What does inpatient treatment mean
What is Inpatient vs Outpatient Care?
What is outpatient care?
Outpatient care—the kind that you don’t have to stay in a hospital for—can vary greatly. Other than an annual check-up or blood test, almost any other kind of care can be defined as outpatient. These may be diagnostic tests, treatments, or other types of procedures.
Outpatient care may be provided in a hospital, as well as a walk-in clinic, an outpatient surgery center, and even your doctor’s office.
What determines if you need inpatient vs. outpatient care?
Whether you need outpatient or inpatient care is often determined by the type of care you require. Intensive care, around-the-clock care, major surgery, and treatment for a serious illness, are examples of medical situations that would require you to be admitted to the hospital.
On the other hand, there are plenty of minor surgeries, procedures, medical screenings, and treatments that do not require overnight stays or hospitalization.
What are some examples of inpatient care?
Types of inpatient care include:
- Serious illness, such as flu, stroke, heart attack
- Traumatic injury
- Severe burns
- Serious mental health issues, treatment for substance use disorder, and overdoses
- Chronic diseases, such as cancer and chronic obstructive pulmonary disease (COPD), that require specialized treatment and ongoing care
- Some cosmetic procedures requiring extensive plastic surgery or reconstruction
What are some examples of outpatient care?
Types of outpatient care include:
- Medical screenings such as mammogram, colonoscopy, and endoscopy
- Oral surgeries and other dental procedures, such as extractions, implants, root canal, and gum grafts
- Minor surgeries and procedures that don’t require advanced medical care, such as laser surgery, hand or foot surgery, mole removal, and Lasik eye surgery
- Certain types of treatment used for ongoing or long-term illnesses, such as dialysis and chemotherapy
What are the costs for outpatient vs.
 inpatient?
inpatient?
The costs for inpatient care can add up. In addition to the cost for the treatment or surgery you’re getting, there are many other costs associated with being cared for in a hospital, including:
- Administrative costs
- Pharmacy costs
- Lab tests
- Costs for nurses, radiologists, technicians, and specialists
- Equipment and supplies that contribute to your care while you’re there
- And more
The costs for outpatient care are typically considerably less than inpatient care. You often have some control over the costs too. For example:
- Costs for diagnostic radiology and imaging can vary greatly, so shop around for things like MRIs, PET, and CT scans to see how you can best keep your cost low.
- When it comes to needing unplanned medical care, understanding the difference between urgent care and the ER can ensure you don’t pay more than you need to.
- There are some outpatient screenings and procedures that are considered preventive care and covered by your plan. Things like a routine mammogram and colonoscopy are often covered 100% by your health plan.*
Learn more about how to pay less for out-of-pocket medical costs.
Do you have coverage for inpatient vs. outpatient health care?
Your health plan covers you for medical care, in general, regardless of whether it’s outpatient or inpatient. And some outpatient care may be covered 100% as part of your preventive care. Things like a routine mammogram or routine colonoscopy are examples of outpatient preventive care.
Here’s how your plan covers you for care and services:
- You pay for care and services until you meet your plan deductible.
- Once you meet your deductible, your health plan kicks in to start sharing costs as part of coinsurance. For example, you may pay 20% of the cost for services and your plan may pay the remaining 80%.
- If you hit your out-of-pocket maximum for the year—that’s the most you’re required to pay out-of-pocket—then your health plan will start paying 100% of the costs for your care.
Understanding the difference between inpatient vs. outpatient care and services can help give you more control over your health care. It gives you more control when you’re comparing health plans, when you’re planning ahead for a medical procedure or treatment, and anticipating costs for inpatient or outpatient services.
Inpatient vs. Outpatient: Differernt Types of Patient Care
Skip to content
More than ever, patients are engaged in their medical care, which is encouraging when you consider most medical school mission statements emphasize patient communication and education. It’s also worth noting that research shows providers are able to drive positive patient outcomes using a teach-back method that involves caring and clear language. Yet even well-informed individuals lack some knowledge, such as the distinction between inpatient versus outpatient care.
So what’s the difference, and why does it matter? This overview can help you advance your health literacy.
Inpatient vs. outpatient: Distinguishing the differences in care
What is an inpatient? In the most basic sense, this term refers to someone admitted to the hospital to stay overnight, whether briefly or for an extended period of time. Physicians keep these patients at the hospital to monitor them more closely.
With this in mind, what is outpatient care? Also called ambulatory care, this term defines any service or treatment that doesn’t require hospitalization. An annual exam with your primary care physician is an example of outpatient care, but so are emergent cases where the patient leaves the emergency department the same day they arrive. Any appointment at a clinic or specialty facility outside the hospital is considered outpatient care as well.
While there’s a clear difference between an inpatient and an outpatient, there is a little bit of gray area as well. Occasionally, physicians will assign a patient observation status while they determine whether hospitalization is required. This period typically lasts for no more than 24 hours.
Occasionally, physicians will assign a patient observation status while they determine whether hospitalization is required. This period typically lasts for no more than 24 hours.
Also note that the location itself doesn’t define whether you’re an inpatient versus outpatient. It’s the duration of stay, not the type of establishment, that determines your status.
Inpatient vs. outpatient: Comparing services
You’re probably starting to get a sense of the varying circumstances that fit under each category. To further recognize the difference between inpatient and outpatient care, review the below treatments and services that are common for these two types of care.
Inpatient care examples
- Complex surgeries, as well as some routine ones
- Serious illnesses or medical issues that require substantial monitoring
- Childbirth, even in cases that don’t require a cesarean section
- Rehabilitation services for psychiatric illnesses, substance misuse, or severe injuries
Outpatient care examples
- X-rays, MRIs, CT scans, and other types of imaging
- Lab tests, such as bloodwork
- Minor surgeries, particularly ones that use less invasive techniques
- Colonoscopies
- Mammograms
- Consultations or follow-ups with a specialist
- Routine physical exams
- Same-day emergent care, often treated at an urgent care facility versus the ER
- Chemotherapy or radiation treatment
Inpatient vs.
 outpatient: The providers in each setting
outpatient: The providers in each settingPrimary care physicians have traditionally been considered outpatient providers, while specialists are thought of as inpatient physicians. But that’s really an oversimplification, particularly when you consider that hospitalists bridge the gap by providing general medical care to inpatients. Effective care requires that doctors work together and effectively leverage health care technology, regardless of their specialties and settings.
Many physicians also divide their time between inpatient and outpatient services. OB/GYNs, for example, provide inpatient care when delivering babies and outpatient care when consulting with pregnant women during prenatal checkups.
Generally speaking, inpatients have contact with a larger group of providers. During a hospital stay, you could interact with physicians, nurse practitioners, lab technicians, physical therapists, pharmacists, and physician assistants.
Inpatient vs. outpatient: Cost considerations
The difference between inpatient versus outpatient care matters for patients because it will ultimately affect your eventual bill.
Outpatient care involves fees related to the doctor and any tests performed. Inpatient care also includes additional facility-based fees. The most recent cost data included in the Healthcare Cost and Utilization Project from the Agency for Healthcare Research and Quality (AHRQ) shows the average national inpatient charges can vary considerably depending on the length of stay and the treatment involved. The exact amount you pay also hinges on your insurance.
Things get a little more complicated if you have Medicare. Outpatient care and physician-related services for inpatient care are covered by Part B. Hospital services like rooms, meals, and general nursing for inpatients are covered by Part A.
But if you stay overnight in the hospital under observation status, Medicare still considers you an outpatient and will not cover care in a skilled nursing facility. It can certainly be confusing, so don’t be afraid to ask the medical team about your status. They’re used to these types of questions.
Expand your medical knowledge
Hopefully, you now have a little more clarity concerning the definition of inpatient versus outpatient. It can go a long way towards helping you understand what you should expect during and after any sort of medical treatment.
You can further deepen your understanding of the health care world by reading our article “50 Must-Know Medical Terms, Abbreviations, and Acronyms.”
*This article was originally published in June 2019. It has since been updated to reflect information relevant to 2021.
More than ever, patients are engaged in their medical care, which is encouraging when you consider most medical school mission statements emphasize patient communication and education. It’s also worth noting that research shows providers are able to drive positive patient outcomes using a teach-back method that involves caring and clear language. Yet even well-informed individuals lack some knowledge, such as the distinction between inpatient versus outpatient care.
So what’s the difference, and why does it matter? This overview can help you advance your health literacy.
Inpatient vs. outpatient: Distinguishing the differences in care
What is an inpatient? In the most basic sense, this term refers to someone admitted to the hospital to stay overnight, whether briefly or for an extended period of time. Physicians keep these patients at the hospital to monitor them more closely.
With this in mind, what is outpatient care? Also called ambulatory care, this term defines any service or treatment that doesn’t require hospitalization. An annual exam with your primary care physician is an example of outpatient care, but so are emergent cases where the patient leaves the emergency department the same day they arrive. Any appointment at a clinic or specialty facility outside the hospital is considered outpatient care as well.
While there’s a clear difference between an inpatient and an outpatient, there is a little bit of gray area as well. Occasionally, physicians will assign a patient observation status while they determine whether hospitalization is required. This period typically lasts for no more than 24 hours.
Occasionally, physicians will assign a patient observation status while they determine whether hospitalization is required. This period typically lasts for no more than 24 hours.
Also note that the location itself doesn’t define whether you’re an inpatient versus outpatient. It’s the duration of stay, not the type of establishment, that determines your status.
Inpatient vs. outpatient: Comparing services
You’re probably starting to get a sense of the varying circumstances that fit under each category. To further recognize the difference between inpatient and outpatient care, review the below treatments and services that are common for these two types of care.
Inpatient care examples
- Complex surgeries, as well as some routine ones
- Serious illnesses or medical issues that require substantial monitoring
- Childbirth, even in cases that don’t require a cesarean section
- Rehabilitation services for psychiatric illnesses, substance misuse, or severe injuries
Outpatient care examples
- X-rays, MRIs, CT scans, and other types of imaging
- Lab tests, such as bloodwork
- Minor surgeries, particularly ones that use less invasive techniques
- Colonoscopies
- Mammograms
- Consultations or follow-ups with a specialist
- Routine physical exams
- Same-day emergent care, often treated at an urgent care facility versus the ER
- Chemotherapy or radiation treatment
Inpatient vs.
 outpatient: The providers in each setting
outpatient: The providers in each settingPrimary care physicians have traditionally been considered outpatient providers, while specialists are thought of as inpatient physicians. But that’s really an oversimplification, particularly when you consider that hospitalists bridge the gap by providing general medical care to inpatients. Effective care requires that doctors work together and effectively leverage health care technology, regardless of their specialties and settings.
Many physicians also divide their time between inpatient and outpatient services. OB/GYNs, for example, provide inpatient care when delivering babies and outpatient care when consulting with pregnant women during prenatal checkups.
Generally speaking, inpatients have contact with a larger group of providers. During a hospital stay, you could interact with physicians, nurse practitioners, lab technicians, physical therapists, pharmacists, and physician assistants.
Inpatient vs. outpatient: Cost considerations
The difference between inpatient versus outpatient care matters for patients because it will ultimately affect your eventual bill.
Outpatient care involves fees related to the doctor and any tests performed. Inpatient care also includes additional facility-based fees. The most recent cost data included in the Healthcare Cost and Utilization Project from the Agency for Healthcare Research and Quality (AHRQ) shows the average national inpatient charges can vary considerably depending on the length of stay and the treatment involved. The exact amount you pay also hinges on your insurance.
Things get a little more complicated if you have Medicare. Outpatient care and physician-related services for inpatient care are covered by Part B. Hospital services like rooms, meals, and general nursing for inpatients are covered by Part A.
But if you stay overnight in the hospital under observation status, Medicare still considers you an outpatient and will not cover care in a skilled nursing facility. It can certainly be confusing, so don’t be afraid to ask the medical team about your status. They’re used to these types of questions.
Expand your medical knowledge
Hopefully, you now have a little more clarity concerning the definition of inpatient versus outpatient. It can go a long way towards helping you understand what you should expect during and after any sort of medical treatment.
You can further deepen your understanding of the health care world by reading our article “50 Must-Know Medical Terms, Abbreviations, and Acronyms.”
*This article was originally published in June 2019. It has since been updated to reflect information relevant to 2021.
Related
Articles
Treatment Information | Hirslanden Switzerland
outpatient treatment
If you are a client of an international insurance company and are interested in an outpatient consultation with one of our doctors, please contact the Hirslanden International Patient Care Center.
We will record all of your personal information, including your health insurance policy, medical problem, and desired medical service.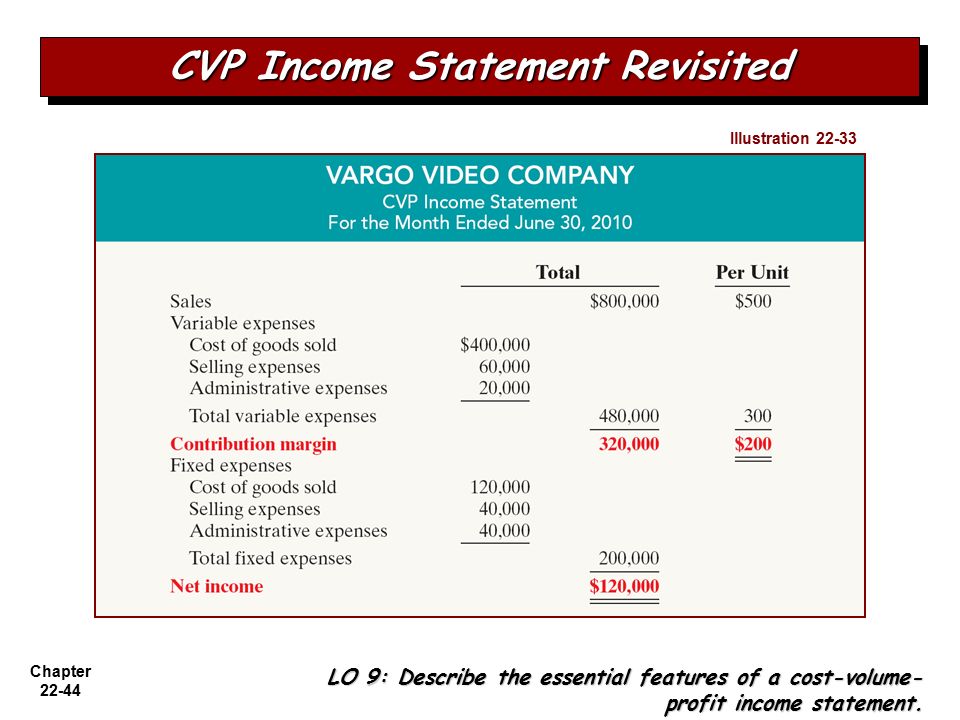 Please send us all relevant medical records, extracts and reports that you have.
Please send us all relevant medical records, extracts and reports that you have.
Once we have received all of your information, we will ask the doctor you have chosen to consult with you for a short medical report on your case. This report will contain details about possible treatment in your case.
If treatment with the doctor you have chosen is possible, we will be happy to assist you in making an appointment with the coordination of dates and times of treatment. If your preferred doctor is unable to provide treatment, we will, if possible, recommend another doctor in one of our clinics.
We kindly ask you to clarify the settlement procedure directly with your attending physician. You can then transfer the invoice to your insurance company.
inpatient treatment
Also in the case of inpatient treatment, you as a patient with international health insurance (insurance from another country) should usually contact the employees of Hirslanden International's International Patient Care Center directly. We will gladly record your personal and medical information and ask you to send us a copy of your health insurance policy and any medical records and documents you have.
We will gladly record your personal and medical information and ask you to send us a copy of your health insurance policy and any medical records and documents you have.
We will get a short medical report on your case from the specialist you have chosen. This report will contain details of possible inpatient treatment (including surgery) and the doctor's fee.
If treatment with the doctor you have chosen is possible, we will prepare for you a preliminary detailed calculation of the costs of treatment (preliminary estimate for treatment). The estimate will also contain possible additional examinations, which will be included at your request. If the doctor you have chosen is unable to provide treatment, we will be happy to suggest you, if possible, another specialist in one of our clinics.
After receiving your consent with the amount of the estimate, the date of the inpatient treatment will be coordinated with you and the doctor.
At the same time, we will fill out an insurance claim form and send it to your insurance company. We will inform you whether your insurance company agrees to reimburse all of your treatment costs, whether it agreed to only part of the costs or refused to reimburse the costs at all. If the insurance company has agreed to compensate for the reimbursement of expenses, then you can process your admission to the clinic by arriving there on the agreed day and time. If your insurance company is ready to take on only part of the costs, or does not agree to cover the costs of your medical case at all, then you need to pay for the treatment from your own funds, as a private person, by transferring a deposit to the account in the clinic in the amount of the full amount that is not covered by your insurance company. Possible payment methods:
We will inform you whether your insurance company agrees to reimburse all of your treatment costs, whether it agreed to only part of the costs or refused to reimburse the costs at all. If the insurance company has agreed to compensate for the reimbursement of expenses, then you can process your admission to the clinic by arriving there on the agreed day and time. If your insurance company is ready to take on only part of the costs, or does not agree to cover the costs of your medical case at all, then you need to pay for the treatment from your own funds, as a private person, by transferring a deposit to the account in the clinic in the amount of the full amount that is not covered by your insurance company. Possible payment methods:
- Cashless payment by bank transfer: please send the appropriate bank confirmation of the transfer of funds to the e-mail address: [email protected]
- Payment by credit card through the payment service Hirslanden: please fill out the form with your credit card details and send it to the email address: international@hirslanden. ch. You will receive a confirmation of the debiting of funds to your e-mail address from the payment system SIX Payment Services.
ch. You will receive a confirmation of the debiting of funds to your e-mail address from the payment system SIX Payment Services.
- Payment by credit card through the electronic payment system online banking: You will receive a link to make a payment through the SIX Payment Services payment system. Using this secure link, you will be able to pay with your bank card, while your credit card details will be entered into the system directly by you.
Additional payment information PDF (only english version).
Once these financial formalities have been settled, you will be admitted to the clinic at the agreed date and time.
After the intervention, we will issue you an itemized invoice, including all the services you have used. If your insurance company takes full responsibility for your costs in the clinic, we will send the final invoice directly to your insurance company. If your insurance company covers only part of the costs, the bill will be sent to you at your address.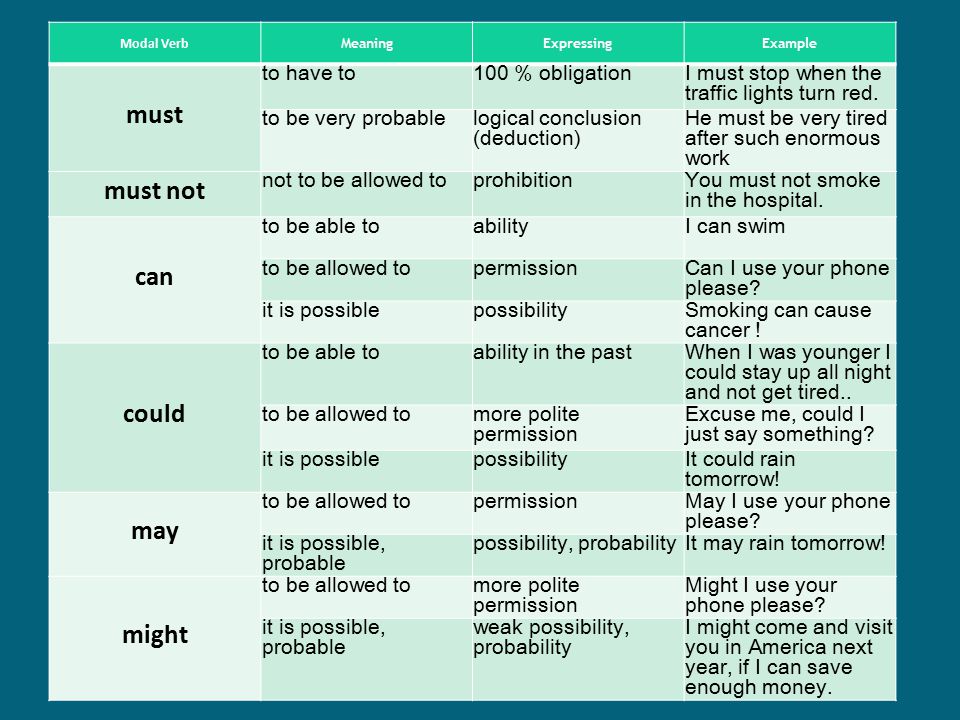 In this case, we will offset the amount of the deposit transferred by you earlier with the final amount of the final invoice of the clinic, and if there is a balance on the deposit, it will be returned to you, and if you have to make an additional payment, you will be issued an additional invoice for the additional payment. You can then send the final invoice to your insurance company to apply for reimbursement of expenses.
In this case, we will offset the amount of the deposit transferred by you earlier with the final amount of the final invoice of the clinic, and if there is a balance on the deposit, it will be returned to you, and if you have to make an additional payment, you will be issued an additional invoice for the additional payment. You can then send the final invoice to your insurance company to apply for reimbursement of expenses.
Coverage of outpatient and inpatient treatment in medical insurance
Updated
Author
Sergey Afanasiev
Inpatient and outpatient care costs are among the most common covered costs in health insurance. When choosing a health insurance program, it is recommended to pay attention to the coverage limits for outpatient and inpatient treatment.
This article provides information on the main differences between the two named treatments.
- As a rule, inpatient treatment is associated with hospitalization, serious medical intervention.
- Outpatient treatment includes visits to a general practitioner and specialist doctors, standard medical examinations.
| Stationary | Outpatient |
|---|---|
| In a medical facility | In a hospital or clinic |
| Admission to hospital | After visiting the doctor, the patient goes home |
| Mandatory nature of treatment | Optional nature of treatment |
| High cost of treatment, low likelihood of requiring inpatient treatment | Low cost treatment |
Treatment services
- Stationary
- Outpatient
- Surgery
- Anesthesia
- Accommodation and meals
- Care
- Doctor visit
- Other expenses related to hospitalization
- GP visit
- Specialist visit
- Emergency room
- Analyzes
- Biopsy, electrocardiogram, endoscopy, colonoscopy, ultrasound, mammography, X-ray, MRI
- Annual medical examinations
- Minor surgical procedures
- Physiotherapy, chemotherapy, manual therapy, immunization
In fact, the treatment is inpatient if the patient received this treatment during their stay in the hospital.