Antipsychotic for anxiety
Role of atypical antipsychotics in the treatment of generalized anxiety disorder
Review
. 2014 Jun;28(6):519-33.
doi: 10.1007/s40263-014-0162-6.
Rachel Hershenberg 1 , Daniel F Gros, Olga Brawman-Mintzer
Affiliations
Affiliation
- 1 VISN 4 Mental Illness Research, Education and Clinical Center at Philadelphia VA Medical Center, 3900 Woodland Ave, Philadelphia, PA, 19104, USA, [email protected].
- PMID: 24794100
- DOI: 10.1007/s40263-014-0162-6
Review
Rachel Hershenberg et al. CNS Drugs. 2014 Jun.
. 2014 Jun;28(6):519-33.
doi: 10.1007/s40263-014-0162-6.
Authors
Rachel Hershenberg 1 , Daniel F Gros, Olga Brawman-Mintzer
Affiliation
- 1 VISN 4 Mental Illness Research, Education and Clinical Center at Philadelphia VA Medical Center, 3900 Woodland Ave, Philadelphia, PA, 19104, USA, [email protected].
- PMID: 24794100
- DOI: 10.1007/s40263-014-0162-6
Abstract
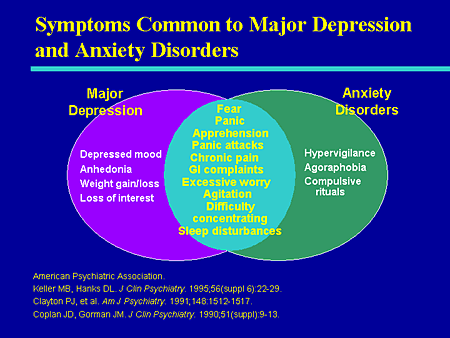
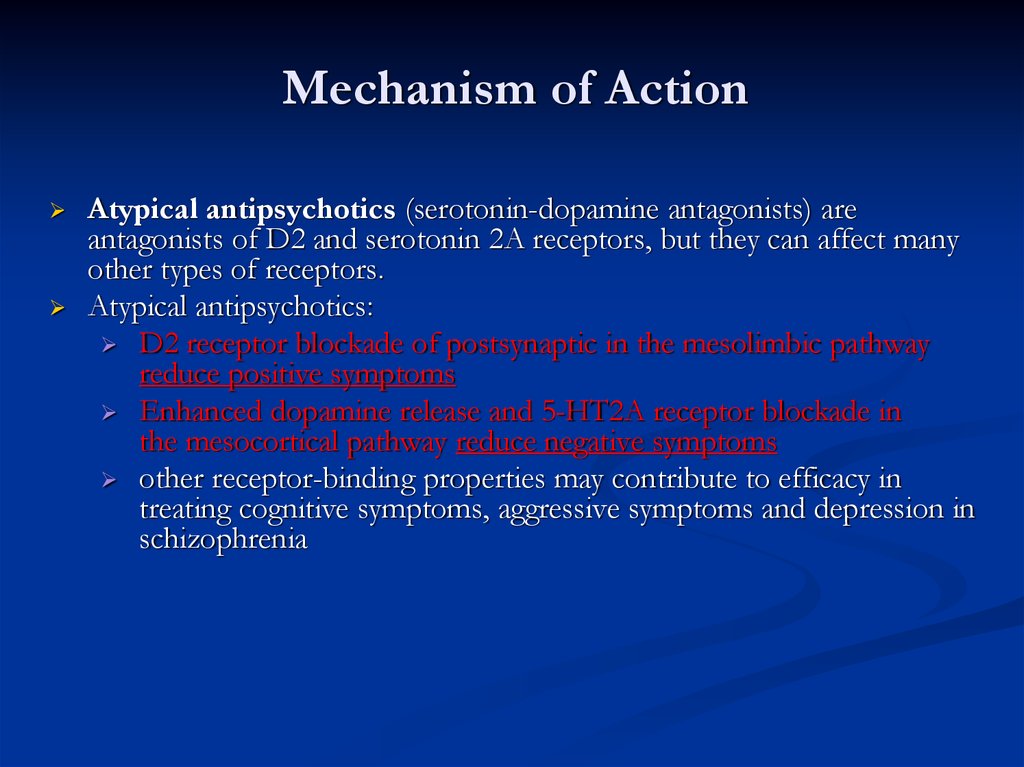
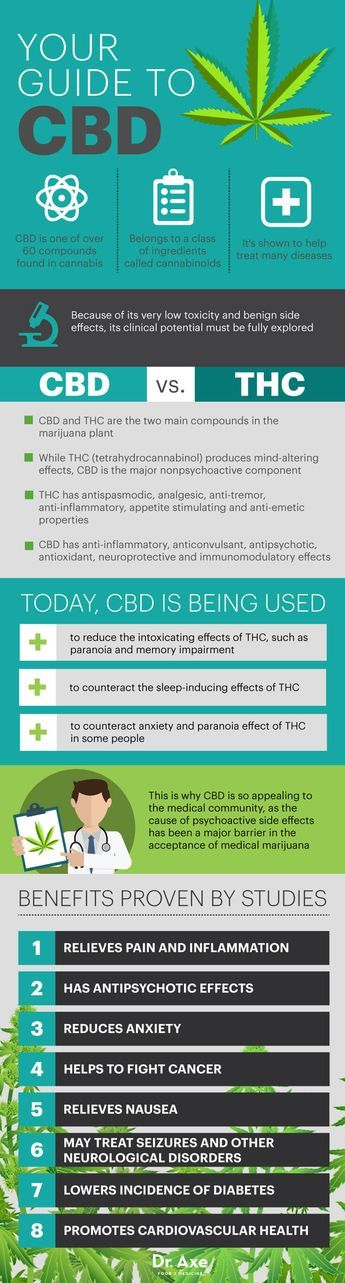
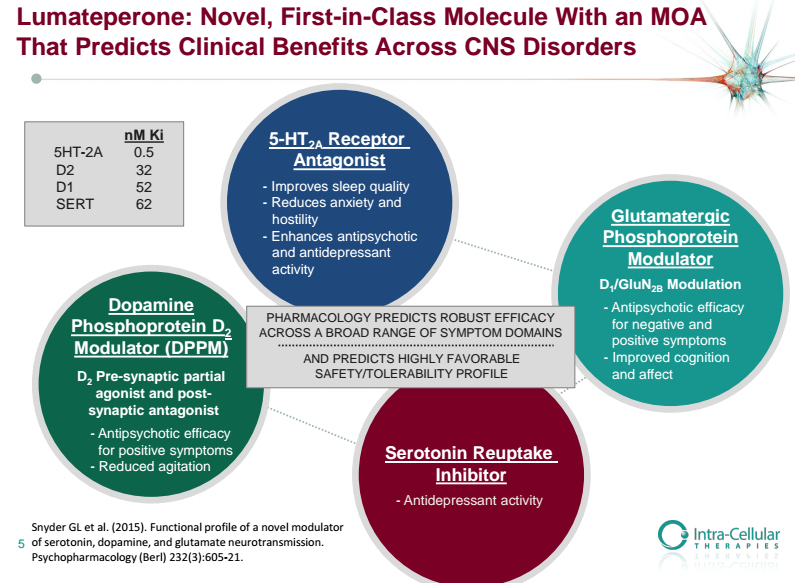
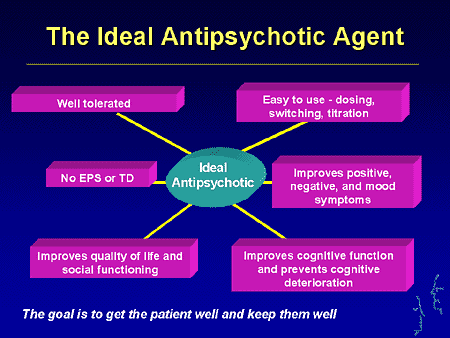
Evidence-based treatment approaches for generalized anxiety disorder (GAD) comprise psychotherapy, pharmacotherapy, or a combination of the two.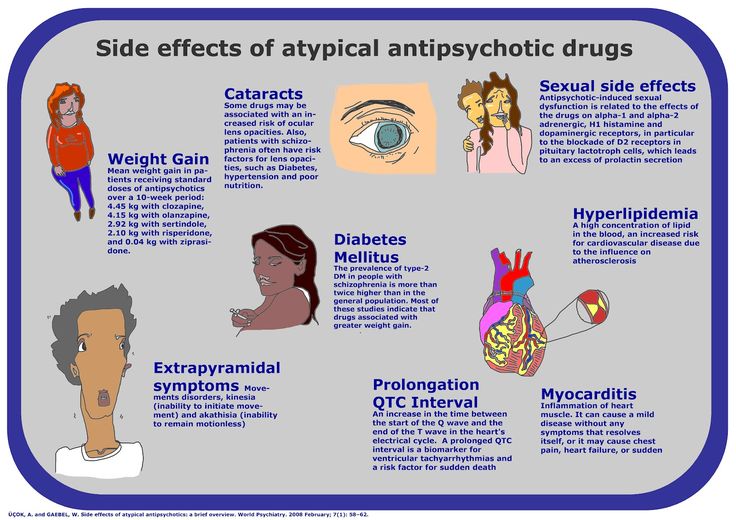 First-line pharmacotherapy agents include selective serotonin reuptake inhibitors, selective serotonin-norepinephrine reuptake inhibitors, and, in certain European guidelines, pregabalin, which gained European Commission approval. Although short- and long-term efficacy have been established for these agents in controlled trials, response rates of 60-70 % are insufficient, remission rates are relatively modest, and relapse rates considerable. Moreover, questions increasingly arise regarding tolerability and side-effect profiles. As an alternative, antipsychotics have long been of interest for the treatment of anxiety disorders, but investigation had been tempered by their potential for irreversible side effects. With the improved side-effect profiles of atypical antipsychotics, these agents are increasingly being investigated across Axis I disorders. Atypical antipsychotics such as quetiapine, aripiprazole, olanzapine, and risperidone have been shown to be helpful in addressing a range of anxiety and depressive symptoms in individuals with schizophrenia and schizoaffective disorders, and have since been used in the treatment of a range of mood and anxiety disorders.
First-line pharmacotherapy agents include selective serotonin reuptake inhibitors, selective serotonin-norepinephrine reuptake inhibitors, and, in certain European guidelines, pregabalin, which gained European Commission approval. Although short- and long-term efficacy have been established for these agents in controlled trials, response rates of 60-70 % are insufficient, remission rates are relatively modest, and relapse rates considerable. Moreover, questions increasingly arise regarding tolerability and side-effect profiles. As an alternative, antipsychotics have long been of interest for the treatment of anxiety disorders, but investigation had been tempered by their potential for irreversible side effects. With the improved side-effect profiles of atypical antipsychotics, these agents are increasingly being investigated across Axis I disorders. Atypical antipsychotics such as quetiapine, aripiprazole, olanzapine, and risperidone have been shown to be helpful in addressing a range of anxiety and depressive symptoms in individuals with schizophrenia and schizoaffective disorders, and have since been used in the treatment of a range of mood and anxiety disorders.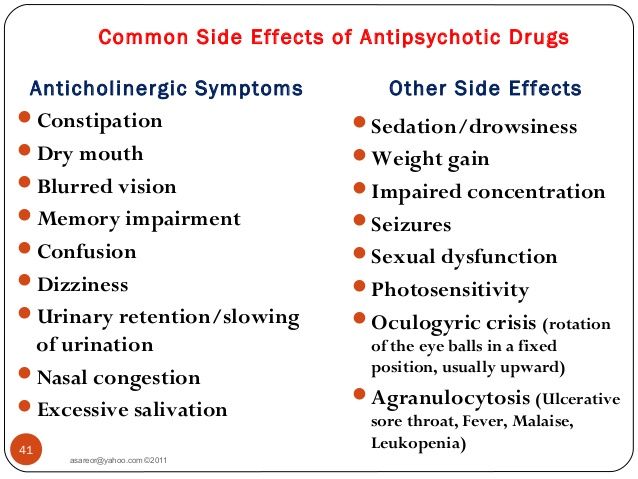 In this article, we review the efficacy and tolerability of atypical antipsychotics as adjunctive therapy and/or monotherapy for individuals with GAD, a currently off-label indication. The most evidence has accumulated for quetiapine. Findings suggest that approximately 50 % of participants tolerate the side effects, most commonly sedation and fatigue. Among this subset, those who continue treatment demonstrate significant reductions in anxiety when used as adjunctive therapy or monotherapy. The appropriateness of the use of antipsychotics in the treatment of GAD is discussed.
In this article, we review the efficacy and tolerability of atypical antipsychotics as adjunctive therapy and/or monotherapy for individuals with GAD, a currently off-label indication. The most evidence has accumulated for quetiapine. Findings suggest that approximately 50 % of participants tolerate the side effects, most commonly sedation and fatigue. Among this subset, those who continue treatment demonstrate significant reductions in anxiety when used as adjunctive therapy or monotherapy. The appropriateness of the use of antipsychotics in the treatment of GAD is discussed.
Similar articles
-
Adjunctive use of atypical antipsychotics for treatment-resistant generalized anxiety disorder.
Lorenz RA, Jackson CW, Saitz M. Lorenz RA, et al. Pharmacotherapy. 2010 Sep;30(9):942-51. doi: 10.1592/phco.30.9.942. Pharmacotherapy. 2010. PMID: 20795849 Review.
-
Comparison of longer-term safety and effectiveness of 4 atypical antipsychotics in patients over age 40: a trial using equipoise-stratified randomization.
Jin H, Shih PA, Golshan S, Mudaliar S, Henry R, Glorioso DK, Arndt S, Kraemer HC, Jeste DV. Jin H, et al. J Clin Psychiatry. 2013 Jan;74(1):10-8. doi: 10.4088/JCP.12m08001. Epub 2012 Nov 27. J Clin Psychiatry. 2013. PMID: 23218100 Free PMC article. Clinical Trial.
-
Second-generation antipsychotics for anxiety disorders.
Depping AM, Komossa K, Kissling W, Leucht S. Depping AM, et al. Cochrane Database Syst Rev. 2010 Dec 8;(12):CD008120. doi: 10.1002/14651858.CD008120.pub2. Cochrane Database Syst Rev. 2010. PMID: 21154392 Review.
-
A randomized trial examining the effectiveness of switching from olanzapine, quetiapine, or risperidone to aripiprazole to reduce metabolic risk: comparison of antipsychotics for metabolic problems (CAMP).
Stroup TS, McEvoy JP, Ring KD, Hamer RH, LaVange LM, Swartz MS, Rosenheck RA, Perkins DO, Nussbaum AM, Lieberman JA; Schizophrenia Trials Network. Stroup TS, et al. Am J Psychiatry. 2011 Sep;168(9):947-56. doi: 10.1176/appi.ajp.2011.10111609. Epub 2011 Jul 18. Am J Psychiatry. 2011. PMID: 21768610 Free PMC article. Clinical Trial.
-
Olanzapine versus other atypical antipsychotics for schizophrenia.
Komossa K, Rummel-Kluge C, Hunger H, Schmid F, Schwarz S, Duggan L, Kissling W, Leucht S. Komossa K, et al. Cochrane Database Syst Rev. 2010 Mar 17;(3):CD006654. doi: 10.1002/14651858.CD006654.pub2. Cochrane Database Syst Rev. 2010. PMID: 20238348 Free PMC article. Review.
See all similar articles
Cited by
-
Antipsychotic Drug-Induced Increases in Peripheral Catecholamines are Associated With Glucose Intolerance.

Boyda HN, Pham M, Huang J, Ho AA, Procyshyn RM, Yuen JWY, Honer WG, Barr AM. Boyda HN, et al. Front Pharmacol. 2022 Feb 15;13:765905. doi: 10.3389/fphar.2022.765905. eCollection 2022. Front Pharmacol. 2022. PMID: 35242029 Free PMC article.
-
Social isolation induces neuroinflammation and microglia overactivation, while dihydromyricetin prevents and improves them.
Al Omran AJ, Shao AS, Watanabe S, Zhang Z, Zhang J, Xue C, Watanabe J, Davies DL, Shao XM, Liang J. Al Omran AJ, et al. J Neuroinflammation. 2022 Jan 4;19(1):2. doi: 10.1186/s12974-021-02368-9. J Neuroinflammation. 2022. PMID: 34983568 Free PMC article.
-
Social Isolation Induces Neuroinflammation And Microglia Overactivation, While Dihydromyricetin Prevents And Improves Them.
Al Omran AJ, Shao AS, Watanabe S, Zhang Z, Zhang J, Xue C, Watanabe J, Davies DL, Shao XM, Liang J. Al Omran AJ, et al. Res Sq. 2021 Oct 1:rs.3.rs-923871. doi: 10.21203/rs.3.rs-923871/v1. Preprint. Res Sq. 2021. PMID: 34611661 Free PMC article. Updated.
-
Synthesis and In Vitro Evaluation of Novel Dopamine Receptor D2 3,4-dihydroquinolin-2(1H)-one Derivatives Related to Aripiprazole.
Juza R, Stefkova K, Dehaen W, Randakova A, Petrasek T, Vojtechova I, Kobrlova T, Pulkrabkova L, Muckova L, Mecava M, Prchal L, Mezeiova E, Musilek K, Soukup O, Korabecny J. Juza R, et al. Biomolecules. 2021 Aug 24;11(9):1262. doi: 10.3390/biom11091262. Biomolecules. 2021. PMID: 34572475 Free PMC article.
-
A Focused Review of the Metabolic Side-Effects of Clozapine.

Yuen JWY, Kim DD, Procyshyn RM, Panenka WJ, Honer WG, Barr AM. Yuen JWY, et al. Front Endocrinol (Lausanne). 2021 Feb 25;12:609240. doi: 10.3389/fendo.2021.609240. eCollection 2021. Front Endocrinol (Lausanne). 2021. PMID: 33716966 Free PMC article. Review.
See all "Cited by" articles
References
-
- CNS Drugs. 2013 May;27 Suppl 1:S29-37 - PubMed
-
- CNS Spectr. 2008 Jun;13(6):522-7 - PubMed
-
- Int Clin Psychopharmacol.
 2000 Nov;15(6):319-28 - PubMed
2000 Nov;15(6):319-28 - PubMed
- Int Clin Psychopharmacol.
-
- BMJ. 2011 Mar 11;342:d1199 - PubMed
-
- J Clin Psychopharmacol. 2005 Aug;25(4):301-10 - PubMed
Publication types
MeSH terms
Substances
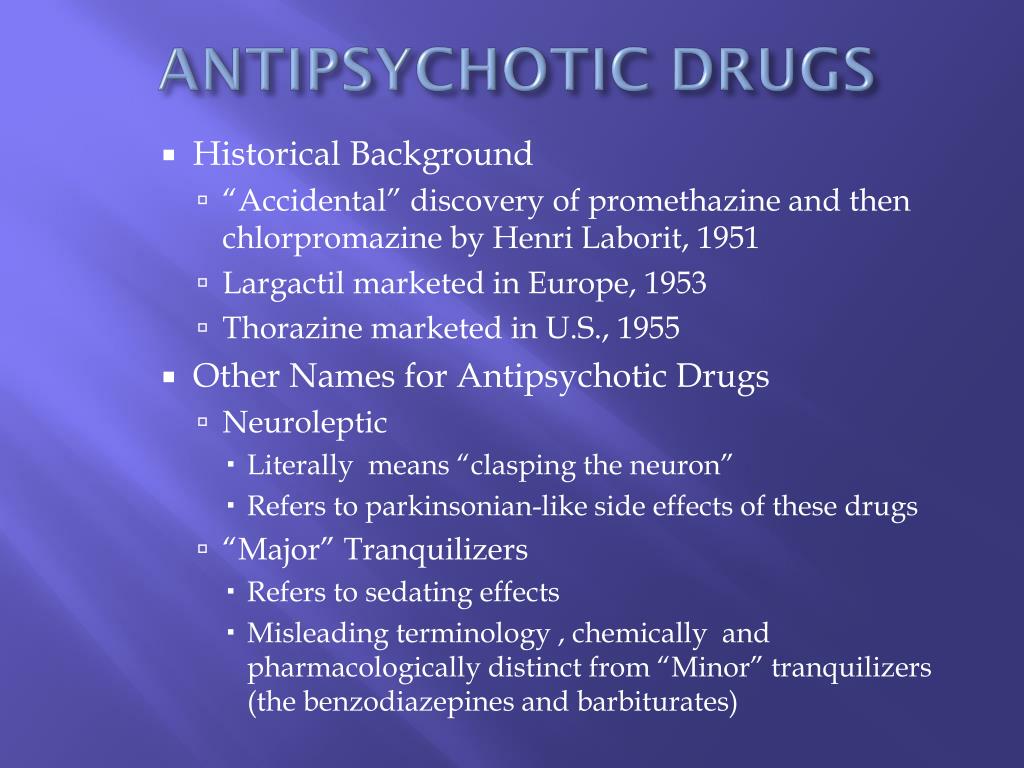
Antipsychotic Medication | CAMH
Overview
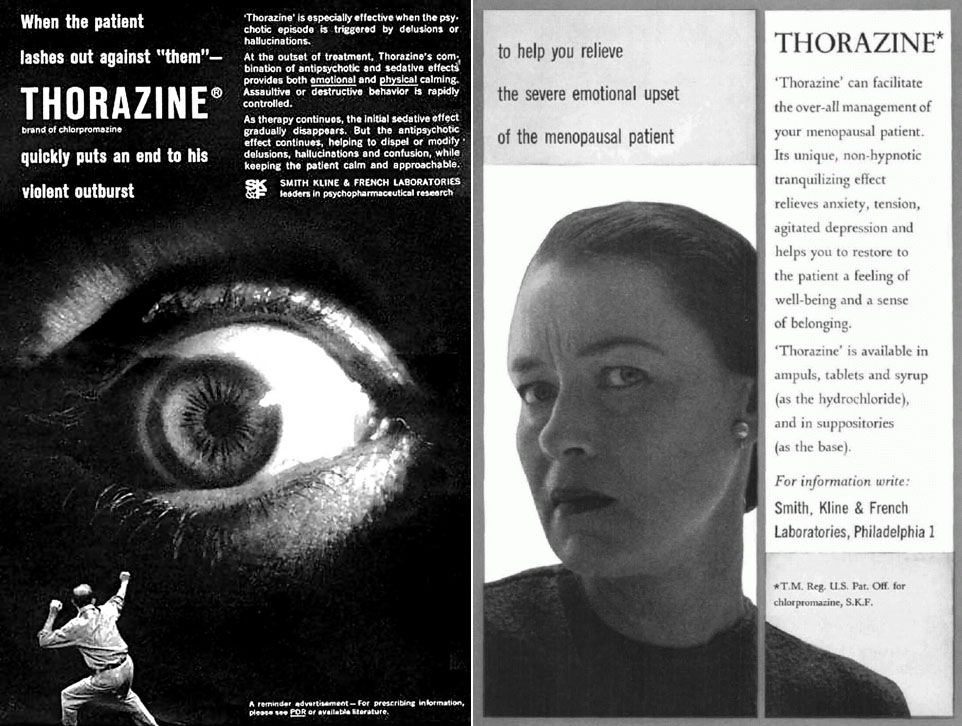
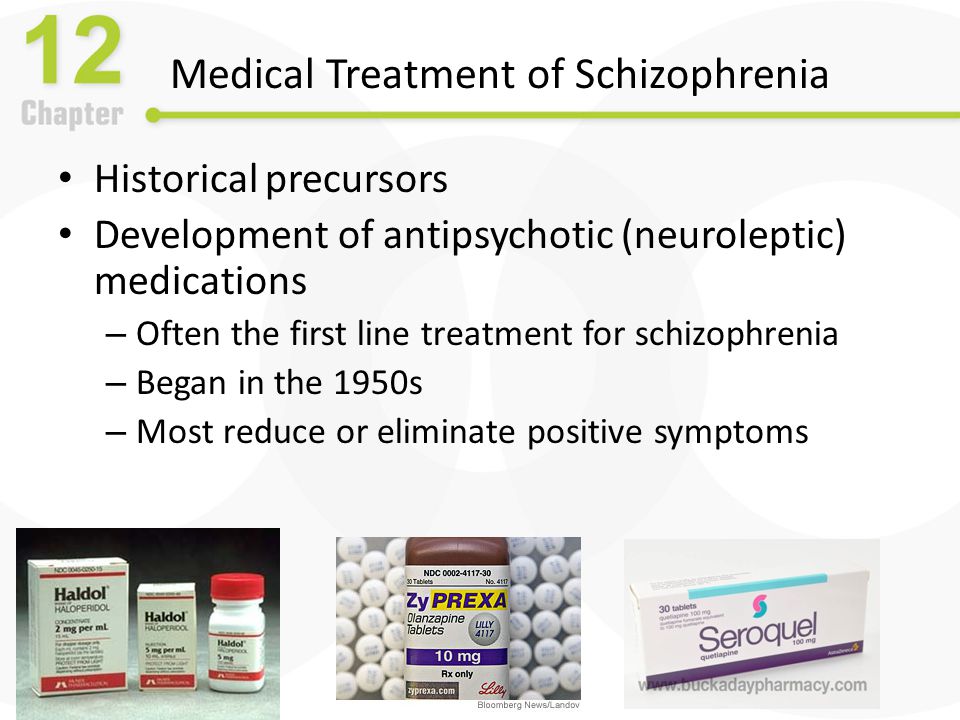
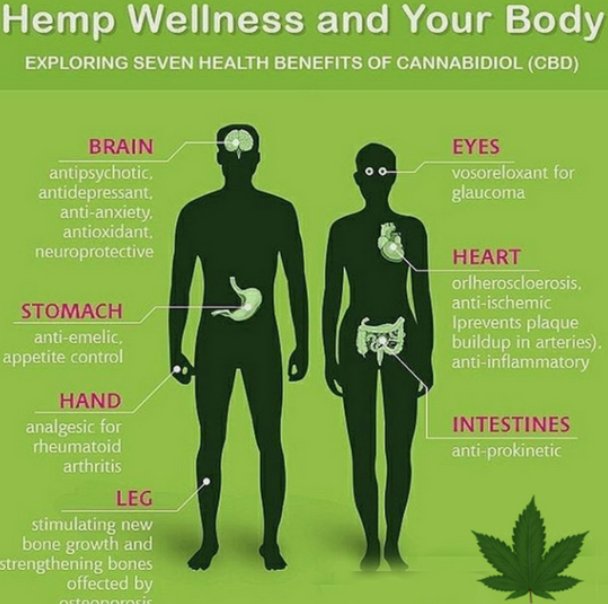
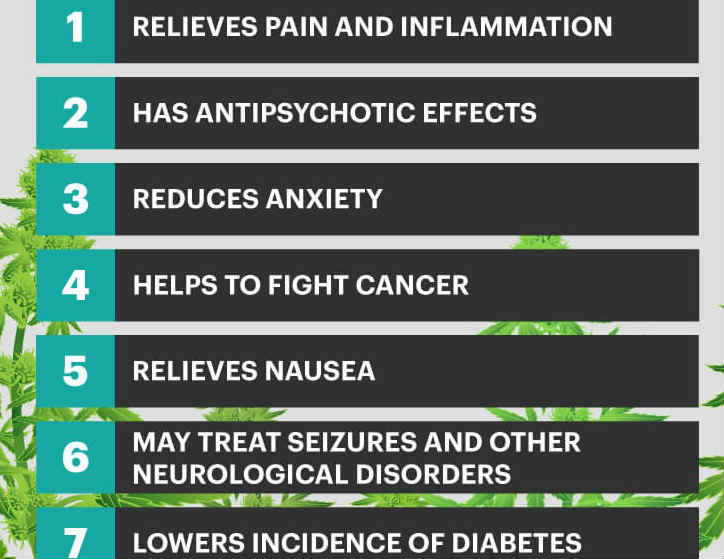
Antipsychotic medications can reduce or relieve symptoms of psychosis, such as delusions (false beliefs) and hallucinations (seeing or hearing something that is not there). Formerly known as major tranquilizers and neuroleptics, antipsychotic medications are the main class of drugs used to treat people with schizophrenia. They are also used to treat people with psychosis that occurs in bipolar disorder, depression and Alzheimer’s disease. Other uses of antipsychotics include stabilizing moods in bipolar disorder, reducing anxiety in anxiety disorders and reducing tics in Tourette syndrome.
Formerly known as major tranquilizers and neuroleptics, antipsychotic medications are the main class of drugs used to treat people with schizophrenia. They are also used to treat people with psychosis that occurs in bipolar disorder, depression and Alzheimer’s disease. Other uses of antipsychotics include stabilizing moods in bipolar disorder, reducing anxiety in anxiety disorders and reducing tics in Tourette syndrome.
Antipsychotic medications can help to calm and clear confusion in a person with acute psychosis within hours or days, but they can take up to four or six weeks to reach their full effect. These medications can help to control symptoms, but they do not cure the underlying condition. When taken over a longer term, antipsychotics can help to prevent further episodes of psychosis.
While antipsychotic medications can help some people with psychosis and mood disorders, these drugs can have serious side-effects. The aim of medication treatment is to reduce and control symptoms while keeping side-effects at a minimum.
Combining antipsychotic medication with other therapy and support can help people to manage symptoms and improve quality of life. Family therapy, peer support, school and job counselling, and housing and employment supports can all be helpful. Some therapists now offer cognitive-behavioural therapy to help people cope with voices and other auditory hallucinations.
Taking care of your physical health is especially important if you take antipsychotic medication. Both schizophrenia and the medications used to treat it can increase the risk of diabetes and other serious health problems. Getting regular checkups and medical care can help you to have good physical health. Eating a nutritious diet, exercising regularly and getting enough sleep can also help you to get and stay well.
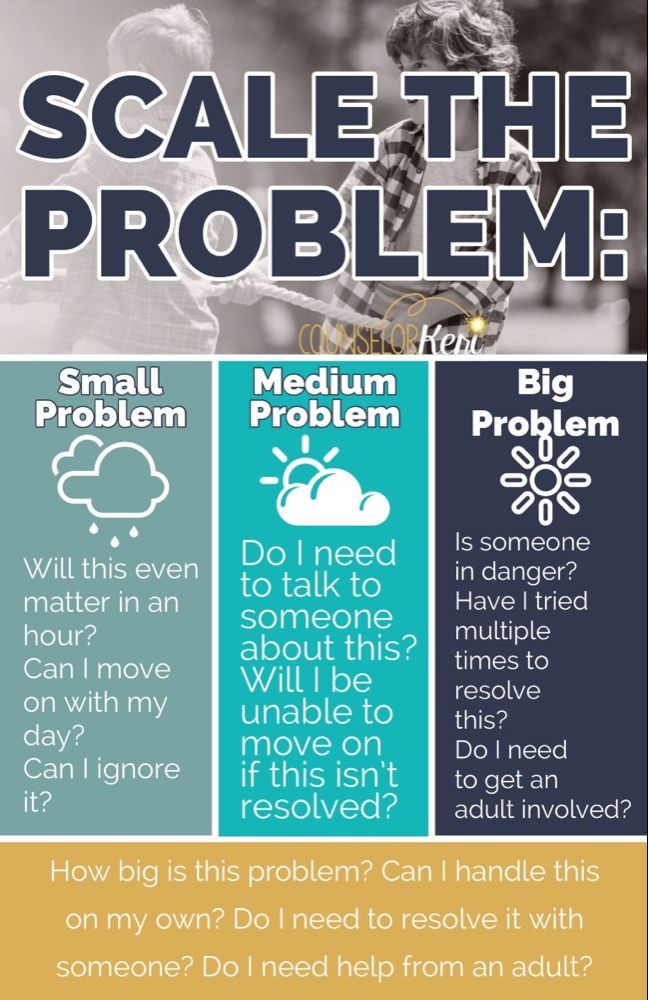
Do I need this treatment?
Psychosis; can be dangerous, frightening, isolating and disabling. Symptoms of psychosis, such as delusions and hallucinations, may come on gradually and build up over time, or they may come on rapidly. People experiencing psychosis may not be aware that the experiences they are having are not normal. To them, what is happening in their minds is very real.
People experiencing psychosis may not be aware that the experiences they are having are not normal. To them, what is happening in their minds is very real.
Recognizing and treating psychosis in the early stages greatly improves a person’s ability to recover and to lead a satisfying and rewarding life. Family, friends, colleagues and health providers play an important role in recognizing the signs of psychosis and in encouraging the person to get treatment. However, the symptoms of psychosis can sometimes lead to a breakdown in the person’s relationships with the people who might be most able to help him or her get treatment. Family members and others who support a person with psychosis may wish to seek support themselves, for example, from a family support group.
People with anxiety and mood disorders may benefit from taking antipsychotics in addition to antidepressants or mood stabilizers. When used in this way, antipsychotics may help to control symptoms such as irritable or depressed mood, disorganized thinking, and trouble concentrating and remembering.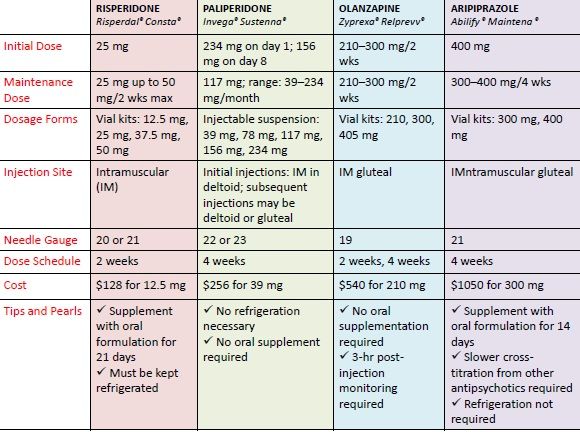
What does Antipsychotic Medications do?
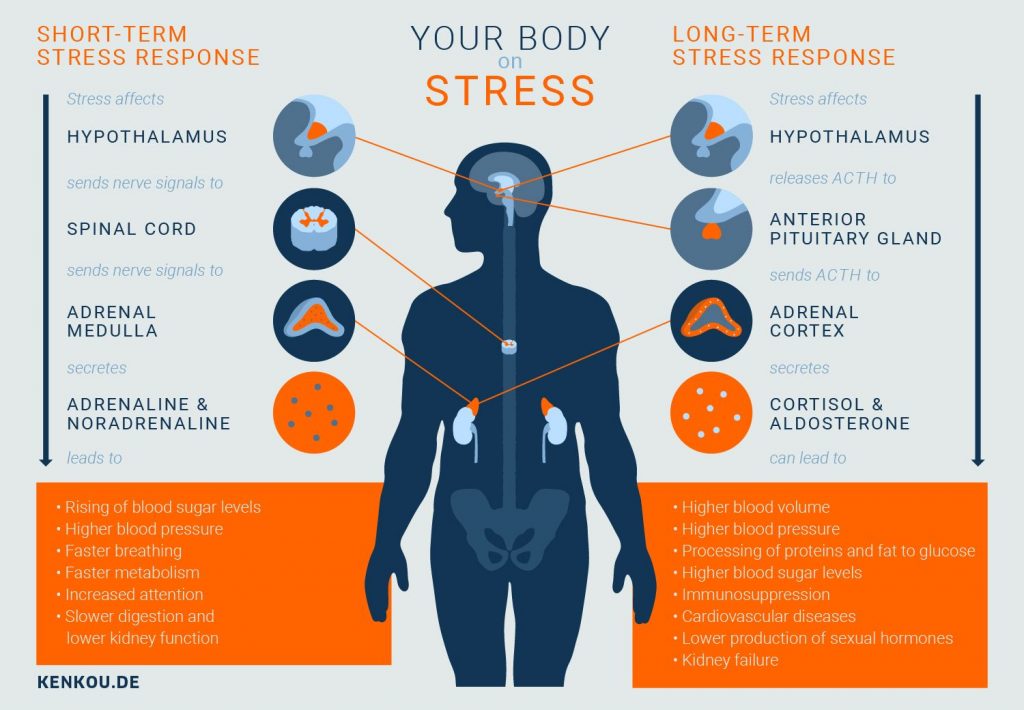
Psychosis is believed to be caused, at least in part, by overactivity of a brain chemical called dopamine, and antipsychotics are thought to work by blocking this dopamine effect. This blocking helps to make the symptoms of psychosis—such as voices and delusions—less commanding and preoccupying, but it does not always make them go away completely. People may still hear voices and have delusions, but they are more able to recognize what isn’t real and to focus on other things, such as work, school or family.
Side effects of Antipsychotic Medications
Antipsychotic medication can cause unpleasant side-effects, especially when the symptoms are severe and a higher dose of medication is used. Side-effects should become mild or at least tolerable when the dose is reduced and as your body adjusts to the presence of the drug.
Most side-effects will go away when you stop taking the drug. There is a risk, however, of a condition that causes people to make involuntary movements, known as tardive dyskinesia, which can be permanent.
There is a risk, however, of a condition that causes people to make involuntary movements, known as tardive dyskinesia, which can be permanent.
Some people accept the side-effects as a trade-off for the relief these drugs can bring. Others find the side-effects distressing and may choose not to take the medication.
Check the information given to you by your doctor or pharmacist to find out the specific side-effects of any drug you have been prescribed. If you are troubled by any of these effects, it is best to continue to take your medication as prescribed and let your doctor know as soon as possible. Your doctor may:
- adjust your dose
- prescribe other medications to help control side-effects
- change your medication.
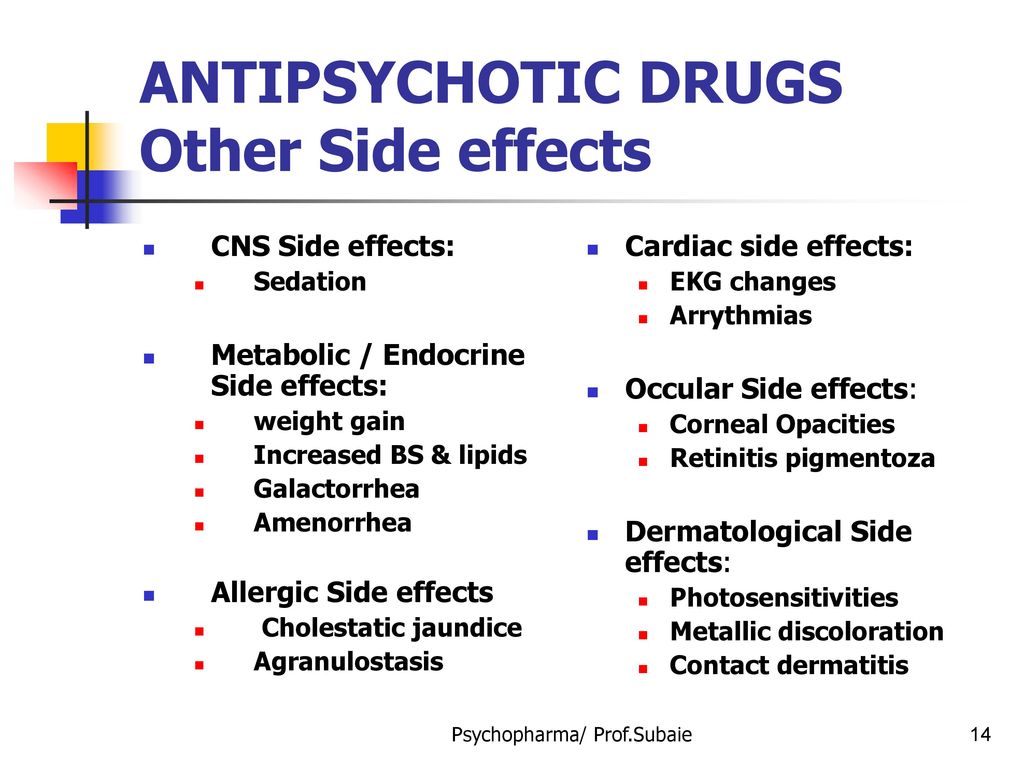
Side-effects of antipsychotics
- Movement effects: Tremors, muscle stiffness and tics can occur. The higher the dose, the more severe these effects.
 The risk of these effects may be lower with the second generation medications than with the older drugs. Other drugs (e.g., benztropine [Cogentin]) can be used to control the movement effects.
The risk of these effects may be lower with the second generation medications than with the older drugs. Other drugs (e.g., benztropine [Cogentin]) can be used to control the movement effects. - Dizziness: Feelings of dizziness may occur, especially when getting up from a sitting or lying position.
- Weight gain: Some of the second generation drugs are thought to affect people’s sense of having had enough to eat. They can also be sedating. These two effects can result in weight gain, which can increase a person’s risk of diabetes and heart disease.
- Diabetes: Schizophrenia is a risk factor for diabetes. Antipsychotic drugs can increase this risk.
- Agitation and sedation: Some people feel “wired” and unable to stop moving when taking antipsychotics. This effect may be mistaken for a worsening of illness rather than a side-effect of the medication.
 These same drugs can also have the opposite effect, making people feel tired. Some people may feel either wired or tired, and some may feel both at the same time.
These same drugs can also have the opposite effect, making people feel tired. Some people may feel either wired or tired, and some may feel both at the same time. - Tardive dyskinesia: For every year that a person takes antipsychotic medication, there is a five per cent chance of developing tardive dyskinesia (TD), a condition that causes people to have repetitive involuntary movements. The risk of TD is highest with the first generation antipsychotics, although it can occur with the second generation drugs. TD can worsen when you stop taking medication and can be permanent .
- Neuroleptic malignant syndrome: This rare but serious complication is usually associated with the use of high doses of typical antipsychotics early in treatment. Signs include fever, muscle stiffness and delirium.
Side-effects vary depending on the type of medication. More information on side-effects is included with each type of antipsychotic.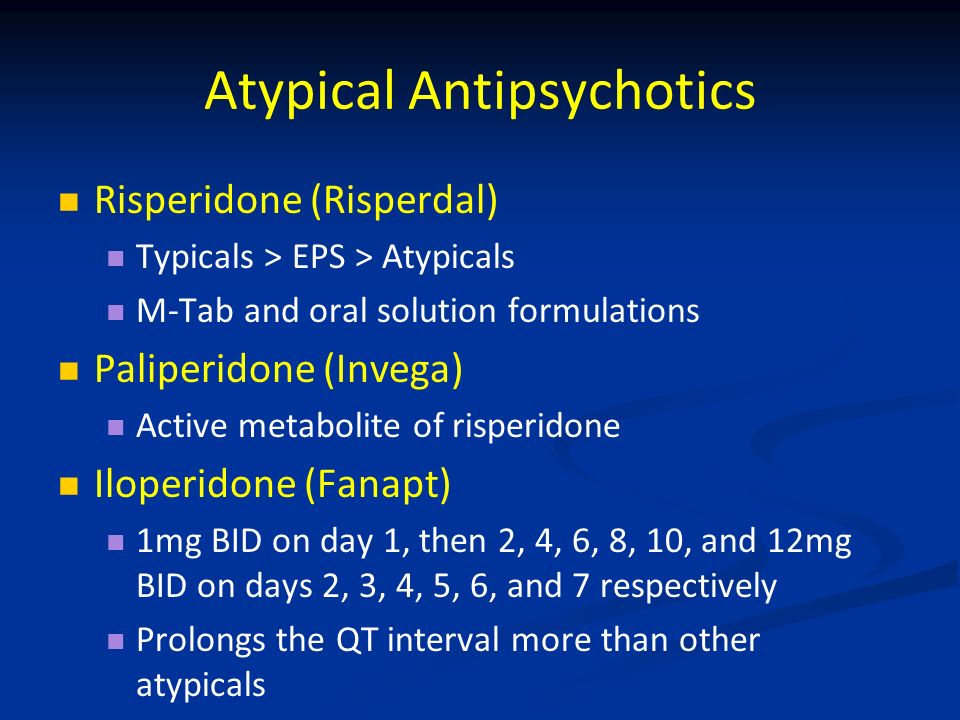
Controlling the side-effects of antipsychotics
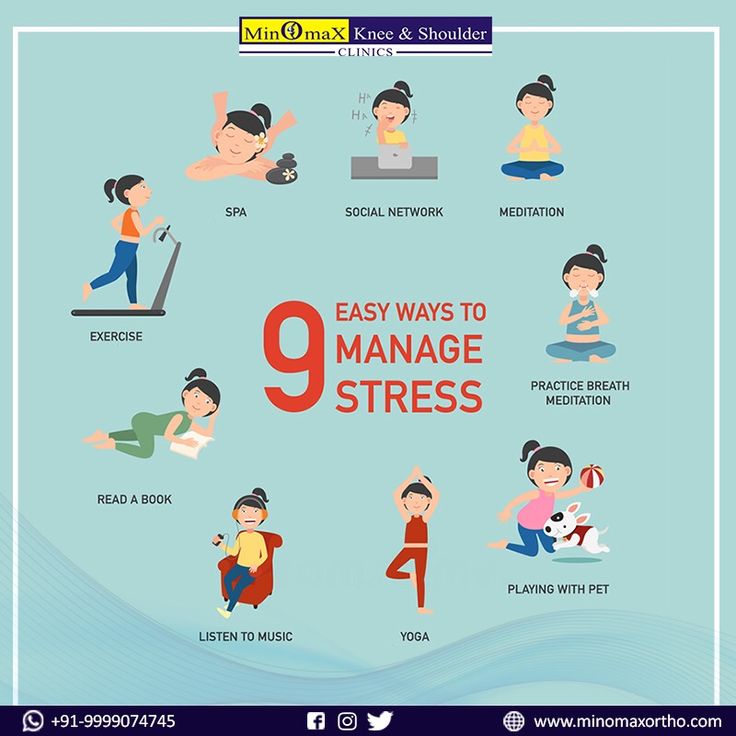
You can help to control possible side-effects on your own by:
- getting regular exercise and eating a low-fat, low-sugar, high-fibre diet (e.g., bran, fruits and vegetables) to reduce the risk of diabetes and help prevent weight gain and constipation
- using sugarless candy or gum, drinking water, and brushing your teeth regularly to increase salivation and ease dry mouth
- getting up slowly from a sitting or lying position to help prevent dizziness.
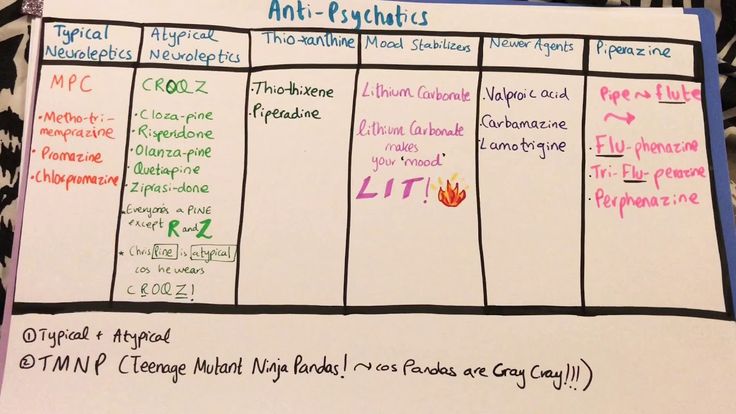
Types of Antipsychotic Medications
NOTE: medications are referred to in two ways: by their generic name and by their brand or trade names. Brand names available in Canada appear in brackets.
Antipsychotic medications are generally divided into two categories:
- atypical (second generation) antipsychotics
- typical (first generation) antipsychotics
The main difference between the two types of antipsychotics is that the first generation drugs block dopamine and the second generation drugs block dopamine and also affect serotonin levels.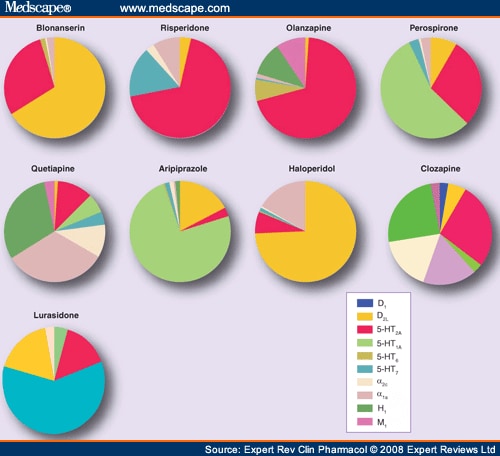 Evidence suggests that some of the second generation drugs have milder movement-related side-effects than the first generation drugs.
Evidence suggests that some of the second generation drugs have milder movement-related side-effects than the first generation drugs.
Both categories of drugs work equally well overall, although no drug or type of drug works equally well for everyone who takes it. When the same drug is given to a group of people, one-third of that group will find that it works well; another third will find that the drug helps only with some symptoms; and the final third will find that it does not help at all. For this reason, people may need to try different antipsychotics before finding the one that works best for them.
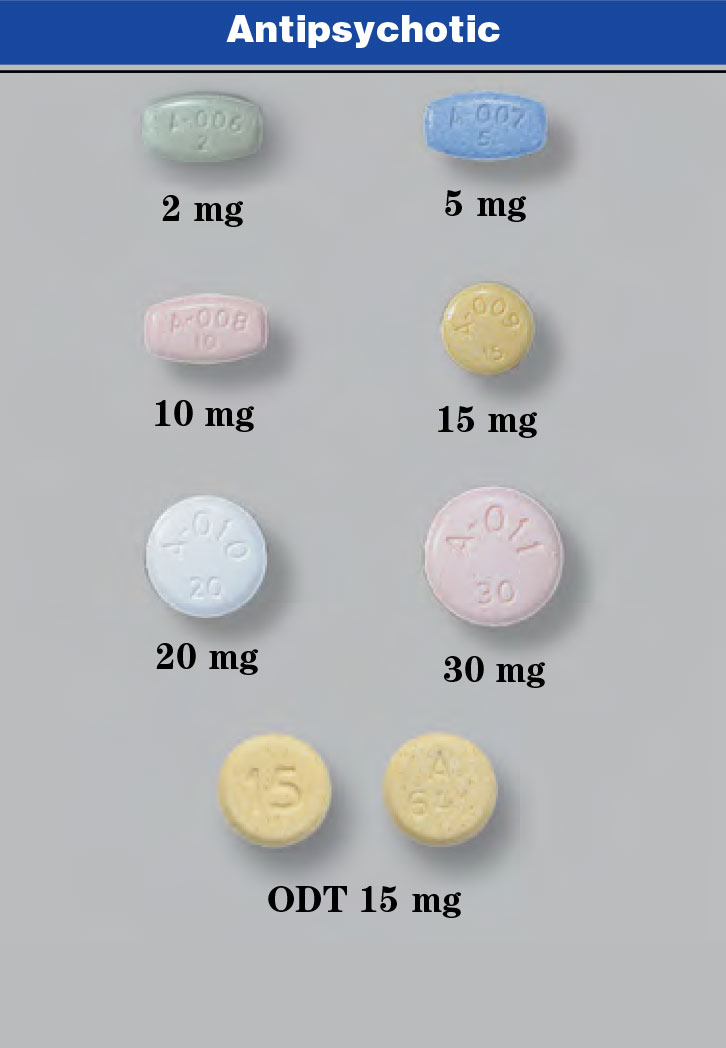
Most of these drugs are given in tablet form, some are liquids and others are given as injections. Some are available as long-lasting (depot) injections, which may be given anywhere from once a week to once a month.
Most people who take antipsychotics over a longer term are now prescribed the second generation (also called atypical) drugs.
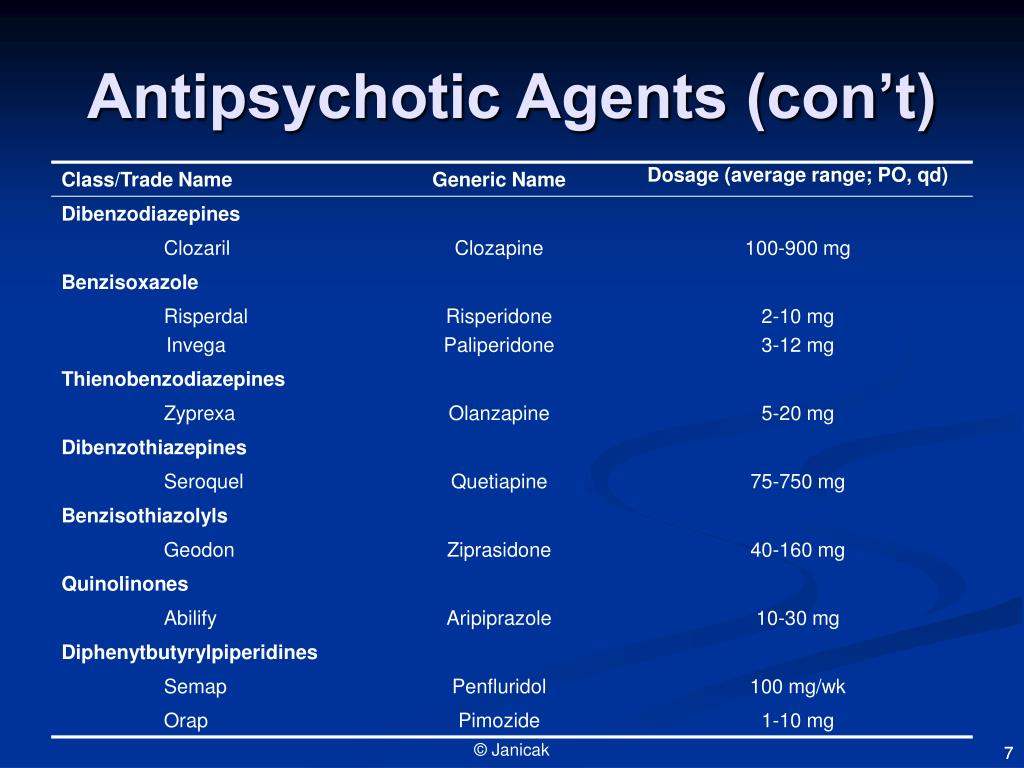
Atypical antipsychotics
The second generation antipsychotics are usually the first choice for the treatment of schizophrenia. Although they may not be officially approved for these other uses, they are sometimes used in the treatment of mood and anxiety disorders, such as bipolar, posttraumatic stress and obsessive-compulsive disorders.
Although they may not be officially approved for these other uses, they are sometimes used in the treatment of mood and anxiety disorders, such as bipolar, posttraumatic stress and obsessive-compulsive disorders.
Medications available in this class include risperidone (Risperdal), quetiapine (Seroquel), olanzapine (Zyprexa), ziprasidone (Zeldox), paliperidone (Invega), aripiprazole (Abilify) and clozapine (Clozaril).
Clozapine is exceptional in that it often works even when other medications have failed; however, because it requires monitoring of white blood cell counts, it is not the first choice for treatment.
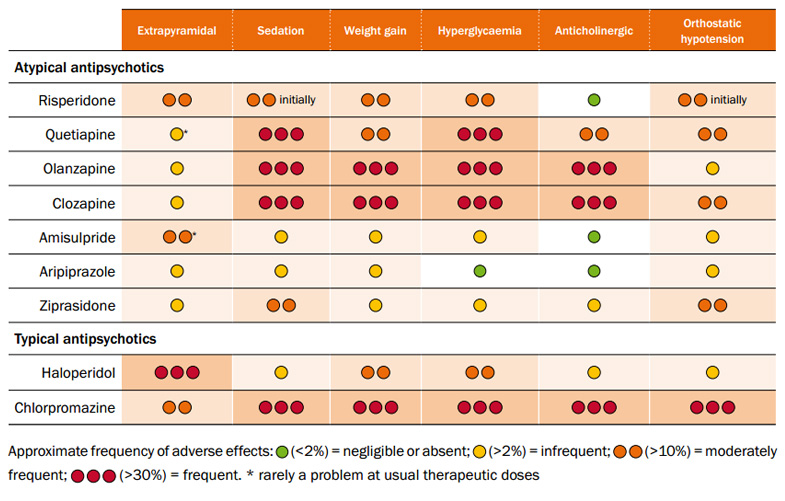
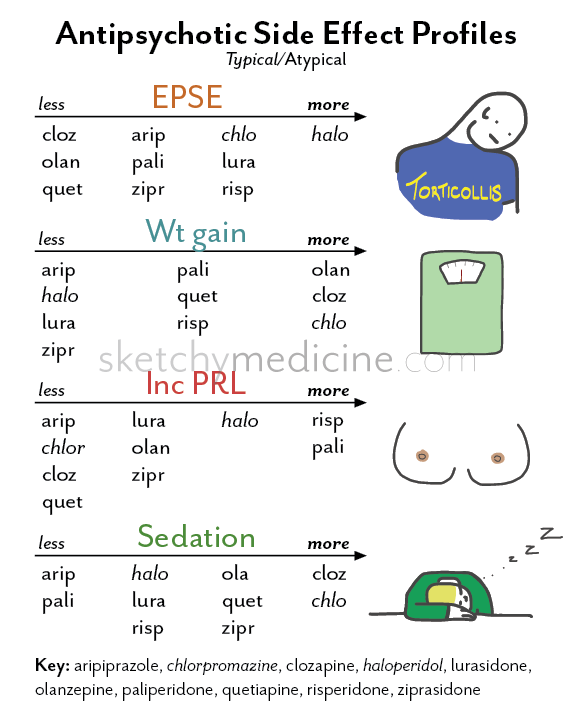
Possible side-effects of atypical antipsychotics include:
- Dry mouth
- dizziness
- blurred vision
- seizures (rarely)
The following list details other side-effects of atypical antipsychotics and which drugs are most likely to least likely to have these effects.
Weight gain, diabetes: clozapine > olanzapine > quetiapine > risperidone > ziprasidone, aripiprazole
Movement effects (e.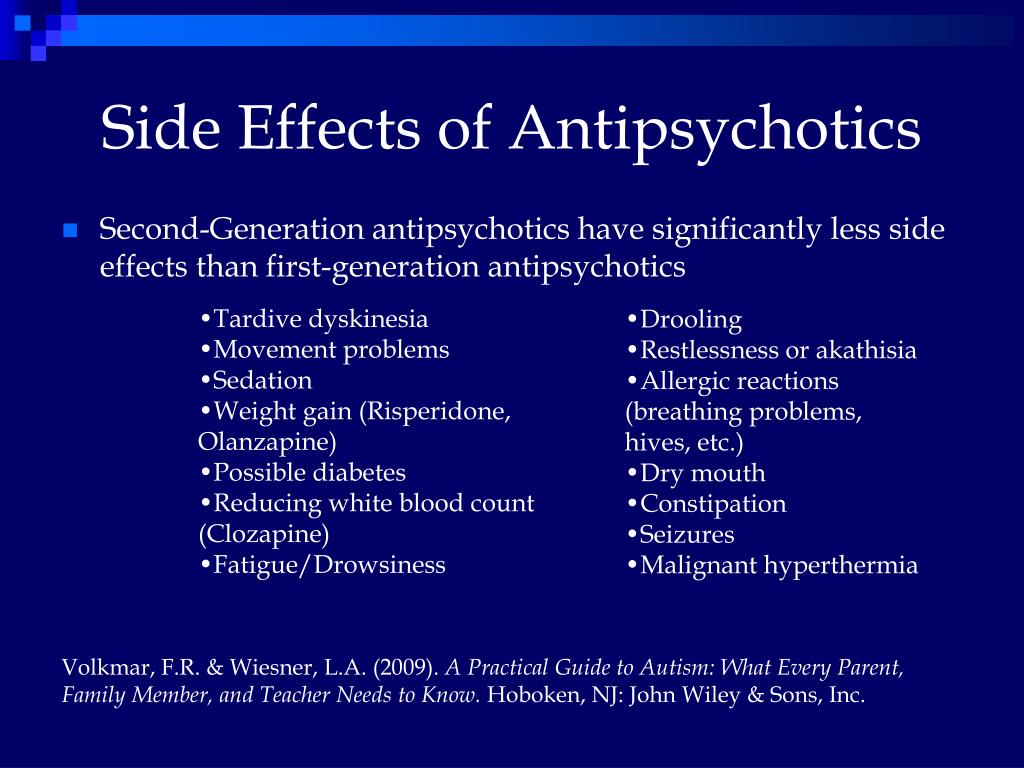 g., tremor, stiffness, agitation): risperidone > olanzapine, quetiapine, ziprasidone, aripiprazole > clozapine
g., tremor, stiffness, agitation): risperidone > olanzapine, quetiapine, ziprasidone, aripiprazole > clozapine
Sedation (e.g., sleepiness, low energy): clozapine, olanzapine and quetiapine > risperidone, ziprasidone, aripiprazole
Decreased sex drive and function, missed periods, discharge from breast: risperidone > olanzapine, quetiapine > clozapine, ziprasidone
Typical (first generation) antipsychotics
These older medications include chlorpromazine (once marketed as Largactil), flupenthixol (Fluanxol), afluphenazine (Modecate), haloperidol (Haldol), loxapine (Loxapac), perphenazine (Trilafon), pimozide (Orap), trifluoperazine (Stelazine), thiothixene (Navane) and zuclopenthixol (Clopixol).
Side-effects of typical antipsychotics vary depending on the drug and may include drowsiness, agitation, dry mouth, constipation, blurred vision, emotional blunting, dizziness, stuffy nose, weight gain, breast tenderness, liquid discharge from breasts, missed periods, muscle stiffness or spasms.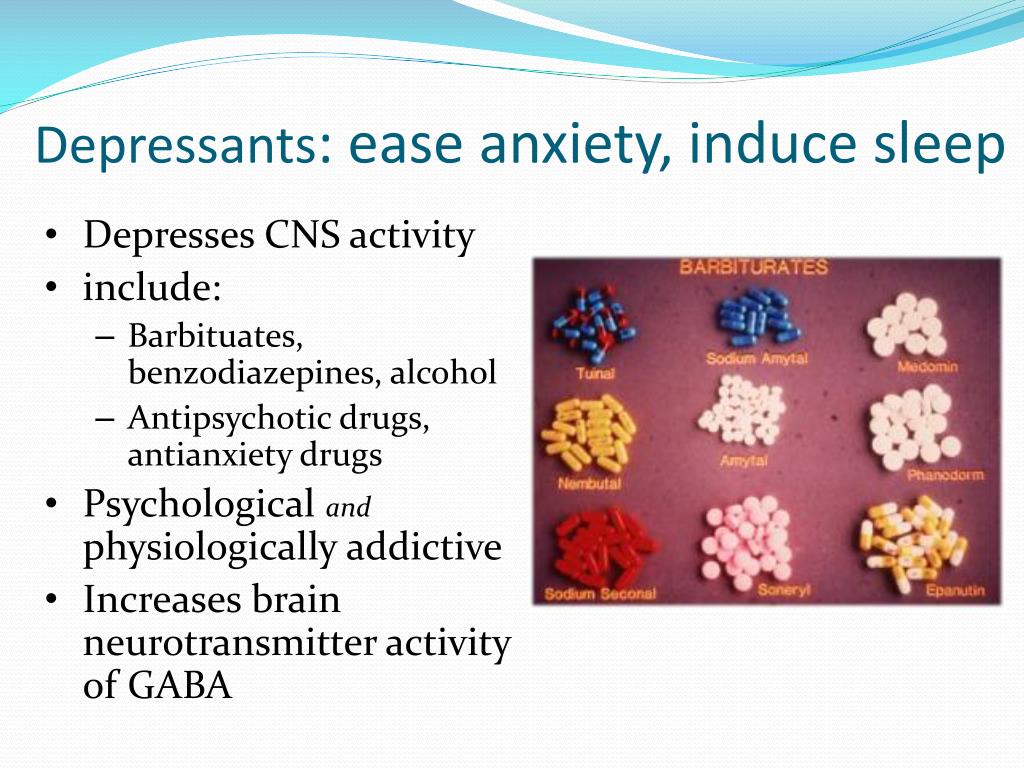
Frequently Asked Questions
| How long should I take antipsychotics? If you take antipsychotics for psychosis, how long you take them depends on what the psychosis is related to and how many episodes you have experienced. In some situations, you may only need to take this medication until the symptoms of psychosis are relieved. In others, antipsychotics may be used over a longer term to help prevent further episodes. When starting a new antipsychotic as a long-term treatment, you should take that drug for at least a month before deciding whether or not it is working for you. Are antipsychotics addictive? Drugs that are addictive produce a feeling of euphoria, a strong desire to continue using the drug, and a need to increase the amount used to achieve the same effect. Antipsychotics do, however, have one thing in common with some addictive drugs—they can cause withdrawal effects when you stop taking them, especially if you stop suddenly. These effects can include nausea, vomiting, diarrhea and stomach pain, dizziness and shakiness. When the time comes to cut down or stop taking the drug, cutting back gradually helps to reduce withdrawal effects. How do I cut down or stop taking antipsychotics? Whether you want to cut down your dose or stop taking a medication, the same rule applies: go slowly. A sudden change in your dose greatly increases the risk that psychotic symptoms will return or become more intense. The first step is to ask yourself if this is the right time. Are you feeling well? Is the level of stress in your life manageable? Do you feel supported by your family and friends? If you think you’re ready, talk to your doctor. If your doctor does agree, he or she will advise you not to skip doses but to reduce your dose gradually—usually by about 10 per cent at a time—with at least two to three weeks between each reduction. This process of cutting back will take several months. Using a pill cutter or a liquid form of your medication can help you to cut your dose down in small amounts. If you want to stop taking more than one medication, your doctor will usually suggest that you lower the dose of one drug at a time. If you start to feel unwell as you cut down, let your doctor know. He or she can help you determine whether you are experiencing withdrawal effects or signs that symptoms are returning. You may want to go back up with your dose. Find the dose that works best for you. Will antipsychotics interact with other medications? Antipsychotics may interact with other medications prescribed by your doctor or dentist or purchased at a drug store, and with herbal remedies or street drugs. Always ask your doctor or pharmacist about potential interactions before taking any medications or herbal remedies, including cold or allergy tablets or cough syrups. Antacids can interfere with absorption of antipsychotics and decrease their effect. If you are taking antacids, you can avoid this by taking them at least two hours before or one hour after taking your medication. What if I smoke cigarettes or drink coffee or alcohol while taking antipsychotics? Smoking cigarettes can increase how quickly some antipsychotics are broken down by the body, meaning that people who smoke heavily may need more medication than those who do not. Drinking coffee has the opposite effect, slowing down the breakdown of antipsychotics. If you change how many cigarettes you smoke or how much coffee you drink, let your doctor know as he or she may need to adjust your dose. Antipsychotic drugs may increase the effects of alcohol, making you more sleepy, dizzy and lightheaded. Having one or two drinks on occasion should be okay—but remember that one drink may have the effect of two or even three drinks. Smoking and problems with alcohol are more common among people with schizophrenia than they are in the general population. The reason for this is unclear; what is clear is that smoking reduces life expectancy, and alcohol can make it even more challenging to manage the symptoms of schizophrenia. Being open and honest about your smoking and drinking lets your doctor know how you are doing and helps him or her to determine whether your medication needs to be adjusted. Talking to your doctor can also give you a chance to think about whether you want to cut down or stop smoking or drinking. What if I use street drugs while taking antipsychotics? Some street drugs, such as marijuana, cocaine and amphetamines, may have effects that feel good in the short term, but they can cause symptoms to return or worsen. Will taking antipsychotics affect my ability to drive safely? Antipsychotic drugs can be sedating, so it’s a good idea not to drive or operate other machinery until you know how the medication affects you. Will taking antipsychotics affect my sex drive and function? People who take antipsychotics can experience decreased sex drive or even problems in sexual functioning. Men may have difficulty getting or keeping an erection or ejaculating. Women may be unable to have an orgasm. Let your doctor know if you experience these side-effects. Often an adjustment in dose or change of medication can help. These drugs can also cause irregular periods and false-positive pregnancy results in women. Is it safe to take antipsychotics while pregnant or breastfeeding? Each woman’s situation is unique and should be discussed with her doctor. Antipsychotics are relatively safe to use during pregnancy and while breastfeeding. If used in high doses close to delivery, the baby may be born with temporary breathing difficulties and/or withdrawal symptoms (e.g., restlessness, feeding problems). Antipsychotic medications pass into breast milk and, depending on the dose, may cause drowsiness in the baby. There are ways, however, to minimize and manage the short-term symptoms that may occur. Your doctor can help you to choose the safest type of medication to take during pregnancy and breastfeeding, and to find a dose that will provide the maximum benefits with the minimum risk. If you decide to stop taking medications during pregnancy or while breastfeeding, it is a good idea to see your doctor more often to help you monitor for a return of symptoms. Is age an issue when taking antipsychotic medications? The effectiveness and risks of antipsychotic medication can vary depending on the age of the person taking it. Can children and teens use antipsychotics? Antipsychotics can be used to treat children and teens with severe psychiatric disorders such as psychosis, bipolar disorder, Tourette syndrome, autism or severe aggression. Most often, psychotherapy also has an important role. Children and teens are more likely than adults to experience side-effects from these medications, especially the second generation (atypical) antipsychotics. Can older adults use antipsychotics? As people age into their 60s and older, they become more sensitive to medication and may require a lower dose. Tardive dyskinesia and other movement-related side-effects can develop in older adults who have used antipsychotics over a long period. Women are twice as likely as men to experience these effects. Antipsychotic medications are sometimes used to calm older adults with psychosis related to dementia. However, use of antipsychotics by older adults has been associated with an increased risk of stroke. Other ways of calming the person should always be tried first, and when antipsychotics are needed, they should only be used until symptoms are relieved. |
Related Programs & Services
- Treatment at CAMH: Access CAMH
- Help for families from CAMH
- ConnexOntario
- Kids Help Phone at 1 800 668-6868
Additional Resources
- For more information on medications, contact your doctor, nurse or pharmacist.
- For information on using medications while pregnant or breastfeeding, contact MotherRisk at 416 813-6780 or visit www.motherisk.org.
Back to top
Turn your reason into action before the new year.
With your support, CAMH can fuel more life-saving mental health research and transform care for those living with mental illness.
Donate
Medicines for mental illness
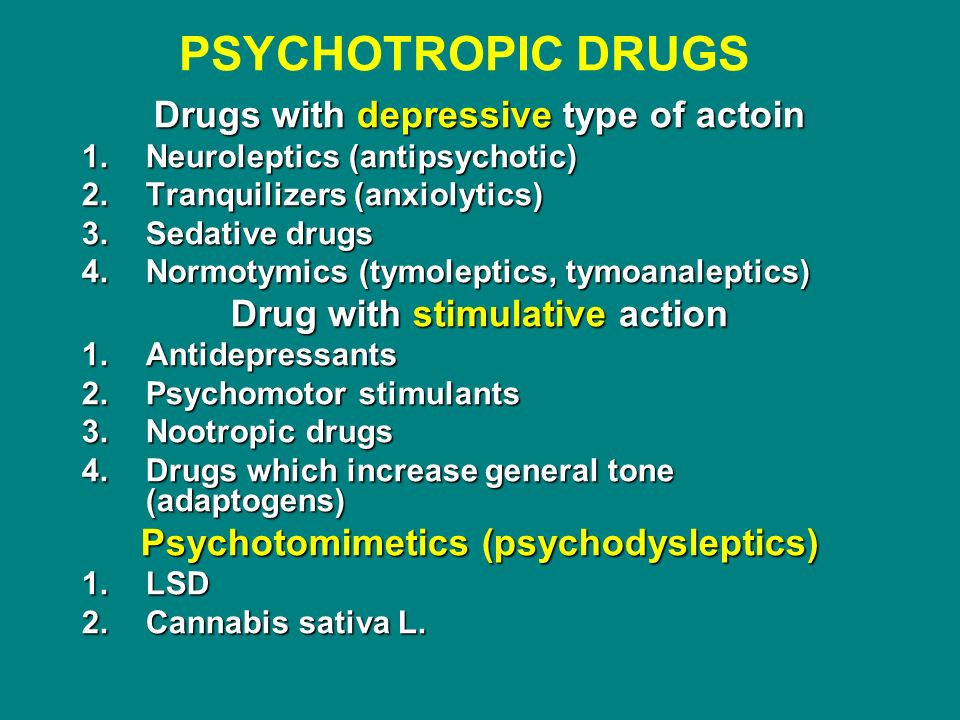
The effectiveness of drug therapy with psychotropic drugs is determined by the compliance of the choice of the drug with the clinical picture of the disease, the correctness of its dosing regimen, the method of administration and the duration of the therapeutic course. As in any field of medicine, in psychiatry it is necessary to take into account the entire complex of drugs that the patient takes, since their mutual action can lead not only to a change in the nature of the effects of each of them, but also to the occurrence of undesirable consequences.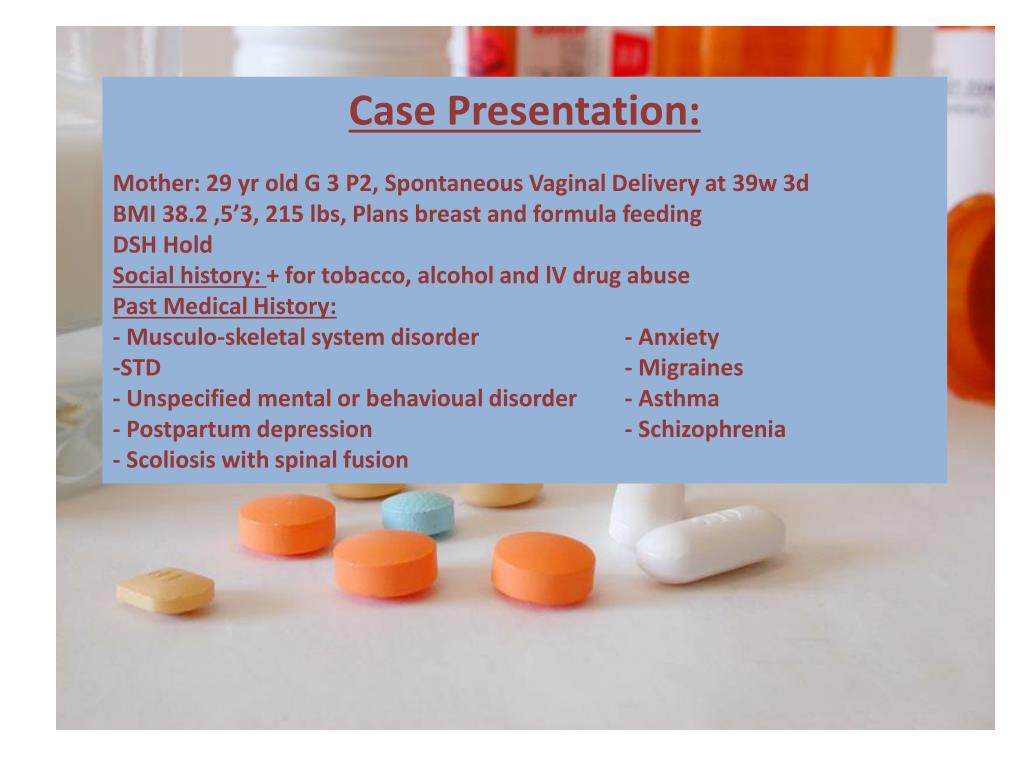
There are several approaches to the classification of psychotropic drugs. Table 1 shows the classification proposed by the WHO in 1990, adapted to include some domestic medicines.
Table 1. Classification of psychopharmacological drugs.
| Grade | Chemical group | Generic and common trade names |
| Antipsychotics | Phenothiazines | Chlorpromazine (chlorpromazine), promazine, thioproperazine (majeptil), trifluperazine (stelazine, triftazine), periciazine (neuleptil), alimemazine (teralen) |
| Xanthenes and thioxanthenes | Chlorprothixene, Clopenthixol (Clopexol), Flupentixol (Fluanxol) | |
| Butyrophenones | Haloperidol, trifluperidol (trisedil, triperidol), droperidol | |
| Piperidine derivatives | Fluspirilene (imap), pimozide (orap), penfluridol (semap) | |
| Cyclic derivatives | Risperidone (rispolept), ritanserin, clozapine (leponex, azaleptin) | |
| Indole and naphthol derivatives | Molindol (moban) | |
| Benzamide derivatives | Sulpiride (eglonil), metoclopramide, racloprid, amisulpiride, sultopride, tiapride (tiapridal) | |
| Derivatives of other substances | Olanzapine (Zyprexa) | |
| Tranquilizers | Benzodiazepines | Diazepam (Valium, Seduxen, Relanium), Chlordiazepoxide (Librium, Elenium), Nitrazempam (Radedorm, Eunoctin) |
| Triazolobenzodiazepines | Alprazolam (Xanax), Triazolam (Chalcion), Madizopam (Dormicum) | |
| Heterocyclic | Brotizopam (lendormin) | |
| Diphenylmethane derivatives | Benactizine (staurodorm), hydroxyzine (atarax) | |
| Heterocyclic derivatives | Busperone (buspar), zopiclone (imovan), clometizol, gemineurin, zolpidem (ivadal) | |
| Antidepressants | Tricyclic | Amitriptyline (Triptisol, Elivel), Imipramine (Melipramine), Clomipramine (Anafranil), Tianeptine (Coaxil) |
| Tetracyclic | Mianserin (Lerivon), Maprotiline (Ludiomil), Pyrlindol (Pyrazidol), | |
| Serotonergic | Citalopram (Seroprax), Sertraline (Zoloft), Paroxetine (Paxil), Viloxazine (Vivalan), Fluoxetine (Prozac), Fluvoxamine (Fevarin), | |
| Noradrenergic and specific serotonergic antidepressants (NaSSA) | Mirtazapine (remeron), milnacipran (ixel) | |
| MAO inhibitors (reversible) | Moclobemide (Aurorix) | |
| Nootropics (as well as substances with a nootropic component of action) | Pyrrolidone derivatives | Piracetam (nootropil) |
| Cyclic derivatives, GABA | Pantogam, Phenibut, Gammalon (Aminalone) | |
| Acetylcholine precursors | Deanol (acti-5) | |
| Pyridoxine derivatives | Pyritinol | |
| Devincan derivatives | Vincamine, Vinpocetine (Cavinton) | |
| Neuropeptides | Vasopressin, oxytocin, thyroliberin, cholecystokinin | |
| Antioxidants | Ionol, mexidol, tocopherol | |
| Stimulants | Phenethylamine derivatives | Amphetamine, salbutamol, methamphetamine (Pervitine) |
| Sydnonimine derivatives | Sydnocarb | |
| Heterocyclic | Methylphnidate (Ritalin) | |
| Purine derivatives | Caffeine | |
| Normotimics | Metal salts | Lithium salts (lithium carbonate, lithium hydroxybutyrate, lithonite, micalite), rubidium chloride, cesium chloride |
| Assembly group | Carbamazepine (finlepsin, tegretol), valpromide (depamide), sodium valproate (depakin, convulex) | |
| Additional group | Assembly group | Amino acids (glycine), opium receptor antagonists (naloxone, naltrexone), neuropeptides (bromocriptine, thyroliberin) |
The main clinical characteristics and side effects of the listed classes of pharmacological drugs are given below.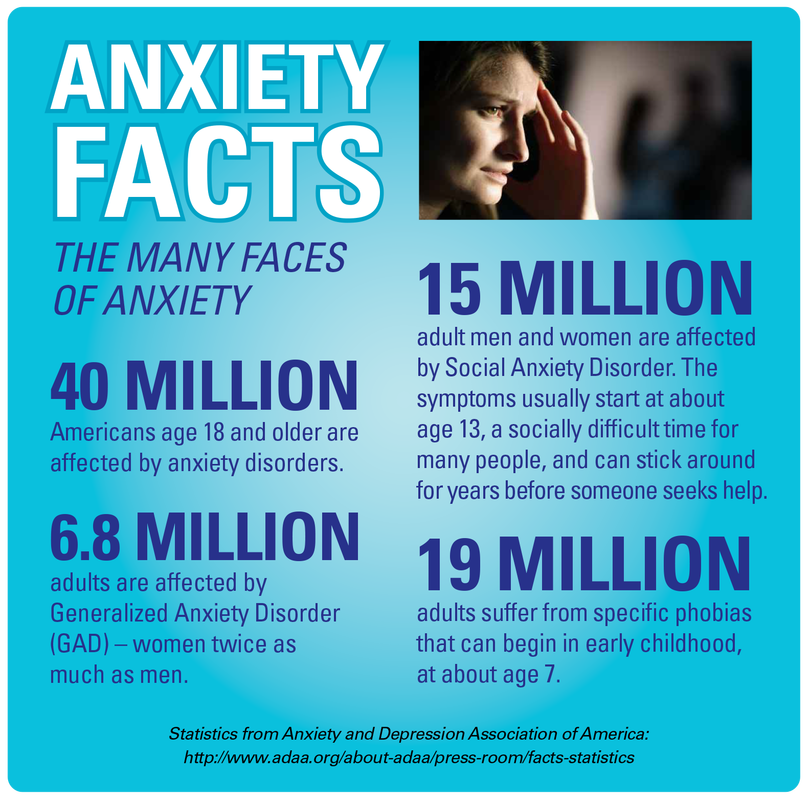
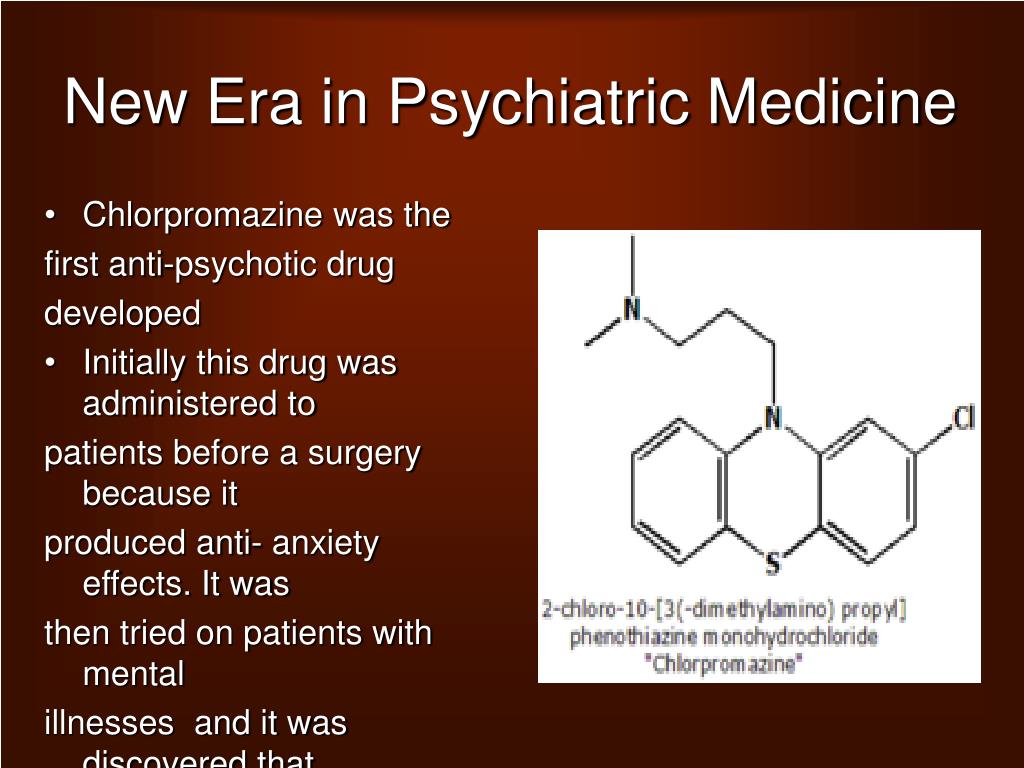
Antipsychotics
Clinical characteristics. This class of drugs is central to the treatment of psychoses. However, the scope of their application is not limited to this, since in small doses in combination with other psychotropic drugs they can be used in the treatment of affective disorders, anxiety-phobic, obsessive-compulsive and somatoform disorders, with decompensation of personality disorders.
Regardless of the characteristics of the chemical structure and mechanism of action, all drugs of this group have similar clinical properties: they have a pronounced antipsychotic effect, reduce psychomotor activity and reduce mental arousal, neurotropic effect, manifested in the development of extrapyramidal and vegetovascular disorders, many of they also have antiemetic properties .
Side effects. The main side effects in the treatment of neuroleptics form the neuroleptic syndrome. The leading clinical manifestations of this syndrome are extrapyramidal disorders with a predominance of either hypo- or hyperkinetic disorders. Hypokinetic disorders include drug-induced parkinsonism, manifested by increased muscle tone, lockjaw, rigidity, stiffness, and slowness of movement and speech. Hyperkinetic disturbances include tremor and hyperkinesis. Usually in the clinical picture in various combinations there are both hypo- and hyperkinetic disorders. The phenomena of dyskinesia can be paroxysmal in nature, localized in the mouth area and manifested by spasmodic contractions of the muscles of the pharynx, tongue, lips, jaws. Often there are phenomena of akathisia - feelings of restlessness, "restlessness in the legs", combined with tasikinesia (the need to move, change position). A special group of dyskinesias includes tardive dyskinesia, which occurs after 2-3 years of taking antipsychotics and is expressed in involuntary movements of the lips, tongue, face.
The leading clinical manifestations of this syndrome are extrapyramidal disorders with a predominance of either hypo- or hyperkinetic disorders. Hypokinetic disorders include drug-induced parkinsonism, manifested by increased muscle tone, lockjaw, rigidity, stiffness, and slowness of movement and speech. Hyperkinetic disturbances include tremor and hyperkinesis. Usually in the clinical picture in various combinations there are both hypo- and hyperkinetic disorders. The phenomena of dyskinesia can be paroxysmal in nature, localized in the mouth area and manifested by spasmodic contractions of the muscles of the pharynx, tongue, lips, jaws. Often there are phenomena of akathisia - feelings of restlessness, "restlessness in the legs", combined with tasikinesia (the need to move, change position). A special group of dyskinesias includes tardive dyskinesia, which occurs after 2-3 years of taking antipsychotics and is expressed in involuntary movements of the lips, tongue, face.
Among the disorders of the autonomic nervous system, orthostatic hypotension, sweating, weight gain, changes in appetite, constipation, diarrhea are most often observed.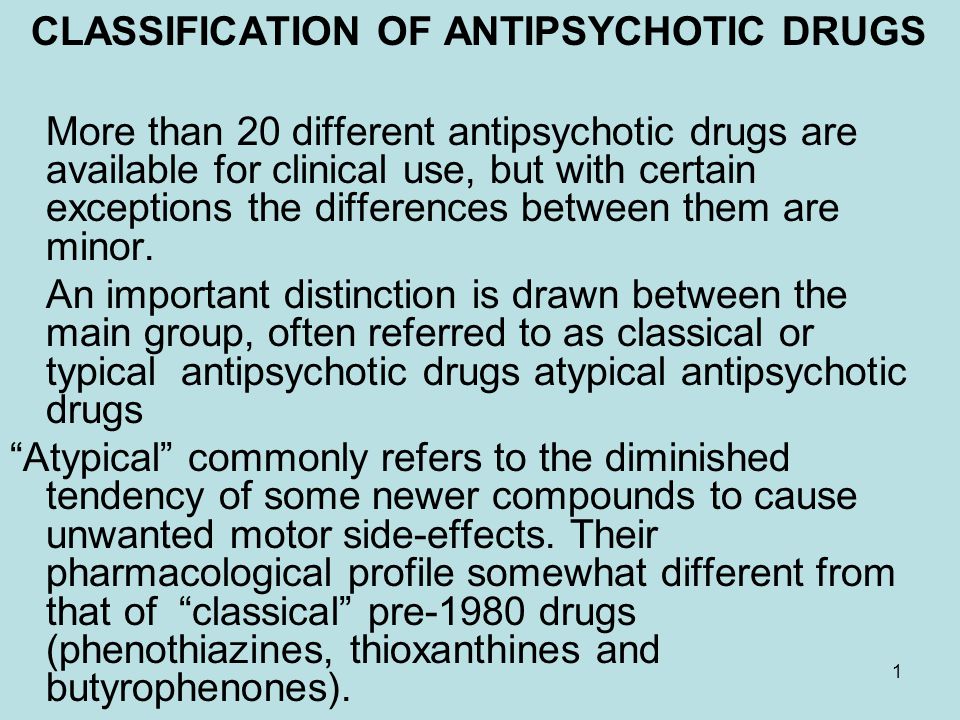 Sometimes there are anticholinergic effects - visual disturbances, dysuric phenomena. Possible functional disorders of the cardiovascular system with changes in the ECG in the form of an increase in the Q-T interval, a decrease in the T wave or its inversion, tachycardia or bradycardia. Sometimes there are side effects in the form of photosensitivity, dermatitis, skin pigmentation; skin allergic reactions are possible.
Sometimes there are anticholinergic effects - visual disturbances, dysuric phenomena. Possible functional disorders of the cardiovascular system with changes in the ECG in the form of an increase in the Q-T interval, a decrease in the T wave or its inversion, tachycardia or bradycardia. Sometimes there are side effects in the form of photosensitivity, dermatitis, skin pigmentation; skin allergic reactions are possible.
Antipsychotics of new generations, compared with traditional derivatives of phenothiazines and butyrophenones, cause significantly fewer side effects and complications.
Tranquilizers
Clinical characteristics. This group includes psychopharmacological agents that relieve anxiety, emotional tension, fear of non-psychotic origin, and facilitate the process of adaptation to stressful factors. Many of them have anticonvulsant and muscle relaxant properties. Their use in therapeutic doses does not cause significant changes in cognitive activity and perception.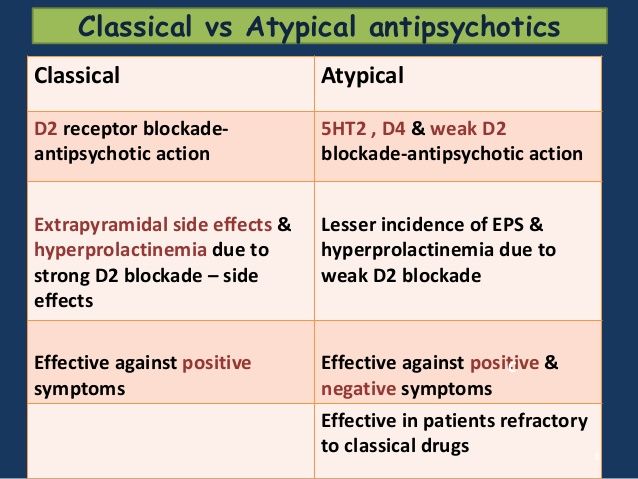 Many of the drugs in this group have a pronounced hypnotic effect and are used primarily as hypnotics. Unlike neuroleptics, tranquilizers do not have a pronounced antipsychotic activity and are used as an additional tool in the treatment of psychosis - to stop psychomotor agitation and correct the side effects of neuroleptics.
Many of the drugs in this group have a pronounced hypnotic effect and are used primarily as hypnotics. Unlike neuroleptics, tranquilizers do not have a pronounced antipsychotic activity and are used as an additional tool in the treatment of psychosis - to stop psychomotor agitation and correct the side effects of neuroleptics.
Side effects of during treatment with tranquilizers are most often manifested by daytime drowsiness, lethargy, muscle weakness, impaired concentration, short-term memory, as well as a slowdown in the speed of mental reactions. In some cases, paradoxical reactions develop in the form of anxiety, insomnia, psychomotor agitation, hallucinations. Among the dysfunctions of the autonomic nervous system and other organs and systems, hypotension, constipation, nausea, urinary retention or incontinence, decreased libido are noted. Long-term use of tranquilizers is dangerous due to the possibility of developing addiction to them, i.e. physical and mental dependence.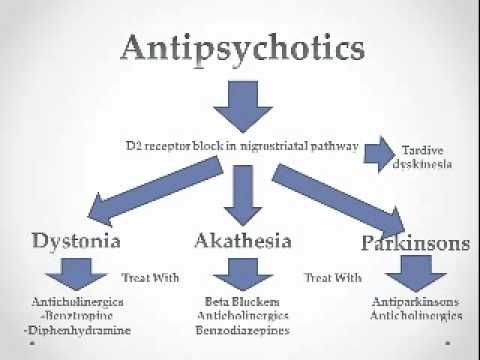
Antidepressants
Clinical characteristics. This class of drugs includes drugs that increase the pathological hypothymic effect, as well as reduce depression-related somatovegetative disorders. A growing body of scientific evidence now suggests that antidepressants are effective for phobic anxiety and obsessive-compulsive disorders. It is assumed that in these cases, not the actual antidepressant, but the anti-obsessional and antiphobic effects are realized. There is data confirming the ability of many antidepressants to increase the threshold of pain sensitivity, to have a preventive effect in migraine and vegetative crises.
Side effects. Side effects related to the central nervous system and the autonomic nervous system are expressed as dizziness, tremor, dysarthria, impaired consciousness in the form of delirium, epileptiform seizures. Possible exacerbation of anxious disorders, activation of suicidal tendencies, inversion of affect, drowsiness or, conversely, insomnia.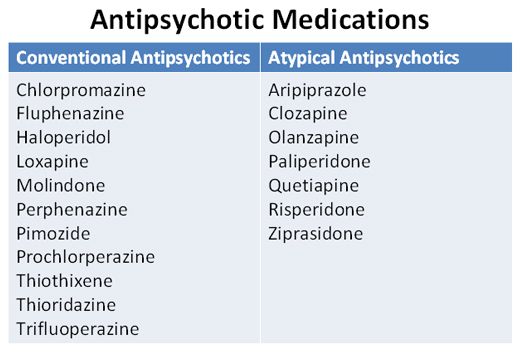 Side effects may be manifested by hypotension, sinus tachycardia, arrhythmia, impaired atrioventricular conduction.
Side effects may be manifested by hypotension, sinus tachycardia, arrhythmia, impaired atrioventricular conduction.
When taking tricyclic antidepressants, various anticholinergic effects are often observed, as well as an increase in appetite. With the simultaneous use of MAO inhibitors with food products containing tyramine or its precursor - tyrosine (cheeses, etc.), a "cheese effect" occurs, manifested by hypertension, hyperthermia, convulsions and sometimes leading to death.
When prescribing serotonin reuptake inhibitors (SSRIs) and reversible MAO-A inhibitors, there may be disturbances in the activity of the gastrointestinal tract, headaches, insomnia, anxiety, and impotence may develop against the background of SSRIs. In the case of a combination of SSRIs with drugs of the tricyclic group, the formation of the so-called serotonin syndrome, which is manifested by an increase in body temperature and signs of intoxication, is possible.
Normotimics
Clinical characteristics. Normotimics include drugs that regulate affective manifestations and have a preventive effect in phasic affective psychoses. Some of these drugs are anticonvulsants.
Normotimics include drugs that regulate affective manifestations and have a preventive effect in phasic affective psychoses. Some of these drugs are anticonvulsants.
Side effects of when using lithium salts are most often tremor. Often there are violations of the function of the gastrointestinal tract - nausea, vomiting, loss of appetite, diarrhea. Often there is an increase in body weight, polydipsia, polyuria, hypothyroidism. Acne, maculo-papular rash, alopecia, as well as worsening of psoriasis are possible.
Signs of severe toxic conditions and overdose of the drug are a metallic taste in the mouth, thirst, severe tremor, dysarthria, ataxia; in these cases, the drug should be stopped immediately.
It should also be noted that side effects may be associated with non-compliance with the diet - a large intake of liquid, salt, smoked meats, cheeses.
Side effects of anticonvulsants are most often associated with functional disorders of the central nervous system and manifest as lethargy, drowsiness, ataxia. Hyperreflexia, myoclonus, tremor can be observed much less frequently. The severity of these phenomena is significantly reduced with a smooth increase in doses.
Hyperreflexia, myoclonus, tremor can be observed much less frequently. The severity of these phenomena is significantly reduced with a smooth increase in doses.
With a pronounced cardiotoxic effect, atrioventricular block may develop.
Nootropics
Clinical characteristics. Nootropics include drugs that can positively affect cognitive functions, stimulate learning, enhance memory processes, increase brain resistance to various adverse factors (in particular, to hypoxia) and extreme stress. However, they do not have a direct stimulating effect on mental activity, although in some cases they can cause anxiety and sleep disturbance.
Side effects - rare. Sometimes there are nervousness, irritability, elements of psychomotor agitation and disinhibition of drives, as well as anxiety and insomnia. Dizziness, headache, nausea and abdominal pain may occur.
Psychostimulants
Clinical characteristics.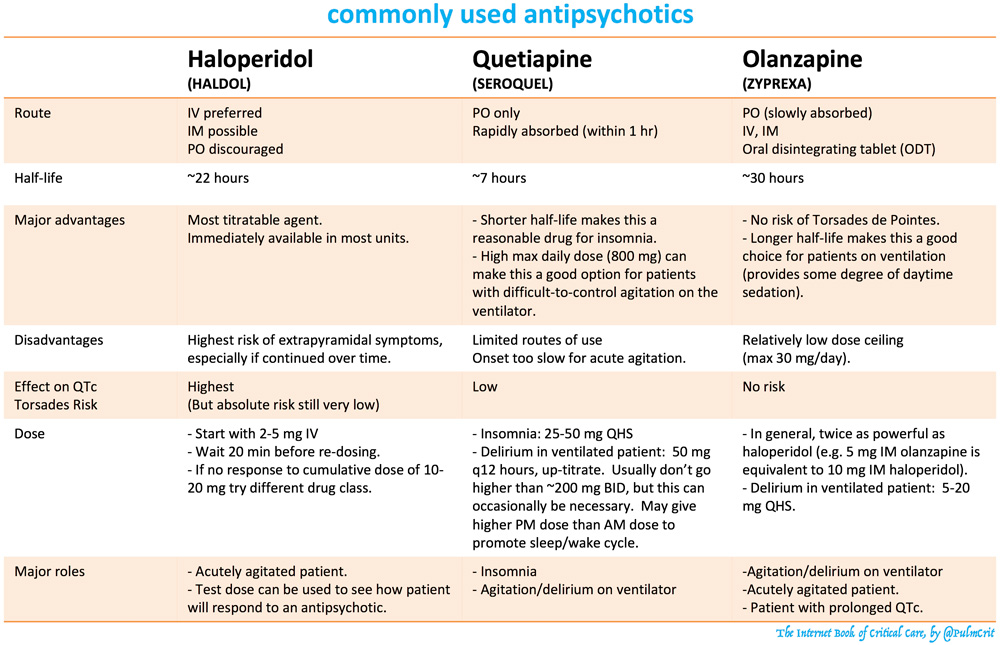 As the name of the class implies, it includes psychotropic drugs that increase the level of wakefulness, have a stimulating effect on mental and physical activity, temporarily increase mental and physical performance and endurance, reduce the feeling of fatigue and drowsiness.
As the name of the class implies, it includes psychotropic drugs that increase the level of wakefulness, have a stimulating effect on mental and physical activity, temporarily increase mental and physical performance and endurance, reduce the feeling of fatigue and drowsiness.
Side effects of are mainly related to effects on the central nervous system (tremor, euphoria, insomnia, irritability, headaches, signs of psychomotor agitation) and the autonomic nervous system (sweating, dry mucous membranes, anorexia). In addition, there may be disorders of cardiovascular activity (arrhythmia, tachycardia, increased blood pressure), as well as a change in the body's sensitivity to insulin in patients with diabetes mellitus. Long-term and frequent use of stimulants can lead to the development of mental and physical dependence.
Arpimed
What Haloperidol is and what it is used for
Haloperidol is the active ingredient in Haloperidol tablets.
Haloperidol belongs to the group of antipsychotic drugs.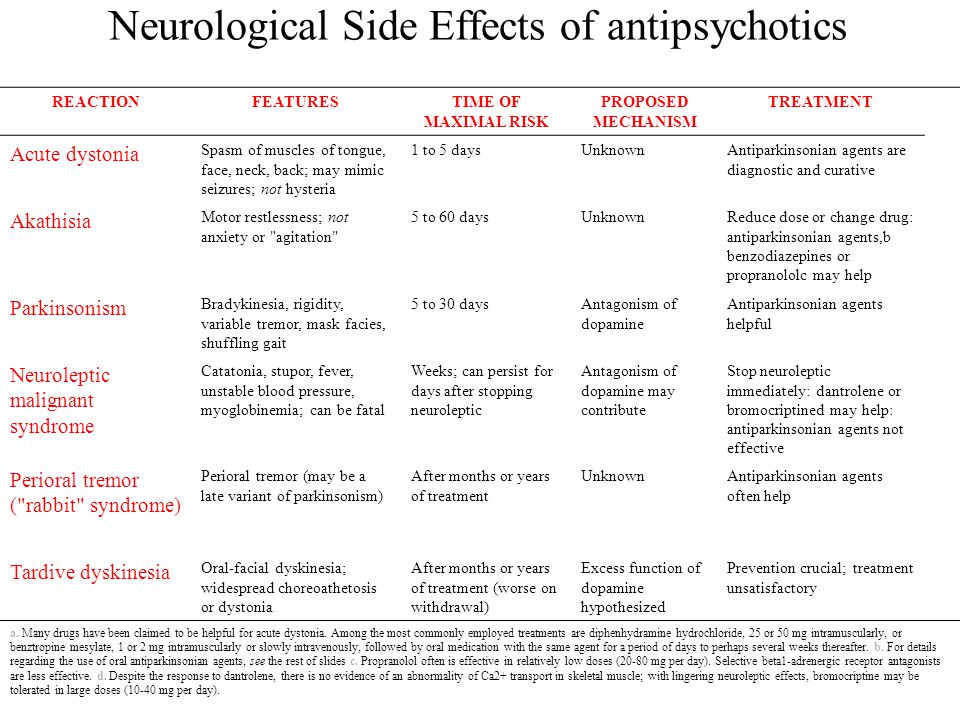
Haloperidol is used to treat:
- Schizophrenia, psychosis, mania and conduct disorders in adults and children.
These symptoms affect thought processes, senses and behavior, resulting in:
- Confusion
- Visual, auditory or tactile hallucinations
- False beliefs
- Delusions (paranoia)
- Feeling overexcited, agitated, excited or hyperactive.
- Feelings of aggressiveness and rage
Haloperidol is also used:
- in Gilles de la Tourette syndrome and uncontrolled tics
- for long-term hiccups
What you need to know before you use Haloperidol
Do not take Haloperidol You should not take this medicine if you have any of the conditions listed above. If you have any doubts about taking the drug, then you should consult your doctor before using Haloperidol. Take special care when taking Haloperidol: Talk to your doctor or pharmacist before taking Haloperidol: You may need to monitor your condition more closely and the dose of Haloperodol may be changed if necessary. If you are in doubt about the presence or absence of any of the above conditions, check with your doctor before using Haloperidol. Medical examination Your doctor needs to take an ECG (electrocardiogram) before or during treatment with Haloperidol. An ECG evaluates the electrical activity of the heart. Blood tests Your doctor will need to check your blood electrolyte levels. Drug interactions Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including OTC and herbal remedies. The thorough Monitoring of the state at The simultaneous appointment of haloperidol with lithium. You should call your doctor immediately and stop taking your medicine if: These are precursors of a syndrome similar to encephalopathy. Haloperidol may affect the effects of the following drugs Tell your doctor or pharmacist if you are taking: Tell your doctor or pharmacist if you are taking any of the above medicines before taking Haloperidol. Some drugs may affect the effects of Haloperidol Tell your doctor or pharmacist if you are taking: It may be necessary to change the dose of haloperidol. Interaction with food and alcohol Haloperidol should be taken with or without food. The tablets should be taken with some water. In patients taking Haloperidol, alcohol intake may lead to the development of drowsiness and decreased alertness. Therefore, you should monitor the amount of alcohol taken. Pregnancy and breast-feeding Talk to your doctor if you are pregnant, think you might be pregnant or plan to become pregnant before taking this medicine. When taking Haloperidol in the last trimester of pregnancy, neonates may develop the following symptoms: tremor, muscle rigidity or weakness, drowsiness, overexcitation, breathing problems and difficulty breastfeeding. If your child has any of these symptoms, you should contact your doctor immediately. You can continue taking Haloperidol only with the permission of your doctor. It is not recommended to take Haloperidol during breastfeeding, as even small amounts of Haloperidol are excreted in breast milk. Consult your healthcare professional if you are pregnant or breastfeeding before taking any medication. Elderly For disorders associated with relative memory loss, you should first consult with your doctor to determine whether further use of Haloperidol is appropriate and explain the possible risks of using the drug. Influence on the ability to drive vehicles and mechanisms Haloperidol may affect the ability to drive vehicles. Do not drive or operate machinery without first talking to your doctor. Important information about the ingredients of Haloperidol Haloperidol tablets contain lactose. If you have been told by your doctor that you have an intolerance to some sugars, talk to your doctor before taking Haloperidol. Available safety data for the use of the drug in children indicates a risk of developing extrapyramidal disorders, including tardive dyskinesia (involuntary, repetitive body movements) and sedation. How to take Haloperidol Haloperidol should be taken exactly as directed by your doctor. If you have any doubts, then you should consult with your doctor. Dosage regimen Your doctor will determine the dosage and duration of Haloperidol. The dose of the drug is set individually. It is very important to take the correct dose. The dose depends on: Adults Children In children, the dose of the drug is determined depending on body weight and age. The daily doses recommended below may be divided into 2-3 doses. Children from 3 to 12 years old In the treatment of childhood schizophrenia, the usual daily dose is 1-4 mg. If necessary, the indicated dose can be increased to 6 mg. In the treatment of agitation (excitation) or conduct disorder, the usual daily dose is 0.5-3 mg, but if necessary, this dose can be increased to 3 mg. Adolescents 13 to 17 years old In the treatment of childhood schizophrenia, the usual daily dose is 1-6 mg per day, but if necessary, this dose can be increased to 10 mg. In the treatment of agitation (agitation) or conduct disorder, the usual daily dose is 2-6 mg, but if necessary, this dose can be increased to 6 mg. Elderly Elderly patients should be treated with half the recommended dose, but if necessary, the dose should be adjusted to that which is optimal for the patient. How to use Haloperidol should be taken orally. Tablets should be taken with some water. Stopping Haloperidol Haloperidol should be continued for as long as prescribed by the doctor. It may take some time before you feel the full effect of the drug. It is necessary to stop taking the drug gradually, unless otherwise prescribed. If you suddenly stop taking Haloperidol, the following symptoms may occur: 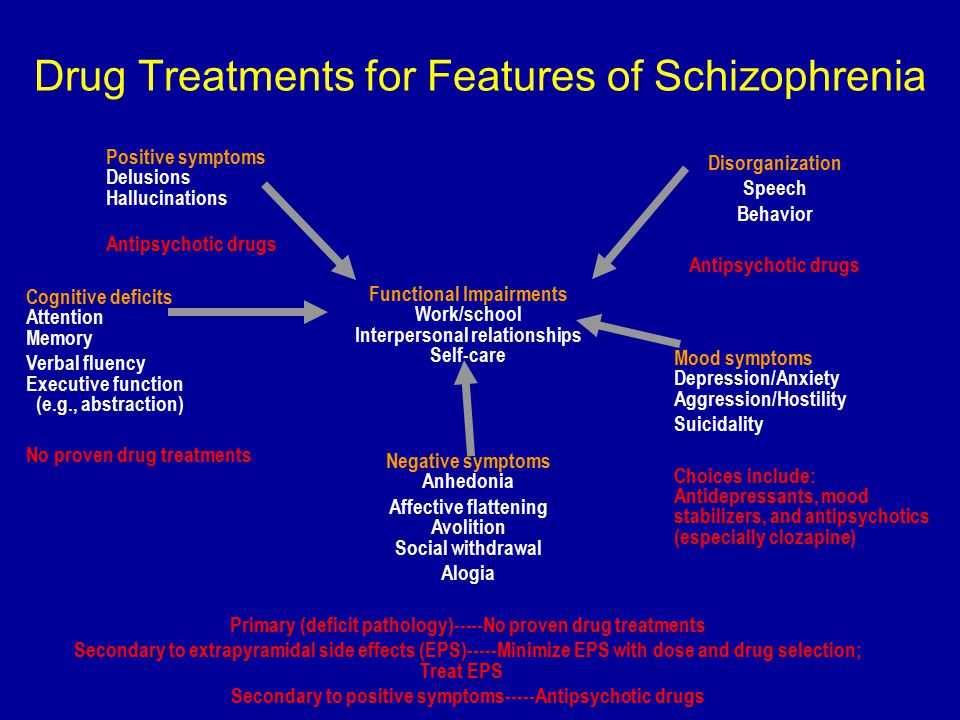

 Long-term safety data are not available.
Long-term safety data are not available.
Follow your doctor's instructions exactly
If you have taken more Haloperidol than recommended to the nearest hospital.
If you forget to take Haloperidol
- If you forget to take Haloperidol, take your next dose at the scheduled time and follow the prescribed dosage regimen.

- Do not double dose.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Possible side effects
Like all medicines, Haloperidol can cause side effects, although not everyone gets them.
Tell your doctor or nurse right away if you notice or suspect any of the following effects. You may need emergency medical treatment.
- Thrombosis of veins, particularly of the lower extremities (symptoms include swelling, tenderness and redness of the lower extremities), which can travel through the blood vessels to the lungs, causing chest pain and difficulty breathing.
- Sudden swelling of the face and throat, urticaria, severe irritation, redness or pustules on the skin. These can be symptoms of severe allergic reactions, although they occur in only a small number of people.
- Development of a very serious condition called neuroleptic malignant syndrome.
 Symptoms include:
Symptoms include:
- Rapid heartbeat, changes in blood pressure and excessive sweating accompanied by fever.
- Rapid breathing, muscle stiffness, impaired consciousness and coma.
- Elevated levels of creatine phosphokinase in the blood.
May affect up to 1 in 1000 people.
- You may develop an abnormal heart rhythm (arrhythmia). An arrhythmia can cause cardiac arrest. In elderly patients with dementia taking antipsychotics, a slight increase in mortality has been reported compared with patients not taking antipsychotics. The exact frequency of development has not been established.
- Jerking movements, slowness of movement, muscle stiffness, trembling and restlessness. Increased salivation, trembling or involuntary movements of the tongue, face, mouth, jaw, larynx, eye rolling. If you have any of these symptoms, you may need additional treatment.
Tell your doctor or nurse immediately if you notice any of these conditions:
- Feeling restless or sleep disturbance.
- Headache
More than 1 in 10 people may experience these symptoms.
- Tremor, muscle stiffness, mask-like face, slow movements and shuffling, uneven gait.
- Feeling restless, tired, depressed or sleepy.
- Feeling dizzy, especially when getting up.
- Symptoms of psychosis such as abnormal thoughts or visual/auditory hallucinations.
- Vision problems, including blurred vision and rapid eye movements.
Less than 1 in 10 people may experience these symptoms.
- Liver dysfunction including yellowing of the skin and whites of the eyes, pale stools and dark urine.
- Confusion
- Decreased levels of white blood cells, which can lead to frequent infections.
- Seizures (epilepsy)
- Difficulty or wheezing
- Hormonal disorders that may lead to:
- to change in body weight
- to dysfunction of the reproductive system, such as erectile dysfunction.

- in some men to develop mammary edema or painful and prolonged erections.
- to loss of sexual desire
- in some women to the development of irregular, painful or heavy menstruation or to the absence of menstruation.
- in some women to an unexpected discharge of breast milk with painful sensations in the mammary glands.
Less than 1 in 100 people may experience these symptoms.
Haloperidol may cause trismus (a toxic spasm of the masticatory muscles leading to limited movement in the temporomandibular joint.)
This symptom may affect less than 1 in 1000 people.
- Bleeding or bruising easily. These symptoms are caused by a decrease in the level of platelets in the blood.
- Fluid retention in the body with negative effects on the brain resulting in weakness, fatigue or confusion.
The exact incidence of these side effects has not been identified.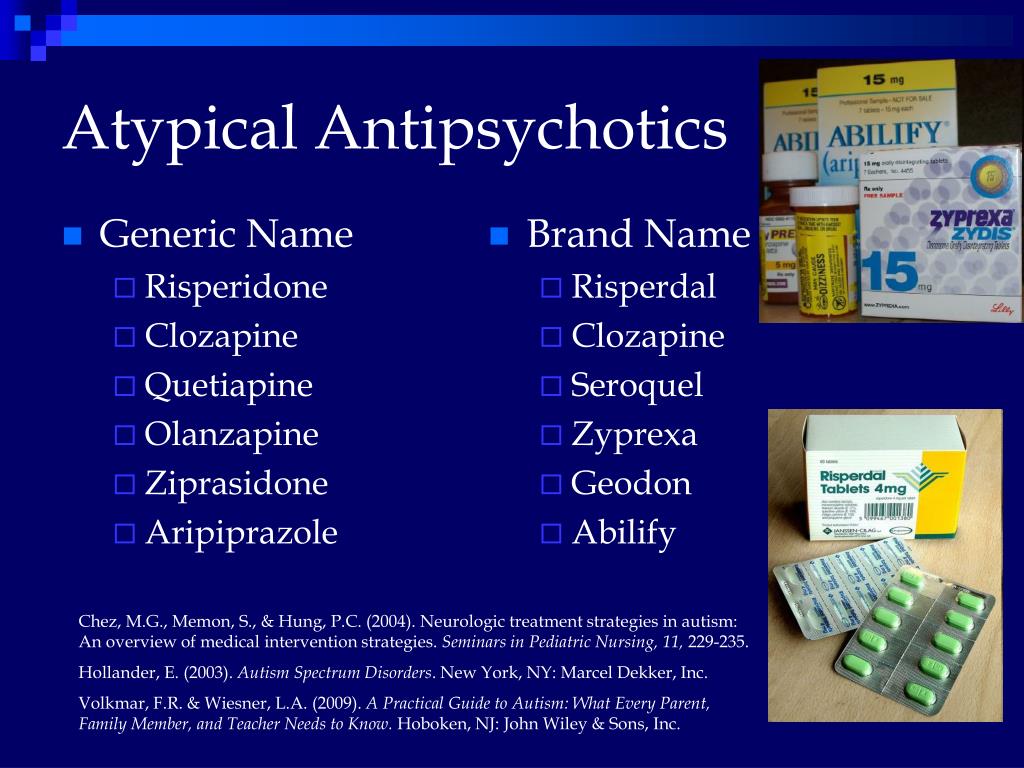 Rash
Rash
Uncommon (may affect up to 1 in 100 people)
- increased skin sensitivity to sunlight
- excessive sweating
- fever
- ankle edema
When taking Haloperidol, the following side effects were observed, but the frequency of these side effects was not identified.
- Peeling and peeling of the skin
- Inflammation of the skin (skin reddened, sensitive, warm to the touch)
- Low body temperature
- Taking Haloperidol during the last trimester of pregnancy may cause tremors, muscle rigidity and/or weakness, drowsiness, agitation, breathing problems and difficulty breastfeeding in newborns.
If your child has any of these symptoms, you should contact your doctor immediately.
Effects on biochemical test results:
- Test results showing abnormal liver function
- Low blood sugar (hypoglycemia)
- Electrocardiogram (ECG) abnormalities
Reporting side effects
If you notice any side effects, tell your doctor, pharmacist or pharmacist, including any side effects not listed in this package insert. You can also report side effects to Arpimed LLC by going to the website www.arpimed.com and filling out the appropriate form “Report a side effect or ineffectiveness of a drug” and to the Scientific Center for Expertise of Drugs and Medical Technologies named after. Academician E.Gabrielyan, by going to the website www.pharm.am in the section “Report a side effect of a drug” and fill out the form “Map of reporting a side effect of a drug”. Scientific center hotline: +37410237665; +37498773368 By reporting side effects, you help provide more information about the safety of this drug.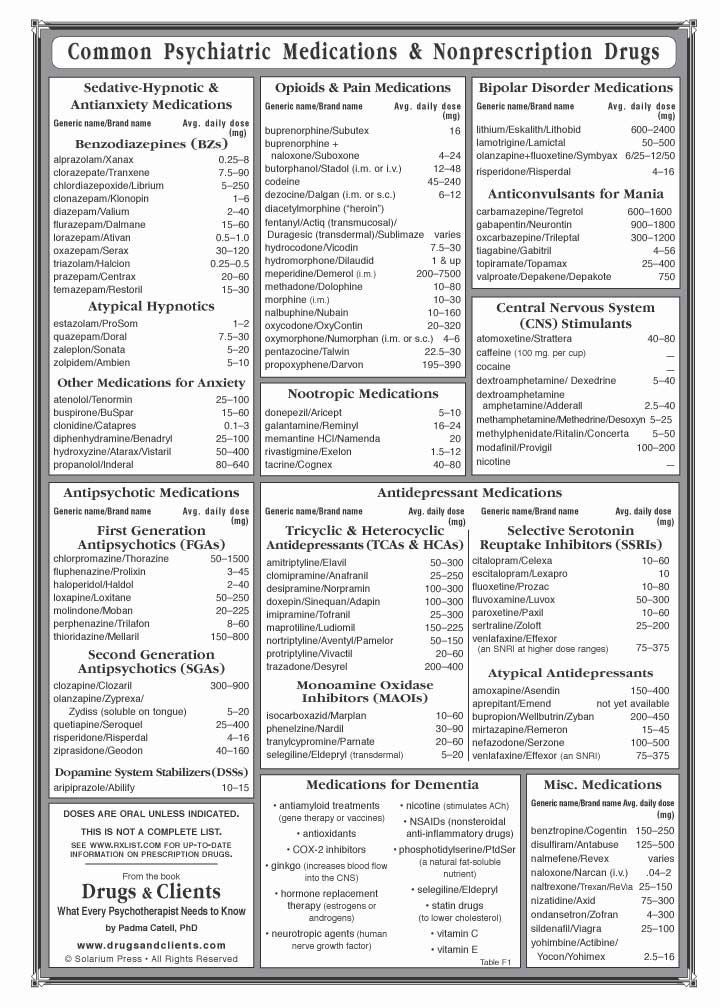
How to store Haloperidol
Haloperidol 5 mg tablets .
The drug should be stored out of the reach of children, dry, dark place at a temperature of 15 0 C -25 0 C.
- Shelf life - 3 years. Do not take Haloperidol after the expiry date which is stated on the package. When specifying the expiration date, the last day of the specified month is meant.
- Keep the tablets in the blister until it is time to take the drug.
- If tablets have changed color or show other signs of deterioration, ask your pharmacist how to dispose of
Important information
This drug has been prescribed just for you. Only your doctor can prescribe this drug for you. It should never be given to others. It can harm them even if they have similar symptoms.
If you have any further questions or doubts about taking a medicine after reading this package leaflet, ask your doctor or pharmacist.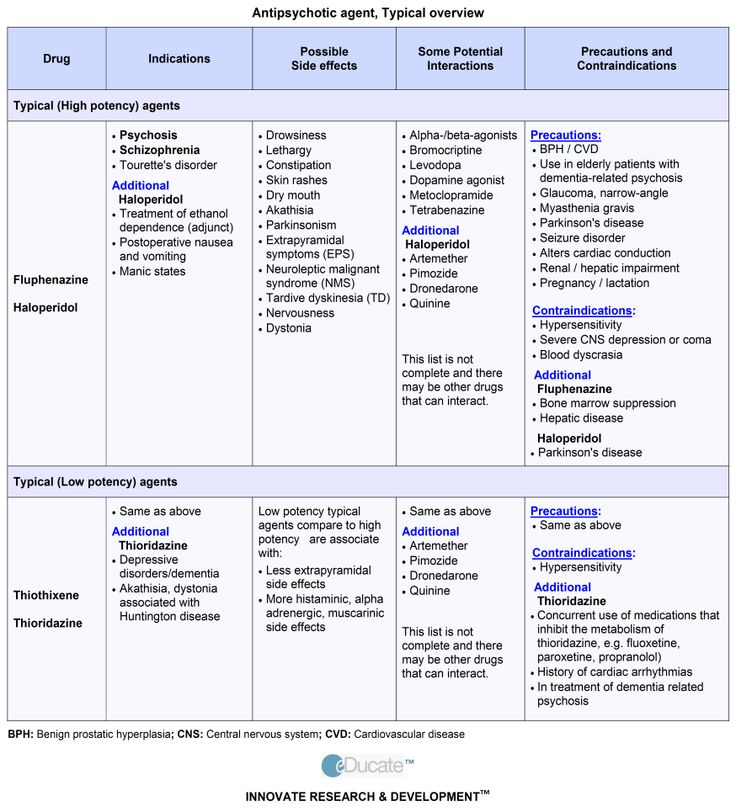
 Antipsychotics do not have these effects.
Antipsychotics do not have these effects.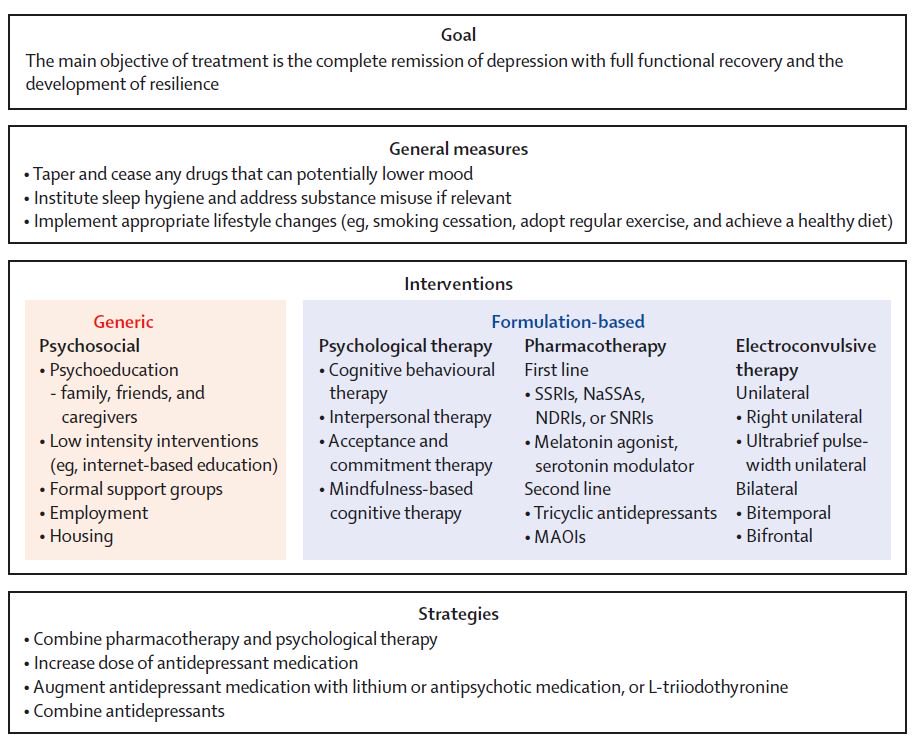 If your doctor doesn’t agree, find out why. If you are not satisfied with his or her reasons, you may want to see another doctor for a second opinion.
If your doctor doesn’t agree, find out why. If you are not satisfied with his or her reasons, you may want to see another doctor for a second opinion.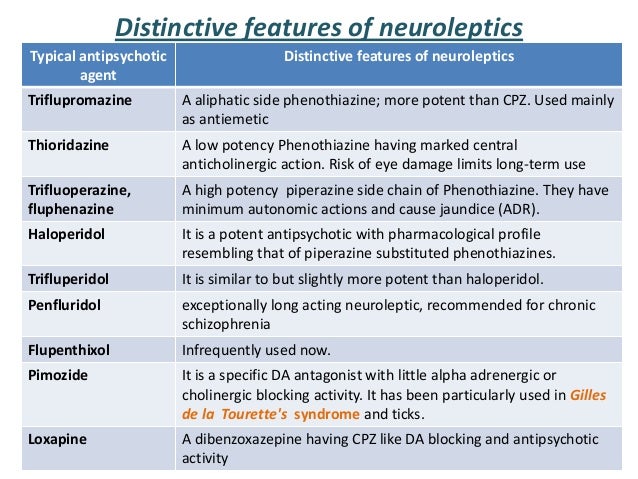 Make sure you tell your doctor about all drugs you are taking.
Make sure you tell your doctor about all drugs you are taking.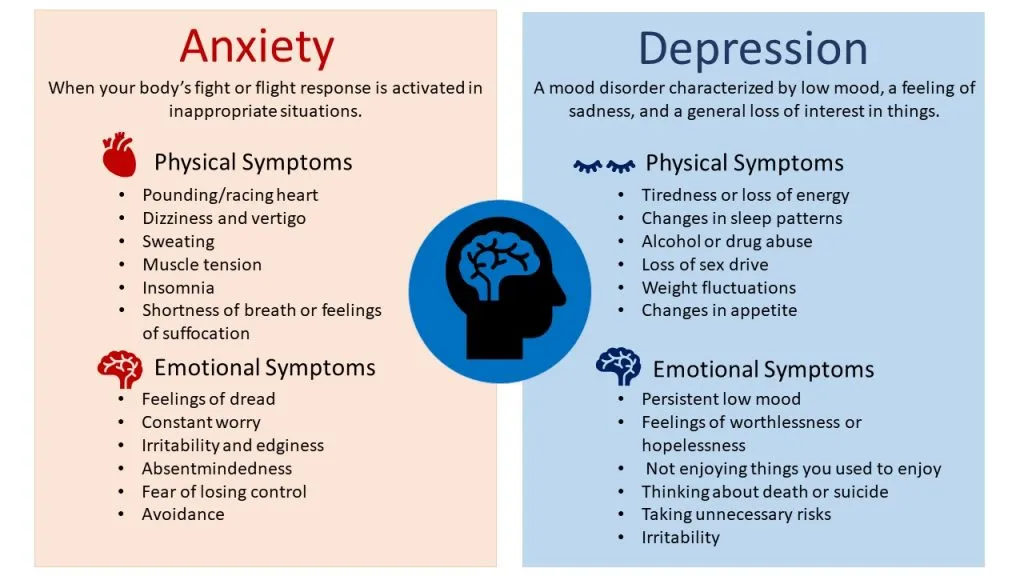
 Using these drugs increases the risk of psychosis, even in people who do not have schizophrenia or another mental health problem. Street drugs may also interfere with your medication or worsen side-effects.
Using these drugs increases the risk of psychosis, even in people who do not have schizophrenia or another mental health problem. Street drugs may also interfere with your medication or worsen side-effects.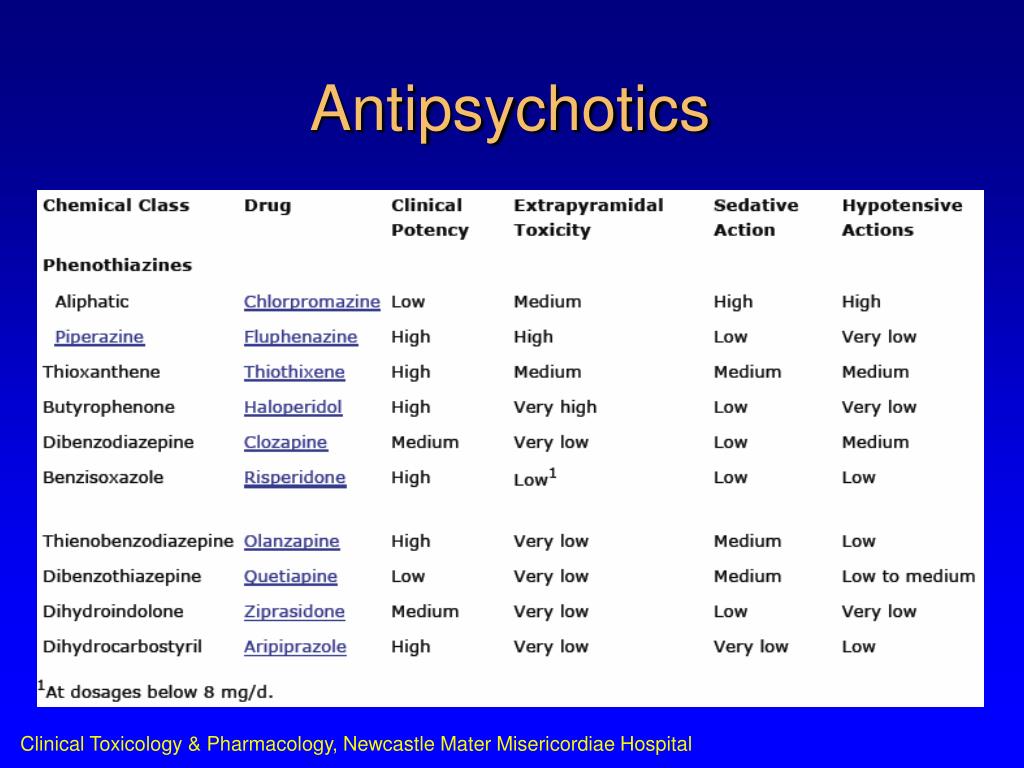 For any pregnant woman with a history of psychosis, the question of taking antipsychotics during pregnancy usually comes down to a risk-benefit analysis. Psychosis can affect prenatal care and a mother’s ability to parent her newborn child. When treatment with an antipsychotic helps to avoid a relapse or to reduce distress, the benefits of continuing the medication may outweigh the risks.
For any pregnant woman with a history of psychosis, the question of taking antipsychotics during pregnancy usually comes down to a risk-benefit analysis. Psychosis can affect prenatal care and a mother’s ability to parent her newborn child. When treatment with an antipsychotic helps to avoid a relapse or to reduce distress, the benefits of continuing the medication may outweigh the risks.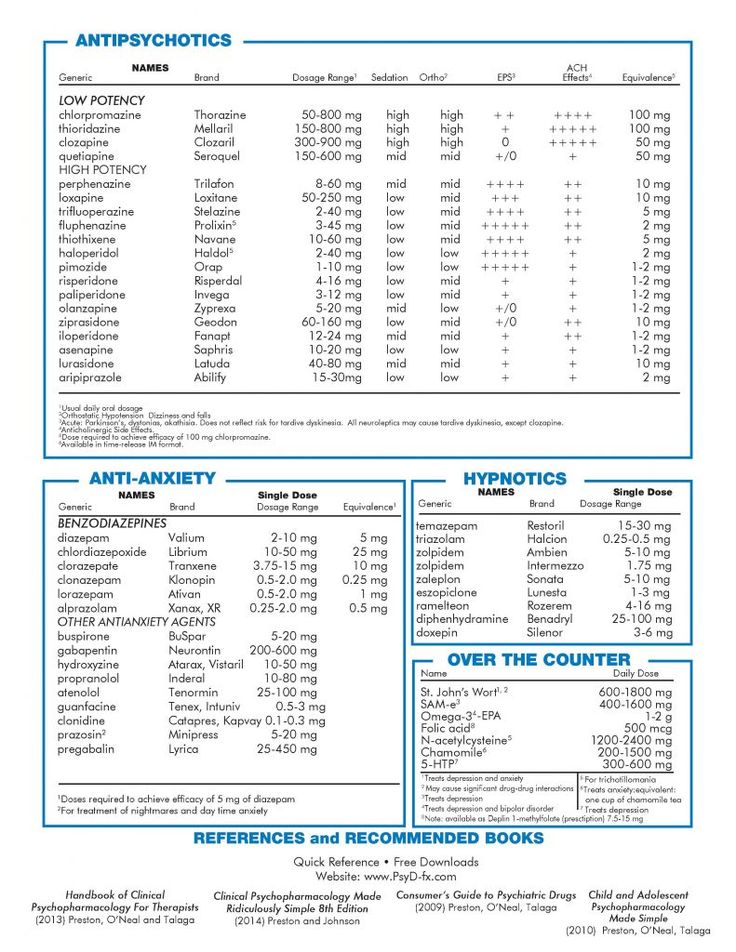
 Being more sensitive also means that older people are more likely to experience side-effects than when they were younger. They are also more likely to have other medical problems and to be taking other medications, which could interact with antipsychotic drugs. Antipsychotics can increase the risk of falls, especially when taken with other drugs.
Being more sensitive also means that older people are more likely to experience side-effects than when they were younger. They are also more likely to have other medical problems and to be taking other medications, which could interact with antipsychotic drugs. Antipsychotics can increase the risk of falls, especially when taken with other drugs.