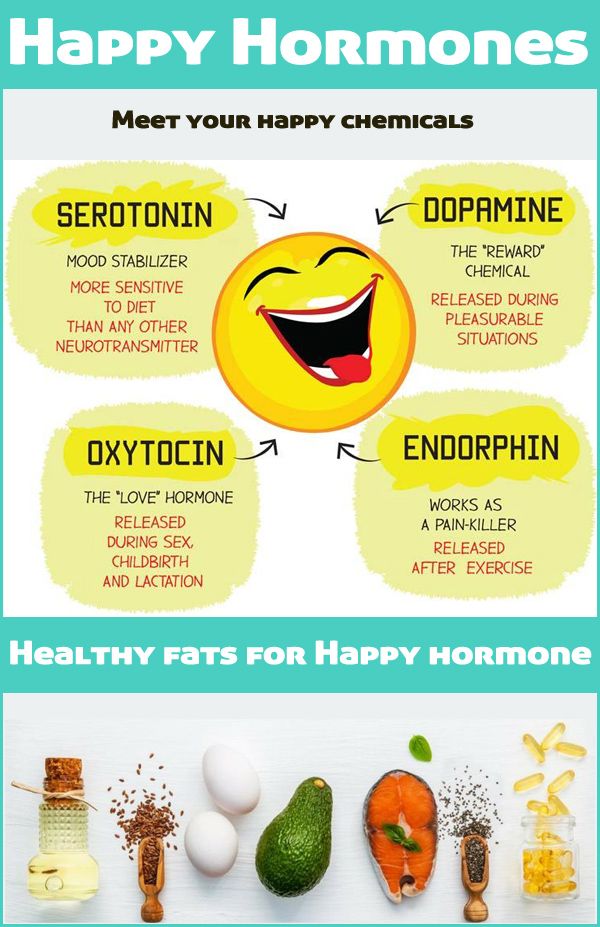
What does a mood stabilizer do
Mood stabilizers - Fraser Health Authority
Mood stabilizers are a group of medications used to reduce or relieve symptoms of mood swings in bipolar disorder and other mental disorders.
What are mood stabilizers commonly prescribed for?
Mood stabilizers are used mainly to treat bipolar disorder, mood swings associated with other mental disorders, and in some cases, to enhance the effect of other medications used to treat depression.
How do mood stabilizers work?
Mood stabilizers work by decreasing abnormal activity in the brain. These medications can help reduce mood swings and prevent manic and depressive episodes.
What mood stabilizers are currently available?
Commonly prescribed mood stabilizers include:
- Lithium
- Carbamazepine
- Lamotrigine
- Oxcarbazepine
- Valproic acid
- Divalproex sodium
What can I expect from mood stabilizers?
Signs that the medication may be helping can include:
- Reduced mood swings
- Relief of symptoms
How long do mood stabilizers take to work?
There can be signs of improvement early on in treatment but it may take up to several months to experience the full effect of the medication and determine whether it is working.
Everybody is different including the way each person’s brain is wired, therefore medications may work differently in each person.
Finding the right mood stabilizer is a process of trial and error. Some people may have to try several different medications before they find one that works.
What are the common side effects of mood stabilizers?
Not everyone will experience side effects. People who experience some side effects may find that many of these side effects go away with time as their body gets used to the medication.
Some common side effects may include:
- Itchy skin, rashes
- Increased thirst
- Frequent urination (peeing too often)
- Nausea and vomiting (stomach upset)
- Slurred speech (difficulty saying words clearly)
- Blackouts (not knowing where you are for brief moments)
- Changes in vision (unable to see things clearly or the way you normally would)
- Seizures (periods of body spasms or jerking movements that cannot be controlled)
- Loss of coordination (for example, some difficulty placing fork to mouth when eating)
If at any time you develop a sudden rash, have any trouble with breathing, sudden pain in any part of the body (e. g. chest, muscles), sudden muscle stiffness, any involuntary movements, trouble staying awake during the day, confusion or difficulty peeing or peeing too much, contact your doctor immediately.
g. chest, muscles), sudden muscle stiffness, any involuntary movements, trouble staying awake during the day, confusion or difficulty peeing or peeing too much, contact your doctor immediately.
Some side effects may go away over time but you should always report to your doctor any symptoms that you feel are bothersome and/or have become worse.
Some suggestions to help reduce risk and/or severity of side effects can include:
- Balanced diet, adequate fluids, daily activity or exercise
- Report any weight gain greater or equal to five per cent (approximately two to 25 lbs)
- Limit excess intake of caffeinated products and sodium
- Decrease smoking
Sometimes a change in the dose and schedule may help manage some side effects. You should follow up with your doctor as there may be other treatments that could help.
Your doctor may also ask you to go for lab work or other tests to make sure you are tolerating the medication and watch for any concern of side effects.
How can I safely use my mood stabilizer?
- Do not take any other medication that is not prescribed by your doctor (e.g. over the counter products, vitamins, herbal supplements) without checking if it is safe to combine with your mood stabilizer. Check with your pharmacist before deciding to take anything new.
- All mood stabilizers should be taken regularly, preferably at around the same time every day. If you miss a dose do not double up, take your next dose at the regularly scheduled time. If you miss more than one dose please contact your doctor to discuss.
- Do not stop taking your mood stabilizers until you have spoken with your doctor to avoid any severe withdrawal effects. If there is a need to stop taking the medication the dose should be gradually reduced.
Resources
- HealthLink BC: Mood-stabilizing medicines
General information about mood-stabilizing medicines. - Centre for Addiction and Mental Health: Mood stabilizers
Learn more about mood stabilizers.
Mood Stabilizing Medications | CAMH
Overview
Mood stabilizers are medications used in the treatment of bipolar disorder, where a person’s mood changes from a depressed feeling to a high “manic” feeling or vice versa. These drugs can help reduce mood swings and prevent manic and depressive episodes.
Mood stabilizers can take up to several weeks to reach their full effect. Because of this, other psychiatric medications such as antipsychotics; are often used in the early stages of treatment to treat acute mania.
Depression in bipolar disorder can be hard to distinguish from other forms of depression. Antidepressant medications can be effective; however, they must never be used alone with bipolar disorder as they can also cause a person who is depressed to switch into mania. Antidepressants may also lead to more frequent mood episodes, known as rapid cycling. This risk is lessened if the person is also taking a mood stabilizer.
Do I need this treatment?
The term “bipolar” refers to the two extremes of mood: mania and depression. People with bipolar disorder usually experience these extremes at different times, although the two mood states can occur together (known as a mixed state). With bipolar disorder, people can also have periods where their mood is balanced. Mood stabilizers can help to keep the mood of a person with bipolar disorder within this balanced range.
People with bipolar disorder usually experience these extremes at different times, although the two mood states can occur together (known as a mixed state). With bipolar disorder, people can also have periods where their mood is balanced. Mood stabilizers can help to keep the mood of a person with bipolar disorder within this balanced range.
Treatment with mood stabilizers can reduce symptoms of bipolar disorder and increase people’s ability to pursue their interests and participate more fully in their relationships.
Medication is generally considered to be the cornerstone of treatment for bipolar disorder; however, combining medication with other types of therapy and support can help you to get and stay well. Forms of talk therapy that have been shown to help with bipolar disorder are interpersonal and social rhythm therapy, cognitive-behavioural therapy and family-focused education about bipolar disorder. Other aids can include peer support, school and job counselling, and housing and employment support.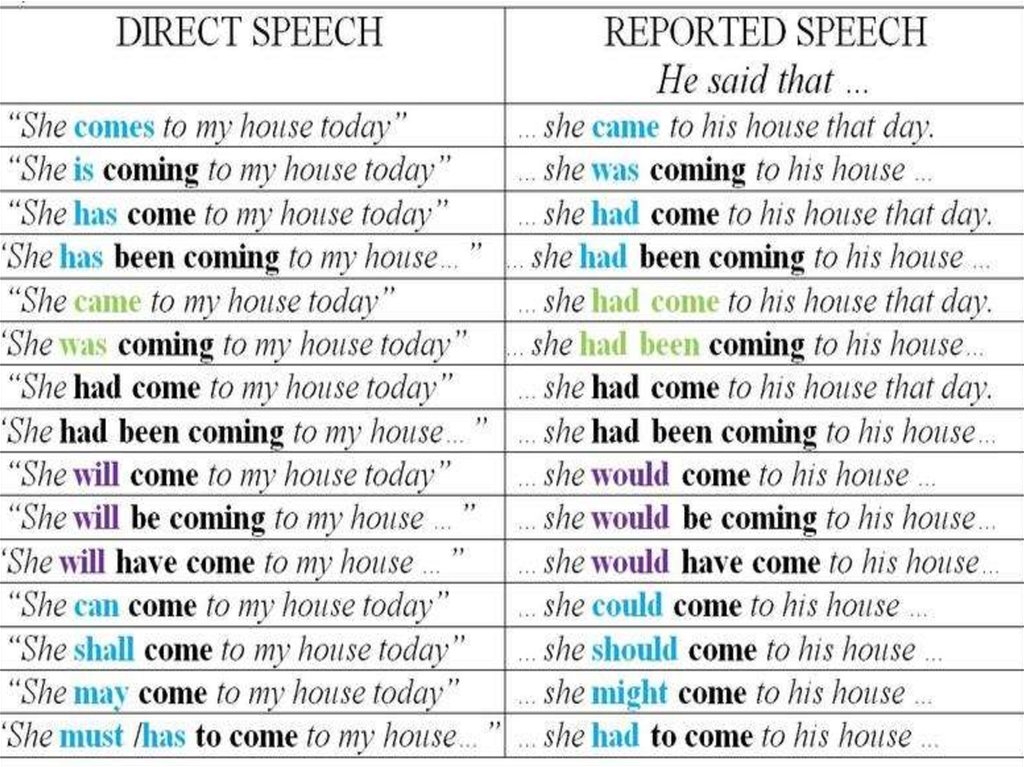 Eating a nutritious diet, exercising regularly and getting enough sleep are also important, as are minimizing your use of alcohol and caffeine and avoiding street drugs.
Eating a nutritious diet, exercising regularly and getting enough sleep are also important, as are minimizing your use of alcohol and caffeine and avoiding street drugs.
What does Mood Stabilizing Medication do?
How mood stabilizers work is not fully understood. It is thought that the drugs work in different ways to bring stability and calm to areas of the brain that have become overstimulated and overactive, or to prevent this state from developing.
Side effects of Mood Stabilizing Medication
The side-effects of mood stabilizers vary depending on the type of medication. With some medications, side-effects are kept to a minimum through regular monitoring of the level of the drug in the blood. Some people experience no side-effects. Others may find the side-effects distressing. Side-effects usually lessen as treatment continues.
Check the information given to you by your doctor or pharmacist on the specific effects of any drug you have been prescribed. If side-effects are not mild and tolerable, let your doctor know as soon as possible. Your doctor may:
If side-effects are not mild and tolerable, let your doctor know as soon as possible. Your doctor may:
- adjust your dose
- suggest you take the medication at a different time of day
- suggest you take your medication with food
- prescribe other medications to help control side-effects
- change your medication.
More information on side-effects is included for each type of mood stabilizer.
Getting the right doseWith lithium, carbamazepine and divalproex, the dose is based on how much of the drug is in your blood and how you respond to treatment. This means that the dose differs for everyone who takes it. Blood samples are taken regularly to make sure that the dose is neither too high nor too low. Taking less may not be effective, and taking more can make you physically sick.
The right dose is within a range, rather than a precise point. It may change over time, depending on whether the medication is being used to treat active symptoms of mania or depression or to help prevent symptoms from returning. On days that you are scheduled to have your blood level tested, wait until after the test to take your morning dose to avoid inaccurate results.
On days that you are scheduled to have your blood level tested, wait until after the test to take your morning dose to avoid inaccurate results.
If you are taking carbamazepine, avoid grapefruit juice as it can raise the level of this drug in your body.
Controlling side-effects- Mood stabilizers can increase your sensitivity to the sun: wear sunscreen when outdoors to prevent burning.
- To reduce stomach upset, take your dose with food or milk.
- If your medication makes you feel drowsy, check with your doctor to see if you can take it at bedtime.
- Taking mood stabilizers can cause weight gain. Getting regular exercise and eating a low-fat, low-sugar, high-fibre diet (e.g., bran, fruits and vegetables) can help prevent weight gain.
- If side-effects are troublesome or severe, you may do better on a lower dose. Talk to your doctor.
Types of Mood Stabilizing Medication
The oldest and most studied of mood stabilizers is lithium.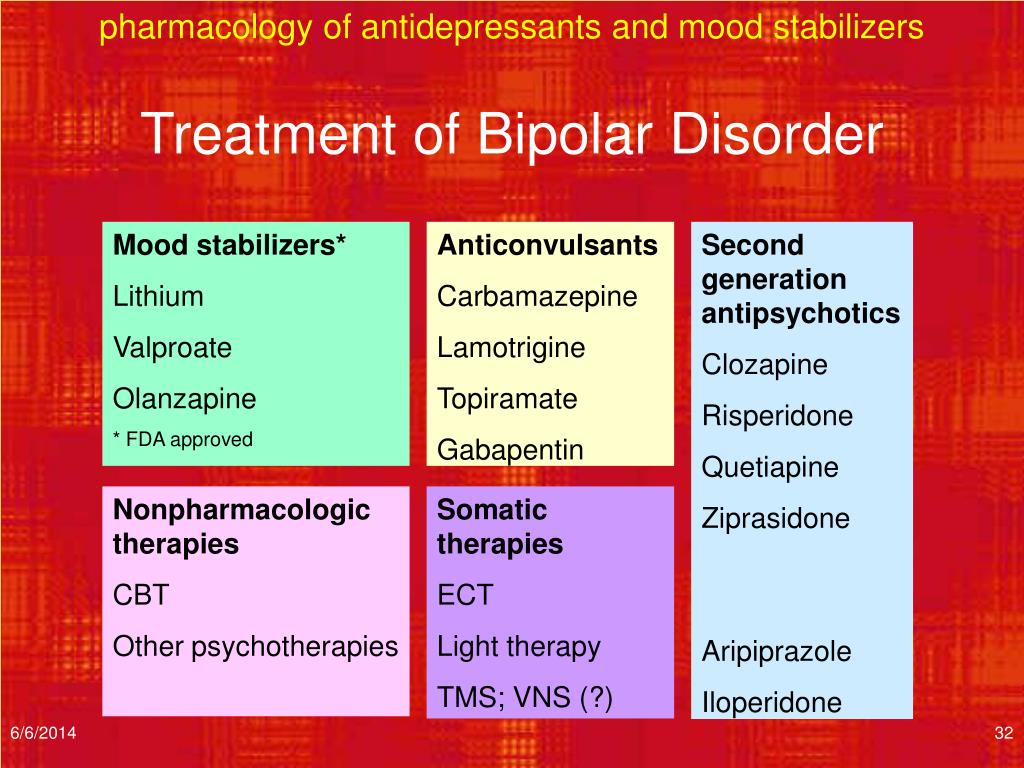 However, many drugs that were first developed as anticonvulsants to treat epilepsy also act as mood stabilizers. These include carbamazepine, divalproex and lamotrigine. Gabapentin and topiramate are also anticonvulsants that may act as mood stabilizers, but they are usually given in addition to other medications.
However, many drugs that were first developed as anticonvulsants to treat epilepsy also act as mood stabilizers. These include carbamazepine, divalproex and lamotrigine. Gabapentin and topiramate are also anticonvulsants that may act as mood stabilizers, but they are usually given in addition to other medications.
Lithium (Carbolith, Duralith, Lithane) is found in nature in some mineral waters and is also present in small amounts in the human body.
Lithium is used to treat mania and to prevent further episodes of mania and depression.
Common side-effects of lithium include increased thirst and urination, nausea, weight gain and a fine trembling of the hands. Less common side-effects can include tiredness, vomiting and diarrhea, blurred vision, impaired memory, difficulty concentrating, skin changes (e.g., dry skin, acne) and slight muscle weakness. These effects are generally mild and fade as treatment continues. If, however, any of these effects are severe, they should be reported to your doctor immediately. Thyroid and kidney function can be affected by lithium in some people and must be monitored regularly by your doctor.
If, however, any of these effects are severe, they should be reported to your doctor immediately. Thyroid and kidney function can be affected by lithium in some people and must be monitored regularly by your doctor.
Signs of lithium overdose: Lithium blood levels can increase to dangerous levels when a person becomes severely dehydrated. Remember to drink eight to 12 cups of fluid per day, especially when it’s hot or when you’re exercising. Severe vomiting, diarrhea or a fever can also cause dehydration. If you have these symptoms, stop taking lithium and see your doctor as soon as possible.
Changing the amount of salt you use can also affect lithium levels: avoid switching to low- or no-salt diets.
Signs that the amount of lithium in the body is higher than it should be include severe nausea, vomiting and diarrhea, shaking and twitching, loss of balance, slurred speech, double vision and weakness.
If you experience any of these effects, see your doctor as soon as possible. In the meantime, stop taking lithium and drink plenty of fluids. If you cannot reach your doctor and the symptoms do not clear up, go to the nearest hospital emergency department.
In the meantime, stop taking lithium and drink plenty of fluids. If you cannot reach your doctor and the symptoms do not clear up, go to the nearest hospital emergency department.
The differing names for this anticonvulsant medication reflect the various ways it is formulated. Divalproex (and its various forms) is used for acute manic episodes. Brand names include Depakene and Epival.
Common side-effects of divalproex include drowsiness, dizziness, nausea and blurred vision. Less common side-effects are vomiting or mild cramps, muscle tremor, mild hair loss, weight gain, bruising or bleeding, liver problems and, for women, changes in the menstrual cycle.
CarbamazepineCarbamazepine (Tegretol) is another anticonvulsant. It is used for mania and mixed states that do not respond to lithium or when the person is irritable or aggressive.
Common side-effects of carbamazepine include dizziness, drowsiness, blurred vision, confusion, muscle tremor, nausea, vomiting or mild cramps, increased sensitivity to sun, skin sensitivity and rashes, and poor co-ordination.
A rare but dangerous side-effect of carbamazepine is reduced blood cell counts. People who take this drug should have their blood monitored regularly for this effect. Soreness of the mouth, gums or throat, mouth ulcers or sores, and fever or flu-like symptoms can be a sign of this effect and should be reported immediately to your doctor. If carbamazepine is the cause of these symptoms, they will go away when the medication is stopped.
Oxcarbazepine (Trileptal), a closely related drug, may have less side-effects and drug interactions than carbamazepine, but is not as well studied for bipolar disorder.
LamotrigineLamotrigine (Lamictal) may be the most effective mood stabilizer for depression in bipolar disorder, but is not as helpful for mania.
The starting dose of lamotrigine should be very low and increased very slowly over four weeks or more. This approach decreases the risk of a severe rash—a potentially dangerous side-effect of this drug.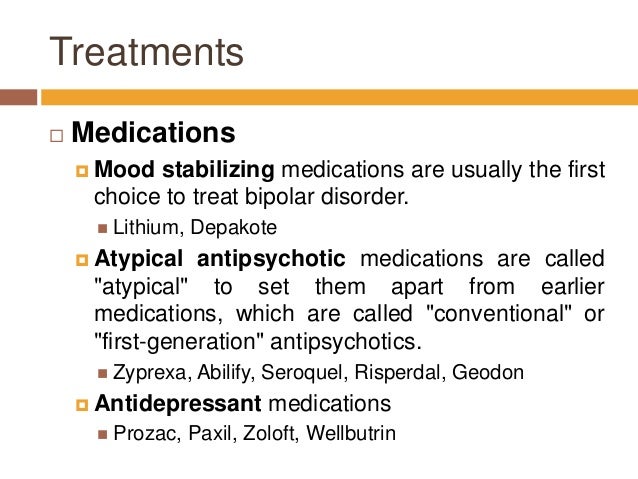
Common side-effects of lamotrigine include fever, dizziness, drowsiness, blurred vision, nausea, vomiting or mild cramps, headache and skin rash. Although it is rare, a severe skin rash can occur with lamotrigine. Any rashes that begin in the first few weeks of treatment should be reported to your doctor.
* Medications are referred to in two ways: by their generic name and by their brand or trade names. Brand names available in Canada appear here in brackets.
Frequently Asked Questions
How long should I take mood stabilizers? When you start taking mood stabilizers, it may be two weeks or more before you notice their effect and four to six weeks before they reach their full effect. It’s important to give them time to work. Once your symptoms are under control, you will be encouraged to continue to take mood stabilizers for at least six months and probably longer. How much longer varies from person to person.
Mood stabilizers can help prevent further episodes of mania or depression. In other words, staying on these medications for the long term can help to keep you well. Going off mood stabilizers, on the other hand, can greatly increase your chances of having another episode.
Once you have been taking mood stabilizers for a while and you are feeling well, you may do fine on a lower “maintenance” dose. Talk to your doctor if you would like to try this.
Are mood stabilizers addictive?Drugs that are addictive produce a feeling of euphoria, a strong desire to continue using the drug, and a need to increase the amount used to achieve the same effect. Mood stabilizers do not have these effects.
While mood stabilizers are not addictive, when you take them (or any drug) over months or years, your body adjusts to the presence of the drug. If you then stop using the drug, especially if you stop suddenly, the absence of the drug may result in withdrawal effects or in return of symptoms. With mood stabilizers, the withdrawal effects are generally mild; the greatest risk with stopping these drugs is the return of symptoms.
With mood stabilizers, the withdrawal effects are generally mild; the greatest risk with stopping these drugs is the return of symptoms.
Whether you want to cut down your dose or stop taking a medication, the same rule applies: go slowly. Sudden changes in your dose can greatly increase your risk of having another mood episode.
The first step is to ask yourself if this is the right time. Are you feeling well? Is the level of stress in your life manageable? Do you feel supported by your family and friends?
If you think you’re ready, talk to your doctor. If your doctor doesn’t agree, find out why. If you are not satisfied with his or her reasons, you may want to see another doctor for a second opinion.
If your doctor does agree, he or she will advise you not to skip doses but to reduce your dose gradually over a four to six week period. This process of cutting back will take several months.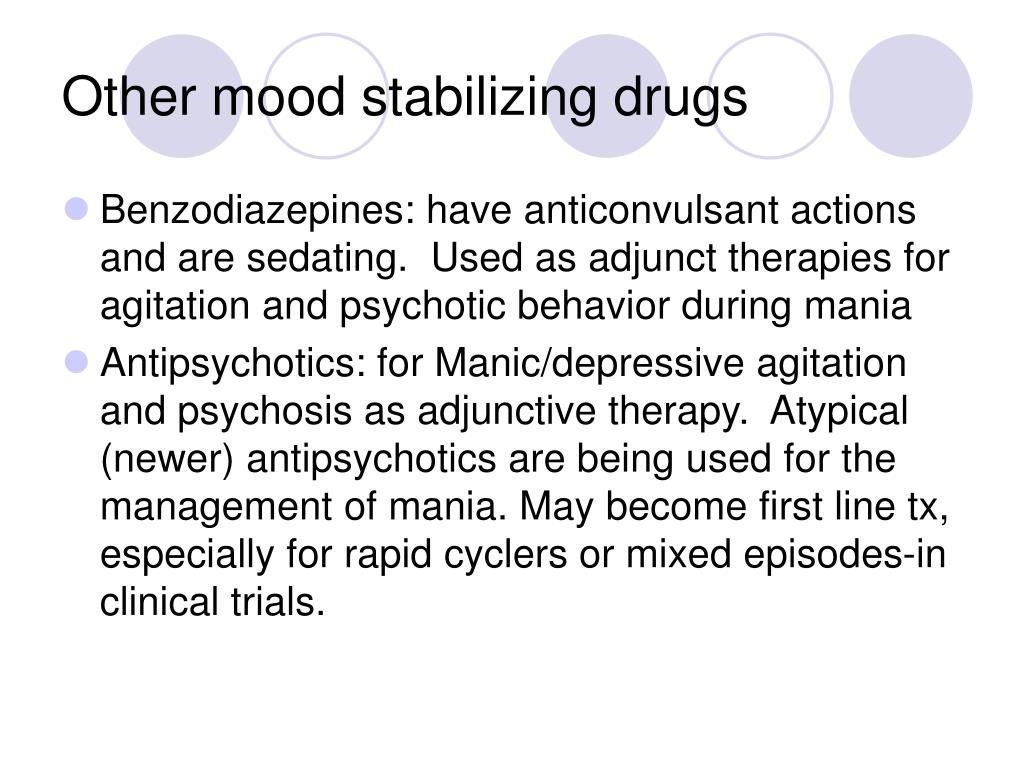
If you want to stop taking more than one medication, your doctor will usually suggest that you lower the dose of one drug at a time.
As you cut down, if you start to feel unwell, let your doctor know. You may want to go back up with your dose. Find the dose that works best for you.
Will mood stabilizers interact with other medications?Some medications can affect the blood levels of mood stabilizers, meaning your dose of mood stabilizer may have to be adjusted while you are taking the other medication. Mood stabilizers, especially carbamazepine, may also reduce the effectiveness of some other drugs. Always make sure your doctor or dentist knows about any drugs you are taking when he or she prescribes another medication. It’s also important to check with your pharmacist before using any over-the-counter medication, including pain medications, herbal remedies, cold or allergy tablets, or cough syrups.
What if I drink coffee or alcohol while taking mood stabilizers? Drinking coffee or other beverages that contain caffeine can lower lithium levels and increase tremor. If you want to dramatically change how much caffeine you have in a day (e.g., cutting back from four cups to one cup of coffee a day), check with your doctor or pharmacist first to see if your mood stabilizer dose should be adjusted.
If you want to dramatically change how much caffeine you have in a day (e.g., cutting back from four cups to one cup of coffee a day), check with your doctor or pharmacist first to see if your mood stabilizer dose should be adjusted.
People with bipolar disorder are generally advised to avoid alcohol. This is recommended because:
- Drinking alcohol can worsen depressive episodes and further impair judgment in mania.
- Many people with bipolar disorder develop addiction problems with alcohol and other drugs, especially when they use these substances to “take the edge off” their symptoms or to offset the effects of medication.
- Combining mood stabilizers with alcohol tends to enhance the negative effects of both drugs, such as drowsiness, nausea and poor co-ordination.
While avoiding alcohol is the best choice for many people with bipolar disorder, having a drink or two on occasion should be okay for those who are stable, feeling well and who have not had a substance use problem.
Street drugs can complicate your situation and create problems. Cocaine and amphetamines, for example, can trigger an episode of mania or depression. Marijuana could lift you up or it could bring you down; its effects on mood can be unpredictable, especially when combined with bipolar disorder. Using any street drugs (or alcohol) regularly to modify your mood increases your risk of addiction.
Will mood stabilizers affect my ability to drive safely?Mood stabilizers, especially early in treatment, may delay your reaction time. This effect could impair your ability to drive a car or operate other machinery. Avoid these activities until you adjust to the medication or if you feel slowed down.
Will mood stabilizers affect my sex drive and function? Taking lithium may reduce your interest in sex. This can be a good thing for some people and not so good for others. If you feel your interest in sex is too low, talk to your doctor about it. Sometimes an adjustment in dose can help.
If you feel your interest in sex is too low, talk to your doctor about it. Sometimes an adjustment in dose can help.
Although not common, some men who take lithium report a decreased ability to maintain an erection or to ejaculate. With bipolar disorder, many complex factors other than medication may contribute to sexual difficulties.
In women, mood stabilizers may cause changes in the menstrual cycle. Carbamazepine and other anticonvulsants may reduce the effectiveness of birth control pills.
Is it safe to take mood stabilizers while pregnant or breastfeeding? Each woman’s situation is unique and should be discussed with her doctor. For any pregnant woman with a history of bipolar disorder, the question of taking mood stabilizers during pregnancy usually comes down to a risk-benefit analysis. All mood stabilizers carry some risk—some more than others; however, episodes of depression or mania can affect prenatal care and a mother’s ability to parent her newborn child. When treatment with a mood stabilizer helps to avoid a relapse or to reduce distress, the benefits may outweigh the risks.
When treatment with a mood stabilizer helps to avoid a relapse or to reduce distress, the benefits may outweigh the risks.
Taking lithium during the first trimester in pregnancy is believed to slightly increase the risk of a heart defect in the baby. This risk has been shown to be .05-.1 per cent (i.e., one in 2,000). Newborns must be monitored for possible toxic effects of lithium; these effects usually resolve within one to two weeks.
Divalproex increases the risk of spinal defects in the developing baby by approximately five to nine per cent. Divalproex is also related to developmental delays and cognitive problems in children. Carbamazepine increases the risk of spinal defects by approximately one per cent. Lamotrigine is associated with a potential increased risk for cleft palate.
Lithium can be passed to the baby through breast milk; however, the amount varies greatly from woman to woman. Some women may be able to breastfeed with close monitoring of lithium levels in the mother’s milk and the baby’s blood.
The amount of anticonvulsant mood stabilizers passed through breast milk is very small and is not considered to be a risk to the baby, especially when weighed against the benefits of breastfeeding.
If you decide to stop taking medications during pregnancy or while breastfeeding, it is a good idea to see your doctor more often to help you monitor for a return of symptoms.
Can children and teens use mood stabilizers?The first signs of bipolar disorder can appear in childhood, usually as depression or behaviour problems. Early substance use problems or petty crime can also be signs. When bipolar disorder in childhood is misdiagnosed as attention-deficit/hyperactivity disorder or unipolar depression, treatment with stimulants or antidepressants can worsen symptoms.
Mood stabilizers were developed and tested on adults. While most of these drugs are not officially approved for use by children and teens, professional guidelines direct their use in this age group.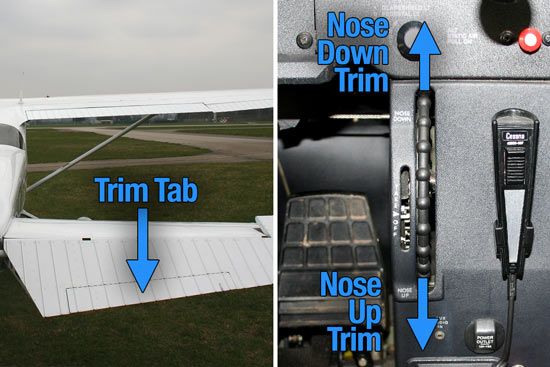 Lithium is approved for treating manic symptoms in children aged 12 and older.
Lithium is approved for treating manic symptoms in children aged 12 and older.
Children and teens may be more prone to the side-effects of these drugs and should be monitored by their doctor regularly for side-effects.
Can older adults use mood stabilizers?As people age into their 60s and older, their bodies become less able to eliminate medications. This means that older people who take mood stabilizers need to have the drug levels in their blood measured more often than younger people. Those taking lithium also need to have their kidney and thyroid function and heart rate monitored more frequently.
As people get older, they also become more sensitive to medications and may require a lower dose. Mood stabilizers can increase the risk of falls, especially when taken with other drugs.
Copyright © 2009, 2012 Centre for Addiction and Mental Health
Related Programs & Services
- Treatment at CAMH: Access CAMH
- Help for families from CAMH
- ConnexOntario
- For information on using medications while pregnant or breastfeeding, contact MotherRisk at 416 813-6780 or visit www.
 motherisk.org.
motherisk.org.
Additional Resources
- When a parent has bipolar disorder - What kids want to know
- Bipolar Disorder: An Information Guide (PDF)
- A free tutorial on bipolar disorder is available on the Mental Health 101 page.
Side Effects of Mood Stabilizers - PsyAndNeuro.ru
In most international guidelines, "classic/traditional" non-antipsychotic mood stabilizers are listed as first or second line drugs for bipolar disorder. Some mood stabilizers may also be effective in treating other mental disorders.
This review compares the safety profiles of mood stabilizers as well as side effects and strategies to prevent life-threatening adverse effects. nine0003
For the review, 1288 relevant studies were selected in English until April 2020.
Set Laboratory Monitoring Stabilizers
9000
The most common side effects , nausea, vomiting, constipation, pruritus, ataxia, anticholinergic effects including dry mouth, blurred vision, asthenia, and speech disturbance, especially at high doses and after rapid titration. Relatively often benign skin reactions (rash) are described. nine0003
Relatively often benign skin reactions (rash) are described. nine0003
In addition, a strong association was found between the alleles of the HLA-B * 1502, HLA-B * 1511 genes, the HLA * 3101 gene and the onset of Stevens-Johnson syndrome and carbamazepine-induced toxic epidermal necrolysis. A strong correlation of the HLA-B*1502 allele with Stevens-Johnson syndrome and carbamazepine-induced toxic epidermal necrolysis in Chinese and other Asian peoples has been documented. The HLA-A*3101 allele is associated with carbamazepine-induced hypersensitivity reactions in northern Europeans and Japanese. The recommendations of the Consortium for the Implementation of Clinical Pharmacogenetics highlight the clinical benefit of genetic testing for the HLA-B*1502 allele in reducing the risk of skin reactions following carbamazepine administration. Some studies also report that the HLA-A*3101 screening test is associated with a significant reduction in the incidence of skin adverse reactions. nine0003
nine0003
Most side effects correlate with plasma concentrations above 9 µg/ml. Uncommon/rare but extremely severe side effects include aplastic anemia, agranulocytosis, hepatotoxicity, renal toxicity, suicidal ideation, lupus erythematosus and hyponatremia (mild, transient and usually reversible). The instructions for use of carbamazepine contain a warning about the possibility of serious dermatological reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis, maculopapular rashes and drug reactions with eosinophilia and systemic symptoms (DRESS syndrome), which usually occur during the first months of treatment. In addition, the instructions contain a warning about the risk of aplastic anemia and the risk of agranulocytosis. nine0003
Due to the increased risk of suicidal behavior, patients should be closely monitored for suicidality and clinical deterioration, especially during the first months of treatment.
Dose adjustment recommended for patients with hepatic impairment. Carbamazepine is contraindicated in patients with a history of hepatic porphyria.
Carbamazepine is contraindicated in patients with a history of hepatic porphyria.
Elderly patients may be more susceptible to side effects and therefore may be better suited to lower doses. According to the International League of Epilepsy (ILAE), carbamazepine is not a first-line drug for the elderly due to its high potential for drug interactions. nine0003
In general, carbamazepine should be administered gradually, with dose titration based on efficacy and side effects (with blood concentrations of carbamazepine ranging from 6 to 12 µg/mL), and dose adjustment based on clinical response and liver function . Carbamazepine should always be stopped gradually, avoiding sudden stops that may lower the seizure threshold.
The most common side effects of gabapentin are sedation, dizziness, ataxia, fatigue, tremor, nystagmus and peripheral edema. Other possible side effects include blurred vision, vomiting, dyspepsia, diarrhea, dry mouth, constipation, and weight gain. nine0003
nine0003
Gabapentin can also cause sexual dysfunction such as loss of libido, inability to achieve orgasm and erectile dysfunction.
Patients with a history of myoclonus or myasthenia gravis should not use gabapentin as it may cause symptoms of both conditions.
In 2009, the FDA issued a warning about the increased risk of suicidal behavior in patients taking anticonvulsants, including gabapentin. There is evidence of a two-fold increase in the likelihood of suicidal thoughts in patients with bipolar I disorder treated with gabapentin compared with patients taking lithium. nine0003
In addition, cases of DRESS syndrome, hypersensitivity, and sudden and unexplained death have been reported in patients with epilepsy, anaphylaxis, and angioedema.
The FDA has issued a warning of serious, life-threatening respiratory depression potentially associated with gabapentin, especially when used with CNS depressants (eg, opioids) and in patients with severe respiratory problems.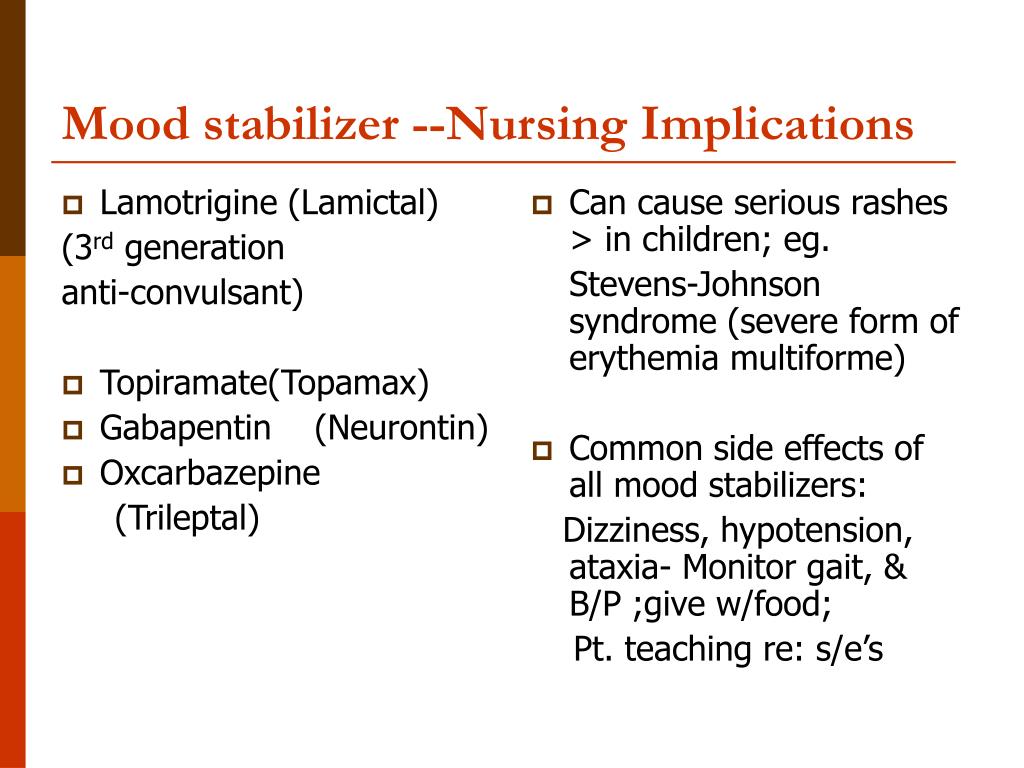
Gabapentin is associated with abuse and dependence, especially in the presence of substance use disorders, most commonly opioids. Withdrawal symptoms, often reminiscent of benzodiazepine withdrawal, play a role in the addiction described by some patients.
Abrupt or rapid discontinuation of gabapentin may lead to an increased risk of seizures in patients with epilepsy and an increased risk of relapse of bipolar disorder. Therefore, if you need to stop taking the drug, you need to gradually reduce the dosage over a period of at least one week. nine0003
Elderly patients may be more susceptible to side effects due to a greater likelihood of withdrawal. It has been hypothesized that the elderly are more vulnerable due to age-related decline in GABA-mediated cortical inhibition and changes in glutamate receptor expression. Since the elderly are at higher risk of respiratory depression, it is recommended to adjust the gabapentin dosage according to the clinical picture, as well as taking into account how the kidneys are functioning. nine0003
nine0003
In known cases of overdose, a wide range of symptoms have been observed, from drowsiness, sedation and blurred vision, to coma and death.
The most common side effects of lamotrigine are: headache, rash, dizziness, nausea, vomiting, diarrhea, dyspepsia, abdominal pain, blurred or double vision, insomnia, tremor, ataxia, accidental injury, rhinitis, pain in the throat, severe cough, infections, back pain, flu-like syndrome, asthenia, mania and emotional lability. These symptoms appear mainly during dose increases and in most cases regress with continued therapy. nine0003
The most common side effects that lead to discontinuation of lamotrigine are rash, but also mania, hypomania, mixed mood episodes. If a rash occurs during titration, it is recommended to monitor the therapeutic concentrations of lamotrigine in the blood.
Maintenance therapy with lamotrigine does not affect body weight.
Instructions for use contain a warning about dangerous skin reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. There is evidence that the inclusion of valproic acid in a multidrug regimen increases the risk of dangerous skin manifestations. nine0003
There is evidence that the inclusion of valproic acid in a multidrug regimen increases the risk of dangerous skin manifestations. nine0003
In 2018, the FDA required the addition of a risk warning for hemophagocytic lymphohistiocytosis, a rare but potentially life-threatening condition. This condition may occur within a few days or a few weeks after starting treatment.
Hypersensitivity reactions, some fatal or life threatening, have also been observed. Manifestations may include multiple organ failure or dysfunction, including hepatic dysfunction and disseminated intravascular coagulation. nine0003
Published reports of dyscrasia, which may or may not be associated with hypersensitivity syndrome. Dyscrasias include neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, and, rarely, aplastic anemia and erythroblastopenia.
Lamotrigine, like other antiepileptic drugs, may increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication.
Lamotrigine increases the risk of aseptic meningitis. Symptoms that need to be addressed immediately include headache, fever, nausea, vomiting, and neck stiffness. In most cases, symptoms disappear when lamotrigine is stopped. Some studies have identified a possible correlation between aseptic meningitis and underlying diagnoses of systemic lupus erythematosus or other autoimmune diseases in patients taking lamotrigine, suggesting that aseptic meningitis was a manifestation of a drug hypersensitivity reaction. nine0003
Lamotrigine-induced neuroleptic malignant syndrome has been reported in people taking antipsychotics.
Multiple organ failure, sometimes fatal or irreversible, is rare and occurs in association with other serious medical conditions.
Several cases of psychiatric symptoms have been described, such as auditory and visual hallucinations, vivid dreams, delirium, and delusions. nine0003
Overdose of lamotrigine is characterized by severe central nervous system depression, convulsions, cardiac conduction delay, wide complex tachycardia and death. Adults with serum concentrations >25 mg/l may develop severe toxic effects.
Adults with serum concentrations >25 mg/l may develop severe toxic effects.
Lamotrigine binds to melanin-containing tissues such as the eyes and pigmented skin. Therefore, in long-term treatment, ophthalmologic examinations may be considered. nine0003
Several studies report the safety of lamotrigine in children and adolescents under 18 years of age for the treatment of bipolar disorder.
The most common side effects of lithium are: fine hand tremor, polyuria, mild thirst, gastrointestinal symptoms (nausea, usually transient and mild; dyspepsia, vomiting and diarrhea), general discomfort, which are mainly observed in at the beginning of treatment, may persist during treatment or disappear spontaneously. These side effects are more likely to occur at higher dosages or higher blood lithium concentrations and therefore appropriate dosage considerations and clinical and laboratory monitoring should be undertaken. Simultaneous intake with food or switching to another lithium preparation may reduce gastrointestinal symptoms. nine0003
nine0003
In the therapeutic range, other side effects may occur, such as mild cognitive impairment (lack of spontaneity, fragmentary memory impairment, decreased reactivity, decreased processing speed, increased reaction time and memory impairment), weight gain (mainly in women) , acne, psoriasis and rare disorders such as hypercalcemia. Weight gain of more than 5 kg in the first year of treatment appears to be a predictor of hypothyroidism. nine0003
Long-term side effects include thyroid disease (hypothyroidism), renal dysfunction (impaired concentrating ability, polyuria, nephrogenic diabetes insipidus with secondary polydipsia), cardiac side effects (usually reversible and rarely symptomatic). Hypothyroidism is usually treated with thyroid hormone replacement therapy.
Benign, dose-dependent postural tremor is common in patients taking lithium, occurring early in treatment and potentially exacerbating physiological tremor. Lithium has various effects on the hypothalamic-pituitary-thyroid axis (goiter, hypothyroidism, hyperthyroidism), predominantly inhibits the release of thyroid hormones, blocks the activity of thyroid-stimulating hormone and enhances the peripheral degradation of thyroxine. Hyperparathyroidism and subsequent hypercalcemia may also occur during long-term lithium treatment. nine0003
Hyperparathyroidism and subsequent hypercalcemia may also occur during long-term lithium treatment. nine0003
In general, due to potential cardiotoxic effects, lithium should not be taken in patients with acute myocardial infarction, Brugada syndrome, or other cardiovascular conditions. Lithium should be taken with caution and under medical supervision in patients with cardiac arrhythmia, reduced kidney function, psoriasis, hypothyroidism, myeloid leukemia, Addison's disease, myasthenia gravis, and epilepsy.
Lithium-associated benign intracranial hypertension (associated with papilledema, headache, decreased vision, and risk of blindness) has been reported and usually resolves with discontinuation of lithium or, occasionally, surgery. nine0003
There have been several cases of the rare Lithium Irreversible Neurotoxicity Syndrome in lithium toxicity, in which there is cerebellar dysfunction with ataxia or unsteady gait.
Instructions for use contain a warning that the toxicity of lithium depends on the blood concentration, which should be checked regularly during therapy.
Morphological changes such as glomerular and interstitial fibrosis and nephron atrophy have been reported in patients receiving long-term lithium therapy. Due to these renal changes, the glomerular filtration rate can decrease up to, in very rare cases, progressive renal failure. In an even smaller subgroup of patients treated with lithium, the condition worsened towards end-stage renal disease or dialysis and/or kidney transplant. However, these morphological changes and their relationship to lithium therapy have not yet been fully established. In fact, these effects are uncommon, highly dependent on age-related decline in kidney function, and can be predicted by an increase in blood creatinine or a decrease in creatinine clearance. Taking into account the above reasons, dose adjustment is recommended for patients with moderate or severe renal insufficiency, with frequent monitoring of lithium and creatinine clearance. In addition, lithium is generally contraindicated in patients with severe renal insufficiency. nine0003
nine0003
Careful monitoring should be carried out in the case of co-administration of the drug with serotonergic agents, due to an increased risk of serotonin syndrome, although there are only a few reports that have analyzed this interaction.
Special dose selection is recommended for the elderly.
The most common side effects of oxcarbazepine are: sedation, dizziness, headache, ataxia, nystagmus, gait disturbance, confusion, nervousness, fatigue, nausea, vomiting, tremor. These side effects are usually dose dependent, occur in the first weeks of treatment, and are reversible. nine0003
Other Uncommon/Rare Side Effects: diplopia, dizziness, visual disturbances, rash, DRESS syndrome/multi-organ hypersensitivity.
Oxcarbazepine can also cause hyponatremia, usually occurring within the first three months of therapy.
Serious dermatological reactions, including Stevens-Johnson Syndrome and toxic epidermal necrolysis, should be observed. An association has been demonstrated between the presence of HLA-B*1502 and the risk of developing Stevens-Johnson Syndrome and toxic epidermal necrolysis after taking oxcarbazepine. nine0003
An association has been demonstrated between the presence of HLA-B*1502 and the risk of developing Stevens-Johnson Syndrome and toxic epidermal necrolysis after taking oxcarbazepine. nine0003
Like all classic mood stabilizers, oxcarbazepine may increase the risk of suicidal thoughts or behavior.
Oxcarbazepine is relatively hematologically safe. Although pancytopenia, agranulocytosis, and leukopenia have been reported in patients treated with oxcarbazepine, it is a relatively hematologically safe drug.
Oxcarbazepine has some effect on female reproductive endocrine function. nine0003
Oxcarbazepine is generally better tolerated in elderly patients than carbamazepine; The most commonly reported side effects are symptomatic hyponatremia with mild symptoms.
Abrupt discontinuation of oxcarbazepine may lead to an increased risk of seizures and status epilepticus in patients with epilepsy, the development of a withdrawal syndrome, and an increased risk of relapse of bipolar disorder.
Most reported pregabalin-induced adverse events are usually reversible and dose-dependent and occur within the first two weeks of treatment initiation. The most common side effects of pregabalin, which are the main reason for discontinuation of treatment, are drowsiness and dizziness.
Other common side effects: blurred vision, difficulty concentrating/attention, dry mouth, peripheral edema, weight gain, headache, increased creatine kinase, ataxia, tremor, dysarthria, paresthesia, incoordination, confusion, euphoric mood, irritability, vomiting, constipation, libido changes and erectile dysfunction. nine0003
Uncommon/rare side effects: angioedema, hypersensitivity, decreased platelet count, prolongation of the PR interval.
In addition, pregabalin may increase the risk of suicidal thoughts or behavior.
The FDA has issued a Special Warning for severe, life-threatening respiratory depression after pregabalin, more likely when pregabalin is co-administered with CNS depressants such as opioids, and in patients with severe respiratory problems. nine0003
nine0003
Because pregabalin is eliminated primarily by renal excretion, dose adjustment is necessary in patients with impaired renal function.
Abrupt discontinuation of pregabalin may lead to increased risk of seizures in patients with epilepsy, withdrawal symptoms such as insomnia, nausea, headache, restlessness, nervousness, irritability, hyperhidrosis and diarrhea. If pregabalin needs to be discontinued, it is recommended that the dosage be tapered gradually over a period of ≥1 week. nine0003
The most common side effects of topiramate are dizziness, weight loss, gastrointestinal symptoms (eg, diarrhea, nausea, constipation), paresthesia, insomnia, drowsiness, fatigue, dry mouth, and depression.
Rarely described: acute myopia and exacerbation of secondary angle-closure glaucoma, as well as other ophthalmic diseases, including myopia, small anterior chamber syndrome, ocular hyperemia, decreased visual acuity and / or eye pain.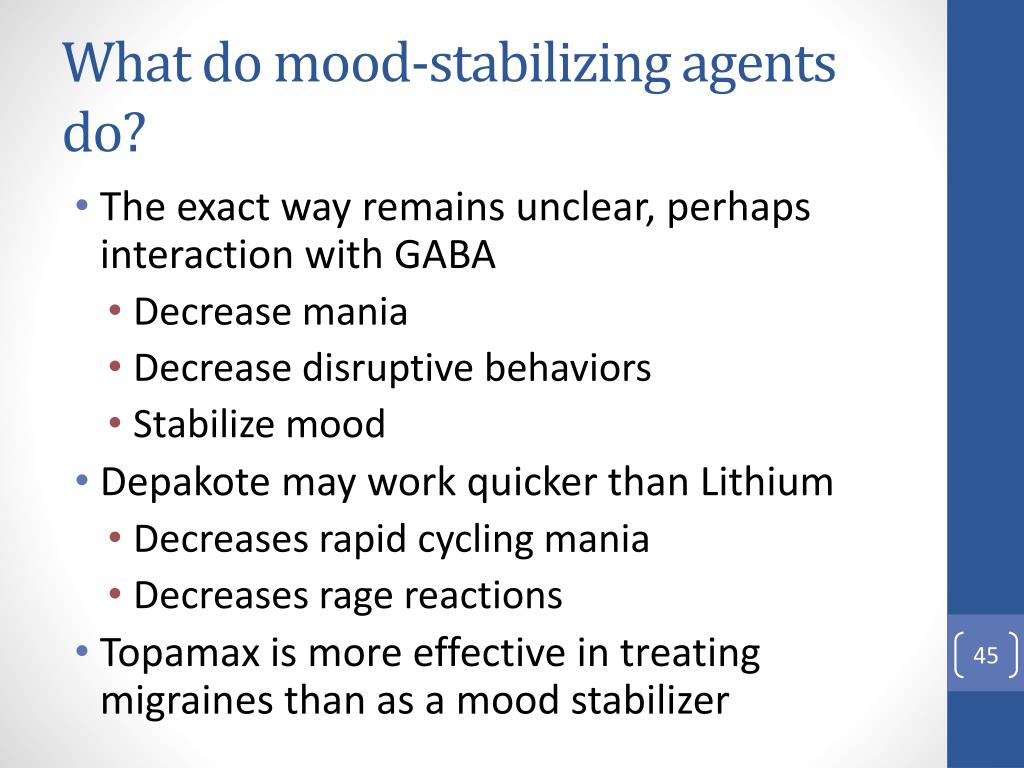 Other commonly reported side effects are dysgeusia and memory impairment. nine0003
Other commonly reported side effects are dysgeusia and memory impairment. nine0003
Cognitive (eg, confusion, psychomotor slowdown, attention/concentration/memory difficulties, speech problems, etc.) and sedative effects are mainly dose dependent and may be attenuated if topiramate is titrated slowly and gradually over eight weeks.
In general, the side effects of topiramate are generally mild to moderate, usually occurring within a month of starting and stopping when the dose is reduced. nine0003
If ophthalmic side effects persist, topiramate should be discontinued.
Renal tubular acidosis or hyperchloremic metabolic acidosis may be caused by topiramate. Topiramate may be accompanied by an acid-base imbalance due to the induction of renal bicarbonate loss, which may be associated with cardiac arrhythmia, a predisposition to nephrolithiasis in approximately 1.5% of patients taking topiramate, or conditions such as oligohidrosis and hyperthermia, in especially in children and / or while taking carbonic anhydrase inhibitors and anticholinergic drugs.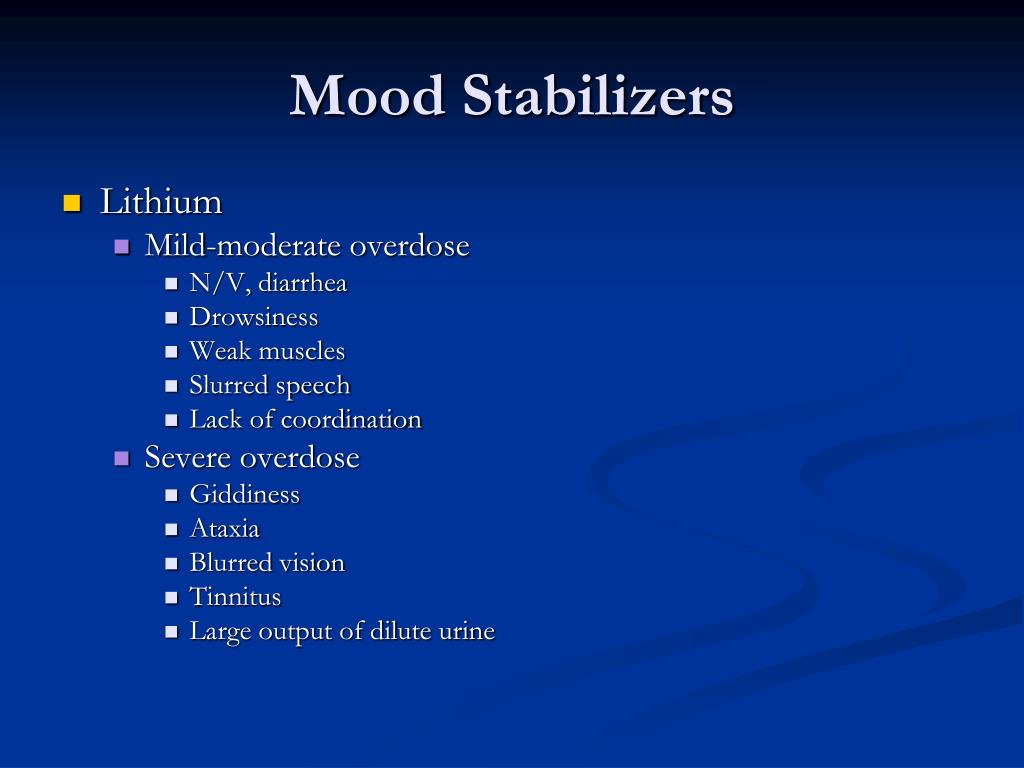 Acidosis may present clinically with dyspnoea, hyperventilation, nonspecific symptoms such as fatigue and anorexia, confusion, or other acute changes in mental status, along with changes in laboratory values reflecting elevated blood chloride levels and decreased bicarbonate levels, in the absence of chronic respiratory alkalosis. This rare event can occur at any time during treatment with topiramate. If a patient receiving topiramate develops acute changes in mental status, an assessment of basic laboratory parameters of metabolism is required. The described cases suggest that this process, as a rule, stops after the abolition of topiramate. nine0003
Acidosis may present clinically with dyspnoea, hyperventilation, nonspecific symptoms such as fatigue and anorexia, confusion, or other acute changes in mental status, along with changes in laboratory values reflecting elevated blood chloride levels and decreased bicarbonate levels, in the absence of chronic respiratory alkalosis. This rare event can occur at any time during treatment with topiramate. If a patient receiving topiramate develops acute changes in mental status, an assessment of basic laboratory parameters of metabolism is required. The described cases suggest that this process, as a rule, stops after the abolition of topiramate. nine0003
Topiramate may cause dose-dependent hyperammonemia with or without encephalopathy, especially in patients taking valproic acid concomitantly.
Like all classic mood stabilizers, topiramate may increase the risk of suicidal thoughts or behavior. It is recommended to adjust the dose in patients with moderate or severe renal and / or hepatic insufficiency.
The most common side effects of valproic acid are gastrointestinal upset (anorexia, nausea, dyspepsia, vomiting, diarrhea), tremor, sedation and weight gain. Most of the common side effects are dose-related, usually occurring at the start of therapy and reversing during treatment, or attenuated by dose reduction. One of the common and unfavorable side effects is alopecia. nine0003
Rare side effects include: persistent increase in liver transaminases, ataxia, dysarthria, asymptomatic leukopenia and thrombocytopenia, usually reversible by dose reduction or discontinuation of the drug. Valproic acid can induce a decrease in bone mineral density. There have been reports of an increase in the incidence of polycystic ovary syndrome and polycystic ovary syndrome in women taking valproic acid, although the correlation is still controversial. Rare but extremely severe side effects: fatal hepatotoxicity, hemorrhagic pancreatitis and agranulocytosis, bleeding disorders, respiratory muscle weakness and respiratory failure, encephalopathy and coma.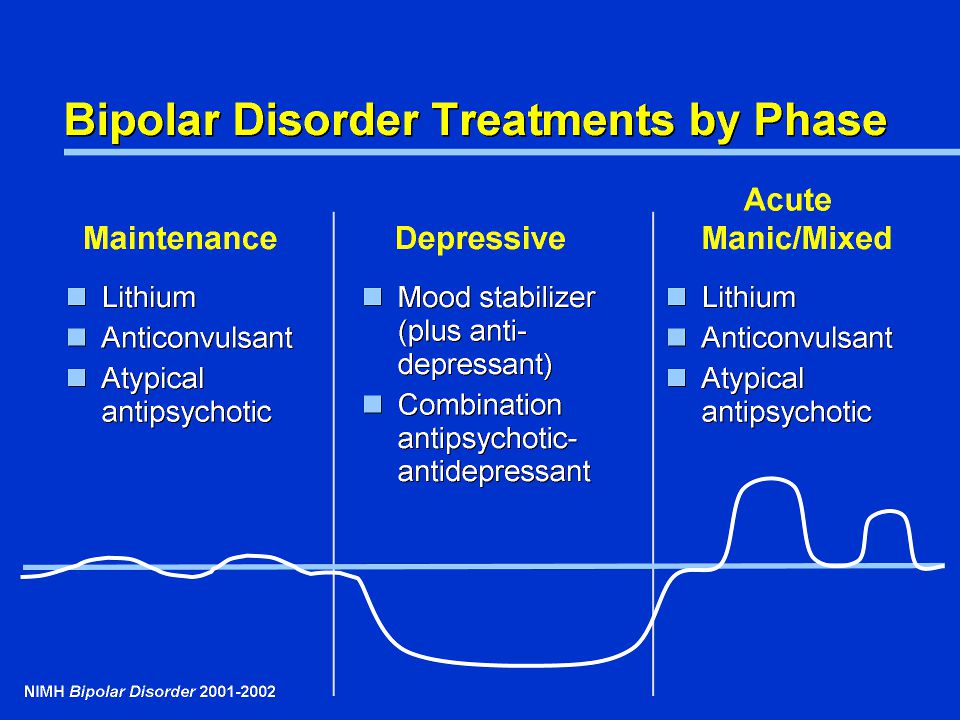 nine0003
nine0003
Valproic acid has a wide therapeutic window, so unintentional overdose is rare. Overdose signs: drowsiness, atrioventricular blockade, coma. Hemodialysis may be helpful, and naloxone may reverse the depressive effect on the CNS. L-carnitine is indicated in patients with acute overdose and as a prophylaxis in patients at high risk. Hypothermia and hyperammonemia have been reported. Hyperammonemic encephalopathy, sometimes fatal, has been observed in patients with urea cycle disorders. The simultaneous use of topiramate and valproic acid is associated with hyperammonemia with or without encephalopathy. Rarely, multi-organ hypersensitivity reactions have been reported. nine0003
The FDA has issued a warning due to an increased risk of liver failure, especially in children and usually occurring within the first six months of taking valproic acid. The instructions for use also contain a warning about the risk of developing pancreatitis, in rare cases hemorrhagic with rapid progression to death.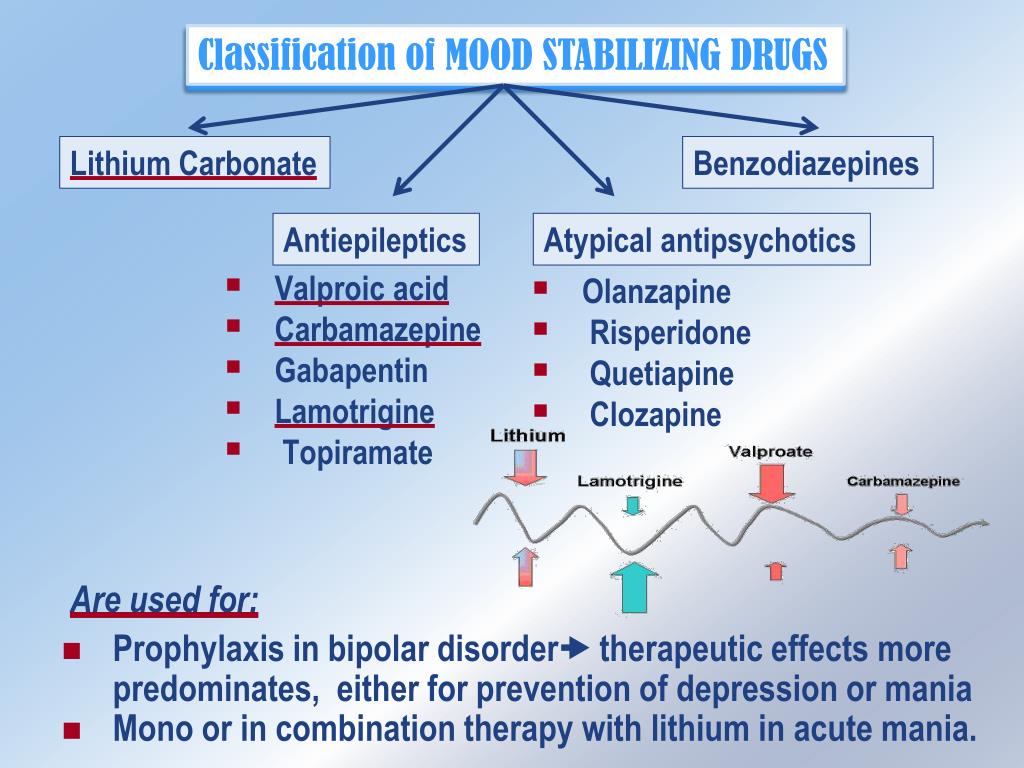
Summary table of laboratory monitoring during treatment with mood stabilizers
Translated by: Filippov D.S.
Source: Laura Orsolini, Simone Pompili & Umberto Volpe (2020) The 'collateral side' of mood stabilizers: safety and evidence-based strategies for managing side effects, Expert Opinion on Drug Safety, 19:11, 1461 -1495
Normotimics (mood stabilizers)0327 mood stabilization
. They are used both for the treatment of affective disorders and for the prevention of relapse. Normotimics also have the ability to alleviate "sharp corners of character", irritability, quarrelsomeness, irascibility, impulsivity, dysphoria in patients with various mental disorders. Lithium preparations, carbamazepine derivatives (carbamazepine and oxcarbazepine), valproates, lamotrigine are used as mood stabilizers. Common to these drugs is the need for strict medical monitoring of the patient's condition. nine0345 Ideally, blood concentrations of these drugs should be monitored regularly. An abrupt cessation of taking mood stabilizers can lead to a rapid resumption of affective fluctuations. Given this, the abolition of preventive therapy is carried out gradually, over several weeks.
nine0345 Ideally, blood concentrations of these drugs should be monitored regularly. An abrupt cessation of taking mood stabilizers can lead to a rapid resumption of affective fluctuations. Given this, the abolition of preventive therapy is carried out gradually, over several weeks.
Basic preparations:
1. Lithium salts.
For many years, lithium salts have been the standard treatment for bipolar disorder and the prevention of flare-ups. nine0003
Lithium preparations have been used for quite a long time and are therefore very well studied. A clear relationship was found between the concentration of the drug in blood plasma and its effect (both positive and side effects). In manic-depressive psychosis, lithium preparations are used as a preventive therapy, and, subject to constant monitoring of the lithium content in the blood, it is well tolerated. And with an increase in concentration above a certain level, the dosage is adjusted.
In the absence of such control, the frequency of side effects increases. Main side effects: increased thirst, tremor, nausea, muscle weakness, drowsiness, arrhythmia, changes in thyroid function.
Main side effects: increased thirst, tremor, nausea, muscle weakness, drowsiness, arrhythmia, changes in thyroid function.
2. Carbazepine derivatives (carbamazepine and oxcarbazepine).
These drugs were originally used as anticonvulsants and for trigeminal neuralgia. Further study showed their effectiveness in the treatment of patients with affective disorders, paroxysmal pain, aggressiveness, behavioral disorders, alcoholism. nine0003
The use of these drugs requires regular monitoring of the blood picture, as it can lead to a serious change in the leukocyte formula (agranulocytosis). In addition, it should be remembered that these drugs weaken the concentration of attention, reduce the effectiveness of anticoagulants and hormonal contraceptives.
3. Valproates.
Valproates are anticonvulsants, but recent studies have also proven the effectiveness of these drugs in the treatment and prevention of affective disorders. nine0003
nine0003
The exact mechanism of action of valproic acid in bipolar disorder is unknown, but there is evidence that it increases the synaptic concentration of gamma-aminobutyric acid (GABA), the brain's main inhibitory neurotransmitter.
Mild side effects usually occur at the start of therapy and usually resolve on their own. These include gastrointestinal disorders (nausea, vomiting, loss of appetite, heartburn, diarrhea), sedation, tremor. At the beginning of therapy, approximately half of the patients have a sedative effect. With continued use of valproic acid, this effect is reduced. Valproic acid can increase the concentration of cyclic antidepressants, as well as SSRIs, phenobarbital and other drugs. nine0003
4. Lamotrigine.
Lamotrigine is a drug originally used to treat epilepsy. Further study revealed its effectiveness in the treatment and prevention of affective disorders (especially depressive ones).
Usually minor side effects, but rash may occur in 10% of patients.