Symptoms of type 2 bipolar disorder
Symptoms, Treatments, Causes, and More
Written by Matthew Hoffman, MD
In this Article
- What Is Bipolar II Disorder?
- Who Is at Risk for Bipolar II Disorder?
- What Are the Symptoms of Bipolar II Disorder?
- What Are the Treatments for Bipolar II Disorder?
- Can Bipolar II Disorder Be Prevented?
- How Is Bipolar II Disorder Different From Other Types of Bipolar Disorder?
What Is Bipolar II Disorder?
Bipolar II disorder (pronounced "bipolar two") is a form of mental illness. Bipolar II is similar to bipolar I disorder, with moods cycling between high and low over time.
However, in bipolar II disorder, the "up" moods never reach full-blown mania. The less-intense elevated moods in bipolar II disorder are called hypomanic episodes, or hypomania.
A person affected by bipolar II disorder has had at least one hypomanic episode in their life. Most people with bipolar II disorder suffer more often from episodes of depression. This is where the term "manic depression" comes from.
In between episodes of hypomania and depression, many people with bipolar II disorder typically live normal lives.
A Visual Guide to Understanding Bipolar Disorder
Who Is at Risk for Bipolar II Disorder?
Virtually anyone can develop bipolar II disorder. About 2.5% of the U.S. population suffers from some form of bipolar disorder - nearly 6 million people.
Most people are in their teens or early 20s when symptoms of bipolar disorder first start. Nearly everyone with bipolar II disorder develops it before age 50. People with an immediate family member who has bipolar are at higher risk.
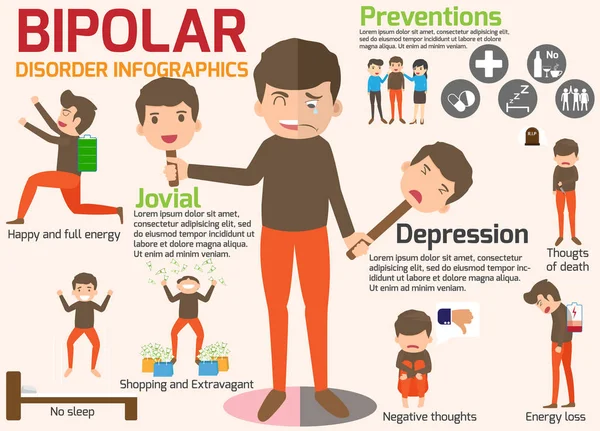
What Are the Symptoms of Bipolar II Disorder?
During a hypomanic episode, elevated mood can manifest itself as either euphoria (feeling "high") or as irritability.
Symptoms during hypomanic episodes include:
- Flying suddenly from one idea to the next
- Having exaggerated self confidence
- Rapid, "pressured" (uninterruptible) and loud speech
- Increased energy, with hyperactivity and a decreased need for sleep
People experiencing hypomanic episodes are often quite pleasant to be around.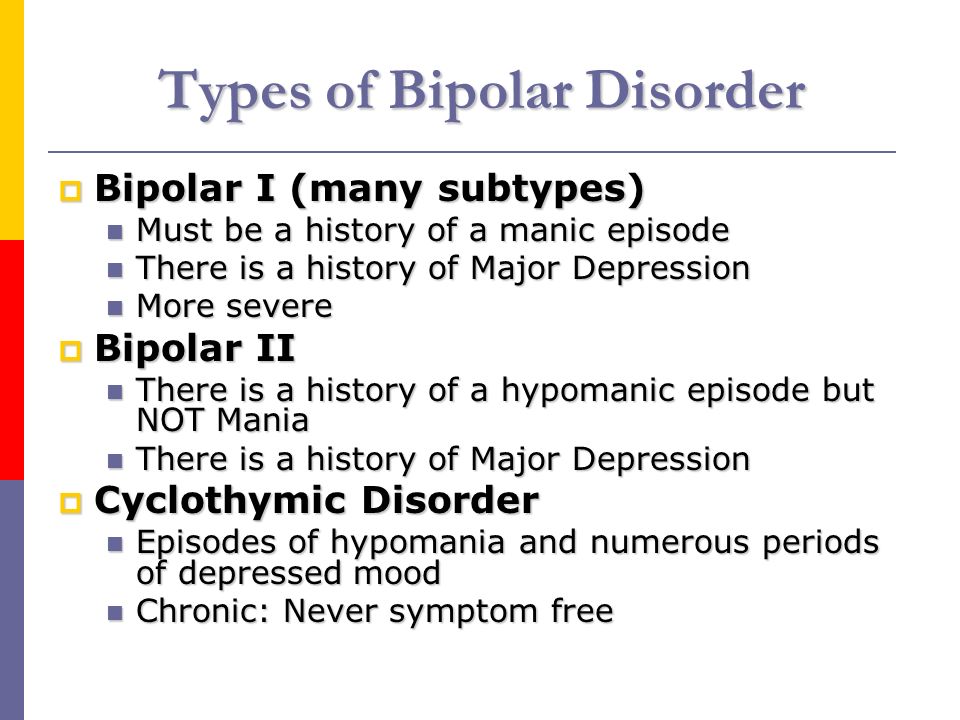 They can often seem like the "life of the party" -- making jokes, taking an intense interest in other people and activities, and infecting others with their positive mood.
They can often seem like the "life of the party" -- making jokes, taking an intense interest in other people and activities, and infecting others with their positive mood.
What's so bad about that, you might ask? Hypomania can also lead to erratic and unhealthy behavior. Hypomanic episodes can sometimes progress onward to full manias that affect a person's ability to function (bipolar I disorder). In mania, people might spend money they don't have, seek out sex with people they normally wouldn't, and engage in other impulsive or risky behaviors with the potential for dangerous consequences.
The vast majority of people with bipolar II disorder experience more time with depressive than hypomanic symptoms. Depressions can occur soon after hypomania subsides, or much later. Some people cycle back and forth between hypomania and depression, while others have long periods of normal mood in between episodes.
Untreated, an episode of hypomania can last anywhere from a few days to several months.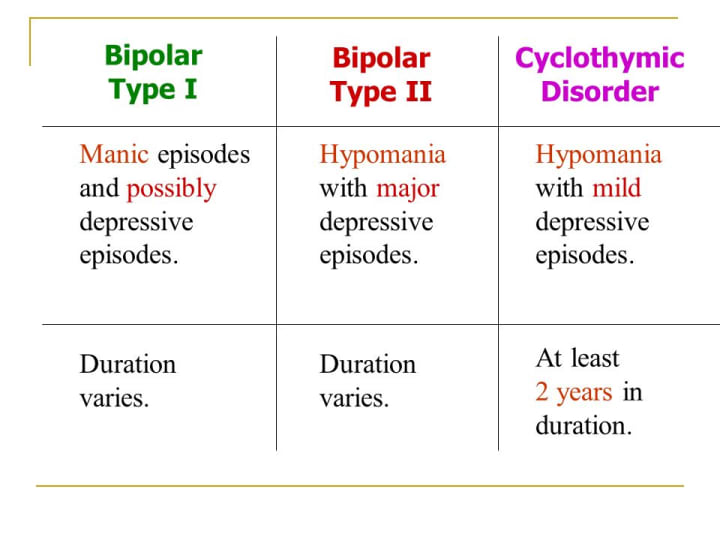 Most commonly, symptoms continue for a few weeks to a few months.
Most commonly, symptoms continue for a few weeks to a few months.
Depressive episodes in bipolar II disorder are similar to "regular" clinical depression, with depressed mood, loss of pleasure, low energy and activity, feelings of guilt or worthlessness, and thoughts of suicide. Depressive symptoms of bipolar disorder can last weeks, months, or rarely years.
What Are the Treatments for Bipolar II Disorder?
Hypomania often masquerades as happiness and relentless optimism. When hypomania is not causing unhealthy behavior, it often may go unnoticed and therefore remain untreated. This is in contrast to full mania, which by definition causes problems in functioning and requires treatment with medications and possibly hospitalizations.
People with bipolar II disorder can benefit from preventive drugs that level out moods over the long term. These prevent the negative consequences of hypomania, and also help to prevent episodes of depression.
Mood Stabilizers
Lithium (Eskalith, Lithobid): This simple metal in pill form is highly effective at controlling mood swings (particularly highs) in bipolar disorder. Lithium has been used for more than 60 years to treat bipolar disorder. Lithium can take weeks to work fully, making it better for long-term treatment than for acute hypomanic episodes. Blood levels of lithium and other laboratory tests (such as kidney and thyroid functioning) must be monitored periodically to avoid side effects.
Lithium has been used for more than 60 years to treat bipolar disorder. Lithium can take weeks to work fully, making it better for long-term treatment than for acute hypomanic episodes. Blood levels of lithium and other laboratory tests (such as kidney and thyroid functioning) must be monitored periodically to avoid side effects.
Carbamazepine (Tegretol): This antiseizure drug has been used to treat mania since the 1970s. It's possible value for treating bipolar depression, or preventing future highs and lows, is less well-established. Blood tests to monitor liver functioning and white blood cell counts also are periodically necessary.
Lamotrigine (Lamictal): This drug is approved by the FDA for the maintenance treatment of adults with bipolar disorder. It has been found to help delay bouts of mood episodes of depression, mania, hypomania (a milder form of mania), and mixed episodes in people being treated with standard therapy. It is especially helpful in preventing lows.
Valproate (Depakote): This antiseizure drug also works to level out moods.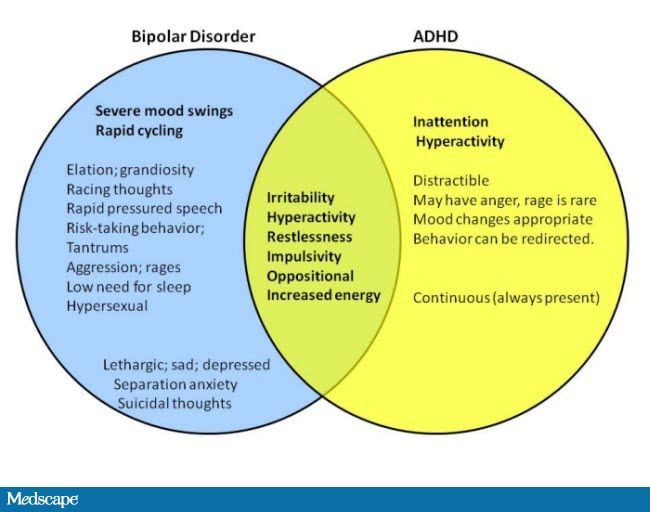 It has a more rapid onset of action than lithium, and it can also be used "off label" for prevention of highs and lows.
It has a more rapid onset of action than lithium, and it can also be used "off label" for prevention of highs and lows.
Some other antiseizure medications, such as oxcarbazepine (Trileptal), are also sometimes prescribed as "experimental" (less-proven) treatments for mood symptoms or associated features in people with bipolar disorder.
Antipsychotics
By definition, hypomanic episodes do not involve psychosis and do not interfere with functioning. Antipsychotic drugs, such as aripiprazole (Abilify), asenapine (Saphris), cariprazine (Vraylar), lumateperone (Caplyta), quetiapine (Seroquel), olanzapine (Zyprexa), risperidone (Risperdal), and ziprasidone (Geodon) and others, are nevertheless sometimes used in hypomania and some (notably, Caplyta and Seroquel) are used for depression in bipolar II disorder.
Benzodiazepines
This class of drugs includes alprazolam (Xanax), diazepam (Valium), and lorazepam (Ativan) and is commonly referred to as minor tranquilizers. They are used for short-term control of acute symptoms associated with hypomania such as insomnia or agitation.
They are used for short-term control of acute symptoms associated with hypomania such as insomnia or agitation.
Antidepressants
Seroquel and Seroquel XR are the only medications FDA-approved specifically for bipolar II depression. Common antidepressants such as fluoxetine (Prozac), paroxetine (Paxil), and sertraline (Zoloft) are also sometimes used in bipolar II depression, and are thought to be less likely to cause or worsen hypomania than is the case in bipolar I disorder. Psychotherapy, such as cognitive-behavioral therapy, may also help.
Because bipolar II disorder typically involves recurrent episodes, continuous and ongoing treatment with medicines is often recommended for relapse prevention.
Can Bipolar II Disorder Be Prevented?
The causes of bipolar disorder are not well understood. It's not known if bipolar II disorder can be prevented entirely.
It is possible to reduce the risk for developing future episodes of hypomania or depression once bipolar disorder has developed.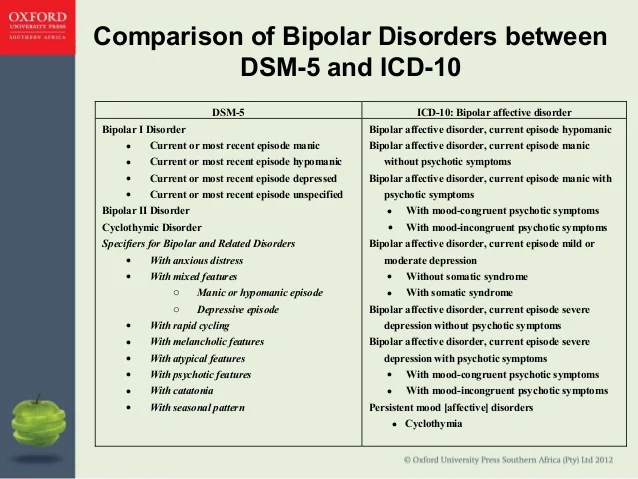 Regular therapy sessions with a psychologist or social worker, in combination with medication, can help efforts to stabilize mood, leading to fewer hospitalizations and feeling better overall. Psychotherapy can help people better recognize the warning signs of a developing relapse before it takes hold, and can also help to ensure that prescribed medicines are being taken properly.
Regular therapy sessions with a psychologist or social worker, in combination with medication, can help efforts to stabilize mood, leading to fewer hospitalizations and feeling better overall. Psychotherapy can help people better recognize the warning signs of a developing relapse before it takes hold, and can also help to ensure that prescribed medicines are being taken properly.
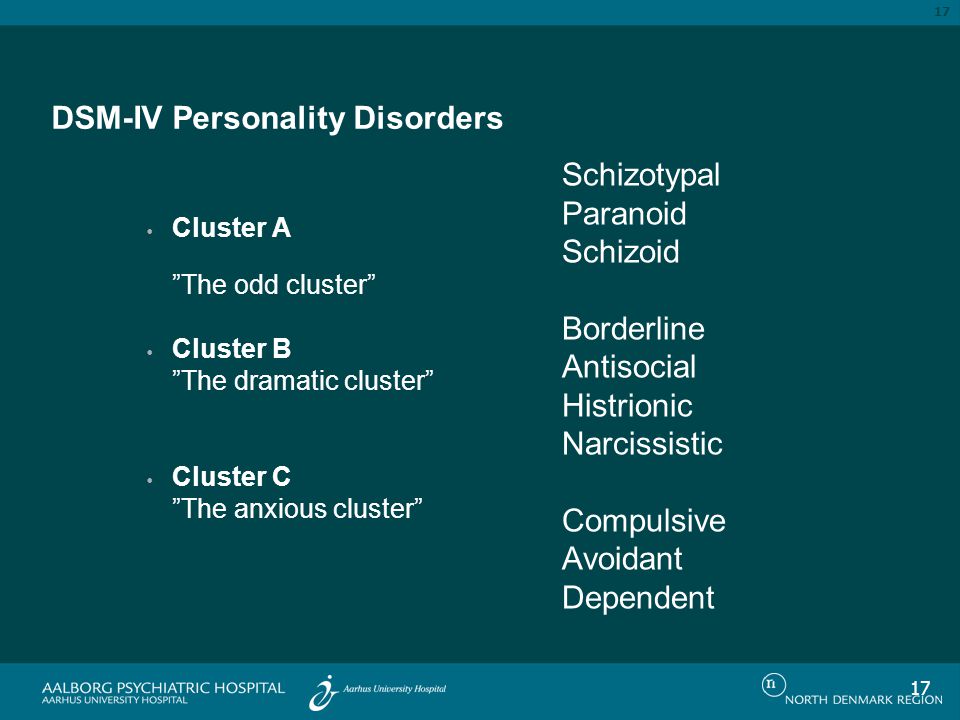
How Is Bipolar II Disorder Different From Other Types of Bipolar Disorder?
People with bipolar I disorder experience full mania -- a severe, abnormally elevated mood with erratic behavior. Manic symptoms lead to serious disruptions in life, causing legal or major personal problems.
In bipolar II disorder, the symptoms of elevated mood never reach full-blown mania. Hypomania in bipolar II is a milder form of mood elevation. However, the depressive episodes of bipolar II disorder are often longer-lasting and may be even more severe than in bipolar I disorder. Therefore, bipolar II disorder is not simply a "milder" overall form of bipolar disorder.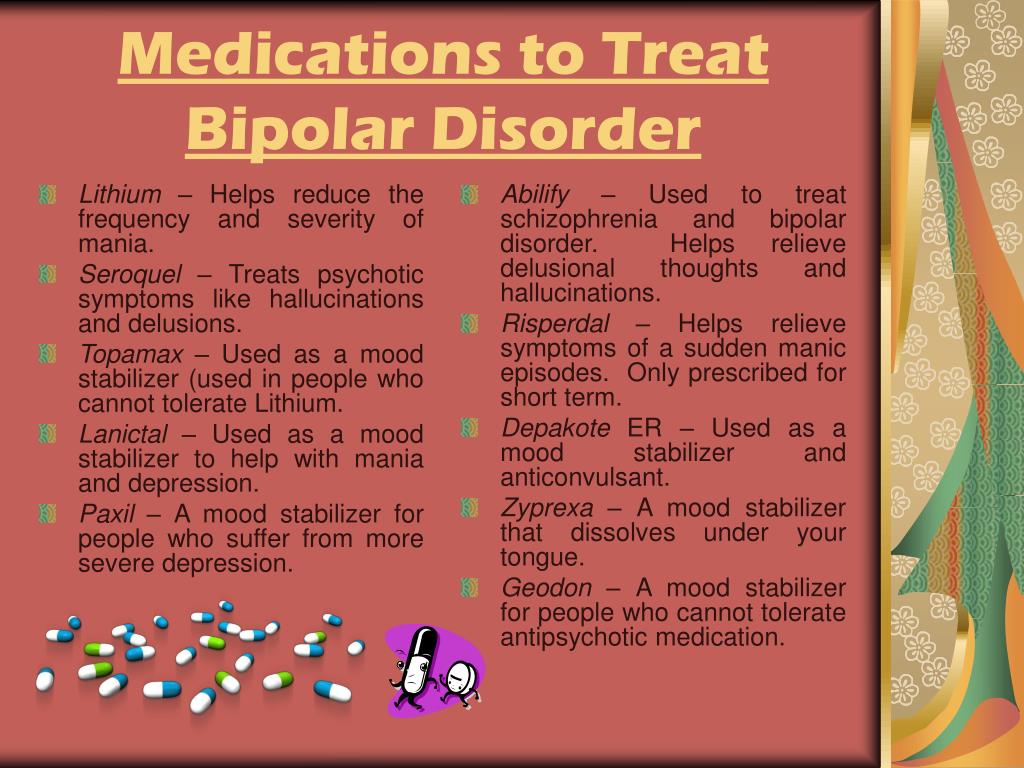
Bipolar Disorder Guide
- Overview
- Symptoms & Types
- Treatment & Prevention
- Living & Support
Bipolar disorder - Symptoms and causes
Overview
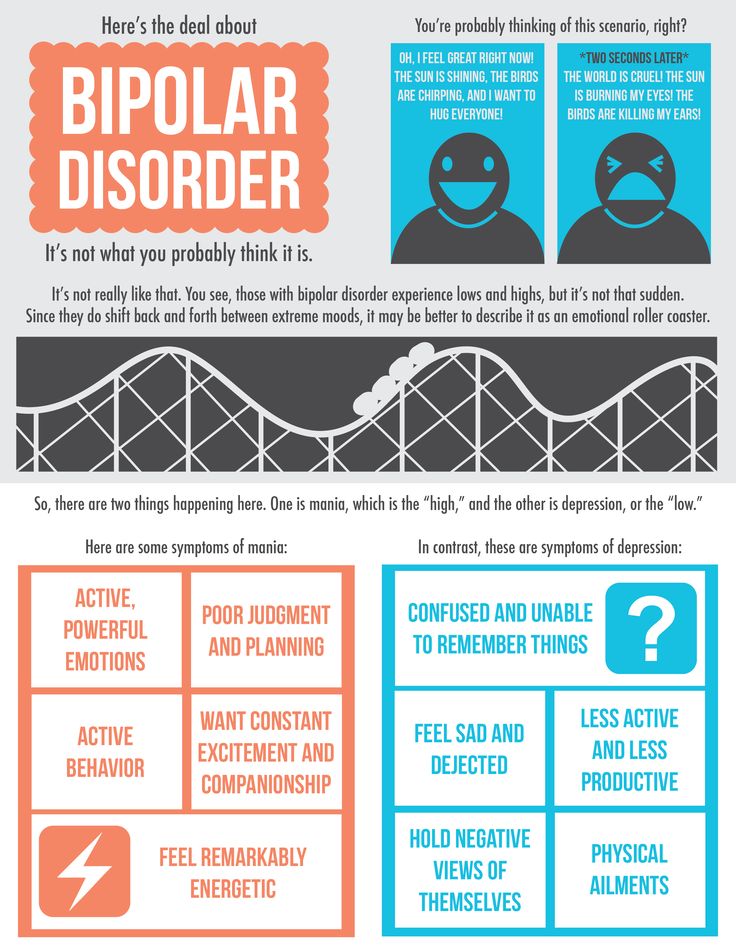
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, activity, judgment, behavior and the ability to think clearly.
Episodes of mood swings may occur rarely or multiple times a year. While most people will experience some emotional symptoms between episodes, some may not experience any.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).
Bipolar disorder care at Mayo Clinic
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
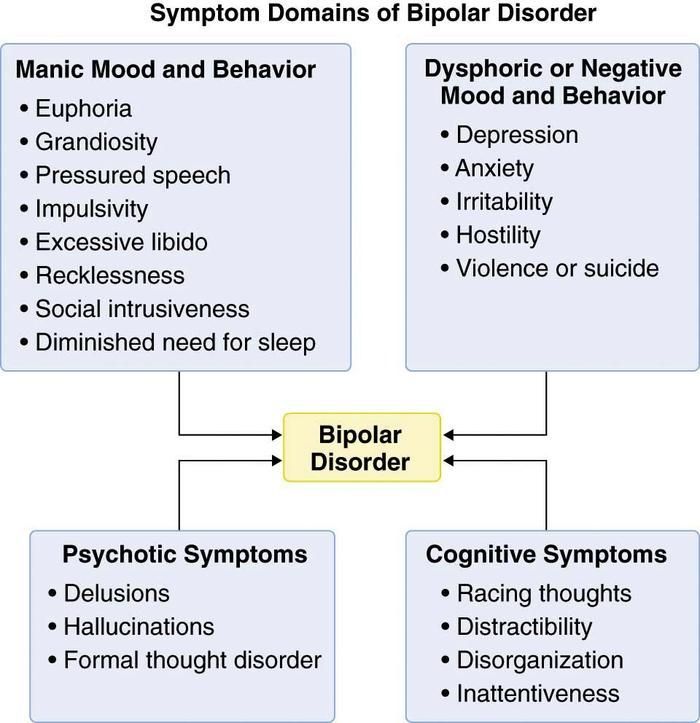
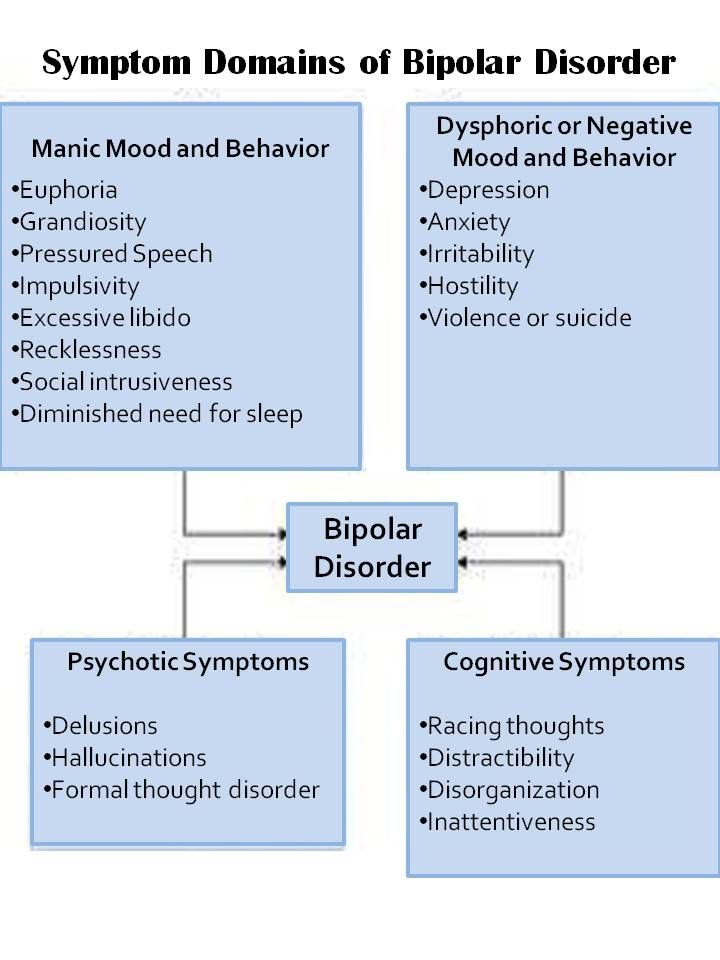
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life.
- Bipolar I disorder. You've had at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis).
- Bipolar II disorder. You've had at least one major depressive episode and at least one hypomanic episode, but you've never had a manic episode.
- Cyclothymic disorder. You've had at least two years — or one year in children and teenagers — of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment.
Although bipolar disorder can occur at any age, typically it's diagnosed in the teenage years or early 20s. Symptoms can vary from person to person, and symptoms may vary over time.
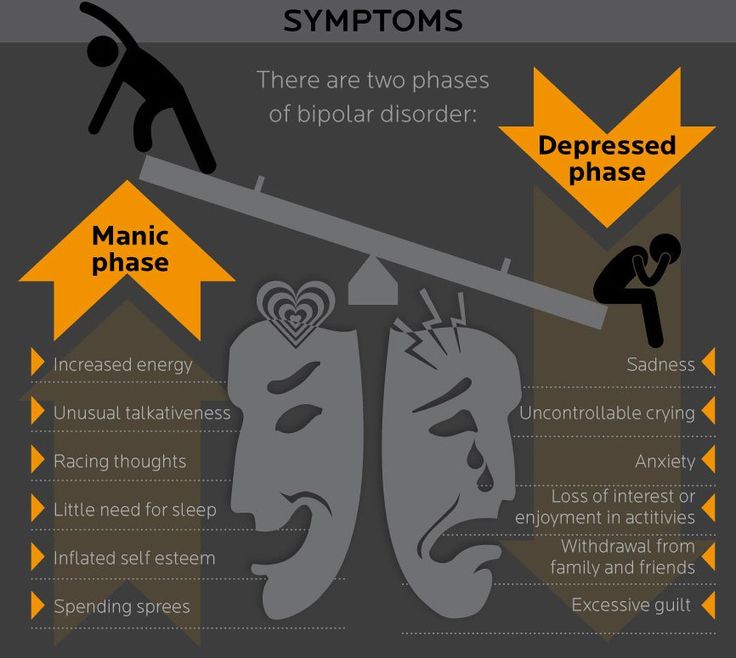
Mania and hypomania
Mania and hypomania are two distinct types of episodes, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making — for example, going on buying sprees, taking sexual risks or making foolish investments
Major depressive episode
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities or relationships. An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless or tearful (in children and teens, depressed mood can appear as irritability)
- Marked loss of interest or feeling no pleasure in all — or almost all — activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight as expected can be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorders may include other features, such as anxious distress, melancholy, psychosis or others.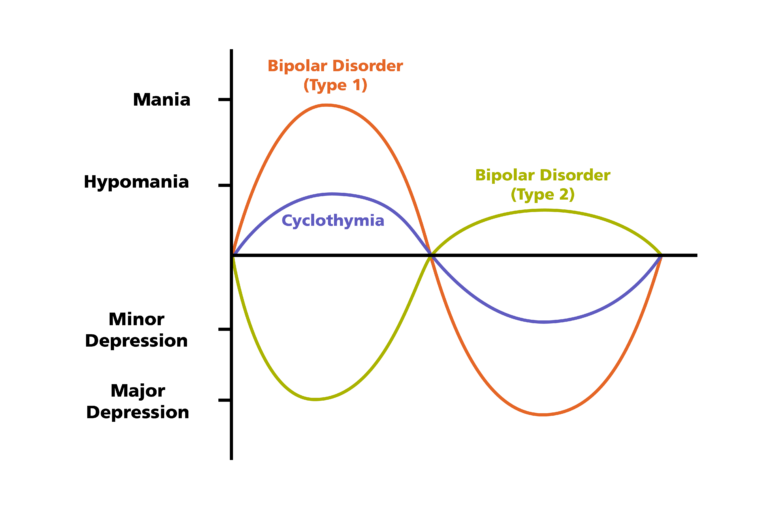 The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
Symptoms in children and teens
Symptoms of bipolar disorder can be difficult to identify in children and teens. It's often hard to tell whether these are normal ups and downs, the results of stress or trauma, or signs of a mental health problem other than bipolar disorder.
Children and teens may have distinct major depressive or manic or hypomanic episodes, but the pattern can vary from that of adults with bipolar disorder. And moods can rapidly shift during episodes. Some children may have periods without mood symptoms between episodes.
The most prominent signs of bipolar disorder in children and teenagers may include severe mood swings that are different from their usual mood swings.
When to see a doctor
Despite the mood extremes, people with bipolar disorder often don't recognize how much their emotional instability disrupts their lives and the lives of their loved ones and don't get the treatment they need.
And if you're like some people with bipolar disorder, you may enjoy the feelings of euphoria and cycles of being more productive. However, this euphoria is always followed by an emotional crash that can leave you depressed, worn out — and perhaps in financial, legal or relationship trouble.
If you have any symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder doesn't get better on its own. Getting treatment from a mental health professional with experience in bipolar disorder can help you get your symptoms under control.
When to get emergency help
Suicidal thoughts and behavior are common among people with bipolar disorder. If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
Or use the Lifeline Chat. Services are free and confidential.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
The exact cause of bipolar disorder is unknown, but several factors may be involved, such as:
- Biological differences. People with bipolar disorder appear to have physical changes in their brains. The significance of these changes is still uncertain but may eventually help pinpoint causes.
- Genetics. Bipolar disorder is more common in people who have a first-degree relative, such as a sibling or parent, with the condition.
 Researchers are trying to find genes that may be involved in causing bipolar disorder.
Researchers are trying to find genes that may be involved in causing bipolar disorder.
Risk factors
Factors that may increase the risk of developing bipolar disorder or act as a trigger for the first episode include:
- Having a first-degree relative, such as a parent or sibling, with bipolar disorder
- Periods of high stress, such as the death of a loved one or other traumatic event
- Drug or alcohol abuse
Complications
Left untreated, bipolar disorder can result in serious problems that affect every area of your life, such as:
- Problems related to drug and alcohol use
- Suicide or suicide attempts
- Legal or financial problems
- Damaged relationships
- Poor work or school performance
Co-occurring conditions
If you have bipolar disorder, you may also have another health condition that needs to be treated along with bipolar disorder. Some conditions can worsen bipolar disorder symptoms or make treatment less successful.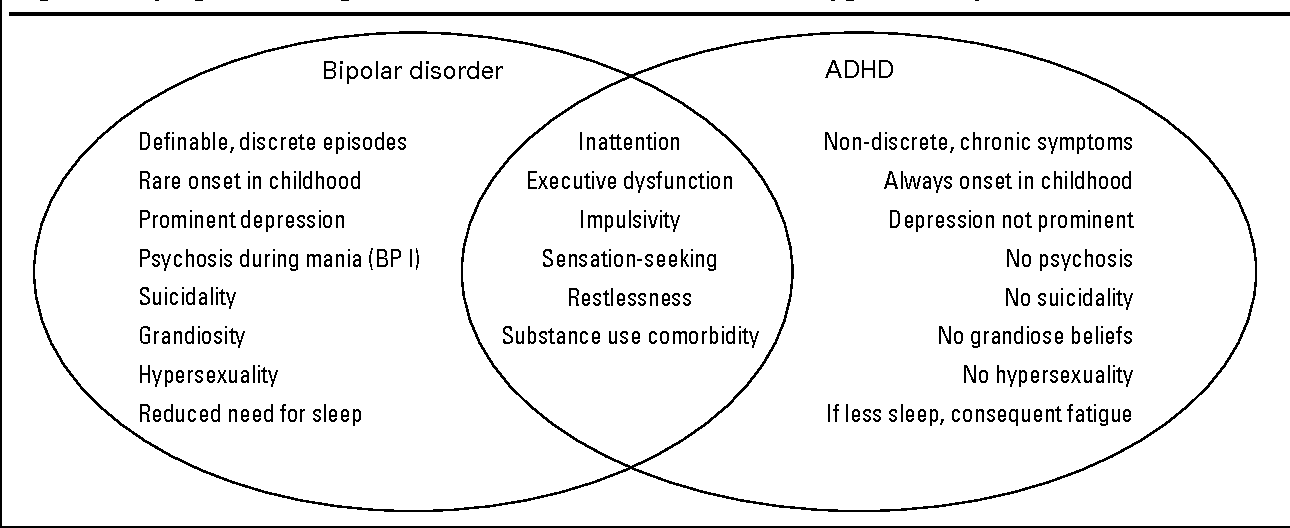 Examples include:
Examples include:
- Anxiety disorders
- Eating disorders
- Attention-deficit/hyperactivity disorder (ADHD)
- Alcohol or drug problems
- Physical health problems, such as heart disease, thyroid problems, headaches or obesity
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar disorder and alcoholism: Are they related?
Prevention
There's no sure way to prevent bipolar disorder. However, getting treatment at the earliest sign of a mental health disorder can help prevent bipolar disorder or other mental health conditions from worsening.
If you've been diagnosed with bipolar disorder, some strategies can help prevent minor symptoms from becoming full-blown episodes of mania or depression:
- Pay attention to warning signs. Addressing symptoms early on can prevent episodes from getting worse. You may have identified a pattern to your bipolar episodes and what triggers them.
 Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs.
Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs. - Avoid drugs and alcohol. Using alcohol or recreational drugs can worsen your symptoms and make them more likely to come back.
- Take your medications exactly as directed. You may be tempted to stop treatment — but don't. Stopping your medication or reducing your dose on your own may cause withdrawal effects or your symptoms may worsen or return.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.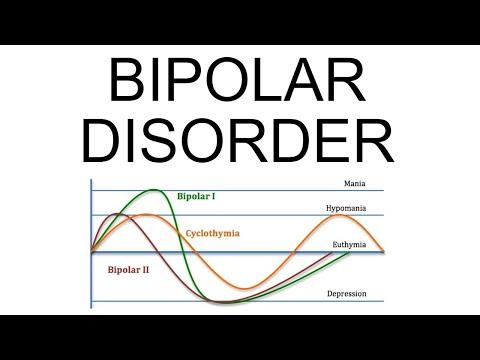
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly. nine0003
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. They may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life. nine0003
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes.
 In some cases, mania can cause a break with reality (psychosis).
In some cases, mania can cause a break with reality (psychosis). - Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode. nine0015 Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke. nine0018
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time. nine0003
Symptoms can vary from person to person, and symptoms can change over time. nine0003
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy nine0015 Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.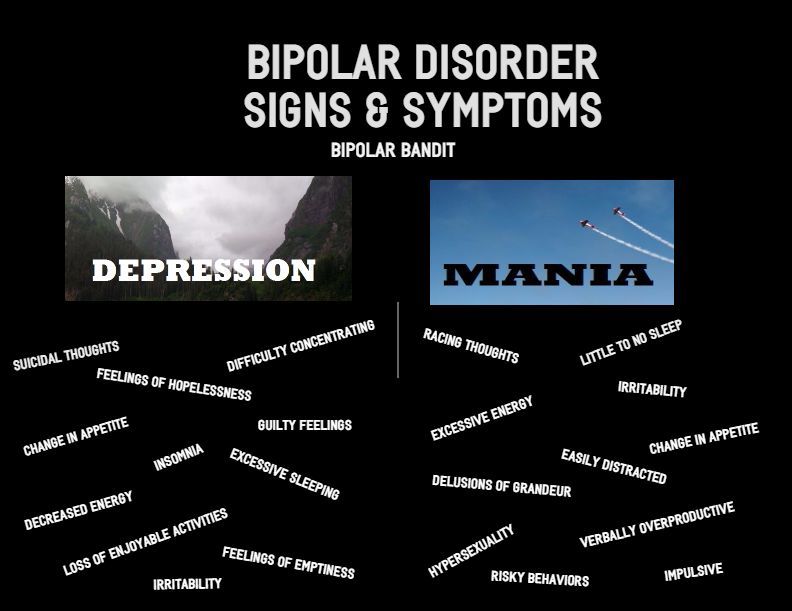 The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons. nine0003
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons. nine0003
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships. nine0003
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Bipolar disorder - Official website of the FGBUZ KB No.
 85 FMBA of Russia
85 FMBA of Russia General brief information
Bipolar disorder, also known as bipolar affective disorder (BAD) and formerly as manic-depressive psychosis (PMD). It is a set of mood disorders characterized by marked fluctuations in mood, thinking, behaviour, energy and ability to perform daily activities. nine0003
A person suffering from this disorder alternates his state of mind between mania or hypomania - a phase of joy, exaltation, euphoria and grandiosity and depression, with sadness, inhibition and ideas of death.
Four types of bipolar disorder were defined by severity and alternation of moods over time:
- Bipolar I disorder
- Bipolar disorder type II
- Cyclothymia
- Non-specific bipolar disorder
Because bipolar disorder occurs in young people, it has a high social cost. It is the second leading cause of disability worldwide. In addition, those who suffer from it pose a higher risk than the general population of deaths from suicide, homicide, accidents, and natural causes such as cardiovascular disease.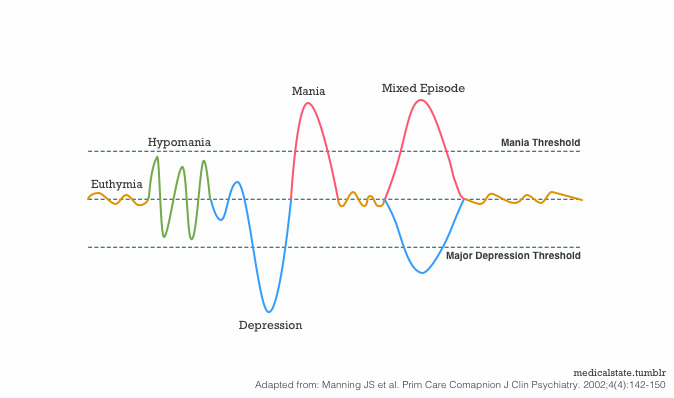
In type 1, the person alternates between depressive episodes with full manic episodes, and in type 2, he alternates between depressive episodes and hypomanic (less severe) episodes. nine0003
The symptoms of this disorder are severe, different from the normal highs and lows of mood. These symptoms can lead to relationship problems, work, school, or even suicide.
During the depression phase a person may experience:
- Negative perception of life.
- Inability to feel the pleasure of life.
- No energy
- Self-criticism.
- In extreme cases, suicide. nine0031
- Denial that there is a problem.
- Sudden change of mood.
- Irrational financial decisions.
- Feeling of great enthusiasm
- Don't think about the consequences of your actions.
- Lack of sleep
- Persistent sadness
- Lack of interest in engaging in pleasurable activities. nine0018
- Apathy or indifference.
- Anxiety or social anxiety.
- Chronic pain or irritability.
- Lack of motivation
- Guilt, hopelessness, social isolation.
- Lack of sleep or appetite.
- Suicidal thoughts
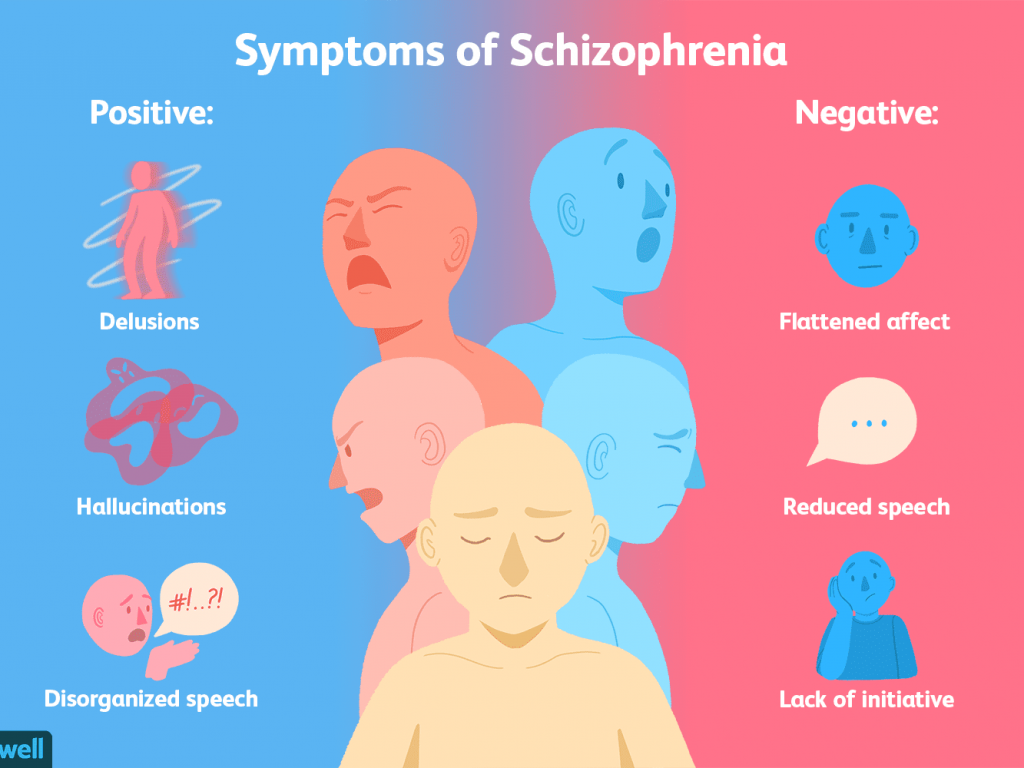
- In extreme cases, there may be psychotic symptoms: delusions or hallucinations are usually unpleasant.
- Great energy and activity.
- Some people may be more creative, while others may be more irritable.
- A person may feel so good that he denies that he is experiencing a state of hypomania.
- Talk quickly and smoothly.
- Accelerated thoughts.
- Agitation.
- Light condition.
- Impulsive and risky behavior.
- Excessive cash expenses
- Hypersexuality.
- A person with mania may also feel sleep deprivation and inadequate judgment.
- On the other hand, maniacs may have problems with alcohol or other substance abuse. nine0018
During a manic phase, a person may experience:
Although childhood onset occurs, the normal age of onset for type 1 is 18 years and for type 2 is 22 years.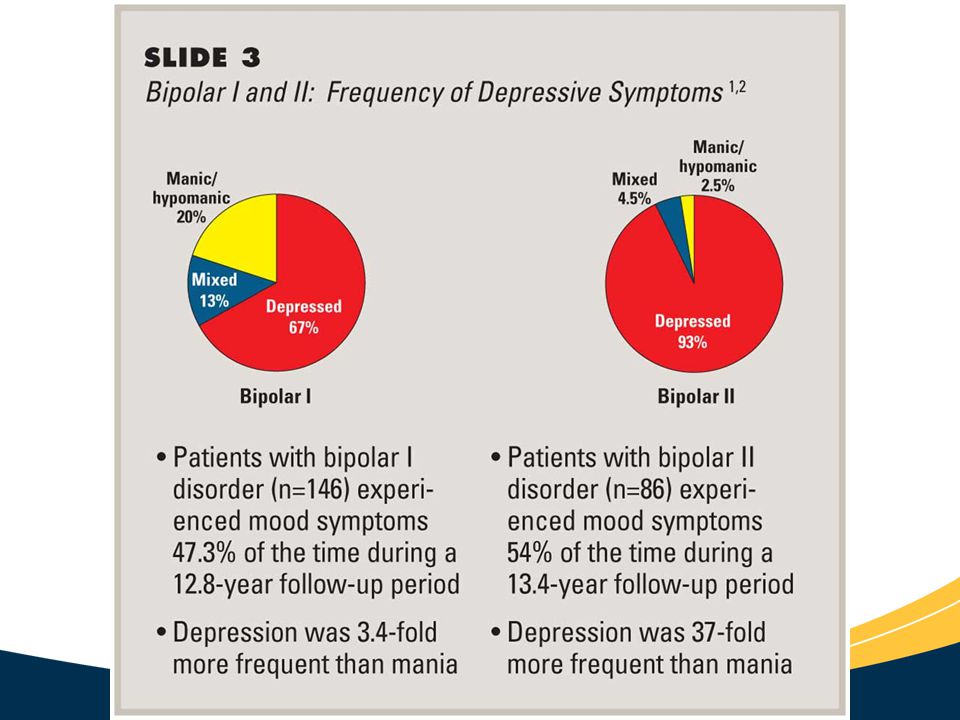
About 10% of bipolar 2 cases develop into type 1.
Although the causes are unclear, genetic and environmental factors (stress, childhood abuse) are involved.
Treatment usually includes psychotherapy, medication, sometimes electroconvulsive therapy may be helpful.
Symptoms
Signs and symptoms of the depressive phase of bipolar disorder include:
Manic symptoms
Mania can occur in varying degrees:
Hypomania
This is the least severe degree of mania and lasts at least 4 days.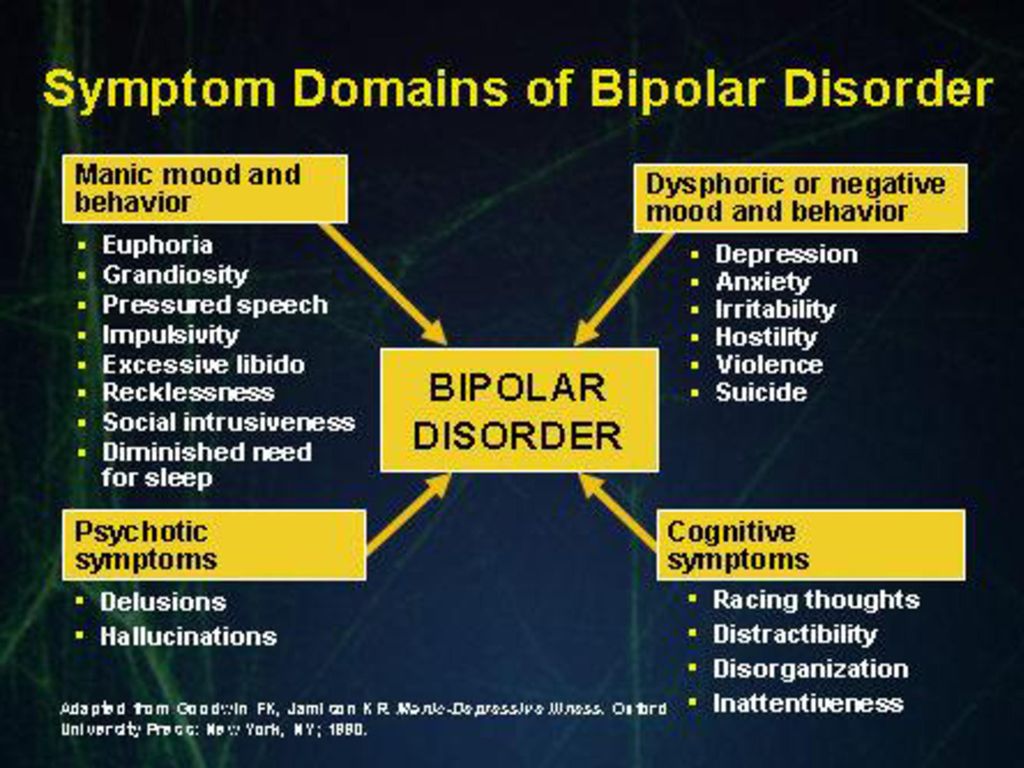 This does not result in a noticeable decrease in a person's ability to work, communicate, or adapt.
This does not result in a noticeable decrease in a person's ability to work, communicate, or adapt.
He also does not require hospitalization and does not have psychotic characteristics.
In fact, general functioning may improve during a hypomanic episode and is considered a natural anti-depression mechanism.
If the event of hypomania is not accompanied by or precedes depressive episodes, it is not considered a problem if the state of mind is uncontrollable. nine0003
Symptoms may last from several weeks to several months.
It is characterized by:
Mania
Mania is a period of euphoria and high mood for at least 7 days. If left untreated, a manic episode can last 3 to 6 months. nine0003
It is characterized by displaying three or more of the following behaviors:
In extreme cases, they may experience psychosis, so that contact with reality is broken, having a high state of mind.
It is something common that a manic person feels incomparable or indestructible and feels chosen to realize a goal.
Approximately 50% of people with bipolar disorder experience hallucinations or delusions, which can lead to violent behavior or admission to a psychiatric hospital.
mixed episodes
In bipolar disorder, a mixed episode is a condition in which mania and depression occur simultaneously.
People who experience this condition may have thoughts of grandiosity while having depressive symptoms such as suicidal thoughts or feelings of guilt.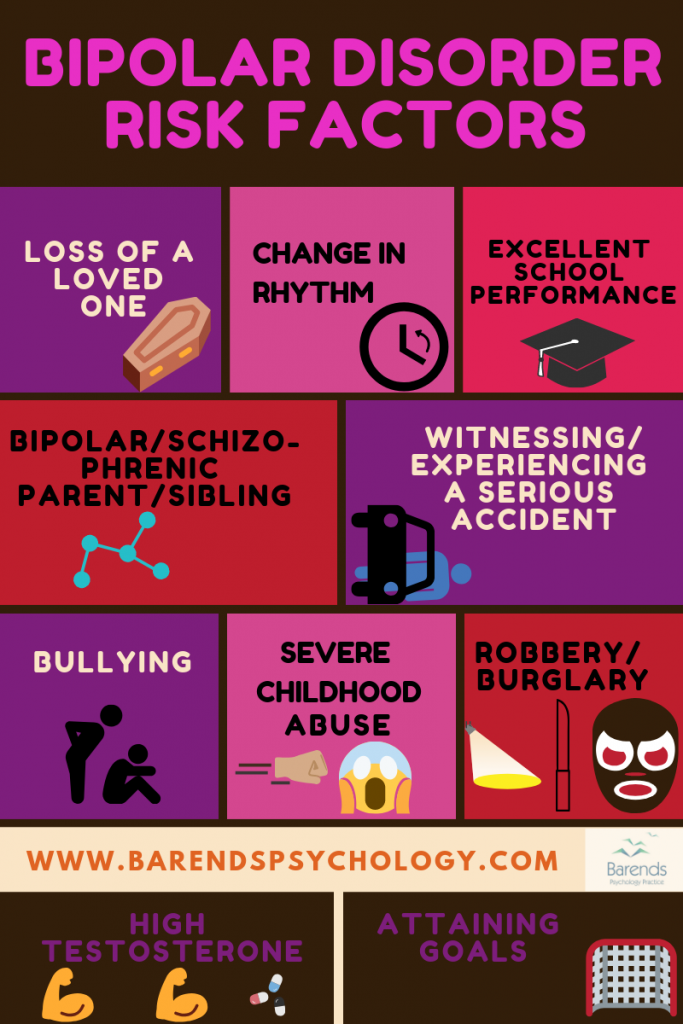
People who are in this state are at high risk of committing suicide because they confuse depressive emotions with mood swings or difficulty controlling impulsivity. nine0003
Causes
The exact causes of bipolar disorder are unclear, although they are thought to be largely genetic and environmental.
Genetic factors
It is believed that 60-70% of the risk of developing bipolarity depends on genetic factors.
Several studies have shown that certain genes and chromosomal regions are associated with susceptibility to develop the disorder, with each gene being more or less important. nine0003
The risk of bipolar disorder in people with family members with the same diagnosis is 10 times higher than in the general population.
Research indicates heterogeneity, meaning that different genes are involved in different families.
Environmental factors
Research shows that environmental factors play an important role in the development of bipolar disorder, and psychosocial variables may interact with genetic dispositions.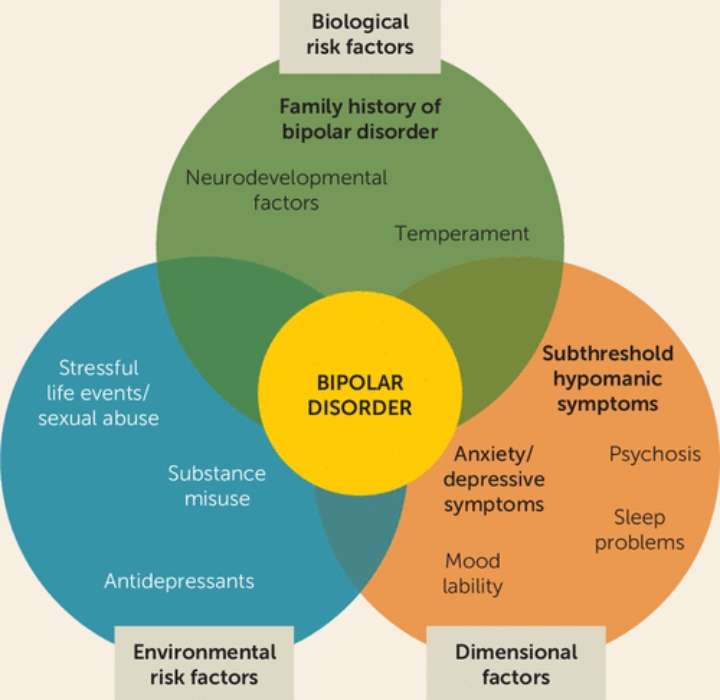
Recent life events and interpersonal relationships contribute to manic and depressive episodes. nine0003
30-50% of adults diagnosed with bipolar disorder have been found to report abuse or trauma in childhood, which is associated with an earlier onset of the disorder and more suicide attempts.
Evolutionary factors
From evolutionary theory one might think that the negative effects that bipolar disorder can have on adaptability cause genes not to be selected by natural selection.
However, there is still a high incidence of BD in many populations, so there may be some evolutionary benefit. nine0003
Doctors of evolutionary medicine suggest that high rates of BR throughout history suggest that the change between depressive and manic states suggested some evolutionary advantage in ancestral humans.
In highly stressed people, depressed mood can serve as a defense strategy to escape external stress, store energy, and increase sleep hours.
Mania could benefit from its relationship with creativity, confidence, high energy levels and greater productivity.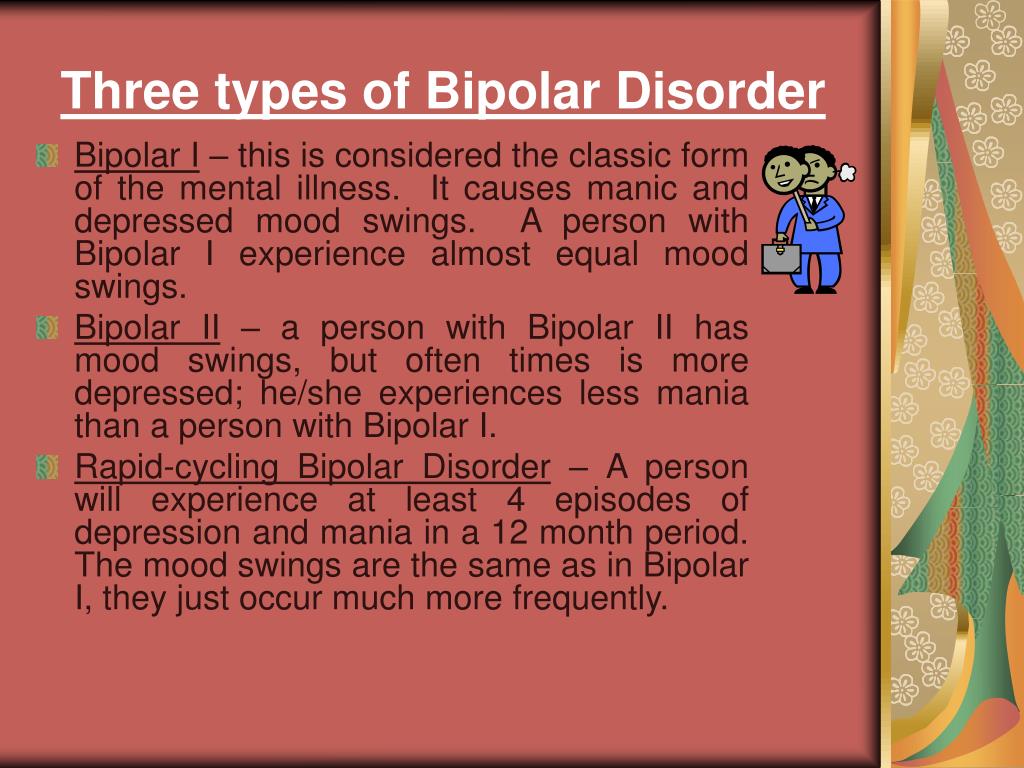 nine0003
nine0003
Physiological, neurological and neuroendocrine factors
Brain imaging studies have shown differences in the volume of various brain areas between patients with bipolar disorder and healthy patients.
An increase in the volume of the lateral ventricles and an increase in the rate of white matter hyperintensity were found.
Magnetic resonance studies have shown that there is an abnormal modulation between the abdominal prefrontal region and the limbic regions, especially the amygdala. This will contribute to poor emotional regulation and mood-related symptoms. nine0003
On the other hand, there is evidence of an association between early stressful experiences and dysfunction of the hypothalamic-pituitary-adrenal axis, leading to hyperactivation.
A less common bipolar disorder may result from trauma or a neurological condition: brain injury, stroke, HIV, multiple sclerosis, porphyria, and temporal lobe epilepsy.
The neurotransmitter responsible for regulating mood, dopamine, has been found to increase its transmission during the manic phase and decrease during the depressive phase.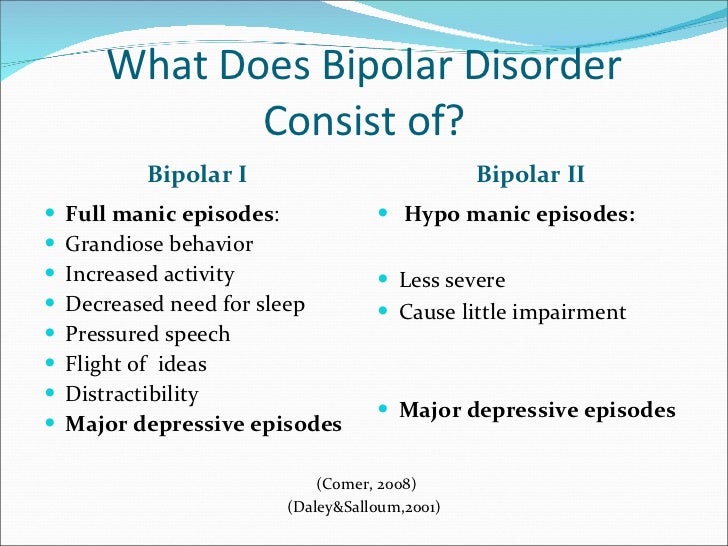 nine0003
nine0003
Glutamate increases in the left dorsolateral prefrontal cortex during the manic phase.
Diagnosis
A patient must have at least two episodes of affective disorder to be diagnosed with bipolar disorder. At the same time, at least one of them must be either manic or mixed. For the correct diagnosis, the psychiatrist must take into account the characteristics of the patient's history, information received from his relatives. Currently, it is believed that the symptoms of bipolar disorder are characteristic of 1% of people, and in 30% of them the disease becomes a severe psychotic form. Determination of the severity of depression is carried out using special scales. The manic phase of bipolar disorder must be differentiated from arousal caused by the use of psychoactive substances, lack of sleep, or other causes, and the depressive phase from psychogenic depression. Psychopathy, neurosis, schizophrenia, as well as affective disorders and other psychoses due to somatic or nervous diseases should be excluded. nine0003
nine0003
Methods of treatment
The main goal of the treatment of bipolar disorder is to normalize the mental state and mood of the patient, to achieve long-term remission. In severe cases of the disease, patients are hospitalized in the psychiatric department. Mild forms of the disorder can be treated on an outpatient basis. Antidepressants are used to relieve a depressive episode. The choice of a specific drug, its dosage and frequency of administration in each case is determined by a psychiatrist, taking into account the age of the patient, the severity of depression, and the possibility of its transition to mania. If necessary, the appointment of antidepressants is supplemented with mood stabilizers or antipsychotics. Antidepressants help to stop depressive states in bipolar disorder. Drug treatment of bipolar disorder in the stage of mania is carried out by normotimics, and in severe cases of the disease, antipsychotics are additionally prescribed. In the stage of remission, psychotherapy (group, family and individual) is shown.