What is a trauma response
Common Reactions After Trauma - PTSD: National Center for PTSD
Available en Español | Ver todos
When you experience a traumatic event, it's common to have an emotional reaction. Such stress reactions are normal and not weakness. Most people recover in time. Learn about stress reactions and problems that occur after trauma.
Reading time: minutes
What Are Common Reactions to Trauma?
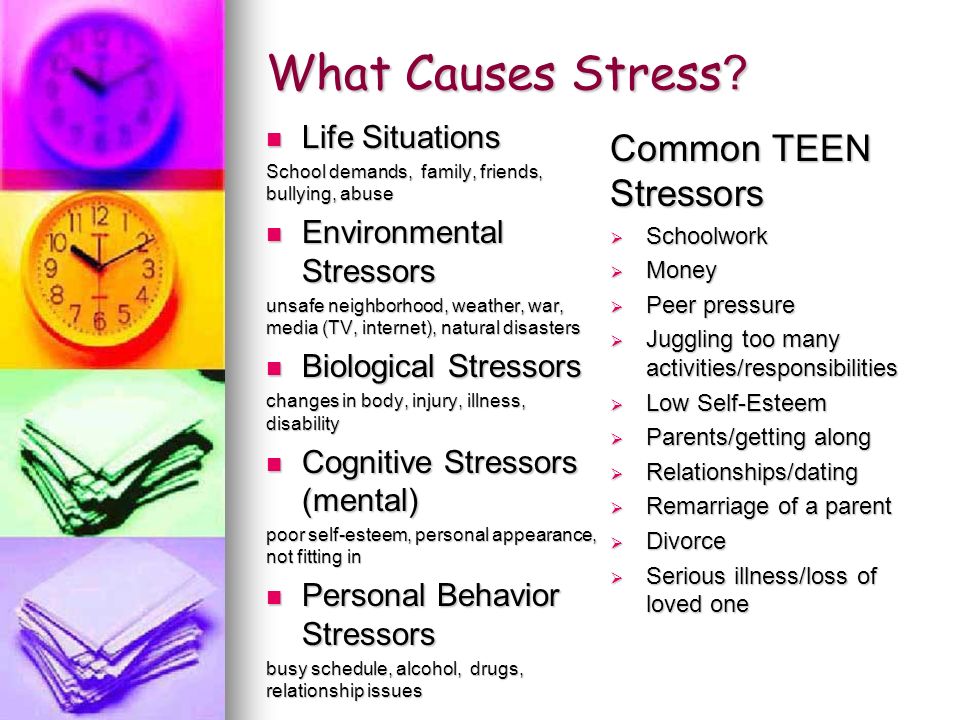
All kinds of trauma create stress reactions. People often say that their first feeling is relief to be alive after a traumatic event. This may be followed by stress, fear and anger. Trauma may also lead people to find they are unable to stop thinking about what happened. Traumatic events can create a high level of arousal—or feeling alert or "on guard"—as well, which causes people to react strongly to sounds and sights around them.
If you understand what is happening when you or someone you know reacts to a traumatic event, you may be less fearful and better able to cope. Reactions are common for anyone, even Service members and Veterans, or disaster rescue and relief workers, who have been trained to respond to crises.
Here are some common reactions to trauma:
- Losing hope for the future
- Feeling distant (detached) or losing a sense of concern about others
- Being unable to concentrate or make decisions
- Feeling jumpy and getting startled easily at sudden noises
- Feeling on guard and alert all the time
- Having dreams and memories that upset you
- Having problems at work or school
- Avoiding people, places and things related to the event
You may also experience more physical reactions such as:
- Stomach upset and trouble eating
- Trouble sleeping and feeling very tired
- Pounding heart, rapid breathing, feeling shaky
- Sweating
- Severe headache if thinking of the event
- Not keeping up with exercise, diet, safe sex or—regular health care
- Smoking more, using alcohol or drugs more, or eating too much
- Having your ongoing medical problems get worse
You may have more emotional troubles such as:
- Feeling nervous, helpless, fearful, sad
- Feeling shocked, numb, or not able to feel love or joy
- Being irritable or having angry outbursts
- Getting easily upset or agitated
- Blaming yourself or having negative views of oneself or the world
- Being unable to trust others, getting into fights, or being trying to control everything
- Being withdrawn, feeling rejected, or abandoned
- Feeling detached, not wanting intimacy
Recovery From Stress Reactions
Turn to your family and friends when you are ready to talk.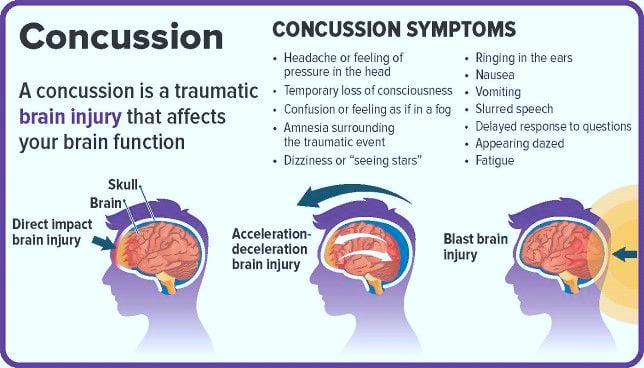 They are your personal support system. Recovery is an ongoing gradual process. Don't look to be "cured" all of a sudden or assume that you will forget what happened. Most people will recover from trauma naturally. If your stress reactions are getting in the way of your relationships, work or other important activities, you may want to talk to a counselor or your doctor. Good treatments are available.
They are your personal support system. Recovery is an ongoing gradual process. Don't look to be "cured" all of a sudden or assume that you will forget what happened. Most people will recover from trauma naturally. If your stress reactions are getting in the way of your relationships, work or other important activities, you may want to talk to a counselor or your doctor. Good treatments are available.
Common Problems That Can Occur After a Trauma
Posttraumatic Stress Disorder (PTSD). PTSD is a condition that can develop after you have gone through a life-threatening event. If you have PTSD, you may have trouble keeping yourself from thinking over and over about what happened to you. You may try to avoid people and places that remind you of the trauma. You may feel numb. Lastly, if you have PTSD, you might find that you have trouble relaxing. You may startle easily, and you may feel on guard most of the time.
Depression. Depression involves feeling down or sad more days than not.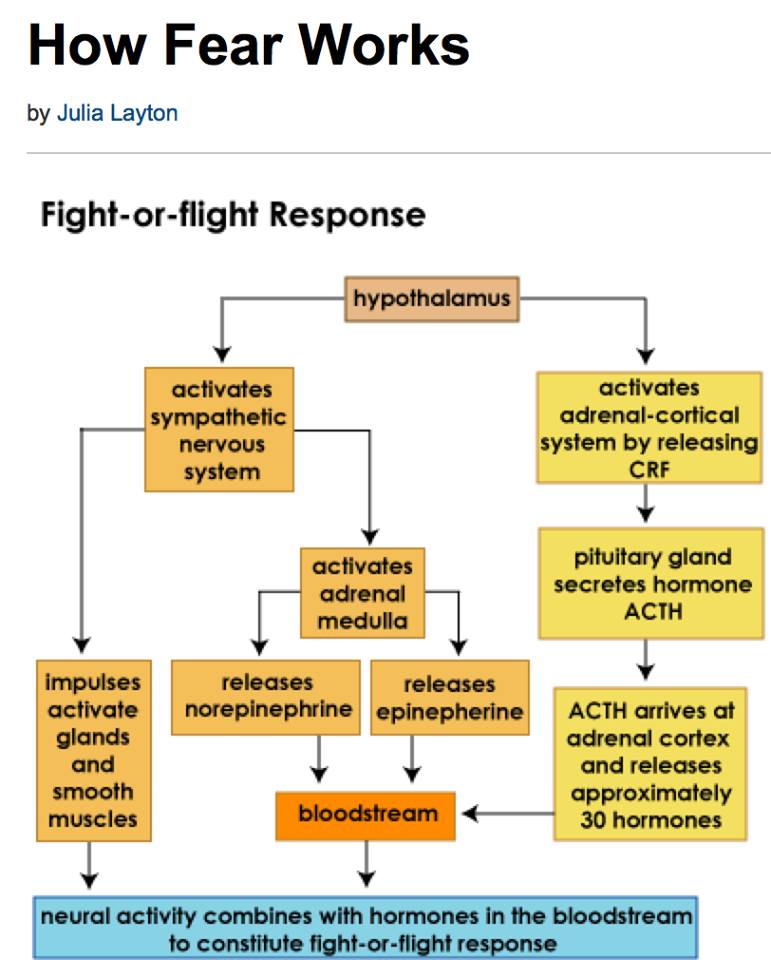 If you are depressed, you may lose interest in activities that you used to enjoy or find fun. You may feel low in energy and be overly tired. You may feel hopeless or in despair, and you may think that things will never get better. Depression is more likely when you have had losses such as the death of close friends. If you are depressed, at times you might think about hurting yourself. For this reason, getting help for depression is very important.
If you are depressed, you may lose interest in activities that you used to enjoy or find fun. You may feel low in energy and be overly tired. You may feel hopeless or in despair, and you may think that things will never get better. Depression is more likely when you have had losses such as the death of close friends. If you are depressed, at times you might think about hurting yourself. For this reason, getting help for depression is very important.
Self-blame, guilt and shame. Sometimes in trying to make sense of a traumatic event, you may blame yourself. You may think you are to blame for bad things that happened, or for surviving when others didn't. You may feel guilty for what you did or did not do. Remember, we all tend to be our own worst critics.
Suicidal thoughts. Trauma and loss can lead someone who is depressed to think about self-harm. If you have thoughts of suicide, talk to someone. If you think someone you know may be thinking about suicide, ask them.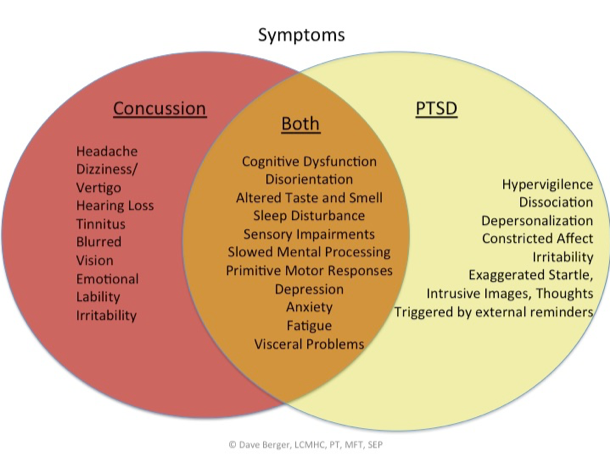 You will NOT put the idea in their head. If you or someone you care about is thinking about suicide:
You will NOT put the idea in their head. If you or someone you care about is thinking about suicide:
- Call the Suicide and Crisis Lifeline at 988 or visit 988lifeline.org.
- If you are a Veteran, or you are concerned about one, call 988 and press 1 to speak with a responder trained to help Veterans. Visit the Veterans Crisis Line.
- You can also call a counselor or doctor; or dial 911 for emergency response services (like police or an ambulance).
Anger or aggressive behavior. Trauma is related to anger in many ways. After a trauma, you might think that what happened to you was unfair or unjust. You might not understand why the event happened and why it happened to you. These thoughts can result in intense anger. Anger is a natural and healthy emotion, but strong feelings of anger and aggressive behavior can cause problems with family, friends or co-workers. If you become violent when angry, it makes the situation worse. Violence can lead to injury, and there may be legal outcomes.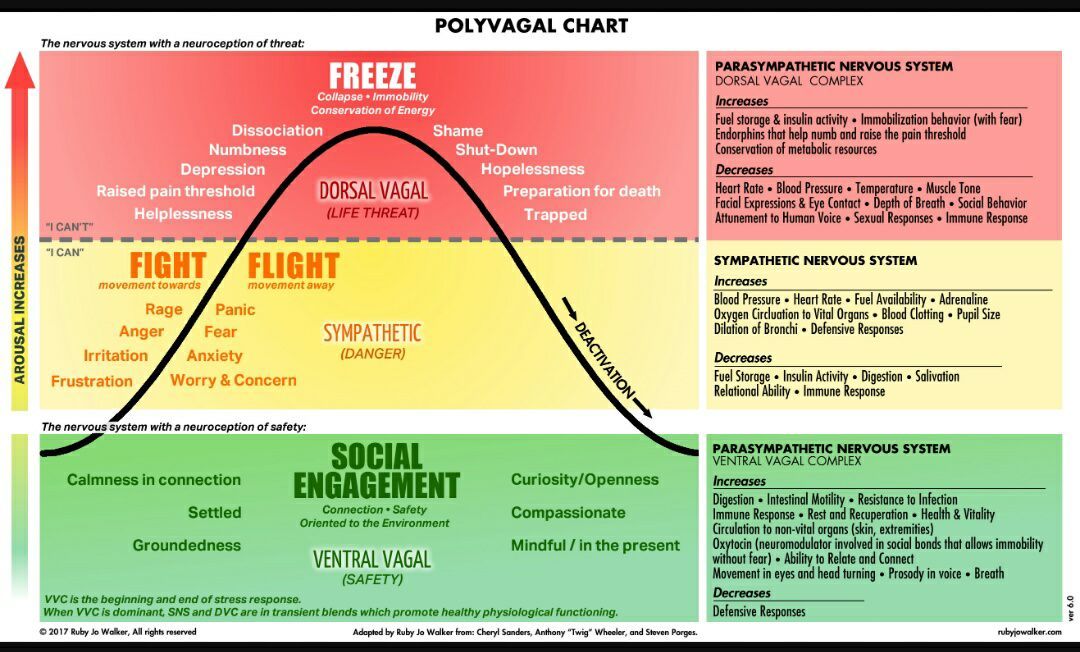
Alcohol or drug abuse. Drinking or "self-medicating" with drugs is a common, and unhealthy, way of coping with upsetting events. You may drink too much or use drugs to numb yourself and to try to deal with difficult thoughts, feelings and memories related to the trauma. While using alcohol or drugs may offer a quick solution, it can lead to more problems. If someone close to you begins to lose control of drinking or drug use, try to get them to see a health care provider about managing their drinking or drug use.
Summing It All Up
Right after a trauma, almost every survivor will find it hard to stop thinking about what happened. Stress reactions—such as fear, anxiety, jumpiness, upsetting memories, and efforts to avoid reminders—will gradually decrease over time for most people.
Use your personal support systems, family and friends, when you are ready to talk. Or, be a support for someone you care about who has been through a trauma. Recovery is an ongoing gradual process that takes time.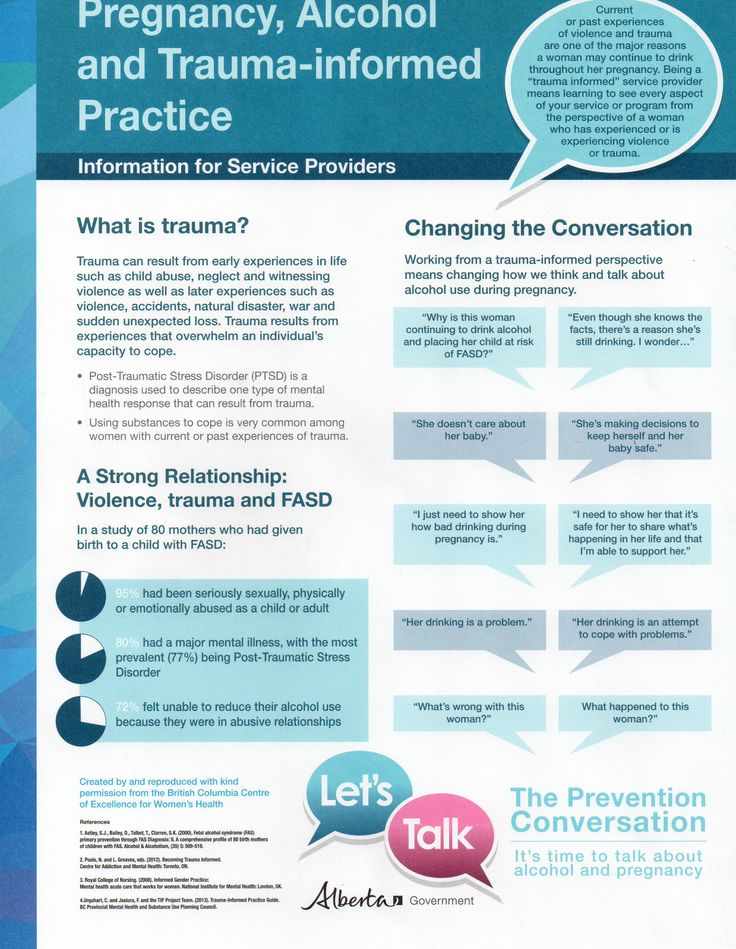 Don't look for a quick "cure" or assume that you will forget what happened. Most people will recover from trauma on their own. If your emotional reactions are getting in the way of your relationships, work or other important activities, you may want to talk to a counselor or your doctor. Good treatments are available.
Don't look for a quick "cure" or assume that you will forget what happened. Most people will recover from trauma on their own. If your emotional reactions are getting in the way of your relationships, work or other important activities, you may want to talk to a counselor or your doctor. Good treatments are available.
Understanding How Trauma Affects Everyone Differently Mental Health -
Trauma can happen to anyone because of an injury, a frightening situation or painful events in your past. It is normal to experience trauma responses, and not a character flaw or a weakness. In fact, your body and brain are hardwired to respond to trauma. When you understand how trauma influences the way you perceive the world and those around us, it will help you live a healthier life and get better medical care.
If you or anyone you know is struggling with trauma, free and confidential support is available 24/7 by calling the National Suicide Prevention Lifeline at 1-800-273-8255.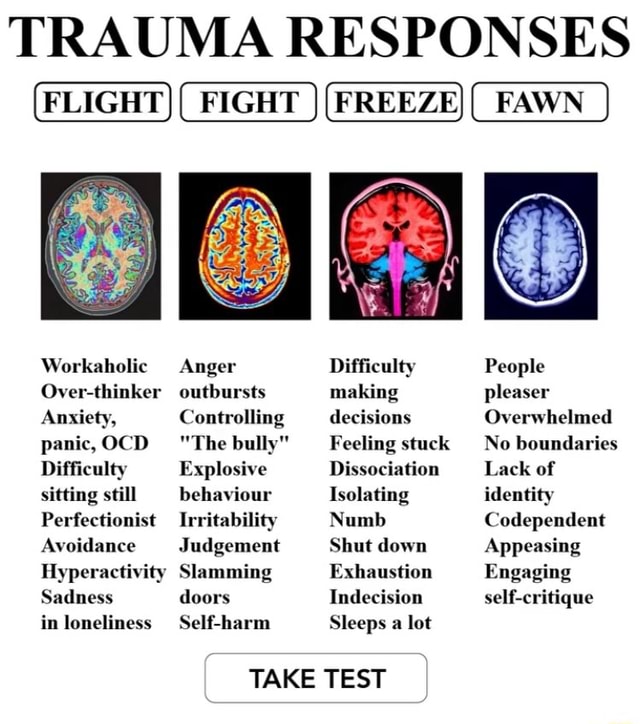
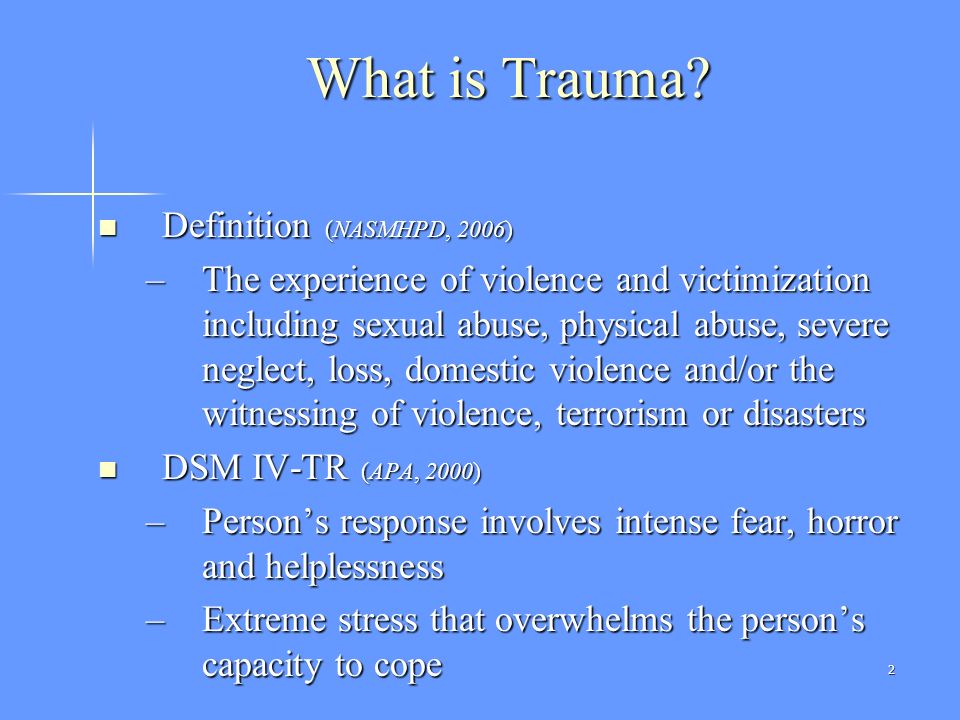
What Is Trauma?
Trauma is “an emotional response to a distressing event or situation that breaks [a] sense of security.” Traumatic events may be life-threatening, yet any events that overwhelm or isolate can result in trauma.
Trauma sets off an “alarm” that triggers the fight or flight response in your body and mind. This heightened state of arousal makes it difficult to feel calm and can be easily reactivated in other situations.
Trauma affects you differently depending on whether you have experienced it once, repeatedly, or over the course of time. Some experience it in obvious forms such as post-traumatic stress disorder, or PTSD, which causes people to revisit the intense emotions they felt during a traumatic event. Others may have a less obvious trauma response. Your life history, support systems and coping skills will alter your experience.
Recognizing a Trauma Response
There’s no “right” way to respond to trauma. How you respond is less concerning to medical providers than how that response influences your life.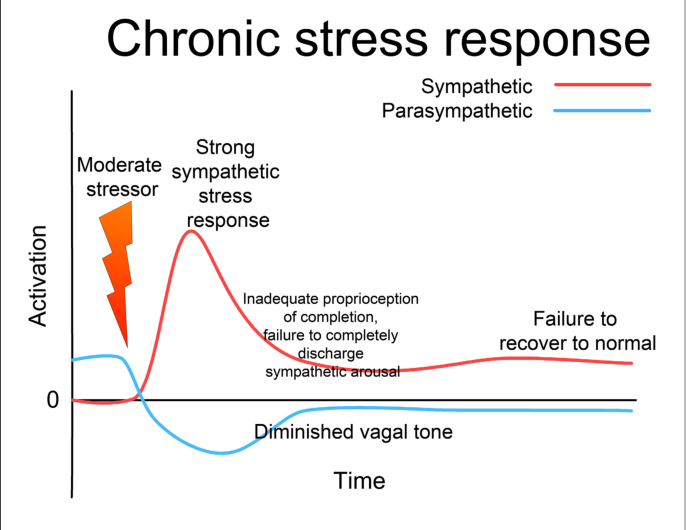 Reactions to trauma may be severe or mild, but neither are a sign of mental illness.
Reactions to trauma may be severe or mild, but neither are a sign of mental illness.
Initial trauma responses may include:
- Anxiety
- Avoidance of similar situations
- Confusion
- Disassociation
- Exhaustion
- Fear
- Feeling or acting “numb”
More severe trauma responses may include:
- Distress with no relief or moments of calm
- Intense, intrusive thoughts of traumatic events
- Severe dissociation
Delayed trauma responses, which occur longer after traumatic events have occurred, may include:
- Anxiety about flashbacks
- Avoiding any feelings or activities related to the event
- Depression
- Fatigue or other sleep disorders
- Fear of the event happening again
A variety of trauma responses can occur after traumatic events. If any symptoms of trauma impact your quality of life, speak with a medical provider right away, especially if these responses persist for more than a month.
Healing from Trauma
Many people will heal from traumatic experiences over time. A single traumatic event does not mean you will develop PTSD. Yet healing from trauma often involves therapeutic, social support and self-care.
Using the following strategies may help someone heal from trauma:
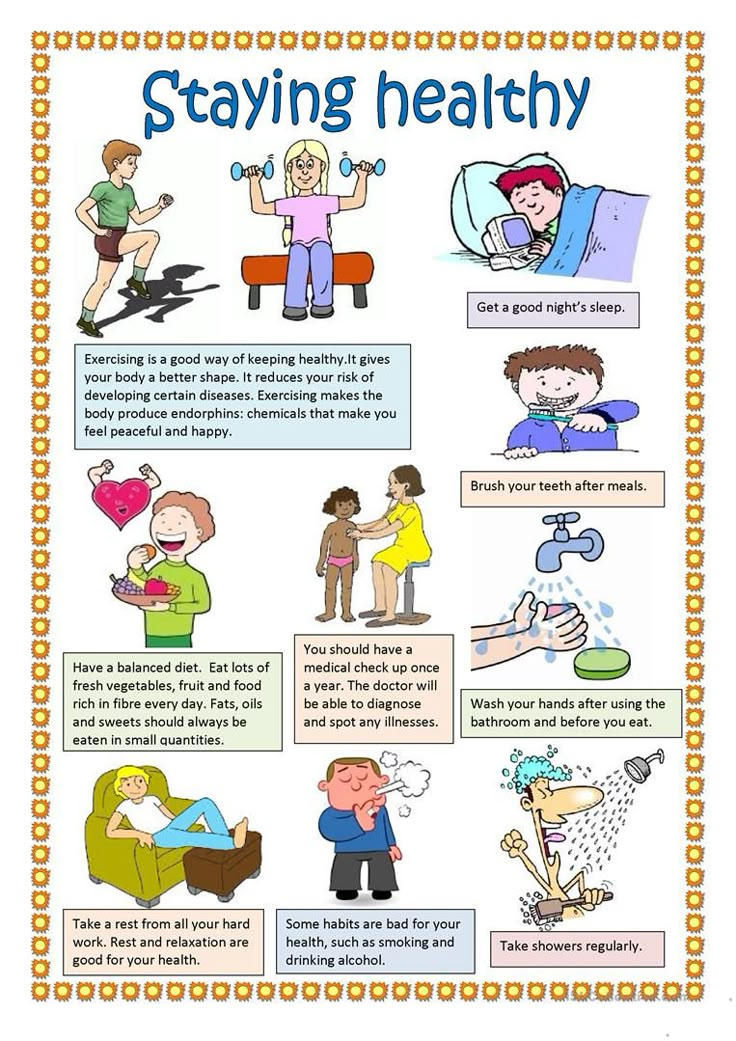
- Avoid negative coping skills. Substance use, risky sexual activity, reenacting the trauma, or other negative copying skills may temporarily relieve trauma symptoms but don’t provide long-term healing.
- Ground yourself. Grounding techniques help keep you in the present during flashbacks, panic attacks or intrusive thoughts. Count backwards from five and, with each number, notice what is around you: five things you see, four you hear, three you can touch, two you smell and one you can taste.
- Practice self-care.
Relaxation techniques such as meditation, exercise, exploring nature, or other activities that promote wellness can help relieve symptoms.
- Social support. The support of friends, family or a faith community are an important part of trauma healing. Sharing your experiences in a non-judgmental environment helps prevent PTSD from developing.
- Therapy. One-on-one or group therapy can provide immense healing from trauma. These can include evidence-based treatments for traumatic stress for people of all ages. A professional therapist may identify patterns and behaviors that prevent healing and help relieve negative symptoms. Visit health.maryland.gov for mental health resources near you.
Just like trauma responses, healing looks different for everyone. Some people may benefit from more than one healing method. Speak to a health care provider for guidance as needed.
Trauma Response in Children
Children can experience trauma similarly to adults, from some of the same types of events. Yet some traumatic events are specific to childhood, including loss of a caretaker or bullying in school.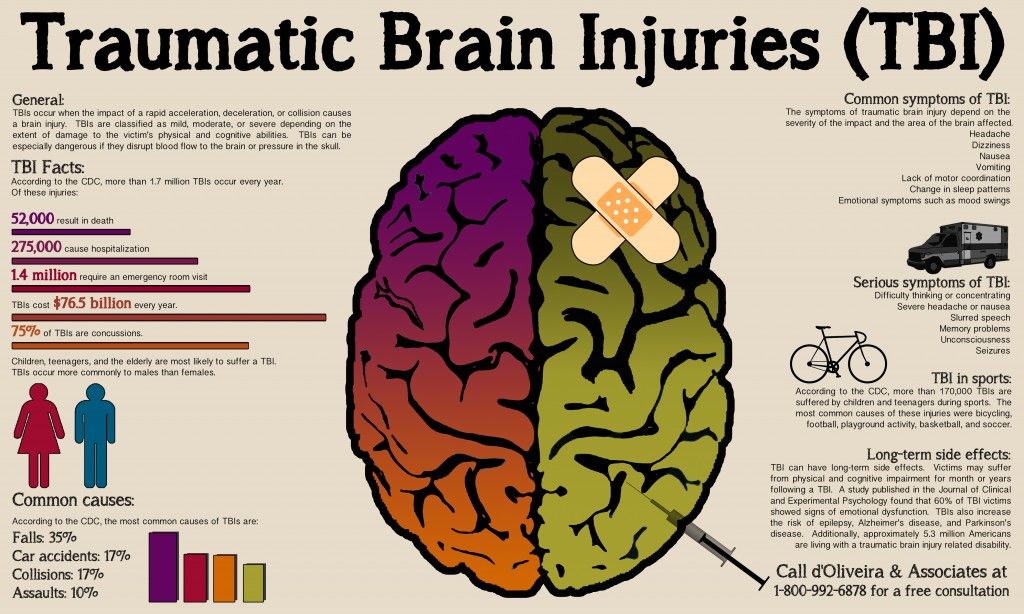
According to the U.S. Department of Health and Human Services, two-thirds of children reported at least one traumatic event by the age of 16. Treating childhood trauma can prevent future problems including learning disorders, behavioral health issues and substance use disorders.
A child’s trauma response may vary by age and individual. It can include:
- Eating disorders or self-harming behaviors
- High-risk sexual behavior
- Problems sleeping and/or nightmares
- Substance abuse
- Tantrums, excessive crying or displays of fear
- Trouble concentrating at home and at school
- Weight gain or loss
Children are capable of healing from trauma like adults. Access to a supportive care network, whether at home, at school or from professionals, is important. The National Child Traumatic Stress Network has resources available for anyone helping children cope with trauma.
Treating Traumatic Injuries at UMMS
While they can sometimes go hand in hand, physical trauma needs a much different approach than emotional trauma.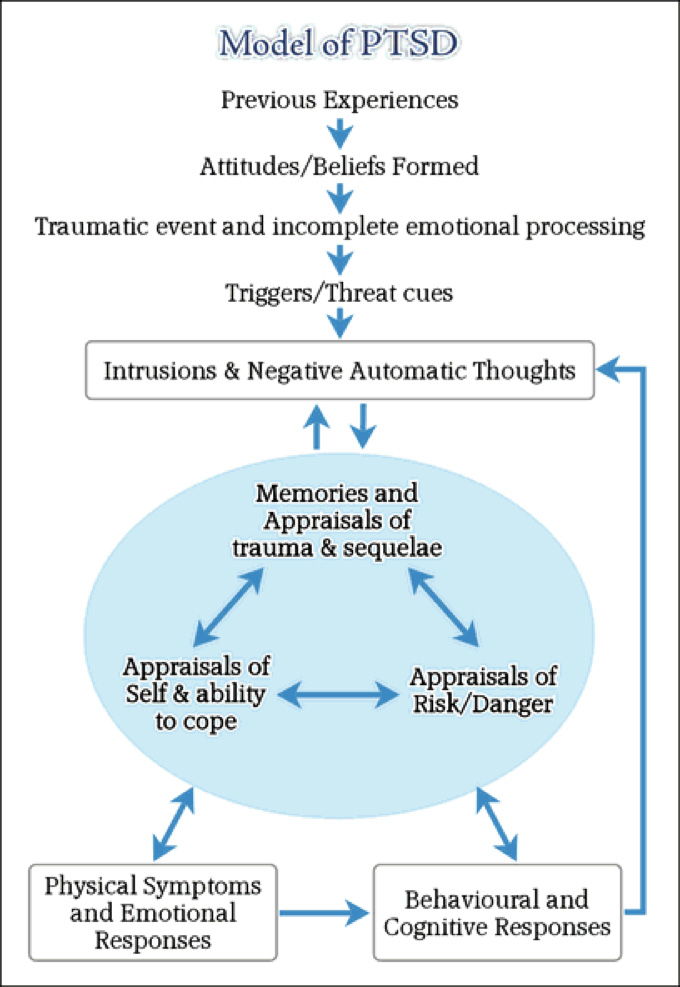 UMMS has experienced medical providers and support staff able to treat individuals who have experienced traumatic injuries. A traumatic injury can alter a patient’s life in many ways. The Shock Trauma Outpatient Pavilion provides follow-up care to all trauma patients. A referral-based clinic, the Shock Trauma Outpatient Pavilion provides physical and mental health services to survivors of traumatic injury.
UMMS has experienced medical providers and support staff able to treat individuals who have experienced traumatic injuries. A traumatic injury can alter a patient’s life in many ways. The Shock Trauma Outpatient Pavilion provides follow-up care to all trauma patients. A referral-based clinic, the Shock Trauma Outpatient Pavilion provides physical and mental health services to survivors of traumatic injury.
Hope in Healing
Surviving trauma and traumatic injury can be difficult. Health care providers at UMMS can be an active member of a patient’s support team. Healing from trauma is possible and there’s reason to hope.
Listen to a Podcast
Important ways to take part in suicide prevention is to understand the issues concerning suicide. Know the risk factors, identify the warning signs, learn how to help others in crisis and change the conversation around suicide. Jennifer Redding, LCSW-C, Executive Director of Behavioral Health at UM Upper Chesapeake Health, explains how to help prevent suicide.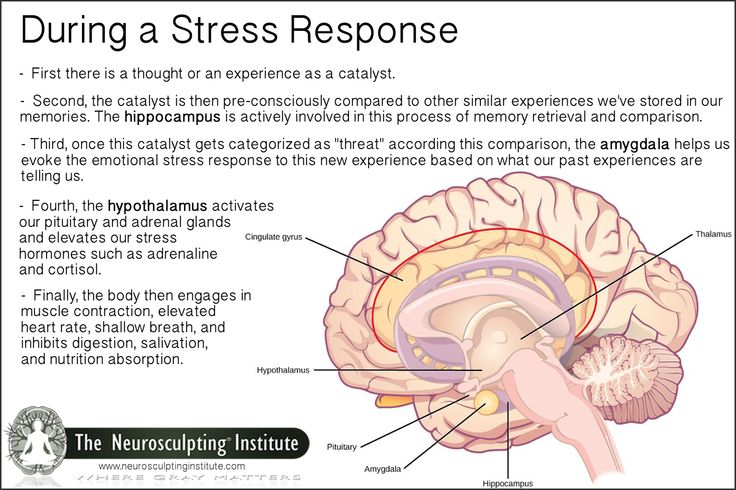
More to Read
- Suicide Prevention: How to Recognize Red Flags—and Where to Reach Out for Help
- Are You Experiencing Situational Depression?
- Feeling Depressed? Find Out How to Cope.
Find hope.
Learn more about the Trauma Survivors Network for survivors of a traumatic injury.
Learn More
GENERAL RESPONSE OF THE ORGANISM TO INJURY
Trauma is always accompanied by a violation of the general condition of the victim. Pain, blood loss, dysfunction of damaged organs, negative emotions, etc. contribute to the development of various pathological reactions of the body.
FAUNTE
Fainting - a sudden short-term loss of consciousness due to acute anemia of the brain. Under the influence of fright, acute pain, sometimes with a sharp change in position from horizontal to vertical, a person suddenly loses consciousness, becomes covered with cold sweat, turns pale sharply. At the same time, the pulse is slowed down, blood pressure is reduced, the pupils are constricted. Rapidly onset anemia of the brain sharply reduces the function of the motor and autonomic centers. Sometimes, before fainting, patients report dizziness, nausea, ringing in the ears, and blurred vision. nine0003
Rapidly onset anemia of the brain sharply reduces the function of the motor and autonomic centers. Sometimes, before fainting, patients report dizziness, nausea, ringing in the ears, and blurred vision. nine0003
Syncope usually lasts 1 to 5 minutes. A longer loss of consciousness indicates more severe pathological disorders in the body.
Treatment. The patient should be laid in a horizontal position, raise his legs, unfasten the collar, belt and all parts of clothing that restrict breathing. Let the ammonia vapor inhale to dilate the vessels of the brain.
COLLAPSE
Collapse (from Latin collapsus - to fall) is a serious condition of the body caused by acute cardiovascular insufficiency. In a complex combination of symptoms accompanying collapse, the main one is severe arterial hypotension. With injuries, the development of collapse is facilitated by damage to the heart, massive blood loss, and severe intoxication. nine0003
Clinical symptoms. In a severely bled patient or suffering from severe intoxication due to anaerobic infection, peritonitis or other diseases, collapse is manifested by general weakness, dizziness, dry throat, thirst, patients have a sharp pallor of the skin and mucous membranes, breathing is shallow, rapid, body temperature is lowered. Collapse in patients with severe injuries is accompanied by significant arterial hypotension, increased and weakened pulse, and loss of consciousness. nine0003
Collapse in patients with severe injuries is accompanied by significant arterial hypotension, increased and weakened pulse, and loss of consciousness. nine0003
The treatment of collapse should be pathogenetic, directed against the causes that caused this serious condition.
If there is blood loss, transfusion of blood and plasma substitutes should be quickly arranged. It is recommended to inject up to 3-4 liters of liquid intravenously. Salt solutions can also be injected under the skin. At the same time, drugs that stimulate the vasomotor and respiratory centers are used. Camphor (3 ml of a 20% solution), caffeine (2 ml of a 10% solution), adrenaline (0.5-1 ml of a 0.1% solution), ephedrine (1-2 ml of a 5% solution) are injected subcutaneously. With collapse caused by severe intoxication, the use of strychnine is indicated (2 ml of a 0.1% solution 2-3 times a day). nine0003
TRAUMATIC SHOCK
Traumatic shock is a severe pathological process that occurs in the body as a general reaction to severe mechanical damage to tissues and organs.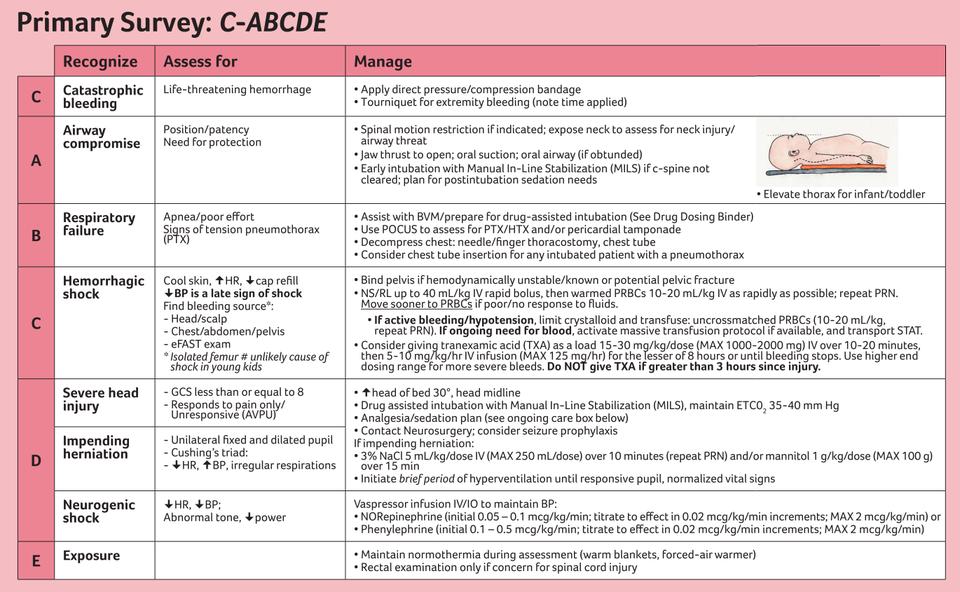 This process is characterized by increasing inhibition of the basic vital functions of the body due to violations of nervous regulation, hemodynamics, respiration and metabolic processes.
This process is characterized by increasing inhibition of the basic vital functions of the body due to violations of nervous regulation, hemodynamics, respiration and metabolic processes.
The severe condition of the victims is primarily associated with massive blood loss, acute respiratory failure, acute disorders of the functions of damaged vital organs (brain, heart), fat embolism, etc. Shock should be expected in patients with multiple bone fractures lower extremities, pelvis, ribs, with damage to internal organs, with open fractures with extensive crushing of soft tissues, etc.
In the clinical picture of traumatic shock, hemodynamic disturbances are most pronounced. The main hemodynamic parameters are: blood pressure, pulse rate, cardiac output (CO), circulating blood volume (CBV) and CVP. The critical level of blood pressure is 70 mm Hg. Art., below which begins the process of irreversible changes in vital organs (brain, heart, kidneys, liver, lungs). You can roughly determine the dangerous level of blood pressure by the pulsation of the main arteries.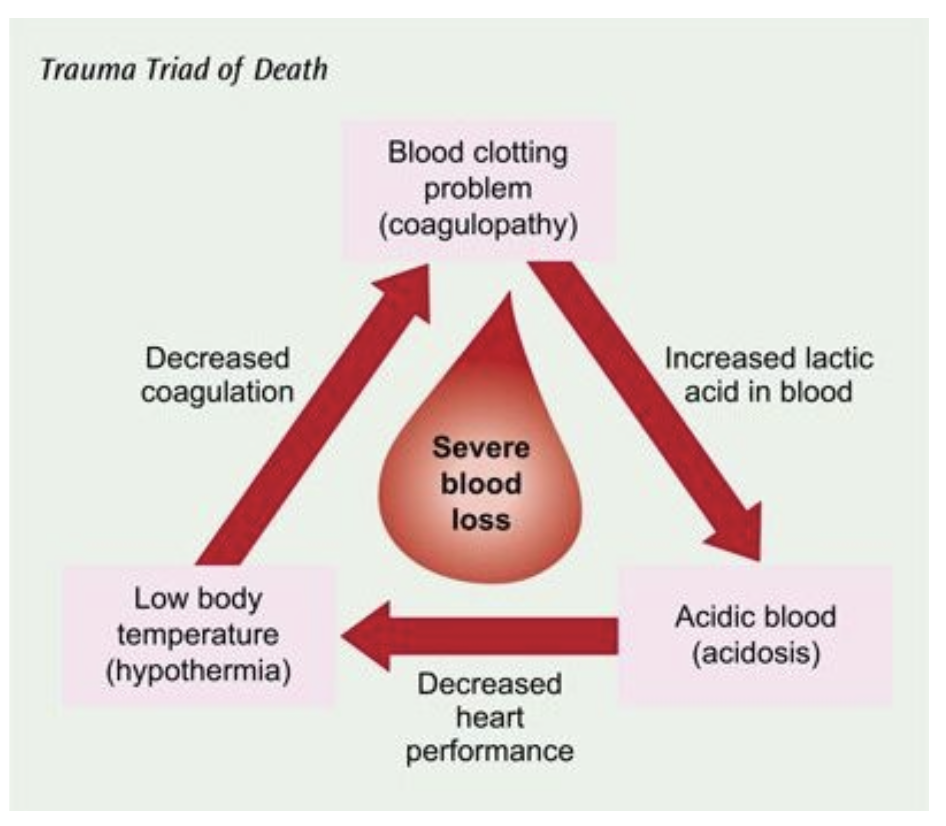 If it is not possible to palpate the pulsation of the radial arteries, but the pulsation of the femoral arteries is preserved, then we can assume that the blood pressure fluctuates around a critical level. If the pulsation is determined only on the carotid arteries, then the blood pressure is below critical. "Threaded", periodically disappearing pulse indicates a decrease in blood pressure below 50 mm Hg. Art., which is typical for the terminal state and the development of dying processes. nine0003
If it is not possible to palpate the pulsation of the radial arteries, but the pulsation of the femoral arteries is preserved, then we can assume that the blood pressure fluctuates around a critical level. If the pulsation is determined only on the carotid arteries, then the blood pressure is below critical. "Threaded", periodically disappearing pulse indicates a decrease in blood pressure below 50 mm Hg. Art., which is typical for the terminal state and the development of dying processes. nine0003
A change in heart rate is an earlier sign of a circulatory disorder than blood pressure.
The safe limit for increased heart rate is 220 -V, where B is the patient's age in years, with more frequent contractions there is a threat of exhaustion of the heart muscle as a result of developing hypoxia.
A pronounced increase (120 beats / min or more) with satisfactory arterial pressure indicates occult bleeding.
More precisely, the amount of blood loss can be judged by the shock index (SHI) proposed by Algover (Table 1):
SHI = heart rate / blood pressure,
where heart rate - heart rate, beats / min; BP - blood pressure, mm Hg. Art.
Art.
DOCC \u003d Mx K,
where DOCC is the due BCC, ml; M - body weight, kg; K - constitutional factor, ml/kg; for obese people K = 65 ml / kg, for asthenics K = 70
ml / kg, for athletes K = 80, for the average person K = 75 ml / kg.
With closed fractures of the lower leg, blood loss up to 0.5 liters should be expected, in the hip - up to 1.5 liters, in the pelvis - up to 3.5 liters.
Clinical signs of impaired regional hemodynamics. Severe pallor of the skin and cold skin to the touch indicate circulatory disorders in the skin and muscles. A parametric indication of these disorders is possible, determined by the time of refilling the capillaries of the patient's forearms or lips with blood after pressing with a finger. This time is normally 2 s. An increase in this period indicates a violation of blood circulation in this zone. This sign is important for predicting the outcome of the injury. nine0003
Hemocirculation disorders reduce the rate of diuresis to 40 ml/h or less.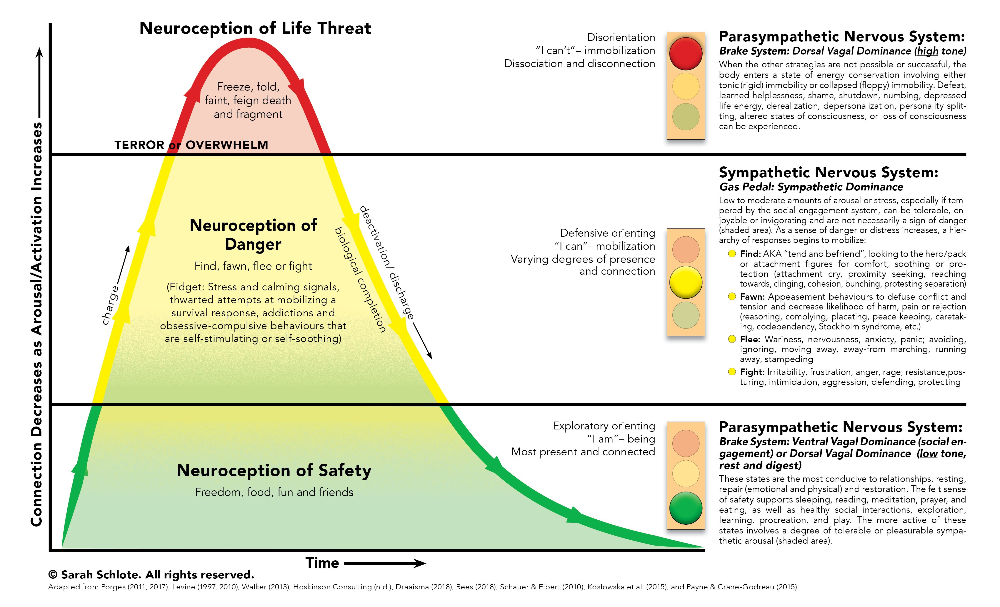 Insufficiency of cerebral blood flow affects the nature of consciousness (stunning, stupor). However, this symptom is rare in patients with traumatic shock, due to the phenomenon of centralization of blood circulation, which ensures adequate blood circulation in the brain, up to the development of a terminal state. More complete information about the state of regional blood circulation can be obtained using impedance rheography. nine0003
Insufficiency of cerebral blood flow affects the nature of consciousness (stunning, stupor). However, this symptom is rare in patients with traumatic shock, due to the phenomenon of centralization of blood circulation, which ensures adequate blood circulation in the brain, up to the development of a terminal state. More complete information about the state of regional blood circulation can be obtained using impedance rheography. nine0003
In the clinical picture of traumatic shock, erectile and torpid phases are distinguished. The erectile phase is characterized by a general excitation of the patient. The victim
is restless, verbose, fussy, extremely and erratically mobile. The pulse is accelerated (up to 100 beats / min), blood pressure rises abruptly, while the pulse pressure reaches 80-100 mm Hg. Art., breathing uneven, frequent, up to 30-40 in 1 min. The appearance of an excited patient, as a rule, does not correspond to the significant severity of his injuries. nine0003
The torpid phase of traumatic shock is characterized by inhibition of all vital functions of the organism. The victim is inhibited, indifferent to the environment, to his condition, his pain sensitivity is reduced, blood pressure drops, the pulse is frequent, of weak filling, breathing is shallow, rapid. Depending on the severity of the condition of the victim, the torpid phase of shock is conditionally divided into 4 degrees.
The victim is inhibited, indifferent to the environment, to his condition, his pain sensitivity is reduced, blood pressure drops, the pulse is frequent, of weak filling, breathing is shallow, rapid. Depending on the severity of the condition of the victim, the torpid phase of shock is conditionally divided into 4 degrees.
/ degree: consciousness is preserved, moderate pallor of the skin and mucous membranes, blood pressure 85100 mm Hg. Art., rhythmic pulse, satisfactory filling, 90-100 beats / min, SI "0.8, blood loss up to 1000 ml.
II degree: consciousness is preserved, depression, lethargy are expressed, skin and mucous membranes are pale, blood pressure is 70-90 mm Hg. Art., pulse 100-120 beats / min, weak filling, SI = (0.9 ... 1.2), blood loss - 1500 ml.
III degree: consciousness is preserved (if the brain is not damaged), the skin and mucous membranes are sharply pale, weakness, blood pressure is below 70 mm Hg. Art., thready pulse, 130-140 beats / min, SHI "1.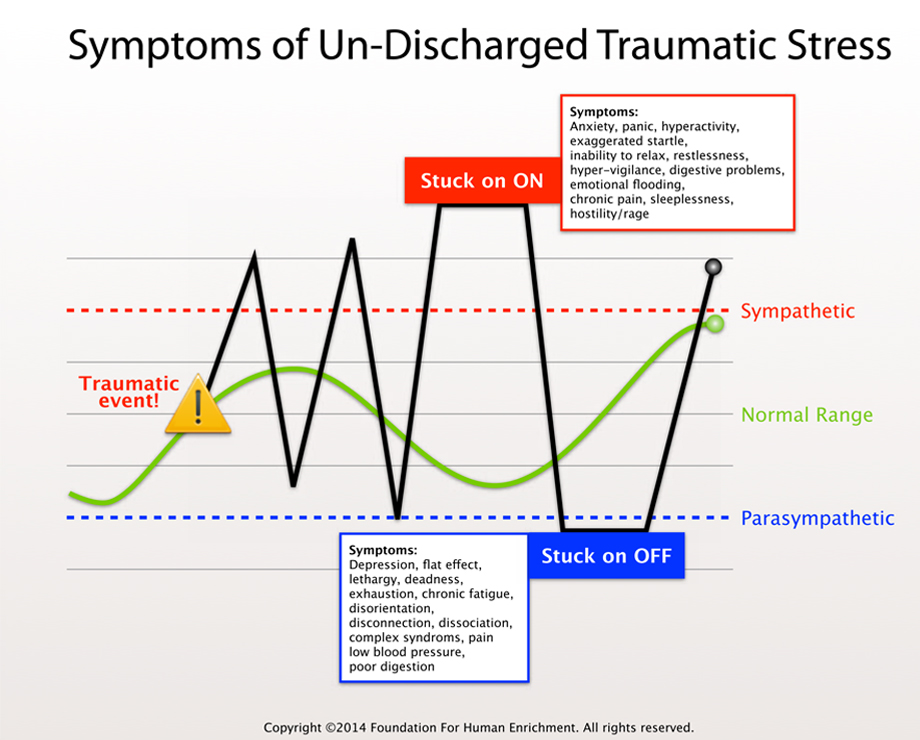 3, blood loss - more than 1500 ml. nine0003
3, blood loss - more than 1500 ml. nine0003
IV degree - a terminal state in which three stages are distinguished (according to VA. Negovsky): preagonal state, atonal state and clinical death.
Preagonal state - consciousness is confused or absent. The skin and mucous membranes are grayish-pale (“earthy”), the body temperature is reduced. Blood pressure and pulse on the peripheral arteries are not determined, the pulse on the carotid and femoral arteries is determined with difficulty, filiform, disappearing, up to 140-150 beats / min, but may be less often. Breathing is shallow, rather rhythmic, blood loss is more than 2000 ml. nine0003
An agonal state - consciousness is absent, weakness, breathing becomes periodic, convulsive, accompanied by general motor excitation, intervals between breaths increase. Flashes of sharp hypoxic excitation are possible. There are general tonic convulsions, involuntary urination, defecation.
Clinical death is the state of the body after the disappearance of all clinical manifestations of life (cessation of blood circulation, cardiac activity, pulsations in all arteries, respiration, complete disappearance of all reflexes).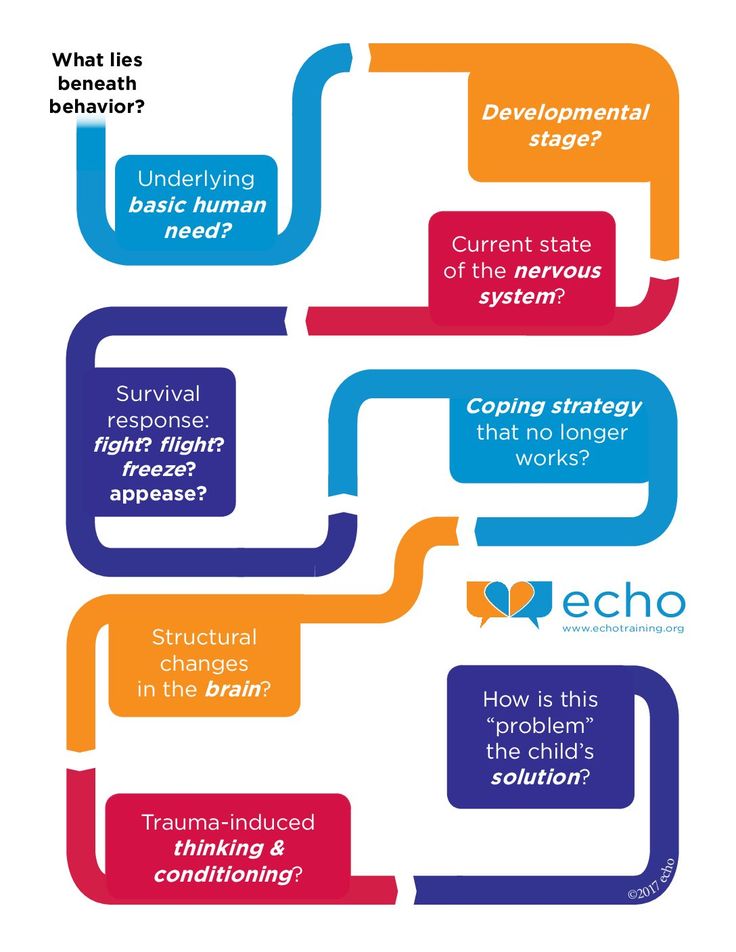 This state lasts an average of 5 minutes (from the moment the pulsation on the carotid arteries ceases), however, with a long previous preagonal state (more than 1-2 hours), the duration of clinical death may be less than 1 minute; on the contrary, with sudden cardiac arrest against the background of sufficiently high hemodynamic parameters, the duration of clinical death can increase up to 7-8 minutes, and with a decrease in brain temperature (hypothermia) - up to 10 minutes or more. During this period, it is still possible to restore the vital activity of the cells of the cerebral cortex with the resumption of cerebral blood flow. If irreversible changes occur in the cells of the cerebral cortex and they die, then we should talk about the onset of brain death. In this state, with the help of active resuscitation, it is possible to restore the activity of the heart and breathing, but it is impossible to restore the function of the cerebral cortex. Clinical signs of decortication of the brain are the maximum dilation of the pupils and their complete absence of reaction to light after the restoration of blood circulation and respiration.
This state lasts an average of 5 minutes (from the moment the pulsation on the carotid arteries ceases), however, with a long previous preagonal state (more than 1-2 hours), the duration of clinical death may be less than 1 minute; on the contrary, with sudden cardiac arrest against the background of sufficiently high hemodynamic parameters, the duration of clinical death can increase up to 7-8 minutes, and with a decrease in brain temperature (hypothermia) - up to 10 minutes or more. During this period, it is still possible to restore the vital activity of the cells of the cerebral cortex with the resumption of cerebral blood flow. If irreversible changes occur in the cells of the cerebral cortex and they die, then we should talk about the onset of brain death. In this state, with the help of active resuscitation, it is possible to restore the activity of the heart and breathing, but it is impossible to restore the function of the cerebral cortex. Clinical signs of decortication of the brain are the maximum dilation of the pupils and their complete absence of reaction to light after the restoration of blood circulation and respiration.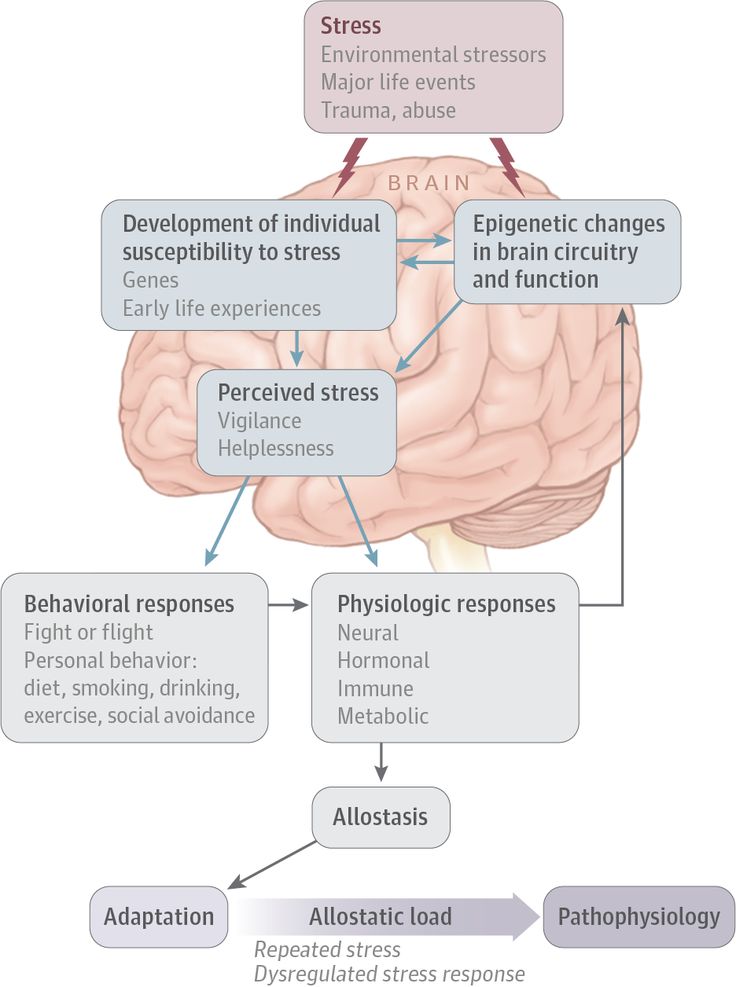 After the death of all structures (departments) of the central nervous system, biological death occurs, although it is possible to temporarily restore the vital activity of individual organs and tissues with the resumption of blood flow in them, however, it is no longer possible to restore the life of the organism as a whole. nine0003
After the death of all structures (departments) of the central nervous system, biological death occurs, although it is possible to temporarily restore the vital activity of individual organs and tissues with the resumption of blood flow in them, however, it is no longer possible to restore the life of the organism as a whole. nine0003
Particularly severe is the course of shock in patients with fractures of the bones of the extremities in combination with fractures of the ribs, spine, and pelvis. The causes of such severe injuries are car accidents, falls from a height, landslides in mines, etc. The most severe group consists of victims with simultaneous damage to several areas of the body, for example, skeletal fractures, ruptures of internal organs, TBI.
Treatment. The provision of early assistance for injuries complicated by shock continues to be one of the main problems in industrial enterprises, agriculture, and large construction sites. In cities, this assistance is provided by specialized resuscitation teams that quickly leave for the scene.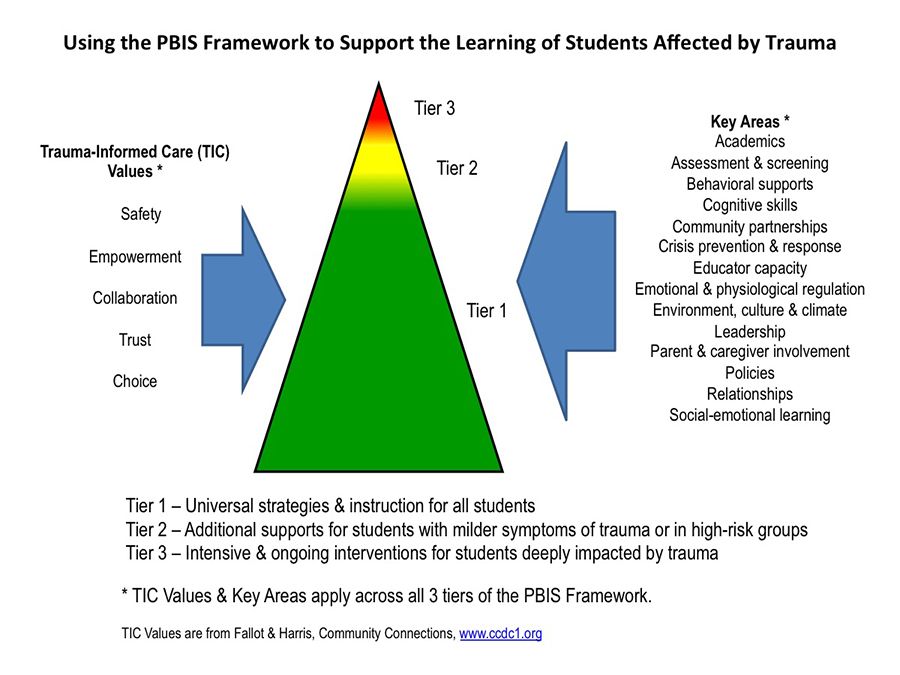 nine0003
nine0003
Resuscitation should be understood not only as the restoration of the vital activity of an organism that is in a state of clinical death, but also all measures aimed at preventing cardiac and respiratory arrest. The main tasks of resuscitation are:
- restoration of cardiac activity, blood circulation and creation of the most favorable conditions for blood supply to the brain;
- restoration of gas exchange in the lungs;
- restoration of the BCC. nine0003
In practice, only the first tasks can be solved at the scene of the accident, and before the arrival of medical workers, only
people around the victim will be able to provide real assistance. Therefore, simple methods of restoring cardiac activity and respiration should be mastered not only by doctors and nursing staff, but by all people.
The main methods of resuscitation are indirect (external) heart massage and mechanical ventilation by blowing air through the victim's mouth or nose (Fig. 8).
8).
Technique of chest compressions. The principle of indirect massage is
periodic compression of the heart between the sternum and the spine, while at the moment of compression, the blood is pushed out of the cavity of the heart into the aorta and pulmonary arteries, and after the cessation of compression, it enters the cavity of the heart from the veins. The absolute indication for the beginning of an indirect heart massage is the cessation of the pulsation of the carotid arteries. The victim is quickly placed on a rigid base or a shield is placed under the back and the sternum is jerkily shifted to the spine 60-120 times in 1 min. Pressure is applied with both hands, while the base of the palm of the right hand is placed on the lower third of the sternum, and the palm of the left hand rests on the right hand from above. If the heart massage is carried out effectively, then a distinct pulsation appears on the carotid arteries, the pupils narrow, the lips turn pink, blood pressure rises to 6080 mm Hg. Art. In children, massage should be done with only one hand, and in newborns - only with your fingers. In this case, complications are possible: fractures of the ribs, sternum, damage to the heart, liver, spleen and other organs. nine0003
Art. In children, massage should be done with only one hand, and in newborns - only with your fingers. In this case, complications are possible: fractures of the ribs, sternum, damage to the heart, liver, spleen and other organs. nine0003
Artificial lung ventilation technique (ALV). It should be noted that squeezing the chest during heart massage restores to some extent the ventilation of the lungs, and thus the gas exchange in them. However, for full ventilation, it is necessary to blow air into the lungs of the victim through the mouth or nose. It is first necessary to check the patency of the upper respiratory tract: insert a finger into the victim’s mouth to determine the presence or absence of foreign bodies (teeth, prostheses, etc.), stretch out the tongue, push the victim’s chin, place a roller under the shoulders so that the head is tilted back, and the neck is arched (if there are no symptoms of a fracture of the cervical vertebrae!). If it is possible to apply the “mouth-to-mouth” method, then after closing the patient’s nasal passages, the resuscitator takes a deep breath and blows air into the victim’s mouth with force until the chest rises, then quickly moves away and takes a deep breath, the victim at this time makes a passive exhalation. The first 5-10 breaths must be done quickly (to eliminate life-threatening hypoxia), then at a frequency of 1220 breaths per 1 minute until spontaneous breathing occurs. If the victim develops bloating, then it is necessary to gently press the area of \u200b\u200bthe stomach with your hand, without stopping the blows. If the victim has a jaw injury or a severe spasm of the masticatory muscles occurs, then mechanical ventilation is carried out through the nose. If it is not possible to carry out mechanical ventilation by blowing air, then rhythmic compression of the chest can be applied, followed by raising the hands of the victim after the pressure stops. nine0003
The first 5-10 breaths must be done quickly (to eliminate life-threatening hypoxia), then at a frequency of 1220 breaths per 1 minute until spontaneous breathing occurs. If the victim develops bloating, then it is necessary to gently press the area of \u200b\u200bthe stomach with your hand, without stopping the blows. If the victim has a jaw injury or a severe spasm of the masticatory muscles occurs, then mechanical ventilation is carried out through the nose. If it is not possible to carry out mechanical ventilation by blowing air, then rhythmic compression of the chest can be applied, followed by raising the hands of the victim after the pressure stops. nine0003
When performing ventilation, it is advisable to use an S-shaped airway and a portable manual respirator.
8. Resuscitation in clinical death, a - closed heart massage; 6 - artificial ventilation of the lungs.
Bleed loss control should be started at the scene by temporarily stopping bleeding. The restoration of the BCC, as a rule, is postponed until the victim is hospitalized in the intensive care unit of a multidisciplinary hospital.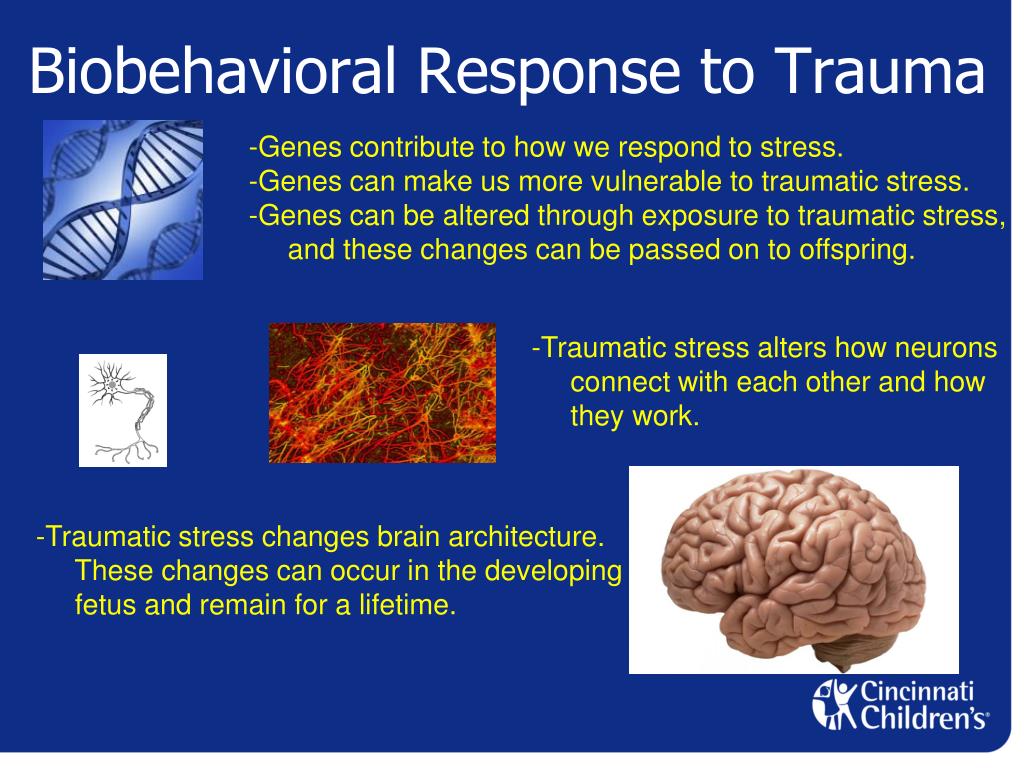
If resuscitation is carried out in a medical setting, then additional medical therapy and defibrillation can be used. To increase the tone of the heart muscle, 1 ml of a 0.1% solution of adrenaline and 5 ml of a 10% solution of calcium chloride are administered intracardiacly. If erratic contractions of myocardial fibers occur, as seen on the ECG, defibrillation is indicated. The electrodes are pre-wrapped with gauze napkins moistened with an isotonic sodium chloride solution, one is placed under the back at the level of the left shoulder blade, the other is pressed tightly against the anterior surface of the chest to the left of the sternum. The electrodes are supplied with a voltage of 2 to 4 kV from the defibrillator. nine0003
After removing the victim from the state of clinical death, it is necessary to carry out intensive therapy within 2-3 days: to carry out mechanical ventilation (with automatic respirators), correction of metabolic acidosis (administration of large doses of corticosteroids, ascorbic acid, concentrated protein solutions), correction of water and electrolyte balance, protein-carbohydrate metabolism and prevention of infectious complications.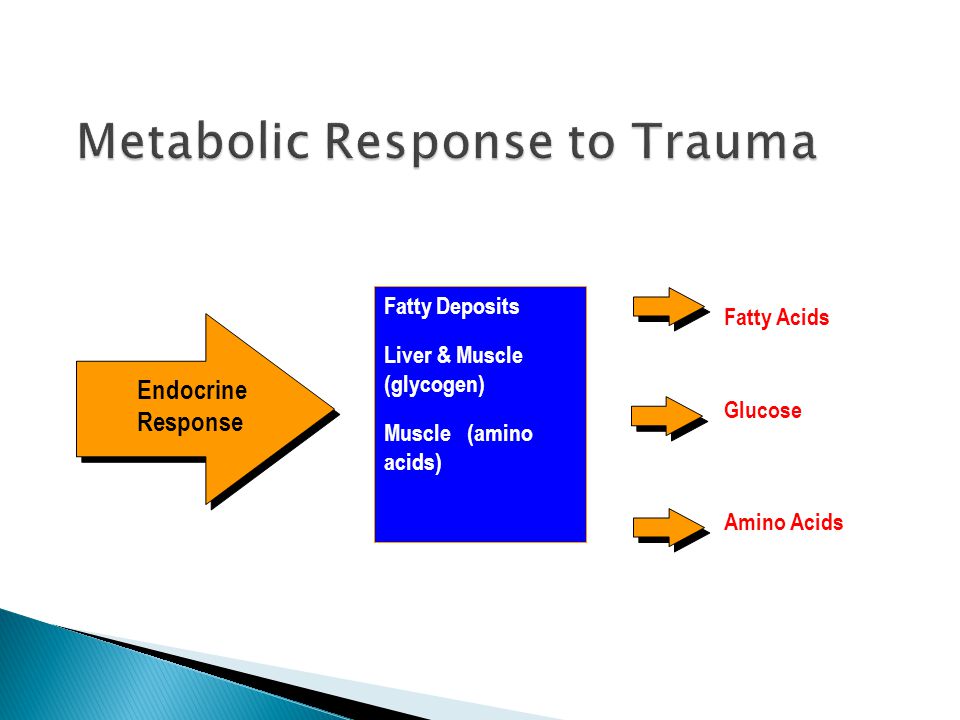
If active resuscitation for 30-40 minutes is not effective (cardiac activity and spontaneous breathing are not restored, the pupils remain as dilated as possible without any reaction to light), then resuscitation should be stopped and the onset of biological death should be ascertained. One of the reliable signs of the onset of biological death is the phenomenon of the "cat's eye", which consists in the fact that when the eyeball is squeezed, the pupil acquires an oval shape (in a living person, the shape of the pupil does not change). This symptom is observed 1 0 - 1 5 minutes after the onset of biological death. nine0003
Resuscitation is inappropriate for severe head injury with severe skull deformity; crushed chest with signs of damage to the internal organs of the abdomen and massive blood loss; severe combined injuries of three or more areas of the body
(for example, avulsion of both thighs in combination with intra-abdominal bleeding and severe TBI). All measures to bring victims out of shock can be conditionally divided into 4
groups: combating blood loss; fight against ODN; the fight against pain and the fight against metabolic disorders.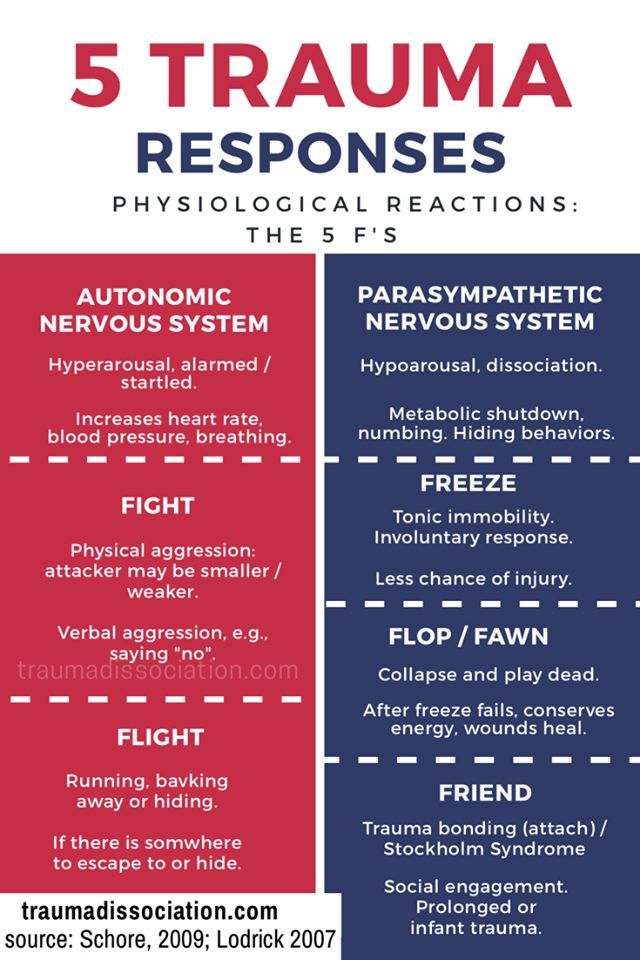 nine0003
nine0003
Effective replenishment of BCC in case of blood loss is possible only after bleeding has stopped. Therefore, victims with intracavitary bleeding must be urgently operated according to vital indications, regardless of the severity of the general condition. Procrastination with surgery is disastrous for them. In acute massive blood loss, the decisive factor is the rapid replenishment of the BCC by intravenous (in two or more veins simultaneously) infusions at high speed (100-150 ml/min) ). Blood transfusion is a powerful anti-shock remedy, but it should be performed only after careful selection of donor blood and all necessary compatibility tests. The more severe the hemodynamic disorders, the greater should be the volume of transfusion therapy. nine0003
The volume of infused fluid in severe shock on the 1st day should be at least 3-4 liters (of which 50% whole blood), in terminal conditions - 6-8 liters (80% blood). Criteria for reducing the rate and volume of transfusion therapy are: increase in blood pressure to 100 mm Hg. Art., pulse rate 90-100 beats / min, satisfactory filling in the peripheral arteries, the appearance of pink lips, warming of the skin. Intra-arterial transfusions are indicated in the absence of the effect of intravenous infusions, more often they are used in a complex of resuscitation measures. nine0003
Art., pulse rate 90-100 beats / min, satisfactory filling in the peripheral arteries, the appearance of pink lips, warming of the skin. Intra-arterial transfusions are indicated in the absence of the effect of intravenous infusions, more often they are used in a complex of resuscitation measures. nine0003
Complications of transfusion therapy: development of acute cardiovascular failure, pulmonary edema, pneumonia.
Oxygen inhalation is used for the treatment of ARF, mechanical ventilation is carried out using automatic respirators, and respiratory analeptics are administered.
Ensuring good airway patency is a necessary condition for the normalization of lung ventilation and the prevention of post-traumatic pulmonary complications. Cleaning of the tracheobronchial tree, nasopharyngeal cavity and mouth is carried out by regular suction of pathological contents through sterile catheters or probes. The effectiveness of the procedure is ensured by a sufficient vacuum in the system (at least 30-40 mm Hg) and a wide lumen of the catheter (at least 3-4 mm).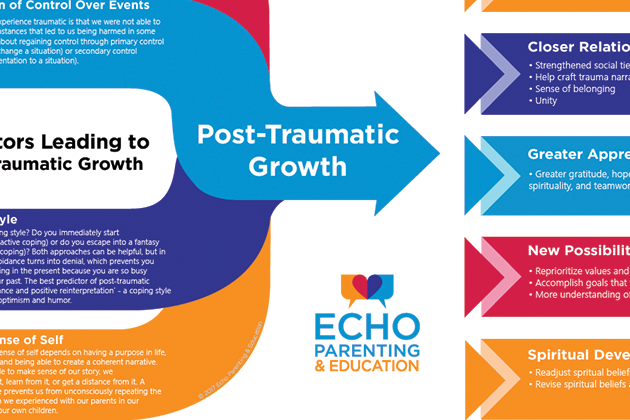 nine0003
nine0003
The duration of suction should not exceed 10-15 s, since during this period ventilation deteriorates sharply. The indication for the transfer of the victim to a ventilator is, as a rule, an extreme degree of ARF. Half-sitting position, insufflation of humidified oxygen through nasal catheters, prevention of tongue retraction, etc. improve respiratory function. carry out mechanical ventilation for many days (Fig. 9).
Pain control is one of the important anti-shock measures. At the scene, analgesics (promedol, morphine) are administered, novocaine blockades (Fig. 10) of fracture sites (40-80 ml of a 0.5% solution), case blockade (100 ml of a 0.5% solution), conduction blockade (20-30 ml 1% solution), cross-section above the applied tourniquet (200-300 ml of 0.25% solution), vagosympathetic (40-60 ml of 0.5% solution), intrapelvic (200 ml of 0.25% solution), mask superficial anesthesia is given nitrous oxide mixed with oxygen
(1:1). Mandatory measures to combat the pain factor are careful immobilization of injured limbs and gentle transportation of the victim. The use of narcotic analgesics is contraindicated in case of head injury, signs of damage to the internal organs of the abdomen, with damage to the cervical spine, in a terminal state, with severe chest injuries. In a specialized anti-shock department to deal with shock
The use of narcotic analgesics is contraindicated in case of head injury, signs of damage to the internal organs of the abdomen, with damage to the cervical spine, in a terminal state, with severe chest injuries. In a specialized anti-shock department to deal with shock
9. Types of tracheotomy. a - thyrotomy; 6 - conicotoia; c - cricotomy; d - upper tracheotomy; e — lower tracheotomy. nine0003
10. Novocaine blockades.
a - blockade of the fracture site; b - case blockade; in - blockade of cross section; d - cervical vagosympathetic blockade according to Vishnevsky;
d - blockade of the pelvis according to Shkolnikov-Selivanov (1, 2, 3 - changes in the position of the needle when moving it deep into the pelvis).
neuroleptics, ganglion blockers, neuro-leptanalgesia, endotracheal anesthesia can be used.
To correct the acid-base state, sodium bicarbonate (150-200 ml of a 4-5% solution), calcium chloride (10-20 ml of a 10% solution), B vitamins, ascorbic acid, and glucose are injected intravenously.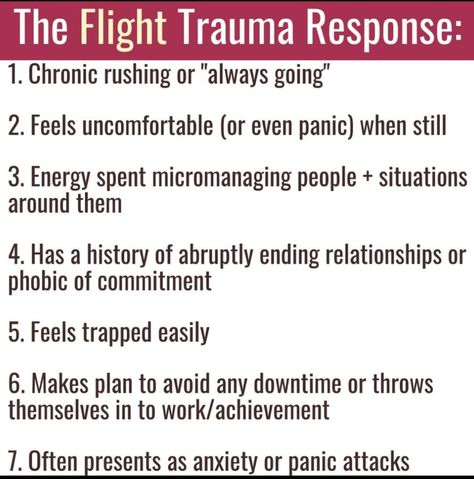 To normalize metabolism, hormonal preparations are used: ACTH (up to 100 U / day), hydrocortisone (up to 250 ml / day), prednisolone (up to 60 mg / day). nine0003
To normalize metabolism, hormonal preparations are used: ACTH (up to 100 U / day), hydrocortisone (up to 250 ml / day), prednisolone (up to 60 mg / day). nine0003
Antishock therapy requires constant dynamic monitoring of biochemical changes in the blood and urine, monitoring of the excretory function of the kidneys, the body's temperature reactions, and the function of the gastrointestinal tract.
Traumatic stress
Traumatic stress is a special form of the general stress reaction. When stress exceeds the psychological, physiological, adaptive capabilities of a person and destroys the defense, it becomes traumatic. nine0003
The following four characteristics of injury were identified:
1) the event that has occurred is realized, that is, the person knows what happened to him and because of which his psychological state worsened;
2) this state is due to external causes;
3) experience destroys habitual way of life;
4) the event that happened causes horror and a feeling of helplessness, impotence to do or undertake anything. nine0003
nine0003
Traumatic stress is a special kind of experience, the result of a special interaction between a person and the surrounding world. This is a normal reaction to abnormal circumstances, a condition that occurs in a person who has experienced something that goes beyond the normal human experience, such as a threat to their physical health or their own life, the death or injury of another person, participation in hostilities, violence, natural disaster and disaster, etc. nine0003
The psychological reaction to trauma includes three relatively independent phases, which allows us to characterize it as a process unfolded over time.
1. Psychological shock phase:
• inhibition of activity, disorientation in the environment, disorganization of activity;
• Denial of what happened is a kind of protective reaction of the psyche (normally, this phase is rather short-lived). nine0185 2. Expressed emotional reactions to the event and its consequences:
Expressed emotional reactions to the event and its consequences:
• strong fear, horror, anxiety, anger, crying, accusation - emotions that are characterized by immediacy of manifestation and extreme intensity;
• Gradually these emotions are replaced by a reaction of criticism or self-doubt. It proceeds according to the "what would happen if ..." type and is accompanied by a painful awareness of the inevitability of what happened, the recognition of one's own powerlessness and self-flagellation. A typical example is the feeling of "survivor's guilt" described in the literature, which often reaches the level of deep depression. The phase under consideration is critical in the sense that after it either the process of recovery begins (reaction, acceptance of reality, adaptation to newly arisen circumstances), that is: nine0003
3. a) normal response phase;
b) fixation on the trauma and subsequent chronization of the post-stress state.