Depression affect memory
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.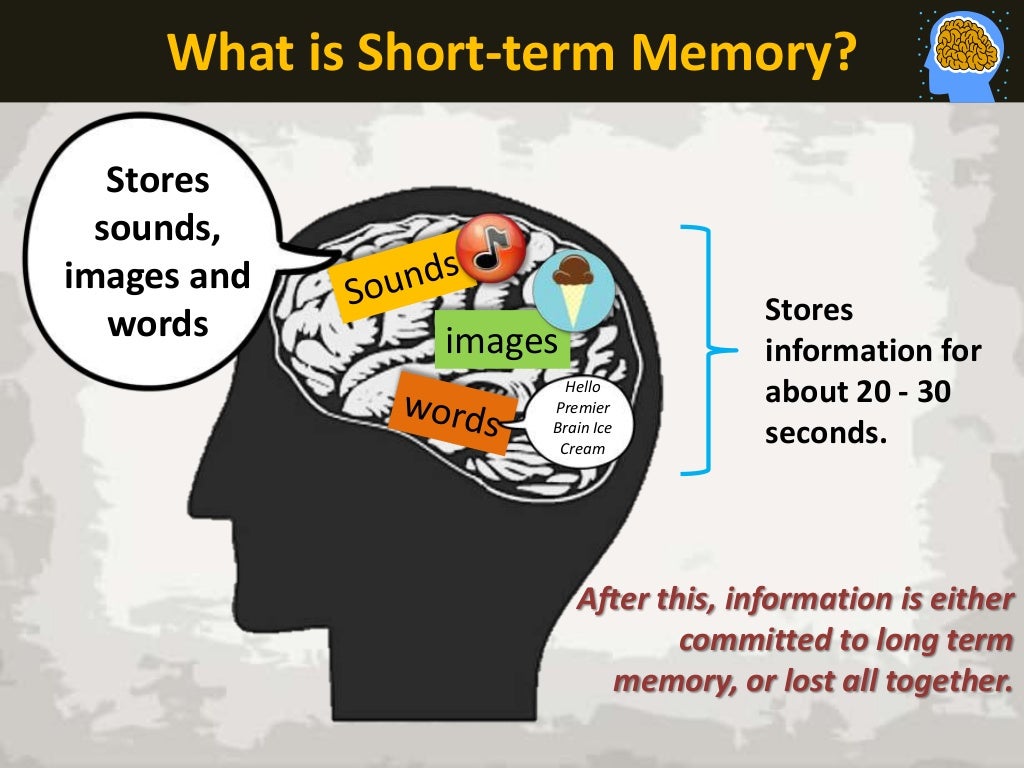 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.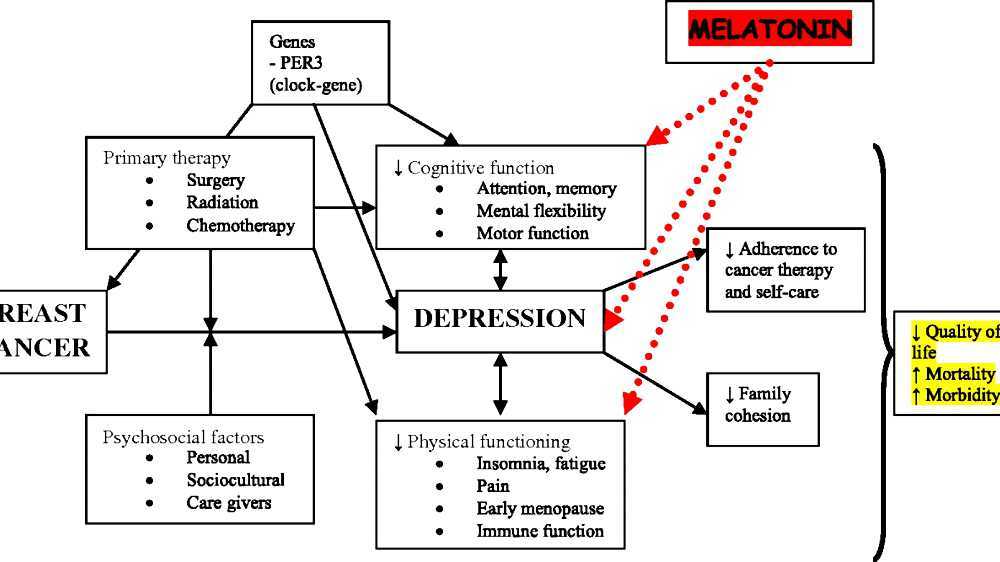 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.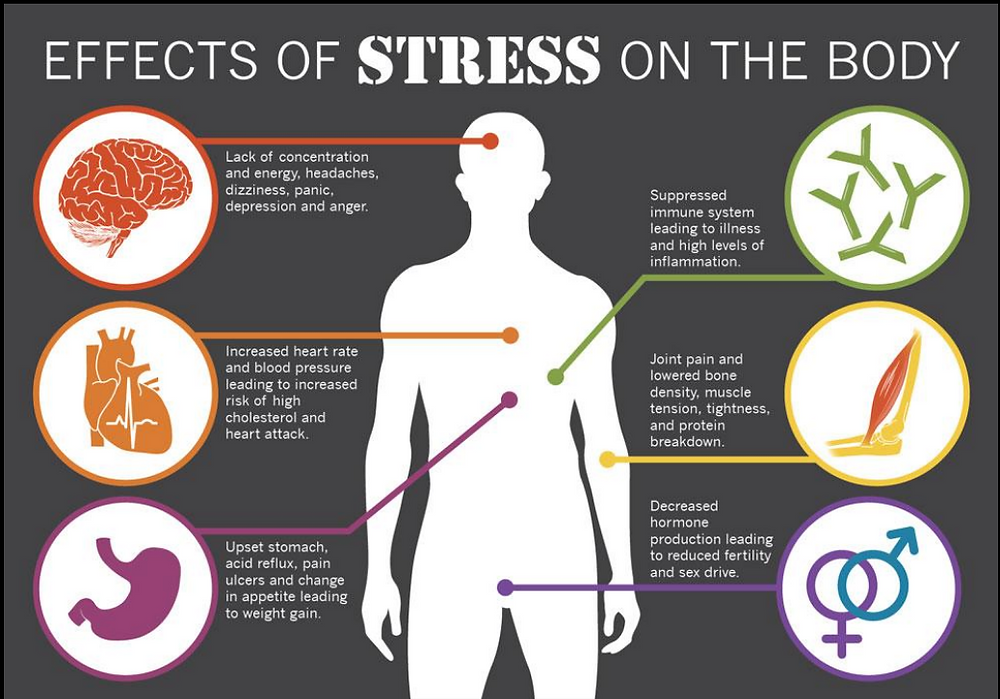 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Ministry of Health of the Republic of Tatarstan
October 9, 2019, Wednesday
Memory is a property of the human brain that allows storing and reproducing information. Memory can be visual (a person remembers what he sees better), auditory (what a person hears is better remembered) and motor (information is remembered when recording). We remember some information for a fraction of a second, and some we store in memory for many years, that is, memory can be immediate, operational and long-term. nine0003
A variety of factors can strengthen or weaken memory.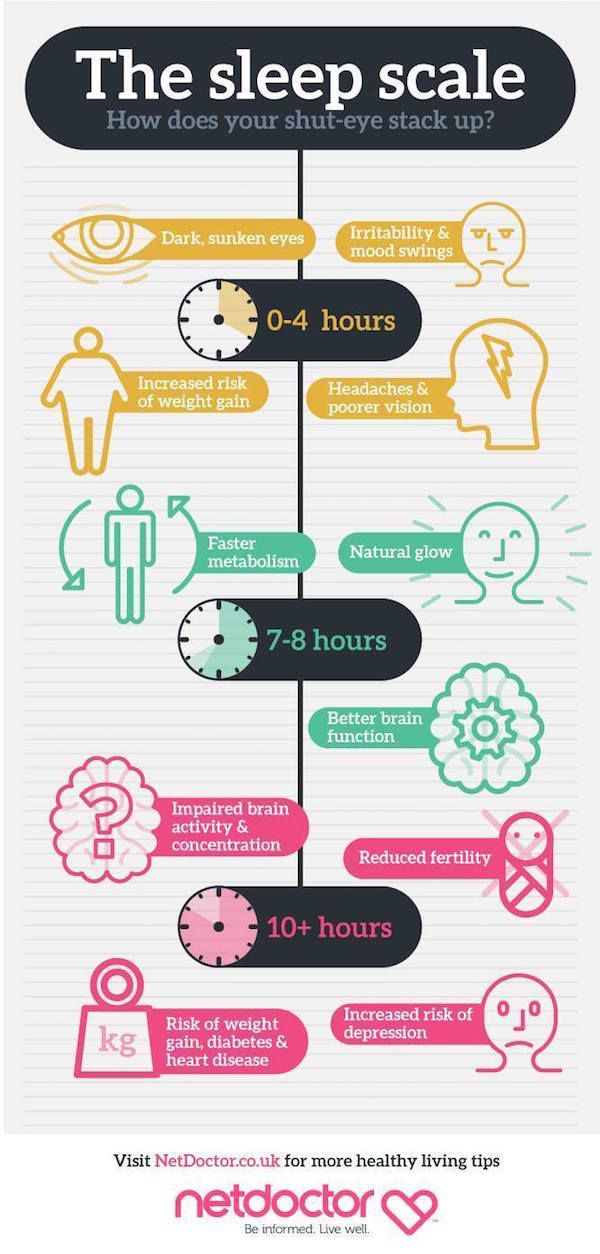 What are the causes of memory impairment in young and mature age?
What are the causes of memory impairment in young and mature age?
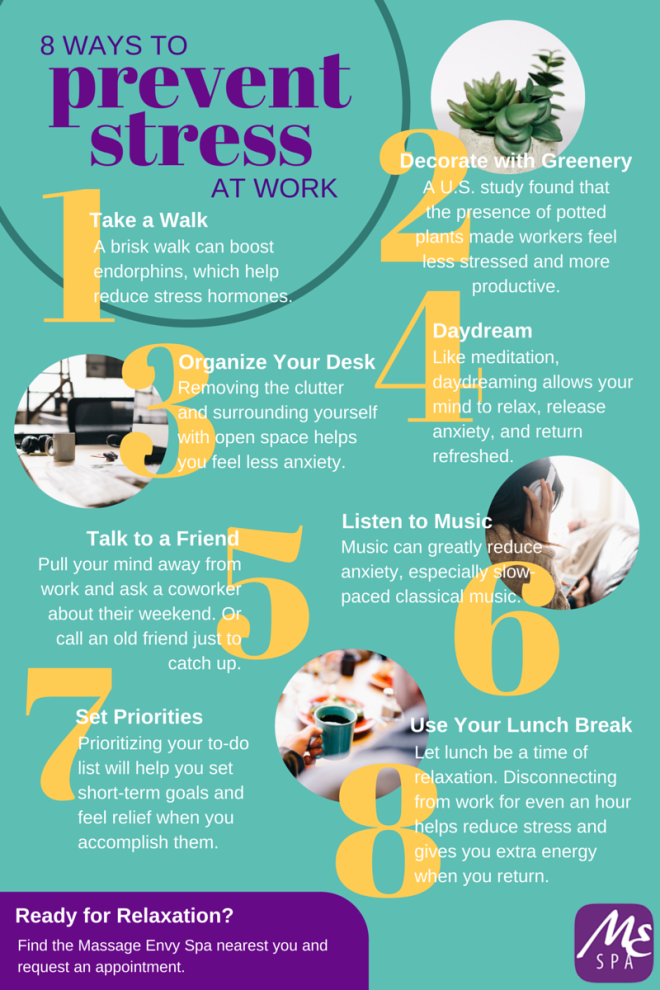
Stress. It is extremely important how a person copes with stress, how strong he is and how long a person is in a stressful situation. It has been established that prolonged exposure to stress psychologically and physically exhausts a person and negatively affects memory. Proper organization of work and rest, proper sleep, and in some cases psychological assistance help to eliminate this problem, emergency situations (catastrophes, injuries) can lead to more severe memory impairment up to complete loss (various types of amnesia), requiring specialized assistance. nine0003
Sleep disorders . Sleep is a necessary part of human life. It is in a dream that the brain works to sort and memorize the information received during the day. On average, a good rest requires 6 hours of sleep daily. Chronic lack of sleep leads to increased absent-mindedness, irritability, and, in particular, to memory impairment. Sleep mode promotes good rest, helps to overcome stressful situations more easily.
Sleep mode promotes good rest, helps to overcome stressful situations more easily.
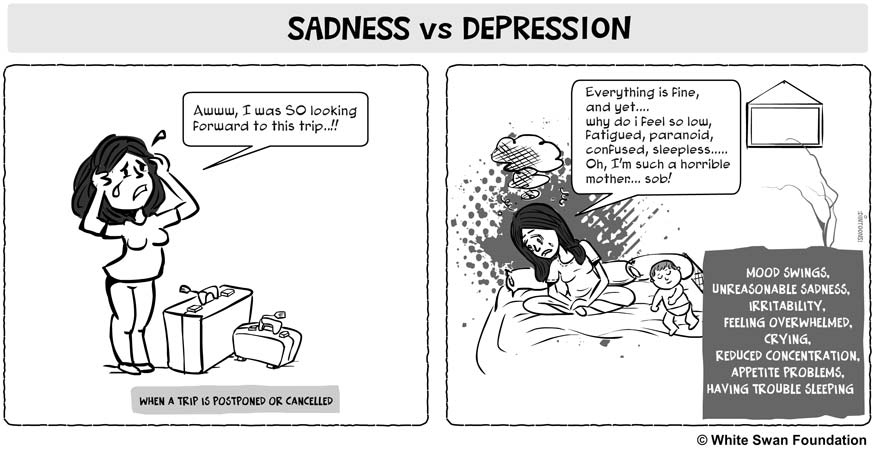
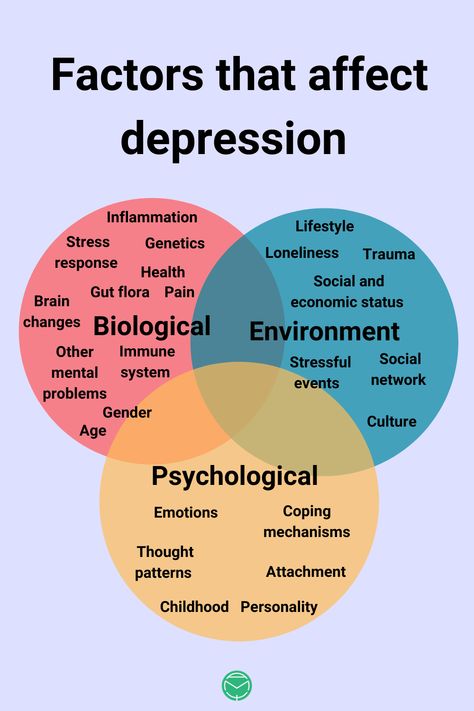
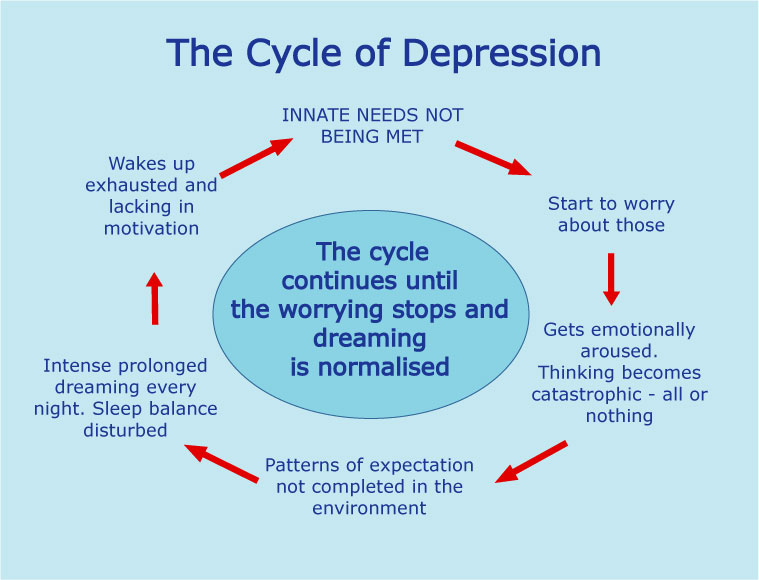
Depressive disorders. Sometimes depression can mimic memory impairment. There is forgetfulness, absent-mindedness, inattention, self-organization worsens. Usually, all these symptoms disappear when depression is eliminated.
Alcoholism. Alcohol abuse impairs memory. Initially, memory impairment manifests itself in the form of separate episodes of forgetfulness or inability to remember events that occur during the use of alcoholic beverages, then memory impairment becomes more severe and is accompanied by a decrease in intelligence. nine0003
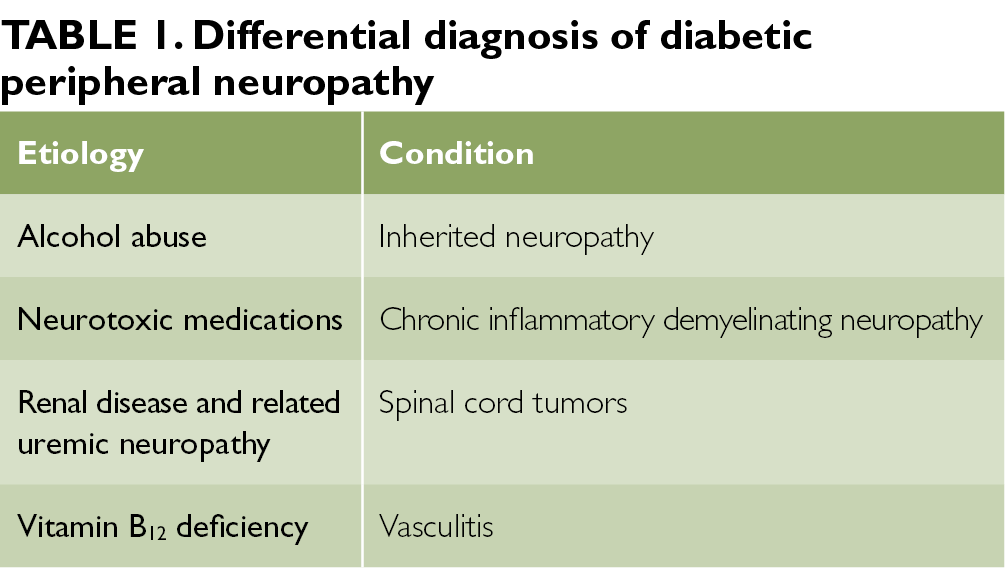
Concomitant somatic diseases. Some infectious (eg, meningitis, encephalitis, etc.) and non-infectious diseases (diabetes, stroke, thyroid disease, etc.) are also accompanied by memory loss.
Vitamin B12 deficiency. Vitamin B12 is necessary for the full functioning of the brain, so its long-term deficiency leads to damage to brain cells and disruption of their functions.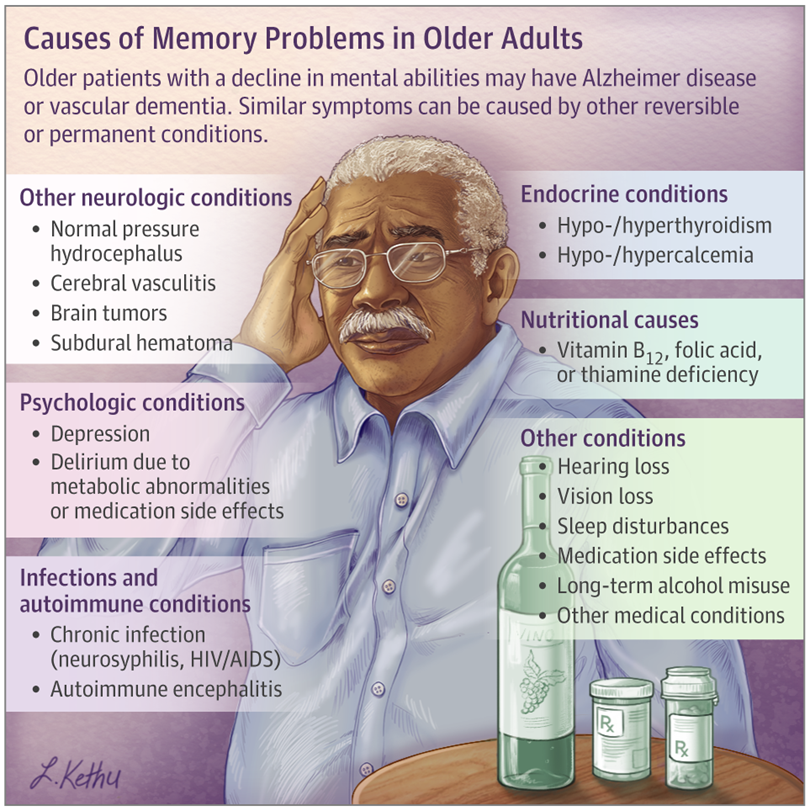
Medications. nine0010 Taking sleeping pills, painkillers, antiallergic drugs, antidepressants can have a negative effect on memory. It is necessary to prescribe these drugs with particular care in patients with impaired liver and kidney function, as their excretion from the body slows down. Usually, the withdrawal of the drug leads to the normalization of memory.
Photo by pixabay.com.
Share:
READ ALL NEWS
Spatial working memory disorders in mild depression and their neurophysiological correlates
Disorders of the function of spatial working memory in mild depression and their neurophysiological correlates Website of the publishing house "Media Sfera"
contains materials intended exclusively for healthcare professionals. By closing this message, you confirm that you are a registered medical professional or student of a medical educational institution.
Galkin S. A. nine0003
A. nine0003
Research Institute of Mental Health, Tomsk National Research Medical Center of the Russian Academy of Sciences, Tomsk, Russia
Peshkovskaya A.G.
Research Institute of Mental Health, Siberian Branch of the Russian Academy of Medical Sciences, Tomsk
Simutkin G.G.
Research Institute of Mental Health of the Tomsk National Research Medical Center of the Russian Academy of Sciences, Tomsk, Russia
Vasilyeva S.N.
Roshina O.V.
Research Institute of Mental Health, Tomsk National Research Medical Center RAS, Tomsk, Russia
Ivanova S.A.
Research Institute of Mental Health, Siberian Branch of the Russian Academy of Medical Sciences, Tomsk
Bokhan N.A.
Research Institute of Mental Health of the Tomsk Scientific Center of the Siberian Branch of the Russian Academy of Medical Sciences
Disorders of the function of spatial working memory in mild depression and their neurophysiological correlates
Authors:
Galkin S. A., Peshkovskaya A.G., Simutkin G.G., Vasilyeva S.N., Roshchina O.V., Ivanova S.A., Bokhan N.A.
A., Peshkovskaya A.G., Simutkin G.G., Vasilyeva S.N., Roshchina O.V., Ivanova S.A., Bokhan N.A.
More about the authors
Journal: Journal of Neurology and Psychiatry. S.S. Korsakov. 2019;119(10): 56‑61
DOI: 10.17116/jnevro201911910156
How to quote:
Galkin S.A., Peshkovskaya A.G., Simutkin G.G., Vasilyeva S.N., Roshchina O.V., Ivanova S.A., Bokhan N.A. Disorders of the function of spatial working memory in mild depression and their neurophysiological correlates. nine0092 Journal of Neurology and Psychiatry. S.S. Korsakov. 2019;119(10):56‑61.
Galkin SA, Peshkovskaia AG, Simutkin GG, Vasil'eva SN, Roshchina OV, Ivanova SA, Bokhan NA. Disorders of spatial working memory in affective disorders with mild current depression and their neurophysiological correlates. Zhurnal Nevrologii i Psikhiatrii imeni S.S. Korsakova. 2019;119(10):56‑61. (In Russ.).
https://doi.org/10.17116/jnevro201911910156
Read metadata
Purpose of the study. Determination of the features of impaired spatial working memory and their neurophysiological correlates in patients with mild depressive disorders. Material and methods. We examined 30 patients (right-handed) with a diagnosis of ICD-10 "Mood disorders" (headings F31.3, F32.0, F33.0, F34.1) before the start of treatment. The average age of patients is 37±8 years. As a control group, 30 mentally and somatically healthy people (mean age 32 ± 7 years) were examined. The study of spatial working memory was carried out using the Corsi Block-Tapping test. Electroencephalography (EEG) was also performed. The spectral power of theta, alpha and beta rhythms was analyzed on the EEG. Results and conclusion. In mild depressive disorders, a decrease in the level of spatial working memory was observed; on the EEG, this corresponded to higher values of the power of the theta rhythm in the frontal and occipital regions and alpha rhythm in the frontal cortex. nine0003
Determination of the features of impaired spatial working memory and their neurophysiological correlates in patients with mild depressive disorders. Material and methods. We examined 30 patients (right-handed) with a diagnosis of ICD-10 "Mood disorders" (headings F31.3, F32.0, F33.0, F34.1) before the start of treatment. The average age of patients is 37±8 years. As a control group, 30 mentally and somatically healthy people (mean age 32 ± 7 years) were examined. The study of spatial working memory was carried out using the Corsi Block-Tapping test. Electroencephalography (EEG) was also performed. The spectral power of theta, alpha and beta rhythms was analyzed on the EEG. Results and conclusion. In mild depressive disorders, a decrease in the level of spatial working memory was observed; on the EEG, this corresponded to higher values of the power of the theta rhythm in the frontal and occipital regions and alpha rhythm in the frontal cortex. nine0003
Keywords:
depression
cognitive functions
spatial working memory
electroencephalographic correlates
Authors:
Galkin S. A.
A.
Research Institute of Mental Health, Tomsk National Research Medical Center of the Russian Academy of Sciences, Tomsk, Russia
Peshkovskaya A.G.
Research Institute of Mental Health, Siberian Branch of the Russian Academy of Medical Sciences, Tomsk
Simutkin G.G.
Research Institute of Mental Health of the Tomsk National Research Medical Center of the Russian Academy of Sciences, Tomsk, Russia
Vasilyeva S.N.
Roshina O.V.
Research Institute of Mental Health, Tomsk National Research Medical Center of the Russian Academy of Sciences, Tomsk, Russia
Ivanova S.A.
Research Institute of Mental Health, Siberian Branch of the Russian Academy of Medical Sciences, Tomsk
Bohan N.A.
Research Institute of Mental Health, Tomsk Scientific Center, Siberian Branch of the Russian Academy of Medical Sciences
Close metadata
Introduction
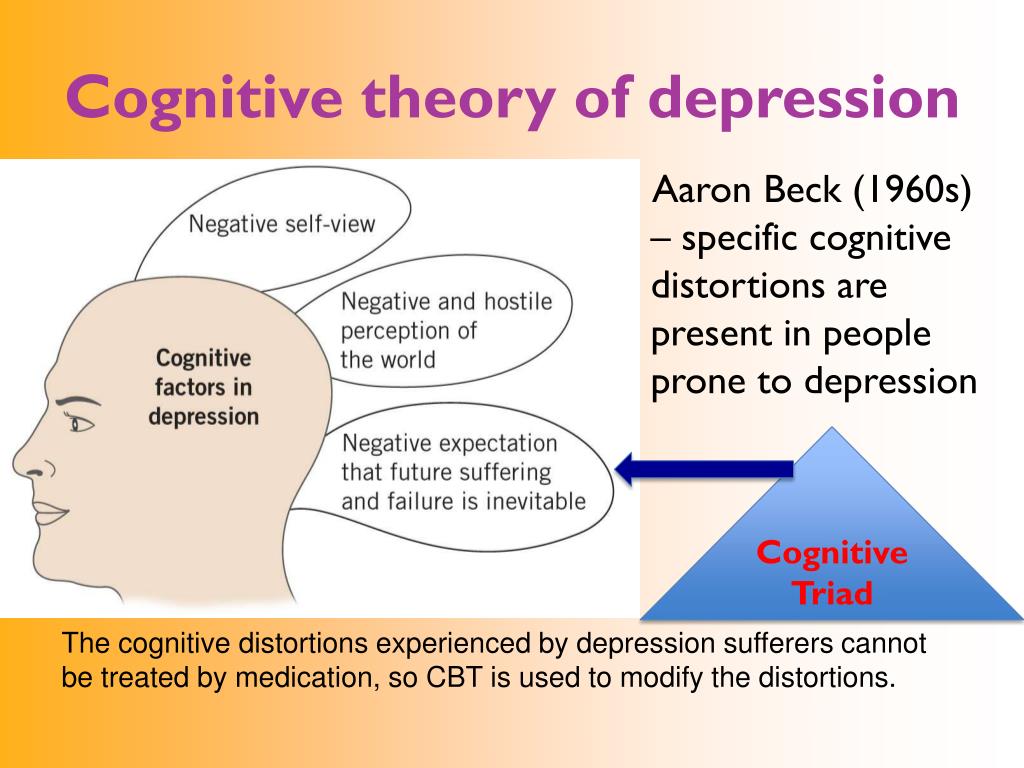
Currently, research on cognitive impairment in mood disorders focuses mainly on information processing, but other cognitive functions such as attention, thinking, and memory may be altered in depressed patients [1-3]. It was found [1, 4] that, in depression, there are, in particular, functional impairments of executive functions and working memory (WP). nine0003
It was found [1, 4] that, in depression, there are, in particular, functional impairments of executive functions and working memory (WP). nine0003
RP - a system that provides temporary storage of information; the basis of many cognitive functions, such as understanding speech, thinking, problem solving, and learning [1]. Neuroimaging studies have shown that dysfunction of the prefrontal cortex reduces the level of RP in patients with major depressive disorder [5]. In a number of studies in which the n-back test was used to study RP (it is required to remember a set of pictures, then a new set is presented, as an answer it is necessary to determine the number of matches with the previous set), it was found that the fidelity of character reproduction was less, and the response time was significantly higher in patients with depression than in healthy individuals [6]. Studies show that negative emotions have different effects on spatial RP in healthy people and patients with depressive disorders of varying severity [5, 6]. For example, in a study of patients with mild depression, it was found that negative emotions did not affect the memorization of words, but they did affect the spatial RP, manifested by a decrease in the ability to memorize a sequence of characters [7]. In other studies [1, 5], when examining patients with severe depression, more severe cognitive impairments were found [1, 5]. As is known, spatial RP requires more attention resources compared to text (non-spatial) memory [7]. Some authors suggest that the evaluation of the spatial RP in patients with depression is a more objective method for diagnosing cognitive impairments [1, 7]. To assess the spatial RP, many researchers use the Corsi Block-Tapping Test [8, 9].
For example, in a study of patients with mild depression, it was found that negative emotions did not affect the memorization of words, but they did affect the spatial RP, manifested by a decrease in the ability to memorize a sequence of characters [7]. In other studies [1, 5], when examining patients with severe depression, more severe cognitive impairments were found [1, 5]. As is known, spatial RP requires more attention resources compared to text (non-spatial) memory [7]. Some authors suggest that the evaluation of the spatial RP in patients with depression is a more objective method for diagnosing cognitive impairments [1, 7]. To assess the spatial RP, many researchers use the Corsi Block-Tapping Test [8, 9].
Assessing the state of the problem in general, it should be noted that most of the previous studies have focused on the evaluation of RP in patients with severe depression, and less data on mild depression, in which social and professional impairments are less pronounced. Currently, there is also insufficient data on the neurophysiological foundations of spatial RP in normal and pathological conditions.
Currently, there is also insufficient data on the neurophysiological foundations of spatial RP in normal and pathological conditions.
The purpose of this study is to evaluate spatial RP disorders and to determine their neurophysiological correlates in patients with mild current depression. nine0003
Material and methods
The study was carried out on the basis of the department of affective disorders of the clinic of the Mental Health Research Institute according to the protocol approved by the local ethics committee of this institute.
30 patients (23 women and 7 men) were examined. The median age of patients was 37 years [28; 42].
According to ICD-10, all the examined patients were diagnosed with mood disorders, mild current depressive episode or dysthymia. nine0003
The distribution of patients by category was as follows: F31.3 - 7 people, F32.0 - 9, F33.0 - 5, F34.1 - 9.
ICD-10, informed consent of the patient to participate in the study, age 18-65 years.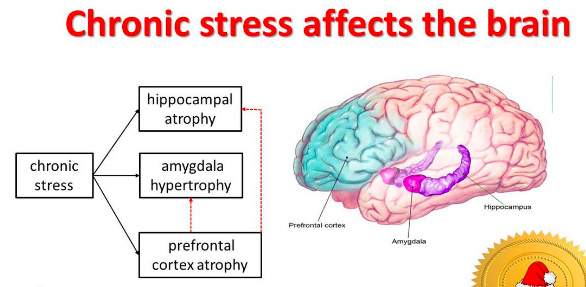 Criteria for non-inclusion : the presence of severe organic disorders of the brain, mental retardation, epilepsy.
Criteria for non-inclusion : the presence of severe organic disorders of the brain, mental retardation, epilepsy.
The control group consisted of 30 mentally and somatically healthy people (20 women and 10 men), comparable in age to the group of patients — a median of 34 years [25; 40]. nine0003
When examining the spatial RP, 9 cubes appear on the computer screen, which turn yellow in turn. The task of the research participant is to remember and reproduce this sequence. The test begins with a sequence of two cubes, with a correct answer, the length of the sequence increases. The test is terminated in the event of two successive erroneous reproductions of the sequence.
To assess the neurophysiological correlates of spatial RP, electroencephalography (EEG) was used, which is considered one of the most adequate methods for assessing the functional state of brain structures [10, 11]. The EEG was recorded using a 16-channel neuropolygraph encephalograph using the 10–20 international system.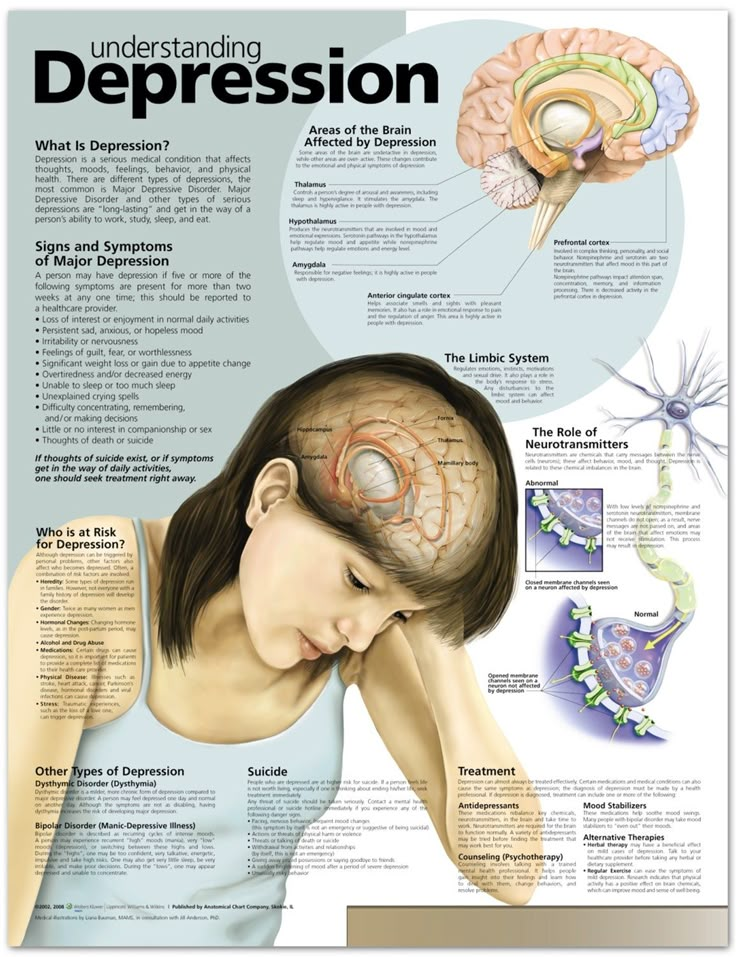 First, a test was performed with eyes closed during a 5-minute rest, then a 2-minute test with eyes opening (background), after which the participant performed the Corsi test simultaneously with the registration of brain biopotentials. Artifact fragments were removed from the obtained EEG records using ICA analysis. The signals were processed using the fast Fourier transform, and the values of the absolute spectral power (µV 2 ) theta - (4-7 Hz), alpha - (8-13 Hz) and beta - (14-30 Hz) rhythms. The cutoff frequencies of the high and low pass filters were 30 and 1.5 Hz.
First, a test was performed with eyes closed during a 5-minute rest, then a 2-minute test with eyes opening (background), after which the participant performed the Corsi test simultaneously with the registration of brain biopotentials. Artifact fragments were removed from the obtained EEG records using ICA analysis. The signals were processed using the fast Fourier transform, and the values of the absolute spectral power (µV 2 ) theta - (4-7 Hz), alpha - (8-13 Hz) and beta - (14-30 Hz) rhythms. The cutoff frequencies of the high and low pass filters were 30 and 1.5 Hz.
Statistical data processing was performed using SPSS Statistics 17.0 software. Results are presented as Median [Q1; Q3]. The agreement with the normal distribution law was checked using the Shapiro–Wilk test. The obtained data did not obey the normal distribution law. Non-parametric U 9009 used3-Mann-Whitney test for assessing differences between two independent samples (control versus patients) and W Wilcoxon test for assessing differences between two dependent samples (background versus test).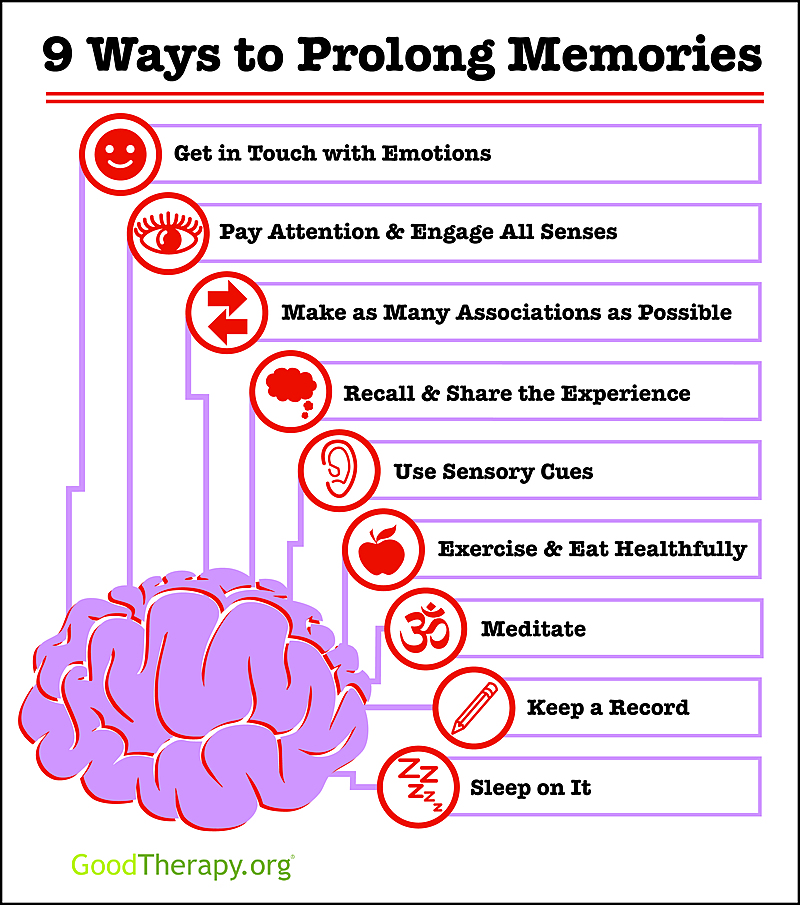 Differences were considered statistically significant at a significance level of p <0.05.
Differences were considered statistically significant at a significance level of p <0.05.
Results
Statistical analysis of Corsi test data between groups is presented in Table. 1.
Table 1. Results of the Corsi test in the study groups Note. Me[Q1; Q3]; p is the level of statistical significance when comparing groups using the Mann-Whitney U-test. nine0040 Received a statistically significant reduction in the maximum number of correctly reproduced sequence in the group of patients compared with the control ( p = 0.01).Statistical analysis of the EEG showed the presence of both intragroup and intergroup changes in theta, alpha, and beta rhythms (Fig. 1—3).
Fig. 2. Spectral power of the alpha rhythm in the control and patient groups. * — level of statistical significance at p<0.05. Fig. 1. 3. Spectral power of the beta rhythm in the control and patient groups. Fig. 3. Beta-rhythm spectral power in control groups and patients. * — level of statistical significance at p<0.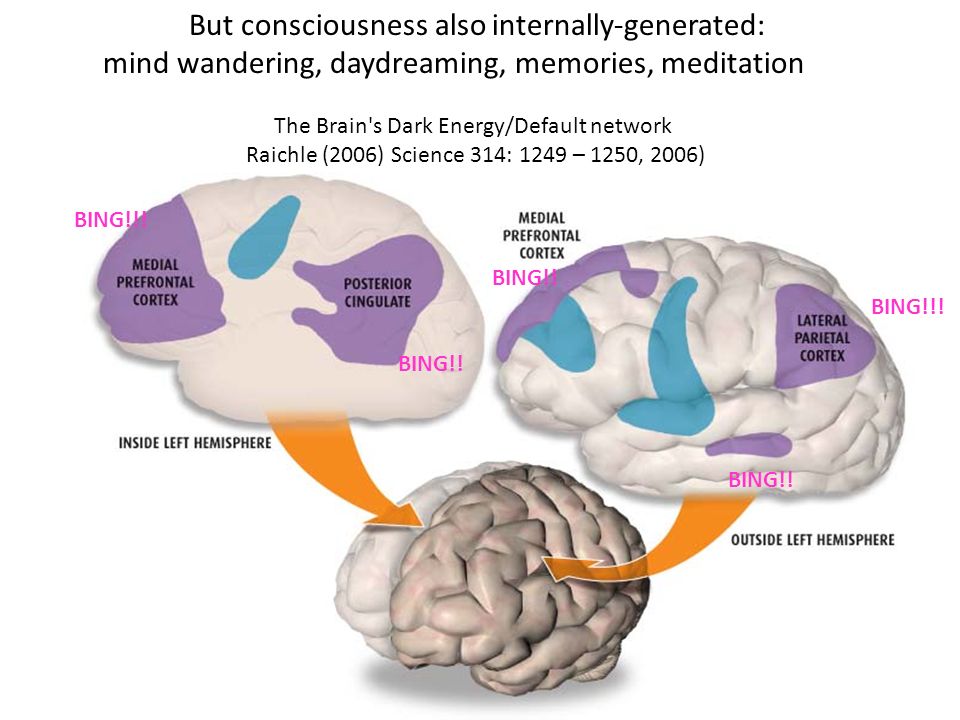 05. Fig. 1. 1. Spectral power of theta rhythm in the control and patient groups. * — level of statistical significance at p<0.05. nine0002 From fig. Table 1 shows that during the test, there is a statistically significant increase in the theta rhythm in the frontal region of the cerebral cortex in the group of patients ( p = 0.00004) and control ( p = 0.0014). However, comparison of the theta power during the test between the study groups (lower left fragment) showed a more significant increase in the theta rhythm in the frontal ( p = 0.0017) and occipital cortex ( p = 0.028) in patients. At the same time, the background recordings (lower right fragment) differed statistically significantly only in the temporal leads on the left ( p = 0.026) and on the right ( p = 0.013).
05. Fig. 1. 1. Spectral power of theta rhythm in the control and patient groups. * — level of statistical significance at p<0.05. nine0002 From fig. Table 1 shows that during the test, there is a statistically significant increase in the theta rhythm in the frontal region of the cerebral cortex in the group of patients ( p = 0.00004) and control ( p = 0.0014). However, comparison of the theta power during the test between the study groups (lower left fragment) showed a more significant increase in the theta rhythm in the frontal ( p = 0.0017) and occipital cortex ( p = 0.028) in patients. At the same time, the background recordings (lower right fragment) differed statistically significantly only in the temporal leads on the left ( p = 0.026) and on the right ( p = 0.013). Changes in the alpha rhythm are shown in fig. 2: during the test, there is a statistically significant decrease in the power of the alpha rhythm in the central and parietal areas of the cortex in the control group ( p = 0. 012 and p = 0.007) and in patients ( p = 0.029 and p = 0.029 and p = 0.0002). Comparison of alpha rhythm power during the test between groups showed statistically significant differences in the frontal cortex ( p = 0.001).
As shown in fig. 3, the test execution caused a statistically significant increase in the power of the beta rhythm in the parietal ( p = 0.02) and occipital ( p = 0.001) cortex in the control group. However, in the group of patients, a significant increase in the beta rhythm was observed only in the temporal lobes on the left ( p = 0.001) and on the right ( p = 0.004). In the group of patients, higher values of the background power of the beta rhythm were observed in the frontal ( p = 0.001), central ( p = 0.00007) and parietal ( p = 0.0015) cortex (lower right fragment).
Discussion
In the present study, the state of spatial RP and EEG changes during the Corsi test in patients with mild current depression compared with healthy individuals (control) were determined. It was found that with mild depression, the level of spatial RP decreases. These changes are manifested in the difficulty of patients memorizing a sequence of characters and, as a result, a decrease in memory volume, which is consistent with the data of other studies [4, 6, 7]. Some authors suggest that the impact of negative emotions on memory is characterized by competition for attention resources [1, 12]. nine0003
It was found that with mild depression, the level of spatial RP decreases. These changes are manifested in the difficulty of patients memorizing a sequence of characters and, as a result, a decrease in memory volume, which is consistent with the data of other studies [4, 6, 7]. Some authors suggest that the impact of negative emotions on memory is characterized by competition for attention resources [1, 12]. nine0003
The results of an electrophysiological study should be considered in two aspects: within-group differences in response to cognitive load (background versus test) and between-group differences (control versus patients), as well as in relation to individual rhythms of bioelectrical activity.
During the performance of the Corsi test on the EEG in both groups, an increase in the power of the theta rhythm in the frontal cortex of the brain was observed in comparison with the initial level. A number of studies have reported such an increase in theta rhythm during the performance of various cognitive tasks [10]. However, in a cross-group comparison of evoked theta activity, patients showed higher values of theta rhythm in the frontal and occipital cortex. It is believed that an increase in the power of the theta rhythm is associated with an activation reaction in the cortex. Thus, it can be assumed that in order to perform tasks with a cognitive load, patients require more activation and, as a result, more resources. It should be noted that patients at rest (background) showed a statistically significant increase in theta rhythm in the temporal lobes. In previous studies, this fact was demonstrated by a number of authors [13, 14], who showed that depression is characterized by an increase in theta activity in the temporal regions of the brain. nine0003
However, in a cross-group comparison of evoked theta activity, patients showed higher values of theta rhythm in the frontal and occipital cortex. It is believed that an increase in the power of the theta rhythm is associated with an activation reaction in the cortex. Thus, it can be assumed that in order to perform tasks with a cognitive load, patients require more activation and, as a result, more resources. It should be noted that patients at rest (background) showed a statistically significant increase in theta rhythm in the temporal lobes. In previous studies, this fact was demonstrated by a number of authors [13, 14], who showed that depression is characterized by an increase in theta activity in the temporal regions of the brain. nine0003
As for the alpha rhythm, during the performance of a cognitive task (test) on the EEG, its depression was observed in the central and parietal areas of the cerebral cortex in both studied samples. The data obtained are characteristic of the activation reaction (decrease in the alpha rhythm) of brain neurons, which is confirmed by numerous studies [9].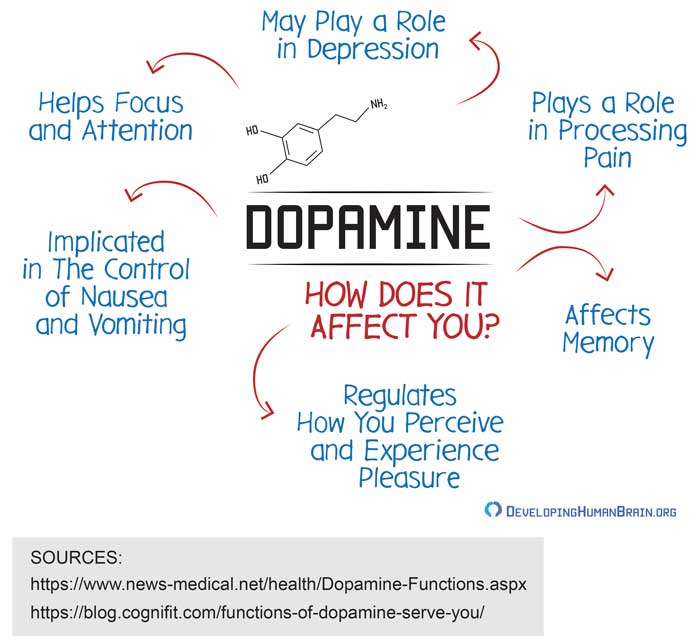 In the intergroup comparison of evoked activity in the group of patients, the power of the alpha rhythm was significantly higher than in the control group in the frontal cortex. In a more detailed analysis, it was found that the increase in the power of the alpha rhythm in patients in response to a cognitive stimulus in the frontal region negatively correlated with the maximum amount of correctly reproduced sequence. Based on the results of the study of neuronal activity using fMRI and PET, it was suggested that the information stored in the central (the "What" system) and parietal (the "Where" system) cortex is read out to the neurons of the prefrontal cortex of the brain, which acts as a short-term buffer during cognitive and executive activity [13]. Thus, a significant decrease in activation during the test (higher values of alpha rhythm power) in the frontal cortex in patients with affective disorders may indicate dysfunction of this brain region. nine0003
In the intergroup comparison of evoked activity in the group of patients, the power of the alpha rhythm was significantly higher than in the control group in the frontal cortex. In a more detailed analysis, it was found that the increase in the power of the alpha rhythm in patients in response to a cognitive stimulus in the frontal region negatively correlated with the maximum amount of correctly reproduced sequence. Based on the results of the study of neuronal activity using fMRI and PET, it was suggested that the information stored in the central (the "What" system) and parietal (the "Where" system) cortex is read out to the neurons of the prefrontal cortex of the brain, which acts as a short-term buffer during cognitive and executive activity [13]. Thus, a significant decrease in activation during the test (higher values of alpha rhythm power) in the frontal cortex in patients with affective disorders may indicate dysfunction of this brain region. nine0003
As noted above, a significant increase in beta activity was observed during the performance of the cognitive task.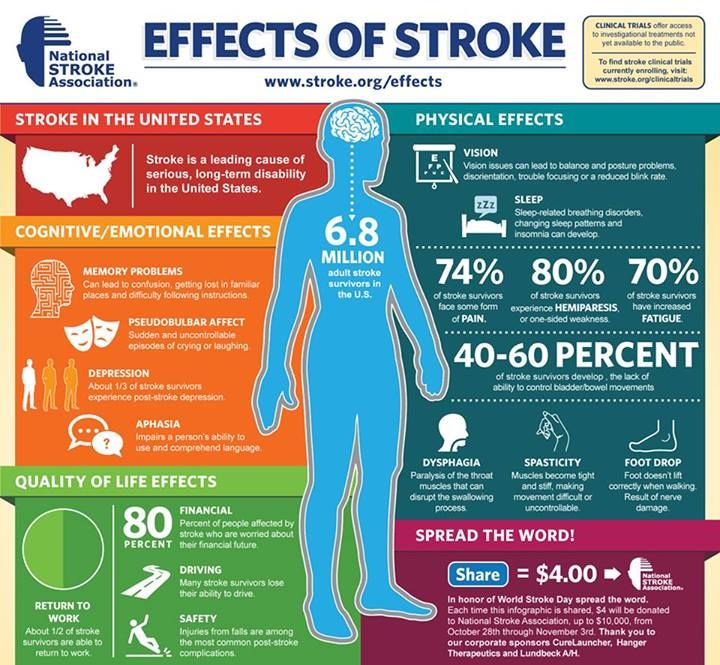 It is known that an increase in the power of the beta rhythm correlates with an increase in the excitability, reactivity, and lability of cortical neurons [13]. However, the localization of changes in the beta rhythm in patients with affective disorders is different than in individuals from the control group. In addition, when comparing the background beta activity between the studied groups, patients were characterized by higher values of the beta rhythm in the frontal centroparietal region of the brain, which indicates a general desynchronization of bioelectrical activity and a change in the functional state of the cortex. These changes likely accounted for the statistically significant differences in evoked beta activity between groups. nine0003
It is known that an increase in the power of the beta rhythm correlates with an increase in the excitability, reactivity, and lability of cortical neurons [13]. However, the localization of changes in the beta rhythm in patients with affective disorders is different than in individuals from the control group. In addition, when comparing the background beta activity between the studied groups, patients were characterized by higher values of the beta rhythm in the frontal centroparietal region of the brain, which indicates a general desynchronization of bioelectrical activity and a change in the functional state of the cortex. These changes likely accounted for the statistically significant differences in evoked beta activity between groups. nine0003
Summarizing the results of the Corsi test and EEG data, we can conclude that in mild depression there is a deficit of spatial RP, the EEG correlates of which are higher values of the power of the theta rhythm in the frontal and occipital regions and the alpha rhythm in the frontal cortex.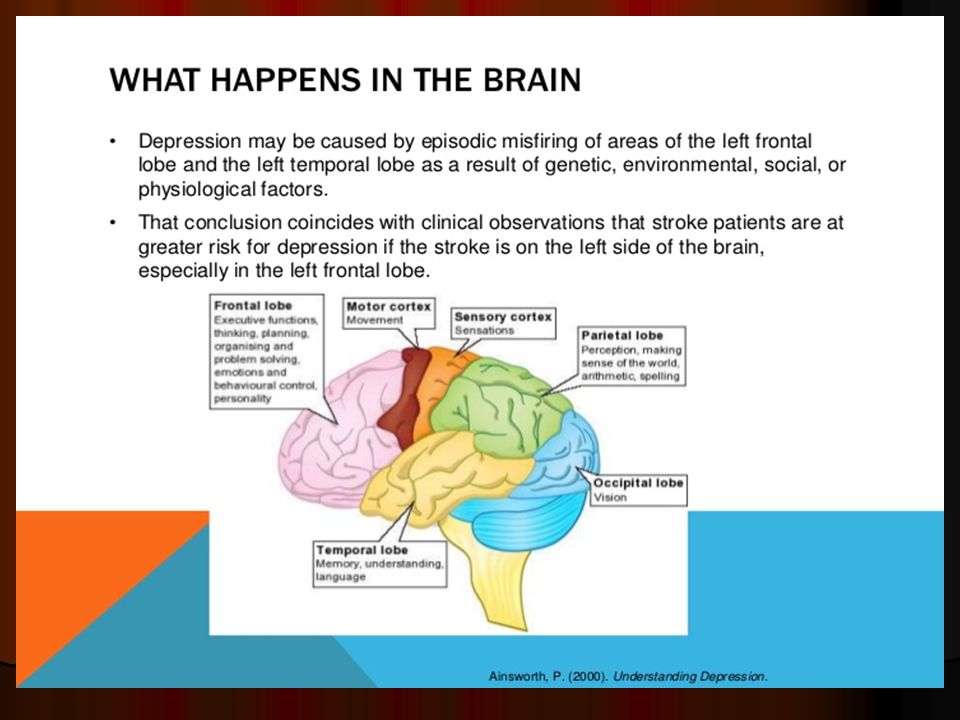 Also important is the atypical localization of changes in beta activity in the temporal regions of the brain in patients during the Corsi test.
Also important is the atypical localization of changes in beta activity in the temporal regions of the brain in patients during the Corsi test.
There is reason to believe that further research into the dynamics of cognitive deficits in patients with affective disorders may contribute to a deeper understanding of the nature of the disease and the development of more effective therapies. nine0003
The study was supported by the Russian Foundation for Basic Research within the framework of the scientific project No. 18-313-00147.
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Information about the authors
Galkin S.A. — https://orcid.org/0000-0002-7709-3917
Peshkovskaya A.G. nine0093 - https://orcid.org/0000-0002-3951-395X
Simutkin G.G. - https://orcid.org/0000-0002-9813-3789
Vasilyeva S.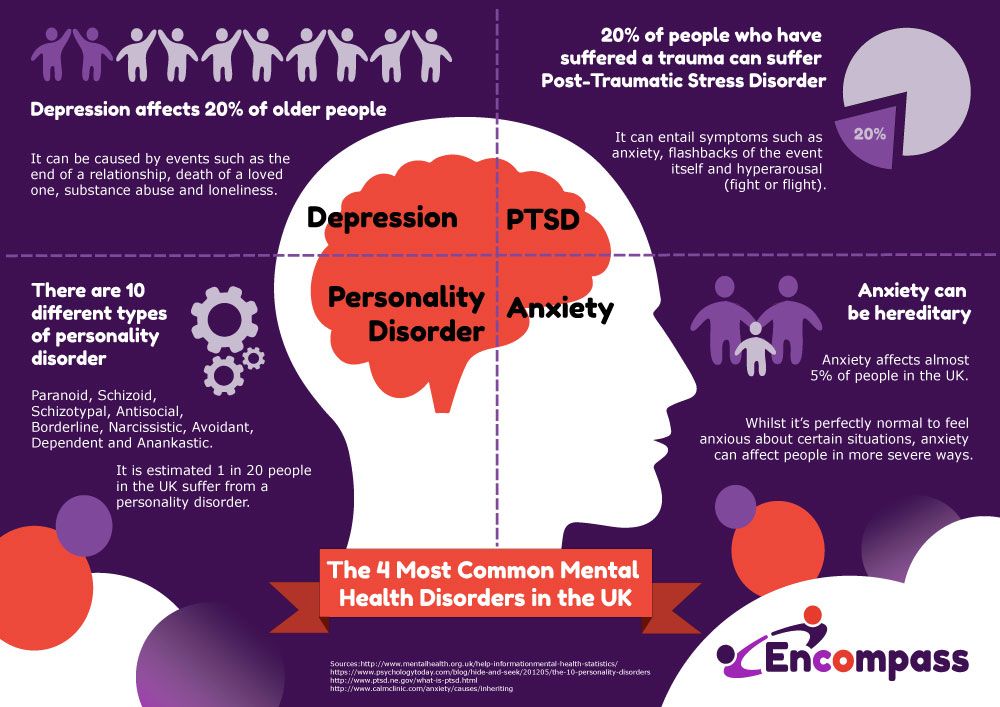
Learn more