Sleep talking medical term
Sleep Talking | Sleep Foundation
Sleep talking, formally known as somniloquy, is a sleep disorder defined as talking during sleep without being aware of it. Sleep talking can involve complicated dialogues or monologues, complete gibberish or mumbling. The good news is that for most people it is a rare and short-lived occurrence.
It’s common for people to experience at least one episode of sleep talking during their life, making it one of the most common abnormal behaviors that can occur during sleep. Research has helped clarify the symptoms and consequences of sleep talking, but there is much that remains unknown about the causes and treatment of this condition.
What Is Sleep Talking?
Sleep talking is a type of parasomnia. Parasomnias are abnormal behaviors during sleep. Unlike most parasomnias that happen only during specific parts of the sleep cycle, sleep talking can occur during either rapid eye movement (REM) or non-REM sleep.
Sleep talking is considered to be distinct from other vocalizations that can occur during sleep such as catathrenia, a breathing disorder that causes audible groaning, or REM sleep behavior disorder (RBD), which involves a person physically acting out their dreams.
What Are the Symptoms of Sleep Talking?
The central symptom of sleep talking is audible expression that occurs during sleep without the person being aware of it happening. It can be gibberish or resemble normal speech.
A linguistic study of somniloquy found that around half of recorded sleep talking was incomprehensible. In these cases, sleep talking was normally mumbling, silent speech (moving the lips with limited noise), or was muffled by pillows or blankets.
The other half of sleep talking that was comprehensible had a number of parallels to typical conversations. For example, it usually followed typical standards of grammar and included pauses as if talking with another person.
Many of the recorded utterances were negative, exclamatory, or profane, indicating that sleep talking may reflect conflict-driven dialogue taking place in the brain during sleep. Sleep talking that is offensive, sexually explicit, or reveals secrets may cause embarrassment or shame; however, people are very rarely aware that they are talking in their sleep at the time and typically have no recollection of the episodes when they wake up.
Episodes of sleep talking tend to be short, and they rarely involve long or drawn-out conversations. The total episode may involve only a handful of words or a few sentences.
Research is mixed about the source of the content during episodes of sleep talking. Speech may not have any clear connection to a person’s life, recent events, or prior conversations. Some evidence indicates that it may at times be related to dreams, but not all sleep talking appears to be closely tied to dream activity.
How Common Is Sleep Talking?
Studies have found that up to 66% of people have experienced episodes of sleep talking, making it one of the most common parasomnias. That said, it does not occur frequently, with just 17% of people reporting sleep talking episodes in the last three months. Even regular sleep talkers may have to be recorded for four nights or more to document an episode.
Sleep talking is found more often in children and is believed to affect fewer adults. It occurs equally in women and men.
It occurs equally in women and men.
Because an individual is very rarely aware of episodes, data about the prevalence of sleep talking may not be exact. Reports of sleep talking usually come from a family member or bed partner.
Is Sleep Talking Dangerous?
In the majority of cases, sleep talking is harmless. It doesn’t usually have a major effect on the person’s sleep, and it normally doesn’t occur frequently enough to cause any serious problems.
However, there are some situations in which sleep talking can cause problems:
- If sleep talking bothers a bed partner or roommate, it may interrupt their sleep and contribute to problems like insomnia or excessive daytime sleepiness.
- If the content of sleep talking is embarrassing, it may create awkwardness or stress between the person talking in their sleep and their bed partner.
- If sleep talking occurs alongside other parasomnias, such as nightmare disorder or sleepwalking, it may be connected to bigger sleeping difficulties that can cause fragmented or insufficient sleep.
What Causes Sleep Talking?
Experts aren’t sure exactly why people talk in their sleep. There is evidence that it may have a genetic component with some studies finding that sleep talking can run in families.
In studies of twins, sleep talking was found to co-occur more frequently with sleepwalking, teeth grinding, and nightmares in both children and adults, and these all may share some genetic relationship. Further research is needed to better understand these potential connections.
Sleep talking appears to occur more often in people with mental health conditions. In particular, it is believed to occur most frequently in people with post-traumatic stress disorder (PTSD). Overall, though, most cases of sleep talking are not thought to be connected to mental illness.
How Can You Stop Sleep Talking?
Because the cause of sleep talking is not fully understood, there is limited knowledge about proven methods to stop sleep talking. In most situations, treatment for sleep talking is unnecessary because of its limited frequency and minimal negative consequences.
In most situations, treatment for sleep talking is unnecessary because of its limited frequency and minimal negative consequences.
For people who want to try to limit or eliminate sleep talking episodes, focusing on sleep hygiene may be a helpful starting point. Most parasomnias are thought to be an abnormal state that blends wakefulness and sleep, and this state may be more likely to arise when normal sleep patterns are disturbed. For that reason, steps that promote consistent and stable sleep may help ward off parasomnias, including sleep talking.
Sleep hygiene includes a person’s sleep environment and their habits that can affect sleep. Improving sleep hygiene can eliminate potential causes of sleep interruptions and create routines that are conducive to higher-quality sleep.
While healthy sleep tips can be adapted to fit an individual’s situation, some of the key ways to enhance sleep hygiene include:
- Keeping a consistent sleep schedule every day, including on weekends.

- Avoiding caffeine or other stimulants late in the afternoon and evening.
- Giving yourself time to wind down and relax, including by dimming lights and putting away electronic devices for at least a half-hour before bedtime.
- Getting regular exposure to daylight and finding time for physical activity during the day.
- Creating a distraction-free sleep space that has limited light or sound pollution.
- Setting up a cozy sleep surface with the best mattresses, best pillows, and best bedding for your needs
People who are bothered by ongoing sleep talking, suffer from other sleeping problems, and/or have excessive drowsiness during the day should talk with their doctor who can help get to the bottom of those issues and recommend the most appropriate treatment.
How Can Bed Partners of Sleep Talkers Get Better Sleep?
It’s often bed partners or roommates of people who talk in their sleep who bear the brunt of the negative consequences of somniloquy. They may find themselves awoken unexpectedly in the night by sleep talking or be bothered or offended by its content.
They may find themselves awoken unexpectedly in the night by sleep talking or be bothered or offended by its content.
If sleep talking is creating these problems on a regular basis, a focus on sleep hygiene may help their bed partner decrease the frequency of sleep talking episodes. In addition, other steps may help cut down on the disturbance from a bed partner’s sleep talking:
- Wearing ear plugs or headphones to block out the sleep talking.
- Using a white noise machine or a fan to create a soothing and stable background noise that drowns out most sleep talking.
- If necessary, sleeping in different rooms can keep the noise of sleep talking from causing nighttime interruptions.
If there are any other sleep disturbances or excessive daytime sleepiness along with sleep talking, sleep apnea should be considered. Consultation with a sleep doctor can help you to evaluate this.
- Was this article helpful?
- YesNo
Sleep Talking Causes and Treatments
Written by Kelli Miller
Have you been told that you whisper sweet nothings in your sleep -- unaware that you ever spoke a word? Or, maybe your child shouts out streams of babble late at night -- only to fall right back to sleep. Have you been hoping your sleep-talking spouse will spill a long-time secret? Go ahead. Pose a question while they are sleeping, and don't be surprised if you get a single-syllable answer! But be warned: A sleep talker usually doesn't remember anything that's said during sleep.
Have you been hoping your sleep-talking spouse will spill a long-time secret? Go ahead. Pose a question while they are sleeping, and don't be surprised if you get a single-syllable answer! But be warned: A sleep talker usually doesn't remember anything that's said during sleep.
Talking in your sleep can be a funny thing. Perhaps you chitchat unconsciously with unseen associates at the midnight hour. Or maybe a family member unknowingly carries on nightly conversations. Here are answers to your questions about talking in your sleep -- what you need to know about sleep talking, from causes to treatments.
What is sleep talking?
Sleep talking, or somniloquy, is the act of speaking during sleep. It's a type of parasomnia -- an abnormal behavior that takes place during sleep. It's a very common occurrence and is not usually considered a medical problem.
The nighttime chatter may be harmless, or it could be graphic, even R rated. Sometimes, listeners find the content offensive or vulgar. Sleep talkers normally speak for no more than 30 seconds per episode, but some people sleep talk many times during a night.
Sleep talkers normally speak for no more than 30 seconds per episode, but some people sleep talk many times during a night.
The late-night diatribes may be exceptionally eloquent, or the words may be mumbled and hard to decipher. Sleep talking may involve simple sounds or long, involved speeches. Sleep talkers usually seem to be talking to themselves. But sometimes, they appear to carry on conversations with others. They may whisper, or they might shout. If you share a bedroom with someone who talks in their sleep, you might not be getting enough shut-eye.
Who talks in their sleep?
Many people talk in their sleep. Half of all kids between the ages of 3 and 10 years old carry on conversations while asleep, and a small number of adults -- about 5% -- keep chit-chatting after they go to bed. The utterances can take place occasionally or every night. A 2004 poll showed that more than 1 in 10 young children converse in their sleep more than a few nights a week.
Girls talk in their sleep as much as boys. And experts think that sleep talking may run in families.
And experts think that sleep talking may run in families.
What are the symptoms of talking in your sleep?
It's hard to tell if you've been talking in your own sleep. Usually, people will tell you they've heard you shout out during the night or while you were napping. Or maybe someone might complain that your sleep talking is keeping them up all night.
What causes sleep talking?
You might think that sleep talking occurs during dreaming. But scientists still are not sure if such chatter is linked to nighttime reveries. The talking can occur in any stage of sleep.
Sleep talking usually occurs by itself and is most often harmless. However, in some cases, it might be a sign of a more serious sleep disorder or health condition.
REM sleep behavior disorder (RBD) and sleep terrors are two types of sleep disorders that cause some people to shout during sleep. Sleep terrors, also called night terrors, usually involve frightening screams, thrashing, and kicking. It's hard to wake someone having a sleep terror. Children with sleep terrors usually sleep talk and sleepwalk.
It's hard to wake someone having a sleep terror. Children with sleep terrors usually sleep talk and sleepwalk.
People with RBD yell, shout, grunt, and act out their dreams, often violently.
Sleep talking can also occur with sleepwalking and nocturnal sleep-related eating disorder(NS-RED), a condition in which a person eats while asleep.
Other things that can cause sleep talking include:
- Certain medications
- Emotional stress
- Fever
- Mental health disorder
- Substance abuse
How is talking in your sleep treated?
It is a good idea to see a sleep specialist if your sleep talking occurs suddenly as an adult or if it involves intense fear, screaming, or violent actions. You might also consider seeing a doctor if unconscious chatter is interfering with your sleep -- or that of your roommates.
If you think your child has sleep problems, make an appointment with your pediatrician.
A sleep specialist will ask you how long you've been talking in your sleep. You'll have to ask your bed partner, roommate -- even your parents -- this question. Keep in mind, you may have started sleep talking in childhood.
You'll have to ask your bed partner, roommate -- even your parents -- this question. Keep in mind, you may have started sleep talking in childhood.
There are no tests needed to diagnose sleep talking. However, your doctor may order tests, such as a sleep study or sleep recording (polysomnogram), if you have signs of another sleep disorder.
Sleep talking rarely requires treatment. However, severe sleep talking may be the result of another more serious sleep disorder or medical condition, which can be treated. Talk to your doctor about your treatment options.
How can someone reduce their amount of sleep talking?
There is no known way to reduce sleep talking. Avoiding stress and getting plenty of sleep might make you less likely to talk in your sleep.
Keeping a sleep diary can help identify your sleep patterns and may help your doctor find out if an underlying problem is causing your sleep talking. Keep a sleep diary for two weeks. Note the times you go to bed, when you think you fell asleep, and when you woke up.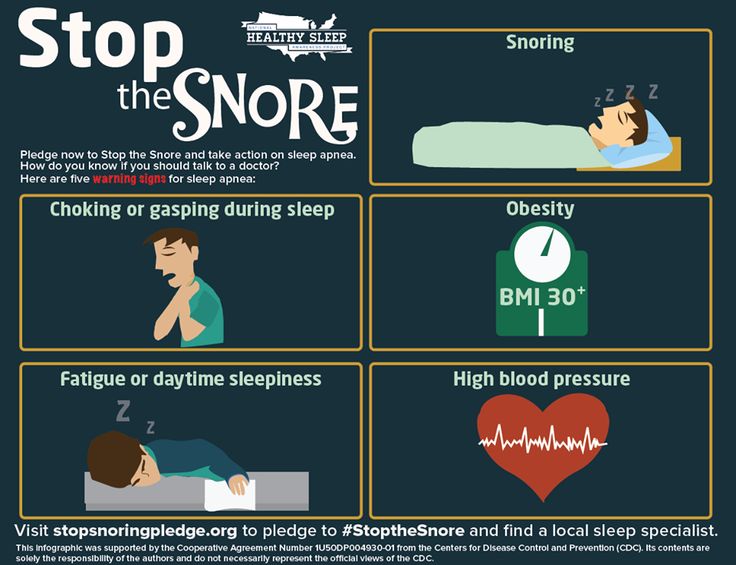 You'll also want to write down the following:
You'll also want to write down the following:
- the medicines you take, and the time of day you take them
- what you drink each day and when, especially caffeinated drinks such as cola, tea, and coffee, as well as alcohol
- when you exercise
Sitemap
|
|
Treatment and diagnosis of obstructive sleep apnea syndrome in St.
 Petersburg Hospital RAS
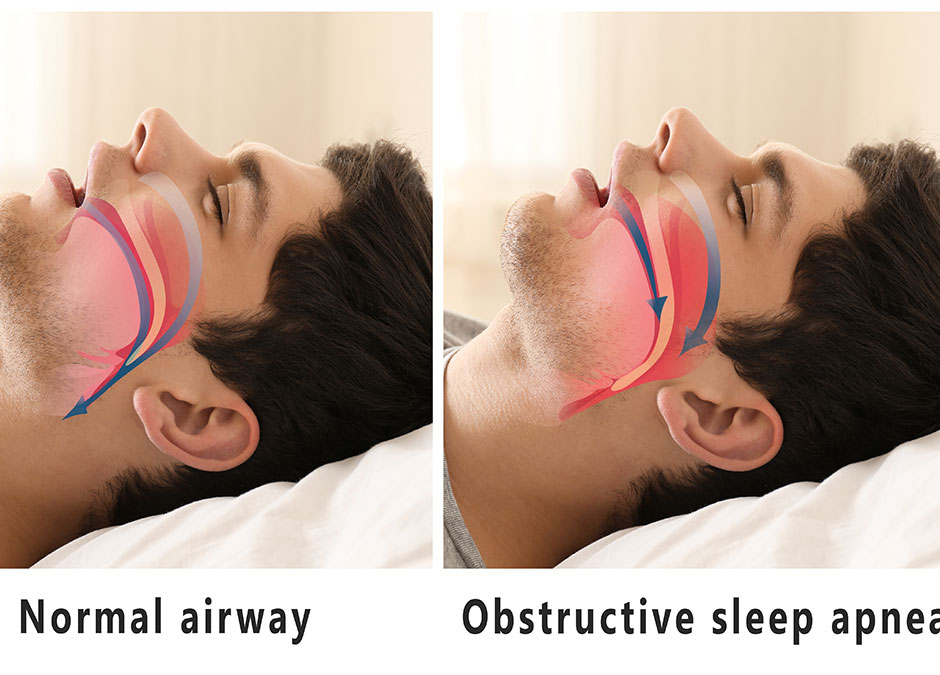
Petersburg Hospital RAS Obstructive sleep apnea syndrome (OSAS, “sleep apnea disease”) is a condition in which snoring suddenly stops during sleep and there is a frightening cessation of breathing, after which the sleeping person snores loudly, sometimes tossing and turning and then starts breathing again. Depending on the severity of the syndrome, from several to 400-500 stops of breathing can be observed during sleep, primarily during the night. Breathing disorders in a sleeping person lead to a serious deterioration in the quality of sleep and create conditions for the development and progression of many serious complications and diseases.
Causes of OSAS
- Weakness of the tone of the muscles of the pharynx, as a result of which, during sleep, the airways collapse with a violation of their air permeability.
- Developmental abnormalities resulting in narrow airways (eg, small mandible, large tongue).
- Anatomical defects at the level of the nose and pharynx (polyps, deviated nasal septum, enlarged tonsils, adenoids (pathological growth of the nasopharyngeal tonsil), tumor formations).
- Obesity.
- Endocrine diseases: for example, hypothyroidism (causes swelling of the pharyngeal structures), acromegaly - all this prevents the normal passage of air through the respiratory tract.
- Neurological diseases leading to a decrease in muscle tone (stroke - an acute violation of cerebral circulation with the death of a section of brain tissue; myopathy, myodystrophy).
- Violation of the tone of the muscles of the pharynx due to the influence of alcohol, certain drugs (hypnotics, tranquilizers).
- Chronic obstructive pulmonary disease - characterized by narrowing of the airways and impaired airflow (bronchial asthma, chronic obstructive pulmonary disease (COPD)).
- Smoking.
- Allergy.
Symptoms of OSA:
- Restless sleep, during sleep there is excessive motor activity (often roll over from side to side).
- Lack of vigor after sleep, there is a feeling of morning fatigue and weakness after waking up.
- Sleepiness during the day, tendency to fall asleep during work breaks, while driving.
- Morning headaches.
- Increased arterial (blood) pressure (mainly at night and in the morning).
- Frequent nighttime urination (>2 times per night).
- Reduced potency.
- Depression, irritability, decreased concentration and memory.
- Palpitations (tachycardia), heart rhythm disorders - arrhythmias
COAS classification
Based on Apnea Index (AI) value.
Apnea - complete cessation of breathing for at least 10 seconds.
Apnea index (AI) - the frequency of apnea attacks per 1 hour of sleep.
Severity:
- Mild course: AI - 5-14.
- Moderate course: AI - 15-29.
- Severe course: AI - 29 or more. In severe forms, up to 300-500 stops of breathing can be observed during sleep, lasting up to 3-4 hours in total.

OSA diagnostics
- ECG Holter monitoring (assesses the work of the heart) with simultaneous registration of pneumogram (recording of respiratory movements), blood oxygen saturation, air flow.
- Cardiorespiratory monitoring is a test that evaluates snoring, respiration, blood oxygen saturation, respiratory movements of the chest and abdominal wall. The device is portable, which makes it possible to conduct research at home.
- Pulse Oximetry - Measures the oxygen saturation curve during sleep.
- Polysomnography is a method of long-term recording of various functions of the human body during a night's sleep: snoring, breathing, blood oxygen saturation, respiratory movements of the chest and abdominal wall, patient's body position, electroencephalogram (registration of brain activity), electrooculogram (registration of eye movements) , electromyogram (registers the tone of the chin muscles, movements of the lower extremities), continuous video recording throughout the patient's sleep.
 The study allows you to make an accurate diagnosis, evaluate changes in the cardiovascular and nervous systems and determine the optimal treatment tactics. It is carried out only in specialized departments.
The study allows you to make an accurate diagnosis, evaluate changes in the cardiovascular and nervous systems and determine the optimal treatment tactics. It is carried out only in specialized departments.
Complications and consequences of OSA
- Increased arterial (blood) pressure.
- Arrhythmias.
- Myocardial infarction.
- Stroke (acute cerebrovascular accident).
- Progressive obesity.
- Worsening of the course of type 2 diabetes mellitus.
- Reduced potency.
- Increased risk of accidents and accidents at work. In some countries, OSAS is included in the list of diseases for which the issuance of a driver's license is prohibited !!!.
- Sudden death during sleep.
Treatment of obstructive sleep apnea
- Weight loss - following a low-calorie, vitamin-rich diet with a significant reduction in fat and carbohydrates.

- Do not eat 3-4 hours before bedtime.
- Smoking and alcohol cessation 2 hours before bedtime.
- Ensuring normal air humidity and hypoallergenic environment in the bedroom (do not use feather and down pillows and blankets, woolen carpets, etc.).
- Ensuring the optimal position of the head and body during sleep. Respiratory disorders are most pronounced when a person is lying on his back, since there is a maximum convergence of the structures of the respiratory tract. You need to sleep on your side.
- Soft palate surgery (laser or radiofrequency) is only effective in patients with a wide pharyngeal lumen and initially elongated uvula.
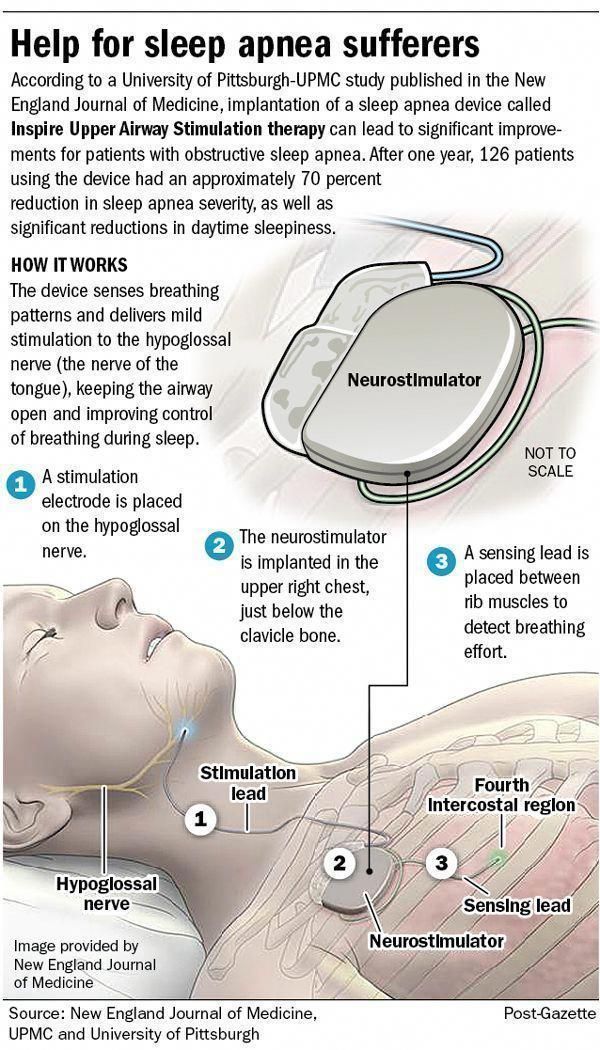
- The main method of treatment at the moment is assisted ventilation of the lungs with constant positive pressure during night sleep (CPAP therapy, CPAP therapy). For this, a special apparatus is used, which feeds air with positive pressure into a mask tightly worn on the patient's face.