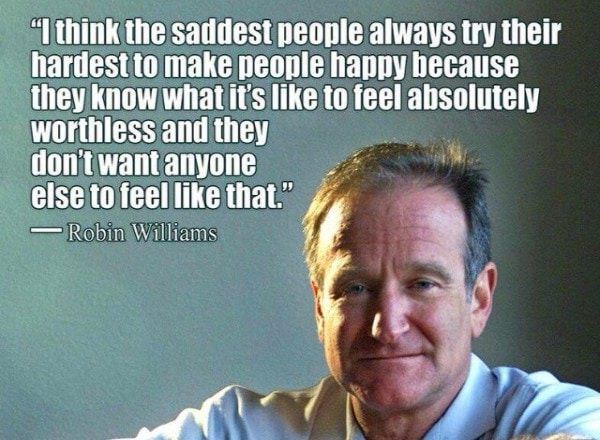
What was robin williams diagnosis
Lewy body dementia: What Robin Williams' widow wants you to know
CNN —
After Robin Williams died by suicide in August 2014, his widow, Susan Schneider Williams, would soon learn about a disease she had never heard of, but one that had haunted both of their lives.
That disease is Lewy body dementia, with which the actor was diagnosed in October 2014 following an autopsy on his brain. “A few months before he passed, he was given a Parkinson’s (disease) diagnosis,” said Schneider Williams, an artist and advocate for LBD awareness and research, at the Life Itself conference, a health and wellness event presented in partnership with CNN.
“But that was just the tip of the iceberg.”
The misdiagnosis occurred in May 2014 after Robin had been experiencing severe memory, movement, personality, reasoning, sleep and mood changes.
The comedian had undergone multiple tests to identify his problem, most of which were negative. “None of the doctors knew that there was this ghost disease underlying all of this,” Schneider Williams told CNN in an interview. “When that was revealed, that was like essentially finding out the name of my husband’s killer.”
Schneider Williams and Robin dine at a restaurant to celebrate her 50th birthday in 2014.
Susan Schneider WilliamsDementia is a disorder of mental processes marked by memory dysfunction, personality changes and impaired reasoning due to brain disease or injury. The exact cause of LBD, which affects about 1.4 million Americans, is unknown. But the disease is associated with the accumulation of the protein alpha-synuclein, which is typically present in the brain and in small amounts in the heart, muscle and other tissues. Alpha-synuclein might help regulate neurotransmitters. But when this protein accumulates and forms masses (called Lewy bodies) within the brain, the effects are devastating.
Lewy body dementia and Parkinson’s disease dementia are the two types of Lewy body dementias, which are the second most common form of dementia after Alzheimer’s disease, according to the Lewy Body Dementia Association.
Because LBD initially presents similarly to Alzheimer’s or Parkinson’s disease, it’s often misdiagnosed. And since Lewy body proteins can’t be tested like Alzheimer’s proteins, LBD cases are often diagnosed after death when families request autopsies for closure or more details, or to donate a loved one’s brain for research.
Close up of woman stirring coffee while sitting at table in cafe || Model approval available Photo by: Channel Partners/picture-alliance/dpa/AP Images
Channel Partners/dpa/picture-alliance/APYour morning cups of coffee and tea could be associated with lower risk of stroke and dementia
Typically for undiagnosed LBD patients who initially exhibit movement issues, doctors first diagnose them with Parkinson’s disease since it is a movement disease. If those patients later develop dementia as well, they are often diagnosed with Parkinson’s disease dementia. More specific changes in cognitive function, too, over time can lead to the diagnosis “dementia with Lewy bodies.” Although Lewy bodies are common with Parkinson’s disease, not all Parkinson’s patients will develop LBD.
If those patients later develop dementia as well, they are often diagnosed with Parkinson’s disease dementia. More specific changes in cognitive function, too, over time can lead to the diagnosis “dementia with Lewy bodies.” Although Lewy bodies are common with Parkinson’s disease, not all Parkinson’s patients will develop LBD.
Misdiagnosis and overlapping symptoms can lead to a world of confusion for patients and their families, so for Schneider Williams, finally learning the truth behind her husband’s “pain and suffering” was a “pinprick of light,” she said.
“That’s when my own healing started to begin,” she said. “We had this experience with something that was invisible and terrifying, truly. And then on the other side of it, I’m left to find out the science underneath it that helped explain this experience. Robin wasn’t crazy. That was one of his biggest fears.”
“We had this experience with something that was invisible and terrifying, truly. And then on the other side of it, I’m left to find out the science underneath it that helped explain this experience. Robin wasn’t crazy. That was one of his biggest fears.”
So that other patients and caregivers can experience the same truth, understanding and healing, Schneider Williams has been in a “rabbit hole of discovery” and advocacy for eight years now. She has served on the board of the American Brain Foundation for six years, helped establish the Lewy Body Dementia Fund and its $3 million research grant award aimed at finding an accurate biomarker, and contributed to the documentaries “Robin’s Wish” and “Spark: Robin Williams and His Battle with Lewy Body Dementia.”
Schneider Williams speaks about LBD awareness and research at the 2021 BioHive Summit in Utah.
“I couldn’t live with myself if I didn’t tell this story,” Schneider Williams said. “I had no idea the journey I was about to begin on. But I had to go there.”
Doctors and researchers wanting to mitigate the kinds of experiences her husband endured “have a tall order,” she said, “but progress is being made.”
Lewy body dementia has more than 40 symptoms that can randomly appear and disappear, Schneider Williams said. Categorically, the signs include impaired thinking, fluctuations in attention, problems with movement, visual hallucinations, sleep disorders, behavioral and mood issues, and changes in bodily functions such as the ability to control urinating.
Categorically, the signs include impaired thinking, fluctuations in attention, problems with movement, visual hallucinations, sleep disorders, behavioral and mood issues, and changes in bodily functions such as the ability to control urinating.
What “marked the beginning of a cascade of symptoms” was when her husband started experiencing never-ending fear and anxiety, Schneider Williams said. It began to happen in 2012 when Williams started to pull back from engaging with people at the Throckmorton Theatre in California, where he would try new material out and riff with other comedians just for fun, she added.
The anxieties persisted beyond what Williams had experienced in the past and what is normal for a beloved actor living with the pressures of being on a world stage.
Eventually, paranoia was another significant symptom, Schneider Williams said. “It was the amygdala region of his brain that had a ginormous amount of the Lewy bodies. So that area of the brain is really our ability to regulate our emotions, particularly fear and anxiety. And Robin’s was basically broken.”
Shutterstock
Find your sleep 'sweet spot' to protect your brain as you age, study suggests
Toward the end, Williams also experienced delusional looping. “Your brain is concocting a story of what you think reality is,” Schneider Williams said. “And the people around you are unable to rationalize with you and bring you back into what is actually real. So it’s incredibly scary for everyone around someone who’s deluded as well as the deluded person.
So it’s incredibly scary for everyone around someone who’s deluded as well as the deluded person.
“As a caregiver, you feel incredibly powerless when you realize, ‘Oh my gosh, nothing I say or do anymore can bring him back to what’s real.’ And that’s a very scary place,” she said. “Lewy body – it really takes over.”
Williams was stressed by work, his sudden forgetfulness and changing personality, and insufficient sleep – which progressed to severe insomnia that removed the separation between day and night in the couple’s home. “Our house was like ‘Night at the Museum’ at night,” Schneider Williams said. Pulling him back from nighttime delusions would take hours, sometimes days, she added. “Imagined fear on fire – that is what it is.”
“Imagined fear on fire – that is what it is.”
Hallucinations are “a key hallmark of LBD that can really help in identifying the disease,” Schneider Williams said, but also a tough symptom many LBD patients don’t want to discuss. She didn’t know about her husband’s hallucinations until her conversation with a medical professional who had reviewed his medical records. A delusion involves a storyline with people who can deconstruct it for you – but a hallucination is something only you see and therefore is easier to hide.
“Lewy body is neurological; it’s a circuitry problem. So the chemical and structural changes happening in Robin’s brain were responsible for the psychiatric symptoms that he was experiencing,” Schneider Williams said at Life Itself. Those included depression.
Those included depression.
The doctors Schneider Williams met with after learning of his diagnosis “indicated his was one of the worst pathologies they had seen. He had about 40% loss of dopamine neurons,” she wrote in her 2016 article “The terrorist inside my husband’s brain” for the journal Neurology. “The massive proliferation of Lewy bodies throughout his brain had done so much damage to neurons and neurotransmitters that in effect, you could say he had chemical warfare in his brain.”
Shutterstock
Is my senior moment the start of dementia?
Antipsychotic medications were dangerous for him and made some symptoms worse, as they do for some LBD patients, Schneider Williams said.
If people experiencing neurodegeneration can still do some routines such as work or walk their dog, those “usual, well-worn pathways can provide comfort,” Schneider Williams said. When people can no longer do those things, symptoms can worsen and lead to devastating feelings of isolation.
Nearly eight years after the diagnosis that catalyzed Schneider Williams’ research journey, she is “just now starting to really pick up the pieces of my own life,” she said.
“I kind of need to go underground for a while and relocate my inspiration and my true passion, which is art and painting,” Schneider Williams said. She plans for a portion of all her future print sales to go to LBD research, and she will stay in touch with efforts related to the documentaries and the Lewy Body Dementia Fund, where she remains lead chair.
She plans for a portion of all her future print sales to go to LBD research, and she will stay in touch with efforts related to the documentaries and the Lewy Body Dementia Fund, where she remains lead chair.
Schneider Williams paints at her home in Marin, California, in 2019.
Richard CormanAs Schneider Williams widens her focus while leaving her door open for LBD advocacy, experts continue their research efforts.
“We’re always learning more and more about the disease, from the basic science studies looking at cells and test tubes, to animal models, to human observational studies,” said Dr. James Galvin, a professor of neurology and director of the Comprehensive Center for Brain Health at the University of Miami Miller School of Medicine.
Recent highlights include the introduction of at least two new diagnostics, Galvin said: a spinal fluid test from the company Amprion and a skin biopsy test from CND Life Sciences. The spinal fluid test tracks misfolded synuclein and helps doctors diagnose brain diseases, including LBD. The skin biopsy test aims to help doctors distinguish between serious neurologic disorders.
“To have diagnostics – that can confirm in life that someone has Lewy body disease – goes a long way both toward confirming the diagnosis and advancing research,” Galvin said. “The earlier you can start people on treatments, the easier to enroll people in clinical trials to test new medications. ”
”
The National Institutes of Health has awarded Galvin and the company Cognition Therapeutics a $29 million grant for studying whether a new drug, CT1812, is safe and effective for patients with LBD.
To treat LBD, doctors “borrow medicines from Alzheimer’s to treat cognitive symptoms, from Parkinson’s to treat motor symptoms, from narcolepsy to treat attention deficits and from psychiatry to treat behavioral symptoms,” Galvin said in a news release. CT1812 could help the brains of LBD patients clear toxic proteins and protect against functional loss.
NEW YORK - APRIL 27: (US TABLOIDS OUT) Actor Robin Williams appears onstage during MTV's Total Request Live at the MTV Times Square Studios on April 27, 2006 in New York City. (Photo by Peter Kramer/Getty Images)
(Photo by Peter Kramer/Getty Images)
Robin Williams: His advice still matters
“When I wrote that editorial ‘The terrorist inside my husband’s brain,’ I was convinced that a diagnosis wouldn’t matter anyway, because there is no cure,” Schneider Williams said at Life Itself. “But my thinking since then has completely changed. Diagnosis is everything – not just for the patients and caregivers, but for the doctors, clinicians and researchers. If we had an accurate diagnosis, we could have sought specialized care.”
The Lewy Body Dementia Association has formed a Research Centers of Excellence Program, with 22 sites across the United States, to collaborate on clinical trials, assess needs for resources and infrastructure, and develop better measures of clinical symptoms, said Angela Taylor, the association’s interim executive director.
“We can’t undo changes that have already occurred,” said Dr. Samantha Holden, an associate professor of neurology at the University of Colorado and director of the Memory Disorders Clinic at UCHealth University of Colorado Hospital. “But if we catch people early enough, can we prevent it from progressing?”
Research progress is being made in baby steps. When asked whether there has ever been a point when she felt like giving up, Schneider Williams said, “Oh, my God. Pick a day.”
“It’s very overwhelming when you look at all the millions and bazillions of dollars that are spent on research and you think, ‘Oh my God, have we really progressed at all?’ ” she added. But with how complex LBD is, “every yard gained matters.”
But with how complex LBD is, “every yard gained matters.”
“Whoever has hope has many days of feeling the darkness,” Schneider Williams said. “But the thing about hope is that no matter what, you dust yourself off, you pick yourself up and you go forward. And you don’t do that alone.”
Robin Williams Would Have Been 70 This Year, Here's What We Know About Lewy Body Dementia, Suicide and Parkinson's
On July 21, actor and comedic genius Robin Williams would have turned 70. Williams not only amplified and brought awareness to the life-changing, prevalent disease known as Lewy Body Dementia, but his passing brought much needed attention to the importance of mental health and the non-movement symptoms of depression and anxiety that can accompany a neurodegenerative disease.
Nearly seven years after his passing, what do we know about Lewy Body Dementia? How can we help people with a neurological disease experiencing suicidal thoughts?
What is Lewy Body Dementia?
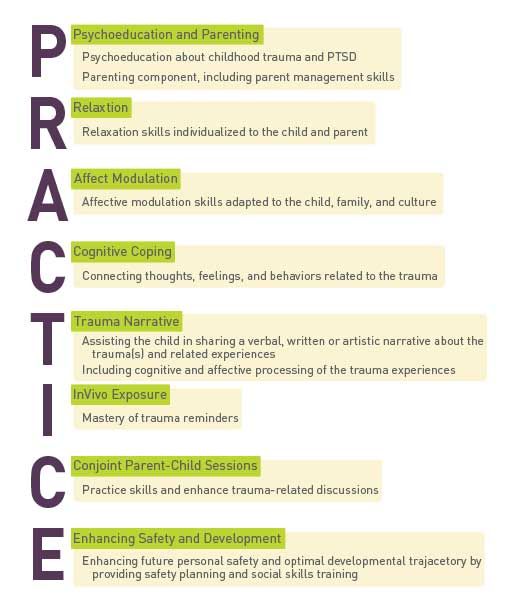
Lewy Body Dementia (LBD), also known as Dementia with Lewy Bodies, is a progressive brain disorder that is diagnosed when cognitive decline is an early symptom. It can also be diagnosed when cognitive decline and motor symptoms begin and develop together.
It can also be diagnosed when cognitive decline and motor symptoms begin and develop together.
“Lewy Body Dementia is a common type of dementia — it is the second most common neurodegenerative dementia behind Alzheimer’s,” said Jennifer G. Goldman, MD, MS, section chief of Parkinson’s Disease and Movement Disorders at Shirley Ryan AbilityLab and a Professor in Physical Medicine and Rehabilitation and Neurology at Northwestern University Feinberg School of Medicine, a Parkinson’s Foundation Center of Excellence. “It is thought to affect 1.4 million people in the U.S. but is not widely recognized. With greater education and awareness, with Lewy Body Dementia including both Dementia with Lewy Body and Parkinson’s disease (PD) dementia, we can start to change that landscape.”
What is the difference between Lewy Body Dementia and Parkinson’s disease dementia?
Lewy Body Dementia is a term used for both Parkinson’s disease dementia and Lewy Body Dementia. They have some things in common, but their progression and treatment are different.
While many people with Parkinson’s can experience cognitive changes, it is important to know that not everyone with Parkinson’s will develop dementia. “When we see more severe cognitive changes, particularly when they affect someone’s function or ability to act independently for activities of daily living, their work or hobbies, we think of that as being a form of dementia,” said Dr. Goldman.
“With Parkinson’s dementia, the motor symptoms precede the dementia. In dementia with Lewy Body the initial core symptom is dementia — cognitive changes are early, and motor features, if present, occur either after the onset of dementia or concurrently,” said Dr. Goldman.
Fight For a Diagnosis
Before Robin Williams was diagnosed with Lewy Body Dementia, it was reported that he had been experiencing paranoia, confusion, insomnia, constipation and lacking the ability to smell. For many, the wide range of early symptoms — not all related to brain function — makes Lewy Body Dementia difficult to diagnose.
Dr. Goldman urges patients to fight to find their diagnosis. “Continue to seek the answers and seek out a specialist to help identify the cause of the cognitive issues or type of dementia,” said Dr. Goldman. “The right doctor can change one’s management, prognosis, and eligibility for participating in research studies. It’s important to have the best understanding of the disease for the chance to have the best outcomes.”
Depression and Suicide
People with neurological conditions, like Parkinson’s, are at higher risk for suicide, according to a study published in in the Journal of the American Medical Association in February 2020. Depression can be a common symptom for both PD and LBD.
People living with Parkinson's benefit most from a comprehensive, team-based healthcare approach that includes a mental health professional. With a team in place, should depression or suicidal thoughts occur, you have an established relationship with a professional you trust. However, it is never too late to add a mental health professional to your care team.
However, it is never too late to add a mental health professional to your care team.
If you or your loved one is having thoughts of suicide:
- Find the resource that works for you: 24-hour suicide prevention hotlines can help, such as the National Suicide Prevention Lifeline at 1-800-273-8255.
- Seek professional help: Find a psychologist, therapist, counselor, or social worker you can trust and lean on.
- Stay engaged: It can be easy for people with Parkinson’s to distance themselves. Try to connect with family and friends, schedule regular phone calls, seek out a support group or wellness class.
- Build your support crew: call the Parkinson's Foundation Helpline at 1-800-4PD-INFO (473-4636) for help finding a local or online support group.
If you are a care partner or family member, learn about suicide warning signs and how you can help here.
Ongoing Hope
There are treatment options for Lewy Body Dementia and Parkinson’s disease dementia. Health care teams are finding that the most effective approach is a combination of medication, physical and mental exercises, and incorporating a mental health professional as part of a care team.
Health care teams are finding that the most effective approach is a combination of medication, physical and mental exercises, and incorporating a mental health professional as part of a care team.
“There is quite a bit of research going on in Lewy Body Dementia,” said Dr. Goldman. “Researchers are trying to understand why it occurs, and whether there are differences between Parkinson’s disease dementia and Lewy Body despite the fact that they share many clinical symptoms and pathology. Ongoing research ranges from trying to predict or detect early changes in people who might go on to develop Lewy Body Dementia all the way to studying different treatments — from medications to newer trials starting to look at the roles of mental and physical exercises.”
More Resources
The Parkinson’s Foundation believes in empowering the Parkinson’s disease community through education. Learn more:
- Podcast Episode 87: What is Lewy Body Dementia and How Does it Relate to Parkinson’s?
- Lewy Body Dementia Association
- Dementia & Parkinson’s
- Caregiver Corner: Lewy What? Explaining Lewy Body Dementia
- Suicide and Parkinson’s
Contact the Parkinson's Foundation Helpline at 1-800-4PD-INFO (1-800-473-4636) for more information about any of these topics and Parkinson’s.
The illness that caused Robin Williams to commit suicide turned out to be even more severe than the doctors' initial diagnosis
Komsomolskaya Pravda
HEALTH medical news not Parkinson's disease, but dementia with Lewy bodies [video]
The "sad clown", as the 63-year-old actor was called, committed suicide a few months after doctors diagnosed him with Parkinson's disease.Photo: REUTERS
Almost a year ago, on August 11, 2014, millions of fans of Hollywood star Robin Williams were saddened. The "sad clown," as the 63-year-old actor was known, took his own life months after doctors diagnosed him with Parkinson's disease. His wife Susan Schneider said that her husband, having learned about the disease, fell into a severe depression. He was very worried that the symptoms of parkinsonism (impaired coordination and movement, trembling of the hands and feet) would soon deprive him of the opportunity to act in films. Life collapsed, because this disease, the rapid development of which, although it is possible to slow down a little with drugs, is still completely incurable. nine0004
nine0004
According to Radar-Online and the Californian media, research on the deceased actor's brain and nerve tissue has just been completed (they can indeed take several months). Pathologists came to the conclusion: the diagnosis is wrong!
The actor did not develop Parkinson's disease, but dementia with Lewy bodies. True, this diagnosis is also not good enough: in addition to motor disorders, the disease also leads to a violation of cognitive abilities (that is, loss of memory, recognition, senile dementia). So, this is the variant of a medical error, when in fact the disease turned out to be even more difficult than the initial diagnosis. nine0004
OPINION OF A SPECIALIST
The actor’s condition could be worsened by drugs for depression
Anna Gorenkova, neurologist, doctor of the highest category: Levi are such tiny protein formations inside the nerve cells of the brain that disrupt its functions). Until the middle of the 20th century, diseases were generally combined into one. Both diseases begin with minor incoordination, the appearance of a "minching" gait, and trembling of the limbs. This, in fact, combines several conditions, which are called parkinsonism syndrome. Hardware diagnostics are also not always accurate: MRI sometimes cannot detect amyloid (that is, protein formations) in the brain in dementia with Lewy bodies, because they are rather loose, not dense. But Parkinson's disease in its pure form can proceed for quite a long time only with movement disorders, then problems with diction, facial expressions, and vision join. But this is stretched over time and can be corrected with drugs. People with Parkinson's disease can maintain mental clarity for many years. nine0004 Lewy body dementia has a worse prognosis. As a rule, it progresses rapidly, cognitive disorders quickly join motor disorders: concentration of attention decreases sharply, patients cannot recognize familiar faces and objects. It is unethical to even imagine what would have happened to the actor if he had been immediately diagnosed with dementia with Lewy bodies. But there is one point. Patients with this diagnosis respond very poorly to antipsychotic drugs, which are often prescribed for depression. Medicines in this group can cause a worsening of the condition and a more rapid increase in all symptoms in those suffering from Lewy dementia. We don’t know what drugs the actor drank for depression and whether he drank at all, but theoretically, if neuroleptics were among them, then this could aggravate the situation. Although there is an observation that with Lewy's dementia, all existing mental disorders progress at a faster pace than, say, with Alzheimer's disease. nine0004  Even experienced neurologists are confused by very similar, almost identical, first symptoms. nine0004
Even experienced neurologists are confused by very similar, almost identical, first symptoms. nine0004  And within five years, severe dementia develops, the patient needs constant care.
And within five years, severe dementia develops, the patient needs constant care. The famous Hollywood actor Robin Williams
Ruslan Rakhmangulov
Read also
Robin Williams. and the whole planet. On August 11, the Oscar winner hanged himself from a doorknob in his home. He was 63 years old, he could not complain about loneliness (he had a family) or lack of work (details)
and the whole planet. On August 11, the Oscar winner hanged himself from a doorknob in his home. He was 63 years old, he could not complain about loneliness (he had a family) or lack of work (details)
MEANWHILE
Before his death, Robin Williams sent his last message to his daughter
American investigators continue to search the home of actor Robin Williams, where he was found dead around noon California time. The preliminary cause of death is suicide. On Sunday evening, the artist was last seen alive at his home, where he lived with his wife (details)
BIOGRAPHY IN PHOTOS
The Funniest Man in the World: From Comedy to Tragedy
Robin Williams' filmography includes about 80 films, not counting television work. And he began his career in ordinary nightclubs, where he worked as an actor-comedian. In one of these clubs, Robin met his future wife, Valeria Velardi. The young couple played a wedding in June 1978 and immediately moved to Los Angeles (details)
Read also
Age category of the site 18+
Online publication (website) registered by Roskomnadzor, certificate El No. ФС77-80505 dated March 15, 2021.
ФС77-80505 dated March 15, 2021.
CHIEF EDITOR — OLESIA VYACHESLAVOVNA NOSOVA.
EDITOR-IN-CHIEF OF THE SITE - KANSK VICTOR FYODOROVICH.
THE AUTHOR OF THE MODERN VERSION OF THE EDITION IS SUNGORKIN VLADIMIR NIKOLAEVICH.
Messages and comments from site readers are posted without preliminary editing. The editors reserve the right to remove them from the site or edit them if the specified messages and comments are an abuse of freedom mass media or violation of other requirements of the law. nine0004
JSC "Publishing House "Komsomolskaya Pravda". TIN: 7714037217 PSRN: 1027739295781 127015, Moscow, Novodmitrovskaya d. 2B, Tel. +7 (495) 777-02-82.
Exclusive rights to materials posted on the website www.kp.ru, in accordance with the legislation of the Russian Federation for the Protection of the Results of Intellectual Activity belong to JSC Publishing House Komsomolskaya Pravda, and do not be used by others in any way form without the written permission of the copyright holder. nine0004
nine0004
Acquiring copyright and contacting the editors: [email protected]
Actor Robin Williams may have hanged himself because he was misdiagnosed
01 July 2015 12:32
EPA
Actor Robin Williams may have committed suicide due to a misdiagnosis. Earlier, the artist's widow said that doctors diagnosed him with Parkinson's disease shortly before his death. However, some Western media say that doctors could be wrong. nine0004
Actor Robin Williams may have committed suicide due to a misdiagnosis. Earlier, the artist's widow said that doctors diagnosed him with Parkinson's disease shortly before his death. However, some Western media say that doctors could be wrong.
The publication Radar Online reported that the editorial office got the conclusion of forensic experts. The study confirmed that the cause of death of Williams was asphyxia - he hanged himself on the doorknob in his bedroom. However, the neurologist's report raised a number of questions. nine0004
The study confirmed that the cause of death of Williams was asphyxia - he hanged himself on the doorknob in his bedroom. However, the neurologist's report raised a number of questions. nine0004
According to the publication, Williams definitely had dementia with Lewy bodies - a disease that involves a chronic loss of cognitive functions, a progressive impairment of memory, speech and thinking. Doctors concluded that he suffered from tremors, anxiety, depression and a number of cognitive impairments. All these symptoms could be signs of both Parkinson's disease and dementia with Lewy bodies, which is diagnosed less often and sometimes confused with Alzheimer's disease.
In May 2014, the actor began treatment for Parkinson's disease, but there was no significant improvement in his condition. Then he started taking Levodopa. One of the side effects of this medication is suicidal thoughts. nine0004
"If Williams had been misdiagnosed during his lifetime, would he have despaired enough to commit suicide? Today, almost a year after his death, there are still questions that apparently will not be answered ", writes Radar Online.