Ptsd differential diagnosis
Is It PSTD or Something Else?
PTSD Differential Diagnosis: Is It PSTD or Something Else?- Conditions
- Featured
- Addictions
- Anxiety Disorder
- ADHD
- Bipolar Disorder
- Depression
- PTSD
- Schizophrenia
- Articles
- Adjustment Disorder
- Agoraphobia
- Borderline Personality Disorder
- Childhood ADHD
- Dissociative Identity Disorder
- Narcissistic Personality Disorder
- Narcolepsy
- Oppositional Defiant Disorder
- Panic Attack
- Postpartum Depression
- Schizoaffective Disorder
- Seasonal Affective Disorder
- Sex Addiction
- Specific Phobias
- Teenage Depression
- Trauma
- Featured
- Discover
- Wellness Topics
- Black Mental Health
- Grief
- Emotional Health
- Sex & Relationships
- Trauma
- Understanding Therapy
- Workplace Mental Health
- Original Series
- My Life with OCD
- Caregivers Chronicles
- Empathy at Work
- Sex, Love & All of the Above
- Parent Central
- Mindful Moment
- News & Events
- Mental Health News
- COVID-19
- Live Town Hall: Mental Health in Focus
- Podcasts
- Inside Mental Health
- Inside Schizophrenia
- Inside Bipolar
- Wellness Topics
- Quizzes
- Conditions
- ADHD Symptoms Quiz
- Anxiety Symptoms Quiz
- Autism Quiz: Family & Friends
- Autism Symptoms Quiz
- Bipolar Disorder Quiz
- Borderline Personality Test
- Childhood ADHD Quiz
- Depression Symptoms Quiz
- Eating Disorder Quiz
- Narcissim Symptoms Test
- OCD Symptoms Quiz
- Psychopathy Test
- PTSD Symptoms Quiz
- Schizophrenia Quiz
- Lifestyle
- Attachment Style Quiz
- Career Test
- Do I Need Therapy Quiz?
- Domestic Violence Screening Quiz
- Emotional Type Quiz
- Loneliness Quiz
- Parenting Style Quiz
- Personality Test
- Relationship Quiz
- Stress Test
- What's Your Sleep Like?
- Conditions
- Resources
- Treatment & Support
- Find Support
- Suicide Prevention
- Drugs & Medications
- Find a Therapist
- Treatment & Support
Medically reviewed by Ashleigh Golden, PsyD — By Brittany VanDerBill — Updated on June 23, 2021
If you’re not sure whether your symptoms are due to PTSD or something else, it may be worth asking your doctor or therapist about differential diagnoses (conditions with similar symptoms).
Going through a jarring or traumatic event isn’t easy. Afterward, you may find it difficult to put the experience behind you. You might continue to feel unusually anxious long after this difficult or traumatizing situation has passed.
A traumatic experience can sometimes lead to post-traumatic stress disorder (PTSD), though not all trauma leads to PTSD. And many other conditions have overlapping symptoms with PTSD, which can make getting an accurate diagnosis more complex.
Having some anxiety or additional worries is natural after something bad happens. But when do your symptoms signal PTSD? And could they be a sign of something other than PTSD?
The condition we know as post-traumatic stress disorder was once used almost exclusively to describe the symptoms of veterans who had experienced combat during war. But in these instances, the condition was referred to as “shell shock.” Today, modern research has helped us understand that PTSD can arise from other trauma, too.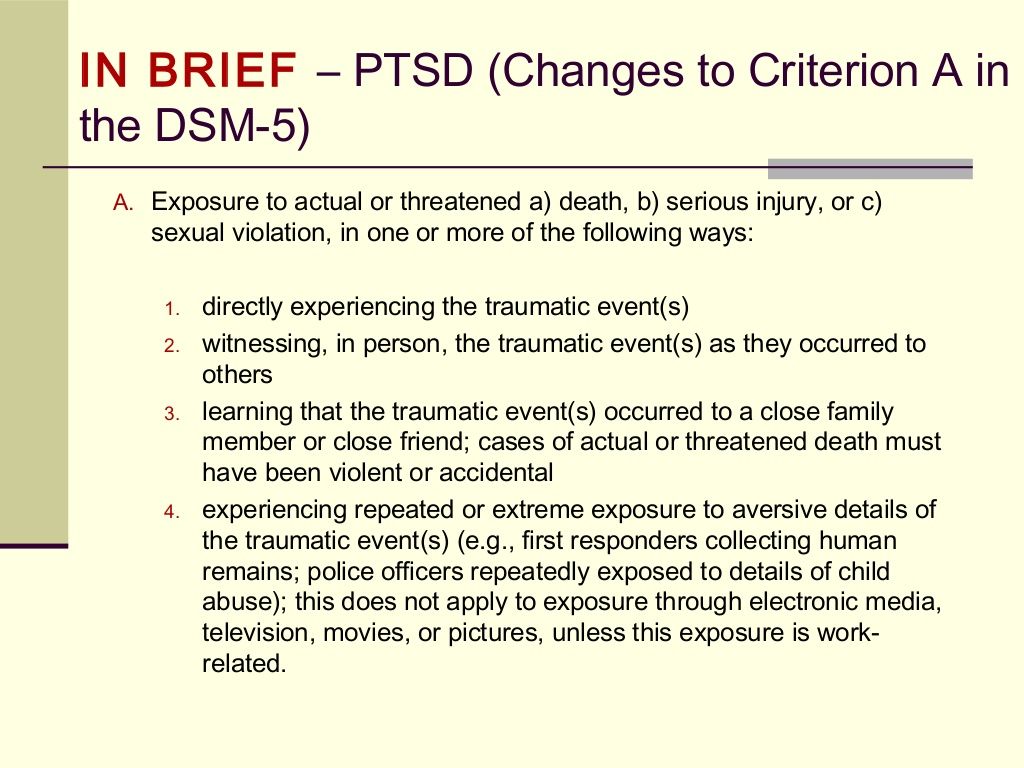
The American Psychological Association notes that PTSD is considered to be an anxiety issue related to a traumatic occurrence.
The Diagnostic and Statistical Manual for Mental Disorders (DSM-5) definition of trauma requires “actual or threatened death, serious injury, or sexual violence.” Examples of trauma can include combat experience, abuse or assault, or surviving a natural disaster.
Some symptoms of PTSD can include:
- vivid and unwanted memories of the traumatic event
- staying away from anything related to the event or where it took place
- shame or guilt about what happened
- changes in mood
- anger or rage
- causing harm to oneself
It’s important to note that not everyone who goes through a traumatic event has PTSD. Additionally, you may discover that you have PTSD along with another condition.
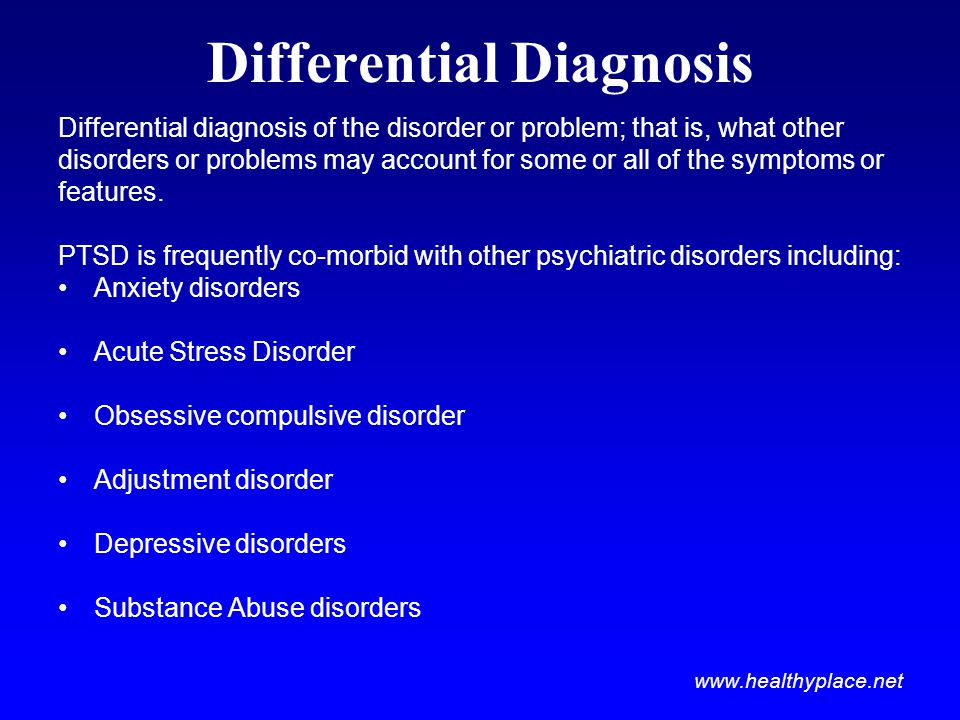
A differential diagnosis is when a doctor works out which disorder someone has when several disorders have overlapping symptoms.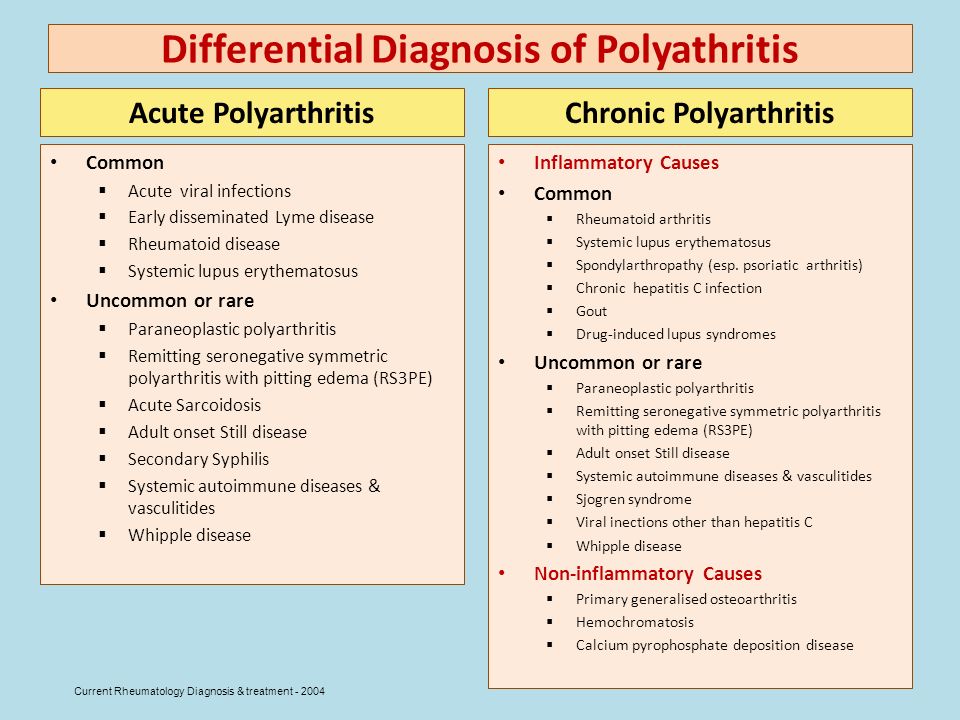
Receiving an accurate diagnosis is often an important first step toward finding the treatments, coping methods, and support networks that will help you heal. Talking with a doctor or therapist about your symptoms and experiences will help you find the right diagnosis and treatment plan for you.
It’s important not to attempt your own differential diagnosis at home — only licensed mental health professionals, like counselors, therapists, clinical social workers, psychologists, and psychiatrists — can make this assessment.
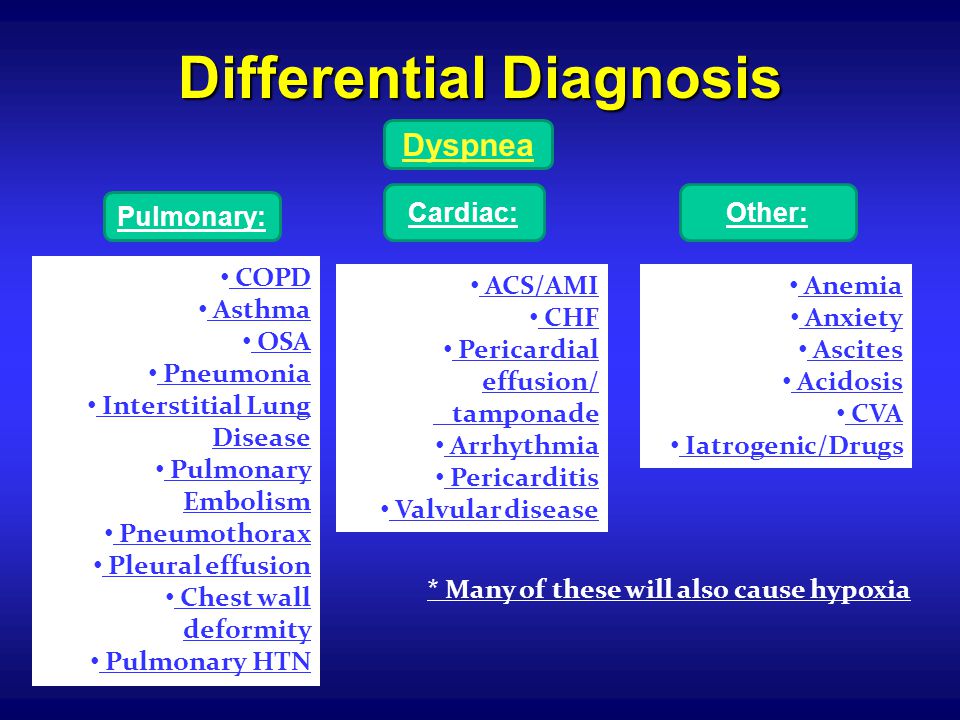
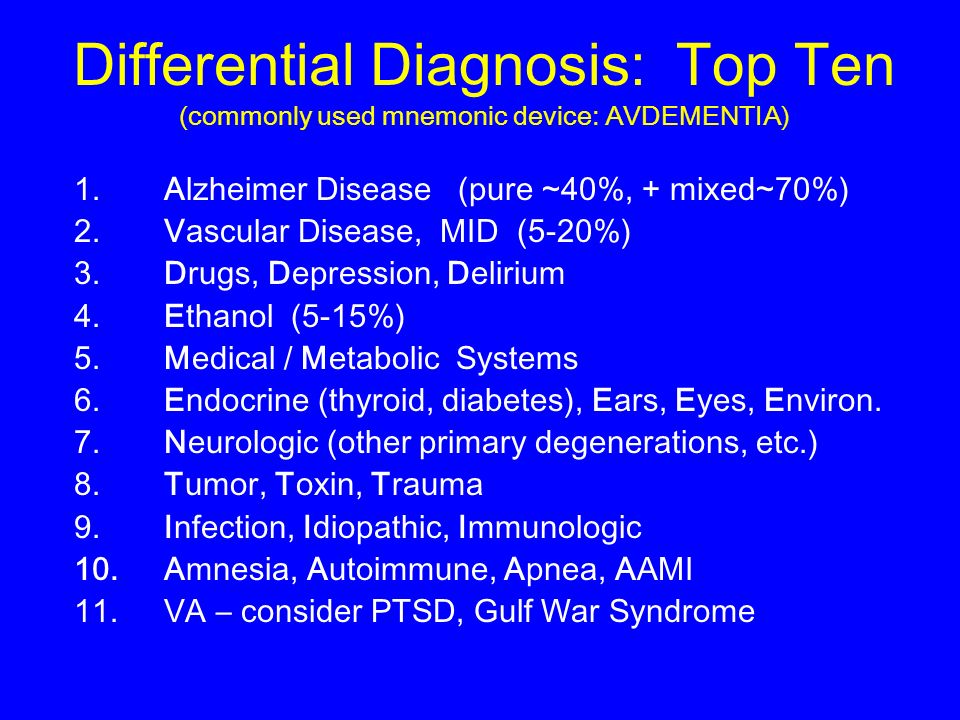
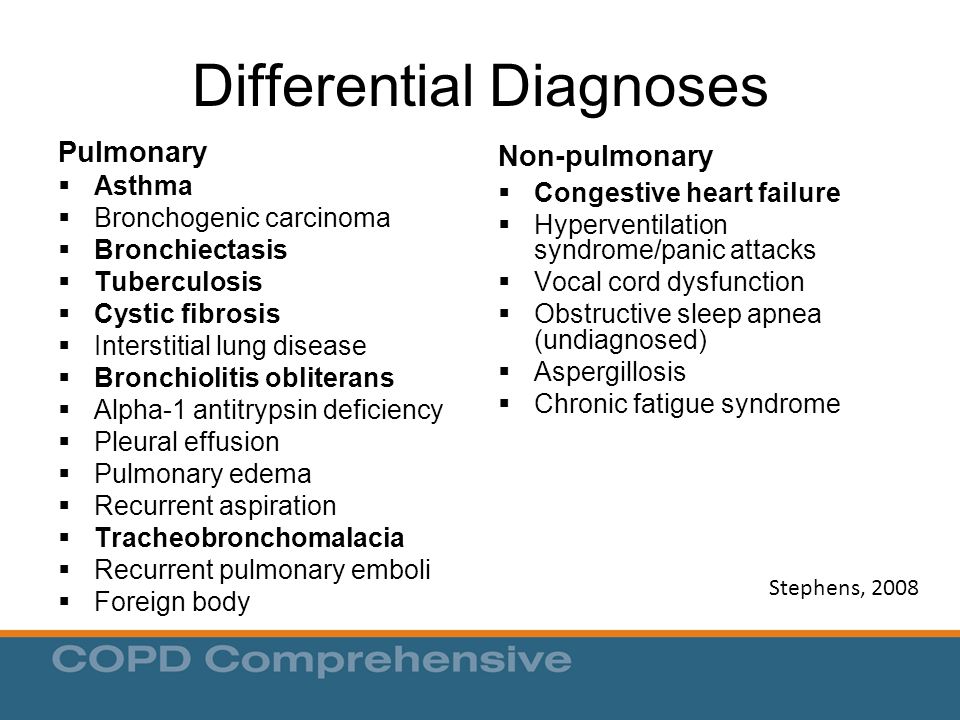
The following conditions share some similarities with PTSD:
- acute stress disorder
- complex PTSD
- dissociative disorders
- adjustment disorder
- generalized anxiety disorder
- depression
- panic disorder
- phobias
- substance use disorders
We look at some of these conditions in more detail below.
Acute stress disorder
This disorder has some highly similar symptoms to PTSD. The main factor that is considered in a PTSD differential diagnosis in this instance is how long you’ve experienced your symptoms. Generally speaking, PTSD requires symptoms to last for at least one month.
The main factor that is considered in a PTSD differential diagnosis in this instance is how long you’ve experienced your symptoms. Generally speaking, PTSD requires symptoms to last for at least one month.
Complex PTSD
Complex PTSD has similar symptoms to PTSD, but the cause is different. While PTSD is usually linked with a single event, complex PTSD develops after repeated exposure to traumatic events, such as childhood neglect or abuse within a relationship.
Complex PTSD is not listed in the DSM-5, but many therapists recognize and treat its symptoms.
Dissociative disorders
Dissociation is one way the body deals with traumatic experiences. When you experience trauma, you might feel a disconnect between your mind and body. This helps give you some distance from the traumatic event.
While dissociation has a useful function in the moment, people with PTSD may notice that dissociation occurs again later on, and it can interrupt their daily lives. For example, someone with PTSD might feel as though they are detached from reality during a flashback.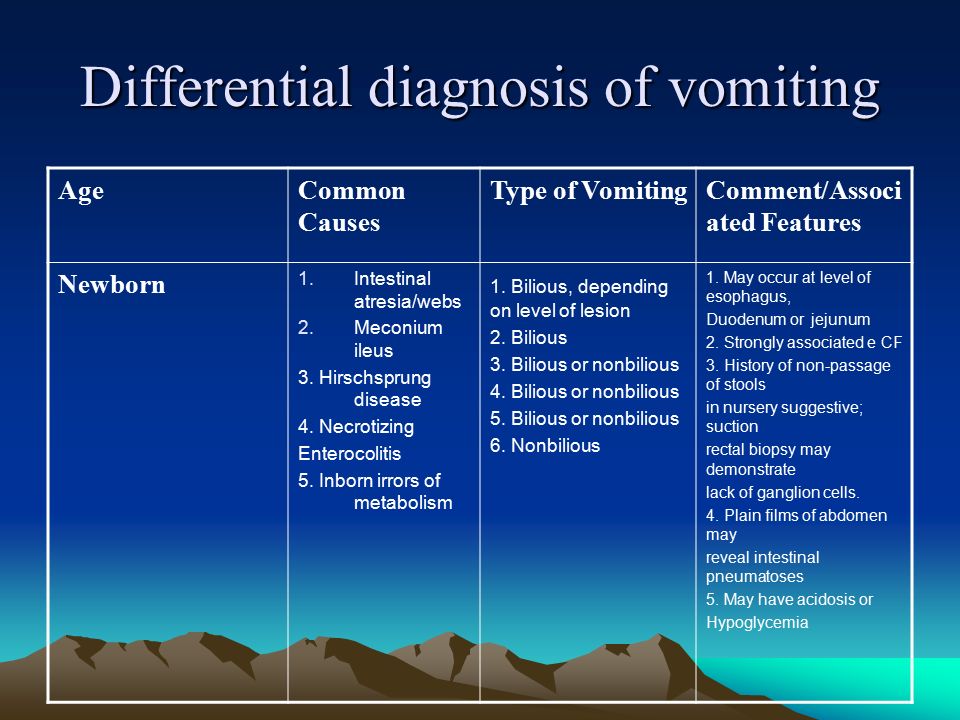
A variety of dissociative disorders exist, and they often share some common symptoms. These include:
- dissociative identity disorder
- depersonalization/derealization disorder
- dissociative amnesia
The causes of dissociative disorders are often rooted in past traumas, so they are closely linked with PTSD. There’s also a subtype of PTSD that is a form of dissociative disorder. It’s important to reach out for professional help to distinguish which condition may be impacting you.
Generalized anxiety disorder
One reason that PTSD can be confused with generalized anxiety disorder is the intense anxiety you experience with both conditions. Intrusive thoughts and a tendency to feel angry or on edge are also fairly common with both.
People with generalized anxiety disorder have a history of anxiety across a wide range of circumstances, whereas people with PTSD often experience anxiety in response to a major trauma.
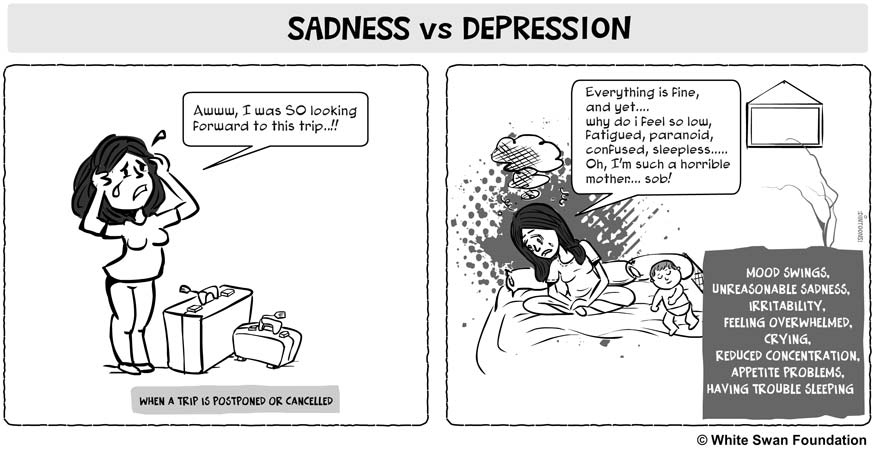
Depression
Sometimes, the symptoms of depression and PTSD can look and feel alike.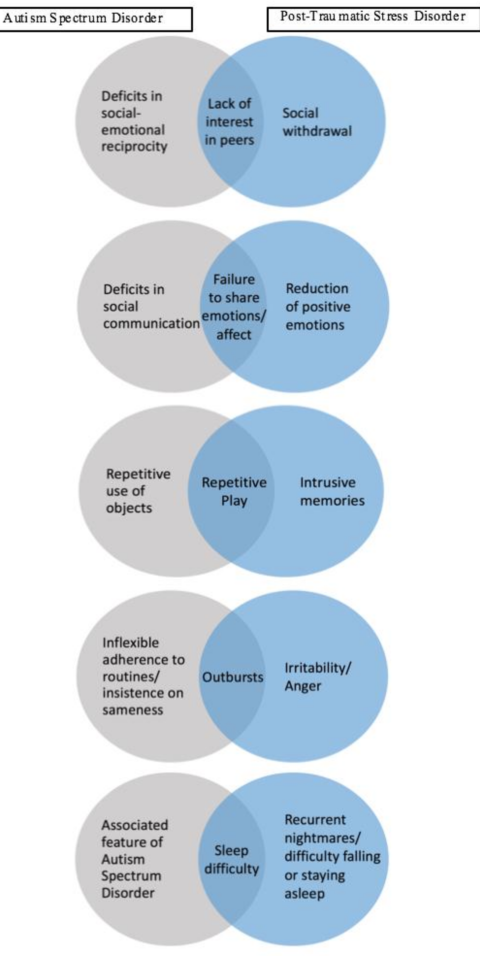 People with depression may feel hopeless, or they may feel intense amounts of shame and guilt. People with PTSD also tend to experience this extreme shame, but it’s primarily focused on the event that occurred.
People with depression may feel hopeless, or they may feel intense amounts of shame and guilt. People with PTSD also tend to experience this extreme shame, but it’s primarily focused on the event that occurred.
Panic disorder
Someone with panic disorder may experience intense feelings of anxiety. This can be related to a specific object or situation. In these cases, you might avoid that specific thing to prevent a panic attack from occurring. A person who experienced trauma may avoid certain situations as well, so these two conditions can feel quite similar in this way.
Substance use disorder
When a person has a substance use disorder, they may experience a few symptoms in common with PTSD. For instance, substance use disorders could cause high anxiety or feelings of being on edge. They could also bring changes in mood and habits, just like with PTSD.
A differential diagnosis can be helpful in distinguishing between PTSD and something else. However, it is possible that you may have both PTSD and another condition with similar characteristics.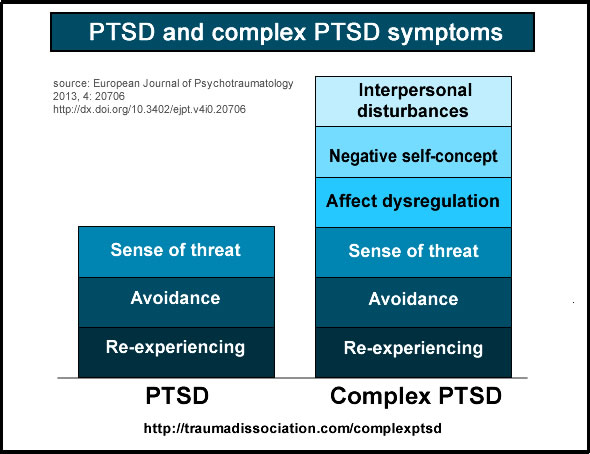
When this happens, it’s referred to as comorbidity.
Substance use disorder is a particularly common comorbidity. The PTSD Alliance reports that more than 7 million people in the United States have PTSD. Of those people, they note that as many as 40% also experience addiction.
Further, researchers estimate that almost 52% of males experiencing PTSD have a substance use disorder.
If you’re living with PTSD and substance use disorder or other conditions, don’t lose hope. Many resources exist for people experiencing these conditions.
You may want to begin by seeking help from your primary care physician. They can provide referrals to additional resources where necessary. If you already have a trusted counselor or psychiatrist, they would be a safe and helpful person to reach out to.
It’s important to be honest and open about all of your symptoms when speaking with any mental health professional you work with. This includes symptoms related to PTSD and those that could be related to other conditions, such as panic disorder or depression. Doing so ensures that you will receive the help that you need to start healing.
Doing so ensures that you will receive the help that you need to start healing.
There are various evidence-based treatments for PTSD, including:
- Cognitive behavioral therapy (CBT). CBT helps people challenge the patterns of behaviors, feelings, and thoughts that are causing distress.
- Cognitive processing therapy (CPT). CPT helps people modify and challenge unhelpful trauma-related beliefs.
- Prolonged exposure therapy. This type of CBT teaches people to gradually approach memories, feelings, and places related to the trauma to learn that they aren’t dangerous.
Suicide prevention
If you or someone you know is considering suicide, you’re not alone. Help is available right now:
- Call the National Suicide Prevention Lifeline 24 hours a day at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.
- Call the Veterans Crisis Line 24 hours a day at 800-273-8255
Not in the U. S.? Find a helpline in your country with Befrienders Worldwide.
S.? Find a helpline in your country with Befrienders Worldwide.
The important thing to remember with PTSD is that there is hope. Millions of other people are also going through PTSD. Many more are also experiencing other conditions as well.
Knowing that you aren’t alone can help give you the courage to reach out and ask for some help. Contact your primary care physician or, if you know of one already, a mental health professional. They will have the training to help you with your PTSD and other conditions. They also can refer you to other professionals who can provide further assistance as needed.
If you’re unsure how to ask someone for help, this guide will assist you in finding the words to begin your path to healing. You might also find that podcasts can be helpful on this journey. While not a substitute for treatment, they may help you feel less alone or more supported on your path to wellness.
Getting help for PTSD is important for healing, and by taking the time to read this article, you’re taking those first steps toward healing.
Last medically reviewed on June 23, 2021
6 sourcescollapsed
- CSTS uniformed services university. (n.d.).
cstsonline.org/assets/media/documents/CSTS_CTC_Asking_for_Help_Do_You_Know_How.pdf - Mann SK, et al. (2021). Posttraumatic stress disorder.
ncbi.nlm.nih.gov/books/NBK559129/ - Pai A, et al. (2017). Posttraumatic stress disorder in the DSM-5: Controversy, change, and conceptual considerations.
ncbi.nlm.nih.gov/pmc/articles/PMC5371751/ - Post-traumatic stress disorder. (n.d.).
apa.org/topics/ptsd - PTSD treatments. (2020).
apa.org/ptsd-guideline/treatments - van Huijstee J, et al. (2018). The dissociative subtype of post-traumatic stress disorder: Research update on clinical and neurobiological features.
pubmed.ncbi.nlm.nih.gov/29063485/
FEEDBACK:
Medically reviewed by Ashleigh Golden, PsyD — By Brittany VanDerBill — Updated on June 23, 2021
Read this next
What Are the Symptoms of PTSD?
Medically reviewed by Karin Gepp, PsyD
How do you know if you have PTSD? There's a long list of symptoms and diagnostic criteria.
 Here's what you need to know.
Here's what you need to know.READ MORE
Can You Recover from Trauma? 5 Therapy Options
Trauma-informed therapy can help you reduce the emotional and mental effects of trauma. Here are the best options for trauma-focused treatments.
READ MORE
Podcast: There’s More to Trauma than PTSD
Learn about the differences between PTSD and other forms of trauma, how to identify it, and what can be done about it.
READ MORE
How Does PTSD Affect Relationships?
Medically reviewed by N. Simay Gökbayrak, PhD
PTSD is a mental health condition that may affect different aspects of your life, including your relationships. Here's how and what to do.
READ MORE
Types of PTSD
Medically reviewed by N.
 Simay Gökbayrak, PhD
Simay Gökbayrak, PhDPost-traumatic stress disorder (PTSD) can be broken down by type and severity of symptoms. Each type has different treatments and ways to manage it.
READ MORE
Residual Symptoms of Post-Traumatic Stress Disorder
Medically reviewed by Kendra Kubala, PsyD
Treatment isn't always the end of PTSD. Some people might have residual symptoms, but they can be managed.
READ MORE
What Is Imagery Rehearsal Therapy (IRT)?
Medically reviewed by Nicole Washington, DO, MPH
If you often have nightmares because of trauma in your past, imagery rehearsal therapy could help you manage and reduce them.
READ MORE
What Causes Depression?
Medically reviewed by Akilah Reynolds, PhD
What causes depression? Experts suggest it's a complex blend of your biology, psychology, and social environment.
READ MORE
What Causes Dissociative Identity Disorder (DID)?
Medically reviewed by Jeffrey Ditzell, DO
An important part of treating dissociative identity disorder is working out its causes and healing the trauma that often underlies this condition.
READ MORE
Feeling Empty? What It Means and What to Do
It's natural to feel empty or numb from time to time. But what happens when you've been feeling empty for a while now?
READ MORE
Is It PSTD or Something Else?
PTSD Differential Diagnosis: Is It PSTD or Something Else?- Conditions
- Featured
- Addictions
- Anxiety Disorder
- ADHD
- Bipolar Disorder
- Depression
- PTSD
- Schizophrenia
- Articles
- Adjustment Disorder
- Agoraphobia
- Borderline Personality Disorder
- Childhood ADHD
- Dissociative Identity Disorder
- Narcissistic Personality Disorder
- Narcolepsy
- Oppositional Defiant Disorder
- Panic Attack
- Postpartum Depression
- Schizoaffective Disorder
- Seasonal Affective Disorder
- Sex Addiction
- Specific Phobias
- Teenage Depression
- Trauma
- Featured
- Discover
- Wellness Topics
- Black Mental Health
- Grief
- Emotional Health
- Sex & Relationships
- Trauma
- Understanding Therapy
- Workplace Mental Health
- Original Series
- My Life with OCD
- Caregivers Chronicles
- Empathy at Work
- Sex, Love & All of the Above
- Parent Central
- Mindful Moment
- News & Events
- Mental Health News
- COVID-19
- Live Town Hall: Mental Health in Focus
- Podcasts
- Inside Mental Health
- Inside Schizophrenia
- Inside Bipolar
- Wellness Topics
- Quizzes
- Conditions
- ADHD Symptoms Quiz
- Anxiety Symptoms Quiz
- Autism Quiz: Family & Friends
- Autism Symptoms Quiz
- Bipolar Disorder Quiz
- Borderline Personality Test
- Childhood ADHD Quiz
- Depression Symptoms Quiz
- Eating Disorder Quiz
- Narcissim Symptoms Test
- OCD Symptoms Quiz
- Psychopathy Test
- PTSD Symptoms Quiz
- Schizophrenia Quiz
- Lifestyle
- Attachment Style Quiz
- Career Test
- Do I Need Therapy Quiz?
- Domestic Violence Screening Quiz
- Emotional Type Quiz
- Loneliness Quiz
- Parenting Style Quiz
- Personality Test
- Relationship Quiz
- Stress Test
- What's Your Sleep Like?
- Conditions
- Resources
- Treatment & Support
- Find Support
- Suicide Prevention
- Drugs & Medications
- Find a Therapist
- Treatment & Support
Medically reviewed by Ashleigh Golden, PsyD — By Brittany VanDerBill — Updated on June 23, 2021
If you’re not sure whether your symptoms are due to PTSD or something else, it may be worth asking your doctor or therapist about differential diagnoses (conditions with similar symptoms).
Going through a jarring or traumatic event isn’t easy. Afterward, you may find it difficult to put the experience behind you. You might continue to feel unusually anxious long after this difficult or traumatizing situation has passed.
A traumatic experience can sometimes lead to post-traumatic stress disorder (PTSD), though not all trauma leads to PTSD. And many other conditions have overlapping symptoms with PTSD, which can make getting an accurate diagnosis more complex.
Having some anxiety or additional worries is natural after something bad happens. But when do your symptoms signal PTSD? And could they be a sign of something other than PTSD?
The condition we know as post-traumatic stress disorder was once used almost exclusively to describe the symptoms of veterans who had experienced combat during war. But in these instances, the condition was referred to as “shell shock.” Today, modern research has helped us understand that PTSD can arise from other trauma, too.
The American Psychological Association notes that PTSD is considered to be an anxiety issue related to a traumatic occurrence.
The Diagnostic and Statistical Manual for Mental Disorders (DSM-5) definition of trauma requires “actual or threatened death, serious injury, or sexual violence.” Examples of trauma can include combat experience, abuse or assault, or surviving a natural disaster.
Some symptoms of PTSD can include:
- vivid and unwanted memories of the traumatic event
- staying away from anything related to the event or where it took place
- shame or guilt about what happened
- changes in mood
- anger or rage
- causing harm to oneself
It’s important to note that not everyone who goes through a traumatic event has PTSD. Additionally, you may discover that you have PTSD along with another condition.
A differential diagnosis is when a doctor works out which disorder someone has when several disorders have overlapping symptoms.
Receiving an accurate diagnosis is often an important first step toward finding the treatments, coping methods, and support networks that will help you heal. Talking with a doctor or therapist about your symptoms and experiences will help you find the right diagnosis and treatment plan for you.
It’s important not to attempt your own differential diagnosis at home — only licensed mental health professionals, like counselors, therapists, clinical social workers, psychologists, and psychiatrists — can make this assessment.
The following conditions share some similarities with PTSD:
- acute stress disorder
- complex PTSD
- dissociative disorders
- adjustment disorder
- generalized anxiety disorder
- depression
- panic disorder
- phobias
- substance use disorders
We look at some of these conditions in more detail below.
Acute stress disorder
This disorder has some highly similar symptoms to PTSD.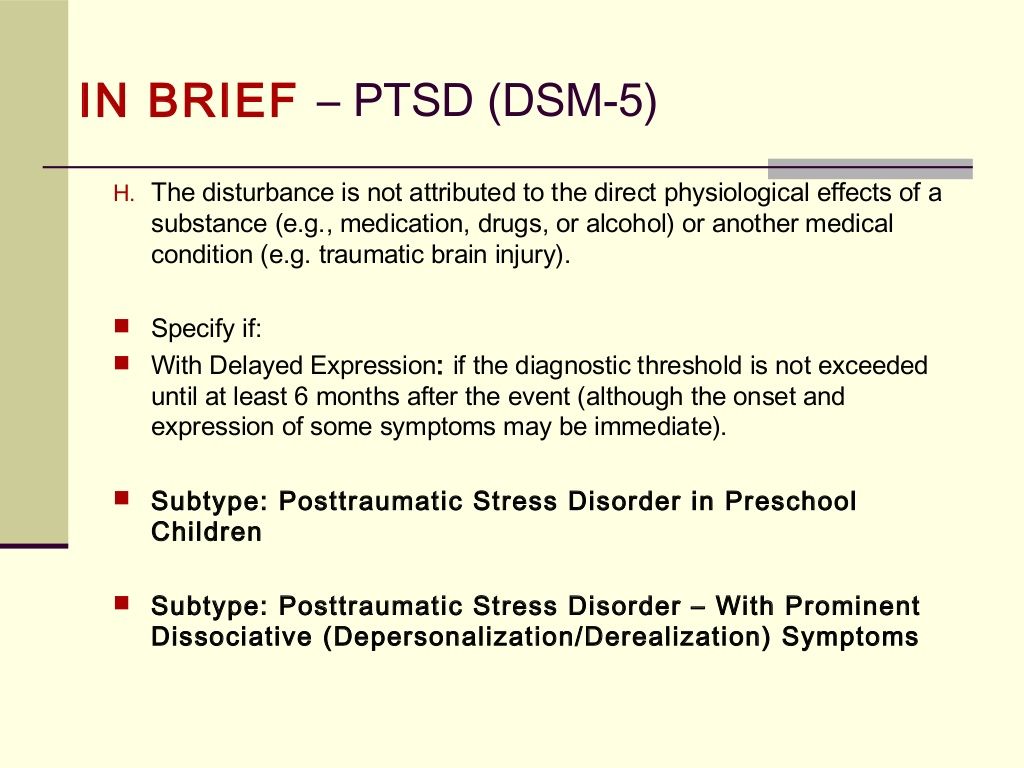 The main factor that is considered in a PTSD differential diagnosis in this instance is how long you’ve experienced your symptoms. Generally speaking, PTSD requires symptoms to last for at least one month.
The main factor that is considered in a PTSD differential diagnosis in this instance is how long you’ve experienced your symptoms. Generally speaking, PTSD requires symptoms to last for at least one month.
Complex PTSD
Complex PTSD has similar symptoms to PTSD, but the cause is different. While PTSD is usually linked with a single event, complex PTSD develops after repeated exposure to traumatic events, such as childhood neglect or abuse within a relationship.
Complex PTSD is not listed in the DSM-5, but many therapists recognize and treat its symptoms.
Dissociative disorders
Dissociation is one way the body deals with traumatic experiences. When you experience trauma, you might feel a disconnect between your mind and body. This helps give you some distance from the traumatic event.
While dissociation has a useful function in the moment, people with PTSD may notice that dissociation occurs again later on, and it can interrupt their daily lives. For example, someone with PTSD might feel as though they are detached from reality during a flashback.
A variety of dissociative disorders exist, and they often share some common symptoms. These include:
- dissociative identity disorder
- depersonalization/derealization disorder
- dissociative amnesia
The causes of dissociative disorders are often rooted in past traumas, so they are closely linked with PTSD. There’s also a subtype of PTSD that is a form of dissociative disorder. It’s important to reach out for professional help to distinguish which condition may be impacting you.
Generalized anxiety disorder
One reason that PTSD can be confused with generalized anxiety disorder is the intense anxiety you experience with both conditions. Intrusive thoughts and a tendency to feel angry or on edge are also fairly common with both.
People with generalized anxiety disorder have a history of anxiety across a wide range of circumstances, whereas people with PTSD often experience anxiety in response to a major trauma.
Depression
Sometimes, the symptoms of depression and PTSD can look and feel alike. People with depression may feel hopeless, or they may feel intense amounts of shame and guilt. People with PTSD also tend to experience this extreme shame, but it’s primarily focused on the event that occurred.
People with depression may feel hopeless, or they may feel intense amounts of shame and guilt. People with PTSD also tend to experience this extreme shame, but it’s primarily focused on the event that occurred.
Panic disorder
Someone with panic disorder may experience intense feelings of anxiety. This can be related to a specific object or situation. In these cases, you might avoid that specific thing to prevent a panic attack from occurring. A person who experienced trauma may avoid certain situations as well, so these two conditions can feel quite similar in this way.
Substance use disorder
When a person has a substance use disorder, they may experience a few symptoms in common with PTSD. For instance, substance use disorders could cause high anxiety or feelings of being on edge. They could also bring changes in mood and habits, just like with PTSD.
A differential diagnosis can be helpful in distinguishing between PTSD and something else. However, it is possible that you may have both PTSD and another condition with similar characteristics.
When this happens, it’s referred to as comorbidity.
Substance use disorder is a particularly common comorbidity. The PTSD Alliance reports that more than 7 million people in the United States have PTSD. Of those people, they note that as many as 40% also experience addiction.
Further, researchers estimate that almost 52% of males experiencing PTSD have a substance use disorder.
If you’re living with PTSD and substance use disorder or other conditions, don’t lose hope. Many resources exist for people experiencing these conditions.
You may want to begin by seeking help from your primary care physician. They can provide referrals to additional resources where necessary. If you already have a trusted counselor or psychiatrist, they would be a safe and helpful person to reach out to.
It’s important to be honest and open about all of your symptoms when speaking with any mental health professional you work with. This includes symptoms related to PTSD and those that could be related to other conditions, such as panic disorder or depression. Doing so ensures that you will receive the help that you need to start healing.
Doing so ensures that you will receive the help that you need to start healing.
There are various evidence-based treatments for PTSD, including:
- Cognitive behavioral therapy (CBT). CBT helps people challenge the patterns of behaviors, feelings, and thoughts that are causing distress.
- Cognitive processing therapy (CPT). CPT helps people modify and challenge unhelpful trauma-related beliefs.
- Prolonged exposure therapy. This type of CBT teaches people to gradually approach memories, feelings, and places related to the trauma to learn that they aren’t dangerous.
Suicide prevention
If you or someone you know is considering suicide, you’re not alone. Help is available right now:
- Call the National Suicide Prevention Lifeline 24 hours a day at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.
- Call the Veterans Crisis Line 24 hours a day at 800-273-8255
Not in the U. S.? Find a helpline in your country with Befrienders Worldwide.
S.? Find a helpline in your country with Befrienders Worldwide.
The important thing to remember with PTSD is that there is hope. Millions of other people are also going through PTSD. Many more are also experiencing other conditions as well.
Knowing that you aren’t alone can help give you the courage to reach out and ask for some help. Contact your primary care physician or, if you know of one already, a mental health professional. They will have the training to help you with your PTSD and other conditions. They also can refer you to other professionals who can provide further assistance as needed.
If you’re unsure how to ask someone for help, this guide will assist you in finding the words to begin your path to healing. You might also find that podcasts can be helpful on this journey. While not a substitute for treatment, they may help you feel less alone or more supported on your path to wellness.
Getting help for PTSD is important for healing, and by taking the time to read this article, you’re taking those first steps toward healing.
Last medically reviewed on June 23, 2021
6 sourcescollapsed
- CSTS uniformed services university. (n.d.).
cstsonline.org/assets/media/documents/CSTS_CTC_Asking_for_Help_Do_You_Know_How.pdf - Mann SK, et al. (2021). Posttraumatic stress disorder.
ncbi.nlm.nih.gov/books/NBK559129/ - Pai A, et al. (2017). Posttraumatic stress disorder in the DSM-5: Controversy, change, and conceptual considerations.
ncbi.nlm.nih.gov/pmc/articles/PMC5371751/ - Post-traumatic stress disorder. (n.d.).
apa.org/topics/ptsd - PTSD treatments. (2020).
apa.org/ptsd-guideline/treatments - van Huijstee J, et al. (2018). The dissociative subtype of post-traumatic stress disorder: Research update on clinical and neurobiological features.
pubmed.ncbi.nlm.nih.gov/29063485/
FEEDBACK:
Medically reviewed by Ashleigh Golden, PsyD — By Brittany VanDerBill — Updated on June 23, 2021
Read this next
What Are the Symptoms of PTSD?
Medically reviewed by Karin Gepp, PsyD
How do you know if you have PTSD? There's a long list of symptoms and diagnostic criteria.
 Here's what you need to know.
Here's what you need to know.READ MORE
Can You Recover from Trauma? 5 Therapy Options
Trauma-informed therapy can help you reduce the emotional and mental effects of trauma. Here are the best options for trauma-focused treatments.
READ MORE
Podcast: There’s More to Trauma than PTSD
Learn about the differences between PTSD and other forms of trauma, how to identify it, and what can be done about it.
READ MORE
How Does PTSD Affect Relationships?
Medically reviewed by N. Simay Gökbayrak, PhD
PTSD is a mental health condition that may affect different aspects of your life, including your relationships. Here's how and what to do.
READ MORE
Types of PTSD
Medically reviewed by N.
 Simay Gökbayrak, PhD
Simay Gökbayrak, PhDPost-traumatic stress disorder (PTSD) can be broken down by type and severity of symptoms. Each type has different treatments and ways to manage it.
READ MORE
Residual Symptoms of Post-Traumatic Stress Disorder
Medically reviewed by Kendra Kubala, PsyD
Treatment isn't always the end of PTSD. Some people might have residual symptoms, but they can be managed.
READ MORE
What Is Imagery Rehearsal Therapy (IRT)?
Medically reviewed by Nicole Washington, DO, MPH
If you often have nightmares because of trauma in your past, imagery rehearsal therapy could help you manage and reduce them.
READ MORE
What Causes Depression?
Medically reviewed by Akilah Reynolds, PhD
What causes depression? Experts suggest it's a complex blend of your biology, psychology, and social environment.
READ MORE
What Causes Dissociative Identity Disorder (DID)?
Medically reviewed by Jeffrey Ditzell, DO
An important part of treating dissociative identity disorder is working out its causes and healing the trauma that often underlies this condition.
READ MORE
Feeling Empty? What It Means and What to Do
It's natural to feel empty or numb from time to time. But what happens when you've been feeling empty for a while now?
READ MORE
diagnostics and treatment //Psychological newspaper
Specialists of the National Medical Research Center for Psychiatry and Neurology. V.M. Bekhterev on September 22 organized and held a webinar "Clinical representation of a person's traumatic experience: from anxiety response mechanisms to PTSD" .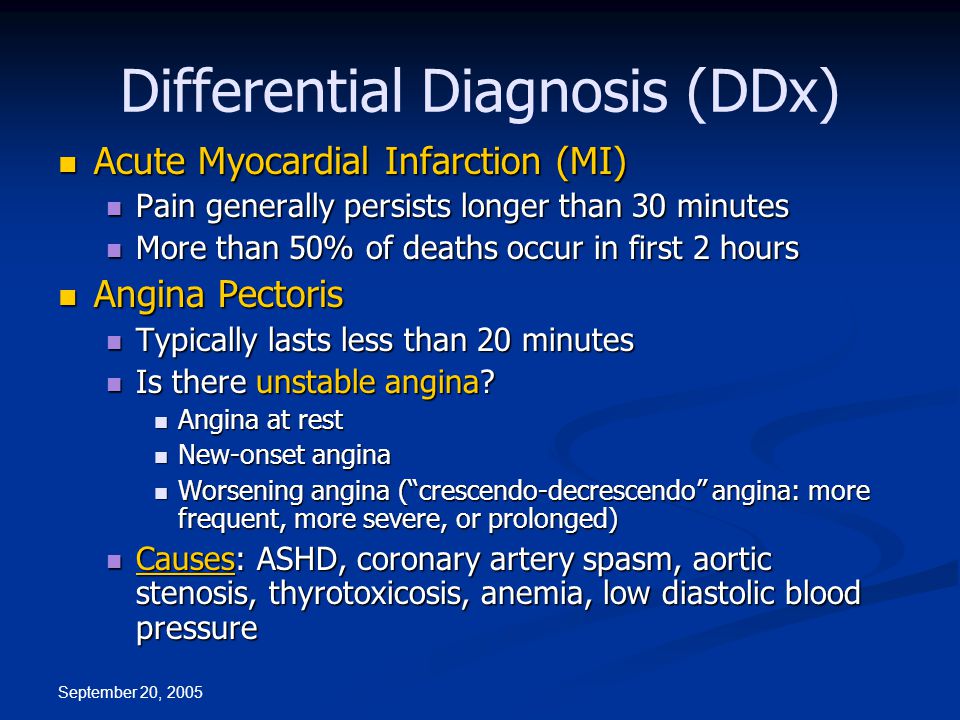 The participants discussed modern approaches to the treatment of anxiety disorders, the possibility of using psychopharmacotherapy, and the features of PTSD after the loss of a loved one. nine0005
The participants discussed modern approaches to the treatment of anxiety disorders, the possibility of using psychopharmacotherapy, and the features of PTSD after the loss of a loved one. nine0005
"Psychological newspaper" publishes excerpts from the speeches of the webinar participants:
Modern approaches to the diagnosis and treatment of neurotic anxiety disorders
Tatiana Arturovna Karavaeva , Head, Chief Researcher of the Department for the Treatment of Borderline Mental Disorders and Psychotherapy of the Federal State Budgetary Institution National Medical Research Center of the PN named after N.N. V.M. Bekhterev” of the Ministry of Health of Russia:
"Stress develops as a consequence of experience:
- situations of incomplete certainty and unpredictability,
- severe physical and psychological working conditions,
- lack of time and other resources,
- natural anxiety and fear of infecting oneself, loved ones, work colleagues,
- human losses in the provision of medical care, nine0017 information pressure from society and the media,
- anxiety before responsibility, punishment, censure,
- possible disciplinary violations by colleagues and employees.

What are the current approaches in the treatment of anxiety spectrum disorders? This is, first of all, the complex use of drug biological therapy and psychotherapy. This combination is possible at all stages of treatment and rehabilitation, however, this combination is not stable at all stages: it can vary flexibly, it can predominate (depending on the clinical condition and tasks) either drug therapy or psychotherapy. This combination depends on various factors - on the characteristics of the patient, on the symptoms, the intensity of its manifestation, on the stage of the disease. The combination of psychotherapy and pharmacotherapy varies depending on the dynamics of the state and the stage of psychotherapy. nine0005
What to choose? And how to combine psychotherapy and pharmacotherapy?
Benefits of pharmacological treatment:
- the rapid action of drugs that significantly alleviate the current condition of the patient.
- taking drugs from the patient does not require any effort,
- drugs are more affordable than psychotherapy,
Limitations or disadvantages of pharmacological treatment:
- drugs do not affect the psychological mechanisms of anxiety disorders, do not change anything in the assessment of what is happening,
- some drugs somewhat limit the emotional response: patients complain that they smooth out not only negative, but also positive emotions,
- often the drugs work while they are being taken, and, accordingly, when the drug is stopped (especially if the drug is stopped incorrectly), we are at risk of developing relapses,
- drugs have side effects, as well as special drug interactions, which is important for people with somatic pathology who are already receiving drug treatment.
Benefits of psychotherapeutic treatment:
- psychotherapy allows you to influence psychological mechanisms, resolve internal conflicts, develop new effective skills for interacting with the world, with people around you, new more constructive emotional stereotypes of response and behavior,
- psychotherapy provides an opportunity to re-evaluate what is happening at the present time, to adjust their perspectives, goals, tasks, to cope with the condition more effectively, to adapt to treatment.
Disadvantages of psychotherapeutic treatment:
- psychotherapy requires active work of the patient, his emotional and intellectual efforts, this process can cause acute feelings, nine0017 psychotherapy is impossible without patient motivation and readiness for change,
- psychotherapy is a long-term method, it takes time to achieve a stable effect,
- psychotherapy is more expensive than drug treatment.
Undoubtedly, for the treatment of patients with anxiety disorders, it is necessary to use an integrated team approach, therefore, in addition to the work of a psychiatrist, psychotherapist, it is necessary to involve a medical psychologist. A medical psychologist can conduct an instrumental psychological study to assess the patient's condition, to assess the dynamics of the condition, an examination, the result of which will be the selection of targets for psychotherapy. nine0005
Psychopharmacotherapy of acute stressful psychopathological disorders
The report "Psychopharmacotherapy of acute stressful psychopathological disorders" was presented by Igor Viktorovich Boev , Head of the Department of Psychiatry, Psychotherapy and Medical Psychology of the Stavropol State Medical University of the Ministry of Health of Russia, Honored Doctor of the Russian Federation:
“Our research material is based on documented case histories of victims in Budenovsk, Beslan, Mineralnye Vody, Stavropol, Armavir, and South Ossetia.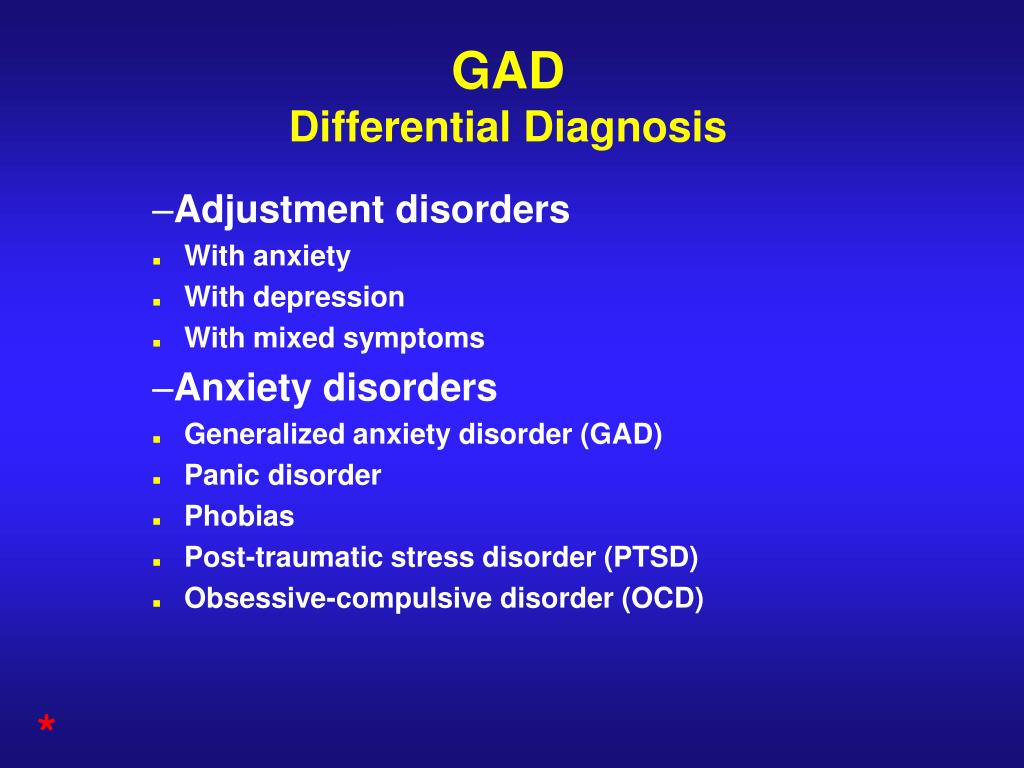 In addition, we conducted clinical-psychological, clinical-psychophysiological studies, which allowed us to create a significant evidence base. nine0005
In addition, we conducted clinical-psychological, clinical-psychophysiological studies, which allowed us to create a significant evidence base. nine0005
Stress stages:
1. Alarm with corresponding manifestations. When anxiety appears, there is a resistance of the body. During global stressors (hostages, terrorist attacks), the body's resistance is destroyed quite quickly, anxiety begins to prevail.
2. Resistance : increases the body's resistance to the action of any irritants.
3. Exhaustion : resistance decreases, changes similar to aging appear in the body. nine0005
What causes aging? Oxidative stress develops, activation of free radical oxidation processes, which leads to rather gross violations: radicals oxidize the walls of blood vessels, protein molecules, DNA, oxidize lipids, oxidative stress causes destruction of a normal cell. Through the attack of free radicals, it leads to gross damage to the cell.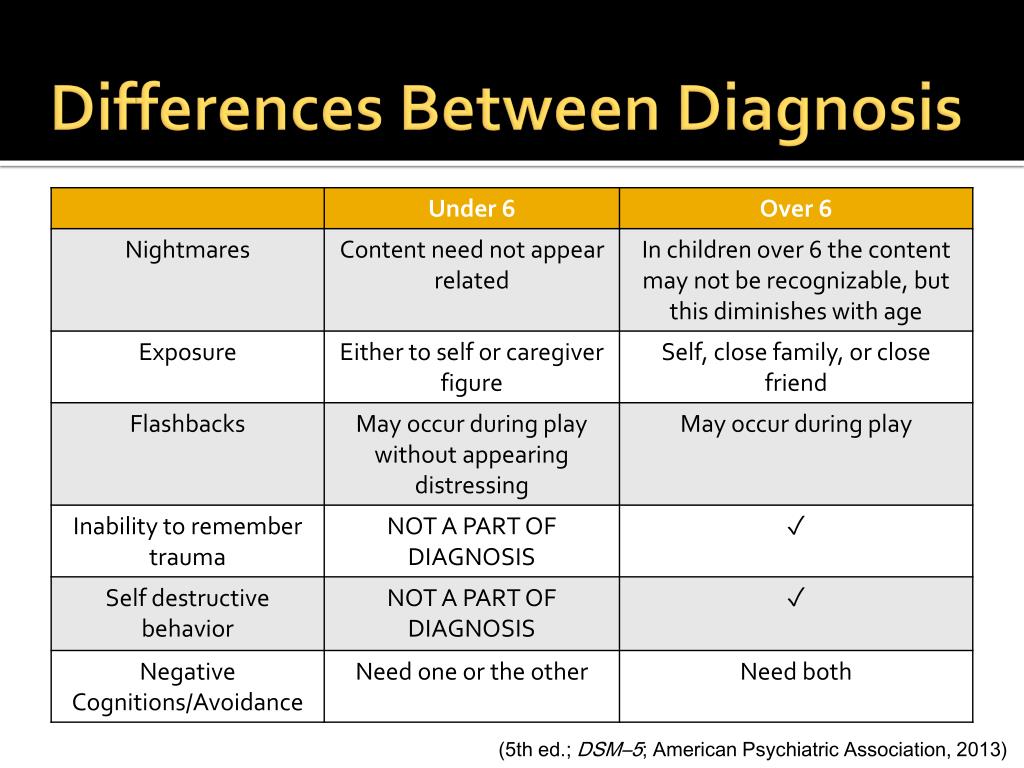
The basis of the system of pathogenetic intensive complex therapy (PICT) are complex pharmacological compositions. The goal is to restore the psychobiological resources of the individual and inhibit the leading links of etiopathogenesis. nine0005
PICT lasts 7–12 days. We came to the site of a terrorist attack, global upheavals, set up a day hospital in a polyclinic, in a hospital, in a tent - where possible, and carried out pathogenetic intensive complex therapy. Only by the 5-7th day of intensive therapy, the victims of Beslan terrorism could begin to hear the psychotherapist and clinical psychologists, before that they simply did not perceive everything that they were trying to say. Therefore, in case of global catastrophes, psychotherapy should be connected a little later. Before that, it was just human interaction. After PICT, we switched to antidepressants, which were used for 3–4 months to a year. It is rather difficult to stop global stress, to eliminate the links of etiopathogenesis. nine0005
nine0005
Practically in all regions where there were terrorist attacks, after 5-6 months, the adaptation mechanisms were depleted among the population. People developed cerebrovascular disorders, psychoendocrine disorders, increased the number of heart attacks, strokes, diabetes, and ulcerative pathologies of the gastrointestinal tract.”
Modern approaches to the diagnosis and therapy of PTSD
9 spoke about modern approaches to the diagnosis and treatment of PTSD0003 Anna Vladimirovna Vasilieva , Chief Researcher of the Department for the Treatment of Borderline Mental Disorders and Psychotherapy, Head of the International Department of the Federal State Budgetary Institution “N. V.M. Bekhterev” of the Ministry of Health of Russia:
“When we talk about the pathogenesis of post-traumatic stress disorder, it is necessary to recall Academician Natalya Petrovna Bekhtereva , who developed the concept of pathologically stable conditions back in the 70s.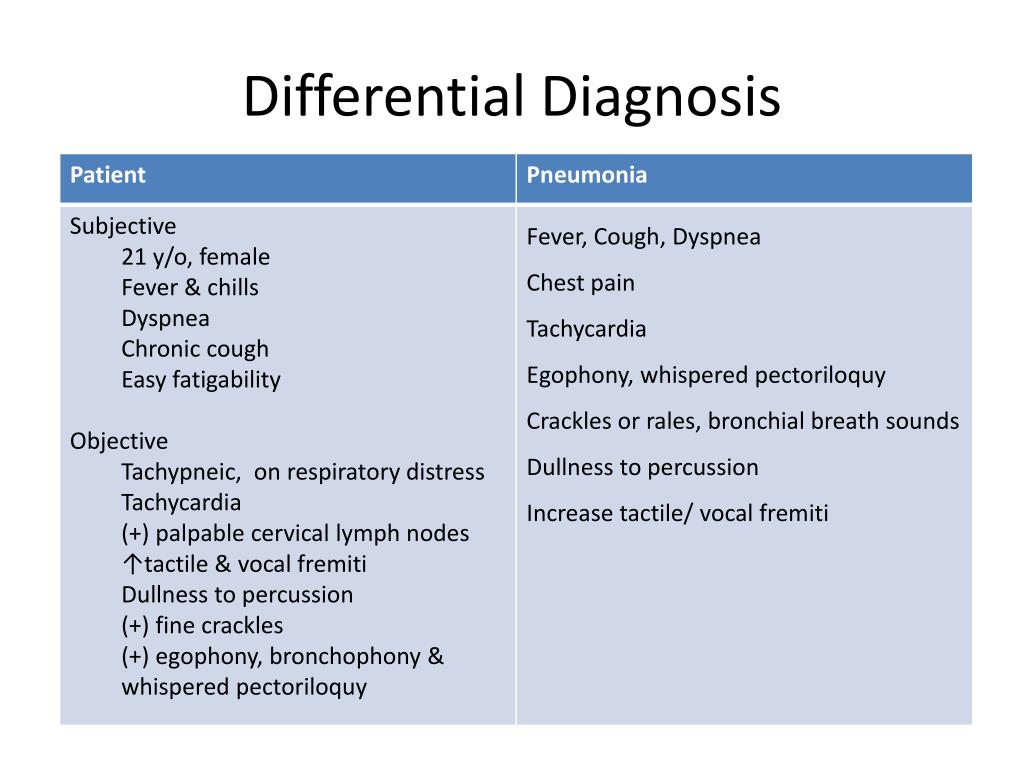 They arise as pathological reactions as a result of one or another traumatic impact with the formation of a long-term memory matrix, which ensures that these states are self-sustaining. Brain plasticity changes, the pathological state becomes stable and functions like a reverberation network. nine0005
They arise as pathological reactions as a result of one or another traumatic impact with the formation of a long-term memory matrix, which ensures that these states are self-sustaining. Brain plasticity changes, the pathological state becomes stable and functions like a reverberation network. nine0005
One of the types of psychotherapy that is currently used to correct this persistent pathological condition is the psychotherapy of desensitization and processing with the help of eye movements. Oculomotor reactions are used to activate the adaptive information-processing mechanism and restore interhemispheric communication, due to which we achieve the integration of traumatic experience and obtain a psychotherapeutic effect.
Stressful negative events lead to an overload of the information processing system. Figuratively speaking, our brain begins to work like a computer that has been infected with a virus. Stressful negative events cannot be integrated, a certain transformation and restoration of this system becomes the task of psychotherapy. Bilateral stimulation is used, in particular, eye movements from side to side, tapping on the knees or alternating auditory stimulation, which is described in detail in the protocols for this technique ...
Bilateral stimulation is used, in particular, eye movements from side to side, tapping on the knees or alternating auditory stimulation, which is described in detail in the protocols for this technique ...
Another method that also has a sufficient evidence base for its effectiveness is trauma-focused cognitive behavioral therapy. In addition, psychodynamic methods (especially if we know that there is a large contribution of cumulative trauma to the patient's condition), dialectical behavioral therapy and body-oriented psychotherapy can be used.
The existing group for the development of international protocols for the management of patients with post-traumatic disorders identifies three main phases of work:
1. Stabilization of the state.
2. Confrontation with traumatic experience.
3. Search for new life guidelines that provide post-traumatic growth.
It is important to focus on a healthy resource of the individual. To do this, we ask a series of questions:
- What were the top five experiences in the patient's life?
- What aspects of life should remain unchanged?
- What positive changes already exist in the process of psychotherapy and how have they been achieved? nine0018
- Try to imagine yourself as an older and wiser person, what advice would you give yourself today?
Post-traumatic stress disorder in situations of loss of an object of extraordinary significance
The report "Post-traumatic stress disorder in situations of loss of an object of extraordinary significance: clinic and pharmacotherapy" was prepared by Stanislav Valerievich Poltorak V. M. Bekhterev” of the Ministry of Health of Russia:
M. Bekhterev” of the Ministry of Health of Russia:
“The formative factor of post-traumatic stress in situations of loss of an object of special affection is the unforeseen loss of a significant other. Unlike other variants of life catastrophes, this traumatic situation affects, first of all, individual personal values. Although the orientation of the psychogenic factor is different than in the case of a threat to physical existence, such a situation is perceived as equivalent to it - the "irreparable" destruction of the personality. nine0005
The loss of a significant other as a result of trauma, death after a life-threatening illness, accident, disappearance, suicide is accompanied by a feeling of complete loss of the "I", a feeling of the impossibility of subsequent recovery and the persistent despair associated with these manifestations. Often this is due to the fact that a person who develops post-traumatic stress is united with the object of loss in a symbiotic relationship.
The formation of post-traumatic stress in case of loss of an object of affection occurs in the first six months after a traumatic event, and lasts from six months to several years. nine0005
Deep grief usually lasts a few days or weeks, then turns into sadness. In uncomplicated cases, the loss reaction goes through three stages:
1. emotional shock with numbness and petrification,
2. awareness of loss with longing, crying, sleep disturbance, appetite and narrowing of consciousness on psychotraumatic experiences,
3. humility - acceptance of what happened and the realization that life goes on.
John Bowlby identified the following stages of grief and bereavement:
1. Numbness or protest. Characterized by severe malaise, fear and anger. Psychological shock can last for moments, days or months.
2. Longing and desire to return the lost person. The world appears empty and without meaning, but self-esteem does not suffer. The patient is preoccupied with thoughts of the lost person; periodically there are physical restlessness, crying and anger. The condition may last for months or years. nine0005
The patient is preoccupied with thoughts of the lost person; periodically there are physical restlessness, crying and anger. The condition may last for months or years. nine0005
3. Disorganization and despair. Restlessness and performance of aimless actions. Increased anxiety, withdrawal, introversion and annoyance. Constant memories of the past.
4. Reorganization. The emergence of new experiences, objects and goals. Grief weakens and is replaced by memories dear to the heart.
Diagnosis of PTSD, treatment of traumatic neurosis in the Allianz Central Medical Health Center
PTSD (post-traumatic stress disorder) is a mental illness that occurs several weeks or months after a severe life-threatening event - military operations (both soldiers and civilians), captivity, man-made disasters, attacks, rape, natural disasters, terrorist acts. nine0005
The diagnosis and treatment of post-traumatic stress disorder is carried out by a psychotherapist.
The disorder may begin weeks or years after the traumatic experience. Traumatic neurosis is a person's "stuck" in an extreme situation, he constantly mentally returns to it and cannot forget.
The criteria for PTSD are as follows:
- The person was in a situation threatening life or health, was a participant or even just a witness. nine0018
- During the event, he experienced helplessness, horror, fear.
- The situation has remained in the past, but the patient with PTSD constantly experiences it - mentally, in nightmares, returns to it again and again. He does not share his experiences with those around him, he keeps everything in himself.
Important
A person is not able to objectively assess his state of health and cope with emotions. He begins to react inadequately to real events, does not perceive new information, tries to isolate himself from communication, reacts sharply to criticism and jokes. nine0005
nine0005
A person becomes a shadow of his former self, because he does not exist in the present. Referring to a psychotherapist is the only effective way to cope with a traumatic disorder.
Features of the development and diagnosis of PTSD
The breakdown is often preceded by a latent period of relative calm. After an injury, a person can lead a normal life for six months or even longer. In PTSD, the signs that signal the disease are as follows: nine0005
- experiences, anxiety and tension appear, which are associated with a traumatic situation. They are repeated at any time of the day: at night - in nightmares, during the day - in thoughts, memories;
- flashbacks occur - a person is "transferred" to a past situation, re-experiencing it very vividly and ceases to orient himself in reality, the state is similar to clouding of consciousness. Last from a few seconds to several hours;
- people withdraw into themselves, lose interest in work and communication.
 At the same time, he can react to innocent remarks and jokes with impulsive, cruel beatings. nine0018
At the same time, he can react to innocent remarks and jokes with impulsive, cruel beatings. nine0018
Post-traumatic stress disorder is characterized by agitation, aggression, increased caution, and suspicion. A person avoids any mention of what happened (actions, places, conversations), becomes anxious and emotionally retarded.
Important
Internal tension leads to fatigue, apathy, emptiness. Memory and attention deteriorate. A person becomes distracted, which leads to constant mistakes at work. Often this condition is accompanied by depressed mood (depression), thoughts of suicide. nine0005
In post-traumatic stress disorder, symptoms may include complaints of:
- insomnia or superficial sleep;
- increased sweating;
- palpitations, interruptions in the work of the heart;
- fatigue, hypersensitivity.
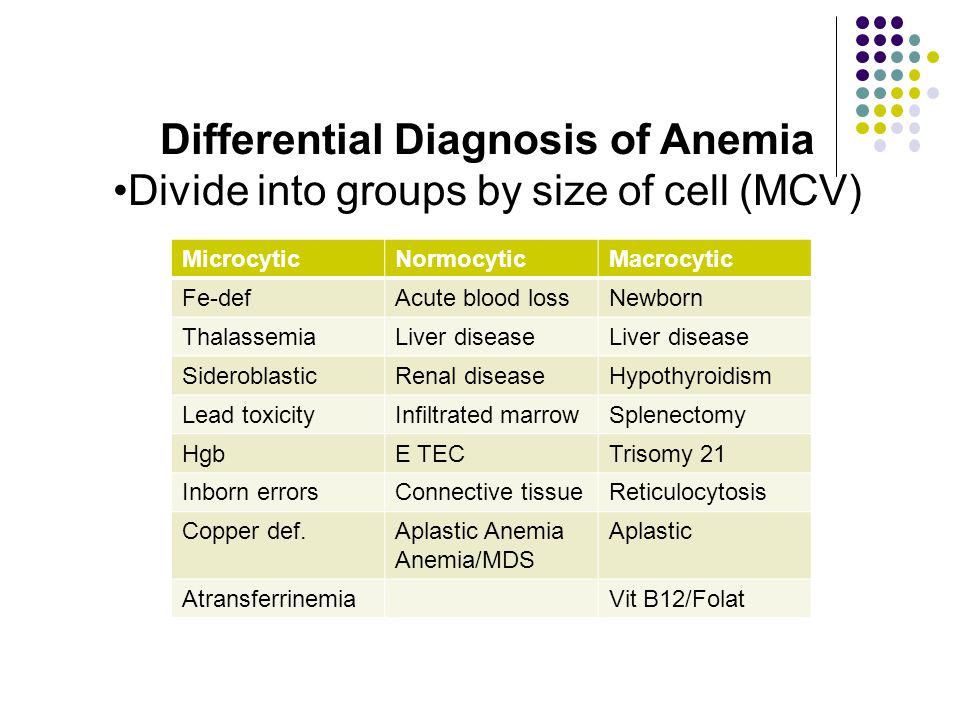
A psychotherapist diagnoses a disease at an individual consultation - collects an anamnesis (life history), evaluates complaints, tries to find out the causes of the disorder. Psychic trauma can trigger the development of other mental illnesses - severe depression, endogenous diseases. For differential diagnosis, a pathopsychological study is also used (performed by a clinical psychologist). nine0005
Psychic trauma can trigger the development of other mental illnesses - severe depression, endogenous diseases. For differential diagnosis, a pathopsychological study is also used (performed by a clinical psychologist). nine0005
Treatment of post-traumatic stress disorder (PTSD)
Psychotherapy sessions are the basis of recovery. They help the patient accept and process the traumatic experience in order to move on. Treatment for PTSD includes:
- Individual psychotherapy.
- Medical correction of symptoms (anxiety, depression, irritability, sleep problems).
- biofeedback therapy.
- Group therapy. nine0201
With PTSD, the disease can be overcome with the help of cognitive-behavioral psychotherapy. The psychotherapist teaches the patient not to run away from the traumatic situation, helps to increase self-control and cope with painful memories.
BFB therapy (biofeedback therapy) is a relaxation technique that relieves internal tension and reduces muscle stiffness.