Relapse of schizophrenia symptoms
Schizophrenia Relapse: What to Know
Even with good management, most people with schizophrenia experience relapses over time. Recognizing and responding to symptoms can help prevent hospitalization.
By Chris Iliades, MDMedically Reviewed by Farrokh Sohrabi, MD
Reviewed:
Medically Reviewed
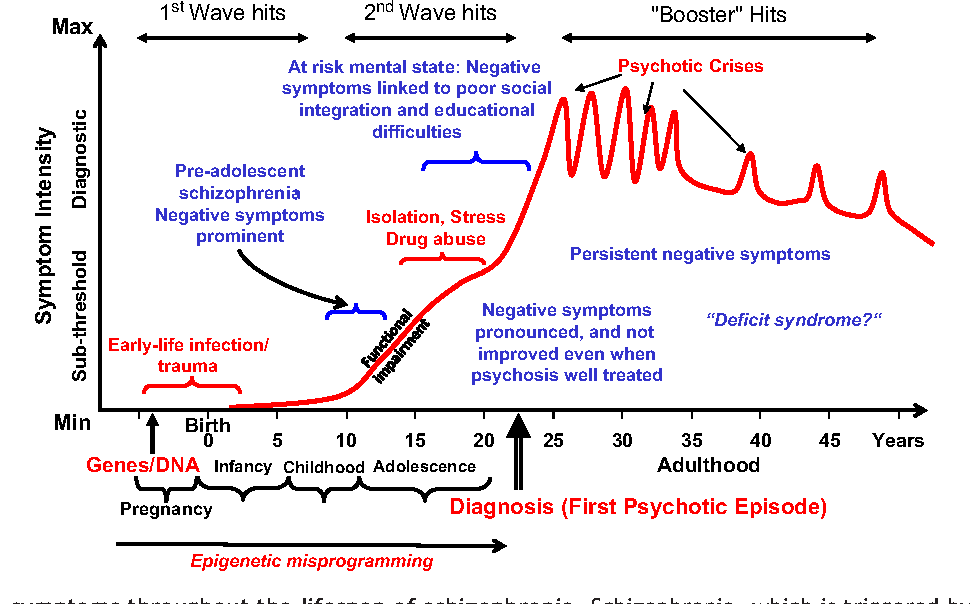
Schizophrenia is a mental illness that demands vigilance. Even with a good response to initial treatment, schizophrenia symptoms often return. A return or worsening of symptoms following a period of remission is called a relapse. The sooner the symptoms of a schizophrenia relapse are recognized, the greater the likelihood is of regaining control.
Only about 10 to 20 percent of people treated for schizophrenia don’t experience a relapse, according to a review published in the journal BMC Psychiatry in 2013. Most people with schizophrenia have multiple relapses over time.
“Complete remission of schizophrenia symptoms is uncommon," says Sophia Frangou, MD, PhD, a psychiatry professor at the Icahn School of Medicine at Mount Sinai Hospital in New York City. "Most people will experience a gradual recurrence of symptoms.”
Warning Signs of a Schizophrenia Relapse
Some schizophrenia relapses occur without warning, but when early signs are present, they're usually a return of symptoms that have occurred in the past.
Common warning signs of a schizophrenia relapse include insomnia, social withdrawal, difficulty concentrating, loss of interest, increasing paranoia, and hallucinations. Knowing these symptoms is important, but knowing the symptoms that are specific to each person with schizophrenia — called “relapse signatures” — is more important. Up to 70 percent of people with schizophrenia will experience these early symptoms before a full relapse sets in.
“These warning symptoms can be very specific," says Michael T. Compton, MD, MPH, chairman of psychiatry at Lenox Hill Hospital in New York City. "For one person, it may be insomnia or worries about the neighbors. For another person, it may be irritability or hearing whispers. " In fact, warning signs may be as specific as avoiding a certain food or color, Dr. Frangou says.
" In fact, warning signs may be as specific as avoiding a certain food or color, Dr. Frangou says.
That's why it's important to know the symptoms of previous episodes and to watch for them. "The first sign of a relapse is repeating symptoms of a previous episode,” Frangou says.
The first symptoms of schizophrenia onset may develop over months or years. Relapse tends to happen more quickly. According to the BMC Psychiatry review, the average time from return of symptoms to a full relapse is less than one month. Recognizing these symptoms early on can help immediate steps be taken to get proper treatment.
Common Causes of a Schizophrenia Relapse
Knowing the common causes of a schizophrenia relapse can tell you when to be on the lookout for a relapse of symptoms.
Not taking medication regularly or as prescribed is by far the most common cause of schizophrenia relapse. Persistent use of drugs or alcohol and criticism from caregivers are next on the list. "Many people with schizophrenia abuse some type of drug, most commonly marijuana," Frangou says.
"Many people with schizophrenia abuse some type of drug, most commonly marijuana," Frangou says.
Stress is particularly problematic. "Stress may contribute to schizophrenia relapse, but symptoms of relapse can also increase stress," she says.
First Steps to Take If a Schizophrenia Relapse Occurs
“You may not be able to prevent a schizophrenia relapse, but early recognition and treatment may prevent a hospital admission," Dr. Compton says. "The first thing to do is call the person’s doctor to find out if his or her medication needs to be adjusted or restarted." Other strategies include:
- Staying on medication
- Avoiding stress
- Avoiding drugs and alcohol
- Sleeping and eating well
- Not withdrawing from friends and loved ones
- Having a social support system
- Getting psychosocial treatments
Psychosocial treatments help people with schizophrenia and their families learn how to live with the condition. They include individual, group, or family education as well as counseling. “Increasing psychosocial treatments can be an important part of relapse prevention,” Compton says.
They include individual, group, or family education as well as counseling. “Increasing psychosocial treatments can be an important part of relapse prevention,” Compton says.
You may not always be able to prevent a schizophrenia relapse, but recognizing relapse symptoms and getting help early can help prevent a more severe episode.
By subscribing you agree to the Terms of Use and Privacy Policy.
What Is Online Therapy and Does It Work?
By Carmen ChaiWhat Is Teletherapy?
We cover what you can expect from teletherapy, including its effectiveness, how much it costs, and whether your insurance will cover it.
By Savannah Bacon
Best Online Therapy Services of 2023: Reviews and Pricing
Online therapy is a way to deliver and receive mental health services via the phone, messaging, or video sessions. Providers offer a variety of plans,...
Providers offer a variety of plans,...
By Nicole Gleichmann
The Road to Recovery: The Best Addiction Therapy Online
Online therapy can provide an accessible way to manage addictions. We reviewed platforms that have special features to support people with addictions ...
By Vanessa Ling
BetterHelp Reviews: Pricing and Plans in 2023
Looking for an affordable and accessible online counseling platform? BetterHelp is a convenient virtual therapy option for people who want to interact...
By Sara Lindberg
Our Review of Calmerry Online Therapy
Calmerry is an online therapy company that offers plans with unlimited messaging and live video therapy sessions. Every subscription includes access to...
Every subscription includes access to...
By Savannah Bacon
The Best Online Therapy for Anxiety in 2023
Online therapy helps people access mental health services from the comfort of their home. Here, we’ve reviewed the current best online therapy platforms...
By Sara Lindberg
Best Online Therapy for Teens in 2023
Our independently researched expert reviews can help you find the right online therapy program for your teenager.
By Jenny McCoy
The Waxing and Waning of Episodes
When symptoms of schizophrenia occur after being managed for some time, you may be experiencing a symptom relapse.
Schizophrenia can affect a person’s behaviors, cognition, mood, and how they connect with others.
While medication, psychotherapy, and learning about schizophrenia can help manage symptoms of the condition, it’s possible to experience “symptom relapses” while receiving treatment.
Symptom relapse is a part of the chronic condition journey, and it doesn’t mean you necessarily did “something wrong.”
The term “schizophrenia relapse” can be confusing, as “addiction relapse” tends to be more familiar.
A symptom relapse in schizophrenia refers to experiencing cognitive and positive symptoms that may have been well managed thus far, including:
- hallucinations
- delusions
- confusion
- difficulty concentrating
- difficulty with movement (catatonia)
When symptoms return, they can cause psychological and social distress, financial hardship, and difficulties with work, school, and relationships.
Symptom relapse can also affect loved ones who care for those living with schizophrenia due to the increased need for supervision when symptoms or behaviors become more unexpected, harmful, or difficult to manage.
Many people who live with schizophrenia experience relapses during their lifetime. Sometimes behaviors can precede relapse. One 2018 study found that behavioral changes detected 2 weeks before relapse was 71% higher than the rate of anomalies during other periods.
Nearly 3 in 5 folks with schizophrenia-spectrum disorders experienced symptom relapse during their lifetime after they began to take medication, according to a 2021 study. The research looked at people receiving follow-up for their condition at hospitals in Ethiopia.
Warning signs of a schizophrenia relapse may include symptoms experienced before treatment, such as:
- paranoia
- sleep difficulties
- changes in eating habits
- confused thinking
- loss of energy
- feelings of anxiety, depression, or anger
- lack of hygiene
- withdrawal from friends and family
- loss of interest in things once enjoyed (anhedonia)
- hallucinations
- delusions
Sometimes symptoms of psychosis can linger while receiving medication or other forms of medication, which can make it hard to define a true relapse, says Stephanie E.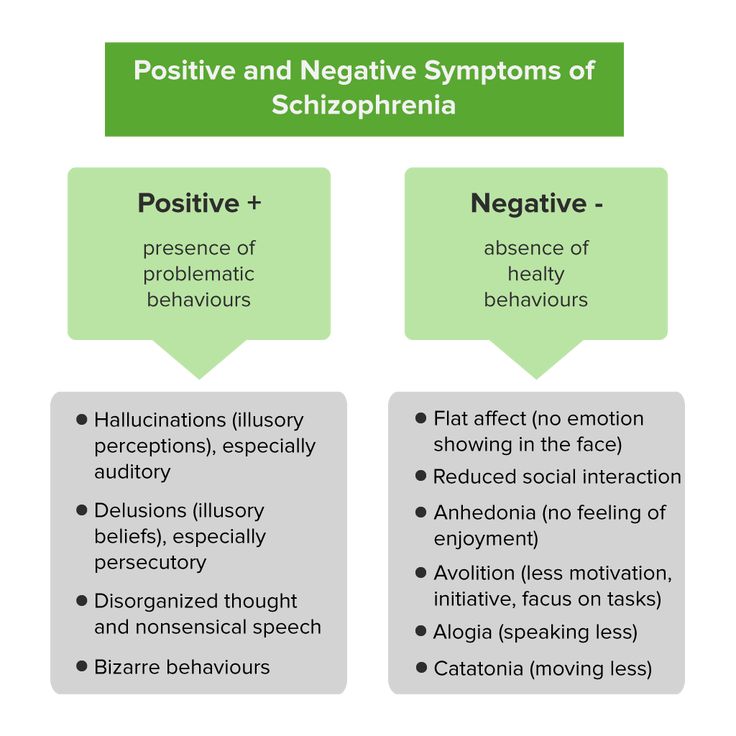 Johnson, a behavioral health consultant, life coach and owner of NaviPsych, in Atlanta, Georgia.
Johnson, a behavioral health consultant, life coach and owner of NaviPsych, in Atlanta, Georgia.
“However, it’s important for family members and individuals experiencing symptoms of psychosis or schizophrenia to keep their own records of symptoms that led to a hospitalization or treatment from a mental health professional at the time of an episode,” Johnson says.
“Receiving the best quality of treatment during a relapse depends heavily on what is reported to medical professionals by the family or the individual,” she adds.
Though prevention of individual episodes may be possible sometimes, preparing relapse contingency plans is wise.
Relapse can be associated with:
- having another mental health condition in addition to schizophrenia
- not taking medication as directed by a doctor
- stopping medication
- stressful life events
- substance use (including prescribed medications)
Effective ways to prevent relapse could include:
- seeing a doctor and psychiatrist regularly for all mental health symptoms
- taking medication as directed by your doctor
- managing stress as best as possible
- psychiatric service dogs for schizophrenia can also often alert owners of symptom onset or help when their person is triggered
You can listen to our podcasts on service dogs for schizophrenia below.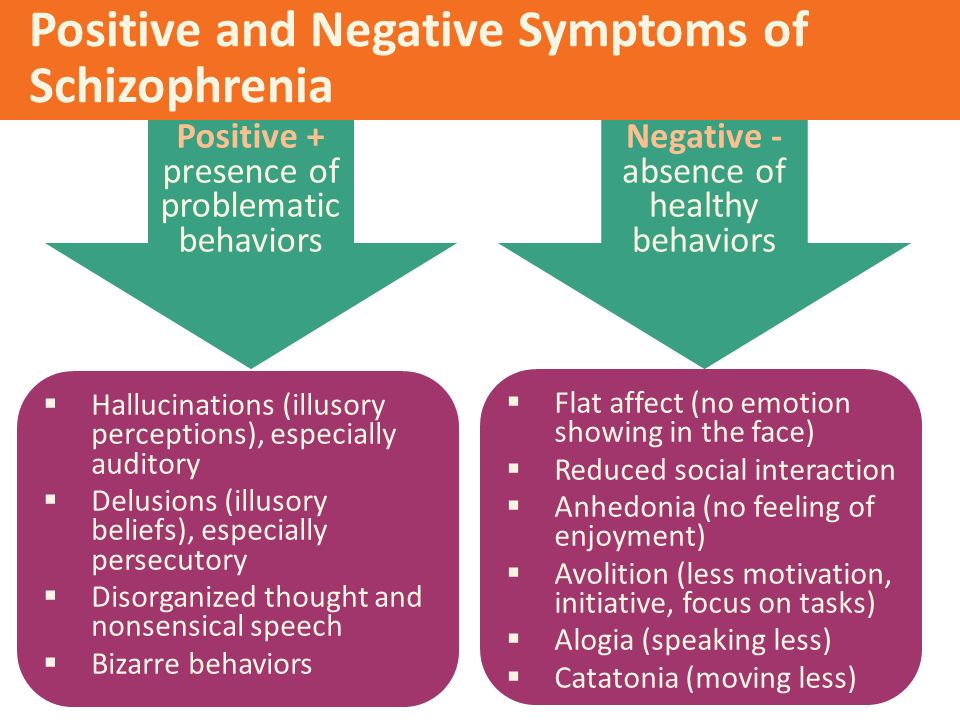
While it’s difficult to prevent symptom relapse after treatment has stopped, Johnson says a “key factor in reducing relapses is remaining engaged in a treatment regimen and reporting side effects from medications as soon as possible to the treating medical professional.”
She says giving a clinician the below information can help them determine the phase of illness:
- symptoms that occurred at the point of a symptom relapse
- time of year that the relapses tend to occur
- intensity of the symptoms
- worsening of symptoms
- appearance of new symptoms
- what’s happening in the person’s life at the time of the relapse
“A well-reported history can … also help doctors determine the most appropriate medications, the most appropriate dosage, as well as if an evaluation is needed to reassess for a change in diagnosis, when necessary,” says Johnson.
She also suggests creating a mental health crisis plan after a relapse and when you’re feeling symptoms are again being managed.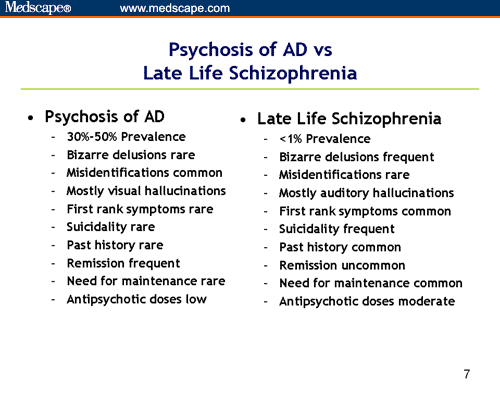
“After relapses occur, sometimes individuals can remember an order of events, certain symptoms that occurred first, the intensity and frequency of the symptoms that let him or her know symptoms were returning,” Johnson says.
She adds that these symptoms or mood journal details are “valuable information to consider when planning the level of care a person may need.”
Planning is also helpful when creating a behavioral health advance directive, which defines a person’s wishes for healthcare and treatment to be carried out if they are incapacitated or unable to communicate their wishes.
“Clear communication, especially written documents, are essential to receiving the most appropriate quality medical care during a relapse,” says Johnson.
When a relapse occurs, it’s wise to contact a mental health professional immediately. Family, partners, or caregivers can be helpful by providing as much information as possible. Johnson suggests supplying doctors with what you know about your person and being ready to ask questions about their care.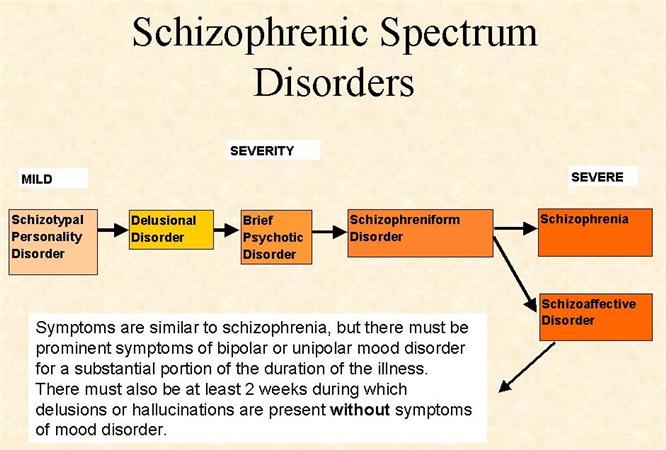
“Families should ask the treating mental health professionals specific questions about the procedures of different levels of care and what to expect at each level. The more information known about the procedures, the easier navigating to receive help can be,” she says.
For more information about schizophrenia, you can bookmark our hub.
Maintenance treatment with antipsychotics for schizophrenia
Antipsychotics are the mainstay of treatment for schizophrenia, not only in acute attacks, but also in long-term treatment. People may want to stop treatment at some point in their treatment. Relapses of psychotic symptoms are known to occur after discontinuation of treatment. Relapse can lead to risk of harm, loss of autonomy, and significant distress for patients and their families.
This report is an update of a systematic review previously published in 2012 based on 75 randomized controlled trials (RCTs) published over a long period since the 1950s, involving more than 9000 participants. The effects of all antipsychotics are compared here with the placebo effect - discontinuation of medication - in maintenance treatment, i.e. relapse prevention. The goal is to explore the benefits and risks of each of the two options. nine0003
The effects of all antipsychotics are compared here with the placebo effect - discontinuation of medication - in maintenance treatment, i.e. relapse prevention. The goal is to explore the benefits and risks of each of the two options. nine0003
The results of this review show that antipsychotics are effective in reducing relapses and the need for hospitalization. Indeed, if treatment is stopped, the risk of relapse within one year is almost three times higher. It appears that antipsychotic medications have a positive effect on the ability to participate in various activities and relationships, as well as the possibility of achieving remission (no symptoms), although there is less evidence in this regard. Based on fewer reports, people who continue treatment tend to experience higher life satisfaction, confirming the negative well-being effects associated with a higher risk of relapse. In contrast, antipsychotics, as a group of drugs, are associated with a number of side effects such as movement disorders, weight gain, and drowsiness.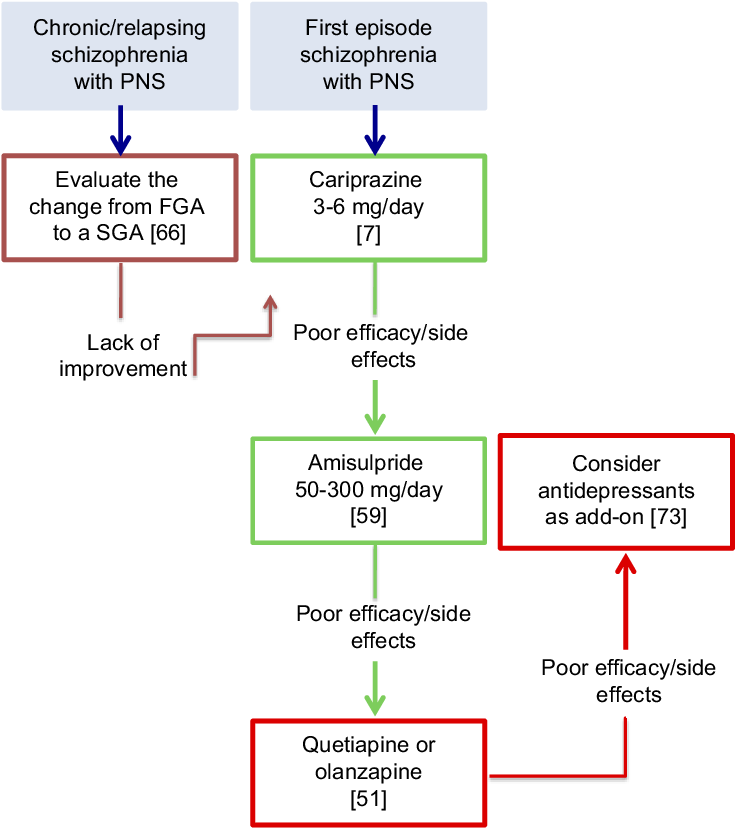 However, this review provides a better understanding of the fact that discontinuing treatment is more harmful than deliberately continuing it. nine0003
However, this review provides a better understanding of the fact that discontinuing treatment is more harmful than deliberately continuing it. nine0003
Unfortunately, the studies included in this review typically lasted less than one year, making it difficult to ascertain the long-term effect of this treatment. However, it is also true that the longer a study lasts, the more likely it is that other factors - such as environmental factors - can accumulate and complicate the interpretation of the results. First of all, this review confirms the benefits of antipsychotics in various study participants. Therefore, the best strategy would be to continue antipsychotic treatment, eventually discussing and adapting it if any adverse effects occur. nine0003
Translation notes:
Translation: Minin Anton Viktorovich. Editing: Yudina Ekaterina Viktorovna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic.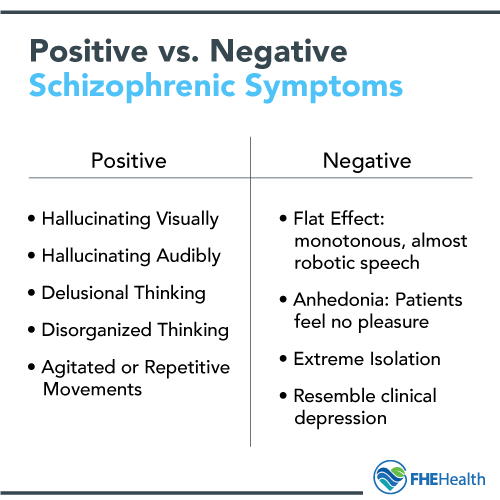 For questions related to this translation, please contact us at: [email protected];
For questions related to this translation, please contact us at: [email protected];
Subacute episode patients
In this section
Characteristics
Patients with subacute schizophrenia are patients in whom the disease has passed from the acute to the subacute phase due to the regression of symptoms (total score on the PANSS scale corresponds to the range of 50-75 points, i.e. moderately severe disease) 1 . Delusions, hallucinations, disorganization of thinking and (or) formal thought disorders expressed in the acute phase are observed in a milder form 2 . At the same time, negative symptoms, cognitive impairment, and social maladjustment may become more pronounced, indicating continued dysfunction 2 . Typically, these patients are hospitalized, but can also be treated on an outpatient basis 2 . Patients in the subacute phase tend to become more aware of their disease due to symptomatic remission; however, increasing criticism towards the state after completion of the acute phase potentially increases the risk of suicide 2 .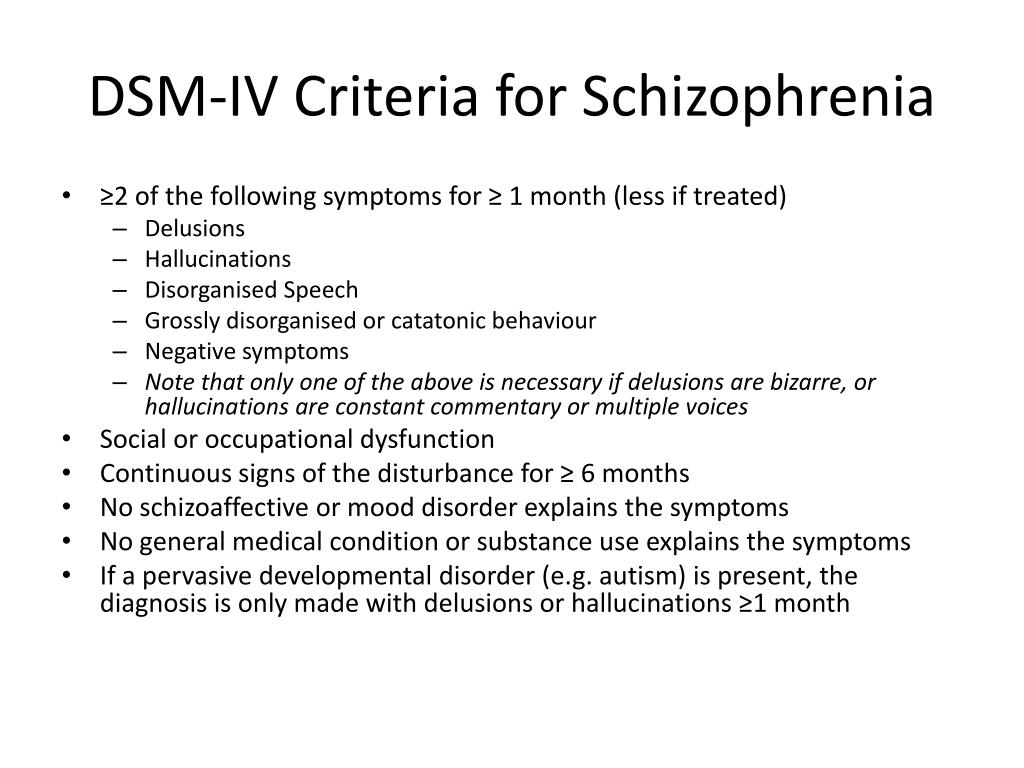
Treatment
The main goals of treatment in the subacute phase are to maintain symptomatic remission, reduce the likelihood of relapse for as long as possible, and promote the patient's social adaptation and overall recovery 2 .
Research has shown that relapses in schizophrenia are common, and the more relapses a patient has, the worse the prognosis: each relapse leads to worsening of symptoms, cognitive impairment, reduced social functioning and poor quality of life 3 . Thus, relapse prevention is critical in the treatment of schizophrenia 3 , and patients in the subacute phase need additional support to live a full life and function successfully in society 2 . Patients who are on inpatient treatment, it is advisable to make an appointment with a district psychiatrist before discharge from the hospital 2 . Adaptation to life in society should be gradual, because high expectations can cause stress and anxiety, which increases the risk of relapse 2 .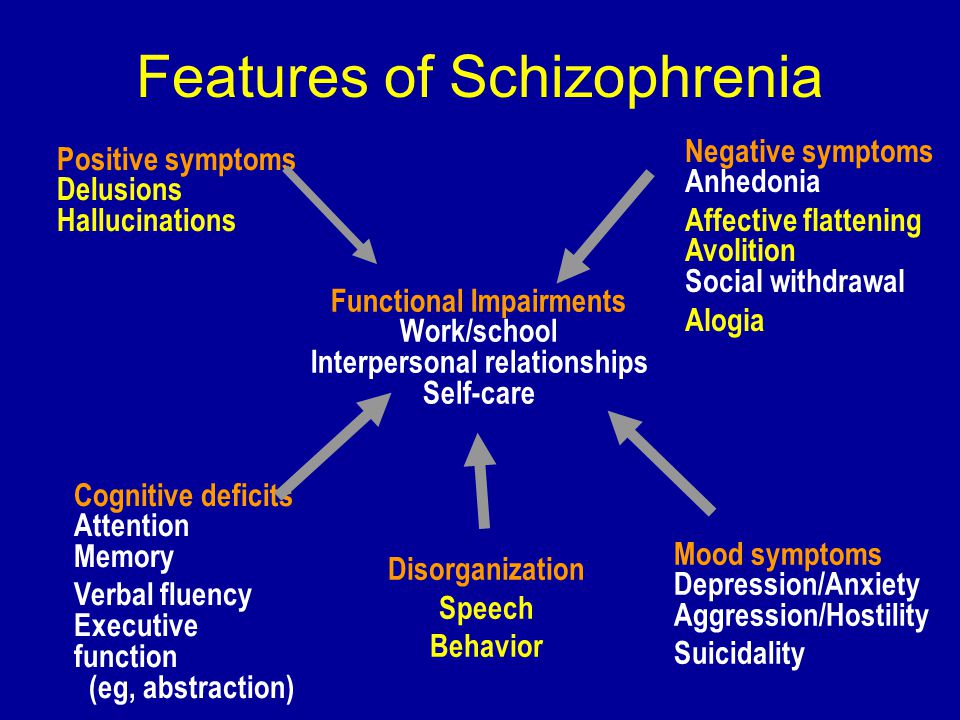
Patients in the subacute phase should continue treatment with atypical antipsychotics to manage persistent positive symptoms, as too rapid dose reduction or discontinuation of therapy may cause symptoms to worsen, recur or even recur 2 . Moreover, more careful monitoring of the side effects of antipsychotics should be ensured and pharmacotherapy adjusted accordingly, otherwise patients may cease to comply with the drug regimen, which will increase the risk of relapse 2 .
Physicians should continue to interact with the patient's relatives and educate them on how to manage schizophrenia, especially in the context of current or planned hospital discharge 2 . Given the high risk of relapse in the subacute phase, patients and their families should be educated to recognize and treat early signs of relapse 2 .
As the patient stabilizes, re-evaluate the need for prolongation of adjuvant therapy (eg, benzodiazepines that may have been given to treat agitation in the acute phase) 2 .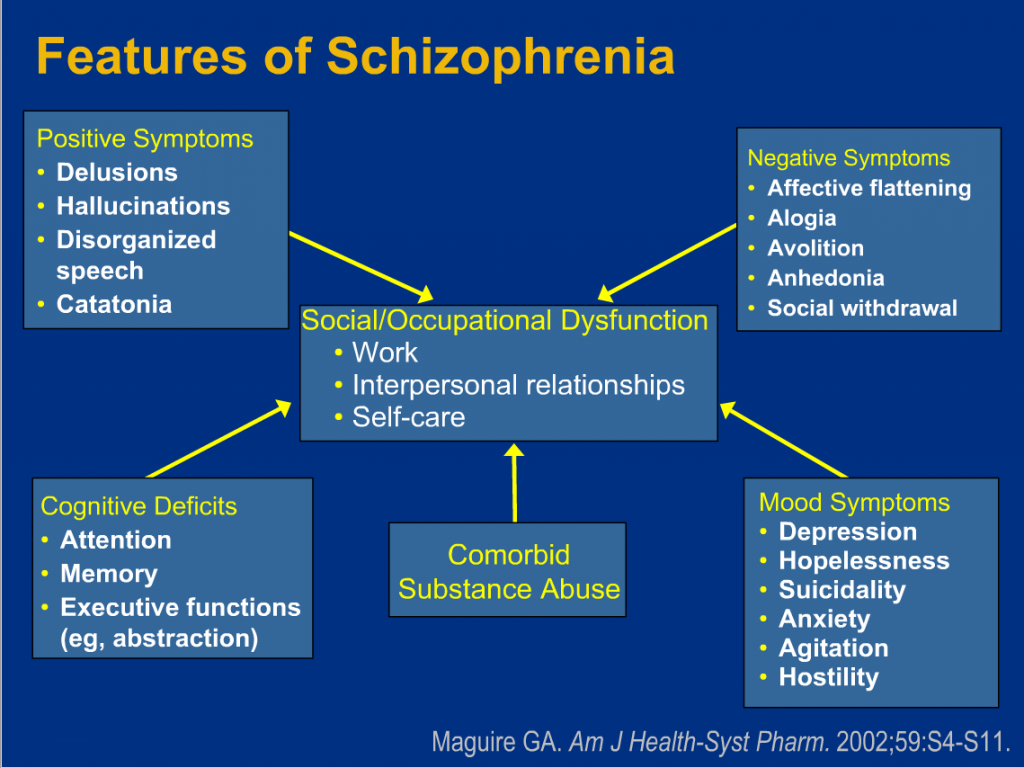 However, comorbidities such as depression or obsessive-compulsive disorder require appropriate medications 2 .
However, comorbidities such as depression or obsessive-compulsive disorder require appropriate medications 2 .
Place of cariprazine in relief of negative symptoms
In the period of decrease in the severity of positive symptoms, it is important to analyze the severity of negative symptoms 2 . If negative symptoms develop or worsen, it may be reasonable to switch the patient to cariprazine if they are receiving another drug, as caripazine is the only neuroleptic that is superior to another antipsychotic (risperidone) in the treatment of negative symptoms 4 .
Significantly greater improvement in 5 out of 7 PANSS 9 negative symptom scores with cariprazine0027 5 .
Patients in the subacute phase treated with cariprazine relapsed significantly later than participants in the placebo group (326 days versus 92 days, respectively) 6 .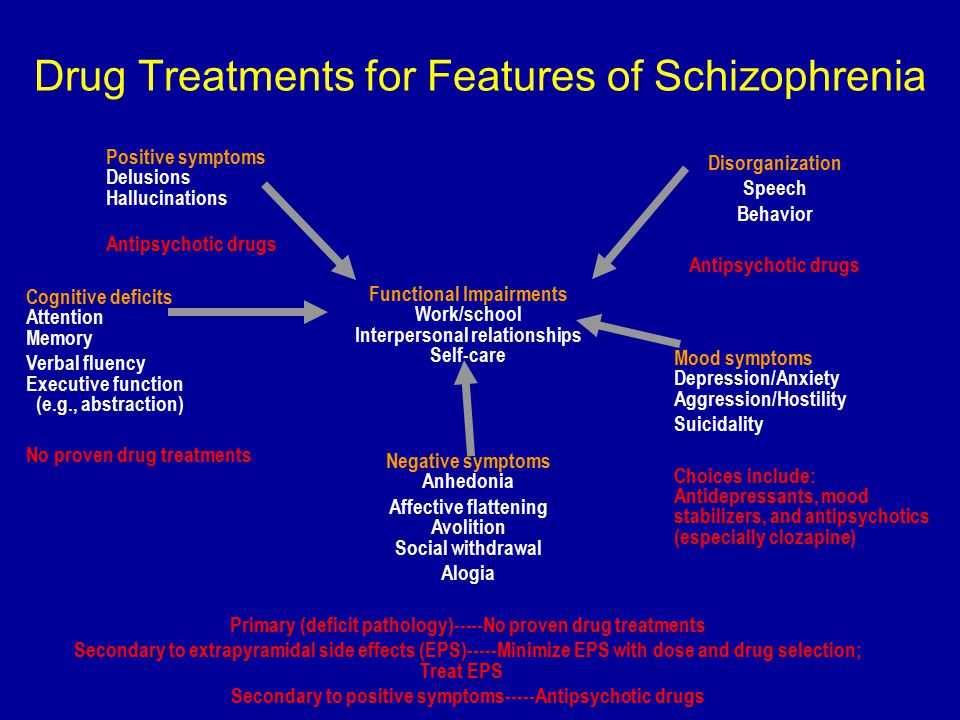
In terms of preventing relapse of schizophrenia, long-term treatment with cariprazine was statistically significantly more effective than placebo, with relapse rates of 21.6% and 49%, respectively 6 .
Treatment with cariprazine in patients with subacute symptoms of schizophrenia was statistically significantly more effective than placebo in terms of long-term relapse prevention 8 .
The use of cariprazine was associated with a statistically significant increase in the duration of sustained remission and an increase in the likelihood of maintaining remission for at least 6 consecutive months compared with placebo 8 .
The results of the study confirmed that in patients treated with cariprazine (at a dose of 3–9 mg/day), the time to relapse was statistically significantly longer and the rate of relapse was lower than in patients treated with placebo (24, 8% vs. 47.5%) 3 . Specifically, the 25th percentile time to relapse was 92 days in the placebo group and 224 days in the cariprazine group 3 .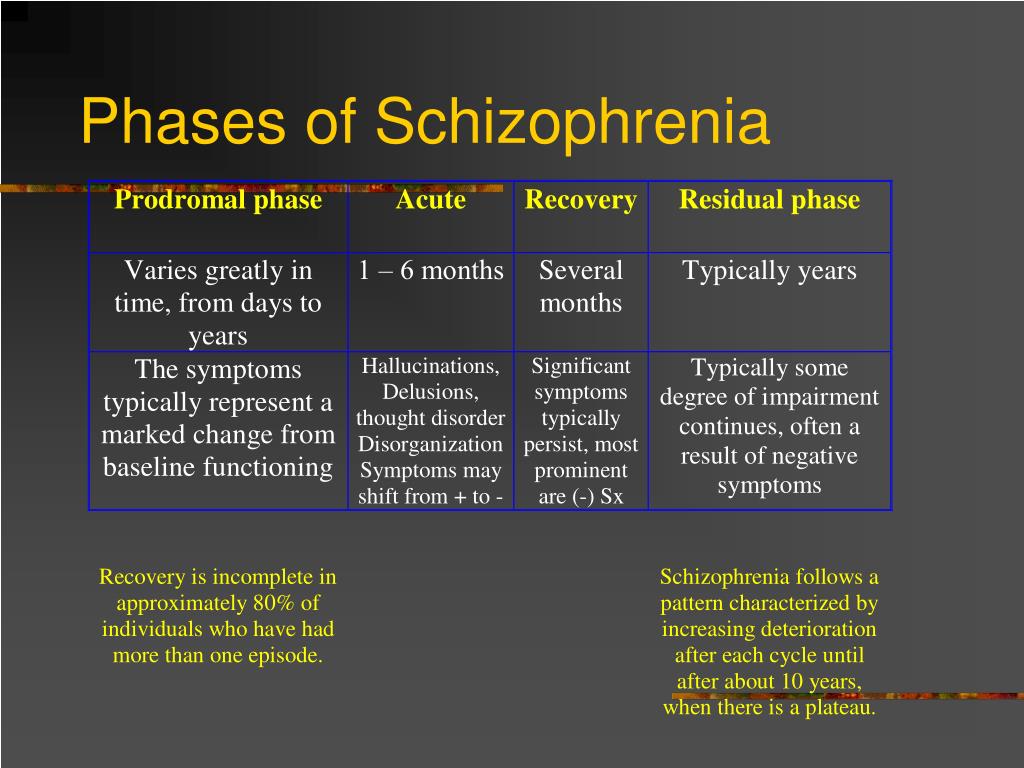 Therefore, treatment with cariprazine can delay or prevent the recurrence of schizophrenia 3 .
Therefore, treatment with cariprazine can delay or prevent the recurrence of schizophrenia 3 .
In patients who are not fully compliant and miss antipsychotics, cariprazine may be an excellent choice due to its long half-life 3 .
Furthermore, cariprazine has been found to be superior to risperidone in terms of improved functioning of daily living 5 .
Dosing regimen
In the acute phase of the disease, the dose of cariprazine was increased rapidly (by 1.5 mg every day or every other day). After stabilization and transition to a subacute state, the dose remained constant 3 .
Instructions for medical use of Reagila® RU: LP-005405 dated 03/18/2019. The instructions can be found on the website: www.grls.rosminzdrav.ru.
Instructions for medical use of Reagila® RU: LP-005405 dated 03/18/2019. The instructions can be found on the website: www.grls.rosminzdrav.ru.
References:
- Leucht, S.
 et al. What does the PANSS mean? Schizophr. Res. 79, 231–238 (2005).
et al. What does the PANSS mean? Schizophr. Res. 79, 231–238 (2005). - Lehman, A. F. et al. Practice Guideline for the Treatment of Patients with Schizophrenia Second Edition. American Psychiatric Association (The Authors, 2004). doi:10.1016/j.schres.2016.06.030.
- Durgam, S. et al. Long-term cariprazine treatment for the prevention of relapse in patients with schizophrenia: A randomized, double-blind, placebo-controlled trial. Schizophr. Res. 176, 264–271 (2016). nine0131
- Németh, G. et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomised, double-blind, controlled trial. Lancet 389, 1103–1113 (2017).
- Fleischhacker, W. et al. The efficacy of cariprazine in negative symptoms of schizophrenia: Post hoc analyzes of PANSS individual items and PANSS-derived factors. Eur. Psychiatry 58, 1–9 (2019).
- Reagila Summary of Product Characteristics.
Learn more