What does crippling depression mean
What Is Crippling Depression? | Talkspace
On a popular thread discussing crippling depression, one woman used her story to exemplify the condition.
“Everything seemed difficult,” she wrote.
She opened up about losing her job because she was unable to perform, neglecting basic hygiene and bills, feeling physically ill and contemplating suicide, among other issues.
“I would call it where you literally don’t want to do anything,” wrote another participant. “You are basically confined to your bed, without eating, without drinking and just want to wither away in your self-pity.”
Therapist Christine Fuchs learned about crippling depression through her work and offered similar descriptions. She listed a pervasive and significant decline in functioning in all areas of life. The illness makes people feel like “everything is overwhelming.”
Crippling Depression Defined
Crippling depression is clinical depression (major depressive disorder) that is severe to the point of limiting basic functioning, including the ability to work and live normally. Some of those afflicted experience episodes that last for a few weeks or months, as in after a loss or the death of a loved one. In other cases crippling depression is resistant to treatment and becomes a lifelong struggle.
Everyone who has lived with crippling depression has a unique experience, but there are some common threads such as difficulty sleeping or getting out of bed. When describing his period of crippling depression, mental health writer Stefan Taylor mentioned dropping out of college and “laying in bed all day.”
Is Crippling Depression the Same as Major Depressive Disorder, or Something More?
Some mental health professionals and people who live with depression believe crippling depression is simply a synonym for clinical depression or major depressive disorder. It is true that many have used the term this way, sometimes without being aware of its more popular meaning.
Sometimes popular phrases used to describe mental illness do not come from research, universities, or mental health organizations. Instead, people who live with certain disorders use unofficial terms to express levels of severity and describe how symptoms are affecting their functioning. Crippling depression is a perfect example of this phenomenon.
Instead, people who live with certain disorders use unofficial terms to express levels of severity and describe how symptoms are affecting their functioning. Crippling depression is a perfect example of this phenomenon.
Nonetheless, there is evidence that what people call “crippling depression” is significantly different than other forms of the disorder. Both the Mayo Clinic and National Institute of Mental Health do not specify an inability to work, for example, in their definitions of depression. These organizations seem to acknowledge the fact that every mental illness has degrees of severity.
Sufferers often live with moderate depression and experience symptoms that qualify for a diagnosis but do not noticeably impact daily functioning. Others cannot work full-time jobs or attend school. The term, “crippling depression,” came from the need to define this distinction.
A Symbol of Accepting Depression as a Disability?
Traditionally, people have used variations on the word, “crippling,” to describe physical disabilities such as the inability to walk, speak, or hear. Most people have accepted these types of disabilities as legitimate and deserving of support. The government often provides benefits to disabled people, especially those who request assistance because of the difficulty they have maintaining employment.
Most people have accepted these types of disabilities as legitimate and deserving of support. The government often provides benefits to disabled people, especially those who request assistance because of the difficulty they have maintaining employment.
Describing oneself as “crippled” — or even “a cripple” — isn’t necessarily pejorative either. In her famous personal essay, “On Being a Cripple,” Nancy Mairs illustrated her life living with a case of multiple sclerosis that robbed her of the full use of her limbs. She chose to identify as “a cripple” and stated she wasn’t ashamed of the label.
Lately an increasing number of employers, mental health professionals, and organizations, including the World Health Organization, have acknowledged depression as a disability. Similar to Mairs, sufferers often declare they have crippling depression and believe such language is both appropriate and accurate. Some people use the term crippling depression to describe when they believe their symptoms have crossed the threshold from a manageable mental health condition to a disability.
How the ‘I Have Crippling Depression’ Meme Raised Depression Awareness
On July 17, 2016, YouTuber Ian Carter, whose channel name is iDubbbzTV, published a video that begins with him jumping into a wheelchair and saying in a silly voice, “I have crippling depression.” The video quickly went viral and became a popular, lasting meme.
There were many commenters who thought the joke was insensitive and offensive. Several responded by writing about how they had depression and believed it was a serious matter.
Before the meme took off, the internet interest for “crippling depression” was relatively low, according to Google Trends data. Once most viewers lost interest in the original video and memes, the frequency of the term plummeted dramatically. Nonetheless, the popularity level stabilized to a range that was about five times greater than in previous years. It is possible that the joke caused more people to use the phrase and galvanized those who felt that it was a legitimate term for a distinct mental health issue.
We Need to Be Accepting of Crippling Depression
Clinical diagnoses are useful and preferable, but people have the right to apply unofficial labels to their illnesses. We need to be accepting of the fact that some people feel that clinical terms do not fully or accurately describe their experience.
If you think you might have crippling depression, consider seeking such as therapy. There are also many online resources that offer advice for dealing with depression. To be there for loved ones who might have the disorder, read up on how to support someone with depression. The illness is much less crippling when you have support and loved ones to lean on.
Talkspace articles are written by experienced mental health-wellness contributors; they are grounded in scientific research and evidence-based practices. Articles are extensively reviewed by our team of clinical experts (therapists and psychiatrists of various specialties) to ensure content is accurate and on par with current industry standards. Our goal at Talkspace is to provide the most up-to-date, valuable, and objective information on mental health-related topics in order to help readers make informed decisions. Articles contain trusted third-party sources that are either directly linked to in the text or listed at the bottom to take readers directly to the source.
Talkspace mental health services
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
What is crippling depression? | Do I have crippling depression?
Paralyzing depression Definition
Crippling depression is a major depressive disorder that affects people worldwide. The condition is severe and limits basic functions, including the person's ability to work and live a normal life.
Some people with this disorder experience episodes that can last weeks or months. These episodes may occur after the loss or death of a loved one. Some cases of severe depression do not respond to treatment. This could be the fight of a lifetime
1 1.JW Kanter, AM Busch, CE Weeks and SJ Landes, The Nature of Clinical Depression: Symptoms, Syndromes, and Behavior Analysis - PMC, PubMed Central (PMC).; Retrieved September 18, 2022 from https://www.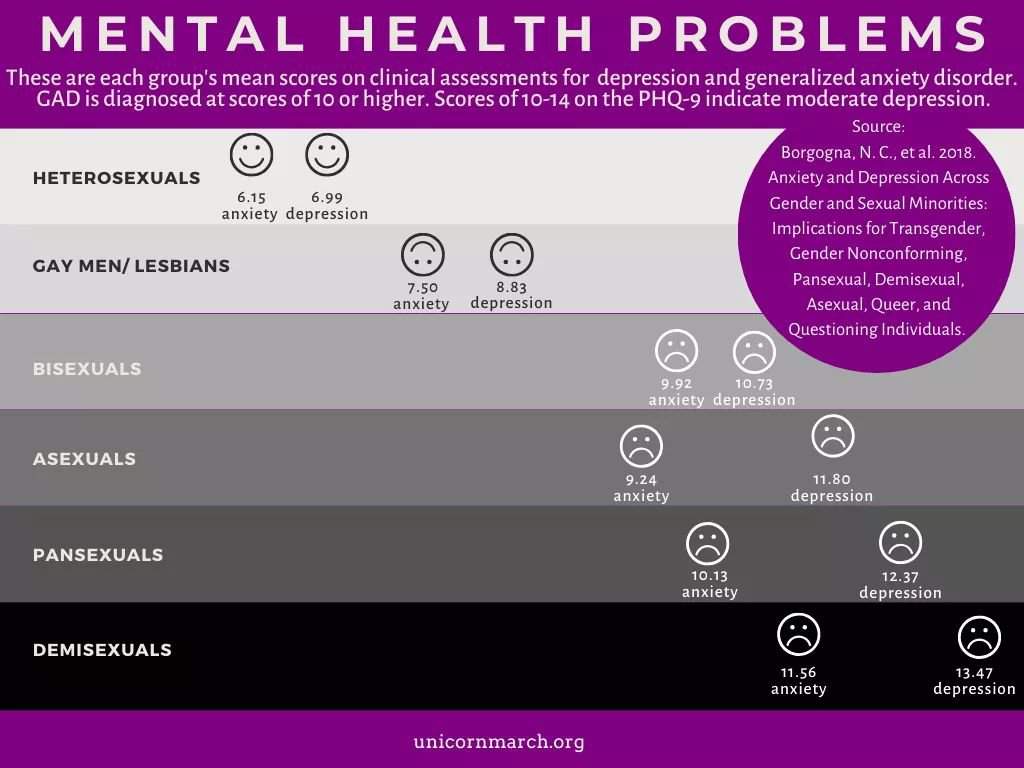 ncbi.nlm.nih.gov/pmc/articles/PMC2395346/..
ncbi.nlm.nih.gov/pmc/articles/PMC2395346/..
Each case of severe depression is a unique experience. There are some common symptoms that people experience with paralyzing depression, including difficulty sleeping or getting out of bed. A person can end a career or study and spend the whole day in bed, not having the strength to get up.
Paralyzing depression versus major depressive disorder
Some mental health experts consider major depression to be synonymous with major depressive disorder or clinical depression. Popular terms used to describe mental illness do not always come from research, universities, or mental health organizations.
Rather, people who experience certain mental health conditions in their lives use informal names to indicate severity and describe how the symptoms affect their lives. The term "crippling depression" is a perfect example of people suffering from the illness that gave it its name.
Evidence shows that the depression experienced by people who call it "crippling depression" is significantly different from other forms of mental illness. Mental health experts do not consider being unable to work part of depression. However, with severe depression, a person may feel unable to engage in activities that others with a depressive disorder do.
Some people refer to crippling depression as high-functioning depression. Some patients do not like it when the term "crippling" is used. It seems to many that the use of the word "cripples" gives the impression that a person has something permanent and preventive for recovery.
Getting a diagnosis of crippling depression
A mental health professional usually diagnoses depression based on the patient's symptoms and behavior patterns. The doctor may ask the patient to fill out a questionnaire to help them determine if they are experiencing depression and how severe it is.
Crippling depression, while not an official label, is often recognized by doctors and mental health experts more than ever before.
Symptoms of paralyzing depression:
- Persistent and strong feelings of sadness, anger or disappointment.
- Thoughts and forebodings of suicide
- Sleep disorders, too much or too short periods of sleep
- Apathy, exhaustion and lack of interest in activities or people
- Difficulties in work and concentration
- Poor personal hygiene
- Severe mood swings or outbursts of anger
- Changes in weight due to weight gain or loss
- Difficulty concentrating on tasks
- Frequent pain such as back pain or headaches.
Crippling Depression Quiz Questions
There are a few key questions you can ask yourself to determine if you are depressed. However, self-examination does not diagnose depression. A mental health professional is needed to properly diagnose depression.
A mental health professional is needed to properly diagnose depression.
If you think you have crippling depression, ask yourself:
- Do you have difficulty falling or staying asleep at night?
- Do you sleep between 10 and 12 hours a day?
- Do you sleep most of the day?
- Have you lost interest in what used to bring you joy or excitement?
- Have you been absent from work more than once in the past month because you were too tired or in pain to work?
- Are you more irritable now and more easily upset?
- Do you have thoughts of self-harm or suicide?
- Has your appetite increased or decreased?
- Are there days when you feel like you don't have the energy to do what needs to be done?
Treatment for crippling depression
Treatment for crippling depression consists of the same treatments as other types of depression. However, this process can be more intense to help you heal and end the worst effects of the illness.
Treatments for overwhelming depression include:
Psychotherapy
Psychotherapy, also known as talking therapy, is a common treatment for depression. People with extreme depression will see a therapist regularly, which can be a catalyst for improvement. A therapist can help you learn to live with stressors and react or respond in ways that evoke healthier feelings and emotions. Many people use online therapy because it is more affordable than waiting for weekly in-person sessions. Online therapy also costs less than traditional depression therapy. Click here for more information
Treatment
Antidepressants are often prescribed by doctors for patients with major depressive disorder and other types of depression. Medications can help regulate hormones and chemicals that combine to create many aspects of emotional and mental health. This includes the balance of neurotransmitters.
Electroconvulsive therapy (ECT)
ECT is usually used when other treatment options have failed. The doctor will electrically stimulate areas of the patient's brain while they are under anesthesia. The ultimate goal of ECT is to change the chemicals in the brain to stop the symptoms of depression.
The doctor will electrically stimulate areas of the patient's brain while they are under anesthesia. The ultimate goal of ECT is to change the chemicals in the brain to stop the symptoms of depression.
Inpatient clinic or depression rehabilitation center
People with paralyzing depression may have suicidal thoughts or even suicide attempts. People may not be able to take care of themselves properly. In such cases, short-term inpatient treatment may be required. Hospitalization and intensive rehabilitation treatment for depression provide patients with individual therapy, medication and group counseling. The goal is to help the patient reach a place in life where they can leave the hospital safely. Their treatment will continue outside the hospital.
Intensive outpatient program
As with a traditional psychotherapy session, intensive treatment uses techniques such as cognitive behavioral therapy, mindfulness, and response to exposure and prevention (ERP).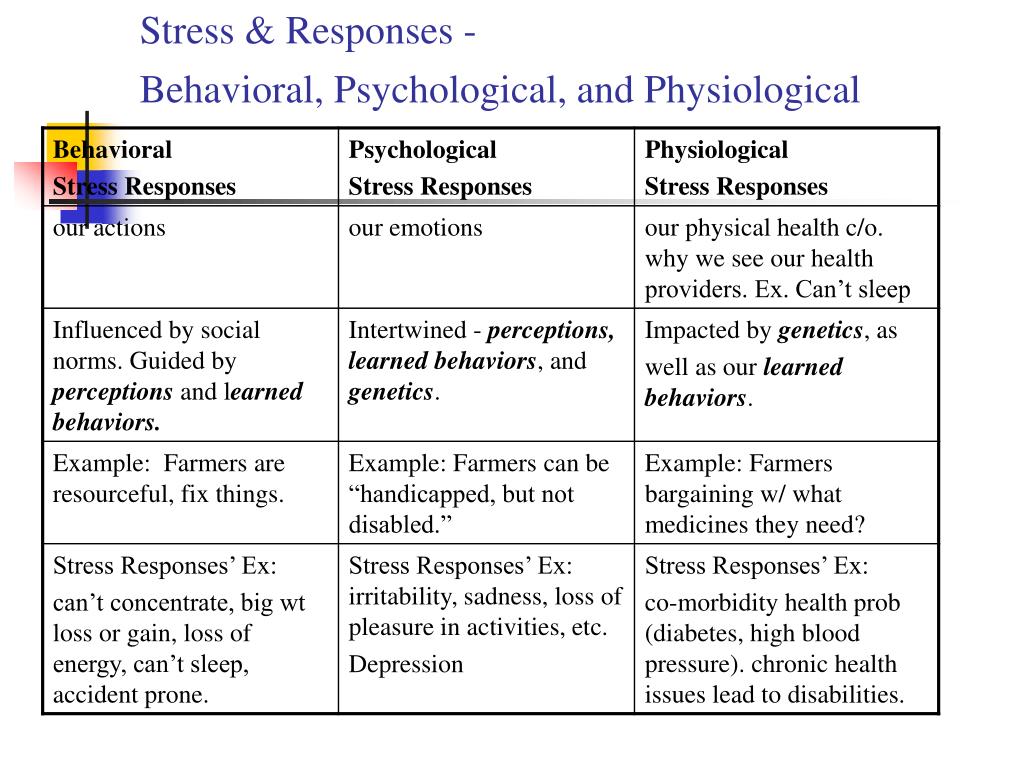 The idea behind intensive training is to teach people strategies to reduce symptoms and provide support, but do so within a framework that allows them to live at home and continue family or personal activities.
The idea behind intensive training is to teach people strategies to reduce symptoms and provide support, but do so within a framework that allows them to live at home and continue family or personal activities.
According to Richard Large, Remedy Wellbeing Consultant, “Depression affects millions of people every year, at every stage of their lives. This debilitating mental illness develops as a result of a combination of social, genetic, biochemical, psychological and physical factors. We understand that depression is more than just feeling sad and that it affects people in different ways, leading to many seeking help, including depression rehab, depression treatment, and other mental health services.” .
Identifying causes of paralyzing depression
Mental health providers are not 100% sure what causes depression in any form. There are certain factors that can increase a person's risk of developing depression. However, it is not known why some people develop depression and others do not.
Risk factors for paralyzing depression in humans include:
- Long-term depression
- Family history of major depressive disorder
- Constant or high levels of stress
- Chemical and hormonal changes
- Other diseases of physical or mental health
- Changes in personal life such as divorce, job loss or death of friends and/or family members
Crippling depression can be cured in most cases. Your doctor or therapist can work with you to find a combination of effective treatments. Depending on how you respond to treatment, your healthcare provider may adjust it as needed.
Previous : Understanding Serotonin Syndrome
Next : High Functional Depression
WHAT IS HIGH-FUNCTIONAL DEPRESSION? - DEPRESSION
Imagine a person who seems to be living an ideal life. She has a great job, a loving and supportive partner, and lots of fun outside of work. Getting to the office on time is no problem and she is one of the most productive employees in her company.
Getting to the office on time is no problem and she is one of the most productive employees in her company.
But there is one problem: she is unhappy and cannot get happiness from anything. Because she lives with high-functioning depression, it's hard for people to see how anything could be wrong.
High Functioning Depression Definition
Like many other illnesses, depression varies in severity from mild to debilitating. Mental health professionals typically measure the impact of a condition by evaluating the level of functioning. At its lowest level is what many therapists and patients refer to as "crippling depression," a condition in which one cannot be kept at work, maintain basic hygiene rules, get out of bed, or engage in any kind of relationship.
The opposite parameter is high-functioning depression, a form of illness that is not severe enough to noticeably affect the ability to perform everyday tasks such as work and household chores. However, high-functioning depression can be the same. symptoms like any other form of the disorder, including:
However, high-functioning depression can be the same. symptoms like any other form of the disorder, including:
- Persistent sad, anxious, or "empty" mood
- Feelings of hopelessness or pessimism
- Irritability
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Decreased energy or fatigue
- Feeling restless or trouble sitting
- Thoughts of appetite and/or death 905905
- Aches or pains, headaches, cramps or digestive problems with no clear physical cause
People with high-functioning depression can sometimes hide these symptoms, he says. Conversation therapist Samantha White. These patients worry about what others will find out about their illness.
Highly Effective Depression for Dysthymia
People with mental illness often come up with informal terms to describe their experiences. Sometimes these new phrases coincide with established diagnoses.
"As a psychotherapist, in my opinion, high-functioning depression is a popular psychological term for what is clinically known as dysthymia," Annie Wright wrote in an interview. article on The Mighty. Psychiatric associations also refer to dysthymia and high-functioning depression. persistent depressive disorder or chronic depression.
Despite many similarities, it is not yet clear whether dysthymia and high-functioning depression are the same. People are still refining the definition of the latter.
self-destructive behavior in relationships
Linking high-functioning depression to success, ambition, and perfectionism
The label "high-functioning depression" does not imply a successful career or additional mental health problems. However, people with this type of depression are likely to be successful, ambitious, perfectionist, lonely, or anxious. These traits are often associated with depressive thinking and behavior. Wright, in her article on high-functioning depression, gave several examples:
- Relentless self-criticism and doubt
- Feelings of guilt and worry about the past and future
- Seeking perfection in work and life
- Inability to rest and slow down
- Frustrated by small problems
 Such is the nature of perfectionism. Nothing like this. There is concern about whether they can get everything they want or if they are good enough to earn their desires. A career-oriented lifestyle can breed loneliness and frustration.
Such is the nature of perfectionism. Nothing like this. There is concern about whether they can get everything they want or if they are good enough to earn their desires. A career-oriented lifestyle can breed loneliness and frustration. Therapist Erika Martinez described the mixture of clients with high-functioning depression as successful professionals who feel empty and dissatisfied.
“They come home late to an empty house or to a family that has already gone to bed,” Martinez said. Stress and burnout can contribute to this type of depression.
The challenge of living with high-functioning depression
Despite their ability to maintain relationships, people with high-functioning depression may find it difficult to get support. Because their symptoms do not significantly affect behavior, friends, colleagues, and family members often do not understand or even believe they have a serious illness.
"Because I can work full time and be successful, own my own home and take care of everything myself, people underestimate how hard I struggle and how hard it is to work some days," said Christine Dolan, member of the Huffington Lifestyle Community. which he revealed about her condition. "It's hard enough to hold back, but it's even harder when you know that people underestimate you and don't praise you just for getting out of bed."
which he revealed about her condition. "It's hard enough to hold back, but it's even harder when you know that people underestimate you and don't praise you just for getting out of bed."
Sometimes people like Dolan face a stigma that makes them feel that their disorder is illegal. It is easy to focus on behavior and lose sight of subtle patterns in emotions and thoughts.
Why high-functioning depression is more difficult to treat than other forms
At first glance, high-functioning depression appears to be - by definition - more treatable than severe forms of the disorder. However, therapists often face unique challenges when working with clients with chronic depression.
Experts say mental health professionals find it easier to manage depressed clients with reduced functioning. therapist Asta Klimaite, because the goals are usually simple and specific. If a severely depressed client cannot leave their apartment, they can make significant progress by going to the grocery store. But what about the experienced leader who wants to "be happy"? With such an uncertain outcome in mind, it can be difficult for consultants and clients to set specific, actionable goals.
But what about the experienced leader who wants to "be happy"? With such an uncertain outcome in mind, it can be difficult for consultants and clients to set specific, actionable goals.
what it means to be emotionally intelligent
People with dysthymia are less likely to seek treatment. Sometimes they don't realize that their symptoms are caused by a mental illness. Others understand the situation but don't want help or think their disorder doesn't warrant concern.
Origin of the term and rise in popularity
Internet users used the phrase "high-functioning depression" as early as 2004, according to data from Google Trends. The date of first personal use is unknown, but both customers and mental health professionals likely mentioned the label well before 2004.
The popularity of this term skyrocketed in April 2016 and has since become commonplace.
"I believe this is probably because the media is using the term 'high-functioning' more frequently in blogs, social media posts, and videos," Martinez suggested.