Transcranial magnetic stimulation reviews
Transcranial magnetic stimulation: A review of its evolution and current applications
1. Muehsam D, Ventura C. Life rhythm as a symphony of oscillatory patterns: Electromagnetic energy and sound vibration modulates gene expression for biological signaling and healing. Glob Adv Health Med. 2014;3:40–55. [PMC free article] [PubMed] [Google Scholar]
2. Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;1:1106–7. [PubMed] [Google Scholar]
3. Horvath JC, Perez JM, Forrow L, Fregni F, Pascual-Leone A. Transcranial magnetic stimulation: A historical evaluation and future prognosis of therapeutically relevant ethical concerns. J Med Ethics. 2011;37:137–43. [PubMed] [Google Scholar]
4. Cohen Kadosh R, Elliott P. Neuroscience: Brain stimulation has a long history. Nature. 2013;500:529. [PubMed] [Google Scholar]
5. Hasey GM. Transcranial magnetic stimulation: Using a law of physics to treat psychopathology. J Psychiatry Neurosci. 1999;24:97–101. [PMC free article] [PubMed] [Google Scholar]
6. Kolin A, Brill NQ, Broberg PJ. Stimulation of irritable tissues by means of an alternating magnetic field. Proc Soc Exp Biol Med. 1959;102:251–3. [PubMed] [Google Scholar]
7. Blumberger DM, Vila-Rodriguez F, Thorpe KE, Feffer K, Noda Y, Giacobbe P, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): A randomised non-inferiority trial. Lancet. 2018;391:1683–92. [PubMed] [Google Scholar]
8. Klomjai W, Katz R, Lackmy-Vallée A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS) Ann Phys Rehabil Med. 2015;58:208–13. [PubMed] [Google Scholar]
9. Mishra BR, Sarkar S, Praharaj SK, Mehta VS, Diwedi S, Nizamie SH, et al. Repetitive transcranial magnetic stimulation in psychiatry. Ann Indian Acad Neurol. 2011;14:245–51. [PMC free article] [PubMed] [Google Scholar]
10. Sorrell RG, Muhlenfeld J, Moffett J, Stevens G, Kesten S.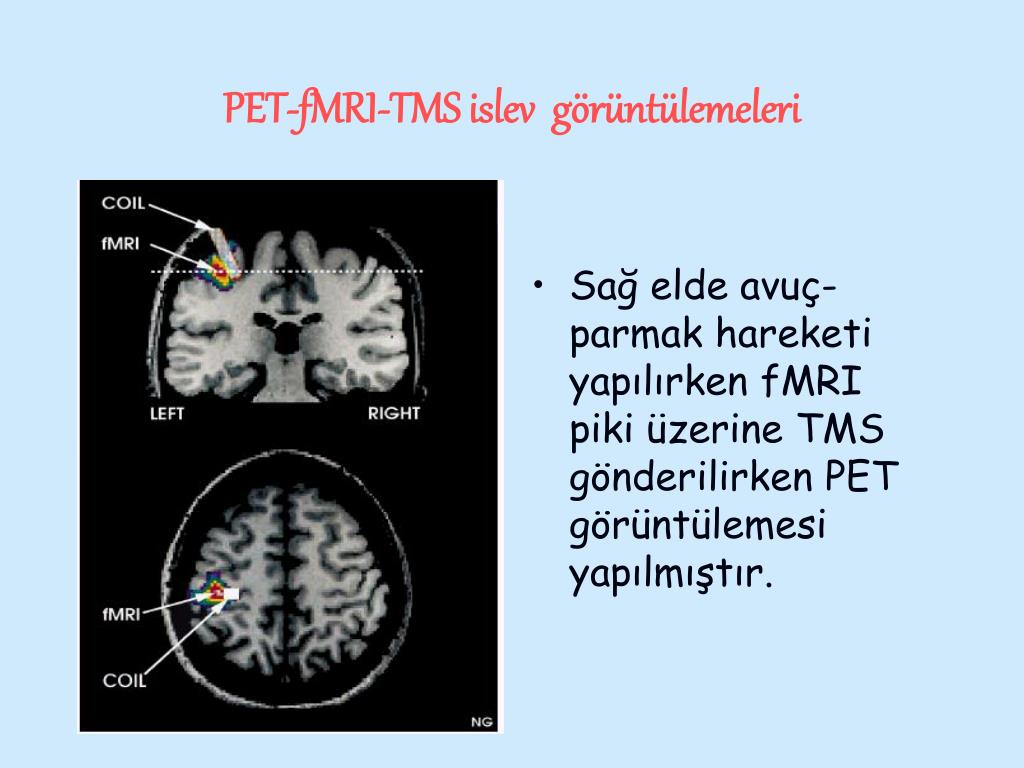 Evaluation of pulsed electromagnetic field therapy for the treatment of chronic postoperative pain following lumbar surgery: A pilot, double-blind, randomized, sham-controlled clinical trial. J Pain Res. 2018;11:1209–22. [PMC free article] [PubMed] [Google Scholar]
Evaluation of pulsed electromagnetic field therapy for the treatment of chronic postoperative pain following lumbar surgery: A pilot, double-blind, randomized, sham-controlled clinical trial. J Pain Res. 2018;11:1209–22. [PMC free article] [PubMed] [Google Scholar]
11. Chen M, Deng H, Schmidt RL, Kimberley TJ. Low-frequency repetitive transcranial magnetic stimulation targeted to premotor cortex followed by primary motor cortex modulates excitability differently than premotor cortex or primary motor cortex stimulation alone. Neuromodulation. 2015;18:678–85. [PMC free article] [PubMed] [Google Scholar]
12. Berlim MT, Van den Eynde F, Jeff Daskalakis Z. Clinically meaningful efficacy and acceptability of low-frequency repetitive transcranial magnetic stimulation (rTMS) for treating primary major depression: A meta-analysis of randomized, double-blind and sham-controlled trials. Neuropsychopharmacology. 2013;38:543–51. [PMC free article] [PubMed] [Google Scholar]
13. Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS) Clin Neurophysiol. 2014;125:2150–206. [PubMed] [Google Scholar]
Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS) Clin Neurophysiol. 2014;125:2150–206. [PubMed] [Google Scholar]
14. Fitzgerald PB, Fountain S, Daskalakis ZJ. A comprehensive review of the effects of rTMS on motor cortical excitability and inhibition. Clin Neurophysiol. 2006;117:2584–96. [PubMed] [Google Scholar]
15. Fidalgo TM, Morales-Quezada JL, Muzy GS, Chiavetta NM, Mendonca ME, Santana MV, et al. Biological markers in noninvasive brain stimulation trials in major depressive disorder: A systematic review. J ECT. 2014;30:47–61. [PMC free article] [PubMed] [Google Scholar]
16. Deng ZD, Lisanby SH, Peterchev AV. Electric field depth-focality tradeoff in transcranial magnetic stimulation: Simulation comparison of 50 coil designs. Brain Stimul. 2013;6:1–3. [PMC free article] [PubMed] [Google Scholar]
17. Suchorska B, Ruge MI. Deep brain stimulation: Current applications and future prospects. Discov Med. 2015;20:403–11. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
18. Rossi S, Hallett M, Rossini PM, Pascual-Leone A. Screening questionnaire before TMS: An update. Clin Neurophysiol. 2011;122:1686. [PubMed] [Google Scholar]
19. Basker M, Moses PD, Russell S, Russell PS. The psychometric properties of beck depression inventory for adolescent depression in a primary-care paediatric setting in India. Child Adolesc Psychiatry Ment Health. 2007;1:8. [PMC free article] [PubMed] [Google Scholar]
20. Wang YP, Gorenstein C. Psychometric properties of the beck depression inventory-II: A comprehensive review. Braz J Psychiatry. 2013;35:416–31. [PubMed] [Google Scholar]
21. Li Y, Gu Y, Wang H, Liu Z, Song B, Yin T, et al. Electric pulses can influence galvanotaxis of Dictyostelium discoideum. Biomed Res Int. 2018;2018:2534625. [PMC free article] [PubMed] [Google Scholar]
22. Huang YJ, Samorajski J, Kreimer R, Searson PC. The influence of electric field and confinement on cell motility. PLoS One. 2013;8:e59447. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
23. Paillère Martinot ML, Galinowski A, Ringuenet D, Gallarda T, Lefaucheur JP, Bellivier F, et al. Influence of prefrontal target region on the efficacy of repetitive transcranial magnetic stimulation in patients with medication-resistant depression: A [(18)F]-fluorodeoxyglucose PET and MRI study. Int J Neuropsychopharmacol. 2010;13:45–59. [PubMed] [Google Scholar]
24. Beam W, Borckardt JJ, Reeves ST, George MS. An efficient and accurate new method for locating the F3 position for prefrontal TMS applications. Brain Stimul. 2009;2:50–4. [PMC free article] [PubMed] [Google Scholar]
25. Fitzgerald PB, Hoy K, McQueen S, Maller JJ, Herring S, Segrave R, et al. A randomized trial of rTMS targeted with MRI based neuro-navigation in treatment-resistant depression. Neuropsychopharmacology. 2009;34:1255–62. [PubMed] [Google Scholar]
26. Vaghefi E, Cai P, Fang F, Byblow WD, Stinear CM, Thompson B, et al. MRI guided brain stimulation without the use of a neuronavigation system. Biomed Res Int. 2015;2015:647510. [PMC free article] [PubMed] [Google Scholar]
Biomed Res Int. 2015;2015:647510. [PMC free article] [PubMed] [Google Scholar]
27. Herwig U, Padberg F, Unger J, Spitzer M, Schönfeldt-Lecuona C. Transcranial magnetic stimulation in therapy studies: Examination of the reliability of “standard” coil positioning by neuronavigation. Biol Psychiatry. 2001;50:58–61. [PubMed] [Google Scholar]
28. Richter L, Neumann G, Oung S, Schweikard A, Trillenberg P. Optimal coil orientation for transcranial magnetic stimulation. PLoS One. 2013;8:e60358. [PMC free article] [PubMed] [Google Scholar]
29. Boutros NN, Gueorguieva R, Hoffman RE, Oren DA, Feingold A, Berman RM. Lack of a therapeutic effect of a 2-week sub-threshold transcranial magnetic stimulation course for treatment-resistant depression. [Last cited on 2018 Oct 08];Psychiatry Res [Internet] 2002 113:245–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12559481 . [PubMed] [Google Scholar]
30. Couturier JL. Efficacy of rapid-rate repetitive transcranial magnetic stimulation in the treatment of depression: A systematic review and meta-analysis [Internet] [Last cited 2018 Oct 08];J Psychiatry Neurosci.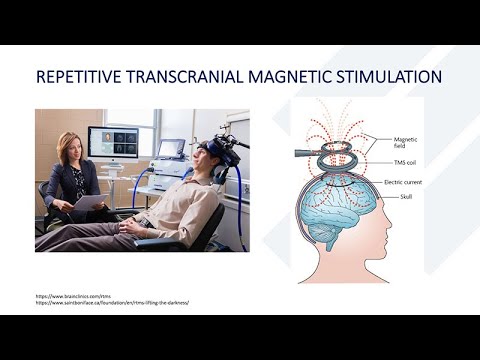 2005 30 Available from: www.cochrane.org . [PMC free article] [PubMed] [Google Scholar]
2005 30 Available from: www.cochrane.org . [PMC free article] [PubMed] [Google Scholar]
31. George MS, Lisanby SH, Avery D, McDonald WM, Durkalski V, Pavlicova M, et al. Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: A shamcontrolled randomized trial. Arch Gen Psychiatry. 2010 [PubMed] [Google Scholar]
32. Hadley D, Anderson BS, Borckardt JJ, Arana A, Li X, Nahas Z, et al. Safety, Tolerability, and Effectiveness of High Doses of Adjunctive Daily Left Prefrontal Repetitive Transcranial Magnetic Stimulation for Treatment-Resistant Depression in a Clinical Setting. [Last cited on 2018 Oct 08];J ECT [Internet] 2011 27:18–25. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21343710 . [PubMed] [Google Scholar]
33. Mantovani A, Aly M, Dagan Y, Allart A, Lisanby SH. Randomized sham controlled trial of repetitive transcranial magnetic stimulation to the dorsolateral prefrontal cortex for the treatment of panic disorder with comorbid major depression. [Last cited on 2018 Oct 08];J Affect Disord [Internet] 2013 144:153–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22858212 . [PubMed] [Google Scholar]
[Last cited on 2018 Oct 08];J Affect Disord [Internet] 2013 144:153–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22858212 . [PubMed] [Google Scholar]
34. Sayar GH, Ozten E, Tan O, Tarhan N. Transcranial magnetic stimulation for treating depression in elderly patients. Neuropsychiatr Dis Treat. 2013 [PMC free article] [PubMed] [Google Scholar]
35. Bulteau S, Sebille V, Fayet G, Thomas-Ollivier V, Deschamps T, Bonnin-Rivalland A, et al. Efficacy of intermittent Theta Burst Stimulation (iTBS) and 10-Hz highfrequency repetitive transcranial magnetic stimulation (rTMS) in treatment-resistant unipolar depression: Study protocol for a randomised controlled trial. Trials. 2017 [PMC free article] [PubMed] [Google Scholar]
36. Pamela D SS. US FDA report on HORIZON TMS therapy system [Internet] Maryland: 2018. [Last cited on 2018 Sep 10]. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf18/K180907.pdf . [Google Scholar]
37. Royal College of Psychiatrists C on E and related treatment. Statement on Repetitive Transcranial Magnetic Stimulation for Depression. 2017. [Last cited on 2018 Oct 08]. Available from: https://www.rcpsych.ac.uk/pdf/Repetative%20Transcranial%20Magnetic%20Stimulation%20-%20ECT%20ctee%20statement%20May18.pdf .
Statement on Repetitive Transcranial Magnetic Stimulation for Depression. 2017. [Last cited on 2018 Oct 08]. Available from: https://www.rcpsych.ac.uk/pdf/Repetative%20Transcranial%20Magnetic%20Stimulation%20-%20ECT%20ctee%20statement%20May18.pdf .
38. Wilson MT, St George L. Repetitive Transcranial Magnetic Stimulation: A Call for Better Data. [Last cited on 2018 Oct 08];Front Neural Circuits [Internet] 2016 10:57. Available from: www.frontiersin.org . [PMC free article] [PubMed] [Google Scholar]
39. Cortes M, Black-Schaffer RM, Edwards DJ. Transcranial magnetic stimulation as an investigative tool for motor dysfunction and recovery in stroke: An overview for neurorehabilitation clinicians. Neuromodulation. 2012;15:316–25. [PMC free article] [PubMed] [Google Scholar]
40. George MS, Wassermann EM, Williams WA, Callahan A, Ketter TA, Basser P, et al. Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. Neuroreport. 1995;6:1853–6. [PubMed] [Google Scholar]
41. Pascual-Leone A, Rubio B, Pallardó F, Catalá MD. Rapid-rate transcranial magnetic stimulation of left dorsolateral prefrontal cortex in drug-resistant depression. Lancet. 1996;348:233–7. [PubMed] [Google Scholar]
Pascual-Leone A, Rubio B, Pallardó F, Catalá MD. Rapid-rate transcranial magnetic stimulation of left dorsolateral prefrontal cortex in drug-resistant depression. Lancet. 1996;348:233–7. [PubMed] [Google Scholar]
42. Liu B, Zhang Y, Zhang L, Li L. Repetitive transcranial magnetic stimulation as an augmentative strategy for treatment-resistant depression, a meta-analysis of randomized, double-blind and sham-controlled study. BMC Psychiatry. 2014;14:342. [PMC free article] [PubMed] [Google Scholar]
43. Padberg F, Zwanzger P, Keck ME, Kathmann N, Mikhaiel P, Ella R, et al. Repetitive transcranial magnetic stimulation (rTMS) in major depression: Relation between efficacy and stimulation intensity. Neuropsychopharmacology. 2002;27:638–45. [PubMed] [Google Scholar]
44. Avery DH, Holtzheimer PE, 3rd, Fawaz W, Russo J, Neumaier J, Dunner DL, et al. A controlled study of repetitive transcranial magnetic stimulation in medication-resistant major depression. Biol Psychiatry. 2006;59:187–94. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
45. O’Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: A multisite randomized controlled trial. Biol Psychiatry. 2007;62:1208–16. [PubMed] [Google Scholar]
46. Dunner DL, Aaronson ST, Sackeim HA, Janicak PG, Carpenter LL, Boyadjis T, et al. A multisite, naturalistic, observational study of transcranial magnetic stimulation for patients with pharmacoresistant major depressive disorder: Durability of benefit over a 1-year follow-up period. J Clin Psychiatry. 2014;75:1394–401. [PubMed] [Google Scholar]
47. Nguyen KH, Gordon LG. Cost-effectiveness of repetitive transcranial magnetic stimulation versus antidepressant therapy for treatment-resistant depression. Value Health. 2015;18:597–604. [PubMed] [Google Scholar]
48. Fregni F, Marcolin MA, Myczkowski M, Amiaz R, Hasey G, Rumi DO, et al. Predictors of antidepressant response in clinical trials of transcranial magnetic stimulation. Int J Neuropsychopharmacol. 2006;9:641–54. [PubMed] [Google Scholar]
Int J Neuropsychopharmacol. 2006;9:641–54. [PubMed] [Google Scholar]
49. Slotema CW, Blom JD, Hoek HW, Sommer IE. Should we expand the toolbox of psychiatric treatment methods to include repetitive transcranial magnetic stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders. J Clin Psychiatry. 2010;71:873–84. [PubMed] [Google Scholar]
50. Chen SJ, Chang CH, Tsai HC, Chen ST, Lin CC. Superior antidepressant effect occurring 1 month after rTMS: Add-on rTMS for subjects with medication-resistant depression. Neuropsychiatr Dis Treat. 2013;9:397–401. [PMC free article] [PubMed] [Google Scholar]
51. Razza LB, Moffa AH, Moreno ML, Carvalho AF, Padberg F, Fregni F, et al. A systematic review and meta-analysis on placebo response to repetitive transcranial magnetic stimulation for depression trials. Prog Neuropsychopharmacol Biol Psychiatry. 2018;81:105–13. [PubMed] [Google Scholar]
52. US FDA. Press Announcements – FDA Permits Marketing of Transcranial Magnetic Stimulation for Treatment of Obsessive Compulsive Disorder. [Last accessed on 2018 Aug 31];Office of the Commissioner. Avaialble from: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm617244.htm . [Google Scholar]
[Last accessed on 2018 Aug 31];Office of the Commissioner. Avaialble from: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm617244.htm . [Google Scholar]
53. Rajapakse T, Kirton A. Non-invasive brain stimulation in children: Applications and future directions [Internet] [Last accessed on 2018 Oct 08];Translational Neuroscience. 2013 4:217–33. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3807696/pdf/nihms-510197.pdf . [Google Scholar]
54. Allen CH, Kluger BM, Buard I. Safety of transcranial magnetic stimulation in children: A systematic review of the literature HHS public access. [Last accessed on 2018 Oct 08];Pediatr Neurol. 2017 68:3–17. Avaialble from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5346461/pdf/nihms-840696.pdf . [PMC free article] [PubMed] [Google Scholar]
55. Hızlı Sayar G, Ozten E, Tufan E, Cerit C, Kaǧan G, Dilbaz N, et al. Transcranial magnetic stimulation during pregnancy. Arch Womens Ment Health. 2014;17:311–5. [PubMed] [Google Scholar]
56. Iriarte IG, George MS. Transcranial magnetic stimulation (TMS) in the elderly. Curr Psychiatry Rep. 2018;20:6. [PubMed] [Google Scholar]
Iriarte IG, George MS. Transcranial magnetic stimulation (TMS) in the elderly. Curr Psychiatry Rep. 2018;20:6. [PubMed] [Google Scholar]
57. [Last accessed on 2018 Aug 31];US FDA. Consumer Updates – Treating Migraines: More Ways to Fight the Pain. Office of the Commissioner. Avaialble from: https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm414707.htm . [Google Scholar]
58. National Institute for Health and Care Excellence. Transcranial Magnetic Stimulation for Treating and Preventing Migraine. National Institute for Health and Care Excellence. 2014:1–8. [Google Scholar]
59. Gorelick DA, Zangen A, George MS. Transcranial magnetic stimulation in the treatment of substance addiction. Ann N Y Acad Sci. 2014;1327:79–93. [PMC free article] [PubMed] [Google Scholar]
60. Dilkov D, Hawken ER, Kaludiev E, Milev R. Repetitive transcranial magnetic stimulation of the right dorsal lateral prefrontal cortex in the treatment of generalized anxiety disorder: A randomized, double-blind sham controlled clinical trial. Prog Neuropsychopharmacol Biol Psychiatry. 2017;78:61–5. [PubMed] [Google Scholar]
Prog Neuropsychopharmacol Biol Psychiatry. 2017;78:61–5. [PubMed] [Google Scholar]
Is There Evidence for Effectiveness of Transcranial Magnetic Stimulation in the Treatment of Psychiatric Disorders?
Psychiatry (Edgmont). 2005 Nov; 2(11): 64–69.
Published online 2005 Nov.
Biju Basil, MD, DPM, Jamal Mahmud, MD, DPM, Maju Mathews, MD, MRCPsych, Dip PSYCH,Carlos Rodriguez, MD, and , MD, DPM
Author information Copyright and License information Disclaimer
Transcranial magnetic stimulation (TMS), since its introduction in 1985, has been studied for its efficacy in different psychiatric disorders. It has been touted to be an effective treatment modality for major depression, obsessive compulsive disorder, Tourette syndrome, and in reducing auditory hallucinations in patients with schizophrenia. In this article, the authors outline the research and evidence toward the efficacy of TMS in psychiatry.
Since the introduction of electroconvulsive therapy (ECT) in 1938, it has been shown to be very effective in treatment for major depression. It has also been shown to be effective in the treatment of acute mania and, to a limited extent, chronic schizophrenia. But ECT still remains one of the most controversial modalities of treatment in the entire field of medicine. Its proponents swear by it, while its opponents hate it. The movie “One Flew over Cuckoo's Nest,” like many other movies before and after, portrayed ECT as a very crude and cruel method of treatment, which is sometimes abused as a form of punishment for behavior control. There has been a steady decline in use of ECT in clinical psychiatry settings, and it remains one of the most underutilized treatments. Less than eight percent of American psychiatrists use ECT.1
It has also been shown to be effective in the treatment of acute mania and, to a limited extent, chronic schizophrenia. But ECT still remains one of the most controversial modalities of treatment in the entire field of medicine. Its proponents swear by it, while its opponents hate it. The movie “One Flew over Cuckoo's Nest,” like many other movies before and after, portrayed ECT as a very crude and cruel method of treatment, which is sometimes abused as a form of punishment for behavior control. There has been a steady decline in use of ECT in clinical psychiatry settings, and it remains one of the most underutilized treatments. Less than eight percent of American psychiatrists use ECT.1
The introduction of transcranial magnetic stimulation (TMS) and vagal nerve stimulation (VNS) have rekindled interest in the use of brain stimulation methods for the treatment of psychiatric disorders. TMS enables the clinician to focally stimulate specific areas of the brain noninvasively and painlessly. The efficacy of TMS in the treatment of depression has been extensively studied. TMS has also been shown to have some beneficial effects in the treatment of posttraumatic stress disorder (PTSD) and obsessive compulsive disorder (OCD).2
The efficacy of TMS in the treatment of depression has been extensively studied. TMS has also been shown to have some beneficial effects in the treatment of posttraumatic stress disorder (PTSD) and obsessive compulsive disorder (OCD).2
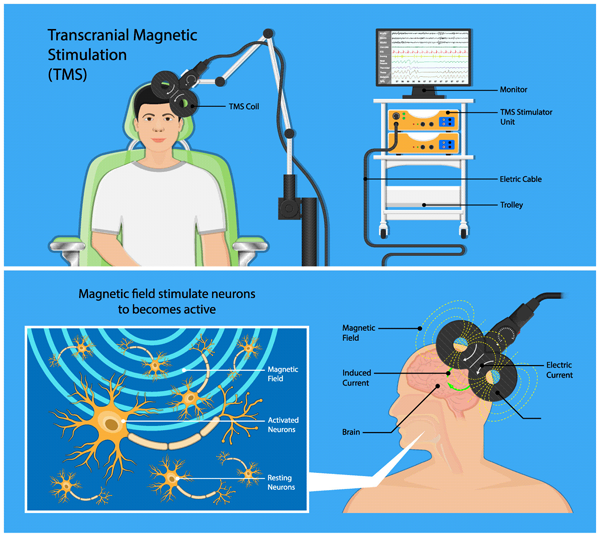
TMS was introduced in 1985 by Anthony Baker at the University of Sheffield in England.3 It was designed to be a neurodiagnostic tool used to produce an evoked potential in muscle tissue by activating neurons in the motor cortex.3 TMS is based on two basic principles in physics:1 Ampere's law2 and Faraday's principle of electromagnetic induction.4
Ampere's law states that the magnetic field in the space around an electric current is proportional to the electric current. According to Faraday's principle of electromagnetic induction, a voltage would be generated across a length of wire if that wire was exposed to a perpendicular magnetic field flux of changing intensity.
The stimulation coil of the TMS instrument consists of multiple wire loops encased in an insulated material. This is connected to powerful capacitors capable of passing a large electrical current through the coil.3 If a pulse of current is passed through this coil and placed over a person's head, it produces rapidly changing magnetic pulses that penetrate the scalp and skull and reach the brain with minimal attenuation.5 When these pulses alternate rapidly enough, a secondary electric current is induced that alters the local electric field in the nerve tissue.4 This leads to depolarization of the underlying superficial neurons.6 High-intensity current is rapidly turned on and off in the electromagnetic coil using discharges from powerful capacitors.6 TMS thus produces brief but very powerful magnetic fields that lead to induction of electric currents in the brain. TMS pulses can be administered repetitively and rhythmically, and this process is called repetitive TMS (rTMS).7 This can be further classified as high frequency rTMS if the frequency is greater than 1Hz, whereas if the speed of stimulation is equal or less than 1Hz it is called low frequency rTMS.
This is connected to powerful capacitors capable of passing a large electrical current through the coil.3 If a pulse of current is passed through this coil and placed over a person's head, it produces rapidly changing magnetic pulses that penetrate the scalp and skull and reach the brain with minimal attenuation.5 When these pulses alternate rapidly enough, a secondary electric current is induced that alters the local electric field in the nerve tissue.4 This leads to depolarization of the underlying superficial neurons.6 High-intensity current is rapidly turned on and off in the electromagnetic coil using discharges from powerful capacitors.6 TMS thus produces brief but very powerful magnetic fields that lead to induction of electric currents in the brain. TMS pulses can be administered repetitively and rhythmically, and this process is called repetitive TMS (rTMS).7 This can be further classified as high frequency rTMS if the frequency is greater than 1Hz, whereas if the speed of stimulation is equal or less than 1Hz it is called low frequency rTMS.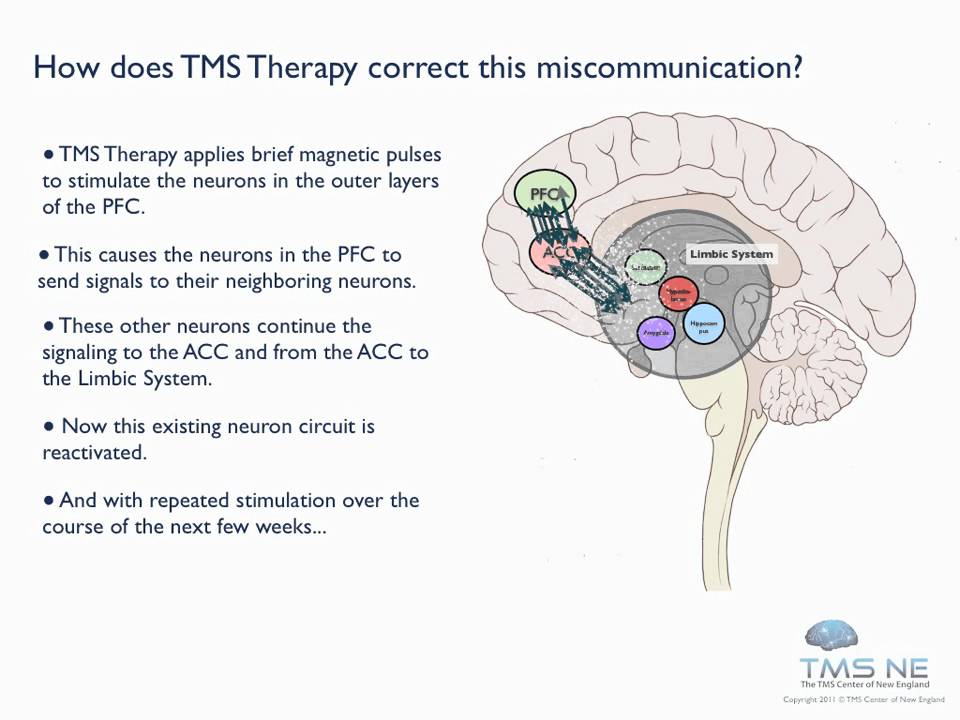 8
8
Major depressive disorder has a prevalence of almost seven percent in the general population.9 Many effective treatments are available, but as many as 30 percent of these depressed patients do not respond to treatment. Brain stimulation techniques are a possible treatment modality that can be used in these patients with treatment resistant depression. There have been more than 20 randomized, controlled trials investigating the efficacy of rTMS in the treatment of major depression. The most common deficiency noted is the relatively small sample sizes of these studies. The sample size varied from 6 to 70. Most of the studies used sample sizes less than 20.8
George, et al.,10 studied the efficacies of rTMS in patients with depression in a double-blind crossover design. Twelve patients were given either active rTMS or sham treatment. The study suggested that daily left prefrontal repetitive transcranial magnetic stimulation has antidepressant activity. 10
10
Klein, et al.,11 in a double-blind, placebo-controlled study assessed the efficacy of slow repetitive TMS (rTMS) in patients with major depression. Seventy patients with major depression were randomly assigned to receive active rTMS or sham rTMS in a double-blind design. It was shown that patients who received active rTMS had a significantly greater improvement in depression scores compared with those who received sham treatment and provided evidence for the short-term efficacy of slow rTMS in patients with recurrent major depression.11
Berman, et al.,12 in a randomized, double-blind, clinical trial, studied the efficacy of rTMS in treatment resistant major depression. Depressed subjects, who had failed to respond to a median of four treatment trials, were assigned in a randomized, double-blind manner to receive either active or sham rTMS. Adjusted mean decreases in HDRS scores were 14.0 (±3.7) and 0.2 (±4.1) points for the active and control groups, respectively (p<0.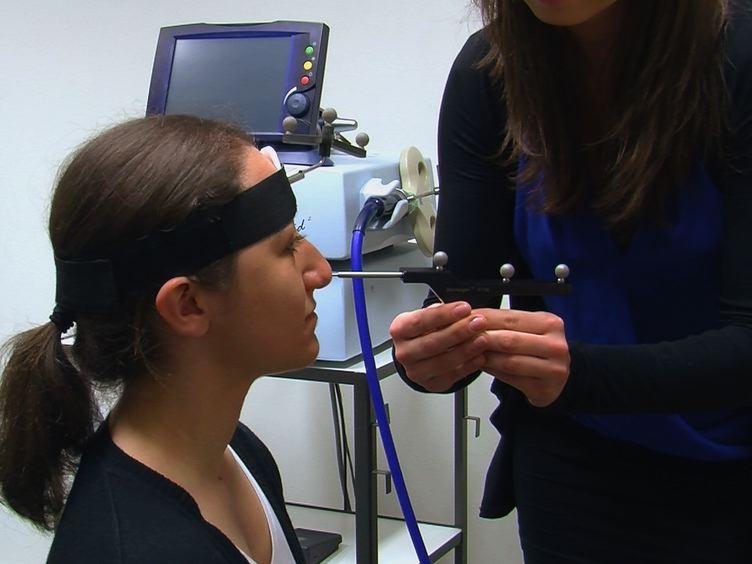 05). A two-week course of active rTMS resulted in statistically significant but clinically modest reductions of depressive symptoms, as compared to sham rTMS.12
05). A two-week course of active rTMS resulted in statistically significant but clinically modest reductions of depressive symptoms, as compared to sham rTMS.12
Toro, et al.,13 studied the efficacy of rTMS in drug-resistant depression. In this randomized, double-blind study, 40 patients received either active rTMS or sham rTMS to the left prefrontal cortex. The authors of this study concluded that real, but not sham, HF-rTMS was associated with a significant decrease in the Hamilton Depression Rating Scale and that left prefrontal high frequency-rTMS was effectively associated with antidepressant treatment. But the size effect was small.13
Toro, et al.,14 in another published study examined the efficacy of high frequency rTMS as add-on treatment to sertraline in the treatment of major depression. The addition of HF-rTMS did not show any benefit in speeding up or strengthening the therapeutic response to sertraline in major depression.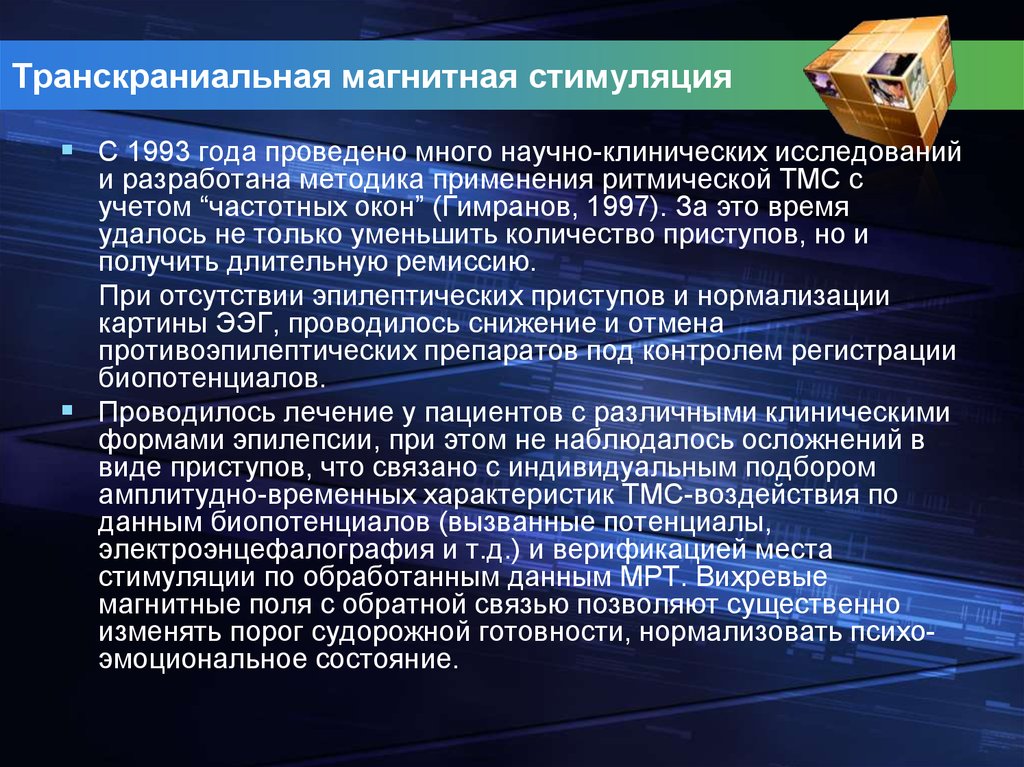 14
14
Boutros, et al.,15 compared active rTMS to sham rTMS in a double-blind controlled trial. Twenty-one treatment-resistant depressed patients were randomized to either active rTMS (n=12) or to sham (n=9) treatment. Sub-motor-threshold (MT) stimulation (80% MT) was delivered for 10 consecutive work days while still receiving medications. It was shown that sub-threshold rTMS stimulation for two weeks is not significantly superior to sham treatment for treatment-resistant depressed patients.15
Hoppner, et al.,16 in a placebo-controlled study compared high frequency rTMS over left versus low frequency rTMS over right prefrontal cortex compared with sham stimulation in patients with major depression. There were no differences in resolution of depressive symptoms between the rTMS procedures. An additional observation made by these authors was that patients with less severe deficits in psychomotor speed and concentration responded more intensively than patients with severe deficits. 16
16
Herwig, et al.,17 in a double-blind, randomized, sham-controlled pilot study investigated the efficacy of neuronavigated rTMS, guided according to the prefrontal metabolic state determined by positron emission tomography (PET). The dorsolateral prefrontal cortex (DLPFC) with lower metabolic activity compared to the contralateral hemisphere, as determined from PET scans, was selected to receive the real stimulation. The preliminary examination of the data showed that stimulation of prefrontal cortex with rTMS may not be advantageous irrespective of the metabolic state.17
Loo, et al.,18 examined the efficacy and safety of bilateral prefrontal repetitive transcranial magnetic stimulation (rTMS) for treating resistant major depression in a double-blind, placebo-controlled study. Nineteen medication-resistant depressed subjects were randomly assigned to three weeks of active or sham rTMS. Bilateral rTMS did not show any superiority to sham in treating resistant depression. 18
18
Hansen, et al.,19 studied the efficacy of rTMS in patients with major depression. Fifteen inpatients were randomized to receive 15 days of active left prefrontal high-frequency rTMS or sham rTMS, as an add-on to conventional antidepressant treatment. More than 50 percent of the patients receiving real rTMS suffered from local discomfort during treatment. Real rTMS did not add to the efficacy of standard antidepressant medication and thus did not confirm the antidepressant effect of left frontal high-frequency rTMS.19
Couturier20 did a meta-analysis of six studies of the efficacy of rTMS in the treatment of depression. Two of these studies reported a significant improvement in mood symptoms versus sham group. When combined in the meta-analysis with the other four studies. it was shown that rTMS was no different from sham treatment in major depression.20
Martin, et al.,8 in a recent review of 16 trials studying the efficacy of rTMS in major depression for Cochrane Data Base concluded that there is no strong evidence for benefit from using transcranial magnetic stimulation to treat depression. though they did not exclude the possibility of benefit.8
though they did not exclude the possibility of benefit.8
Greenberg, et al.,21 investigated whether prefrontal repetitive transcranial magnetic stimulation influenced OCD symptoms. Twelve patients with OCD were randomized to receive rTMS to a right lateral, a left lateral prefrontal, and a midoccipital site, and the patients' symptoms and mood were rated for eight hours afterward. Compulsive urges showed a significant decrease after right lateral prefrontal repetitive transcranial magnetic stimulation. The study concluded that right prefrontal repetitive transcranial magnetic stimulation might affect prefrontal mechanisms involved in obsessive compulsive disorder.21
Sachdev, et al.,22 in a randomized trial evaluated the efficacy of rTMS in OCD. Twelve subjects with resistant OCD were allocated randomly to either right or left prefrontal rTMS daily for two weeks. Subjects were shown to have an overall improvement in the obsessions, compulsions, and total scores on the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) after two weeks and at one-month follow-up.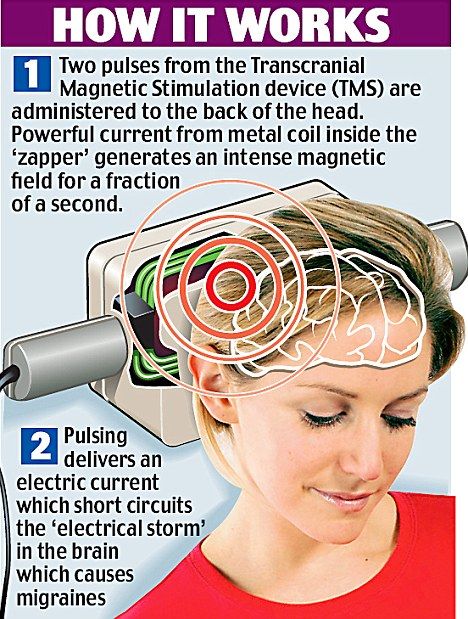 But this study, due to the lack of a sham treatment arm, cannot exclude a placebo response.22
But this study, due to the lack of a sham treatment arm, cannot exclude a placebo response.22
Alonso, et al.,23 examined the efficiency of rTMS of the right prefrontal cortex for patients with OCD in a double-blind, placebo-controlled trial. Patients received either real (low frequency) or sham rTMS. The study concluded that low-frequency rTMS of the right prefrontal cortex did not show any significant improvement of OCD and was not significantly different from sham treatment.23
Martin, et al.,24 in their review of the different studies of rTMS in OCD for Cochrane data Base concluded that there is a lack of evidence for the effect of TMS in the treatment of OCD.24
Munchau, et al.,25 studied the efficacy of low frequency rTMS in 16 patients with with Gilles de la Tourette syndrome (GTS) in a single-blinded, placebo-controlled, crossover trial. The study showed no significant improvement of symptoms as assessed with the Motor Tic, Obsessions and Compulsions, Vocal Tic Evaluation Eurvey. 25
25
Grisaru, el al.,26 investigated the efficacy of slow TMS on PTSD. Ten patients with PTSD were given one session of slow TMS. TMS was found to be effective in lowering the core symptoms of PTSD: avoidance, anxiety, and somatization.The patients also showed a general clinical improvement as measured by the Clinical Global Impression Scale. But this effect was short and transient.26
Rosenberg, et al.,27 studied the efficacy of left frontal cortex low frequency rTMS in 12 patients with PTSD and comorbid major depression. Seventy-five percent of the patients showed a clinically significant response after rTMS and 50 percent showed sustained response after two months. Improvements were also seen in anxiety, hostility, and insomnia. But the study showed minimal improvement in PTSD symptoms.27
Cohen, et al.,28 studied the efficacy of repetitive transcranial magnetic stimulation (rTMS) of the right prefrontal cortex in patients with posttraumatic stress disorder (PTSD) under double-blind, placebo-controlled conditions. Twenty-four patients with PTSD were randomly assigned to receive rTMS at low frequency (1Hz) or high frequency (10Hz) or sham rTMS in a double-blind design. This double-blind, controlled trial suggested that right dorsolateral prefrontal rTMS at a frequency of 10Hz has greater therapeutic effect than slow-frequency or sham stimulation in PTSD.28
Twenty-four patients with PTSD were randomly assigned to receive rTMS at low frequency (1Hz) or high frequency (10Hz) or sham rTMS in a double-blind design. This double-blind, controlled trial suggested that right dorsolateral prefrontal rTMS at a frequency of 10Hz has greater therapeutic effect than slow-frequency or sham stimulation in PTSD.28
Hajak, et al.,29 in a sham-controlled parallel study, treated 20 schizophrenic patients with rTMS of frontal regions. High frequency rTMS led to a significant reduction of negative symptoms and a nonsignificant improvement of depressive symptoms. High frequency rTMS treatment was paradoxically shown to lead to an increase in positive symptoms.29
Fitzgerald, et al.,30 in a randomized sham controlled, double-blind trial, treated 36 patients with treatment-resistant auditory hallucinations with low frequency rTMS (LF-rTMS). Active treatment led to more reduction of loudness than sham treatment, though it did not result in a greater therapeutic effect than sham. 30
30
Saba, et al.,31 in a double-blind, sham-controlled study tested the efficacy of rTMS in schizophrenia. Eighteen patients diagnosed with schizophrenia were randomly treated with active or sham rTMS over left temporoparietal cortex. This study failed to show any superiority for active rTMS over sham treatment.31
Hoffman, et al.,32 in a double-blind, sham-controlled, parallel design study, treated 50 schizophrenic patients with left temporoparietal cortex low frequency rTMS. Hallucination change score showed more improvement for people who received active rTMS than sham group. The active group also showed a significant decrease in a hallucination frequency.32
Chibbaro, et al.,33 investigated the benefits of treating schizophrenic patients with rTMS focused on left temporoparietal cortex in a 16-patient double-blind, sham-controlled study. The patients were treated with low frequency rTMS or sham treatment. This study also showed reduction of frequency of auditory hallucination in patients treated with active rTMS.33
This study also showed reduction of frequency of auditory hallucination in patients treated with active rTMS.33
Sachdev, et al.,34 in a pilot study, treated four patients having stable deficit syndrome of schizophrenia with high frequency rTMS over the left dorsolateral prefrontal cortex (DLPFC). The patients showed a significant reduction in negative symptoms and improvement in function.34
The different studies which investigated the efficacy of rTMS in patients with schizophrenia did not show any significant clinical benefits. But there were some studies which showed some improvement in the frequency and intensity of auditory hallucinations. The benefit of rTMS in schizophrenia need to be studied with more focused rTMS and larger patient samples.
TMS has rekindled interest in the role of brain stimulation in psychiatric disorders. Some of the studies have shown promising but not conclusive evidence for the efficacy of TMS in depression. But TMS has not been shown to be effective in the treatment of obsessive compulsive disorder, posttraumatic disorder, or schizophrenia. The patient sample size has been a cause of concern in most studies. There has been no multicenter study so far. There is a need to develop further consensus on the following parameters in TMS studies: Shape of coil, coil-cortex distance, motor threshold, low frequency versus high frequency stimulation, and location of the correct point of stimulation for each disorders.
But TMS has not been shown to be effective in the treatment of obsessive compulsive disorder, posttraumatic disorder, or schizophrenia. The patient sample size has been a cause of concern in most studies. There has been no multicenter study so far. There is a need to develop further consensus on the following parameters in TMS studies: Shape of coil, coil-cortex distance, motor threshold, low frequency versus high frequency stimulation, and location of the correct point of stimulation for each disorders.
1. Hermann RC, Ettner SL, Dorwart RA, et al. Characteristics of psychiatrists who perform ECT. Am J Psychiatry. 1998;155(7):889–94. [PubMed] [Google Scholar]
2. Sadock BJ, Sadock VA, editors. Comprehensive Textbook of Psychiatry. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2000. [Google Scholar]
3. Hassey G. Transcranial magnetic in the treatment of mood disorders: A review and comparison with electroconvulsive therapy. Can J Psychiatry. 2001;46:720–7. [PubMed] [Google Scholar]
4. Schutter DJLG, van Honk J. A framework for targeting alternative brain regions with repetitive transcranial magnetic stimulation in the treatment of depression. J Psychiatry Neurosci. 2005;30(2):91–7. [PMC free article] [PubMed] [Google Scholar]
Schutter DJLG, van Honk J. A framework for targeting alternative brain regions with repetitive transcranial magnetic stimulation in the treatment of depression. J Psychiatry Neurosci. 2005;30(2):91–7. [PMC free article] [PubMed] [Google Scholar]
5. Kobayashi M, Pascual-Leone A. Transcranial magnetic stimulation in neurology. Lancet Neurol. 2003;2:145–56. [PubMed] [Google Scholar]
6. George MS, Nahas Z, Kozel A, et al. Mechanisms and current state of transcranial magnetic stimulation. CNS Spectr. 2003;8(7):496–514. [PubMed] [Google Scholar]
7. Wassermann EM, Lisanby SH. Therapeutic application of repetitive transcranial magnetic stimulation: A review. Clin Neurophysiol. 2001;112(8):1367–77. [PubMed] [Google Scholar]
8. Martin JLR, Barbanoj MJ, Schlaepfer TE, et al. Transcranial magnetic stimulation for treating depression. [systematic review] Cochrane Database of Systematic Reviews. 2005;4 [PMC free article] [PubMed] [Google Scholar]
9. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Arch Gen Psychiatry. 1994;51:8–19. [PubMed] [Google Scholar]
Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Arch Gen Psychiatry. 1994;51:8–19. [PubMed] [Google Scholar]
10. George MS, Wassermann EM, Kimbrell TA, et al. Mood improvement following daily left prefrontal repetitive transcranial magnetic stimulation in patients with depression: A placebo-controlled crossover trial. Am J Psychiatry. 1997;154(12):1752–6. [PubMed] [Google Scholar]
11. Klein E, Kreinin I, Chistyakov A, et al. Therapeutic efficacy of right prefrontal slow repetitive transcranial magnetic stimulation in major depression: a double-blind controlled study. Arch Gen Psychiatry. 1999;56(4):315–20. [PubMed] [Google Scholar]
12. Berman RM, Narasimhan M, Sanacora G, et al. A randomized clinical trial of repetitive transcranial magnetic stimulation in the treatment of major depression. Biol Psychiatry. 2000;47(4):332–7. [PubMed] [Google Scholar]
13. Garcia-Toro M, Mayol A, Arnillas H, et al. Modest adjunctive benefit with transcranial magnetic stimulation in medication-resistant depression.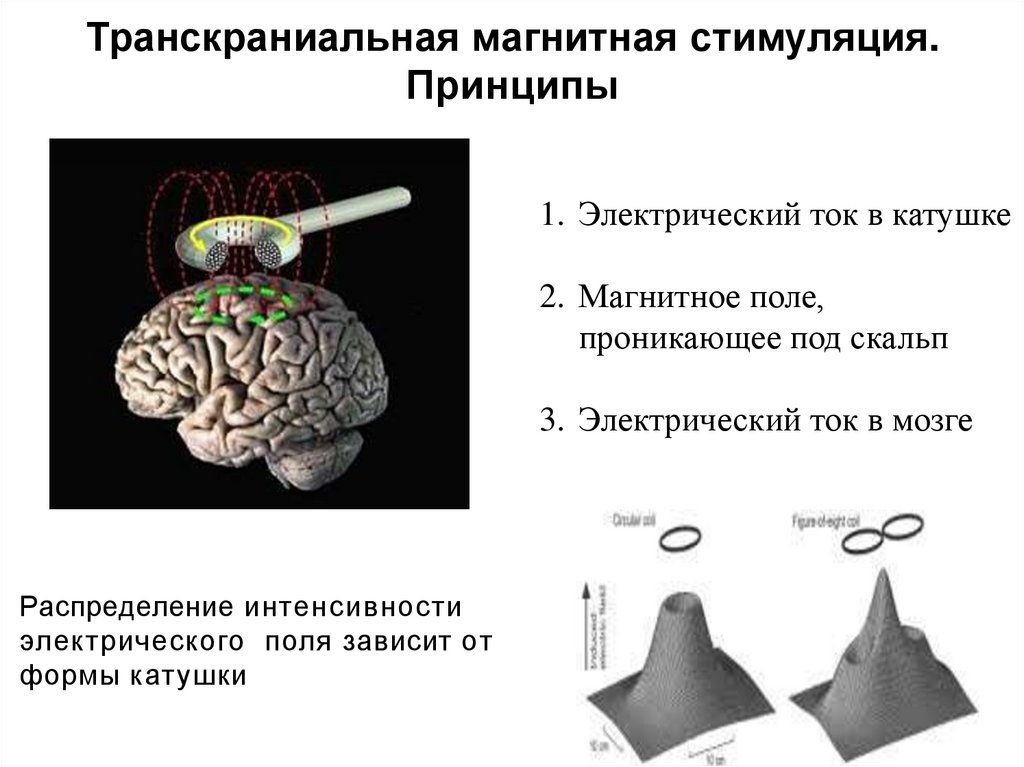 J Affect Disord. 2001;64:271–5. [PubMed] [Google Scholar]
J Affect Disord. 2001;64:271–5. [PubMed] [Google Scholar]
14. Garcia-Toro M, Pascual-Leone A, Romera M, et al. Prefrontal repetitive transcranial magnetic stimulation as add on treatment in depression. J Neurol Neurosurg Psychiatry. 2001;71(4):546–8. [PMC free article] [PubMed] [Google Scholar]
15. Boutros NN, Gueorguieva R, Hoffman RE, et al. Lack of a therapeutic effect of a two-week sub-threshold transcranial magnetic stimulation course for treatment-resistant depression. Psychiatry Res. 2002;113(3):245–54. [PubMed] [Google Scholar]
16. Hoppner J, Schulz M, Irmisch G, et al. Antidepressant efficacy of two different rTMS procedures. High frequency over left versus low frequency over right prefrontal cortex compared with sham stimulation. Eur Arch Psychiatry Clin Neurosci. 2003;253(2):103–9. [PubMed] [Google Scholar]
17. Herwig U, Lampe Y, Juengling FD, et al. Add-on rTMS for treatment of depression: A pilot study using stereotaxic coil-navigation according to PET data.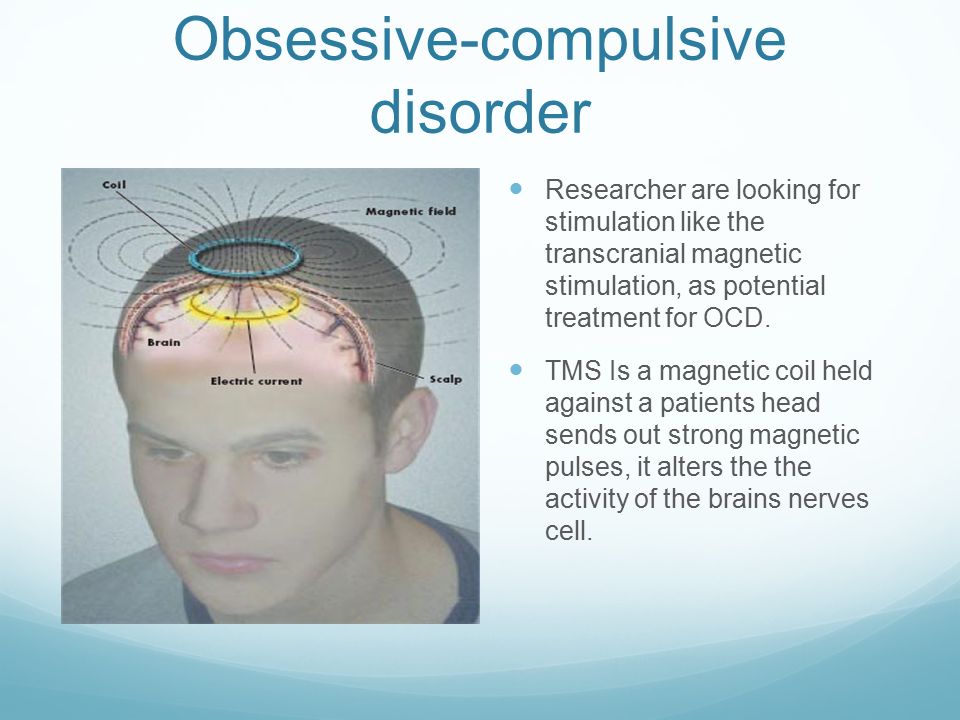 J Psychiatr Res. 2003;37(4):267–75. [PubMed] [Google Scholar]
J Psychiatr Res. 2003;37(4):267–75. [PubMed] [Google Scholar]
18. Loo CK, Mitchell PB, Croker VM, et al. Double-blind controlled investigation of bilateral prefrontal transcranial magnetic stimulation for the treatment of resistant major depression. Psychol Med. 2003;33(1):33–40. [PubMed] [Google Scholar]
19. Hansen PE, Videbech P, Clemmensen K, et al. Repetitive transcranial magnetic stimulation as add-on antidepressant treatment. The applicability of the method in a clinical setting. Nord J Psychiatry. 2004;58(6):455–7. [PubMed] [Google Scholar]
20. Couturier JL. Efficacy of rapid rate repetitive transcranial magnetic stimulation in the treatment of depression: A systematic review and meta-analysis. J psychiatry Neurosci. 2005;30(2):91–7. [PMC free article] [PubMed] [Google Scholar]
21. Greenberg BD, George MS, Martin JD, et al. Effect of prefrontal repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: A preliminary study. Am J Psychiatry. 1997;154(6):867–9. [PubMed] [Google Scholar]
1997;154(6):867–9. [PubMed] [Google Scholar]
22. Sachdev PS, McBride R, Loo CK, et al. Right versus left prefrontal transcranial magnetic stimulation for obsessive-compulsive disorder: A preliminary investigation. J Clin Psychiatry. 2001;62(12):981–4. [PubMed] [Google Scholar]
23. Alonso P, Pujol J, Cardoner N, et al. Right prefrontal repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: A double-blind, placebo-controlled study. Am J Psychiatry. 2001;158(7):1143–5. [PubMed] [Google Scholar]
24. Martin JLR, Barbanoj MJ, Perez V, Sacristan M. Transcranial magnetic stimulation for the treatment of obsessive-compulsive disorder. [Systematic Review] Cochrane Database of Systematic Reviews. 2005;4 [PMC free article] [PubMed] [Google Scholar]
25. Munchau A, Bloem BR, Thilo KV, et al. Repetitive transcranial magnetic stimulation for Tourette syndrome. Neurology. 2002;59(11):1789–91. [PubMed] [Google Scholar]
26. Grisaru N, Amir M, Cohen H, et al. Effect of transcranial magnetic stimulation in posttraumatic stress disorder: A preliminary study. Biol Psychiatry. 1998;44(1):52–5. [PubMed] [Google Scholar]
Effect of transcranial magnetic stimulation in posttraumatic stress disorder: A preliminary study. Biol Psychiatry. 1998;44(1):52–5. [PubMed] [Google Scholar]
27. Rosenberg PB, Mehndiratta RB, Mehndiratta YP, et al. Repetitive transcranial magnetic stimulation treatment of comorbid posttraumatic stress disorder and major depression. J Neuropsychiatry Clin Neurosci. 2002;14(3):270–6. [PubMed] [Google Scholar]
28. Cohen H, Kaplan Z, Kotler M, et al. Repetitive transcranial magnetic stimulation of the right dorsolateral prefrontal cortex in posttraumatic stress disorder: A double-blind, placebo-controlled study. Am J Psychiatry. 2004;161(3):515–24. [PubMed] [Google Scholar]
29. Hajak G, Marienhagen J, Langguth B, et al. High-frequency repetitive transcranial magnetic stimulation in schizophrenia: A combined treatment and neuroimaging study. Psychol Med. 2004;34(7):1157–63. [PubMed] [Google Scholar]
30. Fitzgerald PB, Benitez J, Daskalakis JZ, et al. A double-blind, sham-controlled trial of repetitive transcranial magnetic stimulation in the treatment of refractory auditory hallucinations. J Clin Psychopharmacol. 2005;25(4):358–62. [PubMed] [Google Scholar]
J Clin Psychopharmacol. 2005;25(4):358–62. [PubMed] [Google Scholar]
31. Saba G, Verdon CM, Kalalou K, et al. Transcranial magnetic stimulation in the treatment of schizophrenic symptoms: A double blind sham controlled study. J Psychiatr Res. 2005 Jun 16. [PubMed] [Google Scholar]
32. Hoffman RE, Gueorguieva R, Hawkins KA, et al. Temporoparietal transcranial magnetic stimulation for auditory hallucinations: Safety, efficacy and moderators in a fifty patient sample. Biol Psychiatry. 2005;58(2):97–104. [PubMed] [Google Scholar]
33. Chibbaro G, Daniele M, Alagona G, et al. Repetitive transcranial magnetic stimulation in schizophrenic patients reporting auditory hallucinations. Neurosci Lett. 2005;383(1-2):54–7. [PubMed] [Google Scholar]
34. Sachdev P, Loo C, Mitchell P, et al. Transcranial magnetic stimulation for the deficit syndrome of schizophrenia: A pilot investigation. Psychiatry Clin Neurosci. 2005;59(3):354–7. [PubMed] [Google Scholar]
12 diseases in which TMS will replace drugs
Dr. Vadim Berezhnoy
Vadim Berezhnoy
General practitioner, Medical expert, Head of the department of medical assistance.
Reading time - 11 minutes
Transcranial magnetic stimulation (TMS) is a non-surgical treatment for neurological disorders. The procedure is officially approved by the FDA for the treatment of depression and obsessive-compulsive disorder. Research is now underway around the world to help elucidate the effectiveness of TMS in the treatment of epilepsy, Alzheimer's disease, autism, Parkinson's disease, essential tremor and other diseases. In this article, you will find out what successes doctors have been able to achieve with the help of TMS and how it improves the lives of patients. And at the end of the article, we will tell you in which clinics you can get treatment for diseases for which TMS is officially approved. nine0004
TMS at Parkinson ↓
TMS at depression ↓
TMS for autism ↓
TMS at Alzheimer ↓
TMS during epilepsy ↓
Where to go through TMS ↓
, how does the transcernal work work?
Transcranial magnetic stimulation is a procedure during which a strong magnetic field affects neurons in the brain.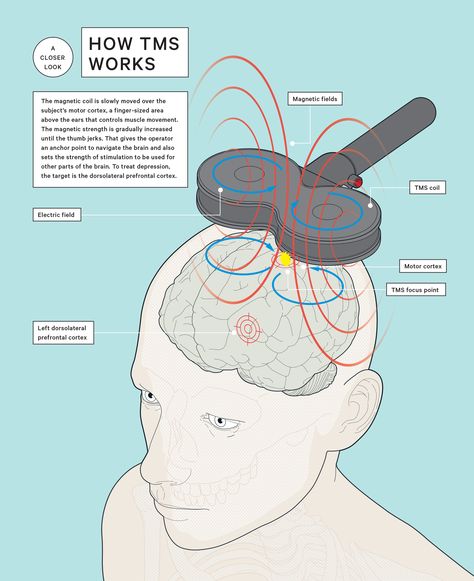 Depending on the strength of the field, the activity of neurons in these areas may increase or decrease. nine0005
Depending on the strength of the field, the activity of neurons in these areas may increase or decrease. nine0005
When a group of neurons simultaneously activates , a stable connection is formed between them. It helps a person to restore lost functions.
When the activity of neurons is suppressed , the connections between them are destroyed. So you can save the patient from unpleasant symptoms.
Rhythmic TMS (rTMS) is most commonly used in patient care. It can create pulses of different frequencies. So with the help of one device, you can simultaneously inhibit and activate different parts of the brain. nine0005
Where can I apply for TMS?
MediGlobus medical coordinators can tell you which clinics accept foreign patients and how much the treatment will cost. Click the button below to book a free consultation with one of our experts.
Book an appointment for TMS
INDICATIONS AND CONTRAINDICATIONS FOR TRANSCRANIAL MAGNETIC STIMULATION
Magnetic pulse therapy is offered to patients who are not helped by medical treatment. TMS may be given to people for whom deep brain stimulation (DBS) is at risk. nine0005
TMS may be given to people for whom deep brain stimulation (DBS) is at risk. nine0005
The procedure should not be performed on those who have metal implants in their body, such as a pacemaker. The procedure is also not performed on patients in a state of acute psychosis.
Diagnoses for which transcranial magnetic stimulation may be effective:
Alzheimer's disease;
major depression;
affective disorder;
Parkinson's disease;
epilepsy; nine0002 autism spectrum disorder;
multiple sclerosis;
tremor;
obsessive-compulsive disorder;
schizophrenia;
chronic pain;
rehabilitation after a stroke.
In this article, we will talk about how these diseases are treated and which organizations have approved the procedure of transcranial magnetic stimulation for these diagnoses. In addition to this list, TMS also shows success in reducing the symptoms of post-traumatic stress disorder (PTSD), aphasia , attention deficit hyperactivity disorder (ADHD). Its efficacy and safety is also being tested to improve the condition of patients after stroke and traumatic brain injury.
Its efficacy and safety is also being tested to improve the condition of patients after stroke and traumatic brain injury.
Diseases for which this procedure is possible vary from country to country. For example, in American clinics, depression and OCD can be treated with TMS. Clinics in Europe have approvals for the use of transcranial stimulation for a wider range of disorders. About which clinic is available to treat your disease with TMS check with our coordinating doctor .
Get a free consultation
TREATMENT OF PARKINSON'S DISEASE WITH TRANSCRANIAL MAGNETIC STIMULATION
In Parkinson's disease, the midbrain and basal ganglia lack a special substance - dopamine . Low dopamine levels cause trembling and muscle weakness. Medications restore dopamine levels, but they have many unpleasant side effects.
With the help of rhythmic TMS, the impulse activates the neurons of the motor cortex of the brain. Clinical studies by Dr. Sibner in Copenhagen have shown that after 4 weeks of treatment with improves gait, reduces tremors and improves well-being in patients. This effect is achieved faster than when taking medication.
Clinical studies by Dr. Sibner in Copenhagen have shown that after 4 weeks of treatment with improves gait, reduces tremors and improves well-being in patients. This effect is achieved faster than when taking medication.
TREATMENT OF ESSENTIAL TREMOR WITH TRANSCRANIAL MAGNETIC STIMULATION
Essential tremor is the second most common movement disorder in adults after restless legs syndrome. It is not life-threatening, but it prevents a person from fully resting and working. nine0005
Tremor is also treated with rhythmic transcranial magnetic stimulation to activate the motor cortex and cerebellum. Patients noticeably reduced hand tremor after the first session. The procedure does not cause drowsiness and lethargy as after taking the medicine.
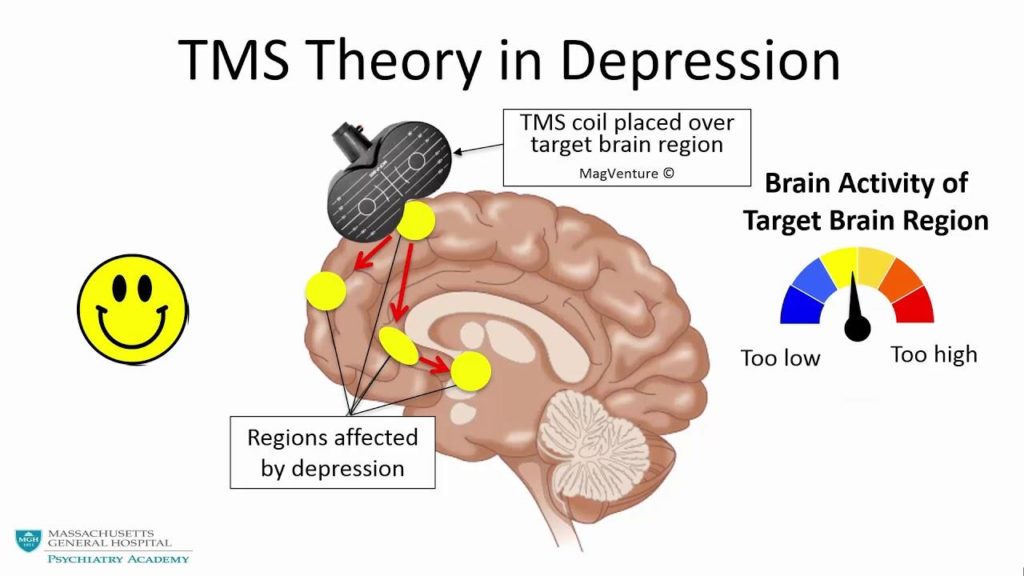
TREATMENT OF DEPRESSION WITH TRANSCRANIAL MAGNETIC STIMULATION
TMS is used to treat depression in people who are not responding to antidepressants or other treatment alternatives.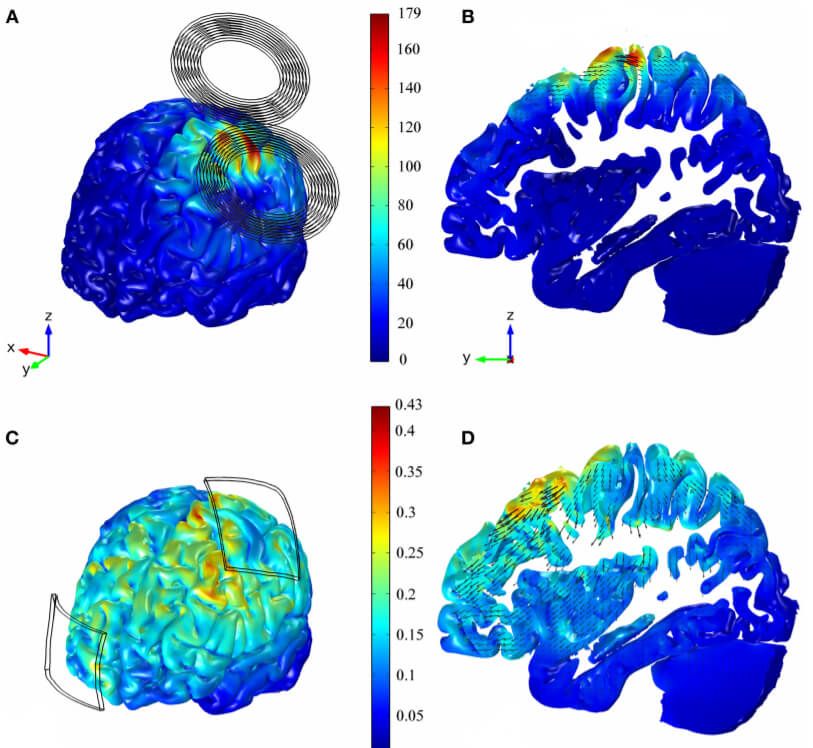 The main advantage of this procedure is that it does not lead to general lethargy, nervousness, nightmares, diarrhea or nausea, which often happens after taking antidepressants. nine0005
The main advantage of this procedure is that it does not lead to general lethargy, nervousness, nightmares, diarrhea or nausea, which often happens after taking antidepressants. nine0005
Patients with depression usually have 5 sessions per week for 1.5-2 months. One session takes from 5 to 30 minutes, depending on the type of device. The procedure does not require hospitalization - after a course of TMS, a person can return to their daily activities.
After sessions of magnetic stimulation, the symptoms of depression completely disappear in the third patient. About 60% of patients report an improvement in well-being. The results of exposure to transcranial magnetic stimulation in the case of treatment of depression persist for 10-12 months. When the symptoms return, you need to repeat the course. nine0005
In 2008, the FDA approved transcranial magnetic stimulation for the treatment of major depression.
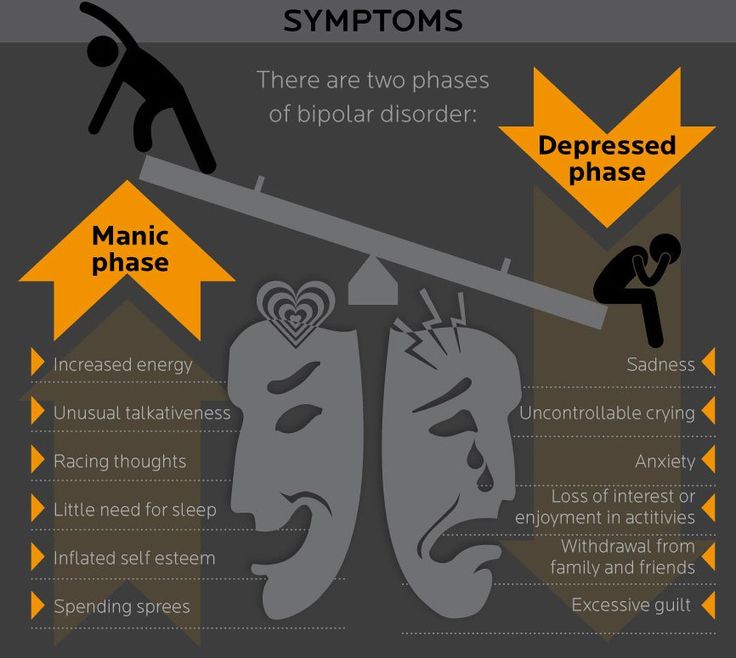
TREATMENT OF BIPOLARIUS DISORDER WITH TRANSCRANIAL MAGNETIC STIMULATION
Every year, more than 7 million people are diagnosed with bipolar disorder.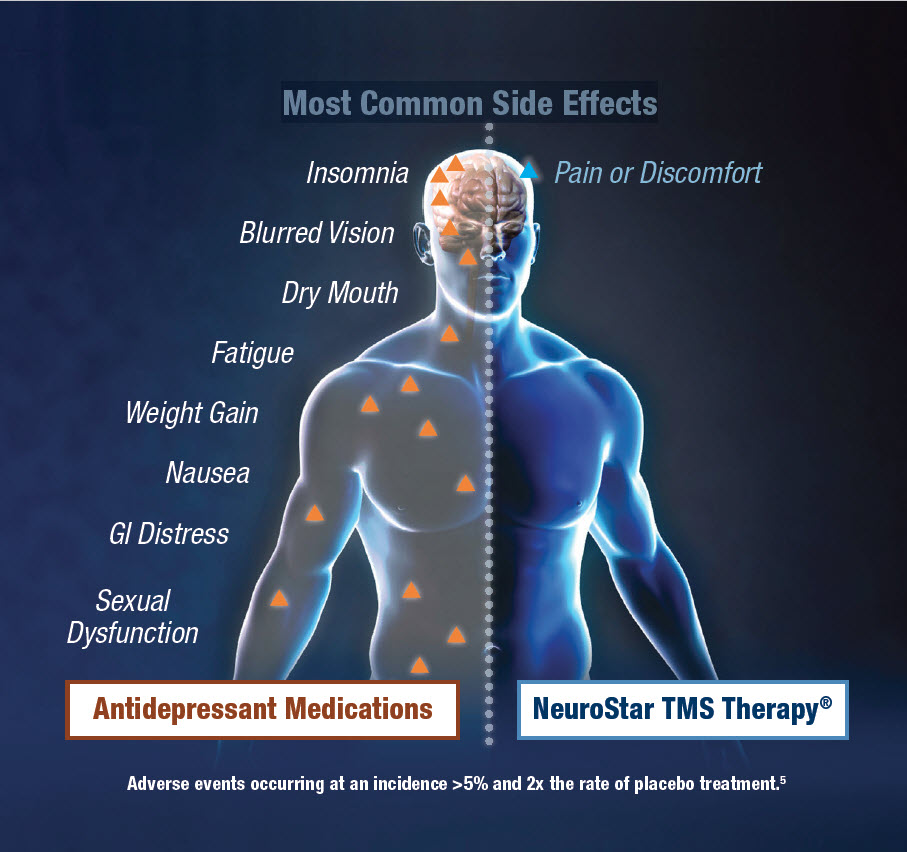 Of these, 480,000 people are resistant to pharmacotherapy. Allowing magnetic field therapy will help solve this problem.
Of these, 480,000 people are resistant to pharmacotherapy. Allowing magnetic field therapy will help solve this problem.
In 2020, FDA began testing the use of TMS to treat manic manifestations of mood disorder in adults who have not responded to drug therapy. In order to stabilize the emotional background, doctors activate neurons in the frontal lobes. nine0005
Mood disorder therapy with TMS is currently CE and ANIVISA approved.
TREATMENT OF OCD WITH TRANSCRANIAL MAGNETIC STIMULATION
Obsessive Compulsive Disorder is a chronic condition where a person suffers from obsessive thoughts or repeats the same actions. However, he cannot consciously stop it. This diagnosis occurs in 1% of people.
Transcranial magnetic stimulation relieves these symptoms. Approximately 38% of people who underwent OCD therapy with TMS confirmed an improvement in well-being. Their values according to obsessive-compulsive Yale-Brown scale has dropped significantly. Among the adverse reactions in patients, headache was the most common.
Among the adverse reactions in patients, headache was the most common.
OCD treatment with TMS received FDA approval in 2018.
GET A CUSTOMIZED TREATMENT PACKAGE
The cost of BMT abroad depends on the country, clinic and doctor performing the procedure. Our medical coordinators can help you find a neurological treatment center based on your budget. Request our call by clicking on the button below, and we will call you back as soon as possible and answer all your questions. nine0005
Call me back
TREATMENT OF CHRONIC PAIN WITH TRANSCRANIAL MAGNETIC STIMULATION
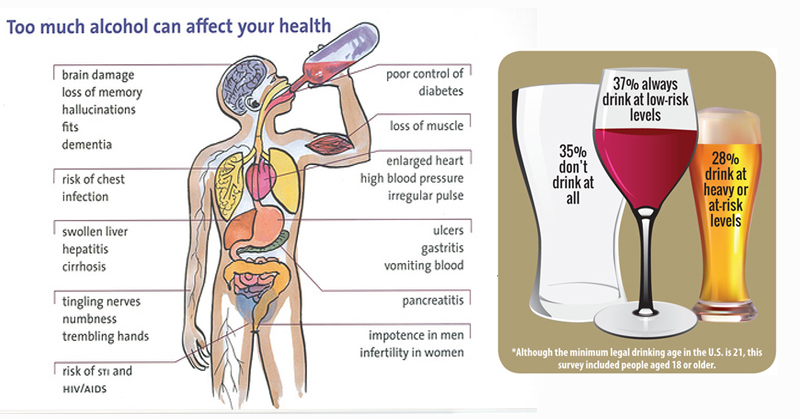
Transcranial stimulation can relieve pain in diabetic neuropathy , migraine and pain after traumatic brain injury. Studies conducted in European and Israeli clinics have proven that rhythmic TMS is especially effective in relieving pain in trigeminal neuralgia.
Therapy of chronic pain is possible by activating those areas of the brain that can feed the perception of pain.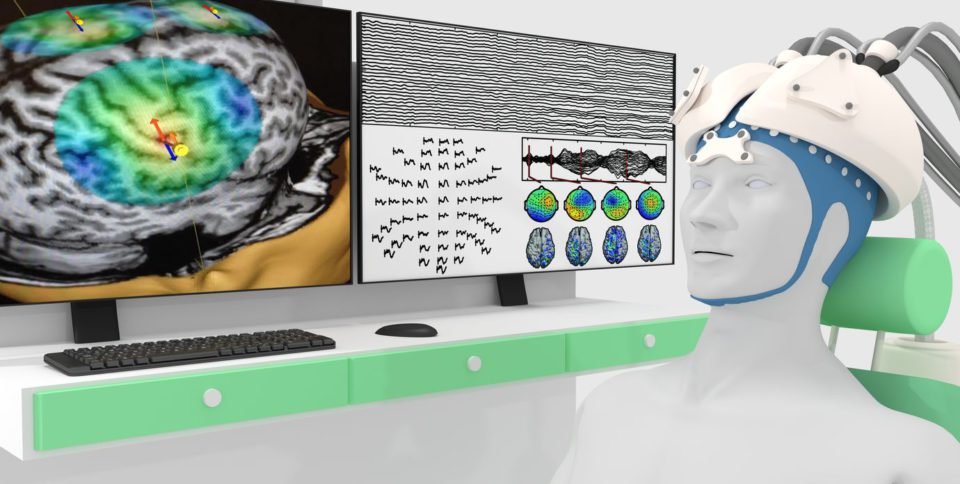 Patients who underwent a 5-week course of stimulation showed significant symptom relief on the Visual Analogue Scale (VAS) and an increase in the RIII pain reflex threshold. nine0013 The results of treatment were preserved after 3 weeks of treatment break.
Patients who underwent a 5-week course of stimulation showed significant symptom relief on the Visual Analogue Scale (VAS) and an increase in the RIII pain reflex threshold. nine0013 The results of treatment were preserved after 3 weeks of treatment break.
In 2013, the FDA praised the potential of TMS for the treatment of chronic headaches. Official approval of the use of transcranial magnetic stimulation for the treatment of pain will bring relief to millions of patients around the world.
TREATMENT OF AUTISM WITH TRANSCRANIAL MAGNETIC STIMULATION
Physicians stimulate the prefrontal cortex during treatment. It contains mirror neurons are a special type of cell that allows people to understand each other's moods, sympathize and empathize.
TMS improves children with low functioning autism ( Kanner's syndrome ) and high functioning autism ( Asperger's syndrome ). After 10 sessions, their MRI shows positive changes in the activation of mirror neurons.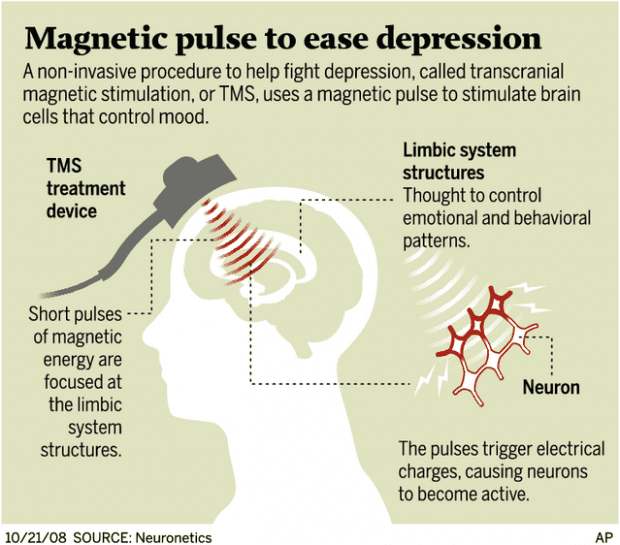
After the procedure, children begin to understand non-verbal signals better, their social skills improve. They show less anxiety when communicating with other people, the manifestation of repetitive monotonous movements is reduced. nine0005
TREATMENT OF ALZHEIMER'S DISEASE WITH TRANSCRANIAL MAGNETIC STIMULATION
Rhythmic TMS shows the greatest efficiency along with cognitive training. In Alzheimer's disease, magnetic impulses stimulate neurons in the temporal lobe, which is associated with the hippocampus, the part of the brain that is responsible for memory and storing memories.
According to clinical studies, as a result of transcranial stimulation, the patient's cognitive abilities improve by 4 points. nine0013 The effect lasts more than 5 months after completion of the course of treatment. Patients show improvements in listening to sentences, explaining actions, and naming objects.
In people with early-stage dementia, doctors have found significantly better cognitive performance than in people with intermediate or advanced dementia.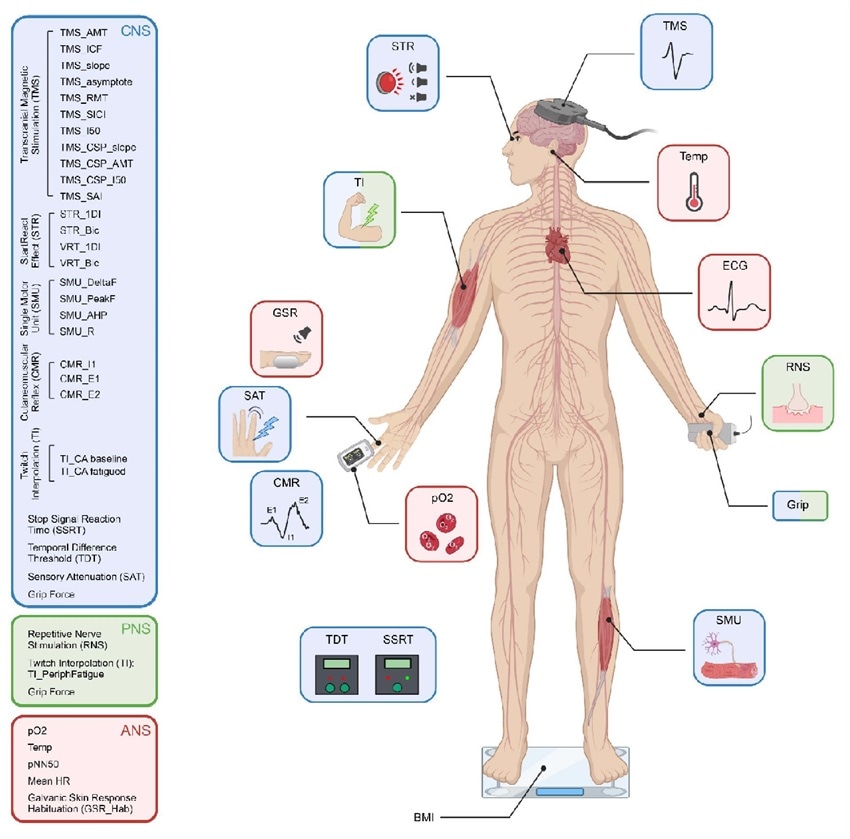
TREATMENT OF MULTIPLE SCLEROSIS WITH TRANSCRANIAL MAGNETIC STIMULATION
Multiple sclerosis is a common autoimmune disease that affects the central nervous system. As of 2020, approximately 2.3 million people worldwide suffer from this disease. nine0005
Medicines can only suppress some symptoms. So multiple sclerosis causes depression in 50% of patients. Depression increases the risk of suicide and prevents a person from investing all his strength in recovery.
The BrainsWay study showed that patients with multiple sclerosis improved after 6 weeks of transcranial magnetic stimulation. Depressive symptoms became less pronounced, fatigue disappeared. TMS stimulation of the motor cortex also helped patients temporarily improve walking skills. nine0005
Treatment of depressive episodes in multiple sclerosis is CE approved.
TREATMENT OF EPILEPSY WITH TRANSCRANIAL MAGNETIC STIMULATION
In patients with generalized epilepsy, the excitability of the cerebral cortex is increased.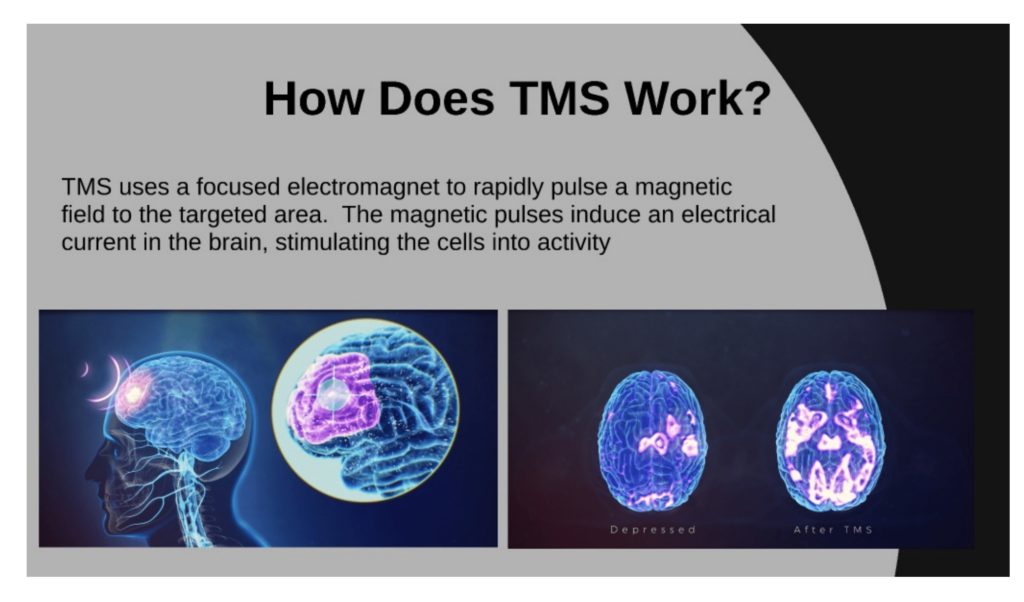 In order to reduce its activity, low-frequency rhythmic TMS is used.
In order to reduce its activity, low-frequency rhythmic TMS is used.
According to the statistics of American clinics, 80% of patients experience a decrease in seizure activity after a week's course. Research of the British organization Cochrane confirm that the risk of unwanted seizures in the treatment of epilepsy with magnetic pulses is very low.
In clinical studies, 8 out of 9 patients with myoclonic epilepsy had reduced frequency and severity of seizures after 5 days of rhythmic stimulation.
TREATMENT OF SCHIZOPHRENIA WITH TRANSCRANIAL MAGNETIC STIMULATION
In the treatment of schizophrenia, antipsychotic drugs are prescribed, which remove positive symptoms: hallucinations, exacerbations of perception, delirium, and so on. However, with schizophrenia, people also suffer from negative symptoms: mental decline, apathy, general lethargy. To date, the FDA has not approved any drugs to treat the negative symptoms of schizophrenia. nine0005
nine0005
Transcranial magnetic stimulation helps reduce negative symptoms of schizophrenia . To do this, with the help of a magnetic field, neurons in the prefrontal cortex are reactivated.
TMS also helps patients to get rid of auditory hallucinations . Neurologists have achieved improvement after reducing the activity of neurons in the temporoparietal region.
STROKE REHABILITATION USING TRANSCRANIAL MAGNETIC STIMULATION
According to World Health Organization statistics , stroke affects 15 million people every year. One third of them die, and the second third becomes incapacitated. Depending on which part of the brain has been affected, a person may lose the ability to walk, speak, see, navigate in space, understand someone else's speech, and so on. The use of transcranial magnetic stimulation in the rehabilitation of patients after a stroke will help restore some of these functions. nine0005
Clinical trial results are encouraging. High-frequency magnetic stimulation of the lower frontal lobe is effective for patients with aphasia after a stroke. After several weeks of courses, the patients again learned to correctly name objects .
High-frequency magnetic stimulation of the lower frontal lobe is effective for patients with aphasia after a stroke. After several weeks of courses, the patients again learned to correctly name objects .
Transcranial magnetic stimulation of the motor cortex helps patients restore walking skills . After TMS courses, patients showed a significant increase in walking speed. After a 4-week break in treatment, the results of the patients not only remained, but also improved due to regular physical training. nine0005
Stroke patient recovery with TMS is CE approved.
IN WHICH CLINICS IS TRANSCRANIAL MAGNETIC STIMULATION POSSIBLE?
For transcranial magnetic stimulation, contact:
Major depression and OCD can be treated at all clinics where TMS is available. Check with our MediGlobus coordinators about the possibility of treating other disorders in a particular clinic. nine0005
Summary
Transcranial magnetic stimulation is a non-invasive treatment for neurological and psychiatric disorders.
 It is offered to patients who have not been helped by medication, and surgery is too risky for health.
It is offered to patients who have not been helped by medication, and surgery is too risky for health. TMS creates a strong magnetic field that activates or inhibits the activity of neurons. This allows a person to form new skills or weaken the symptoms of the disease.
An important advantage of TMS is the low number of side effects compared to medication. After the procedure, patients complain of headache and tingling of the scalp, which go away on their own. Medicines affect the entire body and can cause emotional disturbances, fatigue, tension, and nausea. nine0002 For 2020, the FDA officially approved the treatment of major depression and obsessive-compulsive disorder using transcranial magnetic stimulation.
TMS can also be used to treat epilepsy, Alzheimer's disease, tremor, autism, Parkinson's disease, negative symptoms of schizophrenia, chronic pain, bipolar disorder. Studies of European clinics show promising results of the efficacy and safety of transcranial magnetic stimulation for these diseases.
 nine0002 Transcranial magnetic stimulation sessions are available at the Teknon Clinic in Spain, the Ichilov Medical Center in Israel, the American Hospital in Turkey and the Ludwig-Maximillian Clinic in Germany.
nine0002 Transcranial magnetic stimulation sessions are available at the Teknon Clinic in Spain, the Ichilov Medical Center in Israel, the American Hospital in Turkey and the Ludwig-Maximillian Clinic in Germany. Stay with MediGlobus and be aware of the latest news about the achievements of foreign medicine. If you need the help of a neurologist abroad, leave a request. Our coordinators will help you find a clinic that offers a helpful treatment program.
Get free consultation
Sources:
- 1. What is TMS
- 2. TMS under Parkinson
- 3. Tremore
- 4. TMPs for epilepsy
- 5.TMS for AUTISMED
- 5.TMS for AUTISME TMS for multiple sclerosis
- 7. TMS for affective disorder
- 8. TMS for schizophrenia
- 9. TMS for chronic pain
- 10. CE certification brainsway
- 11. FDA approval for OCD treatment
NeurologyGood to know
Dr. Vadim Berezhnoy
Vadim Berezhnoy
General practitioner, Medical expert, Head of the department of medical assistance.
Albina Golovina
Has been working in the field of medical copywriting for 2 years. She is a postgraduate student at the Faculty of Psychology. Author of several scientific publications in the field of clinical psychology. In addition, he studies the physiology of the central nervous system, neuropsychology and psychiatry. In his free time, he studies mindfulness practices and conducts psychological consultations. nine0004
similar posts
Results of the year - TOP -7 medical discoveries 2022
Read more
Early diagnosis of scattered sclerosis
Read more
transcranial stimulation of the brain in Moscow
Transcranial magnetic stimulation of the brain in Moscow: 70 clinics, price from 250 to 11900 rub (average 2526), record on transcranial magnetic stimulation of the brain. Choose a cheap clinic with the service "Transcranial Magnetic Brain Stimulation" near you and with good patient reviews. all prices for physiotherapy
Choose a cheap clinic with the service "Transcranial Magnetic Brain Stimulation" near you and with good patient reviews. all prices for physiotherapy
Clinic "Family" on Kievskaya
Enroll
The Family Clinic on Kievskaya in Moscow is located in the Dorogomilovo district. A multifunctional institution builds long-term relationships with patients and offers an individual approach. Reception is by appointment. The staff of the clinic… nine0444Transcranial magnetic stimulation of the brain from 3 000 ₽
Clinic "Family" - University Avenue 4
Enroll
Clinic "Family" University Avenue 4 is located in the central part of the Gagarinsky district of Moscow.This is a multidisciplinary institution, within the walls of which professional services are provided in the areas most in demand today ... nine0444
Transcranial magnetic stimulation of the brain from 3 000 ₽
Clinic "Family" at the River Station
Enroll
The Family Clinic at the River Station in Moscow is equipped with advanced imported equipment and certified medicines. Patients are treated by doctors with extensive experience. Patients of the Semeynaya clinic at the River Station are guaranteed individual… nine0444Transcranial magnetic stimulation of the brain from 3 000 ₽
Clinic "Family" on Ilyich Square
Enroll
The Family Clinic on Ilyich Square in Moscow is equipped with advanced equipment.Most specialists have academic degrees, higher medical categories. The Semeynaya clinic on Ilyich Square uses modern methods of diagnostics and treatment… nine0444
Transcranial magnetic stimulation of the brain from 3 000 ₽
"Clinic of Restorative Neurology"
Enroll
The company "Clinic of Restorative Neurology" is located on the territory of the Shchukinsky district of Moscow. It is a modern medical center specializing in the diagnosis and treatment of diseases associated with disorders of the nervous system… nine0444Transcranial magnetic stimulation of the brain from 600 ₽
Clinic "Family" - Kashirskoe shosse 56
Enroll
The clinic "Family" - Kashirskoye shosse 56 of the city of Moscow is equipped with advanced equipment.Most doctors have the highest medical categories and academic degrees. The clinic "Semeynaya" - Kashirskoe shosse 56 uses advanced methods of diagnostics and treatment… nine0444
Transcranial magnetic stimulation of the brain from 3 000 ₽
Clinic "Family" - Pervomayskaya 42
Enroll
The clinic "Family" - Pervomayskaya 42 of the city of Moscow is equipped with certified medicines and advanced equipment. Doctors with solid experience of work conduct reception. All patients of the clinic "Semeynaya" - Pervomayskaya 42 are guaranteed an individual and complex… nine0444Transcranial magnetic stimulation of the brain from 3 000 ₽
Center for Speech Neurology "NeuroSpectrum" Belyaevo
Enroll
The Center for Speech Neurology "NeuroSpektr" on Miklukho-Maklay is based in the Konkovo district, on the territory of the city of Moscow.This is a modern clinic that specializes in the treatment of problems related to speech and mental development. Reception of patients... nine0444
Transcranial magnetic stimulation of the brain from 3 500 ₽
Medical Center "Medicine of the Capital" in Maryino
Enroll
The Medical Center "Medicine of the Capital" in Maryino, Moscow, offers the help of highly qualified doctors, well-known specialists with an impeccable reputation and many years of experience. Acceptance is possible on the same day. The institution operates without… nine0444Transcranial magnetic stimulation of the brain from 1 900 ₽
Center for Speech Neurology "NeuroSpectrum" in Medvedkovo
Enroll
Children's Center "NeuroSpectr" is a center for children's speech neurology and rehabilitation.Experienced specialists of the Children's Center have created a corrective technique, including neurophysiological, pedagogical and hardware correction. With this technique… nine0444
Transcranial magnetic stimulation of the brain from 3 500 ₽
Clinic "NAKFF"
Enroll
The NAKFF clinic in Moscow is a modern multidisciplinary medical complex, fully equipped with expert-level equipment. Own laboratory available. The doctors of the NAKFF clinic practice an individual approach to patients. In cli… nine0444Transcranial magnetic stimulation of the brain from 2 625 ₽
Central Clinical Hospital "RZD-Medicine" on Budayskaya
Enroll
Central Clinical Hospital "RZD-Medicine" was founded in 1914 and is a laureate of the international award "Profession - Life".The long history of the hospital is closely connected with the names of many prominent figures in Russian medicine. Currently, in the structure of the hospital, the function… nine0444
Transcranial magnetic stimulation of the brain from 3 100 ₽
Clinic "Family" on Skhodnenskaya
Enroll
The Family Clinic in Moscow provides assistance in all major areas of medicine to men, women and children of any age. The clinic conducts high-quality instrumental and laboratory diagnostics of various diseases, as well as a wide… nine0444Transcranial magnetic stimulation of the brain from 3 000 ₽
Clinic "Cecile Plus"
Enroll
The Clinic of Neurology and Dentistry "Cecil Plus" in Moscow was founded in 2002 on the basis of the Research Institute of Neurosurgery named after Academician N.N. Burdenko. In the clinic of neurology and dentistry "Cecile +" highly qualified doctors work (8 candidates of medicine… nine0444
Transcranial magnetic stimulation of the brain from 3 200 ₽
European Medical Center on Spiridonievsky
Enroll
Clinic "EMC" on Spiridonievsky city of Moscow works around the clock and seven days a week. Treatment is carried out according to modern European and medical protocols. We have the necessary equipment for complex diagnostics. At the EMC clinic, no… nine0444Transcranial magnetic stimulation of the brain from 11 900 ₽
Central Clinical Hospital "RZD-Medicine" on Volokolamsk Highway
Enroll
The Central Clinical Hospital of JSC "Russian Railways" traces its history back to 1938, when the hospital was founded to provide highly qualified medical care to railway workers.Already by 1950, it included therapeutic, chi… nine0444
Transcranial magnetic stimulation of the brain from 3 100 ₽
European Medical Center on Orlovsky
Enroll
The EMC clinic on Orlovsky in Moscow provides high-tech medical care according to modern international models and standards. Qualified and experienced specialists of the clinic in their practice are guided by the latest methods of treatment. Mn… nine0444Transcranial magnetic stimulation of the brain from 11 900 ₽
Medical center "Mositalmed" on the Arbat
Enroll
For more than 25 years, the Mositalmed Medical Center in Moscow has been providing timely assistance in the treatment and diagnosis of diseases.