. For instance, for children aged 6 to 12 years of age with obsessive-compulsive disorder, a standard starting dose is 25 milligrams once a day.
If you have concerns or questions about your dosing, make sure to discuss it with your doctor before making any changes to your medication regimen.
If you’re taking Zoloft, but aren’t feeling any improvement in your anxiety levels, it can be tempting to simply up your dose – but it’s important not to.
Zoloft is not an instant relief medication. SSRIs do not exert instant effects like, pain relief does. Zoloft (and other SSRIs) is a little more complicated and it takes longer for its full effects to be felt.
Zoloft (and other SSRIs) is a little more complicated and it takes longer for its full effects to be felt.
These medications take time for their effectiveness to peak. Zoloft works by blocking the reuptake of serotonin and it takes repetitive dosing and time for the medication to be able to exert its effects on your system. It can take around two to six weeks before you start to experience a reduction in your anxiety symptoms.
If after this period you still haven’t seen any benefits then you may want to talk to your doctor about altering your Zoloft dose.
While Zoloft can have a positive impact on anxiety, it can also come with some minor side effects. Zoloft can also increase your risk of serious side effects if you have an existing medical condition or are taking other medication.
Therefore, increasing your Zoloft dose without approval from your doctor should not be done under any circumstances. This can have serious detrimental effects on your health and wellbeing and can result in coma and seizures.
Zoloft side effects and drug interactions
The following side effects¹ and potential drug interactions² highlight why it’s important to follow your Zoloft prescription and avoid increasing your dosage without your doctor's approval.
Potential side effects of Zoloft include:
Nausea
Loss of appetite or indigestion
Diarrhea
Excessive sweating
Tiredness or fatigue
Sexual performance issues, e.g. reduced sex drive, failure to ejaculate
Sleep disturbances, e.g. sleepiness or insomnia
Shaking hands
Increased agitation and irritability
Suicidal ideations
Impulsive and dangerous behavior
Worsening of depression and/or anxiety symptoms
Violent behavior
Seizures
Manic behavior, e.g. fast-paced and racing thoughts, extreme high and low emotions, excessive energy, and talking grandiose thinking.

An allergic reaction (typical symptoms include trouble breathing, a rash or hives, and swelling).
Eye problems, e.g. blurred vision, red eyes, pain in the eyes.
Serotonin syndrome includes symptoms such as hallucinations, agitated behavior, loss of consciousness/coma, increased heart rate, vomiting, and rigid muscles
There are also specific side effects that can affect children taking Zoloft:
Nose bleeds
Urine problems, e.g. frequently needing to urinate or leaking urine
Changes to menstruation, specifically heavier periods
Agitation or fidgeting
Aggressive or irritable behavior that is out of the norm
Changes to physical development. You may see your child’s growth rate start to slow down and/or weight gain.
Conditions that can increase your risk of Zoloft side effects:
Glaucoma: People with glaucoma can experience an increase in glaucoma attacks if they take Zoloft and should therefore talk to their doctor to determine if the SSRI is appropriate.
Seizure conditions: Since seizures are already a potential side effect of Zoloft, the medication should be considered carefully in people with a seizure condition lest it increases their frequency or severity³.
Liver issues: Patients with liver problems should take care when starting Zoloft as they can experience stronger effects than normal, due to their liver’s inability to break down the medication.
Bipolar disorder: Bipolar disorder is a possible contraindication for Zoloft as you may experience a higher risk of manic symptoms.
Kidney issues: Much like the liver, if your kidneys aren’t functioning well then you may not be able to filter medications properly, resulting in higher levels of Zoloft in your system.
Side effects that can occur when Zoloft is taken alongside certain medications:
Increased risk of serotonin syndrome can occur when Zoloft is taken with monoamine oxidase inhibitors, linezolid, intravenous methylene blue, triptans, lithium, fentanyl, tramadol, and St John’s wort.

Heart problems can occur when Zoloft is taken with pimozide.
Bruising and bleeding can occur when taken with nonsteroidal anti-inflammatory medications, e.g. aspirin.
A build-up of medications (including Zoloft) can occur in your system when taken with cimetidine, tricyclic antidepressants.
While it’s important to stick to the dose recommended by your doctor, there are legitimate and safe reasons why your doctor may increase your Zoloft dose.
For instance, your doctor may increase your Zoloft dose if you aren’t seeing a significant reduction in your anxiety symptoms, so long as it is safe.
The risks of altering your Zoloft dosage without medical approval are substantial. However, with a prescribed dosage and professional advice, Zoloft can have a positive impact on your anxiety and improve your quality of life.
Research tells us that Zoloft can effectively reduce anxiety scores. One study⁴ found that Zoloft managed to significantly improve anxiety, worry, and depressive symptoms in patients (60 years and older), with an anxiety diagnosis (generalized anxiety disorder, panic disorder, agoraphobia, or social phobia).
One study⁴ found that Zoloft managed to significantly improve anxiety, worry, and depressive symptoms in patients (60 years and older), with an anxiety diagnosis (generalized anxiety disorder, panic disorder, agoraphobia, or social phobia).
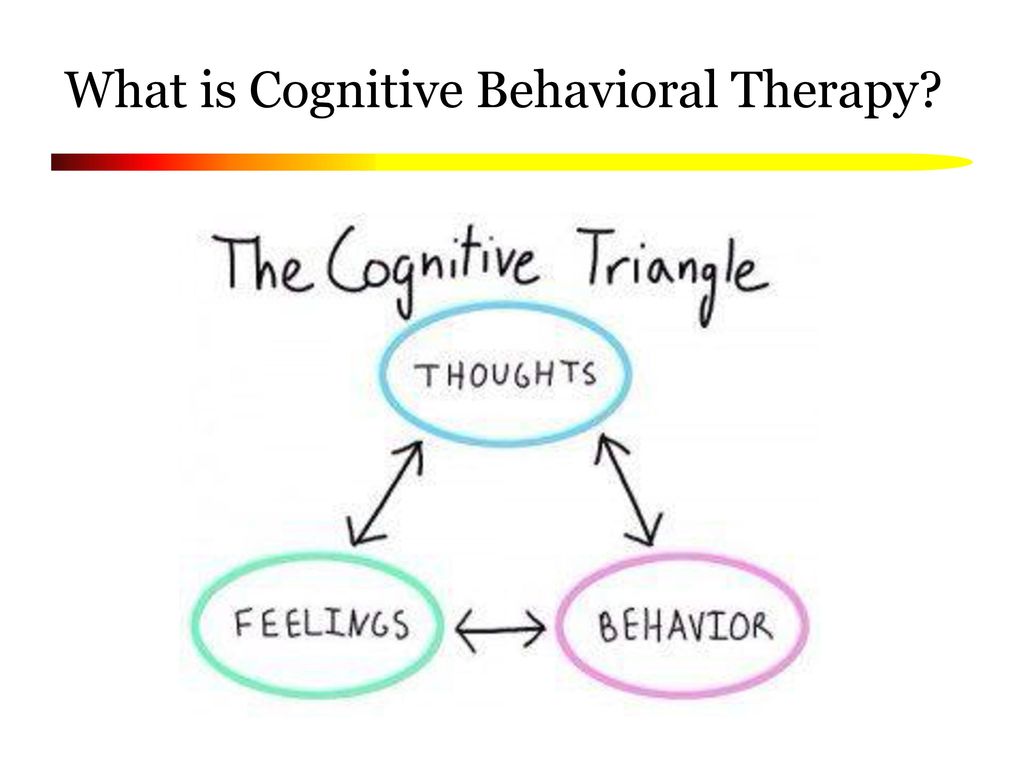
Zoloft is also an effective treatment option for children suffering from anxiety. A 2018 study found that SSRIs significantly reduced anxiety symptoms⁵ in children. The study also found that a combination of Zoloft and cognitive behavioral therapy was a particularly effective treatment option.
What To Expect When You Take Anxiety Medication
Zoloft is an effective treatment for managing anxiety. Your doctor will prescribe Zoloft if they believe it is a good fit, and may gradually increase your dose until you start to see results or reach a maximum dose.
However, since Zoloft can have some serious side effects and can interact negatively with other drugs, do not increase your dosage until you have consulted a medical professional.
Zoloft for anxiety; Dosages, interactions, and more
Zoloft for anxiety | Dosage | How long does it take Zoloft to start working? | Side effects | Warnings | Interactions | Alternatives
Living with anxiety can make daily life difficult. Fortunately, there are many treatment options available for anxiety that can help people find relief from their symptoms. Zoloft is one medication that may help. In this guide, we’ll explain to you what Zoloft is and how to take it for anxiety.
Taking Zoloft for anxiety
Anxiety is a prevalent condition that affects people all over the world. An estimated 31% of all adults will experience an anxiety disorder at some point in their life, and SingleCare’s anxiety survey found that 62% of respondents experienced some degree of anxiety. Zoloft is the brand name of a generic medication called sertraline. It’s a type of antidepressant called a selective serotonin reuptake inhibitor (SSRI) that treats anxiety by slowing down the reabsorption of serotonin. Zoloft treats several mental health conditions:
Zoloft treats several mental health conditions:
- Social anxiety disorder
- Panic disorder
- Depression (also known as major depressive disorder)
- Post-traumatic stress disorder (PTSD)
- Obsessive-compulsive disorder (OCD)
- Premenstrual dysphoric disorder
Zoloft may treat anxiety if psychological treatments, like cognitive behavioral therapy, aren’t working or if your healthcare professional/psychiatrist thinks it will improve your quality of life in combination with other methods like therapy.
What’s the right Zoloft dosage for anxiety?
The right dosage of Zoloft for anxiety varies by the severity of anxiety and whether the patient has other medical conditions. In general, though, the initial therapeutic dosage of Zoloft for anxiety is 25 mg or 50 mg per day.
Zoloft tablets are available in three dosage strengths: 25 mg, 50 mg, and 100 mg. The maximum dose of Zoloft is 200 mg per day (which can be taken as two 100 mg tablets).
The maximum dose of Zoloft is 200 mg per day (which can be taken as two 100 mg tablets).
Most studies suggest that the most effective dose of Zoloft is 50 mg per day. This dose is proven to be the most effective and tolerable dose for most patients. People who don’t respond to 50 mg per day may be advised by their doctor to increase their dose of Zoloft by 50 mg per day at weekly intervals to a maximum of 200 mg per day. For example, a doctor might recommend taking 50 mg daily for one week, then 100 mg daily for one week, etc. Always follow your healthcare provider’s instructions for use—and only change doses under the guidance and direction of your provider. Do not initiate dosage changes on your own.
Zoloft is also available in liquid form as an oral solution. The oral solution comes as a clear, colorless solution with a menthol scent that contains 20 mg of sertraline per mL, at 12% alcohol. It comes in a 60 mL bottle with a calibrated dropper with 25 mg and 50 mg measuring marks.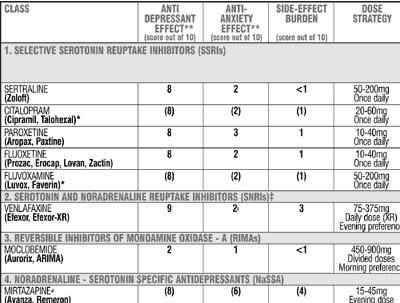 Zoloft oral solution must be mixed (just before taking) into 4 ounces (one-half cup) of water, orange juice, lemonade, ginger ale, or lemon or lime soda before consumption.
Zoloft oral solution must be mixed (just before taking) into 4 ounces (one-half cup) of water, orange juice, lemonade, ginger ale, or lemon or lime soda before consumption.
Always follow your healthcare provider’s instructions for use and do not change the dose of Zoloft on your own. Symptoms of a Zoloft overdose may include seizures, coma, heart problems, high blood pressure, and serotonin syndrome. Serotonin syndrome is a potentially life-threatening condition that can occur from the buildup of excess serotonin and requires emergency medical attention. If you think you overdosed on Zoloft, you can call Poison Control at 1-800-222-1222, but if your symptoms seem severe or life-threatening, you should call 911 and go directly to the emergency room.
When does Zoloft start working for anxiety?
Zoloft doesn’t work immediately, so don’t stop taking Zoloft if your symptoms don’t improve right away. It takes two to six weeks to start reducing anxiety symptoms. Some people may feel a reduction in their anxiety symptoms within the first week of taking Zoloft, but this shouldn’t be expected for everyone.
How does Zoloft make you feel?
According to the National Alliance on Mental Illness, some of the earliest signs that Zoloft is working are improvements in sleep, energy, or appetite. These improvements could happen one to two weeks into taking the medication.
More significant changes, like feeling less depressed or regaining interest in daily life, may take six to eight weeks to occur. Over time, many people will notice a substantial difference in their anxiety symptoms, and some people may eventually have no symptoms at all.
Side effects
Here are the most common side effects of Zoloft you may experience when you start taking it:
- Dizziness
- Loss of appetite
- Lightheadedness
- Dry mouth
- Nausea
- Diarrhea
- Increased sweating
- Restlessness
- Sexual side effects like sexual dysfunction
- Fatigue
- Trouble sleeping
- Nervousness
Some side effects may be more noticeable at first, but then disappear as your body gets used to the medicine.
Sexual side effects
Sometimes, individuals who take an antidepressant like Zoloft may experience sexual side effects. In men, symptoms may include delayed ejaculation, decreased sex drive, and/or problems getting or maintaining an erection—and in women, decreased sex drive and problems having an orgasm. Patients who are experiencing sexual side effects should consult their healthcare provider. Although it may feel uncomfortable to talk about these issues with your prescriber, it is very common and there are solutions available.
Serious side effects
Although it’s rare, Zoloft may cause more serious side effects like unusual weight loss, low sodium blood levels, increased risk of bleeding (especially when combined with certain drugs like blood thinners or NSAIDs), seizures, and serious allergic or skin reactions.
Serious allergic or skin reactions
While rare, having a serious allergic or skin reaction can be life-threatening and cause death. People with symptoms of an allergic reaction (hives, difficulty breathing, swelling of the face, lips, tongue, or throat) should get emergency medical help right away.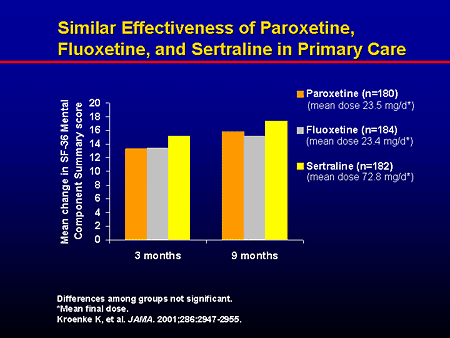 Likewise, those with symptoms of a serious skin reaction (hives, blistering or peeling skin, red or purple rash, fever, burning eyes, sore throat) should seek emergency medical attention.
Likewise, those with symptoms of a serious skin reaction (hives, blistering or peeling skin, red or purple rash, fever, burning eyes, sore throat) should seek emergency medical attention.
Increased risk of bleeding
SSRI drugs, including Zoloft, can increase the risk of bleeding (which may range from mild to life-threatening), especially when taken with certain other medications. Examples of these medicines include:
- Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) such as Celebrex (celecoxib), Mobic (meloxicam), or Motrin (ibuprofen)
- Anticoagulants such as Coumadin (warfarin)
- Antiplatelet drugs such as Plavix (clopidogrel)
Patients should discuss all the drugs they take with their healthcare professionals before taking Zoloft. This includes prescription and OTC drugs, vitamins, and supplements.
Warnings
Zoloft also comes with a black box warning for suicidal thoughts and behaviors. A black box, or boxed, warning, is the strongest warning required by the US Food and Drug Administration (FDA). Short-term studies have shown that antidepressants increased the risk of suicidality in children, adolescents, and young adults compared to a placebo. However, people of any age who take Zoloft should be monitored, so seek medical advice right away if you’re taking Zoloft and start to have mood changes and/or suicidal thoughts or behaviors.
A black box, or boxed, warning, is the strongest warning required by the US Food and Drug Administration (FDA). Short-term studies have shown that antidepressants increased the risk of suicidality in children, adolescents, and young adults compared to a placebo. However, people of any age who take Zoloft should be monitored, so seek medical advice right away if you’re taking Zoloft and start to have mood changes and/or suicidal thoughts or behaviors.
Contraindications
Zoloft is not safe for everyone. Zoloft should not be used in:
- People who are allergic to sertraline or any SSRI medication such as Paxil (paroxetine), Prozac (fluoxetine), or Lexapro (escitalopram)
- People who have taken an MAOI drug in the last 14 days
- People with moderate to severe liver problems (Child-Pugh Class B-C)
Additionally, Zoloft should never be stopped abruptly (with few exceptions, such as in the event of a life-threatening reaction). When it is time to stop taking Zoloft, the healthcare professional will provide a tapering schedule so that the medication is stopped safely and slowly, over a period of time. Stopping Zoloft abruptly can cause withdrawal symptoms such as nausea, sweating, vertigo, shock sensations, confusion, sleep problems, and seizures.
When it is time to stop taking Zoloft, the healthcare professional will provide a tapering schedule so that the medication is stopped safely and slowly, over a period of time. Stopping Zoloft abruptly can cause withdrawal symptoms such as nausea, sweating, vertigo, shock sensations, confusion, sleep problems, and seizures.
There are also certain instances when Zoloft may be used with caution and close monitoring. Before taking Zoloft, tell your prescriber about all of the medications you take and all of your medical conditions, especially if you:
- Consume alcohol
- Are at risk of bleeding
- Have liver problems
- Have mental health conditions or a history of mental health conditions
- Have glaucoma
- Have electrolyte abnormalities
- Have (or have a history of) heart or heart rhythm problems
- Have a history of seizures
Interactions
Talk to your doctor about how to take Zoloft if you’re taking any of the following medications:
- Other medications that increase serotonin because of the risk of serotonin syndrome (such as other antidepressants, opioid pain medications, muscle relaxants, cough suppressants, or migraine medications in the triptan drug class)
- Disulfiram
- Blood thinners such as warfarin
- NSAIDs such as ibuprofen
- St.
 John’s Wort
John’s Wort - Lithium
- Nardil (phenelzine)
- Parnate (tranylcypromine)
- Marplan (isocarboxazid)
- Azilect (rasagiline)
- Emsam (selegiline)
- Orap (pimozide)
Zoloft taken with monoamine oxidase inhibitors (MAOIs) or other drugs that increase serotonin (such as other antidepressants, triptans, and dextromethorphan which is found in cough and cold products) could cause serotonin syndrome, a life-threatening emergency that can cause hallucinations, seizures, comas, tremors, delirium, and other serious side effects.
RELATED: Is it safe to take anti-anxiety medication with alcohol?
What is the most effective antidepressant for anxiety?
There is no single antidepressant that’s best for treating anxiety. What works for one person may not work for another. Depression symptoms will completely go away for about 1 out of every 3 people who take SSRIs, but more research still needs to be done on why SSRIs work for some people and not for others. Your healthcare provider is the best person to ask which antidepressant will be most effective for you.
Your healthcare provider is the best person to ask which antidepressant will be most effective for you.
“Other SSRI medications can be effective for anxiety such as Prozac or Celexa or Paxil, yet each has some side effects—notably lowered libido and weight gain,” says Uma Naidoo, MD, a psychiatrist at Mass General Hospital in Boston. “Benzodiazepines are very effective in the short term while under the care of a doctor, but these are potentially addicting medications and must be used with immense caution and only as a short-term measure, e.g., grief following the death of a family member,” says Dr. Naidoo. Benzodiazepines are controlled substances, and have the potential for abuse and dependence, and include drugs such as Klonopin (clonazepam) and Xanax (alprazolam).
As mentioned earlier, your healthcare provider is the best person to ask about how to treat anxiety. Medications can be effective in treating anxiety, but Dr. Naidoo says you may have other options as well. Some additional ways to combat anxiety, in combination with your prescription medication, may include:
- Talk therapy: Patients with anxiety can benefit from regular sessions with a therapist.
- Physical exercise: Regular physical exercise (as approved by your doctor) can be helpful to many people, improving symptoms of anxiety and helping you sleep better, in addition to improving overall health. Talk to your doctor about an exercise plan that is appropriate for you.
- Mindfulness and breathing exercises: Mindfulness can help people focus on the present and help reduce anxiety and depression.
- Dietary changes: Eating regular, healthy meals will help keep your blood sugar steady, avoiding that jittery feeling from low blood sugar, which may add to anxiety. A registered dietician is often covered by insurance and can be a very helpful resource in instituting dietary changes.
Your physician can help you come up with a treatment plan that will fit well into your life.
When to see a doctor
If you are experiencing anxiety that is interfering with your quality of life, do not hesitate to seek treatment. Start with your primary care provider, who can often recommend some lifestyle changes, start you on a medication, and/or provide recommendations for a therapist. You will be on your way to feeling better soon, and you will be glad you reached out for help.
Start with your primary care provider, who can often recommend some lifestyle changes, start you on a medication, and/or provide recommendations for a therapist. You will be on your way to feeling better soon, and you will be glad you reached out for help.
do they help, treat or relieve symptoms, are they addictive, do they make you gain weight
Daniil Davydov
medical journalist
Author profile
human.
At the same time, the cures for this disease are surrounded by many myths. Antidepressants are accused of ineffectiveness and severe side effects, but often the problem is not with the drugs themselves, but with their misuse.
We collected 8 myths about antidepressants and found out how close they are to the truth.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Myth 1
Antidepressants almost never helpMost likely, this myth arose due to the fact that antidepressants do not work in all patients - so even some doctors and scientists doubt their effectiveness. However, antidepressants cannot be called ineffective, there are just important nuances in the use of these drugs.
Antidepressants are a class of drugs that normalize the level of neurotransmitters, that is, chemicals that help nerve cells in the brain exchange information.
What are Antidepressants - International Drug Database RxLis
What Medications Help Clinical Depression in Adults - International Primer for Physicians UpToDate
How Antidepressants Help Pain - Mayo Clinic Bulletin
All Antidepressants Used to Treat Depression in Adults , work - The Lancet
Who Antidepressants Help and Who Don't - Clinical Guidelines for British PhysiciansPDF, 141 KB
These medicines help people whose problems are due to a deficiency or excess of neurotransmitters. Antidepressants reduce symptoms of depression, obsessive-compulsive disorder, generalized anxiety disorder, post-traumatic stress disorder, and bipolar affective disorder.
Antidepressants reduce symptoms of depression, obsessive-compulsive disorder, generalized anxiety disorder, post-traumatic stress disorder, and bipolar affective disorder.
There is evidence that antidepressants are effective for chronic pain. Antidepressants increase the amount of neurotransmitters in the spinal cord, which reduces pain signals.
Most specialists have no doubts that antidepressants work. For example, according to the British Royal College of Psychiatry, 50-65% of people with depression who take antidepressants feel better - compared with 25-30% of those who take a placebo.
However, there are situations where the benefit of antidepressants is questionable. For example, antidepressants are good for treating moderate to severe depression, but do not work well for people with mild depression - psychotherapy is more suitable for them.
And there are situations when these medicines were prescribed by mistake. Then antidepressants really won't help.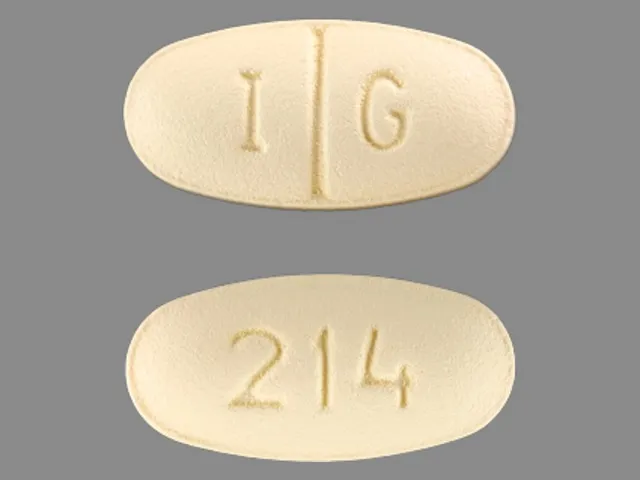
When antidepressants don't help
Sergey Divisenko
psychotherapist
There are three cases when antidepressants most often cause problems.
The antidepressant didn't work because the doctor prescribed the wrong dose. Minimum doses of these drugs do not help in half of the cases. Then competent doctors increase the doses to those recommended in clinical guidelines, while illiterate ones refuse them.
Sometimes, in order for antidepressants to work, they need to be augmented—i.e., enhanced—with other classes of drugs. For example, second-generation antipsychotics, or normothymics, that is, drugs that stabilize mood. If this is not done, the person taking antidepressants will not feel relief.
The antidepressant didn't work because the doctor misdiagnosed and was trying to treat a condition that these drugs don't work for. To help a person, one had to either use other drugs or use non-drug methods of treatment: for example, psychotherapy, transcranial stimulation, or electroconvulsive therapy.
For example, in bipolar disorder, symptoms can be very similar to depression or anxiety. But with bipolar disorder, antidepressants help only if they are used together with other drugs - mood stabilizers. By themselves, they will either work for a short time, or they will not work, or they can cause a phase inversion - that is, a person will switch from a depressive phase to a manic one.
The patient was not helped by a particular antidepressant, but another might. Antidepressants differ in the principle of action - on this basis they are divided into classes. It happens that one antidepressant does not work, but another from the same or another class helps. If the treatment does not work, you should not stop drug therapy, but continue to look for a drug that will help this particular patient.
Myth 2
Antidepressants only relieve symptoms, but do not eliminate the cause of the disorder In most cases, this is not a myth. However, in some situations, antidepressants act on the cause of the disorder.
Depression is a heterogeneous disease. Experts identify a different number of subtypes of depression - from 4 to 12. But for our purposes, depression can be divided into two large subtypes.
American Criteria for Depressive Disorders - A Handbook for Psychiatrists DSM-5PDF, 32 MB
Understanding Depression - An International Primer for Physicians UpToDate
associated with depression. Disorders that can be attributed to this group are more common.
If these causes affect a person long enough and he does not understand how to deal with them, depression may develop. In this situation, antidepressants act as drugs that alleviate the symptoms of the disease. To influence the cause of the problem, psychotherapy is needed.
Depression provoked by internal causes. Approximately 7% of people with depression have the right way of thinking, no internal conflicts and injuries, and no serious illnesses. In this situation, the cause of depression is the lack of neurotransmitters: serotonin, norepinephrine and dopamine in the synapses of brain nerve cells. In such people, the antidepressant acts precisely on the cause of the disease, that is, it corrects the production of serotonin in neuronal synapses.
In such people, the antidepressant acts precisely on the cause of the disease, that is, it corrects the production of serotonin in neuronal synapses.
Myth 3
As soon as it gets better, you can stop taking the antidepressantThis is also not entirely a myth - it would be more correct to call it a belief that is true only for some, but not for all patients with depression.
It is generally advised to continue taking antidepressants for at least six months after remission. If the duration of the disease is short, that is, the person was ill for about two weeks, then for the onset of remission, one or two months usually need to take medication. If the duration of the disease is long, from several months or years, then more time is required for the onset of remission. It’s impossible to say exactly how much: different people with depression have different recovery times.
Some people have recurrent depression. In this case, the period during which you need to take the medicine depends on how many bouts of depression have already been during your life. If more than three, it is recommended to take antidepressants for several years or for life.
If more than three, it is recommended to take antidepressants for several years or for life.
Myth 4
Antidepressants cause addictionPerhaps the roots of this myth are that some people need to take depression medication for life. And at the beginning of treatment, some patients have to increase the dose. But in fact, antidepressants do not cause either true physical or drug dependence.
True physical dependence on a drug is a situation where a person becomes so addicted to a drug that when it is withdrawn, the symptoms of the disease sharply increase. People who are dependent on the drug have to increase the dosage, otherwise the drug stops helping.
What is True Drug Addiction—Bulletin of the National Institute for the Study of Drug AbusePDF, 7 MB
What is Drug Addiction—Bulletin of the American Psychiatric Association
Drug dependence may include physical dependence on a drug. But this addiction has a unique feature. Dependence can also develop in a healthy person who used the drug not to recover, but to enjoy it.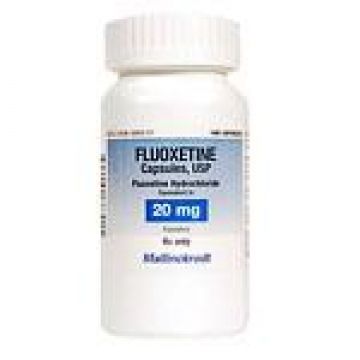 But when he tries to quit the drug, he still experiences physical suffering, which is called the withdrawal syndrome. As a result, a person is forced to look for a new dose of a drug.
But when he tries to quit the drug, he still experiences physical suffering, which is called the withdrawal syndrome. As a result, a person is forced to look for a new dose of a drug.
Although a person who takes antidepressants to treat depression gets better, the drugs themselves are neither pleasurable nor addictive. Taking them as drugs is useless.
Of all the drugs that are used in psychiatry, true physical dependence can only be caused by psychostimulants that activate mental activity and anti-anxiety, that is, benzodiazepine tranquilizers. Antidepressants are not included in this list, because there is no need to increase the dosage of correctly selected drugs from this group.
However, some people who stop taking antidepressants early sometimes experience withdrawal symptoms such as nausea, hand tremors, and some feel “shocks” in the head, similar to the sensations of an electric shock. Depressive symptoms return to patients who need to take the medicine for a very long time.
Antidepressants are sometimes abused, but they cannot cause addiction - Journal of Modern Psychiatry
To avoid unpleasant consequences, stop taking antidepressants only if the attending physician says that they are no longer needed. But even in this situation, it is necessary to cancel antidepressants slowly, that is, gradually reducing the dose. This will help avoid unpleasant side effects.
Myth 5
A person on antidepressants becomes lethargic and loses interest in lifeThis popular myth is based on real but outdated data.
These mental changes are seen in patients taking first-generation tricyclic antidepressants such as amitriptyline. It has a sedative, that is, a sedative effect. A person who takes high doses of amitriptyline can indeed become sleepy and indifferent to the outside world.
Amitriptyline - Sedative - Drugs.com International Drug Database
SSRIs do not sedate - Drugs.com International Drug Database
Current second-generation antidepressants that are recommended to start treatment with, such as selective serotonin reuptake inhibitors, or SSRIs almost never cause drowsiness and apathy.
On the contrary, in most people with depression they return interest in life.
Sometimes SSRIs do cause drowsiness, but this has not yet been proven
Sergey Divisenko
psychotherapist
It is believed that in rare cases, modern antidepressants can provoke SSRI-induced apathy. But this condition is extremely rare.
And even then psychiatrists still doubt that the cause is precisely in the drugs, and not in the patient's condition. After all, some people during the time of taking antidepressants may develop other adverse mental states in which apathy occurs: for example, schizotypal disorder, which was not noticed before.
Myth 6
Antidepressants have many side effectsThis is partly true: both SSRIs and antidepressants from other groups have side effects. But it is quite possible to deal with them.
At the beginning of treatment, when people first start taking antidepressants, many complain of increased anxiety, dry mouth, nausea, and trouble sleeping. But after a few days or weeks after the start of the course of treatment, these symptoms usually disappear. If the side effects do not stop, it makes sense to consult a doctor - he will replace the antidepressant.
But after a few days or weeks after the start of the course of treatment, these symptoms usually disappear. If the side effects do not stop, it makes sense to consult a doctor - he will replace the antidepressant.
Dealing with antidepressant side effects - advice from the Mayo Clinic staff
Here's what to do before the side effects go away:
- take your antidepressant with meals, unless the instructions say otherwise, so the antidepressant will be less annoying stomach;
- put a bottle of clean water on the desktop - if your mouth is dry, you can take a sip. Unsweetened lollipops and chewing gum also help with dry mouth;
- take a walk for at least half an hour before going to bed to make it easier to fall asleep. If you can’t sleep at all, you can ask your doctor to pick up sleeping pills.
The second most common side effect is an increase in anxiety at the beginning of antidepressant use. To avoid this problem, psychiatrists resort to two effective methods:
- titrate the dose - that is, start with the minimum dose of the antidepressant and then gradually increase it;
- at the beginning of the reception, sedatives - tranquilizers are prescribed together with the antidepressant.

The third common side effect of SSRIs, especially sertraline, known as Zoloft, and escitalopram, better known as Cipralex, is decreased libido. Approximately 20-30% of people taking antidepressants from this group experience a decrease in sexual desire to one degree or another. At the same time, it is difficult to say how much the drugs are to blame, because approximately 35-50% of people with depression have already experienced sexual dysfunction.
Many people with depression experience sexual dysfunction before starting antidepressants - Harvard Medical School Bulletin
Switching to another antidepressant usually helps, but many people prefer to wait until the medication can be stopped. In some cases, psychiatrists prescribe antidepressants from other groups in addition to the libido-lowering antidepressant. Sometimes it helps to regain interest in sex.
Myth 7
Weight gain due to antidepressants This is not a myth, but a half-truth. There are both antidepressants that contribute to weight gain, and those that do not have a similar effect.
There are both antidepressants that contribute to weight gain, and those that do not have a similar effect.
The most common complaint about weight gain during treatment is people taking the tetracyclic antidepressant mirtazapine, which actually increases appetite. Another weight gaining antidepressant is paroxetine, better known by the trade name Paxil. But "Zoloft" and "Cipralex" do not contribute to weight gain.
If a patient feels that an antidepressant is causing them to overeat, it is wise to consult a doctor and discuss a change of drug.
Myth 8
Antidepressants are expensiveTrue, but not for all patients. Most people can cure depression and not go broke.
Antidepressants from different groups vary greatly in price. There are both very expensive drugs and relatively low-cost drugs among them. At the same time, both of them work equally well. However, there are situations when a cheap antidepressant cannot be dispensed with.
On the left - inexpensive "Zoloft" for 327 R, a drug based on sertraline, on the right - the most expensive antidepressant "Ixel" based on milnacipran for 2453 R For example, there is a good antidepressant venlafaxine. The maximum dose of venlafaxine can reach up to 375 mg per day. If these are inexpensive tablets of a domestic manufacturer, then a course of treatment for a month costs about 2000 R. But sometimes inexpensive tablets are not very well tolerated: they cause headache, nausea, sweating, tachycardia, that is, rapid heartbeat. In such cases, you need to switch to a prolonged form of venlafaxine - "Venlafaxine Retard", or "Velaxin XR". But this drug is more expensive: a course of treatment will cost about 5000 R per month.
The maximum dose of venlafaxine can reach up to 375 mg per day. If these are inexpensive tablets of a domestic manufacturer, then a course of treatment for a month costs about 2000 R. But sometimes inexpensive tablets are not very well tolerated: they cause headache, nausea, sweating, tachycardia, that is, rapid heartbeat. In such cases, you need to switch to a prolonged form of venlafaxine - "Venlafaxine Retard", or "Velaxin XR". But this drug is more expensive: a course of treatment will cost about 5000 R per month.
The cost of a course of treatment with another good drug, Ixel, based on milnacipran, which is tolerated with minimal side effects, can reach up to 12,500 R. But, unfortunately, there is nothing to replace it, because this medicine does not yet have generics.
For comparison: on the left is a drug based on venlafaxine with immediate release for 443 R, on the right - with a delayed release in the same dosage for 1756 R. The price varies very muchZoloft (sertraline) in clinical practice (review) P.
 B. Gannushkina №05 2008
B. Gannushkina №05 2008 Zoloft (sertraline hydrochloride), a selective serotonin reuptake inhibitor (SSRI), is well known to Russian psychiatrists as a highly effective broad-spectrum antidepressant. The basis of the psychotropic activity profile of the drug is a distinct thymoanaleptic effect with a weak stimulating component (S.A. Mosolov, 1995).
In this review, we will try to summarize the data that shed additional light on the indications for the use of Zoloft in various types of mental pathology.
Depression
Severe and chronic depression
Zoloft is one of the main antidepressants used in severe depressive states, which also tend to become chronic. To achieve an obvious effect in these cases, 3-4 weeks are needed, and sometimes more. Usually, the effect increases as therapy continues. Nevertheless, there is evidence confirming the high effectiveness of Zoloft in the treatment of chronic depression. A long-term (76 weeks) double-blind study was performed by a group of American scientists [1], who compared the results of 77 patients taking Zoloft with a placebo group. After a 3-month treatment of the acute phase of depression, patients received drugs for another 4 months. The main goal of the study was the possibility of preventing a new episode of depression. The study included patients from 12 US medical research centers. The results of the work confirmed the high efficiency of sertraline as a prophylactic agent for preventing exacerbation of depression. Depressive symptoms appeared during treatment with sertraline in only 20 (26%) of 77 patients versus 42 (50%) of 84 patients who received placebo. The authors conclude that sertraline is highly effective in the treatment of chronic depression.
After a 3-month treatment of the acute phase of depression, patients received drugs for another 4 months. The main goal of the study was the possibility of preventing a new episode of depression. The study included patients from 12 US medical research centers. The results of the work confirmed the high efficiency of sertraline as a prophylactic agent for preventing exacerbation of depression. Depressive symptoms appeared during treatment with sertraline in only 20 (26%) of 77 patients versus 42 (50%) of 84 patients who received placebo. The authors conclude that sertraline is highly effective in the treatment of chronic depression.
Another multicenter study compared imipramine and sertraline in the treatment of chronic depression with anxiety [2]. 8 scientific centers of the USA participated in the work. A total of 426 patients treated with sertraline and 209 patients treated with imipramine were studied. In 36% of patients, clinical signs of anxiety were observed. Treatment for 12 weeks showed high efficacy of both drugs in these conditions, with a slight advantage of sertraline in reducing the anxiety component of depression (60% compared with 58%).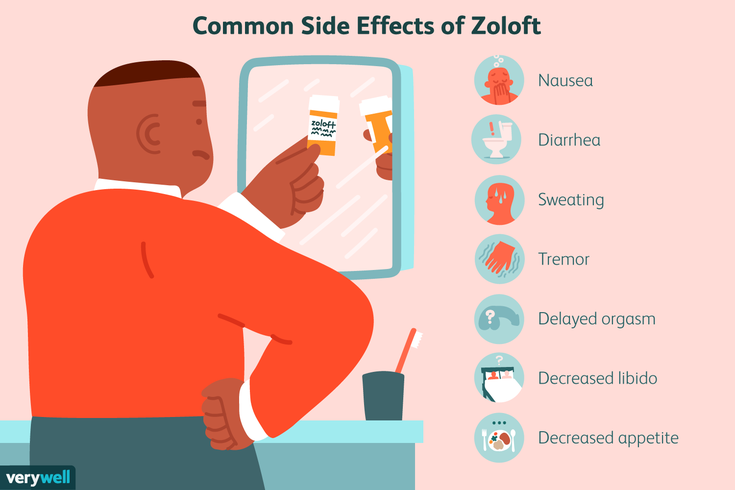 The treatment significantly improved the patients' quality of life and their psychosocial status.
The treatment significantly improved the patients' quality of life and their psychosocial status.
The work of R. Licht and S. Qvitzau is devoted to the therapeutic strategy in case of insufficient effectiveness of the treatment of severe depression. The authors evaluated the results of sertraline therapy (dose 50 mg/day) in 1629 patients with major depression aged 18–65 years. The severity of the disorder was at least 18 points on the 17-point Hamilton Depression Scale. In case of insufficient effectiveness (less than 50% reduction in the severity of disorders) within 4 weeks, treatment with sertraline continued at a dose of 100 mg / day for another 2 weeks. In case of insufficient therapeutic response, a double-blind randomized study was subsequently carried out for 5 weeks using one of three regimens: 1) sertraline 100 mg/day + placebo; 2) sertraline 200 mg/day + placebo; 3) sertraline 100 mg/day + mianserin 30 mg/day. After the first 6 weeks of therapy, a marked improvement was noted in 60% of patients; 22% dropped out of the study. Remaining 295 nonresponders (18%) were randomized. With continued therapy with sertraline at a dose of 100 mg/day, improvement was observed in 70% of patients. Approximately the same number of patients (67%) tested positive when using the combination of sertraline with mianserin, while significantly fewer patients (56%, p<0.05) responded to increasing the dose of sertraline to 200 mg/day. Thus, it was concluded that treatment with sertraline for at least 8 weeks is expedient, even in the absence of the desired effect at the initial stage of therapy.
Remaining 295 nonresponders (18%) were randomized. With continued therapy with sertraline at a dose of 100 mg/day, improvement was observed in 70% of patients. Approximately the same number of patients (67%) tested positive when using the combination of sertraline with mianserin, while significantly fewer patients (56%, p<0.05) responded to increasing the dose of sertraline to 200 mg/day. Thus, it was concluded that treatment with sertraline for at least 8 weeks is expedient, even in the absence of the desired effect at the initial stage of therapy.
Seasonal depressions
Although officially seasonal depression is not an indication for the appointment of Zoloft, this possibility is discussed [3, 4]. A.Moscovich et al. (1995) compared the effectiveness of sertraline and placebo (93 and 94 patients, respectively) in the treatment of this type of pathology for 8 weeks. Sertraline doses ranged from 50 to 200 mg/day. The results of the study demonstrated the high efficacy of sertraline in the treatment of seasonal depression. The authors emphasize the insignificance of side effects, manifested in the form of a runny nose, diarrhea, insomnia and dry mouth. The researchers conclude that sertraline is effective and well tolerated in the treatment of this type of mental illness.
The authors emphasize the insignificance of side effects, manifested in the form of a runny nose, diarrhea, insomnia and dry mouth. The researchers conclude that sertraline is effective and well tolerated in the treatment of this type of mental illness.
C. Blashko et al. evaluated the effect of sertraline in the treatment of winter depression in a double-blind, placebo-controlled study lasting 8 weeks [4]. Zoloft was used in 93 patients and placebo in 94 patients. The average daily dose of the drug was 111.3 mg. The drug showed a statistically significant advantage over placebo in all indicators of the scales used (HAM-D, HAM-A, CGI-I, etc.). In both groups of patients, no differences were recorded upon discontinuation of therapy due to the development of side effects. However, it was found that in the group treated with Zoloft, the average loss of body weight was 1.08 kg versus 0.06 kg in the placebo group. The authors concluded that sertraline is an effective and well-tolerated drug for the treatment of outpatients with seasonal affective disorder.
Atypical depression
The use of Zoloft in atypical depression has been discussed very rarely. In the domestic literature in 1995, S.A. Mosolov mentioned this. P. Beham et al. [5], who studied the efficacy of sertraline and clomipramine in 40 patients with DSM-III-R signs of atypical depression. The course of treatment lasted 8 weeks, the condition was assessed every 2 weeks, the Montgomery-Asberg scale (MADRS) and CGI were used. The authors concluded that Zoloft is at least as effective as clomipramine in the treatment of depressive symptoms in the pattern of atypical depression. Over time, interest in this problem has increased significantly. G. Mazo studied the effectiveness of SSRIs in an 8-week study of 45 patients who did not respond to treatment with amitriptyline [6]. Most of the patients had atypical depression with obsessive and senestohypochondriac symptoms. Daily doses of antidepressants were 50–100 mg of sertraline, 20 mg of fluoxetine, and 100–200 mg of fluvoxamine, respectively. About half of the patients (48.8%) were SSRI responders. The authors conclude that SSRIs were effective when amitriptyline failed to improve.
About half of the patients (48.8%) were SSRI responders. The authors conclude that SSRIs were effective when amitriptyline failed to improve.
J. Sogaard et al. compared the efficacy of sertraline and moclobemide in a 12-week double-blind study in patients with atypical depression [7]. All patients met the DSM-III-R criteria for major depression and had a Colombian criteria score of more than 4 for ADDS (Atypical Depression Diagnostic Scale). The drugs were used in the following doses: sertraline - 50 mg/day (89 patients), moclobemide - 300 mg/day (83 patients). Doses during therapy were increased to 100 mg/day (sertraline) and 450 mg/day (moclobemide).
As a result of treatment, HAM-D scores decreased significantly in patients taking both drugs, however, according to the CGI (general clinical improvement) scale, a statistically significant improvement was noted in the sertraline group from the 6th week of therapy (72.6% vs. 57%; p = 0.012). This was most clearly manifested in the reduction of anxiety symptoms and improved sleep. At the end of the study, only 13% of patients treated with Zoloft met the criteria for atypical depression (25% in the moclobemide group). The quality of life of patients treated with sertraline objectively improved. And although the frequency of side effects did not differ in both groups, the authors conclude that sertraline is more effective in the treatment of atypical depression.
At the end of the study, only 13% of patients treated with Zoloft met the criteria for atypical depression (25% in the moclobemide group). The quality of life of patients treated with sertraline objectively improved. And although the frequency of side effects did not differ in both groups, the authors conclude that sertraline is more effective in the treatment of atypical depression.
Dysthymia
In the last 2–3 years, publications have appeared on the use of Zoloft in the treatment of dysthymia [8–13]. So, A. Ravindran et al. investigated this problem for 5 years in a randomized, multicenter, double-blind, placebo-controlled study [8]. Patients (n=158) received sertraline or placebo (n=152) for 12 weeks, first at 50 mg/day, and from the 2nd week at 200 mg/day. The results showed that patients who received Zoloft got out of depression much faster and better according to the indications of all scales and questionnaires used (HAM-A, HAM-D, MADRS, CGI, etc. ). Most impressive were the improvements in quality of life. The authors conclude that Zoloft is effective in the treatment of dysthymia in cases where they are not accompanied by so-called major depressions. The same authors compared the effectiveness of sertraline and group cognitive behavioral therapy in the treatment of primary dysthymia [9]. Were studied 97 patients who received treatment during the standard 12 weeks (placebo - 50 patients, sertraline - 47 patients). Of these, 25 patients treated with sertraline and 24 with placebo received cognitive therapy. The latter did not show any apparent effectiveness, although it slightly increased the results of treatment with sertraline. In general, it has been shown that Zoloft significantly improves the condition of patients with dysthymia, reduces clinical symptoms compared with placebo. Although behavioral therapy alone is not effective for these conditions, it does improve the outcome of sertraline treatment. G. Browne et al. investigated the efficacy of sertraline in a two-phase, prospective, randomized study of 707 patients with dysthymic disorders (according to DSM-IV) [10].
). Most impressive were the improvements in quality of life. The authors conclude that Zoloft is effective in the treatment of dysthymia in cases where they are not accompanied by so-called major depressions. The same authors compared the effectiveness of sertraline and group cognitive behavioral therapy in the treatment of primary dysthymia [9]. Were studied 97 patients who received treatment during the standard 12 weeks (placebo - 50 patients, sertraline - 47 patients). Of these, 25 patients treated with sertraline and 24 with placebo received cognitive therapy. The latter did not show any apparent effectiveness, although it slightly increased the results of treatment with sertraline. In general, it has been shown that Zoloft significantly improves the condition of patients with dysthymia, reduces clinical symptoms compared with placebo. Although behavioral therapy alone is not effective for these conditions, it does improve the outcome of sertraline treatment. G. Browne et al. investigated the efficacy of sertraline in a two-phase, prospective, randomized study of 707 patients with dysthymic disorders (according to DSM-IV) [10]. During the first 6 months, all patients received sertraline (50–200 mg/day) and individual psychotherapy (IP). In the second, 18-month phase, patients continued to take sertraline or received other treatment as needed. 586 patients completed only one phase, 525 patients completed the entire 2-year study. After 6 months, 59 patients responded positively to sertraline therapy..7% of patients, 57.5% responded to treatment with sertraline with PI (46.6% with PI alone). At the end of the study, after 2 years, Zoloft treatment (with or without PI) was confirmed to be more effective than PI alone (p=0.002).
During the first 6 months, all patients received sertraline (50–200 mg/day) and individual psychotherapy (IP). In the second, 18-month phase, patients continued to take sertraline or received other treatment as needed. 586 patients completed only one phase, 525 patients completed the entire 2-year study. After 6 months, 59 patients responded positively to sertraline therapy..7% of patients, 57.5% responded to treatment with sertraline with PI (46.6% with PI alone). At the end of the study, after 2 years, Zoloft treatment (with or without PI) was confirmed to be more effective than PI alone (p=0.002).
J.Markowitz et al. in a randomized controlled 16-week study compared 4 types of treatment in patients with pure (without "major depression") dysthymic disorders: PI, supportive psychotherapy, sertraline, PI + sertraline [11]. From 93 patients completed the study 71. Although there were no statistically significant differences between groups, the authors showed that sertraline was more effective than other treatments in reducing symptoms.
M.Thase et al. in a multicenter placebo-controlled study compared the efficacy of sertraline and imipramine in 416 patients with dysthymia [14]. Patients received up to 200 mg of sertraline, 300 mg of imipramine, or placebo. A total of 310 patients completed the 12-week study. Complete remission (according to DSM-III-R criteria and HAM-D scale) was achieved in 49.5% of patients treated with Zoloft (43.5% in the imipramine group and 27.8% in the placebo group). In the group of patients treated with sertraline, there were fewer side effects, so more patients (84%) completed treatment (in the imipramine group - 67%). The authors conclude that the good tolerability of Zoloft is an important factor, since the chronic course of dysthymia requires pharmacotherapy.
J.Kocsis et al. assessed the psychosocial aspects of the previous study using a number of special scales and questionnaires (GAFS, SAS, LIFE, Q-LES-Q) [15]. The researchers' findings were consistent in that sertraline was more effective in restoring the patients' social functions. D. Hellerstein et al., analyzing the results obtained by M. Thase, join the conclusions about the high efficiency of sertraline in dysthymia [12]. However, M. Lee [16], who studied the treatment of dysthymia in 48 patients for 6 weeks, did not find significant differences in the effectiveness of sertraline and amitriptyline.
D. Hellerstein et al., analyzing the results obtained by M. Thase, join the conclusions about the high efficiency of sertraline in dysthymia [12]. However, M. Lee [16], who studied the treatment of dysthymia in 48 patients for 6 weeks, did not find significant differences in the effectiveness of sertraline and amitriptyline.
Some attention was paid to the age aspect of the treatment of dysthymia with sertraline. So, S. Bellino et al. compared the efficacy of sertraline and amisulpride (50 mg/day) in elderly patients with dysthymia in an open, prospective 6-month study [17]. The researchers concluded that both drugs were effective and suggested that they continue to study this issue in more depth. M.Nixon et al. studied the effectiveness of Zoloft in the long-term treatment of adolescent dysthymia [13]. In an open 6-month study, sertraline at doses of 50–200 mg/day was given to 23 adolescents aged 12 to 18 years. Completed a 6-week course of treatment 21 patients, 16 - a 12-week course, and 9patients completed the full course of therapy. The greatest effect was observed by the 6th week of treatment (p<0.05). Side effects (headache, runny nose) were minor. The authors conclude that sertraline is effective in adolescents with dysthymia, especially in the acute period.
The greatest effect was observed by the 6th week of treatment (p<0.05). Side effects (headache, runny nose) were minor. The authors conclude that sertraline is effective in adolescents with dysthymia, especially in the acute period.
Thus, the expediency of using Zoloft in the treatment of dysthymia was confirmed.
Postpartum depression
This indication is also not officially registered by the FDA, however, researchers are willing to resort to Zoloft in the treatment of this type of mental pathology. So, C.Epperson et al. presented the results of treatment with sertraline in women who had depression according to the DCM-IV criteria in the postpartum period [18]. This placebo-controlled study was performed double-blind for 6 weeks. Of the 13 women, 6 completed the full course; Of the 6 who completed the study, 4 were responders, with 3 of them receiving sertraline. The authors conclude that Zoloft is effective in the treatment of postpartum depression. In an open prospective study by Z. Stowe et al. studied the effect of sertraline in postpartum depression in 26 patients [19]. The HAM-D status was assessed every 2 weeks, the dose of Zoloft was standard (50–200 mg/day). The entire 8-week course of therapy was completed by 21 women. In all cases, there was an improvement in the condition from the 2nd week of treatment. In 14 patients, after the end of the course, a complete remission was recorded. Sertraline was well tolerated, side effects were minor and completely reduced by dose adjustment. Breastfeeding during treatment was continued by 6 women, which had no effect on the children. The authors draw conclusions about the high efficacy and good tolerability of Zoloft in postpartum depression and note that more in-depth approaches are needed after an open study.
In an open prospective study by Z. Stowe et al. studied the effect of sertraline in postpartum depression in 26 patients [19]. The HAM-D status was assessed every 2 weeks, the dose of Zoloft was standard (50–200 mg/day). The entire 8-week course of therapy was completed by 21 women. In all cases, there was an improvement in the condition from the 2nd week of treatment. In 14 patients, after the end of the course, a complete remission was recorded. Sertraline was well tolerated, side effects were minor and completely reduced by dose adjustment. Breastfeeding during treatment was continued by 6 women, which had no effect on the children. The authors draw conclusions about the high efficacy and good tolerability of Zoloft in postpartum depression and note that more in-depth approaches are needed after an open study.
Drug tolerance for depression in elderly patients
As A. Schmukler rightly points out in his review, indicators that are no less important than the effectiveness of psychopharmacological agents are their tolerability and side effect profile. Sertraline is a fairly “soft” drug. At the same time, no correlations were found between the concentration of the active substance in plasma and the severity of side effects (as well as clinical improvement). This, on the one hand, indicates that there is no need to control the level of the drug in the blood plasma, and on the other hand, it allows its use in elderly patients, including those with various somatic pathologies.
Sertraline is a fairly “soft” drug. At the same time, no correlations were found between the concentration of the active substance in plasma and the severity of side effects (as well as clinical improvement). This, on the one hand, indicates that there is no need to control the level of the drug in the blood plasma, and on the other hand, it allows its use in elderly patients, including those with various somatic pathologies.
The results of using sertraline at a dose of 50–200 mg/day in older patients (over 60 years) confirm its good efficacy in these cases. Along with clinical improvement, an improvement in the quality of life of patients, as well as cognitive performance, was revealed. When using the drug, there were no pronounced side effects and, in general, its tolerability corresponded to that in young patients. It is significant that the presence of somatic pathology (for example, diseases of the cardiovascular system, diabetes mellitus, arthritis) did not reduce the therapeutic effect of sertraline.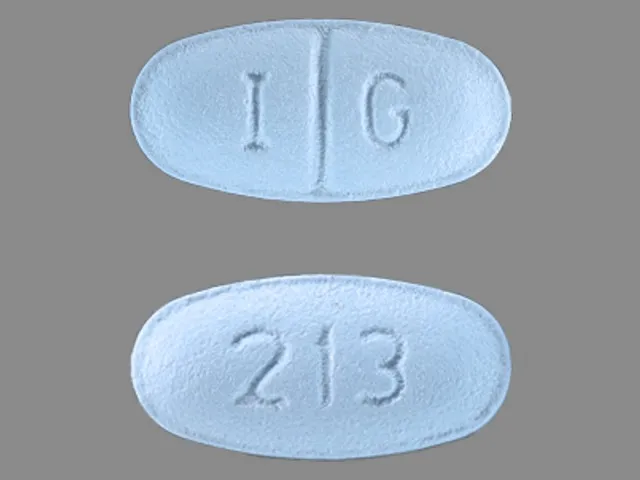 Moreover, the drug had an advantage even compared to other SSRI antidepressants due to a lower level of drug interactions, which allows combining antidepressant treatment with the treatment of somatic disorders often observed in elderly patients.
Moreover, the drug had an advantage even compared to other SSRI antidepressants due to a lower level of drug interactions, which allows combining antidepressant treatment with the treatment of somatic disorders often observed in elderly patients.
Other mental disorders
Obsessive-compulsive disorders
The effectiveness of sertraline in the treatment of obsessive-compulsive disorder (OCD) is well known to psychiatrists, it suffices to recall the work of Chouinard et al. (1990), S.N. Mosolova (1995). Nevertheless, research continues to deepen this issue and expand our understanding of the possibilities of the drug in the treatment of mental pathology of the OCD circle.
Thus, the long-term effectiveness of Zoloft in OCD was evaluated in an 80-week multicenter study consisting of two phases [20].
In phase I (52 weeks), responders (227 patients) were selected. In phase II (28 weeks), sertraline was compared with placebo in a double-blind study.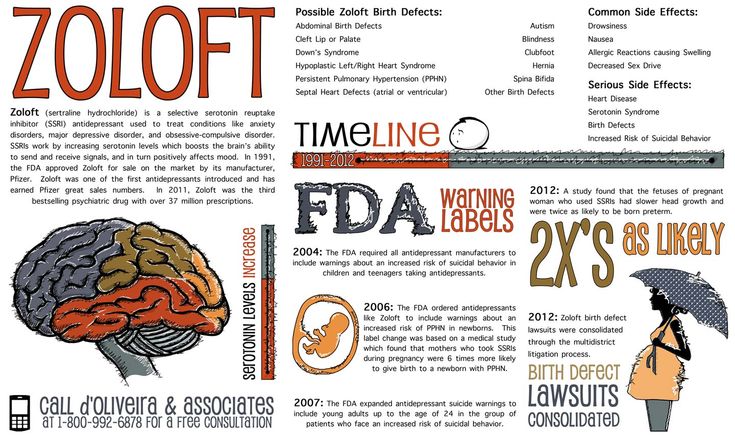 Sertraline doses ranged from 50 to 200 mg/day. Due to a non-significant response to therapy, 9% of patients receiving sertraline and 24% of patients receiving placebo discontinued participation in the study. Acute exacerbation of OCD was observed in 12% of cases with sertraline and 35% with placebo. On several scales, including the CGI, sertraline was significantly more effective than placebo and was generally well tolerated over the long term. The authors conclude that Zoloft is an effective drug for the long-term treatment of OCD, prevents flare-ups and causes few side effects.
Sertraline doses ranged from 50 to 200 mg/day. Due to a non-significant response to therapy, 9% of patients receiving sertraline and 24% of patients receiving placebo discontinued participation in the study. Acute exacerbation of OCD was observed in 12% of cases with sertraline and 35% with placebo. On several scales, including the CGI, sertraline was significantly more effective than placebo and was generally well tolerated over the long term. The authors conclude that Zoloft is an effective drug for the long-term treatment of OCD, prevents flare-ups and causes few side effects.
J.Greist et al. evaluated patients with OCD who responded to sertraline or placebo therapy for 12 weeks and then for 40 weeks, but already in a double-blind study [21]. A total of 118 patients were selected (96 received Zoloft, 22 placebo). All patients who received sertraline (as opposed to those who received placebo) noted an improvement in their condition. Of the 87 patients who completed the 52 weeks of the study, 59 (51 sertraline and 8 placebo) continued treatment in an open study setting.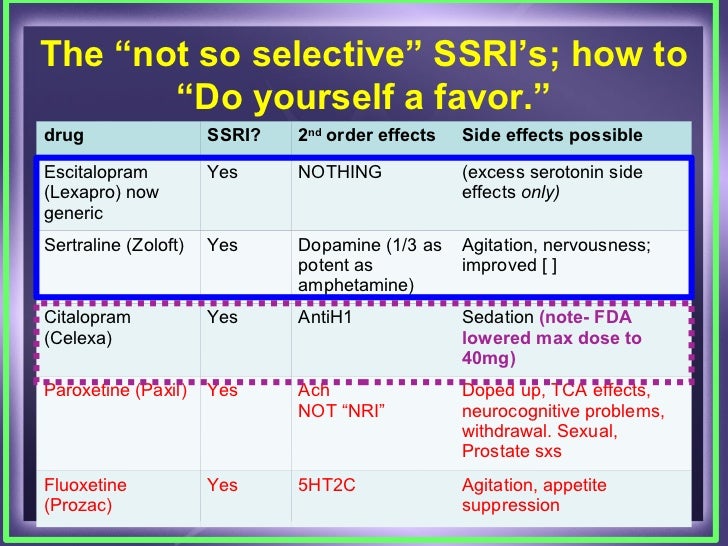 A three-phase long-term study concluded that sertraline was significantly more effective than placebo in the long-term treatment of OCD. The severity of side effects (less than 10% of cases), manifested mainly in the form of headaches, dizziness, insomnia, fatigue, dyspeptic disorders, tremors, dry mouth, decreased libido, was insignificant.
A three-phase long-term study concluded that sertraline was significantly more effective than placebo in the long-term treatment of OCD. The severity of side effects (less than 10% of cases), manifested mainly in the form of headaches, dizziness, insomnia, fatigue, dyspeptic disorders, tremors, dry mouth, decreased libido, was insignificant.
Panic disorders
Despite a slight sedative effect, Zoloft has a positive effect on patients with anxiety and panic disorders. At the same time, the reduction of anxiety occurs faster than with Prozac and some other antidepressants. M.Rapaport et al. studied the effectiveness of sertraline in the treatment of panic disorders in an 80-week multicenter study [22]. Within 52 weeks 39Eight patients received sertraline, starting at a dose of 25 mg/day, which was gradually increased to 200 mg/day depending on tolerability and clinical response of patients. Responders in the III phase of the study were divided into 2 groups (sertraline - 92 patients and placebo - 89 patients). Approximately 70% in the Zoloft group and 50% in the placebo group completed the study. Sertraline was statistically significantly superior to placebo in treatment efficacy (p=0.04) and prevention of new episodes of panic attacks (p=0.005). Zoloft was well tolerated by patients, and tolerance increased with the duration of treatment. Among the side effects in the sertraline group, headaches prevailed, in the placebo group - headaches and insomnia. Laboratory parameters in both groups did not differ significantly. The authors concluded that sertraline is an effective and safe treatment for panic disorder.
Approximately 70% in the Zoloft group and 50% in the placebo group completed the study. Sertraline was statistically significantly superior to placebo in treatment efficacy (p=0.04) and prevention of new episodes of panic attacks (p=0.005). Zoloft was well tolerated by patients, and tolerance increased with the duration of treatment. Among the side effects in the sertraline group, headaches prevailed, in the placebo group - headaches and insomnia. Laboratory parameters in both groups did not differ significantly. The authors concluded that sertraline is an effective and safe treatment for panic disorder.
Post-traumatic stress disorder
P. Londborg et al. studied the efficacy of sertraline in the treatment of post-traumatic stress disorder (PTSD) in an open, multicentre, 24-week study [23]. Sertraline was prescribed in doses starting from 25 mg/day. Depending on tolerability and clinical response, the dose was increased to 200 mg/day. We analyzed the data of 128 patients who were treated with Zoloft in the acute phase. Progressive improvement during therapy was noted using two special scales used to assess the condition of patients with PTSD. 9In 2% of responders, the initial clinical response was confirmed, and 54% of non-responders in phase I became responders in phase II. Sertraline was well tolerated, with only 8.6% of patients withdrawing from the study due to side effects. In general, side effects were manifested in the form of headaches, insomnia, dry mouth, dizziness. The authors believe that sertraline is a highly effective treatment for PTSD in both the acute and chronic phases of the disease.
Progressive improvement during therapy was noted using two special scales used to assess the condition of patients with PTSD. 9In 2% of responders, the initial clinical response was confirmed, and 54% of non-responders in phase I became responders in phase II. Sertraline was well tolerated, with only 8.6% of patients withdrawing from the study due to side effects. In general, side effects were manifested in the form of headaches, insomnia, dry mouth, dizziness. The authors believe that sertraline is a highly effective treatment for PTSD in both the acute and chronic phases of the disease.
In another study 96 patients with PTSD who responded positively to treatment with sertraline (50–200 mg/day) were divided into 2 groups (sertraline and placebo) for 24 weeks to monitor possible exacerbations; Phase II of the study continued until 28 weeks. Patients treated with sertraline showed a more stable condition compared to the placebo group. These differences were statistically significant for both women and men.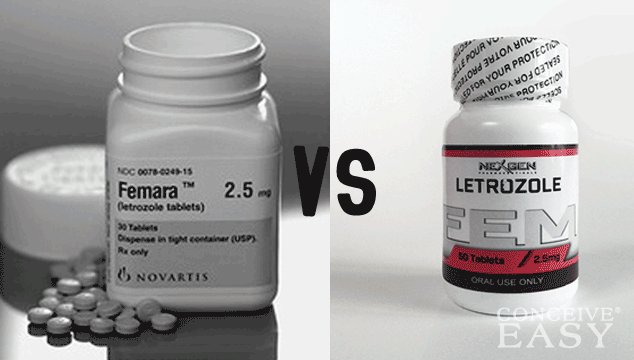
M.Rapaport et al. evaluated the effectiveness of long-term treatment with sertraline in 359patients with PTSD and concluded that long-term treatment with Zoloft provides a stable improvement in the condition of individuals suffering from PTSD.
Alcoholism and drug addiction
In an open 12-week study by K. Brady et al. evaluated the effectiveness of sertraline (at a dose of 110 mg/day) in the treatment of PTSD complicated by alcoholism in 9 patients [25]. Zoloft was shown to reduce alcohol consumption (p≤0.0005) and increase the number of alcohol-free days (p≤0.001) following sertraline treatment. R.George et al. presented preliminary results from an open-label pilot phase of a long-term, two-stage study evaluating the effect of sertraline on alcohol consumption [26]. For 6 months, patients receiving Zoloft at a daily dose of 2.75 mg/kg were regularly assessed for the frequency of use, the severity of manifestations of alcohol dependence, and the craving for alcohol. At the end of treatment, patients who underwent therapy showed a significant (p≤0.01) decrease in alcohol consumption, the severity of alcohol manifestations. It was noted that in 61% of cases the desire to drink alcohol decreased up to the complete rejection of alcohol. The authors draw preliminary conclusions that sertraline treatment has a significant effect on alcohol dependence. D.Eggerth et al. studied the effect of sertraline on the psychosocial problems of alcoholics in the same group of patients [27]. After 6 months of treatment, the scores on the DIC (Drinker Inventory of Consequences) scale decreased by an average of 77.5 points. The greatest improvement was achieved in the first 2 months of therapy. The researchers conclude that treatment with Zoloft not only leads to a reduction in alcohol consumption, but also contributes to significant positive changes in the psychosocial sphere of patients.
At the end of treatment, patients who underwent therapy showed a significant (p≤0.01) decrease in alcohol consumption, the severity of alcohol manifestations. It was noted that in 61% of cases the desire to drink alcohol decreased up to the complete rejection of alcohol. The authors draw preliminary conclusions that sertraline treatment has a significant effect on alcohol dependence. D.Eggerth et al. studied the effect of sertraline on the psychosocial problems of alcoholics in the same group of patients [27]. After 6 months of treatment, the scores on the DIC (Drinker Inventory of Consequences) scale decreased by an average of 77.5 points. The greatest improvement was achieved in the first 2 months of therapy. The researchers conclude that treatment with Zoloft not only leads to a reduction in alcohol consumption, but also contributes to significant positive changes in the psychosocial sphere of patients.
H.Pettinati et al. [28, 29] evaluated the effectiveness of sertraline (200 mg/day) in 100 patients with alcohol dependence (of which 53 were diagnosed with major depression according to DSM-III-R) in a 14-week, double-blind, placebo-controlled study. . Patients with high (type B) and low (type A) risk of alcohol dependence were studied. Sertraline, compared with placebo, significantly reduced the number of days patients drank alcohol for type A (0% vs. 22.4%; p = 0.01), which was not observed in patients at high risk (type B - 82% vs. 4.1%; p=0.46). The authors conclude that Zoloft reduces alcohol consumption, but its effect is less effective in patients at high risk of alcohol dependence.
. Patients with high (type B) and low (type A) risk of alcohol dependence were studied. Sertraline, compared with placebo, significantly reduced the number of days patients drank alcohol for type A (0% vs. 22.4%; p = 0.01), which was not observed in patients at high risk (type B - 82% vs. 4.1%; p=0.46). The authors conclude that Zoloft reduces alcohol consumption, but its effect is less effective in patients at high risk of alcohol dependence.
Child psychiatry
Depressions
The purpose of the study by a group of Russian psychiatrists headed by V.M. Voloshin was to study the effectiveness of sertraline (Zoloft) in depression, anxiety and OCD in children. Mental disorders were diagnosed according to ICD-10. 72 children (59 boys and 13 girls) aged 6–18 years were treated: 32 patients were treated in the hospital and 40 outpatients. Sertraline therapy was carried out for 8 weeks with a gradual increase (titration) and individual selection of the dose of the drug from 12. 5 to 100 mg/day. In the course of treatment, clinical observation was supplemented by examination of patients on a number of scales - Hamilton (HAM-D and HAM-A), the scale of general clinical impression (CGI). It has been established that sertraline in children is highly effective and safe (does not affect cognitive functions, does not have muscle relaxant and sedative effects). The studied drug is distinguished by the rapid onset of both thymoanaleptic and anxiolytic action. In mild depressive states, the average sufficient dose is 50 mg / day, with moderate depression and OCD in adolescents - 100 mg and the duration of therapy is more than 2 months. C. Donnely et al. evaluated the efficacy and safety of sertraline in the treatment of outpatients aged 6 to 17 years with a diagnosis of major depressive disorder [30]. The authors presented the results of two identical, double-blind, multicenter, placebo-controlled studies over 10 weeks. Sertraline received 189patients (25 mg/day, maximum dose 200 mg/day), 187 placebo.
5 to 100 mg/day. In the course of treatment, clinical observation was supplemented by examination of patients on a number of scales - Hamilton (HAM-D and HAM-A), the scale of general clinical impression (CGI). It has been established that sertraline in children is highly effective and safe (does not affect cognitive functions, does not have muscle relaxant and sedative effects). The studied drug is distinguished by the rapid onset of both thymoanaleptic and anxiolytic action. In mild depressive states, the average sufficient dose is 50 mg / day, with moderate depression and OCD in adolescents - 100 mg and the duration of therapy is more than 2 months. C. Donnely et al. evaluated the efficacy and safety of sertraline in the treatment of outpatients aged 6 to 17 years with a diagnosis of major depressive disorder [30]. The authors presented the results of two identical, double-blind, multicenter, placebo-controlled studies over 10 weeks. Sertraline received 189patients (25 mg/day, maximum dose 200 mg/day), 187 placebo. A total of 143 patients completed the study in the Zoloft group and 156 patients in the placebo group. The mean dose of sertraline in those who completed the study was 131.1 mg/day. Children treated with Zoloft, compared with those treated with placebo, showed a significant reduction in symptoms on the CDRS-R (Children's Depression Rating Scale-Revised) scale from the 3rd week of treatment (p<0.05). Sertraline was well tolerated: only 8% of patients discontinued treatment due to side effects (2.1% in the placebo group). Side effects included diarrhea, anorexia, and agitation. The authors conclude that Zoloft is effective in treating depression in children.
A total of 143 patients completed the study in the Zoloft group and 156 patients in the placebo group. The mean dose of sertraline in those who completed the study was 131.1 mg/day. Children treated with Zoloft, compared with those treated with placebo, showed a significant reduction in symptoms on the CDRS-R (Children's Depression Rating Scale-Revised) scale from the 3rd week of treatment (p<0.05). Sertraline was well tolerated: only 8% of patients discontinued treatment due to side effects (2.1% in the placebo group). Side effects included diarrhea, anorexia, and agitation. The authors conclude that Zoloft is effective in treating depression in children.
In a prospective open study by B.McConville et al. studied the efficacy of sertraline in 13 adolescents (12–18 years of age) who were treated for a major depressive episode [31]. Patients were observed in a hospital for 9–38 days with follow-up at home for up to 12 weeks. The dose of sertraline ranged from 25 to 200 mg/day, depending on the clinical response of the patient. To assess the condition, common scales were used: HAM-D, MADRS, CGI-D, etc. Zoloft treatment statistically significantly reduced HAM-D (p=0.027) and MADRS (p=0.022) readings. On other scales, a minimally significant improvement was noted. During the 12-week follow-up, the following side effects were identified: insomnia (69%), lethargy (61%), changes in body weight (46%), nightmares (39%), tension (31%), loss of appetite (31%), headache (31%). During the same period, the severity of side effects decreased significantly in parallel with the disappearance of depressive symptoms. According to the authors, sertraline can be successfully used in child psychiatry for the treatment of "major depression", but it should be borne in mind that side effects are possible.
To assess the condition, common scales were used: HAM-D, MADRS, CGI-D, etc. Zoloft treatment statistically significantly reduced HAM-D (p=0.027) and MADRS (p=0.022) readings. On other scales, a minimally significant improvement was noted. During the 12-week follow-up, the following side effects were identified: insomnia (69%), lethargy (61%), changes in body weight (46%), nightmares (39%), tension (31%), loss of appetite (31%), headache (31%). During the same period, the severity of side effects decreased significantly in parallel with the disappearance of depressive symptoms. According to the authors, sertraline can be successfully used in child psychiatry for the treatment of "major depression", but it should be borne in mind that side effects are possible.
P. Ambrosini et al. conducted a prospective multicenter study on the use of sertraline in the treatment of major depressive disorder in adolescents (12–19years) [32]. After a 2-week evaluation period, patients received Zoloft for 10 weeks. Responders continued treatment for another 12 weeks. The starting dose was 50 mg/day, the maximum dose was reached by the end of the 3rd (100 mg), 6th (150 mg) and 9th (200 mg/day) weeks. In the event of side effects, the dose was reduced. The clinical condition was assessed regularly using standard scales (M-SADS, HAM-DLI, GGI, etc.). 41 patients completed a 6-week course of treatment, and 34 patients underwent a 10-week course of Zoloft therapy. Of the 47 patients, 26 (55.3%) patients showed a reduction in symptoms according to the HAM-D scale by more than 50%. Improvement in all parameters was achieved by the 10th week (p=0.0001). All scores showed a significant reduction in depression from baseline (p=0.0001). Sertraline was well tolerated by adolescents with few side effects. The most frequently observed (less than 10% of patients) headaches, insomnia and dizziness. The authors conclude that sertraline is an effective and well-tolerated antidepressant for the treatment of adolescents suffering from major depressive disorder.
Responders continued treatment for another 12 weeks. The starting dose was 50 mg/day, the maximum dose was reached by the end of the 3rd (100 mg), 6th (150 mg) and 9th (200 mg/day) weeks. In the event of side effects, the dose was reduced. The clinical condition was assessed regularly using standard scales (M-SADS, HAM-DLI, GGI, etc.). 41 patients completed a 6-week course of treatment, and 34 patients underwent a 10-week course of Zoloft therapy. Of the 47 patients, 26 (55.3%) patients showed a reduction in symptoms according to the HAM-D scale by more than 50%. Improvement in all parameters was achieved by the 10th week (p=0.0001). All scores showed a significant reduction in depression from baseline (p=0.0001). Sertraline was well tolerated by adolescents with few side effects. The most frequently observed (less than 10% of patients) headaches, insomnia and dizziness. The authors conclude that sertraline is an effective and well-tolerated antidepressant for the treatment of adolescents suffering from major depressive disorder.
E. Tierney et al. retrospectively assessed the therapeutic and side effects of sertraline at doses of 25-200 mg/day in 33 patients aged 8 to 18 years with a diagnosis of major depressive disorder [33]. The condition of patients was assessed using CGI scales during 45 days of treatment. In 21 patients treated with Zoloft, the condition improved markedly (scores from 5.8 to 3.4 points on the CGI scale), side effects were noted in 16 patients, while 8 patients discontinued therapy due to these manifestations. Changes in behavior were observed in 7 patients (2 patients developed hypomania). The authors conclude that some children and adolescents may respond positively to Zoloft treatment, but the possibility of side effects should be considered.
M.Nixon et al. determined the efficacy, safety and tolerability of sertraline in the long-term treatment of major depressive disorders and dysthymia [34]. In the conditions of an open 6-month study, 21 outpatients aged 12 to 18 years were evaluated. 13 patients were diagnosed with major depressive disorder, 8 with dysthymia. Internal scales HAM-D, HAM-A, CGI were used. Sertraline was prescribed for 24 weeks at doses ranging from 50 to 200 mg/day. 9 patients completed the full course of therapy. Both groups of patients showed significant clinical improvement (the best scores on the HAM-D scale were 76.9% positive response to therapy in depressed patients, 100% in patients with dysthymia). Side effects were minor and manifested only in the form of headaches. The authors conclude that Zoloft can be effective in the treatment of depression and dysthymia in children and adolescents.
13 patients were diagnosed with major depressive disorder, 8 with dysthymia. Internal scales HAM-D, HAM-A, CGI were used. Sertraline was prescribed for 24 weeks at doses ranging from 50 to 200 mg/day. 9 patients completed the full course of therapy. Both groups of patients showed significant clinical improvement (the best scores on the HAM-D scale were 76.9% positive response to therapy in depressed patients, 100% in patients with dysthymia). Side effects were minor and manifested only in the form of headaches. The authors conclude that Zoloft can be effective in the treatment of depression and dysthymia in children and adolescents.
ROC
At one time, Zoloft received official FDA approval for the treatment of OCD in children aged 6 to 17 years. J.March et al. studied the effectiveness of sertraline in the treatment of OCD (in 187 children and adolescents) in a double-blind, placebo-controlled, multicenter study (sertalin dose 25–200 mg/day) [35].
After the first phase of the study, the patients were divided into two groups: the first received sertraline (n=92), the second - placebo (n=95). The full course of treatment was 52 weeks. Patients' condition was assessed using the NINIH-OCS and CGI scales. The results showed a significant reduction in symptoms in the Zoloft group (p=0.005) compared to the placebo group from the 3rd week of the study. In the sertraline group, 13% of patients completed the study earlier due to the development of side effects (insomnia, agitation, tremor). The authors confirmed that sertraline is an effective and safe treatment for OCD in children and adolescents.
The full course of treatment was 52 weeks. Patients' condition was assessed using the NINIH-OCS and CGI scales. The results showed a significant reduction in symptoms in the Zoloft group (p=0.005) compared to the placebo group from the 3rd week of the study. In the sertraline group, 13% of patients completed the study earlier due to the development of side effects (insomnia, agitation, tremor). The authors confirmed that sertraline is an effective and safe treatment for OCD in children and adolescents.
In two open studies, H. Johnston [36] and P. Zombroso et al. [37] also showed the effectiveness of sertraline in the treatment of OCD resistant to therapy with other drugs. Long-term studies undertaken by E.Cook et al. were aimed at studying the efficacy and safety of sertraline in outpatients aged 6 to 12 years (72 patients) and from 13 to 18 years (65 patients) [38]. These patients completed the study conducted by J. March et al. [35]. Evaluation of the effectiveness of treatment at week 52 of the study showed a statistically significant improvement in all measured parameters (p<0. 001). The authors concluded that Zoloft at doses of 50–200 mg/day is an effective and safe treatment for long-term treatment of OCD in patients aged 6–18 years. T.Wibus et al. studied possible adverse cardiovascular effects in the treatment of sertraline in patients suffering from OCD (same sample) [39]. A carefully conducted study led to the conclusion that Zoloft is not only effective, but also does not cause any side effects or complications from the cardiovascular system.
001). The authors concluded that Zoloft at doses of 50–200 mg/day is an effective and safe treatment for long-term treatment of OCD in patients aged 6–18 years. T.Wibus et al. studied possible adverse cardiovascular effects in the treatment of sertraline in patients suffering from OCD (same sample) [39]. A carefully conducted study led to the conclusion that Zoloft is not only effective, but also does not cause any side effects or complications from the cardiovascular system.
Summarizing the data obtained during the work on the review, it should be noted the increased interest of psychiatrists in the use of Zoloft in the treatment of severe and chronic depression. Significantly expanded domestic successful experience in the use of the drug. Most researchers emphasize the balanced action of Zoloft, the absence of cognitive impairment, drowsiness and other undesirable effects. More publications have appeared on sertraline therapy in elderly patients, and the safe combination of Zoloft with benzodiazepines has been accepted.