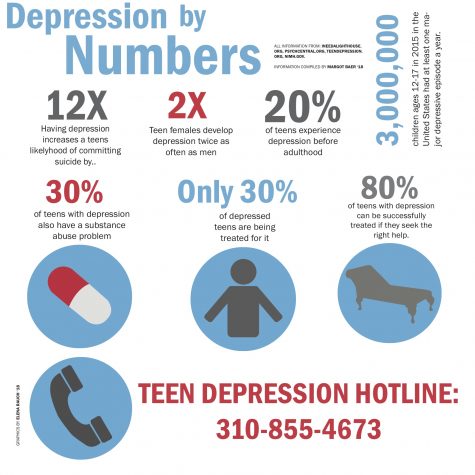
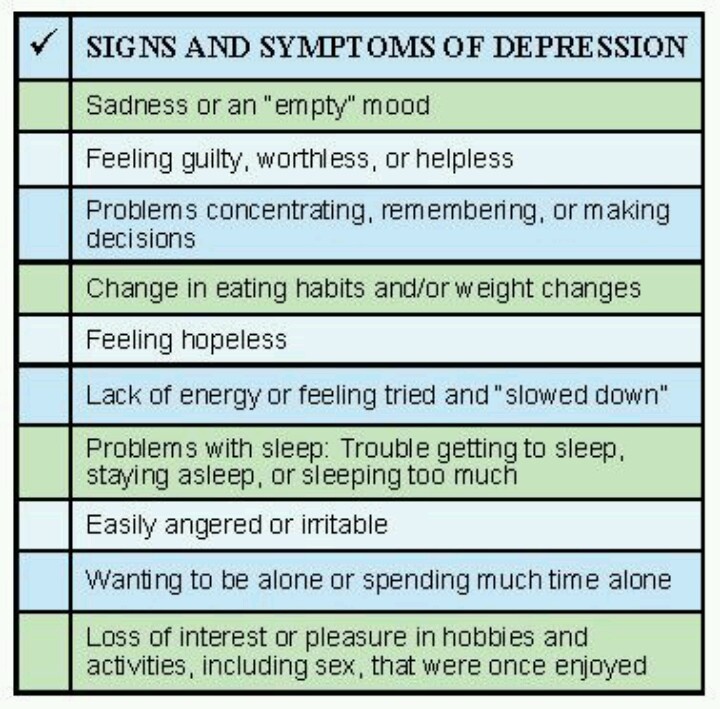
What are signs and symptoms of depression
Depression (major depressive disorder) - Diagnosis and treatment
Diagnosis
Your doctor may determine a diagnosis of depression based on:
- Physical exam. Your doctor may do a physical exam and ask questions about your health. In some cases, depression may be linked to an underlying physical health problem.
- Lab tests. For example, your doctor may do a blood test called a complete blood count or test your thyroid to make sure it's functioning properly.
- Psychiatric evaluation. Your mental health professional asks about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
- DSM-5. Your mental health professional may use the criteria for depression listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Types of depression
Symptoms caused by major depression can vary from person to person. To clarify the type of depression you have, your doctor may add one or more specifiers. A specifier means that you have depression with specific features, such as:
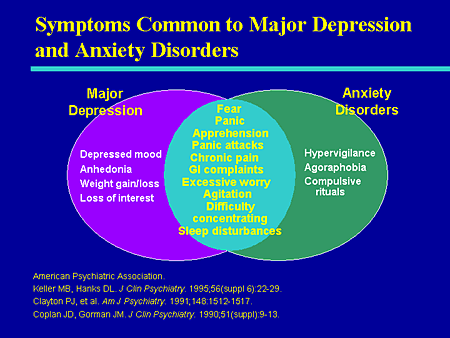
- Anxious distress — depression with unusual restlessness or worry about possible events or loss of control
- Mixed features — simultaneous depression and mania, which includes elevated self-esteem, talking too much and increased energy
- Melancholic features — severe depression with lack of response to something that used to bring pleasure and associated with early morning awakening, worsened mood in the morning, major changes in appetite, and feelings of guilt, agitation or sluggishness
- Atypical features — depression that includes the ability to temporarily be cheered by happy events, increased appetite, excessive need for sleep, sensitivity to rejection, and a heavy feeling in the arms or legs
- Psychotic features — depression accompanied by delusions or hallucinations, which may involve personal inadequacy or other negative themes
- Catatonia — depression that includes motor activity that involves either uncontrollable and purposeless movement or fixed and inflexible posture
- Peripartum onset — depression that occurs during pregnancy or in the weeks or months after delivery (postpartum)
- Seasonal pattern — depression related to changes in seasons and reduced exposure to sunlight
Other disorders that cause depression symptoms
Several other disorders, such as those below, include depression as a symptom.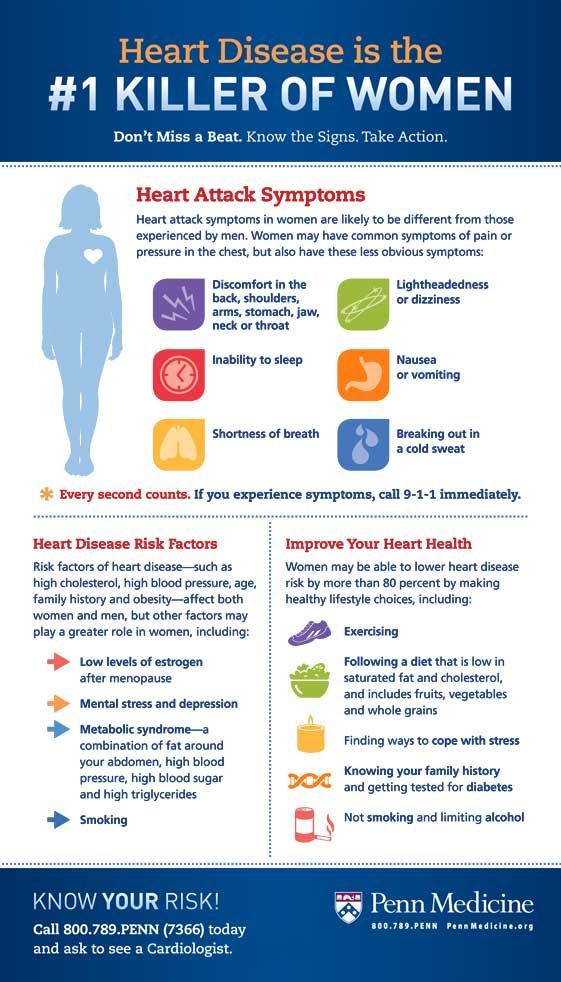 It's important to get an accurate diagnosis, so you can get appropriate treatment.
It's important to get an accurate diagnosis, so you can get appropriate treatment.
- Bipolar I and II disorders. These mood disorders include mood swings that range from highs (mania) to lows (depression). It's sometimes difficult to distinguish between bipolar disorder and depression.
- Cyclothymic disorder. Cyclothymic (sy-kloe-THIE-mik) disorder involves highs and lows that are milder than those of bipolar disorder.
- Disruptive mood dysregulation disorder. This mood disorder in children includes chronic and severe irritability and anger with frequent extreme temper outbursts. This disorder typically develops into depressive disorder or anxiety disorder during the teen years or adulthood.
- Persistent depressive disorder. Sometimes called dysthymia (dis-THIE-me-uh), this is a less severe but more chronic form of depression. While it's usually not disabling, persistent depressive disorder can prevent you from functioning normally in your daily routine and from living life to its fullest.
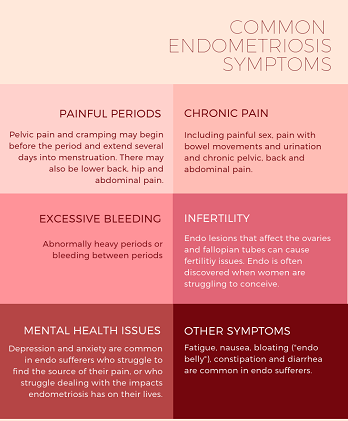
- Premenstrual dysphoric disorder. This involves depression symptoms associated with hormone changes that begin a week before and improve within a few days after the onset of your period, and are minimal or gone after completion of your period.
- Other depression disorders. This includes depression that's caused by the use of recreational drugs, some prescribed medications or another medical condition.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your depression (major depressive disorder)-related health concerns Start Here
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Complete blood count (CBC)
Treatment
Medications and psychotherapy are effective for most people with depression. Your primary care doctor or psychiatrist can prescribe medications to relieve symptoms. However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
If you have severe depression, you may need a hospital stay, or you may need to participate in an outpatient treatment program until your symptoms improve.
Here's a closer look at depression treatment options.
Medications
Many types of antidepressants are available, including those below. Be sure to discuss possible major side effects with your doctor or pharmacist.
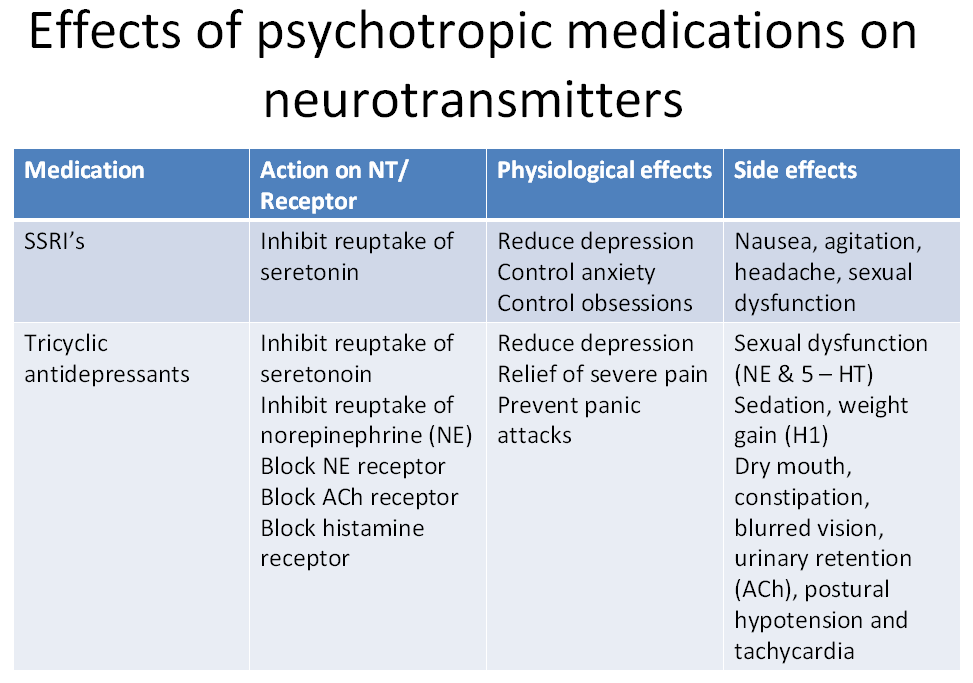
- Selective serotonin reuptake inhibitors (SSRIs). Doctors often start by prescribing an SSRI. These drugs are considered safer and generally cause fewer bothersome side effects than other types of antidepressants. SSRIs include citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft) and vilazodone (Viibryd).
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Examples of SNRIs include duloxetine (Cymbalta), venlafaxine (Effexor XR), desvenlafaxine (Pristiq, Khedezla) and levomilnacipran (Fetzima).

- Atypical antidepressants. These medications don't fit neatly into any of the other antidepressant categories. They include bupropion (Wellbutrin XL, Wellbutrin SR, Aplenzin, Forfivo XL), mirtazapine (Remeron), nefazodone, trazodone and vortioxetine (Trintellix).
- Tricyclic antidepressants. These drugs — such as imipramine (Tofranil), nortriptyline (Pamelor), amitriptyline, doxepin, trimipramine (Surmontil), desipramine (Norpramin) and protriptyline (Vivactil) — can be very effective, but tend to cause more-severe side effects than newer antidepressants. So tricyclics generally aren't prescribed unless you've tried an SSRI first without improvement.
- Monoamine oxidase inhibitors (MAOIs). MAOIs — such as tranylcypromine (Parnate), phenelzine (Nardil) and isocarboxazid (Marplan) — may be prescribed, typically when other drugs haven't worked, because they can have serious side effects. Using MAOIs requires a strict diet because of dangerous (or even deadly) interactions with foods ― such as certain cheeses, pickles and wines ― and some medications and herbal supplements.
 Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs.
Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs. - Other medications. Other medications may be added to an antidepressant to enhance antidepressant effects. Your doctor may recommend combining two antidepressants or adding medications such as mood stabilizers or antipsychotics. Anti-anxiety and stimulant medications also may be added for short-term use.
Finding the right medication
If a family member has responded well to an antidepressant, it may be one that could help you. Or you may need to try several medications or a combination of medications before you find one that works. This requires patience, as some medications need several weeks or longer to take full effect and for side effects to ease as your body adjusts.
Inherited traits play a role in how antidepressants affect you. In some cases, where available, results of genetic tests (done by a blood test or cheek swab) may offer clues about how your body may respond to a particular antidepressant. However, other variables besides genetics can affect your response to medication.
However, other variables besides genetics can affect your response to medication.
Risks of abruptly stopping medication
Don't stop taking an antidepressant without talking to your doctor first. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur.
Stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, and quitting suddenly may cause a sudden worsening of depression. Work with your doctor to gradually and safely decrease your dose.
Antidepressants and pregnancy
If you're pregnant or breast-feeding, some antidepressants may pose an increased health risk to your unborn child or nursing child. Talk with your doctor if you become pregnant or you're planning to become pregnant.
Antidepressants and increased suicide risk
Most antidepressants are generally safe, but the Food and Drug Administration (FDA) requires all antidepressants to carry a black box warning, the strictest warning for prescriptions.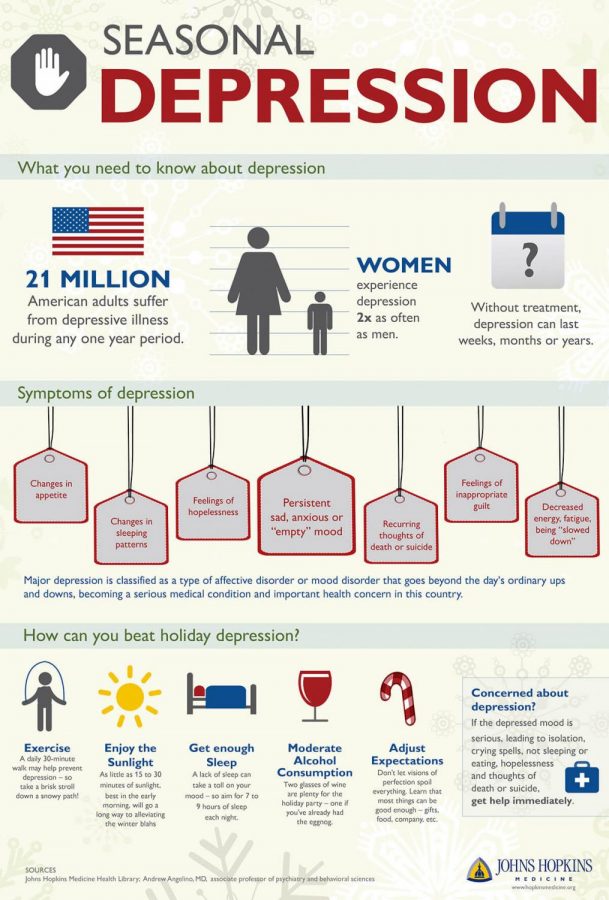 In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
Anyone taking an antidepressant should be watched closely for worsening depression or unusual behavior, especially when starting a new medication or with a change in dosage. If you or someone you know has suicidal thoughts when taking an antidepressant, immediately contact a doctor or get emergency help.
Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
Psychotherapy
Psychotherapy is a general term for treating depression by talking about your condition and related issues with a mental health professional. Psychotherapy is also known as talk therapy or psychological therapy.
Different types of psychotherapy can be effective for depression, such as cognitive behavioral therapy or interpersonal therapy. Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
- Adjust to a crisis or other current difficulty
- Identify negative beliefs and behaviors and replace them with healthy, positive ones
- Explore relationships and experiences, and develop positive interactions with others
- Find better ways to cope and solve problems
- Identify issues that contribute to your depression and change behaviors that make it worse
- Regain a sense of satisfaction and control in your life and help ease depression symptoms, such as hopelessness and anger
- Learn to set realistic goals for your life
- Develop the ability to tolerate and accept distress using healthier behaviors
Alternate formats for therapy
Formats for depression therapy as an alternative to face-to-face office sessions are available and may be an effective option for some people. Therapy can be provided, for example, as a computer program, by online sessions, or using videos or workbooks.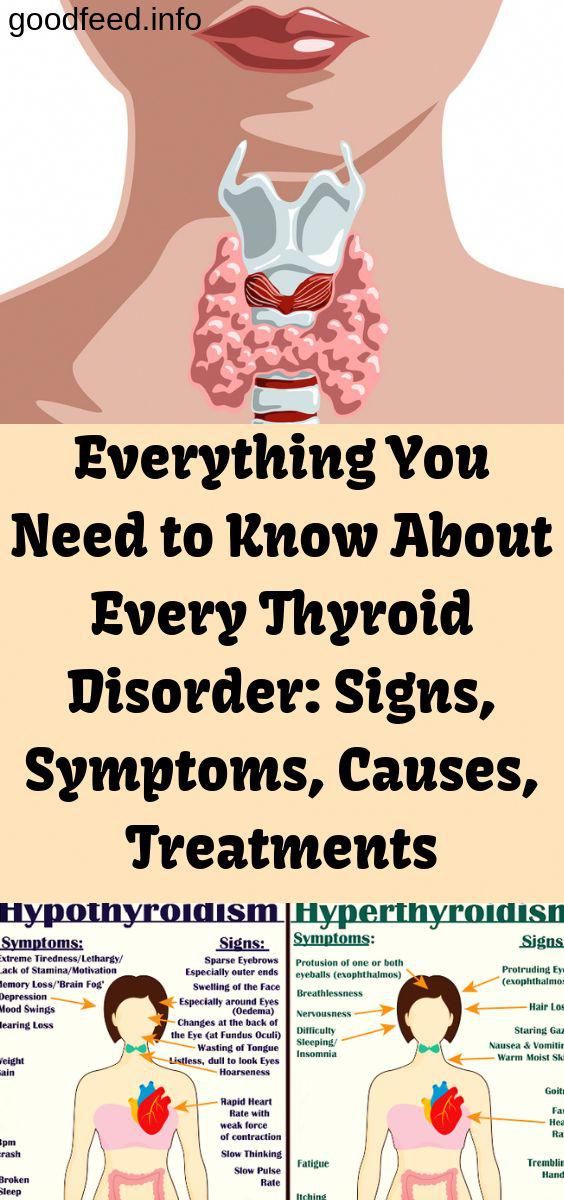 Programs can be guided by a therapist or be partially or totally independent.
Programs can be guided by a therapist or be partially or totally independent.
Before you choose one of these options, discuss these formats with your therapist to determine if they may be helpful for you. Also, ask your therapist if he or she can recommend a trusted source or program. Some may not be covered by your insurance and not all developers and online therapists have the proper credentials or training.
Smartphones and tablets that offer mobile health apps, such as support and general education about depression, are not a substitute for seeing your doctor or therapist.
Hospital and residential treatment
In some people, depression is so severe that a hospital stay is needed. This may be necessary if you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else. Psychiatric treatment at a hospital can help keep you calm and safe until your mood improves.
Partial hospitalization or day treatment programs also may help some people.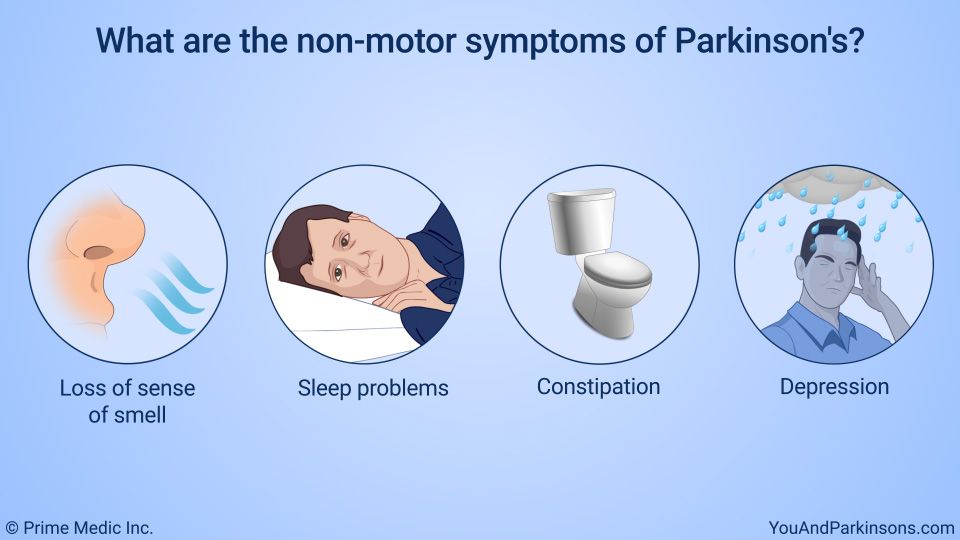 These programs provide the outpatient support and counseling needed to get symptoms under control.
These programs provide the outpatient support and counseling needed to get symptoms under control.
Other treatment options
For some people, other procedures, sometimes called brain stimulation therapies, may be suggested:
- Electroconvulsive therapy (ECT). In ECT, electrical currents are passed through the brain to impact the function and effect of neurotransmitters in your brain to relieve depression. ECT is usually used for people who don't get better with medications, can't take antidepressants for health reasons or are at high risk of suicide.
- Transcranial magnetic stimulation (TMS). TMS may be an option for those who haven't responded to antidepressants. During TMS, a treatment coil placed against your scalp sends brief magnetic pulses to stimulate nerve cells in your brain that are involved in mood regulation and depression.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Atypical antidepressants
- Monoamine oxidase inhibitors (MAOIs)
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- MAOIs and diet: Is it necessary to restrict tyramine?
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Depression generally isn't a disorder that you can treat on your own. But in addition to professional treatment, these self-care steps can help:
- Stick to your treatment plan. Don't skip psychotherapy sessions or appointments. Even if you're feeling well, don't skip your medications. If you stop, depression symptoms may come back, and you could also experience withdrawal-like symptoms. Recognize that it will take time to feel better.
- Learn about depression. Education about your condition can empower you and motivate you to stick to your treatment plan. Encourage your family to learn about depression to help them understand and support you.
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your depression symptoms. Make a plan so that you know what to do if your symptoms get worse. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
 Ask relatives or friends to help watch for warning signs.
Ask relatives or friends to help watch for warning signs. - Avoid alcohol and recreational drugs. It may seem like alcohol or drugs lessen depression symptoms, but in the long run they generally worsen symptoms and make depression harder to treat. Talk with your doctor or therapist if you need help with alcohol or substance use.
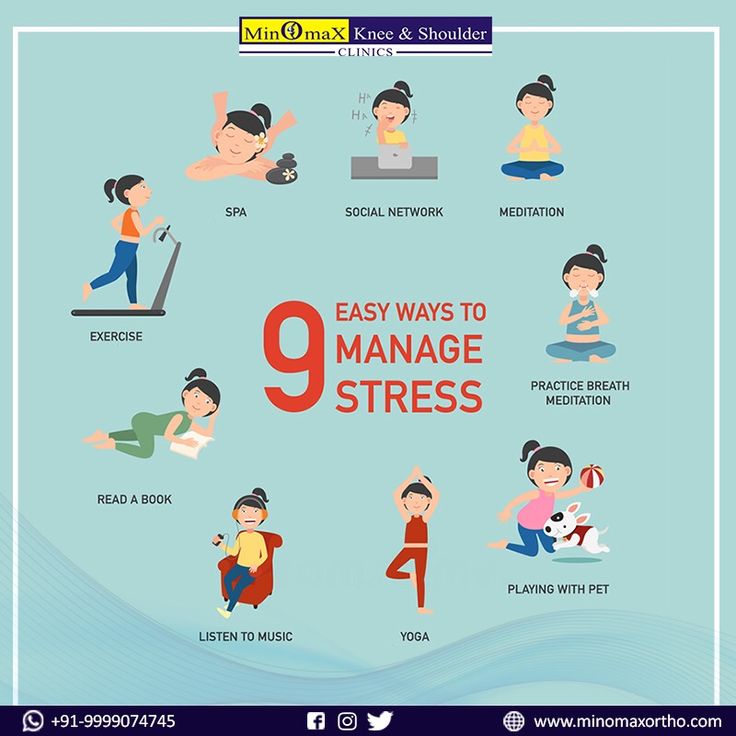
- Take care of yourself. Eat healthy, be physically active and get plenty of sleep. Consider walking, jogging, swimming, gardening or another activity that you enjoy. Sleeping well is important for both your physical and mental well-being. If you're having trouble sleeping, talk to your doctor about what you can do.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Depression, anxiety and exercise
Alternative medicine
Alternative medicine is the use of a nonconventional approach instead of conventional medicine. Complementary medicine is a nonconventional approach used along with conventional medicine — sometimes called integrative medicine.
Make sure you understand the risks as well as possible benefits if you pursue alternative or complementary therapy. Don't replace conventional medical treatment or psychotherapy with alternative medicine. When it comes to depression, alternative treatments aren't a substitute for medical care.
Supplements
Examples of supplements that are sometimes used for depression include:
- St. John's wort. Although this herbal supplement isn't approved by the Food and Drug Administration (FDA) to treat depression in the U.S., it may be helpful for mild or moderate depression. But if you choose to use it, be careful — St. John's wort can interfere with a number of medications, such as heart drugs, blood-thinning drugs, birth control pills, chemotherapy, HIV/AIDS medications and drugs to prevent organ rejection after a transplant. Also, avoid taking St. John's wort while taking antidepressants because the combination can cause serious side effects.
- SAMe.
 Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder.
Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder. - Omega-3 fatty acids. These healthy fats are found in cold-water fish, flaxseed, flax oil, walnuts and some other foods. Omega-3 supplements are being studied as a possible treatment for depression. While considered generally safe, in high doses, omega-3 supplements may interact with other medications. More research is needed to determine if eating foods with omega-3 fatty acids can help relieve depression.
Nutritional and dietary products aren't monitored by the FDA the same way medications are. You can't always be certain of what you're getting and whether it's safe. Also, because some herbal and dietary supplements can interfere with prescription medications or cause dangerous interactions, talk to your doctor or pharmacist before taking any supplements.
Mind-body connections
Integrative medicine practitioners believe the mind and body must be in harmony for you to stay healthy. Examples of mind-body techniques that may be helpful for depression include:
- Acupuncture
- Relaxation techniques such as yoga or tai chi
- Meditation
- Guided imagery
- Massage therapy
- Music or art therapy
- Spirituality
- Aerobic exercise
Relying solely on these therapies is generally not enough to treat depression. They may be helpful when used in addition to medication and psychotherapy.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Natural remedies for depression: Are they effective?
Coping and support
Talk with your doctor or therapist about improving your coping skills, and try these tips:
- Simplify your life. Cut back on obligations when possible, and set reasonable goals for yourself.
 Give yourself permission to do less when you feel down.
Give yourself permission to do less when you feel down. - Write in a journal. Journaling, as part of your treatment, may improve mood by allowing you to express pain, anger, fear or other emotions.
- Read reputable self-help books and websites. Your doctor or therapist may be able to recommend books or websites to read.
- Locate helpful groups. Many organizations, such as the National Alliance on Mental Illness (NAMI) and the Depression and Bipolar Support Alliance, offer education, support groups, counseling and other resources to help with depression. Employee assistance programs and religious groups also may offer help for mental health concerns.
- Don't become isolated. Try to participate in social activities, and get together with family or friends regularly. Support groups for people with depression can help you connect to others facing similar challenges and share experiences.
- Learn ways to relax and manage your stress. Examples include meditation, progressive muscle relaxation, yoga and tai chi.
- Structure your time. Plan your day. You may find it helps to make a list of daily tasks, use sticky notes as reminders or use a planner to stay organized.
- Don't make important decisions when you're down. Avoid decision-making when you're feeling depressed, since you may not be thinking clearly.
Preparing for your appointment
You may see your primary care doctor, or your doctor may refer you to a mental health professional. Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for your appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins or other supplements that you're taking, including dosages
- Questions to ask your doctor or mental health professional
Take a family member or friend along, if possible, to help you remember all of the information provided during the appointment.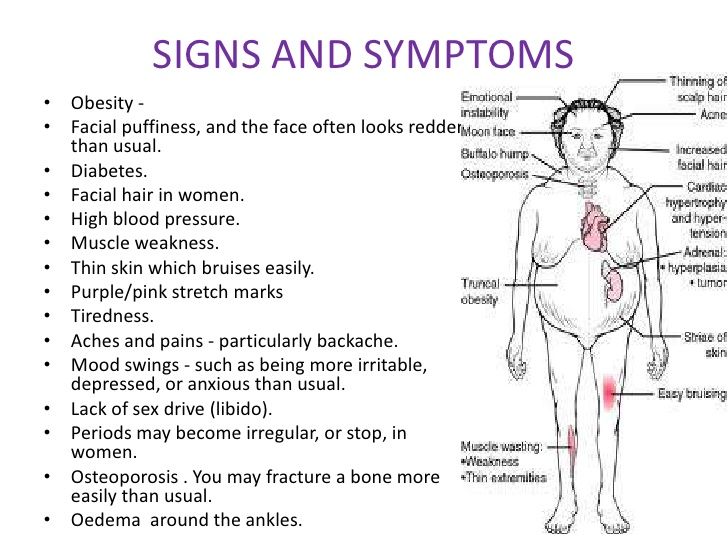
Some basic questions to ask your doctor include:
- Is depression the most likely cause of my symptoms?
- What are other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatment is likely to work best for me?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a psychiatrist or other mental health professional?
- What are the main side effects of the medications you're recommending?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you a number of questions.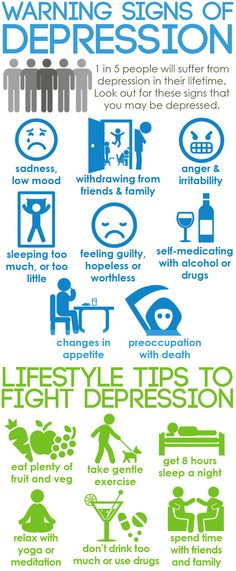 Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first notice your symptoms of depression?
- How long have you felt depressed? Do you generally always feel down, or does your mood fluctuate?
- Does your mood ever swing from feeling down to feeling intensely happy (euphoric) and full of energy?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with depression or another mood disorder?
- What other mental or physical health conditions do you have?
- Do you drink alcohol or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative.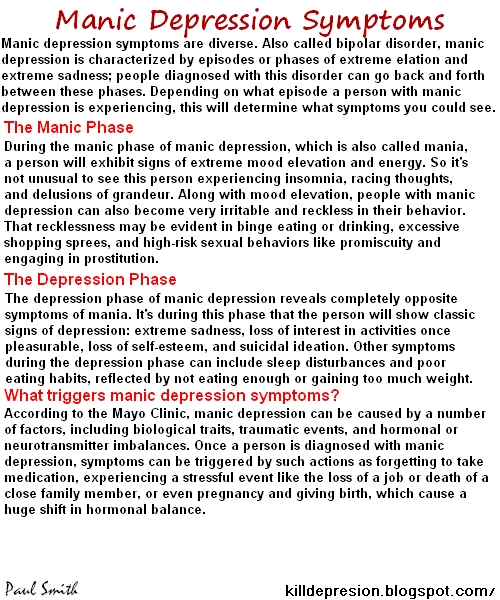 Currently, the 435748 (HELP4U) text messaging service is only available in English.
Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt.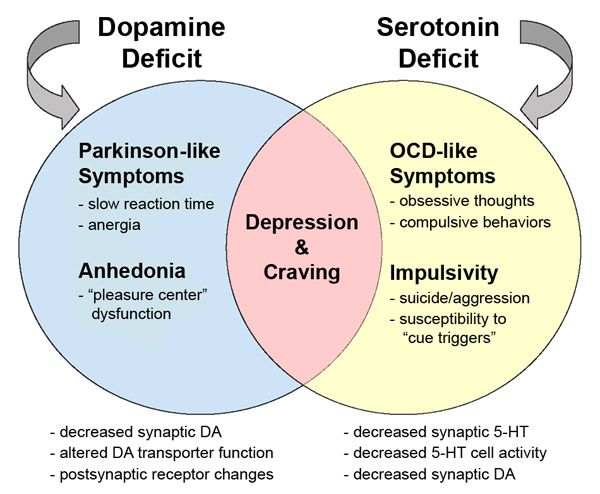 Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.
Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
symptoms, causes in men and women, remedies
Lack of vitality, unwillingness to get out of bed, bad mood for a long time, and even unwillingness to live are all signs of depression. Depression has a negative effect on the health and general well-being of a person. That is why it is so important to get medical help from a specialist in time.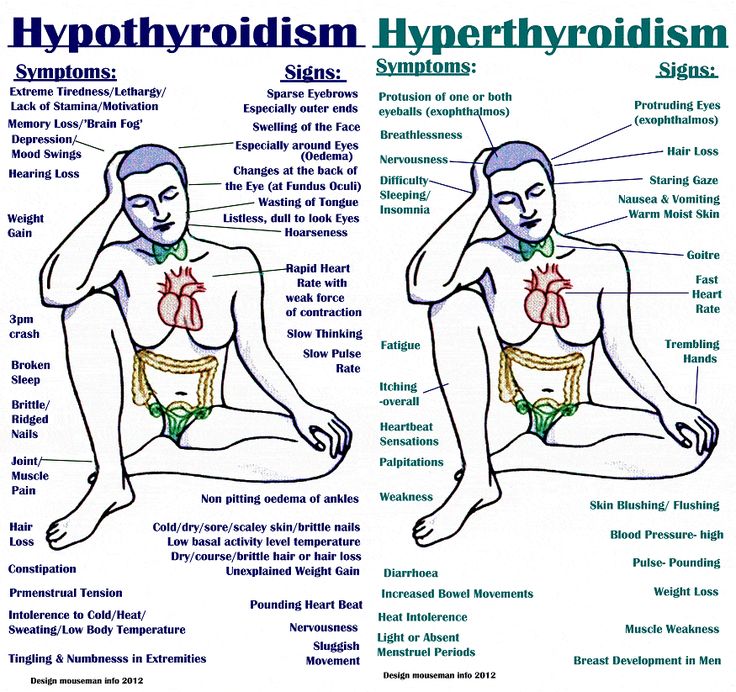
How to determine the presence of depression?
Pathology can appear after experienced stressful situations. If there is no disorder, after the problem is resolved, a good mood returns to the person. But when the cause is eliminated, and apathy, depression and loss of strength do not leave the person, it is necessary to seek help from a specialist. It may also decrease performance.
You can determine the presence of depression on your own, but you should not self-medicate even at an early stage of development. This should be done by a doctor, since self-medication can only aggravate everything.
Depression in women is often postpartum, as their lives change dramatically, and sleepless nights add fatigue. This is where frustration and apathy come in.
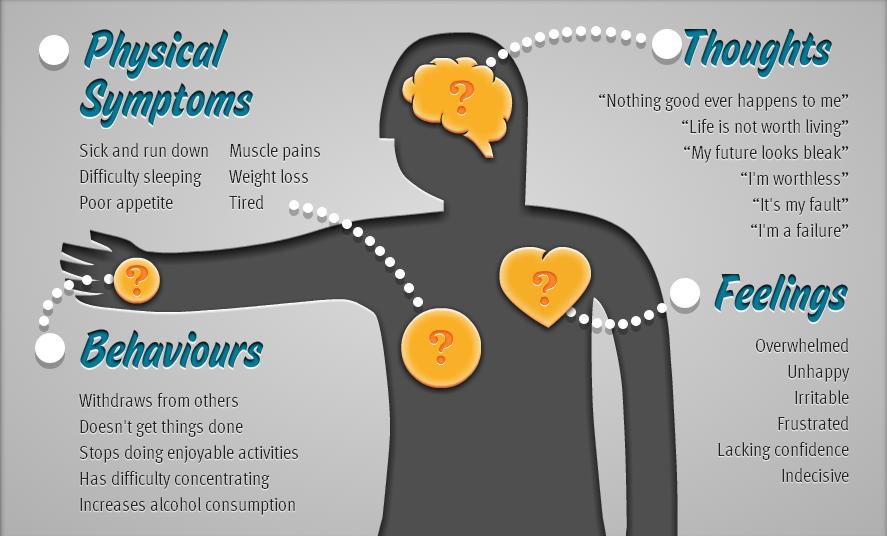
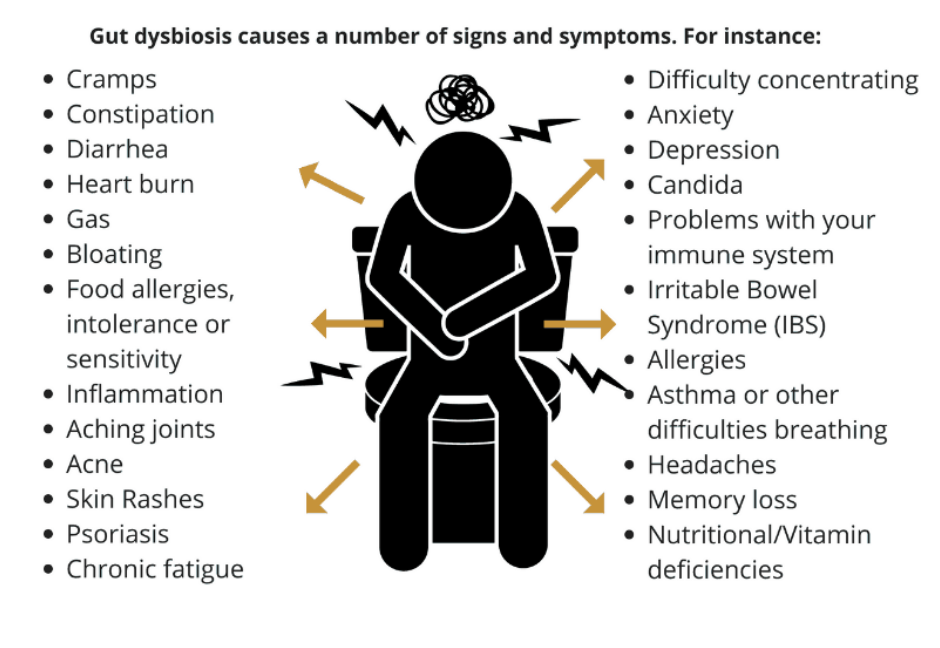
When the pathology is in advanced form, then a person has the following symptoms of depression - not only a bad mood and impotence, but also persistent disorders of the nervous system. There are also symptoms such as: a significant decrease in self-esteem, disadaptation in society, despondency and loss of interest in any events.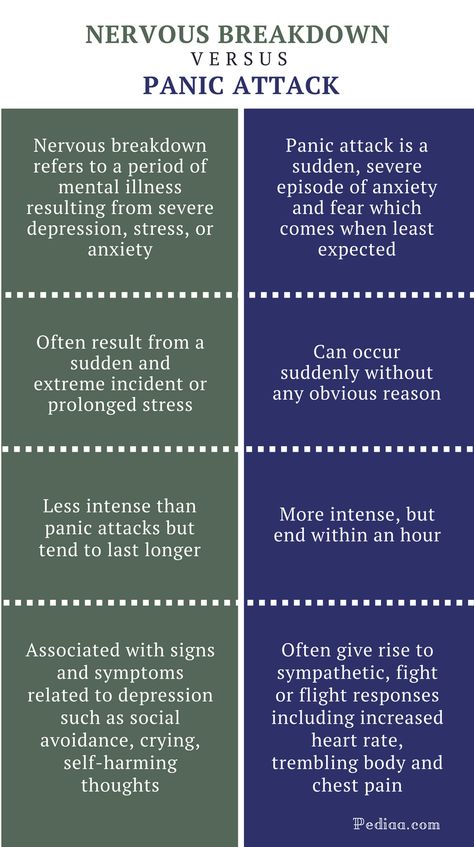
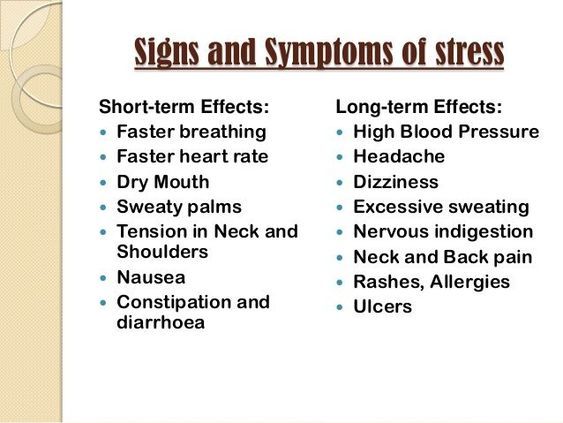
In physiological terms, appetite changes, intimate needs and energy decrease, sleep and bowel function are disturbed (constipation, weakness, fatigue during physical and intellectual stress are observed), pain in the body (in the heart, in muscles, in the stomach area).
The patient shows signs of depression such as loss of interest in other people, a tendency to frequent solitude, refusal of entertainment, use of alcohol and psychotropic substances.
Mental signs of depression include difficulty in concentrating, concentrating, making decisions, slowness of thinking, a pessimistic view of the future with a lack of perspective and thoughts about the meaninglessness of one's existence, suicide attempts, due to their uselessness, helplessness, insignificance.
Causes of depression
The appearance of the disorder is not influenced by age category or social class. Most often, depression appears against the background of stressful negative situations, with constant failures - then a person falls into despair from the inability to somehow influence the course of events.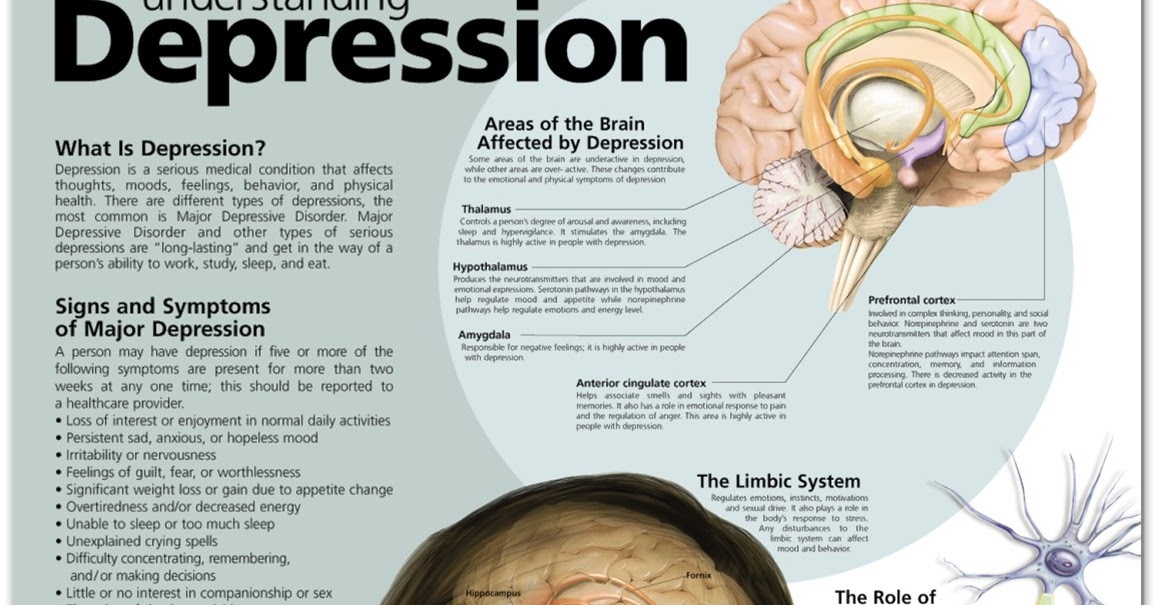
But in addition to the social factor, severe psychological trauma can also lead to the development of depression, for example: family breakup, death of a loved one, a serious illness that affects not only the patient himself, but also his relatives. In this case, depressions are referred to as reactive.
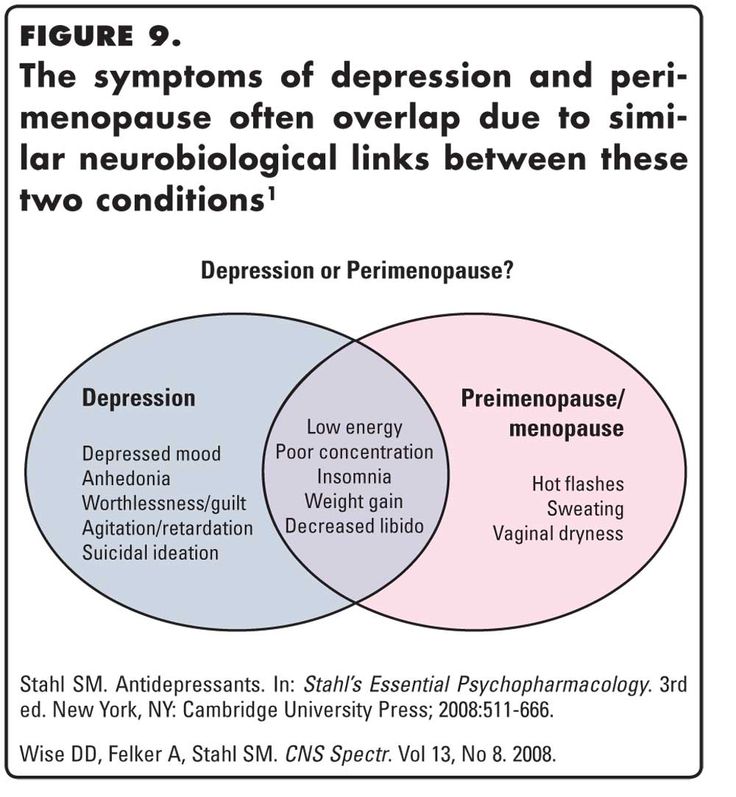
The likelihood of depression increases with changes in hormonal levels: during adolescence, after delivery, with the onset of menopause, and also in old age. It can affect the emotional and physical level.
Another factor is brain damage and somatic pathologies. Often depression affects patients who have had a stroke, suffering from a chronic lack of blood circulation in the brain, after a traumatic brain injury.
The causes of depression can manifest themselves as a result of the side effects of drugs (benzodiazepines, corticosteroids). Often this condition disappears on its own after the drug is discontinued.
Types of depression
-
Neurotic - people with low self-esteem, insecure, straightforward people often suffer.
 They constantly feel a sense of injustice, and apathy arises from this.
They constantly feel a sense of injustice, and apathy arises from this. -
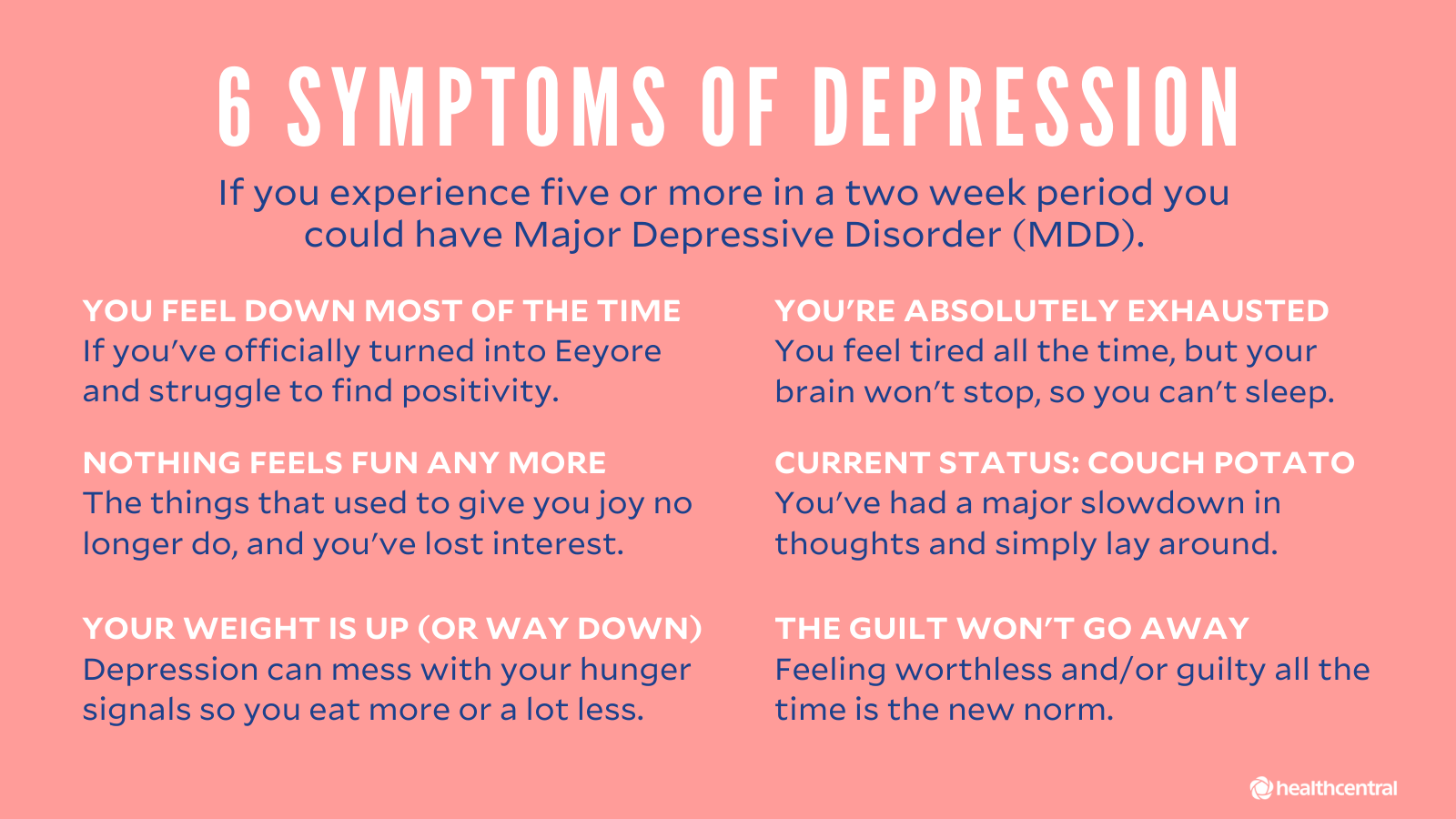
Clinical - bad mood, loss of energy, problems with appetite and sleep. Often there is a tendency to suicide. This clinical picture can last at least 2 weeks.
-
Vegetative - manifested by such signs as tachycardia, a drop in blood pressure, tinnitus.
-
Psychogenic - develops after severe psychological trauma - divorce, loss of a loved one, dismissal from work, betrayal, etc. Accompanied by mood swings, anxiety, excessive sensitivity.
-
Masked - often the disease manifests itself secretly. Apathy, solitude and a decrease in interest in life can only appear as negativity and fatigue accumulate.
-
Asthenic - the condition is manifested by fatigue, sleep disturbance, emotional imbalance due to accumulated difficulties, stress, physical and psychological stress.
-
Postpartum - usually occurs 10-14 days after delivery.
 A young mother shows an increased sense of excitement for the baby, and constant lack of sleep and fatigue worsen the situation even more. In addition, the hormonal background also affects the state of the mother.
A young mother shows an increased sense of excitement for the baby, and constant lack of sleep and fatigue worsen the situation even more. In addition, the hormonal background also affects the state of the mother. -
Somatogenic - attacks occur due to disturbances in the endocrine system, the formation and growth of neoplasms, both benign and malignant.
-
Alcoholic - depression is accompanied by excessive consumption of alcoholic beverages. The post-alcohol state is accompanied by an uncontrolled craving for alcohol and the growth of withdrawal syndrome when alcohol is refused.
-
Bipolar - the patient is changing euphoria depressive, manic disorder. But in the period between these phenomena, caused by various factors: stress, loss of means of popularity, etc., a person lives an ordinary life and does not show symptoms of the disease.
How does depression develop in stages?
First, the patient has a depressed state, which he himself attributes to fatigue, a hard working week, drinking alcohol and other reasons.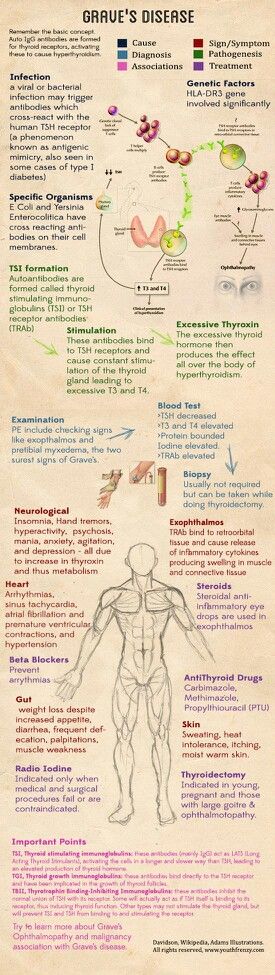 At the same time, he wants to retire from others and at the same time is afraid to be alone.
At the same time, he wants to retire from others and at the same time is afraid to be alone.
Then the stage of acceptance arises: the awareness of the dangerous state comes, the problem worsens, the intensity of negative thoughts grows, the body and the immune system fail.
The third stage - in the absence of adequate therapy, the patient loses control over himself, aggression increases.
Diagnosis and treatment of depression
-
To identify the disease, experienced specialists use short questionnaires - screening tools to identify symptoms: anxiety, anhedonia (loss of pleasure from life), suicidal tendencies. Thanks to this, it is possible to determine whether the patient has chronic depression, symptoms and treatments for depression, what form and severity it is.
To fully understand the picture of the disease, the doctor needs to familiarize himself with the symptoms that indicate depression, and not another psychological disorder.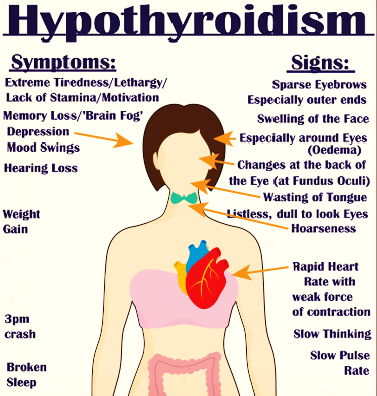
For the treatment of depression, you can contact the following specialists:
-
Psychiatrist - treatment of depression with hypnosis, drugs for acute mental pathologies - schizophrenia, mental retardation, epilepsy, as well as other less severe ailments - neurosis, depression, alcoholism, drug addiction, etc.
-
Psychotherapist – treatment is carried out through special therapy, which provides for explanations, conversations, search for solutions to problems together with the patient.
-
Psychologist - consults the patient, cannot prescribe drugs and examinations. Clinical psychologists use modern test methods to identify problems that caused a psychological disorder.
The main directions of therapy in treatment are psychotherapy, pharmacotherapy, social therapy.
A necessary condition for the effectiveness of treatment is cooperation and trust in the doctor.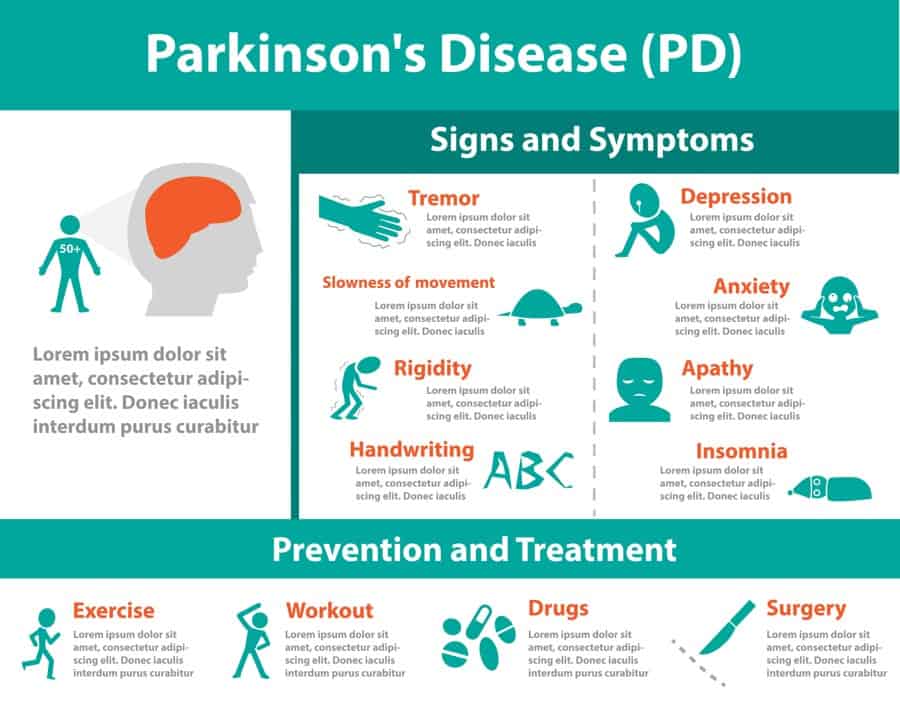 It is important to strictly follow the prescription of the therapy regimen, visit the doctor regularly, and give a detailed account of your condition.
It is important to strictly follow the prescription of the therapy regimen, visit the doctor regularly, and give a detailed account of your condition.
Preparations for the treatment of depression
-
For the treatment of the disorder, antidepressants are used for anxious depression or when the pathology is accompanied by lethargy. Antidepressants are prescribed directly by a doctor and are not recommended for self-administration. The action of many antidepressants manifests itself two weeks after administration, their dosage for the patient is determined individually.
In bipolar depression, depression is treated with insomnia. While it has a negative effect on a healthy person, in a patient with a psychological disorder, sleep deprivation, on the contrary, brings the psyche back to normal.
Moderate or mild depression requires the appointment of drugs on a light, natural basis (herbal).
Where to get tested and treated for depression in Krasnoyarsk?
If you or your loved ones show signs of an emotional disorder, you should immediately contact a specialist.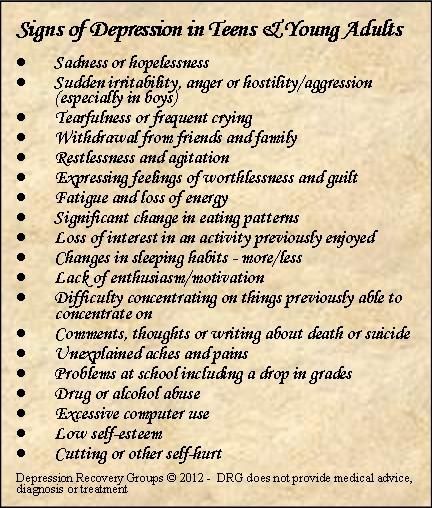 Since depression can lead to dangerous consequences:
Since depression can lead to dangerous consequences:
-
isolation from society
-
deterioration in appearance
-
relationship problems
-
low performance or its complete absence
-
sexual problems
Contact the private clinic "Medunion" in Krasnoyarsk, get examined and treated for depression. Our phone number for appointment +7 (391) 202-95-54.
Depression: symptoms, signs and treatment
Psychotherapist
Kumov
Mikhail Sergeevich
Experience 20 years
Psychotherapist, member of the Russian Professional Psychotherapeutic League
Make an appointment
The concept of "depression", as a whole complex of depressive disorders is called in medicine, indicates a serious violation of a person's activity and a decrease in his interest in the world around him and his own life.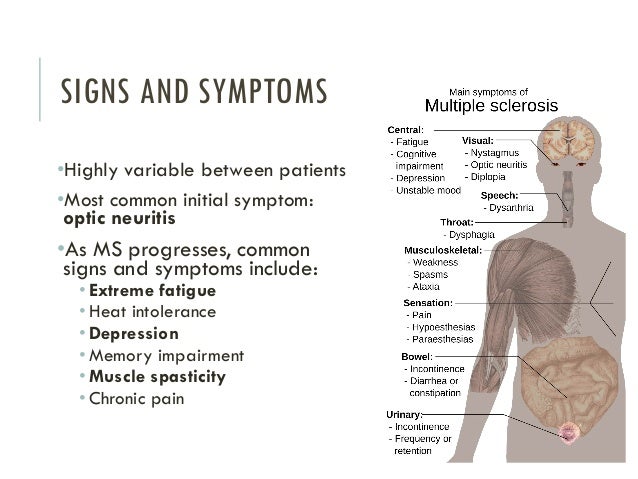 Establishing the exact cause of depression can be difficult, since several factors are possible: hereditary, physiological, neurological and psychosocial. It is possible to make an accurate diagnosis after studying the patient's history. The course of treatment involves a combination of several methods at once: conservative, psychotherapeutic and other measures.
Establishing the exact cause of depression can be difficult, since several factors are possible: hereditary, physiological, neurological and psychosocial. It is possible to make an accurate diagnosis after studying the patient's history. The course of treatment involves a combination of several methods at once: conservative, psychotherapeutic and other measures.
Disease etiology
The classification of depression according to the current edition of the Manual of Mental Disorders implies a division into the following groups:
- major depressive disorder;
- chronic depressive disorder;
- depressive disorder of specified or unspecified etiology: premenstrual disorders, depression due to health disorders, consequences of taking psychoactive drugs.
Most cases of depression have a clear age relationship: adolescence or age 20-30 years. Due to the peculiarities of the psyche, women are more prone to depressive manifestations, the exact causes of this phenomenon have not yet been established. These or other depressive symptoms occur in 30% of patients seeking medical help. Less than 10% of those who applied showed signs of deep depression, requiring competent medical intervention.
These or other depressive symptoms occur in 30% of patients seeking medical help. Less than 10% of those who applied showed signs of deep depression, requiring competent medical intervention.
The state of demoralization associated with unpleasant incidents in the patient's life is significantly different from clinical depression. There are a number of characteristic signs indicating temporary psycho-emotional difficulties that disappear within a few days without specific treatment:
- deterioration in mood is manifested by outbreaks and is not permanent, protracted;
- as events change, a person's mood improves, and the mental state returns to normal;
- low mood may alternate with fun and stable state of health;
- the patient does not have suicidal thoughts, feelings of self-loathing and feelings of worthlessness.
With the patient's tendency to depressive states during demoralization, individual signs of major depression may be observed. But even they do not allow talking about a disease that requires immediate help.
But even they do not allow talking about a disease that requires immediate help.
Causes of depression
Experts associate the manifestations of depression with environmental factors and genetic predisposition. However, they invariably point to the impossibility of accurately identifying the cause of the disease. Official medicine recognizes a hereditary trace in more than half of the diagnosed cases: in first-line relatives, identical twins. According to popular theories, the development of a depressive state can be affected by malfunctions of the hypothalamus, pituitary gland or adrenal glands, which produce hormones important for humans. Violations in the interaction of these organs can cause protracted depressive states.
A significant role in the appearance of signs of major or chronic depression is played by the psycho-emotional state, disturbed due to experienced problems: divorce, loss of a loved one, financial losses. In the absence of a predisposition to severe mental disorders, these events do not cause prolonged depressive states. If the patient has a tendency to anxiety, the risk of dangerous symptoms increases.
If the patient has a tendency to anxiety, the risk of dangerous symptoms increases.
Speaking about the female predisposition to depression, experts indicate as the reasons:
- exposure to daily stress due to high mental stress;
- high risk of thyroid dysfunction;
- hormonal changes associated with the menstrual cycle or menopause;
- an increase in the level of monoamine oxidase, an enzyme that contributes to the destruction of neurotransmitters that determine the patient's mood level.
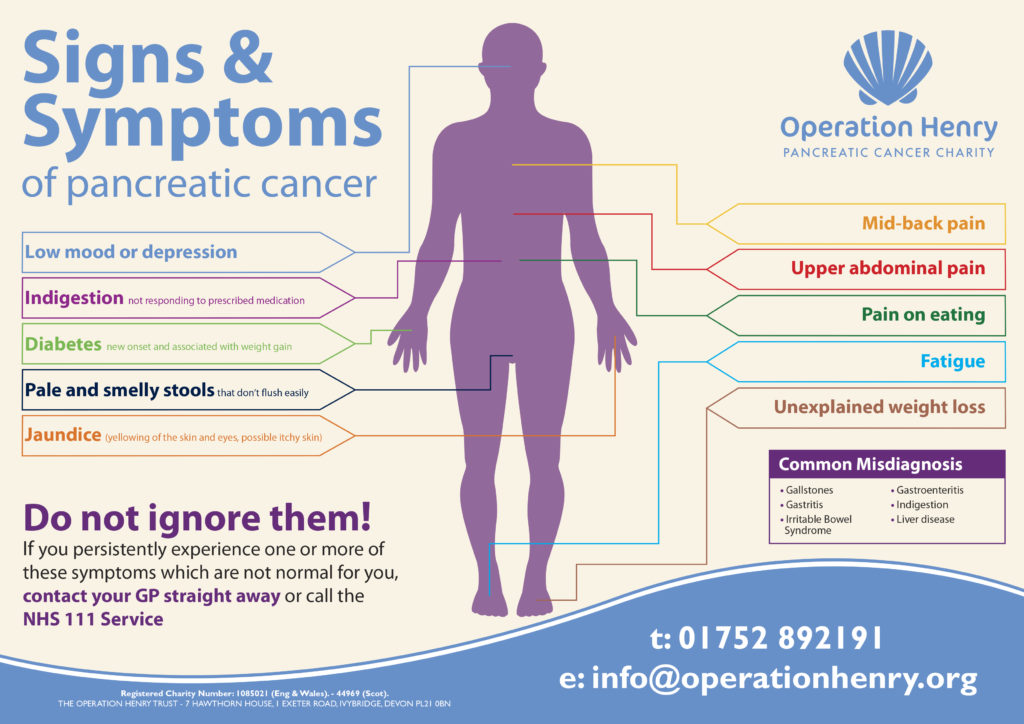
Against the background of clinical depression, the patient may show signs of somatic diseases: hormonal disorders, brain tumors, strokes, multiple sclerosis and Parkinson's disease.
Symptomatic picture of the disease
Signs of depression largely depend on the nature of the disease and help specialists make an accurate diagnosis.
- In a state of major depression, the patient has a tired and sad appearance, lack of eye contact, emotionlessness, depression and restrained speech.
 Violations of diet and personal hygiene are possible. Also among the characteristic symptoms of depression: decreased interest in favorite activities, insomnia, weight loss or rapid weight gain, indecision, inability to concentrate, obsessive thoughts of death or suicide, lethargy.
Violations of diet and personal hygiene are possible. Also among the characteristic symptoms of depression: decreased interest in favorite activities, insomnia, weight loss or rapid weight gain, indecision, inability to concentrate, obsessive thoughts of death or suicide, lethargy. - In chronic depressive disorder, symptoms persist for 2 years or more. The patient has anxiety, obvious personality disorders, increased criticality towards himself and others, isolation and low self-esteem. In addition, increased fatigue, inability to concentrate, a feeling of hopelessness, insomnia or excessive sleepiness, weakness and low mood indicate a chronic condition.
- Against the background of premenstrual depressive disorder in women, a week before the expected date of the start of the cycle, there are sharp mood swings, anger and irritability, a state of anxiety and tension. Interest in habitual activities decreases, concentration of attention falls, increased fatigue and a feeling of depression are noted.
 Up to 6% of women of childbearing age suffer from the listed symptoms of depression in women with PMS at various periods of life.
Up to 6% of women of childbearing age suffer from the listed symptoms of depression in women with PMS at various periods of life. - In depressive disorders with an unknown etiology, patients of both sexes have anxiety, characteristic manic syndromes (feeling of superiority, talkativeness or high spirits), a decrease in emotional reaction to pleasant events, states of delirium or hallucinations, psychomotor retardation.
The symptomatic picture of different types of depression has an individual color for each patient. However, all persons suffering from depression invariably have common features of a particular disease, which simplifies the diagnosis.
Complications of depression
The growth of the pathological situation against the background of the patient's refusal of professional assistance can cause the following dangerous phenomena:
- increase in symptoms of depression;
- increased incidence of depression;
- prolonged illness, the duration of which increases as the attacks become more frequent;
- cases of double depression, when severe psychological problems are superimposed on more “superficial” experiences and stages of depression develop that are difficult to treat;
- difficulties with the selection of appropriate therapy, when the disease is not amenable to classical methods of correction and requires the use of more "heavy" drugs with a high risk of side effects.

Depression diagnostics
The treatment of depression is the field of activity of the therapist, psychologist and psychiatrist, optimally - their collegial cooperation. Special questionnaires, complaints of patients and their relatives about characteristic changes in well-being and mood allow to recognize the signs of depression and make an accurate diagnosis. In personal communication with the patient, the doctor clarifies the duration of the course of the disease, and also delicately finds out the appearance of possible thoughts about harming himself or others. Also, concomitant pathological conditions are subject to mandatory study: a tendency to use alcohol and drugs, smoking, immoderate nutrition, etc.
Of great importance is the differential diagnosis of depression, which makes it possible to distinguish this disease from other similar mental pathologies: bipolar disorder, anxiety, demoralization, signs of dementia, or hormonal disorders associated with impaired thyroid function. At the same time, a number of clinical examinations are carried out: a complete blood count, measurement of thyroid hormone levels, electrolyte balance, blood levels of prohibited psychotropic substances.
At the same time, a number of clinical examinations are carried out: a complete blood count, measurement of thyroid hormone levels, electrolyte balance, blood levels of prohibited psychotropic substances.
Methods of treatment
Treatment for depression includes:
- drug treatment is developed taking into account the patient's condition, response to previous courses and the risk of side effects. Drugs of the antidepressant group suppress the action of certain hormones that contribute to the development of depressive states and restore hormonal balance in the body.
- maintenance treatment implies a regular visit to a specialist to monitor the results of treatment, adjust the chosen course, obtain the necessary clarifications, etc.
- additional methods of influence: psychotherapy, phototherapy, electroshock therapy, methods of deep brain stimulation, etc.
If all the recommendations of the specialist are followed and the course is completed in full, stable positive results can be achieved within a few weeks, while reducing the risk of recurrence of depressive conditions.
Frequently asked questions about depression
How to get rid of depression on your own?
Attempts to deal with depression on their own usually end in failure and the appearance of signs of a deeper disorder. Only an experienced doctor will be able to determine the type of disease and choose the best treatment tactics. Folk remedies, uncontrolled intake of antidepressants "on the advice of friends", withdrawal into oneself - only tighten the knot of the problem and can cause deeper mental disorders with a simultaneous deterioration in physical health.
Why is depression dangerous?
Voluntary refusal of a course of treatment with the intention to overcome the disease on their own can have the most serious consequences: the appearance of suicidal thoughts, deep mental disorders, more frequent seizures, degradation of the personality in professional and family terms, the appearance of addiction to alcohol and drugs.