Thc for adhd
Cannabis Use Disorder in Adults and Teens with ADHD
Cannabis is used by a startling number of people with attention deficit hyperactivity disorder (ADHD). Studies show that more than half of daily and non-daily cannabis users have ADHD1, and about one-third of adolescents with ADHD report cannabis use2. People with ADHD are also three times as likely as their neurotypical peers to have ever used marijuana.3
As with other popular substances, cannabis is commonly abused. In fact, the risk of developing cannabis use disorder (CUD), a problematic pattern of cannabis use linked to clinically significant impairment, is twice as high in people with ADHD3. Contrary to popular belief, individuals can be mentally and chemically dependent on and addicted to cannabis. Contemporary marijuana has concentrations of THC higher than historically reported, which exacerbates this. What’s more, the adverse effects of cannabis are especially amplified in people with ADHD.
What are the Negative Effects of Cannabis?
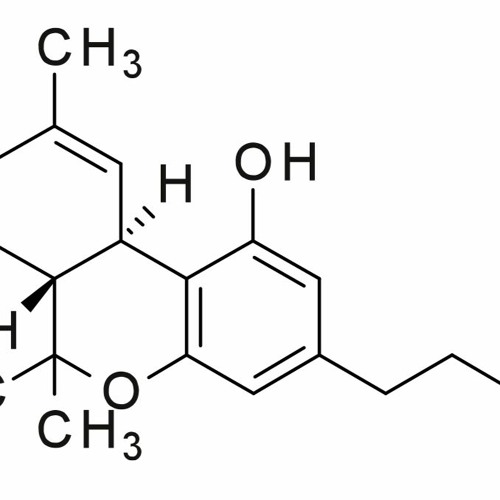
Tetrahydrocannabinol (THC), one of cannabis’ active compounds, inhibits neuronal connections and effectively slows the brain’s signaling process. THC also affects the brain’s dendrite architecture, which controls processing, learning, and the overall health of the brain. Science has not yet fully determined whether THC’s effects are reversible; some parts of the brain show healthy neuronal growth after cannabis use stops, but other parts do not.
Short-term and long-term cannabis use also impairs:
- Motivation (hampering effect)
- Memory, especially in people under 25, by altering the function of the hippocampus and orbitolfrontal cortex, where much of memory is processed
- Performance on complicated task performance with many executive steps. Studies have shown, for example, that driving ability, even while not under the influence, can be impaired in regular marijuana users
Cannabis use may also lead to the following health-related impairments:
- Chronic bronchitis
- Chronic obstructive pulmonary disease (COPD)
- Emphysema
- Cannabinoid hyperemesis syndrome (characterized by severe bouts of vomiting and dehydration)
- Elevated resting heart rate
Cannabis use may exacerbate disorders like paranoia, panic, and mood disorder.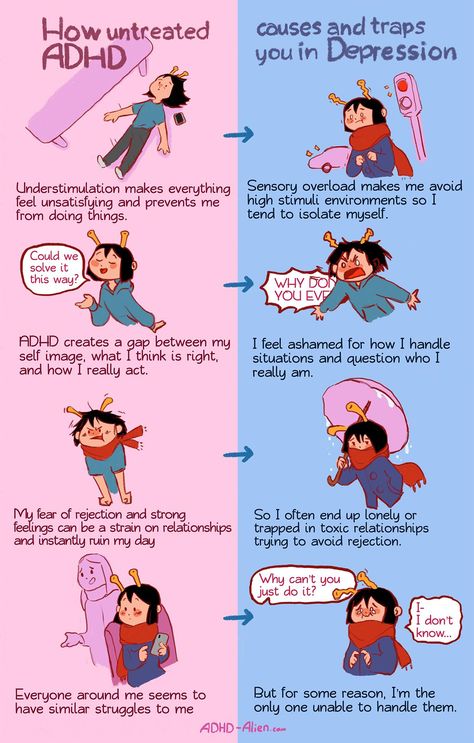 Studies have also found that increased cannabis consumption can uniquely contribute to elevating suicide risk, even when controlling for underlying mental health disorders, like mood disorder or anxiety 45. Individuals who begin regular cannabis use also exhibit more suicidal ideation, even when controlling for pre-existing mood disorders, studies show.67
Studies have also found that increased cannabis consumption can uniquely contribute to elevating suicide risk, even when controlling for underlying mental health disorders, like mood disorder or anxiety 45. Individuals who begin regular cannabis use also exhibit more suicidal ideation, even when controlling for pre-existing mood disorders, studies show.67
What is Cannabis Use Disorder (CUD)?
Cannabis is addictive — 9 percent of people who use cannabis regularly will become dependent on it 8. This figure rises to 17 percent in those who start using cannabis in adolescence.9
CUD can develop after extended cannabis use. It is diagnosed when at least two of the following occur within a 12-month period:
- Taking cannabis in larger amounts over longer periods of time
- Difficulty quitting cannabis use
- Strong desires or cravings to use cannabis
- Lots of time spent trying to obtain, use, or recover from cannabis
- Problems with work, school, or home because of interference from cannabis use
- Social or interpersonal problems due to cannabis use
- Activities given up or reduced because of cannabis use
- Recurrent cannabis use in physically hazardous situations, such as driving
- Physical or psychological problems caused or exacerbated by cannabis use
- Tolerance to cannabis
- Withdrawal from cannabis
How Does Cannabis Affect the ADHD Brain?
Cannabis use impairs areas and functions of the brain that are also uniquely impaired by ADHD.
The substance’s negative effects are most harmful to developing brains. Many studies show that usage earlier in life, particularly before the age of 25, predicts worse outcomes. One study found that heavy marijuana use in adolescence was associated with a loss of 8 IQ points, on average, in adulthood 10. Another study found that people under age 18 are four to seven more times at risk for CUD compared to adults.11
People with ADHD, whose brain development is delayed by slowly maturing frontal lobes, are thus more vulnerable to cannabis’ effects on neuronal connections. Some of these impairments may be irreversible.
Cannabis can also interact significantly with some ADHD medications. Research studies have shown that methylphenidate (Ritalin, Concerta) reacts significantly with the substance, and can cause increased strain on the heart.12
Other studies show that the use of cannabis can decrease the effect of a stimulant medication13. An individual trying to treat their ADHD with stimulants is actually placing themselves at a disadvantage, since the cannabis is impacting them negatively and making the medication less effective.
An individual trying to treat their ADHD with stimulants is actually placing themselves at a disadvantage, since the cannabis is impacting them negatively and making the medication less effective.
The increased risk of suicide associated with cannabis use further complicates marijuana among individuals with ADHD, who already face an elevated risk for suicide compared to neurotypical individuals 14.
What Draws People with ADHD to Cannabis?
Cannabis activates the brain’s reward system, and releases dopamine at levels higher than typically observed. In low-dopamine ADHD brains, THC thus can be very rewarding.
Many people with ADHD also claim that cannabis helps them focus, sleep, or seemingly slow the pace of their thoughts. One analysis of internet threads found that 25 percent of relevant posts described cannabis as therapeutic for ADHD, while 5 percent indicated that it is both therapeutic and harmful 15. Despite some users reporting short-term improvement in symptoms, there is currently no evidence that suggests cannabis is medically or psychologically helpful for managing ADHD in the long-term.![]()
Cannabis’ increased availability and legalization have increased accessibility; many cannabis products are falsely marketed as medicinal for ADHD.
Also contributing to an increased likelihood of cannabis use and CUD among individuals with ADHD is the prevalence of low self-esteem, sleep problems, poor impulse control, and sensation-seeking tendencies in this population.
How is Cannabis Use Disorder Treated in People with ADHD?
There is no approved medication to treat CUD — treatment generally means teaching patients strategies to maintain sobriety. Treatment can include talk therapies, like cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT), and participating in support groups like Marijuana Anonymous.
One small but insightful study looking at motivations to quit cannabis use in a group of adults with ADHD found that saving money was a major contributing factor 16. The same study found that the most common strategy for maintaining abstinence was breaking social connections with people who smoke marijuana.
Treating and targeting ADHD itself in a patient that has CUD is also essential. Stimulant medication can be implemented as part of ADHD treatment, and it is not considered a violation of sobriety.
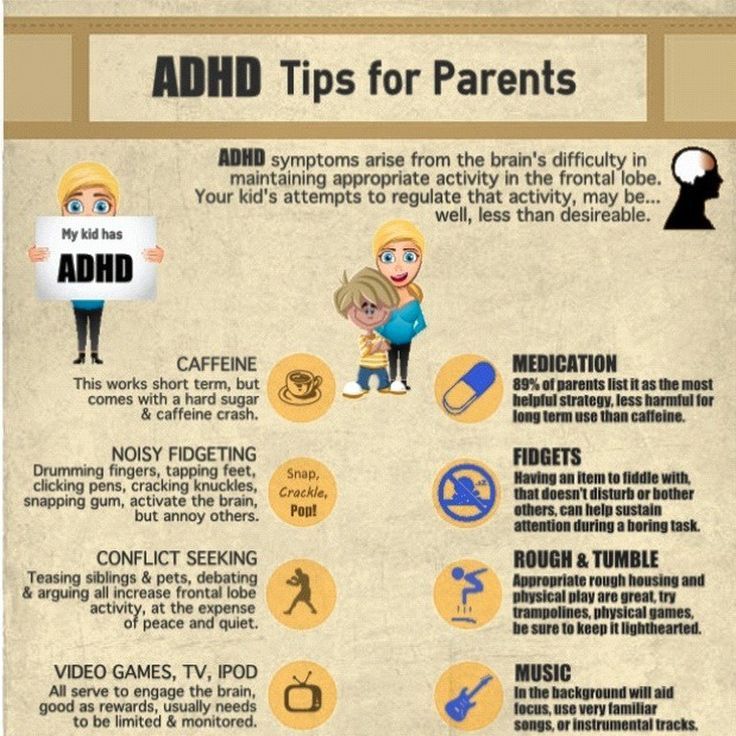
How Should a Parent Help a Teen with ADHD Who Is Using Cannabis?
It’s normal for parents to experience a range of emotions after discovering that their child is using cannabis. The initial gut reaction or emotion is understandably anger and disappointment, but it’s best to release these feelings prior to engaging in conversation. Any dialogue with teens must be done in a controlled, calm way — teens will not listen to parents who are yelling and blurting out things they will later regret.
Seeking consultation with a doctor, pediatrician, or therapist who has experience in substance abuse can help, especially for parents who are struggling with their owns feelings and reactions toward their child.
The next step is for parents to educate themselves on cannabis and how it can be appealing. Parents should try to proactively see what their child might be experiencing, and why they might have turned to the substance. When the conversation does start, parents should work deliberately not to shame their child, and instead focus on understanding their child’s experience on cannabis.
Parents should try to proactively see what their child might be experiencing, and why they might have turned to the substance. When the conversation does start, parents should work deliberately not to shame their child, and instead focus on understanding their child’s experience on cannabis.
Parents should calmly ask questions like:
- “I found this and I’m concerned, but I’d like to know what the appeal of this is for you?”
- “What does this do for you?”
- “How did you feel the very first time that you did this?”
While parents are encouraged to have calm and thoughtful conversations with their teen, they should also set boundaries and consequences for substance use to remind their child that it is not acceptable. Without shaming, parents must establish rules that discourage substance use, especially in the household.
Many parents will say that they would rather have their child smoke in the house than outside with others. But this mentality doesn’t stop teens from smoking or using anywhere else. Instead, allowing at-home use communicates a sense of permission associated with substance use.
Instead, allowing at-home use communicates a sense of permission associated with substance use.
If teens say they are simply experimenting, they should know that experimentation can quickly turn into something more dangerous. Parents should inform them that teens with ADHD are at higher risk for addiction. Teens should also be aware, if they aren’t by this point, of any family history of addiction, which also has a genetic component.
Placing limits on smoking can create some backlash. Teens and young adult may be so gripped by the substance they they are willing to lie about using it to parents. Parents should approach their child if they suspect they are using, even after rules are in place, but should keep in mind that this substance, like any, can have people not always be truthful. That’s very different from thinking that their child can’t be trusted and is a liar.
Children should be reminded that they are loved and that their health is most important. Smoking marijuana doesn’t mean that parents have failed or that they’ve done a bad job with their children.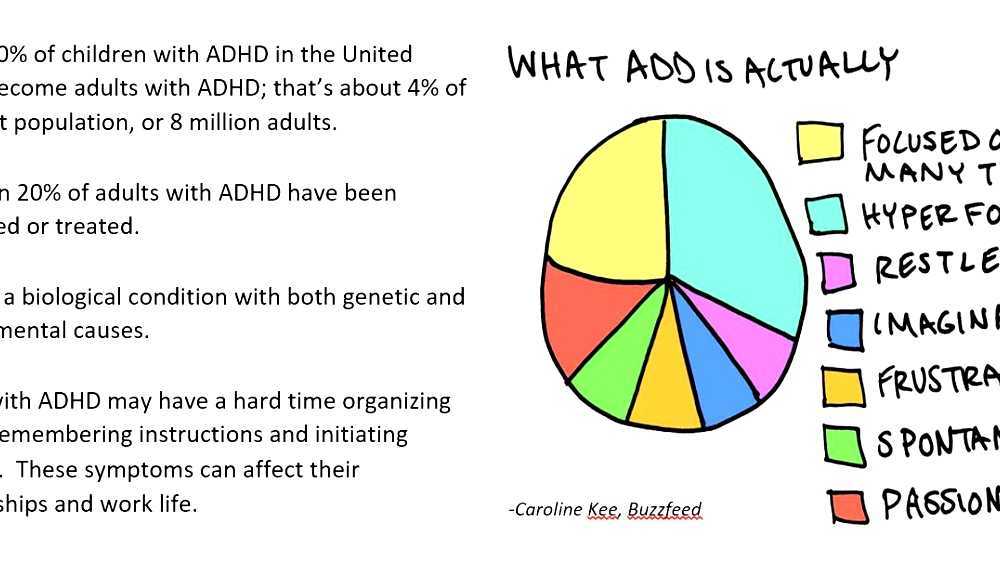 There’s a terrible stigma on addiction surrounding character and morality — it’s important to remember that teens aren’t using drugs because they are bad people. Very, very good people are addicted to substances or experiment with them.
There’s a terrible stigma on addiction surrounding character and morality — it’s important to remember that teens aren’t using drugs because they are bad people. Very, very good people are addicted to substances or experiment with them.
The information in this article is based on Dr. Roberto Olivardia’s two-part Marijuana and the ADHD Brain webinar series. The first part, “Marijuana and the ADHD Brain: How to Identify and Treat Cannabis Use Disorder in Teens and Young Adults” was broadcast live on February 26, 2020. “Marijuana and the ADHD Brain, Part 2” was broadcast live on March 26, 2020.
View Article Sources
1 Loflin, M. et. al. (2014) Subtypes of Attention Deficit-Hyperactivity Disorder (ADHD) and Cannabis Use, Substance Use & Misuse, 49:4, 427-434, DOI: 10.3109/10826084.2013.841251
2 Molina, B. S. et. al. (2013). Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. Journal of the American Academy of Child and Adolescent Psychiatry, 52(3), 250–263. https://doi.org/10.1016/j.jaac.2012.12.014
Journal of the American Academy of Child and Adolescent Psychiatry, 52(3), 250–263. https://doi.org/10.1016/j.jaac.2012.12.014
3 Lee, S. et. al. (2011). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clinical psychology review, 31(3), 328–341. https://doi.org/10.1016/j.cpr.2011.01.006
4 W. Pedersen, “Does cannabis use lead to mood disorder and suicidal behaviors? A population-based longitudinal study,” Acta Psychiatrica Scandinavica, vol. 118, no. 5, pp. 395–403, 2008.https://doi.org/10.1111/j.1600-0447.2008.01259.x
5 Schmidt, K., Tseng, I., Phan, A., Fong, T., & Tsuang, J. (2020, Feb.). A Systematic Review: Adolescent Cannabis Use and Suicide. Addictive Disorders & Their Treatment. doi: 10.1097/ADT.0000000000000196
6 H. Chabrol, J. D. Mabila, and E. Chauchard, “Influence of cannabis use on suicidal ideations among 491 high-school students,” Encephale, vol. 34, no. 3, pp. 270–273, 2008. Doi : 10.1016/j.encep.2007.04.002
34, no. 3, pp. 270–273, 2008. Doi : 10.1016/j.encep.2007.04.002
7 Raja, M., & Azzoni, A. (2009). Suicidal ideation induced by episodic cannabis use. Case reports in medicine, 2009, 321456. https://doi.org/10.1155/2009/321456
8 Lopez-Quintero, C., et. al. (2011). Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug and alcohol dependence, 115(1-2), 120–130. https://doi.org/10.1016/j.drugalcdep.2010.11.004
9 Volkow, N. D. et. al. (2014). Adverse health effects of marijuana use. The New England journal of medicine, 370(23), 2219–2227. https://doi.org/10.1056/NEJMra1402309
10 Meier, M, et. al. (2012). Cannabis use and neuropsychological decline. Proceedings of the National Academy of Sciences. 109 (40) E2657-E2664; DOI: 10. 1073/pnas.1206820109
1073/pnas.1206820109
11 Winters, K. C., & Lee, C. Y. (2008). Likelihood of developing an alcohol and cannabis use disorder during youth: association with recent use and age. Drug and alcohol dependence, 92(1-3), 239–247. https://doi.org/10.1016/j.drugalcdep.2007.08.005
12 Kollins, S. et. al. (2015, Jan). An exploratory study of the combined effects of orally administered methylphenidate and delta-9-tetrahydrocannabinol (THC) on cardiovascular function, subjective effects, and performance in healthy adults. Journal of substance abuse treatment, 48(1), 96-103. https://doi.org/10.1016/j.jsat.2014.07.014
13 Volkow, N. D., Wang, G. J., Telang, F., Fowler, J. S., Alexoff, D., Logan, J., Jayne, M., Wong, C., & Tomasi, D. (2014). Decreased dopamine brain reactivity in marijuana abusers is associated with negative emotionality and addiction severity. Proceedings of the National Academy of Sciences of the United States of America, 111(30), E3149–E3156.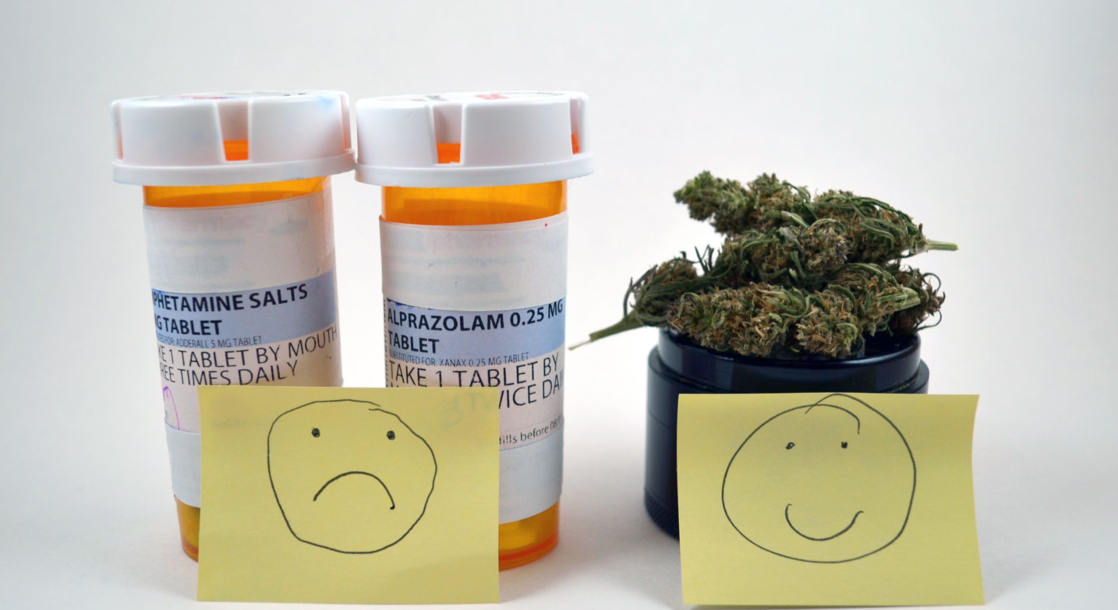 https://doi.org/10.1073/pnas.1411228111
https://doi.org/10.1073/pnas.1411228111
14 Balazs, J., & Kereszteny, A. (2017). Attention-deficit/hyperactivity disorder and suicide: A systematic review. World journal of psychiatry, 7(1), 44–59. https://doi.org/10.5498/wjp.v7.i1.44
15 Mitchell, J. T. et. al. (2016). “I Use Weed for My ADHD”: A Qualitative Analysis of Online Forum Discussions on Cannabis Use and ADHD. PloS one, 11(5), e0156614. https://doi.org/10.1371/journal.pone.0156614
16 Chauchard, E. et. al. (2018). Cannabis Withdrawal in Adults With Attention-Deficit/Hyperactivity Disorder. Prim Care Companion CNS Disord. 20(1). pii: 17m02203. doi: 10.4088/PCC.17m02203.
Previous Article Next Article
Cannabis for the Treatment of Attention Deficit Hyperactivity Disorder: A Report of 3 Cases - FullText - Medical Cannabis and Cannabinoids 2022, Vol.
 5, No. 1
5, No. 1Attention deficit hyperactivity disorder (ADHD) is a chronic neurobehavioral disorder that is highly prevalent in children and adults. An increasing number of patients with ADHD are self-medicating with cannabis, despite a lack of evidence on efficacy and safety. This case report describes 3 males (ages 18, 22, and 23) who have integrated cannabis into their treatment regimen with positive results. Semistructured interviews conducted with the patients describe subjective improvements in symptoms and on quality of life. Improvements on validated rating scales conducted post-cannabis initiation, compared to pre-cannabis initiation obtained from the medical chart, corroborated their personal accounts. Scores on the PHQ-9 (measuring depression) improved by 8–22 points (30–81%), and the SCARED (measuring anxiety) ranged from 0 to 27 points (up to 33%). Improvements on the CEER-9 scale (measuring regulation) ranged from 2 to 7 points (22–78%), and the 9-item SNAP scale (measuring inattention) showed improvements of 2–8 points (7–30%).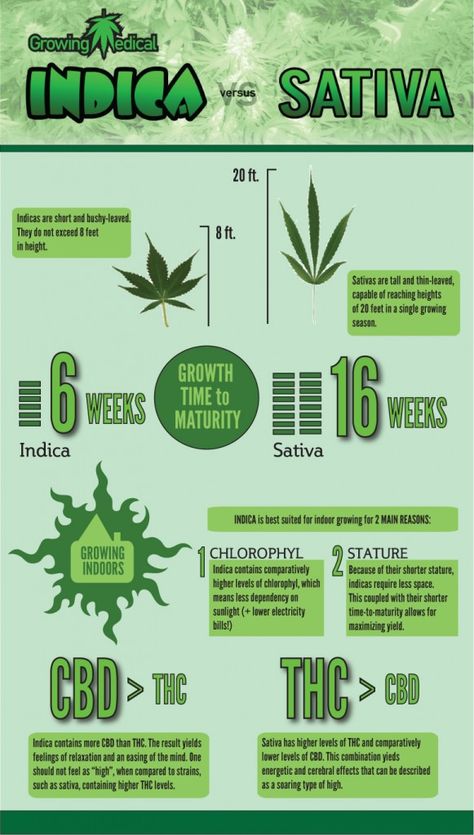 Mild adverse events including short-term memory problems, dry mouth, and sleepiness were reported. Blood samples were also collected from the patients to determine the plasma concentrations of the cannabinoids and relevant metabolites before and after a cannabis administration. After cannabis use, the plasma levels for CBD and THC ranged from 0 to 15.29 ng/mL and 1.32 to 13.76 ng/mL, respectively. Cannabinoids, however, were not detected prior to dosing, suggesting that cannabis played a complimentary role in the therapeutic regimen of these 3 patients. Clinical trials are recommended to confirm the efficacy of cannabis in the treatment of ADHD.
Mild adverse events including short-term memory problems, dry mouth, and sleepiness were reported. Blood samples were also collected from the patients to determine the plasma concentrations of the cannabinoids and relevant metabolites before and after a cannabis administration. After cannabis use, the plasma levels for CBD and THC ranged from 0 to 15.29 ng/mL and 1.32 to 13.76 ng/mL, respectively. Cannabinoids, however, were not detected prior to dosing, suggesting that cannabis played a complimentary role in the therapeutic regimen of these 3 patients. Clinical trials are recommended to confirm the efficacy of cannabis in the treatment of ADHD.
Introduction
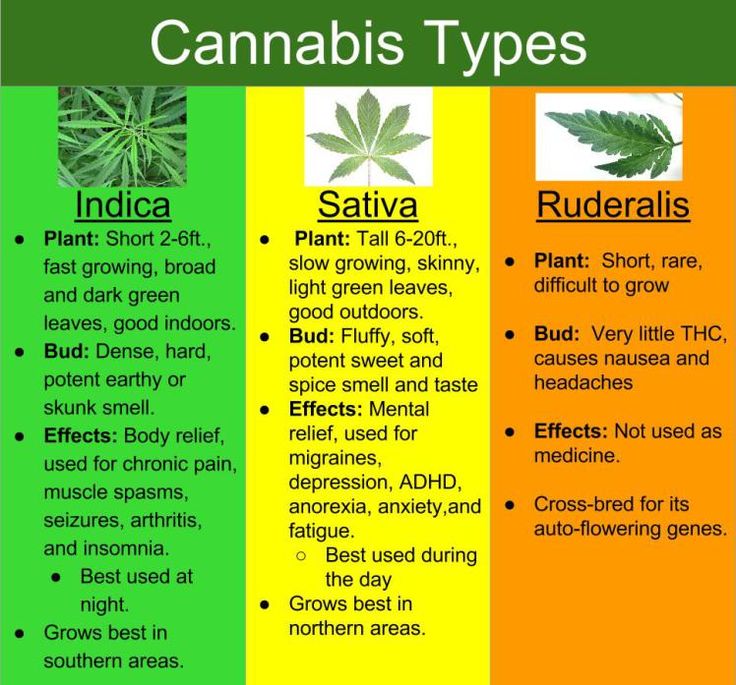
Public acceptance of medical cannabis for the treatment of chronic conditions has increased despite a lack of scientific evidence for safety and efficacy [1, 2]. In Canada, access to both medical and recreational cannabis is now legal, and self-medication with cannabis for a variety of symptoms has become more prevalent. Evidence-based information has not kept pace with the legislation, and many clinicians remain reluctant to authorize cannabis until robust evidence is available to guide treatment [3]. Unfortunately, the limited evidence base may persist due to key challenges such as the difficulty in conducting randomized and placebo-controlled trials with cannabis [4] and the significant variability in cultivars. With >489 distinct compounds in the leaves and flowering tops of cannabis plants, which include at least 120 different phytocannabinoids and other entities such as flavonoids and terpenes [5, 6], cultivars demonstrate important differences in therapeutic effect. Even within a given cultivar, soil and climate conditions and various cultivation techniques can influence its constituent bioactive components. The method of consumption or route of administration further impacts the pharmacokinetics and therapeutic effects of cannabis [7].
Evidence-based information has not kept pace with the legislation, and many clinicians remain reluctant to authorize cannabis until robust evidence is available to guide treatment [3]. Unfortunately, the limited evidence base may persist due to key challenges such as the difficulty in conducting randomized and placebo-controlled trials with cannabis [4] and the significant variability in cultivars. With >489 distinct compounds in the leaves and flowering tops of cannabis plants, which include at least 120 different phytocannabinoids and other entities such as flavonoids and terpenes [5, 6], cultivars demonstrate important differences in therapeutic effect. Even within a given cultivar, soil and climate conditions and various cultivation techniques can influence its constituent bioactive components. The method of consumption or route of administration further impacts the pharmacokinetics and therapeutic effects of cannabis [7].
Attention deficit hyperactivity disorder (ADHD) is one such condition where few clinicians authorize cannabis, but interest in self-medication is high. ADHD is a chronic neurobehavioral disorder characterized by inattention and/or hyperactivity-impulsivity with a prevalence of approximately 7% in children and 2.5% in adults [8, 9]. Over half of the children and adults with ADHD have comorbid psychiatric conditions, such as sleep disorders, mood and anxiety disorders, and oppositional defiant disorder [10, 11]. In addition to the first-line pharmacotherapy with stimulants, internet discussions frequently indicate and advocate use of cannabis for relief of ADHD symptoms [12-14]. In one study, at least 3 times as many online comments attested for its therapeutic benefits in comparison with harm or lack of efficacy [14]. Despite the public interest and anecdotal reports, we only found one study on the use of cannabis in ADHD which compared Sativex Oromucosal Spray to placebo in a pilot study of 30 adults, where participants in the intervention group showed no difference in the primary outcome (cognitive performance as measured by the QbTest), but improved symptoms of hyperactivity/impulsivity (secondary outcome, p = 0.
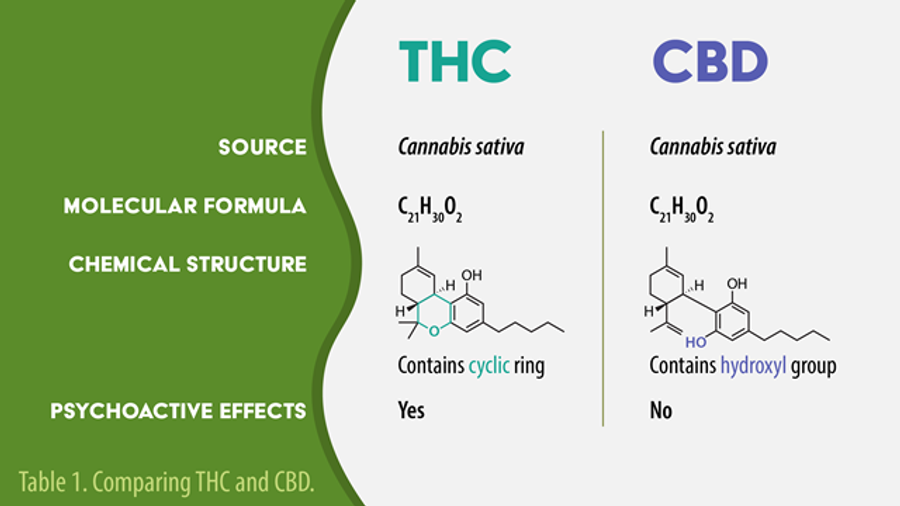
ADHD is a chronic neurobehavioral disorder characterized by inattention and/or hyperactivity-impulsivity with a prevalence of approximately 7% in children and 2.5% in adults [8, 9]. Over half of the children and adults with ADHD have comorbid psychiatric conditions, such as sleep disorders, mood and anxiety disorders, and oppositional defiant disorder [10, 11]. In addition to the first-line pharmacotherapy with stimulants, internet discussions frequently indicate and advocate use of cannabis for relief of ADHD symptoms [12-14]. In one study, at least 3 times as many online comments attested for its therapeutic benefits in comparison with harm or lack of efficacy [14]. Despite the public interest and anecdotal reports, we only found one study on the use of cannabis in ADHD which compared Sativex Oromucosal Spray to placebo in a pilot study of 30 adults, where participants in the intervention group showed no difference in the primary outcome (cognitive performance as measured by the QbTest), but improved symptoms of hyperactivity/impulsivity (secondary outcome, p = 0. 03) [15]. While this study investigated a commercially available product (containing 1:1 cannabidiol [CBD]:Δ9-tetrahydrocannabinol [THC]), a product available in some countries by prescription, many patients are self-medicating with unlicensed products in a variety of formulations [12-14].
03) [15]. While this study investigated a commercially available product (containing 1:1 cannabidiol [CBD]:Δ9-tetrahydrocannabinol [THC]), a product available in some countries by prescription, many patients are self-medicating with unlicensed products in a variety of formulations [12-14].
In the absence of scientific data, case reports are valuable for presenting new observations, generating hypotheses, and providing in-depth examinations of a subject of study as well as its related contextual conditions [16]. In this case report, we identified patients from a psychiatry practice who were prescribed ADHD medications but also self-medicated with cannabis. We explored treatment efficacy and patient perceptions of cannabis use. Since no literature exists to provide guidance for cannabis dosing in patients with ADHD, we also collected patient blood samples to determine plasma concentrations of the cannabinoids and relevant metabolites.
Methods
Three patients who were taking cannabis for symptomatic relief of their ADHD participated in telephone interviews conducted by one of the authors (H. M.). The patients were previously diagnosed using the DSM-V criteria. The interviews lasted between 39 and 59 min. To characterize the patient’s experiences of taking cannabis and its perceived efficacy, a semistructured interview guide facilitated a discussion about the patient’s life prior to initiating cannabis, the decision/reasons for starting it, how (if at all) things have changed since initiating cannabis, logistics on consumption and access, and what (if any) concerns they might have about cannabis. A cannabis side effect survey [17] inquired about potential cannabis side effects experienced by the patients, using the time frame of the previous week.
M.). The patients were previously diagnosed using the DSM-V criteria. The interviews lasted between 39 and 59 min. To characterize the patient’s experiences of taking cannabis and its perceived efficacy, a semistructured interview guide facilitated a discussion about the patient’s life prior to initiating cannabis, the decision/reasons for starting it, how (if at all) things have changed since initiating cannabis, logistics on consumption and access, and what (if any) concerns they might have about cannabis. A cannabis side effect survey [17] inquired about potential cannabis side effects experienced by the patients, using the time frame of the previous week.
Self-report symptom rating scales, including the Swanson Nolan and Pelham (SNAP-IV) (90-item) [18], the Screen for Child Anxiety Related Emotional Disorders (SCARED) [19], and Patient Health Questionnaire (PHQ-9) [20], were performed during the interviews as a measure for treatment efficacy. The SNAP-IV rating scale contains 90 items from the DSM-IV criteria which assess inattention, hyperactivity/impulsivity, and oppositional defiant disorder, as well as items representing a general index of childhood problems.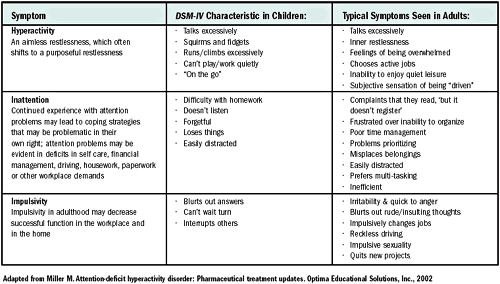 This tool, which is a modified version of the original SNAP questionnaire [18, 21], consists of Likert scale questions that measure the frequency/severity of a symptom or behavior. The items are scaled from 0 to 3 (0 = “not at all,” and 3 = “very much”), and the tool has had good reliability and validity in different study samples [22]. The SCARED rating scale and PHQ-9 assessed symptoms of anxiety and depression, respectively. The 3 rating scales were summed according to standardized methods [18-20] to achieve a composite score, with higher scores equating to higher levels of debility. Baseline symptom scores obtained before cannabis was initiated were collected from the patient’s medical chart and subtracted from the totals, producing an indicator of symptom change. ADHD inattentive symptoms were measured using items 1–9 of the SNAP-IV, while emotional regulation and irritability were measured using the Clinical Evaluation of Emotional Regulation-9 (CEER-9) method, whereby items 21, 23, 25, 26, 28, 34, 38, 39, and 54 from the SNAP-IV questionnaire were converted to a binary score (1 = not at all; 2 = very much) [23].
This tool, which is a modified version of the original SNAP questionnaire [18, 21], consists of Likert scale questions that measure the frequency/severity of a symptom or behavior. The items are scaled from 0 to 3 (0 = “not at all,” and 3 = “very much”), and the tool has had good reliability and validity in different study samples [22]. The SCARED rating scale and PHQ-9 assessed symptoms of anxiety and depression, respectively. The 3 rating scales were summed according to standardized methods [18-20] to achieve a composite score, with higher scores equating to higher levels of debility. Baseline symptom scores obtained before cannabis was initiated were collected from the patient’s medical chart and subtracted from the totals, producing an indicator of symptom change. ADHD inattentive symptoms were measured using items 1–9 of the SNAP-IV, while emotional regulation and irritability were measured using the Clinical Evaluation of Emotional Regulation-9 (CEER-9) method, whereby items 21, 23, 25, 26, 28, 34, 38, 39, and 54 from the SNAP-IV questionnaire were converted to a binary score (1 = not at all; 2 = very much) [23].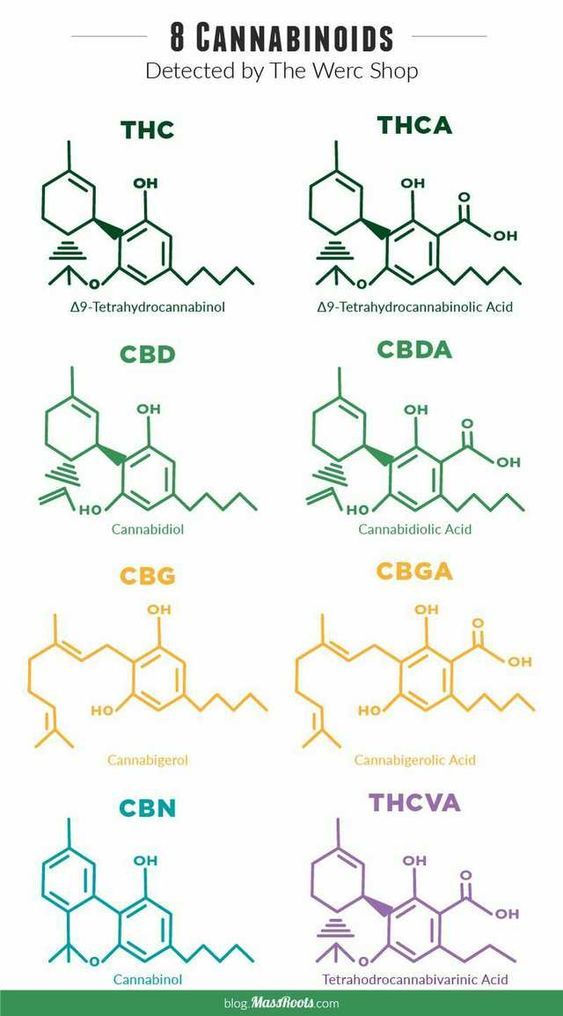
Two blood samples were obtained from each patient by the mobile laboratory to allow quantification of plasma concentrations of cannabinoids and relevant metabolites (THC, CBD, 11-hydroxy-THC, 7-hydroxy-CBD, cannabichromene, and 11-nor-9-carboxy-tertrahydrocannabinol). The samples were collected in BD Vacutainer® BarricorTM tubes [24], centrifuged to separate plasma, transferred to EppendorfTM Protein LoBind microcentrifuge tubes, and stored in a −80°C freezer until they were analyzed by liquid chromatography-tandem mass spectrometry. The method was previously developed and validated within our institution [25] according to FDA guidelines [26]. Written informed consent was obtained from patients for publication of the details of their medical case, and ethical approval for data collection was approved by the Biomedical Research Ethics Boards at the University of Saskatchewan (#1726).
Case Presentations and Patient Perceptions of Cannabis
The case presentations as described in this section represent an account of the patients’ testimonials, with information verified from the medical charts. The patients had the opportunity to review these descriptions for accuracy prior to publication.
The patients had the opportunity to review these descriptions for accuracy prior to publication.
Patient 1
A 23-year-old white male with ADHD and generalized anxiety disorder decided to use cannabis after learning of its effectiveness for ADHD online. Medicated with methylphenidate, pregabalin, fluoxetine, and clonidine, he first tried cannabis in his teens. He used it periodically as cannabis improved his focus. He eventually consulted his physician and received an authorization for medical cannabis in a CBD:THC 20:1 ratio, twice daily. He currently alternates between taking cannabidiol oil orally or smoking flower or bud. Although he realizes oil is less harmful for his lungs and more suitable in some situations, he feels smoking is more relaxing. He describes cannabis as a “really good helping hand” to compliment his other medications, and finds he is more open with others, less anxious, and his emotions are less exaggerated. Cannabis has improved his ability to maintain focus. Regarding his life before cannabis, he says “I was all over the place, bouncing off the walls kind of thing. Couldn’t really stay on one task for long. I’d get halfway to three quarters done one task and then move on and do a completely different task.” Cannabis, as he describes, “levels him out,” and he can complete tasks more efficiently. Although his family members’ reaction to his cannabis have been mixed (with some individuals very supportive and others skeptical), he believes they have all noted a positive impact on his demeanor. Since taking cannabis regularly, he has found and maintained successful employment at a job away from home. The cost of medical cannabis is unaffordable, so he obtains recreational cannabis at half the cost.
Regarding his life before cannabis, he says “I was all over the place, bouncing off the walls kind of thing. Couldn’t really stay on one task for long. I’d get halfway to three quarters done one task and then move on and do a completely different task.” Cannabis, as he describes, “levels him out,” and he can complete tasks more efficiently. Although his family members’ reaction to his cannabis have been mixed (with some individuals very supportive and others skeptical), he believes they have all noted a positive impact on his demeanor. Since taking cannabis regularly, he has found and maintained successful employment at a job away from home. The cost of medical cannabis is unaffordable, so he obtains recreational cannabis at half the cost.
Patient 2
A Caucasian male with ADHD has taken methylphenidate off and on since the third grade. He disliked being medicated with stimulants because he felt they changed his personality, and he continued to struggle with emotional regulation.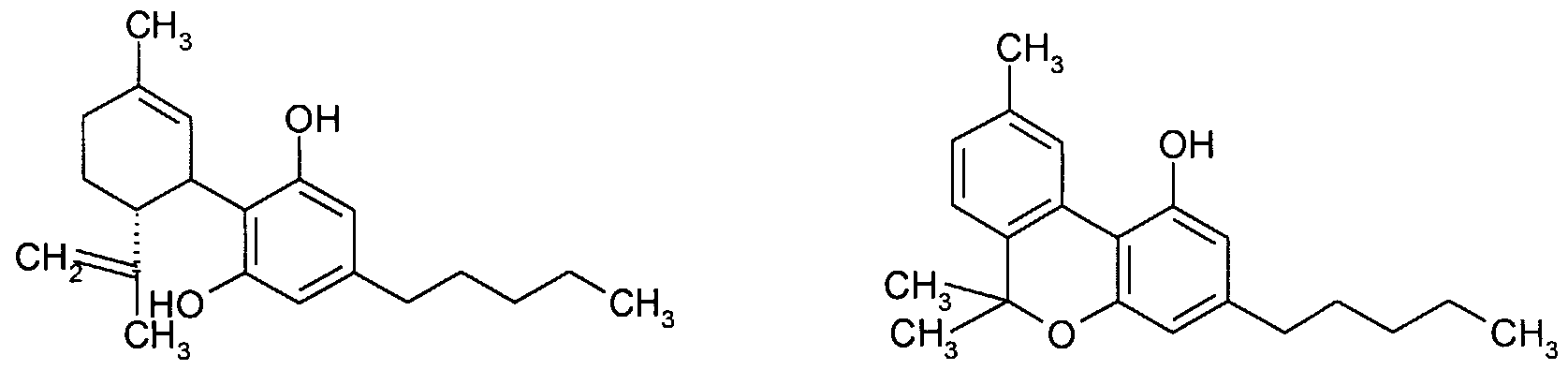 At age 17, he was prescribed lithium, and he decided to start cannabidiol oil (CBD:THC in a 20:1 ratio) once daily (at bedtime) after a family member recommended it to him. Taking cannabis, he says, makes him feel more relaxed and helps him to focus and to feel more “himself.” The combination of lithium (300 mg at bedtime), cannabis (l mL at bedtime), and a good support system he says have completely changed his life. Previously he lacked motivation, did not do well in school, and was admitted for psychiatric care. Since starting cannabis, he was successfully weaned off his other medications for ADHD (takes only lithium for depression and cannabis) and has completely turned his life around. Regarding his life before cannabis he says, “I was definitely a lot more jittery and stuff when I was in school…It [cannabis] helped me to focus a lot more, and it helped me ease off my ADHD meds actually.” He works full time and runs a business, sets long-term goals for future, and has made many new friends, which has improved his social life.
At age 17, he was prescribed lithium, and he decided to start cannabidiol oil (CBD:THC in a 20:1 ratio) once daily (at bedtime) after a family member recommended it to him. Taking cannabis, he says, makes him feel more relaxed and helps him to focus and to feel more “himself.” The combination of lithium (300 mg at bedtime), cannabis (l mL at bedtime), and a good support system he says have completely changed his life. Previously he lacked motivation, did not do well in school, and was admitted for psychiatric care. Since starting cannabis, he was successfully weaned off his other medications for ADHD (takes only lithium for depression and cannabis) and has completely turned his life around. Regarding his life before cannabis he says, “I was definitely a lot more jittery and stuff when I was in school…It [cannabis] helped me to focus a lot more, and it helped me ease off my ADHD meds actually.” He works full time and runs a business, sets long-term goals for future, and has made many new friends, which has improved his social life.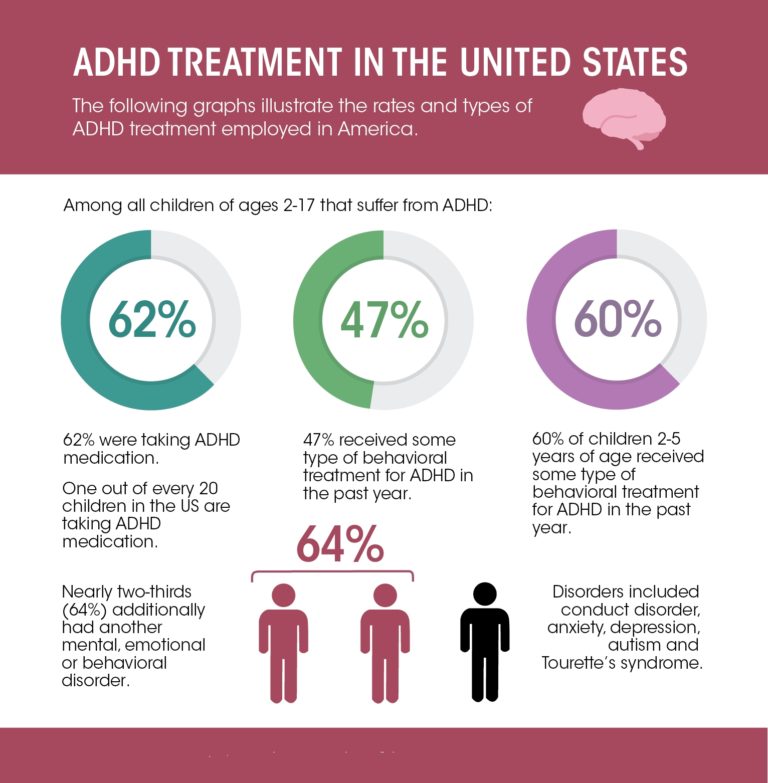
Patient 3
A 22-year-old male was diagnosed with ADHD when he was 20 and started self-medicating with cannabis. He had no prior history of cannabis use, but with dispensaries opening in Canada and a family member who was considering it for anxiety, he decided to try it as well. He feels that cannabis calms him, helps him to slow down and focus on one thing, and to sleep at night. He believes that cannabis works synergistically with his other medications (dextroamphetamine, amantadine, and pregabalin) to improve his concentration and control his racing thoughts, anxiety, and emotions. Prior to treatment with this combination and as a child, he describes, “the lashing out was really bad, not listening to adult figures. And emotions…And forgetting where I placed stuff. I lost my wallet and keys a lot growing up.” Having experimented with various strains, ratios, and methods of consumption, he prefers an Indica blend that is higher in THC and lower in CBD. Sativa caused him to be a bit more hyperactive and increased his anxiety, whereas an Indica dominant blend helps him to cool down. He is currently smoking a product that has a CBD:THC ratio of 0:18–19 at bedtime, and says that this formulation does not make him feel intoxicated. Dabbing (which has a higher concentration of THC), however, has too much THC and puts him in an “unmotivated funk.” He has tried edibles and oils, but they fail to improve his sleep. He avoids vaping because with his addictive personality and convenience of vaping, he found that he vaped more than just at night. He obtains his supply from a recreational cannabis dispensary where it is most affordable.
He is currently smoking a product that has a CBD:THC ratio of 0:18–19 at bedtime, and says that this formulation does not make him feel intoxicated. Dabbing (which has a higher concentration of THC), however, has too much THC and puts him in an “unmotivated funk.” He has tried edibles and oils, but they fail to improve his sleep. He avoids vaping because with his addictive personality and convenience of vaping, he found that he vaped more than just at night. He obtains his supply from a recreational cannabis dispensary where it is most affordable.
Rating Scale Changes before and after Initiation of Cannabis
Table 1 presents the rating scales obtained from the patient’s medical record and on the day of the interview. These scores were (respectively) obtained before and after the patients used cannabis regularly. Consistent with the testimonials, all 3 patients experienced positive improvements on the measures for depression, emotional regulation, and inattention. The scores from patients 1 and 2 also indicate an improvement in the SCARED, which measures symptoms of anxiety.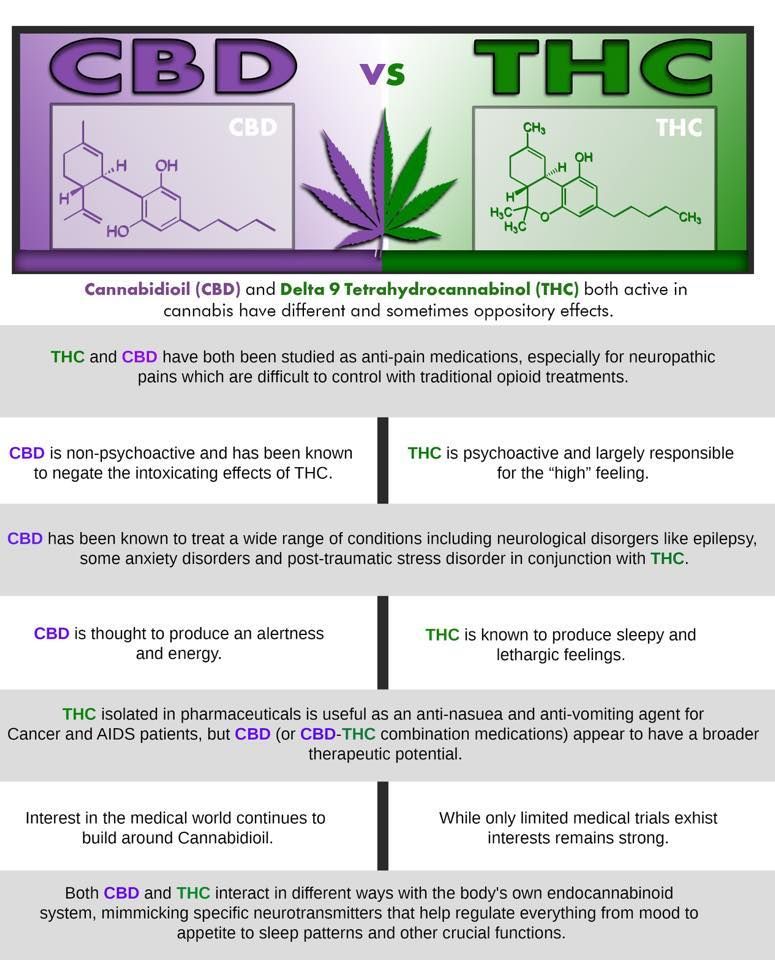
Table 1.
Rating scale scores obtained from 3 ADHD patients’ medical charts prior to and after initiation of cannabis
Cannabis Side Effects
All patients reported mild side effects from cannabis use. Patient 2, who consistently takes oil orally, experienced short-term memory problems. Patients 1 and 3, who alternate between oral and inhalation routes, reported dry mouth and sleepiness. Patient 1 reported occasional experiences of constant desire and more forgetfulness and apathy, and patient 3 reported an altered sense of time.
Blood Sample Analysis
Two blood samples were taken at home just prior to and 2 h after cannabis administration from each patient to quantify plasma concentrations of major cannabinoids and relevant metabolites (Table 2). Each patient self-reported their cannabis product and was not verified by chemical analysis. None of the patients had detectable plasma concentrations of any of the cannabinoids tested during the pre-dose level (trough), which represents the time when plasma levels are the lowest.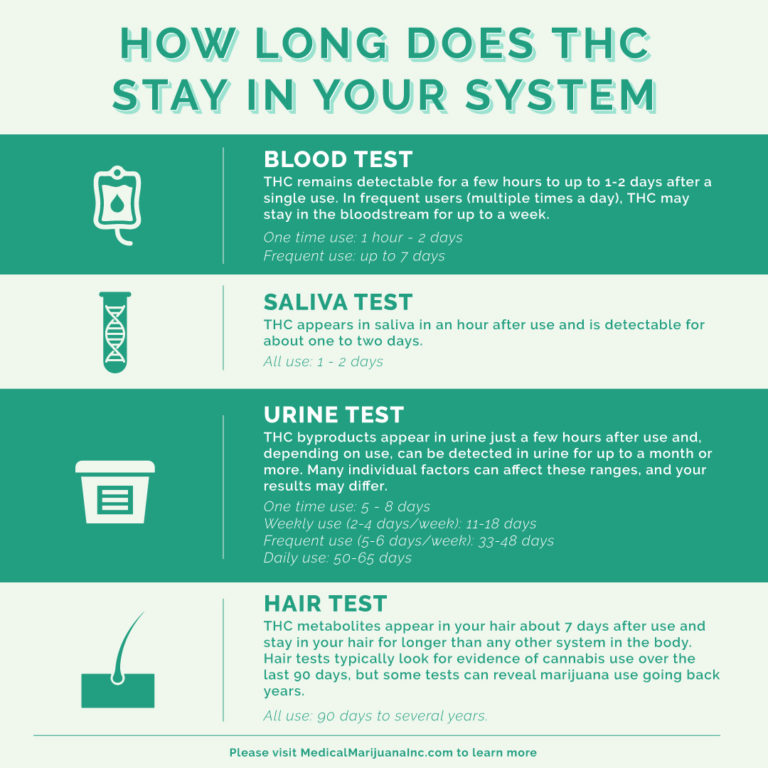 The post-dose level, which is intended to represent the maximum plasma cannabinoid concentration, should be collected at approximately 30 min after smoked cannabis and 2 h for edible formulations [6]. Patient 1, who alternates between routes, ended up smoking cannabis on the day the mobile lab was scheduled to draw levels at 2 h later. Therefore, patient 1’s plasma concentrations are not representative of the true maximum.
The post-dose level, which is intended to represent the maximum plasma cannabinoid concentration, should be collected at approximately 30 min after smoked cannabis and 2 h for edible formulations [6]. Patient 1, who alternates between routes, ended up smoking cannabis on the day the mobile lab was scheduled to draw levels at 2 h later. Therefore, patient 1’s plasma concentrations are not representative of the true maximum.
Table 2.
Plasma concentrations of cannabinoids and relevant metabolites obtained from blood samples of 3 ADHD patients self-medicating with cannabis
Discussion/Conclusion
We describe 3 patients with ADHD who added cannabis to their treatment regimen and experienced positive therapeutic effects. The improvements in their symptoms and quality of life were substantial, such as the ability to keep emotions in check (3 patients) or to obtain and excel at a new job with more responsibility (2 patients). Objective measures accompanied these narratives with all 3 patients experiencing improvements in validated rating scales for measures of mental health. Scores on the PHQ-9, which measure depression, improved by 8–22 points (30–81%). Improvements on the SCARED, which measure anxiety, ranged from 0 to 27 (up to 33%), and the CEER-9 scale, which indicates emotional regulation, ranged from 2 to 7 (22–78%). Finally, the 9-item SNAP scale measuring inattention showed improvements ranging from 2 to 8 points on the raw scale, which equated to 7–30%.
Scores on the PHQ-9, which measure depression, improved by 8–22 points (30–81%). Improvements on the SCARED, which measure anxiety, ranged from 0 to 27 (up to 33%), and the CEER-9 scale, which indicates emotional regulation, ranged from 2 to 7 (22–78%). Finally, the 9-item SNAP scale measuring inattention showed improvements ranging from 2 to 8 points on the raw scale, which equated to 7–30%.
Notably, all 3 patients used cannabis as an adjunct to their other medications (e.g., stimulants, antidepressants, or mood stabilizers). Patient 1 described cannabis as “a really good helping hand” to compliment his other medications. Patient 3 was able to discontinue his stimulant pharmacotherapy, but acknowledged that the “cannabis, in addition to a change in prescription medications to lithium, helped to change his life.” Plasma levels of the cannabinoids were not detectable at trough levels suggesting that the effects of the cannabis may not be sustained throughout the day; however, the patients perceived the effects of the cannabis to last throughout the day. This bespeaks to the importance of the other medications to ensure treatment success.
This bespeaks to the importance of the other medications to ensure treatment success.
All 3 patients discussed the use of cannabis with their psychiatrist and were authorized oral cannabidiol oil CBD:THC (20:1) from a medical source. Our patient interviews and accompanying blood levels, however, indicated that this route and formulation was not consistent, and that the patients sought out a product and regimen that worked for them. Two patients reported taking cannabis once daily, whereas the other patient preferred a twice daily regimen. Two patients preferred smoking cannabis (as opposed to an edible oil). With respect to chemical composition, 1 patient preferred a product high in THC and low in CBD (CBD:THC 0:18–19). Another patient reported using CBD:THC 20:1, but high amounts of THC and no CBD were detected in the post-dose sample, which brings into question the contents of product used by the patient. The use of cannabis is also complicated by the dual supply streams in Canada.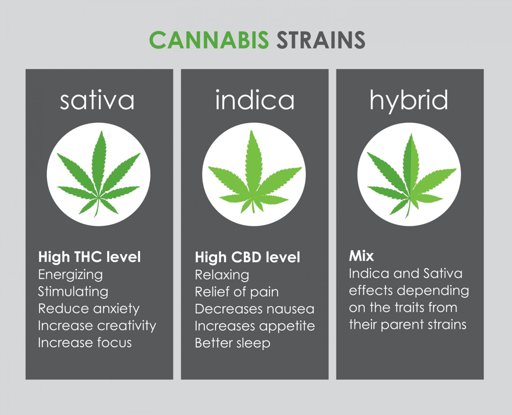 Two patients obtained their cannabis from a recreational cannabis store, versus a medical source due to significant cost differences (double the price for medical cannabis). Unlike other medications, patients are freely available to choose their cannabis product and source. Even within the same source, batch to batch variation is expected, which contributes to significant inter- and intrapatient variability with cannabis-based medicine.
Two patients obtained their cannabis from a recreational cannabis store, versus a medical source due to significant cost differences (double the price for medical cannabis). Unlike other medications, patients are freely available to choose their cannabis product and source. Even within the same source, batch to batch variation is expected, which contributes to significant inter- and intrapatient variability with cannabis-based medicine.
An increasing number of patients are self-medicating with cannabis for the treatment of ADHD. Yet, a dearth of literature exists on this topic, and only 2 other published case reports of patients receiving benefits from cannabis were found in the literature. One publication from 2008 reported improvement in performance tests (ART2020 and TAP) in an adult male smoking cannabis, suggesting that THC may have atypical effects in patients with ADHD [27]. A second case report in 2018 described improved symptoms in an ADHD patient who was taking a product high in THC [28]. Although the potential mechanism of cannabis remains to be determined, cannabinoids, such as THC, may mediate their effects through induction of dopamine release in the human striatum [28, 29]. Elucidating such mechanisms will be particularly challenging since the biochemical composition of cannabis (e.g., phytocannabinoids, terpenes, and flavonoids) varies from strain to strain. Plasma cannabinoid concentrations of 2 of the patients in the present discussion were high in THC (with no CBD), while the other patient had higher CBD concentrations, but THC was still present. In the previous literature, products high in THC or containing both THC and CBD ameliorated ADHD symptoms [15, 27, 28]. While we cannot draw any conclusions on the optimal ratio of CBD:THC, we suggest that future studies involve a product consisting of some amount of THC (instead of a product consisting only of CBD).
Although the potential mechanism of cannabis remains to be determined, cannabinoids, such as THC, may mediate their effects through induction of dopamine release in the human striatum [28, 29]. Elucidating such mechanisms will be particularly challenging since the biochemical composition of cannabis (e.g., phytocannabinoids, terpenes, and flavonoids) varies from strain to strain. Plasma cannabinoid concentrations of 2 of the patients in the present discussion were high in THC (with no CBD), while the other patient had higher CBD concentrations, but THC was still present. In the previous literature, products high in THC or containing both THC and CBD ameliorated ADHD symptoms [15, 27, 28]. While we cannot draw any conclusions on the optimal ratio of CBD:THC, we suggest that future studies involve a product consisting of some amount of THC (instead of a product consisting only of CBD).
An important limitation of case reports is their inability to generalize to a wider population given the selection bias, and there is limited information that can be gleaned from these reports of a few selected patients.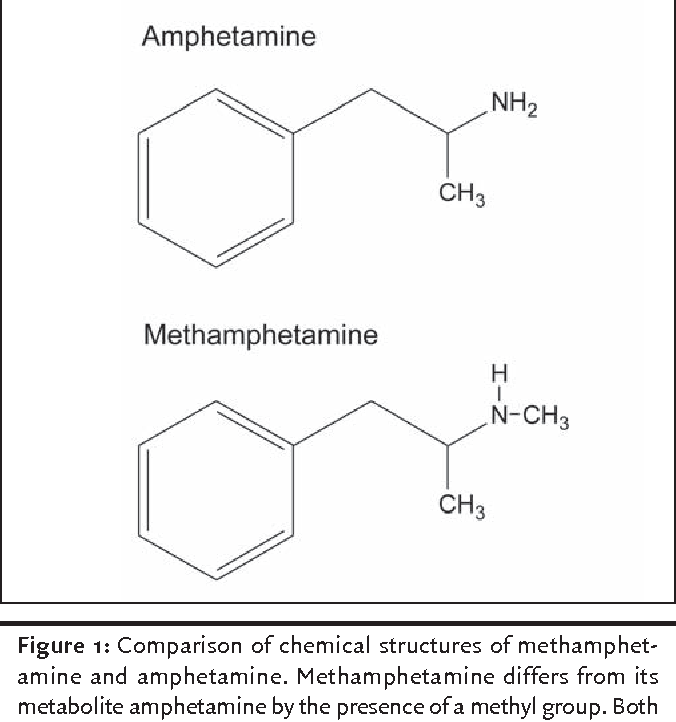 While randomized controlled trials are urgently needed to provide insight on the efficacy of cannabis in the treatment of ADHD, such studies will never be performed with smoked cannabis flower, and we are left to rely on observational data for these exposures. This report adds to the literature by providing detailed personal accounts from 3 patients and objective evidence of improvement on validated measures for ADHD symptoms. Clinicians who care for patients who self-medicate with cannabis should aim to objectively monitor symptoms, using validated scales for ADHD and other comorbidities. The patients presented in this case report were also taking concurrent medications; therefore, the added benefits of cannabis on ADHD symptoms are unclear. Significant variation noted amongst these 3 individuals (e.g., product, chemical composition, dose, route of administration, and supplier) highlights the challenges with cannabis-based medicine development and research.
While randomized controlled trials are urgently needed to provide insight on the efficacy of cannabis in the treatment of ADHD, such studies will never be performed with smoked cannabis flower, and we are left to rely on observational data for these exposures. This report adds to the literature by providing detailed personal accounts from 3 patients and objective evidence of improvement on validated measures for ADHD symptoms. Clinicians who care for patients who self-medicate with cannabis should aim to objectively monitor symptoms, using validated scales for ADHD and other comorbidities. The patients presented in this case report were also taking concurrent medications; therefore, the added benefits of cannabis on ADHD symptoms are unclear. Significant variation noted amongst these 3 individuals (e.g., product, chemical composition, dose, route of administration, and supplier) highlights the challenges with cannabis-based medicine development and research.
Acknowledgments
The authors would like to thank Lorraine Sadler with TLC Mobile Lab and Stephanie Vuong for collection and analysis of blood samples, respectively.
Statement of Ethics
Written informed consent was obtained from patients for publication of the details of their medical case, and ethical approval for data collection was approved by the Biomedical Research Ethics Boards at the University of Saskatchewan (#1726).
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This work was funded by an internal College of Pharmacy and Nutrition Seed Fund Grant.
Author Contributions
H.M. contributed to the research design, data collection, and manuscript writing. D.Q., L.E.K., and J.A. contributed to the research design and reviewed and revised the manuscript.
Data Availability Statement
The data that support the findings of this case report are not publicly available to protect the individual’s anonymity.
This article is licensed under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC). Usage and distribution for commercial purposes requires written permission.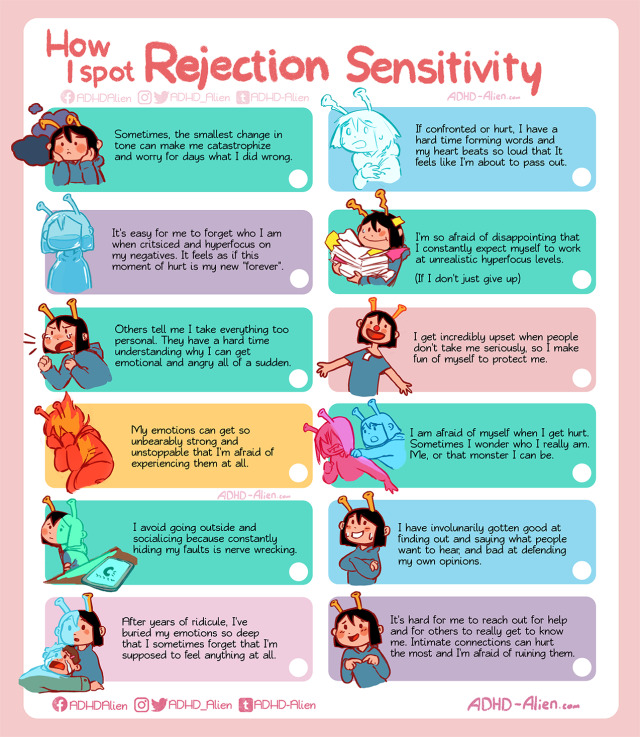 Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any changes in indications and dosage and for added warnings and precautions. This is particularly important when the recommended agent is a new and/or infrequently employed drug. Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor(s). The appearance of advertisements or/and product references in the publication is not a warranty, endorsement, or approval of the products or services advertised or of their effectiveness, quality or safety.
Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any changes in indications and dosage and for added warnings and precautions. This is particularly important when the recommended agent is a new and/or infrequently employed drug. Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor(s). The appearance of advertisements or/and product references in the publication is not a warranty, endorsement, or approval of the products or services advertised or of their effectiveness, quality or safety.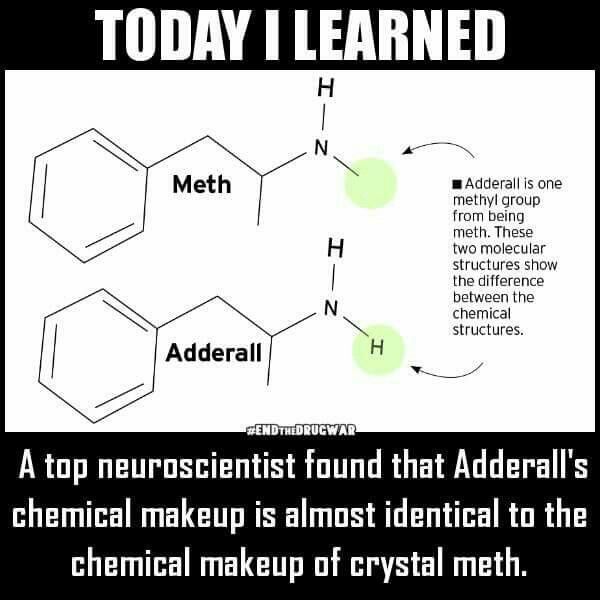 The publisher and the editor(s) disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements.
The publisher and the editor(s) disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements.
CBD for ADHD
We all know someone with ADHD.
Approximately 1 in 20 people worldwide suffer from Attention Deficit Hyperactivity Disorder (ADHD), and most of them are not even aware of it. Take Will Smith, Michael Phelps, Justin Timberlake, Jim Carrey, Michael Jordan, and Cher - they've all publicly announced their ADHD diagnosis without you noticing.
ADHD can cause a number of problems for you at work or for your child at school. Common problems include absenteeism, high error rates, poor concentration, interpersonal conflicts, tardiness, and lack of reliability. And yet, looking at some of the names on the list of the most famous ADHD, it becomes clear that the diagnosis is not a negative trait. Managed well, this can be a blessing. nine0003
Since 2018, interest in CBD for the treatment of ADHD symptoms has skyrocketed. Google Trends data shows that internet searches for 'CBD for ADHD' were in line with growing interest in 'side effects of ADHD medications'. Indeed, parents of children with ADHD and adults with ADHD prefer to treat disorders without creating additional problems in the form of mood swings, dizziness, nausea, shortness, and even height changes, according to WebMD.
Google Trends data shows that internet searches for 'CBD for ADHD' were in line with growing interest in 'side effects of ADHD medications'. Indeed, parents of children with ADHD and adults with ADHD prefer to treat disorders without creating additional problems in the form of mood swings, dizziness, nausea, shortness, and even height changes, according to WebMD.
In this article, we'll look at what the science says about taking CBD for ADHD. We'll also look at a promising case study, as well as recommendations for dosage and selection of quality CBD products. nine0003
Contents
The Science of CBD for ADHD
CBD research is still in its infancy. According to Children and Adults with Attention Deficit/Hyperactivity Disorder (CHADD), there are only two authoritative studies on the effects of CBD on ADHD. None of the studies are conclusive and one looked at cannabis use rather than CBD.
Here is a breakdown of what they found:
- Cannabinoids for attention deficit/hyperactivity disorder: a randomized controlled trial .
 In this small study, researchers assessed symptom levels in people with ADHD who received CBD medication. Participants noted some improvement in impulsivity and hyperactivity, but almost no change in cognitive function or reduction in symptoms. The study authors emphasized that participants did not follow instructions to avoid other drugs or alcohol, which could have affected the results. nine0030
In this small study, researchers assessed symptom levels in people with ADHD who received CBD medication. Participants noted some improvement in impulsivity and hyperactivity, but almost no change in cognitive function or reduction in symptoms. The study authors emphasized that participants did not follow instructions to avoid other drugs or alcohol, which could have affected the results. nine0030 - Effects of ADHD and cannabis use on executive function in young adults. This study showed poor cognitive function later in life in young people using cannabis before the age of 16, including people diagnosed with ADHD. Participants scored low on tests of working memory, verbal memory, decision making, and retention. The authors of the study did not consider CBD however with low THC levels.
While the latest study may put parents off, it's worth noting that CBD is nothing but marijuana. Cannabis sold on the street can have up to 40% THC content - compared to the legal limit of 0. 2% for CBD products in the US, UK and EU and Switzerland. One Study Comparing THC to CBD in 19In the 1980s, they found that THC consumption made participants feel "weak", "withdrawn" and "alarmed", while CBD made participants feel "sharp", "clear" and "calm".
2% for CBD products in the US, UK and EU and Switzerland. One Study Comparing THC to CBD in 19In the 1980s, they found that THC consumption made participants feel "weak", "withdrawn" and "alarmed", while CBD made participants feel "sharp", "clear" and "calm".
However, CHADD conclude their synopsis of CBD for ADHD research with the words of Joe Mitchell, PhD:
find strong support to say, "yes, this should be the cure." When people say CBD works for ADHD, it goes way beyond the data. It's too big a jump." nine0003
Research is ongoing (for example, NYU is currently looking for 7-17 year olds with ADHD and autism to investigate CBD as a cure), and we hope to have more updates soon.
Find out more about CBD healing properties here.
Anecdotal evidence - a case study of CBD for ADHD in children
Despite the lack of scientific evidence supporting CBD for ADHD, interest is still high. This case study published on Scary Mommy covers all the side effect issues and potential benefits of treating ADHD with CBD. The story is:
The story is:
- Concerned parents diagnose their six-year-old son with ADHD and AKI after episodes of anger and aggression.
- Their child's doctor offers a combination of play therapy, medication and occupational therapy.
- Parents wanted to help their son but were concerned about the 'addictive trend' associated with Adderall's recommended drug.
- Parents have acknowledged the limitations of research on CBD for ADHD, although there have been studies demonstrating the benefits of CBD for childhood epilepsy and anxiety. nine0030
- The situation came to a head when the six-year-old son began to influence the couple's three-year-old son.
- The parents decided to try CBD oil for both boys by purchasing a bottle of low quality CBD oil from the grocery store.
- With the first sublingual drop of CBD oil, both boys slept through the night for the first time in months.
- Brennden, a six-year-old child, is now taking 2 vials of 500 mg.
 CBD oil three times a day (sublingually) and Junior, a three year old, takes 2 ampoules of 1000mg. CBD oils twice a day. nine0030
CBD oil three times a day (sublingually) and Junior, a three year old, takes 2 ampoules of 1000mg. CBD oils twice a day. nine0030 - Brenden hasn't stopped taking Adderall as it helps him focus even though he takes less.
- Through the combination of Adderall and CBD therapy, however, parents have seen improvements in their children in the following areas: better sleep, more balanced mood, healthier appetite, better eating habits, fewer tantrums, better concentration at school, academic growth, and healthier relationships with friends , brothers and sisters.
This case study reflects the American Academy of Pediatrics (AAP) recommendations recommending that children aged 6 to 18 years be treated with FDA-approved medications along with therapy and a broader support plan. nine0003
Dosage - how much CBD should I take for ADHD?
In the example above, 1000mg CBD oil typically means 10% strength for the most common 10ml bottle size. 500mg CBD The oil mentioned above should be 5% ABV in a 10ml bottle. According to generally accepted recommendations, you can inject 20 drops of 1 ml and the recommended dose. A serving of CBD oil is 3-6 drops. Provided that Branden takes 3-6 drops of 5% concentration. CBD oil three times a day, this would mean a dose of 22.5 to 45 mg of CBD per day. nine0003
According to generally accepted recommendations, you can inject 20 drops of 1 ml and the recommended dose. A serving of CBD oil is 3-6 drops. Provided that Branden takes 3-6 drops of 5% concentration. CBD oil three times a day, this would mean a dose of 22.5 to 45 mg of CBD per day. nine0003
According to the Open Access Government, the recommended allowance for children is 2.5 to 10 mg per day for optimal effect. However, there is no known limit beyond which a child can overdose. CBD, In fact, 2019 study on CBD for epilepsy in children The recommended daily dose is 10-12mg CBD per kg. For a six-year-old child weighing around 20 kg, this could mean up to 240 mg of CBD per day. The study showed that this dose dramatically reduced seizures without intoxication in children aged 1 to 10 years. nine0003
While the lack of scientific advice can be confusing, especially for parents, it means that CBD dosages can be experimented with and tailored to suit each individual's needs.
Side effects of CBD for ADHD
CBD has a number of known side effects.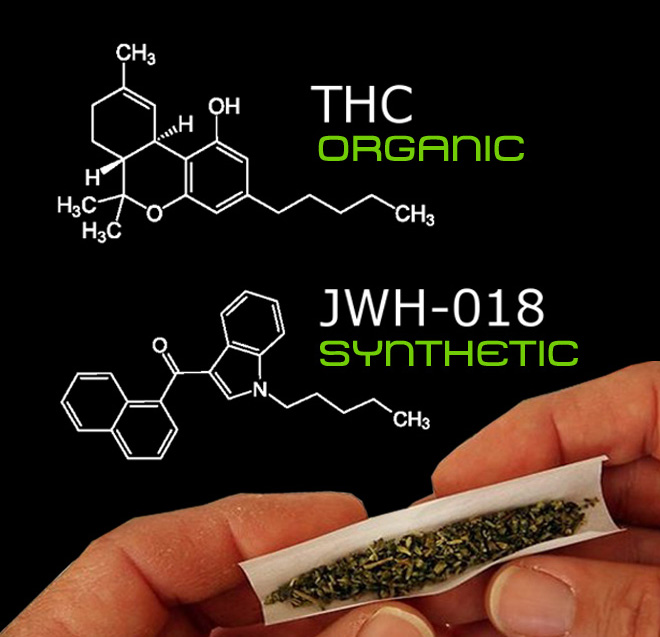 These may include:
These may include:
- Dry mouth
- Fatigue
- Change in appetite
- Low blood pressure
- Diarrhea (often caused by carrier oil)
- Dizziness
At the same time, many scientific studies have examined the risks of growth changes in children taking medication for ADHD. The Addiction Center also reads that conventional ADHD medication Adderall carries a "high risk" of addiction and abuse. While CBD is not known to cause serious side effects such as toxicity or addiction, it is worth recognizing the side effects. You can read more about CBD medicinal properties and side effects here. nine0003
Another problem is the interaction between CBD and other drugs. For example, certain medications known as "prodrugs" can cause complications with CBD. Lisdexamphetamine (brand name Concerta) is an ADHD medication and a "prodrug" that must be metabolized into therapeutic compounds in the liver before it can have a beneficial effect. Taking CBD however may inhibit the amount of active drug compounds that become available in the body. You can read more about CBD and drug interactions here. nine0003
Taking CBD however may inhibit the amount of active drug compounds that become available in the body. You can read more about CBD and drug interactions here. nine0003
Closing Words
Since scientific research has not yet reached a definitive conclusion on taking CBD for ADHD – especially in children – any advice is inappropriate here. Medical guidelines suggest that people with ADHD should not think of CBD as a substitute for other medications. Anyone thinking of taking CBD for ADHD or for their child should check with their doctor or physician.
Sign up and get 20% off your first CBD oil order! nine0019
Get 20% off the best organic CBD oil! Just register and subscribe to our newsletter. Your 20% discount code will be emailed in a few seconds.
CBD for ADHD
We all know someone with ADHD.
Approximately 1 in 20 people worldwide suffer from Attention Deficit Hyperactivity Disorder (ADHD), and most of them are not even aware of it. Take Will Smith, Michael Phelps, Justin Timberlake, Jim Carrey, Michael Jordan, and Cher - they've all publicly announced their ADHD diagnosis without you noticing. nine0003
Take Will Smith, Michael Phelps, Justin Timberlake, Jim Carrey, Michael Jordan, and Cher - they've all publicly announced their ADHD diagnosis without you noticing. nine0003
ADHD can cause a number of problems for you at work or for your child at school. Common problems include absenteeism, high error rates, poor concentration, interpersonal conflicts, tardiness, and lack of reliability. And yet, looking at some of the names on the list of the most famous ADHD, it becomes clear that the diagnosis is not a negative trait. Managed well, this can be a blessing.
Since 2018, interest in CBD for the treatment of ADHD symptoms has skyrocketed. Google Trends data shows that internet searches for 'CBD for ADHD' were in line with growing interest in 'side effects of ADHD medications'. Indeed, parents of children with ADHD and adults with ADHD prefer to treat disorders without creating additional problems in the form of mood swings, dizziness, nausea, shortness, and even height changes, according to WebMD.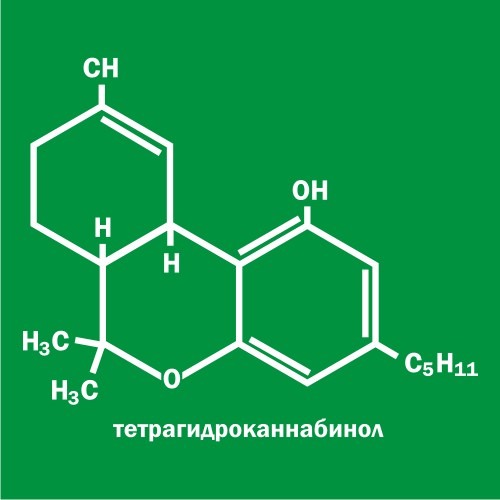 nine0003
nine0003
In this article, we'll look at what the science says about taking CBD for ADHD. We'll also look at a promising case study, as well as recommendations for dosage and selection of quality CBD products.
Contents
The Science of CBD for ADHD
CBD research is still in its infancy. According to Children and Adults with Attention Deficit/Hyperactivity Disorder (CHADD), there are only two authoritative studies on the effects of CBD on ADHD. None of the studies are conclusive and one looked at cannabis use rather than CBD. nine0003
Here is a breakdown of what they found:
- Cannabinoids for Attention Deficit/Hyperactivity Disorder: A Randomized Controlled Trial . In this small study, researchers assessed symptom levels in people with ADHD who received CBD medication. Participants noted some improvement in impulsivity and hyperactivity, but almost no change in cognitive function or reduction in symptoms.
 The study authors emphasized that participants did not follow instructions to avoid other drugs or alcohol, which could have affected the results. nine0030
The study authors emphasized that participants did not follow instructions to avoid other drugs or alcohol, which could have affected the results. nine0030 - Effects of ADHD and cannabis use on executive function in young adults. This study showed poor cognitive function later in life in young people using cannabis before the age of 16, including people diagnosed with ADHD. Participants scored low on tests of working memory, verbal memory, decision making, and retention. The authors of the study did not consider CBD however with low THC levels.
While the latest study may put parents off, it's worth noting that CBD is nothing but marijuana. Cannabis sold on the street can have up to 40% THC content - compared to the legal limit of 0.2% for CBD products in the US, UK and EU and Switzerland. One Study Comparing THC to CBD in 19In the 1980s, they found that THC consumption made participants feel "weak", "withdrawn" and "alarmed", while CBD made participants feel "sharp", "clear" and "calm".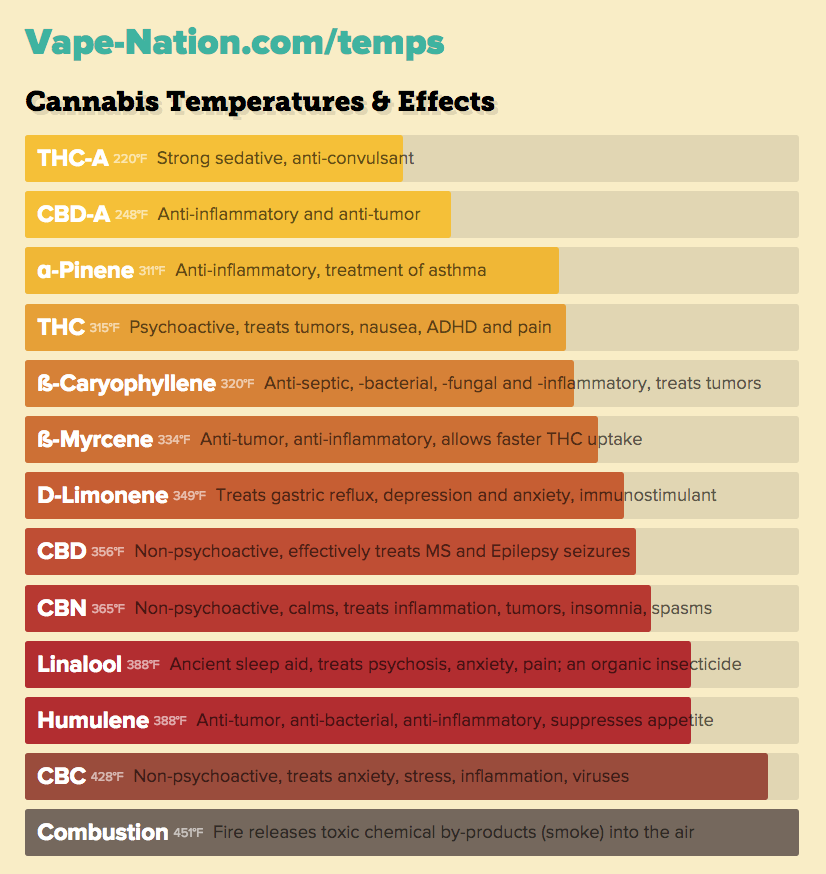
However, CHADD conclude their synopsis of CBD for ADHD research with the words of Joe Mitchell, PhD:
find strong support to say, "yes, this should be the cure." When people say CBD works for ADHD, it goes way beyond the data. It's too big a jump." nine0003
Research is ongoing (for example, NYU is currently looking for 7-17 year olds with ADHD and autism to investigate CBD as a cure), and we hope to have more updates soon.
Find out more about CBD healing properties here.
Anecdotal evidence - a case study of CBD for ADHD in children
Despite the lack of scientific evidence supporting CBD for ADHD, interest is still high. This case study published on Scary Mommy covers all the side effect issues and potential benefits of treating ADHD with CBD. The story is:
- Concerned parents diagnose their six-year-old son with ADHD and AKI after episodes of anger and aggression.
- Their child's doctor offers a combination of play therapy, medication and occupational therapy.
- Parents wanted to help their son but were concerned about the 'addictive trend' associated with Adderall's recommended drug.
- Parents have acknowledged the limitations of research on CBD for ADHD, although there have been studies demonstrating the benefits of CBD for childhood epilepsy and anxiety. nine0030
- The situation came to a head when the six-year-old son began to influence the couple's three-year-old son.
- The parents decided to try CBD oil for both boys by purchasing a bottle of low quality CBD oil from the grocery store.
- With the first sublingual drop of CBD oil, both boys slept through the night for the first time in months.
- Brennden, a six-year-old child, is now taking 2 vials of 500 mg. CBD oil three times a day (sublingually) and Junior, a three year old, takes 2 ampoules of 1000mg. CBD oils twice a day. nine0030
- Brenden hasn't stopped taking Adderall as it helps him focus even though he takes less.
- Through the combination of Adderall and CBD therapy, however, parents have seen improvements in their children in the following areas: better sleep, more balanced mood, healthier appetite, better eating habits, fewer tantrums, better concentration at school, academic growth, and healthier relationships with friends , brothers and sisters.

This case study reflects the American Academy of Pediatrics (AAP) recommendations recommending that children aged 6 to 18 years be treated with FDA-approved medications along with therapy and a broader support plan. nine0003
Dosage - how much CBD should I take for ADHD?
In the example above, 1000mg CBD oil typically means 10% strength for the most common 10ml bottle size. 500mg CBD The oil mentioned above should be 5% ABV in a 10ml bottle. According to generally accepted recommendations, you can inject 20 drops of 1 ml and the recommended dose. A serving of CBD oil is 3-6 drops. Provided that Branden takes 3-6 drops of 5% concentration. CBD oil three times a day, this would mean a dose of 22.5 to 45 mg of CBD per day. nine0003
According to the Open Access Government, the recommended allowance for children is 2.5 to 10 mg per day for optimal effect. However, there is no known limit beyond which a child can overdose. CBD, In fact, 2019 study on CBD for epilepsy in children The recommended daily dose is 10-12mg CBD per kg.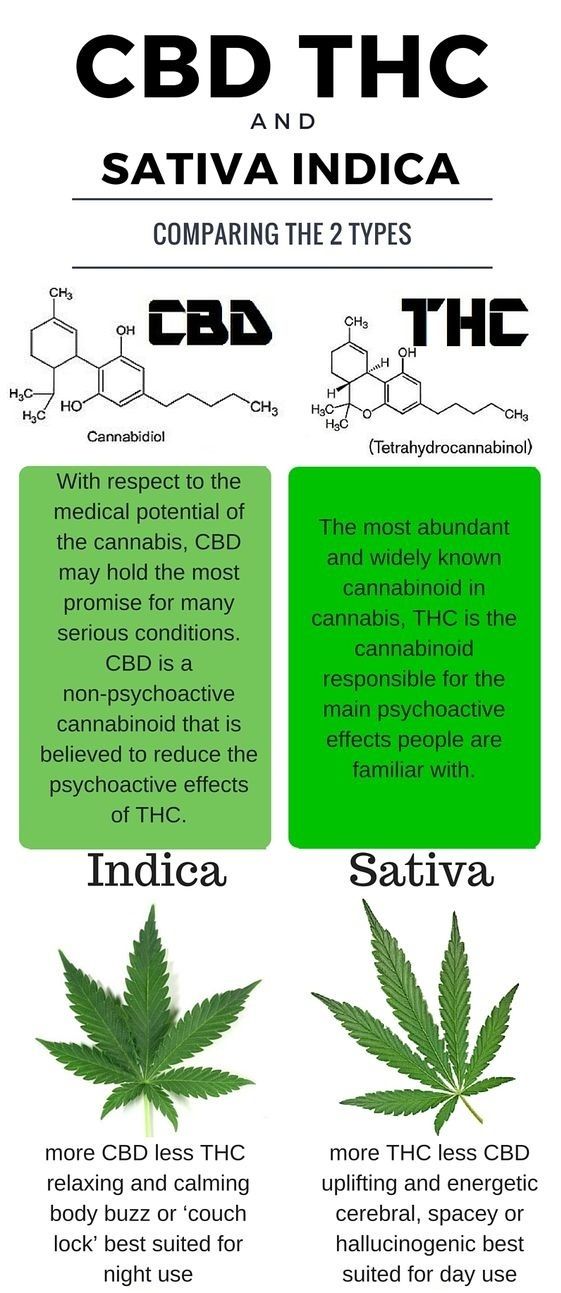 For a six-year-old child weighing around 20 kg, this could mean up to 240 mg of CBD per day. The study showed that this dose dramatically reduced seizures without intoxication in children aged 1 to 10 years. nine0003
For a six-year-old child weighing around 20 kg, this could mean up to 240 mg of CBD per day. The study showed that this dose dramatically reduced seizures without intoxication in children aged 1 to 10 years. nine0003
While the lack of scientific advice can be confusing, especially for parents, it means that CBD dosages can be experimented with and tailored to suit each individual's needs.
Side effects of CBD for ADHD
CBD has a number of known side effects. These may include:
- Dry mouth
- Fatigue
- Change in appetite
- Low blood pressure
- Diarrhea (often caused by carrier oil)
- Dizziness
At the same time, many scientific studies have examined the risks of growth changes in children taking medication for ADHD. The Addiction Center also reads that conventional ADHD medication Adderall carries a "high risk" of addiction and abuse. While CBD is not known to cause serious side effects such as toxicity or addiction, it is worth recognizing the side effects.