Stimulant use disorder dsm 5 code
Stimulant Use Disorder: Diagnosis, Symptoms, and Treatment
Stimulant Use Disorder:
Diagnosis, Symptoms, and Treatment
The misuse and abuse of stimulants are rising worldwide. A 2015-2016 report reported that as many as 5 million Americans had misused a prescription stimulant at least once, with 0.4 million people developing full prescription stimulant use disorder.
What are Stimulants?
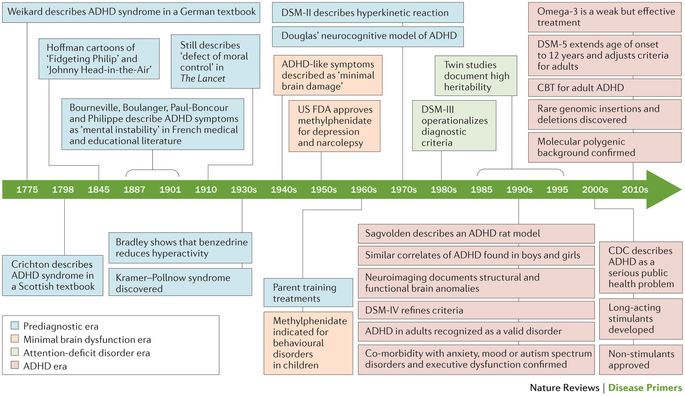
Known by many street and prescription names, stimulants are drugs that speed up the body’s system, resulting in increased alertness, attention, and energy. These highly addictive substances are currently available in legal and illegal forms. Prescribers often recommend the use of prescription stimulants to treat attention deficit hyperactivity disorder, but even the prescription stimulants can be misused, which can lead to addiction and stimulant use disorder.
More Film Previews
Free Trial
Subscription Options
Legal Prescription Stimulants:
- Ritalin
- Strattera
- Adderall
- Concerta
Illegal Stimulants:
- Cocaine (“coke”, “crack”)
- Amphetamine (“speed”)
- Methamphetamine (“meth”)
- MDMA (“Molly”)
Definition and Diagnosis of Stimulant Use Disorder
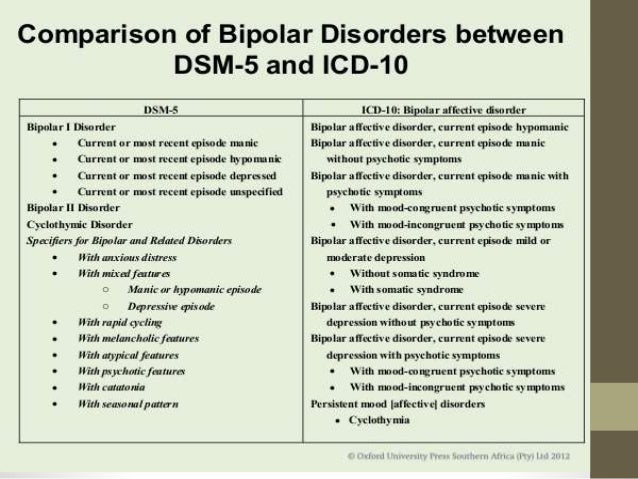
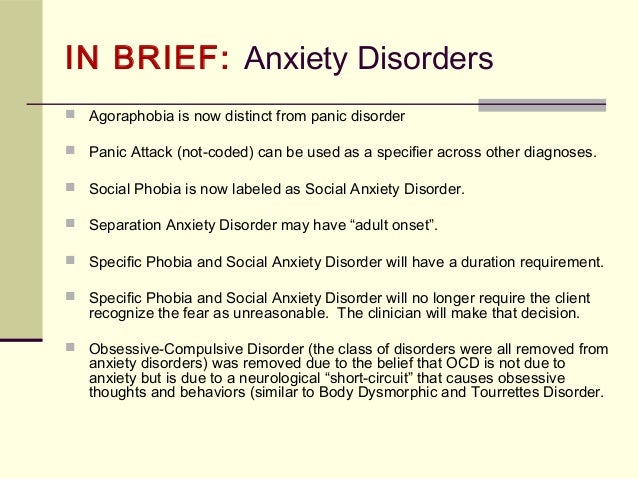
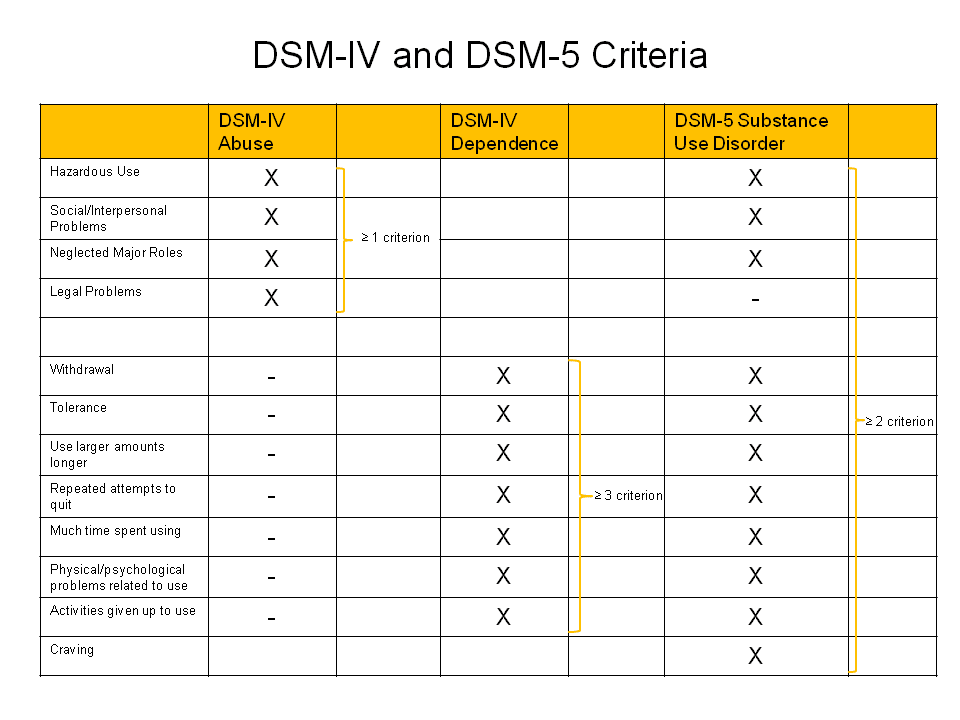
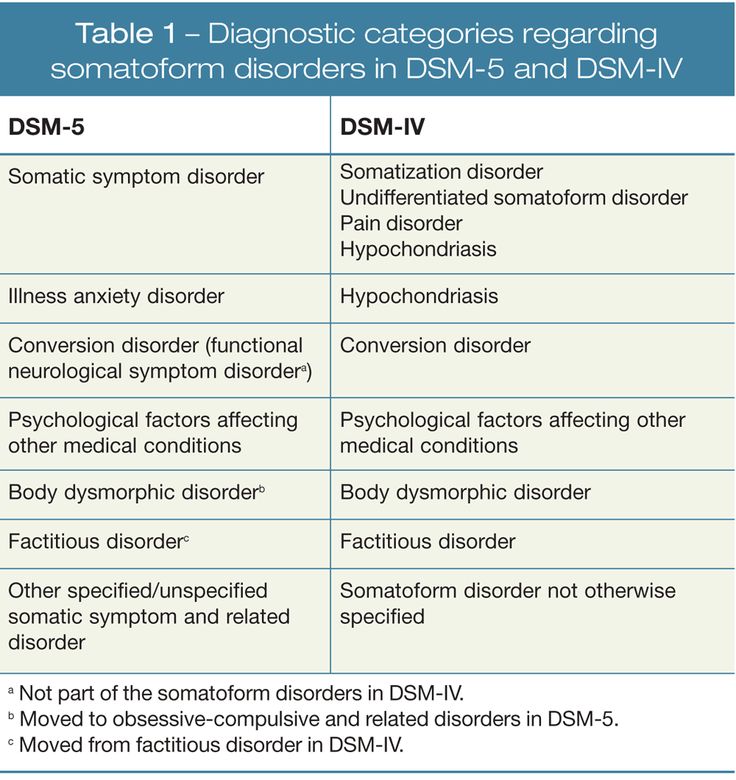
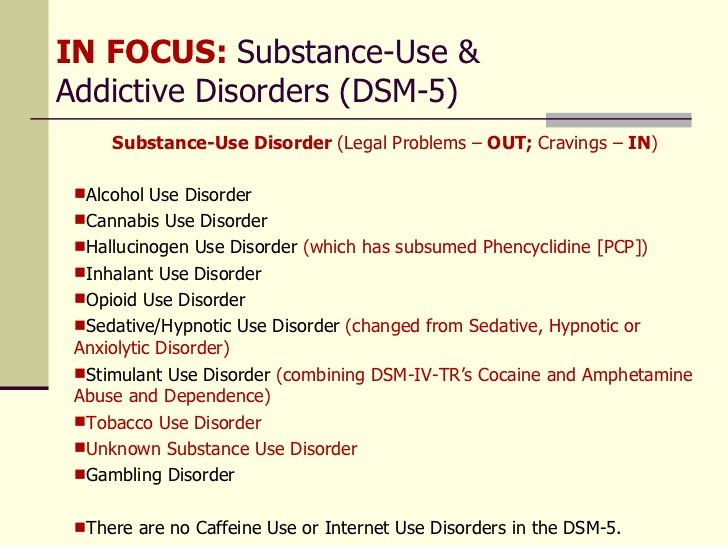
The definition and diagnostic criteria for stimulant use disorder have changed over the years. The current gold standard for diagnosing mental and psychiatric disorders, the Diagnostic and Statistical Manual for Mental Disorders 5, Text Revision (DSM-5-TR), updated the definition and criteria for substance use disorders in the latest 5th edition.
The DSM-5 criteria identify 11 symptoms and clinical features for diagnosing stimulant use disorder. At least two signs must be present to qualify as a disorder, but the individual’s behaviors may still indicate they are misusing the substances. Misuse of stimulants still warrants attention and treatment to prevent escalation of the behavior. Individuals exhibiting six or more symptoms receive a severe stimulant or substance use disorder diagnosis, often referred to as an addiction.
In this course, learners will review the full list of symptoms and view video examples of stimulant use disorder signs.
Symptoms of Stimulant Use Disorder
Another significant change in the diagnostic criteria for stimulant use disorder (and other substances) is the presence of tolerance and withdrawal no longer being a necessary or deciding indicator of addiction. While many addicts do develop a tolerance and experience withdrawal, they can meet the diagnostic criteria for addiction without these symptoms. This change allows more individuals to qualify under the diagnostic criteria, hopefully increasing their ability to receive care and treatment.
While many addicts do develop a tolerance and experience withdrawal, they can meet the diagnostic criteria for addiction without these symptoms. This change allows more individuals to qualify under the diagnostic criteria, hopefully increasing their ability to receive care and treatment.
Those suffering from stimulant use disorder often exhibit some of these hallmark symptoms:
- Taking stimulants more than prescribed (if prescription)
- Difficulty decreasing or stopping use of the stimulant, despite wanting to
- Craves or urges to use
- Continued use of stimulants despite a negative impact on life responsibilities like school or work, or problems in relationships
- Withdrawal symptoms
Discover all 11 signs and symptoms of stimulant use disorder in this Symptom Media DSM-5-TR Guided film.
Treatment
Identifying signs of stimulant use misuse early can positively impact interventions’ effectiveness to prevent escalation to a full-blown disorder.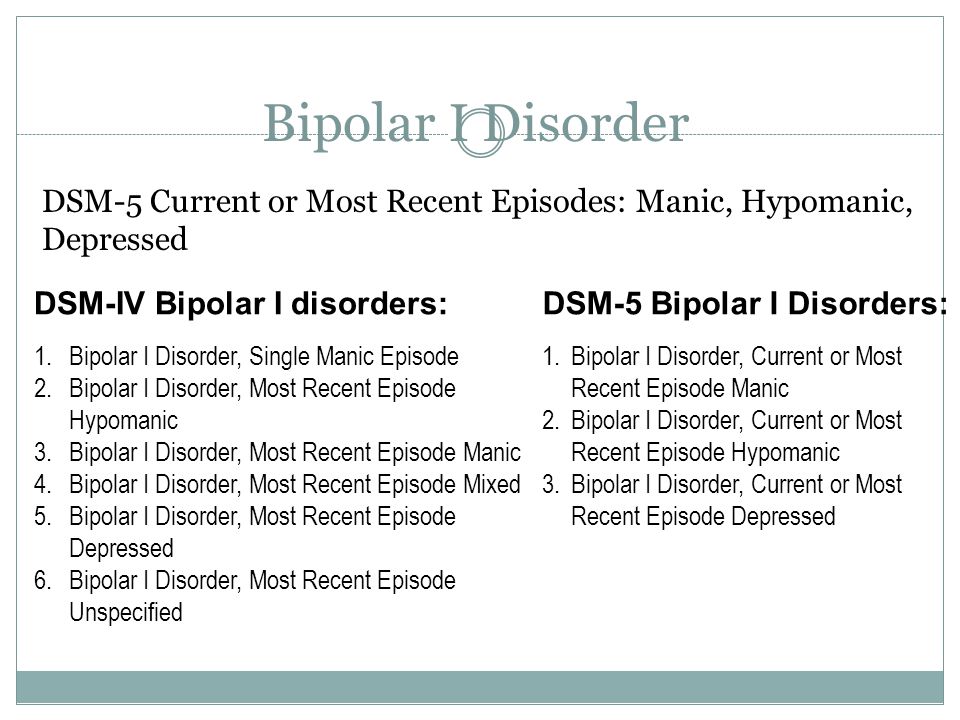 While there are no approved medications to treat stimulant use disorder, counseling, and behavioral therapy (such as Cognitive Behavioral Therapy [CBT] have been proven to be effective, combined with support services.
While there are no approved medications to treat stimulant use disorder, counseling, and behavioral therapy (such as Cognitive Behavioral Therapy [CBT] have been proven to be effective, combined with support services.
Unlike other substances like alcohol, stimulant withdrawal and detoxification are not medically dangerous but may result in unpleasant feelings and severe depression. Because of this risk, mental health professionals and addiction specialists should carefully monitor individuals receiving treatment for stimulant use disorder for risk of suicidal thoughts.
Recovery from stimulant use disorder is possible, but it requires dedication, stability, and support. Ongoing care is necessary for sustainable recovery and overall mental health. Patients should be actively involved in their care at every step, and treatment should always be absent of judgment of prior decisions or choices.
Explore the hallmark symptoms of stimulant use disorder in this DSM-5-TR Guided film, which includes a video demonstration of key signs.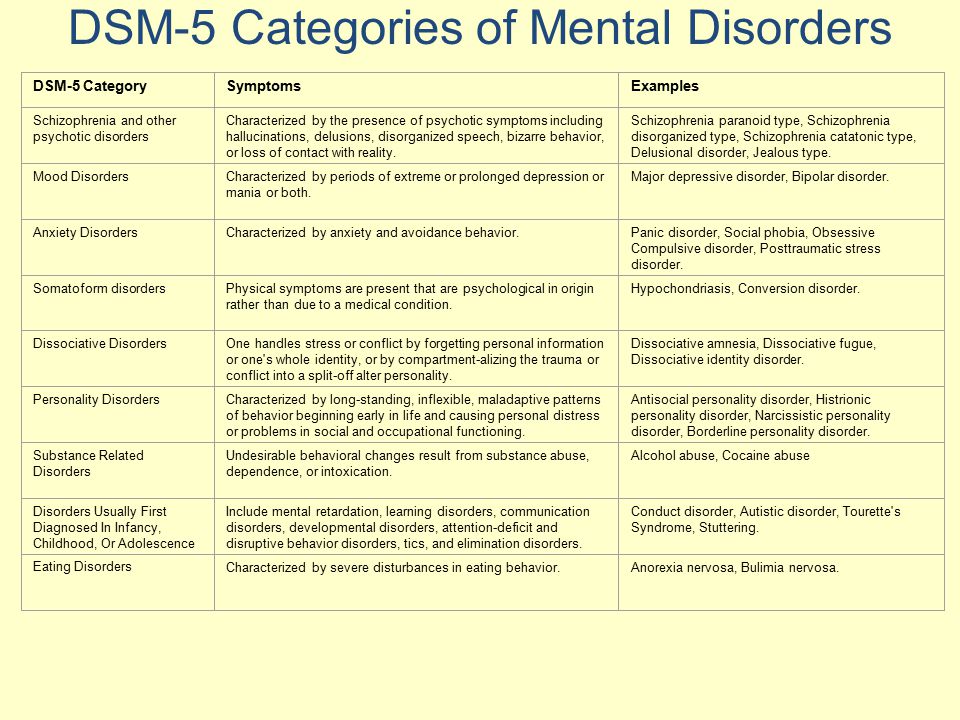
Written by Jessica Dzubak, MSN, RN
The National Alcohol and Drug Knowledgebase
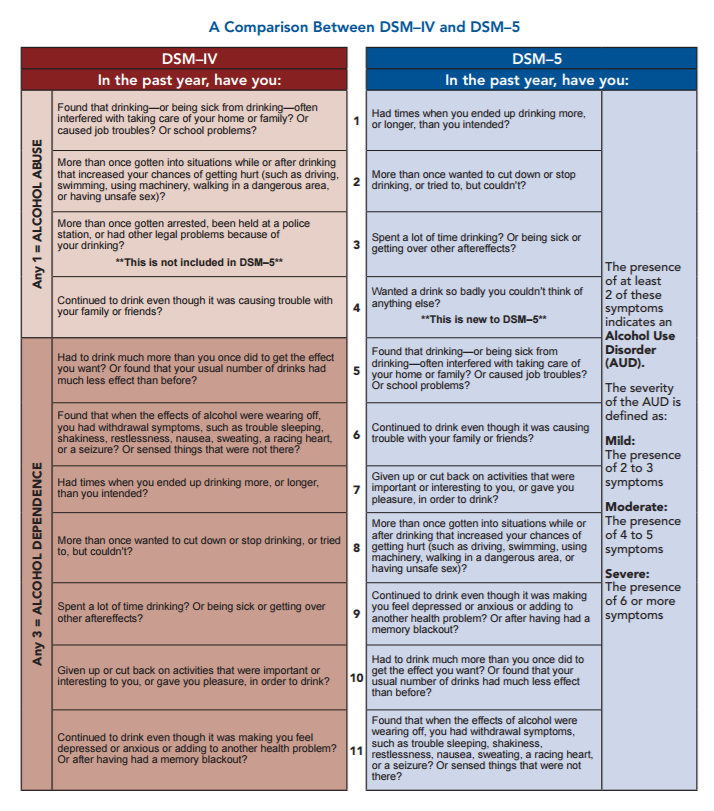
The reference guide used by clinicians to diagnose mental health disorders is known as the Diagnostic and Statistical Manual of Mental Disorders (DSM). The most recent version of the manual, the Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-5), was released in May 2013. Prior to this, the Diagnostic and Statistical Manual of Mental Disorders – 4th Edition, Text Revision (DSM-IV-TR) was used by clinicians and researchers from 2000 to 2013.
The diagnostic criteria for mental health disorders due to methamphetamine use differ significantly between the DSM-IV-TR and the new DSM-5. For the purposes of the NADK, all reported data on methamphetamine-related mental health disorders utilise the DSM-IV-TR diagnostic criteria. This is because the relevant mental health data reported in the NADK was collected prior to the publication of the newer version of the DSM (DSM-5).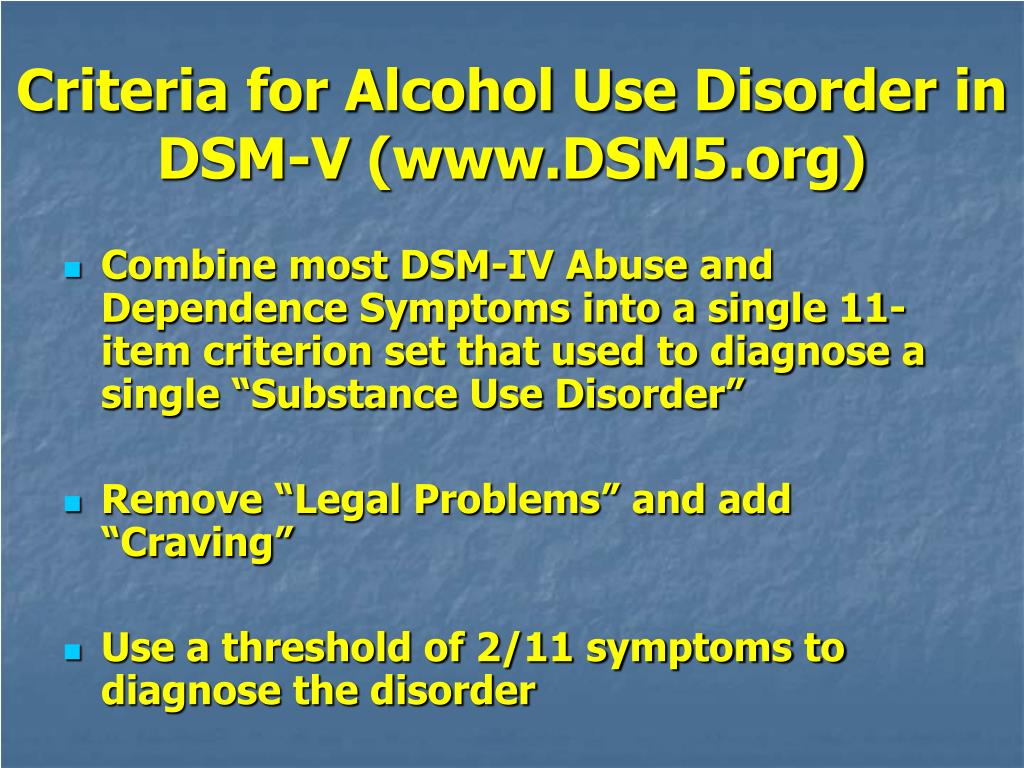
DSM-IV-TR Diagnostic Criteria
According to the DSM-IV-TR, there are two main methamphetamine-related mental health disorders: substance dependence and substance abuse. The diagnostic criteria for each are presented below.
Substance Dependence
A maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by three (or more) of the following, occurring at any time in the same 12-month period:
1. Tolerance, as defined by either of the following:
a. A need for markedly increased amounts of the substance to achieve intoxication or desired effect; or
b. Markedly diminished effect with continued use of the same amount of the substance
2. Withdrawal, as manifested by either of the following:
a. The characteristic withdrawal syndrome for the substance; or
b. The same (or a closely related) substance is taken to relieve or avoid withdrawal symptoms
3. The substance is often taken in larger amounts or over a longer period than was intended
The substance is often taken in larger amounts or over a longer period than was intended
4. There is a persistent desire or unsuccessful efforts to cut down or control substance use
5. A great deal of time is spent on activities necessary to obtain the substance (e.g., visiting multiple doctors or driving long distances), use the substance (e.g., chain-smoking), or recover from its effects
6. Important social, occupational, or recreational activities are given up or reduced because of substance use
7. The substance use is continued despite knowledge of having a persistent physical or psychological problem that is likely to have been caused or exacerbated by the substance (e.g., current cocaine use despite recognition of cocaine-induced depression, or continued drinking despite recognition that an ulcer was made worse by alcohol consumption).
Substance Abuse
A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by one (or more) of the following, occurring within a 12-month period:
1. Recurrent substance use resulting in a failure to fulfil major role obligations at work, school, or home (e.g., repeated absences or poor work performance related to substance use; substance‐related absences, suspensions, or expulsions from school; neglect of children or household)
Recurrent substance use resulting in a failure to fulfil major role obligations at work, school, or home (e.g., repeated absences or poor work performance related to substance use; substance‐related absences, suspensions, or expulsions from school; neglect of children or household)
2. Recurrent substance use in situations in which it is physically hazardous (e.g., driving an automobile or operating a machine when impaired by substance use)
3. Recurrent substance‐related legal problems (e.g., arrests for substance‐related disorderly conduct)
4. Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance (e.g., arguments with spouse about consequence of intoxication, physical fights).
DSM-5 Diagnostic Criteria
According to the DSM-5, there is one main methamphetamine-related mental health disorder: a stimulant use disorder. This is defined as:
A pattern of amphetamine-type substance, cocaine, or other stimulant use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
1. The stimulant is often taken in larger amounts or over a longer period than was intended
The stimulant is often taken in larger amounts or over a longer period than was intended
2. There is a persistent desire or unsuccessful efforts to cut down or control stimulant use
3. A great deal of time is spent in activities necessary to obtain the stimulant, use the stimulant, or recover from its effects
4. Craving, or a strong desire or urge to use the stimulant
5. Recurrent stimulant use resulting in a failure to fulfil major role obligations at work, school, or home
6. Continued stimulant use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the stimulant
7. Important social, occupational, or recreational activities are given up or reduced because of stimulant use
8. Recurrent stimulant use in situations in which it is physically hazardous
9. Stimulant use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the stimulant
10. Tolerance, as defined by either of the following:
Tolerance, as defined by either of the following:
a. A need for markedly increased amounts of the stimulant to achieve intoxication or desired effect.
b. A markedly diminished effect with continued use of the same amount of the stimulant.
Note: This criterion is not considered to be met for those taking stimulant medications solely under appropriate medical supervision, such as medications for attention-deficit/hyperactivity disorder or narcolepsy.
11. Withdrawal, as manifested by either of the following:
a. The characteristic withdrawal syndrome for the stimulant (refer to Criteria A and B of the criteria set for stimulant withdrawal, p. 569).
b. The stimulant (or a closely related substance) is taken to relieve or avoid withdrawal symptoms.
Note: This criterion is not considered to be met for those taking stimulant medications solely under appropriate medical supervision, such as medications for attention-deficit/hyperactivity disorder or narcolepsy.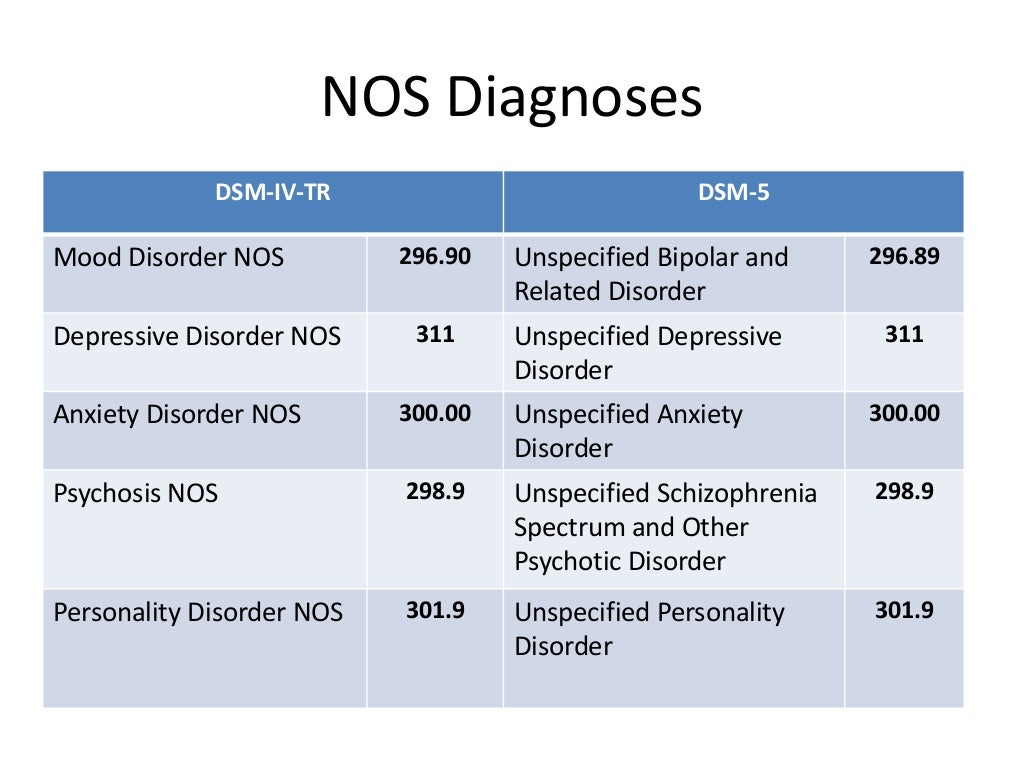
A mild stimulant use disorder is defined as the presence of 2-3 of the above symptoms.
A moderate stimulant use disorder is defined as the presence of 4-5 of the above symptoms.
A severe stimulant use disorder is defined as the presence of 6 or more of the above symptoms.
Stimulant psychosis
Stimulant psychosis or Stimulant-induced psychotic disorder . Occurs most commonly in high dose users (particularly with chronic use), but may rarely occur in patients taking therapeutic doses under medical supervision .
| Stimulant psychosis | |
|---|---|
| μB-11 | 6c46.6c45.6 |
| μb-10 | F14.5, F15.5 |
- 1 asymptoma
- 2 stimulants that cause psychosis
- 2.1 amphetamine
- 2.
 1.1PSihesis with one -time use
1.1PSihesis with one -time use - 2.1.2 DEPARITION OF Psychosis
- 2.1.0041
- 2.
- 2.2KOKain
- 2.3metkatinon (Ephedron)
- 2.4methylphenidate
- 2.5 METUMPETUMETUMETUMIN
- 2.6Kofoofin
- 2.1 amphetamine
- 3 Objects in the ICD-10 900 3.
- 3.3DSM-5
The symptoms caused by different stimulants differ slightly, but have features in common with organic psychoses, such as: hallucinations, delusions, thought disturbances, and, in rare cases, catatonia. nine0010
Physical symptoms in long-term stimulant abuse or overdose often accompany stimulant psychoses (but not organic psychoses). These additional symptoms may include aggression, arrhythmia, pupillary dilation, diarrhea, arterial hypertension, hyperthermia, nausea, shortness of breath, anxiety, convulsions, sleep deprivation, tremors, and vomiting.
Amphetamine
Amphetamine and its derivatives (amphetamines) are known to cause psychosis when used chronically or at high doses .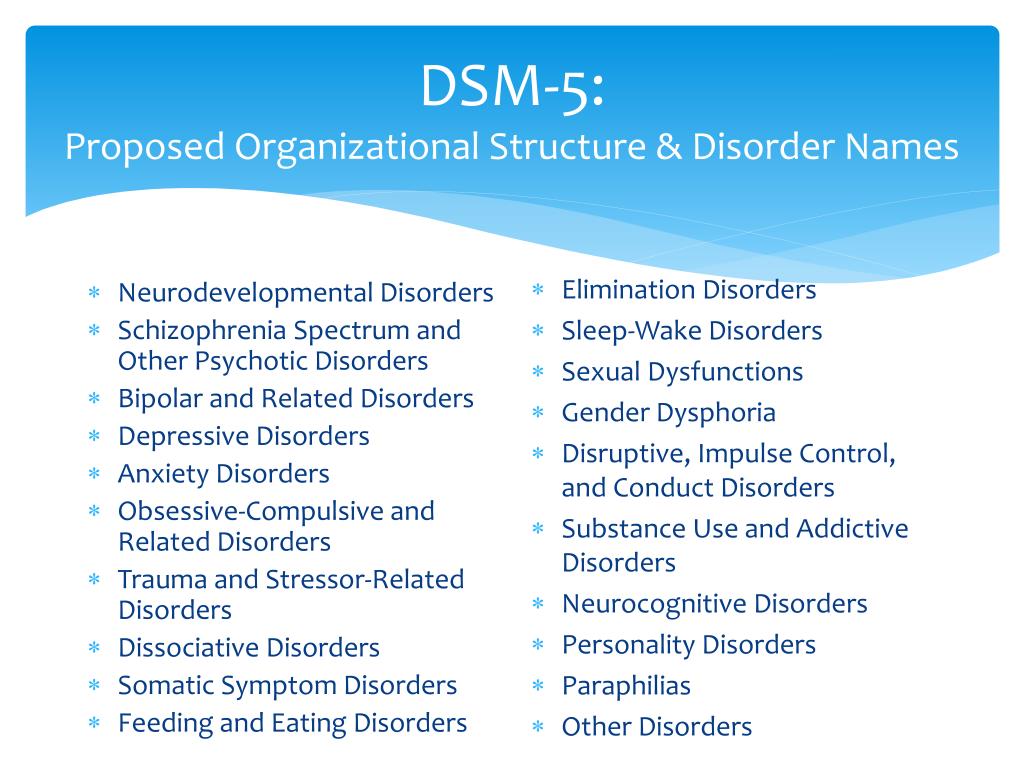 The word "amphetamines" means both (±)-1-phenylpropan-2-amine itself and its substituted derivatives. Examples of amphetamine derivatives: cathinone, ephedron, methamphetamine, methcathinone, methylphenidate.
The word "amphetamines" means both (±)-1-phenylpropan-2-amine itself and its substituted derivatives. Examples of amphetamine derivatives: cathinone, ephedron, methamphetamine, methcathinone, methylphenidate.
Dexamphetamine is used medicinally in Western countries under the trade name Dexedrine, and Adderall is a mixture of amphetamine salts (amphetamine aspartate monohydrate, amphetamine sulfate, dextroamphetamine sulfate, and dextroamphetamine sucrose). In medicine, lisdexamfetamine is also used. All of these drugs can cause stimulant psychosis when abused. nine0010
Symptoms of amphetamine psychosis include auditory and visual hallucinations, delusions of persecution and delusions of attitude along with clear consciousness and extreme agitation , sometimes there may be some signs of the Kandinsky-Clerambault syndrome . In this case, the person experiences tension and anxiety. The hallucinations are usually true, but pseudo-hallucinations may also occur .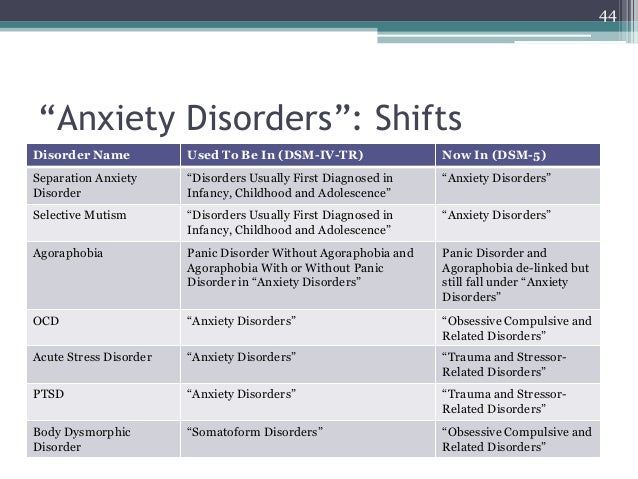
Microhallucinatory-paranoid syndrome sometimes occurs, as with cocaine use . It manifests itself in hallucinatory sensations of small insects on the body, or worms, dots, threads.
In rare cases, there is a catatonic stupor or catatonic excitation, a manic state, a state of ecstasy with fussiness and brightness of perceptions, a syndrome of obsessive-compulsive disorders on the background of a depressive-dysphoric mood .
The symptoms of acute amphetamine psychosis are very similar to the acute phase of schizophrenia . Sometimes people in the state of amphetamine psychosis had a symptom of blocking thoughts (breaks in the associative process), insertion or withdrawal of thoughts, echo of thoughts (sounding of their own thoughts), reasoning, inadequacy of facial expressions .
Only 50 mg of amphetamine have been reported to cause psychosis, but in some cases even 650 mg did not cause psychosis. This amount of the substance was administered 8 times to a healthy person, while he experienced only euphoria, increased libido, increased mental activity and productivity.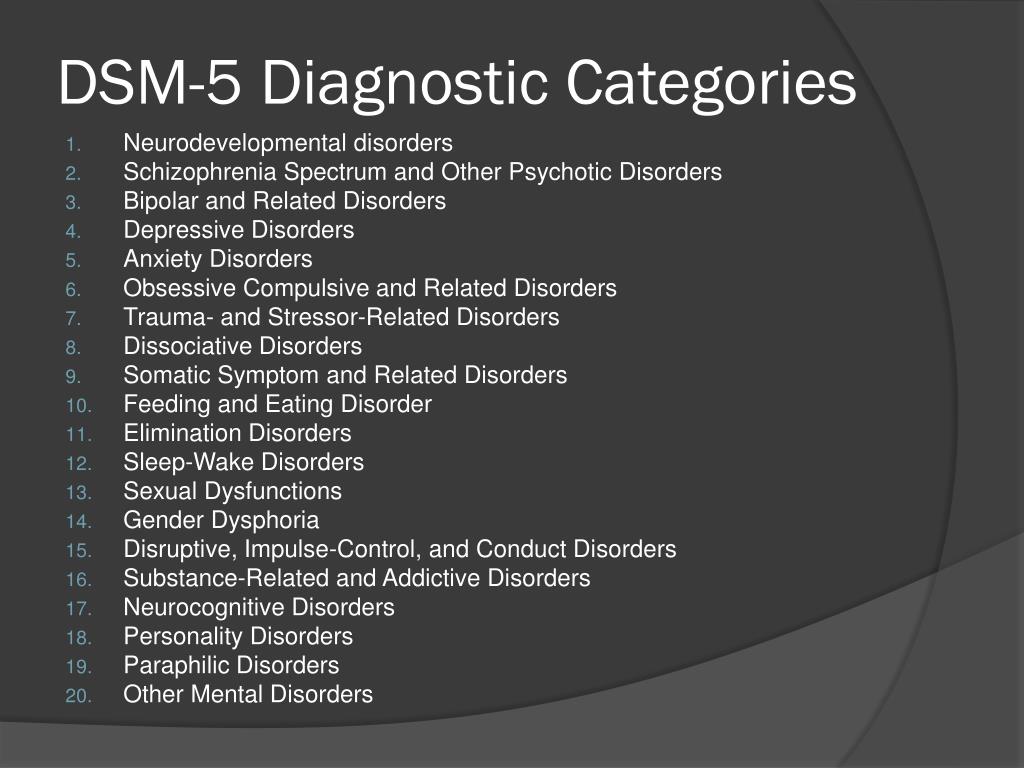 Each time after the end of the action of the substance, depression, memory impairment and a decrease in sexual desire were observed, but psychoses did not occur .
Each time after the end of the action of the substance, depression, memory impairment and a decrease in sexual desire were observed, but psychoses did not occur .
With continued use of amphetamine, psychosis increases, therefore, treatment requires its immediate withdrawal .
Single use psychosis
One patient developed convulsive seizures and further "unclear consciousness" from a single use of 140 mg of amphetamine .
There is a case of delirium in a 7.5-year-old child who consumed 300 mg of amphetamine while recovering from pharyngitis. Delirium was accompanied by hallucinations, the child observed small crawling insects in the corners of the room, experienced horror and was disoriented. At the physical level, there was an increase in temperature, dilated pupils, impaired coordination. The duration of this psychosis was less than a day, and it ended in complete recovery .
Duration of psychosis
The duration of psychosis as a result of acute poisoning usually lasts 1-3 days, in extremely rare cases it can be extended for a maximum of 1 week with a large amount of the drug used.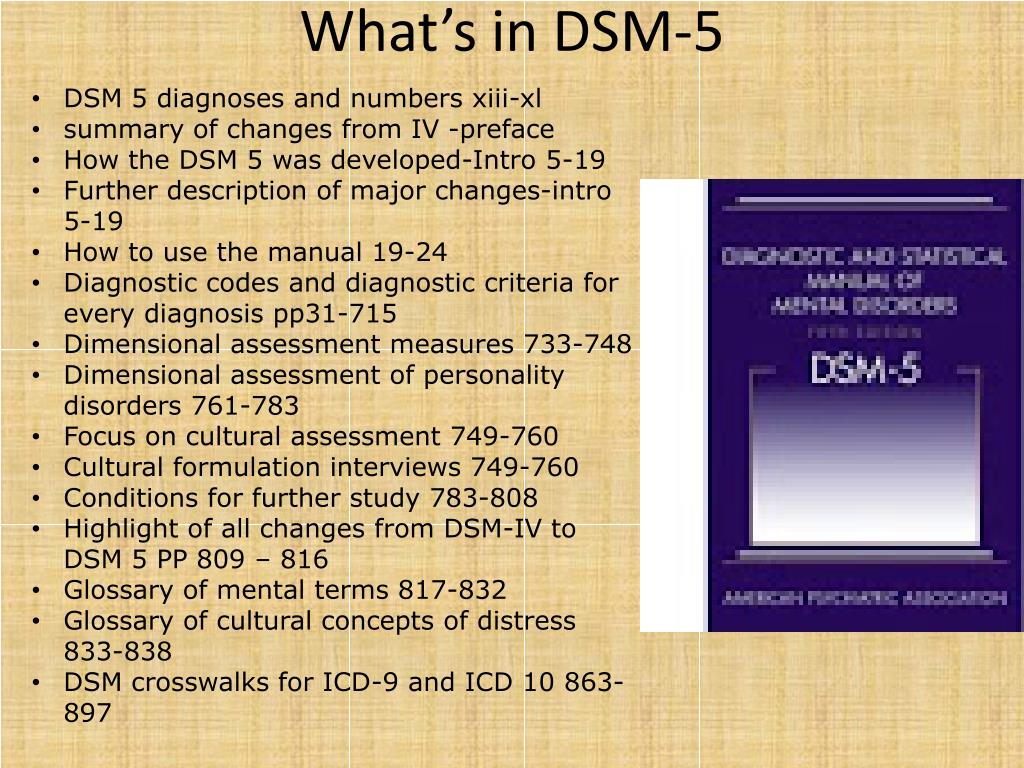
Connell studied 30 amphetamine abusers. In 2 of them, the psychosis was gone in 5-7 weeks, in 5 people - in 2-4 weeks, in 1 - in 2 weeks, and in the majority - 15 people - the psychosis was gone in less than 1 week. The medical history of the remaining 7 is unknown .
In rare cases, psychosis can last 2-7 months and even more than 3 years after stopping the use of amphetamine. Allier described a man who had been ill for 1.5 years with pseudo-hallucinations of a commentary nature ("voice") and a feeling of being controlled. In particular, he wrote that the patient believed that he (and the rest of the people) was being controlled using radar from the Vatican .
According to a study by Sano and Nagasaka, of 599 amphetamine abusers, 62% developed psychoses that resulted in rapid recovery. In 10% of patients, psychosis did not go away after 6 months after discontinuation of the drug .
In Japan, at the time of the amphetamine injection epidemic, there were many cases of chronic, long-term stimulant psychoses .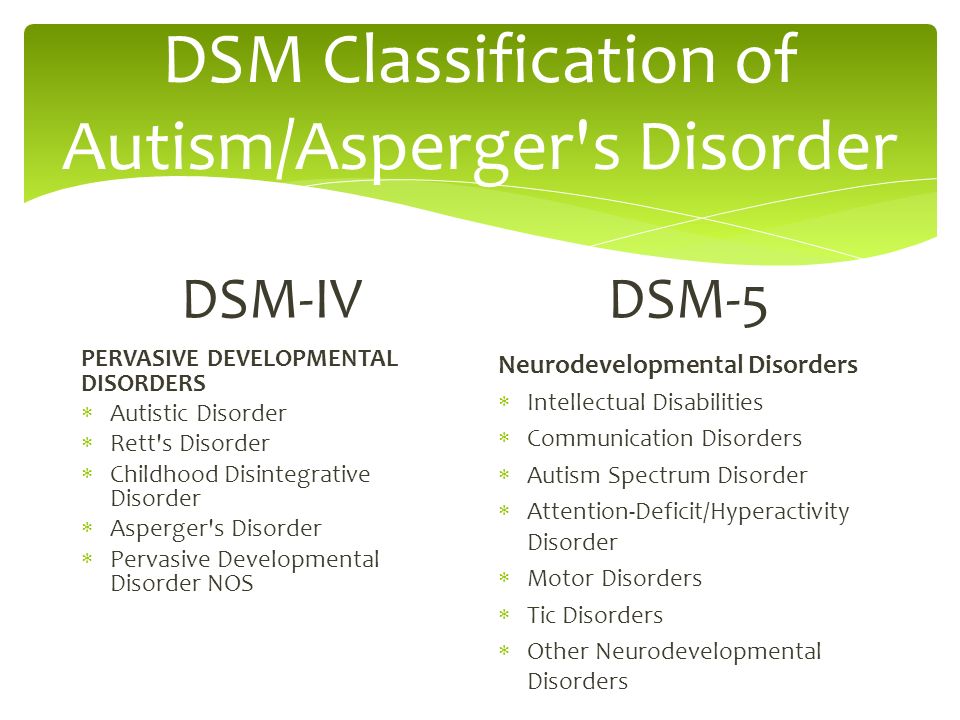
Somatic and neurological symptoms
Acute amphetamine psychosis may be accompanied by the following somatic symptoms: tachycardia, mydriasis, tremor, revitalization of tendon reflexes, dry mouth . However, with prolonged psychosis, these symptoms may be absent. nine0010
Cocaine
Cocaine powder.
Cocaine has the same short-term psychotic potential as amphetamine . More than half of cocaine abusers reported some psychotic symptoms . Typical symptoms include paranoid delusions: people feel they are being watched (specifically, they are being watched for their cocaine use) . Often there are hallucinations associated with delusional ideas . Dermatozoic delirium with goosebumps is also a fairly common reaction .
According to a study by Brady, Lydiard et al., 90% of patients (26 of 29) with cocaine-related stimulant psychosis had paranoid delusions (related to cocaine use), 96% of patients (28 of 29) had hallucinations, 21% (6 of 29) had tactile hallucinations, 38% (11 of 29) had visual hallucinations .
Metcathinone (ephedrone)
Metcathinone psychosis usually develops against the background of severe insomnia and general exhaustion of the body. Occurs in the form of rudimentary or acute paranoid with delusions of persecution, delusions of special significance, visual or verbal hallucinations . Rare are verbal hallucinosis and delusions of jealousy . The literature also describes cases of amental-like psychosis and twilight clouding of consciousness .
Methcathinone psychosis usually lasts 3-4 hours (in some patients it may last up to 1 month) .
Methylphenidate
Pack of Ritalin (active ingredient: methylphenidate).
Methylphenidate, used medically in Western countries under the trade name Ritalin, methylin, metadate, concerta, deutran (in the form of a transdermal patch), is a central nervous system stimulant with a similar mechanism of action to cocaine . This substance can also lead to psychosis if abused chronically .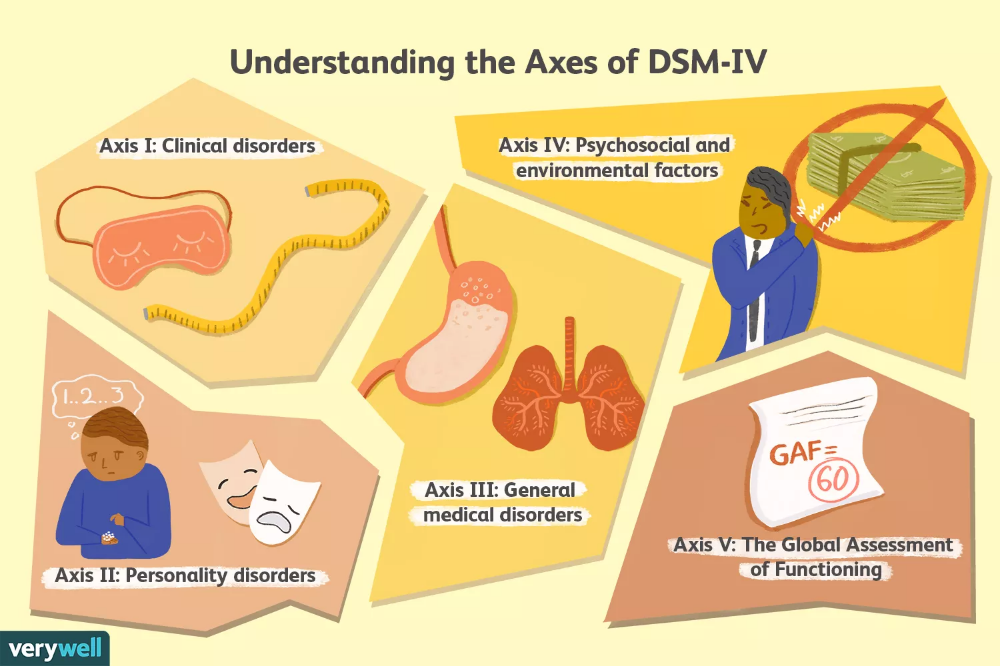
An overdose of methylphenidate results in symptoms similar to those of acute amphetamine intoxication . They include euphoria, delusions, disorientation, hallucinations, delirium, confusion, intoxication psychosis . When taking high doses of methylphenidate, aggressiveness, delirium, hallucinations and a state of panic may be observed .
The clinical picture of methylphenidate intoxication can include a wide range of symptoms, including schizophrenic symptoms, panic states (and panic attacks), manic-like states, anxiety states . When canceled - depressive states .
A case has been described of oral/intravenous administration of methylphenidate to patients with depression, in one of whom it caused severe depersonalization, in another - paranoid psychosis . Another clinical case is paranoid psychosis in a 36-year-old man who used intravenous methylphenidate 100-200 mg daily .
Methamphetamine
Crystal methamphetamine.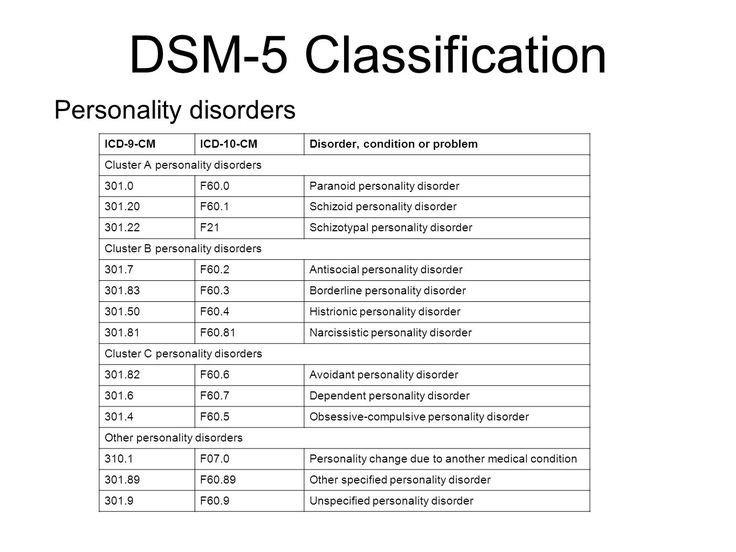
Methamphetamine is used medically in Western countries under the name "deoxin" and is available in 5 mg tablets, but illicit methamphetamine use is more commonly associated with stimulant psychosis and at much higher doses. nine0010
According to one Australian study in 2006, 18% of 309 active methamphetamine users experienced psychosis in the past year .
Symptoms of methamphetamine psychosis: auditory, visual, tactile and olfactory hallucinations, delusions of persecution and delusions of relations (erroneous assessment by the patient of the attitude of other people towards him), compulsive behavior, stereotypes, anhedonia, depression, flattened affect . Most often, psychosis occurs in the form of a rudimentary or acute paranoid with delusions of persecution, special significance, with visual or verbal hallucinations . Like amphetamine psychosis, it is similar to that of schizophrenic patients . The literature also describes manic-delusional psychoses .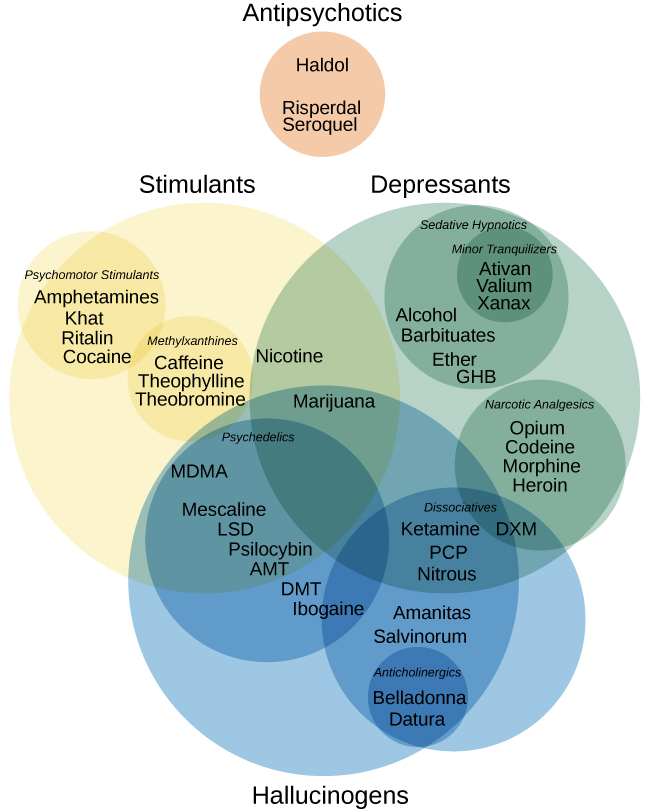
A case of twilight clouding of consciousness in a patient who abused methamphetamine for about 2 years is described. The condition lasted 8 days, while the patient experienced visual and auditory hallucinations, heard the voice of the planet Mars, and believed that in this way this planet tried to make contact with the Earth. Tachycardia up to 120 per minute, mydriasis and arterial hypertension were also observed. nine0010
Methamphetamine psychosis usually occurs after many days of substance use, in doses of 6-11 ml intravenously per day . The duration of the psychotic disorder is usually 8 to 10 hours, but can be up to 1 month .
Caffeine
It has been suggested that caffeine in high doses or chronic abuse may induce psychosis in healthy people or exacerbate pre-existing psychosis in patients with schizophrenia .
Chronic use of caffeine, theobromine, theophylline in high doses can lead to debilitation of the nervous system, which can become the basis for subsequent psychosis .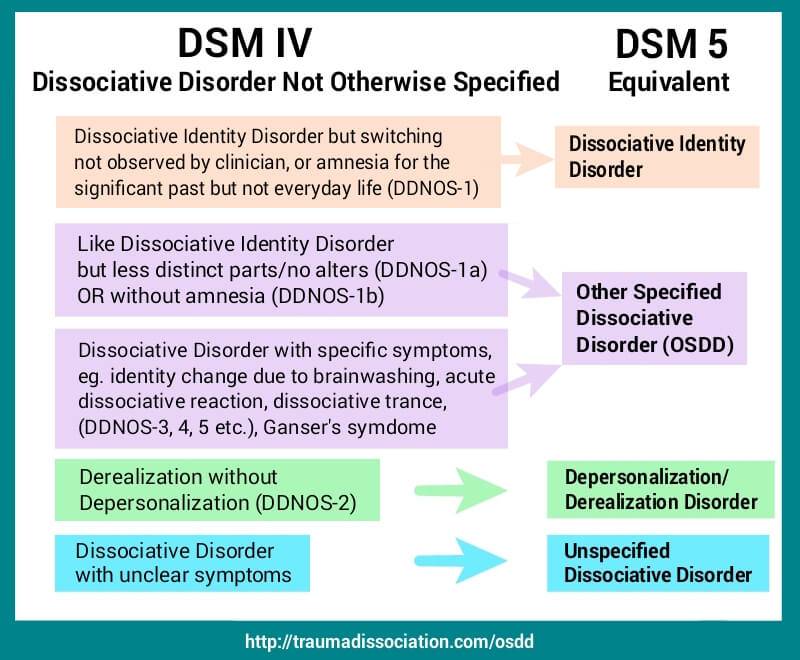
The most commonly reported delirium is caused by an overdose of caffeine . There is an influx of vivid visual hallucinations, sometimes auditory, a person loses orientation in the world around him. After removing caffeine from the body, the memory of the past is usually partially or completely preserved. Some patients lose the ability to judge distances correctly, and objects appear closer to them than they really are. Somatic disorders associated with delirium: mydriasis, hyperemia, ataxia, tachycardia, intense thirst, dry skin and mucous membranes, cyanosis of the skin, sometimes increased blood pressure and fever . Neurological and somatic symptoms are similar to those in atropine poisoning .
In more severe cases, there may be a deeper clouding of consciousness, accompanied by senseless motor excitation . In these cases, subsequent complete amnesia is frequent and the clinical picture is closer to twilight stupefaction .
An elderly woman who consumed 300 grams of coffee daily (about 30 g of pure caffeine) for two years experienced a psychosis with disorientation in the surrounding space, episodic visual hallucinations, euphoria, agitation, which ended in death .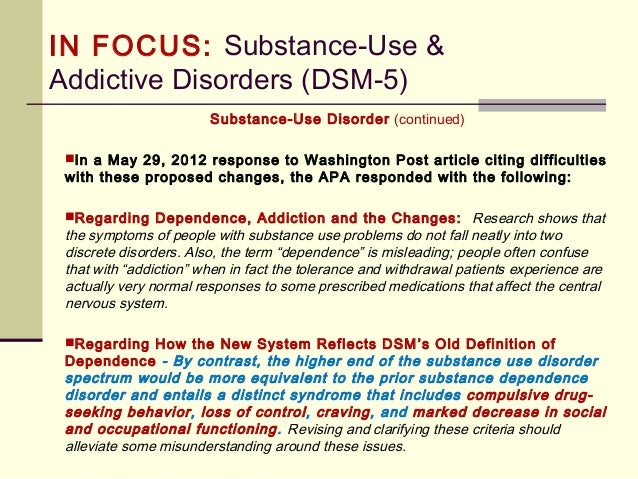
There are also cases of hallucinosis . Protracted psychoses with visual and auditory hallucinations with prolonged abuse of tea are described by VP Polyakov and Wark .
Affective psychoses in long-term caffeine abusers are quite rare, but a case has been described of a state resembling hypomanic .
Caffeine poisoning psychoses with impaired consciousness usually do not last more than a few days . nine0010
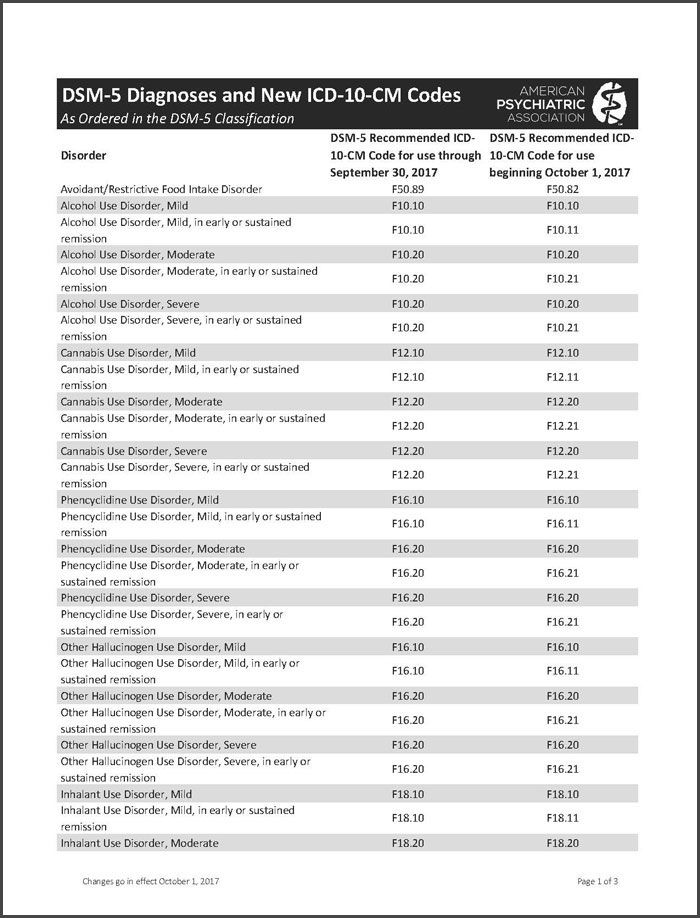
ICD-10
In the International Classification of Diseases, 10th Revision (ICD-10), psychotic disorders associated with the use of stimulants are designated by the following codes:
- F14.50 Schizophrenia-like disorder due to cocaine use cocaine use disorder
- F14.52 Cocaine use predominantly hallucinatory disorder
- F14.53 Cocaine use predominantly polymorphic psychotic disorder
- F14.54 Cocaine use disorder with predominantly depressive psychotic symptoms
- F14.55 Cocaine use disorder with predominantly manic psychotic symptoms
- F15.
50 Other stimulant use disorder (including caffeine) schizophrenia-like disorder (including caffeine)
Predominantly delusional disorder associated with the use of other stimulants (including caffeine) - F15.52 Predominantly hallucinatory disorder associated with the use of other stimulants (including caffeine)
- F15.53 Predominantly polymorphic psychotic disorder associated with the use of other stimulants (including caffeine)
- F15.54 Use disorder associated with the use of other stimulants (including caffeine) with predominantly depressive psychotic symptoms
- F15.55 Use disorder other stimulants (including caffeine) with predominantly manic psychotic symptoms
ICD-11
Exists as a separate category in ICD-11 - "stimulant-induced psychotic disorder, including amphetamines, methamphetamine and methcathinone" (6C46.6) and "cocaine-induced psychotic disorder” (6C45.6) .
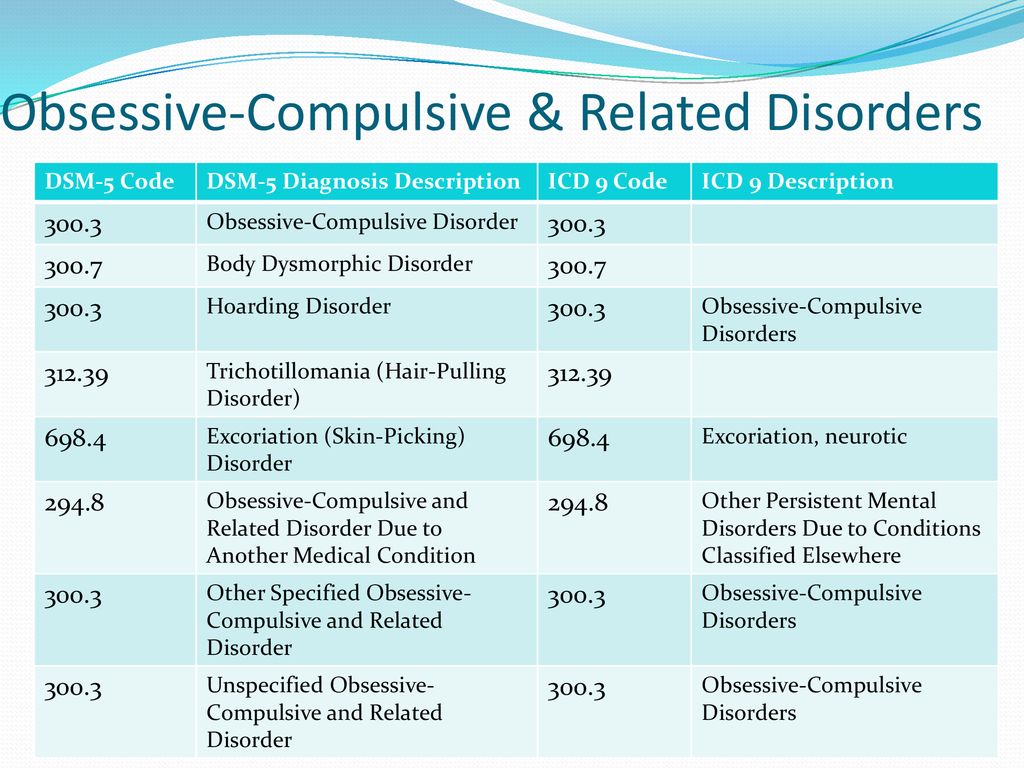
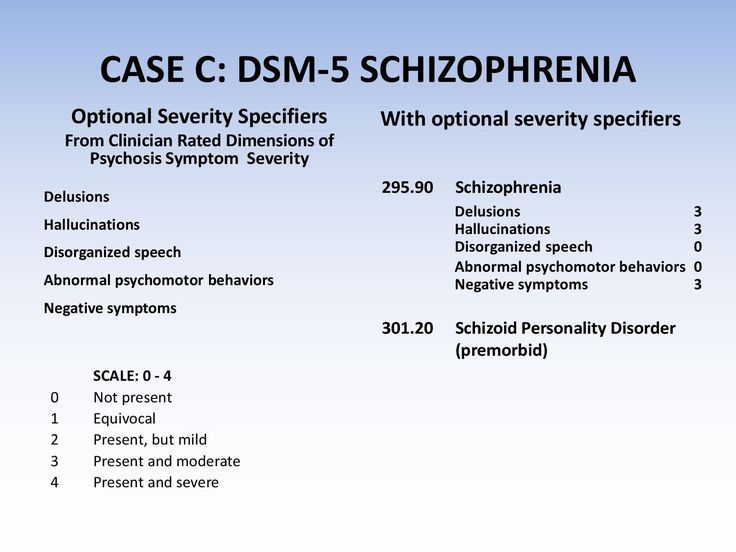
DSM-5
DSM-5 has a diagnosis of substance/medication-induced psychotic disorder.
ICD-9-CM code for amphetamine (or other stimulants) and cocaine: 292.9.
Amphetamine (or other stimulants). ICD-10-KM codes:
- F15.159 With substance use disorder, mild.
- F15.259 With a substance use disorder, moderate or severe.
- F15.959 No use disorder.
Cocaine. ICD-10-KM codes:
- F14.159 With substance use disorder, mild.
- F14.259 With a substance use disorder, moderate or severe.
- F14.959 No use disorder.
Treatment of overdose is to relieve symptoms during the acute phase of intoxication: maintaining normal body temperature, blood pressure and heart rate at an acceptable level until the substance is successfully metabolized and vital body functions return to baseline. nine0010
Short-term use of typical and atypical antipsychotics (neuroleptics) is indicated in the early stages of psychosis treatment . In case of an overdose of psychostimulants, for example, haloperidol 5 mg 2 times a day can be prescribed . These drugs are effective in eliminating delirium and paranoid psychosis.
These drugs are effective in eliminating delirium and paranoid psychosis.
In patients with overdose, with observed arterial hypertension, it is preferable to prescribe chlorpromazine (chlorpromazine), since, in addition to dopamine receptors (D₁, D₂, D₃ and D₄), it blocks α-adrenergic receptors . The standard dosage is 50 mg 4 times a day, but may be increased to 100 mg . For more severe hypertension or tachyarrhythmias, beta-blockers such as propranolol (1 mg IV every 5 to 10 minutes until a dose of 8 mg is reached) are prescribed .
Phenazepam, diazepam, lorazepam, or other benzodiazepines may be used to induce additional sedation that relieves stimulation of higher mental functions and arousal. .
- Long-term hallucinogen-induced perceptual disorder
- Hallucinatory paranoid syndrome
- Health effects of cocaine
- World Health Organization. (English) (2018).
- Curran C., Byrappa N.
 , McBride A. Stimulant psychosis: systematic review. // British Journal of Psychiatry : journal. - Royal College of Psychiatrists (English) Russian, 2004. - Vol. 185.-P. 196-204. — doi:. - .
, McBride A. Stimulant psychosis: systematic review. // British Journal of Psychiatry : journal. - Royal College of Psychiatrists (English) Russian, 2004. - Vol. 185.-P. 196-204. — doi:. - . - Shoptaw S. J., Kao U., Ling W. W. Treatment for amphetamine psychosis.(English) // Cochrane Database of Systematic Reviews : journal. — 2008. —No. 4. doi:. - .
- Dore G., Sweeting M. Drug-induced psychosis associated with crystalline methamphetamine // Australasian Psychiatry (English) Russian. : journal. - 2006. -Vol. 14, no. 1. -P. 86-89. — ISSN. — doi:.
- Srisurapanont M., Ali R., Marsden J., Sunga A., Wada K., Monteiro M. Psychotic symptoms in methamphetamine psychotic in-patients // The International Journal of Neuropsychopharmacology Russian : journal. - 2003. -Vol. 6 no. 4. -P. 347-352. — ISSN. — doi:. nine0041
- L. K. Shaidukova. Classical narcology. - 2008. - S. 47. - 260 p. - ISBN 978-5-94981-091-0.
- Stolyarov, 1964, p.
 120.
120. - Stolyarov, 1964, p. 121.
- Waud S. P. The effects of toxic doses of benzyl methyl carbinamine (Benzedrine) in man // JAMA : journal. - 1938. -Vol. 110 no. 3. -P. 206.-ISSN. — doi:.
- Stolyarov, 1964, p. 122.
- Apfelberg B. - Acta Neurol, 1960, v. 15, p. 355
- Shanson B. . Brit. med. J., 1956, p. I, p. 576
- Connell P. H. Amphetamine Psychosis. - London: Oxford University Press, 1961.
- Alliez, J. (1953) Délire amphétaminique (French). L'Encéphale 42: 21
- Sano I., Nagasaka Uber chronische Weckaminsucht in Japan . Fortschr. Neurol Psychiat., 1956, Bd. 24, S. 391
- Koyama T., Muraki A., Nakayama M. et al (1991) CNS stimulant abuse; long lasting symptoms of amphetamine psychosis. Biological Psychiatry, 2 , 63-65.
- Stolyarov, 1964, p. 123.
- Brady K. T., Lydiard R. B., Malcolm R., Ballenger J. C. Cocaine-induced psychosis. (English) // The Journal of Clinical Psychiatry (English) Russian.
 : journal. - 1991. -Vol. 52, no. 12.-p. 509-512. - .
: journal. - 1991. -Vol. 52, no. 12.-p. 509-512. - . - Jagadisha Thirthalli, Vivek Benegal. . Department of Psychiatry, National Institute of Mental Health and Neuro Sciences (NIMHANS), Bangalore, India. Retrieved 8 March 2017. January 29, 2013.
- Elliott A., Mahmood T., Smalligan R. D. Cocaine bugs: a case report of cocaine-induced delusions of parasitosis. (English) // Am J Addict : journal. - 2012. -Vol. 21, no. 2. -P. 180-181. — doi:. - .
- Ivanets, Tyulpin et al., 2006, p. 737.
- Auriel E., Hausdorff J. M., Giladi N. Methylphenidate for the Treatment of Parkinson Disease and Other Neurological Disorders // Clinical Neuropharmacology (English) Russian. : journal. - 2008. - October (vol. 32, no. 2). -p. 75-81. — doi:. - . nine0041
- Abramowicz M. J., Van Haecke P., Demedts M., Delcroix M. // Eur. Respir. J.: journal. - 2003. -Vol. 22, no. 3. -P. 560-562. — doi:. - .
- Morton W.
 A., Stockton G. G. . The Primary Care Companion to The Journal of Clinical Psychiatry 2000;2:159-64.
A., Stockton G. G. . The Primary Care Companion to The Journal of Clinical Psychiatry 2000;2:159-64. - Spensley J., Rockwell D. // The New England Journal of Medicine : journal. - 1972. - April (vol. 286). -p. 880-881. — doi:.
- Koutsky C. D., Westendorp F., Bransford P. High dosage methylphenidate for depression.(English) // The Journal of Clinical Psychiatry(English) Russian. : journal. - 1960. -Vol. 21.-P. 275-277. - .
- McKetin R., McLaren J., Lubman D. I., Hides L. The prevalence of psychotic symptoms among methamphetamine users. // Addiction : journal. - 2006. -Vol. 101, no. 10. -p. 1473-1478. — doi:. - .
- Bankole A. Johnson, DSc, MD. Addiction Medicine. - volume 1. - Springer, 2011. - P. 501. - ISBN 978-1-4419-0338-9.
- Ivanets, Tyulpin et al., 2006, p. 741.
- Kalus F., Kucher J., Zutt J. Über Psychosen bei chronischem Pervitin-missbrauch . Nervenarzt, 1942, Bd. 15, S. 313
- Hedges D.
 W., Woon F. L., Hoopes S. P. Caffeine-induced psychosis. (English) // CNS Spectrums : journal. - 2009. -Vol. 14, no. 3. -P. 127-129. - .
W., Woon F. L., Hoopes S. P. Caffeine-induced psychosis. (English) // CNS Spectrums : journal. - 2009. -Vol. 14, no. 3. -P. 127-129. - . - Joseph M. Cerimele, Adam P. Stern, Didier Jutras-Aswad. Psychosis following excessive ingestion of energy drinks in a patient with schizophrenia. (English) // The American Journal of Psychiatry : journal. - 2010. -Vol. 167 no. 3. -P. 353.-doi:. - . nine0041
- Broderick P., Benjamin A. B. // The Journal of the Oklahoma State Medical Association. - 2004. - Vol. 97 no. 12. - P. 538-542. - . [edit]
- M. Solinas, S. Ferré, Z. You, M. Karcz-Kubicha, P. Popoli, S. Goldberg. (English) // Journal of Neuroscience (English) Russian. : journal. - 2002. -Vol. 14, no. 3. -P. 127-129.
- Stolyarov, 1964, p. 140.
- Stolyarov, 1964, p. 141.
- Stolyarov, 1964, p. 140-141.
- Stolyarov, 1964, p. 142.
- Wagner W. - Der Nervenarzt, 1939, Bd, 12, S. 296
- Stolyarov, 1964, p.
 143.
143. - Stolyarov, 1964, p. 144.
- Polyakov V.P. - Neurologist. and Psychiatry, 1951, v. 20, p. 77.
- Arana J., Rosenbaum J. Handbook of Psychiatric Drug Therapy. - M. : BINOM Publishing House, 2004. - 416 p. — ISBN 5-9518-0098-6.
- Stolyarov G. V. / ed. V. M. Banshchikov. - nine0483 M. : Medicine, 1964.
- N. N. Ivanets, Yu. G. Tyulpin, V. V. Chirko, M. A. Kinkulkina. Psychiatry and narcology: textbook. - M. : GEOTAR-Media, 2006. - 832 p. — ISBN 5-9704-0197-8.
, stimulant psychosis, portal of doctors of the Chelyabinsk region and the city of Chelyabinsk
Stimulant psychosis , or Psychotical upset, pronounced by a stimulant of , a mental disorder with psychotic symptoms (for example, hallucinations, paranoid ideas, brading ideas and bred thinking and frantic thinking and frantic thinking and frantic thinking.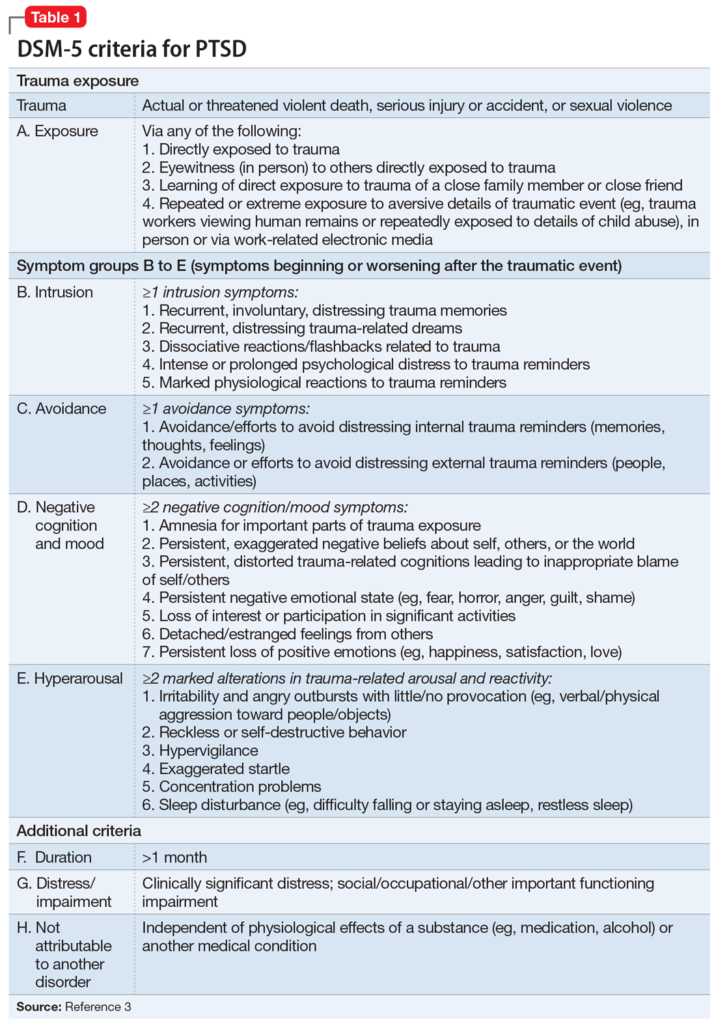 behavior) that occurs in some people who use psychostimulants. Most often occurs in patients taking large doses (especially with chronic use), but, in rare cases, may occur in patients using therapeutic doses under the supervision of a physician. nine0010
behavior) that occurs in some people who use psychostimulants. Most often occurs in patients taking large doses (especially with chronic use), but, in rare cases, may occur in patients using therapeutic doses under the supervision of a physician. nine0010
Contents
- 1 Symptoms
- 2 Stimulants causing psychosis
- 2.1 Amphetamine
- 2.1.1 Single use psychoses
- 2.1.2 Duration of psychosis
- 2.1.3 Somatic and neurological symptoms
- 2.2 Cocaine
- 2.3 Metcathinone (ephedron)
- 2.4 Methylphenidate
- 2.5 Methamphetamine
- 2.6 Caffeine
- 2.1 Amphetamine
- 3 Designation in ICD-10 and DSM-5 nine0039
- 3.1 ICD-10
- 3.2 ICD-11
- 3.3 DSM-5
Symptoms
The symptoms caused by different stimulants differ slightly, but share features with organic psychoses, such as: hallucinations, delusions, thought disturbances, and, in rare cases, catatonia.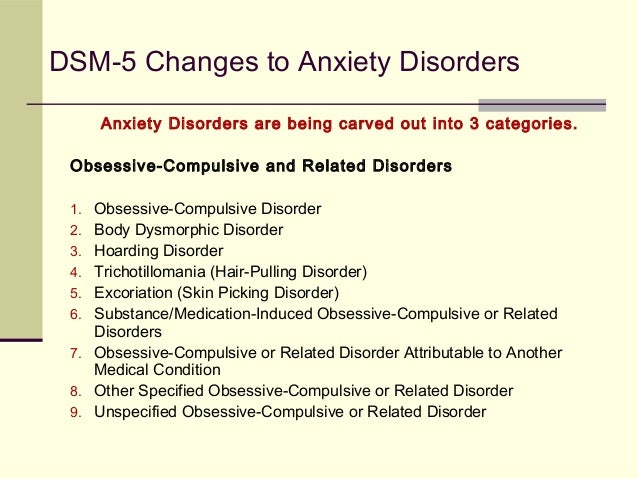
Physical symptoms in long-term stimulant abuse or overdose often accompany stimulant psychoses (but not organic psychoses). These additional symptoms may include aggression, arrhythmia, pupillary dilation, diarrhea, arterial hypertension, hyperthermia, nausea, shortness of breath, anxiety, convulsions, sleep deprivation, tremors, and vomiting. nine0010
Stimulants causing psychosis
Amphetamine
Amphetamine and its derivatives (amphetamines) are known to cause psychosis when used chronically or at high doses. The word "amphetamines" means both (±)-1-phenylpropan-2-amine itself and its substituted derivatives. Examples of amphetamine derivatives: cathinone, ephedron, methamphetamine, methcathinone, methylphenidate.
Dexamphetamine is used medicinally in Western countries under the trade name Dexedrine, and Adderall is a mixture of amphetamine salts (amphetamine aspartate monohydrate, amphetamine sulfate, dextroamphetamine sulfate, and dextroamphetamine sucrose).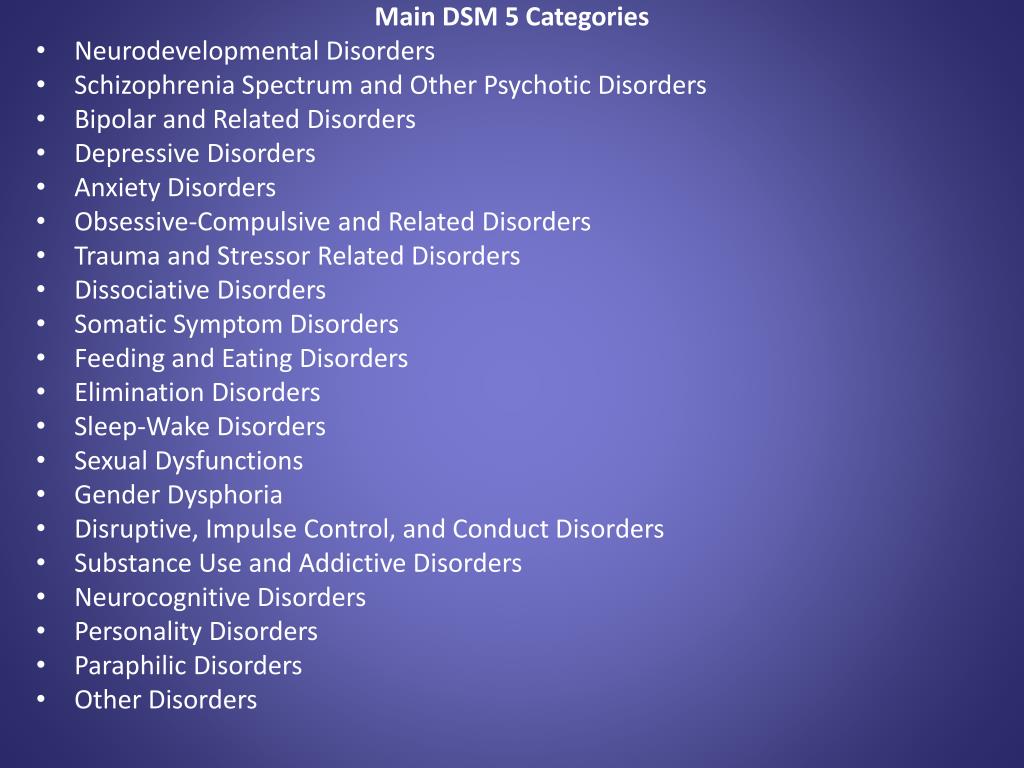 In medicine, lisdexamfetamine is also used. All of these drugs can cause stimulant psychosis when abused. nine0010
In medicine, lisdexamfetamine is also used. All of these drugs can cause stimulant psychosis when abused. nine0010
Symptoms of amphetamine psychosis include auditory and visual hallucinations, delusions of persecution and delusions of attitude along with clear consciousness and extreme agitation, sometimes there may be some signs of mental automatism syndrome (Kandinsky-Clerambault syndrome). In this case, the person experiences tension and anxiety. Hallucinations are usually true, but pseudohallucinations can also be observed.
Sometimes there is a microhallucinatory-paranoid syndrome, as with cocaine use. It manifests itself in hallucinatory sensations of small insects on the body, or worms, dots, threads. nine0010
In rare cases, there is a catatonic stupor or catatonic excitation, a manic state, a state of ecstasy with fussiness and brightness of perceptions, a syndrome of obsessive-compulsive disorders on the background of a depressive-dysphoric mood.
The symptoms of acute amphetamine psychosis are very similar to those of the acute phase of schizophrenia.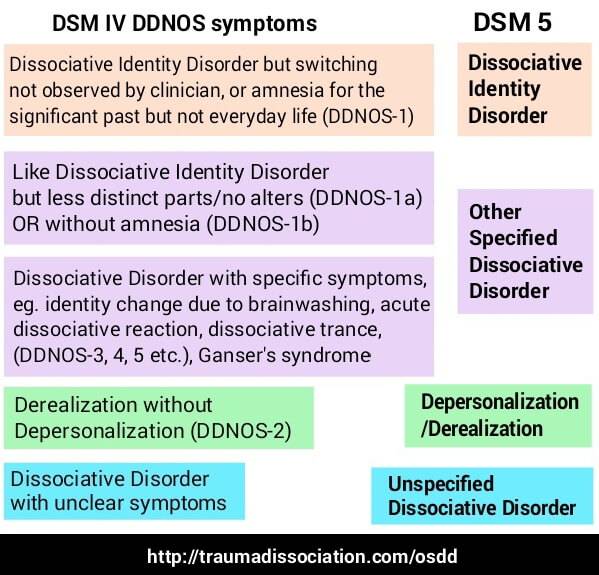 Sometimes people in a state of amphetamine psychosis had a symptom of blocking thoughts (breaks in the associative process), insertion or withdrawal of thoughts, echo of thoughts (sounding of their own thoughts), reasoning, inadequacy of facial expressions. nine0010
Sometimes people in a state of amphetamine psychosis had a symptom of blocking thoughts (breaks in the associative process), insertion or withdrawal of thoughts, echo of thoughts (sounding of their own thoughts), reasoning, inadequacy of facial expressions. nine0010
Only 50 mg of amphetamine have been reported to cause psychosis, but in some cases even 650 mg did not cause psychosis. This amount of the substance was administered 8 times to a healthy person, while he experienced only euphoria, increased libido, increased mental activity and productivity. Each time after the end of the action of the substance, depression, memory impairment and a decrease in sexual desire were observed, but psychoses did not occur.
With continued use of amphetamine, psychosis increases, so treatment requires immediate withdrawal. nine0010
Psychosis with a single use
One patient developed convulsive seizures and further "unclear consciousness" from a single use of 140 mg of amphetamine.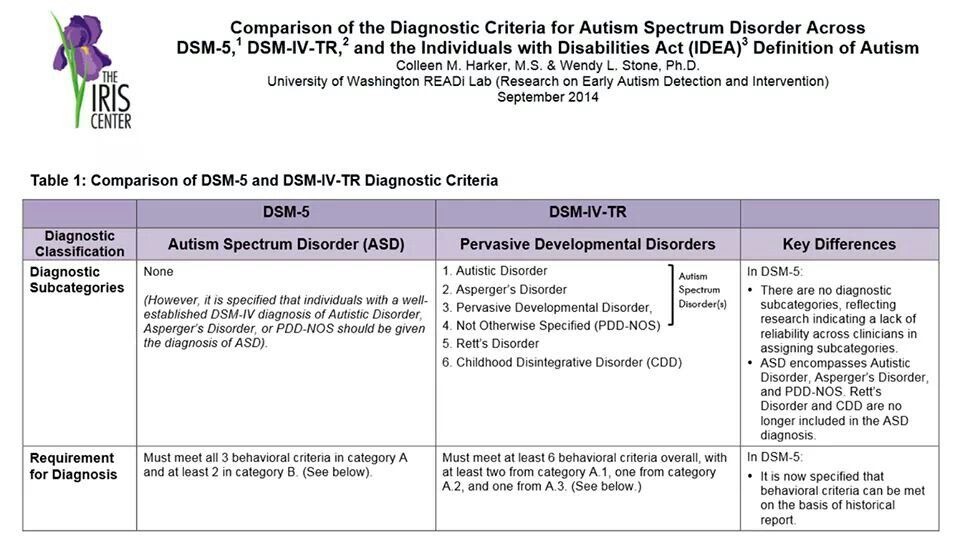
A case of delirium was reported in a 7.5-year-old child who used 300 mg of amphetamine while recovering from pharyngitis. Delirium was accompanied by hallucinations, the child observed small crawling insects in the corners of the room, experienced horror and was disoriented. At the physical level, there was an increase in temperature, dilated pupils, impaired coordination. The duration of this psychosis was less than a day, and it ended in complete recovery. nine0010
Duration of psychosis
The duration of psychosis as a result of acute poisoning usually lasts 1-3 days, in extremely rare cases it is extended by 1 week maximum with a large amount of the drug used.
Connell studied 30 amphetamine abusers. In 2 of them, the psychosis was gone in 5-7 weeks, in 5 people - in 2-4 weeks, in 1 - in 2 weeks, and in the majority - 15 people - the psychosis was gone in less than 1 week. The medical history of the remaining 7 is unknown. nine0010
In rare cases, psychosis can last 2–7 months or even more than 3 years after amphetamine use has been stopped.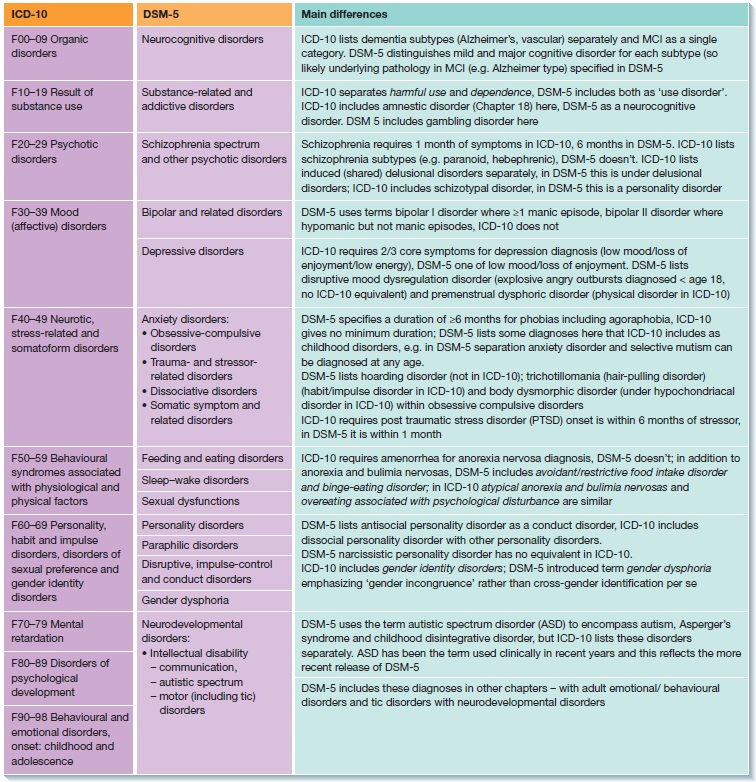 Allier described a man who had been ill for 1.5 years with pseudo-hallucinations of a commentary nature ("voice") and a feeling of being controlled. In particular, he wrote that the patient believed that he (and the rest of the people) was controlled by radar from the Vatican.
Allier described a man who had been ill for 1.5 years with pseudo-hallucinations of a commentary nature ("voice") and a feeling of being controlled. In particular, he wrote that the patient believed that he (and the rest of the people) was controlled by radar from the Vatican.
According to a study by Sano and Nagasaka, of 599 amphetamine abusers, 62% developed psychoses that resulted in rapid recovery. In 10% of patients, psychosis did not go away after 6 months after discontinuation of the drug. nine0010
In Japan, at the time of the amphetamine injection epidemic, there were many cases of chronic, long-term stimulant psychoses.
Somatic and neurological symptoms
Acute amphetamine psychosis may be accompanied by the following somatic symptoms: tachycardia, mydriasis, tremor, revitalization of tendon reflexes, dry mouth. However, with prolonged psychosis, these symptoms may be absent.
Cocaine
Cocaine powder.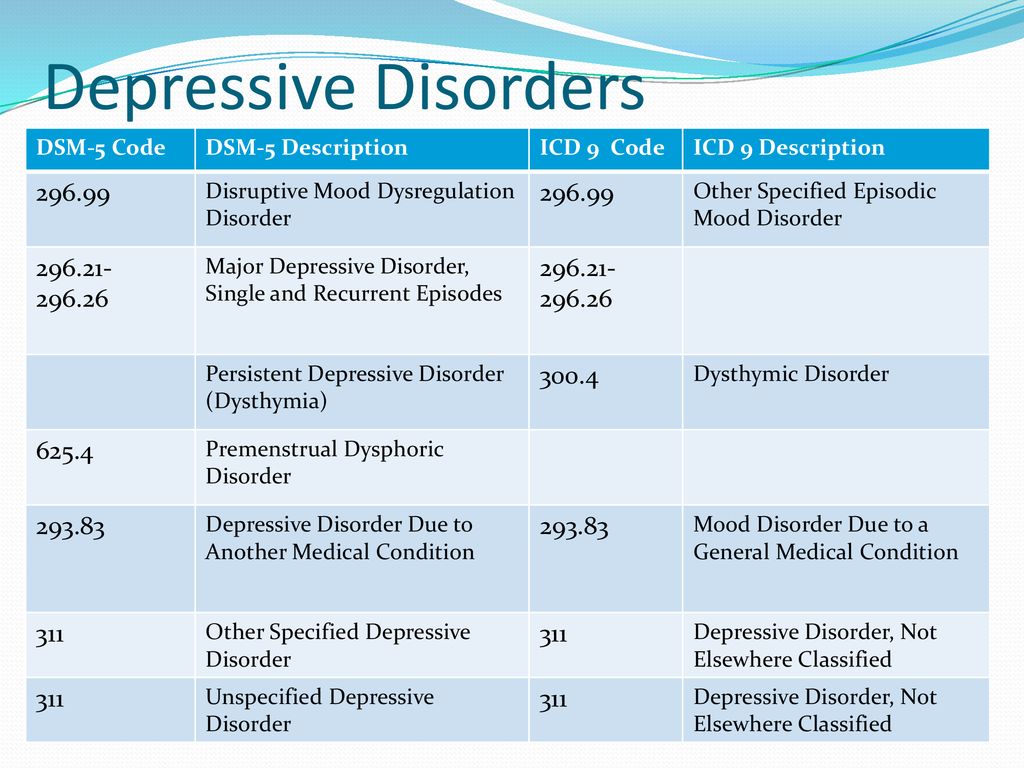
Cocaine has the same potential to cause short-term psychosis as amphetamine. More than half of cocaine abusers reported some psychotic symptoms. Typical symptoms include paranoid delusions: people feel they are being watched (specifically, they are being watched for their cocaine use). Often there are hallucinations associated with delusional ideas. Dermatozoic delirium with goosebumps is also a fairly common reaction. nine0010
According to Brady, Lydiard et al., 90% of patients (26 of 29) with cocaine-related stimulant psychosis had paranoid delusions (related to cocaine use), 96% of patients (28 of 29) had hallucinations, 21% (6 of 29) had tactile hallucinations, 38% (11 of 29) had visual hallucinations.
Metcathinone (ephedron)
Metcathinone psychosis usually develops against the background of severe insomnia and general exhaustion of the body. It proceeds in the form of a rudimentary or acute paranoid with delusions of persecution, delusions of special significance, visual or verbal hallucinations.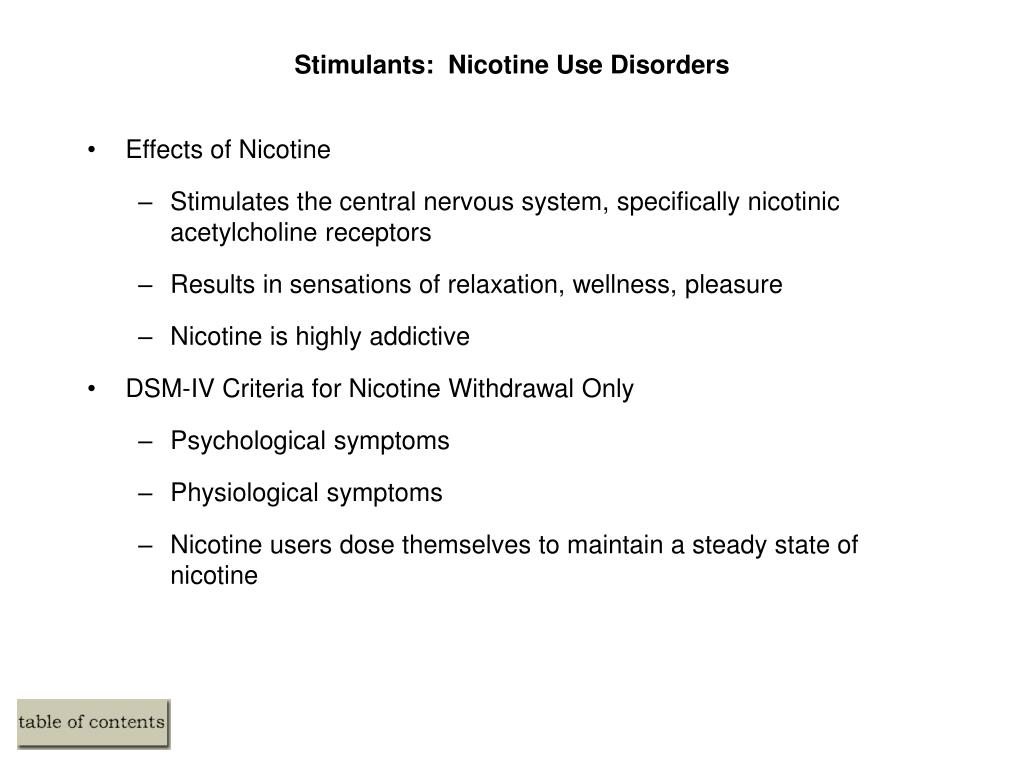 Verbal hallucinosis and delusions of jealousy are rare. The literature also describes cases of amental-like psychosis and twilight clouding of consciousness. nine0010
Verbal hallucinosis and delusions of jealousy are rare. The literature also describes cases of amental-like psychosis and twilight clouding of consciousness. nine0010
Methcathinone psychosis usually lasts 3-4 hours (in some patients it can last up to 1 month).
Methylphenidate
Pack of Ritalin (active ingredient: methylphenidate).
Methylphenidate, used medically in Western countries under the trade name Ritalin, methylin, metadate, concerto, deutran (in the form of a transdermal patch), is a central nervous system stimulant with a similar mechanism of action to cocaine. This substance, when chronically abused, can also lead to psychosis. nine0010
An overdose of methylphenidate results in symptoms similar to those of acute amphetamine intoxication. They include euphoria, delusions, disorientation, hallucinations, delirium, confusion, intoxication psychosis. When taking high doses of methylphenidate, aggressiveness, delirium, hallucinations and a state of panic can be observed.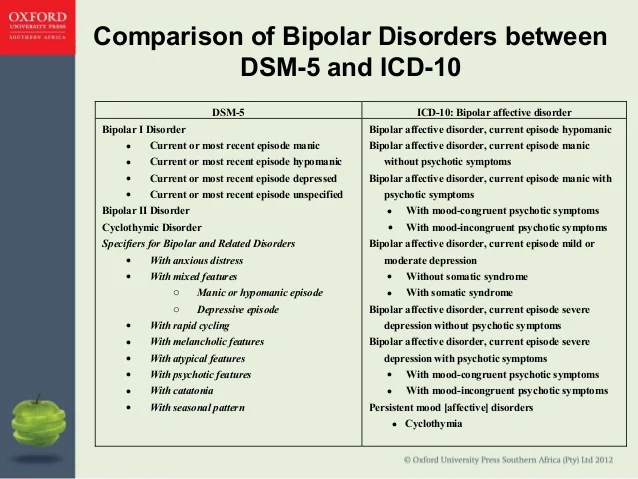
The clinical picture of methylphenidate intoxication can include a wide range of symptoms, including schizophrenic symptoms, panic states (and panic attacks), manic-like states, anxiety states. When canceled - depressive states. nine0010
A case has been described of oral/intravenous administration of methylphenidate to patients with depression, in one of whom it caused severe depersonalization, in another - paranoid psychosis. Another clinical case is paranoid psychosis in a 36-year-old man who used intravenously 100-200 mg of methylphenidate daily.
methamphetamine
Crystal methamphetamine.
Methamphetamine is used medically in Western countries under the name "deoxin" and comes in 5 mg tablets, but illicit methamphetamine use is more commonly associated with stimulant psychosis and at much higher doses. nine0010
According to one Australian study in 2006, 18% of 309 active methamphetamine users experienced psychosis in the past year.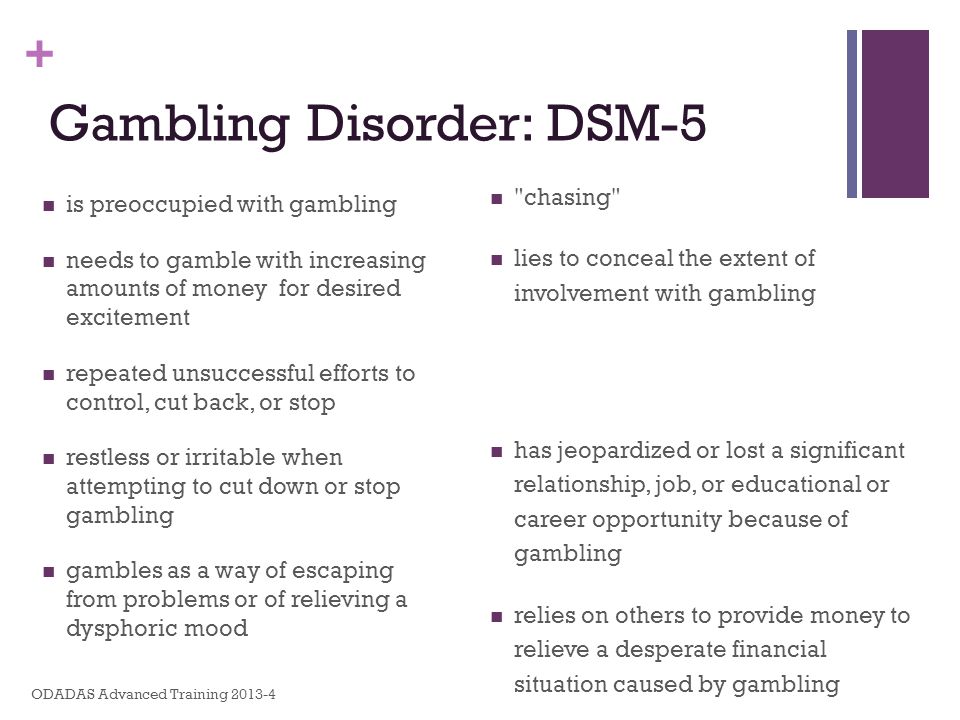
Symptoms of methamphetamine psychosis: auditory, visual, tactile and olfactory hallucinations, delusions of persecution and delusions of relations (erroneous assessment by the patient of the attitude of other people towards him), compulsive behavior, stereotypes, anhedonia, depression, flattened affect. Most often, psychosis occurs in the form of a rudimentary or acute paranoid with delusions of persecution, special significance, with visual or verbal hallucinations. Like amphetamine psychosis, it is similar to the psychosis of schizophrenic patients. The literature also describes manic-delusional psychoses. nine0010
A case of twilight stupefaction in a patient who abused methamphetamine for about 2 years is described. The condition lasted 8 days, while the patient experienced visual and auditory hallucinations, heard the voice of the planet Mars, and believed that in this way this planet tried to make contact with the Earth. Tachycardia up to 120 per minute, mydriasis and arterial hypertension were also observed.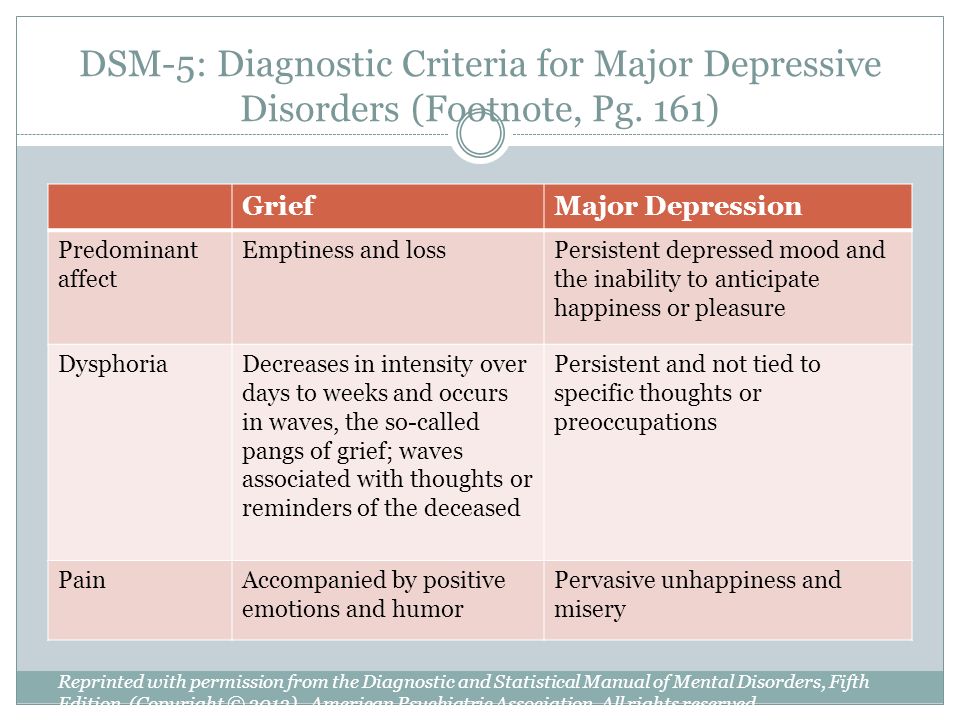
Methamphetamine psychosis usually occurs after many days of substance use, in doses of 6-11 ml intravenously per day. The duration of a psychotic disorder is usually from 8 to 10 hours, but sometimes up to 1 month. nine0010
Caffeine
It has been suggested that caffeine in high doses or chronic abuse may induce psychosis in healthy individuals or exacerbate pre-existing psychosis in schizophrenic patients.
Chronic use of caffeine, theobromine, theophylline in high doses can lead to exhaustion of the nervous system, which can become the basis for subsequent psychosis.
The most commonly reported delirium is caused by an overdose of caffeine. There is an influx of vivid visual hallucinations, sometimes auditory, a person loses orientation in the world around him. After removing caffeine from the body, the memory of the past is usually partially or completely preserved. Some patients lose the ability to judge distances correctly, and objects appear to them to be closer than they really are.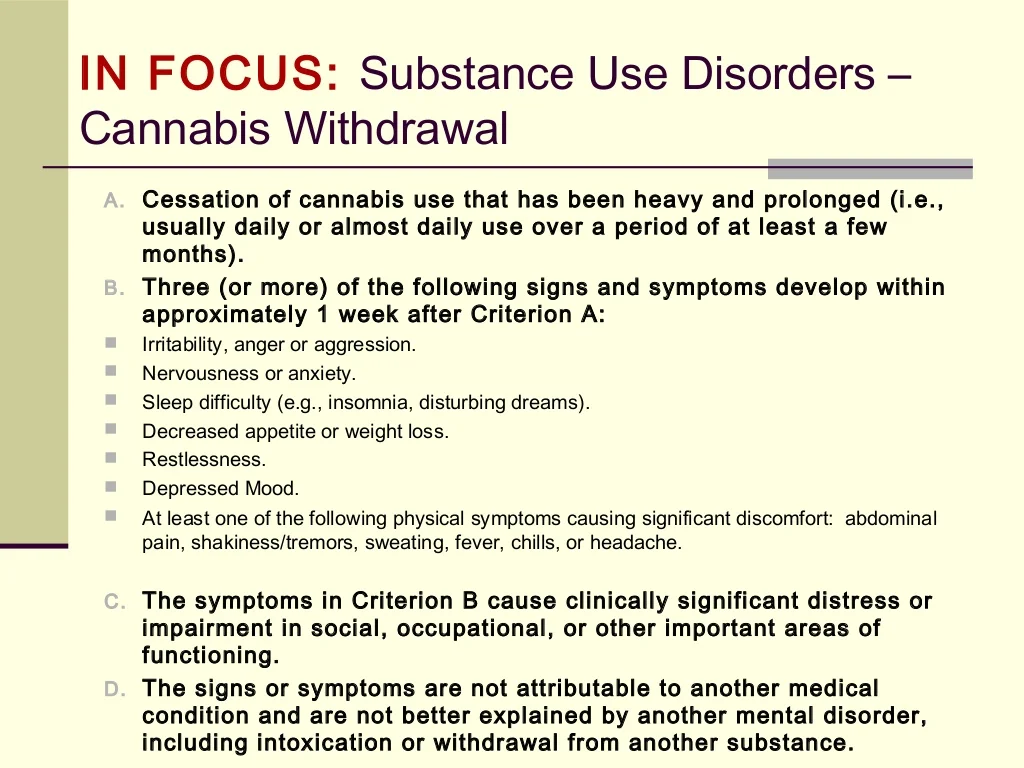 Somatic disorders associated with delirium: mydriasis, hyperemia, ataxia, tachycardia, intense thirst, dry skin and mucous membranes, cyanosis of the skin, sometimes increased blood pressure and fever. Neurological and somatic symptoms in this case are similar to those in atropine poisoning. nine0010
Somatic disorders associated with delirium: mydriasis, hyperemia, ataxia, tachycardia, intense thirst, dry skin and mucous membranes, cyanosis of the skin, sometimes increased blood pressure and fever. Neurological and somatic symptoms in this case are similar to those in atropine poisoning. nine0010
In more severe cases, there may be a deeper clouding of consciousness, accompanied by senseless motor excitement. In these cases, subsequent complete amnesia is frequent and the clinical picture is closer to twilight stupefaction.
There is a case when an elderly woman, who consumed 300 grams of coffee daily (about 30 g of pure caffeine) for two years, experienced a psychosis with disorientation in the surrounding space, episodic visual hallucinations, euphoria, agitation, which ended in death. nine0010
There are also cases of hallucinosis. Protracted psychoses with visual and auditory hallucinations with prolonged abuse of tea are described by V.P. Polyakov and Wark.
Affective psychosis in long-term caffeine abusers is quite rare, but a case has been described of a state resembling hypomania.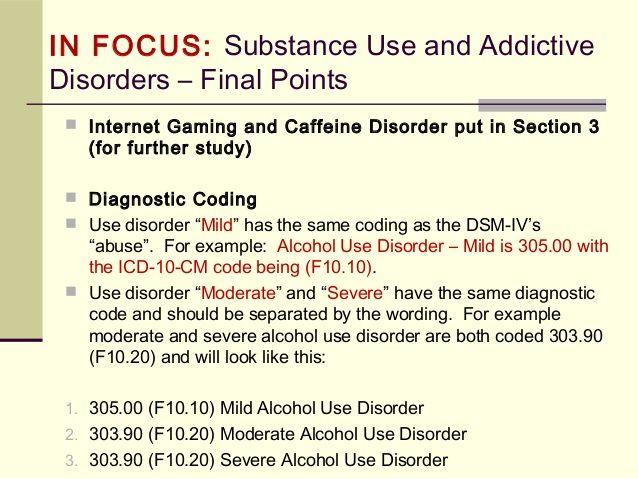
Caffeine poisoning psychoses with impaired consciousness usually do not last more than a few days.
Designation in ICD-10 and DSM-5
ICD-10
In the International Classification of Diseases, Revision 10 (ICD-10), psychotic disorders associated with the use of stimulants are indicated by the following codes:
- F14.50 Schizophrenia-like disorder due to cocaine use
- F14.51 Predominantly delusional disorder due to cocaine use
- F14.52 Predominantly hallucinatory disorder due to cocaine use
- F14.53 Predominantly polymorphic psychotic disorder due to cocaine use
- F14.54 Cocaine use disorder with predominantly depressive psychotic symptoms
- F14.55 Cocaine use disorder with predominantly manic psychotic symptoms
- F15.50 Schizophrenia-like disorder associated with the use of other stimulants (including caffeine)
- F15.51 Predominantly delusional disorder associated with the use of other stimulants (including caffeine)
- F15.
 52 Predominantly hallucinatory disorder associated with the use of other stimulants (including caffeine)
52 Predominantly hallucinatory disorder associated with the use of other stimulants (including caffeine) - F15.53 Predominantly polymorphic psychotic disorder associated with the use of other stimulants (including caffeine)
- F15.54 Other stimulant use disorder (including caffeine) with predominantly depressive psychotic symptoms
- F15.55 Other stimulant use disorder (including caffeine) with predominantly manic psychotic symptoms
ICD-11
In the ICD-11 exists as a separate category - "stimulant-induced psychotic disorder, including amphetamines, methamphetamine and methcathinone" (6C46.6) and "cocaine-induced psychotic disorder" (6C45.6). nine0010
DSM-5
DSM-5 has a diagnosis of substance/medication-induced psychotic disorder.
ICD-9-CM code for amphetamine (or other stimulants) and cocaine: 292.9.
Amphetamine (or other stimulants). ICD-10-KM codes:
- F15.159 Use disorder mild.
- F15.
 259 With a substance use disorder, moderate or severe.
259 With a substance use disorder, moderate or severe. - F15.959 No use disorder.
Cocaine. ICD-10-KM codes:
- F14.159 Use disorder mild.
- F14.259 With a substance use disorder, moderate or severe.
- F14.959 No use disorder.
Treatment
Treatment of overdose is to relieve symptoms during the acute phase of intoxication: maintaining normal body temperature, blood pressure and heart rate at an acceptable level until the substance is successfully metabolized and the vital functions of the body do not return to baseline. nine0010
Short-term use of typical and atypical antipsychotics (neuroleptics) is indicated in the early stages of psychosis treatment. In case of an overdose of psychostimulants, for example, haloperidol 5 mg 2 times a day can be prescribed. These drugs are effective in eliminating delirium and paranoid psychosis.
Patients with overdose, with observed arterial hypertension, it is preferable to prescribe chlorpromazine (chlorpromazine), since, in addition to dopamine receptors (D₁, D₂, D₃ and D₄), it blocks α-adrenergic receptors.