Self test for ocd
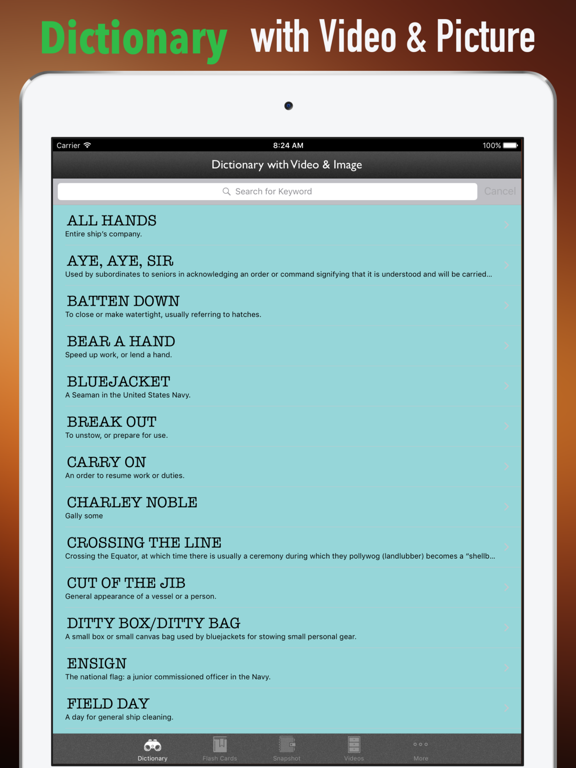
3 Minute Obsessive Compulsive Disorder (OCD) Test
Mood DisordersObsessive-Compulsive Disorder (OCD)
Do I have OCD? Use this quiz to help determine if you might need to consult a mental health professional for diagnosis and treatment of Obsessive-Compulsive Disorder.
Medical ReviewerRandy Bressler, PsyD
Who Is This Obsessive Compulsive Disorder Quiz For?
Below is a list of eight questions designed for people who are experiencing anxiety-inducing thoughts or repetitive behaviors they believe to be uncontrollable. The questions relate to life experiences common among people who have been diagnosed with obsessive compulsive disorder (OCD).
Please read each question carefully, and indicate how often you have experienced the same or similar challenges in the past few months.
How Accurate Is It?
This quiz is NOT a diagnostic tool. Mental health disorders can only be diagnosed by licensed health care professionals.
Psycom believes assessments can be a valuable first step toward getting treatment. All too often people stop short of seeking help out of fear their concerns aren't legitimate or severe enough to warrant professional intervention.
What Does This Test Consist Of?
Eight questions that relate to common thoughts and behaviors experienced by those diagnosed with obsessive compulsive disorder (OCD).
How Is OCD Treated?
OCD is highly treatable often through a combination of cognitive behavior therapy and, in some cases, medication.
Your privacy is important to us. All results are completely anonymous.
Alchemer - amazing survey software for business. Please take my survey now
If you think you or someone you care about may be suffering from OCD, Anxiety, or any other mental health condition, Psycom.net strongly recommends that you seek help from a mental health professional in order to receive a proper diagnosis and support. For those in crisis, we have compiled a list of resources (some even offer free or low-cost support) where you may be able to find additional help.
For those in crisis, we have compiled a list of resources (some even offer free or low-cost support) where you may be able to find additional help.
Obsessive Compulsive Disorder FAQs
How do you know if you have obsessive-compulsive disorder?
OCD is often a term that is misused to describe people who simply like order or have high standards of cleanliness. In reality, OCD is a serious mental health condition that centers on obsessions, compulsions, or both. OCD is not solely related to germs or cleanliness, but those can be common themes. If you find yourself having recurring, unwanted thoughts that disrupt your daily life and compel you to take an action, you may want to speak to a mental health professional about OCD.1
Is OCD an anxiety disorder?
OCD was previously categorized as an anxiety disorder but was reclassified in the 5th edition of the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-5) under the heading of ‘Obsessive-Compulsive and Related Disorders’. This was a controversial decision in the psychiatric community. Prior to the publishing of DSM-5, a paper titled ‘Should OCD be classified as an Anxiety disorder in DSM-V?’ surveyed authors of OCD publications. Approximately 60% of respondents supported moving OCD out of the anxiety disorders section, while 40% disagreed.
This was a controversial decision in the psychiatric community. Prior to the publishing of DSM-5, a paper titled ‘Should OCD be classified as an Anxiety disorder in DSM-V?’ surveyed authors of OCD publications. Approximately 60% of respondents supported moving OCD out of the anxiety disorders section, while 40% disagreed.
What causes obsessive-compulsive disorder?
While the exact cause of OCD is unknown, scientists believe that biological, genetic, and environmental factors play a role in its occurrence. Having another mental health disorder, having parents or other family members with OCD, and experiencing traumatic life events can increase your risk of developing OCD.
Is OCD a serious mental illness?
OCD is a serious mental illness that can become debilitating if left untreated. It is characterized by high levels of fear, anxiety, and emotional distress. In severe cases of OCD, the disorder can prevent the individual from functioning in daily life, interfere with relationships and responsibilities, and significantly impact quality of life.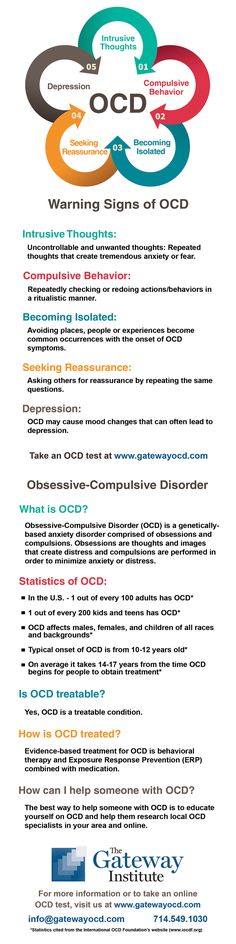
Who is most likely to get OCD?
OCD can affect children, adolescents, and adults alike. Most people with OCD are diagnosed by the age of 19, but onset after age 35 can occur. OCD typically presents earlier in males than in females. Having another mental health disorder, having parents or other family members with OCD, and experiencing traumatic life events can increase your risk of developing OCD.
Does OCD get worse with age?
The symptoms of OCD can worsen with age if left untreated. Those diagnosed with OCD in adolescence have a 60% chance of the illness becoming a lifelong disorder without the guidance of a mental health professional. In most cases, OCD symptoms can be alleviated with time and treatment, but others will be classified as chronic.
What is rumination?
Rumination is the process of obsessively thinking about an idea, situation, or choice, which tends to be negative or troubling. Rumination is a central symptom of OCD that causes the individual to spend a significant amount of time thinking about or analyzing their obsessions.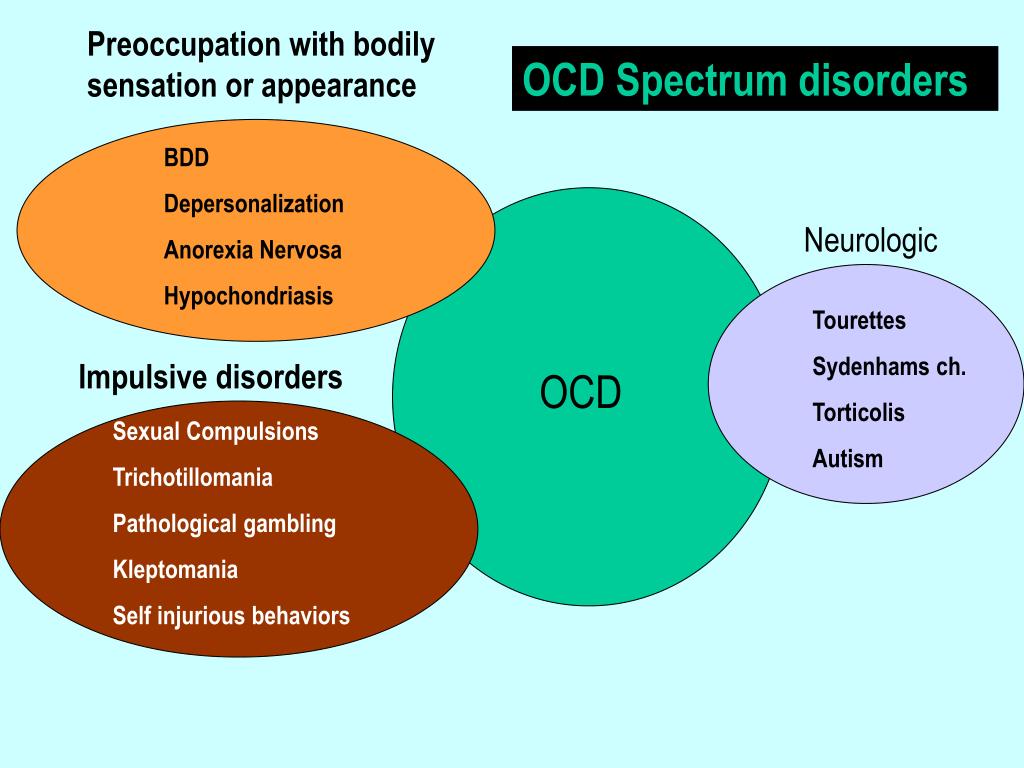 Rumination can be seriously damaging to one’s mental health, as it can interfere with daily functioning and cause the individual to withdraw from their responsibilities and relationships.
Rumination can be seriously damaging to one’s mental health, as it can interfere with daily functioning and cause the individual to withdraw from their responsibilities and relationships.
How do you stop obsessive thoughts?
Cognitive behavioral therapy (CBT) is one means of treatment by which you can stop obsessive thoughts. Through CBT, therapists focus on helping you to recognize negative thoughts and find new ways of responding to them. CBT helps you stand back from these thoughts, look at the evidence closely, and tell yourself something more realistic or accurate. You cannot simply stop obsessive thoughts, but you can change the way you interpret meaning from them and how you respond.
- OCD UK. Diagnostic and Statistical Manual of Mental Disorders and OCD. Accessed April 6, 2021.
- National Institute of Mental Health. Obsessive-Compulsive Disorder. Accessed April 6, 2021.
- Mayo Clinic. Obsessive-compulsive disorder. Accessed April 6, 2021.
Notes: This article was originally published July 9, 2021 and most recently updated January 21, 2022.
Screening for Obsessive-Compulsive Disorder (OCD)
If you suspect that you might suffer from obsessive-compulsive disorder, also known as OCD, answer the questions below, print out the results and share them with your health care professional. You can also download this form here.
All screening tools are downloadable from this website and no permission is required to reproduce, translate, display or distribute them.
To locate a specialist who treats OCD, visit the ADAA Find a Therapist.
This is a screening measure to help you determine whether you might have Obsessive-Compulsive Disorder (OCD) that needs professional attention. This screening tool is not designed to make a diagnosis of OCD but to be shared with your primary care physician or mental health professional to inform further conversations about diagnosis and treatment.
Are you troubled by the following?
| Yes No | Do you have unwanted ideas, images, or impulses that seem silly, nasty, or horrible? |
| Yes No | Do you worry excessively about dirt, germs, or chemicals? |
| Yes No | Are you constantly worried that something bad will happen because you forgot something important, like locking the door or turning off appliances? |
| Yes No | Do you experience shortness of breath? |
| Yes No | Are you afraid you will act or speak aggressively when you really don't want to? |
| Yes No | Are you always afraid you will lose something of importance? |
| Yes No | Do you ever experience “jelly” legs? |
| Yes No | Trouble falling or staying asleep, or restless and unsatisfying sleep |
| Yes No | Are there things you feel you must do excessively or thoughts you must think repeatedly to feel comfortable or ease anxiety? |
| Yes No | Do you wash yourself or things around you excessively? |
| Yes No | Do you have to check things over and over or repeat actions many times to be sure they are done properly? |
| Yes No | Do you avoid situations or people you worry about hurting by aggressive words or actions? |
| Yes No | Do you keep many useless things because you feel that you can’t throw them away? |
Having more than one illness at the same time can make it difficult to diagnose and treat the different conditions. Depression and substance abuse are among the conditions that occasionally complicate obsessive-compulsive disorder.
Depression and substance abuse are among the conditions that occasionally complicate obsessive-compulsive disorder.
| Yes No | Have you experienced changes in sleeping or eating habits? |
More days than not, do you feel...
| Yes No | sad or depressed |
| Yes No | disinterested in life |
| Yes No | worthless or guilty |
During the last year, has the use of alcohol or drugs...
| Yes No | resulted in your failure to fulfill responsibilities with work, school, or family? |
| Yes No | placed you in a dangerous situation, such as driving a car under the influence? |
| Yes No | gotten you arrested? |
| Yes No | continued despite causing problems for you or your loved ones? |
References:
Goodman, WK, Price LH, et al. The Yale-Brown Obsessive Compulsive Scale (Y-BOCS): Part 1. Development, use and reliability. Arch Gen Psychiatry. 46:1006-1011 (1989). Diagnostic and Statistical Manual of Mental Disorders (DSM IV), American Psychiatric Association, 1994, Washington, D.C.
The Yale-Brown Obsessive Compulsive Scale (Y-BOCS): Part 1. Development, use and reliability. Arch Gen Psychiatry. 46:1006-1011 (1989). Diagnostic and Statistical Manual of Mental Disorders (DSM IV), American Psychiatric Association, 1994, Washington, D.C.
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.

- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.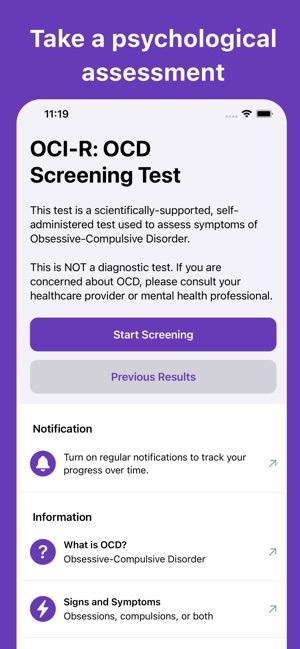
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- Persistent decline in quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, specialists of the Neuro-Psi clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future.