Psychotic eyes and their significance
Eye Characteristics of Schizophrenia
You may not be able to tell if someone has schizophrenia just by looking at their eyes. But certain characteristics and behaviors of a person’s eyes are associated with this mental health condition.
Eye symptoms like a fixed gaze, along with other indications, may point to some types of schizophrenia. A mental health professional can sometimes use these symptoms to determine if a person has this condition.
Read on for an explanation of eye movements and characteristics related to schizophrenia and why they happen.
Visual changes are very common in people who have schizophrenia. Common changes can include:
Nystagmus
If you live with schizophrenia, you might experience involuntary, repetitive eye movements. This is known as nystagmus, which may be a side effect of some medications or caused by atypical characteristics in your:
- optic tract (eye nerves in your brain)
- brain
- inner ear
Your eyes might move:
- side to side
- up and down
- in a circular pattern
Smooth pursuit eye movements (SPEM)
People with schizophrenia and their relatives may experience atypical eye movements when following a moving object. Research suggests that unusual SPEM can occur in 50 to 85 percent of people with schizophrenia.
Strabismus
Also known as “crossed eyes,” strabismus occurs when your eyes are not looking in the same direction. In most cases, one eye turns in more than the other, but one eye may turn out as well. Strabismus is associated with schizophrenia.
Impaired visual acuity
Visual acuity describes the sharpness of a person’s vision. People with schizophrenia have lower visual acuity. Psychiatric medications may affect your vision.
Corneal temperature
Someone with schizophrenia may have a significantly higher corneal temperature.
Increased blink rate
People with schizophrenia often blink faster than people without this mental health condition.
Atypical retinal characteristics
The retina is a thin layer of tissue lining the back of the eye. Individuals with schizophrenia may have atypical structural characteristics of their retinas.
Visual processing impairments
Visual processing involves interpreting things you see. Impairment in visual processing is also common in people with schizophrenia. These impairments can include:
- difficulties in contrast sensitivity, the abilkity to see varying shades of light and dark
- difficulty with form and motion processing, the ability to process speed and movement in objects
- visual distortions, objects may look bent or wavy
You may not be able to tell if someone has schizophrenia just by looking at their eyes. You might notice an atypical gaze or stare, but you will not be able to tell if a person has schizophrenia from that alone.
There are a variety of symptoms of schizophrenia. Symptoms are typically grouped into two categories: positive and negative.
The categorization reflects activity in your brain. Increased activity in specific brain areas causes positive symptoms, and decreased activity of other areas causes negative symptoms.
Positive symptoms respond well to therapeutic medications. These symptoms can include:
- disordered thoughts and speech
- hallucinations and delusions
Negative symptoms do not respond as well to medications. These symptoms might include:
- lack of desire for social contact
- trouble or inability to feel pleasure
- difficulty functioning
Medical professionals are not sure exactly what causes eye changes in people with schizophrenia. But some research suggests that genetics play a role. Specific genes like RGS4 and the catechol-O-methyltransferase (COMT) gene are associated with schizophrenia and changes in a person’s eye tracking.
Eye inflammation may also be linked to schizophrenia. People with this mental health condition sometimes have elevated blood markers of inflammation, which suggests that an infection might be causing some of these eye symptoms.
Researchers have also found changes in chromosome 6 in some people with schizophrenia. This chromosome is involved in the immune response, and changes in this chromosome may affect how an individual responds to infection and the level of inflammation in their body.
This chromosome is involved in the immune response, and changes in this chromosome may affect how an individual responds to infection and the level of inflammation in their body.
Individuals with schizophrenia may show symptoms of atypical characteristics in parts of their brain during visual processing tasks. These characteristics can affect input to their visual system.
More research is needed to find out possible causes of eye changes associated with schizophrenia.
Eye changes in people with schizophrenia may be related to several factors.
Widening of small veins in the retinas, known as the retinal venules, may cause symptoms of psychosis in childhood and adulthood. Experiencing visual distortions may also indicate that a person has a mental health condition.
If you have schizophrenia, the fluctuations of dopamine that occur in your brain might also occur in your retina. This can affect your visual processing and eye movement.
Medical professionals need more research to determine the full risk factors for eye changes in people with schizophrenia. If you have concerns, talk with your doctor and contact an eye specialist. They can do an eye exam and provide you with appropriate treatments and assistance if needed.
If you have concerns, talk with your doctor and contact an eye specialist. They can do an eye exam and provide you with appropriate treatments and assistance if needed.
Finding care for schizophrenia
If you or a friend or loved one has schizophrenia, here are resources to find help:
- National Alliance on Mental Illness (NAMI) HelpLine page
- Substance Abuse and Mental Health Services Administration (SAMHSA) Behavioral Health Treatment Services Locator
- Schizophrenia & Psychosis Action Alliance
There’s no cure for schizophrenia, but a mental health professional can help you manage this condition.
You may receive a variety of treatments to help with your symptoms. Your treatment team can talk with you and determine the best treatment for your situation and symptoms.
Treatments can include:
- medication
- therapy or social skills training
- vocational rehabilitation, or job skills training
- inpatient hospital care
Sometimes people pursue complementary medication like vitamins and supplements, but it’s always best to speak with your doctor before doing so. Your doctor can let you know if this method will interfere with any medications you’re taking and whether it’s safe to try.
Your doctor can let you know if this method will interfere with any medications you’re taking and whether it’s safe to try.
Treating eye-related symptoms
While there’s no specific treatment for eye symptoms related to schizophrenia, a medical professional can help diagnose and treat any underlying infection and associated inflammation related to atypical eye characteristics.
While a mental health professional can’t cure schizophrenia, they can help you manage it. With proper diagnosis and appropriate treatment, your symptoms may decrease.
The exact outlook can vary, depending on the seriousness of your schizophrenia and whether you follow your treatment plan. With medication, counseling, and social support, you can reduce your symptoms and improve your quality of life.
People with schizophrenia may have structural eye changes and movements.
Although experienced mental health professionals may add these symptoms to their clinical observations, they can’t diagnose schizophrenia in a person based on these characteristics alone.
If you have schizophrenia and are experiencing visual symptoms, talk with your doctor and contact an eye specialist. They will be able to do an exam and let you know how they can help you.
Eyes hint at hidden mental-health conditions
Credit: Taj Francis
Schizophrenia — a severe mental-health condition that often involves psychosis — has long been an enigma. Before the early twentieth century, psychiatrists thought that it comprised several disorders, which were given labels such as ‘catatonic syndrome’ or ‘adolescent insanity’. And for much of the past century, researchers considered schizophrenia to be an illness of only the mind, and sometimes even attributed it to bad parenting. Although it has since been established that schizophrenia’s symptoms have biological origins, and some risk factors have been identified, its precise causes remain unclear, and its diagnosis is complicated and can be subjective.
Part of Nature Outlook: The eye
To improve diagnosis and tracking of schizophrenia, researchers have been hunting for biomarkers — measurable physiological signals that can indicate a condition’s onset and progression. And in the past decade, research has begun to point to a promising source of such signals: the eye. For instance, the thickness of a person’s retina — the layer of light-sensitive tissue at the back of the eye — or the retina’s response to light could provide early signs that an individual is affected by or at risk of schizophrenia. “The retina is essentially a proxy for what’s happening in the brain,” says Steven Silverstein, a clinical psychiatrist at Rutgers University in Piscataway, New Jersey.
And in the past decade, research has begun to point to a promising source of such signals: the eye. For instance, the thickness of a person’s retina — the layer of light-sensitive tissue at the back of the eye — or the retina’s response to light could provide early signs that an individual is affected by or at risk of schizophrenia. “The retina is essentially a proxy for what’s happening in the brain,” says Steven Silverstein, a clinical psychiatrist at Rutgers University in Piscataway, New Jersey.
The potential to use the eye as a window on the brain goes beyond just schizophrenia. As understanding of the links between eye and brain health deepens, evidence is building that changes in the condition or function of the eye can hint at the presence and progression of neurological disorders, as well as brain injuries such as concussion. With that in mind, researchers are now taking advantage of improved imaging technology to develop simple, minimally invasive tools for examining the eye and vision to help screen for, diagnose and monitor neurological and mental-health conditions.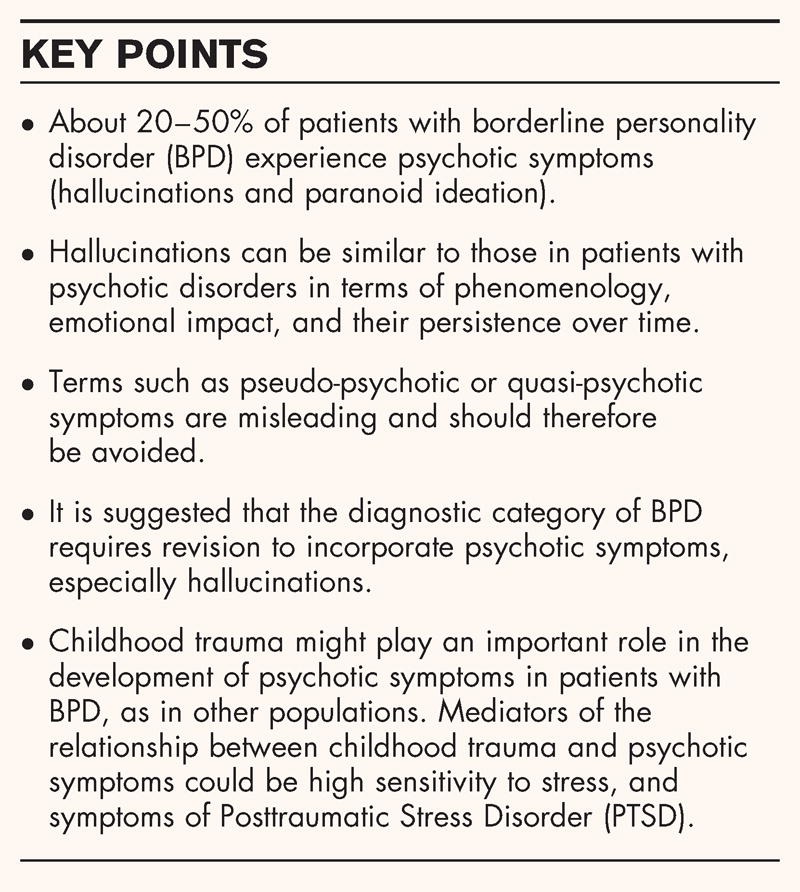
Vision changes
Vision is thought to require the use of about half of the brain’s neural pathways, says Laura Balcer, a neuro-ophthalmologist at New York University Langone Health in New York City. Anything that affects a person’s brain — whether it be a disease or a blow to the head — therefore has a strong chance of affecting their sight. Indeed, researchers have known for decades that certain neurological disorders can bring about changes in vision and eye motion.
Much of the work to assess neurological conditions through the eye has been done in the context of multiple sclerosis. In this disorder, the immune system disrupts communication in the central nervous system by attacking myelin, a fatty substance that forms a protective layer around nerve fibres. The process damages several parts of the brain, including those involved in pathways that are responsible for vision, and the optic nerve, which carries impulses between the eye and the brain.
Although people with multiple sclerosis often report having vision problems, standard eye tests — in which a person reads letters printed in black from a chart with a white background — typically fail to uncover any issues. So, in the early 2000s, Balcer and her collaborator Steven Galetta, also a neuro-ophthalmologist at Langone Health, helped to develop an alternative test that uses the Sloan low-contrast letter-acuity chart, in which a person has to identify grey letters on a white background — a task that is more difficult for people with multiple sclerosis, because they require greater levels of contrast than do people without the condition. The test has since become the leading tool for monitoring and studying vision problems associated with the condition.
So, in the early 2000s, Balcer and her collaborator Steven Galetta, also a neuro-ophthalmologist at Langone Health, helped to develop an alternative test that uses the Sloan low-contrast letter-acuity chart, in which a person has to identify grey letters on a white background — a task that is more difficult for people with multiple sclerosis, because they require greater levels of contrast than do people without the condition. The test has since become the leading tool for monitoring and studying vision problems associated with the condition.
Researchers are also developing tests that make use of other visual pathways to diagnose multiple sclerosis. The King-Devick test, developed by King-Devick technologies in Oakbrook Terrace, Illinois, assesses the brain pathways that control eye movement by requiring a person to read rapidly from a page of single-digit numbers. And a test known as the Mobile Universal Lexicon Evaluation System (MULES) asks participants to name images of objects as fast as they can to test pathways for colour perception, memory and object recognition.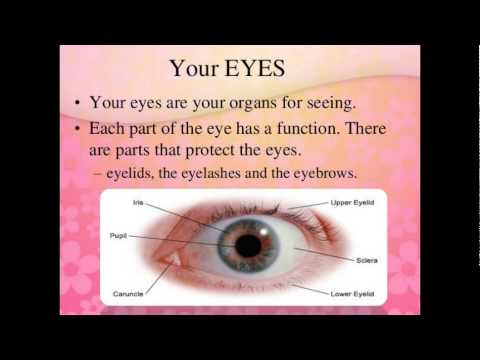
These new tests can also help to diagnose concussion that is incurred while playing sport. Currently, a medical professional or athletic trainer has to assess a person for a range of symptoms, including dizziness, nausea and general confusion — a task that is often subjective. Simple tests of visual pathways, however, could provide an objective and standardized procedure for assessing concussion that can be performed anywhere — including at sporting events. In May 2018, US racing company NASCAR announced that it would begin to use the King-Devick test to assess drivers who are involved in crashes.
Mapping the eye
Neurological injuries and disorders can also cause physical damage to the retina and optic nerve that could give researchers an insight into the underlying condition. That’s because the brain and the eye are linked physically by the optic nerve. In fact, certain parts of the eye, including the retina, are essentially an extension of the brain, having developed from the same embryonic tissue.
Examining the retina has become much easier since the advent of a non-invasive imaging technique called optical coherence tomography (OCT), about 30 years ago. In OCT, the eye is scanned with a beam of light. The light that is reflected back is analysed to produce a 3D image of the retina. Used mainly to monitor and diagnose eye conditions such as glaucoma or age-related macular degeneration, OCT has now become a tool for studying, monitoring and potentially diagnosing neurological disorders.
The technique has revealed, in detail, how multiple sclerosis thins the retina and damages the optic nerve, leading to inflammation — a condition called optic neuritis. And by combining OCT with tests for low-contrast vision, researchers have uncovered a correlation between a thinning retina and vision problems in multiple sclerosis1.
Galetta and Balcer say that OCT-based observations of the optic nerve should be incorporated into standard criteria for diagnosing the condition. At present, such a diagnosis requires the identification of lesions in the central nervous system by magnetic resonance imaging (MRI). Although optic-nerve lesions are often present before symptoms appear, they are rarely used in diagnosis. The optic nerve is difficult to image by MRI because it is small and the eye moves constantly. OCT, however, boasts a resolution that is 1,000 times greater than that of MRI, and the technique is therefore more sensitive to optic-nerve lesions.
At present, such a diagnosis requires the identification of lesions in the central nervous system by magnetic resonance imaging (MRI). Although optic-nerve lesions are often present before symptoms appear, they are rarely used in diagnosis. The optic nerve is difficult to image by MRI because it is small and the eye moves constantly. OCT, however, boasts a resolution that is 1,000 times greater than that of MRI, and the technique is therefore more sensitive to optic-nerve lesions.
OCT also holds promise for identifying early signs of the neurological conditions Parkinson’s disease and Alzheimer’s disease, which could enable people to be treated before symptoms develop. In September, a team of researchers at Seoul National University used OCT to show that thinning of the retina was correlated with both an increasing severity of Parkinson’s disease and the death of neurons that produce the neurotransmitter dopamine2, the loss of which causes Parkinson’s disease.
In November, researchers in the United States combined OCT with angiography, a technique for imaging blood vessels, as part of efforts to find early biomarkers of Alzheimer’s disease. The team compared healthy retinas with those of people who had elevated levels of amyloid-β — a peptide linked to Alzheimer’s disease — but who did not yet exhibit symptoms of the condition. They found that the foveal avascular zone, a region of the retina that lacks blood vessels, was about one-third larger, on average, in people with elevated amyloid-β3.
The team compared healthy retinas with those of people who had elevated levels of amyloid-β — a peptide linked to Alzheimer’s disease — but who did not yet exhibit symptoms of the condition. They found that the foveal avascular zone, a region of the retina that lacks blood vessels, was about one-third larger, on average, in people with elevated amyloid-β3.
The data are limited but promising, says Gregory Van Stavern, a neuro-ophthalmologist at Washington University in St. Louis, Missouri, who co-led the study. “We’re very enthusiastic to see if we can replicate it, and see if we can show this could be a really useful tool for screening down the line,” he says.
From eye to mind
Researchers are also looking to the eye for early biomarkers of neuropsychiatric disease, which could enable clinicians to intervene before their onset or thwart their progression. For instance, there is evidence that, in people with schizophrenia, the small veins, or venules, of the retina are wider and the retina is thinner4.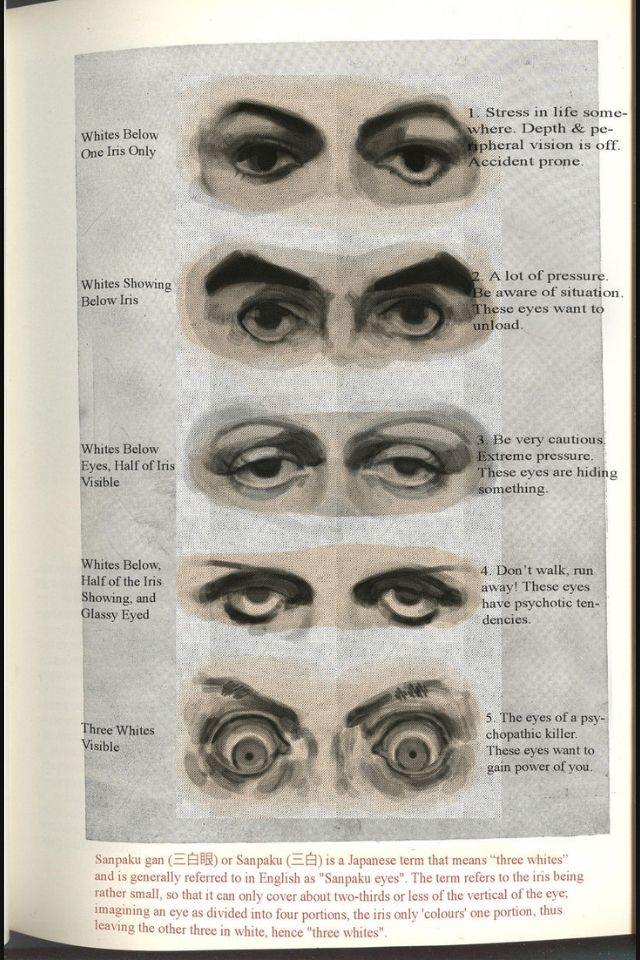
Electroretinography, which measures the retina’s response to light, is being tested as a possible tool for identifying people at risk of developing schizophrenia.Credit: LKC Technologies
Perhaps the most promising tool in the short term for identifying people at risk of developing schizophrenia is electroretinography, a simple and minimally invasive test that measures the retina’s electrical response to light. That signal is captured using a small electrode that is attached to the cheek below the eye or placed under the upper or lower eyelid. “It feels like you have a hair in your eye for about a minute and then you don’t really notice it anymore,” Silverstein says.
A team of researchers led by clinical psychiatrist Michel Maziade at Laval University in Quebec City, Canada, has used electroretinography to identify how the response of light-sensitive cells in the retina called rods and cones changes in people at risk of or diagnosed with neuropsychiatric conditions such as schizophrenia and major depressive disorder5. In 2010, the researchers found that the rods of young people with a high genetic risk of developing schizophrenia respond more weakly to light than do those of young people without that risk6. Individuals considered to be at risk had one parent who had been diagnosed with bipolar disorder or schizophrenia, but showed no symptoms themselves, which suggests that electroretinography can help to identify people who might benefit from medical intervention before symptoms appear. A 2015 study with a larger population size found similar photoreceptor responses to light in 100 adults with schizophrenia7.
In 2010, the researchers found that the rods of young people with a high genetic risk of developing schizophrenia respond more weakly to light than do those of young people without that risk6. Individuals considered to be at risk had one parent who had been diagnosed with bipolar disorder or schizophrenia, but showed no symptoms themselves, which suggests that electroretinography can help to identify people who might benefit from medical intervention before symptoms appear. A 2015 study with a larger population size found similar photoreceptor responses to light in 100 adults with schizophrenia7.
More from Nature Outlooks
The data are impressive, says Anne Giersch, a neuroscientist at the University of Strasbourg in France. But they need to be replicated, she says, and further studies will be required to establish the relationships between the retina and the symptoms of schizophrenia before the technique can be used to help to determine whether treatment is necessary.
Nevertheless, Maziade is confident that electroretinography will soon enter the clinic. In 2015, he co-founded diaMentis, a personalized-medicine company in Quebec City that is developing software for electroretinography-signal analysis. Within three years, Maziade says, the company’s software should be advanced enough to help clinicians to make accurate diagnoses of schizophrenia. Further down the line, clinicians might even be able to use the technique to distinguish between neuropsychiatric disorders. In unpublished work, Maziade says, his team has shown that the electroretinography signals for schizophrenia and bipolar disorder are distinct.
Ethical considerations
As with any screening tool, care must be taken when using emerging techniques to minimize the chances of overdiagnosis or misdiagnosis. No single test such as an electroretinography examination can accurately predict the presence of neurological and mental-health conditions, Maziade says; people would still have to be evaluated in the context of their symptoms, genetics and exposure to environmental factors for clinicians to obtain reliably accurate diagnoses. For instance, if OCT were shown to be effective at detecting Alzheimer’s disease, such screening would probably be targeted at at-risk populations such as older people or those with a family history of the condition. “You have to decide what population you’re going to screen and what you’re going to do with that tool,” Van Stavern says.
For instance, if OCT were shown to be effective at detecting Alzheimer’s disease, such screening would probably be targeted at at-risk populations such as older people or those with a family history of the condition. “You have to decide what population you’re going to screen and what you’re going to do with that tool,” Van Stavern says.
But despite these concerns, eye tests have the potential to change how neurological and mental-health conditions are diagnosed, and Silverstein is excited to see this unusual idea move forward. “I’ve been studying vision and schizophrenia for 30 years,” he says. “Nobody ever thought of looking into the eye.”
Ophthalmological glossary of the clinic Krugozor from A to Z
ABERRATION — image distortion on the retina due to imperfection of the optical system of the eye.
ACCOMMODATION - the ability of the eye to clearly see objects at different distances. Focusing is carried out with the help of the muscles of the eye and the lens.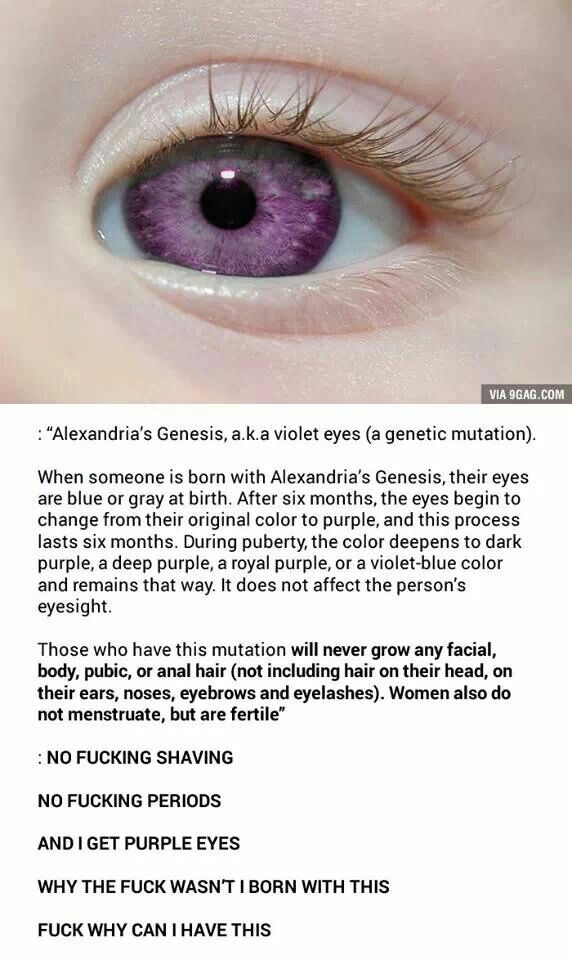 In order to read up close or to see objects at close range clearly, the lens of the eye must increase its curvature, thereby focusing light rays onto the retina.
In order to read up close or to see objects at close range clearly, the lens of the eye must increase its curvature, thereby focusing light rays onto the retina.
ALBINISM (lat. albus - white) - congenital absence of melanin pigment, which gives color to the skin, hair, iris and pigment membranes of the eye. There are complete and partial albinism. Currently, it is believed that the cause of albinism is the absence (or blockade) of the enzyme tyrosinase, which is necessary for the normal synthesis of melanin, a special substance on which the color of tissues depends.
AMBLYOPIA ("lazy eye") - visual impairment of a functional and often secondary nature (in the absence of structural changes in the visual analyzer), which cannot be corrected with glasses or contact lenses. The frequency of amblyopia is about 1-1.5% in the general population.
AMETROPIA is a change in the refractive power of the human eye, the consequence of which is that the back focus of the eye does not fall on the retina when the accommodative muscle is relaxed.
ANISOMETROPIA - an eye disease expressed in different refraction of the eyes. The disease can occur with or without astigmatism.
With this anomaly, one eye may have a normal refraction and the other an impaired one, or both eyes may have the same refractive error, but to a different degree, or the refractive error may be different in both eyes.
ASTHENOPIA - visual discomfort or fatigue that comes on quickly during visual work. Especially often this feeling appears during the work of the eyes at a close distance from the object of attention. Currently, Asthenopia is not considered as a disease. As part of the timely understanding of this phenomenon, it is assessed as a disorder that may precede an already pathological change in vision and even ophthalmological diseases.
ASTIGMATISM is a special kind of optical structure of the eye. Astigmatism is most often caused by an irregular curvature of the cornea: its front surface is not the surface of a ball, where all radii are equal, but a segment of a rotating ellipsoid, where each radius has its own length, and therefore a special refraction that differs from the nearby meridian. Astigmatism in one eye combines the effects of nearsightedness, farsightedness and normal vision. This condition is often congenital and hereditary, but may be the result of surgery or eye trauma. The image of objects with astigmatism is fuzzy, sometimes blurry, straight lines look curved. In addition to defects in visual perception, astigmatism is usually accompanied by rapid eye fatigue, decreased vision, and headaches.
Astigmatism in one eye combines the effects of nearsightedness, farsightedness and normal vision. This condition is often congenital and hereditary, but may be the result of surgery or eye trauma. The image of objects with astigmatism is fuzzy, sometimes blurry, straight lines look curved. In addition to defects in visual perception, astigmatism is usually accompanied by rapid eye fatigue, decreased vision, and headaches.
OPTIC NERVE ATROPHY is a degenerative disease. Most often it occurs as a result of a complication of a viral, infectious or inflammatory eye disease, it can also develop after an injury to the optic nerve. The disease can also be hereditary.
AFAKIA - absence of the lens. The result of surgery (for example, cataract removal), severe trauma, in rare cases, a congenital anomaly.
WELLMO - persistent cicatricial clouding of the cornea of the eye after injury, inflammation or ulceration. Belmo, located against the pupil, reduces vision (sometimes to blindness).
BINOCULAR VISION - the ability to simultaneously clearly see an image of an object with both eyes; in this case, the person sees one image of the object he is looking at. Binocular vision is not innate but develops in the first few months of life. Allows you to clearly see distant objects, and also creates a three-dimensional image.
BIOCOMPATIBILITY (Biocompatibility of a contact lens with the tissues of the eye) is a property of the lens material that allows it to be in contact with the eye without causing allergies, hypersensitivity reactions and other negative effects. Biocompatible lenses have the following properties - high biocompatibility with eye tissues, increased oxygen permeability, resistance to dehydration (loss of moisture), increased surface wettability and resistance to deposit accumulation.
BIFOCAL (glasses, contact lenses) are used to focus both distance and near vision. Used to correct presbyopia. They have two zones of different refraction - for distance (upper) and for near (lower), between which there is a dividing line, as a result of which the refraction from far to near changes abruptly.
BLEPHARITIS - inflammation of the eyelids.
Myopia (myopia) is a refractive error in which parallel light rays focus in front of the retina rather than on it. In this case, a person sees distant objects indistinctly, blurry, since he cannot achieve a clearer image of them with the help of accommodation. Myopia is corrected by wearing special glasses with concave spectacle lenses; at present, it can also be eliminated surgically.
INTRAOCULAR PRESSURE is the fluid pressure inside the eye.
LENS LOSS is a serious ophthalmic disease, manifested in congenital underdevelopment, weakness or partial absence of zinc ligaments, or their rupture due to degeneration or eye injury. One of the varieties of the disease is partial dislocation, or subluxation of the lens, its partial displacement from a permanent point.
Eversion of the eyelids (synonym: ectropion) is a change in the position of one or both eyelids, in which the edge of the eyelid lags behind the eyeball or is turned down, as a result of which the mucous membrane is turned outward. There are spastic, paralytic, senile and cicatricial eversion.
There are spastic, paralytic, senile and cicatricial eversion.
HETEROCROMIA - a color difference in the color of the iris (usually it is congenital, but sometimes it can develop after suffering inflammation of the iris). In the presence of heterochromic irises, the irises of both eyes differ from each other; in the case of a heterochromic iris, one part of the iris differs in color from the other part of it.
HEMERALOPIA or nyctalopia (“night blindness”) is a disorder in which the ability to see in the dark becomes difficult or disappears. It is a symptom of a number of eye diseases. Hemeralopia can be congenital or developed as a result of malnutrition (for example, a lack of vitamin A).
HYPERMETROPIA (farsightedness) is an eye condition in which parallel rays of light are focused behind the retina, resulting in a weakening of the eye's accommodation. A small degree of hypermetropia may not lead to visual impairment in children and young people due to their ability to accommodate, however, in older people, as well as with a high degree of hypermetropia, there is a weakening of near vision compared to far vision.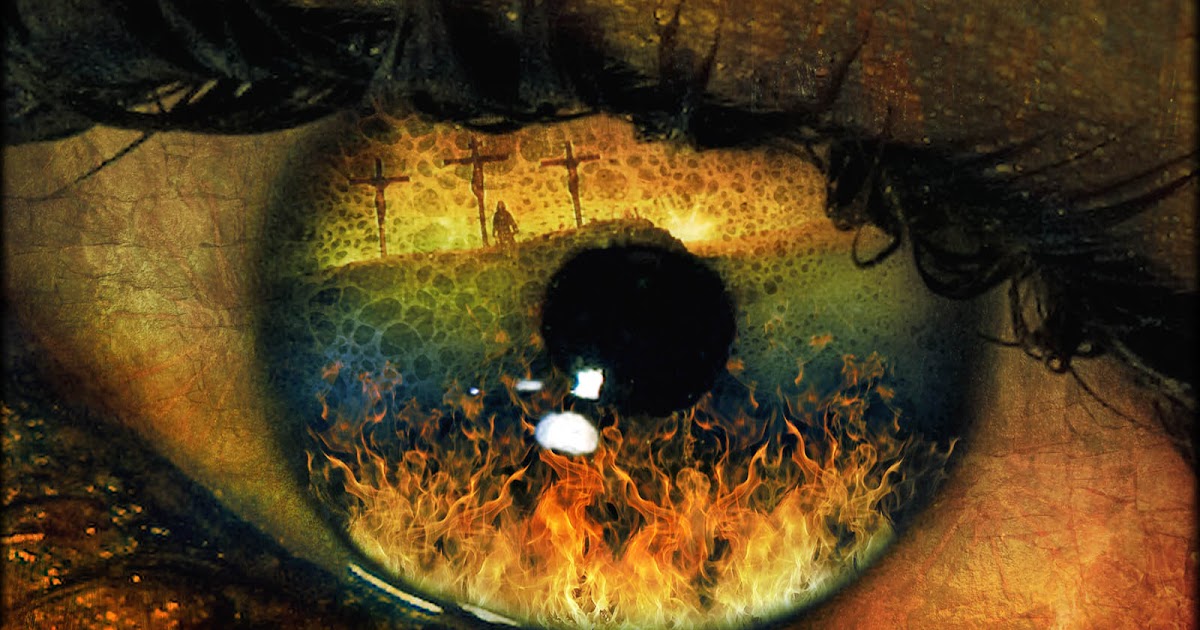 Normal vision can be restored with special glasses with convex spectacle lenses.
Normal vision can be restored with special glasses with convex spectacle lenses.
EYE — a paired organ located in the orbit. The shape of the eye varies from round to oval. In a newborn, the eye is as if squeezed in the anteroposterior direction, so the image goes beyond the eyeball, resulting in farsightedness. As the eyeball grows, such farsightedness disappears. It should be noted that a child is born with an already well-developed organ of vision. From childhood, the eye increases no more than twice.
EYEBALL - the inner surface of the eye as seen through an ophthalmoscope.
EYEBALL — is a spherical chamber containing light-conducting media - the cornea, moisture of the anterior chamber, the lens and gelatinous fluid - the vitreous body, the purpose of which is to refract light rays and focus them in the area of the receptors on the retina. The walls of this spherical chamber are 3 shells. The outer opaque shell - the sclera - passes in front into the transparent cornea. The middle or choroid in front of the eye forms the ciliary body and the iris, which determines the color of the eyes. In the middle of the iris there is a hole - the pupil, which regulates the amount of light rays transmitted into the eye. The inner shell - the retina - contains the photoreceptors of the eye (rods and cones) and serves to convert light energy into nervous excitation.
GLAUCOMA is a chronic eye disease characterized by a constant or periodic increase in intraocular pressure, a special form of optic nerve atrophy (glaucomatous excavation) and characteristic changes in the visual field. There are primary, secondary and congenital glaucoma.
HIPEROPIA (Hypermetropia) - a condition of the eye in which parallel rays of light are focused behind the retina, which leads to a weakening of the accommodation of the eye. A small degree of hypermetropia may not lead to visual impairment in children and young people due to their ability to accommodate, however, in older people, as well as with a high degree of hypermetropia, there is a weakening of near vision compared to far vision. Normal vision can be restored with special glasses with convex spectacle lenses.
Normal vision can be restored with special glasses with convex spectacle lenses.
DIOPTER is the unit of measure for the refraction of the eye.
DIPLOPIA - double vision: taking two images of the same object at the same time. Usually, diplopia is associated with a limitation of the mobility of one eye, so that two eyes cannot look at the same object at the same time. This may be due to a defect in the nerves or muscles that control the movement of the eye, or to a mechanical limitation in the movement of the eyeball in the orbit of the eye. Double vision that does not disappear when one eye is closed may be associated with incipient cataracts.
PUPILE is the hole in the center of the iris that appears black because the inside of the eye is dark (red-eye in flash photography is nothing more than the appearance of a pupil when light reflects off the retina). Pupil size depends on the amount of light falling on the eye, age, degree of focus, and so on.
VISUAL SYSTEM - serves for the perception and analysis of light stimuli. The peripheral part of this system is represented by a complex organ - the eye, containing photoreceptors and the bodies of the first and second neurons. The fibers of the second neurons make up the optic nerve, through which excitation is transmitted to the third neurons in the diencephalon, and then to the neurons of the occipital region of the cerebral cortex.
The peripheral part of this system is represented by a complex organ - the eye, containing photoreceptors and the bodies of the first and second neurons. The fibers of the second neurons make up the optic nerve, through which excitation is transmitted to the third neurons in the diencephalon, and then to the neurons of the occipital region of the cerebral cortex.
VISUAL PURPLE (Rhodopsin) - contains inside the rods the pigment of the retina, which includes retinaldehyde - vitamin A and protein. The presence of rhodopsin in the retina is necessary for normal vision in dim light. Under the influence of light, this pigment changes, which leads to the appearance of a nerve impulse.
CATARACT - clouding of the lens of the eye. Normally, the lens is completely transparent. However, with age, a violation of its nutrition can cause persistent blurring and blurred vision. The development of the disease is facilitated by metabolic disorders (in particular, diabetes mellitus), toxic or traumatic effects on the eye, diseases of the inner membranes of the eye (inflammation, a high degree of myopia, glaucoma, etc. ).
).
The disease can be congenital or acquired. Congenital cataracts usually do not progress. The rate of progression of acquired cataract varies from person to person and largely depends on the general condition of the body and eye tissues. Traumatic cataracts can progress very quickly.
In the initial stage of the disease, there is a flickering of dark stripes, strokes, spots before the eyes. When looking at light sources (a candle, a lantern, etc.), the image often splits in two. Gradually, clouding of the lens becomes pronounced. With a developed cataract, the pupil area is grayish, grayish-white or milky-white. At the same time, visual acuity decreases, with a complete (“ripe”) cataract, the patient feels only the presence or absence of light.
KERATITIS - inflammation of the cornea - the transparent anterior shell of the eyeball. The most important in the occurrence of keratitis is an infection, the pathogens of which penetrate the cornea from the outside, or from the blood and lymph in various infectious diseases. The main signs of keratitis are photophobia, lacrimation, spasm of the eyelids, reddening of the vessels of the conjunctiva, a feeling of the presence of a foreign body in the eye.
The main signs of keratitis are photophobia, lacrimation, spasm of the eyelids, reddening of the vessels of the conjunctiva, a feeling of the presence of a foreign body in the eye.
CONJUCTIVA — a thin mucous membrane that covers the front of the eyeball and the inner surface of the eyelids. The conjunctiva that lines the inner surface of the eyelids contains more blood vessels than the conjunctiva that covers the eyeball, the latter being transparent.
CONJUNCTIVITIS - inflammation of the conjunctiva.
strabismus — deviation of the visual axis of one of the eyes from the common point of fixation. There are paralytic strabismus caused by damage to the nerves that innervate the muscles of the eye, and concomitant strabismus, the causes of which may be diseases of the central nervous system, general infections and intoxications, mental trauma, ametropia, a sharp decrease in vision or blindness in one eye. As a result of the action of these factors, various departments and sensory-motor connections of the visual analyzer are affected, on which binocular vision depends, which leads to its disorder or prevents its formation.
Concomitant strabismus usually develops in early childhood. The visual axis of one eye is deviated from the object fixed by the other eye. Doubling, as a rule, does not happen. Binocular vision is absent. A functional scotoma appears in the field of view of the squinting eye. Both eyes (squinting and fixing) move approximately in the same volume. These movements in all directions are not limited or slightly limited. The visual acuity of the constantly squinting eye is significantly reduced. Paralytic strabismus differs from concomitant diplopia, the absence or sharp limitation of eye movements in the direction of the paralyzed muscle.
MACULA — part of the retina of a straight-looking eye, on which light rays focused by the cornea and lens of the eye meet. The macula is a very small area in the center of the retina. This small area of the retina is responsible for the central vision necessary for reading and doing other light work.
MYOPIA (nearsightedness) is a refractive error in which parallel light rays focus in front of the retina rather than on it. In this case, a person sees distant objects indistinctly, blurry, since he cannot achieve a clearer image of them with the help of accommodation. Myopia is corrected by wearing special glasses with concave spectacle lenses; at present, it can also be eliminated surgically.
In this case, a person sees distant objects indistinctly, blurry, since he cannot achieve a clearer image of them with the help of accommodation. Myopia is corrected by wearing special glasses with concave spectacle lenses; at present, it can also be eliminated surgically.
VISUAL ACUITY - the ability to distinguish individual objects. It is measured by the minimum angle at which two points are perceived as separate - approximately 0.5 arcminutes. In the center of the retina, the cones are smaller and much denser, so the ability for spatial discrimination is 4-5 times higher here than at the periphery of the retina. Therefore, central vision has a higher visual acuity than peripheral vision. For a detailed examination of objects, a person by turning his head and eyes moves their image to the center of the retina. Visual acuity depends not only on the density of the receptors, but also on the clarity of the image on the retina - on the refractive properties of the eye, on the degree of accommodation, on the size of the pupil. In the aquatic environment, the refractive power of the cornea decreases, since its refractive index is close to that of water. As a result, visual acuity decreases underwater.
In the aquatic environment, the refractive power of the cornea decreases, since its refractive index is close to that of water. As a result, visual acuity decreases underwater.
OPHTHALMOSCOPY - examination of the fundus.
FIELD OF VISION - the field of view is the part of space visible when the eye is stationary. For black and white signals, the field of view is usually limited by the structure of the bones of the skull and the position in the eye sockets of the eyeballs. For colored stimuli, the field of view is smaller, since the cones that perceive them are located in the central part of the retina. When tired, it decreases.
PRESBYOPIA - a decrease in the ability of the eye to focus on close objects with age.
Symptoms: slowly progressive deterioration of near vision. With emmetropia, presbyopia occurs at the age of 40-45 years, with myopia - later, with hypermetropia - earlier, often accompanied by a deterioration in distance vision. Looking at small objects is facilitated by moving them away from the eye. The diagnosis is based on taking into account the nature of visual disorders, the age of the patient and data on the refraction of the eyes.
Looking at small objects is facilitated by moving them away from the eye. The diagnosis is based on taking into account the nature of visual disorders, the age of the patient and data on the refraction of the eyes.
IRIS (iris) - the iris is a kind of rounded screen, consisting of thin, concentrically and radially located muscles, with contraction and relaxation of which the shape of the pupil changes. The color of the eyes is determined precisely by the iris and depends on the number of pigment cells in it - those with blue eyes have few pigment cells, and those with brown eyes have many.
The cornea is a transparent tissue that covers the front of the eye, much like the glass on a watch covers the dial. In addition to its transparency, the cornea is distinguished by the absence of blood vessels in it and high sensitivity (which is especially important for those who wear contact lenses).
RHODOPSIN (visual purple) is a retinal pigment contained inside the rods, which includes retinaldehyde - vitamin A and protein. The presence of rhodopsin in the retina is necessary for normal vision in dim light. Under the influence of light, this pigment changes, which leads to the appearance of a nerve impulse.
The presence of rhodopsin in the retina is necessary for normal vision in dim light. Under the influence of light, this pigment changes, which leads to the appearance of a nerve impulse.
RETINA is a paper-thin tissue that covers the inner back of the eyeball. It consists of special light-sensitive cells (receptors), several layers of various nerve cells and a large number of blood vessels.
SCLERA - the outer layer of the eye.
TEAR FLUID - the outer surface of the cornea is permanently covered with a thin layer of tear fluid, which improves the optical properties of the eye surface. This fluid is produced by the lacrimal glands, and thanks to the regular movements of the eyelids, it is evenly distributed over the cornea. The tear fluid protects the cornea and conjunctiva from drying out. Its composition is close to that of blood plasma ultrafiltrate. The tear fluid contains substances that have a bactericidal effect, and thus protects the eye from infections.
Vitreous is a transparent jelly-like substance that occupies the posterior two-thirds of the eye. A small space between the cornea and the lens is filled with a transparent liquid medium - intraocular fluid.
A small space between the cornea and the lens is filled with a transparent liquid medium - intraocular fluid.
UVEITIS — inflammation of the choroid (uveal tract). This disease is a common cause of low vision and blindness (about 25%). If you have uveitis, you should immediately consult an ophthalmologist. The main symptoms of the disease are "fog" before the eyes, blurred vision (even complete blindness is possible), redness of the eyes, photophobia and lacrimation.
PHOTORECEPTORS are highly specialized cells that convert light stimuli into nervous excitation. Photoreception begins in the outer segments, where visual pigment molecules are located on the discs (in rods - rhodopsin, in cones - iodopsin). Under the action of light, a series of very rapid transformations and discoloration of the visual pigment occurs. Rods and cones differ in their functions. The rods are more sensitive than the cones and are organs of twilight vision. They perceive a black and white (colorless) image. Cones are organs of daytime vision. They provide color vision. There are 3 types of cones in humans: predominantly red, green, and blue-violet. Their different color sensitivity is determined by differences in visual pigment. Combinations of excitations of these receivers of different colors give sensations of the whole gamut of color shades. Uniform excitation of all 3 types of cones causes a sensation of white color.
Cones are organs of daytime vision. They provide color vision. There are 3 types of cones in humans: predominantly red, green, and blue-violet. Their different color sensitivity is determined by differences in visual pigment. Combinations of excitations of these receivers of different colors give sensations of the whole gamut of color shades. Uniform excitation of all 3 types of cones causes a sensation of white color.
THE LENS OF THE EYE is a transparent, elastic and semi-rigid solid body that can change its shape so that objects at different distances from the eye are in focus. In its place, it is held by thin fixing fibers - the ciliary girdle, or the ligament of zon, which is attached to the ciliary body. To bring a close object into focus, the muscle of the ciliary body contracts, thereby weakening the pressure of this ligament on the lens and allowing it to expand, which, in turn, increases the optical power of this system. With age, the elasticity of the lens decreases somewhat, and it can no longer expand to the required degree. This phenomenon is known as presbyopia (senile farsightedness), and because of it, people after forty years of age often require reading glasses.
This phenomenon is known as presbyopia (senile farsightedness), and because of it, people after forty years of age often require reading glasses.
BARLEY - acute limited purulent inflammation of the edge of the eyelid, the cause of which is infection of the hair follicle or sebaceous gland.
Symptoms: limited sharply painful swelling along the edge of the eyelid. After 2-4 days, a yellowish head is formed on its top, upon opening of which pus and particles of necrotic tissue are released. Sometimes, especially when squeezing out pus, barley can cause phlegmon of the orbit (diffuse purulent inflammation of fatty tissue), thrombosis of the cavernous sinus, meningitis.
How to read other people's thoughts? Look into the eyes
- Mo Kostandi
- BBC Future
Sign up for our 'Context' newsletter to help you sort things out.
Image copyright Thinkstock
Pay attention to eye movements and you can figure out what's going on in the other person's head, says BBC Future .
They say that the eyes are the mirror of the soul. They give away deep emotions that we might not want to advertise. Although modern science denies the existence of a soul in a person, there is a grain of truth in this old saying - even according to scientists. It turns out that the eyes not only reflect what is happening in our brain, but can also influence how we remember information and make decisions.
(Similar articles from the "Journal" section)
Our eyes are constantly moving. Some of these movements we consciously control, but many of them occur subconsciously. For example, while reading, their rapid spasmodic movement occurs: our gaze moves rapidly, stopping at each of the words. Similarly, the eyes move when we enter a room - this time the movement is wider, allowing us to look around. While walking, our eyes make small involuntary movements in order to compensate for the movement of the head in this way and stabilize our picture of the world. And, of course, the rapid movement of the eyeballs is characteristic of the so-called phase of REM sleep.
While walking, our eyes make small involuntary movements in order to compensate for the movement of the head in this way and stabilize our picture of the world. And, of course, the rapid movement of the eyeballs is characteristic of the so-called phase of REM sleep.
Also, eye movements can sometimes tell others what we are thinking.
Image copyright Thinkstock
Image captionDilated pupils indicate decision uncertainty
According to a study published last year, pupil dilation is related to how confident we are in our decision making. If a person does not feel full determination, he is in a state of emotional arousal, as a result of which his pupils dilate.
By sensing this change, we can in some cases predict what the decision maker will say. As one group of researchers found, if you observe the degree of pupil dilation, you can guess when a cautious person, not used to agreeing to the options offered to him, nevertheless decides to say yes.
By paying attention to eye movements, we can even predict, with some degree of probability, what number a person has in mind. Tobias Lötscher and his colleagues at the University of Zurich recruited 12 volunteers, asked them to read aloud a list of 40 numbers, and tracked how their eyes moved as they did so.
Scientists have found an exact correspondence between the direction of movement of the eyes of the subjects, the angle of rotation of the pupils and whether the number that the subjects were going to pronounce was more or less than the previous one. In addition, it was possible to predict how much more or less this number was.
Image copyright Thinkstock
Image captionWhat number did I think?
Image copyright Thinkstock
Image caption...big because I'm looking up and to the right
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of Story Podcast
Each subject looked up and to the right before reading a larger number; if the number was less, then the person looked down and to the left. The more the pupils turned to the side, the greater was the difference between the numbers.
It turns out that we somehow connect the abstract images of numbers in our brain with movement in space. However, this study did not make it clearer what happens first: either we think of a certain number and our eyes move accordingly, or the position of the eyes affects our mental activity.
In 2013, Swedish scientists published data showing that the latter is more likely to be true: it seems that eye movements help to retrieve the necessary information from memory.
They recruited more than two dozen students to participate in an experiment and asked them to carefully examine a series of objects that were shown to them in one corner of a computer screen. The subjects were then asked to listen to a series of statements about some of the objects they saw (for example, "The car was turned to the left") and indicate as quickly as possible whether each of the statements was true or false. Some participants were allowed to look where they wanted to, while others were asked to keep their eyes on the cross in the center of the screen, or in the corner where they saw the item they were looking for.
The subjects were then asked to listen to a series of statements about some of the objects they saw (for example, "The car was turned to the left") and indicate as quickly as possible whether each of the statements was true or false. Some participants were allowed to look where they wanted to, while others were asked to keep their eyes on the cross in the center of the screen, or in the corner where they saw the item they were looking for.
Image copyright, Thinkstock
Image caption,Certain eye movements aid recall
The researchers found that subjects whose eyes moved spontaneously during the experiment performed significantly better than those who looked at the cross. Interestingly, those who looked at the corner where they had previously seen the object did a better job than those who looked at the other corner. The greater the overlap between participants' eye movements during encoding and retrieval of that information, the easier it was for them to describe the items. Perhaps the fact is that eye movements help us remember the relative position of objects in space at the time of encoding (that is, information processing).
Perhaps the fact is that eye movements help us remember the relative position of objects in space at the time of encoding (that is, information processing).
These movements may occur subconsciously. "When a person is confronted with a familiar place or situation, their eyes often turn to information they have already seen, even if they don't consciously remember what they saw before," says Roger Johansson, a psychologist at Lund University who led the study.
Watching eye movements can also influence the decisions a person makes. As a recent study has shown, gaze tracking can be used to influence our moral choice of whether we like it or not.
Researchers asked participants difficult moral questions (eg, "Can murder be justified?") and then showed them response options ("sometimes" or "never" on a computer screen). By tracking the subject's eye movements and removing the answer options from the screen after the participant looked at one of them for a certain time, the scientists found that as a result, he leaned towards this option.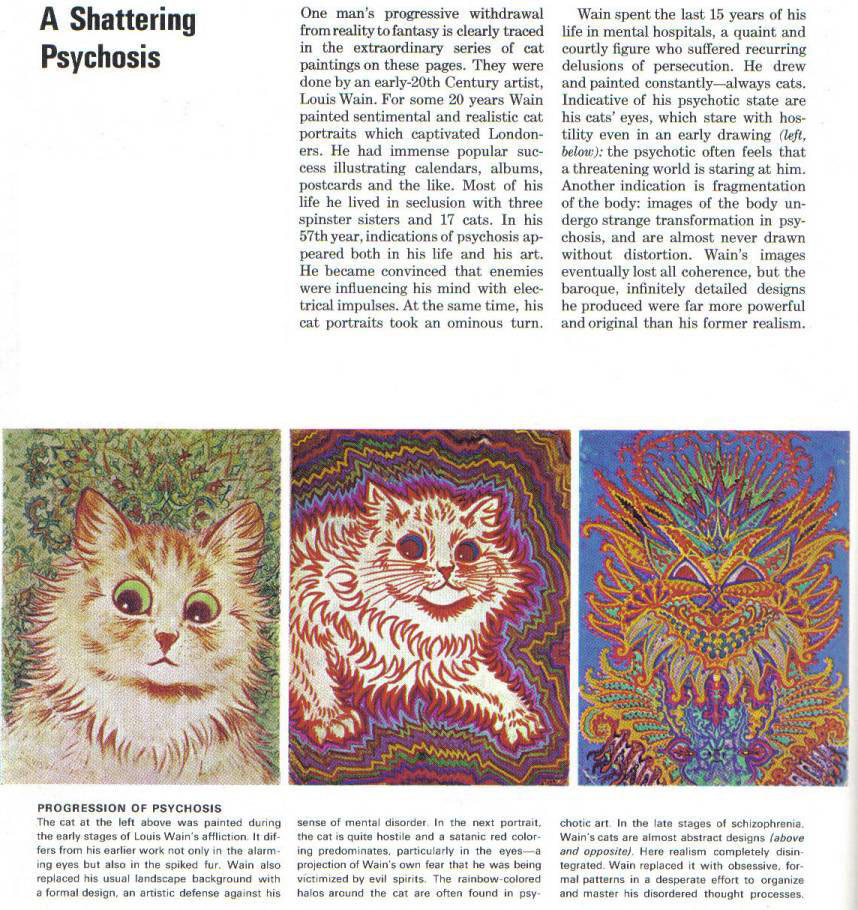
"We didn't give them any other information," says neuroscientist Daniel Richardson of University College London, lead author of the study. simply by controlling the moment of decision making.
Image copyright Thinkstock
Image captionYou don't need to take an X-ray to get inside someone's head
As Richardson points out, successful salespeople probably have some idea of this and use similar tactics to better convince customers . "We think persuasive people are good talkers, but maybe they also follow the decision-making process," he says. discount or present the goods from a new side.
There are many applications for smartphones and other mobile devices that track eye movement. Can they be used to remotely influence the decision-making process of device users? "Apps like this can push you to make certain choices while shopping online, offering you, for example, free shipping the moment you look at a particular product," the neuroscientist suggests.