The adhd solution
The ADHD Solution Card Deck – Dr. Sharon Saline
How to use the ADHD Solution Card Deck!
The ADHD Solution Card Deck
Order online from PESI and Amazon.
Over 5,000 sold!
“Thank you Dr Sharon! We ordered your ADHD cards. Ever since our zoom meeting I feel lighter and I’m having a great time with my kids. I’m staying present and have been using your suggestions. I can’t wait for the cards to arrive! Sending you a sunshine hug from Florida!”
The ADHD Solution Deck offers effective strategies for reducing stress, building skills and fostering self-esteem. The cards provide adults with a unique window into what kids with ADHD are thinking, common problems they face, and how you can work with them to create lasting solutions.
Each card offers a quote from a child, teen or parent living with ADHD, a quick summary of a typical challenge, and a coping or intervention tool(s).
What is ADHD?
Attention-deficit/hyperactivity disorder (ADHD) is a biologically-based behavioral condition that impacts the management systems of the brain called executive functions. These functions include impulse and emotional control, working memory, initiation, time management, planning, organization, flexibility, sustained attention, and self-evaluation.
How to Use the Deck
The ADHD Solution Deck gives you practical tools to help kids with ADHD improve their abilities for regulating words and actions, managing feelings, initiating, planning, organizing, staying on task, improving working memory, increasing focus, and learning self-awareness.
The deck is divided into five color-coded suits to reflect the 5C’s approach:
Self- Control – Manage your own feelings first so you can act effectively and teach your child with ADHD to do the same.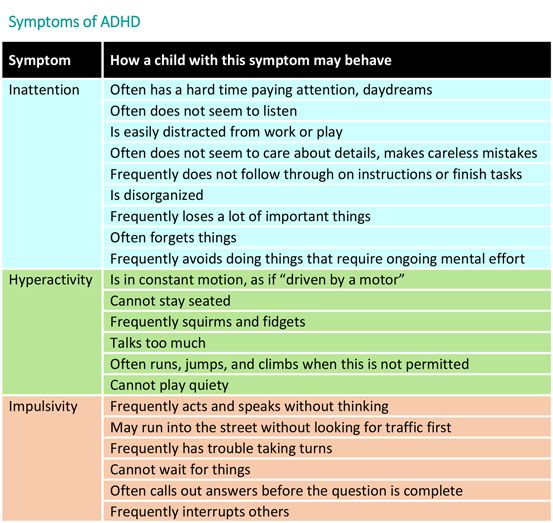
Compassion – Meet your child where they are, not where you expect them to be, with empathy and patience that’s appropriate to their stage of development.
Collaboration – Work together with your child to find solutions to daily concerns, using a “we” attitude instead of a “you should” approach. Make agreements about solutions with their input. Focus on changing one thing at a time.
Consistency – Do what you say you will do, as much as possible, without expecting perfection from yourself or your child. Aim for steadiness. Nurture your child’s efforts to do their best and focus on cause-and-effect learning. Notice and acknowledge what’s working by continuously offering words and actions ofnencouragement, praise, and validation. Identify traits, behaviors, or skills at which your child excels and nurture them.
Celebration – Notice and acknowledge what’s working by continuously offering words and actions of encouragement, praise, and validation. Identify traits, behaviors, or skills at which your child excels and nurture them.
Identify traits, behaviors, or skills at which your child excels and nurture them.
You can select a card at random at any given time for guidance and support or work in a specific category for a period of time. Learning new skills takes time and practice, so plan to revisit the cards.
Order cards from PESI and Amazon
How to use the ADHD Solution Card Deck with Laura, The ADHD Mama
Testimonial from Louise Clarke (Author of Parenting The Modern Teen & Podcast Host of Parenting In The Thick Of It)Check out Louise’s podcast episode featuring Dr. Sharon Saline!
“Dr. Sharon Saline has created a wonderful, innovative, and user-friendly tool for parents and families with ADHD. The ADHD Solution Deck indeed provides solutions. The cards provide powerful strategies and skills to better manage ADHD, bolster self-esteem, enhance family connections, and reduce stress. I love how the cards provide focus and assistance in five specific areas (Dr.
Saline’s famous “Five C’s model” of ADHD Parenting: self-control, compassion, collaboration, consistency, and celebration). Each card has a quote from a child or teen, defines a challenge, and then provides the tool to succeed in the area. The cards are colorful, perfectly sized, and engaging to promote repeated reading so the information can be absorbed over time until the skill is mastered. The cards are easier to read than a book, but still provide the vital tools to help families with ADHD thrive. Highly recommended!”
— Gene Carroccia, Psy.D.
“Great for Parents — This is awesome and great for therapists to use with parents of ADHDers. Highly recommended.”
— Katie Mc on Amazon
“A Great Tool to Help Parents and Kids in an ADHD Family — The ADHD Solution Deck is like an ADHD Parenting Coach in box!! At a loss for how to help your ADHD kid? Did you learn some great parenting skills, but seem to forget them when everything is “hitting the fan.
” When parents get stressed- for any reason- they can have difficulty remembering skills to help their ADHD kids. Dr. Saline’s cards provide proven tools and reminders to help parents and their kids manage the challenges of ADHD. If you can’t have Dr. Saline move in to help you in person, this is the next best thing!”
— Kirsten on Amazon
“Pick a Card – Any Card! — Managing ADHD is complicated, and sometimes you just need a helpful, little boost. Sharon Saline’s ADHD Solution Deck is fun to use. Pull a card in the morning and let it guide your parenting throughout the day; or pull a card instead of pulling your hair out when tensions start to rise. Manage your kids’ ADHD one strategy at a time!”
—
Elaine Taylor-Klaus, ImpactADHD®
“An incredible resource! — I am so grateful for this ADHD Solutions deck! I love how it offers not only practical tools and strategies, but also honest insights into what kids and parents are thinking and feeling, which helps support the very suggestions being offered.
This is a gem of a resource for parents, educators and therapists!”
— Debbie Zeichner, LCSW, Parent Coach and Mindfulness Instructor on Amazon
“A MUST-HAVE for parents of kids with ADHD! — Words can’t describe how much I wish The ADHD Solution Deck was available when my son was diagnosed with ADHD 12 years ago, or anytime since. The 5 themes Dr. Saline focuses are spot on for effective ADHD parenting. It’s a positive parenting approach that actually WORKS for kids with ADHD. If you want to help your child develop confidence and confidence so they can thrive, you must have The ADHD Solutions Deck in your parenting toolbox.”
— Penny Williams, Parenting ADHD & Autism, Parenting ADHD Coach & Award-Winning Author of 4 Books on ADHD, including “Boy Without Instructions” on Amazon
Treatment of ADHD | CDC
Get information and support from the National Resource Center on ADHD
My Child Has Been Diagnosed with ADHD – Now What?
When a child is diagnosed with attention-deficit/hyperactivity disorder (ADHD), parents often have concerns about which treatment is right for their child. ADHD can be managed with the right treatment. There are many treatment options, and what works best can depend on the individual child and family. To find the best options, it is recommended that parents work closely with others involved in their child’s life—healthcare providers, therapists, teachers, coaches, and other family members.
ADHD can be managed with the right treatment. There are many treatment options, and what works best can depend on the individual child and family. To find the best options, it is recommended that parents work closely with others involved in their child’s life—healthcare providers, therapists, teachers, coaches, and other family members.
Types of treatment for ADHD include
- Behavior therapy, including training for parents; and
- Medications.
Treatment recommendations for ADHD
For children with ADHD younger than 6 years of age, the American Academy of Pediatrics (AAP) recommends parent training in behavior management as the first line of treatment, before medication is tried. For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.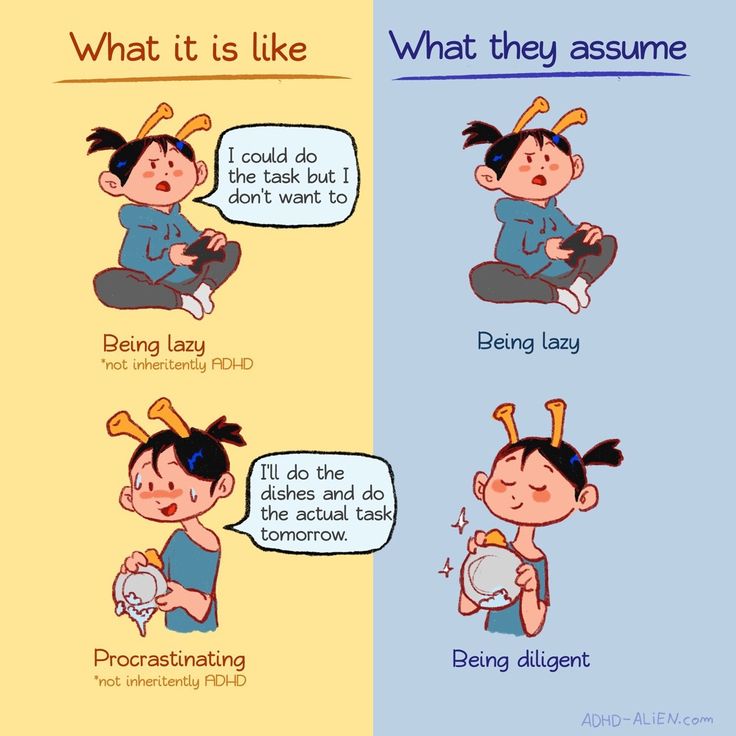 AAP recommendations also include adding behavioral classroom intervention and school supports. Learn more about how the school environment can be part of treatment.
AAP recommendations also include adding behavioral classroom intervention and school supports. Learn more about how the school environment can be part of treatment.
Good treatment plans will include close monitoring of whether and how much the treatment helps the child’s behavior, as well as making changes as needed along the way. To learn more about AAP recommendations for the treatment of children with ADHD, visit the Recommendations page.
Behavior Therapy, Including Training for Parents
ADHD affects not only a child’s ability to pay attention or sit still at school, it also affects relationships with family and other children. Children with ADHD often show behaviors that can be very disruptive to others. Behavior therapy is a treatment option that can help reduce these behaviors; it is often helpful to start behavior therapy as soon as a diagnosis is made.
The goals of behavior therapy are to learn or strengthen positive behaviors and eliminate unwanted or problem behaviors.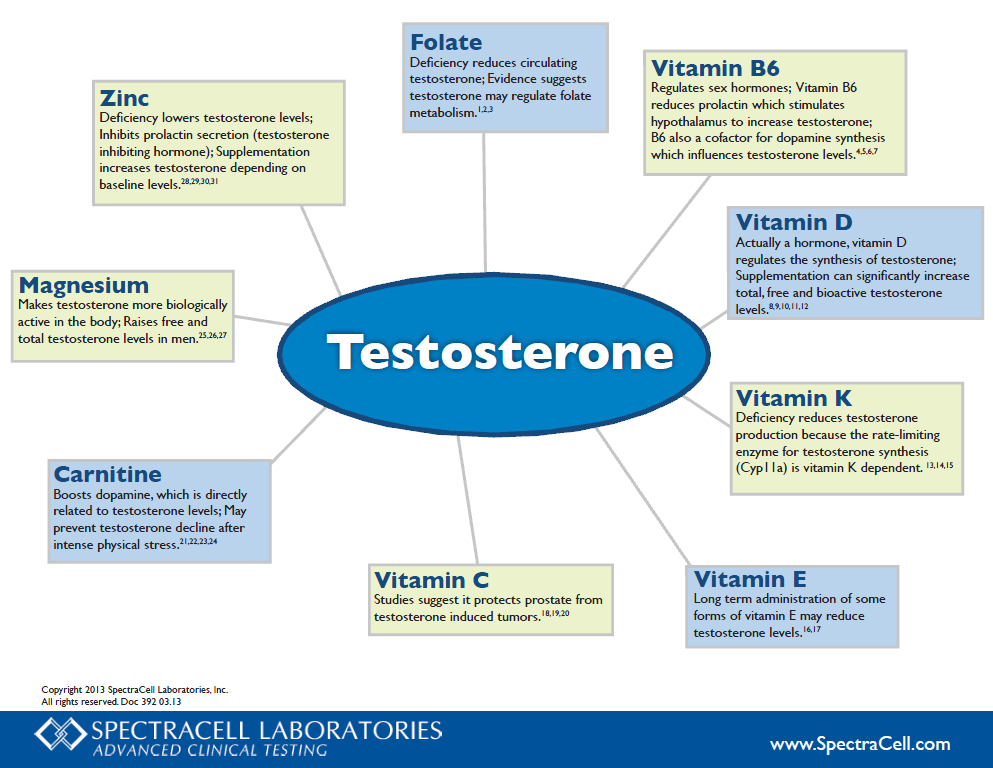 Behavior therapy for ADHD can include
Behavior therapy for ADHD can include
- Parent training in behavior management;
- Behavior therapy with children; and
- Behavioral interventions in the classroom.
These approaches can also be used together. For children who attend early childhood programs, it is usually most effective if parents and educators work together to help the child.
Children younger than 6 years of age
For young children with ADHD, behavior therapy is an important first step before trying medication because:
- Parent training in behavior management gives parents the skills and strategies to help their child.
- Parent training in behavior management has been shown to work as well as medication for ADHD in young children.
- Young children have more side effects from ADHD medications than older children.
- The long-term effects of ADHD medications on young children have not been well-studied.
Behavior Therapy for Younger and Older Children with ADHD [PDF – 466 KB]
School-age children and adolescents
For children ages 6 years and older, AAP recommends combining medication treatment with behavior therapy. Several types of behavior therapies are effective, including:
Several types of behavior therapies are effective, including:
- Parent training in behavior management;
- Behavioral interventions in the classroom;
- Peer interventions that focus on behavior; and
- Organizational skills training.
These approaches are often most effective if they are used together, depending on the needs of the individual child and the family.
Learn more about behavior therapy
Learn more about ADHD treatment and support in school
Read about the evidence for effective therapies for ADHD
Top of Page
Medications
Medication can help children manage their ADHD symptoms in their everyday life and can help them control the behaviors that cause difficulties with family, friends, and at school.
Several different types of medications are FDA-approved to treat ADHD in children as young as 6 years of age:
- Stimulants are the best-known and most widely used ADHD medications.
 Between 70-80% of children with ADHD have fewer ADHD symptoms when taking these fast-acting medications.
Between 70-80% of children with ADHD have fewer ADHD symptoms when taking these fast-acting medications. - Nonstimulants were approved for the treatment of ADHD in 2003. They do not work as quickly as stimulants, but their effect can last up to 24 hours.
Medications can affect children differently and can have side effects such as decreased appetite or sleep problems. One child may respond well to one medication, but not to another.
Healthcare providers who prescribe medication may need to try different medications and doses. The AAP recommends that healthcare providers observe and adjust the dose of medication to find the right balance between benefits and side effects. It is important for parents to work with their child’s healthcare providers to find the medication that works best for their child.
Top of Page
Parent Education and Support
CDC funds the National Resource Center on ADHD (NRC), a program of Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD).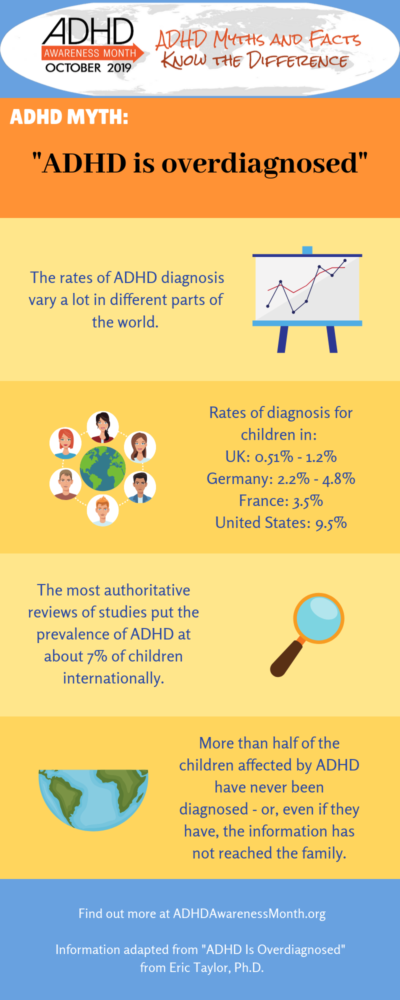 The NRC provides resources, information, and advice for parents on how to help their child. Learn more about the services of the NRC.
The NRC provides resources, information, and advice for parents on how to help their child. Learn more about the services of the NRC.
Tips for Parents
The following are suggestions that may help with your child’s behavior:
- Create a routine. Try to follow the same schedule every day, from wake-up time to bedtime.
- Get organized. Encourage your child to put schoolbags, clothing, and toys in the same place every day so that they will be less likely to lose them.
- Manage distractions. Turn off the TV, limit noise, and provide a clean workspace when your child is doing homework. Some children with ADHD learn well if they are moving or listening to background music. Watch your child and see what works.
- Limit choices. To help your child not feel overwhelmed or overstimulated, offer choices with only a few options. For example, have them choose between this outfit or that one, this meal or that one, or this toy or that one.
- Be clear and specific when you talk with your child. Let your child know you are listening by describing what you heard them say. Use clear, brief directions when they need to do something.
- Help your child plan. Break down complicated tasks into simpler, shorter steps. For long tasks, starting early and taking breaks may help limit stress.
- Use goals and praise or other rewards. Use a chart to list goals and track positive behaviors, then let your child know they have done well by telling them or by rewarding their efforts in other ways. Be sure the goals are realistic—small steps are important!
- Discipline effectively. Instead of scolding, yelling, or spanking, use effective directions, time-outs or removal of privileges as consequences for inappropriate behavior.
- Create positive opportunities. Children with ADHD may find certain situations stressful. Finding out and encouraging what your child does well—whether it’s school, sports, art, music, or play—can help create positive experiences.
- Provide a healthy lifestyle. Nutritious food, lots of physical activity, and sufficient sleep are important; they can help keep ADHD symptoms from getting worse.
Top of Page
ADHD in Adults
ADHD lasts into adulthood for at least one-third of children with ADHD1. Treatments for adults can include medication, psychotherapy, education or training, or a combination of treatments. For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHD and the National Institutes of Mental Health
More information
For more information on treatments, please click one of the following links:
National Resource Center on ADHD
National Institute of Mental Health
Information for parents from the American Academy of Pediatrics
References:
- Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: A prospective study.
 Pediatrics 2013;131(4):637-644.
Pediatrics 2013;131(4):637-644.
Parents typically attend 8-16 sessions with a therapist and learn strategies to help their child. Sessions may involve groups or individual families.
- The therapist meets regularly with the family to monitor progress and provide support
- Between sessions, parents practice using the skills they’ve learned from the therapist
After therapy ends families continue to experience improved behavior and reduced stress.
Attention Deficit Hyperactivity Disorder and Cognition
Nanda Rommels, PhD
Radboud University Medical Center, Department of Psychiatry, The Netherlands
(English). Translation: November 2015
Attention deficit hyperactivity disorder (ADHD) is characterized by a triad of symptoms: inattention, hyperactivity and impulsivity.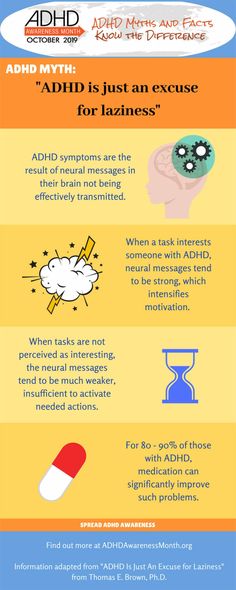 1 This disorder is highly heritable and affects about 3-5% of school-age children. 2.3 In recent decades, the cognitive problems of ADHD have been widely studied. Cognition can be defined as the acquisition of knowledge and its comprehension, including thinking, knowing, remembering, judging, and problem solving. nine0008
1 This disorder is highly heritable and affects about 3-5% of school-age children. 2.3 In recent decades, the cognitive problems of ADHD have been widely studied. Cognition can be defined as the acquisition of knowledge and its comprehension, including thinking, knowing, remembering, judging, and problem solving. nine0008
Subject
In an attempt to combine research findings on the biological and cognitive impairments common in ADHD, several causal models have been proposed. All proposed cognitive models agree that executive functioning (EF) impairments are one of the most significant characteristics of ADHD. EFs were defined as "those abilities that allow a person to successfully carry out independent and purposeful behavior, to act in their own interests." nine0014 4 Many studies of ADHD patients have documented UF impairments, with inhibition and working memory problems being the most common. 5 UV disturbances are closely associated with abnormalities in the prefrontal lobe and fronto-subcortical connections, which are often found in patients with ADHD.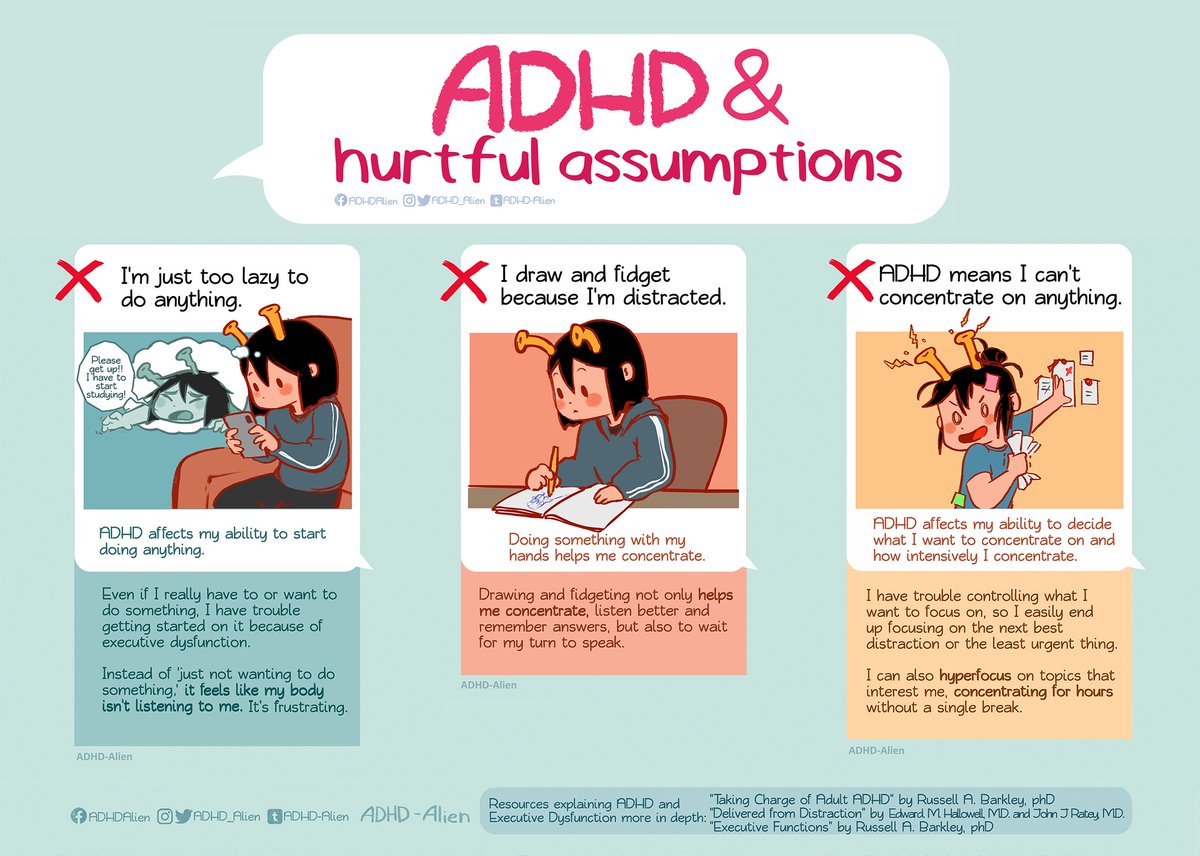 6.7
6.7
Issues
Although most causal models of ADHD include UV deficiency as an important factor, it is not really known whether ADHD is caused by UV deficiency, and to what extent. In other words, given that ADHD is a highly inherited disorder, is EF an inherited trait that increases the risk of developing ADHD, and for what percentage of patients would EF be a causative factor? nine0008
Key questions
Two questions are central to establishing a causal relationship between UV deficiency and ADHD:
- the same genes as ADHD?
- What percentage of children with ADHD actually suffer from UV problems?
Latest research results
Are UV problems hereditary, and are they linked to the same genes as ADHD?
Twin studies are the first necessary step to determine if UV deficiency is hereditary. This approach makes it possible to distinguish between the influence of hereditary and environmental factors on UV.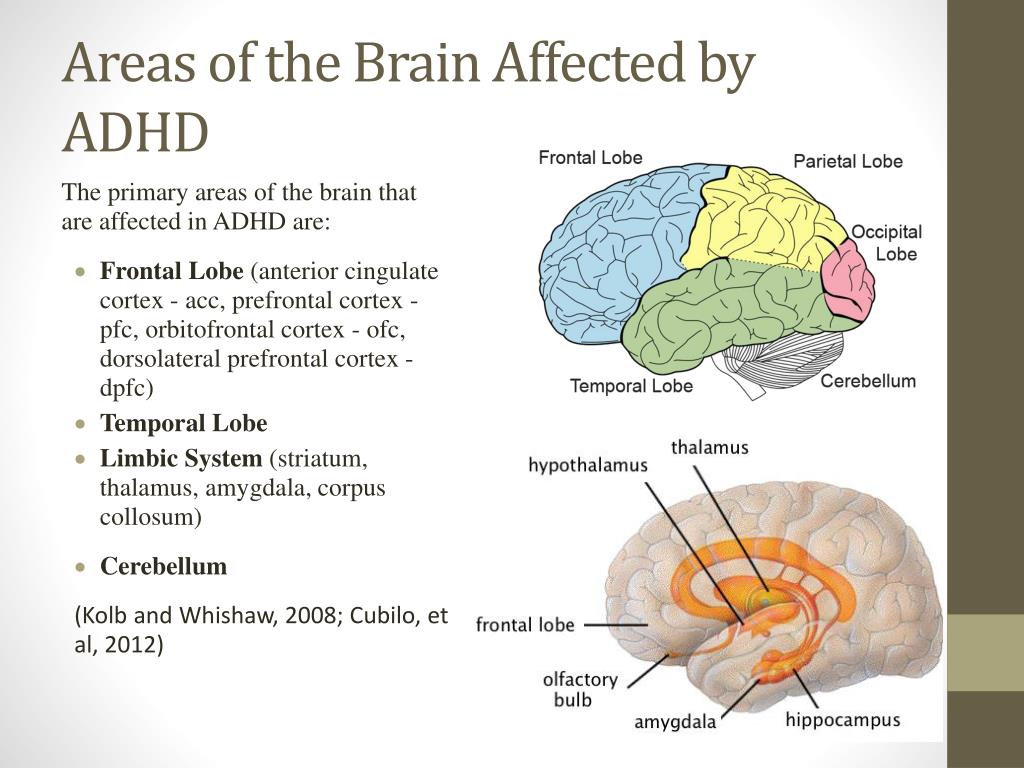 Problem solving on UV has been studied in several twin studies. 12-16 At ages 5 and 12, approximately 50% of success on multiple EF tasks was found to be related to genetic factors. nine0014 16 Other studies have found similar rates of 40 to 50%, 12,13,15 suggesting that success on EF tasks is moderately heritable. Moreover, genetic factors are an important mediator of UV resistance in childhood. 14
Problem solving on UV has been studied in several twin studies. 12-16 At ages 5 and 12, approximately 50% of success on multiple EF tasks was found to be related to genetic factors. nine0014 16 Other studies have found similar rates of 40 to 50%, 12,13,15 suggesting that success on EF tasks is moderately heritable. Moreover, genetic factors are an important mediator of UV resistance in childhood. 14
The second step to determine whether UV deficiency is inherited and related to the same genes as ADHD is to study the success of UV tasks in relatives of patients with ADHD. This sheds light on the familial nature of UV deficiency in ADHD. Siblings, for example, share up to 50% of the same genes on average. It is therefore possible that non-affected siblings of a child with ADHD carry risk genes without having the phenotypic manifestation of ADHD. If EF deficiency is indeed familial with ADHD, non-affected siblings will show the same EF deficiency, perhaps to a lesser extent than their ADHD siblings.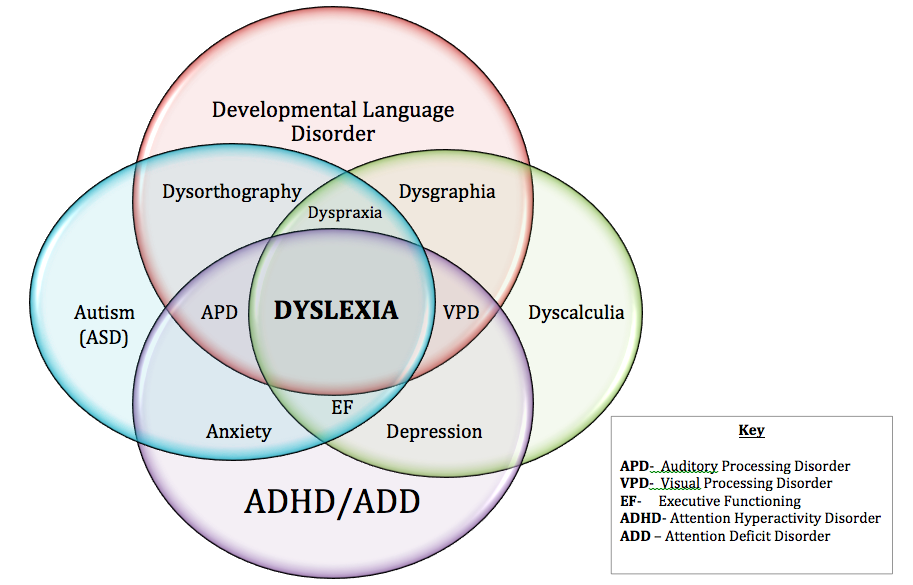 nine0008
nine0008
Several studies have specifically examined UV in families with ADHD, and the results support the hypothesis that UV deficiency is familial and is also present (to a lesser extent) in non-affected relatives of ADHD patients. 5.17-21 Studies specifically targeting inhibition control or intervention as an executive function have also produced encouraging results, with relatives finding similar results in performance and non-affected relatives showing minor weaknesses in this area. nine0014 22-26 These results suggest that UV deficiency is familial. Although these data are insufficient to suggest that UV problems are hereditary; but at least they are consistent with this hypothesis.
The last step in investigating whether UV deficiency is associated with the same genes as ADHD is to investigate the performance of UV against ADHD candidate genes and/or use UV performance to analyze linkage in pedigrees with a history of ADHD. Both of these strategies are rarely implemented due to the large sample size required for the statistical power they require. Preliminary results indicate that polymorphisms in a gene (the dopamine D4 receptor gene) that has been most reliably replicated for ADHD are in fact also related to UV. nine0014 15.27-30 One linkage study identified a genome-wide linkage trait on chromosome 13q12. 11 using the verbal working memory score in ADHD pedigrees, suggesting that genes at this location may influence both ADHD and the level of solving tasks on the UV. 31 In addition, another linkage study found that a region on chromosome 3q13 was associated with both composite UF and ADHD inattention symptoms, indicating that this lack of UF may be associated with the same genes which is ADHD. nine0014 32
Preliminary results indicate that polymorphisms in a gene (the dopamine D4 receptor gene) that has been most reliably replicated for ADHD are in fact also related to UV. nine0014 15.27-30 One linkage study identified a genome-wide linkage trait on chromosome 13q12. 11 using the verbal working memory score in ADHD pedigrees, suggesting that genes at this location may influence both ADHD and the level of solving tasks on the UV. 31 In addition, another linkage study found that a region on chromosome 3q13 was associated with both composite UF and ADHD inattention symptoms, indicating that this lack of UF may be associated with the same genes which is ADHD. nine0014 32
What percentage of children with ADHD have UV problems?
The percentage of children with ADHD who suffer from EF problems is highly dependent on the definition that there is an executive function deficit (DEF). 8 There is no agreement on what the DUV actually is, but most definitions imply performance below the 10th percentile level compared to a demographically matched control group on at least one, two, or three tasks per day.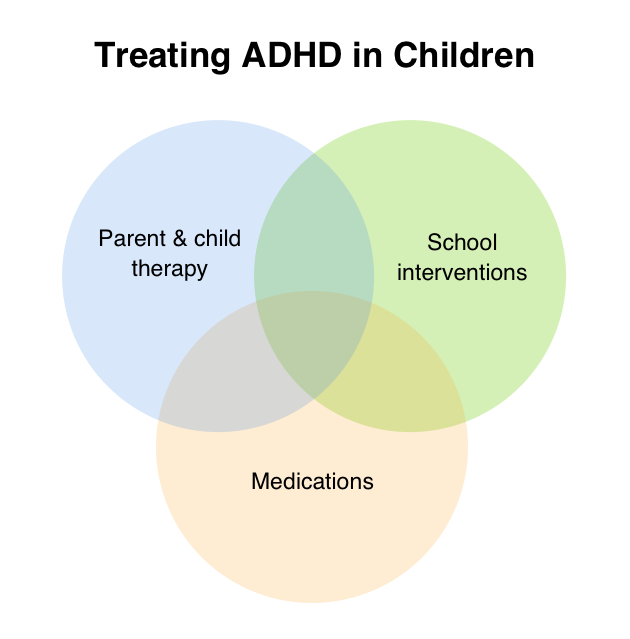 UV. At the group level, children with ADHD almost always perform worse on EF tasks than children in the control group. However, at the individual level, a certain proportion of children with ADHD outperform the corresponding proportion of children in the control group. nine0014 9 In other words, not every child with ADHD has DUV. Weaknesses in EF are not necessary or sufficient causes for all cases of ADHD. 9 Rather, other cognitive functions, motivational problems, or, in some cases, reactions to family distress or peer problems may lead to ADHD. 10.11 About a third of children have moderately severe DUV, diagnosed as having poor results on three or more UV measures. 11
UV. At the group level, children with ADHD almost always perform worse on EF tasks than children in the control group. However, at the individual level, a certain proportion of children with ADHD outperform the corresponding proportion of children in the control group. nine0014 9 In other words, not every child with ADHD has DUV. Weaknesses in EF are not necessary or sufficient causes for all cases of ADHD. 9 Rather, other cognitive functions, motivational problems, or, in some cases, reactions to family distress or peer problems may lead to ADHD. 10.11 About a third of children have moderately severe DUV, diagnosed as having poor results on three or more UV measures. 11
Unexplored areas
Determining whether the UV deficiency diagnosed in a proportion of patients with ADHD is the real cause of ADHD in this group requires a more comprehensive approach than has been used to date. This means that only a few studies have examined EF in a familial context, and most of them lacked the statistical power for genetic analysis.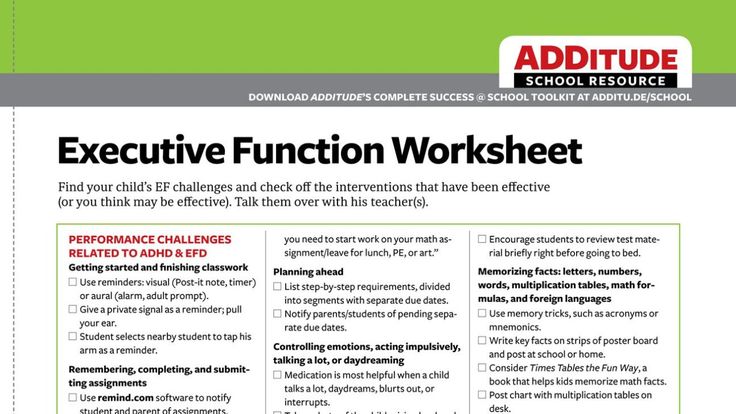 An even more serious problem is that their results are difficult to compare with each other due to the use of different tasks and methods to measure the same control function. This becomes a particularly acute problem when attempting to combine corpora of cognitive data obtained from different institutions in order to increase the statistical power of genetic analysis. Thus, in order to determine whether the EF deficiency diagnosed in a proportion of patients with ADHD is the real cause of ADHD, it is necessary to offer EF tasks that have good norms and data on validity, reliability, and heritability. The use of the same tasks in the spirit of the "gold standard" would allow the combination of samples from different research sites. This would greatly increase the comparability of data and increase the power of genetic analysis, leading to more reliable results that can hopefully be applied in clinical practice. nine0008
An even more serious problem is that their results are difficult to compare with each other due to the use of different tasks and methods to measure the same control function. This becomes a particularly acute problem when attempting to combine corpora of cognitive data obtained from different institutions in order to increase the statistical power of genetic analysis. Thus, in order to determine whether the EF deficiency diagnosed in a proportion of patients with ADHD is the real cause of ADHD, it is necessary to offer EF tasks that have good norms and data on validity, reliability, and heritability. The use of the same tasks in the spirit of the "gold standard" would allow the combination of samples from different research sites. This would greatly increase the comparability of data and increase the power of genetic analysis, leading to more reliable results that can hopefully be applied in clinical practice. nine0008
Conclusions
Success on EF tasks is moderately heritable, and genetic factors are an important mediator of EF resistance in childhood. Recommendations for parents, services and administrative policies Cognitive tests are not yet fine-tuned and narrow enough to be used in the daily practice of diagnosing ADHD. We still need to rely on parent and teacher reports (or self-reports of teenagers and adults with suspected ADHD) for diagnosis. However, recent data from longitudinal studies indicate that childhood EF is predictive of future academic achievement, social functioning, and general functioning in patients with ADHD. nine0014 33 As these results suggest, diagnosing and treating EF disorders may benefit clinical practice, especially in cases with a high risk of negative outcome, to prevent long-term problems in important areas of life functioning. Literature  UV deficiency is associated with ADHD within the family and may be related, among other things, to the dopamine D4 receptor gene, which is also related to ADHD. In other words, a (partly) genetic UV deficiency can cause ADHD. However, only a certain subset of patients with ADHD (about 30%) suffer from moderately severe EF problems, indicating that EF weaknesses are not necessary or sufficient causes responsible for all cases of ADHD. nine0008
UV deficiency is associated with ADHD within the family and may be related, among other things, to the dopamine D4 receptor gene, which is also related to ADHD. In other words, a (partly) genetic UV deficiency can cause ADHD. However, only a certain subset of patients with ADHD (about 30%) suffer from moderately severe EF problems, indicating that EF weaknesses are not necessary or sufficient causes responsible for all cases of ADHD. nine0008 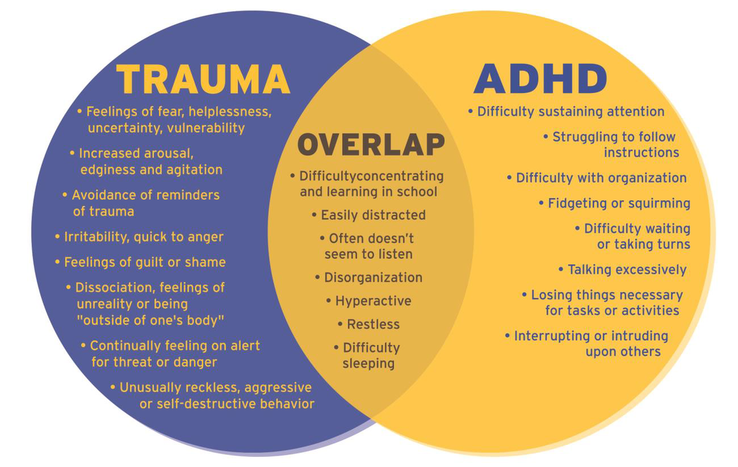 33 Strategies for corrective interventions to address UV deficiency are still in the early stages of development, but positive results have already been obtained. 34.35 These interventions may be useful for the subgroup of children with ADHD who suffer from moderately severe UV deficiency (+/- 30%). nine0008
33 Strategies for corrective interventions to address UV deficiency are still in the early stages of development, but positive results have already been obtained. 34.35 These interventions may be useful for the subgroup of children with ADHD who suffer from moderately severe UV deficiency (+/- 30%). nine0008
2005;57(11):1313-1323.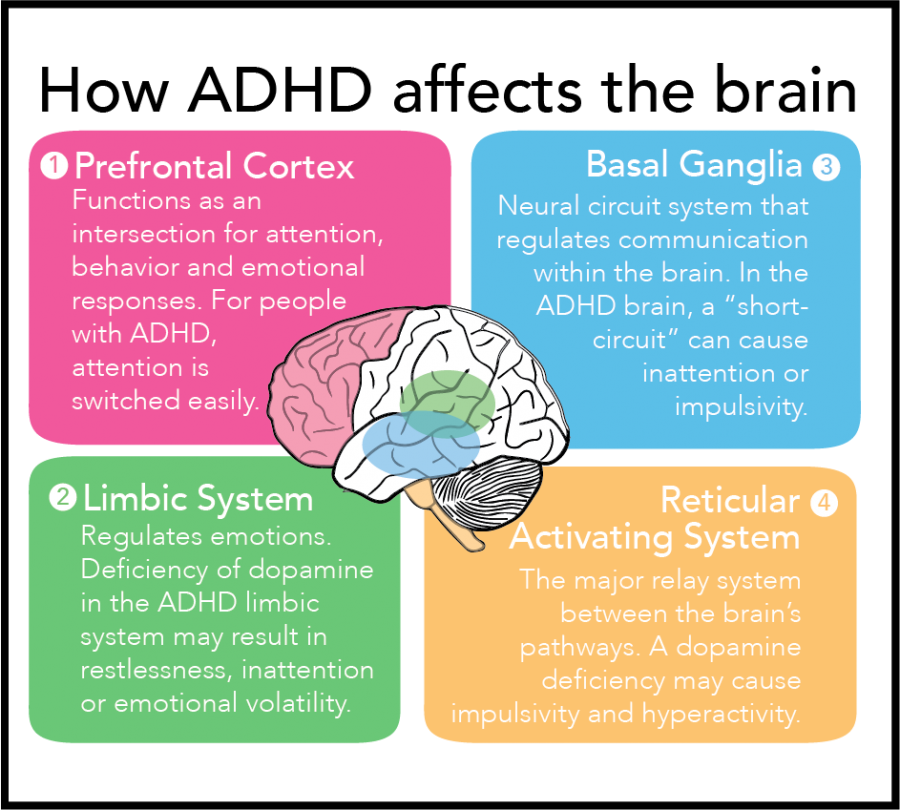
 Journal of Consulting and Clinical Psychology 2004;72(5):757-766.
Journal of Consulting and Clinical Psychology 2004;72(5):757-766.  nine0054 Twin Research and Human Genetics 2007;10(6):829-834.
nine0054 Twin Research and Human Genetics 2007;10(6):829-834. 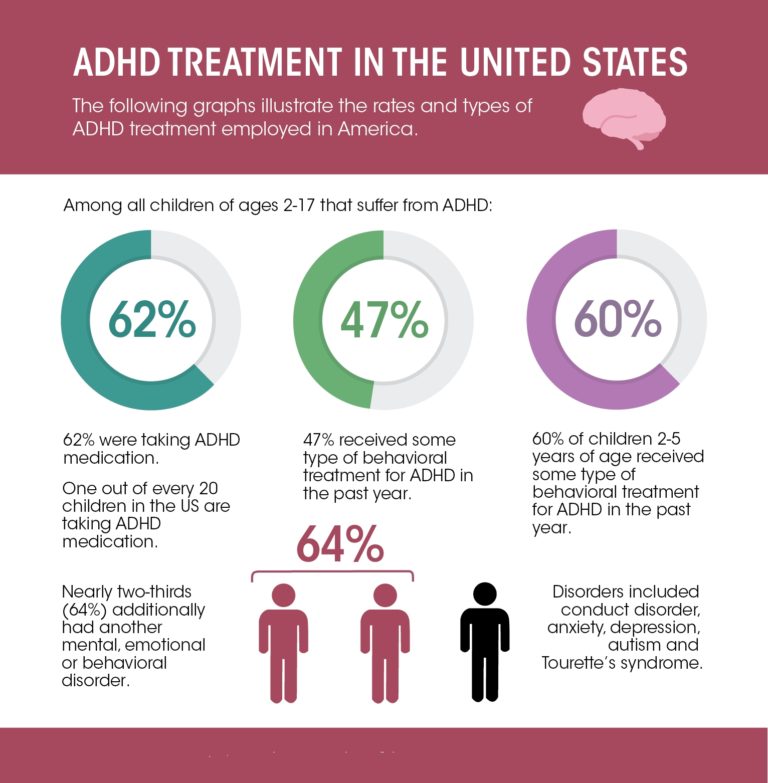 nine0054 Journal of Abnormal Psychology 2000;109(2):252-265.
nine0054 Journal of Abnormal Psychology 2000;109(2):252-265.  Performance variability, impulsivity errors and the impact of incentives as gender-independent endophenotypes for ADHD. nine0054 Journal of Child Psychology and Psychiatry 2010;51(2):210-218.
Performance variability, impulsivity errors and the impact of incentives as gender-independent endophenotypes for ADHD. nine0054 Journal of Child Psychology and Psychiatry 2010;51(2):210-218. 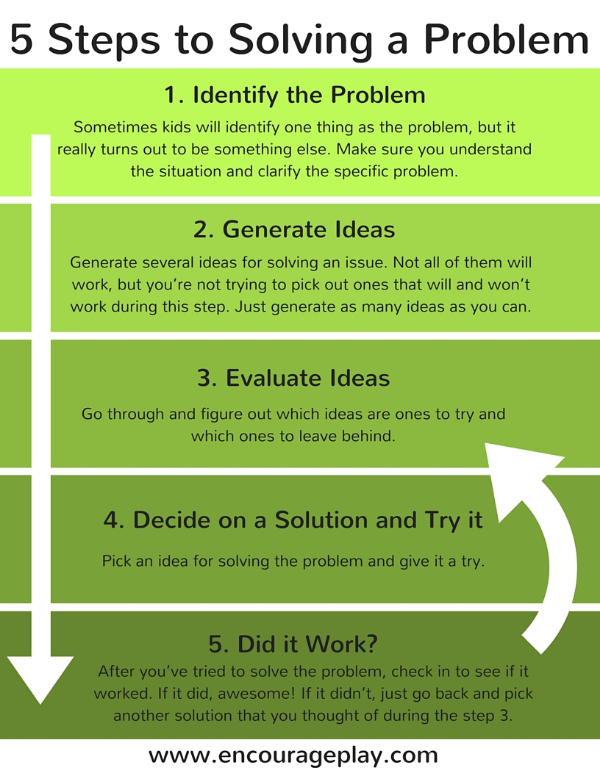 Inhibition of motor responses in siblings concordant and discordant for Attention Deficit Hyperactivity Disorder. nine0054 American Journal of Psychiatry 2005;162(6):1076-1082.
Inhibition of motor responses in siblings concordant and discordant for Attention Deficit Hyperactivity Disorder. nine0054 American Journal of Psychiatry 2005;162(6):1076-1082.  Journal of Child Psychology and Psychiatry . In press.
Journal of Child Psychology and Psychiatry . In press. 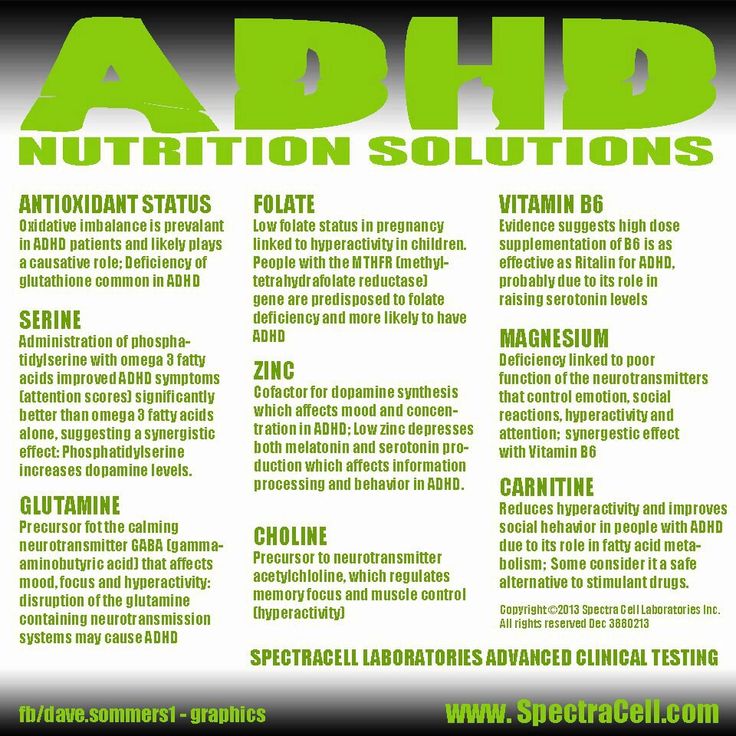 Multivariate genomewide linkage scan of neurocognitive traits and ADHD symptoms: suggestive linkage to 3q13. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics 2008;147B(8):1399-1411.
Multivariate genomewide linkage scan of neurocognitive traits and ADHD symptoms: suggestive linkage to 3q13. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics 2008;147B(8):1399-1411. 
A good solution to the problem of ADHD ⋆ School of Journalism
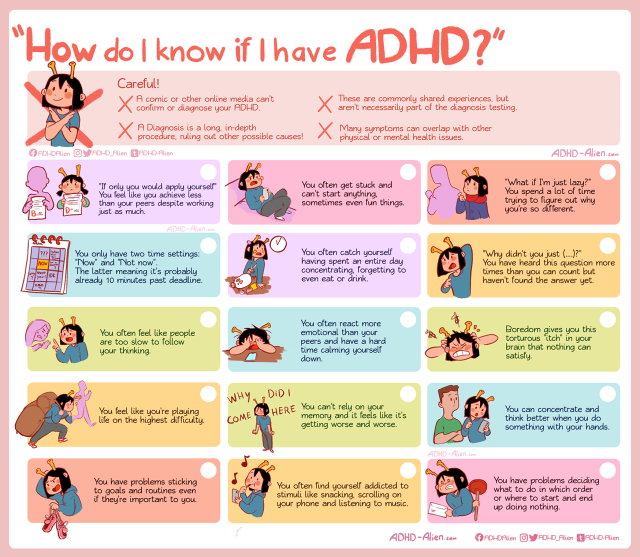
These children are very mobile and talkative. At the first glance at them, adults smile and are surprised at their activity. Watching them for longer, we understand that they are overly active, cause a lot of inconvenience to their parents and their behavior looks strange. Attention Deficit Hyperactivity Disorder (ADHD) - Many parents are frightened by this diagnosis, some of them refuse to admit that their children have problems that require the attention of specialists. nine0008
And if teachers and specialists can identify such children with their “trained” look, then children with attention deficit disorder, but without hyperactivity (ADD) do not attract attention to themselves, their features sometimes go unnoticed. As a rule, these are calm, quiet girls, although attention deficit disorder without hyperactivity disorder also occurs in boys.
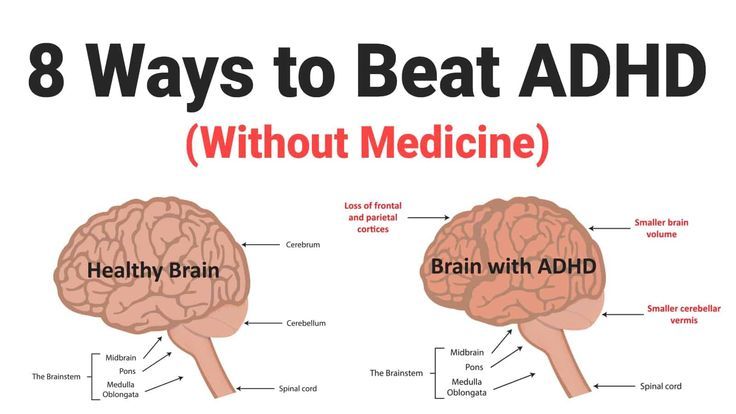
What is it and does it require treatment? ADHD is a neurological-behavioral developmental disorder that begins in childhood.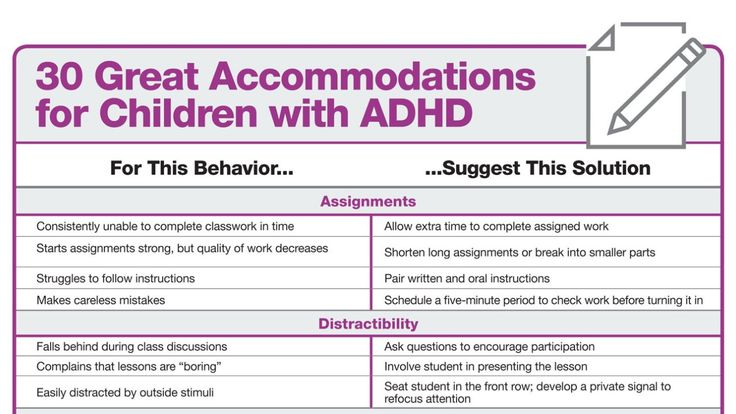 At the level of neurotransmitter balance in ADHD, the levels of dopamine and norepinephrine are reduced. The well-known American neurologist and psychiatrist, author of many bestsellers on this topic, J. Amen writes that in ADHD, there is low activity in the frontal cortex. Some children outgrow ADHD and adjust to it over the years. But most of them, having matured, experience some or other difficulties associated with ADHD. nine0008
At the level of neurotransmitter balance in ADHD, the levels of dopamine and norepinephrine are reduced. The well-known American neurologist and psychiatrist, author of many bestsellers on this topic, J. Amen writes that in ADHD, there is low activity in the frontal cortex. Some children outgrow ADHD and adjust to it over the years. But most of them, having matured, experience some or other difficulties associated with ADHD. nine0008
In practice, the syndrome is expressed in inability to concentrate, restlessness, talkativeness or, on the contrary, isolation, difficulties in learning and contacts with people, and many other unpleasant manifestations.
Attention deficit signs:
Inability to focus on details
Inattention errors.
Inability to listen to addressed speech.
Inability to complete tasks.
Poor organizational skills.
Negative attitude to tasks that require mental effort. nine0004 Loss of essential items while completing a mission.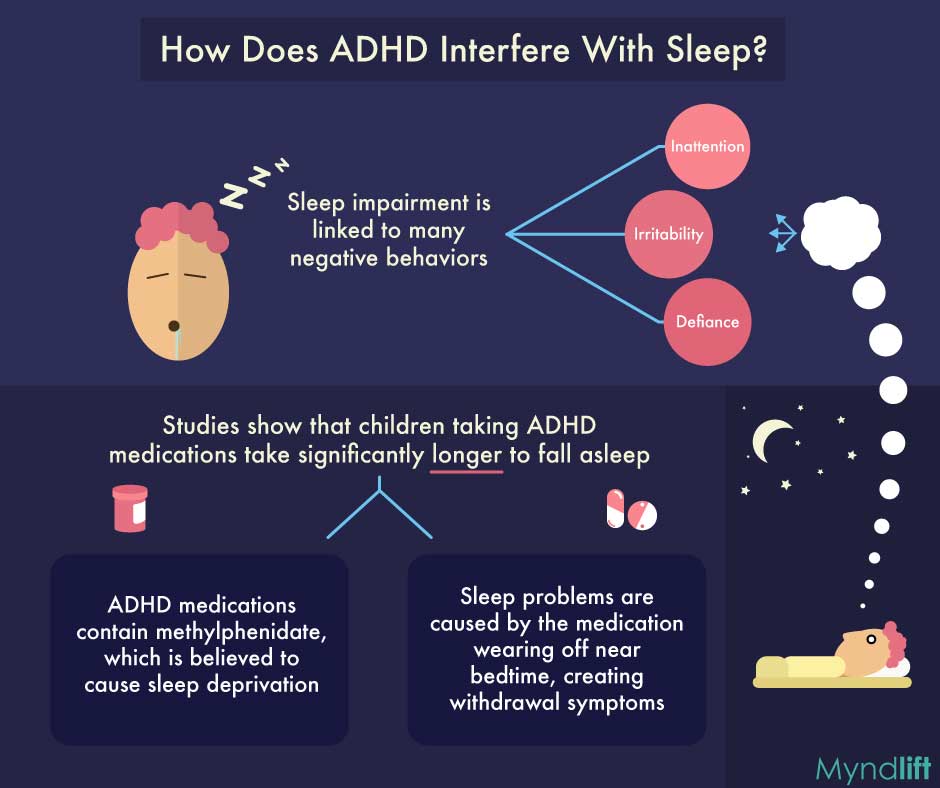
Distractibility to extraneous stimuli.
forgetfulness.
Hyperactivity:
Fussy movements of arms and legs.
Frequent jumping up from one's seat.
Hypermobility in situations where hypermobility is unacceptable.
Inability to play silent games.
Constantly on the move.
Verbose.
Impulsivity:
Aspiration to answer a question without listening to it. nine0004 Inability to wait for one's turn.
Intrusion into the conversations and games of others.
Taking actions without assessing possible consequences.
At the same time, ADHD and ADHD are the same disorder, but manifested in different ways. It is believed that for effective treatment it is necessary to combine medication, psychotherapy and various methods of rehabilitation. Among the latter, in the West, the most promising are special computer programs that correct the child's behavior, improve blood supply to the frontal lobes of the brain, and restore neurotransmitter balance. nine0008
nine0008
And if the use of amphetamine psychostimulants, practiced in the US and European countries for this disorder, causes a lot of criticism and is not used in the CIS countries, then the use of special programs is perceived positively by all specialists. They have no contraindications and side effects, and in terms of effectiveness they are not inferior to medicines.
There are some foreign computer programs, but they are expensive and not suitable for Russian speaking patients. Among the programs in Russian, a unique development by a child psychologist and defectologist at the Institute of Special Psychology and Pedagogy, Yulia Milovanova, stands out. The author of the program has many years of successful experience working with children and adolescents diagnosed with ADHD. The program with the cheerful name "Focusballs" improves all the functions of attention and memory and works online via the Internet. nine0008
Exercises include following objects (visual and auditory), performing actions on objects and receiving feedback - reporting errors, scoring a task in percentage, etc. Progress statistics are kept in the training, where you can see all the grades received. There is a professional support of a psychologist who monitors the results and gives the necessary recommendations for progress in the training. Individual online counseling is possible. Feedback on the program is encouraging. nine0008
Progress statistics are kept in the training, where you can see all the grades received. There is a professional support of a psychologist who monitors the results and gives the necessary recommendations for progress in the training. Individual online counseling is possible. Feedback on the program is encouraging. nine0008
“My wife purchased the program for my youngest son,” says Denis Ozerov. - With my son, everything is really very difficult - ADHD flourished, interfering with full-fledged studies. Even just 5 minutes to focus on reading a book was a challenge for us. Now, at least with a tutor, we are able to study and cope with the curriculum.”
“At the age of 4, we noticed that it was difficult for Dani to draw and memorize poems,” says the mother of 7-year-old Daniel. - At the age of 5 and 6, he still did not want to play board games on his own (drawing, Lego, puzzles, etc.), he had to be guided. It was necessary to repeat several times before he would fulfill the request.