Post ect complications
Electroconvulsive therapy (ECT) - Mayo Clinic
Overview
Electroconvulsive therapy (ECT) is a procedure, done under general anesthesia, in which small electric currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry that can quickly reverse symptoms of certain mental health conditions.
ECT often works when other treatments are unsuccessful and when the full course of treatment is completed, but it may not work for everyone.
Much of the stigma attached to ECT is based on early treatments in which high doses of electricity were administered without anesthesia, leading to memory loss, fractured bones and other serious side effects.
ECT is much safer today. Although ECT may still cause some side effects, it now uses electric currents given in a controlled setting to achieve the most benefit with the fewest possible risks.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Electroconvulsive therapy (ECT) can provide rapid, significant improvements in severe symptoms of several mental health conditions. ECT is used to treat:
- Severe depression, particularly when accompanied by detachment from reality (psychosis), a desire to commit suicide or refusal to eat.
- Treatment-resistant depression, a severe depression that doesn't improve with medications or other treatments.
- Severe mania, a state of intense euphoria, agitation or hyperactivity that occurs as part of bipolar disorder. Other signs of mania include impaired decision-making, impulsive or risky behavior, substance abuse, and psychosis.
- Catatonia, characterized by lack of movement, fast or strange movements, lack of speech, and other symptoms. It's associated with schizophrenia and certain other psychiatric disorders. In some cases, catatonia is caused by a medical illness.
- Agitation and aggression in people with dementia, which can be difficult to treat and negatively affect quality of life.
ECT may be a good treatment option when medications aren't tolerated or other forms of therapy haven't worked. In some cases ECT is used:
- During pregnancy, when medications can't be taken because they might harm the developing fetus
- In older adults who can't tolerate drug side effects
- In people who prefer ECT treatments over taking medications
- When ECT has been successful in the past
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Risks
Although ECT is generally safe, risks and side effects may include:
- Confusion. Immediately after treatment, you may experience confusion, which can last from a few minutes to several hours. You may not know where you are or why you're there. Rarely, confusion may last several days or longer. Confusion is generally more noticeable in older adults.
- Memory loss. Some people have trouble remembering events that occurred right before treatment or in the weeks or months before treatment or, rarely, from previous years. This condition is called retrograde amnesia. You may also have trouble recalling events that occurred during the weeks of your treatment. For most people, these memory problems usually improve within a couple of months after treatment ends.
- Physical side effects. On the days of an ECT treatment, some people experience nausea, headache, jaw pain or muscle ache. These generally can be treated with medications.
- Medical complications. As with any type of medical procedure, especially one that involves anesthesia, there are risks of medical complications. During ECT, heart rate and blood pressure increase, and in rare cases, that can lead to serious heart problems. If you have heart problems, ECT may be more risky.
How you prepare
Before having your first ECT treatment, you'll need a full evaluation, which usually includes:
- Medical history
- Complete physical exam
- Psychiatric assessment
- Basic blood tests
- Electrocardiogram (ECG) to check your heart health
- Discussion of the risks of anesthesia
These exams help make sure that ECT is safe for you.
What you can expect
The ECT procedure takes about five to 10 minutes, with added time for preparation and recovery. ECT can be done while you're hospitalized or as an outpatient procedure.
Before the procedure
To get ready for the ECT procedure:
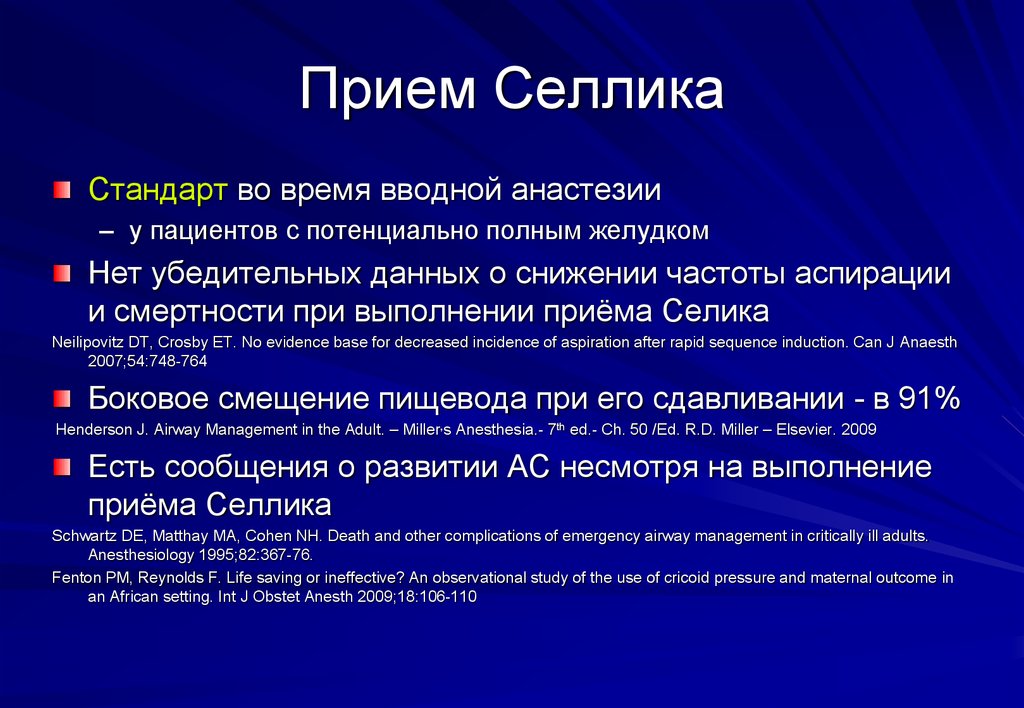
- You'll have general anesthesia. So you can expect dietary restrictions before the procedure. Typically, this means no food or water after midnight and only a sip of water to take any morning medications. Your health care team will give you specific instructions before your procedure.
- You may have a brief physical exam.This is basically to check your heart and lungs.
- You'll have an intravenous (IV) line inserted. Your nurse or other team member inserts an IV tube into your arm or hand through which medications or fluids can be given.
- You'll have electrode pads placed on your head. Each pad is about the size of a silver dollar.
 ECT can be unilateral, in which electric currents focus on only one side of the brain, or bilateral, in which both sides of the brain receive focused electric currents.
ECT can be unilateral, in which electric currents focus on only one side of the brain, or bilateral, in which both sides of the brain receive focused electric currents.
Anesthesia and medications
At the start of the procedure, you'll receive these medications through your IV:
- An anesthetic to make you unconscious and unaware of the procedure
- A muscle relaxant to help minimize the seizure and prevent injury
You may receive other medications, depending on any health conditions you have or your previous reactions to ECT.
Equipment
During the procedure:
- A blood pressure cuff placed around one ankle stops the muscle relaxant medication from entering your foot and affecting the muscles there. When the procedure begins, your doctor can monitor seizure activity by watching for movement in that foot.
- Monitors check your brain, heart, blood pressure and oxygen use.
- You may be given oxygen through an oxygen mask.
- You may also be given a mouth guard to help protect your teeth and tongue from injury.
Inducing a brief seizure
When you're asleep from the anesthetic and your muscles are relaxed, the doctor presses a button on the ECT machine. This causes a small amount of electric current to pass through the electrodes to your brain, producing a seizure that usually lasts less than 60 seconds.
- Because of the anesthetic and muscle relaxant, you remain relaxed and unaware of the seizure. The only outward indication that you're having a seizure may be a rhythmic movement of your foot if there's a blood pressure cuff around your ankle.
- Internally, activity in your brain increases dramatically. A test called an electroencephalogram (EEG) records the electrical activity in your brain. Sudden, increased activity on the EEG signals the beginning of a seizure, followed by a leveling off that shows the seizure is over.
A few minutes later, the effects of the short-acting anesthetic and muscle relaxant begin to wear off. You're taken to a recovery area, where you're monitored for any potential problems. When you wake up, you may experience a period of confusion lasting from a few minutes to a few hours or more.
You're taken to a recovery area, where you're monitored for any potential problems. When you wake up, you may experience a period of confusion lasting from a few minutes to a few hours or more.
Series of treatments
In the United States, ECT treatments are generally given two to three times weekly for three to four weeks — for a total of six to 12 treatments. Some doctors use a newer technique called right unilateral ultrabrief pulse electroconvulsive therapy that's done daily on weekdays.
The number and type of treatments you'll need depend on the severity of your symptoms and how rapidly they improve.
You can generally return to normal activities a few hours after the procedure. However, some people may be advised not to return to work, make important decisions, or drive until one to two weeks after the last ECT in a series, or for at least 24 hours after a single treatment during maintenance therapy. Resuming activities depends on when memory loss and confusion are resolved.
Results
Many people begin to notice an improvement in their symptoms after about six treatments with electroconvulsive therapy. Full improvement may take longer, though ECT may not work for everyone. Response to antidepressant medications, in comparison, can take several weeks or more.
No one knows for certain how ECT helps treat severe depression and other mental illnesses. What is known, though, is that many chemical aspects of brain function are changed during and after seizure activity. These chemical changes may build upon one another, somehow reducing symptoms of severe depression or other mental illnesses. That's why ECT is most effective in people who receive a full course of multiple treatments.
Even after your symptoms improve, you'll still need ongoing depression treatment to prevent a recurrence. Ongoing treatment may be ECT with less frequency, but more often, it includes antidepressants or other medications, or psychological counseling (psychotherapy).
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
By Mayo Clinic Staff
Related
Products & Services
Electroconvulsive Treatment (ECT) - Side effects of having ECT
ECT can have side effects. Most people we spoke to had some side effects from the treatment. Side effects ranged from the pleasant "being woozy is actually really nice” right through to the extremely unpleasant e.g. complete disorientation or deeply upsetting such as the loss of treasured memories. Some only lasted in the short-term, like headaches and tiredness, others were long-term e.g. memory being ‘foggy’. Memory loss is the side effect that caused the most concern to people.
Apart from the side effects of having ECT, there were also suspected side effects from having the general anaesthetic and sometimes it was difficult to tell the difference. For example Dafydd said it was hard to tell how much of his wife’s tiredness was due to the effects of the general anaesthetic and how much was due to the ECT.
For example Dafydd said it was hard to tell how much of his wife’s tiredness was due to the effects of the general anaesthetic and how much was due to the ECT.
However, a few of the people we interviewed experienced little if any side effects of having ECT, and some pointed out the side effects of taking medication could be worse. John Z, said that he experienced no bad effects from ECT at all, and it was like having a cataract operation.
Immediate side-effects after having ECT treatment
The people we spoke to reported the following side effects immediately after the ECT treatment, which lasted only a short while (hours or sometimes a few days):
• fear, anxiety and confusion
• feeling strange afterwards, e.g. light headed, dissociated, numbing, “mixing up the emotions”
• headaches (which could be severe and “indescribable”)
• jaw ache
• memory loss surrounding their treatment time
• disorientation
• problems thinking e. g. “they fried my brain”
g. “they fried my brain”
• fatigue
• “wooziness”, “groggy”, dizziness
• nausea
• drooling
• looking like you’d “had a stroke”
• muscle stiffness
• feeling shaky
• inability to eat
• intense sleepiness
• hallucinations
Headache and jaw ache sometimes only happened following the first ECT sessions, and people felt their bodies adjusted better to treatment as they went along. For others, this was something they always experienced after having ECT. Kathleen said the dosage of her ECT made an impact on the severity of the side effects. When she first had ECT, the headache and jaw ache was so bad she couldn’t eat, but when the dose was reduced for the following treatments, the effects were not so bad.
Some people we spoke to said looking like someone who had ‘had a stroke’ and drooling was a very upsetting side effect both for the person having the treatment and for those who saw them. Annie and Lorraine said that seeing their mother after her first treatment was scary.
Annie and Lorraine said that seeing their mother after her first treatment was scary.
Yvonne remembers having terrible headaches, and felt that other patients seeing her drooling as she was wheeled through the ward after ECT could be scary for them.
Yvonne remembers having terrible headaches, and felt that other patients seeing her drooling as she was wheeled through the ward after ECT could be scary for them.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
They kept assuring me that I would feel better but I wasn’t convinced. And I remember going through treatment being absolutely petrified and, I remember being put to bed after treatment and I remember having a really, really bad headache.What happened at [name of hospital] was that after your treatment you were wheeled back through a ward in front of everybody, after your treatment, but you would come in and you’d may be, be drooling, or you’d be I suppose you kind of looked as if somebody who had had a stroke or something and the knock on effect was that it really affected the other patients.
 So much so that one of the boys that I’d met there, he was actually a soldier who had been in the first Gulf, that he totally flipped out and thought that they’d harmed me somehow.
So much so that one of the boys that I’d met there, he was actually a soldier who had been in the first Gulf, that he totally flipped out and thought that they’d harmed me somehow. The headaches were like something that I’ve experienced, sort of before or since. It’s completely indescribable. The headaches that I had afterwards. I do think that ECT is given that there should be a way of getting the patient back into bed without have to trail them through in front of everybody. Because everybody is in hospital because they’re ill and it becomes really frightening for them, and it may be that one of these patients that are witnessing somebody coming back are going to need that treatment which is going to make it even scarier for them.
People often found they were very sleepy immediately after their treatment and wanted to go to bed. Carys said that her daughter would sleep for up to twelve to fourteen hours afterwards.
Most people remembered having the treatment, sometimes in great detail and some were able to resume their normal activities immediately afterwards. But others did not remember having the treatment at all, or remember other things going on at the time of the treatment. Some were very disoriented and couldn’t find their room afterwards, or were unable to remember how they got home. Helen, who had her treatment in 1970 said she struggled to remember her own name after the treatment, her mind was “just black, like you’re in a different universe”.
But others did not remember having the treatment at all, or remember other things going on at the time of the treatment. Some were very disoriented and couldn’t find their room afterwards, or were unable to remember how they got home. Helen, who had her treatment in 1970 said she struggled to remember her own name after the treatment, her mind was “just black, like you’re in a different universe”.
Alka’s husband was often disoriented after his ECT treatments. He would not remember having had the treatment or being given something to eat and drink afterwards.
Alka’s husband was often disoriented after his ECT treatments. He would not remember having had the treatment or being given something to eat and drink afterwards.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
[Husband’s name] was always terribly disorientated after he’d had his treatment to the extent that he didn’t even know that he’d received his treatment. He would be taken into another room where he was given something to eat and drink by the nurses after, after I’d taken him home he would have no recollection at all of having eaten or drunk something. He would always come home and have a sleep for at least two or three hours. And that’s where as I mentioned earlier his short term memory is completely shot to pieces because if you were to ask him what happened in his life during those ECT treatments he would have no recollection of those. But some of his memory would come back if I reminded him of what had happened.
He would be taken into another room where he was given something to eat and drink by the nurses after, after I’d taken him home he would have no recollection at all of having eaten or drunk something. He would always come home and have a sleep for at least two or three hours. And that’s where as I mentioned earlier his short term memory is completely shot to pieces because if you were to ask him what happened in his life during those ECT treatments he would have no recollection of those. But some of his memory would come back if I reminded him of what had happened.
When Kathleen had maintenance ECT as an outpatient she felt highly disoriented and had no recollection of leaving the hospital alone or of the two days following the treatment.
Text only
Read below
When Kathleen had maintenance ECT as an outpatient she felt highly disoriented and had no recollection of leaving the hospital alone or of the two days following the treatment.
View full profile
HIDE TEXT
PRINT TRANSCRIPT
Well yes, I was discharged. I went home and about a week afterwards I went for an outpatient maintenance ECT treatment at my local hospital. And that is the worst ECT I have ever had and I didn’t have any more, maintenance ECT I refused to have any more after that. Maintenance ones anyway. I think they totally fried my brain, because I can remember going there. The preparation and everything. It was a Friday. And the next thing I remember is Monday. I have absolutely no memory for the rest of Friday, Saturday, Sunday.And yet apparently I walked home. I had someone fixed up to give me a ride home. But they couldn’t get hold of them and I asked if I could walk home apparently and they let me walk home which I think was a big mistake [laughs]. Because I was not at all with it. And I walked home, and my daughter when she saw what I was like. I must have been disorientated or something and she called various people. My psychiatrist and GP and whatnot and they admitted me, you know, to recover from this one ECT and the next thing I remember is on Monday. I don’t remember anything for about three days really. So that put me off a bit [laughs].
I don’t remember anything for about three days really. So that put me off a bit [laughs].
Suzanne felt that memory loss was a price she paid for getting well again. Like others, she judged that it was worth it in the end. She also said there were other periods of her life she couldn’t remember and didn’t find this particularly unusual or upsetting.
Jane managed to compete in a school sports day event in the afternoon after having had ECT in the morning. But she says she felt dissociated from reality.
Jane managed to compete in a school sports day event in the afternoon after having had ECT in the morning. But she says she felt dissociated from reality.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
During the time that I was having it, a friend of mine would come down to the hospital and we’d go running together and I certainly on some days ran with her after having ECT [laughs] and I certainly went at the school, because I’m quite, what’s the word? Competitive. And they had the school sports then. They had the mums race and I did quite well a couple of years before, so I ran in the Mum’s race having had ECT and almost won but I kind of tried to lunge myself over the finishing line so that I could beat the person next to me and fell over unsurprisingly, as I’d had ECT earlier in the day [laughs]. So I didn’t win. But it was incredible what I could manage to do afterwards. Because I think I was so dissociated from what was going on that I just kind of did whatever I liked.
And they had the school sports then. They had the mums race and I did quite well a couple of years before, so I ran in the Mum’s race having had ECT and almost won but I kind of tried to lunge myself over the finishing line so that I could beat the person next to me and fell over unsurprisingly, as I’d had ECT earlier in the day [laughs]. So I didn’t win. But it was incredible what I could manage to do afterwards. Because I think I was so dissociated from what was going on that I just kind of did whatever I liked. Memory Loss
Most of the people we spoke to did experience memory loss following ECT. This seemed to be the case whether or not the ECT had had any effect on their mental illness. Frequently, the memory loss was judged to be relatively minor, such as forgetting people’s names, or not being able to find their way back to their room, or around their local town, and forgetting their passwords and bank pin number, or how to spell. These did come back to them in time, or once they were reminded. David Z found that although his ability to recall sometimes is “a bit fuzzy” he’s learnt to deal with it and if someone reminds him it comes back “and stays back”.
David Z found that although his ability to recall sometimes is “a bit fuzzy” he’s learnt to deal with it and if someone reminds him it comes back “and stays back”.
People did worry about the long-term effects of ECT on the brain, e.g. problems thinking, and said that their doctors were likely to deny that long term effects were possible.
Sunil mentioned his own psychiatrist had found research suggesting that severe depression that is not treated was more likely to cause dementia than having ECT.
Sunil mentioned his own psychiatrist had found research suggesting that severe depression that is not treated was more likely to cause dementia than having ECT.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
But really to be very honest with you, apart from the effect on short term memory I think ECT is a treatment which is very, very effective and has very little in the way of side effects. I mean I did worry about whether there’s any long lasting effects of ECT like maybe brain damage or dementia or something like that, but my consultant psychiatrist has strongly reassured me that there is absolutely no evidence whatsoever that ECT makes you more likely to develop either Alzheimers disease or dementia, and in actual fact, she’s told me that’s there’s actual medical evidence, and published evidence, that untreated episodes of severe depression are much more associated with dementia than treatment with ECT. So if you don’t get adequately treated and you have long periods of recurrent depression which is severe, you’re much more likely to develop dementia.
I mean I did worry about whether there’s any long lasting effects of ECT like maybe brain damage or dementia or something like that, but my consultant psychiatrist has strongly reassured me that there is absolutely no evidence whatsoever that ECT makes you more likely to develop either Alzheimers disease or dementia, and in actual fact, she’s told me that’s there’s actual medical evidence, and published evidence, that untreated episodes of severe depression are much more associated with dementia than treatment with ECT. So if you don’t get adequately treated and you have long periods of recurrent depression which is severe, you’re much more likely to develop dementia. However some people, especially those who had ECT over ten years ago, did find they had lost memories of important events such as a daughter’s dedication, a surprise birthday party, a holiday, or the birth of a child. Not being able to remember events in their lives could be frustrating and distressing. Although a few suspected they might have lost unpleasant memories “I want to forget” and asked themselves if that might have been part of their recovery.
Although a few suspected they might have lost unpleasant memories “I want to forget” and asked themselves if that might have been part of their recovery.
Cathy has found long-term memory loss frustrating and sad. Big chunks of her life are missing, and she can’t remember the time when her son was born.
Cathy has found long-term memory loss frustrating and sad. Big chunks of her life are missing, and she can’t remember the time when her son was born.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
And how, how were you sort of feeling for the rest of the day then?A bit sort of zonked out. And it, like I said earlier, it definitely does affect your short-term memory. You know, I’d struggle to remember what had happened, you know, that day or the day before. So that’s a bit scary.
So that’s a bit scary.
Was it just sort of events that you struggled to remember or was it sort of names for things?
No, not names for things. I could remember that sort of thing. But it, more events, things that had happened in the last few days.
And what was the emotional effect of that?
Of, of having memory loss?
[mhm]
I don’t really remember, to be honest. I think I’ve felt more emotions about the long-term memory, memory problems that I’ve had, which I attribute to ECT, although doctors will tell you that’s not possible. Because, you know, big chunks of my life are now missing, some of which were probably important or worth remembering [laugh]. So I feel quite sad about that, you know, round when my son was born and, you know, there’s big bits of it I don’t remember, you know. He was young and I don’t remember some of his milestones.
It’s quite an odd question to ask in a, a way. Sort of what, how do you know that you can’t remember as the whole…?
Sort of what, how do you know that you can’t remember as the whole…?
Well, because people tell me things, people will talk about things and I’ll say, “Well, I don’t remember that.” You know, not disputing that it happened but just not remembering that it, either not remembering it at all or, well, yes, not remembering it at all as...
And were these sort of whole months at a time or just small events?
It would be weeks, weeks that I wouldn’t remember or, you know, certain events that happened. And I, and people would say, “Oh, you remember so-and so?” and I would say, and I don’t think it’s just because I’m getting older, because this was happening when I was in my 30s, you know, 30s, late 30s and, you know, dementia hadn’t set in then [laugh]. But, yes, so that does bring some sadness, to be honest, and a bit of frustration because, you know, you don’t like to forget things.
When Beattie had ECT over thirty years ago, she lost 7 years of her memory, which included the birth of one of her children.
When Beattie had ECT over thirty years ago, she lost 7 years of her memory, which included the birth of one of her children.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
And when I, in 1970 they gave me ECT when I was depressed. I had psychotic symptoms. And it actually took away seven years of my memory which never came back. And I don’t remember my son being born, I don’t remember the 1960s and that was in 1970.And I feel like an incomplete person because of it.
What impact has it had in your life, you were saying the memory loss?
Well it bothers me you know, because there’s no one alive now that I could ask about it really. My parents I can’t ask them they’ve gone. And it’s rotten to not remember the sixties and my son’s birth and everything else.
Tracy struggled to remember some of her daughter’s Dedication and feels frustrated. ECT didn’t work for her and she thinks it is barbaric and it was taking time out that actually helped her.
Tracy struggled to remember some of her daughter’s Dedication and feels frustrated. ECT didn’t work for her and she thinks it is barbaric and it was taking time out that actually helped her.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
But the one particular thing that’s hit me recently that my daughter has given me that picture of her Dedication and I can remember who her godparents were. I can remember the songs that were sung at the Dedication, but the picture, the building is completely alien to me, the posters on the wall, and I’m just so frustrated thinking “Why can’t I get that memory back?” And I blame that on the ECT. You know, my first daughter said before I became depressed, so it was a memory before the ECT, but I think well of course I don’t remember, I don’t know how much memory loss I’ve had because you can’t remember what you’ve lost [laughs].
You know, my first daughter said before I became depressed, so it was a memory before the ECT, but I think well of course I don’t remember, I don’t know how much memory loss I’ve had because you can’t remember what you’ve lost [laughs].And, you know, even now I go back to things and the memory is just gone, and personally I think ECT is awful. I think it’s barbaric. I don’t think they understand how it works. I know my GP, my current GP thinks it’s very good and it does work. But I just, to me personally it doesn’t, and go back to previous patient, you know, perhaps the time out is what actually does work.
For many, the memory loss was short lived, around the time of - or before - the treatments. Tania says that although she had not suffered long term memory loss, she does have “gaps” in her memory from the months when she was receiving weekly or fortnightly ECT treatments (although this didn’t happen when she had less frequent maintenance ECT). Otherwise she says ECT has not affected her ability to think and write. Like others, she was concerned her thinking would be affected, but feels “sharper than [she’s] ever been”. Catherine Z said she is able to think “just as quickly and clearly” as before the ECT.
Otherwise she says ECT has not affected her ability to think and write. Like others, she was concerned her thinking would be affected, but feels “sharper than [she’s] ever been”. Catherine Z said she is able to think “just as quickly and clearly” as before the ECT.
For others the effects have been more permanent. Sue experienced long term “fogginess”, which she was told would go away, but it never cleared. She still has ongoing short-term memory problems, which are getting worse, though she does wonder if this could be related to her chronic fatigue and pains. Albert had ECT in the 1960s and wasn’t aware of the side effects of memory loss until recently. He said he suffered badly with memory loss and he had difficulties using his mind and that affected his life. He thought it was “[him] that was the problem” but now believes it was a side effect of the ECT and has met others who have suffered long term memory loss after having ECT. Sunil says for him memory loss is the most distressing effect of ECT. On a daily basis his wife tells him about something that has happened in the recent past which he has no memory of. His wife keeps a diary so he can look back at what has happened in the last few weeks. Dafydd’s wife watches repeats of television programmes but has no recollection of having seen them before.
On a daily basis his wife tells him about something that has happened in the recent past which he has no memory of. His wife keeps a diary so he can look back at what has happened in the last few weeks. Dafydd’s wife watches repeats of television programmes but has no recollection of having seen them before.
David Y doesn’t think ECT helped his wife. Now, twenty years on, she will talk about something that happened months or years ago, which she thinks has just happened.
David Y doesn’t think ECT helped his wife. Now, twenty years on, she will talk about something that happened months or years ago, which she thinks has just happened.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
I don’t know whether the ECT actually helped her or not. I mean they say it kick starts, re-kick starts the brain for them and it would take, it seemed to take too long and then to turn round and say it worked, I don’t think it did.
I mean they say it kick starts, re-kick starts the brain for them and it would take, it seemed to take too long and then to turn round and say it worked, I don’t think it did.And I know you talked to me about the shock of finding that there was memory loss in the short term, what’s been the effect on memory, if any, in the longer term?
She still doesn’t know or can’t remember the things that she’s done with the kids. I mean whether that is because of that I don’t know, she couldn’t remember, it’s easier for her to remember things prior to her illness even now than it is since. I’ll always have things repeated numerous times and it gets, to be told oh I’ve, I’ve seen such and such a body today and I’ve seen such, and you know full well that you’ve heard this story seven times today but it happened six months ago, that I just sit there now and say yes, yes [inaudible speech] yeah, yeah anything for a quiet life. But still she tells me things as if it happened just, but I know full well it was months ago, in some cases years ago.
As mentioned above, where the ECT had worked, some felt the memory loss was minor in relation to the benefits they got, or that the memory loss served a helpful purpose. Jane felt that although she doesn’t remember much of her own childhood or her son’s childhood, this was because her brain was used to shutting off painful memories “as a protective thing” and not as a result of having the ECT. Others wondered whether the memory loss might have actually been a part of what got them better, because they had forgotten the bad things that happened to them. Helen said, “It's so beautiful now because I can forget”. She has found innovative ways to get around the inconvenience of memory loss, like reading so that she remembers how to spell words or writing down the date every morning. Nevertheless, many people who experienced memory loss just found it difficult and upsetting.
Other consequences of having ECT
While some were neutral about the ECT experience, or even found it pleasant (one man looked forward to his ECT), feelings like a lack of control or having been abused during their treatment were profoundly difficult for others. Sue, who had been sexually abused in her childhood, felt that having ECT left her traumatised, and having the anaesthetic felt like she was being held down. She said abuse by members of hospital staff, and the feelings of powerlessness she experienced had long-term consequences for her and her husband. Tracy felt ECT did nothing for her except remove her memory and she called it barbaric.
Sue, who had been sexually abused in her childhood, felt that having ECT left her traumatised, and having the anaesthetic felt like she was being held down. She said abuse by members of hospital staff, and the feelings of powerlessness she experienced had long-term consequences for her and her husband. Tracy felt ECT did nothing for her except remove her memory and she called it barbaric.
While some felt included in their loved ones treatment, as a carer, Carys struggled with her own lack of control over the ECT treatments given to her daughter, and felt side lined and unimportant. Her daughter repeatedly ran away from the hospital and was incredibly unhappy and she still struggles with the feeling that she let her daughter down.
Some people who had bipolar disorder described experiencing a ‘high’ after the ECT. John Z, who was catatonic when he had the treatment, went high and “off the scale” after his ECT treatment (see for more ‘How effective did people find ECT’). Sometimes this was short lived and left them feeling worse than before.
Jenny says that while she was having ECT she was in a daze. She was less driven to harm herself, but there were things she couldn’t do like baking, as her mind was foggy and it affected her sense of self.
Jenny says that while she was having ECT she was in a daze. She was less driven to harm herself, but there were things she couldn’t do like baking, as her mind was foggy and it affected her sense of self.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
I think it was a, it had some sort of buffering effect. I stumbled through those few months in a complete daze. And I was safer in a daze, I was less driven to do harm to myself, less driven to do impulsive things. But it, it meant probably that the challenge of self-belief and self-esteem was more difficult, because you couldn’t even, you couldn’t even make a cake, let alone do anything else, because everything was just in a bit of a sort of foggy mist really. So I don’t think I felt like a real person. And I would have said that although I felt less anguished, I didn’t shift very much from believing myself to be fairly, fairly convincingly a waste of space because I did nothing useful and I couldn’t function very well at all. But, but I, I think it would be difficult to know really quite how much of a part ECT played in that. I wouldn’t want to look as if I was blaming it for something that may have been a corollary of lots of losses at the time. So, but I think the thing it, it definitely did was made me less clear thinking and less coordinated. So I was less likely to throw myself off a motorway bridge or that sort of thing, because I just wouldn’t have been well enough organised to do those things, I don’t think.
So I don’t think I felt like a real person. And I would have said that although I felt less anguished, I didn’t shift very much from believing myself to be fairly, fairly convincingly a waste of space because I did nothing useful and I couldn’t function very well at all. But, but I, I think it would be difficult to know really quite how much of a part ECT played in that. I wouldn’t want to look as if I was blaming it for something that may have been a corollary of lots of losses at the time. So, but I think the thing it, it definitely did was made me less clear thinking and less coordinated. So I was less likely to throw myself off a motorway bridge or that sort of thing, because I just wouldn’t have been well enough organised to do those things, I don’t think.
Julian had a kind of high after the ECT treatment but then went downhill after two weeks and was ‘more suicidal’ than he’d been before, although lithium helped him recover.
Julian had a kind of high after the ECT treatment but then went downhill after two weeks and was ‘more suicidal’ than he’d been before, although lithium helped him recover.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
All I remember is that I was kind of well. I mean he described it as being kind of high. Whatever, it had quite a beneficial effect that was very short-lived. And, so it was like being given a tantalising look into what it would be like to be better. And in a way that was very difficult to feel, it was very difficult to cope with, that when I then went downhill again, having reached the treatment of last resort, well, that was it, I was finished. And I probably became more suicidal than I’d been before. In fact I guess I’m quite lucky to be here really, yeah, I guess it was quite close to just finishing it.
Sunil finds now that he gets hypomania, though he is not sure if that is as a result of the ECT or the anti-depressants he is taking. His wife finds this very difficult and it has stopped him going back to work.
Sunil finds now that he gets hypomania, though he is not sure if that is as a result of the ECT or the anti-depressants he is taking. His wife finds this very difficult and it has stopped him going back to work.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
But I did find out, from my consultant and my wife that during this latest episode of illness which is now into its eighth month, just over seven months, I had a total of 39 ECT treatments which is a fantastically huge amount of ECT and my last ECT treatment was given on New Year’s Eve, and I’ve been reasonably well since the beginning of this year. But in actual fact whether it’s due to the fact that I’ve had ECT or whether it’s due to the fact that I’m on two different anti-depressants in addition to the ECT I have actually been a little bit on the high side. In other words slightly hypomanic. And never severely, but it has actually caused a lot of problem, because my wife can cope with me, no matter how severely depressed I am, and even if I’m suicidal she can cope with me. But the one thing she finds very, very challenging and difficult to cope with, is when I’m hypomanic. Because that’s when you tend to be more argumentative, and all the rest of it.
But in actual fact whether it’s due to the fact that I’ve had ECT or whether it’s due to the fact that I’m on two different anti-depressants in addition to the ECT I have actually been a little bit on the high side. In other words slightly hypomanic. And never severely, but it has actually caused a lot of problem, because my wife can cope with me, no matter how severely depressed I am, and even if I’m suicidal she can cope with me. But the one thing she finds very, very challenging and difficult to cope with, is when I’m hypomanic. Because that’s when you tend to be more argumentative, and all the rest of it.Anyway even if I’m only very slightly hypomanic, she finds that really difficult. And in fact the clinical psychologist I’ve been seeing, we’ve got a scale for people with bipolar illness where you actually monitor your mood on a daily basis and you grade it on a scale of plus five to minus five, with a middle zero being when you are completely normal mood, neither high nor low. Minus 5 is when you are in the depths of depression and plus 5 is when you are not just hypomanic, you are actually manic. Plus 5 is a very severe illness which requires hospitalisation. And I think in my estimation, even the highest that I’ve actually been in the last month has been only plus one no more than that, although my wife thinks I’ve probably been a little bit more than plus one, perhaps something like plus one and a half.
Minus 5 is when you are in the depths of depression and plus 5 is when you are not just hypomanic, you are actually manic. Plus 5 is a very severe illness which requires hospitalisation. And I think in my estimation, even the highest that I’ve actually been in the last month has been only plus one no more than that, although my wife thinks I’ve probably been a little bit more than plus one, perhaps something like plus one and a half.
And that is the main reason why I’m not actually back at work yet. Because had I been given the choice, I would have actually gone back to work at least a fortnight ago. But I have actually now finally got a fit to return to work note from both my general practitioner and my psychiatrist. So hopefully the people at work will not really stop me from going back.
Last reviewed January 2018.
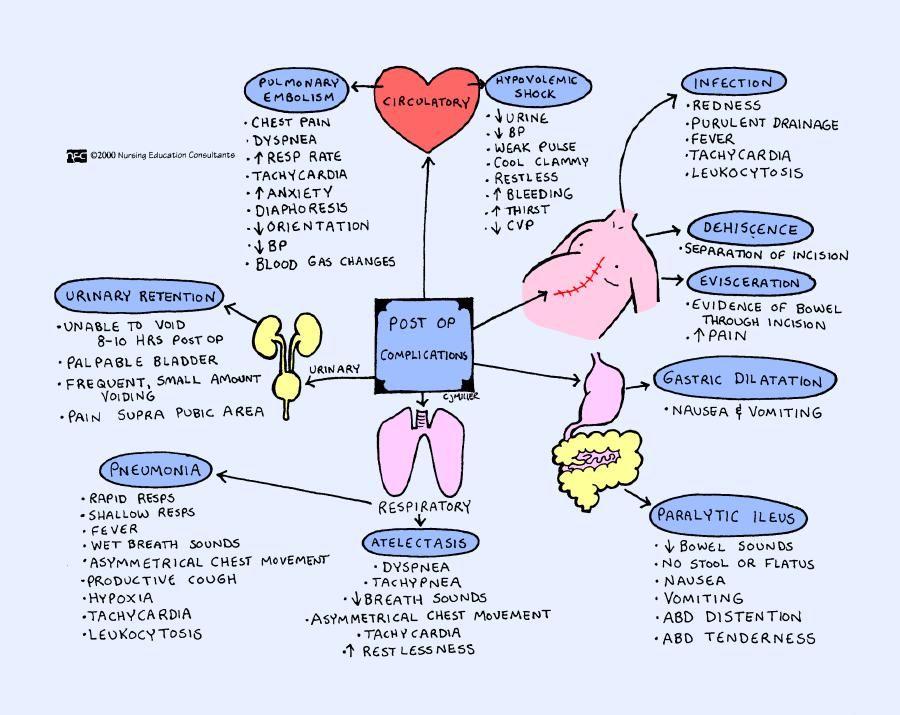
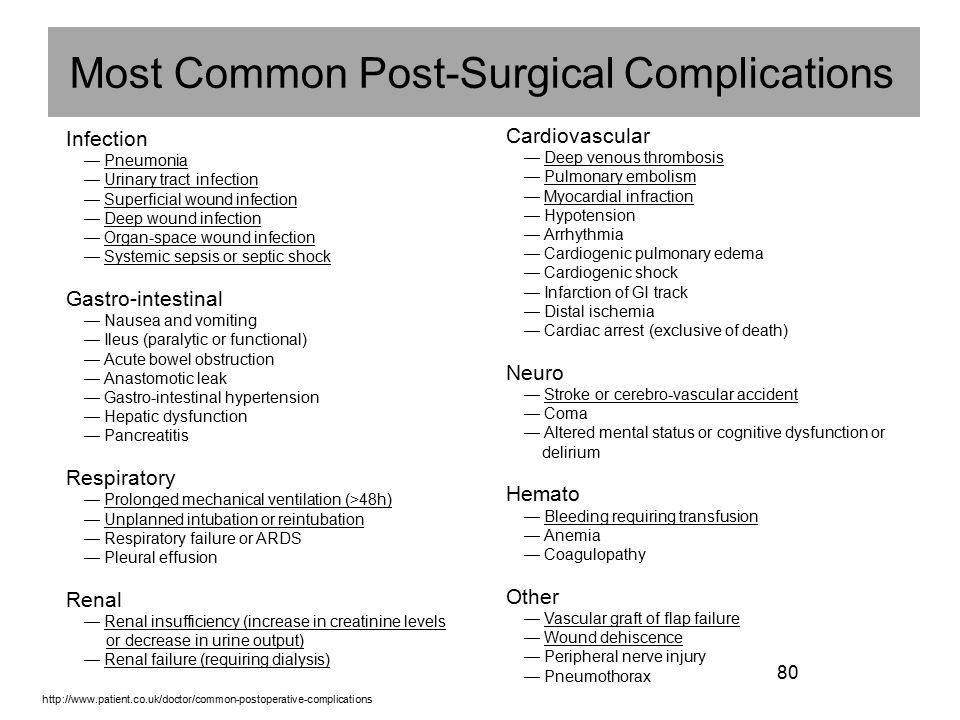
Postoperative complications \ ConsultantPlus
Postoperative complications
The most common early complications after hemodynamic correction are neurological disorders, respiratory failure, superior vena cava syndrome, increased extravasation [43, 45, 56].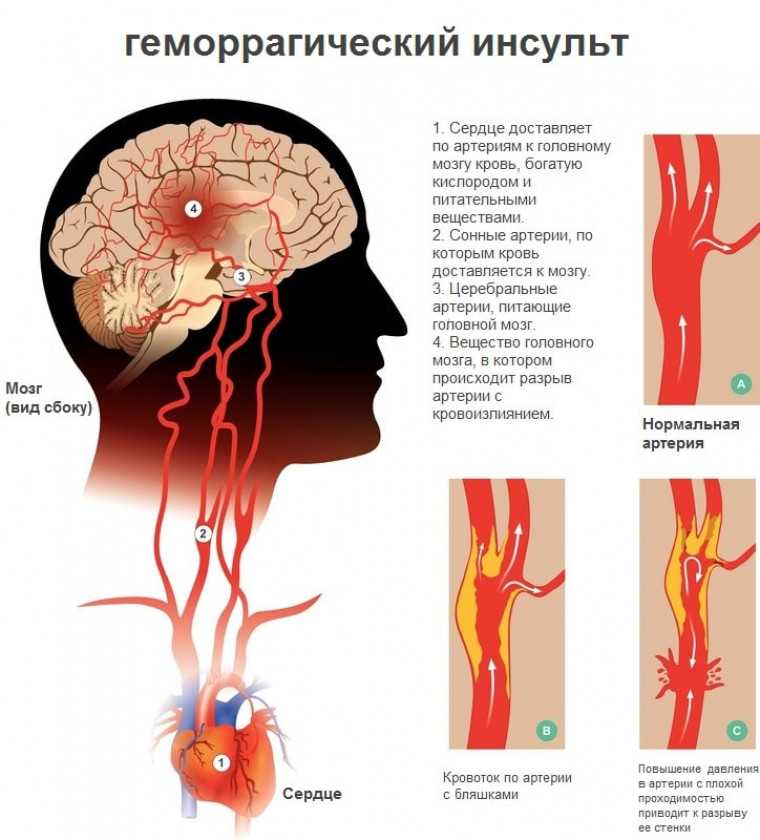
- To reduce the risk of postoperative complications, early (1st postoperative day) extubation of patients after hemodynamic correction is recommended [57–62].
(UUR C, UDD 4)
Comments: The main complications are often associated with an increase in venous pressure in the cavopulmonary tract, which in turn may be due to PVR fluctuations in the early postoperative period and insufficient compensation of pulmonary circulation to increase blood flow. Artificial ventilation of the lungs increases intrathoracic pressure and slows down venous return through the systemic veins, which is an additional factor in increasing venous pressure.
Among the long-term complications after hemodynamic correction, the most important are venous hypertension, cardiac arrhythmias, protein-deficient enteropathy, hepatic dysfunction, and thromboembolic complications [2, 8]. nine0003
Venous hypertension is the main cause of the development and progression of NK (hepatomegaly, ascites, hydrothorax, peripheral edema, cyanosis) in the medium-long term after Fontan operation. Factors that increase the likelihood of developing venous hypertension include stenosis of the PA, DILK, insufficiency of the AV valve, stenosis of the vena cava or vascular prosthesis between the IVC and the PA (for example, due to the "overgrowth" of the prosthesis), the development of venous collaterals, SF dysfunction, protein-deficient enteropathy (BDEP), feasibility study, liver failure [2]. nine0003
Factors that increase the likelihood of developing venous hypertension include stenosis of the PA, DILK, insufficiency of the AV valve, stenosis of the vena cava or vascular prosthesis between the IVC and the PA (for example, due to the "overgrowth" of the prosthesis), the development of venous collaterals, SF dysfunction, protein-deficient enteropathy (BDEP), feasibility study, liver failure [2]. nine0003
- Elimination of local LA stenoses is recommended if they develop in patients after certain stages of hemodynamic correction [2, 10, 11, 22].
(URL C, LDD 5)
Comments: In most cases, their elimination is possible by endovascular means.
- Endovascular removal of DILC is recommended in case of their recanalization or development after DKPA or Fontan operation with persistent signs of NK [2, 10, 11, 22].
(LEV C, ELA 5)
Comments: Aortopulmonary collateral arteries may not be diagnosed before surgery or develop early or late after surgery. Recanalization of the PA trunk can occur 1–2 years after surgery (the situation is true for cases where the pulmonary trunk was ligated intraoperatively, and is irrelevant for patients with concomitant pulmonary artery atresia). nine0003
nine0003
- With progression of AV valve insufficiency of more than moderate degree, corrective surgery is recommended for patients [2, 10, 11, 22].
(LEV C, LDD 5)
Comments: Correction of AV valve insufficiency can be performed as a separate procedure or simultaneously with the Fontan procedure. In some cases, this complication occurs in the late postoperative period due to infective endocarditis or dilatation of the fibrous ring of the valve as a result of progressive SF dysfunction. nine0003
- After the Fontan operation in the modification of the ECC, patients are recommended surgery to replace the vascular prosthesis in the event of venous hypertension due to insufficient size of the conduit relative to the growth and development of the patient [2, 10, 11, 22].
(LEC C, LDD 5)
- To increase blood oxygen saturation in case of development of venous collaterals after DCPA, patients are recommended to embolize them [2, 10, 11, 22].
(LEV C, LDD 5)
Comments: In the absence of such factors as severe AV valve insufficiency, residual PA stenoses and increased pressure in the pulmonary circulation, the results of DKPA surgery are good. However, as the patient grows, there is a gradual decrease in arterial oxygen saturation, which is due to an age-related decrease in the proportion of venous return through the SVC system, as well as the development of pulmonary arteriovenous fistulas. Progressive cyanosis in the long term after DCPA surgery may also be associated with the development of collateral vessels between the systems of the superior and inferior vena cava, due to the pressure difference between them, leading to the discharge of blood from the SVC to the IVC and a decrease in pulmonary blood flow. The hemodynamic causes of this complication can also be obstruction of the pulmonary blood flow at various levels, increased PVR, dysfunction of the SF or AV valves, thrombosis of the vena cava, and other factors leading to an increase in venous pressure. According to A. Magee et al. venous collateral vessels develop in 31% of cases after DKPA surgery. The most common collateral vessels are the unpaired and semi-unpaired veins, as well as the veins of the pericardium and the anterior chest wall.
However, as the patient grows, there is a gradual decrease in arterial oxygen saturation, which is due to an age-related decrease in the proportion of venous return through the SVC system, as well as the development of pulmonary arteriovenous fistulas. Progressive cyanosis in the long term after DCPA surgery may also be associated with the development of collateral vessels between the systems of the superior and inferior vena cava, due to the pressure difference between them, leading to the discharge of blood from the SVC to the IVC and a decrease in pulmonary blood flow. The hemodynamic causes of this complication can also be obstruction of the pulmonary blood flow at various levels, increased PVR, dysfunction of the SF or AV valves, thrombosis of the vena cava, and other factors leading to an increase in venous pressure. According to A. Magee et al. venous collateral vessels develop in 31% of cases after DKPA surgery. The most common collateral vessels are the unpaired and semi-unpaired veins, as well as the veins of the pericardium and the anterior chest wall. Collateral venous embolization is an effective method of increasing blood oxygen saturation in cases where the risk of Fontan operation is increased. nine0003
Collateral venous embolization is an effective method of increasing blood oxygen saturation in cases where the risk of Fontan operation is increased. nine0003
- Heart transplantation is recommended for patients with severe SF dysfunction refractory to conservative therapy [2].
(LEC C, LDD 5)
Comments: SF dysfunction may be due to both its morphology and the initial severity of the defect or past infectious diseases (including myocarditis) in the postoperative period [6].
- Immediate hospital admission is recommended for patients with suspected BDEP [2, 53, 54].
(UUR C, UDD 3)
Comments: The term "protein-deficient enteropathy" refers to a condition characterized by impaired absorption of protein in the small intestine. The frequency of this complication averages 3.8%. The terms of development of BDEP range from 1 month to 16 years (average 2.7 years), while in one third of patients the complication develops over 5 years after surgery. The reasons for the development of BDEP after the Fontan operation are still not fully understood. One of the probable mechanisms is the development of lymphangiectasias in the abdominal organs, including the intestines, as a result of constantly increased venous and lymphatic pressure after the Fontan operation. Clinically, BDEP is manifested by hypoalbuminemia, and as a result, edema, ascites, pleural extravasation or chylothorax, immunodeficiency and hypocalcemia. In the later stages of development, most of the manifestations of this complication correspond to the clinical picture of NK. The method of early diagnosis of BDEP is to determine the level of fecal 1-antitrypsin, the concentration of which increases significantly in BDEP. The prognosis in the case of the development of BDEP is usually unfavorable. Most studies report high mortality among these patients. If within 5 years from the moment the complication develops, the survival rate is about 60%, then after 10 years less than 20% of patients remain alive. nine0003
One of the probable mechanisms is the development of lymphangiectasias in the abdominal organs, including the intestines, as a result of constantly increased venous and lymphatic pressure after the Fontan operation. Clinically, BDEP is manifested by hypoalbuminemia, and as a result, edema, ascites, pleural extravasation or chylothorax, immunodeficiency and hypocalcemia. In the later stages of development, most of the manifestations of this complication correspond to the clinical picture of NK. The method of early diagnosis of BDEP is to determine the level of fecal 1-antitrypsin, the concentration of which increases significantly in BDEP. The prognosis in the case of the development of BDEP is usually unfavorable. Most studies report high mortality among these patients. If within 5 years from the moment the complication develops, the survival rate is about 60%, then after 10 years less than 20% of patients remain alive. nine0003
Possible postoperative complications . Neurosurgery in Latvia
Possible postoperative complications. Every time an operation is planned, the doctor is obliged to inform the patient about the progress of the planned operation and possible complications.
Every time an operation is planned, the doctor is obliged to inform the patient about the progress of the planned operation and possible complications.
Since both the doctor and the patient expect and plan only a good outcome of the operation, this conversation, of course, is unpleasant for both parties, but it is an indispensable part of modern preparation for surgery.
The purpose of the interview is to explain to the patient in as much detail as possible exactly what will be done during the operation, so that the patient can better understand what to expect after the operation. The purpose of the conversation is also to inform the patient about possible complications - both during the operation and after it. During this conversation, the doctor can answer additional questions if the patient has any, as well as inform about the planned actions in the event of any of the complications. nine0003
In general, operations are considered relatively safe - the risk of any complications during or after the operation is relatively small, but unfortunately it always exists. The operation can be compared to going outside - in general it is safe, but no one is completely immune from accidents. In most cases, surgeries are planned in situations where the risk of surgery is lower than the health risk without surgery, i.e. the operation is the safest of all alternatives.
The operation can be compared to going outside - in general it is safe, but no one is completely immune from accidents. In most cases, surgeries are planned in situations where the risk of surgery is lower than the health risk without surgery, i.e. the operation is the safest of all alternatives.
It should be noted that the operation is a complex process in which not everything is under the control of doctors. Naturally, in preparation for surgery and during surgery, doctors do everything possible to minimize the possibility of any complications. Some of the complications may be associated with the actions of doctors, but some may occur and occur for a number of other reasons - most often they are associated with the characteristics of the patient's body. This circumstance explains the fact that complications occur even in the world's best hospitals and among the most famous doctors. nine0003
Possible postoperative complications of standard spinal surgery are listed below and described in more detail.
Some specific surgeries may involve additional risks, which your doctor will inform you about during your pre-op interview.
The combined overall risk (probability of developing one or more of the following complications) for standard spinal surgery is in the range of 2-4%.
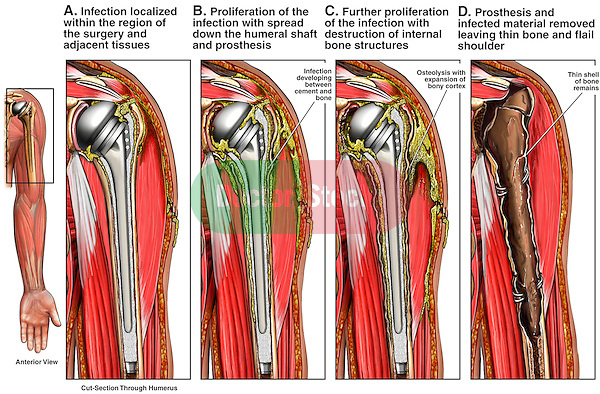
- Infection. Although the operation is performed under sterile conditions using sterile instruments, there is a small chance that bacteria can enter the wound during or after the operation, which may cause infection of the wound. To reduce this risk, the patient is always given a prophylactic dose of antibiotics (drugs that kill bacteria) at the start of surgery. The risk of infection is slightly increased in patients with diabetes mellitus, in immunocompromised patients, and elderly patients. Infection usually starts 4-6 days after surgery, but may occur later. The most common manifestations of infection are fever, redness in the wound area, poor wound healing, increased pain in the wound area, discharge from the wound.
 nine0080
nine0080 - Hemorrhage in the area of operation - At the end of the operation, before closing the wound, surgeons always stop any bleeding, even the slightest, but there is a small risk that after closing the wound, a hematoma still develops. If the hematoma is large and causing symptoms, a second operation is sometimes necessary to flush the hematoma out of the wound.
- Damage to the dura mater/liquorrhea. The spinal cord and/or nerves in the spinal canal are located inside a special sheath called the dura mater. In addition to the nerves and spinal cord, there is also cerebrospinal fluid (CSF) inside the membrane - which washes the spinal cord and nerves. If mechanical damage to the dura occurs during surgery, cerebrospinal fluid may leak outside the membrane and may even seep through the wound and make it difficult to heal (liquorrhea). And also, if liquorrhea is formed, there is a high probability of infection getting into the wound and into the membranes of the brain, thereby causing inflammation of the membranes of the brain (meningitis).
 To prevent this complication, sparing microsurgical methods are used during the operation. In those cases, if the shell injury did occur, the defect is immediately closed during the operation by stitching or gluing the shell, so this complication rarely causes problems. nine0080
To prevent this complication, sparing microsurgical methods are used during the operation. In those cases, if the shell injury did occur, the defect is immediately closed during the operation by stitching or gluing the shell, so this complication rarely causes problems. nine0080 - Mechanical damage to the nerve/spinal cord during surgery. Injury to a nerve or spinal cord can cause numbness and/or loss of sensation and/or immobility in the nerve's innervation area (the supply area of the particular nerve). This complication is extremely rare. To avoid such a complication, operations are performed under visual control, under microscope magnification and using safe microsurgical techniques.
- Failure of surgery to improve symptoms. Each operation has its scientifically proven level of effectiveness. With a correct diagnosis and well-placed indications for surgery, the probability of a successful outcome of most operations is very high - about 95%.
 However, in a very small number of patients (up to 5%), the improvement after surgery may not be complete, or the operation may not be effective at all. The reasons for this may be the following: A. The patient has a list of problems with the spine, which manifest themselves in a similar way. The operation solves one or two of several problems, but does not solve others. Therefore, the effect of the operation may be incomplete or absent, despite the fact that the operation was performed technically correctly. To minimize the possibility of disappointment, the neurosurgeon always informs the patient about the expected effect of the operation before the operation. B. The patient has another disease that mimics a spinal problem (such as a stroke), but this fact is not known at the time of the operation, so the operation does not improve symptoms. Detailed and accurate diagnosis of the disease, analysis of complaints and symptoms of the patient, the belief that the symptoms correspond to the results of visual diagnostics, avoid problems of this nature.
However, in a very small number of patients (up to 5%), the improvement after surgery may not be complete, or the operation may not be effective at all. The reasons for this may be the following: A. The patient has a list of problems with the spine, which manifest themselves in a similar way. The operation solves one or two of several problems, but does not solve others. Therefore, the effect of the operation may be incomplete or absent, despite the fact that the operation was performed technically correctly. To minimize the possibility of disappointment, the neurosurgeon always informs the patient about the expected effect of the operation before the operation. B. The patient has another disease that mimics a spinal problem (such as a stroke), but this fact is not known at the time of the operation, so the operation does not improve symptoms. Detailed and accurate diagnosis of the disease, analysis of complaints and symptoms of the patient, the belief that the symptoms correspond to the results of visual diagnostics, avoid problems of this nature. C. As a result of the disease, the patient has suffered irreversible damage to the nervous system, and despite the technically accurate and correctly performed operation, the patient does not show improvement in symptoms. This is a normal practice in some diseases, such as surgery in cases of spinal stenosis with spinal cord injury (myelopathy). The purpose of the operation is to prevent further damage to the spinal cord, i.e. so that the person does not get worse. Improvements are also often observed, but in the context of this operation, this is considered as an additional benefit, and not as the main goal of the operation. nine0080
C. As a result of the disease, the patient has suffered irreversible damage to the nervous system, and despite the technically accurate and correctly performed operation, the patient does not show improvement in symptoms. This is a normal practice in some diseases, such as surgery in cases of spinal stenosis with spinal cord injury (myelopathy). The purpose of the operation is to prevent further damage to the spinal cord, i.e. so that the person does not get worse. Improvements are also often observed, but in the context of this operation, this is considered as an additional benefit, and not as the main goal of the operation. nine0080 - Recurrence - most often in the context of an operation to remove a herniated disc. When operating on a herniated disc, the neurosurgeon never removes the entire disc, because the disc performs a very important function in the spine: it is a shock absorber between the bone vertebrae, which dampens vertical loads and shocks.
 During surgery, only the portion of the disc that is compressing the nerve and causing symptoms is removed. Because the disc is never completely removed, there is a chance that the disc herniation will recur. In some cases, if a recurrence presses again on the nerve and causes symptoms and complaints, a second operation may be necessary. The term "relapse" can also be used in the context of spinal tumor surgery. Tumor recurrence - re-growth of the tumor, which may require a second - revision surgery. In very rare cases, recurrence of stenosis (narrowing) of the spinal canal may also occur after the primary operation, which may require a second operation. nine0080
During surgery, only the portion of the disc that is compressing the nerve and causing symptoms is removed. Because the disc is never completely removed, there is a chance that the disc herniation will recur. In some cases, if a recurrence presses again on the nerve and causes symptoms and complaints, a second operation may be necessary. The term "relapse" can also be used in the context of spinal tumor surgery. Tumor recurrence - re-growth of the tumor, which may require a second - revision surgery. In very rare cases, recurrence of stenosis (narrowing) of the spinal canal may also occur after the primary operation, which may require a second operation. nine0080 - The need for a repeat, revision surgery - may occur in cases described in point number 6, as well as in cases of wound infection or hematoma (hemorrhage) in the area of operation.
- Need for future spinal fixation surgery . In a normal situation, the vertebrae of the spine are relatively immobile in relation to each other - this is called "spinal stability".
 This immobility is provided by the intervertebral joints and ligaments between the vertebrae. During any operation on the spine, there is an intervention in the structures that ensure the stability of the spine. In very rare cases, as a result of the operation, the so-called "instability of the spine" can develop - increased mobility between two adjacent vertebrae. If the instability causes problems for the patient (most often back pain), a "stabilizing" operation - fixation of the vertebrae - may be required. To avoid this complication, neurosurgeons only use surgical techniques that have proven to be safe and do not cause spinal instability. However, in rare cases, most often with a congenital predisposition to instability, such a complication may occur. It should be noted that spinal instability itself can occur in various diseases of the spine. nine0080
This immobility is provided by the intervertebral joints and ligaments between the vertebrae. During any operation on the spine, there is an intervention in the structures that ensure the stability of the spine. In very rare cases, as a result of the operation, the so-called "instability of the spine" can develop - increased mobility between two adjacent vertebrae. If the instability causes problems for the patient (most often back pain), a "stabilizing" operation - fixation of the vertebrae - may be required. To avoid this complication, neurosurgeons only use surgical techniques that have proven to be safe and do not cause spinal instability. However, in rare cases, most often with a congenital predisposition to instability, such a complication may occur. It should be noted that spinal instability itself can occur in various diseases of the spine. nine0080 - Damage to the main blood vessels - due to the location of the main blood vessels (abdominal aorta and vena cava) in the anterior part of the spine, during the operation, in extremely rare cases, mechanical damage to these blood vessels is possible, which can lead to severe bleeding.
 This complication is potentially life-threatening. To prevent this complication, during surgery, neurosurgeons never deliberately perform mechanical actions in the anterior part of the spine, except for rare, specific operations that require access to the spine from the front, but in such cases, vascular surgeons are involved to ensure the safety of such access. nine0080
This complication is potentially life-threatening. To prevent this complication, during surgery, neurosurgeons never deliberately perform mechanical actions in the anterior part of the spine, except for rare, specific operations that require access to the spine from the front, but in such cases, vascular surgeons are involved to ensure the safety of such access. nine0080 - Failed back surgery syndrome (FBSS). This term is inherently misleading, as it does not refer to a specific disease or syndrome, but refers to a fairly broad group of patients who develop new pain or persist (preoperative) pain after spinal surgery due to back pain or legs. Since the SNOP group includes a wide variety of patients and cases, the causes of the development of the syndrome are varied. In general, the causes of SNOP can be divided into 3 groups: A - these are patients in whom surgery was not required from the very beginning (indications for surgery were not correctly established) or patients in whom the probability of success of surgical intervention was low from the very beginning and the operation was a “step desperation" with little chance of a good result.
 B - these are patients who needed the operation, but its technical execution was incomplete or the wrong technical solution was chosen. C - these are patients for whom the operation was necessary and its technical execution was correct, but the pain after the operation occurs as a result of irreversible damage to the spinal nerves caused by the disease that was before the operation (the so-called neuropathic pain or pain caused by damage to the nerve itself). To reduce To minimize the risk of developing SNOP, neurosurgeons when planning operations are guided by the following principles: nine0136
B - these are patients who needed the operation, but its technical execution was incomplete or the wrong technical solution was chosen. C - these are patients for whom the operation was necessary and its technical execution was correct, but the pain after the operation occurs as a result of irreversible damage to the spinal nerves caused by the disease that was before the operation (the so-called neuropathic pain or pain caused by damage to the nerve itself). To reduce To minimize the risk of developing SNOP, neurosurgeons when planning operations are guided by the following principles: nine0136 - operations are performed in cases where the probability of a good outcome of the operation is high or very high.
- Particular attention is paid to the technical execution of the operation and the chosen surgical method - the operation must fully achieve the goal (removal of the cause of the disease) by applying the correct, as minimally invasive and safe intervention as possible.
- In difficult cases, where the originally planned goal of the operation is to improve the patient's condition, but not a complete cure, it is important to discuss with the patient the expected result of the operation (improvement, but not a cure) in order to avoid disappointment after the operation. nine0080
- Disappointment - this problem may arise in a situation where the patient expects a certain result from the operation, but in fact the result is different from the expected one, and the patient feels disappointed. To prevent this problem, the task of the surgeon is to take the time to explain in detail to the patient what effect is expected from the operation.
- Pain. After any operation, pain to a greater or lesser extent is considered a normal situation and not a complication. The intensity of pain depends both on the volume of the operation performed and on the pain threshold of each individual patient.
 Thanks to modern, minimally invasive surgical techniques, the problem of pain is often minor and can be solved with conventional painkillers. In rare cases, stronger pain relievers may need to be used. nine0080
Thanks to modern, minimally invasive surgical techniques, the problem of pain is often minor and can be solved with conventional painkillers. In rare cases, stronger pain relievers may need to be used. nine0080 - Wound healing problems . Most surgical wounds heal easily and quickly, but some people heal worse and take longer to heal than others and sometimes with larger scarring. Patients with diabetes, overweight, patients who do not follow a regular nutritious diet, have an increased risk of problems with wound healing. Sometimes difficult-to-heal wounds require additional attention from the surgeon - it may be necessary to re-suture the wound or “refresh” the edges of the wound with a small operation. nine0080
- Allergic reactions to medications - although rare, any medication used before, during, or after surgery could theoretically cause an allergic reaction. To reduce the risk of this complication, physicians should determine if the patient has a history of allergies and/or intolerance to drugs in order to avoid their use.
- Risks of anesthesia (narcosis). Anesthesia is the process of providing medical sleep and pain relief for the operation. During this process, medications are administered to the patient and measures are taken to support life processes that have their own individual risks. Your anesthetist will talk to you about these risks and strategies to reduce them before surgery. nine0080
- Deep vein thrombosis, pulmonary embolism. A very rare but serious complication that is more common in older, overweight, sedentary people. Additional risk factors for deep vein thrombosis are cancer, long surgery time, prolonged immobility / lying down after surgery, smoking, oral contraception or hormone replacement therapy (HRT), some genetic diseases. Because patients may be less mobile before, during, and after surgery due to their condition, slow blood flow in the deep veins (most often in the legs) can cause blood clots (clots) to form.
 If a clot breaks away from the vein wall and travels through the bloodstream, the clot can eventually enter and clog the pulmonary artery. Occlusion (blockage) of the pulmonary artery due to a clot (thromboembolism) is a potentially life-threatening condition. To reduce the risk of this complication, patients are advised to be as active as possible even while in bed (move their legs, arms, often change position and posture in bed), drink plenty of fluids, mobilize (get out of bed) as soon as possible - usually in the first postoperative day. The use of prophylactic compression stockings (worn up to the middle of the thigh) is also recommended. Compression socks squeeze out blood from the veins of the legs, prevent the formation of blood clots, improve blood circulation in the veins, thereby reducing the risk of this complication. In addition, for patients at risk, special medications (low molecular weight heparins) are often used after surgery, which reduce the risk of blood clotting and blood clots.
If a clot breaks away from the vein wall and travels through the bloodstream, the clot can eventually enter and clog the pulmonary artery. Occlusion (blockage) of the pulmonary artery due to a clot (thromboembolism) is a potentially life-threatening condition. To reduce the risk of this complication, patients are advised to be as active as possible even while in bed (move their legs, arms, often change position and posture in bed), drink plenty of fluids, mobilize (get out of bed) as soon as possible - usually in the first postoperative day. The use of prophylactic compression stockings (worn up to the middle of the thigh) is also recommended. Compression socks squeeze out blood from the veins of the legs, prevent the formation of blood clots, improve blood circulation in the veins, thereby reducing the risk of this complication. In addition, for patients at risk, special medications (low molecular weight heparins) are often used after surgery, which reduce the risk of blood clotting and blood clots. nine0080
nine0080 - Bedsores is a soft tissue injury that occurs when soft tissues are compressed against a bone for a long time due to a long stay in one position. Bedsores can occur both during surgery - the patient lies in one position on the operating table for a long time, and after surgery - the patient lies motionless in one position in bed for a long time. The risk of pressure ulcers increases with prolonged surgery, increased body weight, prolonged immobility/lying down in the postoperative period, and neurological deficits. To avoid this complication, during the operation, the patient is positioned on the operating table in such a way that the soft tissues do not press against the bones in the risk areas, and in the postoperative period, it is important to mobilize the patient as early as possible or, if this is not possible, frequent changes in position are practiced - positioning the patient in bed. nine0080
- Urinary tract infection - For surgeries lasting more than 2 hours, most often a catheter is inserted into the patient's bladder before surgery to allow urine to flow and to measure urine volume.
 Insertion of a urinary catheter, although sterile, is itself a risk factor for urinary tract infection. However, if a urinary tract infection does develop, it is a relatively easily treatable complication that may require the use of urinary acidifiers and/or antibiotics. To prevent urinary tract infections, the patient is advised to drink plenty of fluids after surgery. nine0080
Insertion of a urinary catheter, although sterile, is itself a risk factor for urinary tract infection. However, if a urinary tract infection does develop, it is a relatively easily treatable complication that may require the use of urinary acidifiers and/or antibiotics. To prevent urinary tract infections, the patient is advised to drink plenty of fluids after surgery. nine0080 - Stroke. Theoretically, anyone can have a stroke at any time, but since the patient is immobile on the operating table for a long time during the operation, this risk is slightly increased. Undoubtedly, this risk is more characteristic of older people.
- Heart attack (heart attack) - similar to the previous paragraph, a heart attack can theoretically hit anyone, almost at any time, but during the operation this probability increases slightly. A heart attack is a potentially life-threatening condition. nine0080
In cases of suspected neurosurgical disease or already in a situation with a confirmed diagnosis, it is necessary to consult a specialist - a neurosurgeon.