Which is an effect of short term exposure to stress
How it Affects the Body
Written by WebMD Editorial Contributors
In this Article
- Fight-or-flight
- Stress in the Brain
- Stress on the Body
Feeling stressed? You’re not the only one. According to a recent study, about 25% of Americans say they’re dealing with high levels of stress and another 50% say their stress is moderate.
These numbers may not surprise you since we all deal with work, family, and relationship stressors. But, what you may not know is that stress isn’t always a bad thing. In some cases, like when you’re starting a new job or planning a big event like a wedding, stress can help you focus, motivate you to do well, and even improve your performance.
But some of the reasons stress can be positive in these situations is that it’s short-term and it’s helping you get through a challenge you know you can handle.
Experiencing stress over the long-term, however, can take a real physical and mental toll on your health. Research has shown a connection between stress and chronic problems like high blood pressure, obesity, depression, and more.
Fight-or-flight
Stress can serve an important purpose and can even help you survive. For our ancestors, stress was a helpful motivator for survival, allowing them to avoid real physical threats. That’s because it makes your body think it’s in danger, and triggers that “fight-or-flight” survival mode.
Fight-or-flight mode refers to all the chemical changes that go on in your body to get it ready for physical action. In some cases, these changes can also make you freeze.
While this stress response can still help us survive dangerous situations, it’s not always an accurate response and it’s usually caused by something that’s not actually life-threatening. That’s because our brains can’t differentiate between something that’s a real threat and something that’s a perceived threat.
Stress in the Brain
When you encounter a stressor -- whether it’s an angry bear or an unreasonable deadline -- a chain of events kicks off in your brain. First, the amygdala, an area of your brain that processes emotion, gets information about the stressor through your senses. If it interprets that information as something threatening or dangerous, it sends a signal to your brain’s command center, known as the hypothalamus.
First, the amygdala, an area of your brain that processes emotion, gets information about the stressor through your senses. If it interprets that information as something threatening or dangerous, it sends a signal to your brain’s command center, known as the hypothalamus.
The hypothalamus connects to the rest of your body through the autonomic nervous system. This controls automatic functions like your heartbeat and breathing through two different systems: the sympathetic and the parasympathetic.
The sympathetic nervous system triggers the fight-or-flight response, giving you the energy you need to respond to a threat. The parasympathetic does the opposite; it allows your body to go into “rest and digest” mode so that you can feel calm when things are safe.
When your hypothalamus gets a signal from your amygdala that you’re in danger, it sends signals to the adrenal glands and activates your sympathetic nervous system. The adrenals pump out adrenaline, causing your heart to beat faster, forcing more blood into your muscles and organs.
Your breathing might also quicken, and your senses might get sharper. Your body will also release sugar into your bloodstream, sending energy to all different parts.
Next, the hypothalamus activates a network called the HPA axis, which is made up of the hypothalamus, pituitary, and adrenals. This can cause these areas to release more stress hormones, including cortisol, which forces your body to stay wired and alert.
Stress on the Body
All of these chemical changes have short- and long-term effects on almost every system in your body:
- Musculoskeletal system
- Short term: Your muscles tense up suddenly and then release when the stressor is gone.
- Long term: If your muscles are always tense, you can develop problems like tension headaches and migraines, as well as other chronic pains.
- Respiratory system
- Short term: You breathe harder and faster, and can even hyperventilate, which can cause panic attacks in some people.
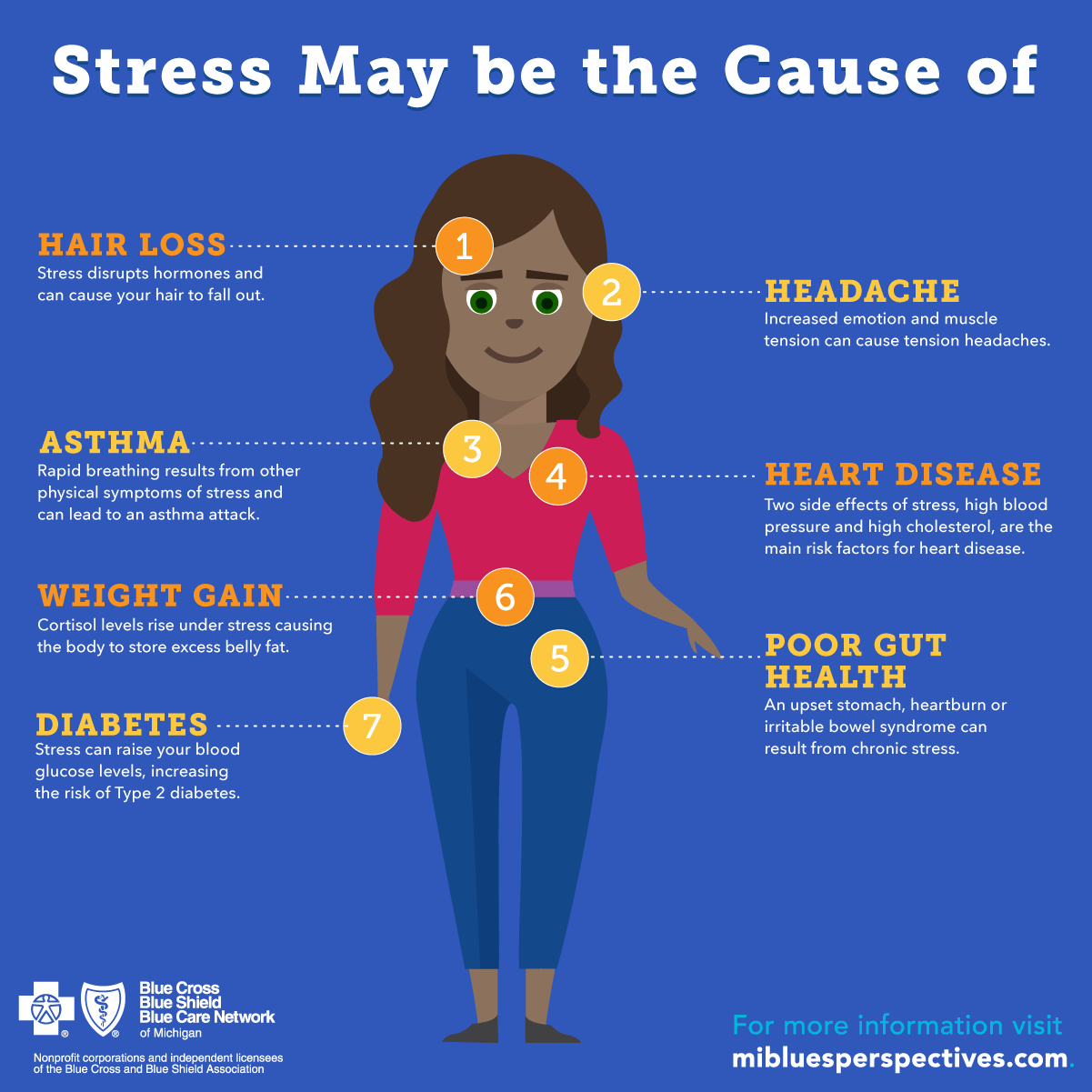
- Long term: If you have asthma or emphysema, breathing hard can make it difficult to get enough oxygen.
- Short term: You breathe harder and faster, and can even hyperventilate, which can cause panic attacks in some people.
- Cardiovascular system
- Short term: Your heart beats harder and faster and your blood vessels dilate, pushing more blood into your large muscles and raising your blood pressure.
- Long term: Consistently elevated heart rate, blood pressure, and stress hormones can increase your odds of heart attack, stroke, and hypertension. These can also affect cholesterol levels and cause inflammation in your circulatory system.
- Endocrine system
- Short term: Stress hormones like adrenaline and cortisol give your body energy to either fight or run away from a stressor. Your liver also produces more blood sugar to give your body energy.
- Long term: Some people don’t reabsorb the extra blood sugar that their liver pumps out, and they may be more likely to develop type 2 diabetes.
 Overexposure to cortisol can lead to thyroid problems and affect your ability to think clearly. It can also cause excess abdominal fat.
Overexposure to cortisol can lead to thyroid problems and affect your ability to think clearly. It can also cause excess abdominal fat.
In men, chronic stress can also affect sperm and testosterone production, and cause erectile dysfunction and infections in the testes, prostate, or urethra. In women, chronic stress can worsen PMS, cause changes in the menstrual cycle, and missed periods. It can also aggravate symptoms of menopause and decrease sexual desire.
- Gastrointestinal system
- Short term: You may feel butterflies in your stomach, pain, or nausea, or might even vomit. Your appetite can change and you can have diarrhea, constipation, or heartburn.
- Long term: Stress can lead to severe chronic pain and changes in your eating habits. You can also develop acid reflux.
Toxic Stress
Key Concepts
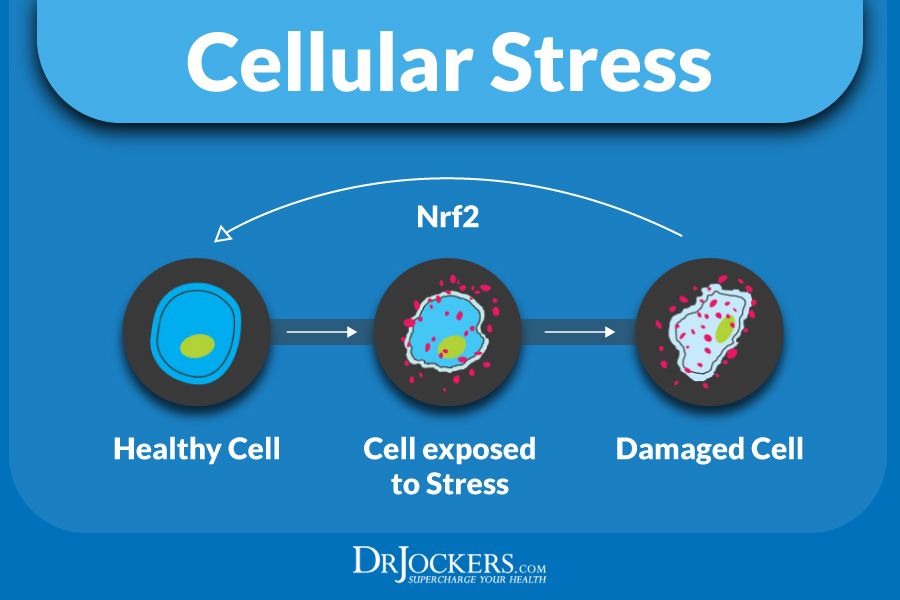
The future of any society depends on its ability to foster the healthy development of the next generation.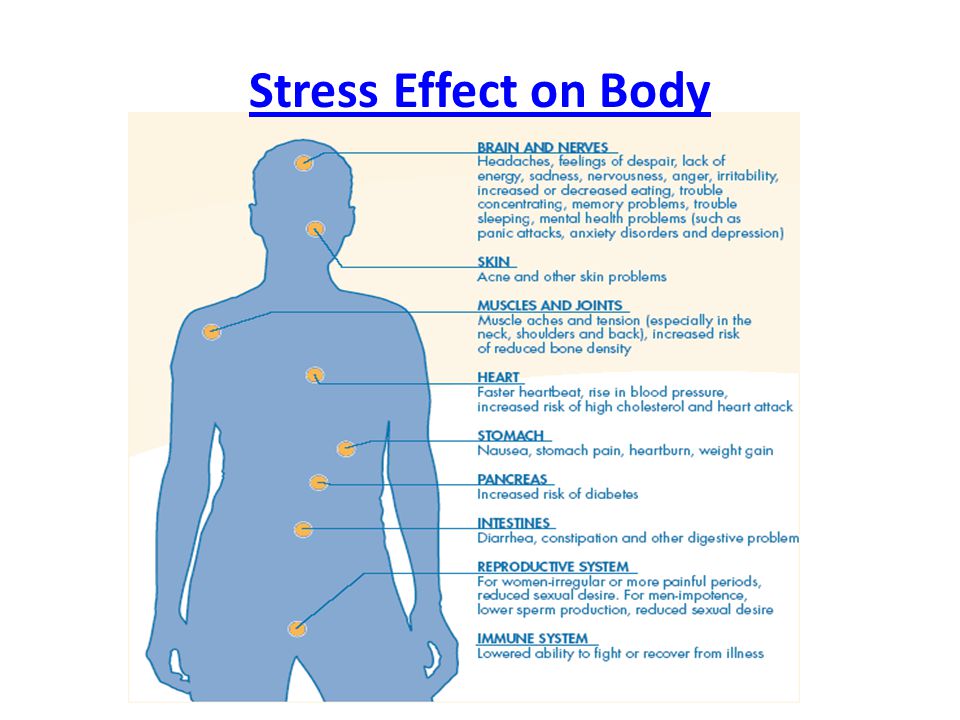 Extensive research on the biology of stress now shows that healthy development can be derailed by excessive or prolonged activation of stress response systems in the body and brain. Such toxic stress can have damaging effects on learning, behavior, and health across the lifespan.
Extensive research on the biology of stress now shows that healthy development can be derailed by excessive or prolonged activation of stress response systems in the body and brain. Such toxic stress can have damaging effects on learning, behavior, and health across the lifespan.
Learning how to cope with adversity is an important part of healthy child development. When we are threatened, our bodies prepare us to respond by increasing our heart rate, blood pressure, and stress hormones, such as cortisol. When a young child’s stress response systems are activated within an environment of supportive relationships with adults, these physiological effects are buffered and brought back down to baseline. The result is the development of healthy stress response systems. However, if the stress response is extreme and long-lasting, and buffering relationships are unavailable to the child, the result can be damaged, weakened systems and brain architecture, with lifelong repercussions.
It’s important to distinguish among three kinds of responses to stress: positive, tolerable, and toxic. As described below, these three terms refer to the stress response systems’ effects on the body, not to the stressful event or experience itself:
- Positive stress response is a normal and essential part of healthy development, characterized by brief increases in heart rate and mild elevations in hormone levels. Some situations that might trigger a positive stress response are the first day with a new caregiver or receiving an injected immunization.
- Tolerable stress response activates the body’s alert systems to a greater degree as a result of more severe, longer-lasting difficulties, such as the loss of a loved one, a natural disaster, or a frightening injury. If the activation is time-limited and buffered by relationships with adults who help the child adapt, the brain and other organs recover from what might otherwise be damaging effects.
- Toxic stress response can occur when a child experiences strong, frequent, and/or prolonged adversity—such as physical or emotional abuse, chronic neglect, caregiver substance abuse or mental illness, exposure to violence, and/or the accumulated burdens of family economic hardship—without adequate adult support. This kind of prolonged activation of the stress response systems can disrupt the development of brain architecture and other organ systems, and increase the risk for stress-related disease and cognitive impairment, well into the adult years.
When toxic stress response occurs continually, or is triggered by multiple sources, it can have a cumulative toll on an individual’s physical and mental health—for a lifetime. The more adverse experiences in childhood, the greater the likelihood of developmental delays and later health problems, including heart disease, diabetes, substance abuse, and depression. Research also indicates that supportive, responsive relationships with caring adults as early in life as possible can prevent or reverse the damaging effects of toxic stress response.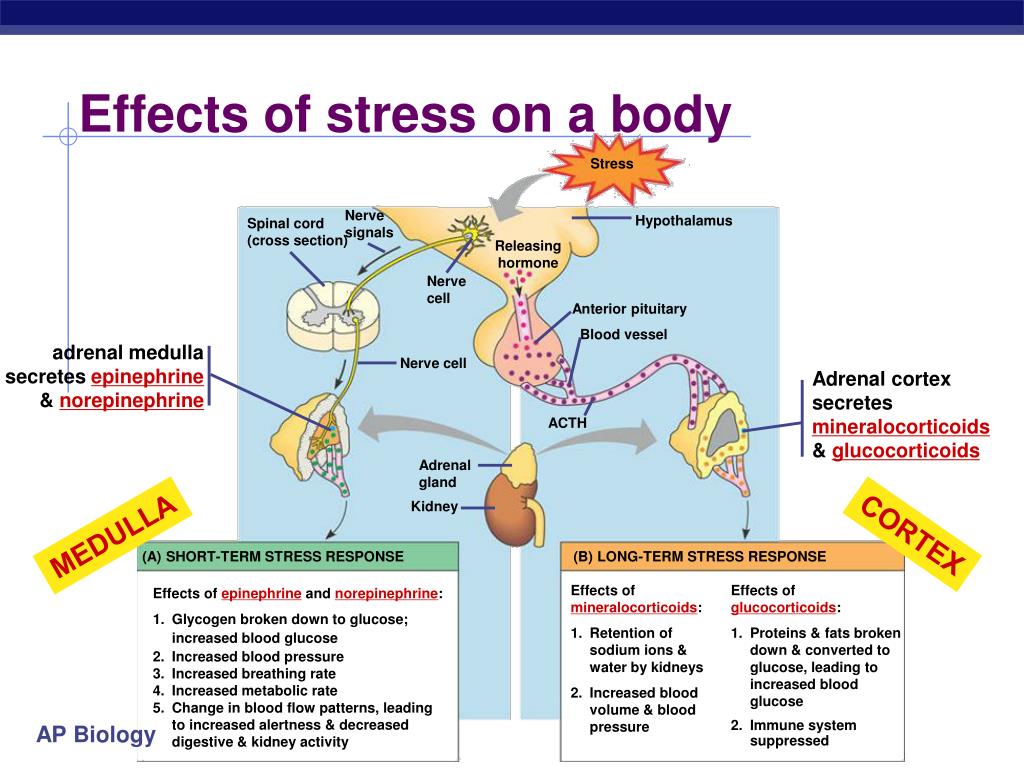
- The JPB Research Network on Toxic Stress, a project of the Center on the Developing Child, is committed to reducing the prevalence of lifelong health impairments caused by toxic stress in early childhood. Its work addresses the need to develop rigorous, versatile methods for identifying young children and adults who experience toxic stress.
- “Tackling Toxic Stress,” a multi-part series of journalistic articles, examines how policymakers, researchers, and practitioners in the field are re-thinking services for children and families based on the science of early childhood development and an understanding of the consequences of adverse early experiences and toxic stress.
Questions & Answers
-
No. The prolonged activation of the body’s stress response systems can be damaging, but some stress is a normal part of life. Learning how to cope with stress is an important part of development.
 We do not need to worry about positive stress, which is short-lived, or tolerable stress, which is more serious but is buffered by supportive relationships. However, the constant activation of the body’s stress response systems due to chronic or traumatic experiences in the absence of caring, stable relationships with adults, especially during sensitive periods of early development, can be toxic to brain architecture and other developing organ systems.
We do not need to worry about positive stress, which is short-lived, or tolerable stress, which is more serious but is buffered by supportive relationships. However, the constant activation of the body’s stress response systems due to chronic or traumatic experiences in the absence of caring, stable relationships with adults, especially during sensitive periods of early development, can be toxic to brain architecture and other developing organ systems. -
The terms positive, tolerable, and toxic stress refer to the stress response systems’ effects on the body, not to the stressful event itself. Because of the complexity of stress response systems, the three levels are not clinically quantifiable—they are simply a way of categorizing the relative severity of responses to stressful conditions. The extent to which stressful events have lasting adverse effects is determined in part by the individual’s biological response (mediated by both genetic predispositions and the availability of supportive relationships that help moderate the stress response), and in part by the duration, intensity, timing, and context of the stressful experience.
-
The most effective prevention is to reduce exposure of young children to extremely stressful conditions, such as recurrent abuse, chronic neglect, caregiver mental illness or substance abuse, and/or violence or repeated conflict. Programs or services can remediate the conditions or provide stable, buffering relationships with adult caregivers. Research shows that, even under stressful conditions, supportive, responsive relationships with caring adults as early in life as possible can prevent or reverse the damaging effects of toxic stress response.
-
If at least one parent or caregiver is consistently engaged in a caring, supportive relationship with a young child, most stress responses will be positive or tolerable. For example, there is no evidence that, in a secure and stable home, allowing an infant to cry for 20 to 30 minutes while learning to sleep through the night will elicit a toxic stress response.
 However, there is ample evidence that chaotic or unstable circumstances, such as placing children in a succession of foster homes or displacement due to economic instability or a natural disaster, can result in a sustained, extreme activation of the stress response system. Stable, loving relationships can buffer against harmful effects by restoring stress response systems to “steady state.” When the stressors are severe and long-lasting and adult relationships are unresponsive or inconsistent, it’s important for families, friends, and communities to intervene with support, services, and programs that address the source of the stress and the lack of stabilizing relationships in order to protect the child from their damaging effects.
However, there is ample evidence that chaotic or unstable circumstances, such as placing children in a succession of foster homes or displacement due to economic instability or a natural disaster, can result in a sustained, extreme activation of the stress response system. Stable, loving relationships can buffer against harmful effects by restoring stress response systems to “steady state.” When the stressors are severe and long-lasting and adult relationships are unresponsive or inconsistent, it’s important for families, friends, and communities to intervene with support, services, and programs that address the source of the stress and the lack of stabilizing relationships in order to protect the child from their damaging effects.
View Related Key Concepts
Explore Related Resources
Psychology of stress: theory and practice
%PDF-1.5 % 10 obj > /Metadata 4 0 R >> endobj 5 0 obj /Author /Title >> endobj 20 obj > endobj 3 0 obj > endobj 40 obj > stream
 L.1.5Microsoft® Word 20102018-11-16T12:28:31+05:002018-11-16T12:28:31+05:00 endstream endobj 6 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] /XObject> >> /MediaBox[0 0 595.
L.1.5Microsoft® Word 20102018-11-16T12:28:31+05:002018-11-16T12:28:31+05:00 endstream endobj 6 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] /XObject> >> /MediaBox[0 0 595.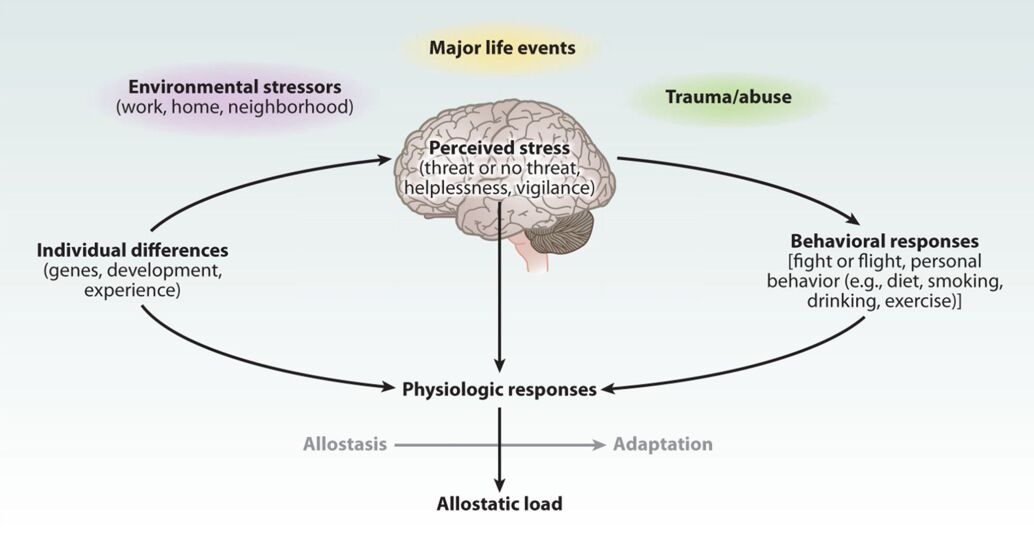 32 841.92] /Contents[129 0 R 130 0 R 131 0 R] /group> /Tabs /S /StructParents 0 /Annots [132 0R] >> endobj 70 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 134 0 R /group> /Tabs /S /StructParents 1 >> endobj 80 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 135 0 R /group> /Tabs /S /StructParents 2 >> endobj 9 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 136 0 R /group> /Tabs /S /StructParents 3 >> endobj 10 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 137 0 R /group> /Tabs /S /StructParents 4 >> endobj 11 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 138 0 R /group> /Tabs /S /StructParents 5 >> endobj 12 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 140 0R /group> /Tabs /S /StructParents 6 >> endobj 13 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents[129 0 R 130 0 R 131 0 R] /group> /Tabs /S /StructParents 0 /Annots [132 0R] >> endobj 70 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 134 0 R /group> /Tabs /S /StructParents 1 >> endobj 80 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 135 0 R /group> /Tabs /S /StructParents 2 >> endobj 9 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 136 0 R /group> /Tabs /S /StructParents 3 >> endobj 10 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 137 0 R /group> /Tabs /S /StructParents 4 >> endobj 11 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 138 0 R /group> /Tabs /S /StructParents 5 >> endobj 12 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 140 0R /group> /Tabs /S /StructParents 6 >> endobj 13 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 141 0 R /group> /Tabs /S /StructParents 7 >> endobj 14 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 142 0R /group> /Tabs /S /StructParents 8 >> endobj 15 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 143 0 R /group> /Tabs /S /StructParents 9 >> endobj 16 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 145 0R /group> /Tabs /S /StructParents 10 >> endobj 17 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 148 0 R /group> /Tabs /S /StructParents 11 >> endobj 18 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 149 0 R /group> /Tabs /S /StructParents 12 >> endobj 19 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 150 0 R /group> /Tabs /S /StructParents 13 >> endobj 20 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 141 0 R /group> /Tabs /S /StructParents 7 >> endobj 14 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 142 0R /group> /Tabs /S /StructParents 8 >> endobj 15 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 143 0 R /group> /Tabs /S /StructParents 9 >> endobj 16 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 145 0R /group> /Tabs /S /StructParents 10 >> endobj 17 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 148 0 R /group> /Tabs /S /StructParents 11 >> endobj 18 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 149 0 R /group> /Tabs /S /StructParents 12 >> endobj 19 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 150 0 R /group> /Tabs /S /StructParents 13 >> endobj 20 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.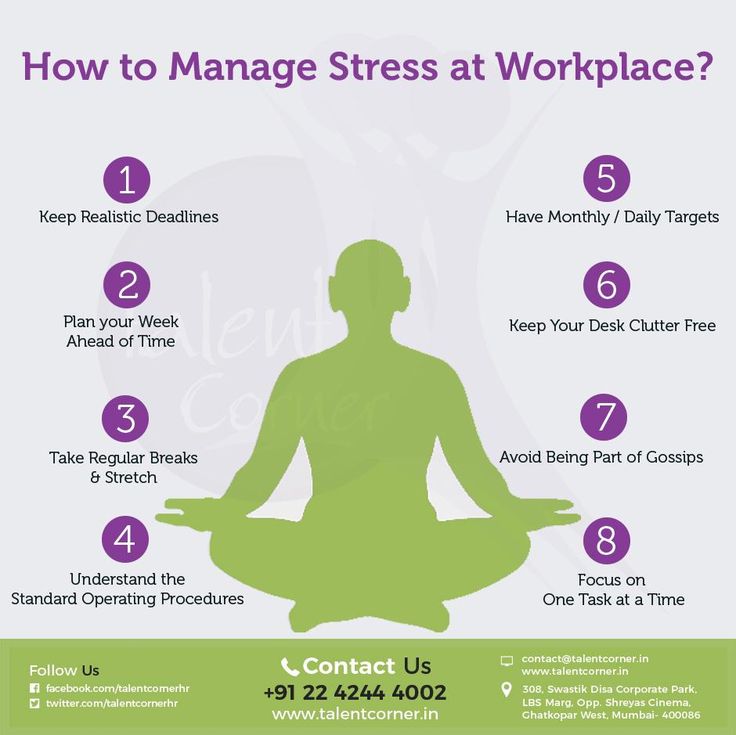 32 841.92] /Contents 151 0 R /group> /Tabs /S /StructParents 14 >> endobj 21 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 152 0R /group> /Tabs /S /StructParents 15 >> endobj 22 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 153 0R /group> /Tabs /S /StructParents 16 >> endobj 23 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 154 0 R /group> /Tabs /S /StructParents 17 >> endobj 24 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 155 0 R /group> /Tabs /S /StructParents 18 >> endobj 25 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 156 0 R /group> /Tabs /S /StructParents 19 >> endobj 26 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 157 0 R /group> /Tabs /S /StructParents 20 >> endobj 27 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 151 0 R /group> /Tabs /S /StructParents 14 >> endobj 21 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 152 0R /group> /Tabs /S /StructParents 15 >> endobj 22 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 153 0R /group> /Tabs /S /StructParents 16 >> endobj 23 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 154 0 R /group> /Tabs /S /StructParents 17 >> endobj 24 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 155 0 R /group> /Tabs /S /StructParents 18 >> endobj 25 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 156 0 R /group> /Tabs /S /StructParents 19 >> endobj 26 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 157 0 R /group> /Tabs /S /StructParents 20 >> endobj 27 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595. 32 841.92] /Contents 160 0R /group> /Tabs /S /StructParents 21 >> endobj 28 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 161 0 R /group> /Tabs /S /StructParents 22 >> endobj 29 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 162 0 R /group> /Tabs /S /StructParents 23 >> endobj 30 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 163 0 R /group> /Tabs /S /StructParents 24 >> endobj 31 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 164 0 R /group> /Tabs /S /StructParents 25 >> endobj 32 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 165 0 R /group> /Tabs /S /StructParents 26 >> endobj 33 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 166 0R /group> /Tabs /S /StructParents 27 >> endobj 34 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 160 0R /group> /Tabs /S /StructParents 21 >> endobj 28 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 161 0 R /group> /Tabs /S /StructParents 22 >> endobj 29 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 162 0 R /group> /Tabs /S /StructParents 23 >> endobj 30 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 163 0 R /group> /Tabs /S /StructParents 24 >> endobj 31 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 164 0 R /group> /Tabs /S /StructParents 25 >> endobj 32 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 165 0 R /group> /Tabs /S /StructParents 26 >> endobj 33 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 166 0R /group> /Tabs /S /StructParents 27 >> endobj 34 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.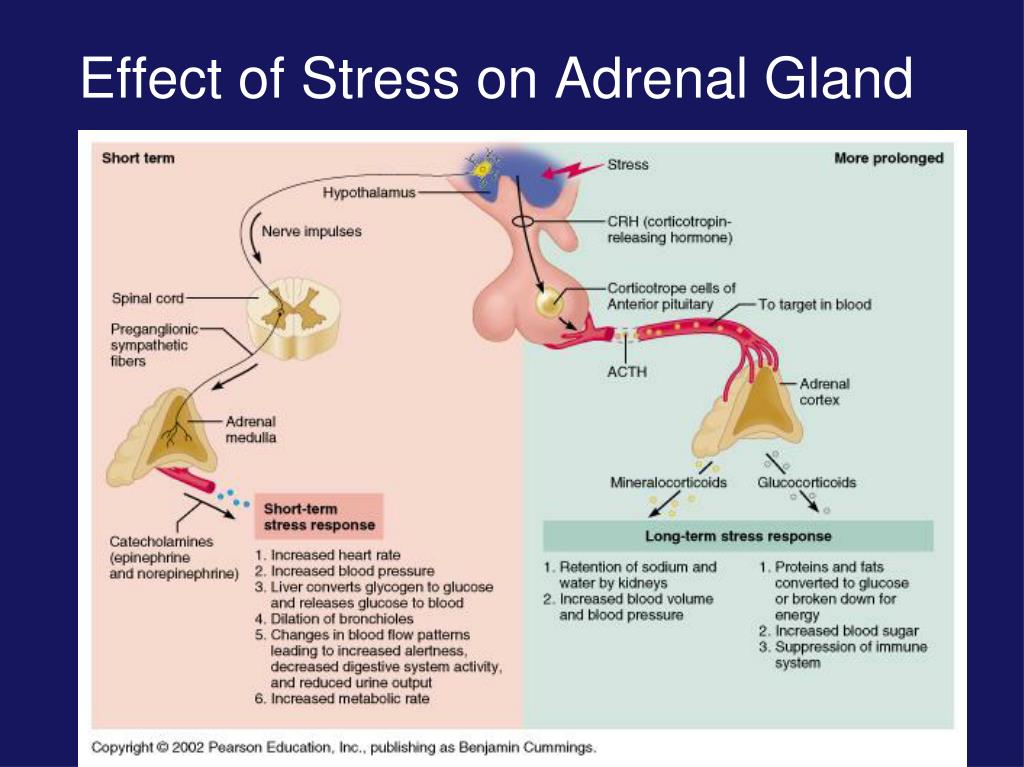 32 841.92] /Contents 167 0R /group> /Tabs /S /StructParents 28 >> endobj 35 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 168 0 R /group> /Tabs /S /StructParents 29 >> endobj 36 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 169 0 R /group> /Tabs /S /StructParents 30 >> endobj 37 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 170 0 R /group> /Tabs /S /StructParents 31 >> endobj 38 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 171 0R /group> /Tabs /S /StructParents 32 >> endobj 39 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 173 0R /group> /Tabs /S /StructParents 33 >> endobj 40 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 176 0R /group> /Tabs /S /StructParents 34 >> endobj 41 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 167 0R /group> /Tabs /S /StructParents 28 >> endobj 35 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 168 0 R /group> /Tabs /S /StructParents 29 >> endobj 36 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 169 0 R /group> /Tabs /S /StructParents 30 >> endobj 37 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 170 0 R /group> /Tabs /S /StructParents 31 >> endobj 38 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 171 0R /group> /Tabs /S /StructParents 32 >> endobj 39 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 173 0R /group> /Tabs /S /StructParents 33 >> endobj 40 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 176 0R /group> /Tabs /S /StructParents 34 >> endobj 41 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.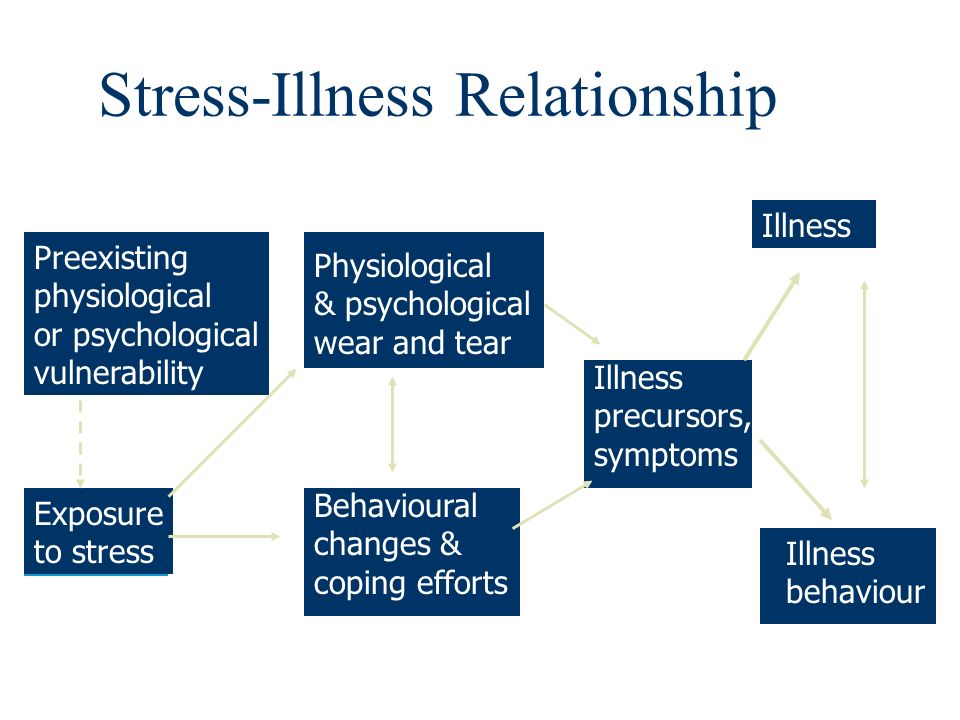 32 841.92] /Contents 177 0R /group> /Tabs /S /StructParents 35 >> endobj 42 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 178 0 R /group> /Tabs /S /StructParents 36 >> endobj 43 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 179 0 R /group> /Tabs /S /StructParents 37 >> endobj 44 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 180 0 R /group> /Tabs /S /StructParents 38 >> endobj 45 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 181 0 R /group> /Tabs /S /StructParents 39 >> endobj 46 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 182 0 R /group> /Tabs /S /StructParents 40 >> endobj 47 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 183 0 R /group> /Tabs /S /StructParents 41 >> endobj 48 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 177 0R /group> /Tabs /S /StructParents 35 >> endobj 42 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 178 0 R /group> /Tabs /S /StructParents 36 >> endobj 43 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 179 0 R /group> /Tabs /S /StructParents 37 >> endobj 44 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 180 0 R /group> /Tabs /S /StructParents 38 >> endobj 45 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 181 0 R /group> /Tabs /S /StructParents 39 >> endobj 46 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 182 0 R /group> /Tabs /S /StructParents 40 >> endobj 47 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 183 0 R /group> /Tabs /S /StructParents 41 >> endobj 48 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.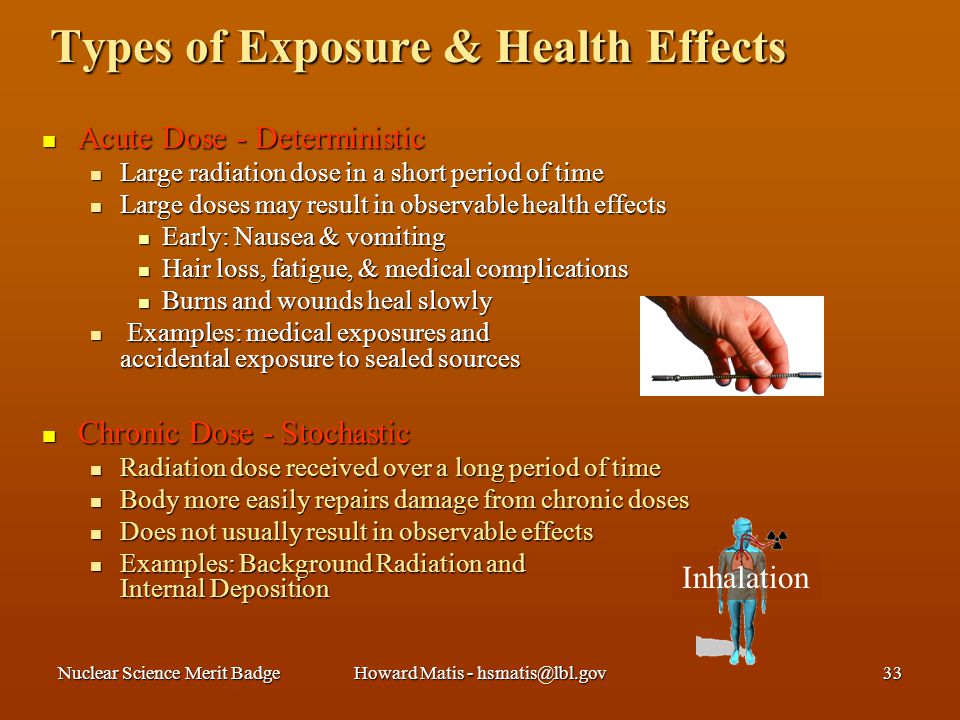 32 841.92] /Contents 184 0R /group> /Tabs /S /StructParents 42 >> endobj 49 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 185 0R /group> /Tabs /S /StructParents 43 >> endobj 50 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 186 0 R /group> /Tabs /S /StructParents 44 >> endobj 51 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 187 0 R /group> /Tabs /S /StructParents 45 >> endobj 52 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 188 0R /group> /Tabs /S /StructParents 46 >> endobj 53 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 189 0 R /group> /Tabs /S /StructParents 47 >> endobj 54 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 190 0 R /group> /Tabs /S /StructParents 48 >> endobj 55 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 184 0R /group> /Tabs /S /StructParents 42 >> endobj 49 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 185 0R /group> /Tabs /S /StructParents 43 >> endobj 50 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 186 0 R /group> /Tabs /S /StructParents 44 >> endobj 51 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 187 0 R /group> /Tabs /S /StructParents 45 >> endobj 52 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 188 0R /group> /Tabs /S /StructParents 46 >> endobj 53 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 189 0 R /group> /Tabs /S /StructParents 47 >> endobj 54 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 190 0 R /group> /Tabs /S /StructParents 48 >> endobj 55 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.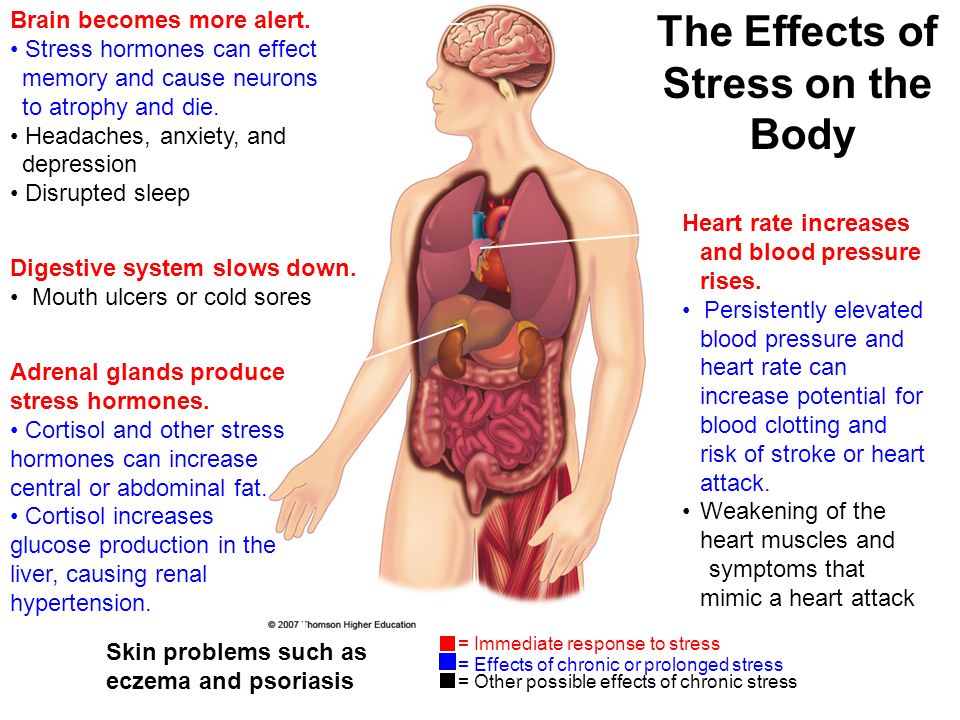 32 841.92] /Contents 191 0 R /group> /Tabs /S /StructParents 49 >> endobj 56 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 192 0 R /group> /Tabs /S /StructParents 50 >> endobj 57 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 193 0 R /group> /Tabs /S /StructParents 51 >> endobj 58 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 194 0 R /group> /Tabs /S /StructParents 52 >> endobj 59 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 195 0 R /group> /Tabs /S /StructParents 53 >> endobj 60 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 196 0 R /group> /Tabs /S /StructParents 54 >> endobj 61 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 197 0 R /group> /Tabs /S /StructParents 55 >> endobj 62 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 191 0 R /group> /Tabs /S /StructParents 49 >> endobj 56 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 192 0 R /group> /Tabs /S /StructParents 50 >> endobj 57 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 193 0 R /group> /Tabs /S /StructParents 51 >> endobj 58 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 194 0 R /group> /Tabs /S /StructParents 52 >> endobj 59 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 195 0 R /group> /Tabs /S /StructParents 53 >> endobj 60 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 196 0 R /group> /Tabs /S /StructParents 54 >> endobj 61 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 197 0 R /group> /Tabs /S /StructParents 55 >> endobj 62 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.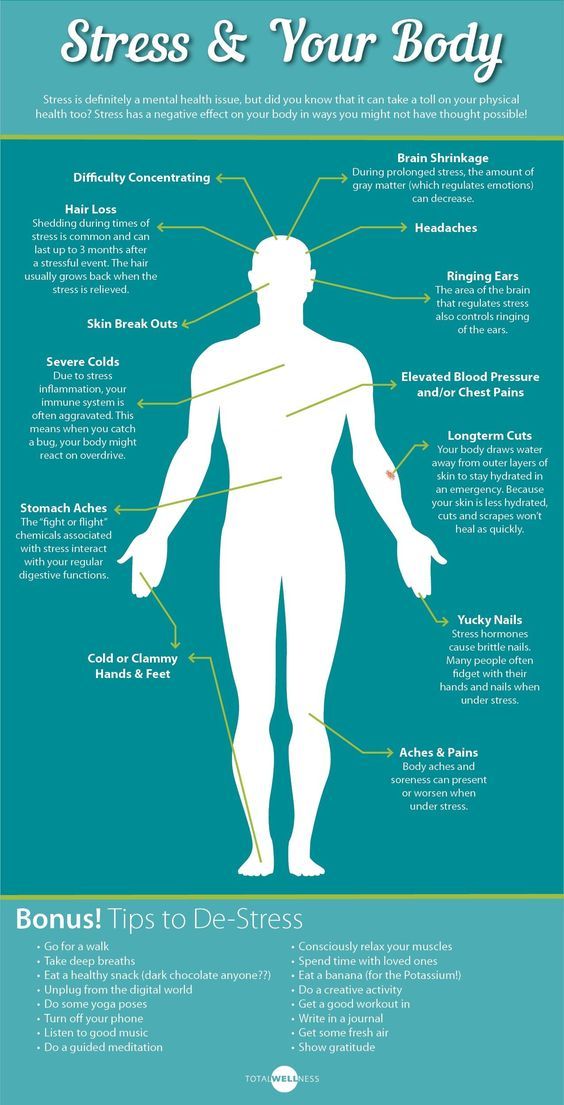 32 841.92] /Contents 198 0 R /group> /Tabs /S /StructParents 56 >> endobj 63 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 199 0 R /group> /Tabs /S /StructParents 57 >> endobj 64 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 200 0R /group> /Tabs /S /StructParents 58 >> endobj 65 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 201 0 R /group> /Tabs /S /StructParents 59 >> endobj 66 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 202 0 R /group> /Tabs /S /StructParents 60 >> endobj 67 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 203 0 R /group> /Tabs /S /StructParents 61 >> endobj 68 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 204 0 R /group> /Tabs /S /StructParents 62 >> endobj 69 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 198 0 R /group> /Tabs /S /StructParents 56 >> endobj 63 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 199 0 R /group> /Tabs /S /StructParents 57 >> endobj 64 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 200 0R /group> /Tabs /S /StructParents 58 >> endobj 65 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 201 0 R /group> /Tabs /S /StructParents 59 >> endobj 66 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 202 0 R /group> /Tabs /S /StructParents 60 >> endobj 67 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 203 0 R /group> /Tabs /S /StructParents 61 >> endobj 68 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 204 0 R /group> /Tabs /S /StructParents 62 >> endobj 69 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.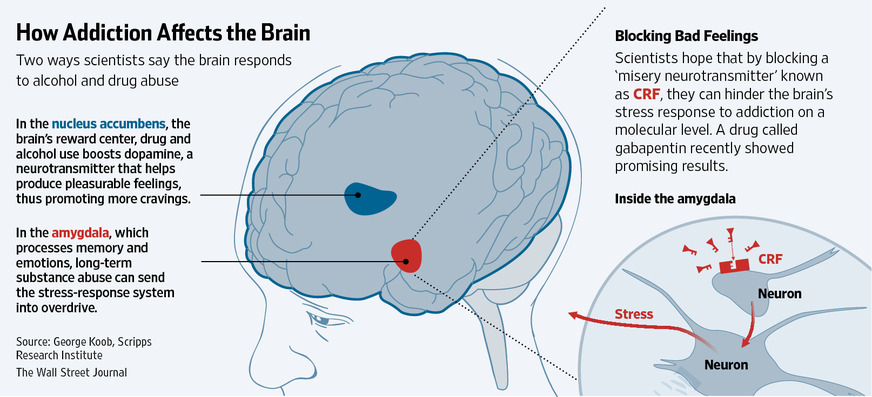 32 841.92] /Contents 212 0 R /group> /Tabs /S /StructParents 70 >> endobj 77 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 213 0R /group> /Tabs /S /StructParents 71 >> endobj 78 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 214 0R /group> /Tabs /S /StructParents 72 >> endobj 79 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 215 0R /group> /Tabs /S /StructParents 73 >> endobj 80 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 216 0R /group> /Tabs /S /StructParents 74 >> endobj 81 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 217 0 R /group> /Tabs /S /StructParents 75 >> endobj 82 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 218 0 R /group> /Tabs /S /StructParents 76 >> endobj 83 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 212 0 R /group> /Tabs /S /StructParents 70 >> endobj 77 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 213 0R /group> /Tabs /S /StructParents 71 >> endobj 78 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 214 0R /group> /Tabs /S /StructParents 72 >> endobj 79 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 215 0R /group> /Tabs /S /StructParents 73 >> endobj 80 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 216 0R /group> /Tabs /S /StructParents 74 >> endobj 81 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 217 0 R /group> /Tabs /S /StructParents 75 >> endobj 82 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 218 0 R /group> /Tabs /S /StructParents 76 >> endobj 83 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 219 0 R /group> /Tabs /S /StructParents 77 >> endobj 84 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 220 0 R /group> /Tabs /S /StructParents 78 >> endobj 85 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 221 0 R /group> /Tabs /S /StructParents 79 >> endobj 86 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 222 0 R /group> /Tabs /S /StructParents 80 >> endobj 87 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 223 0R /group> /Tabs /S /StructParents 81 >> endobj 88 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 224 0R /group> /Tabs /S /StructParents 82 >> endobj 89 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 225 0R /group> /Tabs /S /StructParents 83 >> endobj 90 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 219 0 R /group> /Tabs /S /StructParents 77 >> endobj 84 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 220 0 R /group> /Tabs /S /StructParents 78 >> endobj 85 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 221 0 R /group> /Tabs /S /StructParents 79 >> endobj 86 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 222 0 R /group> /Tabs /S /StructParents 80 >> endobj 87 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 223 0R /group> /Tabs /S /StructParents 81 >> endobj 88 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 224 0R /group> /Tabs /S /StructParents 82 >> endobj 89 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 225 0R /group> /Tabs /S /StructParents 83 >> endobj 90 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595. 32 841.92] /Contents 226 0R /group> /Tabs /S /StructParents 84 >> endobj 91 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 227 0R /group> /Tabs /S /StructParents 85 >> endobj 92 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 228 0R /group> /Tabs /S /StructParents 86 >> endobj 93 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 229 0 R /group> /Tabs /S /StructParents 87 >> endobj 94 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 230 0 R /group> /Tabs /S /StructParents 88 >> endobj 95 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 231 0R /group> /Tabs /S /StructParents 89 >> endobj 96 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 232 0R /group> /Tabs /S /StructParents 90 >> endobj 97 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 226 0R /group> /Tabs /S /StructParents 84 >> endobj 91 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 227 0R /group> /Tabs /S /StructParents 85 >> endobj 92 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 228 0R /group> /Tabs /S /StructParents 86 >> endobj 93 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 229 0 R /group> /Tabs /S /StructParents 87 >> endobj 94 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 230 0 R /group> /Tabs /S /StructParents 88 >> endobj 95 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 231 0R /group> /Tabs /S /StructParents 89 >> endobj 96 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 232 0R /group> /Tabs /S /StructParents 90 >> endobj 97 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 234 0 R /group> /Tabs /S /StructParents 91 >> endobj 98 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 235 0R /group> /Tabs /S /StructParents 92 >> endobj 99 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 237 0R /group> /Tabs /S /StructParents 93 >> endobj 100 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 238 0 R /group> /Tabs /S /StructParents 94 >> endobj 101 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 239 0 R /group> /Tabs /S /StructParents 95 >> endobj 102 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 240 0 R /group> /Tabs /S /StructParents 96 >> endobj 103 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 241 0 R /group> /Tabs /S /StructParents 97 >> endobj 104 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 234 0 R /group> /Tabs /S /StructParents 91 >> endobj 98 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 235 0R /group> /Tabs /S /StructParents 92 >> endobj 99 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 237 0R /group> /Tabs /S /StructParents 93 >> endobj 100 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 238 0 R /group> /Tabs /S /StructParents 94 >> endobj 101 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 239 0 R /group> /Tabs /S /StructParents 95 >> endobj 102 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 240 0 R /group> /Tabs /S /StructParents 96 >> endobj 103 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 241 0 R /group> /Tabs /S /StructParents 97 >> endobj 104 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 242 0 R /group> /Tabs /S /StructParents 98 >> endobj 105 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 243 0R /group> /Tabs /S /StructParents 99 >> endobj 106 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 244 0 R /group> /Tabs /S /StructParents 100 >> endobj 107 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 245 0R /group> /Tabs /S /StructParents 101 >> endobj 108 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 246 0 R /group> /Tabs /S /StructParents 102 >> endobj 109 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 247 0 R /group> /Tabs /S /StructParents 103 >> endobj 110 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.
32 841.92] /Contents 242 0 R /group> /Tabs /S /StructParents 98 >> endobj 105 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 243 0R /group> /Tabs /S /StructParents 99 >> endobj 106 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 244 0 R /group> /Tabs /S /StructParents 100 >> endobj 107 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 245 0R /group> /Tabs /S /StructParents 101 >> endobj 108 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 246 0 R /group> /Tabs /S /StructParents 102 >> endobj 109 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 247 0 R /group> /Tabs /S /StructParents 103 >> endobj 110 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841. 92] /Contents 248 0 R /group> /Tabs /S /StructParents 104 >> endobj 111 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 249 0 R /group> /Tabs /S /StructParents 105 >> endobj 112 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 250 0 R /group> /Tabs /S /StructParents 106 >> endobj 113 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 251 0 R /group> /Tabs /S /StructParents 107 >> endobj 114 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 252 0 R /group> /Tabs /S /StructParents 108 >> endobj 115 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 253 0 R /group> /Tabs /S /StructParents 109 >> endobj 116 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 254 0 R /group> /Tabs /S /StructParents 110 >> endobj 117 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
92] /Contents 248 0 R /group> /Tabs /S /StructParents 104 >> endobj 111 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 249 0 R /group> /Tabs /S /StructParents 105 >> endobj 112 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 250 0 R /group> /Tabs /S /StructParents 106 >> endobj 113 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 251 0 R /group> /Tabs /S /StructParents 107 >> endobj 114 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 252 0 R /group> /Tabs /S /StructParents 108 >> endobj 115 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 253 0 R /group> /Tabs /S /StructParents 109 >> endobj 116 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 254 0 R /group> /Tabs /S /StructParents 110 >> endobj 117 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595. 32 841.92] /Contents 255 0 R /group> /Tabs /S /StructParents 111 >> endobj 118 0 obj > endobj 119 0 obj > endobj 120 0 obj > endobj 121 0 obj > endobj 122 0 obj > endobj 123 0 obj > endobj 124 0 obj > endobj 125 0 obj > endobj 126 0 obj > endobj 127 0 obj > endobj 128 0 obj > stream x
32 841.92] /Contents 255 0 R /group> /Tabs /S /StructParents 111 >> endobj 118 0 obj > endobj 119 0 obj > endobj 120 0 obj > endobj 121 0 obj > endobj 122 0 obj > endobj 123 0 obj > endobj 124 0 obj > endobj 125 0 obj > endobj 126 0 obj > endobj 127 0 obj > endobj 128 0 obj > stream x Short-term restless sleep - symptoms, diagnosis, treatment in Zheleznodorozhny
04/22/2017
Sleep disturbance is a fairly common problem. Frequent complaints of poor sleep are made by 8-15% of the adult population of our planet, and 9-11% use different sleeping pills. This figure is even higher among the elderly. Sleep disorders can be found at any age, and each age category has its own disorders. There are sleep disorders that begin in childhood and do not leave a person all his life, for example, narcolepsy.
Sleep disturbance can be primary, which is not associated with organ pathology, or secondary, resulting from other diseases. Sleep disorders occur as a result of various diseases of the central nervous system or mental disorders. A number of somatic diseases cause insomnia in patients under the influence of shortness of breath, pain, angina attacks, coughing or arrhythmia, frequent urination, itching, etc. Intoxication of various origins, including in patients with oncology, causes drowsiness. Sleep problems that are pathological in nature can develop due to hormonal abnormalities, for example, during the pathology of the hypothalamic-mesencephalic region (tumor, epidemic encephalitis, etc.).
A number of somatic diseases cause insomnia in patients under the influence of shortness of breath, pain, angina attacks, coughing or arrhythmia, frequent urination, itching, etc. Intoxication of various origins, including in patients with oncology, causes drowsiness. Sleep problems that are pathological in nature can develop due to hormonal abnormalities, for example, during the pathology of the hypothalamic-mesencephalic region (tumor, epidemic encephalitis, etc.).
Classification of sleep disorders
1. Insomnia is insomnia, a violation of the process of falling asleep and sleeping.
-
Psychological refers to the psychological state, can be situational (temporary) or permanent.
-
As a result of taking alcohol or drugs:
1. chronic alcoholism;
2. prolonged use of drugs that activate or depress the central nervous system;
3. syndrome of withdrawal of sleeping pills, sedatives or other drugs;
syndrome of withdrawal of sleeping pills, sedatives or other drugs;
1. syndrome of decreased alveolar ventilation;
2. sleep apnea syndrome;
2. Hypersomnia, which is increased sleepiness
-
Psychophysiological, which is associated with the psychological sphere, can be permanent or temporary
-
As a result of taking alcohol or medications;
-
As a result of mental illness;
-
As a result of various breathing disorders during sleep;
-
Narcolepsy
-
As a result of other pathological conditions
3. Wrong mode of wakefulness and sleep
1. slow sleep syndrome
2. premature sleep syndrome
3. syndrome in which there is no 24-hour cycle of sleep and wakefulness
4. Parasomnia, which is characterized by impaired functioning of systems and organs associated with sleep or awakening:
Sleep disturbance symptoms
Symptoms of sleep disorders can be varied and are determined by the type of disorder. However, regardless of sleep disturbance, in a short period of time it can lead to a change in the emotional background, performance and attentiveness of a person. Children at school age have learning problems, they learn new information worse. It is not uncommon for a patient to come to the doctor complaining of worsening health, while not realizing that this is related to disturbed sleep.
However, regardless of sleep disturbance, in a short period of time it can lead to a change in the emotional background, performance and attentiveness of a person. Children at school age have learning problems, they learn new information worse. It is not uncommon for a patient to come to the doctor complaining of worsening health, while not realizing that this is related to disturbed sleep.
Psychosomatic insomnia. Insomnia is situational when it lasts no more than three weeks. People who suffer from insomnia are less likely to fall asleep, often waking up in the middle of the night, and find it difficult to get back to sleep. They are characterized by early morning awakening, feel the lack of sleep after sleep. Because of this, they experience irritability, emotional instability, overwork. The situation is complicated by the constant worries of patients about disturbed sleep and the anxious expectation of the night. The time during which they try to fall asleep lasts twice as long for them. Situational insomnia is caused by the emotional state of a person under the influence of certain psychological phenomena. Often after the effects of stressful conditions cease, sleep returns to normal. But in certain cases, difficulties in falling asleep, as well as nighttime wakefulness, become commonplace, and the fear of insomnia further worsens the situation, which leads to the formation of regular insomnia.
Situational insomnia is caused by the emotional state of a person under the influence of certain psychological phenomena. Often after the effects of stressful conditions cease, sleep returns to normal. But in certain cases, difficulties in falling asleep, as well as nighttime wakefulness, become commonplace, and the fear of insomnia further worsens the situation, which leads to the formation of regular insomnia.
Insomnia resulting from the use of alcoholic beverages or medications. Long-term regular consumption of alcohol can lead to deviations in the organization of sleep. There is a shortening of the phase of REM sleep and the patient often wakes up in the middle of the night. After the alcohol intake is stopped, the problem usually disappears after two weeks.
Disturbed sleep may be a side effect of medications taken that excite the nervous system. Long-term use of sleeping pills and sedatives also leads to insomnia. Over time, the effect of the drug declines, and increasing the dose leads to a short-term improvement in the situation. Due to disturbed sleep, aggravation is possible, despite increased doses. In such situations, systematic short-term awakenings are noted, and a clear boundary between sleep phases also disappears.
Due to disturbed sleep, aggravation is possible, despite increased doses. In such situations, systematic short-term awakenings are noted, and a clear boundary between sleep phases also disappears.
When a mentally ill person has insomnia, he has a constant feeling of intense anxiety at night, quite sensitive and superficial sleep, frequent awakenings, daytime apathy, and fatigue.
Sleep apnea or sleep apnea is a short-term interruption in the flow of air into the upper respiratory tract that occurs during sleep. Such a pause in breathing is usually accompanied by snoring or restlessness. There are obstructive apneas, which begin as a result of the closure of the lumen of the upper respiratory canals during inspiration, and central apneas, related to deviations in the work of the respiratory center.
Insomnia during restless legs syndrome begins to develop as a result of a feeling that forms in the depths of the calf muscles, which requires movement of the legs.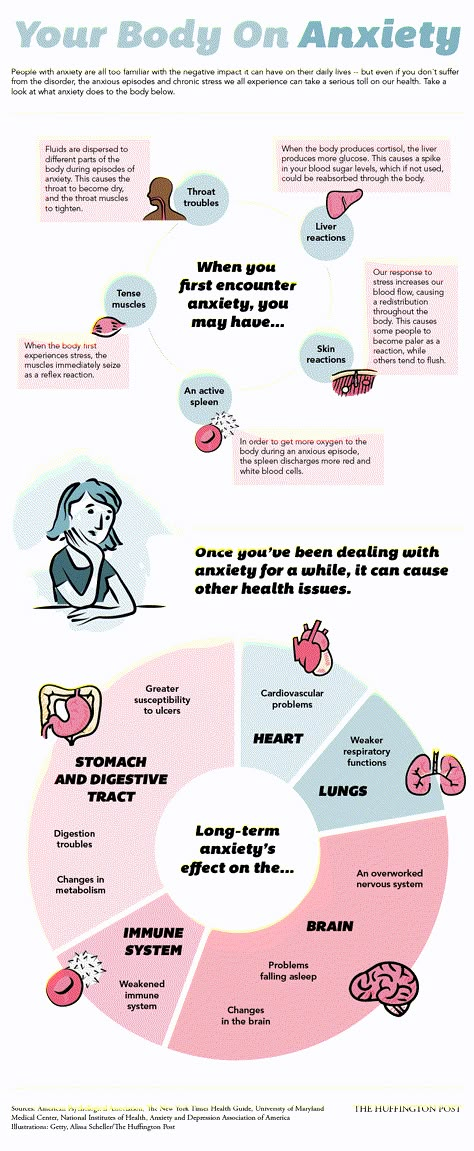 The desire to move the legs appears before sleep and disappears when walking begins, but then it may resume again.
The desire to move the legs appears before sleep and disappears when walking begins, but then it may resume again.
Diagnosis of sleep disorders
Polysomnography is the most common way to study sleep disorders. This examination is carried out by a somnologist in a specialized laboratory in which the patient spends the night. While the patient is sleeping, various sensors simultaneously record the bioelectrical activity of the brain (EEG), cardiac activity (ECG), respiratory actions of the anterior abdominal wall and chest, the air flow that is inhaled and exhaled, oxygen saturation of the blood, etc. Everything that happens in the ward is filmed and a doctor is on duty. Thanks to this examination, it is possible to examine the state of brain activity and the work of the main body systems during each five stages of sleep, to establish deviations and find the cause of disturbed sleep. Another way to diagnose sleep disorders is to study the average sleep latency (SLS). It is used in identifying the causes of drowsiness and plays an important role in the process of diagnosing narcolepsy. The study includes five attempts to fall asleep that are made while awake. Each attempt is given 20 minutes, the interval between these attempts is two hours. The average sleep latency is the time it takes the patient to fall asleep. When it is more than 10 minutes, this is normal, from 10 to 5 minutes is a borderline indicator, less than 5 minutes already indicates pathological drowsiness.
It is used in identifying the causes of drowsiness and plays an important role in the process of diagnosing narcolepsy. The study includes five attempts to fall asleep that are made while awake. Each attempt is given 20 minutes, the interval between these attempts is two hours. The average sleep latency is the time it takes the patient to fall asleep. When it is more than 10 minutes, this is normal, from 10 to 5 minutes is a borderline indicator, less than 5 minutes already indicates pathological drowsiness.
Treatment
Depending on the cause of sleep disturbance, treatment by a neurologist is prescribed. With somatic pathology, therapy is directed to the underlying disease. The reduction in the depth of sleep, as well as its duration, which occurs in the elderly, is a natural process and often only needs an explanatory consultation with the patient. Before resorting to sleeping pills, it is recommended to monitor compliance with the basic principles of healthy sleep: do not go to bed in a state of excitement or anger, do not eat before bedtime, do not drink alcohol, strong tea, coffee at night, do not fall asleep during the day, do not forget about the lesson sports, but do not exercise at night, keep the bedroom clean. Patients who have disturbed sleep are advised to go to bed and wake up at the same time every day. If you haven’t been able to fall asleep for 30-40 minutes, you need to get up and keep busy until sleep appears. Evening relaxing treatments will be useful: a warm bath or a walk. Psychotherapy, various soothing techniques often help to solve the problems of disturbed sleep.
Patients who have disturbed sleep are advised to go to bed and wake up at the same time every day. If you haven’t been able to fall asleep for 30-40 minutes, you need to get up and keep busy until sleep appears. Evening relaxing treatments will be useful: a warm bath or a walk. Psychotherapy, various soothing techniques often help to solve the problems of disturbed sleep.
In the medical treatment of sleep disorders, benzodiazeline drugs are often used. Tablets with a short period of exposure - triazolam, midazolam are prescribed when the process of falling asleep is disturbed. However, their reception is often accompanied by side reactions: confusion, agitation, disturbed morning sleep, amnesia. Long-acting sleeping pills - diazelam, chlordiazepoxide, flurazelam are used for frequent nocturnal or early morning awakenings. But, they often cause daytime sleepiness. In such situations, they resort to the help of drugs of the average period of exposure - zolpidem and zopiclone.