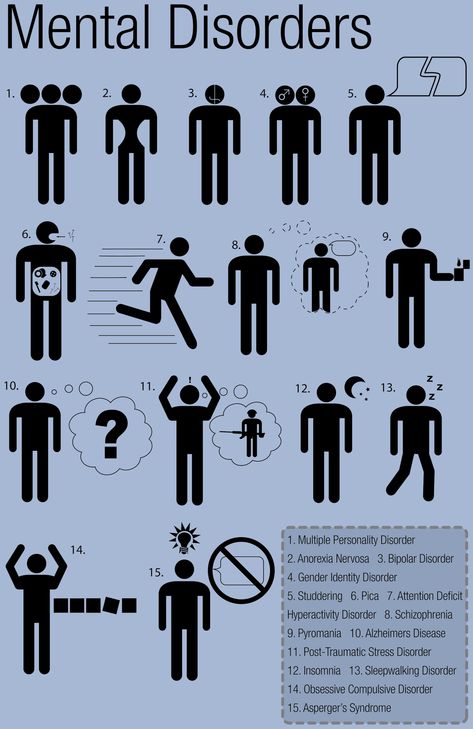
What is multiple personalities
Causes, Symptoms, Types & Treatment
Overview
What is delusional disorder?
Delusional disorder is a type of psychotic disorder. Its main symptom is the presence of one or more delusions.
A delusion is an unshakable belief in something that’s untrue. The belief isn’t a part of the person’s culture or subculture, and almost everyone else knows this belief to be false.
People with delusional disorder often experience non-bizarre delusions. Non-bizarre delusions involve situations that could possibly occur in real life, such as being followed, deceived or loved from a distance. These delusions usually involve the misinterpretation of perceptions or experiences. In reality, these situations are either untrue or are highly exaggerated.
Non-bizarre delusions are different from bizarre delusions, which include beliefs that are impossible in our reality, such as believing someone has removed an organ from your body without any physical evidence of the procedure.
People with delusional disorder often continue to socialize and function well, apart from the subject of their delusion. Generally, they don’t behave in an odd or unusual manner. This is unlike people with other psychotic disorders, who might also have delusions as a symptom. In some cases, however, people with delusional disorder might become so preoccupied with their delusions that their lives are disrupted.
What are the types of delusional disorder?
There are different types of delusional disorder, which are determined based on the main theme of the delusions the person experiences. The types of delusional disorder include:
- Erotomanic: People with this type of delusional disorder believe that another person, often someone important or famous, is in love with them. They may attempt to contact the person of the delusion and engage in stalking behavior.
- Grandiose: People with this type of delusional disorder have an overinflated sense of self-worth, power, knowledge or identity.
 They may believe they have a great talent or have made an important discovery.
They may believe they have a great talent or have made an important discovery. - Jealous: People with this type of delusional disorder believe that their spouse or sexual partner is unfaithful without any concrete evidence.
- Persecutory: People with this type of delusional disorder believe someone or something is mistreating, spying on or attempting to harm them (or someone close to them). People with this type of delusional disorder may make repeated complaints to legal authorities.
- Somatic: People with this type of delusional disorder believe that they have a physical issue or medical problem, such as a parasite or a bad odor.
- Mixed: People with this type of delusional disorder have two or more of the types of delusions listed above.
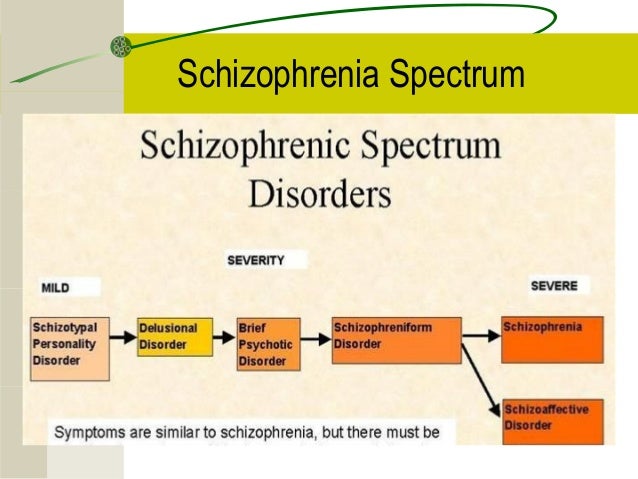
What is the difference between delusional disorder and schizophrenia?
Schizophrenia is a spectrum (or range) of conditions that involve psychotic symptoms, which include:
- Disorganized speech or behavior.
- Negative symptoms (a decrease in emotion in a person’s facial expressions and motivation).
Delusional disorder is different from schizophrenia because there aren’t any other psychotic symptoms other than delusions.
In addition, in contrast to schizophrenia, delusional disorder is relatively rare, and daily functioning isn’t as impaired as it is in schizophrenia.
Who does delusional disorder affect?
Delusional disorder most often occurs in middle to late life, with the average age of onset being 40 years.
The persecutory and jealous types of delusional disorder are more common in people assigned male at birth (AMAB), and the erotomanic type is more common in people assigned female at birth (AFAB).
People who tend to be socially isolated are more likely to develop delusional disorder. These populations include:
- Immigrants who have language barriers.
- People who are deaf.
- People who are visually impaired.
- Elderly people.
How common is delusional disorder?
Although delusions might be a symptom of more common disorders, such as schizophrenia, delusional disorder itself is rather rare. Approximately 0.05% to 0.1% of the adult population has delusional disorder.
What is the most common type of delusional disorder?
The most common type of delusional disorder is the persecutory type — when someone believes others are out to harm them despite evidence to the contrary.
Symptoms and Causes
What are the signs and symptoms of delusional disorder?
The presence of delusions is the most obvious sign of delusional disorder, which vary based on the type.
Another characteristic of this condition is that the person often lacks self-awareness that their delusions are problematic. They’re unable to accept that their delusions are irrational or inaccurate, even if they recognize that other people would describe their delusions this way.
Anger and violent behavior may be present if someone is experiencing persecutory, jealous or erotomanic delusions.
People with delusional disorder may also develop anxiety and/or depression as a result of the delusions.
Early symptoms of delusional disorder may include:
- Feelings of being exploited.
- Preoccupation with the loyalty or trustworthiness of friends.
- A tendency to read threatening meanings into benign remarks or events.
- Persistently holding grudges.
- A readiness to respond and react to perceived slights.
What causes delusional disorder?
As with many other psychotic disorders, researchers don’t yet know the exact cause of delusional disorder. Researchers are, however, looking at the role of various factors that may contribute to the development of the condition, including:
- Genetic factors: The fact that delusional disorder is more common in people who have family members with delusional disorder or schizophrenia suggests there might be a genetic factor involved. Researchers believe that, as with other mental disorders, a tendency to develop delusional disorder might be passed on from parents to their biological children.

- Biological factors: Researchers are studying how abnormalities of certain areas of your brain might be involved in the development of delusional disorder. An imbalance of certain chemicals in your brain, called neurotransmitters, has been linked to the formation of delusional symptoms.
- Environmental and psychological factors: Evidence suggests that delusional disorder can be triggered by stress. Alcohol use disorder and substance use disorder might contribute to the condition. Hypersensitivity and ego defense mechanisms like reaction formation, projection and denial are some psychodynamic theories for the development of delusional disorder. Social isolation, envy, distrust, suspicion and low self-esteem are also some psychological factors that may lead to a person seeking an explanation for these feelings and, thus, forming a delusion as a solution.
Diagnosis and Tests
How is delusional disorder diagnosed?
Healthcare providers — mainly mental health professionals — diagnose delusional disorder when a person has one or more delusions for one month or more that can’t be explained by any other condition. The person must also not have the characteristic symptoms of other psychotic disorders, such as schizophrenia.
The person must also not have the characteristic symptoms of other psychotic disorders, such as schizophrenia.
If someone is experiencing signs and symptoms of delusional disorder, a healthcare provider will perform a complete medical history and physical examination. Although there aren’t any laboratory tests to diagnose delusional disorder, their healthcare provider might use various diagnostic tests — such as imaging tests, a urine drug screen and blood tests — to rule out any physical conditions, medications or substances that could be causing the symptoms.
If their healthcare provider finds no physical reason for the symptoms, a consultation with a psychiatrist or psychologist will likely be made. Psychiatrists and psychologists use specially designed interview and assessment tools to evaluate a person for a psychotic disorder. They’ll ask questions about the delusions and assess the person’s mental status.
The psychiatrist or psychologist may also interview family members and friends so they can provide further details about the person’s delusions and a timeline of the symptoms.
As other mental health conditions can cause delusions, mental health professionals carefully assess the person for other symptoms. Delusional disorder can be misdiagnosed as any of the following conditions:
- Obsessive-compulsive disorder.
- Schizophrenia.
- Delirium/major neurocognitive disorder.
- Bipolar disorder.
- Personality disorders, especially borderline personality disorder and paranoid personality disorder.
Management and Treatment
How is delusional disorder treated?
Treatment for delusional disorder most often includes psychotherapy (talk therapy) and medication, but delusional disorder is highly resistant to treatment with medication alone.
People with delusional disorder often don’t seek treatment for the condition on their own because most people with delusional disorder don’t realize their delusions are problematic or incorrect. It’s more likely they’ll seek help due to other mental health conditions such as depression or anxiety.
People with severe symptoms or who are at risk of hurting themselves or others might need to be admitted to the hospital until the condition is stabilized.
Psychotherapy for delusional disorder
Psychotherapy is a term for a variety of treatment techniques that aim to help people identify and change troubling emotions, thoughts and behaviors. Working with a mental health professional, such as a psychologist or psychiatrist, can provide support, education and guidance to the person and their family.
Through therapy, people with delusional disorder can learn to manage their symptoms, identify early warning signs of relapse and develop relapse prevention plans. Types of psychotherapy include:
- Individual psychotherapy: This type of therapy can help a person recognize and correct the underlying thinking that has become distorted.
- Cognitive behavioral therapy (CBT): This is a structured, goal-oriented type of therapy.
 A mental health professional helps people take a close look at their thoughts and emotions. They’ll come to understand how their thoughts affect their actions. Through CBT, they can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits.
A mental health professional helps people take a close look at their thoughts and emotions. They’ll come to understand how their thoughts affect their actions. Through CBT, they can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits. - Family-focused therapy: This therapy can help people with delusional disorder and their families. This treatment involves psychoeducation regarding delusional disorder, communication improvement training and problem-solving skills training.
Medications for delusional disorder
The primary medications used to help treat delusional disorder are called antipsychotics (neuroleptics). Medications include the following:
- First-generation (“typical”) antipsychotics: Healthcare providers have used these medications to treat mental health conditions since the mid-1950s. These medicines work by blocking dopamine receptors in your brain. Dopamine is a neurotransmitter believed to be involved in the development of delusions.
 First-generation antipsychotics include chlorpromazine (Thorazine®), fluphenazine (Prolixin®), haloperidol (Haldol®), thiothixene (Navane®), trifluoperazine (Stelazine®), perphenazine (Trilafon®) and thioridazine (Mellaril®).
First-generation antipsychotics include chlorpromazine (Thorazine®), fluphenazine (Prolixin®), haloperidol (Haldol®), thiothixene (Navane®), trifluoperazine (Stelazine®), perphenazine (Trilafon®) and thioridazine (Mellaril®). - Second-generation (“atypical”) antipsychotics: These newer antipsychotics are also effective in treating the symptoms of delusional disorder. They work by blocking dopamine and serotonin receptors in your brain. These drugs include risperidone (Risperdal®), clozapine (Clozaril®), quetiapine (Seroquel®), ziprasidone (Geodon®) and olanzapine (Zyprexa®). These medications are usually better tolerated than first-generation antipsychotics.
Other medications that healthcare providers might prescribe to treat delusional disorder include anxiolytics and antidepressants. Anxiolytics might help if the person has a very high level of anxiety and/or problems sleeping. Antidepressants can help treat depression, which often occurs in people with delusional disorder.
Prevention
Can delusional disorder be prevented?
There’s no known way to prevent delusional disorder. However, early diagnosis and treatment can help decrease the disruption to the person’s life, family and friendships.
Outlook / Prognosis
What is the prognosis (outlook) for delusional disorder?
The prognosis (outlook) for people with delusional disorder varies depending on a few factors, including:
- The type of delusional disorder.
- The severity of the delusions.
- The person’s life circumstances, including the availability of support and a willingness to stick with treatment.
Delusional disorder doesn’t usually significantly affect a person’s daily functioning, but the severity of the delusion may gradually get worse. Most people with delusional disorder can remain employed as long as their work doesn’t involve things related to their delusions.
The prognosis of delusional disorder is better if the person sticks to their treatment plan. Almost 50% of people have a full recovery, more than 20% of people report a decrease in symptoms and less than 20% of people report minimal to no change in symptoms.
Almost 50% of people have a full recovery, more than 20% of people report a decrease in symptoms and less than 20% of people report minimal to no change in symptoms.
Unfortunately, many people with this condition don’t seek help. It’s often difficult for people with mental health conditions to recognize they’re not well. They also might be too embarrassed or afraid to seek treatment. Without treatment, delusional disorder can be a life-long condition.
What are the possible complications of delusional disorder?
If left untreated, delusional disorder might lead to:
- Depression, often as a consequence of difficulties associated with the delusions.
- Social isolation.
- Legal issues — for example, stalking or harassing the person involved with the delusion could lead to arrest.
- Self-harm or harm to others. This is more common in the jealous and persecutory types.
Living With
How can I help someone with delusional disorder?
If you know someone with delusional disorder, you can help by providing support and encouragement for them to seek help and treatment.
People with delusional disorder who feel pressured or repeatedly criticized by others will likely experience stress, which may worsen their symptoms. Because of this, a positive approach may be more helpful and effective.
The friends and family members of people with delusional disorder often experience stress, depression, grief and isolation. It’s important to take care of your mental health and seek help if you’re experiencing these symptoms.
A note from Cleveland Clinic
It’s important to remember that delusional disorder is a mental health condition. As with all mental health conditions, seeking help as soon as symptoms appear can help decrease the disruptions to life. Mental health professionals can offer treatment plans that can help manage thoughts and behaviors.
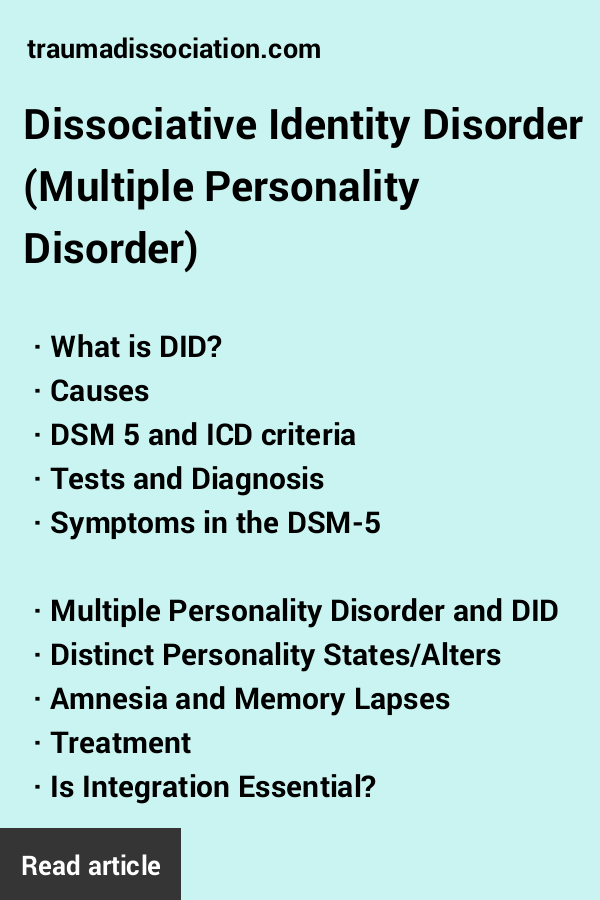
Dissociative Identity Disorder (Multiple Personality Disorder): Signs, Symptoms, Treatment
Written by WebMD Editorial Contributors
In this Article
- What Is Dissociative Identity Disorder?
- Who Is At Risk for DID?
- How to Recognize Dissociative Identity Disorder and Its Associated Mental Disorders
- How Is Dissociative Identity Disorder Diagnosed?
- What Other Psychiatric Illnesses Might Occur With DID?
- Are There Famous People With Dissociative Identity Disorder?
- What's the Treatment Plan for Dissociative Identity Disorder?
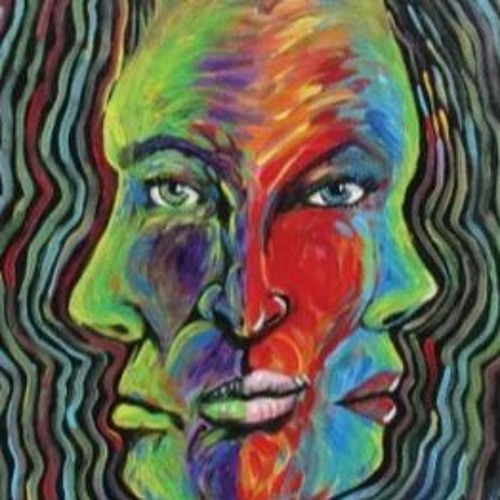
Dissociative identity disorder (previously known as multiple personality disorder) is thought to be a complex psychological condition that is likely caused by many factors, including severe trauma during early childhood (usually extreme, repetitive physical, sexual, or emotional abuse).
What Is Dissociative Identity Disorder?
Dissociative identity disorder is a severe form of dissociation, a mental process which produces a lack of connection in a person's thoughts, memories, feelings, actions, or sense of identity. Dissociative identity disorder is thought to stem from a combination of factors that may include trauma experienced by the person with the disorder. The dissociative aspect is thought to be a coping mechanism -- the person literally shuts off or dissociates themselves from a situation or experience that's too violent, traumatic, or painful to assimilate with their conscious self.
Who Is At Risk for DID?
Research indicates that the cause of DID is likely a psychological response to interpersonal and environmental stresses, particularly during early childhood years when emotional neglect or abuse may interfere with personality development. As many as 99% of individuals who develop dissociative disorders have recognized personal histories of recurring, overpowering, and often life-threatening disturbances or traumas at a sensitive developmental stage of childhood (usually before age 6).
Dissociation may also happen when there has been persistent neglect or emotional abuse, even when there has been no overt physical or sexual abuse. Findings show that in families where parents are frightening and unpredictable, the children may become dissociative. Studies indicate DID affects about 1% of the population.
How to Recognize Dissociative Identity Disorder and Its Associated Mental Disorders
Dissociative identity disorder is characterized by the presence of two or more distinct or split identities or personality states that continually have power over the person's behavior. With dissociative identity disorder, there's also an inability to recall key personal information that is too far-reaching to be explained as mere forgetfulness. With dissociative identity disorder, there are also highly distinct memory variations, which may fluctuate.
Although not everyone experiences DID the same way, for some the "alters" or different identities have their own age, sex, or race. Each has their own postures, gestures, and distinct way of talking. Sometimes the alters are imaginary people; sometimes they are animals. As each personality reveals itself and controls the individuals' behavior and thoughts, it's called "switching." Switching can take seconds to minutes to days. Some seek treatment with hypnosis where the person's different "alters" or identities may be very responsive to the therapist's requests.
Each has their own postures, gestures, and distinct way of talking. Sometimes the alters are imaginary people; sometimes they are animals. As each personality reveals itself and controls the individuals' behavior and thoughts, it's called "switching." Switching can take seconds to minutes to days. Some seek treatment with hypnosis where the person's different "alters" or identities may be very responsive to the therapist's requests.
Other symptoms of dissociative identity disorder may include headache, amnesia, time loss, trances, and "out of body experiences." Some people with dissociative disorders have a tendency toward self-persecution, self-sabotage, and even violence (both self-inflicted and outwardly directed). As an example, someone with dissociative identity disorder may find themselves doing things they wouldn't normally do, such as speeding, reckless driving, or stealing money from their employer or friend, yet they feel they are being compelled to do it. Some describe this feeling as being a passenger in their body rather than the driver. In other words, they truly believe they have no choice.
In other words, they truly believe they have no choice.
There are several main ways in which the psychological processes of dissociative identity disorder change the way a person experiences living, including the following:
- Depersonalization. This is a sense of being detached from one's body and is often referred to as an "out-of-body" experience.
- Derealization. This is the feeling that the world is not real or looking foggy or far away.
- Amnesia. This is the failure to recall significant personal information that is so extensive it cannot be blamed on ordinary forgetfulness. There can also be micro-amnesias where the discussion engaged in is not remembered, or the content of a meaningful conversation is forgotten from one second to the next.
- Identity confusion or identity alteration. Both of these involve a sense of confusion about who a person is. An example of identity confusion is when a person has trouble defining the things that interest them in life, or their political or religious or social viewpoints, or their sexual orientation, or their professional ambitions.
 In addition to these apparent alterations, the person may experience distortions in time, place, and situation.
In addition to these apparent alterations, the person may experience distortions in time, place, and situation.
It is now acknowledged that these dissociated states are not fully mature personalities, but rather they represent a disjointed sense of identity. With the amnesia typically associated with dissociative identity disorder, different identity states remember different aspects of autobiographical information. There is usually a "host" personality within the individual, who identifies with the person's real name. Ironically, the host personality is usually unaware of the presence of other personalities.
How Is Dissociative Identity Disorder Diagnosed?
Making the diagnosis of dissociative identity disorder takes time. It's estimated that individuals with dissociative disorders have spent seven years in the mental health system prior to accurate diagnosis. This is common, because the list of symptoms that cause a person with a dissociative disorder to seek treatment is very similar to those of many other psychiatric diagnoses. In fact, many people who have dissociative disorders also have coexisting diagnoses of borderline or other personality disorders, depression, and anxiety.
In fact, many people who have dissociative disorders also have coexisting diagnoses of borderline or other personality disorders, depression, and anxiety.
The DSM-5 provides the following criteria to diagnose dissociative identity disorder:
- Two or more distinct identities or personality states are present, each with its own relatively enduring pattern of perceiving, relating to, and thinking about the environment and self.
- Amnesia must occur, defined as gaps in the recall of everyday events, important personal information, and/or traumatic events.
- The person must be distressed by the disorder or have trouble functioning in one or more major life areas because of the disorder.
- The disturbance is not part of normal cultural or religious practices.
- The symptoms cannot be due to the direct physiological effects of a substance (such as blackouts or chaotic behavior during alcohol intoxication) or a general medical condition (such as complex partial seizures).
The distinct personalities may serve diverse roles in helping the individual cope with life's dilemmas. For instance, there's an average of two to four personalities present when the patient is initially diagnosed. Then there's an average of 13 to 15 personalities that can become known over the course of treatment. Environmental triggers or life events cause a sudden shift from one alter or personality to another.
What Other Psychiatric Illnesses Might Occur With DID?
Along with the dissociation and multiple or split personalities, people with dissociative disorders may experience a number of other psychiatric problems, including symptoms:
- Depression
- Mood swings
- Suicidal tendencies
- Sleep disorders (insomnia, night terrors, and sleep walking)
- Anxiety, panic attacks, and phobias (flashbacks, reactions to stimuli or "triggers")
- Alcohol and drug abuse
- Compulsions and rituals
- Psychotic-like symptoms (including auditory and visual hallucinations)
- Eating disorders
Are There Famous People With Dissociative Identity Disorder?
Famous people with dissociative identity disorder include comedienne Roseanne Barr, Adam Duritz, and retired NFL star Herschel Walker.
Walker wrote a book about his struggles with DID, along with his suicide attempts, explaining he had a feeling of disconnect from childhood to the professional leagues. To cope, he developed a tough personality that didn't feel loneliness, one that was fearless and wanted to act out the anger he always suppressed. These "alters" could withstand the abuse he felt; other alters came to help him rise to national fame. Treatment helped Walker realize that these alternate personalities are part of dissociative identity disorder, which he was diagnosed with in adulthood.
What's the Treatment Plan for Dissociative Identity Disorder?
There are currently no formal, evidence-based guldelines to treat DID. Many treatments are based on case reports or are even controversial.
While there's also no "cure" for dissociative identity disorder, long-term treatment can be helpful, if the patient stays committed. Effective treatment includes:
- Psychotherapy: Also called talk therapy, the therapy is designed to work through whatever triggered and triggers the DID.
 The goal is to help “fuse” the separate personality traits into one consolidated personality that can control the triggers. This therapy often includes family members in the therapy.
The goal is to help “fuse” the separate personality traits into one consolidated personality that can control the triggers. This therapy often includes family members in the therapy. - Hypnotherapy. Used in conjunction with psychotherapy, clinical hypnosis can be used to help access repressed memories, control some of the problematic behaviors which accompany DID as well as help integrate the personalities into one.
- Adjunctive therapy. Therapies such as art or movement therapy have been shown to help people connect with parts of their mind that they have shut off to cope with trauma.
There are no established medication treatments for dissociative identity disorder, making psychologically-based approaches the mainstay of therapy. Treatment of co-occurring disorders, such as depression or substance use disorders, is fundamental to overall improvement. Because the symptoms of dissociative disorders often occur with other disorders, such as anxiety and depression, medicines to treat those co-occurring problems, if present, are sometimes used in addition to psychotherapy.
how multiple personality arises - T&P
Multiple personality disorder is a bright but rather controversial disease that still causes heated discussions among doctors and scientists. Someone doubts whether it exists at all, someone doubts whether this state should be considered a deviation from the norm. "Theories and Practices" remembered how the research of this psychiatric phenomenon began and why one should not rush to evaluate it.
Dissociative identity disorder is a condition in which, in addition to the main personality, the patient has at least one (and often more) subpersonality that periodically “takes control” of the body and acts in accordance with their own ideas about life. These ideas can be very different from the habits and philosophy of the real owner of the body.
Despite the fact that some experts consider this disease iatrogenic - that is, provoked by the careless words of doctors or watching a "scientific" TV show - there is a number of evidence that indicates the opposite. One of the most impressive is the history of the disease. Cases of dissociative disorder were also recorded when neither psychotherapists nor TV shows were in sight. However, psychiatry itself did not exist.
One of the most impressive is the history of the disease. Cases of dissociative disorder were also recorded when neither psychotherapists nor TV shows were in sight. However, psychiatry itself did not exist.
One of the first described cases of dissociative personality disorder occurred at the end of the 18th century in the German city of Stuttgart. A revolution had just taken place in France, and the aristocrats, saving their lives, fled from their native country to neighboring states, including Germany. A young resident of Stuttgart took their misfortunes too close to her heart. She suddenly had a second personality - a Frenchwoman. She not only spoke her “native language” perfectly, but also coped noticeably worse with German, she had a noticeable accent. The Frenchwoman who appeared was of aristocratic blood, and her manners and habits fully corresponded to her status. It is noteworthy that the German girl did not remember what the "Frenchwoman" was doing, and she did not know anything about the legal mistress of the body.
The young German woman was not the only person with this disease in her century, but nevertheless her illness turned out to be extremely rare - in total, 76 cases of dissociative identity disorder were documented up to the middle of the 20th century. Interestingly, in recent decades, much more of them have been described - today more than 40 thousand people with this diagnosis live in the world. However, this does not mean the beginning of an "epidemic" - psychiatry, with all its arsenal of medicines, appeared only in the middle of the last century, and, accordingly, control over the incidence of such disorders began not much earlier.
To date, quite a lot of books and articles have been written about multiple personality disorder, both popular and academic. The most interesting thing about it is, perhaps, the moment of the onset of the disease in childhood. No one is born a “ready-made”, whole person. Growing up, the child experiences many emotions and experiences that are loosely related to each other. Over time, they integrate together, forming one common identity. However, the development of a child does not always go smoothly. In cases where children at an early age (about 2 years) are separated from their mother when they experience abuse or some traumatic experience, childhood experiences can remain segregated and lead to the formation of two or more personalities. Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Over time, they integrate together, forming one common identity. However, the development of a child does not always go smoothly. In cases where children at an early age (about 2 years) are separated from their mother when they experience abuse or some traumatic experience, childhood experiences can remain segregated and lead to the formation of two or more personalities. Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Dissociative identity disorder often begins in childhood, but may appear later. Over the years, patients, as a rule, have an increasing number of "tenants". Since individuals, as a rule, perform certain functions, help to cope with certain life situations, with the emergence of new tasks and problems, new residents appear who are able to cope with them. Each of the subpersonalities has its own worldview, its own habits, gestures and facial expressions, even age and intelligence. At certain moments, by the good will of the "owner" or against it, some of the personalities gain control over the body, and everything done by it during use, as a rule, is not controlled and is not remembered by the patient himself.
At certain moments, by the good will of the "owner" or against it, some of the personalities gain control over the body, and everything done by it during use, as a rule, is not controlled and is not remembered by the patient himself.
A key issue in the lives of patients with dissociative personality disorder is the relationship that has developed in the “team”. Sub-personalities may or may not be aware of each other's existence, be aggressive or silently roam museums at their own time, negotiate rental schedules with the owner of the body, or regularly stage power grabs. The treatment strategy also depends on these factors - it is based on psychotherapy, and although its ultimate goal is to come to the integration of personalities into one, an important task in the process is the "neutralization" of dangerous tenants, and the organization of harmonious relations between all subpersonalities.
More than one person in one body is unfortunately not the only symptom of dissociative identity disorder. It is often accompanied by depression, anxiety disorders, phobias, sleep and eating disorders, even hallucinations. Dissociative disorder is sometimes confused with schizophrenia, but these diseases can be distinguished - in schizophrenia, as a rule, the symptoms are perceived as enemy actions of aliens, the KGB or members of the Masonic lodge, which is not the case with dissociative disorder. In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not just separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
It is often accompanied by depression, anxiety disorders, phobias, sleep and eating disorders, even hallucinations. Dissociative disorder is sometimes confused with schizophrenia, but these diseases can be distinguished - in schizophrenia, as a rule, the symptoms are perceived as enemy actions of aliens, the KGB or members of the Masonic lodge, which is not the case with dissociative disorder. In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not just separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
Treatment of patients diagnosed with multiple personality disorder is usually long, difficult and emotionally costly. However, not everyone agrees that it should be treated at all. The American psychologist James Hillman, the founder of the school of archetypal psychology, is convinced that the position that multiple personality syndrome is considered a disorder is nothing more than a stereotype that can and should be fought, advocating the right of people with this diagnosis to be considered no less normal than others. The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
The American psychologist James Hillman, the founder of the school of archetypal psychology, is convinced that the position that multiple personality syndrome is considered a disorder is nothing more than a stereotype that can and should be fought, advocating the right of people with this diagnosis to be considered no less normal than others. The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
Flora Schreiber
A serious and very detailed book written by a doctor about her own patient who is trying to get along with her sixteen subpersonalities.
Daniel Keyes
Incredible biography of the most famous criminal diagnosed with multiple personality disorder. 24 personalities coexisted in the body of Billy Milligan, including a Yugoslav communist, a lesbian poet, and a three-year-old girl. By the way, the book has a sequel - Milligan's War.
Truddy Chase
The most interesting thing about this very positive biographical book is that it was written by Truddy Chase in collaboration with subpersonalities, and by reading it you can see from the inside the teamwork of all Truddy's alters.
Robert Oxnam
Oxnam, president of the Asia Society and well-known public figure, talks in his book about how he tried to disguise his illness with alcoholism, struggled with memory lapses and worked in a rehabilitation center to integrate his 11 sub-personalities.
Elena Foer
Tags
#Psychiatry
#Likbez
#Science
-
73 575
- Dissociative Identity Disorder (DSM-IV)
- Multiple Personality Disorder (ICD-10)
- Multiple Personality Syndrome [1]
- Organic Dissociative Personality Disorder [2]
- Split personality [3]
- 1 Dissociative identity disorder
- 2 Diagnostic criteria
- 2.
 1 Multiple personality disorder and schizophrenia
1 Multiple personality disorder and schizophrenia
- 2.
- 3 Chronology of the development of the understanding of multiple personality
- 3.1 1640s-1880s
- 3.2 1880s-1950s
- 3.3 After 1950s
- 4 Determination of dissociation
- 5 Divergence of opinion on multiple personality
- 5.1 Critical attitude towards the diagnosis
- 5.2 Multiple personality as a healthy state
- 5.3 Intercultural studies
- 6 Potential causes of multiple personality disorder
- 7 Treatment
- 8 Notes
- 9 Bibliography
- 10 See also
- 11 Links
- 11.1 General information
- 11.2 Related materials
- 11.3 Thematic Internet resources
- 1784 — The Marquis de Puysegur, a student of Franz Anton Mesmer, uses magnetic techniques to put his worker Victor Race ( Victor Race ) into a kind of somnambulistic state: Victor has shown the ability to stay awake during sleep. Upon awakening, he is unable to remember what he did in the altered state of consciousness, while in the latter he retained full awareness of the events that happened to him both in the normal state of consciousness and in the altered one. Puysegur comes to the conclusion that this phenomenon is similar to somnambulism, and calls it "magnetic somnambulism" [8] .
- 1791 - Eberhard Gmelin describes a case of "changing personality" in a 21-year-old German girl. She developed a second personality who spoke French and claimed to be a French aristocrat. Gmelin saw a similarity between this phenomenon and magnetic sleep, and considered that such cases could help in understanding the formation of personality [8] .
- 1816 - The case of Mary Reynolds, who had a "dual personality", is described in the Medical Repository.
- 1838 - Charles Despin describes a case of dual personality in Estella, an 11-year-old girl.
- 1876 - Eugène Azam describes a case of dual personality in a young French girl whom he called Felida X. He explains the phenomenon of multiple personality with the help of the concept of hypnotic states, which became widespread at that time in France [8] .
- 1888 Physicians Bourru ( Bourru ) and Burrot ( Burrot ) publish the book Variations de la personnalité () in which they describe the case of Louis Vivé ( Louis Vivé) who had personalities, each with their own muscle contraction patterns and individual memories.
 The memories of each person were rigidly tied to a certain period of Louis' life. As a treatment, physicians used hypnotic regression during these periods; they viewed the personalities of this patient as successive variations of one personality. Another researcher, Pierre Janet, introduced the concept of "dissociation" and suggested that these personalities were coexisting mental centers within the same individual [8] .
The memories of each person were rigidly tied to a certain period of Louis' life. As a treatment, physicians used hypnotic regression during these periods; they viewed the personalities of this patient as successive variations of one personality. Another researcher, Pierre Janet, introduced the concept of "dissociation" and suggested that these personalities were coexisting mental centers within the same individual [8] . - 1899 - Théodore Flournoy's From India to the Planet Mars: A Case of Somnambulism with Fictional Languages ( Des Indes à la Planète Mars: Etude sur un cas de somnambulisme avec glossolalie ) is published.
- 1906 Morton Prince's The Dissociation of a Personality describes the case of a multiple personality patient, Clara Norton Fowler, also known as Miss Christine Beschamp. As a treatment, Prince proposed to unite the two personalities of Besham, and to force the third into the subconscious [8] .
- 1908 - G.
 G. Evers publishes the story "The Death of Baron von Friedel", which was originally called "Second Self". The story is about the splitting of consciousness into male and female components. Both components in turn take over the personality and, in the end, enter into an irreconcilable dispute. The baron shot himself, and at the end of the story it says: “Of course, suicide is out of the question here. Rather like this: he, Baron Jesus Maria von Friedel, shot Baroness Jesus Maria von Friedel; or vice versa - she killed him. I do not know this. I wanted to kill - he or she - but not myself, I wanted to kill something else. And so it happened."
G. Evers publishes the story "The Death of Baron von Friedel", which was originally called "Second Self". The story is about the splitting of consciousness into male and female components. Both components in turn take over the personality and, in the end, enter into an irreconcilable dispute. The baron shot himself, and at the end of the story it says: “Of course, suicide is out of the question here. Rather like this: he, Baron Jesus Maria von Friedel, shot Baroness Jesus Maria von Friedel; or vice versa - she killed him. I do not know this. I wanted to kill - he or she - but not myself, I wanted to kill something else. And so it happened." - 1915 - Walter Franklin Prince publishes the case of a patient, Doris Fisher, The Doris Case of Multiple Personality (). Doris Fisher had five personalities. Two years later, he published a report on the experiments performed with the participation of Fisher and her other personalities.
- 1943 - Stengel states that the state of multiple personality no longer occurs.

- 1954 - Thigpen and Cleckley's The Three Faces of Eve, based on a psychotherapy story involving Chris Costner-Sizemore, a patient with multiple personalities, is published. The release of this book stirred up the interest of the general public in the nature of the phenomenon of multiple personality [8] .
- 1957 - Film adaptation of The Three Faces of Eve (film) starring Joanne Woodward.
- 1973 - Publication of Flora Schreiber's best-selling book Sybil, which tells the story of Shirley Mason (Sibyl Dorsett in the book).
- 1976 TV adaptation of Sybil (Sybil (film)), starring Sally Field.
- 1977 - Chris Costner-Sizemore ( eng. ) publishes an autobiography, I'm Eve ( I'm Eve ), in which he claims that Thigpen and Cleckley's book misinterpreted her life story.
- 1980 - Publication of Michelle Remembers, co-authored by psychiatrist Lawrence Pazder and Michelle Smith, a patient with multiple personalities.

- 1981 Daniel Keyes publishes The Minds of Billy Milligan based on extensive interview material with Billy Milligan and his therapist.
- 1981 - Publication of Truddy Chase ( English ) "When Rabbit Howls".
- 1994 - Publication in Japan of Daniel Keyes' second book about Billy Milligan titled "Milligan Wars"
- 1995 - Launch of Astraea's Web, the first online resource dedicated to recognizing multiple personality as a healthy condition.
- 1998 - New Yorker article "Creating Hysteria" published by Joan Akocella, describing the excesses of multiple personality psychotherapy.
- 1999 Cameron West publishes First Person Plural: My Life as a Multiple.
- 2005 - Robert Oxnam's autobiography A Fractured Mind is published.
- 2007 - Second television adaptation of "Sybil".
- ↑ Talbot M. Holographic Universe. - K .: Sofia, 2004. Ch. Therapy for Multiple Personality Syndrome ISBN 5-9550-0482-3
- ↑ Comer R. Fundamentals of pathopsychology. - M: "Prime-Eurosign", 2005. Ch. 13: Disorders of memory and other cognitive functions.
- ↑ Sharma, Sanjeev. [http://ezinearticles.com/?Split-Personality---A-Myth-or-a-Reality?&id=45153 Split Personality - A Myth or a Reality?]. June 2005. (English)
- ↑ ICD-10. International classification of diseases.
- ↑ Diagnostic criteria for 300.
 14 Dissociative Identity Disorder // Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM), Revised. (English)
14 Dissociative Identity Disorder // Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM), Revised. (English) - ↑ Dell P., Carena Etzel et al. Why the diagnostic criteria for dissociative identity disorder should be changed // Journal of trauma & dissociation. 2001, vol. 2, no1, pp. 7-72. ISSN 1529-9732. (English)
- ↑ 1 2 3 F44.81 Multiple personality disorder (RML) // View V. D., Popov Yu. V. Modern Clinical psychiatry. - St. Petersburg: 2000.
- ↑ 1 2 3 4 5 6 7 8 Crabtree A & J. Multiple personality before Eve. - Website: Psychotherapy Arts. (English)
- ↑ 1 2 Acocella, Joan.
 Creating Hysteria: Women and Multiple Personality Disorder. - San Francisco: Jossey-Bass Publishers, 1999. ISBN 0-7879-4794-6 (English)
Creating Hysteria: Women and Multiple Personality Disorder. - San Francisco: Jossey-Bass Publishers, 1999. ISBN 0-7879-4794-6 (English) - ↑ Ross, Colin. Dissociative Identity Disorder: Diagnosis, Clinical Features and Treatment of Multiple Personality, Second Edition - John Wiley & Sons, Inc, 1997. ISDN: 0471-13265-9
- ↑ 3484. Dissociative Disorders. eMedicine Clinical Knowledge Base. (English)
- ↑ Marmer SS, Fink D. Rethinking the comparison of borderline personality disorder and multiple personality disorder // The Psychiatric clinics of North America. — 1994, vol. 17, no 4 (i-xiv, 701-879 [189 p.]) (157 ref.), [Note(s) : VI, 743-771 [30 p.]]. ISSN 0193-953X
- ↑ A History of Dissociative Identity Disorder (formerly called Multiple Personality Disorder). - Website: Demonic Possession and Psychiatry. (English)
- ↑ Adams, Cecil. Does multiple personality disorder really exist? // The Straight Dope.
 October 2003. (English)
October 2003. (English) - ↑ Adams, Michel Vanney. archetypal school. Jung on archetypes and archetypal images.
- ↑ Luh Ketut Suryani, Gordon D. Jensen. Trance and Possession in Bali: A Window on Western Multiple Personality, Possession Disorder, and Suicide. - Oxford University Press, 1994. ISBN 0-19-588610-0 (English)
- ↑ 1 2 3 — Website: MERCK. February 2003
- Ross, Colin. Dissociative Identity Disorder: Diagnosis, Clinical Features and Treatment of Multiple Personality, Second Edition - John Wiley & Sons, Inc, 1997. ISDN 0471-13265-9.
- Luh Ketut Suryani, Gordon D. Jensen. Trance and Possession in Bali: A Window on Western Multiple Personality, Possession Disorder, and Suicide. — Oxford University Press, 1994. ISBN 0-19-588610-0.
- Putnam FW Diagnosis and treatment of multiple personality disorder.
 - M .: Kogito-Centre, 2003. ISBN 5-89353-106-X.
- M .: Kogito-Centre, 2003. ISBN 5-89353-106-X. - Freud Z. Splitting I in the process of defense (1938) / Psychology of the unconscious. M., 2006. S. 415-424.
- Multiple personality in popular culture
- Dissociative disorders
- Billy Milligan
- Splitting consciousness
- Dissociative Identity Disorder is a dictionary entry for multiple personality disorder or dissociative identity disorder. (English)
- Multiple Personality Before Eve is a history of the early research and concepts of multiple personality. (English)
- Overview of dissociative identity disorder at WebMD.com. (English)
- Multiple Personality Disorder at Skepdic.com. (English)
- International Society for the Study of Dissociation
- Piper A, Merskey H. The persistence of folly: A critical examination of dissociative identity disorder.
 Part I. The excesses of an improbable concept. Can J Psychiatry 2004;49:592-600 — A critical review of the diagnosis of multiple personality as being iatrogenic. (English)
Part I. The excesses of an improbable concept. Can J Psychiatry 2004;49:592-600 — A critical review of the diagnosis of multiple personality as being iatrogenic. (English) - Piper A, Merskey H. The persistence of folly: A critical examination of dissociative identity disorder. Part II. The defense and decline of multiple personality or dissociative identity disorder. Can J Psychiatry 2004;49:678-83. — Continuation of the article. (English)
- Alexandria K. Cherry. Multiple Personality Disorder: Fact or Fiction?. Rochester Institute of Technology. 2005. - Peer-reviewed review study on multiple personality disorder. (English)
- James A. Chu, MD. Guidelines for Treating Dissociative Identity Disorder in Adults (2005) (English)
- David V. James MA, MRCPsych. Multiple Personality Disorder in the Courts. - Dissociative identity disorder and litigation. (English)
- Thigpen & Cleckley (1954): A case of multiple personality. — Study of the treatment of the treatment method of Chris Costner-Sizemore, who became the heroine of the work "The Three Faces of Eve".
 (English)
(English) - The Layman's Guide to Multiplicity — Healthy multiplicity pamphlet written by a group of people with multiple personalities. (English)
- Motov VV Multiple Personality Disorder in the USA: Clinical and Forensic Psychiatric Aspects // Independent Psychiatric Journal. Q1 2005.
- Putnam FM Diagnosis and treatment of multiple personality disorder // Journal of Practical Psychology and Psychoanalysis. No. 1, March 2004. - A chapter from a book.
- Lecture "Schizotypal disorder and multiple personality".
- The Layman's Guide — A guide to multiple personalities written by a group of people with multiple personalities. (English)
- Amorpha: Collective Phenomenon - An online community dedicated to multiple personality as a healthy state. (English)
- Astraea - Collection of articles and links on multiple personality as a healthy state. (English)
- Pavilion - An activist website dedicated to functional (or healthy) multiple personality.
Multiple personality | it's.
 .. What is Multiple Personality?
.. What is Multiple Personality? Alternative names:
"Split Personality" is redirected here; see also other meanings.
Not to be confused with schizophrenia.
Multiple Personality is a psychic phenomenon in which a person has two or more distinct personalities or ego states. Each alter personality in this case has its own patterns of perception and interaction with the environment. People with multiple personalities are diagnosed with dissociative identity disorder, or multiple personality disorder. This phenomenon is also known as "split personality" and "split personality".
|
Contents |
Dissociative identity disorder
Dissociative identity disorder personality. To define dissociative identity disorder (or multiple personality disorder) in a person, it is necessary to have at least two personalities who regularly take turns controlling the behavior of the individual, as well as memory loss that goes beyond normal forgetfulness. Memory loss is usually described as a "switch". Symptoms should occur regardless of substance abuse (alcohol or drugs) or general medical condition. Dissociative identity disorder is also known as multiple personality disorder [4] . In North America, this disorder is commonly referred to as "dissociative identity disorder" because of the divergence of opinion in the psychiatric and psychological environment regarding this concept, according to which one (physical) individual can have more than one personality, where personality can be defined as the sum total of mental states given (physical) individual.
Memory loss is usually described as a "switch". Symptoms should occur regardless of substance abuse (alcohol or drugs) or general medical condition. Dissociative identity disorder is also known as multiple personality disorder [4] . In North America, this disorder is commonly referred to as "dissociative identity disorder" because of the divergence of opinion in the psychiatric and psychological environment regarding this concept, according to which one (physical) individual can have more than one personality, where personality can be defined as the sum total of mental states given (physical) individual.
Although dissociation is a demonstrable psychiatric condition associated with a number of different disorders, especially those related to early childhood trauma and anxiety, multiple personality as a real psychological and psychiatric phenomenon has been questioned for some time. Despite differences of opinion regarding the diagnosis of multiple personality disorder, many psychiatric institutions (such as McLean Hospital) have rooms specifically designed for dissociative identity disorder.
According to one of the classifications, dissociative identity disorder is considered as a type of psychogenic amnesia (that is, having only a psychological, not a medical, nature). Through such amnesia, a person gains the ability to repress memories of traumatic events or a certain period of life. This phenomenon is called the splitting of the "I", or, in other terminology, the self, as well as the experiences of the past. Having multiple personalities, an individual can experience alternative personalities with individually distinguishable characteristics: such alternative personalities can have different ages, psychological sex, different health conditions, different intellectual abilities, and even different handwriting. Long-term therapies are usually considered for the treatment of this disorder.
Two characteristic features of dissociative identity disorder are depersonalization and derealization. Depersonalization is an altered (mostly described as distorted) perception of oneself and one's own reality. Such a person often appears detached from consensual reality. Patients often define depersonalization as "a feeling outside of the body and being able to observe it from a distance." Derealization is an altered (distorted) perception of others. With derealization, other people will not be perceived as really existing for this person; patients with derealization have difficulty identifying the other person.
Such a person often appears detached from consensual reality. Patients often define depersonalization as "a feeling outside of the body and being able to observe it from a distance." Derealization is an altered (distorted) perception of others. With derealization, other people will not be perceived as really existing for this person; patients with derealization have difficulty identifying the other person.
Study [ source unspecified 1149 days ] showed that patients with dissociative identity disorder often hide their symptoms. The average number of alternate personalities is 15 and usually appear in early childhood, which is probably why some of the alternate personalities are children. Many patients have a comorbidity, that is, along with a multiple personality disorder, they also have other disorders, such as generalized anxiety disorder.
Diagnostic criteria
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), a diagnosis of dissociative identity disorder is made when a person has two or more distinct identities or personality states (with each having its own relatively continuous pattern of perception and relationship with the environment and oneself), at least two of these identities recurrently seize control over human behavior, the individual is unable to recall important personal information, which is beyond ordinary forgetfulness, and the disorder itself is not caused by the direct physiological effects of any either a substance (eg, intoxication or erratic behavior from alcohol intoxication) or a general medical condition (eg, complex partial seizures). At the same time, it is noted that in children these symptoms should not be attributed to imaginary friends or other types of fantasy games [5] .
At the same time, it is noted that in children these symptoms should not be attributed to imaginary friends or other types of fantasy games [5] .
The criteria for diagnosing dissociative identity disorder published by the DSM-IV have been criticized. One study (2001) highlighted a number of shortcomings of these diagnostic criteria: this study argues that they do not meet the requirements of modern psychiatric classification, are not based on a taxometric analysis of symptoms of dissociative identity disorder, describe the disorder as a closed concept, have poor content validity, ignore important data, hinder taxonomic research, have a low degree of reliability and often lead to misdiagnosis, they contain a contradiction and the number of cases with dissociative personality disorder is artificially low in it. This study proposes a solution to the DSM-V in the form of new, according to researchers, more user-friendly polythetic diagnostic criteria for dissociative disorders [6] .
Multiple personality disorder and schizophrenia
Distinguishing schizophrenia from multiple personality disorder is difficult to diagnose, and is mainly based on structural features of the clinical picture, uncharacteristic of dissociative disorders. In addition, the corresponding symptoms are perceived by patients with schizophrenia more often as a result of external influences, and not belonging to their own personality. The splitting of personality in multiple disorder is massive or molecular, forming rather complex and self-integrated personality substructures. Splitting in schizophrenia, referred to as discrete, nuclear or atomic, is a splitting of individual mental functions from the personality as a whole, which leads to its disintegration [7] .
Chronology of the development of the understanding of multiple personality
1640s-1880s
The period of the theory of magnetic somnambulism as an explanation of multiple personality [8] .
1880s-1950s
Introduction of the concept of dissociation and that a person can have multiple mental centers that occur when the psyche tries to deal with traumatic experiences [8] .
After 1950s
Definition of dissociation
Main article: Dissociative disorder
Main article: Dissociation (psychology)
Dissociation is a protective mechanism of the psyche, usually triggered in painful and / or traumatic situations. Dissociation is characterized by the disintegration of the ego. Ego integrity can be defined as the ability of a person to successfully incorporate external events or social experiences into their perception and then act in a consistent manner during such events or social situations. A person unable to cope successfully with this can experience both emotional dysregulation and a potential collapse of ego integrity. In other words, the state of emotional dysregulation can in some cases be so intense as to force ego disintegration, or what, in extreme cases, is diagnosed as dissociation.
Dissociation is characterized by the disintegration of the ego. Ego integrity can be defined as the ability of a person to successfully incorporate external events or social experiences into their perception and then act in a consistent manner during such events or social situations. A person unable to cope successfully with this can experience both emotional dysregulation and a potential collapse of ego integrity. In other words, the state of emotional dysregulation can in some cases be so intense as to force ego disintegration, or what, in extreme cases, is diagnosed as dissociation.
Dissociation describes the collapse of ego integrity so severe that the personality literally splits. For this reason, dissociation is often referred to as "splitting," although that term is reserved for another mental mechanism. Less profound manifestations of this condition are in many cases clinically described as disorganization or decompensation. The difference between a psychotic manifestation and a dissociative manifestation is that although the person experiencing the dissociation is formally detached from a situation that he or she cannot control, some part of that person remains connected to reality. While the psychotic "breaks" with reality, the dissociative disconnects from it, but not completely.
While the psychotic "breaks" with reality, the dissociative disconnects from it, but not completely.
Since the person experiencing dissociation is not completely disconnected from his reality, he can, in some cases, have many "personalities". In other words, there are different "people" (read personalities) to deal with different situations, but generally speaking, none of the personalities is completely separate.
Divergence of opinions about multiple personality
Until now, the scientific community has not come to a consensus on what is considered a multiple personality, since in the history of medicine up to 19There were too few documented cases of this disorder in the 1950s. In the 4th edition of the Diagnostic and Statistical Handbook of Mental Disorders (DSM-IV), the name of the condition in question was changed from "multiple personality disorder" to "dissociative identity disorder" to remove the confusing term "personality." The same designation was adopted in ICD-9, but in ICD-10 the variant "multiple personality disorder" is used. It should be noted that a blunder is often made in the media when confusing multiple personality disorder and schizophrenia. [ source unspecified 1264 days ]
It should be noted that a blunder is often made in the media when confusing multiple personality disorder and schizophrenia. [ source unspecified 1264 days ]
A 1944 study of multiple personality sources in the medical literature of the 19th and 20th centuries found only 76 cases. In recent years, the number of cases of dissociative identity disorder has increased dramatically (according to some reports, between 1985 and 1995, about 40,000 cases were registered) [9] . However, other studies have shown that the disorder does have a long history, spanning some 300 years in the literature, and that it itself affects less than 1% of the population [10] . According to other data, dissociative identity disorder occurs among 1-3% of the general population [11] . Thus, epidemiological evidence indicates that dissociative identity disorder is actually as common in the population as schizophrenia.
Currently, dissociation is considered as a symptomatic manifestation in response to trauma, critical emotional stress, and it is associated with emotional dysregulation and borderline personality disorder [12] . According to a longitudinal (long-term) study by Ogawa et al., the strongest predictor of dissociation in young adults was lack of access to mother at age 2 years. Many recent studies have shown an association between early childhood broken attachments and subsequent dissociative symptoms, and there is clear evidence that childhood abuse and neglect often contribute to the formation of broken attachments (manifested, for example, when a child is very closely monitoring whether parental attention is paid on it or not).
According to a longitudinal (long-term) study by Ogawa et al., the strongest predictor of dissociation in young adults was lack of access to mother at age 2 years. Many recent studies have shown an association between early childhood broken attachments and subsequent dissociative symptoms, and there is clear evidence that childhood abuse and neglect often contribute to the formation of broken attachments (manifested, for example, when a child is very closely monitoring whether parental attention is paid on it or not).
Criticism of the diagnosis
Some psychologists and psychiatrists believe that dissociative identity disorder is iatrogenic or contrived, or argue that cases of true multiple personality are very rare and most documented cases should be considered iatrogenic.
Critics of the dissociative identity disorder model argue that the diagnosis of a multiple personality condition is a phenomenon more common in English-speaking countries. Under 19In the 1950s, cases of split personality and multiple personality were sometimes described and treated as rare in the Western world [13] . In 1957, the publication of the book The Three Faces of Eve and later the release of the film of the same name contributed to the growth of public interest in the phenomenon of multiple personalities. In 1973, the subsequently filmed book Sybil was published, describing the life of a woman with a multiple personality disorder. However, the diagnosis of multiple personality disorder itself was not included in the Diagnostic and Statistical Handbook of Mental Disorders until 1980 years. Between the 1980s and 1990s, the number of reported cases of multiple personality disorder increased to twenty to forty thousand [9] [14]
In 1957, the publication of the book The Three Faces of Eve and later the release of the film of the same name contributed to the growth of public interest in the phenomenon of multiple personalities. In 1973, the subsequently filmed book Sybil was published, describing the life of a woman with a multiple personality disorder. However, the diagnosis of multiple personality disorder itself was not included in the Diagnostic and Statistical Handbook of Mental Disorders until 1980 years. Between the 1980s and 1990s, the number of reported cases of multiple personality disorder increased to twenty to forty thousand [9] [14]
Multiple personality as a healthy state
Main article: Multiple personality as a healthy state
Some people, including those who self-identified as having a multiple personality, believe that this condition may not be a disorder, but a natural variation human consciousness, which has nothing to do with dissociation. Truddy Chase, author of the bestseller When Rabbit Howls, is one of the staunch supporters of this version. Although she acknowledges that in her case multiple personalities have emerged as a result of violence, at the same time she claims that her personalities have refused to be integrated and live together as a collective.
Truddy Chase, author of the bestseller When Rabbit Howls, is one of the staunch supporters of this version. Although she acknowledges that in her case multiple personalities have emerged as a result of violence, at the same time she claims that her personalities have refused to be integrated and live together as a collective.
Within depth or archetypal psychology, James Hillman argues against defining multiple personality syndrome as a single disorder. Hillman supports the idea of the relativity of all personifications and refuses to recognize the "multiple personality syndrome". According to him, to view multiple personalities as either a "mental disorder" or as a failure to integrate "private personalities" is to exhibit a cultural bias that misidentifies one particular personality, "I", with the entire personality as such.0076 [15] .
Intercultural studies
Anthropologists L. K. Suryani and Gordon Jensen are convinced that the phenomenon of pronounced trance states in the Bali community has the same phenomenological nature as the phenomenon of multiple personality in the West [16] . It is argued that people in shamanistic cultures who experience multiple personalities define these personalities not as parts of themselves, but as independent souls or spirits. There is no evidence of an association between multiple personality, dissociation, and recollection of memories and sexual abuse in these cultures. In traditional cultures, plurality, such as that shown by shamans, is not considered a disorder or disease.
It is argued that people in shamanistic cultures who experience multiple personalities define these personalities not as parts of themselves, but as independent souls or spirits. There is no evidence of an association between multiple personality, dissociation, and recollection of memories and sexual abuse in these cultures. In traditional cultures, plurality, such as that shown by shamans, is not considered a disorder or disease.
Potential causes of multiple personality disorder
Dissociative identity disorder is believed to be caused by a combination of several factors: intolerable stress, the ability to dissociate (including the ability to separate one's memories, perceptions or identity from consciousness), the manifestation of protective mechanisms in ontogeny and - during the period childhood - lack of care and participation in relation to a child with a traumatic experience or lack of protection from subsequent unwanted experiences. Children are not born with a sense of a unified identity, the latter develops from multiple sources and experiences. In critical situations, child development is hindered and many parts of what should have been integrated into a relatively unified identity remain segregated [17] .
In critical situations, child development is hindered and many parts of what should have been integrated into a relatively unified identity remain segregated [17] .
North American studies show that 97-98% of adults with dissociative identity disorder describe experiences of childhood abuse and that abuse can be documented in 85% of adults and 95% of children and adolescents with multiple personality disorder and other similar forms of dissociative disorder. These data indicate that childhood abuse is the main cause of the disorder among North American patients, while in other cultures the effects of war or natural disaster may play a larger role. Some patients may not have experienced violence but have experienced an early loss (such as the death of a parent), a serious illness, or another highly stressful event [17] .
Human development requires the child to be able to successfully integrate various types of complex information. In ontogenesis, a person goes through a number of stages of development, in each of which different personalities can be created.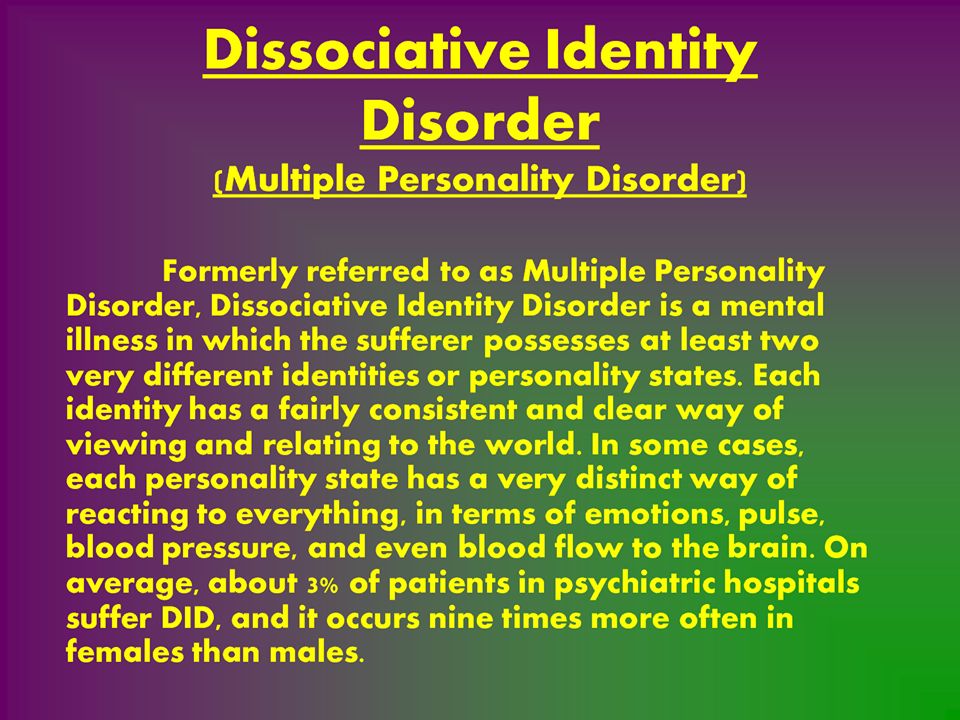 The ability to generate multiple personalities is not observed or manifested in every child who has experienced abuse, loss or trauma. Patients with dissociative identity disorder have the ability to easily enter trance states. This ability, in relation to the ability to dissociate, is believed to act as a factor in the development of the disorder. Be that as it may, most children with these abilities also have normal adaptive mechanisms and are not in an environment that can cause dissociation [17] .
The ability to generate multiple personalities is not observed or manifested in every child who has experienced abuse, loss or trauma. Patients with dissociative identity disorder have the ability to easily enter trance states. This ability, in relation to the ability to dissociate, is believed to act as a factor in the development of the disorder. Be that as it may, most children with these abilities also have normal adaptive mechanisms and are not in an environment that can cause dissociation [17] .
Treatment
The most common approach to treating multiple personality disorder is to alleviate symptoms to keep the individual safe and to reintegrate the different personalities into one well-functioning identity. Treatment can take place using various types of psychotherapy—cognitive psychotherapy, family therapy, clinical hypnosis, etc. protective mechanisms. A possible satisfactory result of treatment is the provision of a conflict-free cooperative relationship between individuals. The therapist is encouraged to treat all alter personalities with equal respect, avoiding taking sides in internal conflict [7] .
Medical therapy does not achieve noticeable success and is purely symptomatic; there is no pharmacological treatment for dissociative identity disorder itself, but some antidepressants are used to relieve comorbid depression and anxiety [7] .