Sounds schizophrenics hear
Hearing Voices With Schizophrenia
Written by Shishira Sreenivas
Medically Reviewed by Jennifer Casarella, MD on May 13, 2022
In this Article
- What Treatments Can Help With Hearing Voices?
- What Are Some Self-Help Tips for Schizophrenia?
If you have schizophrenia and you hear voices, know that it’s not uncommon for people with the condition. Up to 80% of people diagnosed with schizophrenia have this symptom, too.
Doctors call them auditory hallucinations. It’s as if someone is speaking to you, but they’re not actually there. The voices feel very real and can be distracting and stressful. This can affect your overall quality of life. In severe cases, these voices may trigger thoughts of suicide or violence.
While the voices go away for some, for many, they never completely fade. But it’s possible to learn to manage them and take back some control in your day-to-day life.
What Treatments Can Help With Hearing Voices?
Prescription medications and talk therapy can help.
Medications. Antipsychotic medications are commonly prescribed for schizophrenia and can help in a number of ways. The drugs can:
- Lessen the urge to interact with voices or listen to them
- Help you ignore some of the criticism you may hear
- Make the voices less frightening
- Make the voices less intrusive or “in your face”
Drugs work differently for everyone. Tell your doctor if you don’t think your medication is helping. They may switch you to another one or change the dose. They might also try a combination of drugs.
It’s also important to give whatever medication you’re on a chance to do its job. If our doctor says it may take 2 weeks, 3 months, or whatever time frame to work, allow that much time to pass before deciding to try something else.
Cognitive behavioral therapy (CBT). This is when a mental health professional helps you work through what the voices mean, how they make you feel, and how they control what you think about yourself.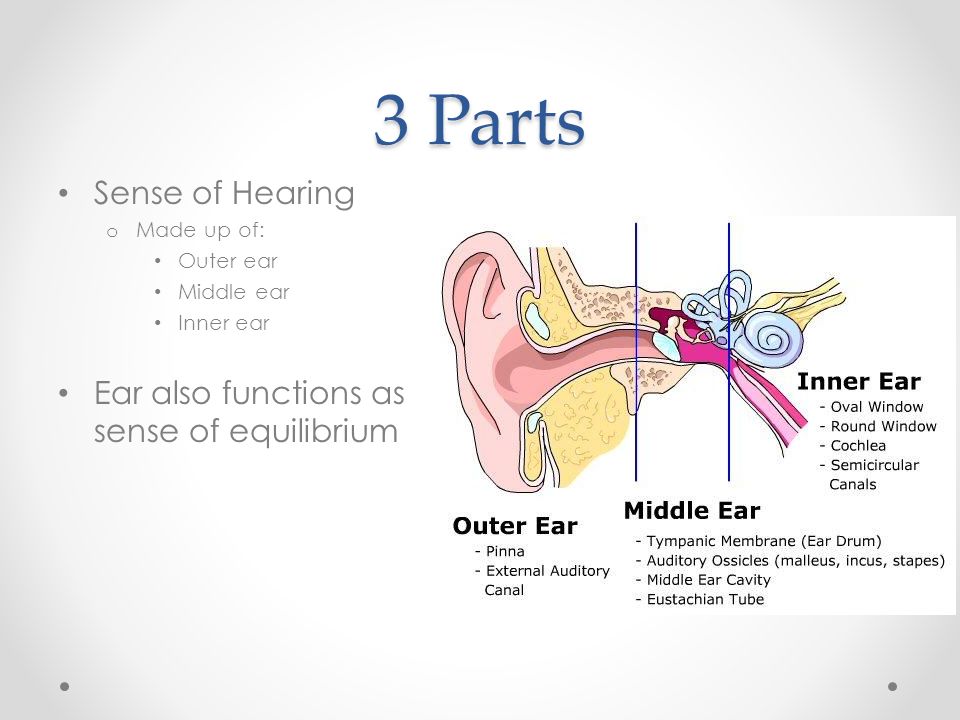
CBT can:
- Lessen anxiety about hearing voices
- Help you stand up to them
- Help you build control over the voices
If you can’t go in person, look into telehealth options. This way, you can get help from the comfort of your own home. If you’re not sure how to get started, ask your doctor about it.
Avatar therapy. This is a newer form of talk therapy where computer technology is used to make an avatar, or animated version, of the voices you hear. The avatar can be human or nonhuman. It can also be built to mimic the gender, tone, and accent of the voices you hear. The goal of avatar therapy is to use the computer-generated form of your voices to learn ways to resist them and gain more self-control. The therapist usually sits in another room and is there for support if you need it.
A few small-scale studies have shown that avatar therapy may help make the voices appear less often and ease overall stress. But more research is needed to learn about how effective it is and the long-term effects. This type of therapy may be right for you if you’re still hearing voices even with medication. It usually lasts 6 weeks, with 30-minute sessions once a week.
This type of therapy may be right for you if you’re still hearing voices even with medication. It usually lasts 6 weeks, with 30-minute sessions once a week.
Support groups. This can help you connect with others who also hear voices or live with similar schizophrenia-related issues. You can build community and find support, while also sharing what works for you to manage your day-to-day life with this condition. The National Alliance on Mental Illness (NAMI) is a good support resource.
Repetitive transcranial magnetic stimulation (RTMS). It’s a painless, noninvasive procedure in which an electromagnetic coil is placed on your scalp near your forehead. The coil sends magnetic pulses that stimulate nerve cells in this area. Experts are not entirely sure how it works, but they think it affects the regions of your brain that control mood and depression. Research suggests RTMS sessions can help make the voices appear less often and make them less intense.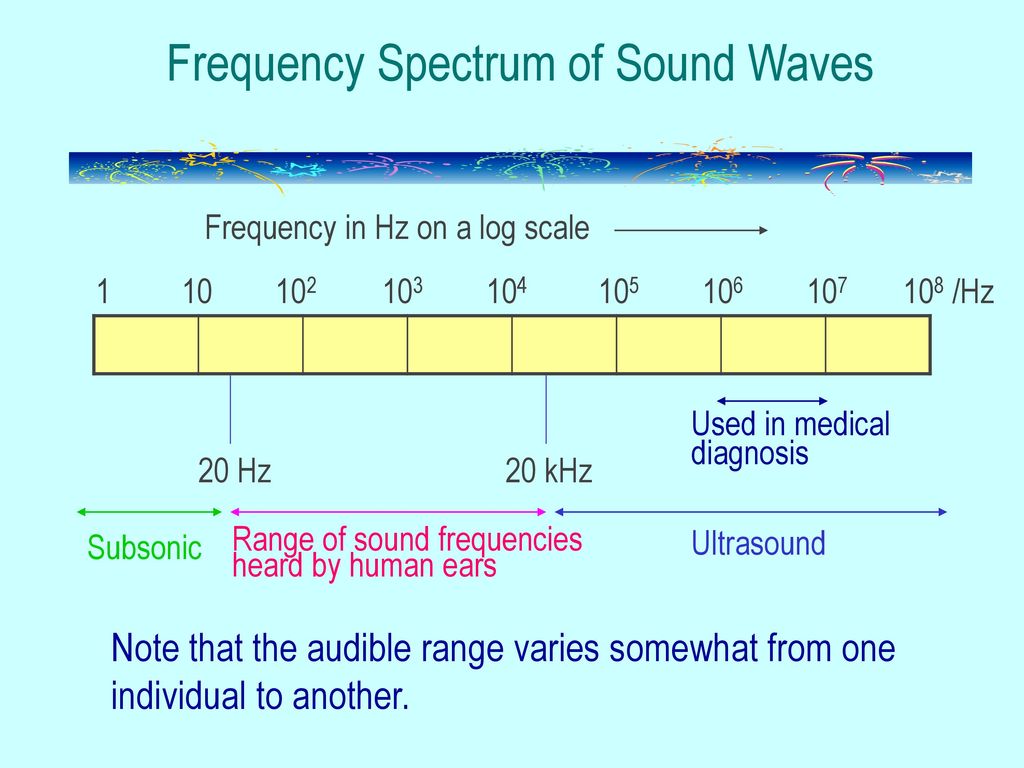 It may even keep voices at bay for up to 3 months after treatment. More research is needed.
It may even keep voices at bay for up to 3 months after treatment. More research is needed.
What Are Some Self-Help Tips for Schizophrenia?
Ways you can try to control the effects of voices include:
Find distractions. Staying busy or focusing on something else to keep your mind occupied may help. This might drown out the voices or distract you from them.
Options include:
- Puzzles or games
- Listening to music
- Reading a book
- Watching TV
- Writing
- Household chores
Try out a few different things to see what works best for you.
Vocalization. Talking out loud might help keep the voices from flooding your thoughts and causing trouble. Besides talking, you can hum tunes, sing, or read out loud.
Keep a diary. Write down each time you hear voices, how they make you feel, and what effect they have on your mental and physical health. Try to write down the date, time, and place. Make a note of what you were doing right before the voices started. This can help you:
Make a note of what you were doing right before the voices started. This can help you:
- Recognize a pattern if there is one
- Build self-awareness
- Find what triggers the voices
Sharing it with your doctor or therapist can also give them a better idea of the help you need.
Avoid drugs and alcohol. They can worsen symptoms and may trigger paranoia or visual hallucinations (when you see things that aren’t there). Drugs and alcohol can also affect how well your antipsychotic medication works.
Find ways to relax. Schizophrenia symptoms tend to get worse if you’re stressed. Try relaxation techniques like yoga, meditation, or mindful breathing to manage stress and lower anxiety.
Be assertive. If the voices are gaining control over your actions and thoughts, try to confidently speak back. For example, you can say out loud, “I’m too busy to talk right now” or “I can talk after 7 p.m.” This may help you gain some control and “negotiate” or set boundaries with the voices.
Practice selective listening. Voices can often range from positive to negative. Try to pay attention or engage only when the voices are positive. This may take time and practice. Talk to your doctor or therapist if you’re not sure how to do this.
Call 911 or head to the nearest hospital If the voices get too strong, mean, or dangerous.
The Propensity to Hear “Voices” in Schizophrenia May Be Established by Infancy, Many Years Before Symptom Onset | Mount Sinai
- Press Release
Findings reveal how auditory hallucinations may arise in patients with schizophrenia and provide potential new targets for early detection and treatment
Newsroom
- New York, NY
- (October 02, 2019)
Some people suffering from severe mental illness, particularly schizophrenia, hear “voices,” known as auditory hallucinations. This symptom, which afflicts more than 80% of patients, is among the most prevalent and distressing symptoms of schizophrenia. Patients “hear voices” speaking to them or about them without anyone actually being there. Auditory hallucinations, which usually begin in adolescence and young adulthood, “sound” very real to patients and can have a devastating impact on their quality of life because the “voices” are typically distressing and distracting, sometimes compelling the sufferer into suicidal or violent actions. Uncovering the biological origins of auditory hallucinations is essential for reducing their contribution to the disease burden of schizophrenia.
This symptom, which afflicts more than 80% of patients, is among the most prevalent and distressing symptoms of schizophrenia. Patients “hear voices” speaking to them or about them without anyone actually being there. Auditory hallucinations, which usually begin in adolescence and young adulthood, “sound” very real to patients and can have a devastating impact on their quality of life because the “voices” are typically distressing and distracting, sometimes compelling the sufferer into suicidal or violent actions. Uncovering the biological origins of auditory hallucinations is essential for reducing their contribution to the disease burden of schizophrenia.
To investigate the biological origins of hearing “voices” in patients with schizophrenia, a team led by researchers at the Icahn School of Medicine at Mount Sinai used ultra-high field imaging to compare the auditory cortex of schizophrenic patients with healthy individuals. They found that schizophrenic patients who experienced auditory hallucinations had abnormal tonotopic organization of the auditory cortex. Tonotopy is the ordered representation of sound frequency in the auditory cortex, which is established in utero and infancy and which does not rely on higher-order cognitive operations. The study findings, which appears this week in the Nature Partner Journal NJP Schizophrenia, suggest that the vulnerability to develop “voices” is probably established many years before symptoms begin.
Tonotopy is the ordered representation of sound frequency in the auditory cortex, which is established in utero and infancy and which does not rely on higher-order cognitive operations. The study findings, which appears this week in the Nature Partner Journal NJP Schizophrenia, suggest that the vulnerability to develop “voices” is probably established many years before symptoms begin.
“Since auditory hallucinations feel like real voices, we wanted to test whether patients with such experiences have abnormalities in the auditory cortex, which is the part of the brain that processes real sounds from the external environment,” says Sophia Frangou, MD, PhD, Professor of Psychiatry at the Icahn School of Medicine at Mount Sinai. “
Specifically, the research team used an ultra-high field scanner with a powerful 7 Tesla magnet to obtain high-resolution images of brain activity while study participants listened passively to tones across a range of very low to very high frequencies.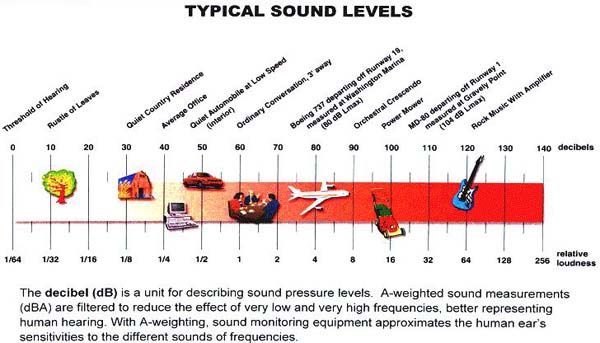 In healthy brains, these sounds are processed in a very organized fashion; each frequency activates a specific part of the auditory cortex forming a tonotopic map. The team obtained tonotopic maps from 16 patients with schizophrenia with a history of recurrent auditory hallucination and 22 healthy study participants. They found that patients showed greater activation in response to most sound frequencies. Additionally, the mapping of most sound frequencies to parts of the auditory cortex appeared “scrambled” in patients with schizophrenia, suggesting that the normal processes for the organized representation of sound in the brain are disrupted in schizophrenia.
In healthy brains, these sounds are processed in a very organized fashion; each frequency activates a specific part of the auditory cortex forming a tonotopic map. The team obtained tonotopic maps from 16 patients with schizophrenia with a history of recurrent auditory hallucination and 22 healthy study participants. They found that patients showed greater activation in response to most sound frequencies. Additionally, the mapping of most sound frequencies to parts of the auditory cortex appeared “scrambled” in patients with schizophrenia, suggesting that the normal processes for the organized representation of sound in the brain are disrupted in schizophrenia.
“Because the tonotopic map is established when people are still infants and remains stable throughout life, our study findings suggest that the vulnerability to develop “voices” is linked a deviance in the organization of the auditory system that occurs during infancy and precedes speech development and the onset of psychotic symptoms by many years. This is particularly exciting because it means that it might be possible to identify potential vulnerable individuals, such as the offspring of schizophrenia patients, very early on.”
This is particularly exciting because it means that it might be possible to identify potential vulnerable individuals, such as the offspring of schizophrenia patients, very early on.”
According to the authors, in addition to helping doctors spot people who are likely to experience hallucinations before the symptoms appear or become severe, the auditory cortex may be an area of consideration for novel neurmodulation methods to help patients who already have symptoms.
Looking ahead, Dr. Frangou’s research team will replicate and expand the current observations in larger samples to determine their relevance to hallucinations across diagnoses and to quantify the association of tonotopic disruption to auditory cortical activation and connectivity during actual hallucinatory experiences.
The study was supported by the National Institutes of Mental Health, the National Cancer Institute, The Netherlands Organisation for Health Research and Development, the Stanley Foundation and the Brain and Behavior Research Foundation.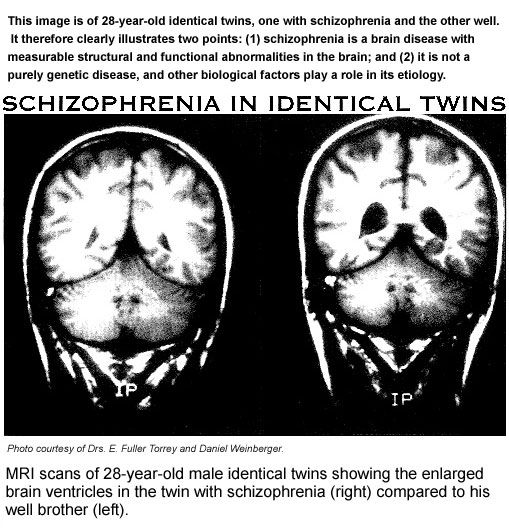
Tags: Icahn School of Medicine at Mount Sinai, Mount Sinai Health System, Psychiatry, Research, The Friedman Brain Institute, Sophia Frangou, MD, PhD
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.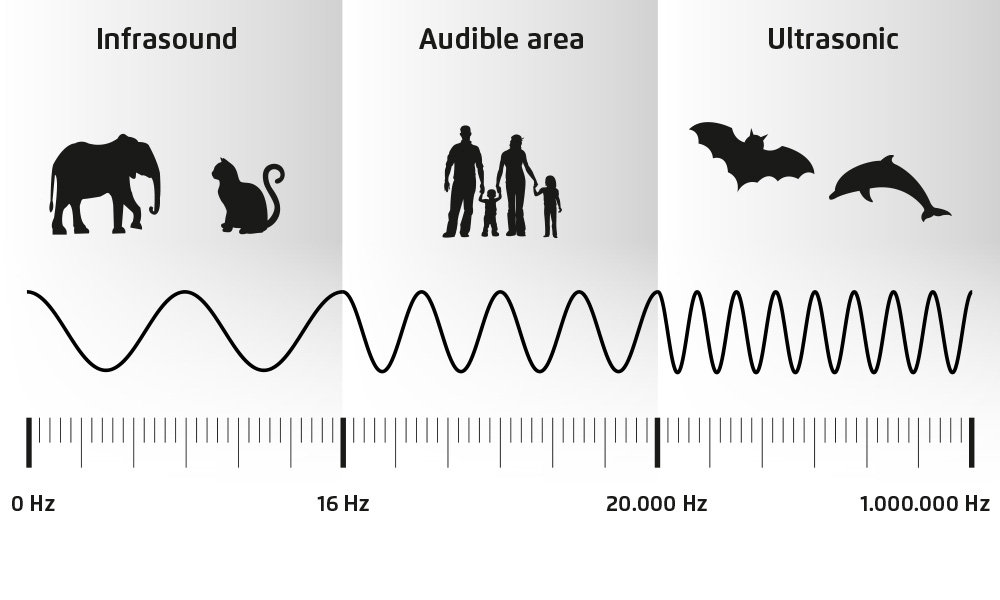 S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties. The Icahn School of Medicine at Mount Sinai is one of three medical schools that have earned distinction by multiple indicators: It is consistently ranked in the top 20 by U.S. News & World Report's "Best Medical Schools," aligned with a U.S. News & World Report "Honor Roll" Hospital, and top 20 in the nation for National Institutes of Health funding and top 5 in the nation for numerous basic and clinical research areas.
S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties. The Icahn School of Medicine at Mount Sinai is one of three medical schools that have earned distinction by multiple indicators: It is consistently ranked in the top 20 by U.S. News & World Report's "Best Medical Schools," aligned with a U.S. News & World Report "Honor Roll" Hospital, and top 20 in the nation for National Institutes of Health funding and top 5 in the nation for numerous basic and clinical research areas.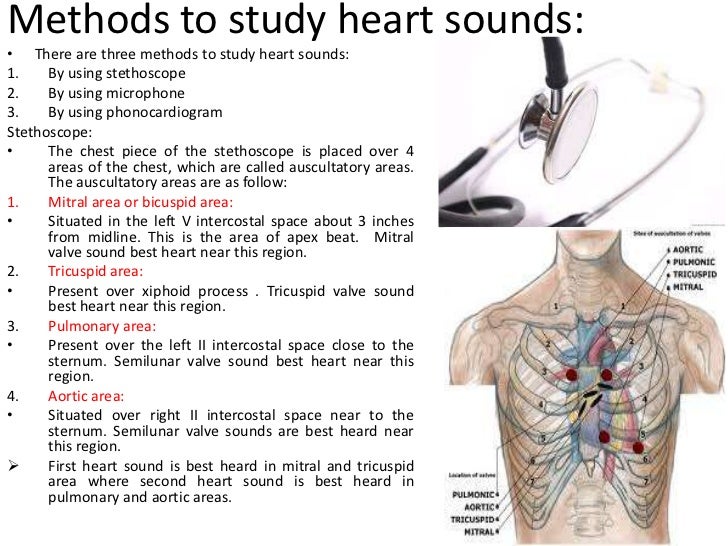 Newsweek’s “The World’s Best Smart Hospitals” ranks The Mount Sinai Hospital as No. 1 in New York and in the top five globally, and Mount Sinai Morningside in the top 20 globally.
Newsweek’s “The World’s Best Smart Hospitals” ranks The Mount Sinai Hospital as No. 1 in New York and in the top five globally, and Mount Sinai Morningside in the top 20 globally.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
Newsroom
In This Story
Show More
For Media Inquiries
View All Media Contacts
For Media Inquiries
View All Media Contacts
Scientists have found out how voices appear in the head of schizophrenics - RIA Novosti, 11/29/2016
Scientists have found out how voices arise in the head of schizophrenics
Scientists have discovered an unusual signaling RNA molecule in the human brain, the absence of which leads to the development of schizophrenia and the appearance of voices in the head. nine0003
2016-11-28T19:00
2016-11-28T19:00
2016-11-29T14:40
/html/head/meta[@name='og:title']/@content
2 /html/head/meta[@name='og:description']/@content
USA
RIA Novosti
1
5
4. 7
7
96
7 495 645-6601
FSUE MIA "Russia Today"
https: //xn---C1acbl2abdlkab1og.xn--p1ai/Awards/
2016
RIA Novosti
1
5
4.7 9000 9000 9000 9000
Internet-GROUP @rian.ru
7 495 645-6601
Rossiya Segodnya
https://xn--c1acbl2abdlkab1og.xn--p1ai/awards/
/ria.ru/docs/about/copyright.html
https://xn--c1acbl2abdlkab1og.xn--p1ai/
RIA Novosti
1,000 .xn-p1ai/awards/
1920
1080
True
1920
1440
True
https://cdnn21.img.ria.ru/images/148187/80/148187878042_ 5304:3744_1920x0_80_0_0_47b680fa7228ce7335f8fb3da43a0db6.jpg
1920
1920
True
RIA Novosti
1
5
4.7
9000
7 495 645-6601 9000
Federal State Unitary Enterprise MIA “Russia Today”
https: //xn---c1acbl2abdlkab1og.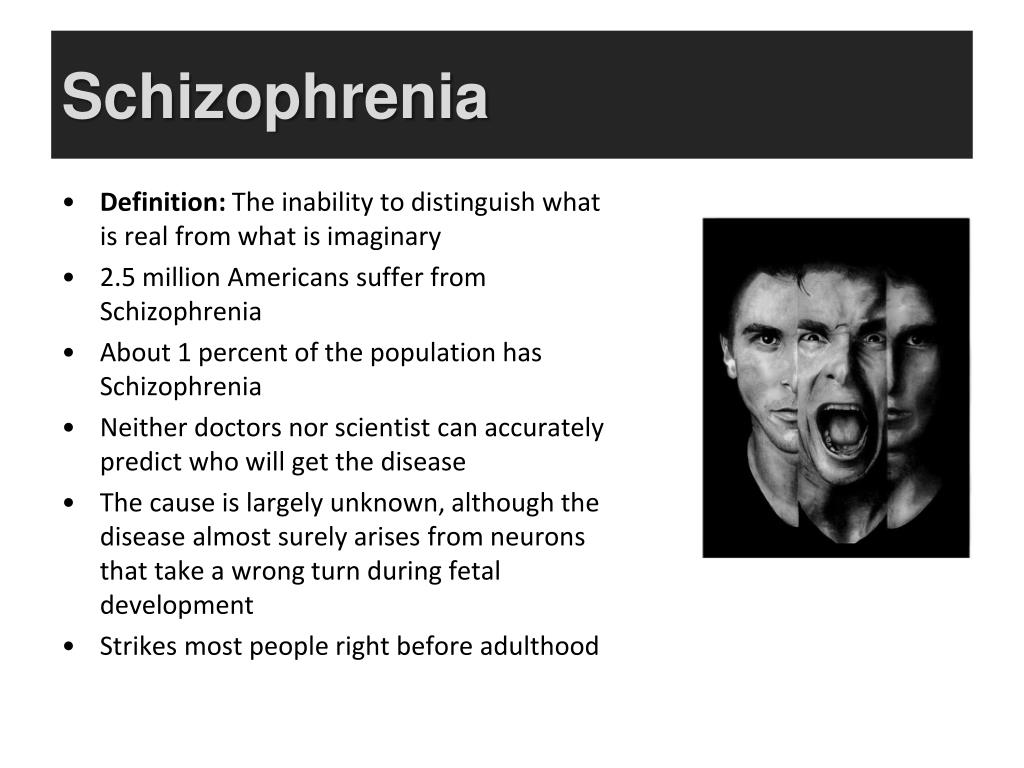 xn--p1ai/Awards/
xn--p1ai/Awards/
RIA Novosti
1
5
4.7
96 9000
7 495 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 646 646 495 64 64 64 646 646 495 64 64 64 64 64 64 64 64 64 64 64 64 64 646 646 495 64 646 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64 64AP
Federal State Unitary Enterprise MIA "Russia Today"
https://xn--c1acbl2abdlkab1og.xn--p1ai/awards/
discoveries - RIA Science, USA, schizophrenia, genetics
Discoveries - RIA Science, Science, USA, schizophrenia, genetics
MOSCOW, 2 November - RIA Novosti . Scientists have discovered an unusual signaling RNA molecule in the human brain, the absence of which leads to the development of schizophrenia and the appearance of "voices in the head," according to an article published in the journal Nature Medicine.
"Two years ago, we discovered a specific chain of neurons in the brain that is affected by well-known antipsychotic drugs. All of them, however, cause severe side effects. We isolated a micro-RNA molecule, which is a key element in the operation of this chain of cells, and showed that the destruction of these micro-RNAs leads to the development of the disorders that are observed in schizophrenics," said Stanislav Zakharenko from the St. Jude Children's Hospital in Memphis (USA). nine0003
All of them, however, cause severe side effects. We isolated a micro-RNA molecule, which is a key element in the operation of this chain of cells, and showed that the destruction of these micro-RNAs leads to the development of the disorders that are observed in schizophrenics," said Stanislav Zakharenko from the St. Jude Children's Hospital in Memphis (USA). nine0003
Today, about 24 million people worldwide suffer from schizophrenia. According to WHO statistics, every seven people out of a thousand are schizophrenics, and most of them begin to suffer from such problems between the ages of 15 and 35.
There is still no consensus among scientists on how such disorders arise and how they should be properly treated. In recent years, geneticists have found several dozen genes relatively loosely associated with schizophrenia, but they have not been able to understand how mutations in these DNA regions cause schizophrenia and its associated effects - hallucinations or "voices in the head". nine0003
nine0003
June 3, 2015, 07:35 PM
Scientists have discovered the main genetic cause of schizophrenia Comparison of the DNA of tens of thousands of schizophrenics has shown that this psychiatric disorder occurs due to malfunctions of inhibitory neurons in the brain, their incorrect interaction with excitatory nerve cells and associated with these things mutations in the genes.
Zakharenko and his colleagues found that the latter effect could be caused by defects in the assembly of a small RNA molecule known as miR-338-3p. This small sequence of genetic code, as scientists explain, controls the assembly and operation of Drd2 receptors on the surface of nerve cells that read dopamine, one of the main information carriers in the brain and the hormone of pleasure. nine0003
People with a mutation in the gene that assembles this receptor, or micro-RNA, very often suffer from behavioral problems in childhood, and approximately 40% of them become victims of schizophrenia. All this prompted Zakharenko and his colleagues to check how both of these elements of the genome affect the brain by removing or blocking similar regions in the DNA of mice.
All this prompted Zakharenko and his colleagues to check how both of these elements of the genome affect the brain by removing or blocking similar regions in the DNA of mice.
Experiments have shown that disabling miR-338-3p leads to a sharp increase in the number of Drd2 receptors in neurons located in the center of hearing in the cerebral cortex of mice, which increases their sensitivity to dopamine molecules. As a result, their connection with the thalamus, the center for processing and distributing information, was disrupted, and the cortex began to work, as it were, on its own. nine0003
August 1, 2016, 12:27
Scientists have discovered what gave rise to the "voices in the head" of Joan of Arc form of epilepsy.
This, according to scientists, can generate voices in the head, since information about perceived sounds usually undergoes primary processing in the thalamus and is probably cleared of noise and random signals.
As the experiment of Zakharenko and his colleagues showed, if the work of miR-338-3p is restored, then this cleaning is resumed, which had a positive effect on the behavior of mice, which, when new sources of sounds appeared, behaved extremely inadequately compared to normal individuals.
Accordingly, miR-338-3p molecules, or mechanisms that stimulate their production, can be used to treat schizophrenia relatively safely, or at least relieve its symptoms. In addition, a decrease in miR-338-3p concentrations in old age may explain why older people are more likely to suffer from schizophrenia and other brain problems than younger people, the authors of the article conclude. nine0184 B
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find a country »
- A
- B
- C
- Г
- Д
- Е
- Ё
- Ж
- З
- И
- Й
- К
- Л
- М
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- Э
- Ю
- Я
- WHO in countries » nine0183
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0185
- Developments
- Photo reports
- Questions and answers
- Latest information
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0185
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/
- Newsletters/
- Read more/ nine0184 Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations. nine0152
- Globally, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others; nine0185
- disorganized thinking, often expressed in incoherent or pointless speech;
- significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, flatness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms. nine0003
Magnitude of the problem and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease. nine0003
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
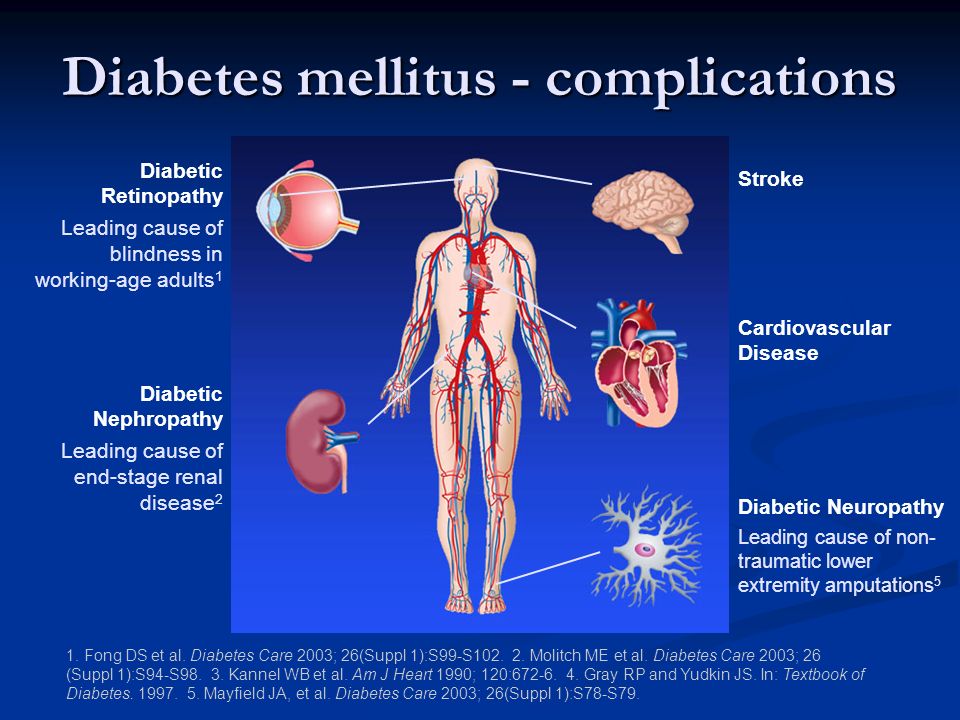
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment. nine0003
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, cause isolation and disrupt health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0003
People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0003
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.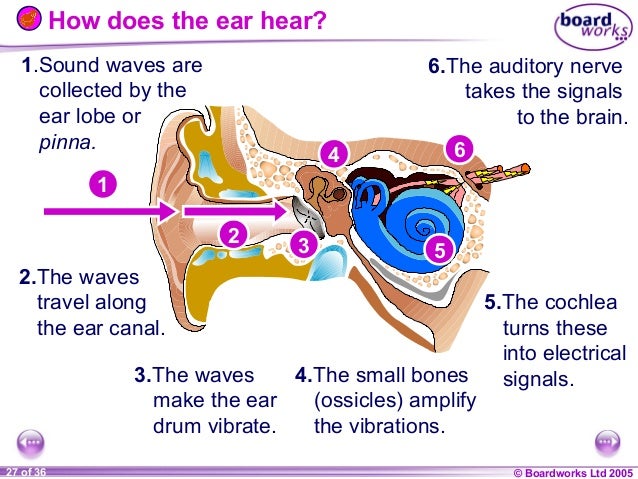
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities. nine0003
nine0003
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0003
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.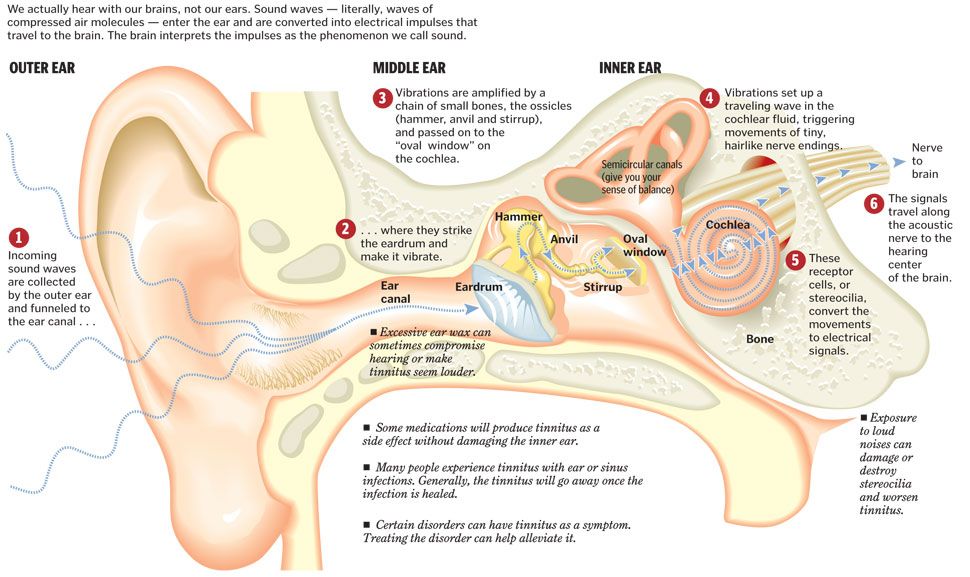 nine0003
nine0003
The WHO Mental Health Gap Action Program (mhGAP) is developing evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0003
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services.