Types of catatonia
Catatonia: Symptoms, Causes, Diagnosis, Treatment
Written by Matt Smith
Catatonia is a group of symptoms that usually involve a lack of movement and communication, and also can include agitation, confusion, and restlessness.
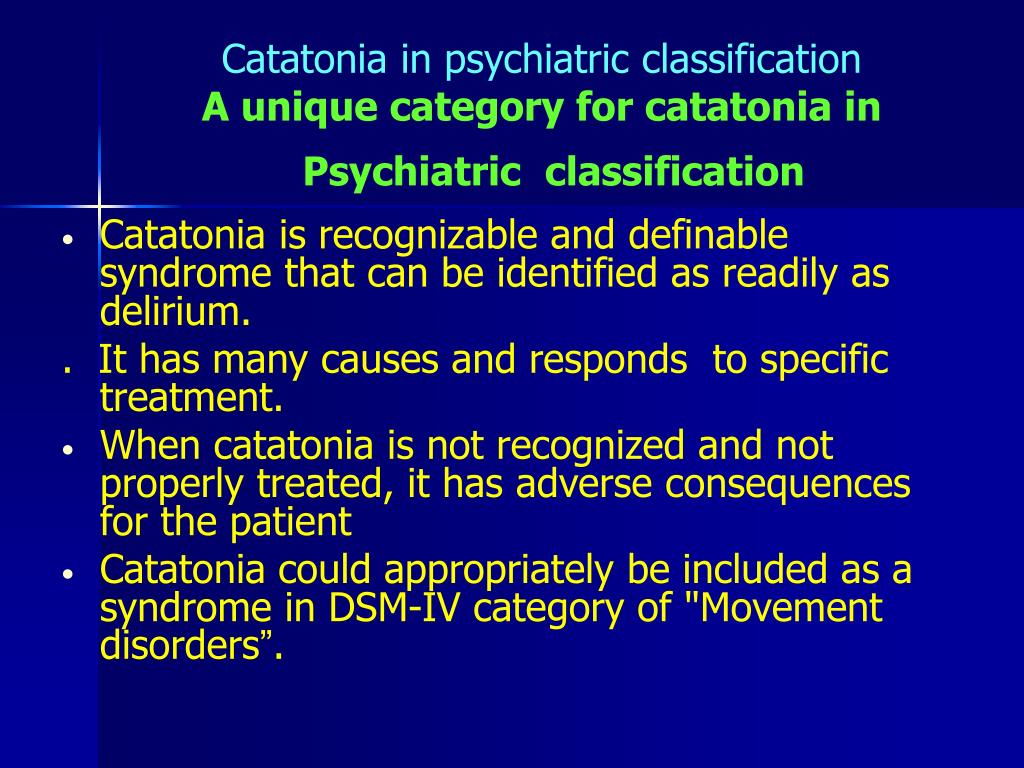
Until recently, it was thought of as a type of schizophrenia. But doctors now understand that other mental illnesses and some conditions that throw off your body’s metabolism also can make you catatonic. About 1 person in 10 who has a severe mental illness will have catatonia at some point.
Catatonia can be treated, but if it’s not, it can lead to life-threatening problems.
Symptoms and Diagnosis
Doctors can diagnose someone as catatonic if they have any three of these signs:
- Not responding to other people or their environment
- Not speaking
- Holding their body in an unusual position
- Resisting people who try to adjust their body
- Agitation
- Repetitive, seemingly meaningless movement
- Mimicking someone else’s speech
- Mimicking someone else’s movements
Types
There are three types of catatonia:
- Akinetic catatonia.
This is the most common. Someone with akinetic catatonia often stares blankly and won’t respond when you speak to them. If they do respond, it may only be to repeat what you said. Sometimes they sit or lie in an unusual position and won’t move.
- Excited catatonia. With this type, the person may move around, but their movement seems pointless and impulsive. They may seem agitated, combative, or delirious, or they may mimic the movements of someone who’s trying to help them.
- Malignant catatonia. This type happens when the symptoms lead to other health problems, like dangerous changes in blood pressure, body temperature, or breathing or heart rate. Someone who’s catatonic for a long time may be more likely to have problems like dehydration, blood clots, or kidney failure as a result of the symptoms.
Causes
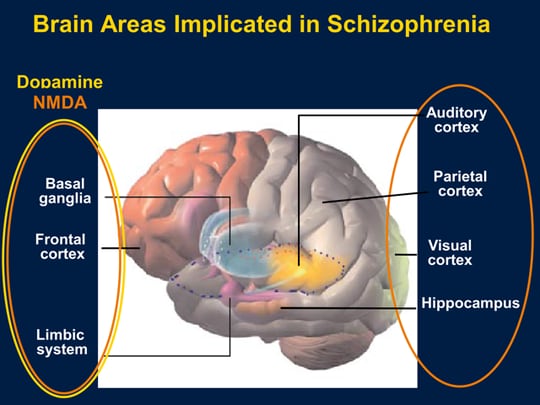
Doctors aren’t sure exactly what makes someone become catatonic. It happens most often with people who have mood disorders or psychotic disorders, like depression, bipolar disorder, and schizophrenia. About a third of people who are catatonic also have bipolar disorder.
About a third of people who are catatonic also have bipolar disorder.
Several physical conditions can lead to catatonia in people who don’t have a mental illness. These include:
- Conditions that affect your body chemistry, like kidney problems, diabetes, and thyroid conditions
- Parkinson’s disease, which attacks your body’s nervous system
- Encephalitis, an infection that affects your brain
Treatment
Doctors usually treat catatonia with a kind of sedative called a benzodiazepine that’s often used to ease anxiety.
Another treatment option is electroconvulsive therapy (ECT). It sends electrical impulses to the person’s brain through electrodes placed on their head. (They’re given medicine to sleep through the procedure.) It might be recommended if:
- Sedatives don’t work.
- The catatonia is severe.
- The person has had catatonia before.
- Quick action is needed to save someone’s life.
Catatonia: Our current understanding of its diagnosis, treatment and pathophysiology
1. Rosebush PI, Hildebrand AM, Furlong BG, Mazurek MF. Catatonic syndrome in a general psychiatric inpatient population: frequency, clinical presentation, and response to lorazepam. J Clin Psychiatry. 1990;51:357–362. [PubMed] [Google Scholar]
Rosebush PI, Hildebrand AM, Furlong BG, Mazurek MF. Catatonic syndrome in a general psychiatric inpatient population: frequency, clinical presentation, and response to lorazepam. J Clin Psychiatry. 1990;51:357–362. [PubMed] [Google Scholar]
2. Peralta V, Cuesta MJ. Motor features in psychotic disorders. II. Development of diagnostic criteria for catatonia. Schizophr Res. 2001;47:117–126. [PubMed] [Google Scholar]
3. Peralta V, Campos MS, de Jalon EG, Cuesta MJ. DSM-IV catatonia signs and criteria in first-episode, drug-naive, psychotic patients: psychometric validity and response to antipsychotic medication. Schizophr Res. 2010;118:168–175. [PubMed] [Google Scholar]
4. Morrison JR. Catatonia. Retarded and excited types. Arch Gen Psychiatry. 1973;28:39–41. [PubMed] [Google Scholar]
5. Mann SC, Caroff SN, Bleier HR, Welz WK, Kling MA, Hayashida M. Lethal catatonia. Am J Psychiatry. 1986;143:1374–1381. [PubMed] [Google Scholar]
6. Mann SC, Caroff SN, Bleier HR, Antelo RE, Un H. Electroconvulsive Therapy of the Lethal Catatonia Syndrome. Convuls Ther. 1990;6:239–247. [PubMed] [Google Scholar]
Electroconvulsive Therapy of the Lethal Catatonia Syndrome. Convuls Ther. 1990;6:239–247. [PubMed] [Google Scholar]
7. Francis A, Fink M, Appiani F, Bertelsen A, Bolwig TG, Bräunig P, Caroff SN, Carroll BT, Cavanna AE, Cohen D, et al. Catatonia in Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. J ECT. 2010;26:246–247. [PMC free article] [PubMed] [Google Scholar]
8. Rosebush PI, Mazurek MF. Catatonia and its treatment. Schizophr Bull. 2010;36:239–242. [PMC free article] [PubMed] [Google Scholar]
9. England ML, Ongür D, Konopaske GT, Karmacharya R. Catatonia in psychotic patients: clinical features and treatment response. J Neuropsychiatry Clin Neurosci. 2011;23:223–226. [PMC free article] [PubMed] [Google Scholar]
10. Medda P, Toni C, Luchini F, Giorgi Mariani M, Mauri M, Perugi G. Catatonia in 26 patients with bipolar disorder: clinical features and response to electroconvulsive therapy. Bipolar Disord. 2015;17:892–901. [PubMed] [Google Scholar]
11. Raja M, Altavista MC, Cavallari S, Lubich L. Neuroleptic malignant syndrome and catatonia. A report of three cases. Eur Arch Psychiatry Clin Neurosci. 1994;243:299–303. [PubMed] [Google Scholar]
Raja M, Altavista MC, Cavallari S, Lubich L. Neuroleptic malignant syndrome and catatonia. A report of three cases. Eur Arch Psychiatry Clin Neurosci. 1994;243:299–303. [PubMed] [Google Scholar]
12. White DA, Robins AH. An analysis of 17 catatonic patients diagnosed with neuroleptic malignant syndrome. CNS Spectr. 2000;5:58–65. [PubMed] [Google Scholar]
13. Paparrigopoulos T, Tzavellas E, Ferentinos P, Mourikis I, Liappas J. Catatonia as a risk factor for the development of neuroleptic malignant syndrome: report of a case following treatment with clozapine. World J Biol Psychiatry. 2009;10:70–73. [PubMed] [Google Scholar]
14. Strawn JR, Keck PE, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry. 2007;164:870–876. [PubMed] [Google Scholar]
15. Carroll BT, Taylor RE. The nondichotomy between lethal catatonia and neuroleptic malignant syndrome. J Clin Psychopharmacol. 1997;17:235–238. [PubMed] [Google Scholar]
16. Fink M. Neuroleptic malignant syndrome and catatonia: one entity or two? Biol Psychiatry. 1996;39:1–4. [PubMed] [Google Scholar]
1996;39:1–4. [PubMed] [Google Scholar]
17. Worku B, Fekadu A. Symptom profile and short term outcome of catatonia: an exploratory clinical study. BMC Psychiatry. 2015;15:164. [PMC free article] [PubMed] [Google Scholar]
18. Clinebell K, Azzam PN, Gopalan P, Haskett R. Guidelines for preventing common medical complications of catatonia: case report and literature review. J Clin Psychiatry. 2014;75:644–651. [PubMed] [Google Scholar]
19. Levenson JL. Medical aspects of catatonia. Prim Psychiatry. 2009;16:23–26. [Google Scholar]
20. McCall WV, Mann SC, Shelp FE, Caroff SN. Fatal pulmonary embolism in the catatonic syndrome: two case reports and a literature review. J Clin Psychiatry. 1995;56:21–25. [PubMed] [Google Scholar]
21. Medda P, Fornaro M, Fratta S, Callari A, Manzo V, Ciaponi B, Perugi G. A case of deep venous thrombosis following protracted catatonic immobility recovered with electroconvulsive therapy: the relevance for an early intervention. Gen Hosp Psychiatry. 2012;34:209.e5–209.e7. [PubMed] [Google Scholar]
2012;34:209.e5–209.e7. [PubMed] [Google Scholar]
22. Rosebush PI, Mazurek MF. Catatonia: re-awakening to a forgotten disorder. Mov Disord. 1999;14:395–397. [PubMed] [Google Scholar]
23. Kahlbaum KL. Catatonia. Levij Y, Pridan T. Baltimore: Johns Hopkins University Press; 1973. [Google Scholar]
24. Fink M, Shorter E, Taylor MA. Catatonia is not schizophrenia: Kraepelin’s error and the need to recognize catatonia as an independent syndrome in medical nomenclature. Schizophr Bull. 2010;36:314–320. [PMC free article] [PubMed] [Google Scholar]
25. Abrams R, Taylor MA. Catatonia. A prospective clinical study. Arch Gen Psychiatry. 1976;33:579–581. [PubMed] [Google Scholar]
26. Kakooza-Mwesige A, Wachtel LE, Dhossche DM. Catatonia in autism: implications across the life span. Eur Child Adolesc Psychiatry. 2008;17:327–335. [PubMed] [Google Scholar]
27. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160:1233–1241. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
28. Tandon R, Heckers S, Bustillo J, Barch DM, Gaebel W, Gur RE, Malaspina D, Owen MJ, Schultz S, Tsuang M, et al. Catatonia in DSM-5. Schizophr Res. 2013;150:26–30. [PubMed] [Google Scholar]
29. Bush G, Fink M, Petrides G, Dowling F, Francis A. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93:129–136. [PubMed] [Google Scholar]
30. Miller DD, Caroff SN, Davis SM, Rosenheck RA, McEvoy JP, Saltz BL, Riggio S, Chakos MH, Swartz MS, Keefe RS, et al. Extrapyramidal side-effects of antipsychotics in a randomised trial. Br J Psychiatry. 2008;193:279–288. [PMC free article] [PubMed] [Google Scholar]
31. Rosebush PI, Mazurek MF. Neurologic side effects in neuroleptic-naive patients treated with haloperidol or risperidone. Neurology. 1999;52:782–785. [PubMed] [Google Scholar]
32. Gelenberg AJ, Mandel MR. Catatonic reactions to high-potency neuroleptic drugs. Arch Gen Psychiatry. 1977;34:947–950. [PubMed] [Google Scholar]
33. Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T. Neuroleptic malignant syndrome and atypical antipsychotic drugs. J Clin Psychiatry. 2004;65:464–470. [PubMed] [Google Scholar]
Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T. Neuroleptic malignant syndrome and atypical antipsychotic drugs. J Clin Psychiatry. 2004;65:464–470. [PubMed] [Google Scholar]
34. Addonizio G, Susman VL, Roth SD. Symptoms of neuroleptic malignant syndrome in 82 consecutive inpatients. Am J Psychiatry. 1986;143:1587–1590. [PubMed] [Google Scholar]
35. Rosebush P, Stewart T. A prospective analysis of 24 episodes of neuroleptic malignant syndrome. Am J Psychiatry. 1989;146:717–725. [PubMed] [Google Scholar]
36. Drislane FW. Presentation, evaluation, and treatment of nonconvulsive status epilepticus. Epilepsy Behav. 2000;1:301–314. [PubMed] [Google Scholar]
37. Maganti R, Gerber P, Drees C, Chung S. Nonconvulsive status epilepticus. Epilepsy Behav. 2008;12:572–586. [PubMed] [Google Scholar]
38. Marin RS, Wilkosz PA. Disorders of diminished motivation. J Head Trauma Rehabil. 2005;20:377–388. [PubMed] [Google Scholar]
39. Muqit MM, Rakshi JS, Shakir RA, Larner AJ. Catatonia or abulia? A difficult differential diagnosis. Mov Disord. 2001;16:360–362. [PubMed] [Google Scholar]
Catatonia or abulia? A difficult differential diagnosis. Mov Disord. 2001;16:360–362. [PubMed] [Google Scholar]
40. Bauer G, Gerstenbrand F, Rumpl E. Varieties of the locked-in syndrome. J Neurol. 1979;221:77–91. [PubMed] [Google Scholar]
41. Kennard C, Illingworth R. Persistent vegetative state. J Neurol Neurosurg Psychiatry. 1995;59:347–348. [PMC free article] [PubMed] [Google Scholar]
42. Cruse D, Chennu S, Chatelle C, Bekinschtein TA, Fernández-Espejo D, Pickard JD, Laureys S, Owen AM. Bedside detection of awareness in the vegetative state: a cohort study. Lancet. 2011;378:2088–2094. [PubMed] [Google Scholar]
43. Owen AM, Coleman MR, Boly M, Davis MH, Laureys S, Pickard JD. Detecting awareness in the vegetative state. Science. 2006;313:1402. [PubMed] [Google Scholar]
44. Kulkarni VP, Lin K, Benbadis SR. EEG findings in the persistent vegetative state. J Clin Neurophysiol. 2007;24:433–437. [PubMed] [Google Scholar]
45. McKeon A, Robinson MT, McEvoy KM, Matsumoto JY, Lennon VA, Ahlskog JE, Pittock SJ.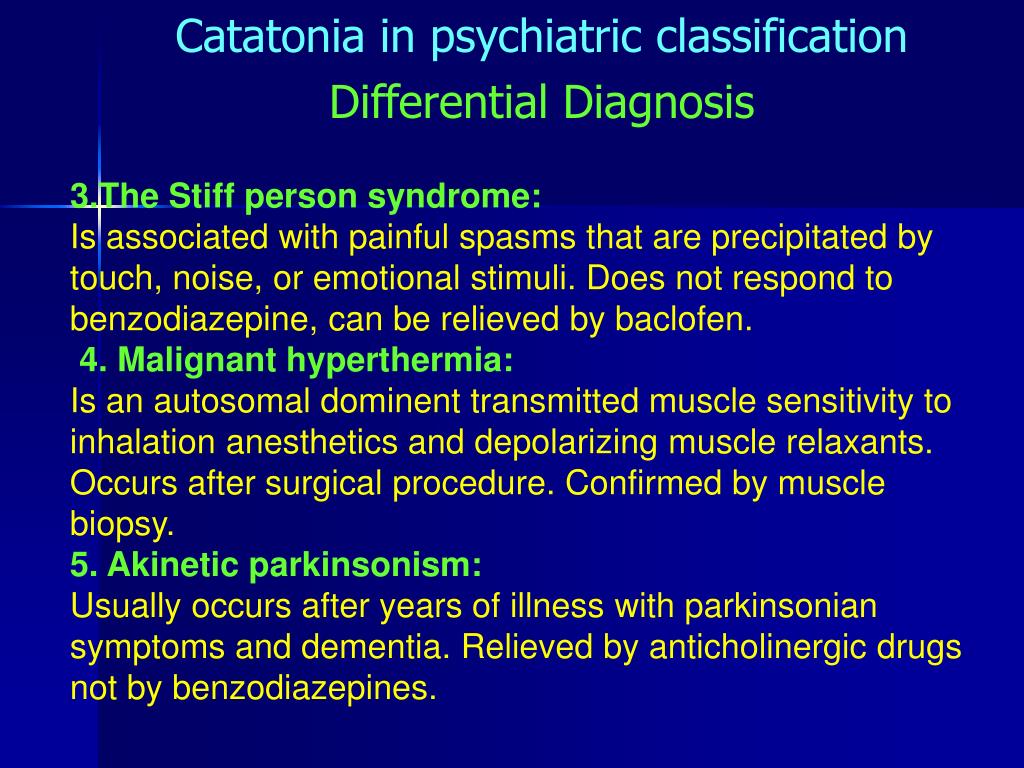 Stiff-man syndrome and variants: clinical course, treatments, and outcomes. Arch Neurol. 2012;69:230–238. [PubMed] [Google Scholar]
Stiff-man syndrome and variants: clinical course, treatments, and outcomes. Arch Neurol. 2012;69:230–238. [PubMed] [Google Scholar]
46. Ungvari GS, Leung CM, Wong MK, Lau J. Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285–288. [PubMed] [Google Scholar]
47. Smith JH, Smith VD, Philbrick KL, Kumar N. Catatonic disorder due to a general medical or psychiatric condition. J Neuropsychiatry Clin Neurosci. 2012;24:198–207. [PubMed] [Google Scholar]
48. Rosebush PI, Mazurek MF. Serum iron and neuroleptic malignant syndrome. Lancet. 1991;338:149–151. [PubMed] [Google Scholar]
49. Fricchione G, Mann SC, Caroff SN. Catatonia, lethal catatonia, and neuroleptic malignant syndrome. Psychiatr Ann. 2000;30:347–355. [Google Scholar]
50. Lee JW. Serum iron in catatonia and neuroleptic malignant syndrome. Biol Psychiatry. 1998;44:499–507. [PubMed] [Google Scholar]
51. Rosebush PI, Mazurek MF. Catatonia after benzodiazepine withdrawal. J Clin Psychopharmacol. 1996;16:315–319. [PubMed] [Google Scholar]
J Clin Psychopharmacol. 1996;16:315–319. [PubMed] [Google Scholar]
52. Brown M, Freeman S. Clonazepam withdrawal-induced catatonia. Psychosomatics. 2009;50:289–292. [PubMed] [Google Scholar]
53. Lee JW, Schwartz DL, Hallmayer J. Catatonia in a psychiatric intensive care facility: incidence and response to benzodiazepines. Ann Clin Psychiatry. 2000;12:89–96. [PubMed] [Google Scholar]
54. Sienaert P, Dhossche DM, Vancampfort D, De Hert M, Gazdag G. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181. [PMC free article] [PubMed] [Google Scholar]
55. Weder ND, Muralee S, Penland H, Tampi RR. Catatonia: a review. Ann Clin Psychiatry. 2008;20:97–107. [PubMed] [Google Scholar]
56. Rosebush PI, Hildebrand A, Mazurek MF. The syndrome of recurring catatonia: treatment and relationship to underlying illness. Proceedings of the 147th Annual Meeting of the American Psychiatric Association. USA: Philadelphia; 1994. p. 129. [Google Scholar]
57. Grover S, Aggarwal M. Long-term maintenance lorazepam for catatonia: a case report. Gen Hosp Psychiatry. 2011;33:82.e1–82.e3. [PubMed] [Google Scholar]
Grover S, Aggarwal M. Long-term maintenance lorazepam for catatonia: a case report. Gen Hosp Psychiatry. 2011;33:82.e1–82.e3. [PubMed] [Google Scholar]
58. Ungvari GS, Chiu HF, Chow LY, Lau BS, Tang WK. Lorazepam for chronic catatonia: a randomized, double-blind, placebo-controlled cross-over study. Psychopharmacology (Berl) 1999;142:393–398. [PubMed] [Google Scholar]
59. Gaind GS, Rosebush PI, Mazurek MF. Lorazepam treatment of acute and chronic catatonia in two mentally retarded brothers. J Clin Psychiatry. 1994;55:20–23. [PubMed] [Google Scholar]
60. Hawkins JM, Archer KJ, Strakowski SM, Keck PE. Somatic treatment of catatonia. Int J Psychiatry Med. 1995;25:345–369. [PubMed] [Google Scholar]
61. Girish K, Gill NS. Electroconvulsive therapy in Lorazepam non-responsive catatonia. Indian J Psychiatry. 2003;45:21–25. [PMC free article] [PubMed] [Google Scholar]
62. Hatta K, Miyakawa K, Ota T, Usui C, Nakamura H, Arai H. Maximal response to electroconvulsive therapy for the treatment of catatonic symptoms. J ECT. 2007;23:233–235. [PubMed] [Google Scholar]
J ECT. 2007;23:233–235. [PubMed] [Google Scholar]
63. Rosebush PI, Mazurek MF. Risk of NMS in patients with catatonia (Proceedings of the 149th Annual Meeting of the American Psychiatric Association) USA: New York; 1996. p. 30. [Google Scholar]
64. Adityanjee YA, Mathews T. Epidemiology of neuroleptic malignant syndrome. Clin Neuropharmacol. 1999;22:151–158. [PubMed] [Google Scholar]
65. Caroff SN, Mann SC. Neuroleptic malignant syndrome. Med Clin North Am. 1993;77:185–202. [PubMed] [Google Scholar]
66. Bastiampillai T, McGovern V, Lloyd B, Hittur Lingappa S, Nelson A. Treatment refractory chronic catatonia responsive to zolpidem challenge. Aust N Z J Psychiatry. 2016;50:98. [PubMed] [Google Scholar]
67. Peglow S, Prem V, McDaniel W. Treatment of catatonia with zolpidem. J Neuropsychiatry Clin Neurosci. 2013;25:E13. [PubMed] [Google Scholar]
68. Thomas P, Cottencin O, Rascle C, Vaiva G, Goudemand M, Bieder J. Catatonia in French psychiatry: implications of the zolpidem challenge test. Psychiatr Ann. 2007;37:45–54. [Google Scholar]
Psychiatr Ann. 2007;37:45–54. [Google Scholar]
69. Carroll BT, Goforth HW, Thomas C, Ahuja N, McDaniel WW, Kraus MF, Spiegel DR, Franco KN, Pozuelo L, Muñoz C. Review of adjunctive glutamate antagonist therapy in the treatment of catatonic syndromes. J Neuropsychiatry Clin Neurosci. 2007;19:406–412. [PubMed] [Google Scholar]
70. Ellul P, Rotgé JY, Choucha W. Resistant Catatonia in a High-Functioning Autism Spectrum Disorder Patient Successfully Treated with Amantadine. J Child Adolesc Psychopharmacol. 2015;25:726. [PubMed] [Google Scholar]
71. Moskowitz AK. “Scared stiff”: catatonia as an evolutionary-based fear response. Psychol Rev. 2004;111:984–1002. [PubMed] [Google Scholar]
72. Northoff G. Catatonia and neuroleptic malignant syndrome: psychopathology and pathophysiology. J Neural Transm (Vienna) 2002;109:1453–1467. [PubMed] [Google Scholar]
73. Dhossche DM, Stoppelbein L, Rout UK. Etiopathogenesis of catatonia: generalizations and working hypotheses. J ECT.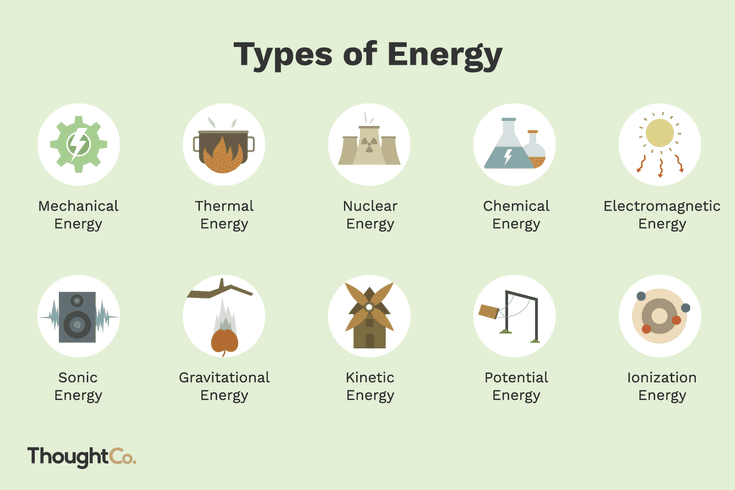 2010;26:253–258. [PubMed] [Google Scholar]
2010;26:253–258. [PubMed] [Google Scholar]
Treatment of catatonic schizophrenia in St. Petersburg
- Main
- Psychiatry
- Treatment of schizophrenia
- Catatonic schizophrenia
The catatonic form (ICD-10 F20.2) is diagnosed in no more than 3% of the total number of people suffering from schizophrenia. As a rule, the first signs of a mental disorder manifest already in childhood or adolescence, but parents do not attach any importance to them. In addition, catatonic schizophrenia can occur much later, due to severe stress, certain diseases, or TBI. Therefore, an examination is necessary to make an accurate diagnosis.
Therefore, an examination is necessary to make an accurate diagnosis.
Catatonic schizophrenia, left untreated, poses a threat to the life of the patient and the people around him: attacks of catatonic stupor or excitement can cause trauma, as in these states a person loses touch with the surrounding reality.
Catatonic stupor is one of the main symptoms of this form of schizophrenia. An attack can catch a patient at a pedestrian crossing, driving a car or in another situation that could lead to an accident. Therefore, if a person from time to time "plunges into himself" and stops responding to people around him, relatives should not hesitate to make an appointment with a psychiatrist.
In 2009 the Oxford Academy published an article in the Schizophrenia Bulletin (Fink M, Shorter E, Tailor M, "Catatonia is not schizophrenia: kraepelin's error and the need to recognize catatonia as an independent syndrome in medical nomenclature") in which there is a dominant superiority of manic and depressive disorders over schizophrenia in the event of a catatonic stupor. Thus, it is necessary to understand that stupor can be not only a symptom of catatonic schizophrenia, but also other mental disorders, somatic or neurological diseases.
Thus, it is necessary to understand that stupor can be not only a symptom of catatonic schizophrenia, but also other mental disorders, somatic or neurological diseases.
Doctor's consultation on the treatment of catatonic schizophrenia:
+7 (812) 407-18-00
Thank you for your trust!
- Examination at the clinic
- Expert level psychopharmacologists
- Post-discharge management
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A. V. (Associate Professor, PhD) V. (Associate Professor, PhD) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | For free | |
| Standard Chamber | 8 900 ₽ | |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Types of catatonic stupor
Usually a person learns about his diagnosis already being hospitalized, when catatonic stupor finds him in a public place.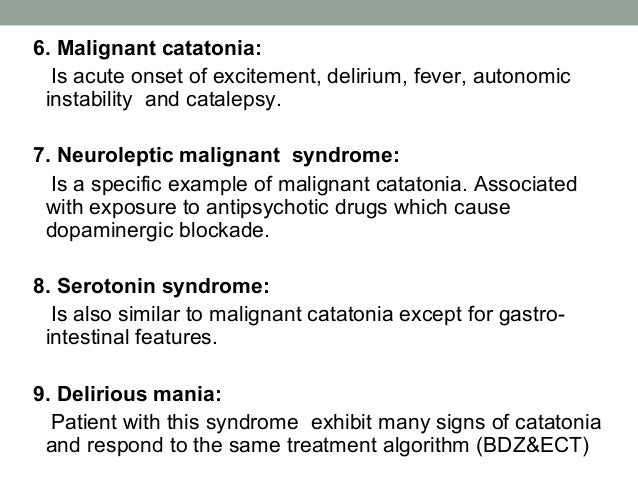 There are several types of stupor that differ in clinical dynamics and human response to external stimuli. However, stupor does not mean complete incapacity, but such a person certainly needs the help of others.
There are several types of stupor that differ in clinical dynamics and human response to external stimuli. However, stupor does not mean complete incapacity, but such a person certainly needs the help of others.
Pathetic catatonic excitation
Pathetic catatonic excitation develops over time. At first, moderate motor and speech activity is observed. Speech can be pathos, bright, sometimes with the repetition of other people's phrases (echolalia). This state is often accompanied by euphoria and causeless laughter. With all this, a person does not lose touch with reality.
Impulsive catatonic excitation
Impulsive catatonic excitation develops rapidly. Such a person becomes cruel, prone to destructive behavior and aggression. Speech becomes impoverished and reduced to a chaotic set of phrases, echolalia. Movements can copy others, there is a high probability of self-harm and suicide.
Silent catatonic excitement
In case of silent catatonic excitement, a person makes senseless chaotic movements, resists attempts to calm him down. In addition, in an affective state there is a risk of self-harm and suicide, as well as mutilation of others.
In addition, in an affective state there is a risk of self-harm and suicide, as well as mutilation of others.
Catatonic stupor
Catatonic stupor can last from several hours to several months. A person stops talking, moving and paying attention to external stimuli. Activity appears only at the time of satisfaction of natural needs. Communication with reality is broken - as a rule, at this time a person sees vivid hallucinations.
Cataleptic stupor
When a cataleptic stupor occurs, a person may be in an uncomfortable position for a long time, but succumb to external influences (for example, attempts to put him to bed). Sometimes such a person may respond to whispers and wake up at night.
Negativistic stupor
Negativistic stupor, in contrast to cataleptic one, is characterized by active resistance when trying to change a person's posture.
Stupor with torpor
In stupor with stupor, motor inhibition is most pronounced. As a rule, a person takes the fetal position, in which he arrives for a long time.
As a rule, a person takes the fetal position, in which he arrives for a long time.
Syndromokinesis
In some cases, people with catatonic schizophrenia may experience alternating types of stupor, including arousal.
We treat catatonic schizophrenia including drug intolerance and drug resistance. In addition, our clinic employs psychotherapists and psychologists with clinical experience who are also involved in the treatment of mental disorders associated with schizophrenia.
Symptoms of catatonic schizophrenia
Catatonic stupor is not the only symptom of this type of schizophrenia. Another symptom of the disease and the exact opposite of stupor is catatonic excitement. Excitation can be expressed in motor and speech activity that does not make sense to others. Excitation is no less dangerous and poses a risk both to the life of the patient and to those around him.
In a state of catatonic arousal, a person may lose control of himself, resulting in self-harm and unintentional suicide attempts (eg, going out a window or on the roadway, self-mutilation with sharp objects).
Some other symptoms of catatonic schizophrenia include:
- grimacing;
- repetition of words or phrases;
- activities that make no sense;
- alternating activity with immobility;
- unquestioning execution of other people's instructions;
- copying the movements of people around;
- aggression, cruelty, negativism;
- assuming unusual postures.
In addition, the course of the disease may be accompanied by general symptoms of schizophrenia - hallucinations, delusions, social self-isolation, depression, emotional dullness, inactivity, unwillingness to take care of oneself, memory disorder.
In its early stages, catatonic schizophrenia may present with inappropriate behavior (foolishness), frilly or bizarre speech, grimacing, and pathological 'reverie'. When the first signs of the disease occur, we recommend that you seek the advice of a psychiatrist and begin treatment of the catatonic form of schizophrenia in advance.
Treatment of catatonic schizophrenia in our clinic
Physical examination, neuro- and psychological testing is usually sufficient to make a diagnosis. However, in some cases, in order to accurately determine the cause of catatonic schizophrenia and related diseases, an additional examination may be prescribed:
- EEG;
- MRI;
- CT.
Treatment of catatonic schizophrenia in the clinic
Treatment of catatonic schizophrenia in our clinic includes examination, selection of drugs in the minimum effective dosage and psychotherapeutic assistance. As a rule, 1-2 weeks of treatment in a hospital is enough to stop psychosis and normalize the patient's psycho-emotional state.
If there are contraindications to drug treatment (for example, if there is a risk of developing neuroleptic malignant syndrome) or drug resistance, the patient can undergo electroconvulsive therapy (ECT).
Psychotherapeutic treatment of catatonic schizophrenia
Psychotherapy is an important adjunct to the main (drug) treatment of catatonic schizophrenia.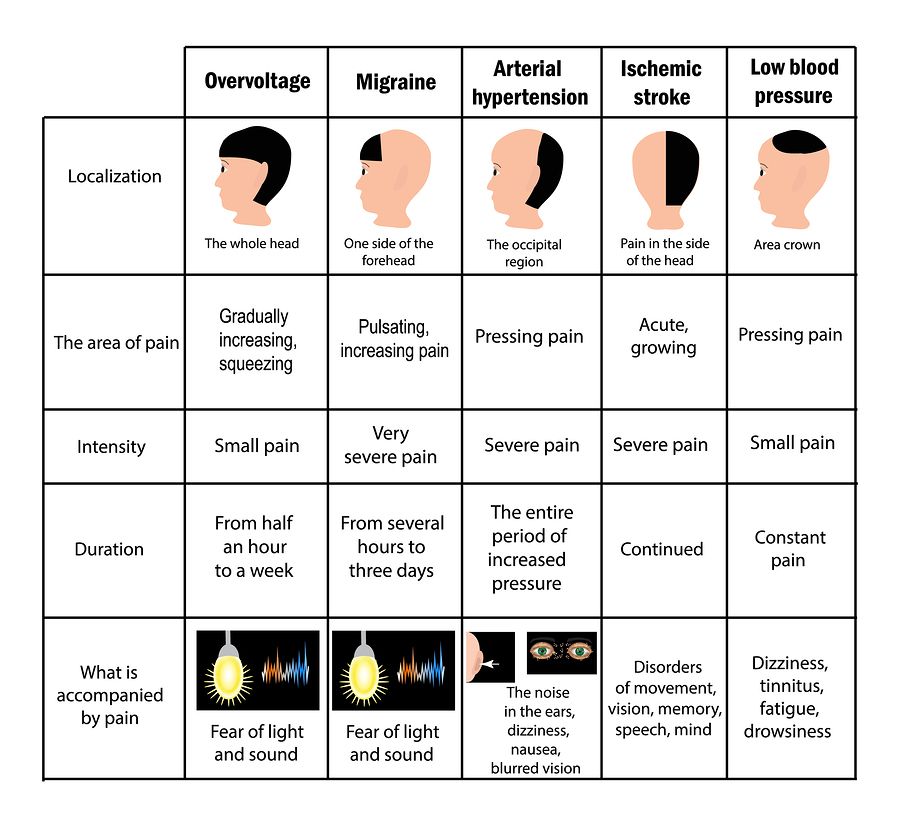 Often, against the background of the disease, such people develop fears, phobias and behaviors that complicate life. In the process of treatment, all our patients receive psychotherapeutic assistance in the form of group sessions under the guidance of clinical psychologists. If necessary, psychotherapeutic treatment can be continued after discharge.
Often, against the background of the disease, such people develop fears, phobias and behaviors that complicate life. In the process of treatment, all our patients receive psychotherapeutic assistance in the form of group sessions under the guidance of clinical psychologists. If necessary, psychotherapeutic treatment can be continued after discharge.
Patient management after discharge
Outpatient treatment of catatonic schizophrenia is necessary for the correction of pharmacotherapy, timely prevention of possible side effects and relapse of the disease. As a rule, in the first few months the patient visits the attending physician once every 2-3 weeks, and then once a month.
Treatment of catatonic schizophrenia in St. Petersburg is carried out at: st. Marata, 78. For patients from other cities, after completion of treatment in a hospital, there is the possibility of consultations with the attending physician via Skype.
Comorbidities of catatonic schizophrenia
Causes of catatonic schizophrenia
Sources
Catatonic schizophrenia - https://pubmed. ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
— https://www.webmd.com
Schizophrenia with prominent catatonic features: A selective review — https://pubmed.ncbi.nlm.nih.gov
Update date: 11/30/2022
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Tomorrow
April 18
Wednesday
April 19
Thursday
April 20
Friday
April 21
Saturday
April 22
Sunday
April 23
Monday
April 24
Tuesday
April 25
Wednesday
April 26
Thursday
April 27
Friday
April 28
Saturday
April 29
Sunday
April 30
Catatonic schizophrenia is being treated
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 42 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 42 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 23 years
Psychiatrist, psychotherapist, narcologist
Work experience 23 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Work experience 34 years
Psychiatrist, narcologist, psychotherapist
Work experience 34 years
Lisitsyna Elena Alekseevna
Psychiatrist
Top category
Work experience 34 years
Psychiatrist
Work experience 34 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb. branch
branch
Work experience 16 years
Psychiatrist
Work experience 16 years
Voronina Elvira
Vladimirovna
Psychiatrist
First category
Experience 28 years
Psychiatrist
Work experience 28 years
Gorobets Elena
Vasilievna
Psychiatrist
First category
Work experience 17 years
Psychiatrist
Work experience 17 years
Travnikova Oksana
Mikhailovna
Psychiatrist
First category
Work experience 22 years
Psychiatrist
Work experience 22 years
Kurochkina Nadezhda
Pavlovna
Psychiatrist
First category
Work experience 20 years
Psychiatrist
Experience 20 years
Suslennikova Elena
Viktorovna
Psychiatrist, psychotherapist
First category
Experience 26 years
Psychiatrist, psychotherapist
Work experience 26 years
Chuban Olga
Ivanovna
Psychiatrist, psychotherapist
First category
Work experience 14 years
Psychiatrist, psychotherapist, psychologist
Work experience 14 years
Popov Andrey
Petrovich
Psychiatrist
Top category
Experience 36 years
Psychiatrist
Work experience 36 years
Stetsiv Ludmila
Gennadievna
Psychiatrist, psychotherapist
PhD
Work experience 32 years
Psychiatrist, psychotherapist
Work experience 32 years
Prokhorchev Konstantin
Sergeevich
Psychiatrist, psychotherapist
First category
Work experience 13 years
Psychiatrist, psychotherapist
Work experience 13 years
Gulevsky Roman
Aleksandrovich
Psychiatrist, narcologist
Head of Hospital
Experience 26 years
Psychiatrist, narcologist
Work experience 26 years
Konoplin Dmitry
Alekseevich
Narcologist, psychiatrist
PhD
Work experience 25 years
Narcologist, psychiatrist
Work experience 25 years
Stavitskaya Svetlana
Yurievna
Psychiatrist
Top category
Work experience 25 years
Psychiatrist
Work experience 25 years
Pylskaya Anna
Nikolaevna
Psychiatrist
Second category
Work experience 8 years
Psychiatrist
Work experience 8 years
Trofimova Alexandra
Olegovna
Psychiatrist, child psychiatrist
First category
Experience 29 years
Psychiatrist, child psychiatrist
Work experience 29years
Zhelobetskaya Maria
Sergeevna
Psychiatrist, psychotherapist
Top category
Work experience 23 years
Psychiatrist, psychotherapist
Work experience 23 years
Endrzheevskaya Diana
Vadimovna
Psychiatrist, psychotherapist
Second category
Work experience 15 years
Psychiatrist, child psychiatrist, psychotherapist
Work experience 15 years
Usov Grigory
Mikhailovich
Psychiatrist, psychotherapist
MD
Work experience 25 years
Psychiatrist, psychotherapist
Work experience 25 years
Ivanov Alexander
Nikolaevich
Psychiatrist, narcologist
Top category
Work experience 21 years
Psychiatrist, narcologist
Work experience 21 years
Leave a request for a call:
+7 (812) 407-18-00
What is catatonia and why is it dangerous
November 7, 2020 Likbez Health
If a person falls into a stupor, speaks badly and adopts a strange posture, he urgently needs the help of a doctor.
What is catatonia
Catatonia, or catatonic syndrome, is a condition in which a person becomes immune to external stimuli and loses the ability to move and speak normally.
Until the beginning of the 20th century, it was believed that this only happens with schizophrenia. But then scientists found that more than 50% of cases of catatonia appear in bipolar disorder, about 10-15% are schizophrenia, and 21% are not associated with mental illness at all.
Catatonia is similar to mental disorders and other illnesses and is therefore difficult to recognize. For example, with it, as with a stroke, a person may respond with incomprehensible phrases or stop talking altogether. Urgent help is needed in both cases, but it will be different.
Catatonia may develop rapidly or gradually over several days. In the first case, the symptoms are usually strong and obvious; jumps in pressure or temperature are added to motor and speech disorders. This can lead, for example, to a stroke. In the second option, the symptoms are hardly noticeable, and this is the most dangerous: complications may appear in 3-4 days or the person will die.
In the second option, the symptoms are hardly noticeable, and this is the most dangerous: complications may appear in 3-4 days or the person will die.
Imagine a grandmother with dementia. She often sits on the edge of the bed and looks out the window. But suddenly she spends the whole day like this. Then the grandmother stops talking, reacting to others, but continues to sit. Then she refuses food, water.
The body is exhausted, and 2–3 days after the onset of the first symptoms, blood clots form in the legs from a long immobile posture. At some point, they come off and clog the vessel. The person is dying. But he would have been saved if the dangerous symptoms had been noticed on the first day.
Why catatonia occurs
Catatonia was first described in detail in 1874, but its causes have not yet been established. Scientists have several theories that roughly explain what changes in the body lead to the onset of catatonic symptoms.
Some researchers believe that the problem lies in the disruption of the transmission of nerve impulses in those areas of the brain that are responsible for muscle contractions. Others associate catatonia with a change in the balance of neurotransmitters - substances that are produced by brain neurons and are involved in the transmission of signals from cell to cell and many biochemical processes. Still others blame the excess or lack of certain hormones of the hypothalamus and pituitary gland, the production of antibodies to brain proteins.
Others associate catatonia with a change in the balance of neurotransmitters - substances that are produced by brain neurons and are involved in the transmission of signals from cell to cell and many biochemical processes. Still others blame the excess or lack of certain hormones of the hypothalamus and pituitary gland, the production of antibodies to brain proteins.
Such disturbances in the functioning of the body appear in many diseases:
- psychiatric, eg bipolar disorder, schizophrenia, autism, depression, anorexia nervosa;
- endocrine: Cushing's syndrome, hyperthyroidism, Sheehan's syndrome and others;
- neurological, eg epilepsy, multiple sclerosis, Parkinson's disease, brain tumors, dementia;
- metabolic - this is when the body accumulates substances that have a bad effect on the brain: this happens with Wilson's disease - Konovalov, an increase and decrease in the concentration of sodium in the blood, kidney failure and other diseases;
- autoimmune, eg systemic lupus erythematosus, antiphospholipid syndrome;
- caused by psychoactive substances: alcohol, antipsychotics, sedatives, drugs;
- infectious: HIV, typhoid fever, tuberculosis, meningoencephalitis, herpes and others;
- vascular, eg thrombosis of arteries and veins of the brain, stroke, cerebral hemorrhage.
What are the symptoms of catatonia
There are many signs of catatonia. The DSM-5, used by psychiatrists around the world, identifies 12 main ones. But doctors add other symptoms to them:
- Remaining immobile (stupor).
- Long-term maintenance of the posture that has been given to the body (catalepsy). If a person is planted or placed, he will not move.
- Prolonged silence (mutism). The person does not respond, even if you address him by name. On the contrary, he is likely to turn away.
- Changing the position of the limbs, like a plasticine figurine (wax flexibility). Some patients obey easily and can follow any command, like robots.
- Passive and strong resistance to any attempt to change the position of the arms and legs (negativism). Sometimes it is physically impossible to bend or straighten the limbs.
- Maintaining an uncomfortable posture (posing). For example, a person can arch on the bed without touching the pillow with his head, as if hanging in the air.

- Pretentiousness of movements (mannership). A catatonic person may gesticulate strangely and inappropriately.
- Repetitive monotonous movement (stereotype). Recall how in horror movies the possessed are constantly swaying, tapping their fingers, or moving their mouths terribly. Most likely, they have an attack of catatonia.
- Excessive excitement without external stimuli. A person can rush around the room, show aggression, rush at others.
- Involuntary movements of lips, eyebrows. Grimaces that are not built to amuse others.
- Repetition of other people's words (echolalia). Moreover, speech often becomes incoherent, monotonous, words and phrases are spoken continuously, sometimes for a very long time.
- Copying other people's movements (echopraxia).
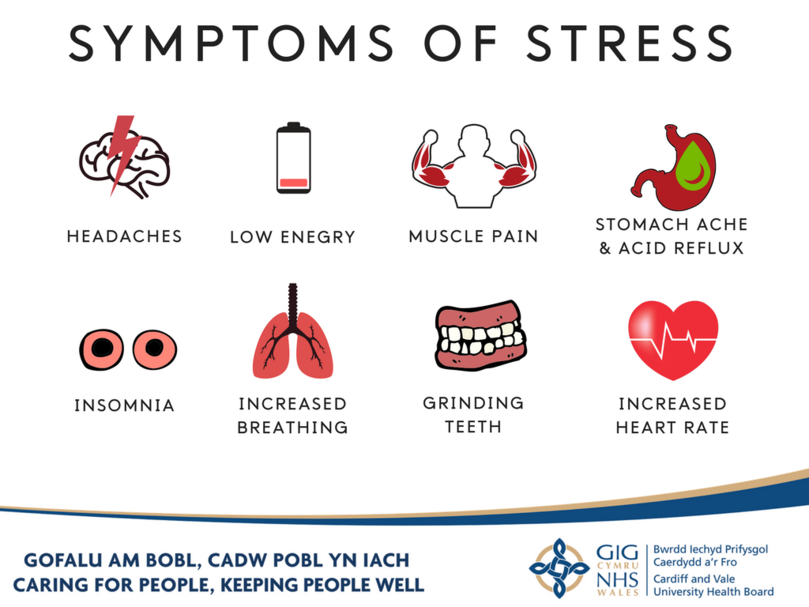
In addition, there may be symptoms associated with disruption of the autonomic nervous system. With catatonia, the temperature rises, thirst increases, saliva flows, blood pressure rises and the pulse quickens.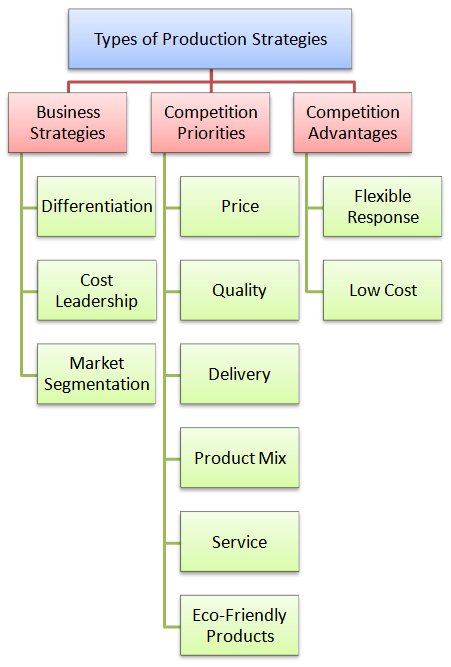 Often patients refuse water and food.
Often patients refuse water and food.
When a doctor makes a diagnosis, he looks for a combination of several signs. But medical attention is needed even with the appearance of one symptom. Otherwise, you can miss not only catatonia, but also a stroke, the debut of schizophrenia, a complication of meningitis or another disease.
How is catatonia treated? If the symptoms are mild, it is important to go to the therapist as soon as possible.
Based on the words of relatives or by analyzing the medical record, the doctor will determine whether there are mental illnesses, alcohol dependence or other pathologies that can cause catatonia. And if necessary, send to a psychiatrist.
He will prescribe medication or electroconvulsive therapy as soon as possible.
If there is no danger to the patient's life, examination will help to find the causes of catatonia:
- complete blood count;
- biochemical examination;
- blood electrolyte test;
- liver function tests;
- CT or MRI of the brain.
An electroencephalogram will be done if there is a suspicion of a brain tumor or seizures.
What medications are prescribed
The psychiatrist uses strong prescription medications to treat catatonia. Taking them on your own is dangerous.
First of all, drugs from the group of second-generation anxiolytics based on benzodiazepine are given. They reduce muscle spasm, soothe, help remove the symptoms of catatonia. Benzodiazepines are effective in 66-100% of patients.
If these drugs do not help, the treatment regimen is changed. Sometimes alternative drugs with sedative, anticonvulsant and muscle relaxant effects give the best effect. For example, lithium preparations will not allow a recurrence of an attack of catatonia.
Medicines from the group of neuroleptics are rarely prescribed: it is impossible to guess how the patient's body will react. On the one hand, drugs can remove muscle spasm. But at the same time, they can cause neuroleptic malignant syndrome. This is a condition when the temperature and pressure rise and the symptoms of catatonia intensify.
This is a condition when the temperature and pressure rise and the symptoms of catatonia intensify.
When electroconvulsive therapy is used
Electroconvulsive therapy is a treatment method in which an electric current is passed through the brain. It suppresses the foci that emit the wrong impulses and helps relieve muscle spasm and cramps.
Electroconvulsive therapy is used if benzodiazepines have failed or if the patient is at risk of death.
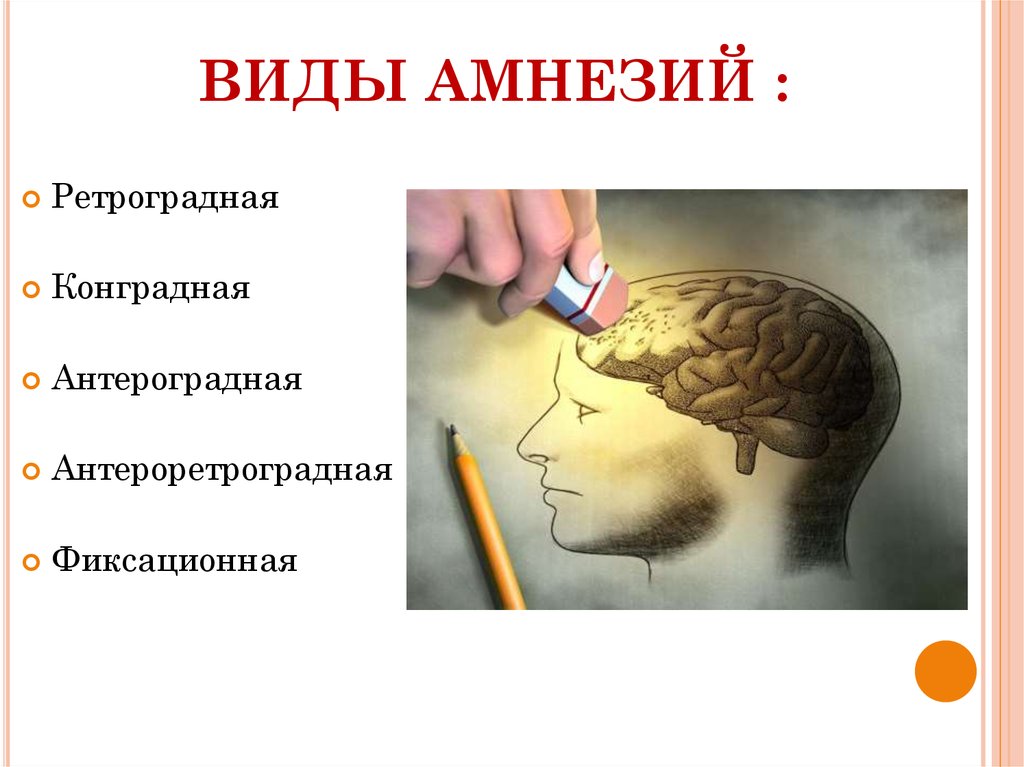
Catatonic attacks sometimes stop completely after electroconvulsive therapy. But there is a risk of side effects: headache, amnesia, confusion.
How successful is catatonia treated?
The sooner catatonia is treated, the better for the patient. Prompt help helps avoid complications and save lives.
But not everyone recovers. According to statistics, 12-40% of patients are successfully cured. Poor prognosis in children and adolescents with schizophrenia, as well as in the elderly. They may need ongoing psychiatric care.
If a person has been suffering from kidney failure, alcoholism, Parkinson's disease or other pathology for a long time, then the disturbances in the brain function are already chronic. Therefore, at any time, the catatonic syndrome can recur. In order not to be late with help, you need to remember the dangerous symptoms and follow the doctor's recommendations.
How not to get catatonic
Scientists have not yet learned how to prevent catatonia, like other mental illnesses or brain tumors. But, given the causes of the syndrome, we can advise the following:
- Reduce alcohol consumption and treat addiction symptoms.
- Never use drugs.
- Do not ignore symptoms of depression.
- Do not take hypnotics, sedatives, antipsychotics without a prescription from a specialist.
- Seek medical attention if headaches, dizziness, flies in the eyes.
- Treat kidney and liver diseases in time.
- Avoid casual sex to protect against HIV and syphilis.

Learn more