What to do when you relapse
9 Steps to Help You Get Back on Track and Sober
Clinically reviewed by Sarah Fletcher, LPC, LAC
- How Do You Get Back On Track After A Relapse?
- What Is A Relapse?
- What Are The Stages Of Relapse?
- What Is An Emotional Relapse?
- What Is A Mental Relapse?
- What Is A Physical Relapse?
- How To Detox After A Relapse
- What Is The Addiction Recovery Process Like After A Relapse?
- What Is Relapse Prevention?
How Do You Get Back On Track After A Relapse?
After a relapse, you can get back on track by realizing that relapsing is just a setback in your addiction recovery.
You might feel like you failed after a relapse. You might feel like you let your loved ones down. You might struggle to get back on track because you feel that relapsing means that recovery and sobriety are not meant for you.
You might feel hopeless after a relapse or that getting better is impossible for you.
Addiction and relapse might make you feel like no one else shares your issues or understands what you are going through. Just like when you first got into treatment, remember that you met others struggling with addiction like you.
To get back on track after an addiction relapse, go easy on yourself. Remember that long-term sobriety is a process and not an end goal. Every long-term process will have setbacks along the way.
Addiction recovery is hard, which is why many avoid facing their issues. But you went through the process and faced your challenges. There is no shame in having a setback. Now, you can come back better than before.
Shame and self-blame will not be helpful after a relapse. Admit that a relapse happened and work towards figuring out what caused your relapse.
Life, for better or worse, continues during your addiction recovery process.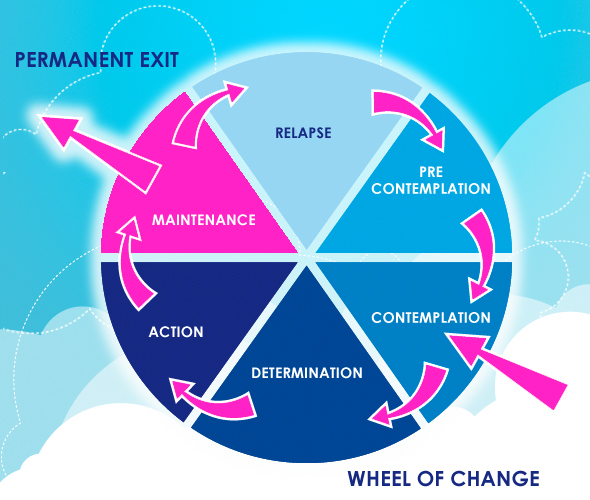
Maybe you were doing great, and then an unexpected life event threw you off the right path. You might lose a loved one, lose your job, go through a breakup, or another life event. A natural and unexpected event, like a pandemic or a hurricane, might uproot your entire life.
Sometimes, life is going great for a long time. Sobriety is easy. Then, you get bad news, and suddenly, you feel triggered. You go back to using or drinking as a way to cope with the unexpected. Suddenly, you are right back to where you were before you began recovery.
Other times, you follow all the rules of recovery for a long time, and you feel safe from relapsing.
You have been following your recovery plan for years. You have been sober and drug-free for a long time. You might stop going to support groups or stop making time for self-care. You feel like you are “cured” of your substance use disorder.
Many people relapse following long-term sobriety because they feel like they conquered their addiction. They feel like they can go back to using substances again because they won’t get addicted. Not again, they are cured.
They feel like they can go back to using substances again because they won’t get addicted. Not again, they are cured.
You might fall into this mindset. Success can make you feel invincible. However, addiction is a disease, and you are still vulnerable to relapsing.
Whether you have been sober for 20 years or one month, drug and alcohol addiction are never really “cured.”
It would be best if you thought about relapse prevention, even when things are going well. Continue to take care of your mental health, attend support groups, and look out for other addictive behaviors.
Sometimes, relapsing might be a change from alcohol or drug addiction to another addictive behavior.
You might be sober and drug-free, but now you are gambling, eating, or working in excess. Relapse does not always mean a return to alcohol or substance abuse.
You can get back on the right path by reaching out for help.
You might need to go back to your support system and admit that you need treatment again.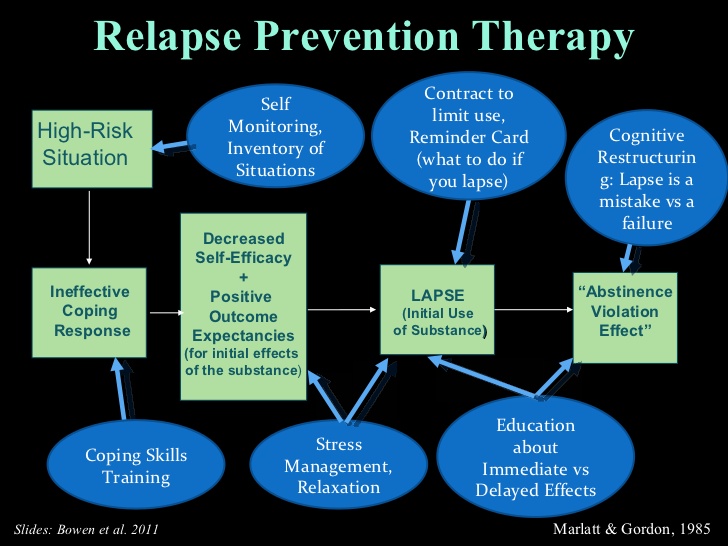 You might feel like you let your loved ones down. You might feel like you failed.
You might feel like you let your loved ones down. You might feel like you failed.
But, if you relapse, go easy on yourself. You are human and will make mistakes. Get help today and learn from your mistakes to prevent future relapses.
Knowing what a relapse is will help you understand when you or a loved one are in the middle of one. Being aware of relapse behaviors in earlier stages will help you prevent relapse from getting worse.
What Is A Relapse?
A relapse is a return to using harmful coping skills while in addiction recovery.
You might believe that relapse is a return to the same addictive behaviors that you have faced before. For example, if you had an addiction to opioids, a relapse is a return to using those same drugs.
Relapse can be trading one addiction for another. For example, you might be drinking instead of using illicit drugs. You might also engage in addictive behaviors that can be just as harmful as substance and alcohol abuse.
Relapse can be any use of addictive behaviors to cope with stress and mental health issues.
Maybe you are working late to avoid problems at home. Or you spend all your after-work hours at the gym instead of going to the bar.
Any of the following addictive behaviors can be as harmful as alcohol or substance abuse:
- Technology addiction, like the internet, social media, phones, and video games
- Overeating
- Excessive exercise
- Becoming a “workaholic”
- Sex and porn addiction
- Gambling
Using these behaviors as a way of coping can be a relapse, even if you aren’t using drugs or alcohol again.
Remember that addiction is often the result of coping with an underlying mental health issue.
A relapse occurs when you find yourself no longer following your treatment program. You stop using healthy coping skills. You start avoiding dealing with life on life’s terms.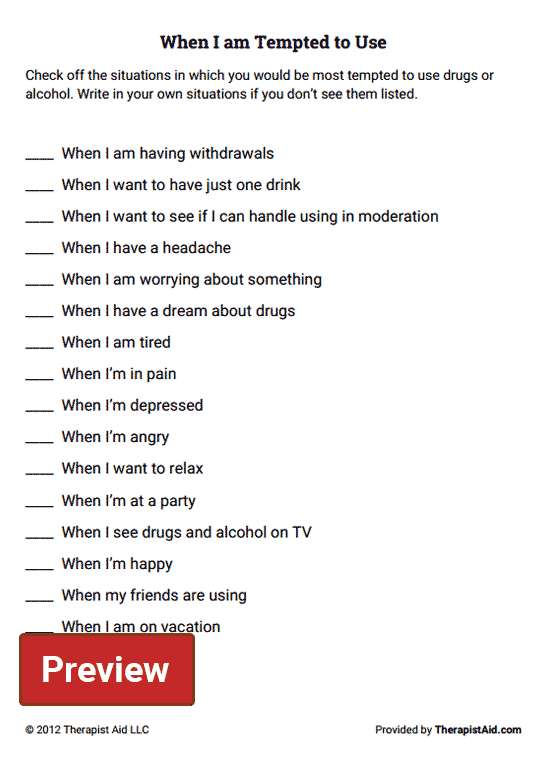
Addiction treatment is not a cure. Addiction recovery means that you take things one day at a time. When you find yourself avoiding problems, or you stop doing healthy self-care activities, you might be on your way to a relapse.
When you stop following your recovery plan, you need to figure out what’s happening. Do you need a change in your treatment plan? Are you dealing with something new, and your coping skills aren’t helpful?
Sometimes, you can intervene in a relapse before things get out of control. Depending on what stage of relapse you are in, you can get help before finding yourself dealing with drug or alcohol addiction again.
What Are The Stages Of Relapse?
Relapse occurs in three stages: emotional, mental, and physical.
When you are aware of the different stages of relapse, you can get out ahead of a full-blown relapse. You might be able to catch your relapse in the early stages.
What Is An Emotional Relapse?An emotional relapse occurs when you are not even thinking about using alcohol or substances but are also not taking care of your emotional health.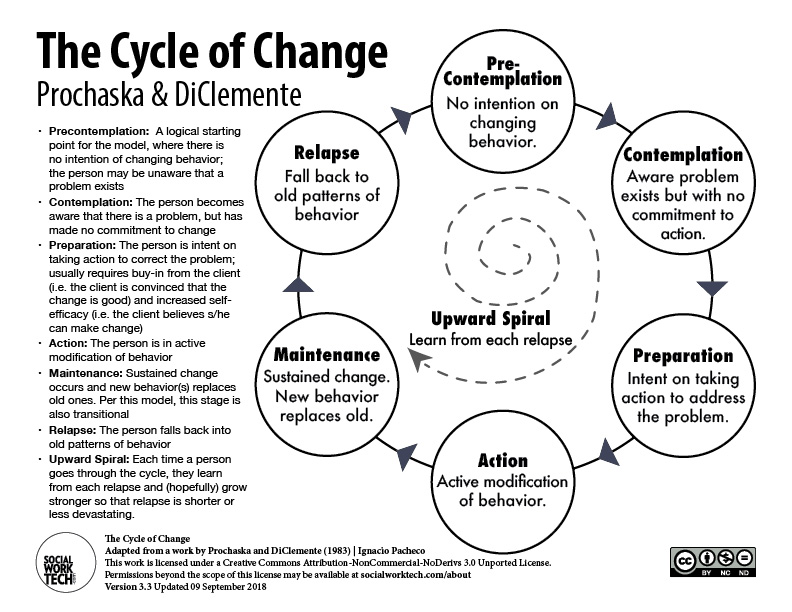
During this stage, you are not using, and you are maintaining your sobriety. You are following the rules of recovery, but only on the surface. You might be “going through the motions.”
In this stage, you continue to follow your recovery plan. You are attending alcoholics anonymous and other 12-step meetings regularly. You stay away from drugs and alcohol and avoid triggering situations.
But you aren’t speaking during meetings. You aren’t talking about what is really going on in your life. You are closed up or in denial of any emotional issues.
During the emotional stage of relapse, you might be:
- Focusing on other people’s problems, but not your own
- Bottling up your emotions
- Not doing basic self-care activities, like proper sleep, healthy eating, or regular exercise
- Skipping meetings or not sharing if you do go
If you notice these behaviors, reach out for help. You can get back on track more easily during this stage of relapse.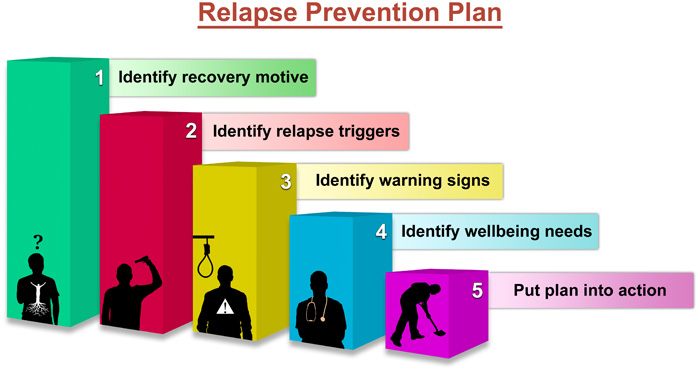
Maybe a family member loved one, or other people in your support network address a concern to you. Remember that they might notice things that you are not aware of yet.
What Is A Mental Relapse?
A mental relapse is when you start thinking about using or going back to your addictive behaviors.
You start thinking about using drugs or alcohol. You might even bargain with yourself in your own head: I’ve been good; I can have just one drink. During a mental relapse, you start to have a war within yourself.
Some of the following signs might mean you are in the mental stage of relapse:
- Cravings and urges for drugs or alcohol
- Changing your thinking about the negative effects of your drug or alcohol addiction:
- It wasn’t so bad
- I really had a lot of fun, and I miss that
- Nothing too bad happened; everyone else overreacted and made me change
- Glorifying past experiences with alcohol or substance abuse
- Thinking about places and people associated with your alcohol or substance abuse
- Lying to others about skipping 12-step meetings or about not following other rules of recovery
- Planning how you can drink or use drugs without getting caught
- Looking for an excuse to use again
You cannot win this battle without reaching out for help. You cannot deny the power of cravings and urges. If you keep these thoughts to yourself, you are in danger of physical relapse.
You cannot deny the power of cravings and urges. If you keep these thoughts to yourself, you are in danger of physical relapse.
What Is A Physical Relapse?
Physical relapse is when you begin using substances or alcohol again.
The physical stage of relapse is what you might have always defined as a relapse. You might define this as a “true” relapse. But, if you understand that relapse can occur in earlier stages before actually drinking or using, you can prevent a physical relapse.
A physical relapse can be a brief “slip.” You might be at a party, and you have a drink to celebrate.
While just one drink might not seem like a big deal, this can lead to thinking, “I can handle just one.” Then, you find yourself drinking again, but slowly and in control. You might think, “It’s different this time.”
But, as time goes on, you find yourself back to where you were before you started addiction recovery in the first place.
Remember that after a physical relapse, recovery is not hopeless. You might just need additional coping skills for long-term sobriety. You can learn from your mistakes and get back on the right path.
How To Detox After A Relapse
Detox after a relapse can be easier than your first detox because now you know what to expect.
But, if you had a painful experience detoxing the first time, you might avoid addiction treatment for your relapse.
Withdrawal symptoms from substance or alcohol abuse can vary. Your detox after relapse depends on how long your relapse has occurred and how much you used.
Now, you have experience with detox and treatment. You might remember some things that were helpful the first time. Or, you might have ideas about what could have made the process easier.
Talk to your primary healthcare provider about the best way to detox after a relapse.
Your doctor might make a referral to a detox center. If you have gone to an addiction treatment provider in the past, they might have suggestions and options for alumni of their treatment program.
If you have gone to an addiction treatment provider in the past, they might have suggestions and options for alumni of their treatment program.
Detox alone at home is never recommended for those diagnosed with alcohol or substance use disorders.
It would be best to look into detox at an inpatient treatment center for additional support and medical help. Medical staff and other support people can help you deal with the physical and mental withdrawal symptoms.
Withdrawal after relapse can be unpleasant to think about. You might have bad memories of how hard detox was. You might remember how painful your withdrawal symptoms felt.
Remember that you have been through this before and can get through it again.
Now that you have been in addiction recovery, you likely have a strong support network to help you through. When you first began addiction treatment, you might have had no coping skills and very little support.
Following a relapse, you most likely have a support system, self-help skills, and experience that can help you get back on track quickly.
What Is The Addiction Recovery Process Like After A Relapse?
The addiction recovery process after a relapse might be easier than early recovery.
After a relapse, you know what works and what does not work in recovery. You have experience in addiction treatment. Now, you have a better sense of your triggers, know who you can go to, and what you can do.
Unlike your first stay at a treatment center, now you know how to get on the right track. You also know that you can get on the right path.
You’ve done this before, and you will get through it again.
Overcoming substance and alcohol use disorder is difficult. You might have been sober after treatment for three months before a relapse. Or maybe you have been sober for years before relapsing.
No matter what, you’ve proven that you can do this.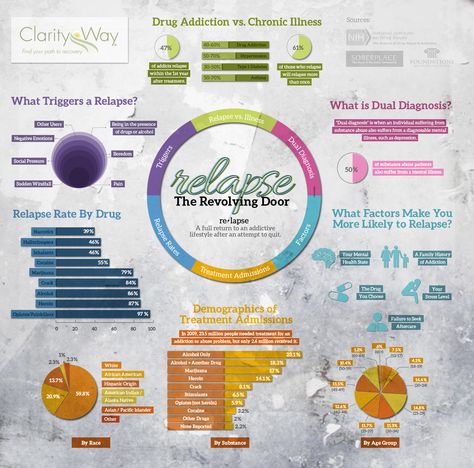 Relapse is a setback and a learning experience to get better through your addiction recovery process.
Relapse is a setback and a learning experience to get better through your addiction recovery process.
During your first stay at a treatment center, you might not have thought about future relapses. You might have been focused on just getting sober and getting out of treatment. After relapsing, you can create a more effective relapse prevention plan.
Look back on what caused your relapse. Could you have prevented a physical relapse by paying attention to your emotional and mental health? Did you find yourself going back to triggering people and places after feeling “cured” of your addiction?
Relapse is an opportunity to come back better and stronger than before.
What Is Relapse Prevention?
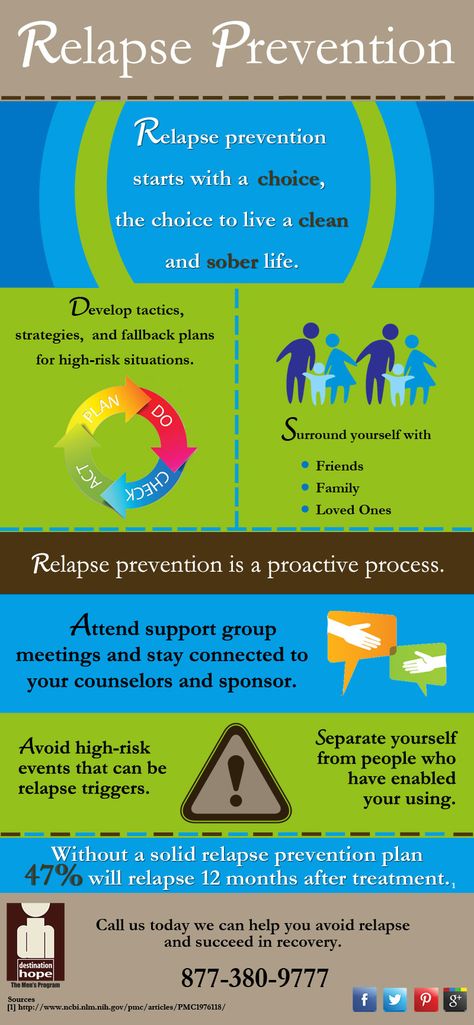
Relapse prevention means looking at your recovery plan as a way of preventing future relapses.
You might consider addiction treatment as a way of learning relapse prevention. After all, you are trying to learn healthy ways of living without alcohol or drug use during treatment.
You and your family members can work on relapse prevention during your treatment by focusing on your discharge planning while you are in a treatment center.
According to the Partnership to End Addiction, effective discharge plans include the following:
- Continuing outpatient therapy services
- Treatment for underlying mental health issues, including psychiatric care and medication
- Involving family members in your support system and treatment planning
- Getting into a social support group, such as:
- 12-Step Meetings, like Narcotics or Alcoholics Anonymous
- SMART Recovery
- Support groups for other addictive behaviors, like video games or gambling
- Creating structure and accountability:
- How will you and your loved ones hold you accountable for your recovery?
- How often will you attend therapy, support group meetings, and other activities to keep you on the right path?
- Planning for a future relapse:
- What are your warning signs of alcohol or drug abuse?
- What should your family members do if you deny treatment while under the influence?
- Who is in your support network that you can count on if you do relapse?
- What are your preferred treatment options in the event of relapse?
- Create a safe and supportive home environment to reduce the chances of relapse
Don’t wait to create a relapse prevention plan. You might be in denial of the possibility of a future relapse. Addiction, like all chronic diseases, carries the risk of relapse.
You might be in denial of the possibility of a future relapse. Addiction, like all chronic diseases, carries the risk of relapse.
According to the National Institute on Drug Abuse (NIDA), relapse rates for substance use disorders are 40-60%.
While this might seem high or make you think that treatment doesn’t work, this rate is actually low compared to other chronic diseases.
By taking proactive steps and understanding the stages of relapse, you and your loved ones can prevent a relapse from occurring or becoming dangerous.
Relapse is not a sign of failure. Instead, you can learn what to do better as you continue your addiction recovery. Sandstone Care is here to treat young adults and teens with substance use disorders and co-occurring mental health issues. Call us today at (855) 958-5511.
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.

Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.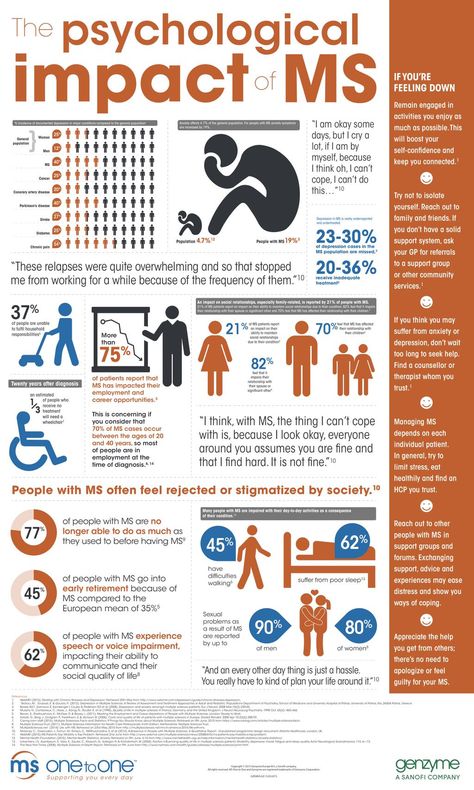
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.
Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
00215. Clinics
Reading time - 10 minutes
Leukemia is also called blood or leukeosis. This is an extensive group of diseases that involves malignant changes in the hematopoietic system. Pathology can appear at any age. According to the rate of progression, leukemias are chronic or acute, and according to the type of cells - lymphocytic or myeloid. Options for dealing with the disease are varied. However, the cancer may return after treatment. Relapse of leukemia is the recurrence of the disease after remission. This often happens with many types of leukemia. Find out what measures are taken abroad for recurrent leukemia, how effective the therapy is and where it is better to undergo treatment - find out in our article.
According to the rate of progression, leukemias are chronic or acute, and according to the type of cells - lymphocytic or myeloid. Options for dealing with the disease are varied. However, the cancer may return after treatment. Relapse of leukemia is the recurrence of the disease after remission. This often happens with many types of leukemia. Find out what measures are taken abroad for recurrent leukemia, how effective the therapy is and where it is better to undergo treatment - find out in our article.
Relapse of leukemia in children and adults
Relapse of leukemia can occur after successful treatment in both adult and pediatric patients. The exact causes of disease are unknown. But, some factors increase the risk of blood cancer recurrence. This is resistance to the original methods of struggle and the preservation of cancer cells that could not be detected in time during therapy.
The likelihood of recurrence of leukemia also varies depending on the type of pathology itself. For example:
For example:
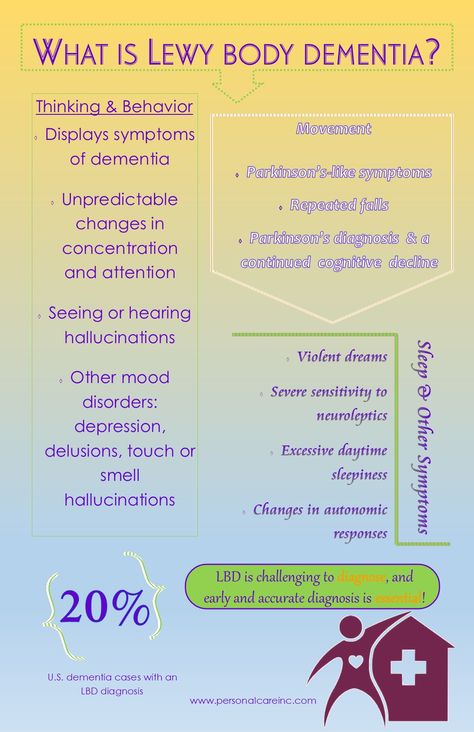
| Acute lymphoblastic leukemia (ALL) | This is a type of leukemia characterized by the production of excessive numbers of immature lymphocytes. The disease mainly affects children. It is one of the most common types of blood cancer in this category of patients. Adults can also suffer from this disease, but less frequently. Relapse of acute lymphoblastic leukemia occurs in 10% of children and 50% of adults. It usually occurs within two years of treatment. |
| Acute myeloid leukemia (AML) | A type of leukemia in which there is an increased number of immature leukocytes in the blood. The disease occurs in adults and children, but in the latter category more often. It is the second most common form of blood cancer in children under 2 years of age and adolescents. Relapse in acute myeloid leukemia develops 2-3 years after treatment. It occurs in half of the patients. |
| Chronic lymphocytic leukemia (CLL) | The disease involves an increased production of immature lymphocytes and their gradual replacement of normal blood cells. She progresses slowly. As a rule, the disease is diagnosed in adults. However, there are cases of the development of the disease in children. Most patients experience a recurrence of CLL within 5 years of starting treatment. |
| Chronic myeloid leukemia (CML) | This pathology implies a violation of the production of leukocytes. It develops slowly and is usually found in older people. More than 60% of patients have CML recurrence after the end of initial therapy. In this case, most cases of recurrence of chronic myeloid leukemia occur in the first six months. |
Each of the above groups has its own subtypes. This is taken into account when developing an oncotherapy program and predicting the effectiveness of treatment. To receive a full-time or remote consultation on the recurrence of leukemia from the best foreign doctors, leave a request on our website. We will help you with the choice of a specialist who is most competent in your matter.
To receive a full-time or remote consultation on the recurrence of leukemia from the best foreign doctors, leave a request on our website. We will help you with the choice of a specialist who is most competent in your matter.
Book an appointment
Symptoms of recurrent leukemia
In leukemia, the bone marrow produces an excess of abnormal immature blood cells. They enter the bloodstream and gradually replace healthy lymphocytes, erythrocytes and leukocytes. This causes the appearance of symptoms of the disease. In case of recurrence of blood cancer, the signs of are similar to the onset of the disease. Among the general symptoms stands out:
elevated body temperature,
Strengthened sweating at night,
Increased lymph nodes,
Frequent infectious diseases,
Head and muscle pain,
Increased fatigue and weakness,
The appearance of bruises and bruises on the body without cause,
Pain in the pain in abdominal area,
loss of appetite,
weight loss.
Leukemia relapse treatment
After initial treatment recurrence of blood cancer may recur soon or after some time. This is an early and late recurrence of leukemia. The choice of methods to combat this pathology depends on the timing of its occurrence and type.
If leukemia recurs early after treatment, the chances of success with a single drug therapy are greatly reduced. In most cases, bone marrow transplantation is indicated for such patients.
All types of recurrent leukemia can be treated with chemotherapy. The intensity of such treatment will be higher than initially. Patients require a combination of several drugs - polychemotherapy . The duration of the treatment program is calculated on an individual basis.
Together with chemotherapeutic drugs, the patient is prescribed additional treatment for the side effects that occur (nausea, vomiting, headache). Medicines are also used to prevent cancer cells from affecting the central nervous system.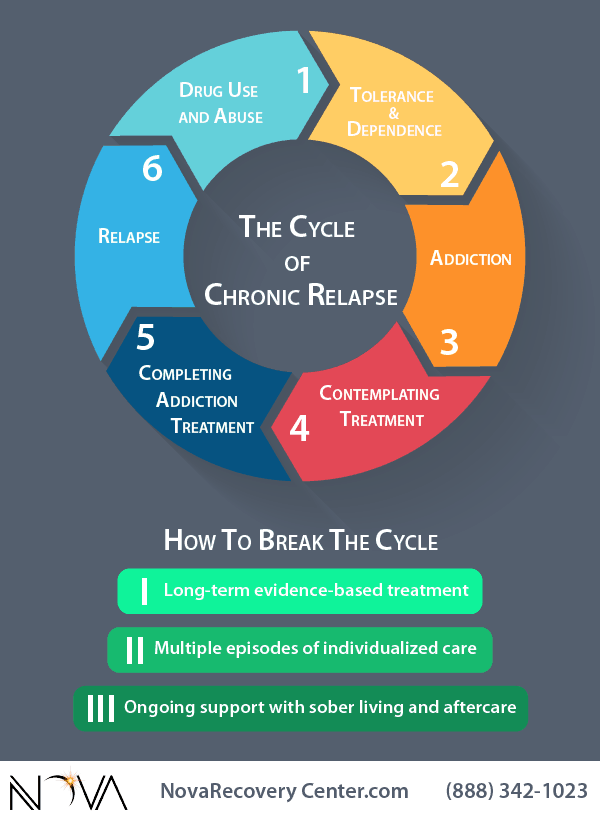
If chemo does not work or is ineffective, patients are recommended a bone marrow transplant. Usually donor material is used for transplantation. Donors can be first-line relatives or unrelated individuals from the Donor Bank.
For some types of acute lymphoblastic leukemia, patients may be given immune therapy , specifically CAR-T cells. Sometimes chemotherapy is combined with radiation. This is necessary to remove metastases in the brain, neck, bones, etc.
Treatment of recurrent leukemia of various types
Treatment involves intensive chemotherapy in several stages . Patients without serious comorbidities may undergo BMT. Targeted or immune therapies may be used to alleviate symptoms.
Treatment includes intensive or non-intensive care. The goal of the first option is to achieve remission, and the second option is to improve the quality of life. Intensive care includes high dose TCM chemo . Non-intensive treatment is less aggressive chemotherapy drugs, as well as immune or targeted therapy.
Non-intensive treatment is less aggressive chemotherapy drugs, as well as immune or targeted therapy.
If CLL recurs several years after initial treatment, the treatment program may not change. These are chemistry, targeted or immune drugs. Some patients will require TCM.
CML relapse is also treated with first or second line chemotherapy drugs in combination with targeted (tyrosine kinase inhibitors) or immune drugs . It is possible to increase the dosage of drugs. If patients develop resistance to these drugs, TCM is recommended.
For the treatment of leukemia in adults or children abroad, please contact the medical coordinators of the international medical platform MediGlobus. We will help you choose the clinic that best suits your needs.
Leave a request
Prognosis of relapse of acute and chronic leukemia
The prognosis for relapse of leukemia differs from the type and severity of oncopathology, duration of remission, general health and age of the patient.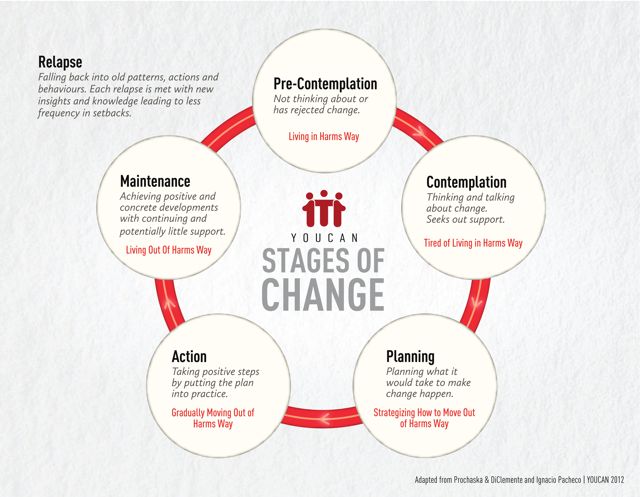 Also, this indicator is influenced by the choice of methods to combat the disease. With relapse of acute lymphoblastic or myeloid leukemia, the prognosis is worse than with the chronic form.
Also, this indicator is influenced by the choice of methods to combat the disease. With relapse of acute lymphoblastic or myeloid leukemia, the prognosis is worse than with the chronic form.
In children, the overall 5-year survival after the first recurrence of ALL is about 50%, and in adults it is about 10%.
For the first recurrence of AML, children show a 5-year survival rate of 40% and adults about 46%.
Thanks to advances in modern medicine, many patients with chronic leukemia can have a good life expectancy, even if they relapse. Overall 10-year survival rates for CLL and CML are estimated at 85% and 80-95% , respectively. At the same time, the best prognosis is demonstrated by patients whose first remission lasted at least three years.
Where is leukemia recurrence treated abroad?
Summary
Recurrent leukemia is the return of blood cancer after successful treatment.
 It appears when not all cancer cells have been destroyed after initial therapy, or if the disease has developed resistance to proven methods of control. The development of recurrence of leukemia in adults and children depends on the type of disease.
It appears when not all cancer cells have been destroyed after initial therapy, or if the disease has developed resistance to proven methods of control. The development of recurrence of leukemia in adults and children depends on the type of disease. The reappearance of leukemia for signs resembles the debut of the disease. The relapse has the following symptoms: fever, frequent infections, weight loss, bruising and bruising on the body, constant fatigue, swollen lymph nodes, headache, muscle weakness, etc.
Treatment of all types of leukemia involves a more intensive program of polychemotherapy. It is also possible to use targeted, immune drugs and radiation therapy. In some cases, after aggressive chemotherapy, patients undergo a bone marrow transplant.
Acute forms of pathology often affect children, and chronic ones - people of mature or old age. The second option has more favorable treatment prognosis. The overall 10-year survival rate for chronic patients is 80-95%.
 With relapse of acute leukemia, the 5-year survival rate is maximum 50%.
With relapse of acute leukemia, the 5-year survival rate is maximum 50%. To go for treatment of leukemia in one of the leading clinics abroad, click on the button below and fill out the feedback form. We will help with the solution of all organizational issues and will be in touch with the patient 24/7.
Leave a request
Oncology
Dr. Vadim Berezhnoy
General practitioner, Medical expert, Head of the department of medical assistance.
Nina Vorobey
Editor
Has been writing medical texts for more than 2 years. Over 6 years of experience in copywriting. He has an education in the direction of "Social and Legal Protection". Mastered the program of medical courses. Learns communication techniques for negotiating with patients. In her free time, she attends trainings and seminars on medical psychology.
Related Posts
How much does adrenal cancer treatment cost abroad?
Read more
Questions for an oncologist: what to do with sigmoid colon cancer
Read more
Is there any hope for stage 4 lung cancer?
Read more
What to do if you have a relapse.
 Step by step action plan
Step by step action plan Relapse is a natural process during treatment for eating disorders
Most people with eating disorders experience a relapse while recovering from their illness. It is important to understand that relapse is the norm and does not mean failure in the recovery process. Instead, relapse should be seen as a normal, natural part of recovery.
People with eating disorders need to view relapse as an opportunity to learn from experience and improve their skills so they know how to handle relapse next time.
How likely is it to relapse?
While most people with eating disorders will relapse as they recover, there are categories with certain risk factors who are more likely to relapse during recovery.
When considering how likely it is to relapse, consider the following:
- The amount of time a person has lived with an eating disorder. The longer the duration of the disease, the higher the likelihood of relapse.
- The age of the person at the onset of their eating disorder. The older the person is at the time of onset, the more likely the disease is to recur.
- Whether the person has previously been treated at a specialized eating disorder clinic. Patients treated at an eating disorder clinic are much less likely to relapse.
- Does the person exercise excessively, even after full recovery.
- Does a person have an increased attention to his body, even after recovery.
- Whether there is low self-esteem or poor ability to interact with others.
- Is it possible for negative and stressful life events to occur.
Specific risk factors for relapse
In addition to the above risk factors, there are also additional data that apply to people with anorexia. The following risk factors have been associated with relapse in patients with anorexia:
- Low body fat in women who have recently regained their weight
- Lower desired weight (when a person wants to have a lower weight even after recovery, the likelihood of relapse is increased)
- Eating low-calorie foods or limiting the variety of foods consumed
If you have a relapse
It is very important not to get frustrated, panic, or drop out of treatment, even when you have a relapse. Do not criticize yourself and do not despair. Believe in yourself! Remember that relapse is a natural process in coming out of an eating disorder.
Do not criticize yourself and do not despair. Believe in yourself! Remember that relapse is a natural process in coming out of an eating disorder.
Although a relapse may feel like a step back, you can still learn a lot from a relapse. For example, you can identify the triggers that caused the relapse, or you can learn new problem-solving techniques that will help you recover faster and easier next time.
If you relapse, these tips can help:
- Remind yourself that relapse is a normal part of recovery. Don't beat yourself up, don't hurt yourself. Remember that you are coming out of a serious psychological, and in some cases medical, addiction. This takes time!
- Try not to obsess over the fact that you're having a relapse. Instead, focus on finding a path back to recovery.
- Get help from your doctors or support circle and don't be afraid to let them know you're having a relapse.
- Try to identify the triggers that caused the relapse and think about how you can deal with those triggers next time.

- Use the coping skills and techniques you learned in the recovery process.
- Boost your self-esteem by spending time in a supportive circle and/or participating in activities you enjoy.
At the Anna Nazarenko Clinic for Eating Disorders, you will receive highly qualified assistance during the recovery process. Restorative therapy specially developed by our specialists will help reduce the number of relapses and, as a result, completely get rid of them.
What is RPP? Causes, Symptoms, Signs and Treatments in 2019
Tags:
What is an Eating Disorder? Types of Eating Disorders Causes of Eating Disorders Signs and Symptoms of Eating Disorders Treatment of Eating Disorders Theses on Eating Disorders
Five irreversible health effects of bulimia
Tags:
Most girls and women are captivated by stereotypes and in pursuit of an ideal appearance and figure are constantly trying to change themselves.