Triggers for bipolar disorder
9 Most Common Triggers for Bipolar Mood Episodes
Spats with your sweetheart, chilly weather, grief — a number of scenarios may provoke bipolar mania or depression.
By Madeline R. Vann, MPHMedically Reviewed by Kathryn Keegan, MD
Reviewed:
Medically Reviewed
Justin Case/Getty ImageBipolar disorder is characterized by symptoms including unusual shifts in mood and energy. These mood shifts or episodes last at least a week in the case of mania, and at least two weeks in the case of depression, according to psychiatrist Jeffrey Bennett, MD, an associate professor of psychiatry at the Southern Illinois University School of Medicine in Springfield.
There are several types of bipolar and related disorders. In order to be diagnosed with bipolar I, you must have had at least one manic episode that may have been preceded or followed by hypomanic or depressive episodes. In the case of bipolar II, you must have had at least one major depressive episode and at least one hypomanic episode, but never experienced a manic episode.
Both mania and hypomania share the same symptoms, which include feeling unusually upbeat, euphoric, or irritable, with increased energy, mood elevation, a decreased need for sleep, racing thoughts, trouble concentrating, and poor judgment. In cases of mania, these symptoms are severe enough to be causing significant problems in your day-to-day life.
For example, you might be unable to go to work or school, or you may be compulsively spending money. Hypomania is considered a less severe form of mania. In cases of hypomania, your daily functioning isn't significantly impacted. For example, you are able to work and socialize.
When mood shifts are severe enough, they can have a profound effect on your life. Some episodes of depression and mania are accompanied by loss of reality or psychosis, characterized by hallucinations or delusions. "And unfortunately, suicide is common, with some sources estimating it to be as high as 10 to 15 percent," explains Dr. Bennett.
Can these episodes be avoided? Perhaps not.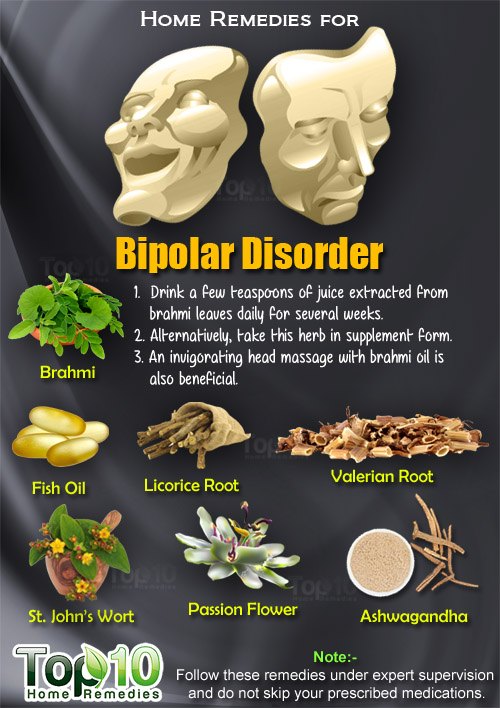 But understanding certain triggers can help you better manage bipolar disorder.
But understanding certain triggers can help you better manage bipolar disorder.
One of the most common bipolar triggers is stress. In a study published in June 2014 in the Journal of Affective Disorders, negative or stressful life events were associated with subsequent mood swings. Earlier in their course, episodes of depression or mania in bipolar disorder appear to be triggered more often by stressful life events.
In addition, with recurrent episodes, some people with bipolar disorder may experience less complete periods of remission and a greater likelihood of relapse, either to depression or mania, according to Bennett.
While causes of stress are highly individual, certain life events and lifestyle patterns may act as triggers. Watch out for these common culprits.
Changes in Sleep Patterns or Lack of Sleep
Getty ImagesA change in your sleep pattern is a hallmark symptom of bipolar disorder — but it can also be a trigger.
Shift workers, people who work long hours, and students who are short on sleep are all at risk for having a recurrence of a mood episode related to a lack of sleep. "In addition, travel beyond one's time zone can be another trigger for a mood episode," says Bennett.
"In addition, travel beyond one's time zone can be another trigger for a mood episode," says Bennett.
Interpersonal and social rhythms therapy (IPSRT) is one of the most effective preventions, Bennett says. This treatment approach, available in group as well as individual sessions, helps you develop an orderly life schedule of sleep, diet, and exercise habits, to make you more effective at managing bipolar disorder.
Other forms of therapy, including psychoeducation and cognitive-behavioral therapy (CBT), can also be helpful in managing the illness.
Blowout Arguments With Partners, Coworkers, or Friends
Paul Simcock/Getty ImagesBroken relationships are too often the result of untreated bipolar disorder.
But getting into a spat with a loved one could also be a red flag: Your argument could be due to the irritability that often occurs during a manic or depressive episode, or could itself cause stress that becomes a contributing factor for a recurrent episode.![]()
Any type of relationship conflict — whether it’s with your partner, coworker, family member, or friend — can trigger stress and send you over the edge. In a study published in May 2015 in the Journal of Affective Disorders, people with bipolar disorder said negative social experiences were among the events that triggered suicidal thinking for them.
The Stress of a Bad Breakup or Failed Marriage
Getty ImagesA number of people with bipolar disorder — especially those with a history of severe manic episodes — have failed marriages. If you’re going through a divorce, working with your therapist through what is often a drawn-out and extremely stressful process can help.
You might consider a durable power of attorney that allows someone else to make major decisions for you, such as financial ones, when you are going through an episode of depression or mania in relation to or during a breakup.
In fact, assigning a durable power of attorney could be useful for anyone who might be experiencing an episode of bipolar disorder.
Alcohol Abuse and Drug Intoxication, and the Aftereffects
Ivan Kmit/AlamyAbusing drugs and alcohol doesn’t cause bipolar disorder, but it can cause an episode to suddenly occur, or it can worsen the underlying illness. What’s more, about one in five people with bipolar disorder have a substance abuse disorder, according to an analysis of data on young adults with mental illness from an article published in February 2015 in the journal Social Psychiatry and Psychiatric Epidemiology.
Intoxication with drugs such as cocaine and amphetamines can cause or worsen manic symptoms, while the aftereffects of cocaine or use of alcohol are associated with worsening of depressive symptoms.
Antidepressants, Corticosteroids, and Other Medication
Jeff Wasserman/StocksyCan antidepressants make you manic?
The treatment of bipolar disorder can trigger episodes of mania by further setting off unstable moods and behaviors. Many psychiatrists say they've seen patients enter a manic phase after starting antidepressants — and some feel uncomfortable prescribing them to bipolar patients.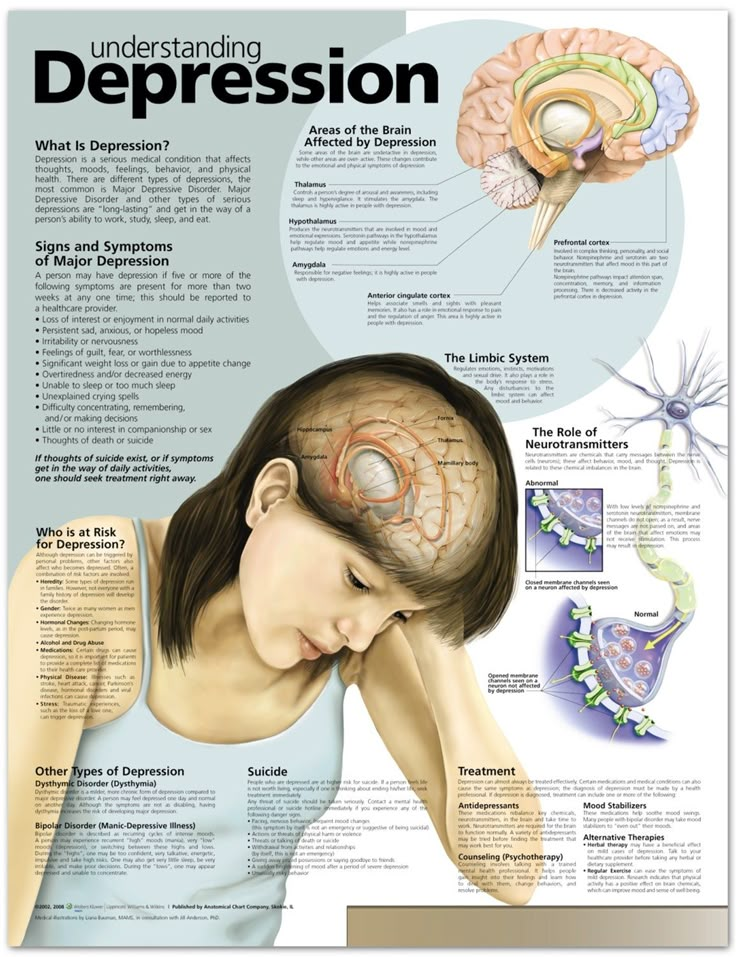
What should you do about bipolar depression? Until more research is available on long-term safety, Keming Gao, MD, PhD, a professor of psychiatry at Case Western Reserve School of Medicine in Cleveland, suggests the following: For bipolar I depression, antidepressants should only be used with a mood stabilizer or stabilizers after symptoms haven't responded to FDA-approved treatment options (such as mood stabilizers).
Dr. Gao says that while some recent studies suggest that using an antidepressant alone is as effective as lithium taken alone for some bipolar II patients (those who haven't experienced a manic episode), they should never be used alone for bipolar I depression, and patients and doctors should consider discontinuing use of antidepressants once symptoms have responded.
Other drugs that have been linked to manic symptoms include corticosteroids, thyroid medication, and appetite suppressants.
A Brand-New Season and Abnormal 'Clock Genes'
Noelia Ramon/Getty ImagesAbout 20 percent of people with bipolar disorder experience fluctuations in mood when the weather changes.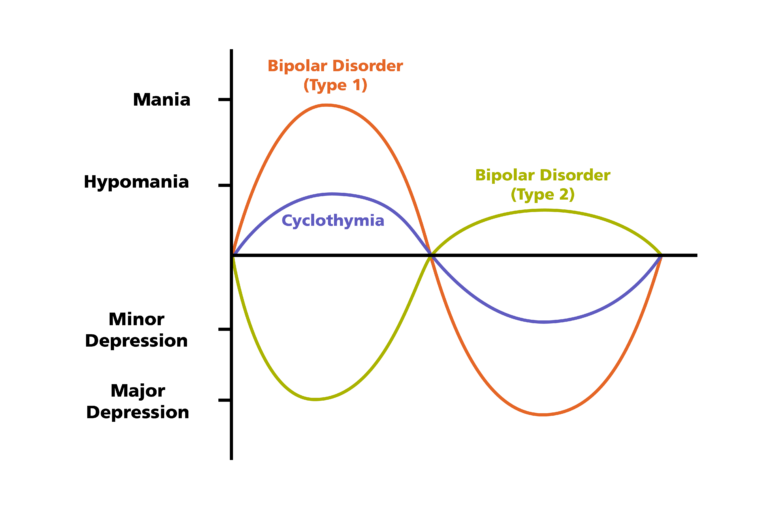 Specifically, they're more likely to undergo seasonal depression during the early winter, and mania or hypomania during the spring or summer, according to a research review published in October 2014 in the Journal of Affective Disorders.
Specifically, they're more likely to undergo seasonal depression during the early winter, and mania or hypomania during the spring or summer, according to a research review published in October 2014 in the Journal of Affective Disorders.
Experts chalk this up to sunlight: Your circadian rhythm, the body’s internal response to changes in a 24-hour day, is affected by the amount of sunlight you experience. This response is controlled by a complex set of genes commonly referred to as “clock genes.” If some of these genes are abnormal, you could be at risk for seasonal bipolar disorder.
A Visit From the Stork Along With Altered Sleep Patterns and Shifting Hormones
Catherine Delahaye/Getty ImagesThe American College of Obstetrics and Gynecology estimates that women with bipolar disorder have up to a 67 percent chance of experiencing an episode of bipolar disorder in the postpartum period — the weeks and months after birth.
Changing sleep patterns, altered medication prescriptions, and shifting hormones after delivery can combine to serve as risk factors for a postpartum mood or psychotic episode, according to research published in November 2014 in the journal The Lancet.
Use the nine months of pregnancy to work with your entire medical team — your bipolar disorder specialists and your ob-gyn — on treatment approaches you can try during and after pregnancy to help prevent postpartum depression, postpartum mania, or postpartum psychosis.
Bipolar disorder is also strongly associated with postpartum psychosis, a severe mental illness characterized by an inability to respond emotionally to one's newborn, or thoughts of harming one's baby.
Financial and Emotional Strains Due to a Job Loss
Audtakorn Sutarmjam/AlamyOne of life’s most unpredictable stressors? Losing your job.
And the emotions you may feel about your job loss can be equally unpredictable. People who weren’t satisfied with their work can find it liberating. For others, the financial and emotional strains involved can trigger major stress. Either way, the dramatic shift in emotions could trigger a bipolar episode.
It may be a good idea to put away three to six months of savings to help with the transition, should you lose your job.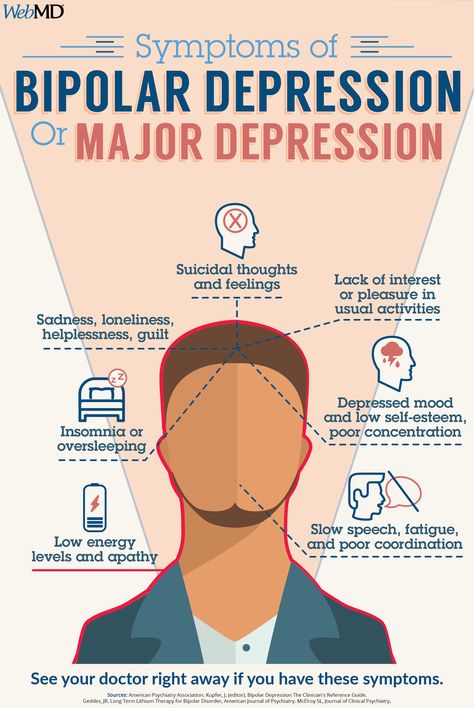
The Death of a Loved One and Bereavement
Getty ImagesThe death of a loved one may be the most stressful life event any of us will ever face. Many people continue managing bipolar disorder successfully through their mourning, but it may have extreme consequences for others, who can develop “funeral mania,” says Bennett.
This occurs when someone with controlled bipolar disorder attends the funeral of the loved one and has a manic episode over the course of the following week. The period of bereavement should be one of increased monitoring and heightened support, advises Bennett.
Prevention of a bipolar mood episodes may not be possible, but understanding triggers may help you better manage your illness.
Bipolar Episode Triggers | Everyday Health
Bipolar disorder is a mental health condition that affects millions of people in the United States. According to the National Institute of Mental Health (NIMH), an estimated 4.4 percent of American adults experience bipolar disorder at some point.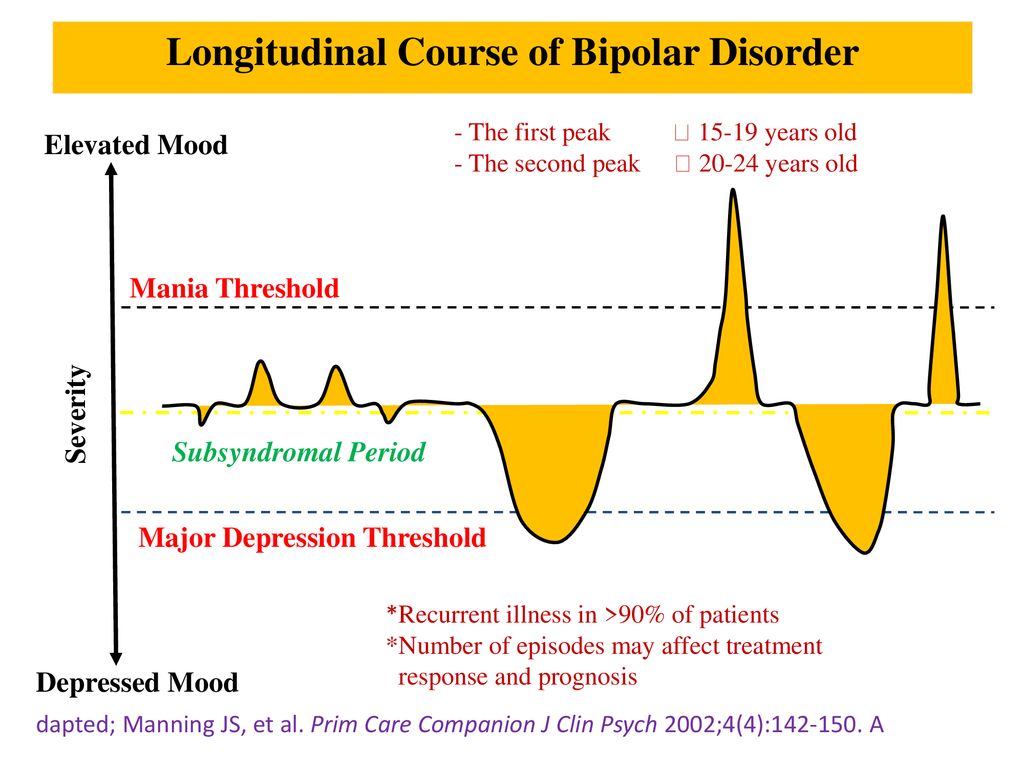 The disorder, which can cause extreme shifts in mood, energy, activity levels, and the ability to think clearly, can affect individuals differently, and the severity and types of symptoms can vary from one person to another.
The disorder, which can cause extreme shifts in mood, energy, activity levels, and the ability to think clearly, can affect individuals differently, and the severity and types of symptoms can vary from one person to another.
Although the exact cause of bipolar disorder is unknown, it is thought that several factors, such as genes, brain structure, and stress response and management, could play a role in how often symptoms occur, how severe they become, and how long they last, according to the National Alliance on Mental Illness (NAMI). Certain lifestyle and environmental factors can also trigger or aggravate the extreme highs and lows, known as bipolar episodes, which are a hallmark of the condition. Once you’re aware of these triggers, you can gain better control over your disorder.
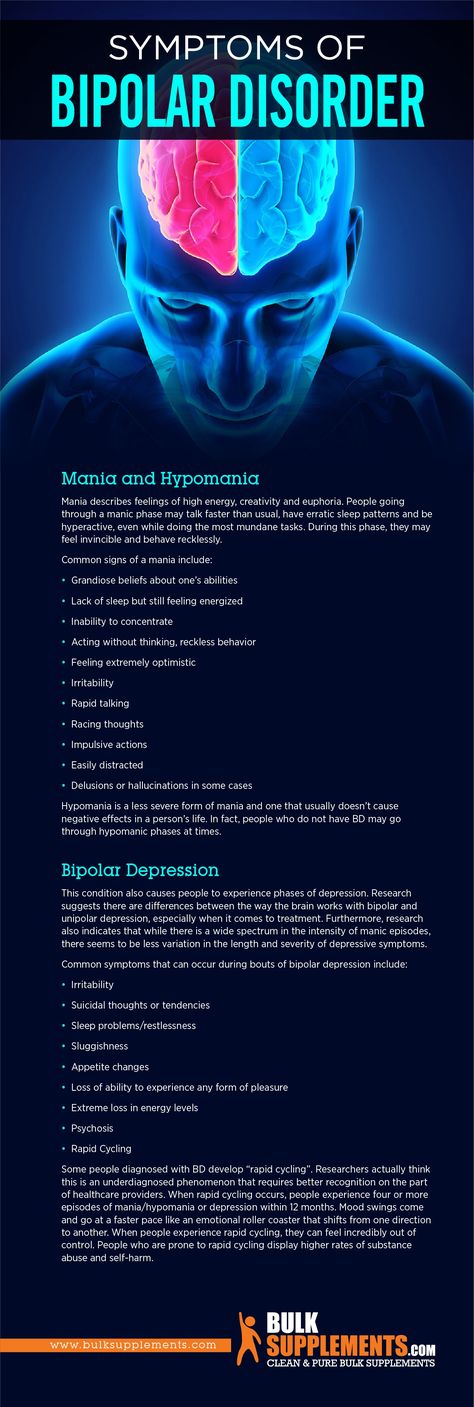
Types of Bipolar EpisodesThe main difference between bipolar disorder and conditions such as depression is the possibility of experiencing the overly excited state called mania, says Amit Anand, MD, a professor of medicine at the Lerner College of Medicine, vice-chair for research for the Center for Behavioral Health, and the director of the Mood and Emotional Disorders Across the Life Span program, all at the Cleveland Clinic in Ohio. People who are manic are unusually outgoing or happy. In some cases, mania also causes intense irritability and restlessness. During depressive episodes, intense sadness or hopelessness may lead to fatigue, trouble concentrating, and thoughts of suicide.
People who are manic are unusually outgoing or happy. In some cases, mania also causes intense irritability and restlessness. During depressive episodes, intense sadness or hopelessness may lead to fatigue, trouble concentrating, and thoughts of suicide.
But bipolar mood swings are not always extreme, Dr. Anand notes. For instance, some people experience a less severe form of mania, known as hypomania. Those who are hypomanic may not feel anything is wrong, making diagnosis more difficult, he adds.
Complicating matters is that it’s possible to experience both mania and depression at the same time, known as mixed features. When this happens, you may feel overly energized yet be extremely irritated, sad, hopeless, or empty.
Understanding and Managing Bipolar TriggersBipolar episodes can be triggered by lifestyle and environmental factors. Recognizing your triggers and avoiding them, Anand says, is often key to managing the condition.
Factors that may worsen bipolar symptoms or trigger an episode include:
- Stress In many cases, a major life change or stressful event, such as losing a loved one or having financial troubles, can trigger an initial episode.
 How you cope with stress can also affect how your bipolar disorder progresses. According to a meta-analysis published in January 2017 in the Journal of Affective Disorders, people with bipolar disorder having a relapse of their condition reported experiencing more stressful life events compared with those who were in a more stable mood phase. The researchers concluded that individuals with bipolar disorder tend to be more “sensitive” to stressors, suggesting that psychosocial treatments are an important component of successfully managing your condition. (Psychosocial treatments include psychotherapy, support groups, and education on the disease for loved ones so they can assist with coping strategies and spot the signs of relapse, according to NAMI.)
How you cope with stress can also affect how your bipolar disorder progresses. According to a meta-analysis published in January 2017 in the Journal of Affective Disorders, people with bipolar disorder having a relapse of their condition reported experiencing more stressful life events compared with those who were in a more stable mood phase. The researchers concluded that individuals with bipolar disorder tend to be more “sensitive” to stressors, suggesting that psychosocial treatments are an important component of successfully managing your condition. (Psychosocial treatments include psychotherapy, support groups, and education on the disease for loved ones so they can assist with coping strategies and spot the signs of relapse, according to NAMI.) - Childbirth The link between childbirth and bipolar disorder has been well documented in a number of scientific studies. A systematic review of nine papers published in October 2016 in the journal BMC Pregnancy and Childbirth found that the risk for mood disorder episodes increases during pregnancy in the postpartum period in women with bipolar disorder.
 In one of the studies included in the review, researchers found that nearly 50 percent of women with bipolar disorder experienced at least one mood episode during pregnancy or within 12 months after childbirth. It’s also worth noting that both men and women with bipolar disorder may be triggered by childbirth. While there is very limited research examining the effect of a new baby on fathers, a study published in May–June 2017 in American Journal of Lifestyle Medicine found that available evidence suggests fathers with bipolar disorder may have an increased risk of hypomanic episodes after the child is born.
In one of the studies included in the review, researchers found that nearly 50 percent of women with bipolar disorder experienced at least one mood episode during pregnancy or within 12 months after childbirth. It’s also worth noting that both men and women with bipolar disorder may be triggered by childbirth. While there is very limited research examining the effect of a new baby on fathers, a study published in May–June 2017 in American Journal of Lifestyle Medicine found that available evidence suggests fathers with bipolar disorder may have an increased risk of hypomanic episodes after the child is born. - Medication Treatment for bipolar disorder includes medications, such as mood stabilizers, antipsychotics, and antidepressants, according to NAMI. Interestingly, some antidepressants, such as Prozac (fluoxetine) and Zoloft (sertraline), may worsen bipolar symptoms and possibly even trigger a manic episode, Anand says, adding that if you have bipolar disorder, you should not take an antidepressant without also taking a mood stabilizer or antipsychoticmedication.
 Stimulants used to treat attention deficit hyperactivity disorder (ADHD) may also trigger a manic episode. If you have more than one condition (such as obsessive-compulsive disorder or ADHD) that is treated with medication, NAMI recommends that you develop a treatment plan with your doctor to best manage both conditions and monitor your side effects.
Stimulants used to treat attention deficit hyperactivity disorder (ADHD) may also trigger a manic episode. If you have more than one condition (such as obsessive-compulsive disorder or ADHD) that is treated with medication, NAMI recommends that you develop a treatment plan with your doctor to best manage both conditions and monitor your side effects. - Seasonal changes For some people with bipolar disorder, there’s a seasonal pattern to mood episodes. Anand says there’s some evidence that more manias occur during the spring and summer months, while more episodes of depression take place in the fall and winter. But some people experience the opposite. According to an Austrian study published in January 2019 in the Journal of Affective Disorders, which examined data on over 60,000 people who were admitted to a hospital for a manic, depressive, or mixed featured episode between 2001 and 2014, seasonal patterns in hospitalization rates during manic episodes were found for both men and women.
 (Women were more likely to experience manic episodes in summer and autumn, depressive episodes in winter, and mixed features in summer, whereas men were more likely to experience manic episodes in summer.) Women under age 35 were also more likely to have this seasonal pattern in manic and mixed episodes. There may be a seasonal pattern to your shifts in mood because of changes in sleep, intensity of sunshine, and number of daylight hours, as well as changes in melatonin levels. Closely monitoring your symptoms during seasonal changes can help you manage your bipolar disorder.
(Women were more likely to experience manic episodes in summer and autumn, depressive episodes in winter, and mixed features in summer, whereas men were more likely to experience manic episodes in summer.) Women under age 35 were also more likely to have this seasonal pattern in manic and mixed episodes. There may be a seasonal pattern to your shifts in mood because of changes in sleep, intensity of sunshine, and number of daylight hours, as well as changes in melatonin levels. Closely monitoring your symptoms during seasonal changes can help you manage your bipolar disorder. - Poor sleep Lack of sleep is a frequent trigger of bipolar mood episodes, according to Anand. Poor sleep or a disruption in normal sleeping patterns, including jet lag, can trigger these intense mood swings. But there is evidence that psychological treatment may help. In a study published in June 2015 in the Journal of Consulting and Clinical Psychology, researchers treated half of the 58 study participants who had bipolar disorder and insomnia with a bipolar-specific modified form of cognitive behavior therapy that involved incorporating good sleep habits, relaxation, and dim lights at bedtime and reducing anxiety about sleep into daily routines.
 The other half of the study participants were given information about how sleep, stress, diet, exercise, and mood are related to each other but no plan or intervention designed to change behavior. The results were eye opening: Six months after these interventions, the people who received cognitive behavior therapy had experienced just 3.3 days in a bipolar episode compared with the 25.5 days experienced by those who were given only education materials. The cognitive behavior therapy group also had a lower rate of relapse and less severe insomnia. These results show that it may be beneficial for you to ask your doctor for a plan to ensure you’re getting enough quality sleep if you have bipolar disorder.
The other half of the study participants were given information about how sleep, stress, diet, exercise, and mood are related to each other but no plan or intervention designed to change behavior. The results were eye opening: Six months after these interventions, the people who received cognitive behavior therapy had experienced just 3.3 days in a bipolar episode compared with the 25.5 days experienced by those who were given only education materials. The cognitive behavior therapy group also had a lower rate of relapse and less severe insomnia. These results show that it may be beneficial for you to ask your doctor for a plan to ensure you’re getting enough quality sleep if you have bipolar disorder. - Drug and alcohol use According to NAMI, substance abuse is common among people with mental illness as a way to cope with their symptoms. In fact, 30 to 50 percent of people with bipolar disorder will develop a substance abuse disorder, notes the Substance Abuse and Mental Health Services Administration (SAMHSA).
 Anand cautions against using drugs or alcohol to “treat” symptoms of the condition. Drinking or taking drugs, he says, can worsen your bipolar mood swings and lead to an increase in suicidal thoughts or behaviors. As SAMHSA notes, substance use or withdrawal can cause symptoms attributed to bipolar disorder, including agitation, anxiety, and paranoia. Drinking alcohol in particular can make you less likely to respond to treatment and more likely to be hospitalized. Try medication and psychosocial therapy instead.
Anand cautions against using drugs or alcohol to “treat” symptoms of the condition. Drinking or taking drugs, he says, can worsen your bipolar mood swings and lead to an increase in suicidal thoughts or behaviors. As SAMHSA notes, substance use or withdrawal can cause symptoms attributed to bipolar disorder, including agitation, anxiety, and paranoia. Drinking alcohol in particular can make you less likely to respond to treatment and more likely to be hospitalized. Try medication and psychosocial therapy instead. - Caffeine Caffeine is a stimulant. As such, it may trigger manic episodes, change sleeping patterns, and affect the way your body breaks down the medications you take to treat your condition, according to a review published in September 2020 in the journal Bipolar Disorders. Talk to your doctor about your caffeine consumption and how it may affect your symptoms.
While these culprits can lead to a bipolar episode, it’s also important to keep in mind that episodes can occur even without a trigger.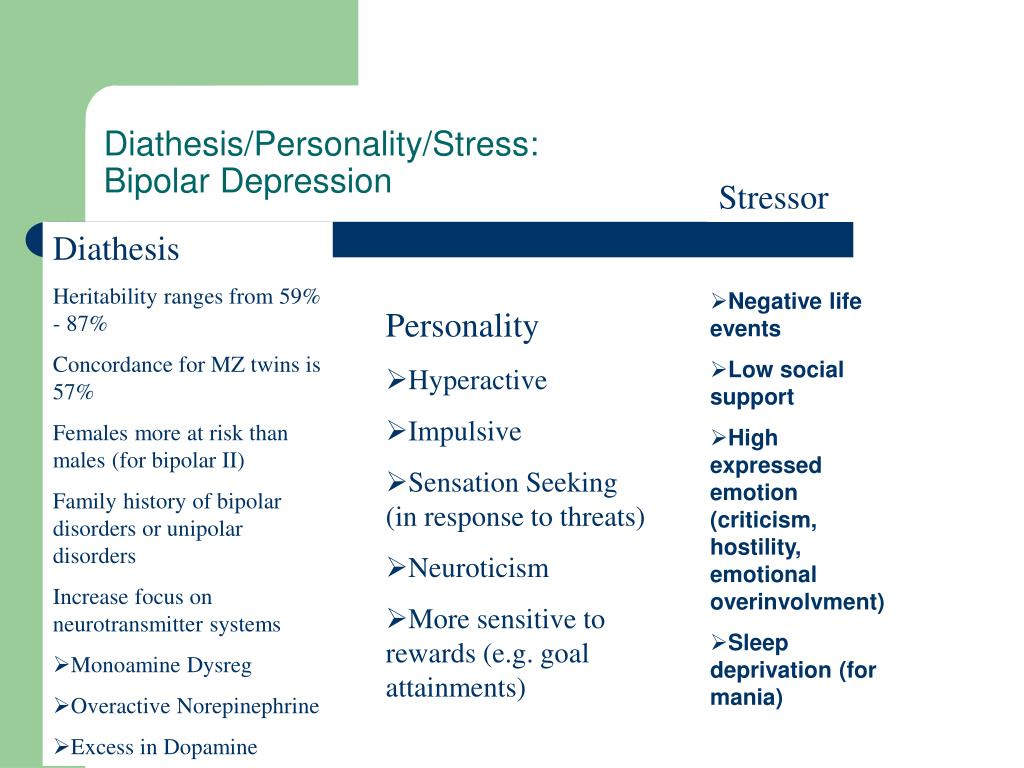 “Bipolar episodes can come out of the blue,” Anand notes. Do what you can to manage your stress, get good sleep, and avoid using alcohol or any other substance, and work with your doctor to find the best strategies for you to manage your bipolar disorder.
“Bipolar episodes can come out of the blue,” Anand notes. Do what you can to manage your stress, get good sleep, and avoid using alcohol or any other substance, and work with your doctor to find the best strategies for you to manage your bipolar disorder.
Additional Reporting by Jessica Migala
Triggers and Early Signs of Mania and Depression
Contents
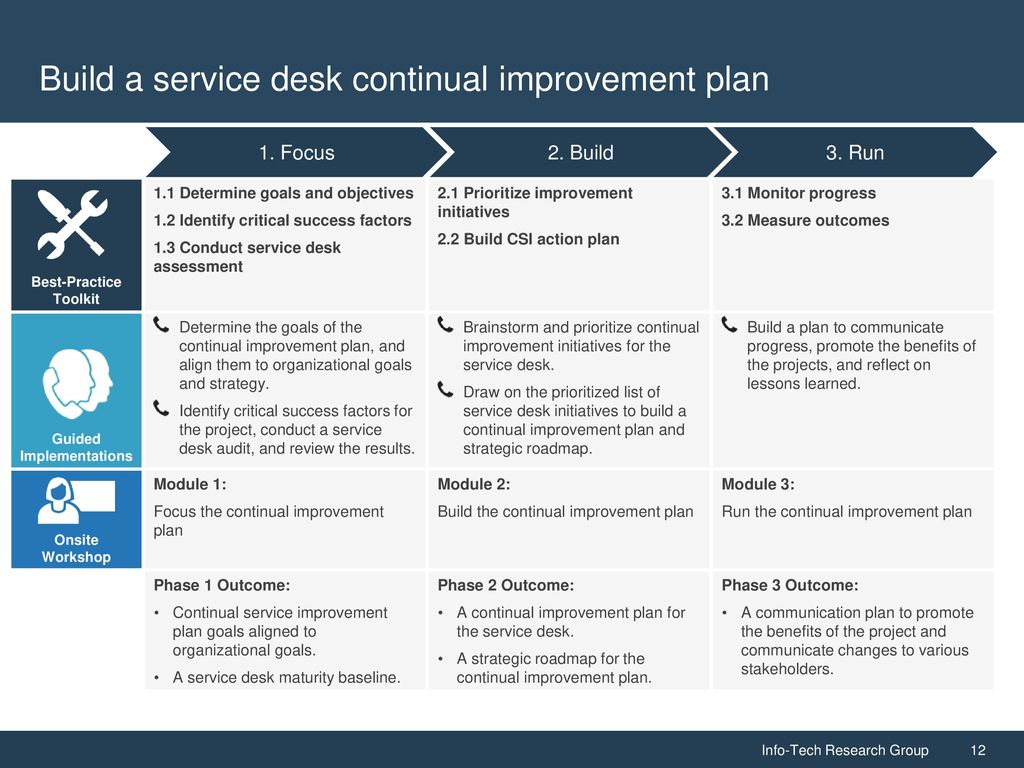
Introduction: Bipolar Toolkit
Chapter 1. Graph and Mood Charts
Chapter 2.1. Your Wellness Plan
Chapter 2.2. Triggers and Early Signs of Depression and Mania
Chapter 3 Treatment Agreement
Common Triggers of Depression
- Alcohol or Drugs
- Change of Seasons
- Relationship breakdown
- Job loss
- Another negative life event
- Conflicts with others
- Stopping medication
- Lack of physical activity
- Unhealthy diet. In particular, lack of vitamin B and folic acid, or consumption of large amounts of sweets
- Social isolation
- Negative way of thinking: self-criticism, self-blame
- Physical illness.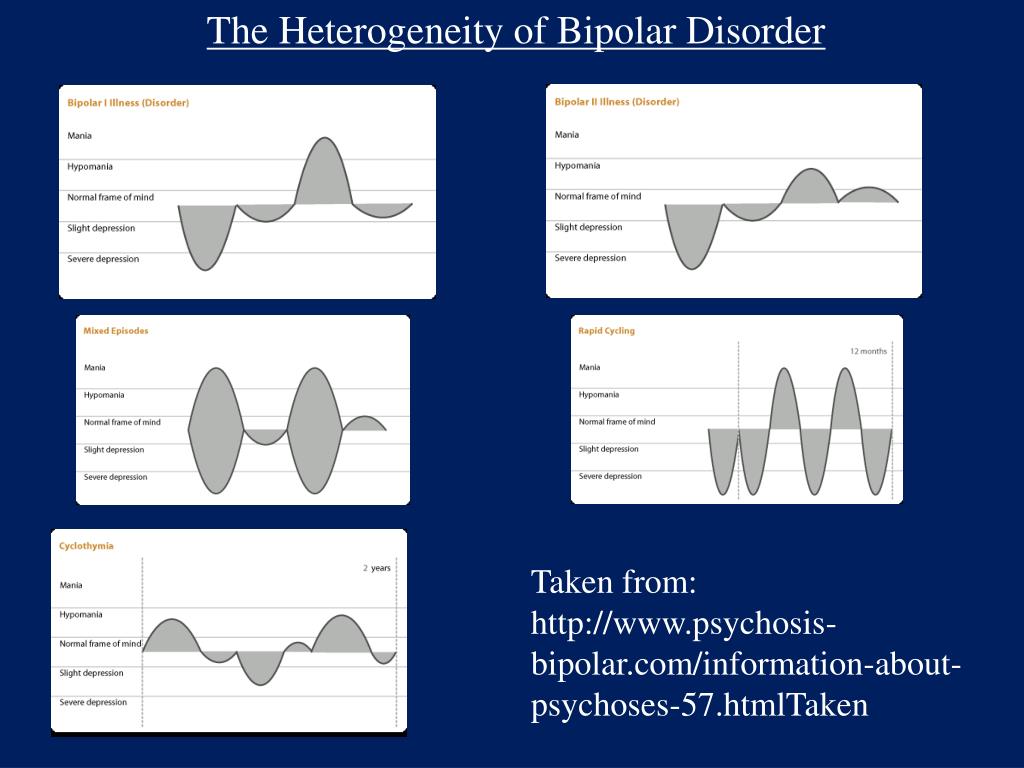 It can be a severe and long-term illness, chronic pain, but it can also be a common flu
It can be a severe and long-term illness, chronic pain, but it can also be a common flu
- provocation of depressive mood with sad and difficult books, music, communication with negatively configured people
- Mental Stygma Pressure
- Nightsmares, heavy dreams
Typical triggers of mania
- lack of sleep
- change of seasons - change of seasons - change of season
- Alcohol, drugs
- Stimulant drugs, such as antidepressants
- Some traditional treatments, such as St. John's wort
- Stress at school or work
- Money problems
- Travel, especially jet lag mood
- Starting or stopping smoking
- Breaking up a relationship
- Gambling activities, such as online games, internet chats, cards, stock trading
- Some hormonal diseases, in particular diabetes, thyroid disease
- Unsuitable diet, especially excess sweets, caffeine.
Early signs of mania and hypomania
- the need for a dream of
is reduced - more thoughts and ideas
- the well -being of energy
- increased irritability
- Exacerbation: Colors seem brightly, music more expressive
- Increased sexual arousal
- Change in sexual behavior. People who were not noticed before begin to seem attractive, interest in types of sex that are unusual for you
People who were not noticed before begin to seem attractive, interest in types of sex that are unusual for you
- Desire to take risks
- Feeling invulnerable, endowed with special powers and abilities
- Impatience, inability to wait, annoyance at the "slowness" of others
- Jumping from thought to thought
- Feeling of love
-
to everyone around, but exactly as long as they do not start to object to you- Unusual sociability, desire to talk with random people you meet
- Talkativeness
- Impulse buying
- Interest in risky financial affairs, questionable investments
- Paranoid thoughts, feeling that people are discussing, criticizing, persecuting you affairs, ambitious projects
Early signs of depression
- Avoiding people, not wanting to go to meetings
- You quit the things you normally do: exercising, walking the dog, going to church, reading books, dating, playing games with children
- You don't leave the house, even if you have something important to do: go to the store, the post office, the bank .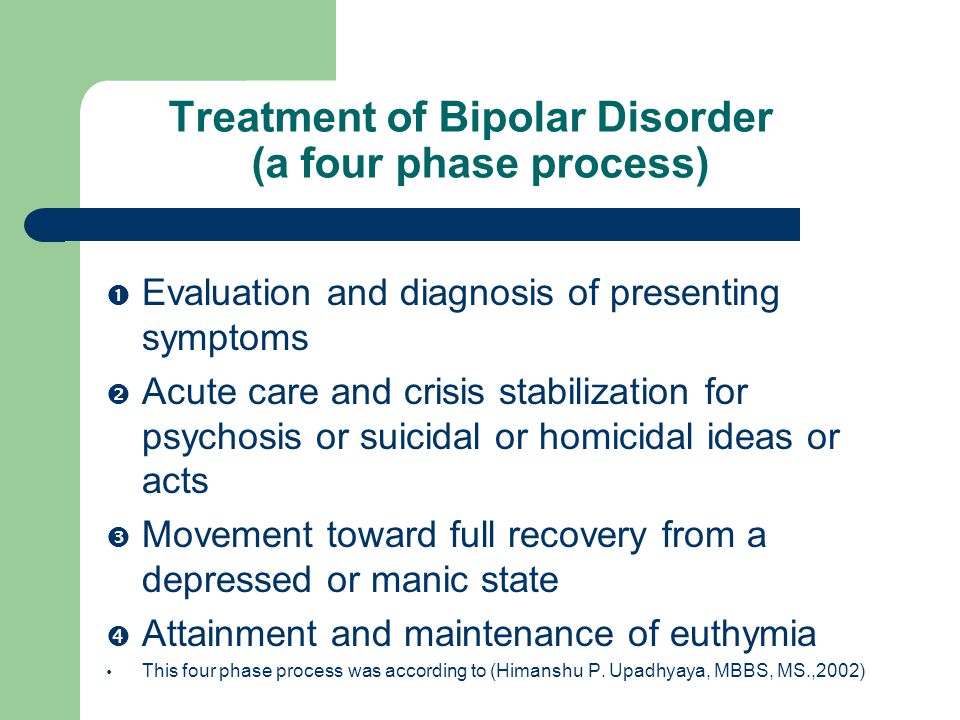 You have difficulty falling asleep, you sleep longer, you want to sleep during the day
You have difficulty falling asleep, you sleep longer, you want to sleep during the day
- Changing your diet. You don't want to eat, or you eat more than usual, especially "junk food"
- Stop paying attention to your appearance, hygiene.
– Self-care seems harder
- you feel hopelessly
- you are sad, you are suppressed by
,- you feel guilty
,- you lose interest in sex
,- become irritable
- feel anxiety
- insensibility
- lack of motivation 9000,
- loss of interest to the environment
- Things you used to like no longer bring you joy
- Thinking is slow and difficult
- You find it difficult to concentrate
- You are critical of yourself, you blame yourself
- You find it difficult to make decisions
- You have many anxious thoughts
- Obsessive thoughts
- Thoughts of self-harm
- Negative thoughts about others, about your future
Health Strategies
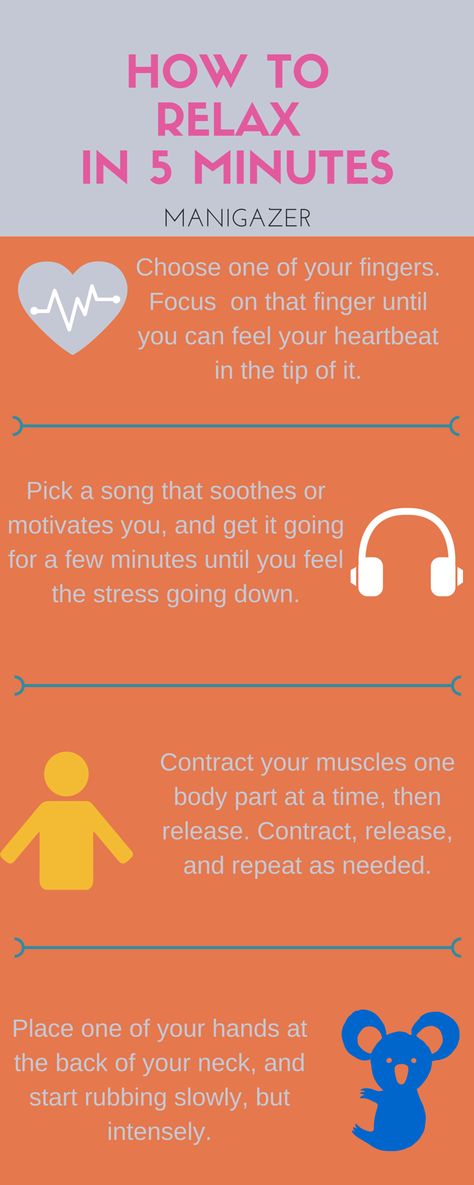
- Regular adequate sleep
- Selection of suitable medications
- Psychotherapy in addition to drugs
- Regular consultations with a psychiatrist
- At the first signs of an episode, immediately make an appointment with a doctor, strictly follow the doctor's recommendations that have already caused you seizures in the past
- Stable daily routine
- Regular and good quality meals.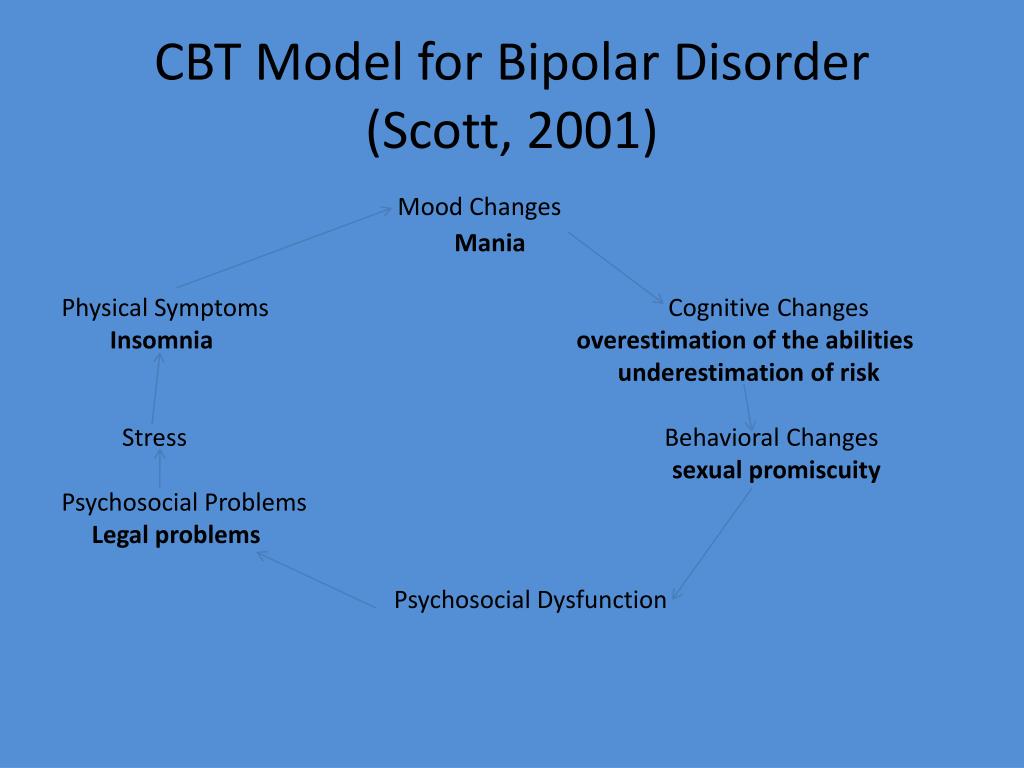
Important: enough protein, minimum of simple carbohydrates and animal fat, enough omega-3 acids (fish oil), vitamin B12, folic acid
Daily exercise that brings you pleasure
Avoid overstimulation, overly stimulating environments
Maintain health, treat co-morbidities such as thyroid disease and diabetes
Learn and use healthy thinking techniques: reality testing, self-support.
Sample Recovery Plan
| Trigger | Early Signs | Wellness Strategy |
| Time Zone Change | Use sleeping pills to help you fall asleep on time. Use additional mood stabilizers. | |
| Sleep interruption | Difficulty falling asleep | Use sleeping pills until sleep is restored. More exercise. |
| Stress due to work, problems in personal life, money | Increased irritability, paranoid thoughts, tendency to argue and conflict0239 | More physical activity.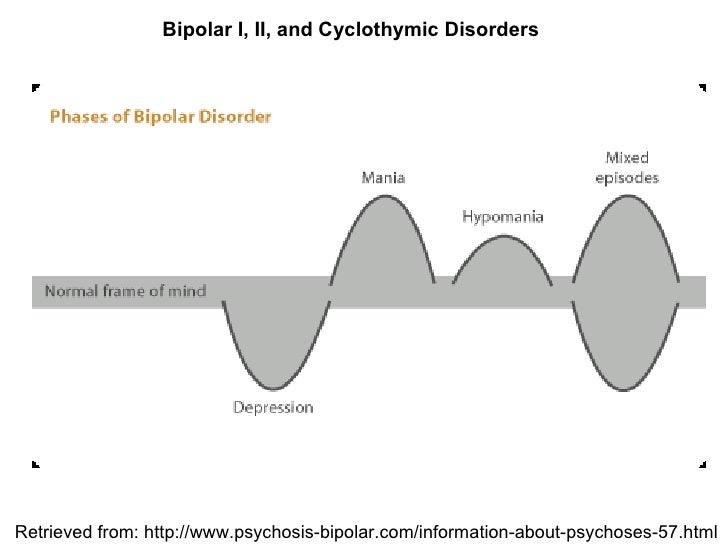 Proper diet. With the help of a loved one, take a "reality test". |
| Stress due to work, personal life, money | Impulsive, extravagant purchases | Entrust the purchases to your spouse. Avoid online shopping, do not carry credit cards with you. |
Read more Treatment agreement or crisis plan
Summary
Causes, triggers, and factors for bipolar disorder
Analyzing the data of various researchers studying the causes of the development of bipolar affective disorders, both in the framework of traditional medicine and in an alternative, holistic approach, we can identify 20 main factors that contribute to the onset, or provoke and exacerbate the course of the disorder.
Genetic predisposition
both parents. However, according to studies among identical twins, one of whom is diagnosed with bipolar disorder, the second twin also suffers from this disorder in only 65% of cases.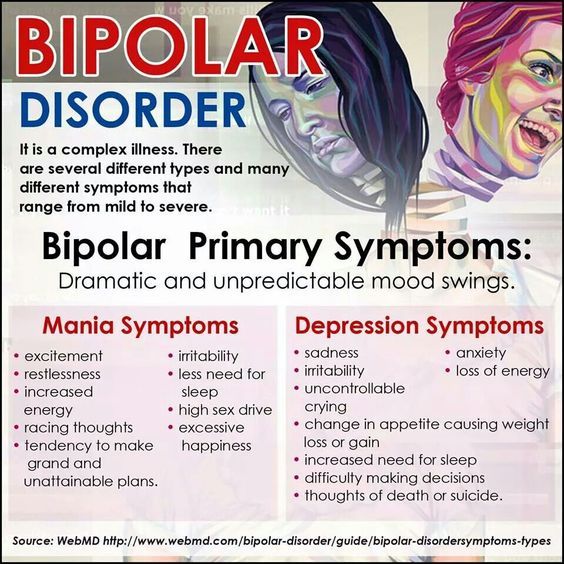 These data convincingly indicate the presence of not only the genetic nature of the occurrence of BAD, but also the significant role of other, "environmental" factors that are not related to the gene program.
These data convincingly indicate the presence of not only the genetic nature of the occurrence of BAD, but also the significant role of other, "environmental" factors that are not related to the gene program.
Stress
Stress, in fact, is a necessary addition to the genetic predisposition to trigger the mechanisms that lead to the development of bipolar disorder. All subsequent factors can be characterized as stress factors leading to a chronic stress state. A manic or depressive episode during the manifestation of bipolar disorder, or the subsequent course, is very often preceded by stressful situations, leading at the physical level to a decrease in immunity and a decrease in the content of nutrients in the body, which in turn leads to a decrease in the body's ability to resist stress factors and independently restore internal balance. As researcher Peter C. Whybrow points out, people born with a genetic predisposition to develop bipolar disorder “initially have a reduced ability to smoothly adapt to a changing planetary environment—or adjust to the chaotic cycle of chronic stress—and to restore homeostatic balance.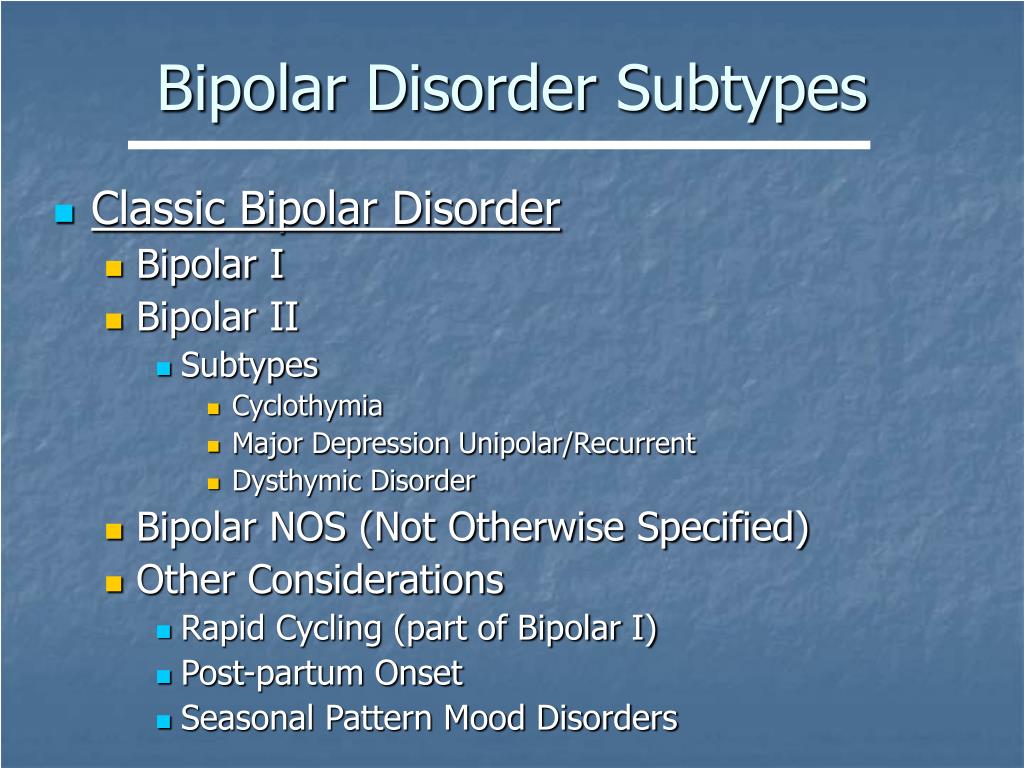 as stressors disappear.
as stressors disappear.
Chemical toxicity
The current level of chemical pollution in the environment allows us to talk about the unprecedented impact of a huge number of unusual chemicals on the human body. At least 250 chemical pollutants can be found in the body fat depots of any modern person (even those living at a sufficient distance from pollution sources). According to Sherry A. Rogers, M.D., “The chemicals we encounter in our daily lives have the ability to influence the metabolism of neurotransmitters, including “happiness hormones,” in a myriad of ways. They interfere with their synthesis and metabolism, affect the location of receptors, poison enzymes and much more.
Toxic heavy metals
A long history of medical observation has shown a correlation between exposure to metals such as mercury, copper, lead and aluminum and their derivatives and mood disorders. Many of these substances, recognized as neurotoxins, are also bioaccumulative, that is, they are not able to decompose when they get inside the human body and can remain in it for years, having a destructive effect on it. So, for example, in a study of the condition of 762 patients after replacing their mercury amalgam dentures with non-toxic composite dentures, it was recorded that out of 23.5% of respondents who complained of signs of depression (fatigue, loss of strength, irritability, inability to concentrate) up to replacement of prostheses, 100% reported the disappearance of these symptoms after replacement of prostheses.
So, for example, in a study of the condition of 762 patients after replacing their mercury amalgam dentures with non-toxic composite dentures, it was recorded that out of 23.5% of respondents who complained of signs of depression (fatigue, loss of strength, irritability, inability to concentrate) up to replacement of prostheses, 100% reported the disappearance of these symptoms after replacement of prostheses.
Food allergies
Headaches, chronic fatigue and depression are common symptoms of food allergies in the adult population. Leaving aside the energy aspect of allergic reactions to food, at the physical level, undigested large protein molecules enter the intestines, after which they are partially absorbed into the bloodstream and are perceived by the body's immune system as hostile. In response, antibodies (immunoglobulins) are launched, leading to allergic reactions. The reason for the inability of the body to adequately perceive certain types of products may, among other things, lie in intestinal dysbacteriosis.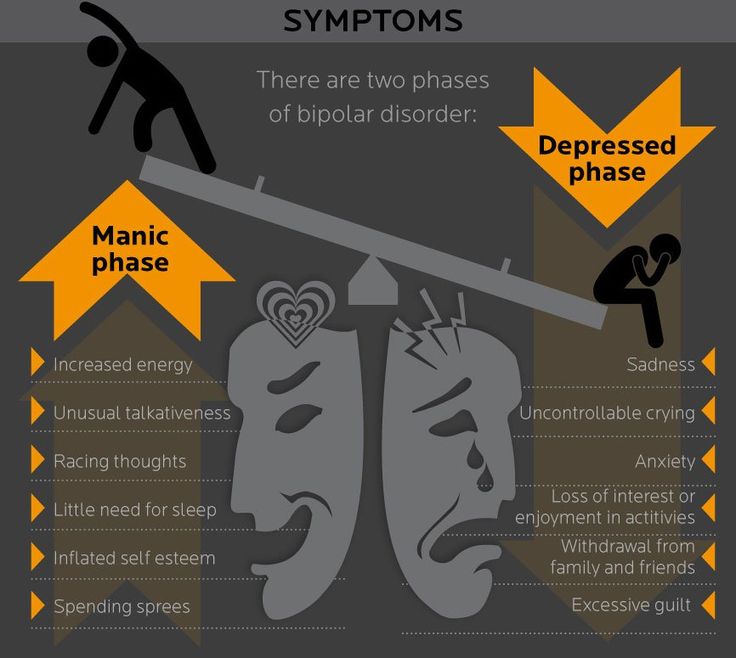
Intestinal dysbacteriosis
Recent studies confirm the relationship between the state of the human intestinal microflora and his mood: the waste products of small intestine bacteria are able to be absorbed through its walls into the blood and reach the brain, affecting the function of neurotransmitter production. With a certain imbalance in the quantitative ratio of beneficial bacteria (probiotics Lactobacillus acidophilus and Bifidobacterium bifidum) and potentially dangerous bacteria E. Coli and Clostridium, as well as the diploid fungus Candidia Albicans (thrush), the level of toxic waste products of the latter increases to such an extent that the intestine loses the ability to effectively cope with them, and the liver does not have time to filter them out of bile. A side effect of this process is inflammation of the intestinal walls, which does not allow proper absorption of nutrients, which also affects the state of the body and its ability to produce substances that precede the synthesis of neurotransmitters (precursors).
Food additive sensitivity
Over 3,000 commonly used food additives, including flavor enhancers and substitutes, preservatives, food colors, thickeners, humectants, and sweeteners, have not been tested for their neurotoxicity or their effects on the nervous system and human behavior. Among those food additives, the action of which causes a wide range of negative effects (depression, insomnia, nervousness, hyperactivity, dizziness), the artificial sweetener Aspartame (aspartic acid), which according to the results of studies is recognized as neurotoxic. In addition, depressive symptoms are the subject of the most frequent complaints to the U.S. Department of Health Food and Drug Administration (FDA) related to the use of Aspartame.
Nutritional deficiencies and imbalances
This aspect of bipolar affective disorder is so extensive that it needs to be studied separately. Within the framework of this work, we can only state that a deficiency of unsaturated fatty acids (omega-3, omega-6), amino acids, B vitamins, magnesium and zinc, which are precursors and constituent elements for the independent production of neurotransmitters, can play a key role in the development of BAD.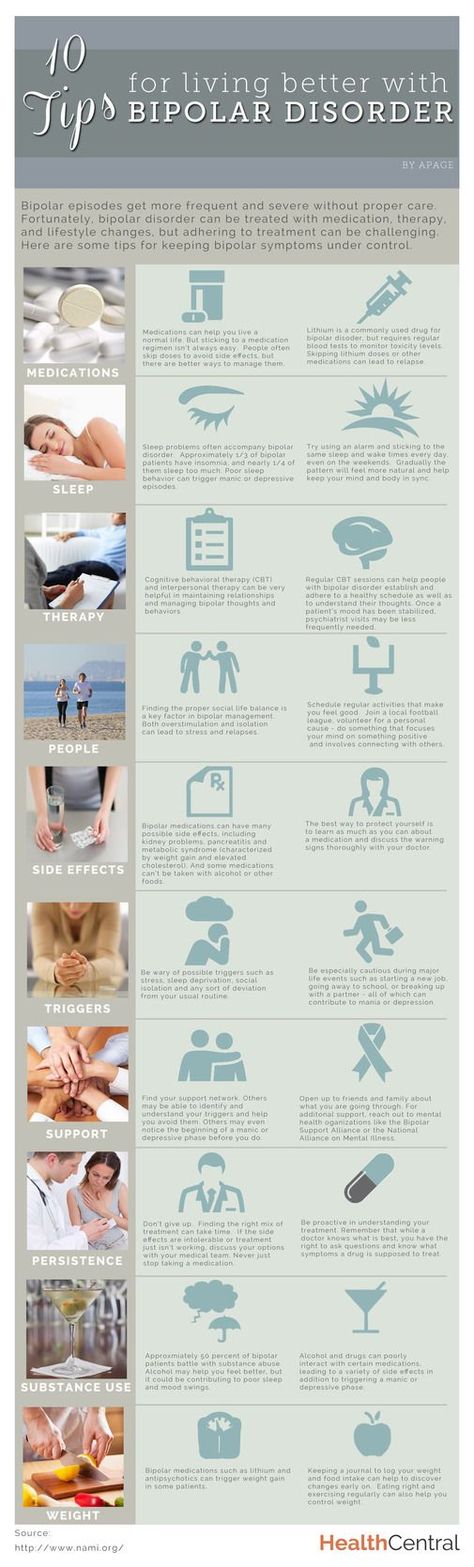 organism. The reasons for the deficiency of these substances in the body can be violations of the absorption and processing of nutrients, including those laid down genetically, but most often this situation develops due to an unbalanced and depleted diet.
organism. The reasons for the deficiency of these substances in the body can be violations of the absorption and processing of nutrients, including those laid down genetically, but most often this situation develops due to an unbalanced and depleted diet.
Deficiency and dysfunction of neurotransmitters
In addition to the above, it should be noted that the development of BAD can be caused not only by reduced levels of production of such neurotransmitters as serotonin, dopamine, noradrenaline, GABA, but also by a decrease in the ability of the corresponding parts of the brain to adsorb them and use.
Hormonal imbalance
Among the hormones that most prominently influence mood swings and affective disorders, researchers include hormones produced by the thyroid gland, adrenal glands (cortisol, dehydroepiandrosterone (DHEA), epinephrine and norepinephrine) and reproductive hormones (estrogen, progesterone, testosterone).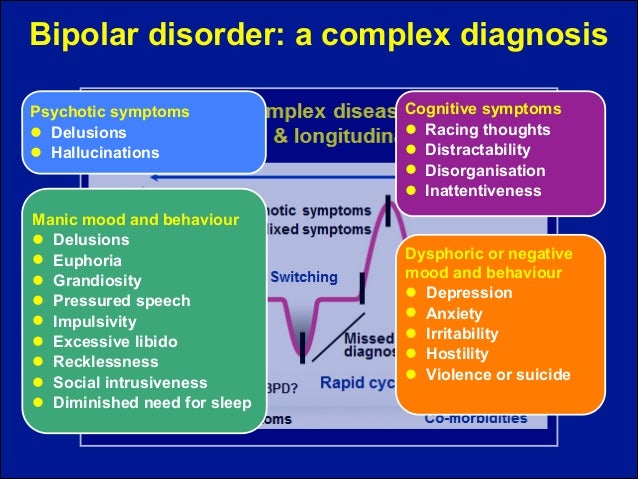
Hypoglycemia
Low blood glucose leads to a whole range of symptoms that can become stress factors and provoke the development of bipolar disorder: irritability, excitability, pathological fatigue and, in severe cases, mental impairment. According to psychiatrist and orthomolecular physician Michael Lesser, clinical practice shows that bipolar patients have a very wide range of blood glucose levels depending on the phase of their condition (depression corresponds to lower levels). “Lithium salts, as a substance that limits mood swings during the course of bipolar disorder, also levels blood glucose levels. It is possible that this is the reason, including why it is effective, ”says researcher Lesser.
Organic factors
Physiological factors such as changes in intracranial pressure can also influence the production of neurotransmitters and the functioning of the brain in general. Violation of normal intracranial pressure can be both the result of birth trauma and the consequence of subsequent physical head injuries received during life.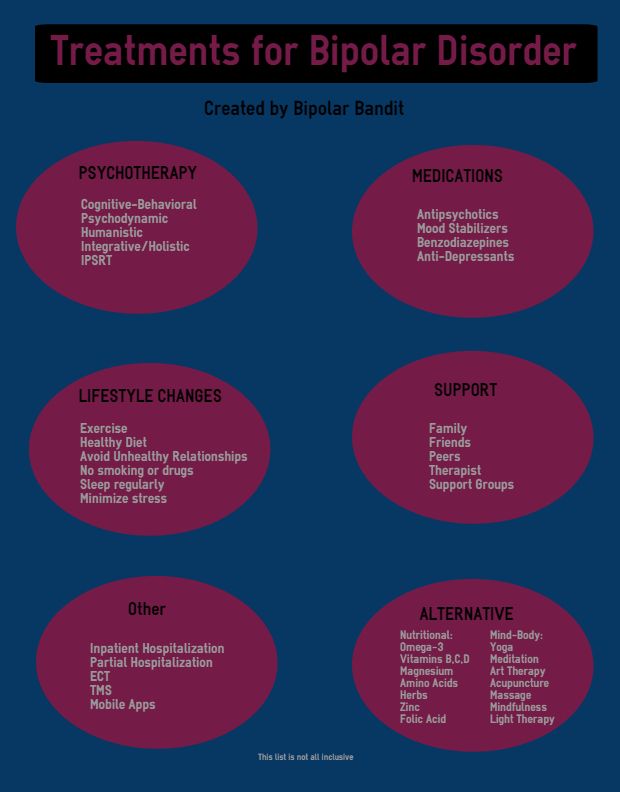
Medical conditions
According to the DSM-IV classification, symptoms of the following conditions may be misdiagnosed as signs of bipolar disorder: Parkinson's disease, Huntington's disease, cerebrovascular disease (including stroke), hyper- and hypothyroidism, lupus, viral infections ( including HIV), hepatitis, mononucleosis, pancreatic cancer. Vitamin B12 deficiency is rated by the DSM-IV as an obvious condition for the onset of mood disorders.
Medications
Clinical practice shows that the use of most antidepressants and stimulants contains the threat of transition of bipolar disorder to the manic phase of the disorder. The DSM-IV classifier also contains a list of other drugs that can provoke mood changes: analgesics, painkillers, anticonvulsants, antihypertensive drugs, antipsychotics, antiulcer drugs, benzodiazepines (tranquilizers), agents for restoring the functioning of the heart muscle, oral contraceptives, muscle relaxants, steroids.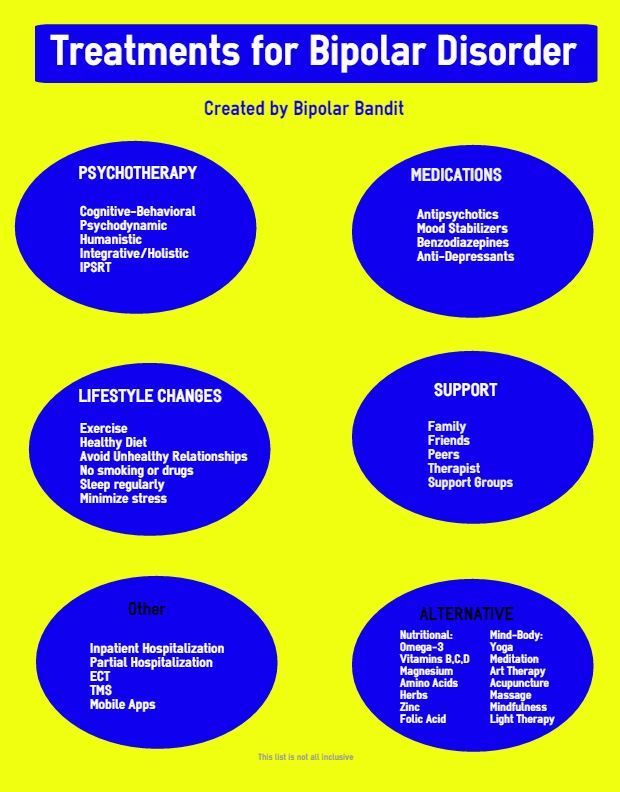 At the same time, a sharp cessation of drug therapy traditionally used to treat bipolar disorders (lithium salts, tranquilizers and antidepressants) can lead to a similar effect.
At the same time, a sharp cessation of drug therapy traditionally used to treat bipolar disorders (lithium salts, tranquilizers and antidepressants) can lead to a similar effect.
Alcohol and stimulants
According to DSM-IV, the use of cocaine-containing substances and amphetamines, as well as the abrupt cessation of this process, can lead to permanent mood disorders, including bipolar disorder. Alcohol also affects the normal functioning of neurotransmitters by interfering with the supply of tryptophan to the brain, which in turn reduces the production of serotonin. This can cause depression and insomnia. Also, regular consumption of alcohol, as well as caffeinated products, provokes hypoglycemia and nutritional deficiencies, especially B vitamins, vitamin C, folic acid, potassium and magnesium.
Lack of sleep
Sleep deprivation is one of the most common antidepressant treatments. However, clinical practice shows that the forced lack of sleep for a day or more is capable of provoking both manic and depressive episodes in those suffering from bipolar disorder, and in the case of bipolar disorder with a rapid course, it is a trigger for a phase change.
Lack of physical activity
Exercise and physical activity stimulate the release of adrenaline, norepinephrine and serotonin along with endorphins that improve mood and reduce stress levels. Studies of patients with major depressive disorder have shown that regular 30-minute walks reduce depressive symptoms in a faster period of time than antidepressant drug therapy, and 30-minute runs 3 times a week are equivalent or more effective than a course of psychotherapy.
Lack of natural light
Reduced exposure to natural sunlight (full spectrum light) caused by modern working and living conditions in artificial lighting conditions leads to a decrease in serotonin levels and sleep disorders due to a decrease in melatonin production. The same reason is associated with an increase in the number of depressive episodes of bipolar disorder during periods of insufficient natural light (autumn-winter period) and the maximum number of development of manic phases (after mid-summer) in those suffering from bipolar disorder. In modern clinics, therapy of patients with depressive disorders with full spectrum lamps has been used for several decades.
In modern clinics, therapy of patients with depressive disorders with full spectrum lamps has been used for several decades.
Energy imbalance
There are several different approaches to the issue of energy balance in the body. Within the framework of this work, there is no need to dwell on the approaches of traditional Chinese medicine (acupuncture techniques, restoring the flow of Qi energy along the meridians of the human body), the homeopathic approach, or the energy practices of national healers of different peoples (for example, shamanism). Consideration of the issue of the energy balance of the body within the framework of the traditional medical approach, however, also seems to be relevant, due to the fact that the biochemistry of the nervous system functions due to weak electrical impulses, which means that it forms an electromagnetic field that is subject to disturbances, including through the influence of external sources (strong electromagnetic fields near power lines, locators, etc. ), affecting well-being and mood). One way or another, all of the above approaches are aimed at achieving an energy balance in the body and bringing it to its original homeostatic state.
), affecting well-being and mood). One way or another, all of the above approaches are aimed at achieving an energy balance in the body and bringing it to its original homeostatic state.
Psychotherapeutic aspect
Modern psychotherapy, in particular the cognitive approach, affirms a close relationship between the physical state of a person, the work of his brain, consciousness, emotional experiences and spiritual aspects of human existence. Violation of this relationship in the broadest sense of the word, in my opinion, can be considered a deep root cause of such chronic mood disorders as bipolar disorder. In a more applied aspect, cognitive psychotherapy techniques have proven in clinical practice to be effective for patients with bipolar disorder. They are able to effectively change thought patterns, which has a beneficial effect on the emotional sphere of patients, promotes the acceptance of the disease and mobilizes the strength of patients for proactive participation in bipolar disorder therapy.